Hypercalcemic Disorders Hasan AYDIN MD Yeditepe University Hospital








- Slides: 34

Hypercalcemic Disorders Hasan AYDIN, MD Yeditepe University Hospital Endocrinology and Metabolism
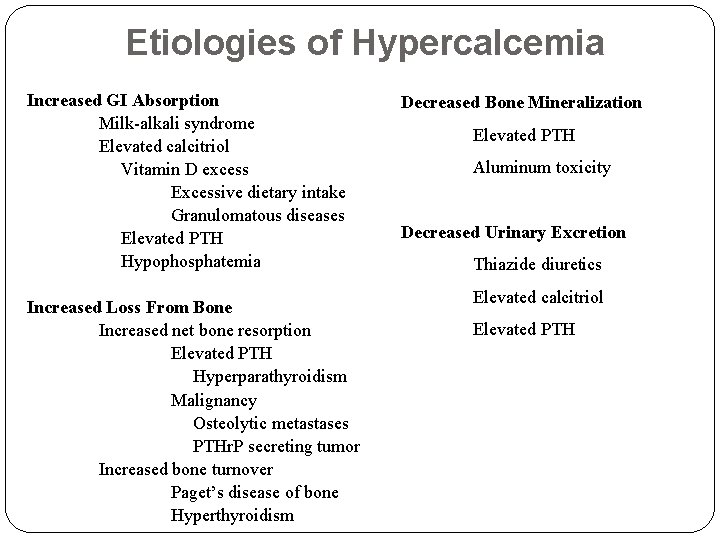
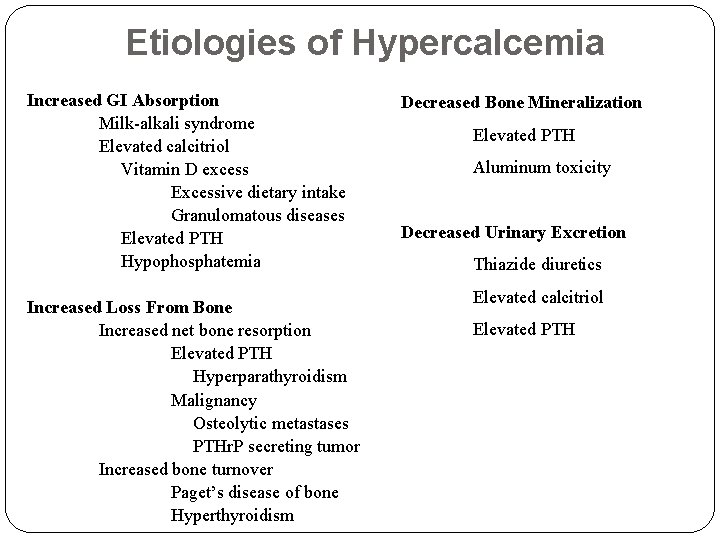
Etiologies of Hypercalcemia Increased GI Absorption Milk-alkali syndrome Elevated calcitriol Vitamin D excess Excessive dietary intake Granulomatous diseases Elevated PTH Hypophosphatemia Increased Loss From Bone Increased net bone resorption Elevated PTH Hyperparathyroidism Malignancy Osteolytic metastases PTHr. P secreting tumor Increased bone turnover Paget’s disease of bone Hyperthyroidism Decreased Bone Mineralization Elevated PTH Aluminum toxicity Decreased Urinary Excretion Thiazide diuretics Elevated calcitriol Elevated PTH
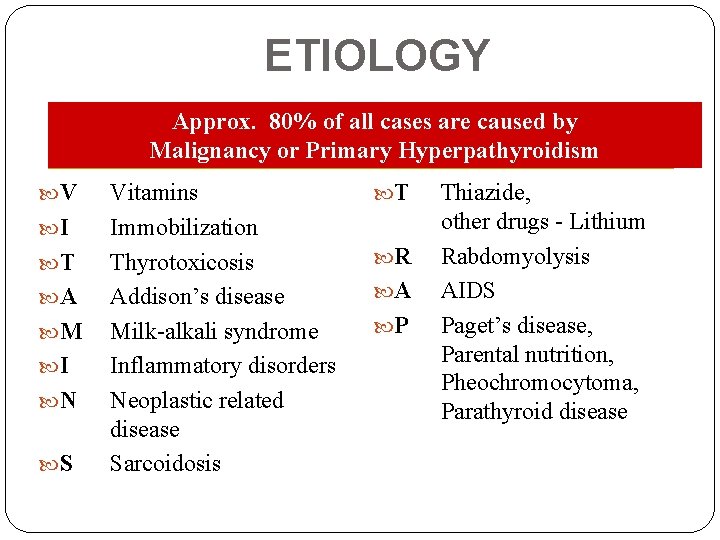
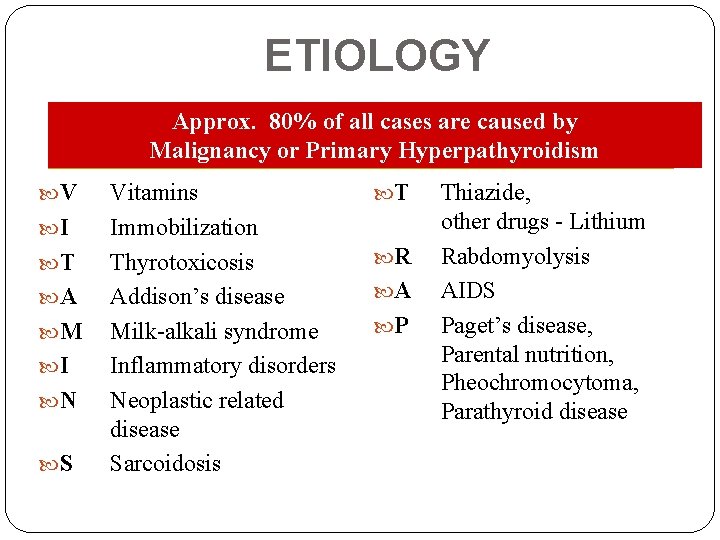
ETIOLOGY Approx. 80% of all cases are caused by Malignancy or Primary Hyperpathyroidism V I T A M I N S Vitamins Immobilization Thyrotoxicosis Addison’s disease Milk-alkali syndrome Inflammatory disorders Neoplastic related disease Sarcoidosis T R A P Thiazide, other drugs - Lithium Rabdomyolysis AIDS Paget’s disease, Parental nutrition, Pheochromocytoma, Parathyroid disease
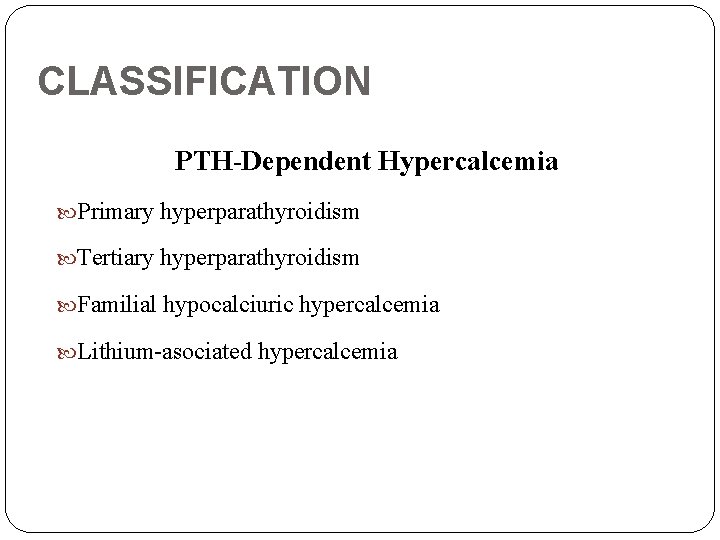
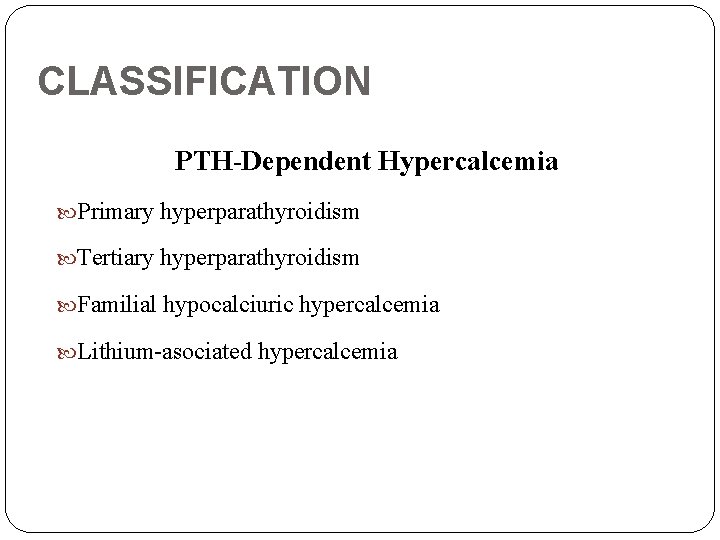
