Hypoglycemia Hasan AYDIN MD Yeditepe University Medical Faculty







- Slides: 47
Hypoglycemia Hasan AYDIN, MD Yeditepe University Medical Faculty Department of Endocrinology and Metabolism
What is it? • Hypoglycemia refers to a low level of serum glucose • Occurs when a mismatch of endogenous glucose need with exogenous and endogenous glucose availability • Often defined as a plasma glucose level < 45 -50 mg/d. L
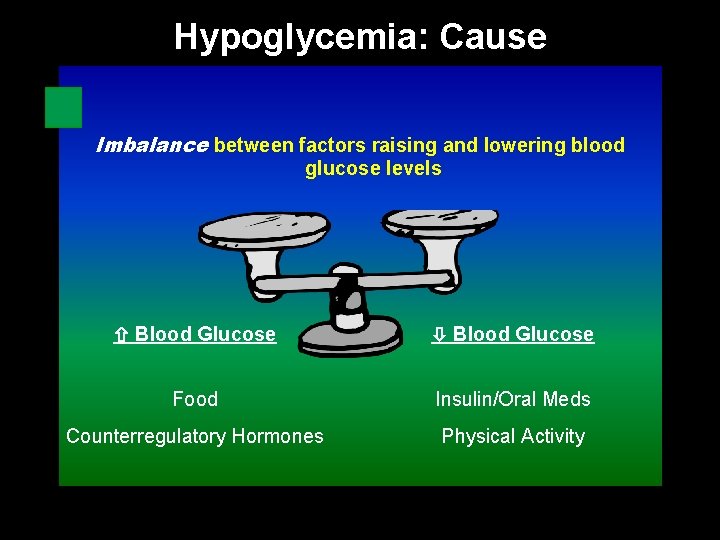
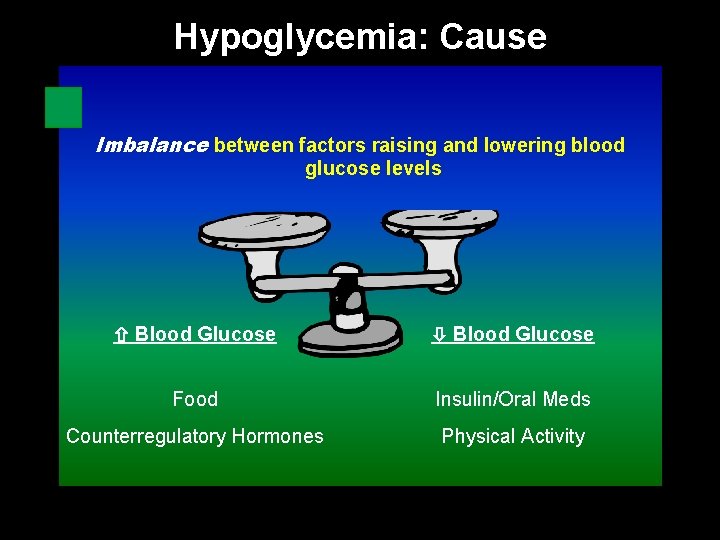
Hypoglycemia: Cause Imbalance between factors raising and lowering blood glucose levels Blood Glucose Food Insulin/Oral Meds Counterregulatory Hormones Physical Activity
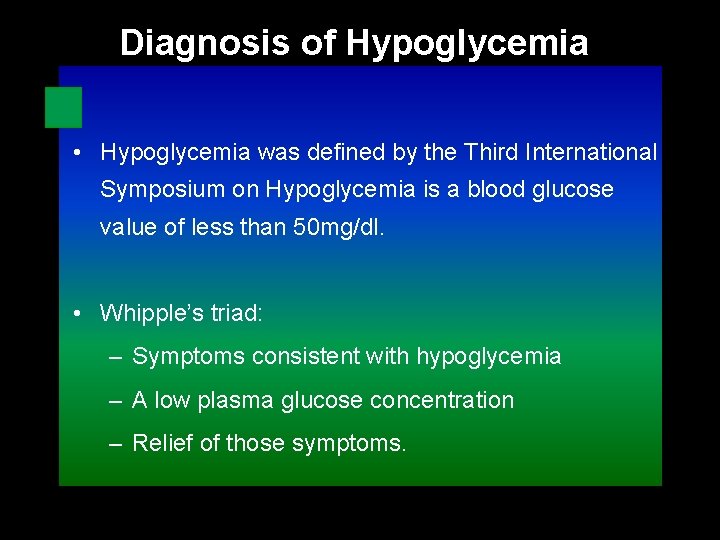
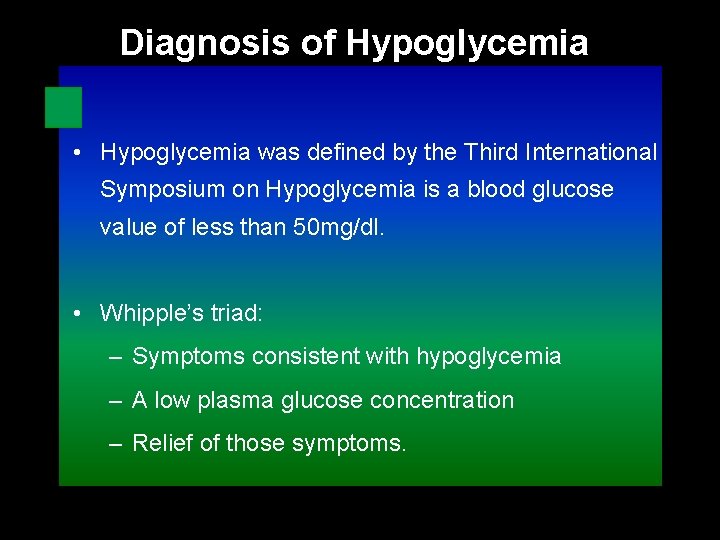
Diagnosis of Hypoglycemia • Hypoglycemia was defined by the Third International Symposium on Hypoglycemia is a blood glucose value of less than 50 mg/dl. • Whipple’s triad: – Symptoms consistent with hypoglycemia – A low plasma glucose concentration – Relief of those symptoms.
Definition • An abnormality, not a disease • Abnormally low blood glucose level • Caused by – Pathologic conditions or disease states – Physiological conditions
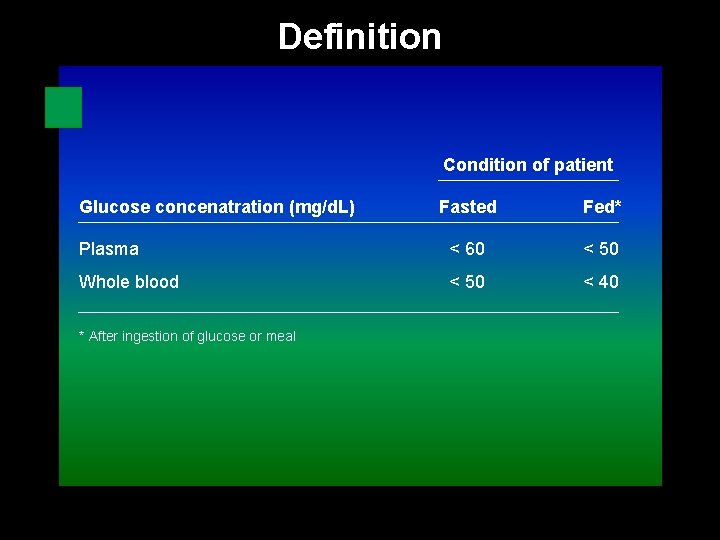
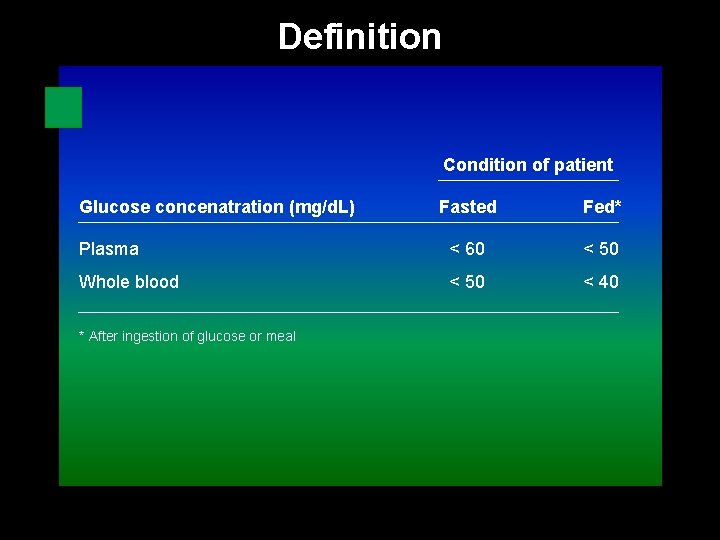
Definition Condition of patient Glucose concenatration (mg/d. L) Fasted Fed* Plasma < 60 < 50 Whole blood < 50 < 40 * After ingestion of glucose or meal
General Approach • Documentation of low blood glucose concentration • Systematic efforts to determine what condition is responsible for • Fasting or fed state – Symptoms developing when missing a meal – Symptoms developing after meals

Insulin is the “key” that allows special “gates” for sugar transport across cell membranes to be opened
Why do we care about it? Because hypoglycemia can kill
Why do we care about it? Physiology – Glucose is an obligate metabolic fuel for the brain under physiologic conditions, while other organs can use other forms of fuel (i. e. fatty acids) – The brain can not synthesize its own glucose; it requires a continuous supply via arterial blood
