VASCULITIS FERDA ZKAN M D YEDITEPE UNIVERSITY MEDICAL
- Slides: 74
VASCULITIS FERDA ÖZKAN M. D. YEDITEPE UNIVERSITY MEDICAL FACULTY
OBJECTIVES l Review vessel structure l Explain inflammatory processes of vessels l Describe types of vasculitis
The basic constituents of the walls of blood vessels are endothelial cells and smooth muscle cells, and extracellular matrix (ECM), including elastin, collagen, and glycosoaminoglycans.
The three concentric layers: Ø -intima, Ø -media, Ø -adventitia are most clearly defined in the larger vessels, particularly arteries.
In normal arteries, the intima consists of a single layer of endothelial cells with minimal underlying subendothelial connective tissue. l It is separated from the media by a dense elastic membrane called the internal elastic lamina. l The smooth muscle cell layers of the media near the vessel lumen receive oxygen and nutrients by direct diffusion from the vessel lumen, facilitated by holes in the internal elastic membrane l
However, diffusion from the lumen is inadequate for the outer portions of the media in large and medium-sized vessels, therefore these areas are nourished by small arterioles arising from outside the vessel (called vasa vasorum, literally "vessels of the vessels") coursing into the outer one half to two thirds of the media.
l The outer limit of the media of most arteries is a well-defined external elastic lamina. External to the media is the adventitia, consisting of connective tissue with nerve fibers and the vasa vasorum
ARTERIES l Arteries are divided into three types: l (1) large or elastic arteries, including the aorta, l (2) medium-sized or muscular arteries, l (3) small arteries
l Large or elastic arteries, including the aorta, its large branches (particularly the innominate, subclavian, common carotid, and iliac), and pulmonary arteries;
l 2 -medium-sized or muscular arteries, comprising other branches of the aorta (e. g. , coronary and renal arteries); and l 3 - small arteries (less than approximately 2 mm in diameter) and arterioles (20 to 100 μm in diameter), within the substance of tissues and organs.
l Capillaries, approximately the diameter of a red blood cell (7 to 8 μm), have an endothelial cell lining but no media.
VEINS l Veins have larger diameters, larger lumens, and thinner and less well organized walls l Thus, because of their poor support, veins are predisposed to irregular dilation, compression, and easy penetration by tumors and inflammatory processes.
VEINS l The venous system collectively has a large capacity; approximately two thirds of all the blood is in veins. Reverse flow is prevented by venous valves in the extremities, where blood flows against gravity.
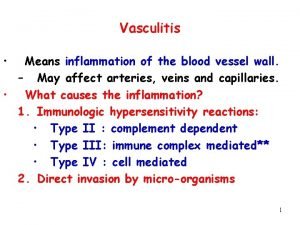
VASCULITIS l Vasculitis is a general term for vessel wall inflammation. l The clinical features of the various vasculitides are diverse and largely depend on the vascular bed affected (e. g. , central nervous system vs. heart vs. small bowel).
VASCULITIS l This is a heterogenous group of disorders characterized by inflammation & damage of blood vessels followed by thrombosis & ischemic manifestations in the tissues supplied by the blood vessels.
VASCULITIS l Besides the findings referable to the specific tissue(s) involved, the clinical manifestations typically include constitutional signs and symptoms such as fever, myalgias, arthralgias, and malaise.
INFECTIOUS VASCULITIS l Localized arteritis may be caused by the direct invasion of infectious agents, usually bacteria or fungi, and in particular Aspergillus and Mucor species.
INFECTIOUS VASCULITIS l Vascular invasion can be part of a localized tissue infection (e. g. , bacterial pneumonia or adjacent to abscesses), or l less commonly-it can arise from hematogenous seeding of bacteria during septicemia or embolization from sepsis of infective endocarditis.
NONINFECTIOUS VASCULITIS l The main immunological mechanisms that initiate noninfectious vasculitis are: Ø (1) immune complex deposition, Ø (2) antineutrophil cytoplasmic antibodies, and Ø (3) anti-endothelial cell antibodies.
Immune Complex-Associated Vasculitis The lesions resemble those found in experimental immune complexmediated conditions such as the Arthus reaction and serum sickness Many systemic immunological diseases, such as systemic lupus erythematosus (SLE) and polyarteritis nodosa, manifest as immune complex-mediated vasculitis.
Immune Complex-Associated Vasculitis l Antibody and complement are typically detected in vasculitic lesions, although the nature of the antigens responsible for their deposition cannot usually be determined.
Immune Complex-Associated Vasculitis l Circulating antigen-antibody complexes may also be seen (e. g. , DNA-anti-DNA complexes in SLEassociated vasculitis.
