Thyroid Function Tests Hasan AYDIN MD Yeditepe University




- Slides: 34
Thyroid Function Tests Hasan AYDIN, MD Yeditepe University Medical Faculty Endocrinology and Metabolism
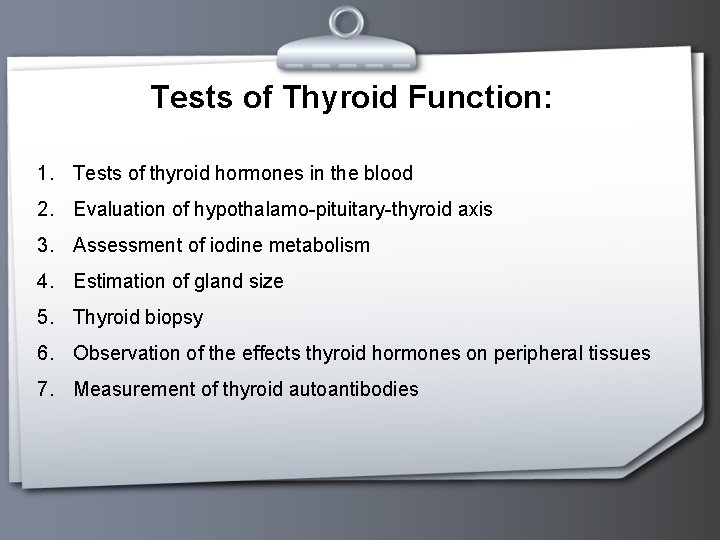
Tests of Thyroid Function: 1. Tests of thyroid hormones in the blood 2. Evaluation of hypothalamo-pituitary-thyroid axis 3. Assessment of iodine metabolism 4. Estimation of gland size 5. Thyroid biopsy 6. Observation of the effects thyroid hormones on peripheral tissues 7. Measurement of thyroid autoantibodies
Tests of Thyroid Hormones in Blood p Total serum T 4 p Free T 4 level p Total serum T 3 p FT 4 -I p FT 3 and r. T 3 p Thyroglobulin
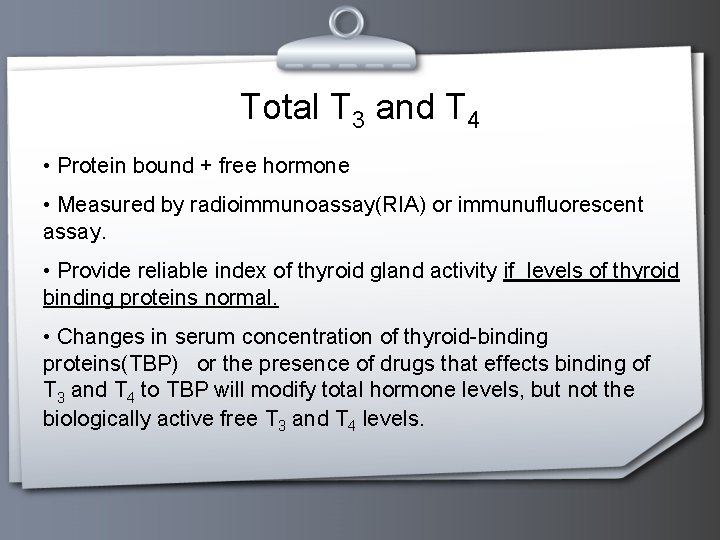
Total T 3 and T 4 • Protein bound + free hormone • Measured by radioimmunoassay(RIA) or immunufluorescent assay. • Provide reliable index of thyroid gland activity if levels of thyroid binding proteins normal. • Changes in serum concentration of thyroid-binding proteins(TBP) or the presence of drugs that effects binding of T 3 and T 4 to TBP will modify total hormone levels, but not the biologically active free T 3 and T 4 levels.
