Diseases of Posterior Pituitary Hasan AYDIN MD Yeditepe




- Slides: 46
Diseases of Posterior Pituitary Hasan AYDIN, MD Yeditepe University Medical Faculty Department of Endocrinology and Metabolism
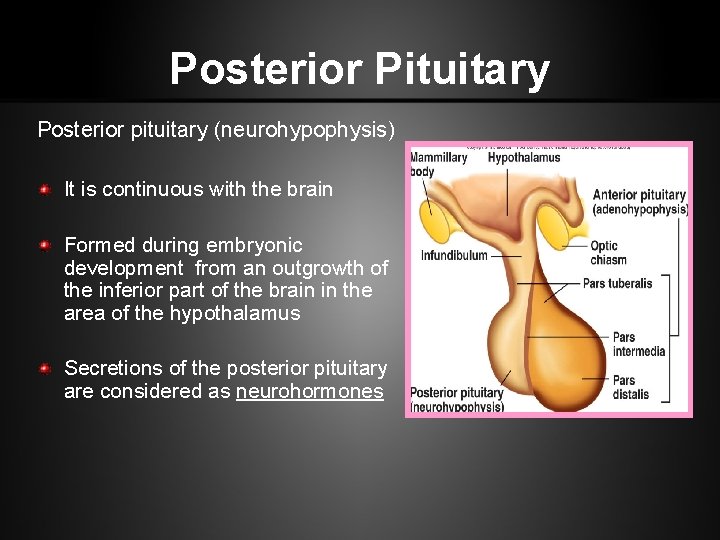
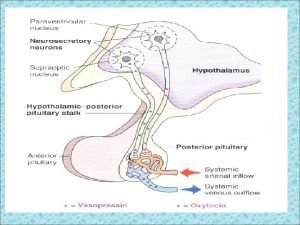
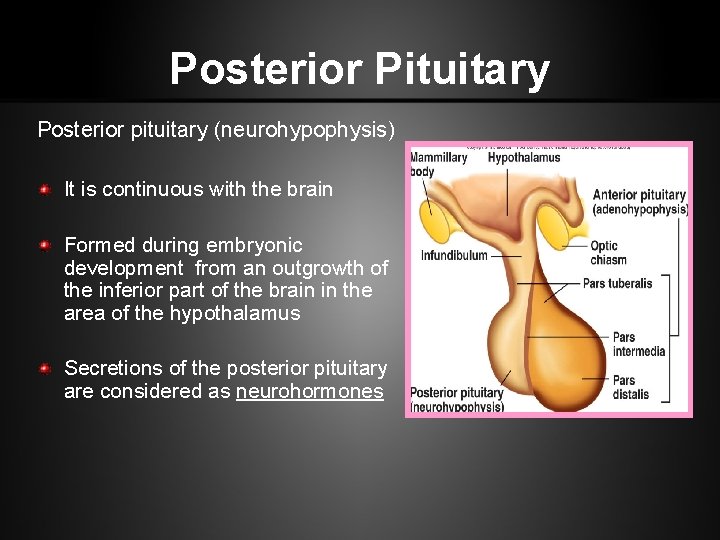
Posterior Pituitary Posterior pituitary (neurohypophysis) It is continuous with the brain Formed during embryonic development from an outgrowth of the inferior part of the brain in the area of the hypothalamus Secretions of the posterior pituitary are considered as neurohormones
Antidiuretic Hormone (ADH) Named so because it prevents the output of large amounts of urine Constricts blood vessels and raises blood pressure when large amounts of urine are released Its primary target tissue is the kidneys, where it promotes the retention of water, and reduces urine volume Urine volume increases within minutes to a few hours in response to increased water intake, and decreases if water is not consumed.