Antineutrophil Cytoplasmic Antibodies Patients with vasculitis have circulating antibodies that react with neutrophil cytoplasmic antigens, so-called antineutrophil cytoplasmic antibodies (ANCAs).
Antineutrophil Cytoplasmic Antibodies ANCAs are a heterogeneous group of autoantibodies directed against constituents (mainly enzymes) of neutrophil primary granules, monocyte lysosomes, and endothelial cells
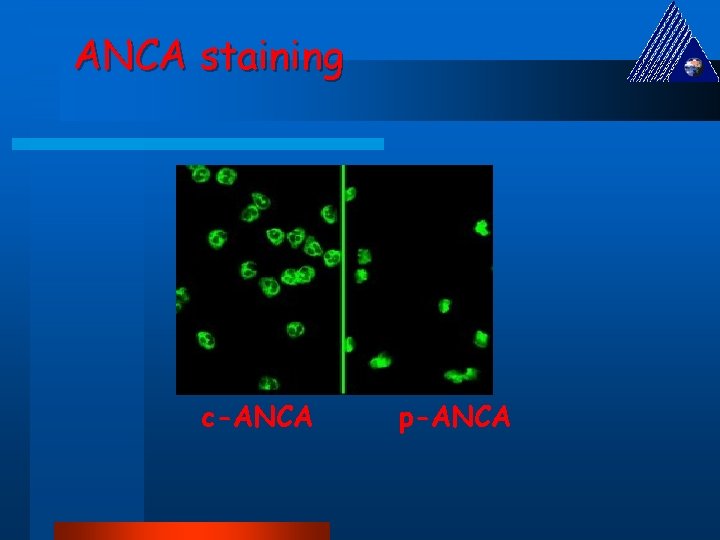
Antineutrophil Cytoplasmic Antibodies These were previously classified according to their intracellular distribution, either cytoplasmic (c. ANCA) or perinuclear (p-ANCA).
ANCAS They are discriminated based on their target antigens: Anti-myeloperoxidase (MPO-ANCA): MPO is a lysosomal granule constituent normally involved in generating oxygen free radicals. MPO-ANCAs can be induced by a variety of therapeutic agents, in particular propylthiouracil. These have been called p-ANCA.
ANCAS Anti-proteinase-3 (PR 3 -ANCA): PR 3 is also a neutrophil azurophilic granule constituent. That it shares homology with numerous microbial peptides may explain how PR 3 -ANCAs develop. These have been called c-ANCA.
Mechanism for ANCA vasculitis - Drugs or cross-reactive microbial antigens induce ANCAs; alternatively, neutrophil surface expression or release of PR 3 and MPO (e. g. , in the setting of infections) incites ANCA formation in a susceptible host.
Mechanism for ANCA vasculitis Subsequent infection, endotoxin exposure, or other inflammatory stimuli elicit cytokines such as TNF that cause surface expression of PR 3 and MPO on neutrophils and other cell types.
Mechanism for ANCA vasculitis ANCAs react with these cytokineactivated cells and either cause direct injury (e. g. , to endothelial cells) or induce further activation (e. g. , in neutrophils). l ANCA-activated neutrophils degranulate and also cause injury by releasing reactive oxygen species, engendering endothelial cell toxicity and other indirect tissue injury. l
Mechanism for ANCA vasculitis l ANCAs directed against constituents other than PR 3 and MPO are also found in some patients with inflammatory disorders that do not involve vasculitis (e. g. , inflammatory bowel disease, primary sclerosing cholangitis, rheumatoid arthritis
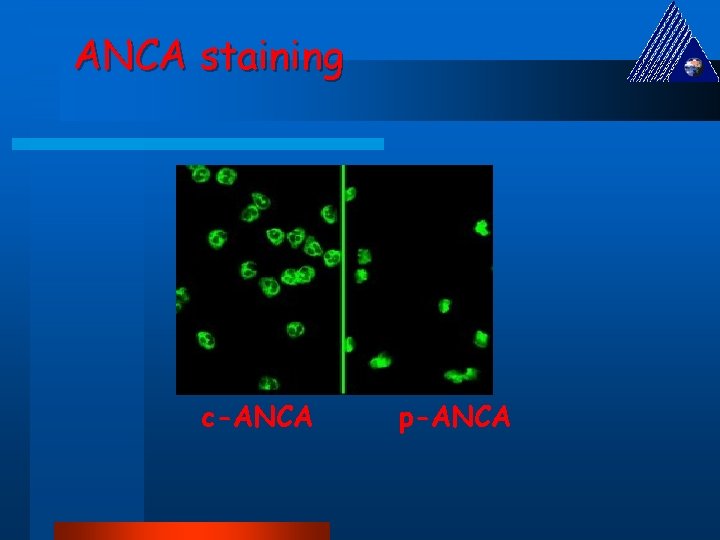
ANCA staining c-ANCA p-ANCA
Anti-Endothelial Cell Antibodies to endothelial cells may predispose to certain vasculitides, for example, Kawasaki disease
Pathology: Small vessels Henoch-Schönlein Purpura form of hypersensitivity vasculitis in kids, young adults l clinical: l – – purpura on buttocks, arms, legs necrotizing vasculitis involving small dermal vessels arthritis abdominal pain – often with bloody diarrhea/other evidence of intestinal bleeding, due to mucosal/submucosal vasculitis – kidney involvement in 1/3 – proteinuria, nephrotic syndrome, gross/microscopic hematuria. Pathology: l glomerulonephritis is often focal, mesangial proliferative in type; often self-limiting l Ig. A is predominant Ab in glomerular and skin lesions.