Total T 3 (Normal: 95 -190 ng/dl) • The T 3 is increased in almost all cases of hyperthyroidism and usually goes up before the T 4 does. • T 3 is a more sensitive indicator of hyperthyroidism than the Total T 4. • In hypothyroidism the T 3 is often normal even when the T 4 is low. • The T 3 is decreased during acute illness and starvation, and is affected by several medications including beta blocker, steroids and amiodarone.
Total T 4 (Normal: 5 -12 ng/dl) • In circulation most T 4 (99. 8%) is bound to specific plasma proteins. TBG (60 -75%), Prealbumin/transthyretin 15 -30%, albumin 10% • In the absence of thyroid dysfunction, abnormal results are usually due to an abnormal level of serum TBG. • The TT 4 level may not always correspond to the FT 4 concentration • Free hormone is only 0. 03 % of the total.
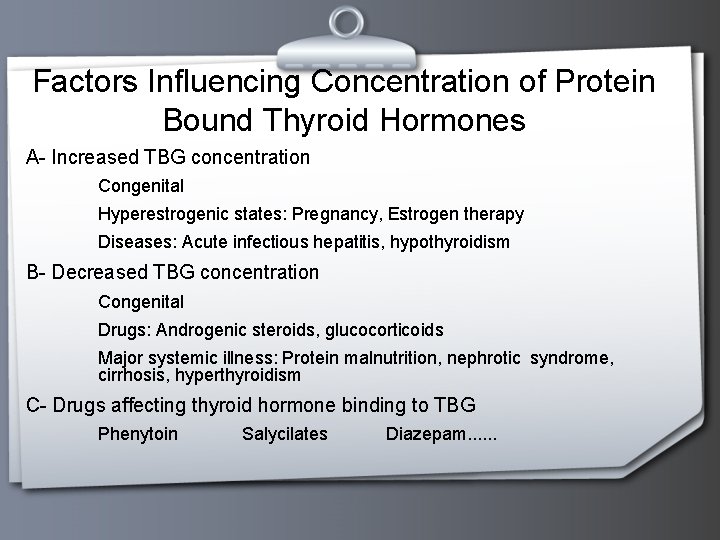
Factors Influencing Concentration of Protein Bound Thyroid Hormones A- Increased TBG concentration Congenital Hyperestrogenic states: Pregnancy, Estrogen therapy Diseases: Acute infectious hepatitis, hypothyroidism B- Decreased TBG concentration Congenital Drugs: Androgenic steroids, glucocorticoids Major systemic illness: Protein malnutrition, nephrotic syndrome, cirrhosis, hyperthyroidism C- Drugs affecting thyroid hormone binding to TBG Phenytoin Salycilates Diazepam. . .

Free T 3 and Free T 4 Free T 3 (N: 0. 2 - 0. 52 ng/dl) and T 4 hormone levels can be measured directly by dialysis method by chemiluminescent assay estimated using free thyroxine index Free T 4 (Normal: 0. 9 - 2 ng/dl) • The FT 4 measures the concentration of free thyroxine, the only biologically active fraction in the serum. • The free thyroxine is not affected by changes in concentrations of binding proteins Thus such conditions as pregnancy, or estrogen androgen therapy do not affect the FT 4.
Thyroid Stimulating Hormone • A glycoprotein secreted by the anterior pituitary • Structurally similar to FSH, LH and chorionic gonadotropin (h. CG) • Composed of two dissimilar non-covalently bound α-subunit and β-subunits • The α-subunit is hormone non-specific • The β-subunit is distinct for each hormone and confers biological and immunological specificity • Antibodies used in immunoassays of TSH target the β-subunit
Thyroid Stimulating Hormone • Measures the response of the pituitary gland to circulating T 4 and T 3. • Elevated in hypothyroidism due to primary thyroid disease, iodine deficient goiter. • In hyperthyroidism, TSH will be suppressed. • This is probably the most important test that can be performed to assess thyroid function. • Highly sensitive TSH test is available. This method utilizes monoclonal antibodies directed against the beta subunit of the molecule and is therefore specific for TSH.