CLASSIFICATION PTH-Dependent Hypercalcemia Primary hyperparathyroidism Tertiary hyperparathyroidism Familial hypocalciuric hypercalcemia Lithium-asociated hypercalcemia
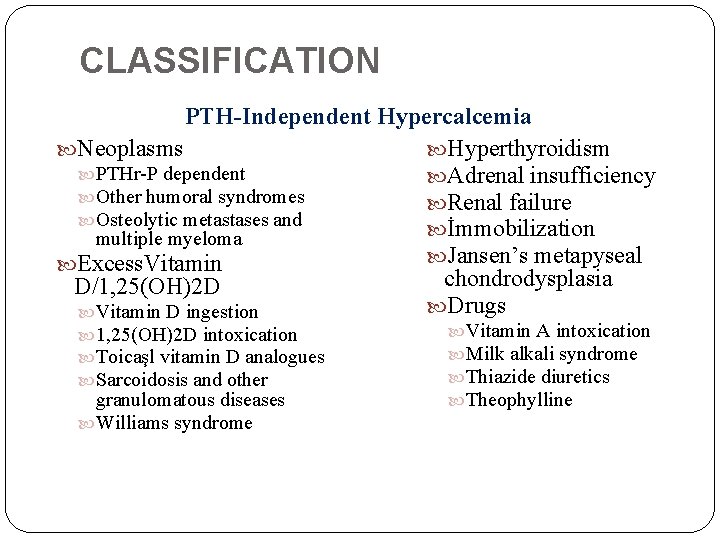
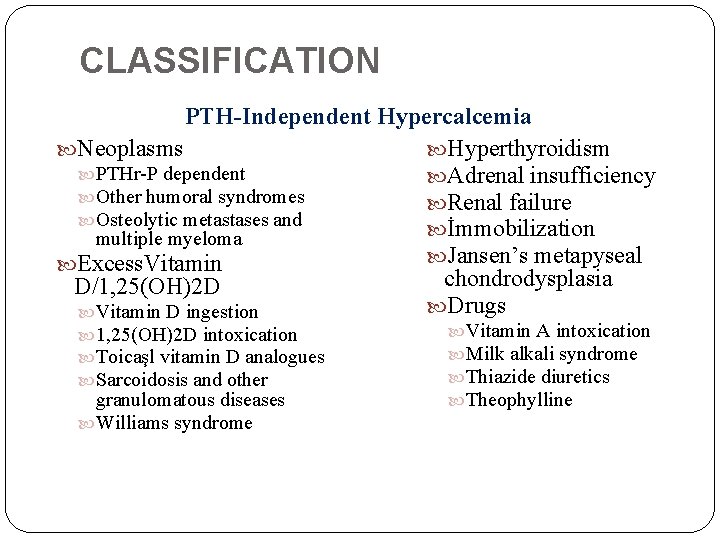
CLASSIFICATION PTH-Independent Hypercalcemia Neoplasms Hyperthyroidism PTHr-P dependent Adrenal insufficiency Other humoral syndromes Renal failure Osteolytic metastases and İmmobilization multiple myeloma Jansen’s metapyseal Excess. Vitamin chondrodysplasia D/1, 25(OH)2 D Drugs Vitamin D ingestion 1, 25(OH)2 D intoxication Toicaşl vitamin D analogues Sarcoidosis and other granulomatous diseases Williams syndrome Vitamin A intoxication Milk alkali syndrome Thiazide diuretics Theophylline
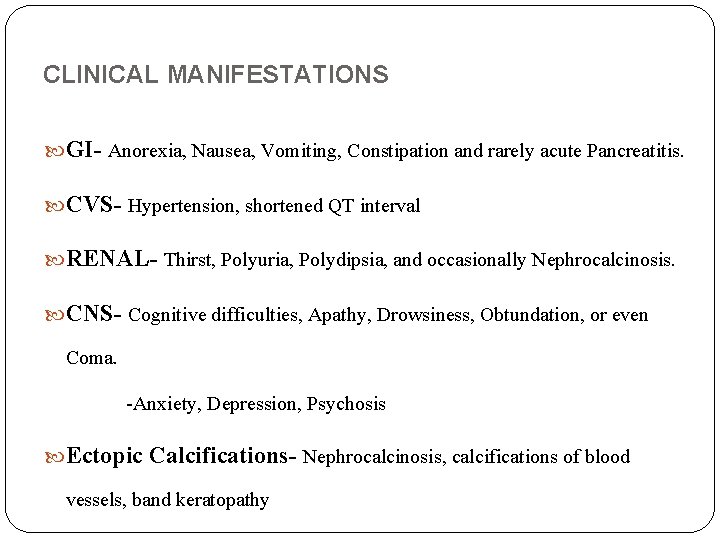
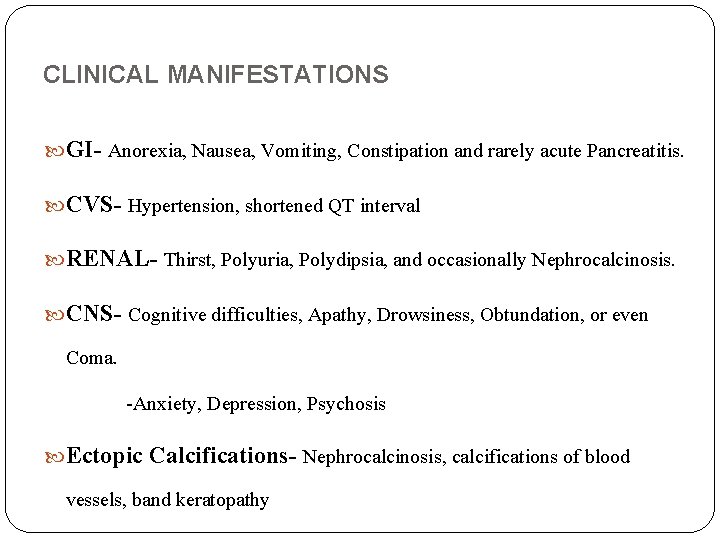
CLINICAL MANIFESTATIONS GI- Anorexia, Nausea, Vomiting, Constipation and rarely acute Pancreatitis. CVS- Hypertension, shortened QT interval RENAL- Thirst, Polyuria, Polydipsia, and occasionally Nephrocalcinosis. CNS- Cognitive difficulties, Apathy, Drowsiness, Obtundation, or even Coma. -Anxiety, Depression, Psychosis Ectopic Calcifications- Nephrocalcinosis, calcifications of blood vessels, band keratopathy

SYMPTOMS More than 50% of all patients with primary hyperparathyroidism are asymptomatic when hypercalcemia is first discovered.

