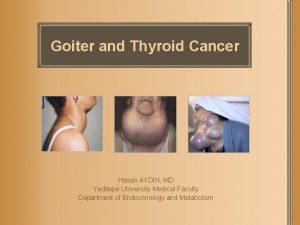
Hypothyroidism Hasan AYDIN MD Yeditepe University Medical Faculty












- Slides: 57
Hypothyroidism Hasan AYDIN, MD Yeditepe University Medical Faculty Endocrinology and Metabolism Page
Definition A deficiency of thyroid hormones, which in turn results in a generalized slowing down of metabolic processes. Page 2
Page
Hypothyroidism Epidemiology – Most common endocrine disease – Females > Males – 8 : 1 Presentation – Often unsuspected and grossly under diagnosed – 90 % of the cases are Primary Hypothyroidism – Menstrual irregularities, miscarriages, growth retard. – Vague pains, anaemia, lethargy, gain in weight – In clear cut cases - typical signs and symptoms Page 4
Disease Burden 5% of the general population are “Subclinically Hypothyroid” 15 % of all women > 65 yrs. are hypothyroid Detecting sub-clinical hypothyroidism in pregnancy is highly essential Page 5 All persons aged above 60 years – Order for TSH

Etiology Page
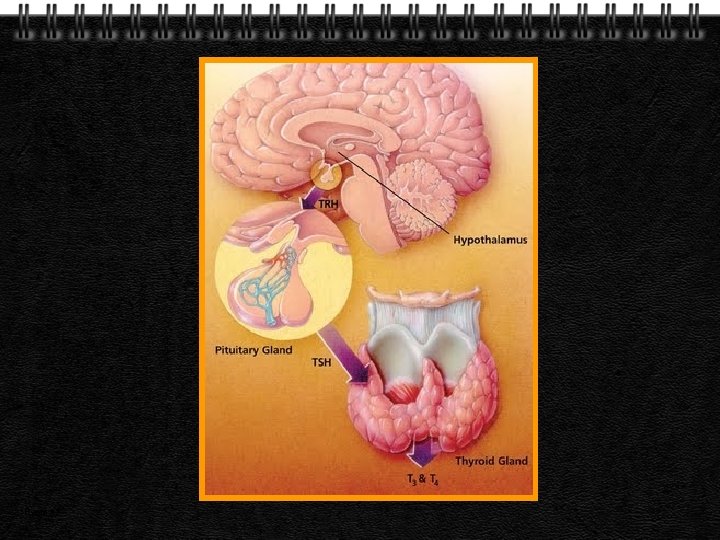
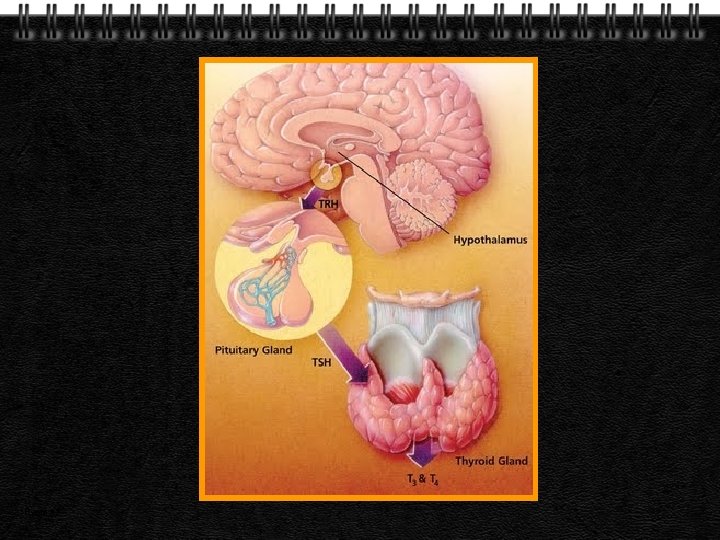
Causes of Hypothyroidism Primary – Congenital – Acquired – Transient Secondary – Pituitary – Hypothalamic Page 7
Congenital Hypothyroidism Athyreosis Dyshormonogenesis – Sodium/iodide symporter mutations – TPO mutations – Thyroglobulin gene mutations – Deiodinase defects Thyroid hormone resistance TSH-receptor defect Page 8