Why do we care about it? Maintenance of glucose homeostasis – Narrow plasma glucose range is normally maintained despite fluctuations in food intake and activity levels – Maintenance through diet, glycogen breakdown (liver) and gluconeogenesis (liver and kidney)
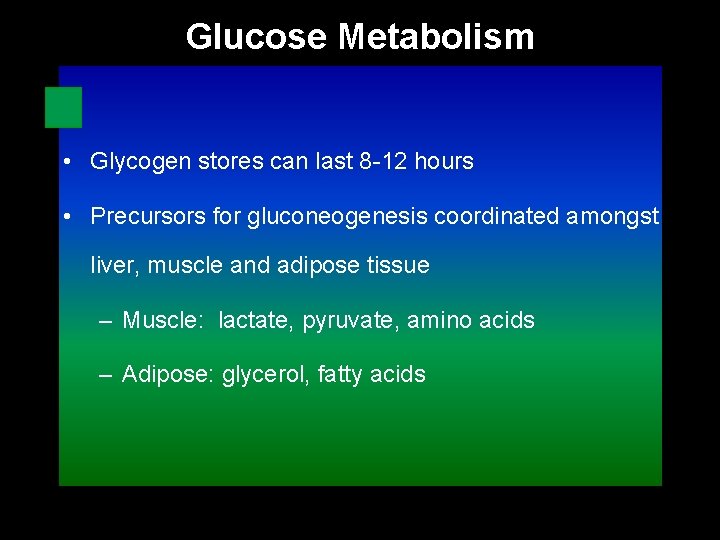
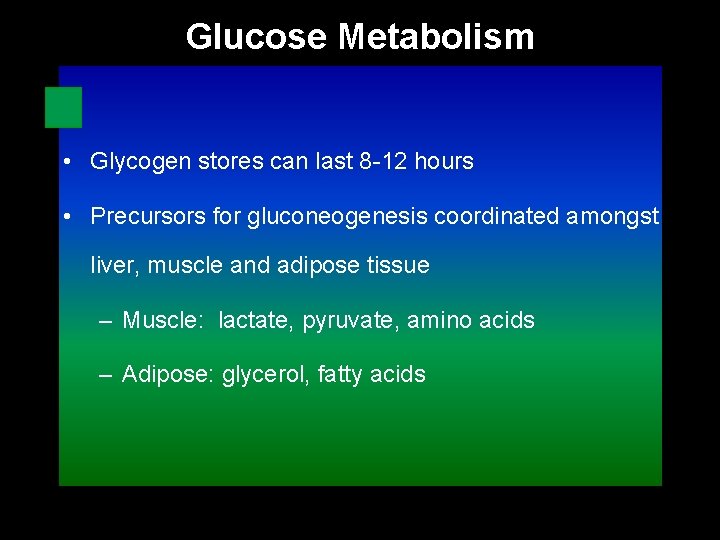
Glucose Metabolism • Glycogen stores can last 8 -12 hours • Precursors for gluconeogenesis coordinated amongst liver, muscle and adipose tissue – Muscle: lactate, pyruvate, amino acids – Adipose: glycerol, fatty acids
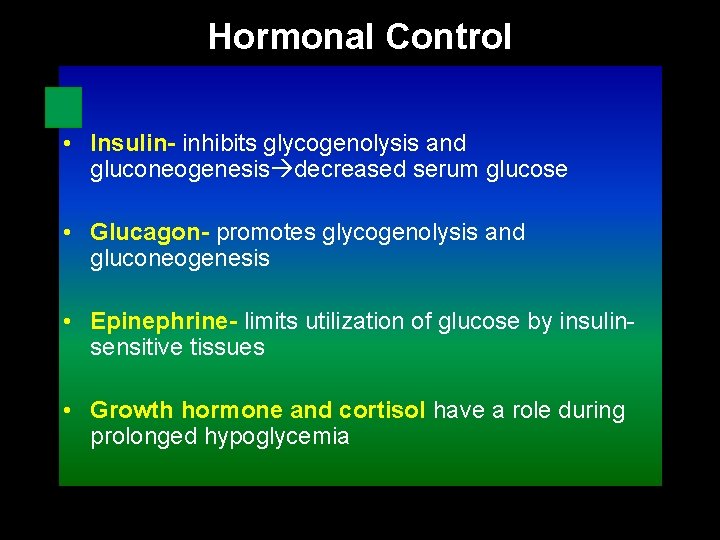
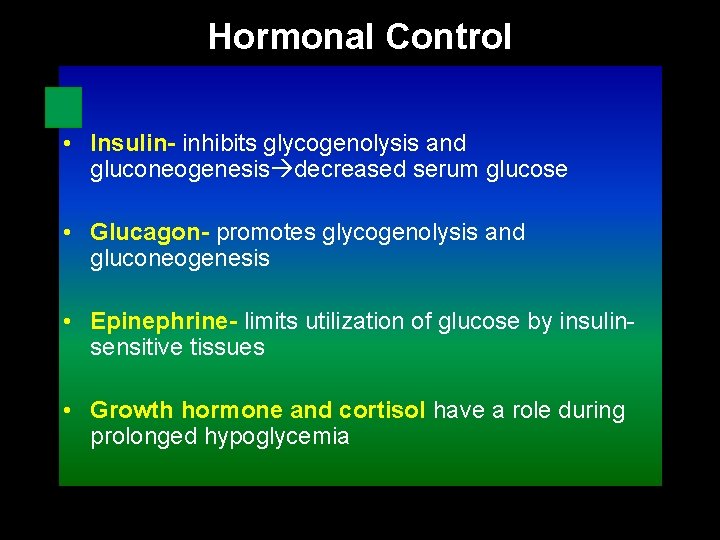
Hormonal Control • Insulin- inhibits glycogenolysis and gluconeogenesis decreased serum glucose • Glucagon- promotes glycogenolysis and gluconeogenesis • Epinephrine- limits utilization of glucose by insulinsensitive tissues • Growth hormone and cortisol have a role during prolonged hypoglycemia

Signs and Symptoms • Adrenergic – – – Weakness Sweating Tachycardia Palpitations Tremor Nervousness Irritability Tingling of mouth Hunger Nausea Vomiting • Neuroglucopenic – – – – Headache Hypothermia Visual disturbances Mental dullness Confusion Amnesia Seizures Coma
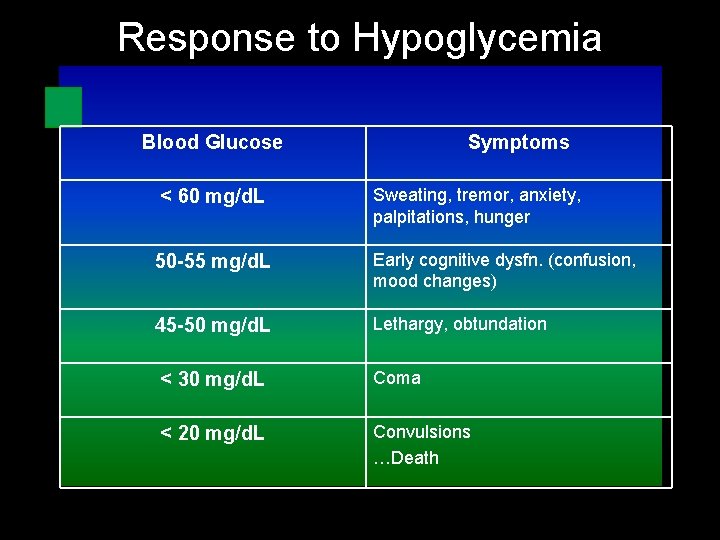
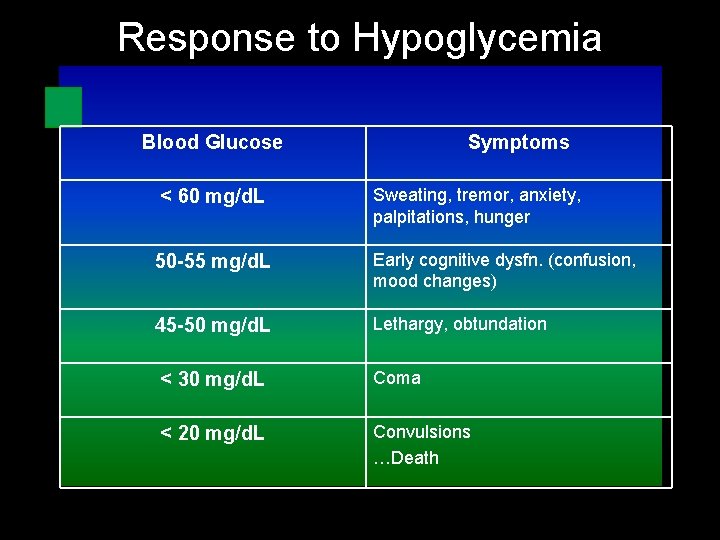
Response to Hypoglycemia Blood Glucose < 60 mg/d. L Symptoms Sweating, tremor, anxiety, palpitations, hunger 50 -55 mg/d. L Early cognitive dysfn. (confusion, mood changes) 45 -50 mg/d. L Lethargy, obtundation < 30 mg/d. L Coma < 20 mg/d. L Convulsions …Death
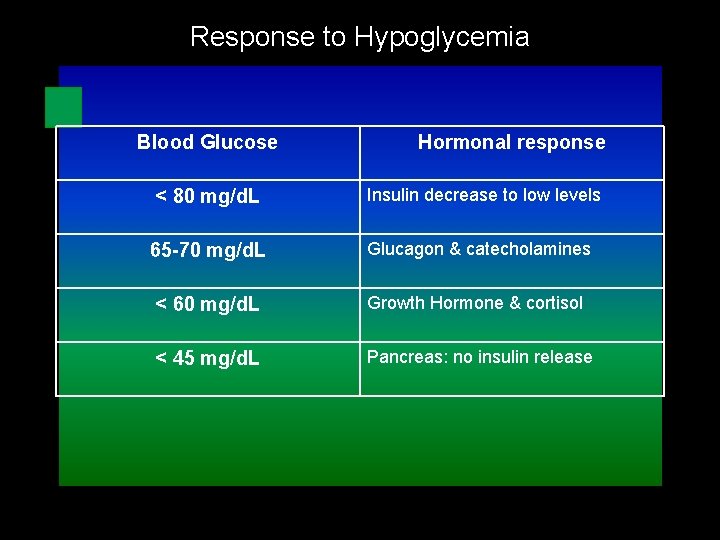
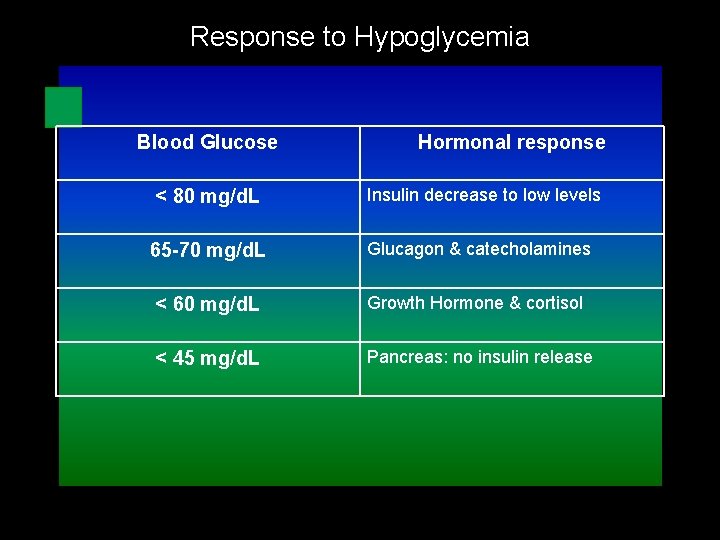
Response to Hypoglycemia Blood Glucose Hormonal response < 80 mg/d. L Insulin decrease to low levels 65 -70 mg/d. L Glucagon & catecholamines < 60 mg/d. L Growth Hormone & cortisol < 45 mg/d. L Pancreas: no insulin release
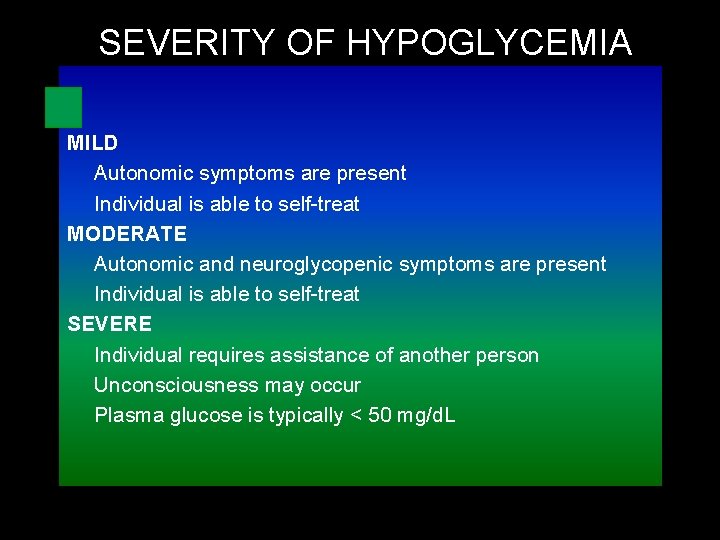
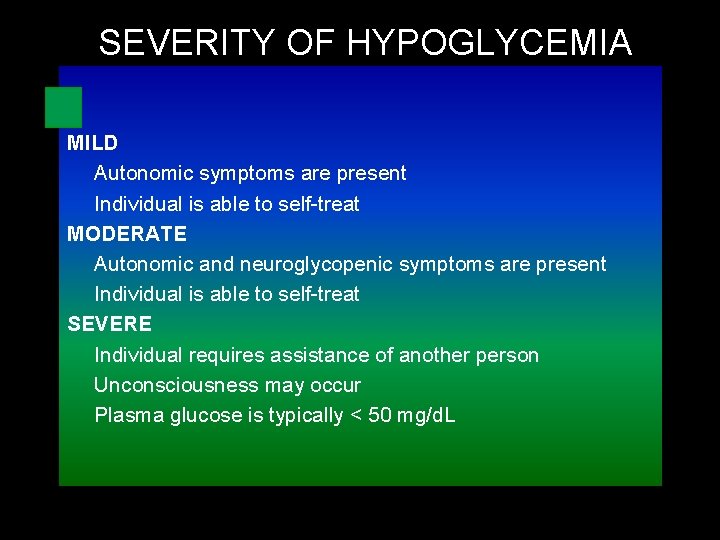
