Welcome to Peninsula Health Mental Health Undergraduate Nursing







- Slides: 48
Welcome to Peninsula Health Mental Health Undergraduate Nursing Students 2020

Acknowledgement of Country I/we would like to acknowledge Aboriginal and Torres Strait Islander people as the First Peoples and Traditional Owners and Custodians of this Land. I/we pay respects to the ancestors of this country, Elders, Knowledge Holders and Leaders, past, present and emerging. We extend that respect to all Aboriginal and Torres Strait Islander people. We at Peninsula Health acknowledge the local Traditional Owners the Bunurong and Boon Wurrung and people of the Kulin Nation.
Placement at Peninsula Health
Vision and Purpose Peninsula Health is the major health care provider serving the metropolitan and rural areas on Victoria’s Mornington Peninsula OUR VISION: To provide exceptional health and community care OUR PURPOSE: We work together to build a healthy community ‘The Health Service works with community and service partners to promote health and healthy lifestyles and to plan for the future needs of the community

Values Be the Best We strive for excellence in all that we do Be a Role Model Together, our behaviors build our culture Be Open and Honest We are transparent, accountable and innovative Be Compassionate and Respectful We embrace diversity, advocate and care for consumers, support our peers and grow our teams in a safe, kind and meaningful way Be Collaborative Our impact is better and stronger when we are inclusive and engaging of a broad network of people

