Hypoglycemia Unawareness Joan P Frizzell Ph D RN






- Slides: 29
Hypoglycemia Unawareness Joan P Frizzell Ph. D. RN
Hypoglycemia Unawareness Loss of warning signs and symptoms of hypoglycemia Decreased counter – regulatory hormonal response to hypoglycemia Associated failure to treat hypoglycemia
Hypoglycemia Most commonly occurs from treatment of Diabetes mellitus 25. 8 Million People in the US have DM 8. 3% of American People 1. 9 million cases diagnosed each year One third of people are as yet undiagnosed Direct & Indirect costs exceed $174 Billion

Hypoglycemia Defined as glucose level of < 60 mg/dl Associated with specific symptoms and physiologic responses Symptoms may occur at higher glucose levels in some patients Symptoms and physiologic responses may be decreased due to repeated episodes of hypoglycemia
Etiology Medications Especially those used in the treatment of Diabetes mellitus Pentamidine, quinine Edogenous hyperinsulinism Insulinoma and other pancreatic B cell disorders Starvation Endocrine deficiencies Reduction in secretion of glucocorticoids, growth hormone, glucagons
Increased Risk of Hypoglycemia Patients with Type 1 DM “Tight” or near normal glycemic control Approximately 25% of patients with DM have a major hypoglycemic event
Risk Factors Insulin or insulin secretagogue is given in an excessive amount Insulin or insulin secretagogue is given at the wrong time Reduction in carbohydrate intake Glucose utilization is increased Exercise Insulin clearance is reduced Renal disease

Diagnosis – Whipple’s triad Symptoms consistent with hypoglycemia Low plasma glucose level Raising plasma glucose level relieves symptoms
Glucose Homeostasis Insulin secretion Counter-regulatory Hormones
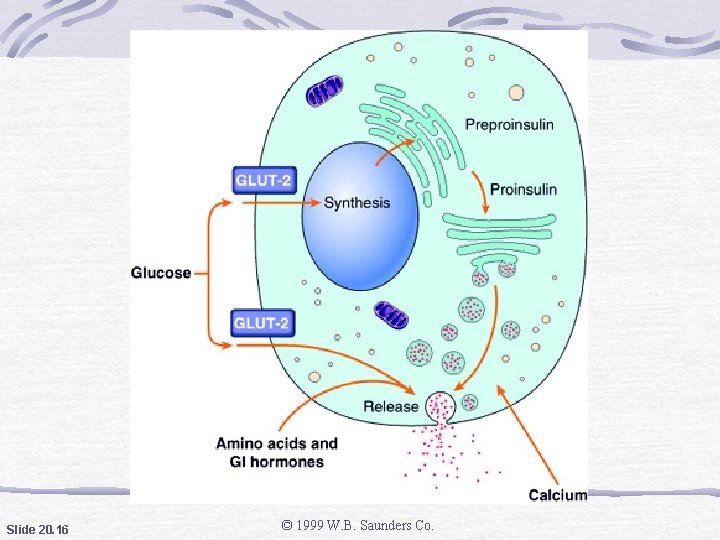
Insulin Secretion Daily basilar level 40 -50 U/day Stimulated secretion BS 80 -100 mg/dl Secreted through glucose metabolism mediated depolarization Membrane changes promote Ca influx and insulin secretion
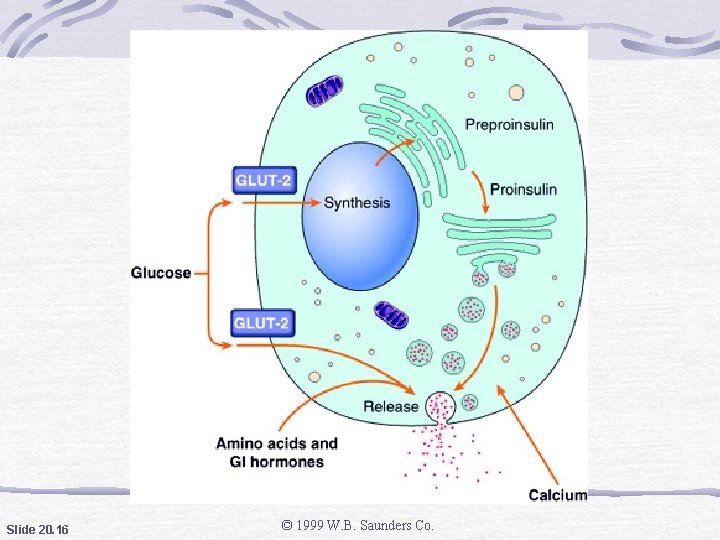
Slide 20. 16 © 1999 W. B. Saunders Co.