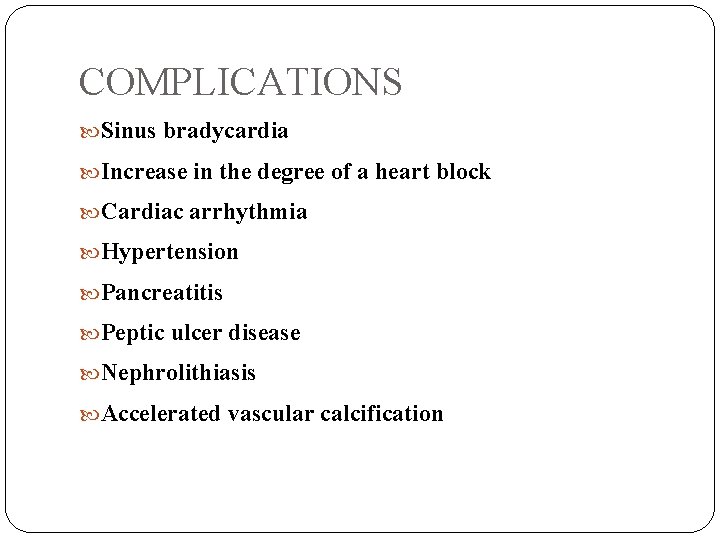
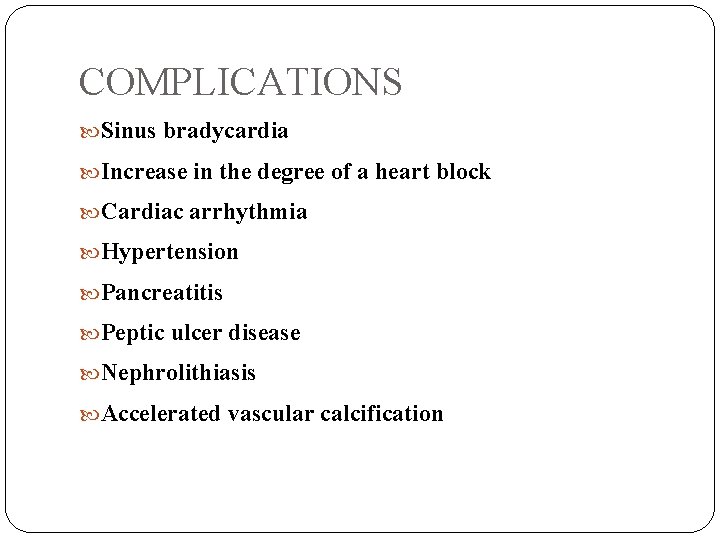
COMPLICATIONS Sinus bradycardia Increase in the degree of a heart block Cardiac arrhythmia Hypertension Pancreatitis Peptic ulcer disease Nephrolithiasis Accelerated vascular calcification
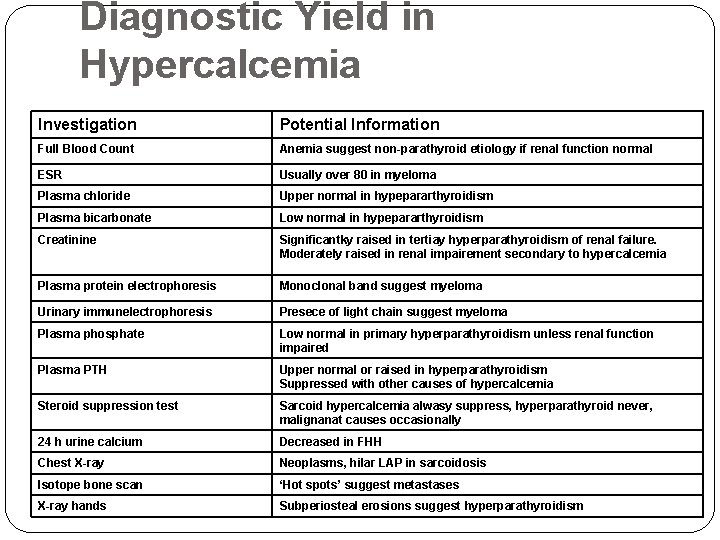
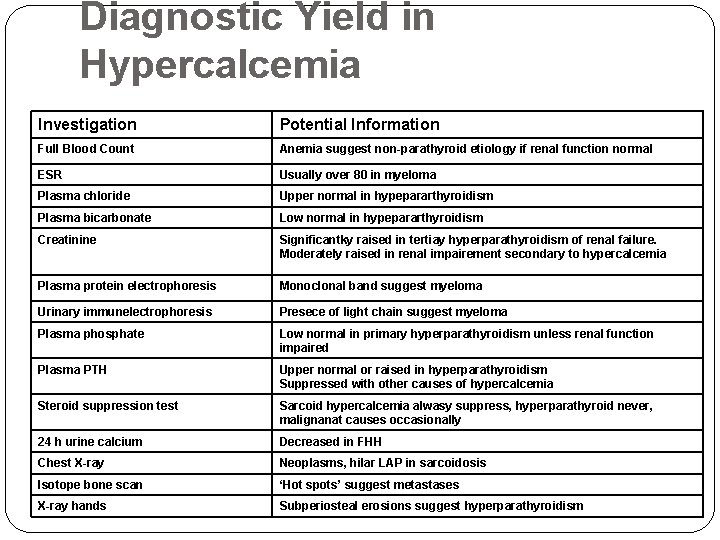
Diagnostic Yield in Hypercalcemia Investigation Potential Information Full Blood Count Anemia suggest non-parathyroid etiology if renal function normal ESR Usually over 80 in myeloma Plasma chloride Upper normal in hypepararthyroidism Plasma bicarbonate Low normal in hypepararthyroidism Creatinine Significantky raised in tertiay hyperparathyroidism of renal failure. Moderately raised in renal impairement secondary to hypercalcemia Plasma protein electrophoresis Monoclonal band suggest myeloma Urinary immunelectrophoresis Presece of light chain suggest myeloma Plasma phosphate Low normal in primary hyperparathyroidism unless renal function impaired Plasma PTH Upper normal or raised in hyperparathyroidism Suppressed with other causes of hypercalcemia Steroid suppression test Sarcoid hypercalcemia alwasy suppress, hyperparathyroid never, malignanat causes occasionally 24 h urine calcium Decreased in FHH Chest X-ray Neoplasms, hilar LAP in sarcoidosis Isotope bone scan ‘Hot spots’ suggest metastases X-ray hands Subperiosteal erosions suggest hyperparathyroidism
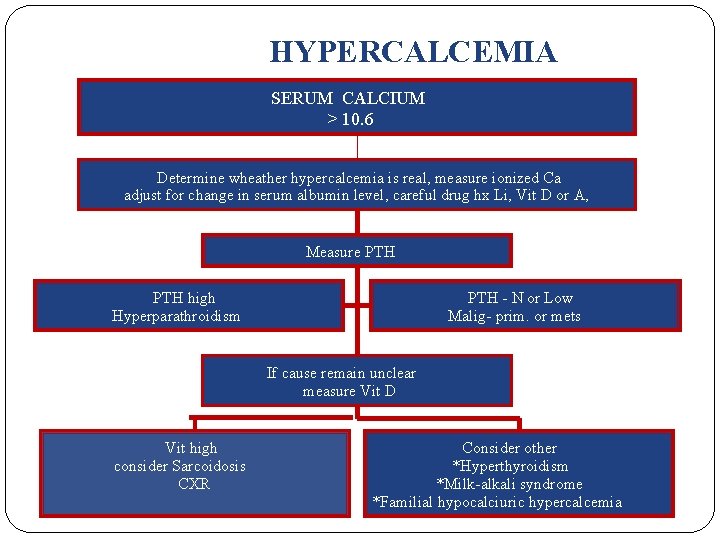
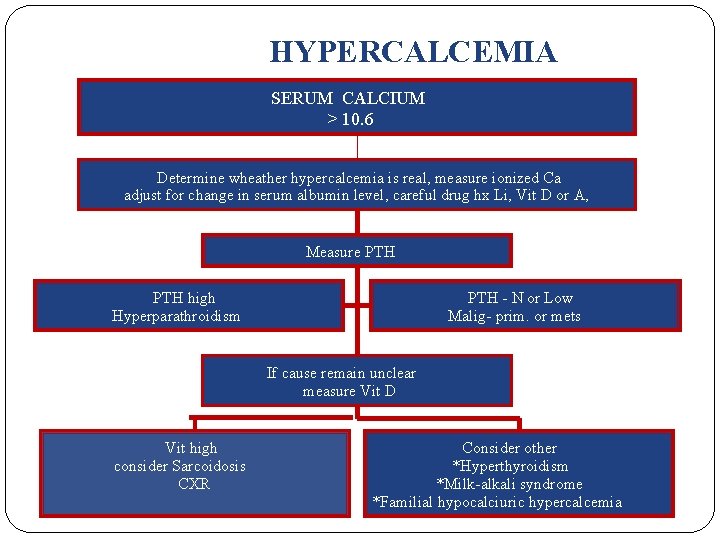