Pathology: Small vessels Mixed Cryoglobulinemia syndrome l Clinical: – widespread small vessel vasculitis, often associated with severe glomerulonephritis – purpura – arthralgia or arthritis – cryoglobulins – reversibly precipitatie in the cold – consist of Ig. M rheumatoid factors – most seen in patients with HCV
l Pathology: – vessels show deposits containing cryoglobulins and complement – leukocytoclastic vasculitis.
Pathology: Medium-sized vessels Polyarteritis Nodosa l 40 -50 s, May be life threatenting; fever, myalgia, weight loss, foot drop, weakness, abdominal pain, hypertension from renal arteriole involvement mononeuritis complex - asymmetric peripheral neuropathy with sudden or subacute onset due to nerve infarction; many modalities lost in one nerve local ischemia, inflammation of affected organs kidney, GI tract, joints/muscles, heart, nervous system, skin, lungs may be affected.
Polyarteritis Nodosa l Polyarteritis nodosa (PAN) is a systemic vasculitis of small or medium-sized muscular arteries (but not arterioles, capillaries, or venules), typically involving renal and visceral vessels but sparing the pulmonary circulation
Polyarteritis Nodosa l There is no association with ANCAs, but about 30% of patients with PAN have chronic hepatitis B with HBs. Ag -Hbs. Ab complexes in affected vessels, indicating an immune complex-mediated etiology
Polyarteritis Nodosa l The cause remains unknown in the majority of cases; there may be etiologic and important clinical distinctions between classic idiopathic PAN, the cutaneous forms of PAN, and the PAN associated with chronic hepatitis. Clinical manifestations result from ischemia and infarction of affected tissues and organs.
Findings l Digital gangrene, ulceration l Renal - Hypertension, hematuria, renal failure l GIS - hematemesis, melena l RS - pneumonitis, pleural effusion l CNS - mononeuritis multiplexa l Skin - urticaria, palpable purpura, livedo reticularis.
l Diagnosis: – microaneurysms on angiography if medium vessels are target – segmental damage to artery walls; present in up to 50% of cases – aneurysms or stenosis in mesenteric vessels in absence of atherosclerosis is very helpful to make diagnosis. l Treatment: steroids, immunosuppressive drugs, some respond to bactrim.
Pathology All stages of activity may coexist in different vessels, even in one vessel. Early: focal, fibrinoid necrosis of artery/arteriole wall; transmural inflammation – PMN, eosinophilic poly infiltrate Intermediate: mural/occlusive thrombi Late: aneurysms if segmental involvement with healing, wall infiltrated by fibroblasts -> fibrous thickening of wall -> nodular appearance.