SEVERITY OF HYPOGLYCEMIA MILD Autonomic symptoms are present Individual is able to self-treat MODERATE Autonomic and neuroglycopenic symptoms are present Individual is able to self-treat SEVERE Individual requires assistance of another person Unconsciousness may occur Plasma glucose is typically < 50 mg/d. L

TREATMENT GOALS: To detect and treat a low blood glucose level promptly by using an intervention that provides a rapid rise is blood glucose to a safe level, eliminating the risk of injury, and relieving symptoms quickly. It is also important to avoid overtreatment with resulting rebound hyperglycemia and risk of weight gain. Ø 15 g of glucose will usually increase blood glucose by 40 mg/d. L within 20 minutes with adequate symptom relief for most people. Ø 20 g will usually increase blood glucose by 65 mg/d. L within 45 minutes.
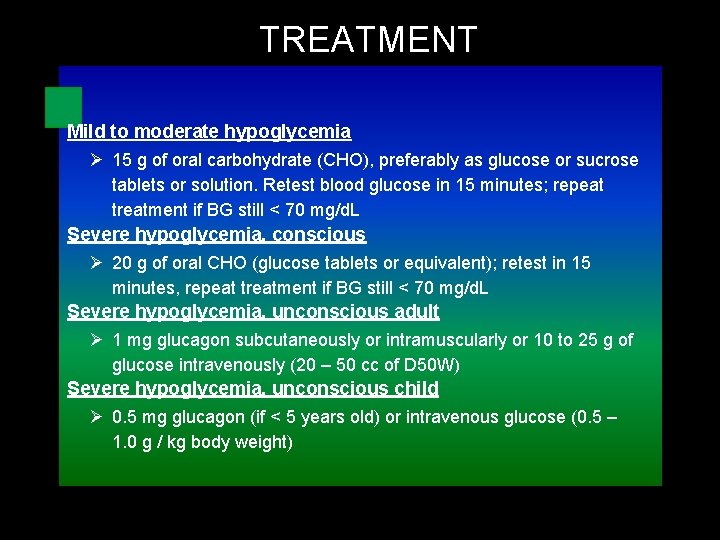
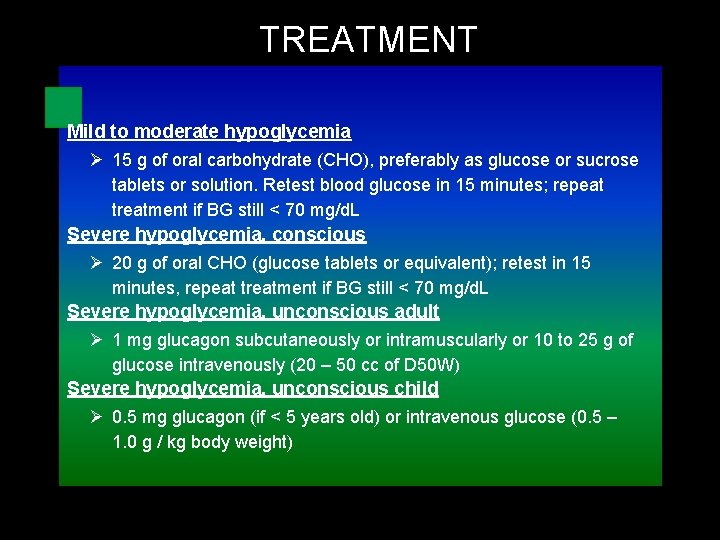
TREATMENT Mild to moderate hypoglycemia Ø 15 g of oral carbohydrate (CHO), preferably as glucose or sucrose tablets or solution. Retest blood glucose in 15 minutes; repeat treatment if BG still < 70 mg/d. L Severe hypoglycemia, conscious Ø 20 g of oral CHO (glucose tablets or equivalent); retest in 15 minutes, repeat treatment if BG still < 70 mg/d. L Severe hypoglycemia, unconscious adult Ø 1 mg glucagon subcutaneously or intramuscularly or 10 to 25 g of glucose intravenously (20 – 50 cc of D 50 W) Severe hypoglycemia, unconscious child Ø 0. 5 mg glucagon (if < 5 years old) or intravenous glucose (0. 5 – 1. 0 g / kg body weight)
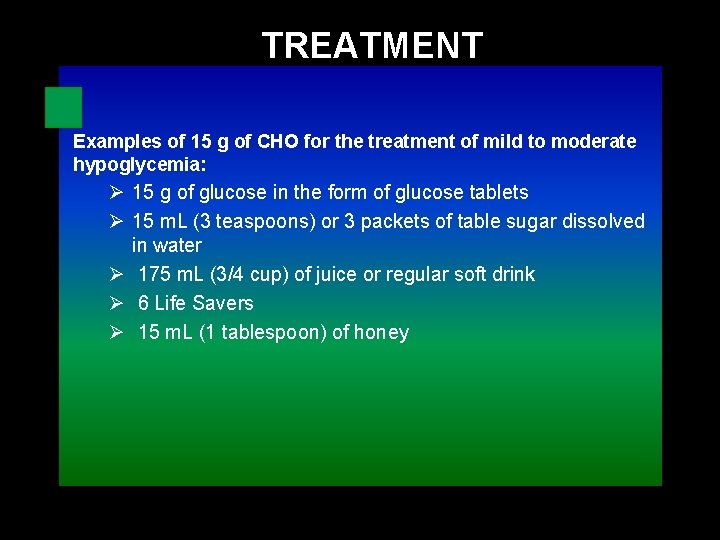
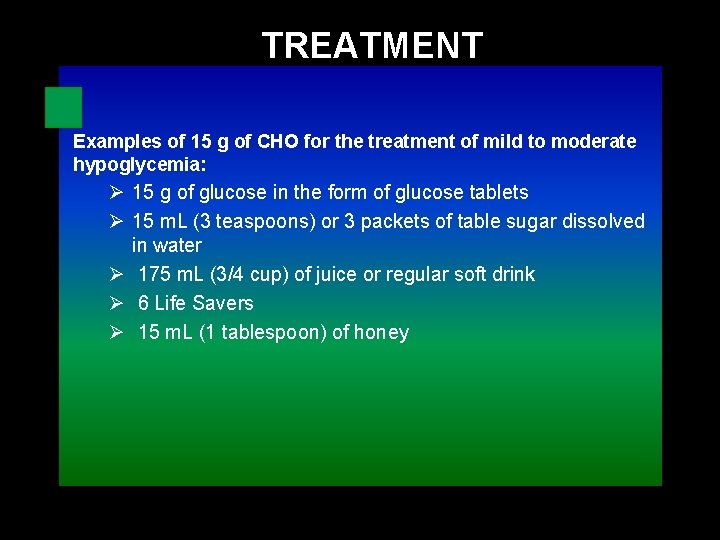
TREATMENT Examples of 15 g of CHO for the treatment of mild to moderate hypoglycemia: Ø 15 g of glucose in the form of glucose tablets Ø 15 m. L (3 teaspoons) or 3 packets of table sugar dissolved in water Ø 175 m. L (3/4 cup) of juice or regular soft drink Ø 6 Life Savers Ø 15 m. L (1 tablespoon) of honey
Etiology Classified into three groups: 1. Medications or toxins. 2. Disorders associated with fasting hypoglycemia. 3. Disorders associated postprandial hypoglycemia.