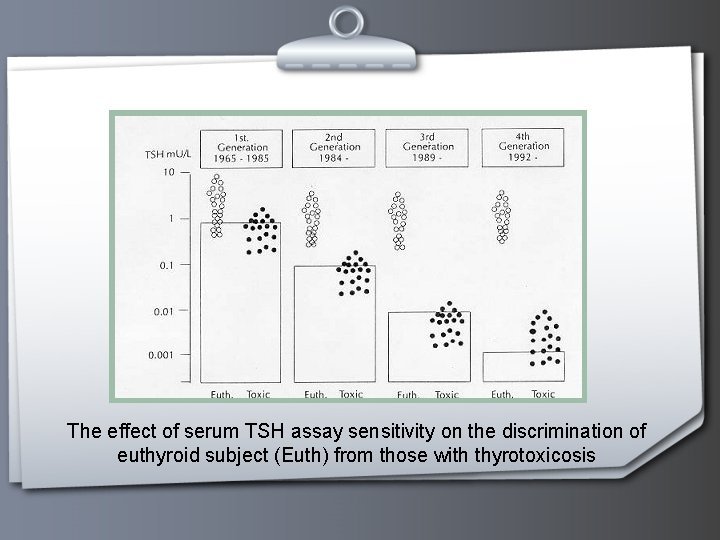
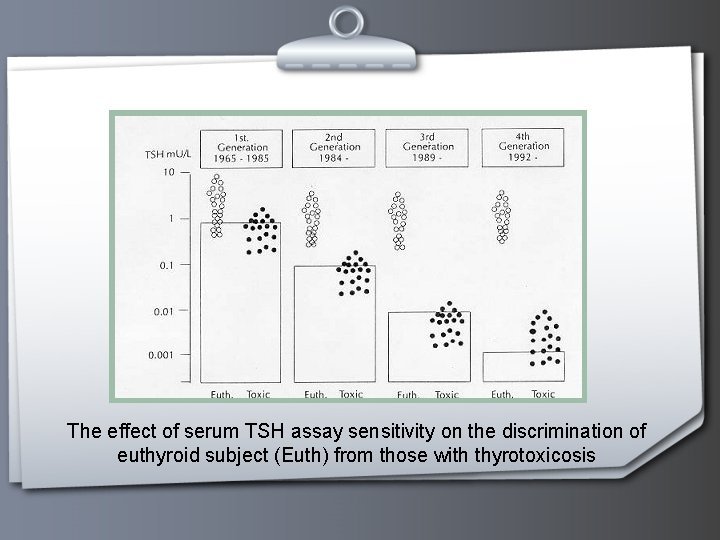
The effect of serum TSH assay sensitivity on the discrimination of euthyroid subject (Euth) from those with thyrotoxicosis
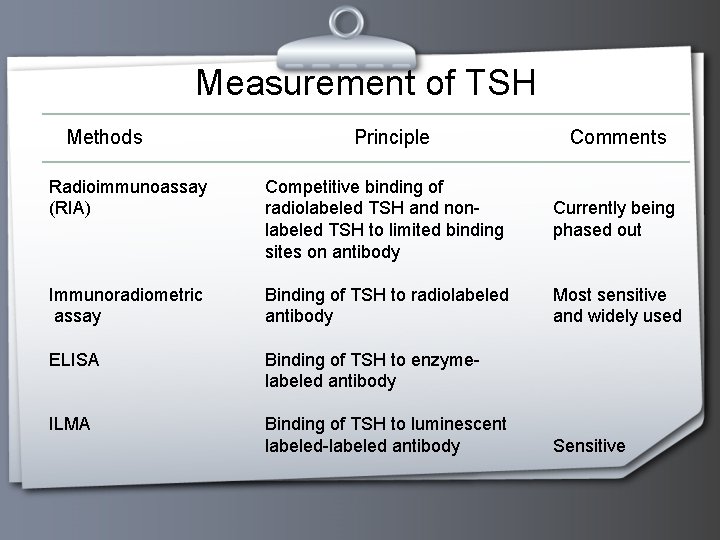
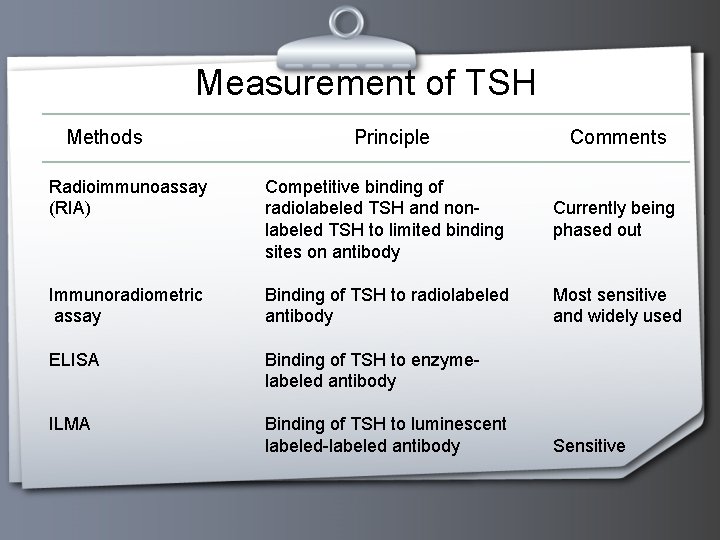
Measurement of TSH Methods Principle Comments Radioimmunoassay (RIA) Competitive binding of radiolabeled TSH and nonlabeled TSH to limited binding sites on antibody Currently being phased out Immunoradiometric assay Binding of TSH to radiolabeled antibody Most sensitive and widely used ELISA Binding of TSH to enzymelabeled antibody ILMA Binding of TSH to luminescent labeled-labeled antibody Sensitive