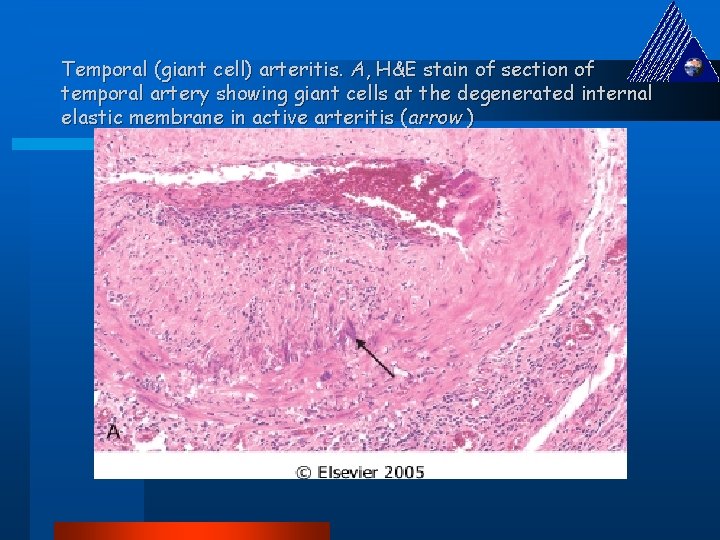
Pathology: Large vessels Giant cell arteritis and temporal arteritis l Mean age of onset 70 years; l Commonly associated with clinical syndrome polymyalgia rheumatica: o pain, stiffness in shoulder & pelvic girdles in absence of evidence of weakness or atrophy o ESR o response to low-moderate steroid doses. l Etiology: likely mediated by immune reactions to elastin
l Granulomatous inflammatory process can affect any elastic and muscular artery: – most often seen in superficial temporal artery, other cranial arteries – chief clinical risk is blindness – clinical presentation: headache, scalp tenderness, claudication of the jaw (tired jaw on chewing), transient visual disturbances, musculoskeletal symptoms (polymyalgia rheumatica) , fever, malaise, weight loss, anemia.
l Extracranial disease in 10 -15%: o intermittent claudication is common o arterial bruits, blood pressure abnormalities. l Treatment: responds well to steroids. Complications coronary artery involvement myocardial ischemia aortic valve incompetence aortic dissection aortic aneurysm, may rupture.
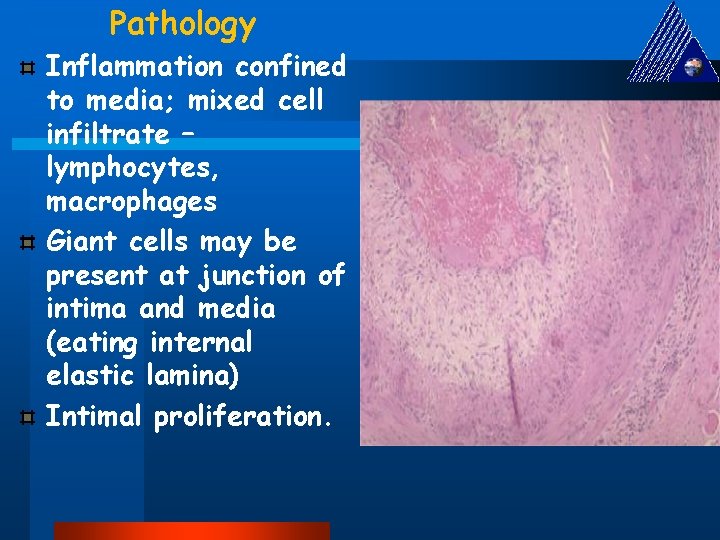
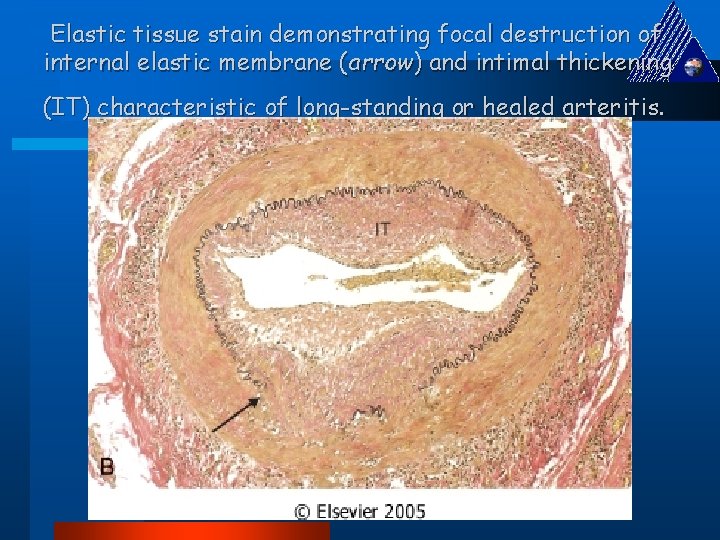
Pathology Inflammation confined to media; mixed cell infiltrate – lymphocytes, macrophages Giant cells may be present at junction of intima and media (eating internal elastic lamina) Intimal proliferation.