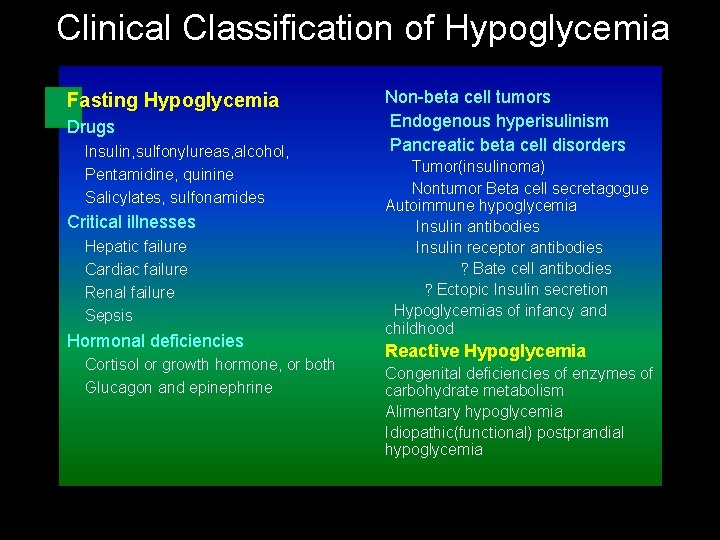
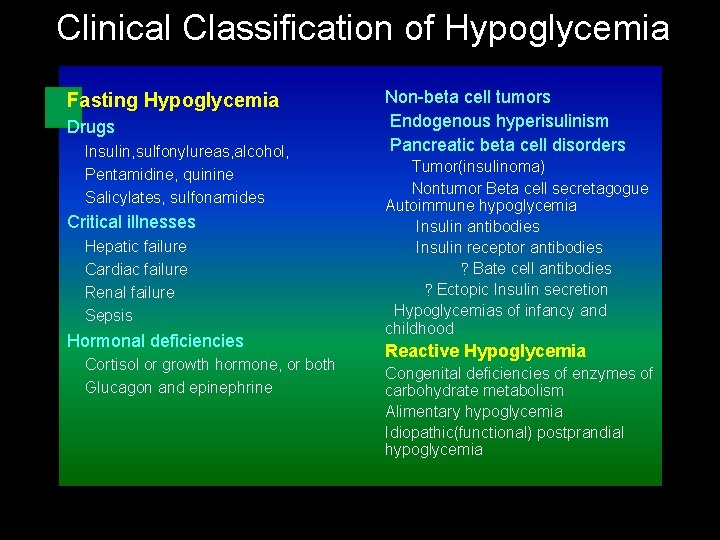
Clinical Classification of Hypoglycemia Fasting Hypoglycemia Drugs Insulin, sulfonylureas, alcohol, Pentamidine, quinine Salicylates, sulfonamides Critical illnesses Hepatic failure Cardiac failure Renal failure Sepsis Hormonal deficiencies Cortisol or growth hormone, or both Glucagon and epinephrine Non-beta cell tumors Endogenous hyperisulinism Pancreatic beta cell disorders Tumor(insulinoma) Nontumor Beta cell secretagogue Autoimmune hypoglycemia Insulin antibodies Insulin receptor antibodies ?Bate cell antibodies ?Ectopic Insulin secretion Hypoglycemias of infancy and childhood Reactive Hypoglycemia Congenital deficiencies of enzymes of carbohydrate metabolism Alimentary hypoglycemia Idiopathic(functional) postprandial hypoglycemia

Fasting Hypoglycemia
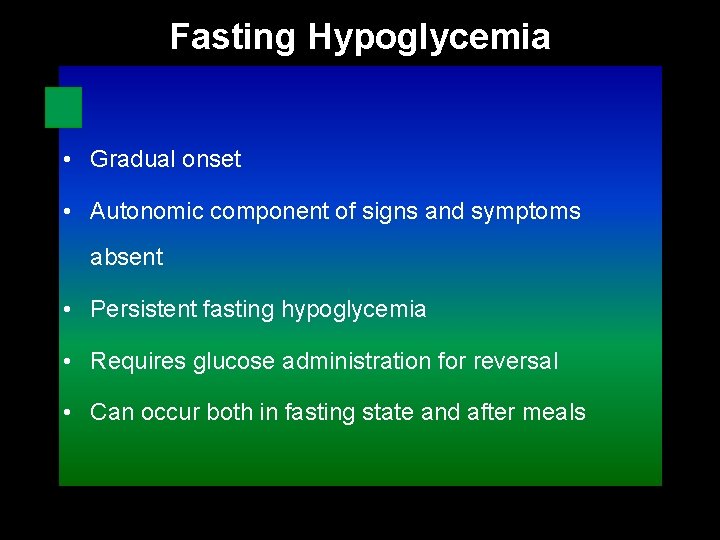
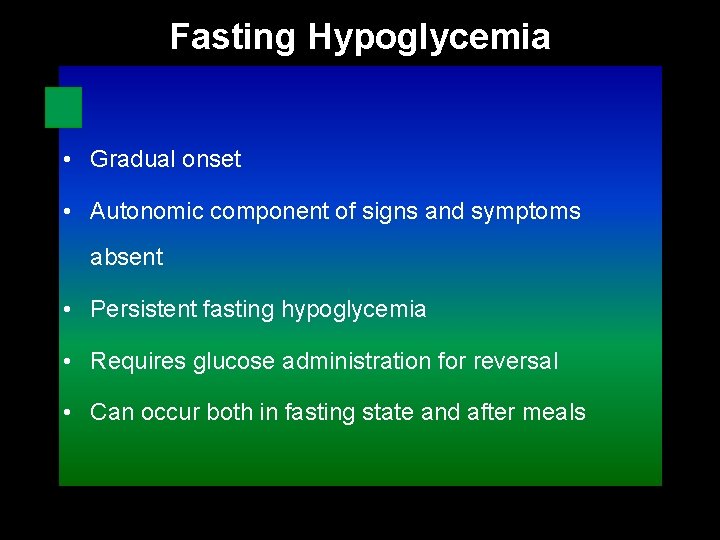
Fasting Hypoglycemia • Gradual onset • Autonomic component of signs and symptoms absent • Persistent fasting hypoglycemia • Requires glucose administration for reversal • Can occur both in fasting state and after meals
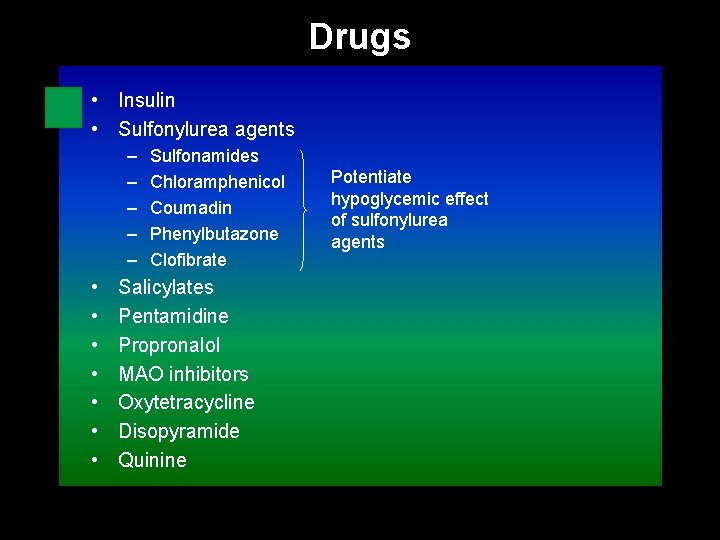
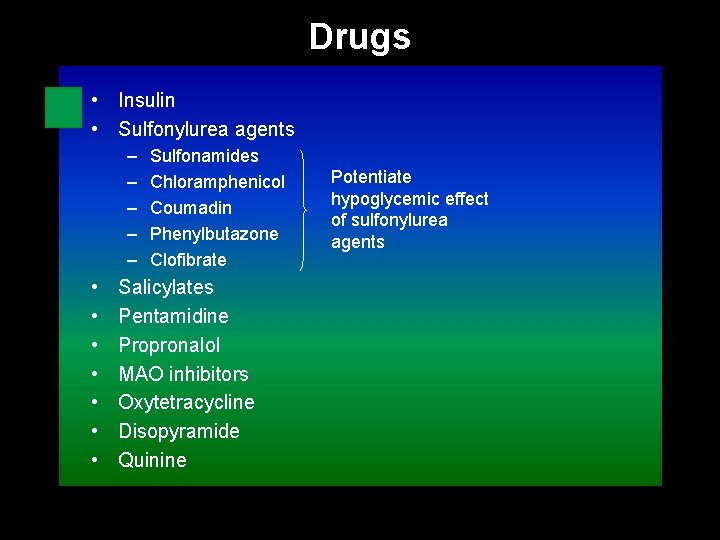
Drugs • Insulin • Sulfonylurea agents – – – • • Sulfonamides Chloramphenicol Coumadin Phenylbutazone Clofibrate Salicylates Pentamidine Propronalol MAO inhibitors Oxytetracycline Disopyramide Quinine Potentiate hypoglycemic effect of sulfonylurea agents
Treatment • Insulin induced hypoglycemia treated with iv glucose • Hypoglycemia often relapses and recovery takes time----- hospitalization – Discontinue offending agent – IV glucose can stimulate further insulin release – Octreaotide or oral diazoxide
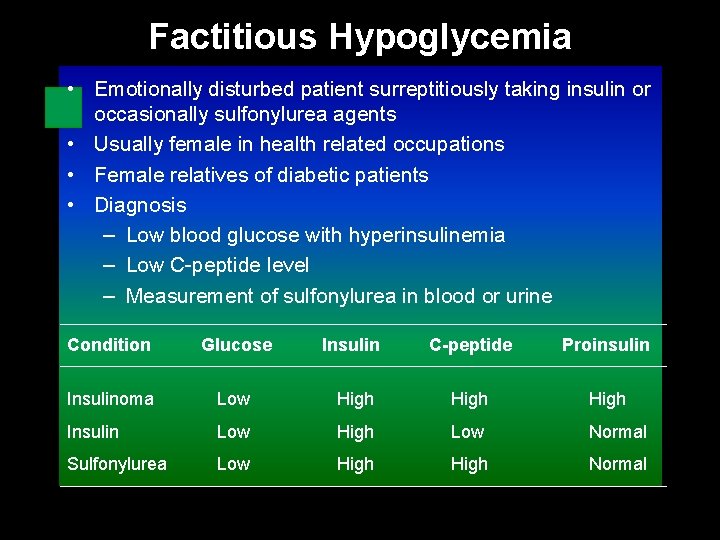
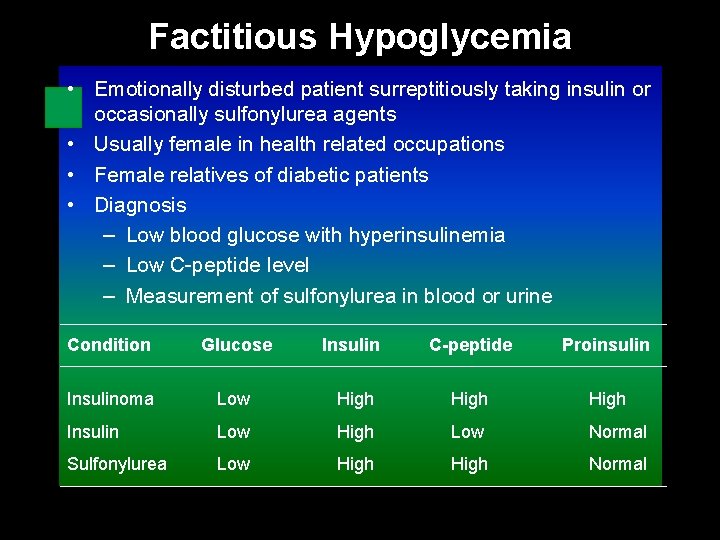
Factitious Hypoglycemia • Emotionally disturbed patient surreptitiously taking insulin or occasionally sulfonylurea agents • Usually female in health related occupations • Female relatives of diabetic patients • Diagnosis – Low blood glucose with hyperinsulinemia – Low C-peptide level – Measurement of sulfonylurea in blood or urine Condition Glucose Insulin C-peptide Proinsulin Insulinoma Low High Insulin Low High Low Normal Sulfonylurea Low High Normal