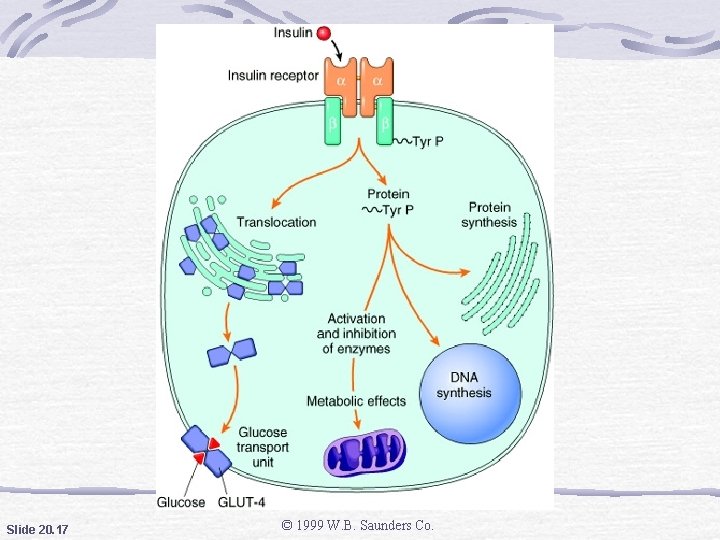
Insulin Action Insulin dependent glucose transporters Storage of energy substrates fats amino acids glucose to glycogen Enhancement of growth factor activity Increase cellular uptake of K, Phosphorus, and Mg
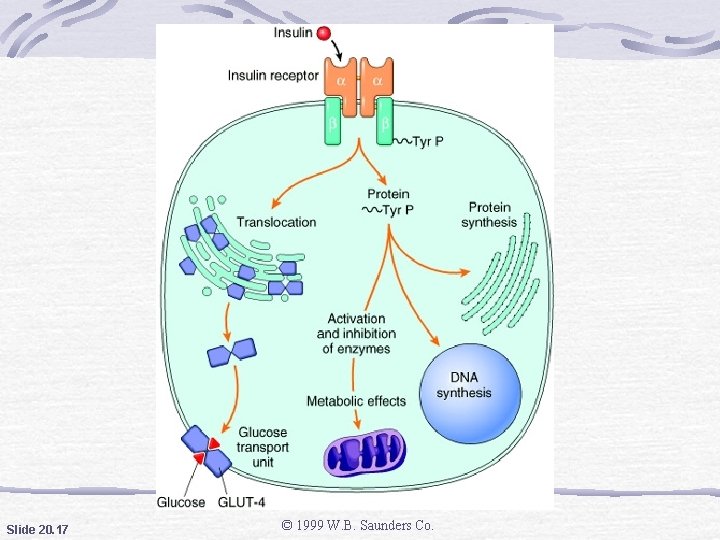
Slide 20. 17 © 1999 W. B. Saunders Co.