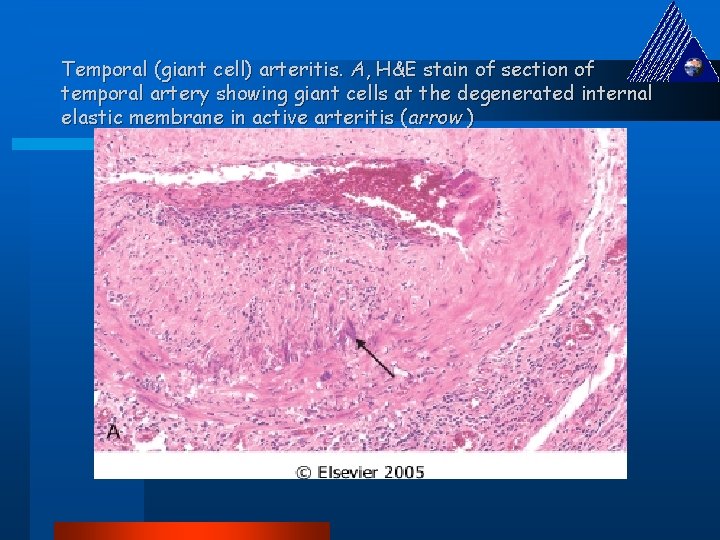
Temporal (giant cell) arteritis. A, H&E stain of section of temporal artery showing giant cells at the degenerated internal elastic membrane in active arteritis (arrow )
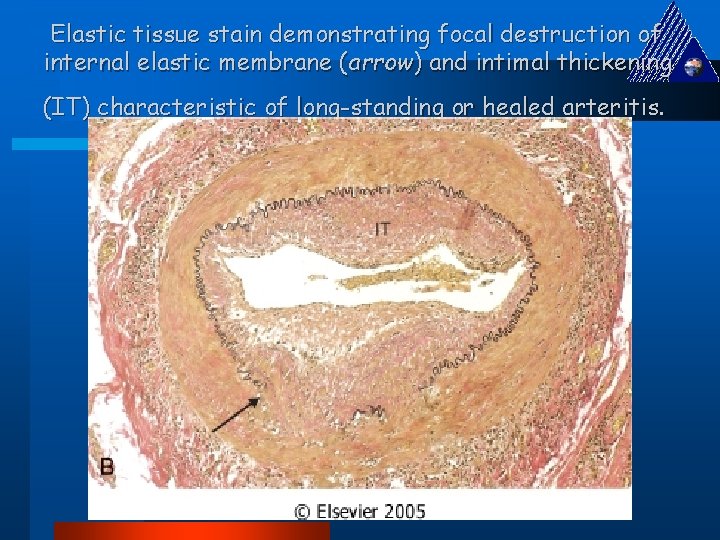
Elastic tissue stain demonstrating focal destruction of internal elastic membrane (arrow) and intimal thickening (IT) characteristic of long-standing or healed arteritis.
Cogan's disease is another rare disease usually affecting young adults. l It features abrupt onset of – nerve deafness, – interstitial keratitis, and/or – a systemic vasculitis often with – aortic aneurysm formation. l It's apparently caused by an autoantibody against inner ear and endothelium l
Pathology: Small to Medium-sized vessels Wegener’s Granulomatosis l can occur from teens to old age; peak at age 40, l slight male proponderance. l 82% die in a year without treatment
Wegener’s Granulomatosis Wegener granulomatosis is a necrotizing vasculitis characterized by a triad of: l Acute necrotizing granulomas of the upper respiratory tract (ear, nose, sinuses, throat) or the lower respiratory tract (lung) or both
Wegener’s Granulomatosis Necrotizing or granulomatous vasculitis affecting small to medium-sized vessels (e. g. , capillaries, venules, arterioles, and arteries), most prominent in the lungs and upper airways but affecting other sites as well l Renal disease in the form of focal necrotizing, often crescentic, glomerulonephritis l
l Symptoms: – upper respiratory tract (sinusitis, epistaxis, nasal obstruction, otitis media, deafness), – lower respiratory tract (productive cough, hemoptysis, dyspnea), – renal failure.