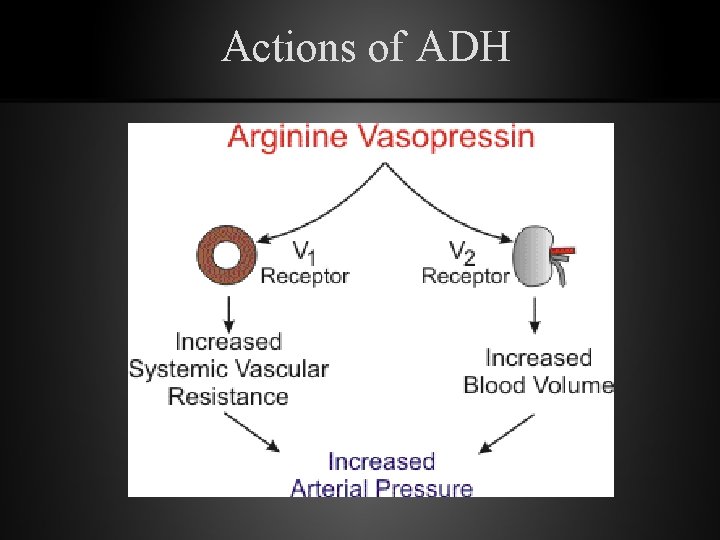
Antidiuretic Hormone (ADH) 1 % increase in osmolality (3 m. Osm/kg H 2 O) stimulates ADH secretion. Serum osmolality above 290 m. Osm/kg H 2 O (N: 285 m. Osm/kg H 2 O) stimulates thirst center. The actions of ADH is mediated by G-protein coupled cell surface receptors V 1, V 2, V 3
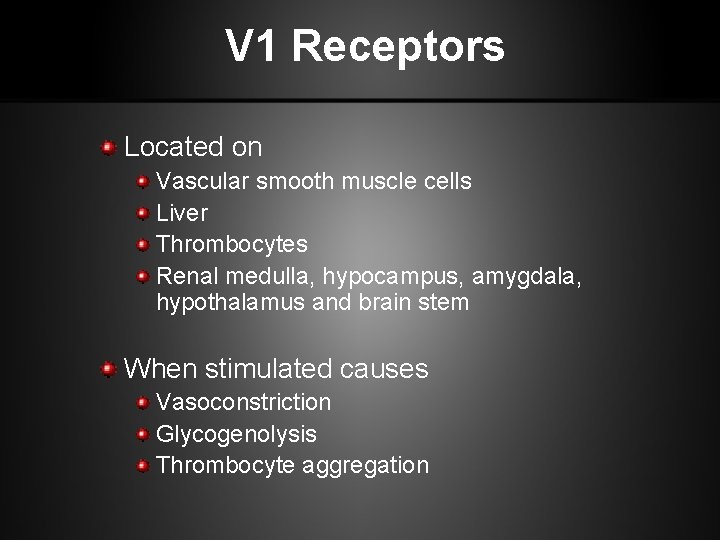
V 1 Receptors Located on Vascular smooth muscle cells Liver Thrombocytes Renal medulla, hypocampus, amygdala, hypothalamus and brain stem When stimulated causes Vasoconstriction Glycogenolysis Thrombocyte aggregation
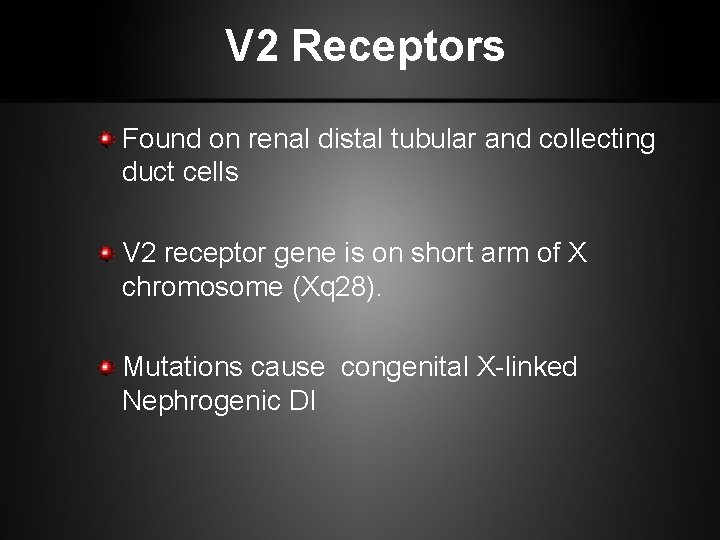
V 2 Receptors Found on renal distal tubular and collecting duct cells V 2 receptor gene is on short arm of X chromosome (Xq 28). Mutations cause congenital X-linked Nephrogenic DI
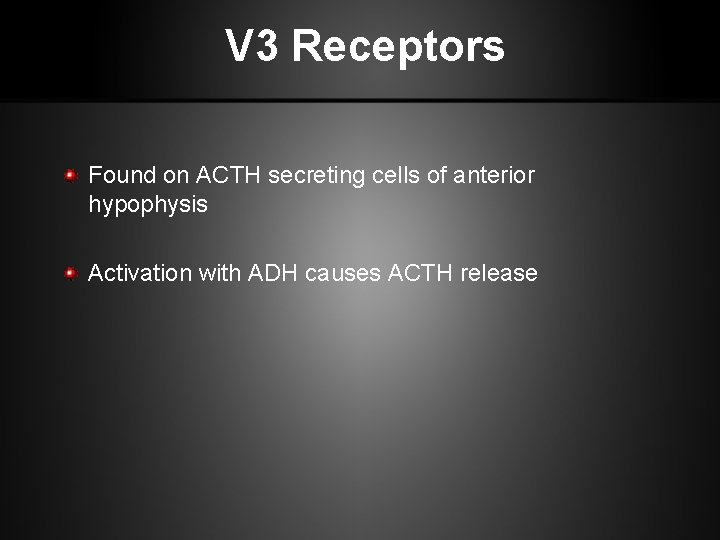
V 3 Receptors Found on ACTH secreting cells of anterior hypophysis Activation with ADH causes ACTH release