Ethanol • Inhibits gluconeogenesis in liver • Common in case of restricted food intake – Malnourished chronic alcoholics – Heavy weekend drinkers – Social drinker who miss meals – Children • Neuroglycopenic signs and symptoms predominate • Failure to recognition – Mortality 25% in children, 10 % in adults • Treatment – Glucagon not effective – Good response to iv glucose
Non-β-Cell Tumors • Excess glucose consumption by tumor tissue • Secrete incompletely processed IGF-II – Normally IGF-II binds IGFBP-3 and acid-labile protein and mediates actions of GH • IGHBP-3 and IGF-1 levels decreased • Diagnosis – Other causes should be ruled out – Usually a late manifestation – Low IGF-1 diagnostic – DHEAS elevated in adrenal carcinoma • Treatment – Surgical removal of tumor – Effective radio or chemotherapy – Parenteral glucocorticoids can stimulate gluconeogenesis – Continuous iv glucoıse is not practical
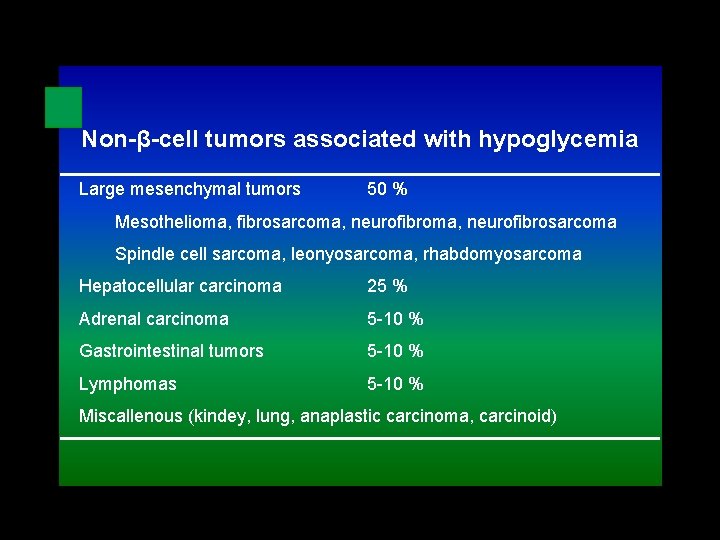
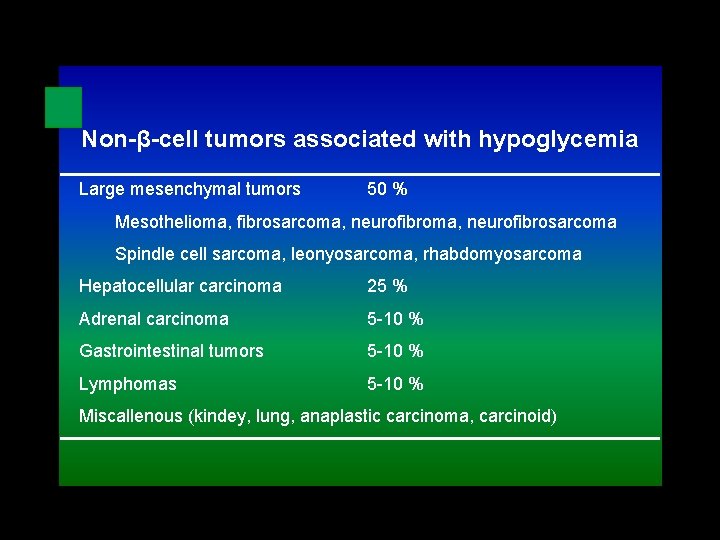
Non-β-cell tumors associated with hypoglycemia Large mesenchymal tumors 50 % Mesothelioma, fibrosarcoma, neurofibrosarcoma Spindle cell sarcoma, leonyosarcoma, rhabdomyosarcoma Hepatocellular carcinoma 25 % Adrenal carcinoma 5 -10 % Gastrointestinal tumors 5 -10 % Lymphomas 5 -10 % Miscallenous (kindey, lung, anaplastic carcinoma, carcinoid)
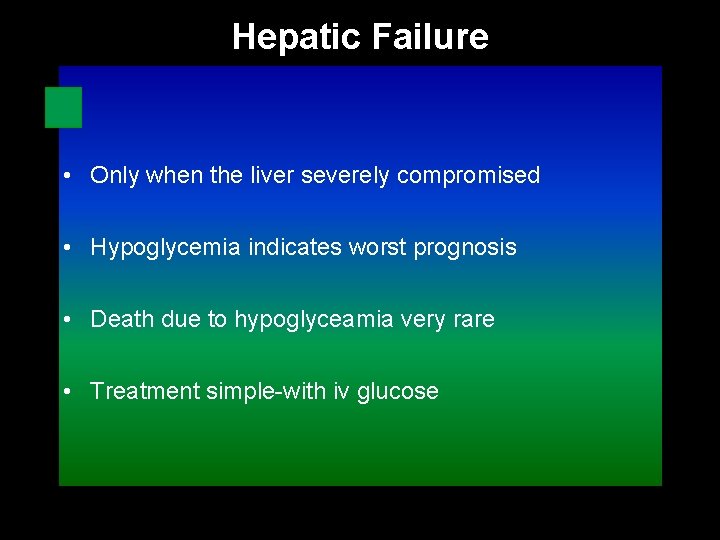
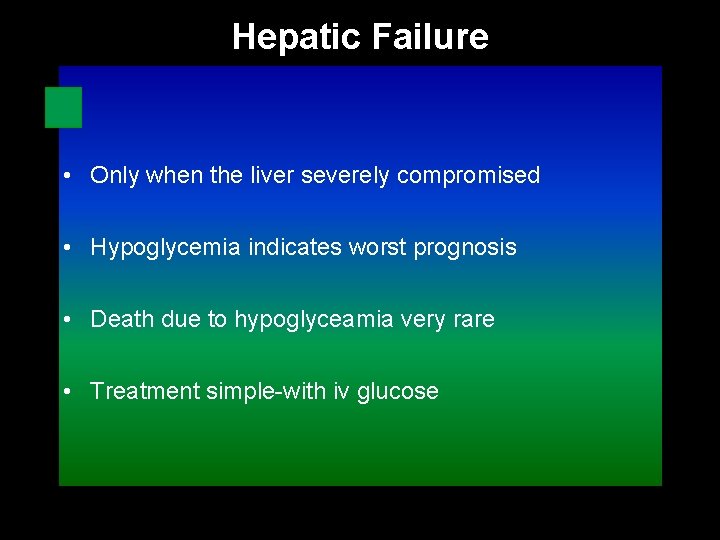
Hepatic Failure • Only when the liver severely compromised • Hypoglycemia indicates worst prognosis • Death due to hypoglyceamia very rare • Treatment simple-with iv glucose
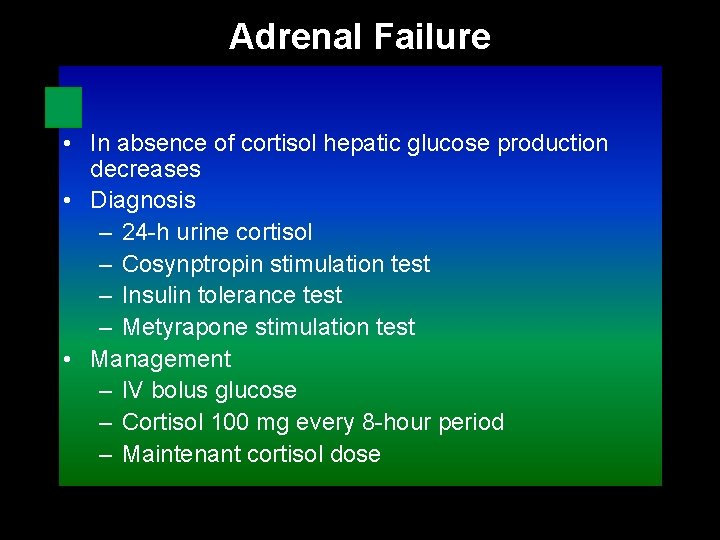
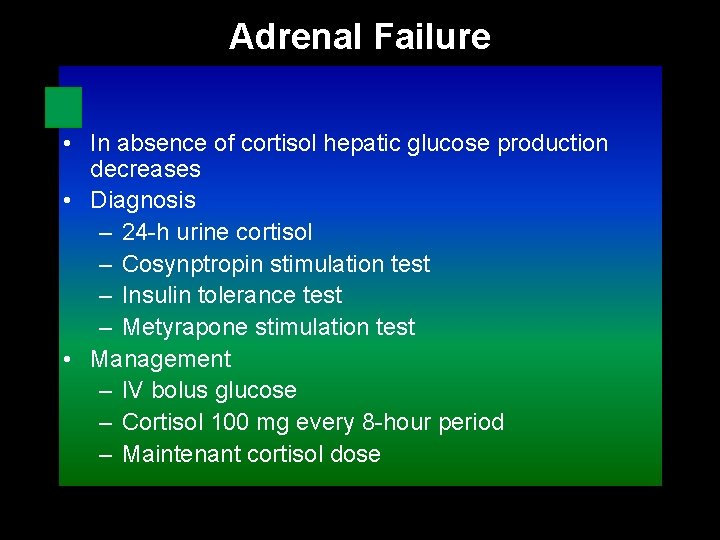
Adrenal Failure • In absence of cortisol hepatic glucose production decreases • Diagnosis – 24 -h urine cortisol – Cosynptropin stimulation test – Insulin tolerance test – Metyrapone stimulation test • Management – IV bolus glucose – Cortisol 100 mg every 8 -hour period – Maintenant cortisol dose