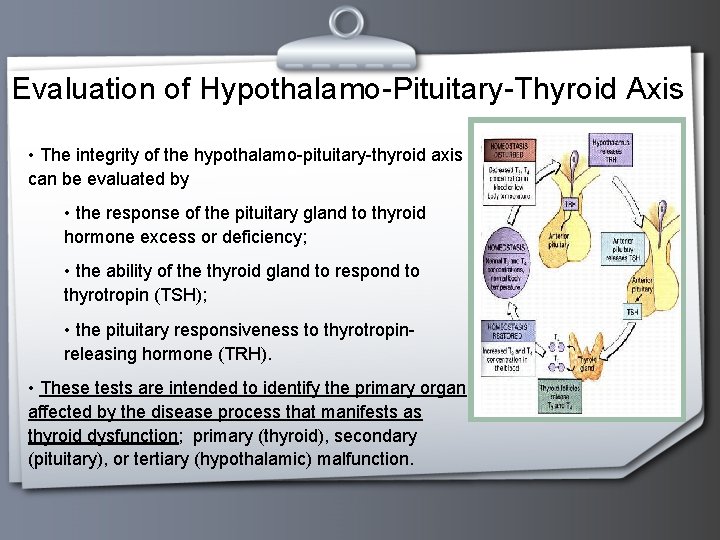
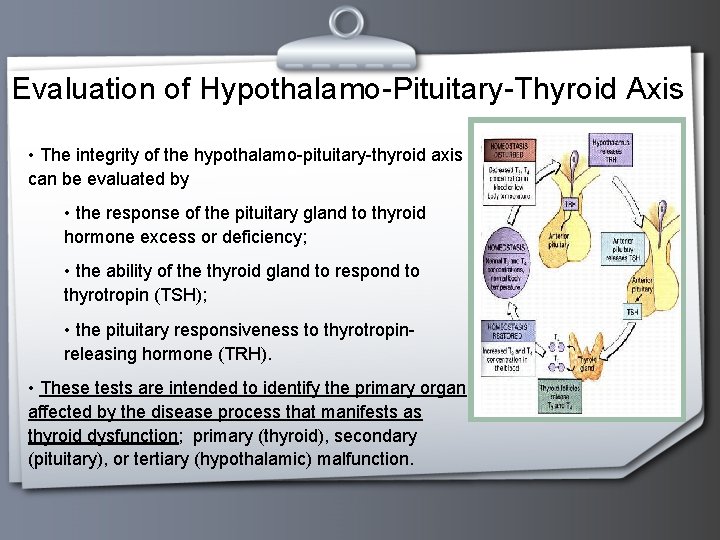
Evaluation of Hypothalamo-Pituitary-Thyroid Axis • The integrity of the hypothalamo-pituitary-thyroid axis can be evaluated by • the response of the pituitary gland to thyroid hormone excess or deficiency; • the ability of the thyroid gland to respond to thyrotropin (TSH); • the pituitary responsiveness to thyrotropinreleasing hormone (TRH). • These tests are intended to identify the primary organ affected by the disease process that manifests as thyroid dysfunction; primary (thyroid), secondary (pituitary), or tertiary (hypothalamic) malfunction.