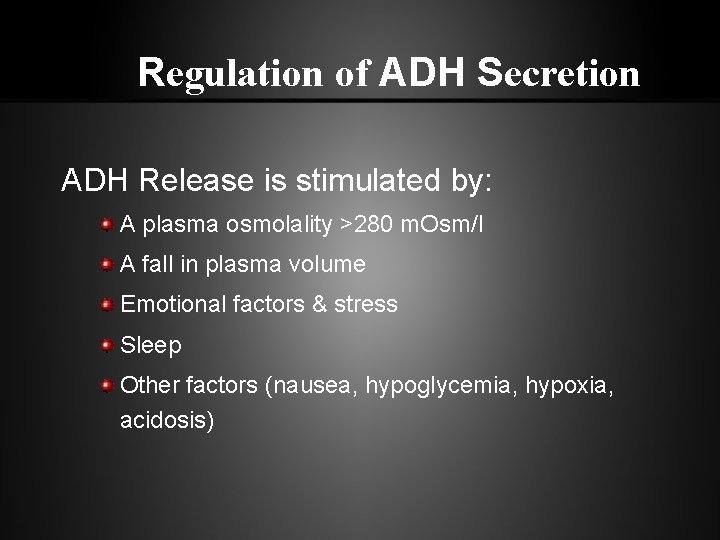
Regulation of ADH Secretion ADH Release is stimulated by: A plasma osmolality >280 m. Osm/l A fall in plasma volume Emotional factors & stress Sleep Other factors (nausea, hypoglycemia, hypoxia, acidosis)
Other ADH Stimulants Cholinergic stimulation Αlpha-adrenergic stimulation Angiotensin II Prostoglandin E Opiates Nicotine Histamine Ether Phenobarbitone
ADH Secretion is Inhibited by: Alcohol Oropharengeal water reflex β-adrenergic stimulants Atrial natriuretic factors (ANF) Phenytoin
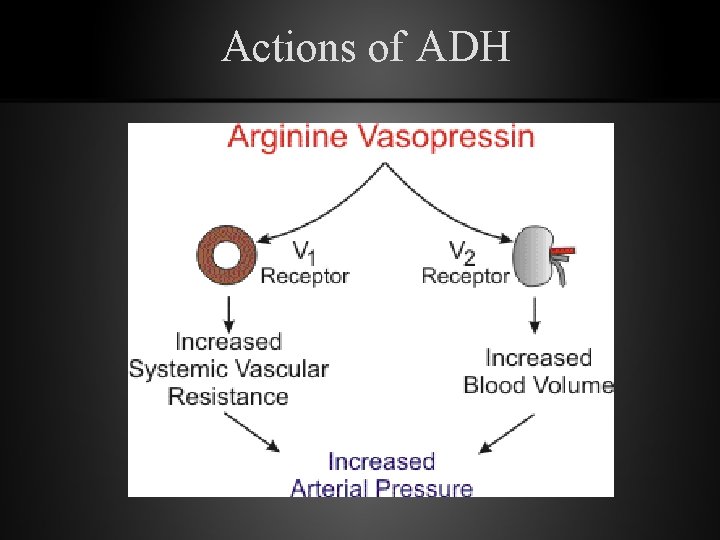
Actions of ADH
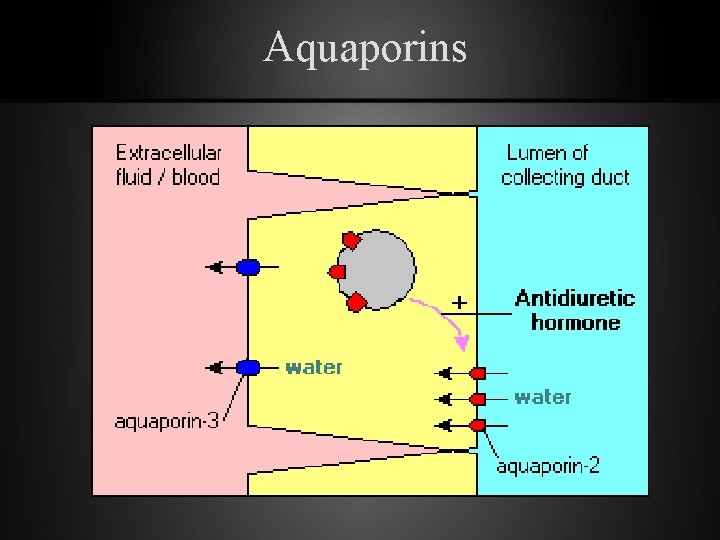
Functions of ADH • Primary Effect – Water reabsorbtion from the distal tubules and collecting ducts of the kidney – Mediated by V 2 receptors through the activation of c. AMP and formation of a spesific protein known as “AQUAPORIN”
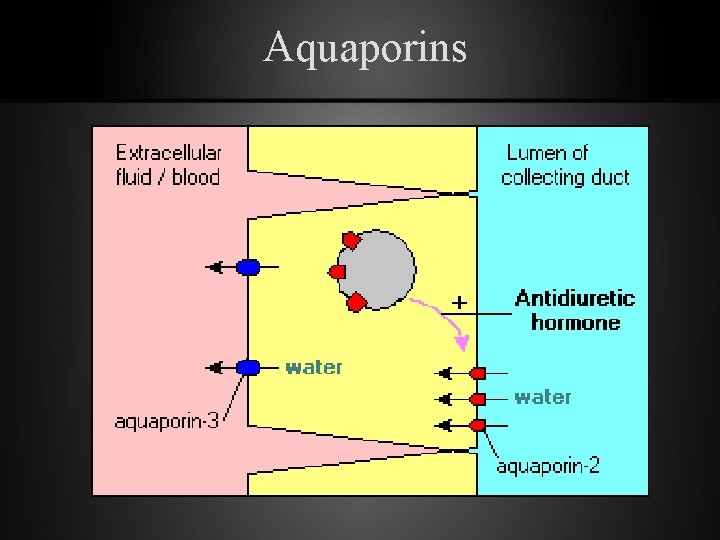
Aquaporins
Actions of ADH • During hypovolemia plasma levels of ADH maintain tissue perfusion • Via V 2 stimulates synthesis and release of factor VIII & Von Willebrand factor
Pathological States
Disorders/diseases resulting from dysfunction – Excess: Syndrome of Inappropriate ADH secretion (SIADH) – Deficiency: Diabetes Insipidus
DIABETES INSIPIDUS
Diabetes Insipidus • Syndrome of posterior pituitary hypofunction • S/S – Increased thirst - polydipsia – Increased urination - polyruia • Results from – ADH (Vasopression) deficiency, which prevents the kidneys from reabsorbing water – Inability to conserve water
Types of Diabetes Insipitus – Cental Diabetes Insipidus – Nephrogenic Diabetes Insipidus – Dispogenic Diabetes Insipidus – Gestational Diabetes Insipidus
Central Diabetes Insipitus (Neurogenic DI) • Results from damage to the pituitary gland • Results in a deficiency of antidiuretic hormone (ADH).