HYPERCALCEMIA SERUM CALCIUM > 10. 6 Determine wheather hypercalcemia is real, measure ionized Ca adjust for change in serum albumin level, careful drug hx Li, Vit D or A, Measure PTH high Hyperparathroidism PTH - N or Low Malig- prim. or mets If cause remain unclear measure Vit D Vit high consider Sarcoidosis CXR Consider other *Hyperthyroidism *Milk-alkali syndrome *Familial hypocalciuric hypercalcemia
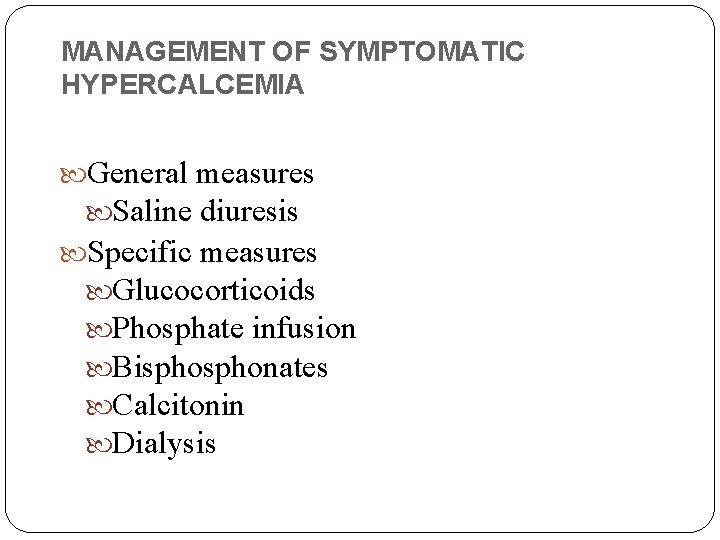
MANAGEMENT OF SYMPTOMATIC HYPERCALCEMIA General measures Saline diuresis Specific measures Glucocorticoids Phosphate infusion Bisphonates Calcitonin Dialysis
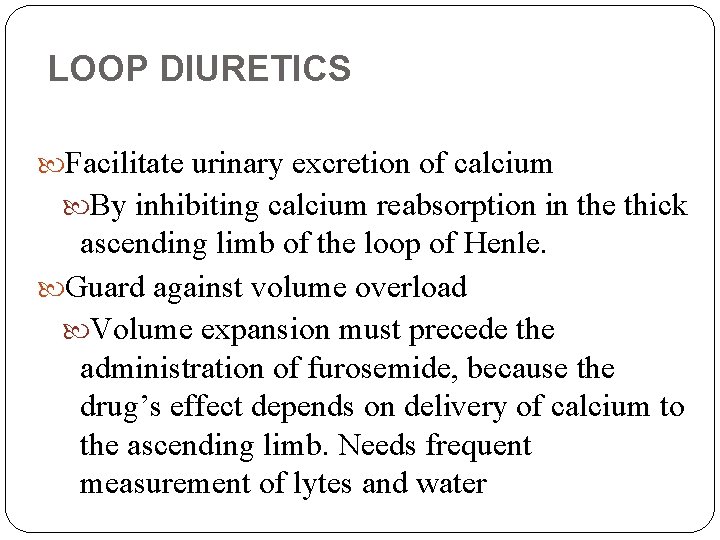
LOOP DIURETICS Facilitate urinary excretion of calcium By inhibiting calcium reabsorption in the thick ascending limb of the loop of Henle. Guard against volume overload Volume expansion must precede the administration of furosemide, because the drug’s effect depends on delivery of calcium to the ascending limb. Needs frequent measurement of lytes and water
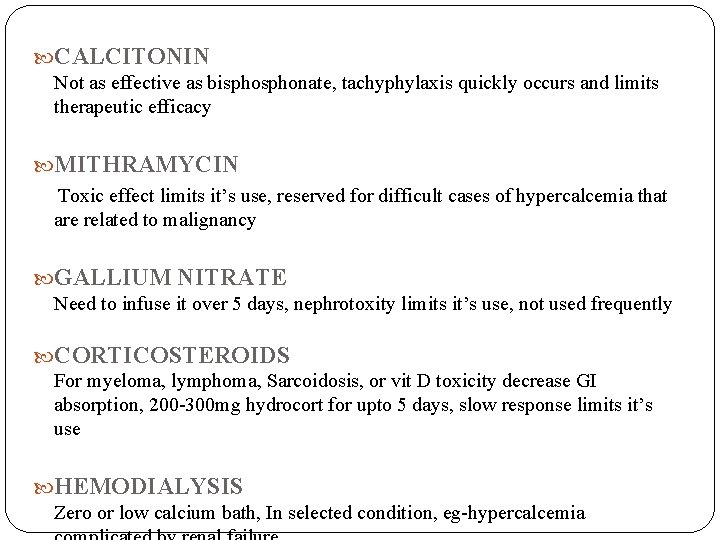
CALCITONIN Not as effective as bisphonate, tachyphylaxis quickly occurs and limits therapeutic efficacy MITHRAMYCIN Toxic effect limits it’s use, reserved for difficult cases of hypercalcemia that are related to malignancy GALLIUM NITRATE Need to infuse it over 5 days, nephrotoxity limits it’s use, not used frequently CORTICOSTEROIDS For myeloma, lymphoma, Sarcoidosis, or vit D toxicity decrease GI absorption, 200 -300 mg hydrocort for upto 5 days, slow response limits it’s use HEMODIALYSIS Zero or low calcium bath, In selected condition, eg-hypercalcemia
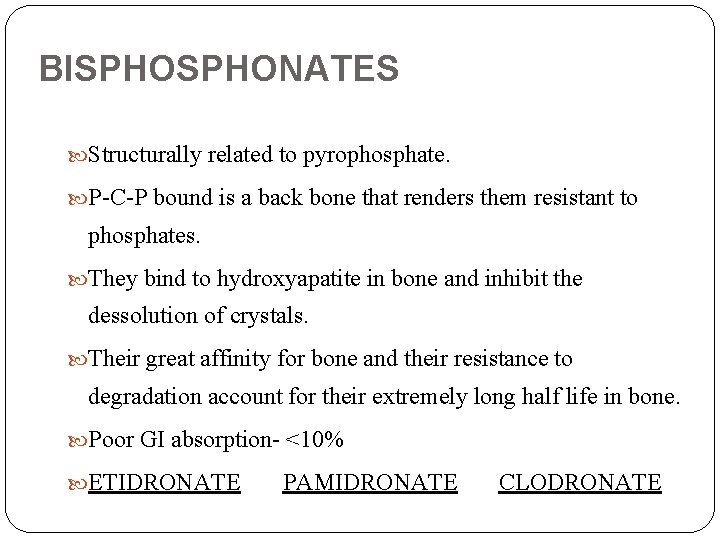