Education • In addition to providing quality, accessible health care services Peninsula Health is a teaching hospital and has a history of contributing to medical research • Undergraduate o Nursing o Medical o Allied Health • Nursing o Postgraduate o Staff Development • Post Registration • Variety of educational opportunities - Research opportunities across all disciplines
Expectations While you are on placement at Peninsula Health and a valued member of our team, our EXPECTATIONS are: All Compulsory Documents are current You practice within your Scope of Practice You adhere to Professional Code of Conduct You adhere to Peninsula Health’s Policies & Procedures and Values You are aware of Emergency Procedures You are aware of OH&S requirements You maintain your own personal safety and make this a priority
Compulsory Documents • Ensure you have submitted the following documents prior to placement: – Police Check* – Working With Children Check* – Current Immunisations – Aged care check (if applicable) * Must be carried with you at all times
Scope of Practice • You must not perform any clinical practice/s unless you have successfully completed theory and educational preparation specific to those practices and have been instructed by your education provider that they are within your scope of practice for your placement. • All procedures, medication delivery, & interaction with medical equipment such as IV pumps needs to be under direct supervision of your buddy nurse. • You must report any alteration in a patient’s physical or mental condition, any adverse event or change in physiological observations of a patient; to the senior nurse immediately
Policies and Procedures • Ensure your practice adheres to Peninsula Health’s Policies and Procedures at all times • These can be accessed on Peninsula Health Intranet • Clinical Practice Guidelines are also accessible