Acquired Hypothyroidism Iodine deficiency Autoimmune thyroid disease – Hashimoto’s , Graves disease Iatrogenic – Post-thyroidectomy – Radioactive iodine treatment – Thyroid irradiation – Medications/goitrogens Page 9
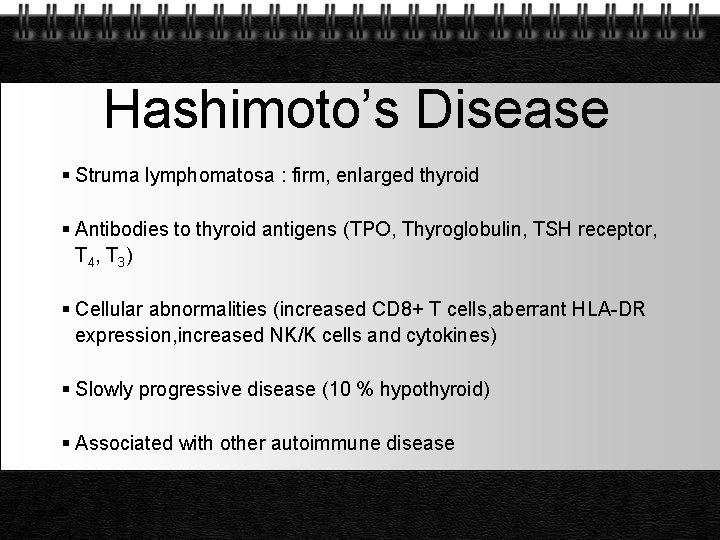
Hashimoto’s Disease Struma lymphomatosa : firm, enlarged thyroid Antibodies to thyroid antigens (TPO, Thyroglobulin, TSH receptor, T 4 , T 3 ) Cellular abnormalities (increased CD 8+ T cells, aberrant HLA-DR expression, increased NK/K cells and cytokines) Slowly progressive disease (10 % hypothyroid) Associated with other autoimmune disease Page 10
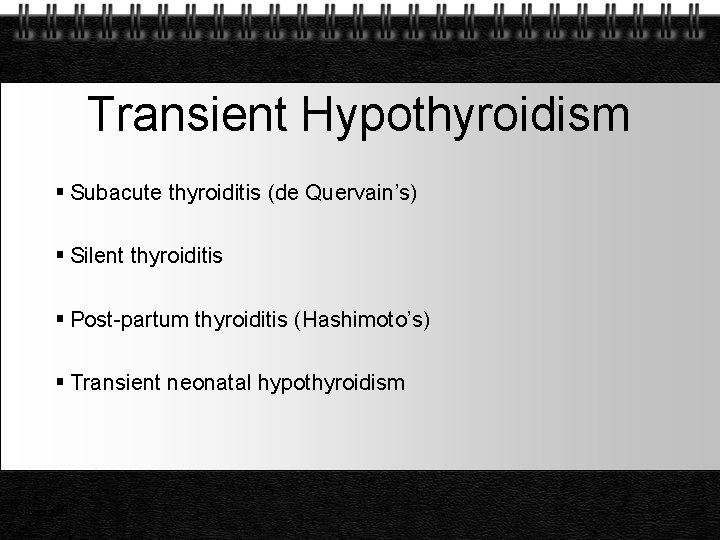
Transient Hypothyroidism Subacute thyroiditis (de Quervain’s) Silent thyroiditis Post-partum thyroiditis (Hashimoto’s) Transient neonatal hypothyroidism Page 11