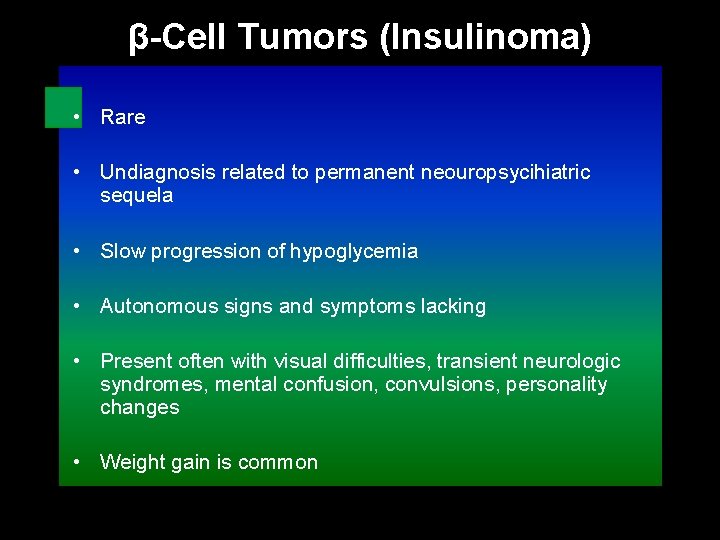
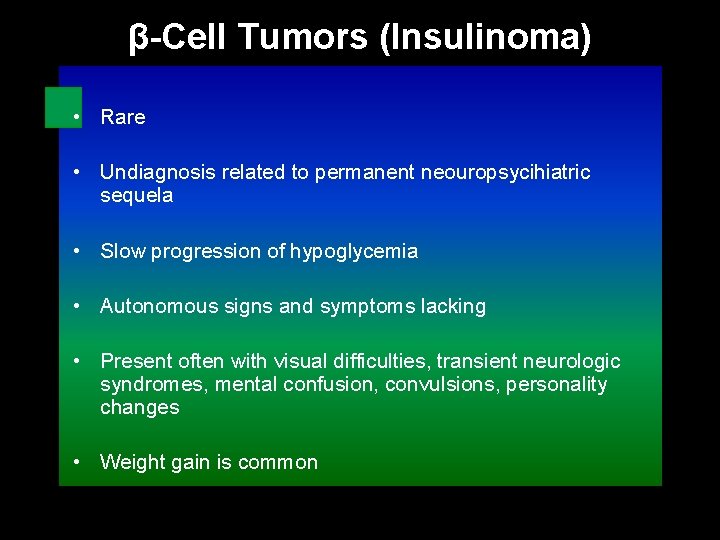
β-Cell Tumors (Insulinoma) • Rare • Undiagnosis related to permanent neouropsycihiatric sequela • Slow progression of hypoglycemia • Autonomous signs and symptoms lacking • Present often with visual difficulties, transient neurologic syndromes, mental confusion, convulsions, personality changes • Weight gain is common
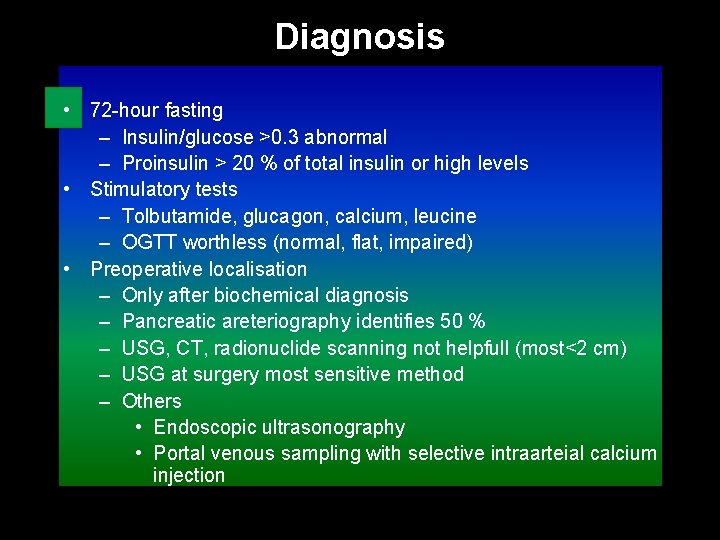
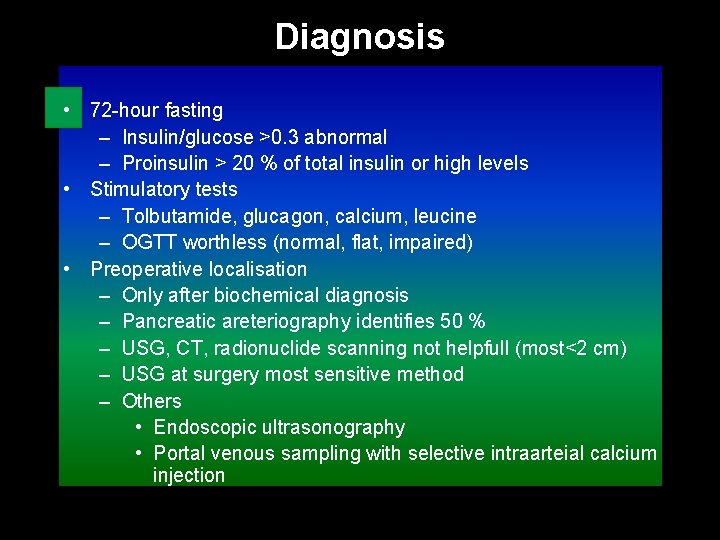
Diagnosis • 72 -hour fasting – Insulin/glucose >0. 3 abnormal – Proinsulin > 20 % of total insulin or high levels • Stimulatory tests – Tolbutamide, glucagon, calcium, leucine – OGTT worthless (normal, flat, impaired) • Preoperative localisation – Only after biochemical diagnosis – Pancreatic areteriography identifies 50 % – USG, CT, radionuclide scanning not helpfull (most<2 cm) – USG at surgery most sensitive method – Others • Endoscopic ultrasonography • Portal venous sampling with selective intraarteial calcium injection
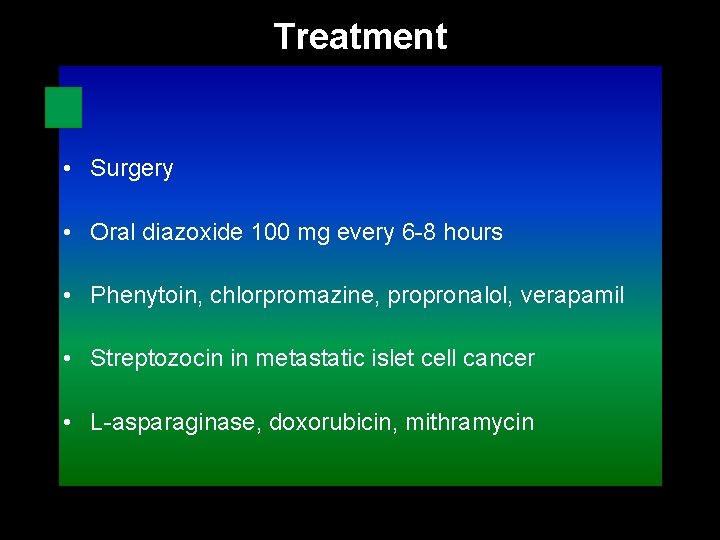
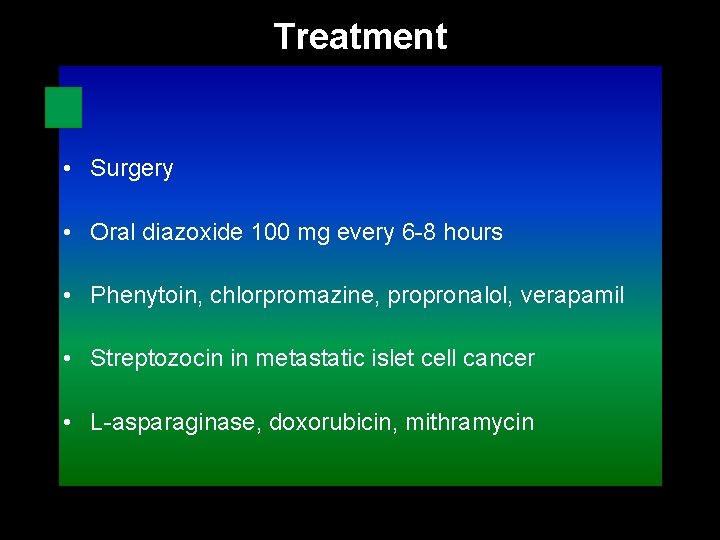
Treatment • Surgery • Oral diazoxide 100 mg every 6 -8 hours • Phenytoin, chlorpromazine, propronalol, verapamil • Streptozocin in metastatic islet cell cancer • L-asparaginase, doxorubicin, mithramycin
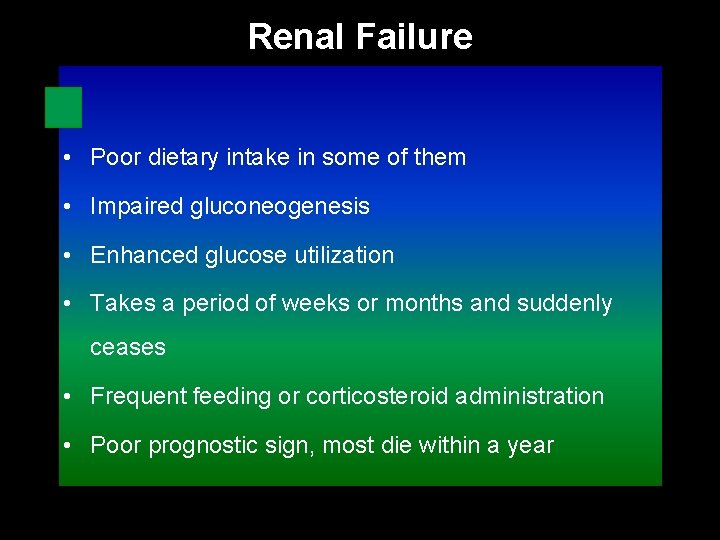
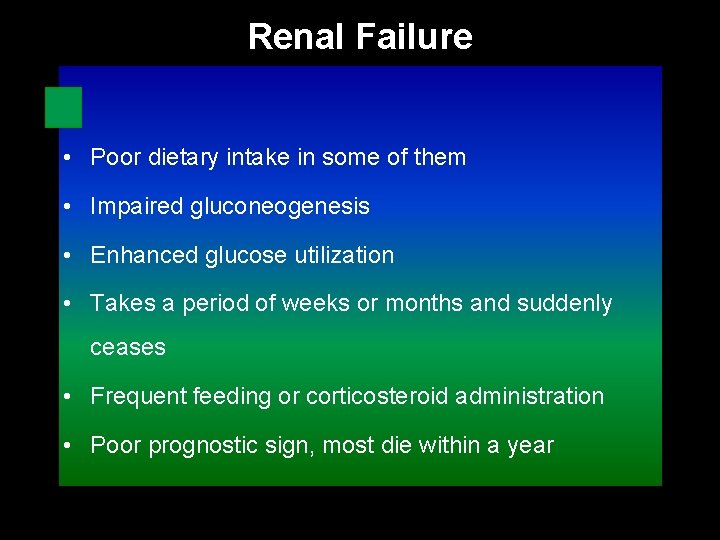
Renal Failure • Poor dietary intake in some of them • Impaired gluconeogenesis • Enhanced glucose utilization • Takes a period of weeks or months and suddenly ceases • Frequent feeding or corticosteroid administration • Poor prognostic sign, most die within a year
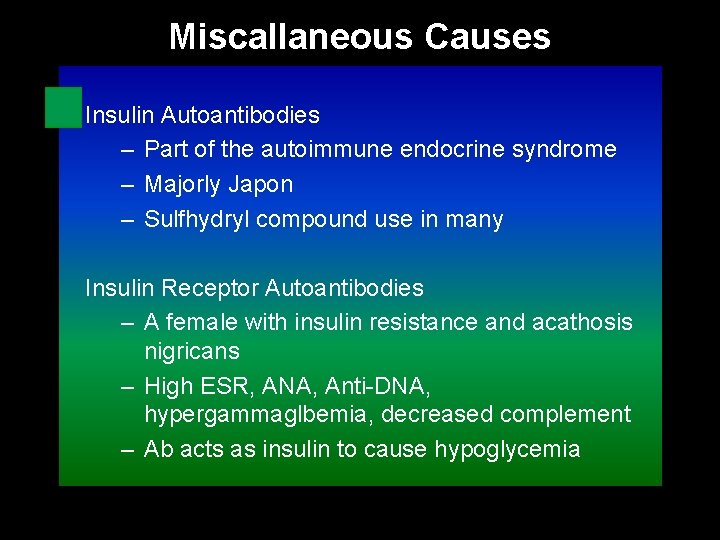
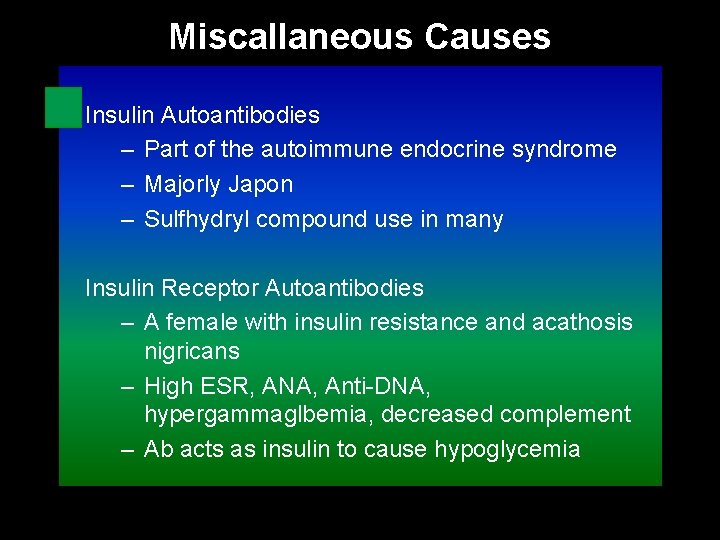
Miscallaneous Causes Insulin Autoantibodies – Part of the autoimmune endocrine syndrome – Majorly Japon – Sulfhydryl compound use in many Insulin Receptor Autoantibodies – A female with insulin resistance and acathosis nigricans – High ESR, ANA, Anti-DNA, hypergammaglbemia, decreased complement – Ab acts as insulin to cause hypoglycemia