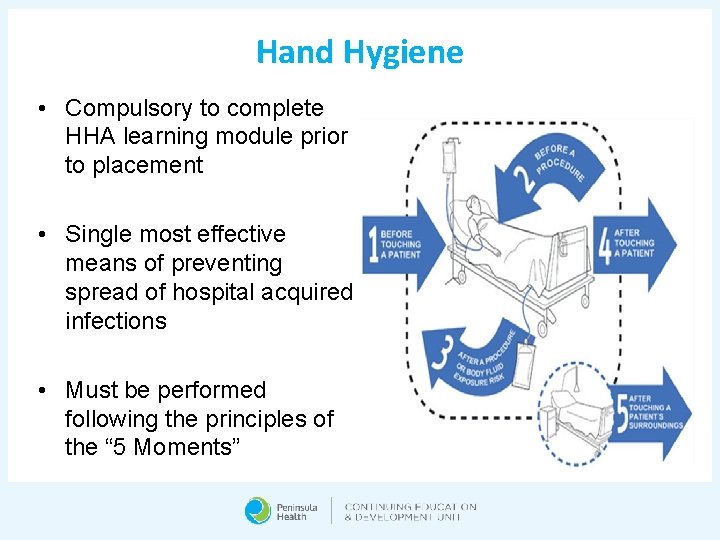
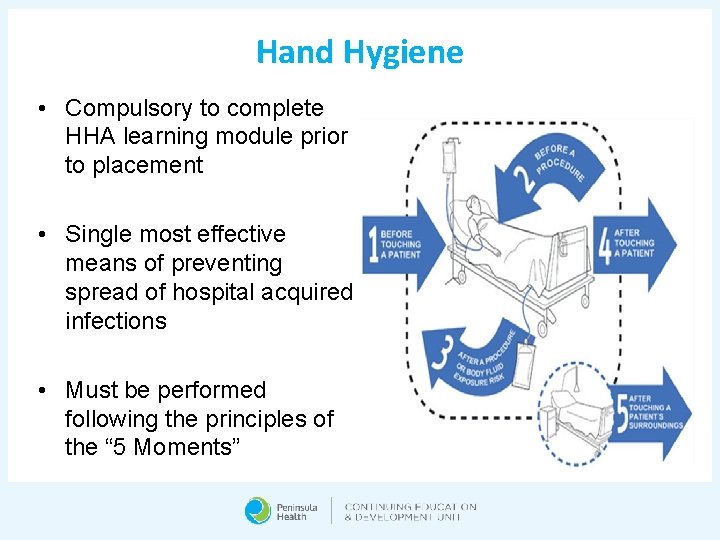
Hand Hygiene • Compulsory to complete HHA learning module prior to placement • Single most effective means of preventing spread of hospital acquired infections • Must be performed following the principles of the “ 5 Moments”
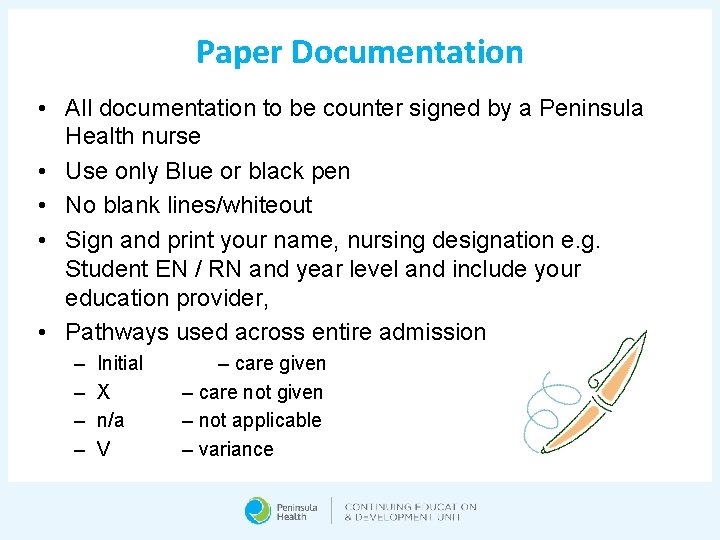
Paper Documentation • All documentation to be counter signed by a Peninsula Health nurse • Use only Blue or black pen • No blank lines/whiteout • Sign and print your name, nursing designation e. g. Student EN / RN and year level and include your education provider, • Pathways used across entire admission – – Initial X n/a V – care given – care not given – not applicable – variance
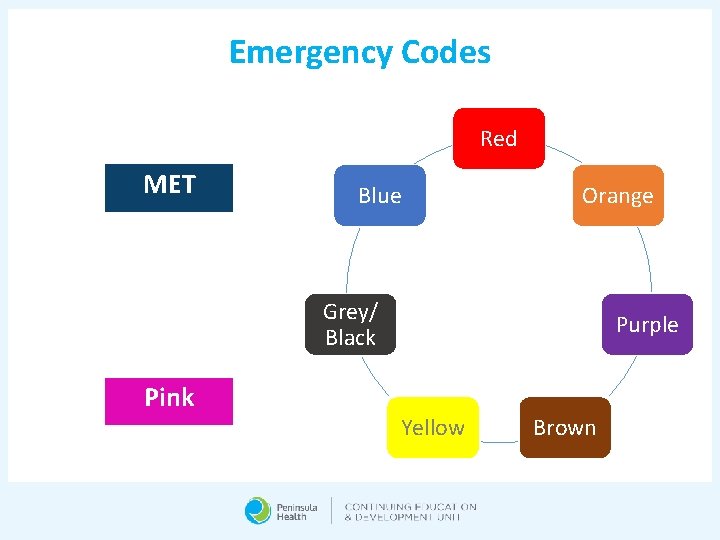
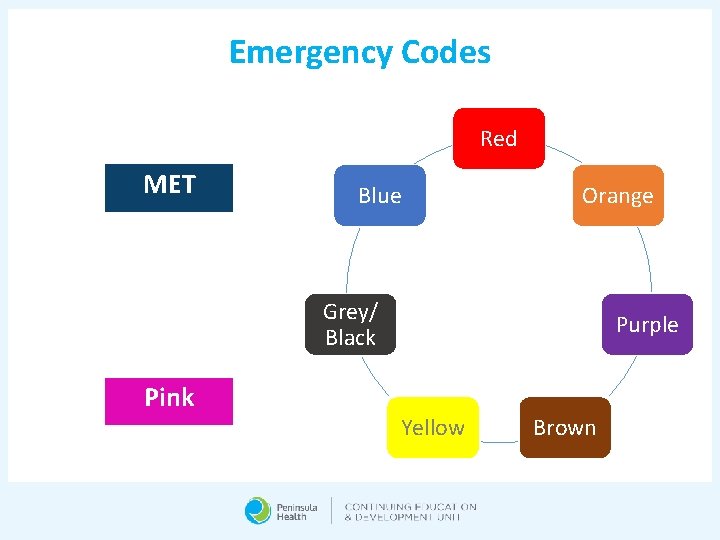
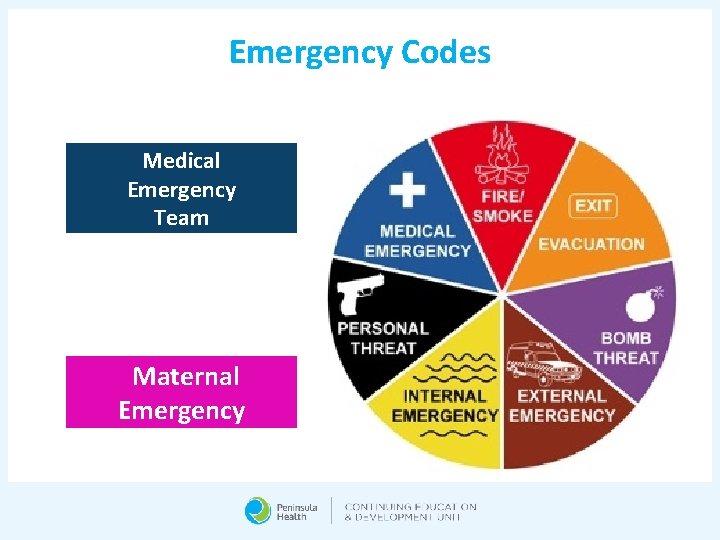
Emergency Codes Red MET Blue Orange Grey/ Black Pink Purple Yellow Brown
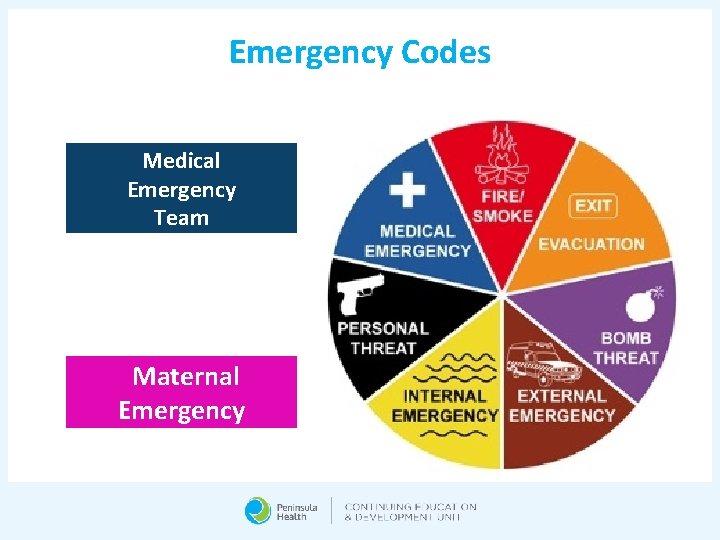
Emergency Codes Medical Emergency Team Maternal Emergency
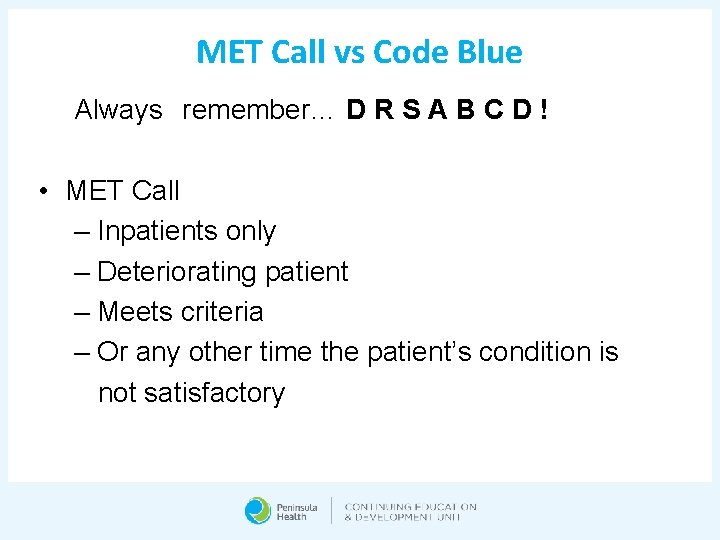
MET Call vs Code Blue Always remember… D R S A B C D ! • MET Call – Inpatients only – Deteriorating patient – Meets criteria – Or any other time the patient’s condition is not satisfactory
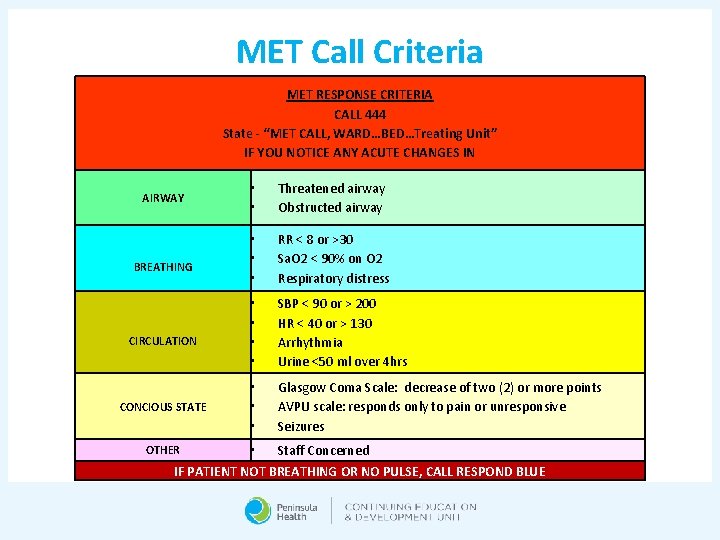
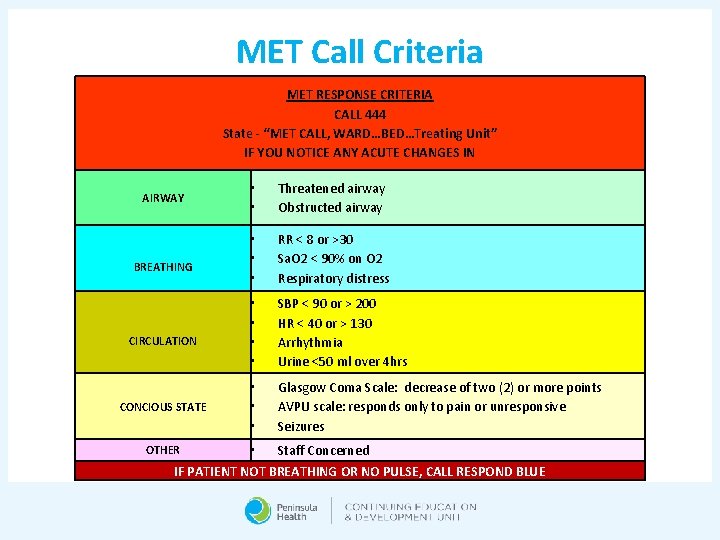
MET Call Criteria MET RESPONSE CRITERIA CALL 444 State - “MET CALL, WARD…BED…Treating Unit” IF YOU NOTICE ANY ACUTE CHANGES IN AIRWAY • • Threatened airway Obstructed airway BREATHING • • • RR < 8 or >30 Sa. O 2 < 90% on O 2 Respiratory distress CIRCULATION • • SBP < 90 or > 200 HR < 40 or > 130 Arrhythmia Urine <50 ml over 4 hrs CONCIOUS STATE • • • Glasgow Coma Scale: decrease of two (2) or more points AVPU scale: responds only to pain or unresponsive Seizures • Staff Concerned IF PATIENT NOT BREATHING OR NO PULSE, CALL RESPOND BLUE OTHER