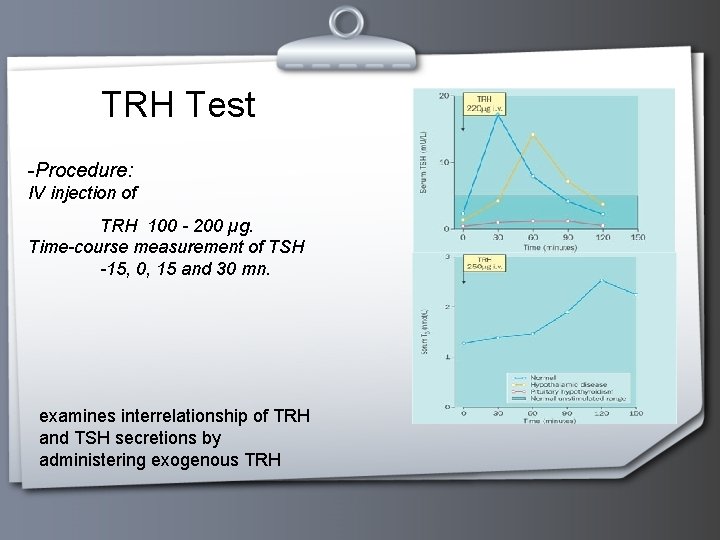
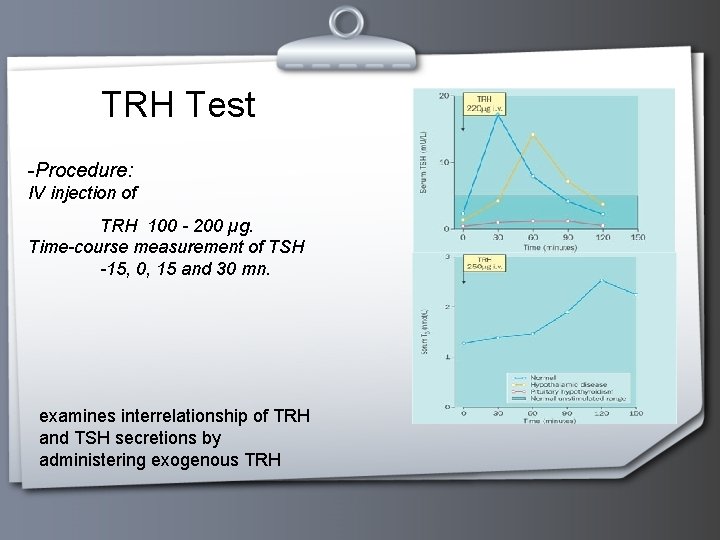
TRH Test -Procedure: IV injection of TRH 100 - 200 µg. Time-course measurement of TSH -15, 0, 15 and 30 mn. examines interrelationship of TRH and TSH secretions by administering exogenous TRH
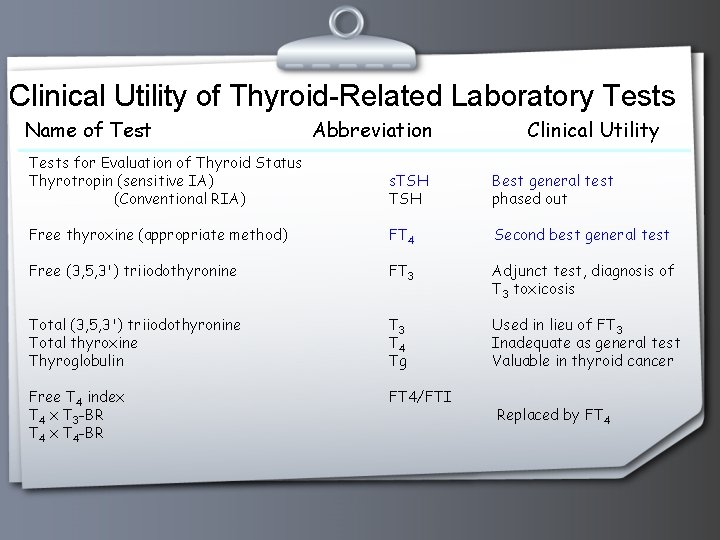
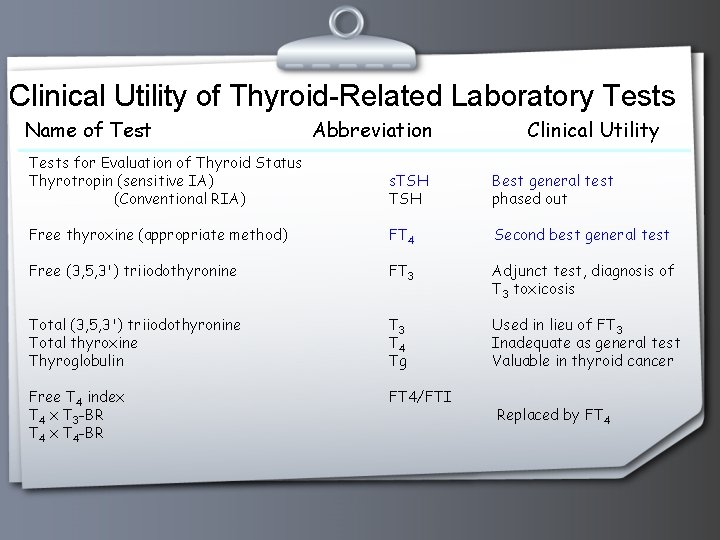
Clinical Utility of Thyroid-Related Laboratory Tests Name of Test Abbreviation Clinical Utility Tests for Evaluation of Thyroid Status Thyrotropin (sensitive IA) (Conventional RIA) s. TSH Best general test phased out Free thyroxine (appropriate method) FT 4 Second best general test Free (3, 5, 3') triiodothyronine FT 3 Adjunct test, diagnosis of T 3 toxicosis Total (3, 5, 3') triiodothyronine Total thyroxine Thyroglobulin T 3 T 4 Tg Used in lieu of FT 3 Inadequate as general test Valuable in thyroid cancer Free T 4 index T 4 x T 3 -BR T 4 x T 4 -BR FT 4/FTI Replaced by FT 4

Thyroglobulin (Tg) p In serum by double antibody immunoassay p The normal range vary with method and laboratory , p Normal range is less than 40 ng/m. L ( < 40 mikrogram/L) in the euthyroid individual p <5 ng/m. L in a thyroidectomized individual. p The major problem endogenous Tg Ab p Spuriously low or spuriously high values.
Thyroglobulin (Tg) Elevations p Graves ' disease p Toxic MNG p Acute or chronic thyroiditis p Papillary or follicular thyroid carcinoma. p Following thyroidectomy and 131 -I therapy, p serum thyroglobulin greater than 10 ng/d. L (> 10 ~g/L) indicates the presence of metastatic disease p rise in a patient with known metastases indicates progression of the disease.