Miscallaneous Causes • Sepsis • Falciparum malaria – Glucose utilization by parasite – Pregnant patients and cerebral-involved are prone – Quinine may contribute • Congestive Heart Failure – Secondary to decreased delivery of gluconeogenic substrates to liver – Wight loss, anoreksia, low cardiac output
Fed (Reactive) Hypoglycemia
Fed (Reactive) Hypoglycemia • Symptoms predominantly autonomic • Onset characteristically rapid • Neuroglycopenic component unusual • Transient and normalized by normal hormonal response • Exogenous glucose reverses condition rapidly • Three main causes – Hyperalimentation – Impaired glucose tolerance – Idiopathic reactive hypoglycemia

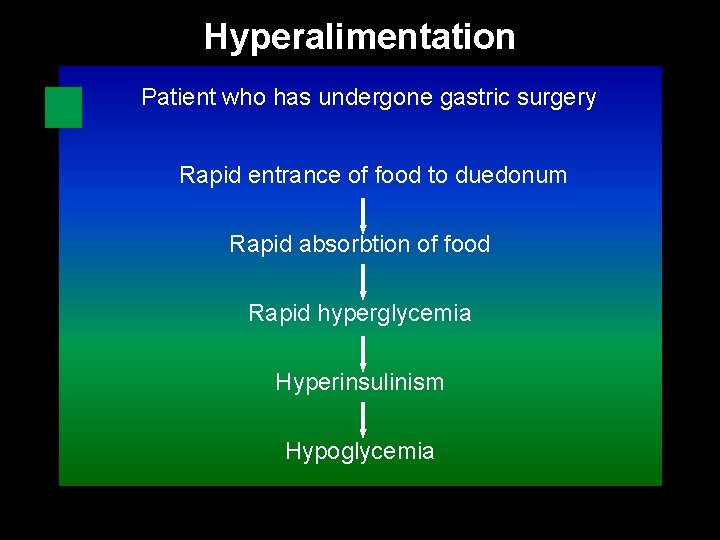
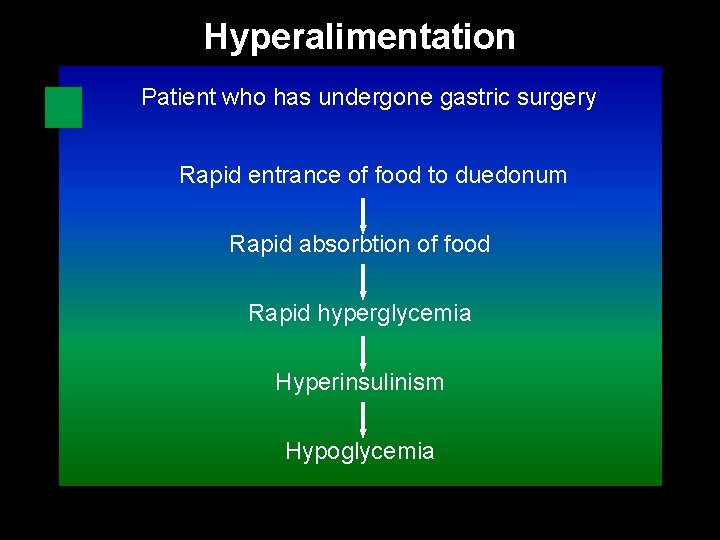
Hyperalimentation Patient who has undergone gastric surgery Rapid entrance of food to duedonum Rapid absorbtion of food Rapid hyperglycemia Hyperinsulinism Hypoglycemia
Impaired Glucose Tolerance • Patient with impaired glucose tolerance test • Late hypoglycemia after 3 hours
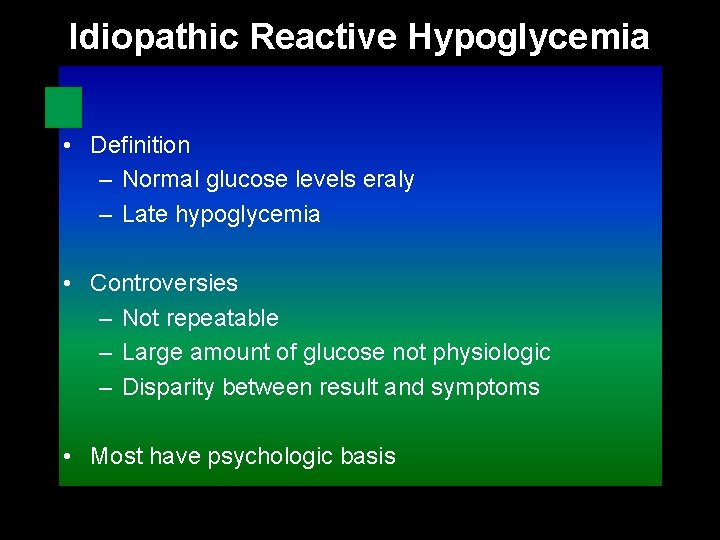
Idiopathic Reactive Hypoglycemia • Definition – Normal glucose levels eraly – Late hypoglycemia • Controversies – Not repeatable – Large amount of glucose not physiologic – Disparity between result and symptoms • Most have psychologic basis
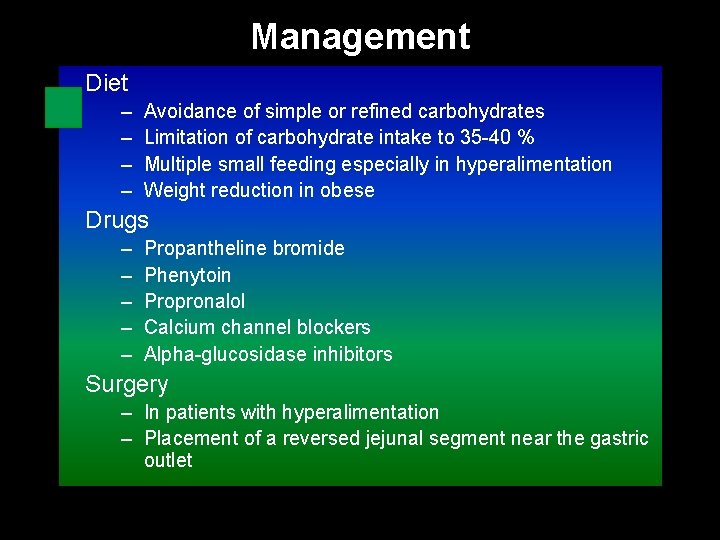
Management Diet – – Avoidance of simple or refined carbohydrates Limitation of carbohydrate intake to 35 -40 % Multiple small feeding especially in hyperalimentation Weight reduction in obese Drugs – – – Propantheline bromide Phenytoin Propronalol Calcium channel blockers Alpha-glucosidase inhibitors Surgery – In patients with hyperalimentation – Placement of a reversed jejunal segment near the gastric outlet

 Masaryk university medical faculty
Masaryk university medical faculty Chronic meningitis
Chronic meningitis Yeditepe üniversitesi hastanesi
Yeditepe üniversitesi hastanesi Coadsys exam yeditepe
Coadsys exam yeditepe Yeditepe coadsys exam
Yeditepe coadsys exam Whipple triad
Whipple triad Insulin action