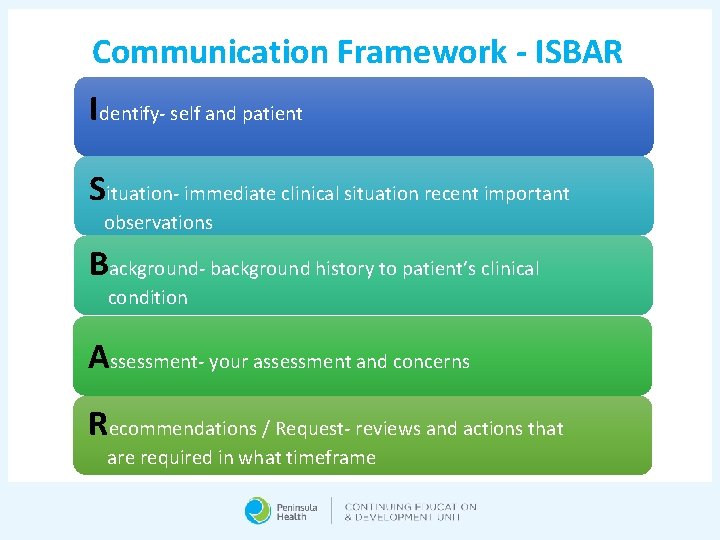
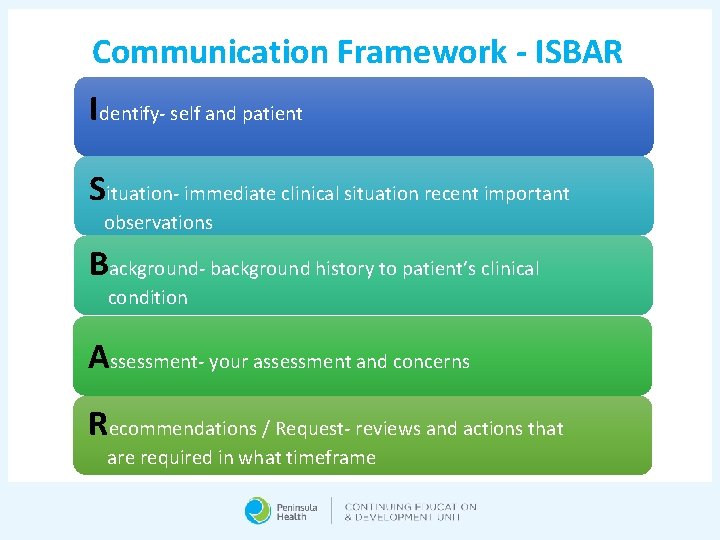
Communication Framework - ISBAR Identify- self and patient Situation- immediate clinical situation recent important observations Background- background history to patient’s clinical condition Assessment- your assessment and concerns Recommendations / Request- reviews and actions that are required in what timeframe
Rosters • There is a maximum number of students allowed per shift on Peninsula Health wards. This cannot be exceeded in any circumstances. • All requested shift changes MUST be addressed with the Clinical Facilitator, then the ward before changes can be made • Students are not permitted to change wards midplacement and must remain in their allocated area for the entirety of the placement • Name in allocation book-at the beginning of each shift so the in charge can allocate you to a buddy nurse • Breaks- go at the same time as your buddy nurse
Sick Calls • Students who are sick on the day of placement must not attend. • They should notify the clinical area they are rostered to, asking to speak to the nurse in charge, stating their name, education provider and shift they were allocated to • Students must also notify their clinical facilitator and their education provider. • There is not generally scope for them to make-up any sick or missed placement days up at Peninsula Health. • Students are not permitted to work any additional hours per day to make-up for missed days.