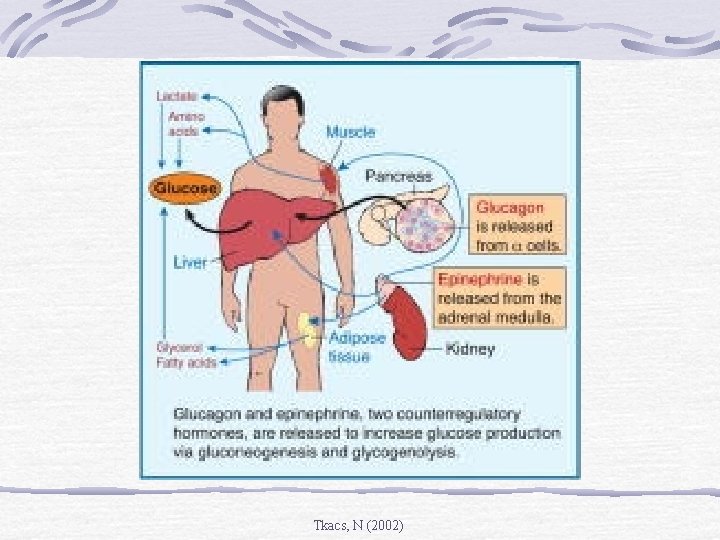
Counter Regulatory Hormones Glucagon opposes insulin Epinephrine mobilization of glucose stores Glucocorticoids decreases peripheral utilization of glucose Growth Hormone decreases glucose uptake by tissues
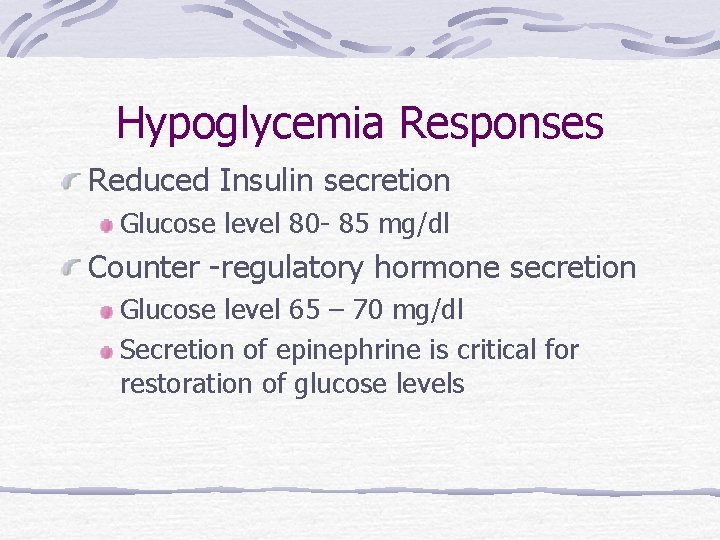
Hypoglycemia Responses Reduced Insulin secretion Glucose level 80 - 85 mg/dl Counter -regulatory hormone secretion Glucose level 65 – 70 mg/dl Secretion of epinephrine is critical for restoration of glucose levels
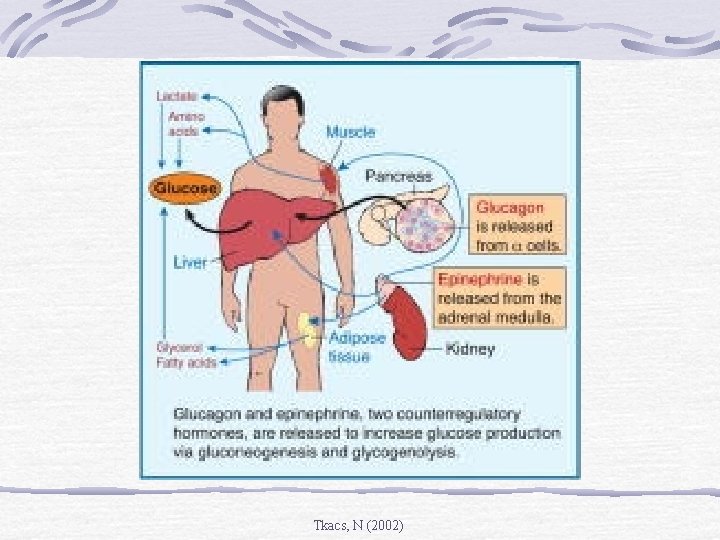
Tkacs, N (2002)
Hypoglycemia Symptoms Neurogenic or ANS responses Neuroglycopenic responses

Tkacs, N (2002)
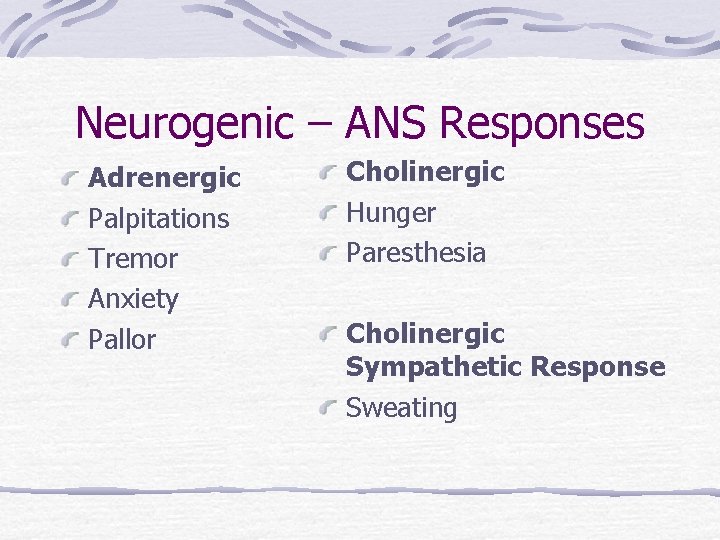
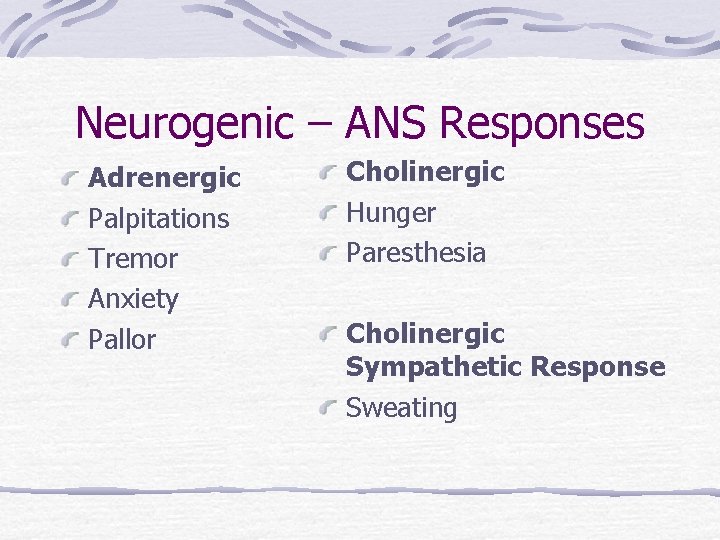
Neurogenic – ANS Responses Adrenergic Palpitations Tremor Anxiety Pallor Cholinergic Hunger Paresthesia Cholinergic Sympathetic Response Sweating
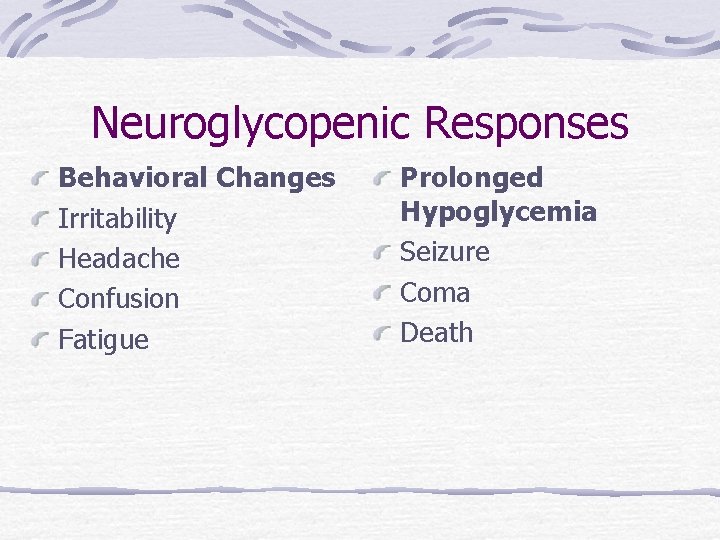
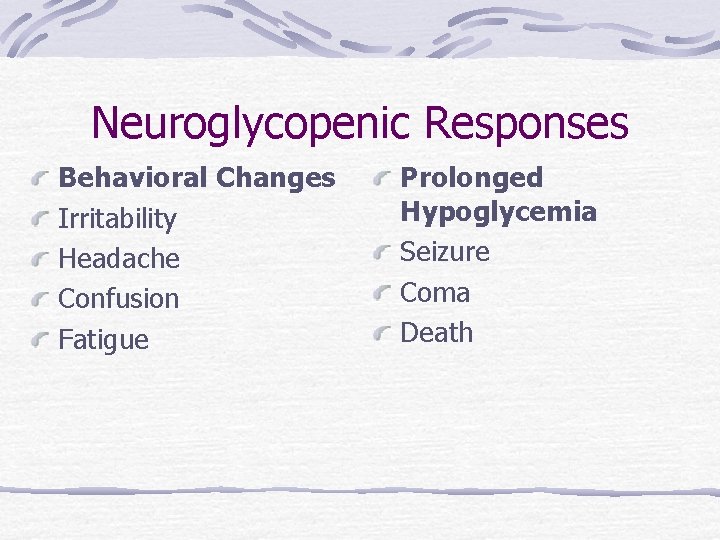