Insulin action Sulfonylurea drugs mnemonic
Sulfonylurea drugs mnemonic Dka management mnemonic
Dka management mnemonic Nursing care plan for diabetes mellitus slideshare
Nursing care plan for diabetes mellitus slideshare Hypoglycemia factitia
Hypoglycemia factitia Starvation hypoglycemia
Starvation hypoglycemia Hypoglycemia
Hypoglycemia Hypoglycemia cpg
Hypoglycemia cpg Hypoglycemia without diabetes
Hypoglycemia without diabetes Sinan aydın mali müşavir
Sinan aydın mali müşavir Nizamettin aydin
Nizamettin aydin Nizamettin aydin
Nizamettin aydin Aydın kendirci
Aydın kendirci Thede loder
Thede loder Sevil aydın
Sevil aydın Aydın bir türk kadınıyım
Aydın bir türk kadınıyım Xahra franklin
Xahra franklin Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Coordination
Coordination Nizamettin aydin
Nizamettin aydin Aydin marine
Aydin marine Aydın başar
Aydın başar Mega giga tera peta
Mega giga tera peta Nazmi aydın
Nazmi aydın Aydin bal
Aydin bal Aydın kekemelik merkezi
Aydın kekemelik merkezi Medical faculty in novi sad dean
Medical faculty in novi sad dean University of split faculty of maritime studies
University of split faculty of maritime studies Bridgeport engineering department
Bridgeport engineering department Computer science tutor bridgeport
Computer science tutor bridgeport Hubert kairuki memorial university faculty of medicine
Hubert kairuki memorial university faculty of medicine Semmelweis university faculty of medicine
Semmelweis university faculty of medicine King abdulaziz university faculty of medicine
King abdulaziz university faculty of medicine Fsu cs faculty
Fsu cs faculty Faculty of business and economics mendel university in brno
Faculty of business and economics mendel university in brno Singularity executive program
Singularity executive program Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Feup university of porto
Feup university of porto Charles university faculty of humanities
Charles university faculty of humanities Faculty of veterinary medicine cairo university logo
Faculty of veterinary medicine cairo university logo