Incidents - Who To Call, What To Do! • You must immediately inform: - your buddy/preceptor - your Clinical Facilitator (they are to call CEDU immediately) - the nurse In-Charge of the ward • A Peninsula Health incident report must be completed by your buddy/preceptor • If required fill out any incident forms for education provider • All necessary follow-up care is to be provided to the student, same process followed as for staff.

Culture & Diversity • Peninsula Health embraces cultural diversity and the ongoing knowledge journey to embrace all diverse groups to be a culturally inclusive organisation • Developing cultural competence results in an ability to understand, communicate with, and effectively interact with people across cultures
Workplace Behaviour • All students are expected to adhere to the Peninsula Health values • Inappropriate workplace behaviours include: • • • Bullying Poor attendance Criminal conduct Sexual harassment Workplace violence Discrimination Serious misconduct Risking patient/resident safety Failure to perform to required standard
Patient Confidentiality • A patient/client/resident’s right to privacy must be respected at all times • This includes verbal, written, social media, filmed or photographic records and documents of any kind
No Smoking • All peninsula Health sites are no smoking areas • This includes the hospital grounds, community clinics, and car parks.
Mental Health Service
Vision and Philosophy • Peninsula Health Mental Health Service will acknowledge and appreciate the lived experience of our clients and carers, and support their individual resourcefulness, strengths and abilities through the provision of excellent specialised mental health care
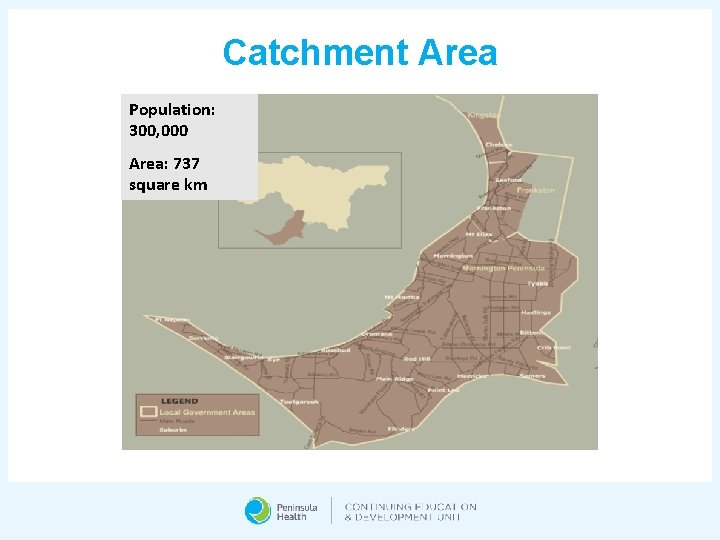
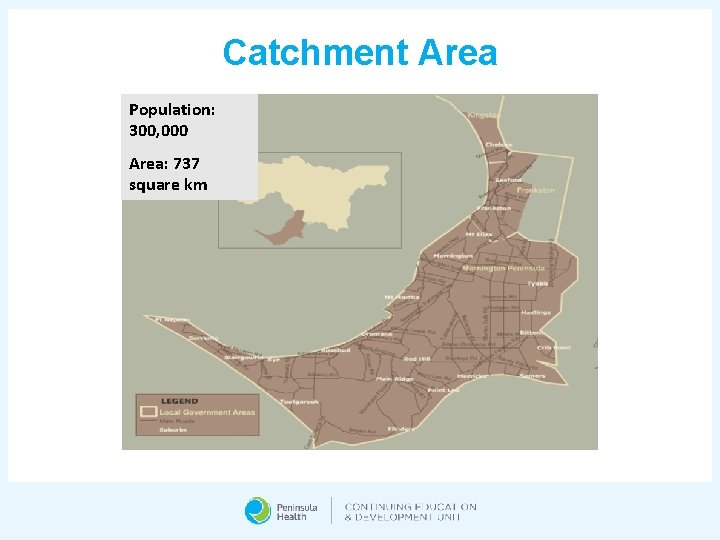
Catchment Area Population: 300, 000 Area: 737 square km
Statistics • An estimated 45% of people will experience mental illness in their lifetime • 3% of people will experience severe mental illness each year • In 2015 -2016, PHMHS supported: • Approximately 3, 000 clients • Across 5, 000 episodes • Of which, one third are new to the service
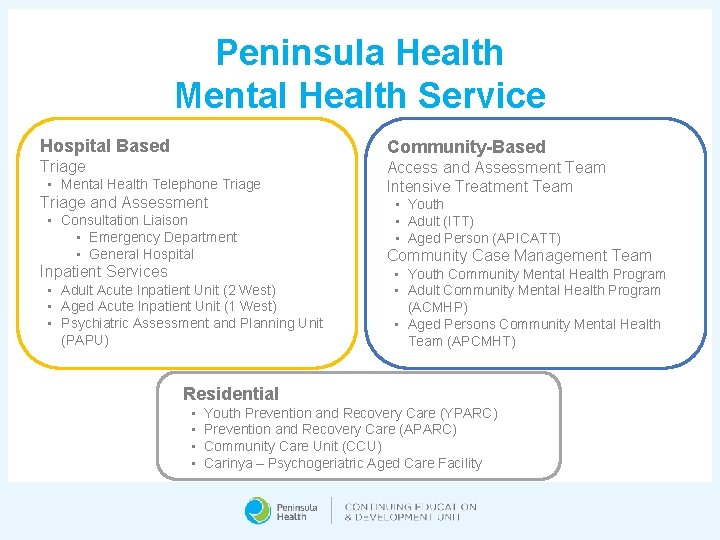
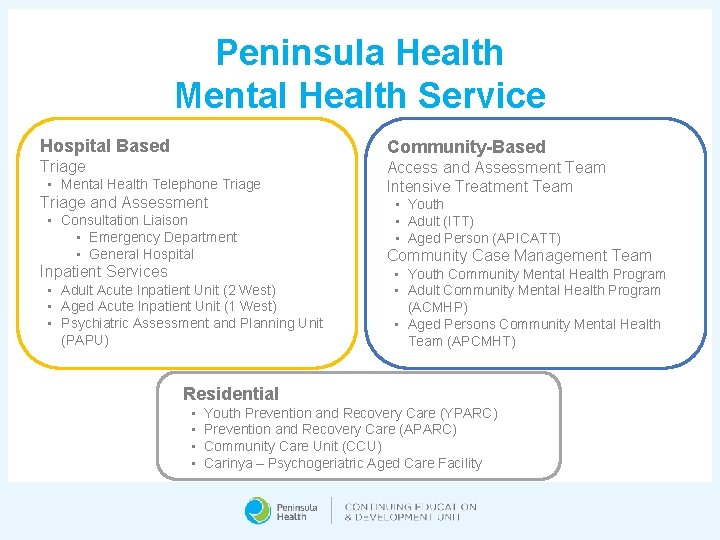
Peninsula Health Mental Health Service Hospital Based Community-Based Triage Access and Assessment Team Intensive Treatment Team • Mental Health Telephone Triage and Assessment • Consultation Liaison • Emergency Department • General Hospital Inpatient Services • Adult Acute Inpatient Unit (2 West) • Aged Acute Inpatient Unit (1 West) • Psychiatric Assessment and Planning Unit (PAPU) • Youth • Adult (ITT) • Aged Person (APICATT) Community Case Management Team • Youth Community Mental Health Program • Adult Community Mental Health Program (ACMHP) • Aged Persons Community Mental Health Team (APCMHT) Residential • • Youth Prevention and Recovery Care (YPARC) Prevention and Recovery Care (APARC) Community Care Unit (CCU) Carinya – Psychogeriatric Aged Care Facility