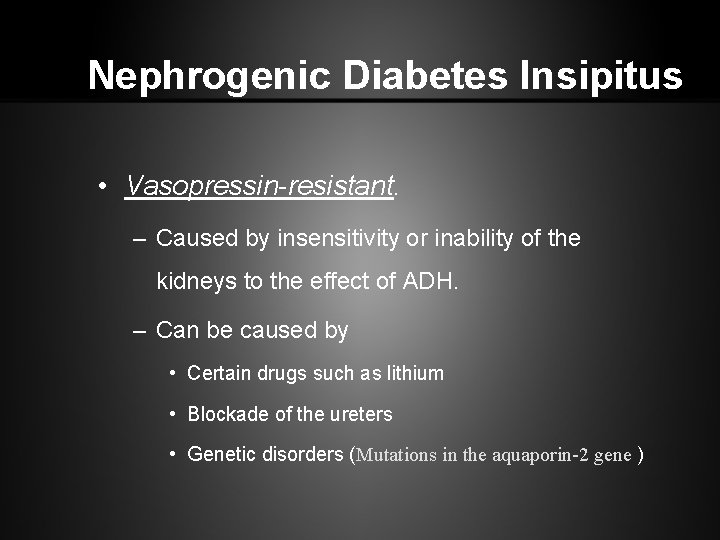
Nephrogenic Diabetes Insipitus • Vasopressin-resistant. – Caused by insensitivity or inability of the kidneys to the effect of ADH. – Can be caused by • Certain drugs such as lithium • Blockade of the ureters • Genetic disorders (Mutations in the aquaporin-2 gene )
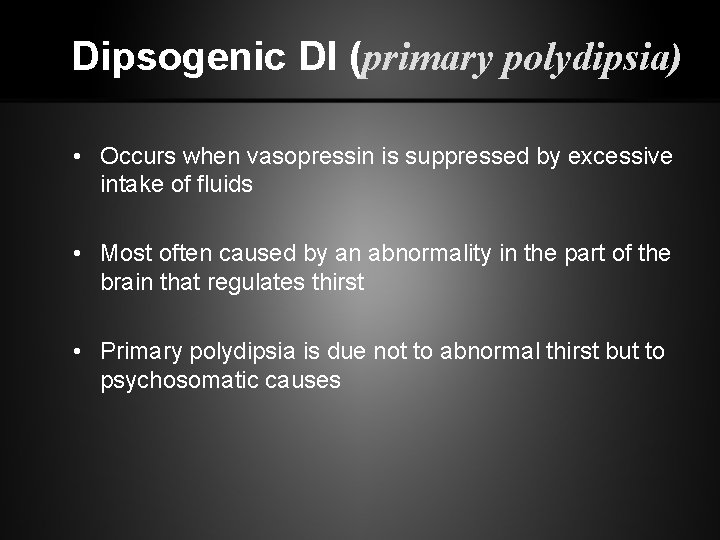
Dipsogenic DI (primary polydipsia) • Occurs when vasopressin is suppressed by excessive intake of fluids • Most often caused by an abnormality in the part of the brain that regulates thirst • Primary polydipsia is due not to abnormal thirst but to psychosomatic causes

Gestational DI • Occurs during pregnancy • An enzyme made by the placenta destroys ADH in the mother • DI often disappear 4 to 6 weeks after delivery • Often recur with subsequent pregnancies
Causes of Diabetes Insipitus
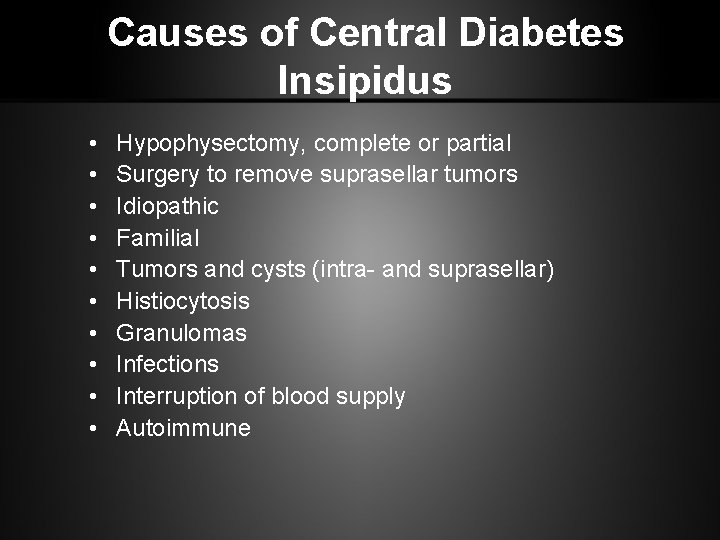
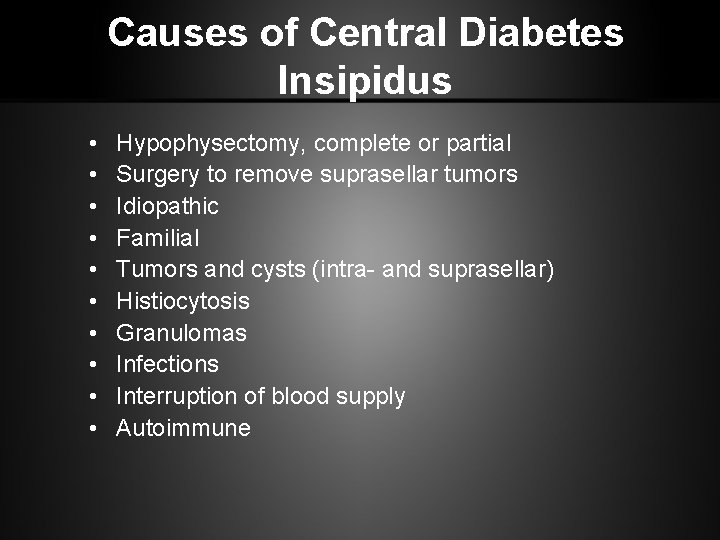
Causes of Central Diabetes Insipidus • • • Hypophysectomy, complete or partial Surgery to remove suprasellar tumors Idiopathic Familial Tumors and cysts (intra- and suprasellar) Histiocytosis Granulomas Infections Interruption of blood supply Autoimmune

Causes of Nephrogenic Diabetes Insipidus • • Chronic renal disease Hypokalemia Protein starvation Hypercalcemia Sickle cell anemia Sjögren's syndrome Drugs, eg, lithium, fluoride, methoxyflurane anesthesia, demeclocycline, colchicine, foscarnet, cidofovir • Congenital defect • Familial
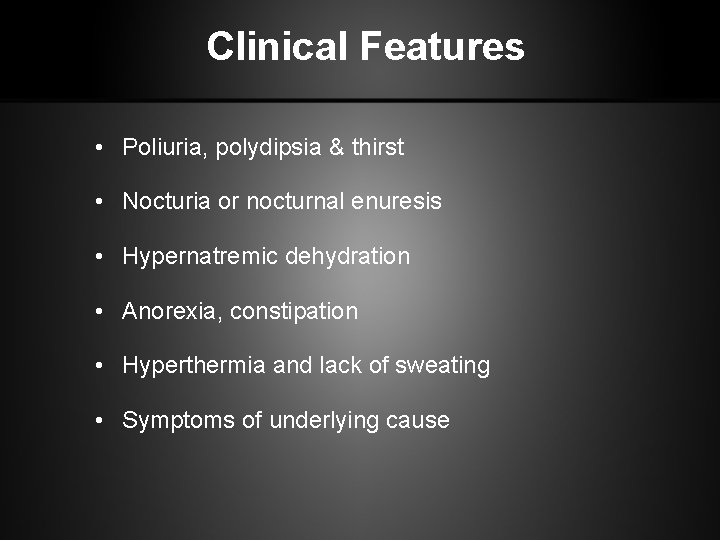
Clinical Features • Poliuria, polydipsia & thirst • Nocturia or nocturnal enuresis • Hypernatremic dehydration • Anorexia, constipation • Hyperthermia and lack of sweating • Symptoms of underlying cause