Thyroid Autoantibodies Thyroid peroxidase (TPO) (or antimicrosomal (TMAb) and antithyroglobulin (Tg. Ab) antibodies are measured to confirm or rule out autoimmune thyroid disease. High titers of these antibodies are present in 97 % of patients with Grave’s disease or Hashimoto’s thyroiditis. Not specific for the type of disease. Generally these are measured using RIA, ELISA or IRMA techniques Reported prevalence of thyroid antibodies in population is highly variable ( %2 -30) Thyroid receptor stimulating antibody is characteristic of Grave’s disease (Present in 90%). Helpful in diagnosis of euthyroid Grave’s ophtalmopathy and in predicting possible occurrence of thyroid dysfunction in neonates Thyroid receptor blocking antibody is characteristic of autoimmune thyroid disease
Thyroid peroxidase (TPO) and Antithyroglobulin (Tg. Ab) p Measured to confirm or rule out autoimmune thyroid disease. p High titers of these antibodies are present in 97 % of patients with Grave’s disease or Hashimoto’s thyroiditis. p Not specific for the type of disease. p Generally these are measured using RIA, ELISA or IRMA techniques p Reported prevalence of thyroid antibodies in population is highly variable (2 -30%)
Iodine Metabolism & Biosynthetic Activity p Radioactive iodine uptake p RAIU supression test
RAIU p Radioactive iodine allows assessment of the turnover of iodine by the thyroid gland in vivo. p Iodine-123 is the ideal isotope for this purpose p Administered orally at a dose of 100 -200 mic. Ci, p Radioactivity over the thyroid area is measured with a scintillation counter at 4 or 6 hours and again at 24 hours
RAIU p Vary with the iodide intake. p In areas of low iodide intake and endemic goiter, the 24 -hour RAIU may be as high as 60 -90%. p The normal uptake at 6 hours is 5 -15% and at 24 hours 8 -30%. p In thyrotoxicosis due to Graves' disease or toxic nodular goiter, the 24 - hour RAIU is markedly elevated
RAIU Supression Test p 75 -100 microgram of T 3 in divided doses daily for 5 days p Reduce the 24 -hour RAIU by more than 50% (suppression test). p Failure of the thyroid to suppress on this treatment indicates autonomous thyroid function, as in Graves' disease, or autonomously functioning thyroid nodules.
Thyrotoxicosis with a Very Low Thyroidal RAIU p Subacute thyroiditis p During the active phase of Hashimoto's thyroiditis, p Thyrotoxicosis factitia due to oral ingestion of a large amount of thyroid hormone p As a result of excess iodide intake (amiodarone therapy), inducing thyrotoxicosis in a patient with latent Graves ' disease or multinodular goiter, the low uptake being due to the huge iodide pool; p Struma ovarii p Ectopic functioning metastatic thyroid carcinoma after total thyroidectomy.
Thyroid Imaging p Radionuclide imaging p Radioisotope Scanning p Fluorescent Scanning p Thyroid Ultrasonography p Magnetic Resonance Imaging
Radionuclide Imaging p 123 -Iodine ora. Ily in dose of 200 -300 micro. Ci, scan of the thyroid at 8 -24 hours p Technetium Tc 99 m pertechnetate (99 m. Tc as 4) intravenously in a dose of 1 -10 m. Ci scan is obtained at 30 -60 minutes. p Images can be obtained either a rectilinear scanner or a gamma camera.
Radionuclide Imaging p Both the size and shape of the thyroid gland p The geographic distribution of functional activity in the gland. Functioning thyroid nodules ''hot'' nodules, Non-functioning ones ''cold'' nodules. p The incidence of malignancy in hot nodules is about 1%, but they may become toxic, producing enough hormone to suppress the rest of the gland induce thyrotoxicosis.
Fluorescent Scanning p Advantage of this procedure patient receives no radioisotope gland can be imaged even when it is loaded with iodine ( after IV contrast media) p Disadvantage requires specialized equipment that may not be generally available.

Thyroid Ultrasonography p Thyroid size and nodularity much better detail p Useful for measuring the size of the gland or individual nodules p Evaluating the results of therapy. p Differentiating solid from cystic lesions p Guide the operator to a deep nodule during fine- needle thyroid aspiration biopsy. p Limited to thyroid tissue in the neck, ie, it cannot be used for substernal lesions.