Mental Health Telephone Triage • This service is generally the first point of contact for people seeking a specialist mental health response – for themselves, their carer/family or friend • It is a 24 hour, 7 days a week service providing comprehensive and timely telephone screening, triage and a review • It takes calls for referrals of people of all ages
Consultation Liaison ED & GH • Assessment, treatment and planning service for patients with mental health and physical health needs who have presented or are admitted to medical wards at Frankston Hospital or the Emergency Department • It is located at the Frankston Hospital and is available 24 hours, 7 days a week for people of all ages • Mental Health CL services are provided to the General Medical/Surgical Wards, Paediatric, Intensive Care Unit, Coronary Care Unit and Women’s Health Unit during business hours with after-hours on call service
Adult Acute Inpatient Unit (2 West) • 29 bed Mental Health inpatient unit that provides tailored to people aged 18 -65 • Multidisciplinary team provide mental health assessment, treatment, recovery and discharge planning during an acute phase of a person’s mental illness • Therapeutic activity programs are run, which include assisting with daily living skills and group activities • The Acute Management Area (AMA) is a low stimulus environment for clients who may require a more intensive treatment during their admission
Aged Acute Inpatient Unit (1 West) • 15 bed Mental Health inpatient unit for clients over the age of 65 years old • Inpatient care allows the multi-disciplinary team to make a detailed assessment of people’s needs and provide assistance or treatment • Care may be addressing physical, psychological, social needs and residential needs
Psychiatric Assessment & Planning Unit (PAPU) • 6 bed, short-stay unit for the provision of accelerated access to specialist psychiatric assessment and short-term treatment • Ideally the length of stay is less than 72 hours • The aim is to ensure clients receive timely access to short-term assessment and treatment • Minimises the need for acute inpatient stay by ensuring clients are well supported in the community