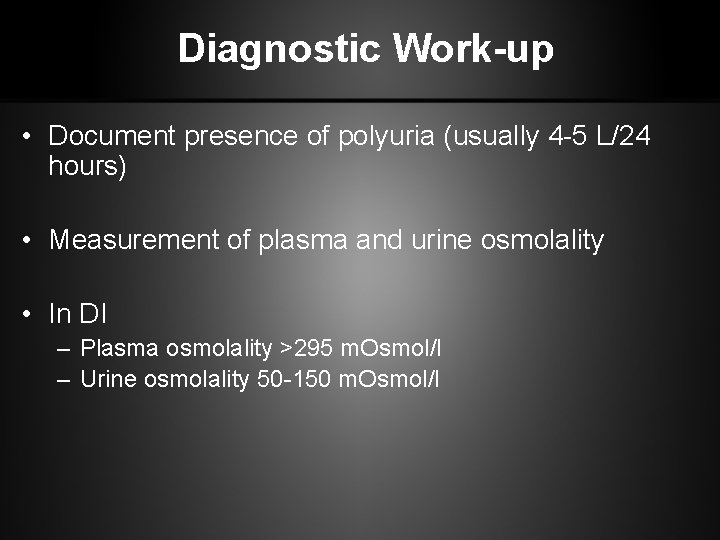
Diagnostic Work-up • Document presence of polyuria (usually 4 -5 L/24 hours) • Measurement of plasma and urine osmolality • In DI – Plasma osmolality >295 m. Osmol/l – Urine osmolality 50 -150 m. Osmol/l
Water Deprivation Test • Useful in patients with partial ADH deficiency • Differentiate DI from primary polydipsia
Water Deprivation Test • Should be done in the morning under supervision • Weigh hourly and measure plasma and urine osmolality every 2 hours • In pts with DI plasma but not urine osmolality rises, U/P osm ratio < 1. 5 • Testing can proceed if urinary osmolality stabilized for 3 samples and 3% wt loss is noted • At the end of the test ADH given (20 mg DDAVP intranasally or 2 mg im) and fluid intake allowed • Concentration of dilute urine confirms central DI and failure suggests nephrogenic causes

Differential Diagnosis • Psychogenic polidipsia • Medullary cystic disease • Drugs (Lithium, diuretics) • Osmotic diuresis (DM) • Hypercalcemia, hypokalemia • Postobstructive diuresis (pyelonefritis, renal tubular acidosis, sickle cell anemia) • Hyperthyroidism
Treatment • Desmopressin (DDAVP): – – – A synthetic analogue Longer duration of action (8 -10 h vs 2 -3 h) More potent ADH activity 3000 x greater than pressor activity Usually given intranasally but sc and oral administration possible
Treatment of Nephrogenic DI • • • Provision of adequate fluids and calorie Low sodium diet Diuretics High dose of DDAVP Correction of underlying cause Drugs (Indomethacin, Chlorprooramide, Clofibrate & Carbamazepine)