BISPHONATES Structurally related to pyrophosphate. P-C-P bound is a back bone that renders them resistant to phosphates. They bind to hydroxyapatite in bone and inhibit the dessolution of crystals. Their great affinity for bone and their resistance to degradation account for their extremely long half life in bone. Poor GI absorption- <10% ETIDRONATE PAMIDRONATE CLODRONATE
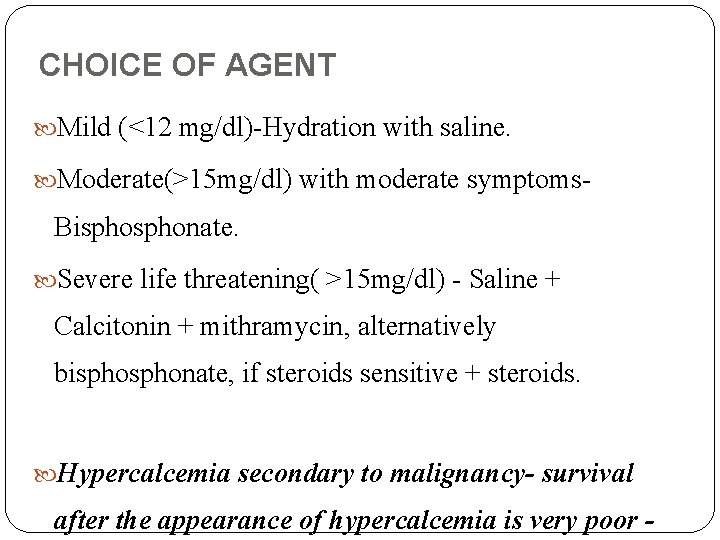
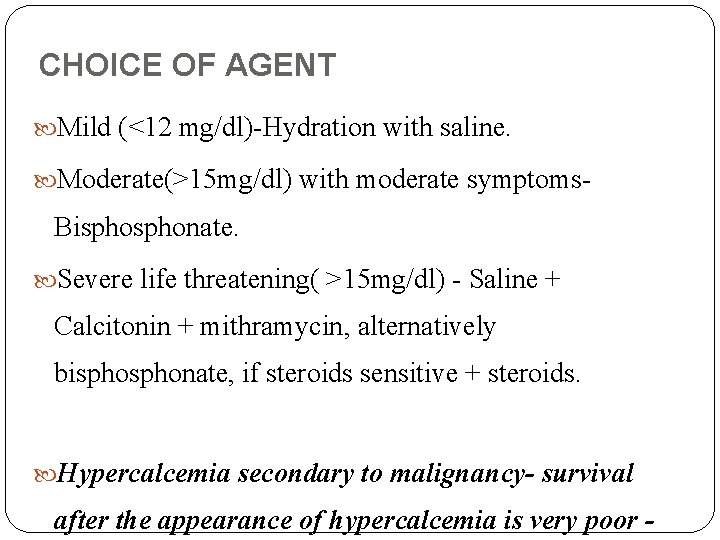
CHOICE OF AGENT Mild (<12 mg/dl)-Hydration with saline. Moderate(>15 mg/dl) with moderate symptoms- Bisphonate. Severe life threatening( >15 mg/dl) - Saline + Calcitonin + mithramycin, alternatively bisphonate, if steroids sensitive + steroids. Hypercalcemia secondary to malignancy- survival after the appearance of hypercalcemia is very poor -
SPECIFIC CAUSES OF HYPERCALCEMIA
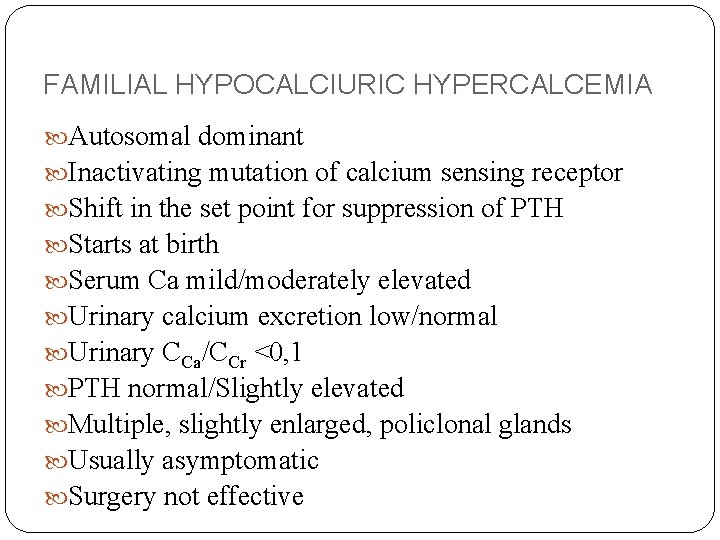
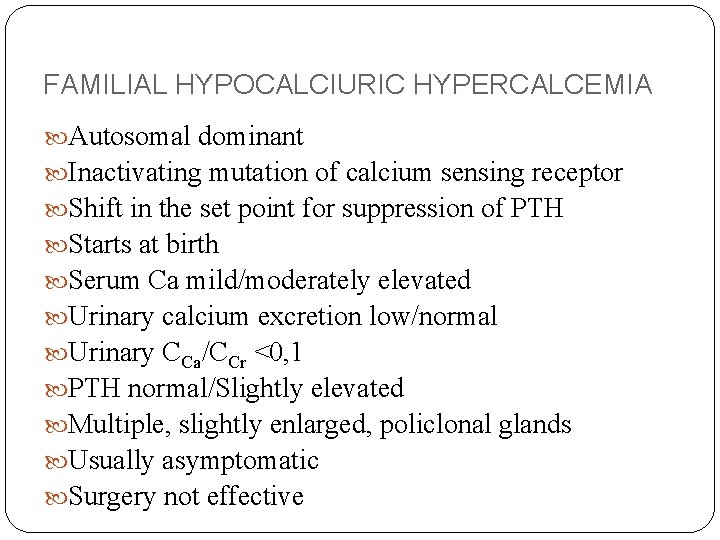
FAMILIAL HYPOCALCIURIC HYPERCALCEMIA Autosomal dominant Inactivating mutation of calcium sensing receptor Shift in the set point for suppression of PTH Starts at birth Serum Ca mild/moderately elevated Urinary calcium excretion low/normal Urinary CCa/CCr <0, 1 PTH normal/Slightly elevated Multiple, slightly enlarged, policlonal glands Usually asymptomatic Surgery not effective
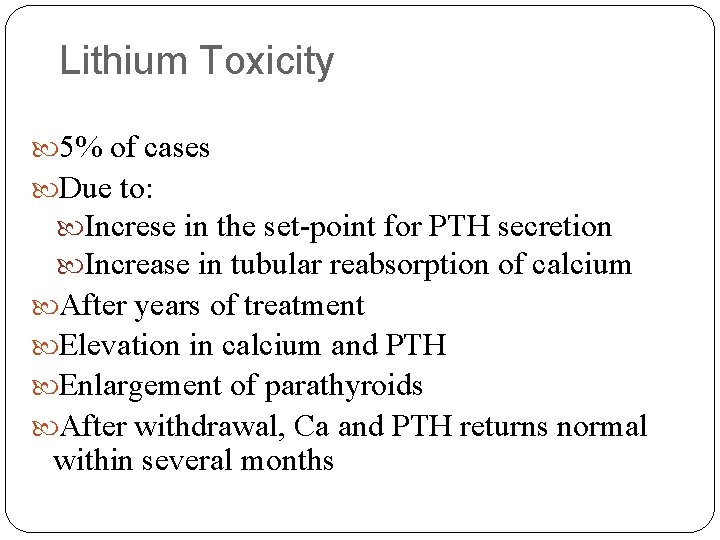
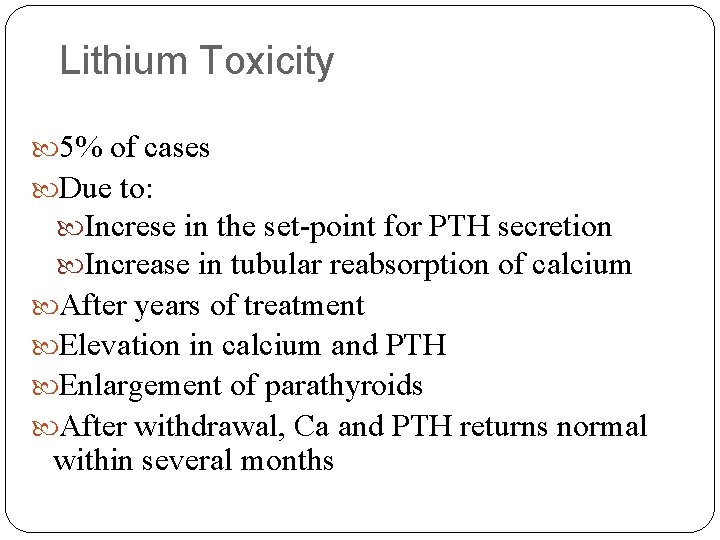
Lithium Toxicity 5% of cases Due to: Increse in the set-point for PTH secretion Increase in tubular reabsorption of calcium After years of treatment Elevation in calcium and PTH Enlargement of parathyroids After withdrawal, Ca and PTH returns normal within several months

Hypercalcemia of Malignancy Most common cause in hospitalized patients Most common in Sq. Cell Ca. , Breast. Renal Bladder Ca, MM, Lymphoma Uncommon in colon and prostate ca. Occurs in the late course of malignancy Dehydration, immobilization and treatment with certain drugs contribute to or potentiate development of hypercalcemia