Clinical Findings Respiratory System – upper respiratory tract infections, saddle nose deformity, pneumonitis, pleural effusion l Renal - hematuria, hypertension, renal failure l Ocular - conjunctivitis, uveitis l Skin - urticaria, palpable purpura, livedo reticularis. l
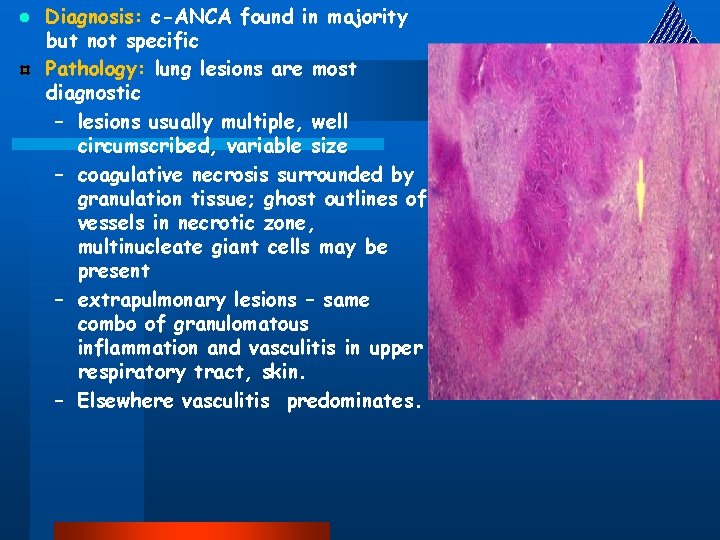
l Diagnosis: c-ANCA found in majority but not specific Pathology: lung lesions are most diagnostic – lesions usually multiple, well circumscribed, variable size – coagulative necrosis surrounded by granulation tissue; ghost outlines of vessels in necrotic zone, multinucleate giant cells may be present – extrapulmonary lesions – same combo of granulomatous inflammation and vasculitis in upper respiratory tract, skin. – Elsewhere vasculitis predominates.
Pathology: Medium-sized vessels Bürger’s Disease (thromboangitis obliterans) predominates in young adult male (20 -45) tobacco smokers; female smokers as well. Sligtly more common in Asians, Ashkenazi Jews. l clinical: – ischemia, usually of lower limbs, progressing to gangrene – absence of atherosclerotic stigmata or risk factors – associated with migratory thrombophlebitis l
Pathology l sharply segmental, thrombosing acute and chronic inflammation of medium sized arteries with secondary spread to veins l thrombus may undergo organization and recanalization l improvement with smoking cessation.
Pathology: Large vessels Takayasu Arteritis or Aortitis Common in Far east; women 15 -45 affected l Chronic inflammatory disease involving both systemic and pulmonary circulations Aorta & major branches most commonly affected – coronaries l Clinical: stenosis is characteristic l Pathology: artery wall inflammation fibromuscular intimal proliferation, mural thrombi granulomatous panarteritis vessel converted into rigid tube, associated with stenosis. l
Aortitis is literally inflammation of the aorta, and it is representative of a cluster of large-vessel diseases that have various or unknown etiologies. l While inflammation can occur in response to any injury, including trauma, the most common known causes are infections or connective tissue disorders. l Infections can trigger a noninfectious vasculitis by generating immune complexes or by cross-reactivity. l The etiology is important because immunosuppressive therapy, the main treatment for vasculitis, could aggravate an active infectious process. l
Inflammation of the aorta can cause aortic dilation, resulting in aortic insufficiency. l Also, it can cause fibrous thickening and ostial stenosis of major branches, resulting in reduced or absent pulses, low blood pressure in the arms, possibly with central hypertension due to renal artery stenosis. l Depending on what other vessels are involved, ocular disturbances, neurological deficits, claudication, and other manifestations of vascular impairment may accompany this disorder. l
l Infectious agents: – Neisseria (eg, gonorrhea) – Rickettsia (eg, Rocky Mountain spotted fever) species, – spirochetes (eg, syphilis), – fungi (eg, aspergillosis, mucormycosis), – viruses (eg, herpes, varicellazoster, hepatitis B and C).
Immune disorders: – serum sickness, – cryoglobulinemia, – SLE, – rheumatoid arthritis, – Henoch-Schönlein purpura, – postinfectious immune complex disease, – drug-induced immune complex disease.
– Anti-neutrophil cytoplasmic autoantibody (ANCA) can affect the large vessels, as in Wegener granulomatosis, polyangiitis, and Churg-Strauss syndrome. – Other antibodies such as antiglomerular basement membrane (ie, Goodpasture syndrome) and antiendothelial (ie, Kawasaki disease) also can be culprits. – Transplant rejection, inflammatory bowel diseases, and paraneoplastic vasculitis also may afflict the large vessels.
l The disease has 3 phases: – Phase I is (prepulseless inflammatory period) – Phase II (vascular inflammation) – Phase III (fibrosis stage)
• ischemic symptoms and signs secondary to dilation, narrowing, or occlusion of the proximal or distal branches of the aorta. • Extremities become cool, and pain develops with use (ie, arm or leg claudication). • In advanced cases, occlusion of the vessels to the extremities may result in ischemic ulcerations or gangrene, and with the involvement of cerebral arteries, strokes can occur.
l Pathologic changes involved in Takayasu arteritis are the same as for giant cell arteritis. – Involved vessel walls develop irregular thickening and intimal wrinkling. – Early in the disease, mononuclear infiltration with perivascular cuffing is seen. – That extends to the media, followed by granulomatous changes and patches of necrosis and scarring (fibrosis) of all layers, especially the intima. – Late stages have lymphocytic infiltration.