Neuroglycopenic Responses Behavioral Changes Irritability Headache Confusion Fatigue Prolonged Hypoglycemia Seizure Coma Death
Nocturnal Hypoglycemia
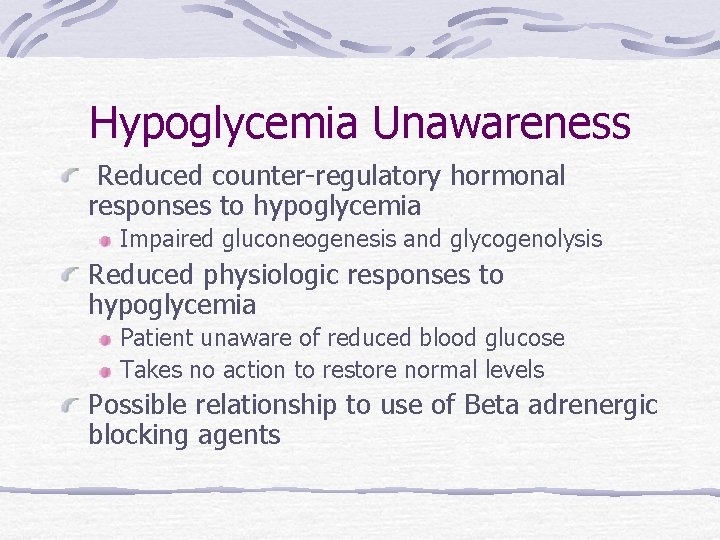
Hypoglycemia Unawareness Reduced counter-regulatory hormonal responses to hypoglycemia Impaired gluconeogenesis and glycogenolysis Reduced physiologic responses to hypoglycemia Patient unaware of reduced blood glucose Takes no action to restore normal levels Possible relationship to use of Beta adrenergic blocking agents
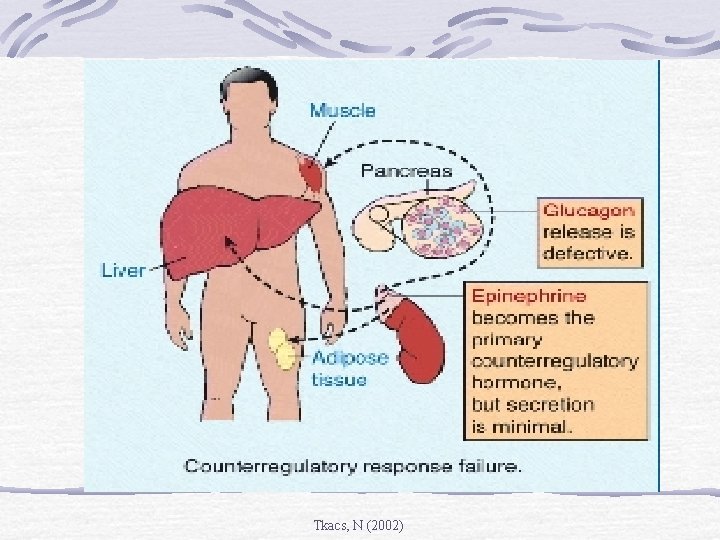
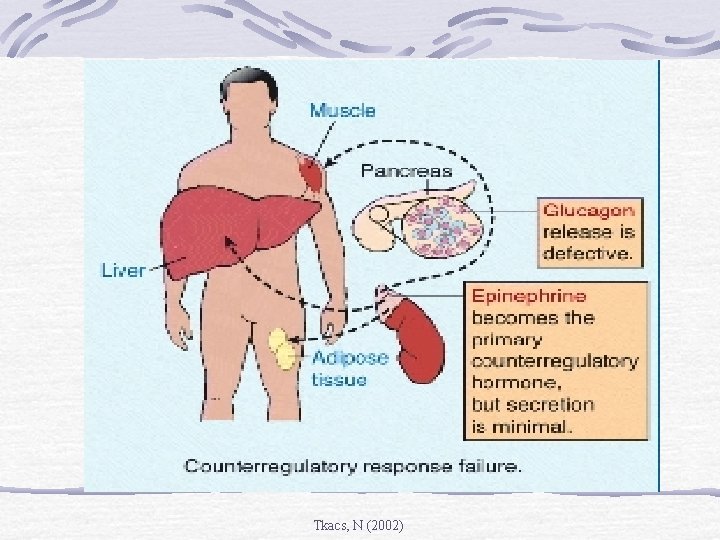
Tkacs, N (2002)
Reduced Hormonal Responses Decreased glucagon secretion often occurs in Type 1 DM Prior episodes of hypoglycemia reduce threshold for epinephrine secretion Hypoglycemia unawareness indicates that prior episodes of hypoglycemia have occured
Hypoglycemia Risk Reduction Patient Education and empowerment Frequent self monitoring Flexible medication regimens Blood Glucose Awareness Training