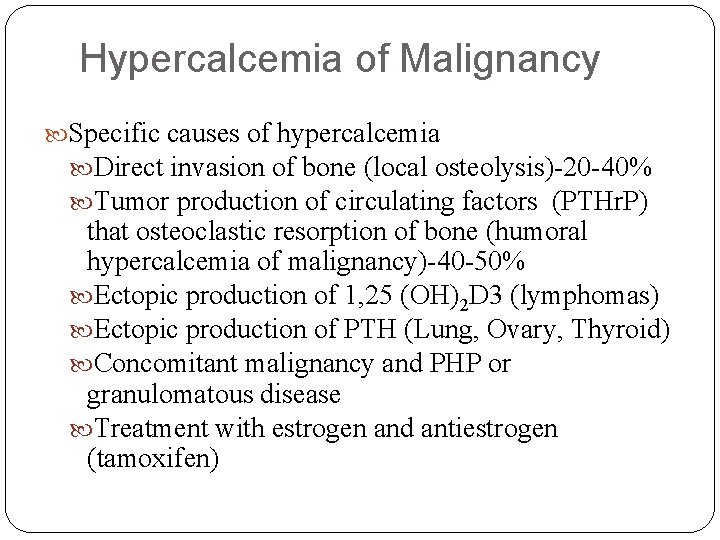
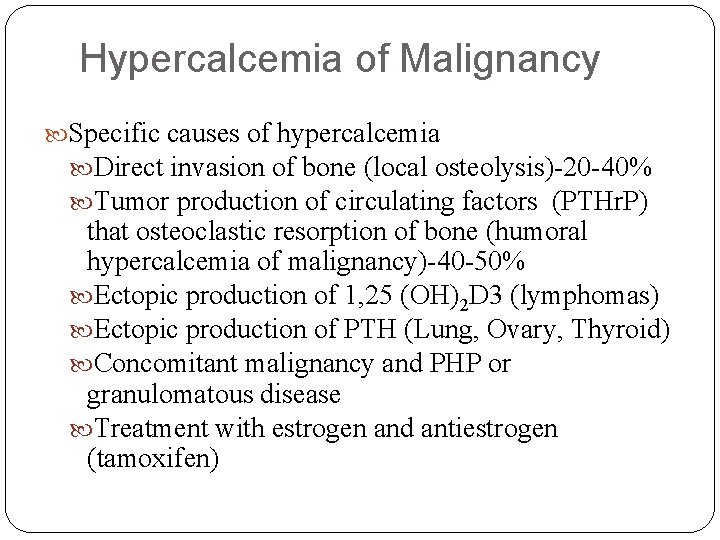
Hypercalcemia of Malignancy Specific causes of hypercalcemia Direct invasion of bone (local osteolysis)-20 -40% Tumor production of circulating factors (PTHr. P) that osteoclastic resorption of bone (humoral hypercalcemia of malignancy)-40 -50% Ectopic production of 1, 25 (OH)2 D 3 (lymphomas) Ectopic production of PTH (Lung, Ovary, Thyroid) Concomitant malignancy and PHP or granulomatous disease Treatment with estrogen and antiestrogen (tamoxifen)
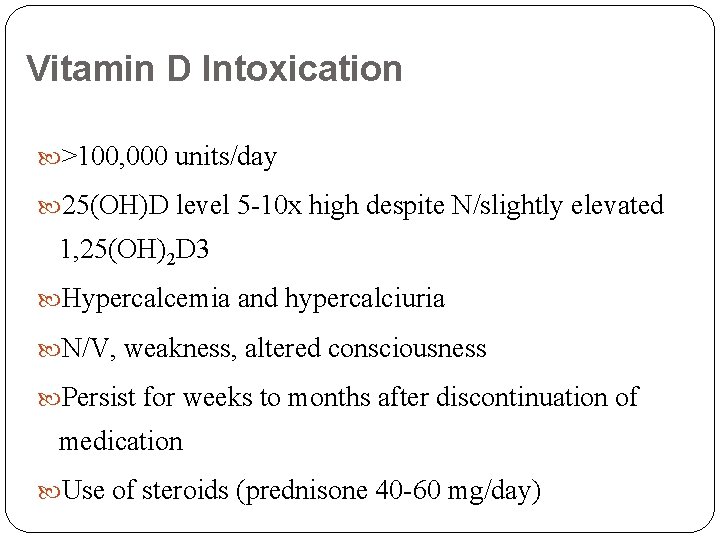
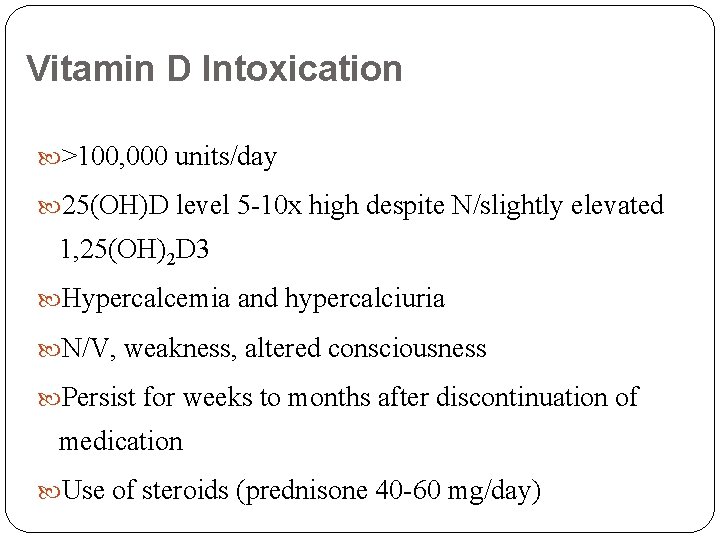
Vitamin D Intoxication >100, 000 units/day 25(OH)D level 5 -10 x high despite N/slightly elevated 1, 25(OH)2 D 3 Hypercalcemia and hypercalciuria N/V, weakness, altered consciousness Persist for weeks to months after discontinuation of medication Use of steroids (prednisone 40 -60 mg/day)

Granulomatous Diseases Hypercalcemia in 10%, hypercalciuria 50% of sarcoidosis Correlate with degree of severity and level of ACE Causes High level of 1, 25(OH)2 D 3 Overproduction of bone resorbing cytokines Production of PTHr. P Treatment with steroids (prednisone 40 -60 mg/d)
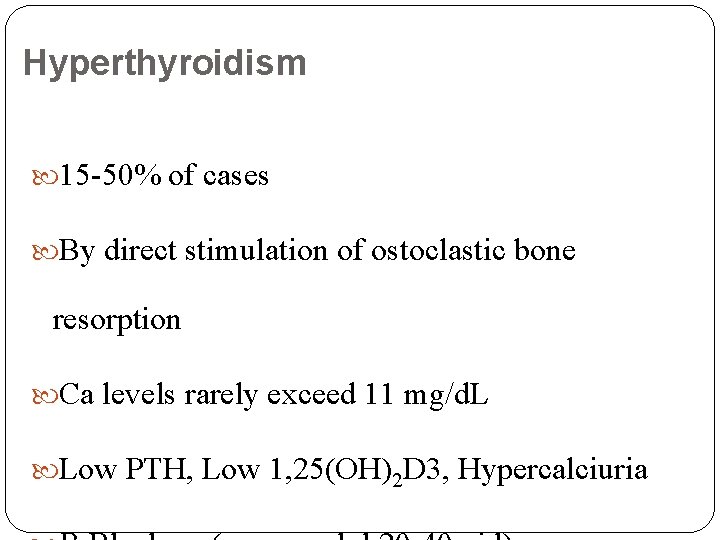
Hyperthyroidism 15 -50% of cases By direct stimulation of ostoclastic bone resorption Ca levels rarely exceed 11 mg/d. L Low PTH, Low 1, 25(OH)2 D 3, Hypercalciuria

Vitamin A Intoxication >50, 000 IU/day Treatment with cis-retinoic acid or all- transretinoic acid Dry skin, pruritus, headache, bone pain By direct stimulation of bone resorption Treatment with hydration and steroids