Histologic Findings: l Focal panarteritis: – The intima is markedly thickened by accumulation of mucopolysaccharides. – The media and adventitia demonstrate mixed cellular infiltration with granuloma and giant cells. – The lesions usually are focal skip lesions rather than the diffuse involvement observed in patients with syphilitic aortitis.
l When the abdominal aorta and its branches, eg, the renal arteries, are involved, central hypertension may develop. – Accurate blood pressure measurement may be difficult because of arterial lesions affecting supply to the extremities. l Takayasu arteritis primarily involves the aorta, its main branches, and, in 50% of cases, the pulmonary artery. – The initial vascular lesions frequently occur in or at the origin of the left subclavian artery, which can cause weakened radial pulse and easy fatigability in the left arm. – As the disease progresses, the left common carotid, vertebral, brachiocephalic, right-middle or proximal subclavian, right carotid, and vertebral arteries, as well as the aorta, also are affected, as well as retinal vessels.
l Complications: l Aortic insufficiency, l angina pectoris, l myocardial infarction, l stroke, l limb ischemia, l renal artery hypertension, l all consequences of vascular diseases.
Kawasaki's disease A febrile disease which resembles adult polyarteritis nodosa histologically but occurs in babies. l Need to see five of these six signs: l o o fever (will last more than five days) non-purulent conjunctivitis in both eyes rash red cracked lips and/or strawberry tongue and/or red oral mucosa o red palms and soles (later they desquamate) o a big (1. 5 cm or more) lymph node in the neck.
l Most patients are of Japanese of Korean ancestry, regardless of where they live, but no HLA links are found. l The most serious concern is coronary vasculitis, which causes myocardial infarcts. Healing can produce coronary aneurysms, l The cause remains obscure.
Raynaud's disease & phenomenon Spasm and occlusion of the arteries supplying the fingers, which turn white, then red, then blue. l Triggered by cold weather, it's most often idiopathic; known causes range from vasculitis syndromes to operating jack-hammers. l Scleroderma patients and some others have this process greatly exacerbated by hyperplastic arteriolar sclerosis in the digital arteries. l
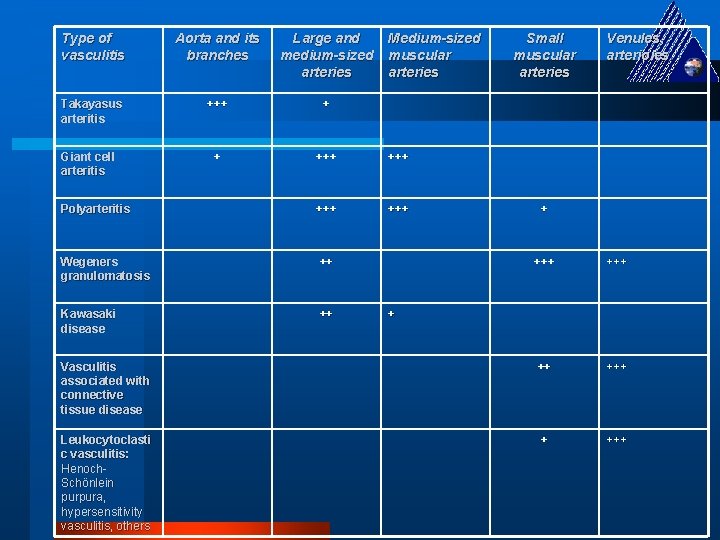
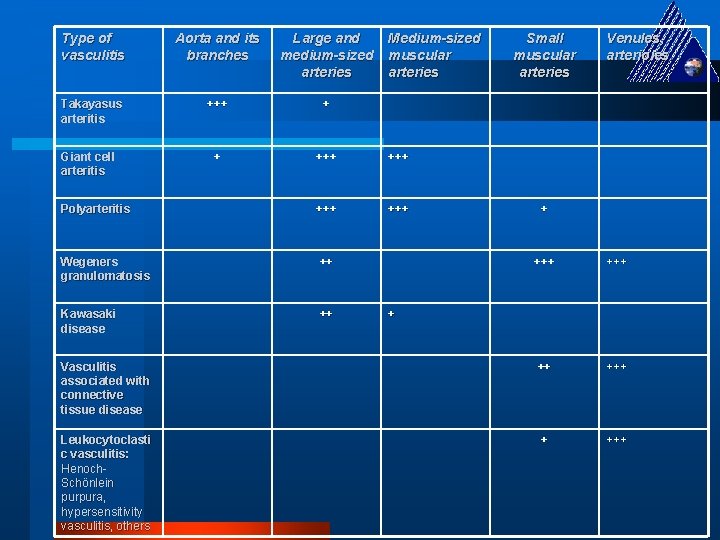
Type of vasculitis Aorta and its branches Large and medium-sized arteries Takayasus arteritis +++ + + +++ Polyarteritis +++ Wegeners granulomatosis ++ Kawasaki disease ++ Giant cell arteritis Medium-sized muscular arteries Small muscular arteries Venules, arterioles + +++ Vasculitis associated with connective tissue disease ++ +++ Leukocytoclasti c vasculitis: Henoch. Schönlein purpura, hypersensitivity vasculitis, others + +++ +
 Gencon 76
Gencon 76 Zkan
Zkan Oš ferda vesela
Oš ferda vesela Yeditepe üniversitesi hastanesi
Yeditepe üniversitesi hastanesi Ferda ernawan
Ferda ernawan Mravenec ferda ocitne ve vězení a je odsouzen
Mravenec ferda ocitne ve vězení a je odsouzen Ferda pictures meaning
Ferda pictures meaning Coadsys exam yeditepe
Coadsys exam yeditepe Nazivi zemljinih gibanja
Nazivi zemljinih gibanja Coadsys exam
Coadsys exam Birmingham vasculitis activity score
Birmingham vasculitis activity score Vasculitis
Vasculitis Vasculitis
Vasculitis Vasculitis