Syndrome of Inapproriate Secretion of ADH (Posterior Pituitary Hypersecretion)
SIADH occurs: • When there is too much vasopression (ADH) with inappropriate water retention and decreased blood Na levels
Syndrome of Inappropriate Antidiuretic Hormone Secretion SIADH • Results from – – – Inability to produce & secrete dilute urine Water retention Increased extra cellular fluid volume Hyponatremia Diseases that affect the hypothalamus
Etiology • 1. Central Nervous System Diseases – Menengitis, Ensephalitis, Abcess, Trauma, – Hypoxic ischemic state, Tumor, – Guillain Barre Syndrome, – Ventriculo- atrial shant obstruction, – Acute intermittant porfiria, – Sinus thrombosis, – Hemorrhagia (Intracerebral, subarachnoid).
2. Respiratory system diseases Pneumonia, aspergillosis, tbc, Positive pressure ventilation, Pneumotorax, atelectasia, astma, cystic fibrosis, 3. Malignancy, Thymoma, Lymphoma, Ewing sarcoma, Duedonum, Pancreas, Ureter, Prostate, Baldder and Bronchogenic carcinoma, 4. Drugs eg. vincristin, 5. Myxedema 6. Idiopathic.
SIADH Increased secretion of AVP causes euvolemic hyponatremia. This causes abnormal thirst and intake of excess water leading to accumulation of water and at the end dilutional hyponatremia. As a result, serum Na decreased. urinary excreation of Na increased. urine density and osmolality increased.
Clinical Findings • Anorexia, apathy, confusion, headache, weakness, cramps in abdominal and extremity muscles , nausea, vomiting, abdominal floating • Neurological signs include slowness in DTR, pathological reflexes, in severe cases convulsions and coma.