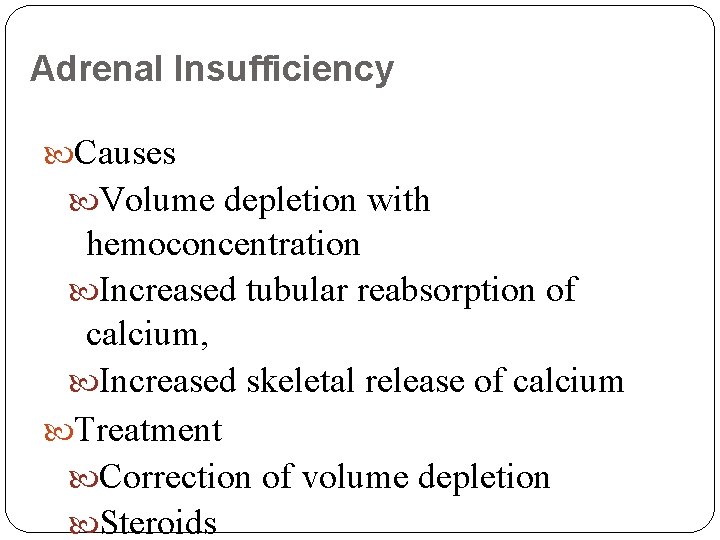
Adrenal Insufficiency Causes Volume depletion with hemoconcentration Increased tubular reabsorption of calcium, Increased skeletal release of calcium Treatment Correction of volume depletion Steroids
Thiazide Diuretics Rarely cause hypercalcemia by themselves Causes ↑ renal tubular reabsorption of Ca ↑ bone resorption activity Diuretic-induced volume depletion
Milk Alkali Syndrome Ingestion of excessive amounts of milk (calcium supplements) or soluble alkali (antacids) Acute form Triad of hypercalcemia, metabolic alkalosis, renal failure Treatment with rehydration and if necessary dialysis Chronic form (Burnett syndrome) Soft tissue calcifications in kidney and nephrocalcinosis
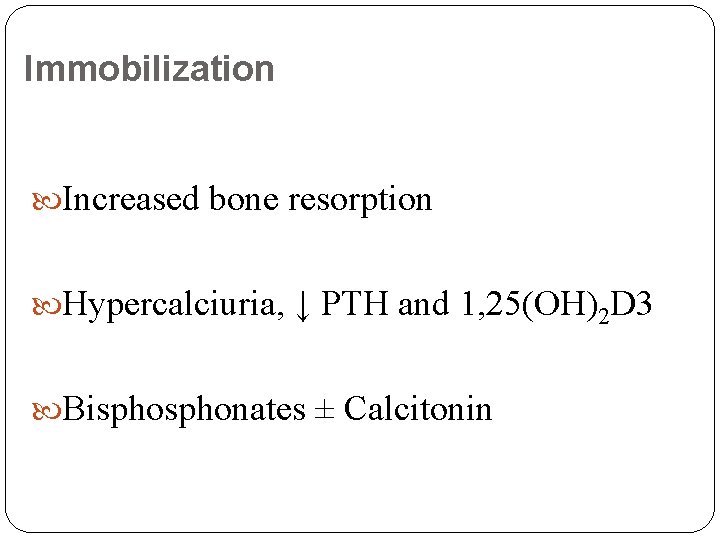
Immobilization Increased bone resorption Hypercalciuria, ↓ PTH and 1, 25(OH)2 D 3 Bisphonates ± Calcitonin
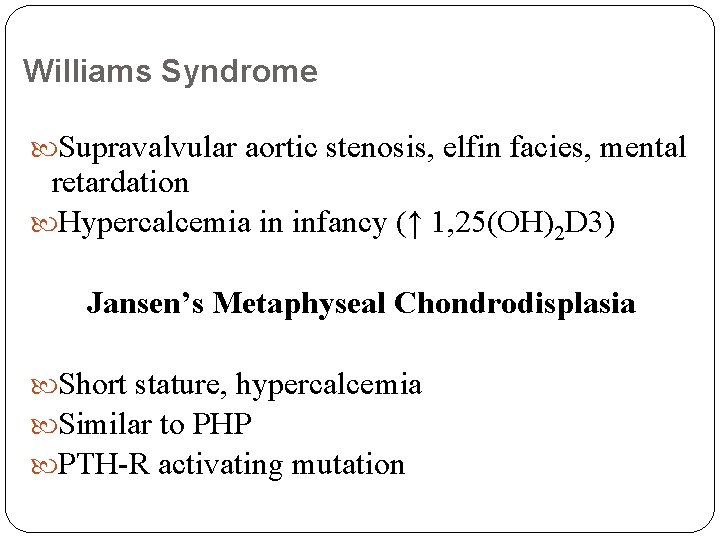
Williams Syndrome Supravalvular aortic stenosis, elfin facies, mental retardation Hypercalcemia in infancy (↑ 1, 25(OH)2 D 3) Jansen’s Metaphyseal Chondrodisplasia Short stature, hypercalcemia Similar to PHP PTH-R activating mutation
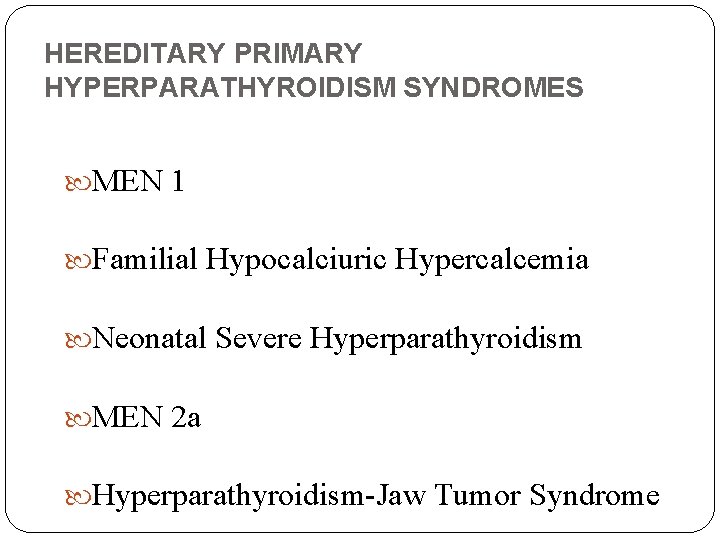
HEREDITARY PRIMARY HYPERPARATHYROIDISM SYNDROMES MEN 1 Familial Hypocalciuric Hypercalcemia Neonatal Severe Hyperparathyroidism MEN 2 a Hyperparathyroidism-Jaw Tumor Syndrome
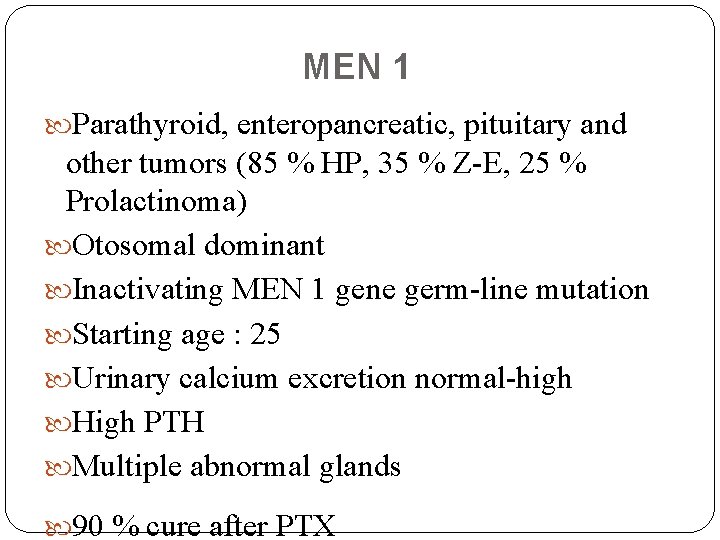
MEN 1 Parathyroid, enteropancreatic, pituitary and other tumors (85 % HP, 35 % Z-E, 25 % Prolactinoma) Otosomal dominant Inactivating MEN 1 gene germ-line mutation Starting age : 25 Urinary calcium excretion normal-high High PTH Multiple abnormal glands 90 % cure after PTX