Vasculitis Segmental thrombosing vasculitis
Segmental thrombosing vasculitis Vasculitis
Vasculitis Sle vasculitis
Sle vasculitis Sle vasculitis
Sle vasculitis Perforacion septal
Perforacion septal Takayasu arteritis
Takayasu arteritis Clasificacion chapel hill vasculitis 2012
Clasificacion chapel hill vasculitis 2012 Vasculitis
Vasculitis Dr donna braham
Dr donna braham Anca p
Anca p California medical license for foreign medical graduates
California medical license for foreign medical graduates Gbmc infoweb
Gbmc infoweb Hepburn osteometric board
Hepburn osteometric board Torrance memorial transitional care unit
Torrance memorial transitional care unit Cartersville medical center medical records
Cartersville medical center medical records University medical centre maribor
University medical centre maribor Liaoning medical university
Liaoning medical university Vietnam military medical university
Vietnam military medical university M.gorky donetsk national medical university
M.gorky donetsk national medical university Masaryk university medical faculty
Masaryk university medical faculty Serum vs plasma
Serum vs plasma Seoul national university history
Seoul national university history Kirovohrad medical university
Kirovohrad medical university University of maryland capital region health
University of maryland capital region health Stavropol state medical university
Stavropol state medical university Empp university medical center
Empp university medical center Ljubljana medical school
Ljubljana medical school Maribor gluten free
Maribor gluten free Columbia university medical center
Columbia university medical center Columbia university medical center
Columbia university medical center Lorenzo azzalini
Lorenzo azzalini Kaohsiung medical university hospital
Kaohsiung medical university hospital Medical academy of lublin
Medical academy of lublin Osh state medical university logo
Osh state medical university logo Mongolian national university of medical sciences
Mongolian national university of medical sciences Hawler medical university college of nursing
Hawler medical university college of nursing Google citations
Google citations Bled health centre
Bled health centre Uq som
Uq som Palm harbor university high school medical program
Palm harbor university high school medical program Masaryk university medical faculty
Masaryk university medical faculty 詹景裕
詹景裕 Wyndham houston medical center
Wyndham houston medical center Medical manuscript writing
Medical manuscript writing Three types of word parts
Three types of word parts Wootton medical centre
Wootton medical centre Woodlane medical centre doctors
Woodlane medical centre doctors Tifr medical section
Tifr medical section Plumb line posture
Plumb line posture Patient centered medical home conference
Patient centered medical home conference Queen anne medical electrolysis and laser
Queen anne medical electrolysis and laser Plan odo268 swiss medical
Plan odo268 swiss medical Chapter 11 medical terminology
Chapter 11 medical terminology Pte aok timetable
Pte aok timetable Examples of eponyms
Examples of eponyms Umass anesthesiology residency
Umass anesthesiology residency 同善医院中医部医生
同善医院中医部医生 Medical gas slide
Medical gas slide Chemetron medical gas alarm panel
Chemetron medical gas alarm panel Tiu medical analysis
Tiu medical analysis Vermont medical examiner
Vermont medical examiner