Magnetic Resonance Imaging p Thyroid size and nodularity much better detail p Excellent image of the thyroid gland, including posterior or substernal extension of a goiter or malignancy. p Both transverse and coronal images p Lymph nodes as small as 1 cm p Invaluable for the demonstration of tracheal compression from a large goiter, tracheal invasion or local extension of a thyroid malignancy , or metastases to local or mediastinal lymph nodes.
Fine-Needle Aspiration Biopsy p The best method for differentiation of benign from malignant thyroid disease. p Outpatient procedure p Requires no preparation. p The skin over the nodule is cleansed with alcohol, p If desired, a small amount of 1 % lidocaine can be injected intracutaneously for local anesthesia.
Effects of Thyroid Hormones on Peripheral Tissues p A measurement of basal oxygen in the intact organism the basal metabolic rate (BMR). p However, this test is nonspecific and insensitive and is rarely used today p Photomotogram. The traction and relaxation time of the Achilles tendon
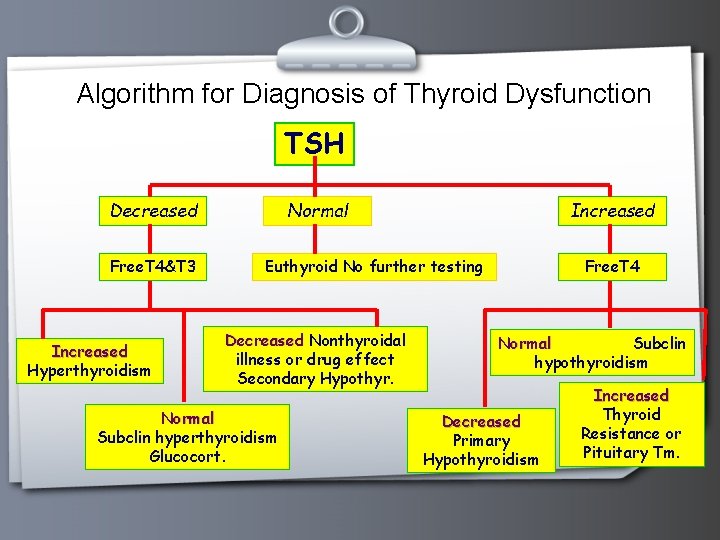
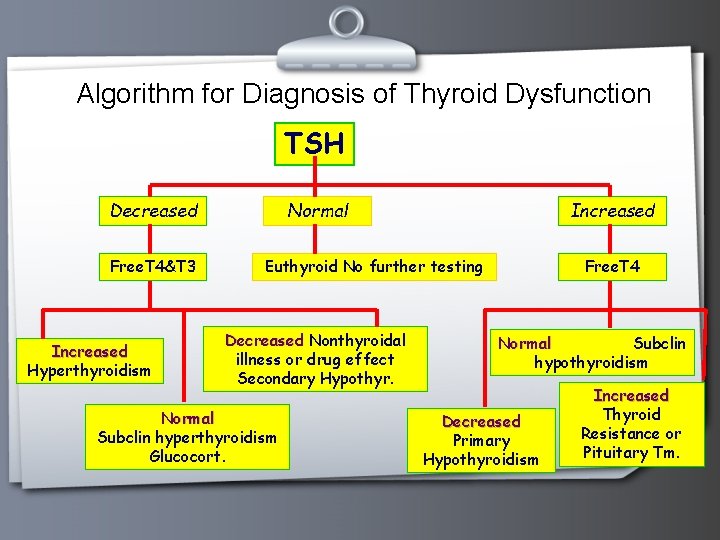
Algorithm for Diagnosis of Thyroid Dysfunction TSH Decreased Free. T 4&T 3 Increased Hyperthyroidism Normal Increased Euthyroid No further testing Decreased Nonthyroidal illness or drug effect Secondary Hypothyr. Normal Subclin hyperthyroidism Glucocort. Free. T 4 Normal Subclin hypothyroidism Decreased Primary Hypothyroidism Increased Thyroid Resistance or Pituitary Tm.