Access & Assessment Team (AAT) • Initial comprehensive assessment service based in the community • Conduct Face-to-face holistic assessments in the Frankston or Rosebud community clinics and/or the client’s home • Provide referral and integrated planning strategies to both PHMHS service programs and external service providers which includes the needs of the carer/family supporting the client • Also provide brief time limited intervention treatment services with a particular focus on suicide prevention
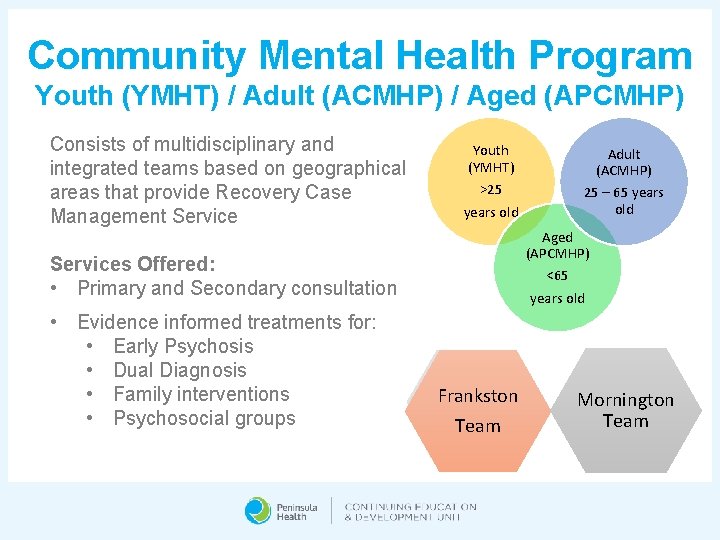
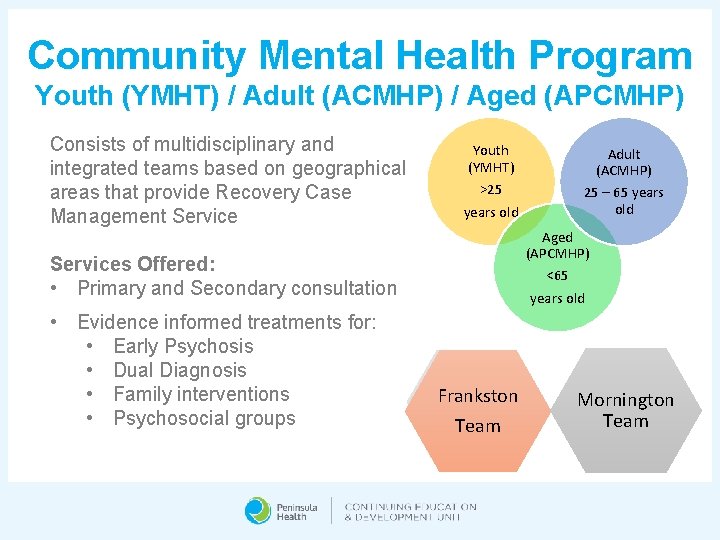
Community Mental Health Program Youth (YMHT) / Adult (ACMHP) / Aged (APCMHP) Consists of multidisciplinary and integrated teams based on geographical areas that provide Recovery Case Management Service Youth (YMHT) >25 years old Aged (APCMHP) <65 Services Offered: • Primary and Secondary consultation • Evidence informed treatments for: • Early Psychosis • Dual Diagnosis • Family interventions • Psychosocial groups Adult (ACMHP) 25 – 65 years old Frankston Team Mornington Team
Community Mental Health Service The service ensures access to treatment and support based on their needs by: • Providing client centred care and information about treatment and encouraging healthy lifestyles • Effective medication management • Providing support with any drug and alcohol issues • Developing relapse prevention plans with clients/carers and families • Supported to have access to other services and specialists in assisting them with addressing AOD issues, resuming interests, social activities and employment or study options
Prevention and Recovery Centre Youth (YPARC) & Adult (APARC) • YPARC - 10 bed facility for people aged 16 – 25 years • APARC - 10 bed facility for people aged 25 – 65 year • The service is a partnership between PHMHS, Mind Australia and Peninsula Support Services • Eligibility includes: • Reside in the PHMHS catchment area • Have a significant mental health issue • Able to receive treatment and support safely and effectively within a community residential setting • Not be at significant risk of harming to self or others • Agree to not use illicit substances or alcohol • Agree to participate in programs voluntarily (including those on a Community Treatment Order)
Community Care Unit (CCU) • Located in a residential street in Frankston, containing 9 purpose built residence in a cluster arrangement • This residential service provides short- to medium-term residential psychosocial rehabilitation for up to 20 clients • Referrals are for current clients of the PHMHS • Staffed 24 hours a day with a multidisciplinary team of health professionals including nurses, occupational therapists, psychologists and doctors

Multidisciplinary Team • Medical Staff • Nursing Staff • Occupational Therapists • Social Workers • Psychologists • Pharmacist • Peer Workers • Students!