Dx of SIADH • The following criteria should be fulfilled before a diagnosis of SIADH can be made: – persistent excretion of concentrated urine with no reason for ADH release – normal renal and adrenal function – no edema or hypovolaemia should be present – the urine osmolarity should be greater than the serum osmolarity
Lab Assessment in SIADH • Elevated urine sodium levels and specific gravity reflect an increased concentration of the urine • Serum sodium levels are decreased, often as low as 110 m. Eq/L (normal serum sodium 135 -145 m. Eq/L) due to extracellular volume expansion and increased Na excretion • Fluid retention causes changes in both plasma and urine osmolality • Plasma osmolality is decreased, and the urine is hyperosmolar in relation to the plasma
SIADH Treatment • Water Restriction is the cornerstone of treatment • Decreased water intake allows serum sodium level to rise normally. • The maximum amount of water that pt with SIADH are allowed to drink is just slightly more that the amount of urine they produce • Pt must have regular serum sodium measurements to ensure that the water restriction has been effective • Dehydration- The most concerning potential side effect from treatment is dehydration.
SIADH Treatment • • Restrict fluid intake (800 -1000 cc/day) Daily weight Strict I & O Monitor urine specific gravity 0. 9 NS infusion(to raise the serum Na level if water intoxication is severe) • Monitor for hyponatremia • Furosemide may be admin to block circulatory overload • Drugs-demeclocyclin HCL & lithium-may be admin to block renal response to ADH, intereferes with action of ADH • Drugs - Phenytoin - inhibits ADH release • Surgery & Chemo -to remove or destroy neoplasms that may be the underlying cause of this syndrome
SIADH Treatment • Demeclocycline (Declomycin) • Lithium • Used for: – Excess secretion of ADH or SIADH • Action: – Inhibits ADH action in kidney – Blocks renal response to ADH, interferes with action of ADH • Therapeutic outcome: – Decreased urine specific gravity

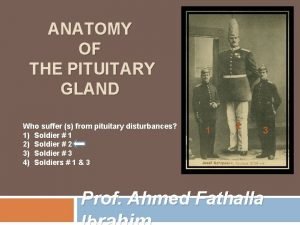
 Posterior pituitary
Posterior pituitary Dwrfism
Dwrfism Difference between anterior and posterior pituitary
Difference between anterior and posterior pituitary Origin of posterior pituitary gland
Origin of posterior pituitary gland Posterior pituitary
Posterior pituitary Difference between anterior and posterior pituitary
Difference between anterior and posterior pituitary Pancreas artery
Pancreas artery Pakigri
Pakigri Coadsysexam yeditepe
Coadsysexam yeditepe Coadsys exam
Coadsys exam Aydın kendirci
Aydın kendirci Mega giga tera peta
Mega giga tera peta Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Sinan aydın ymm
Sinan aydın ymm Package diagram
Package diagram Sevil aydın
Sevil aydın Thede loder
Thede loder Nazmi aydın
Nazmi aydın Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Aydin marine
Aydin marine Aydın bir türk kadınıyım
Aydın bir türk kadınıyım Aydin bal
Aydin bal Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Nizamettin aydin
Nizamettin aydin Aydın başar
Aydın başar Bushra hasan
Bushra hasan Aydın kekemelik merkezi
Aydın kekemelik merkezi Ilknur aydın avcı
Ilknur aydın avcı Pituitary gland hormones
Pituitary gland hormones Blood supply of pituitary gland
Blood supply of pituitary gland Diaphragm sella
Diaphragm sella Endocrine organ
Endocrine organ Anterior pituitary gland
Anterior pituitary gland Subdivision of pituitary gland
Subdivision of pituitary gland Pituitary
Pituitary Endocrine organ
Endocrine organ Hypothalamohypophyseal
Hypothalamohypophyseal Propothiouracil
Propothiouracil N
N Endocrine organ histology
Endocrine organ histology Dopamine agonists
Dopamine agonists Brainstem glioma
Brainstem glioma Pituitary gland and pineal gland spiritual
Pituitary gland and pineal gland spiritual What is the name
What is the name Pituitary fossa
Pituitary fossa Pituitary gland
Pituitary gland