MEN 2 A Pheochromocytoma, medullary thyroid CA, mild hyperparathyroidism Activating mutation of the RET proto- oncogene Otosomal dominant

 Medivia
Medivia Coadsys exam yeditepe
Coadsys exam yeditepe Coadsys exam
Coadsys exam Sinan aydın ymm
Sinan aydın ymm Nizamettin aydin
Nizamettin aydin Nizamettin aydin
Nizamettin aydin Aydın kendirci
Aydın kendirci Thede loder
Thede loder Sevil aydın
Sevil aydın Aydın bir türk kadınıyım
Aydın bir türk kadınıyım Dr bushra hasan
Dr bushra hasan Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Coordination
Coordination Package diagram
Package diagram Aydin marine
Aydin marine Aydın başar
Aydın başar Mega giga tera
Mega giga tera Nazmi aydın
Nazmi aydın Aydin bal
Aydin bal Aydın kekemelik merkezi
Aydın kekemelik merkezi Hospital pharmacy defination
Hospital pharmacy defination University hospital of pisa
University hospital of pisa Bezmialem vakıf university hospital
Bezmialem vakıf university hospital Benha university hospital
Benha university hospital Kyorin university ranking
Kyorin university ranking University hospital tuebingen
University hospital tuebingen Pisa university hospital
Pisa university hospital Patras university hospital
Patras university hospital Pisa university hospital
Pisa university hospital Hospital university of pennsylvania
Hospital university of pennsylvania Portsmouth hospital trust values
Portsmouth hospital trust values Kyung hee university hospital at gangdong
Kyung hee university hospital at gangdong Kaohsiung medical university hospital
Kaohsiung medical university hospital