Supporting Mental Health Services • Consumer/Carer Consultant • Forensic Specialist • Frankston and Mornington Drug and Alcohol Service (Fa. MDAS) • Hospital Outreach Post-suicidal Engagement (HOPE) • Families Where a Parent has a Mental Illness (Fa. PMI) • Clozapine Co-ordinator/GP Shared Care
Role as a Mental Health Nurse • Establish therapeutic relationships • Assessments • Mental State Examination • Risk Assessment • Physical Assessment • Mental Health Act • Education • Advocacy • Provide treatment
Common Treatments: • Medication • Antipsychotic • Mood Stabiliser • Antidepressant • Electroconvulsive Therapy (ECT) • Cognitive Behavioural Therapy (CBT) • Dialectical Behavioural Therapy (DBT)
Education • The client and family/carers should receive as much education regarding their mental illness, including diagnosis, signs and symptoms, treatment, medications • Psychoeducation aids the individual to enhance their understanding, assisting managing their mental illness in the future – including relapse detection
Therapeutic Relationship • Significant aspect of mental health care is demonstrating respect and positive regard of the client • The expectation is to not harm or exploit the vulnerability of the client Understand yourself Take care of yourself Understand your patient Form an alliance/develop trust Reflect and think…. . Don’t react Treat whatever is treatable Seek support
Breaching of Boundaries • Breaching of professional boundaries is going outside the limits of therapeutic relationship • These breaches may occur when establishing a social, economic or personal relationship with the client and may include, but are not limited to, physical, verbal or psychological abuse

Keeping Healthy • It is important to: • Be aware that some situations, conversations or clients may impact your mental health • Recognise you may feel anxious or overwhelmed • Look after yourself • Approach your preceptor or your clinical facilitator for support Kenzo, Peninsula Health Director of Happiness

Clinical Facilitator Grace Mosely Mobile 0409 426 606 Monday – Friday 08: 00 – 16: 30
 Chapter 20 mental health and mental illness
Chapter 20 mental health and mental illness Mental health jeopardy game
Mental health jeopardy game Psychiatric nursing definition
Psychiatric nursing definition 3 part nursing diagnosis examples
3 part nursing diagnosis examples Conclusion of community mental health nursing
Conclusion of community mental health nursing Papu frankston
Papu frankston Undergraduate meaninh
Undergraduate meaninh Portland state university undergraduate tuition and fees
Portland state university undergraduate tuition and fees Uci ics building
Uci ics building Undergraduate graduate postgraduate
Undergraduate graduate postgraduate Definition of undergraduate student
Definition of undergraduate student Nyu undergraduate research conference
Nyu undergraduate research conference Difference between postgraduate and undergraduate
Difference between postgraduate and undergraduate Difference between postgraduate and undergraduate
Difference between postgraduate and undergraduate Cornell university neuroscience
Cornell university neuroscience Los angeles city college
Los angeles city college Acadia university undergraduate programs
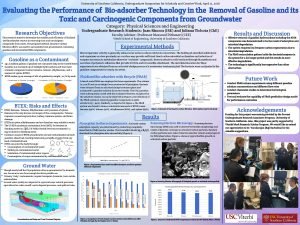
Acadia university undergraduate programs Usc undergraduate symposium
Usc undergraduate symposium Dean of undergraduate studies fsu
Dean of undergraduate studies fsu Csub orientation
Csub orientation What is an undergraduate degree
What is an undergraduate degree Acu undergraduate research festival
Acu undergraduate research festival Temple university undergraduate bulletin
Temple university undergraduate bulletin Acu undergraduate
Acu undergraduate Neuroscience major usc
Neuroscience major usc King's undergraduate research fellowship
King's undergraduate research fellowship Unb undergraduate calendar
Unb undergraduate calendar Ncsu undergraduate research symposium
Ncsu undergraduate research symposium Welcome welcome this is our christmas story
Welcome welcome this is our christmas story Nursing diagnosis mental retardation
Nursing diagnosis mental retardation Nursing diagnosis mental retardation
Nursing diagnosis mental retardation Is wales a peninsula
Is wales a peninsula Scandinavian peninsula
Scandinavian peninsula Yucatan peninsula south america map
Yucatan peninsula south america map Western lower peninsula michigan
Western lower peninsula michigan Mountainous peninsula
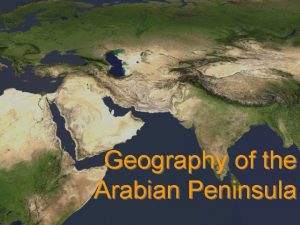
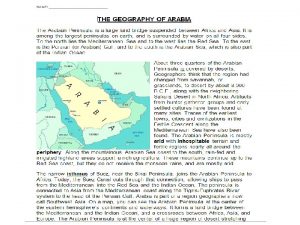
Mountainous peninsula Geography of the arabian peninsula
Geography of the arabian peninsula Aegean peninsula
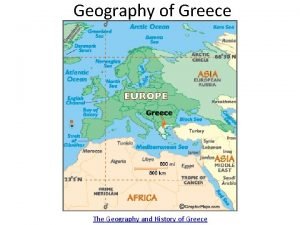
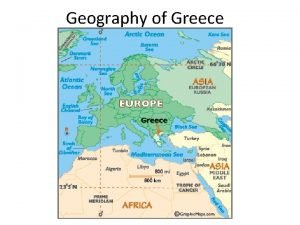
Aegean peninsula What peninsula is greece located on
What peninsula is greece located on Where was ancient greece located on a map
Where was ancient greece located on a map Peninsula unde era situată roma
Peninsula unde era situată roma Fauna of saudi arabia
Fauna of saudi arabia What separates europe from asia
What separates europe from asia Physical features of northern ireland
Physical features of northern ireland Choke points definition ap human geography
Choke points definition ap human geography Ancient greece balkan peninsula
Ancient greece balkan peninsula Balkan peninsula ancient greece
Balkan peninsula ancient greece Sparta peninsula
Sparta peninsula Qatar politica
Qatar politica