Patient Family Education Signs and symptoms of hypoglycemia Test blood sugar before driving a car or operating any hazardous equipment Carry glucose tablets or snack at all times Teach family members to administer glucagon, if patient is non responsive

Treatment Oral treatment with 15 -20 gm of glucose Appropriate oral replacement includes ½ cup of fruit juice and crackers ½ cup of milk and crackers After treatment, retest blood sugar in 15 minutes. If blood sugar is less than 60 mg/dl give an additional source of carbohydrates
Urgent Treatment Oral treatment with 20 gm of glucose tablets Parenteral 25 gm of glucose in a 50% solution Parenteral 1 mg glucagon
Blood Glucose Awareness Training Developed by Recognize symptoms of hypoglycemia Estimate blood glucose level Compare with self blood glucose monitoring
 Hypoglycemia unawareness
Hypoglycemia unawareness Hypoglycemia without diabetes
Hypoglycemia without diabetes Antidiabetic drugs mnemonics
Antidiabetic drugs mnemonics Starvation hypoglycemia
Starvation hypoglycemia Hypoglycemia mnemonic
Hypoglycemia mnemonic Hypoglycemia
Hypoglycemia Nursing diagnosis for diabetes mellitus slideshare
Nursing diagnosis for diabetes mellitus slideshare Hypoglycemia cpg
Hypoglycemia cpg Niphs syndrome
Niphs syndrome Hypoglycemia factitia
Hypoglycemia factitia Keys to content writing
Keys to content writing Inequalities warm up
Inequalities warm up Ustadistica
Ustadistica Institut joan oliver
Institut joan oliver The death of a righteous man
The death of a righteous man Balletprøve
Balletprøve Joan duveen
Joan duveen Joan plummer
Joan plummer Margus kreinin
Margus kreinin Joan scott experience
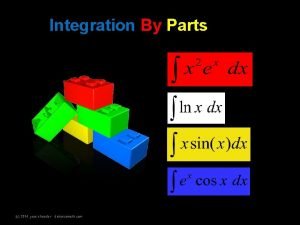
Joan scott experience Integration by parts lipet
Integration by parts lipet Joan condell
Joan condell Mood of the third wish
Mood of the third wish Joan vaccaro
Joan vaccaro Biblioteca joan regla
Biblioteca joan regla Joan of arc timeline
Joan of arc timeline Joan vaccaro
Joan vaccaro Joan gillis
Joan gillis Joan eriksen
Joan eriksen Joan miro paysage catalan
Joan miro paysage catalan