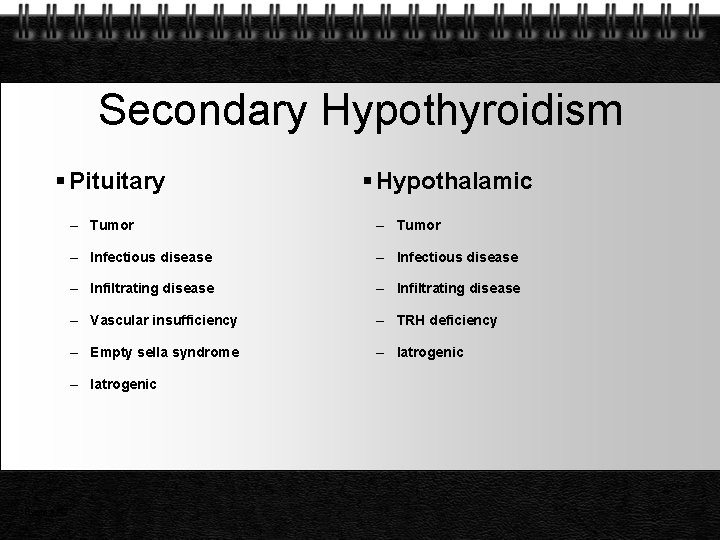
Secondary Hypothyroidism Pituitary – Tumor – Infectious disease – Infiltrating disease – Vascular insufficiency – TRH deficiency – Empty sella syndrome – Iatrogenic Page 12 Hypothalamic
Manifestations Page
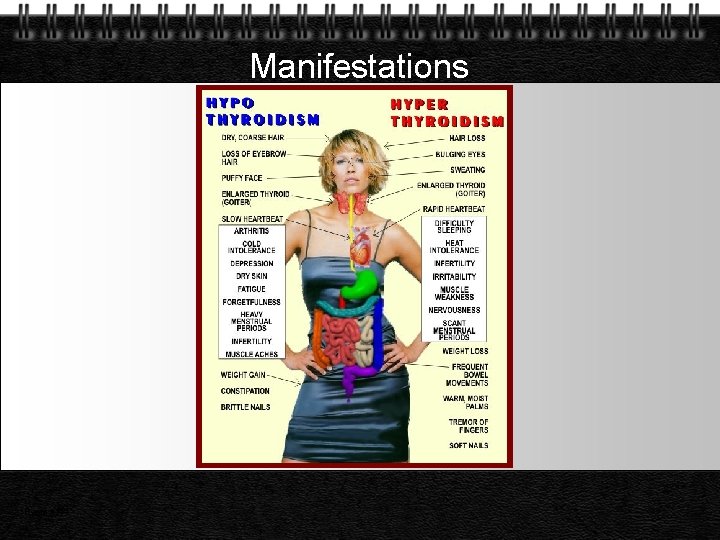
Manifestations Page 14

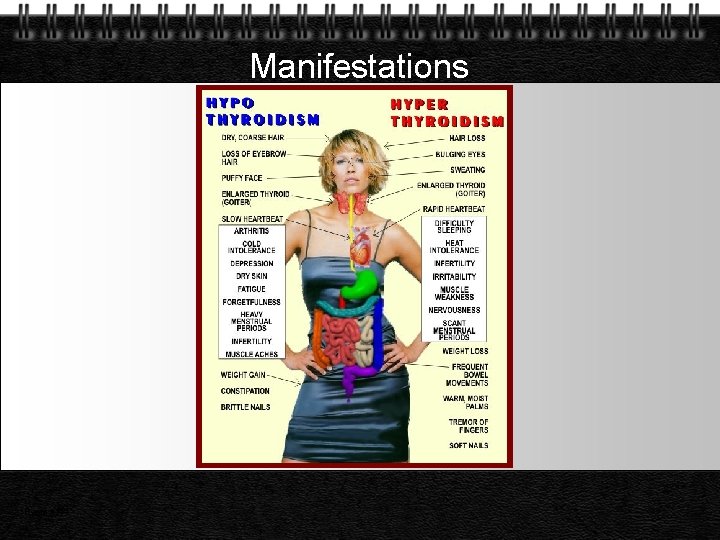
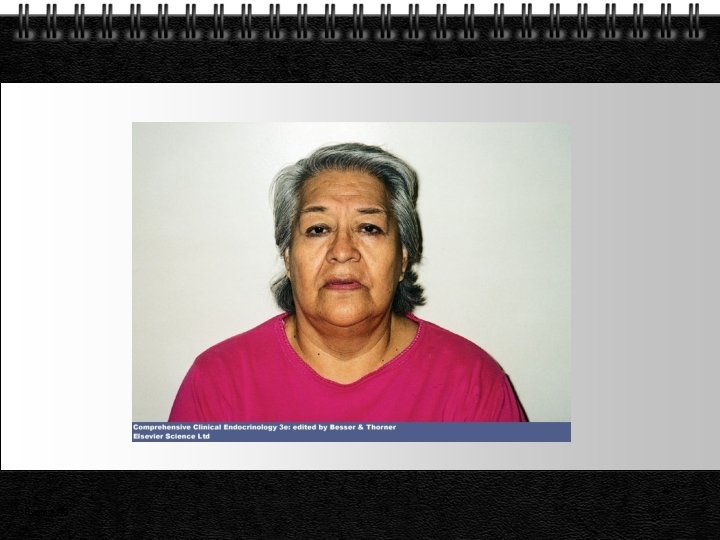
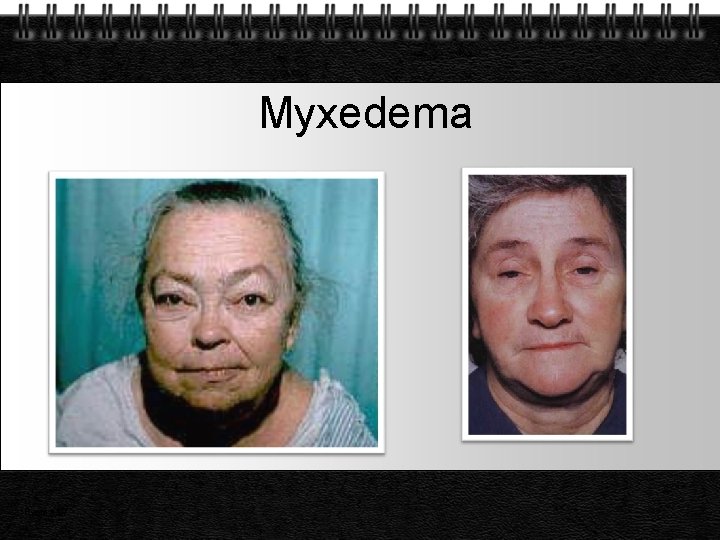
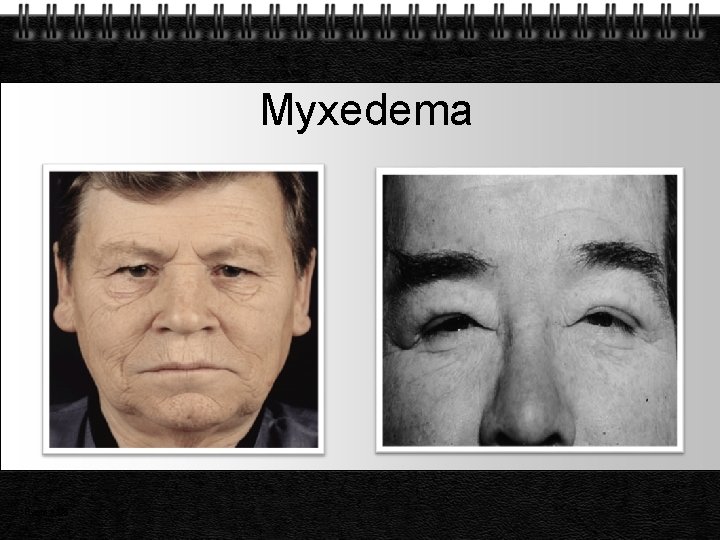
Skin and Appendages – Myxedema (hyaluronic acid accumulation) – Pale, cool and dry skin, hypercarotenemia – Tongue is enlarged – Thickened laryngeal/pharyngeal mucous membranes – Slow wound healing, bruising – Dry, brittle hair – Temporal loss of eyebrows – Brittle nails Page 15
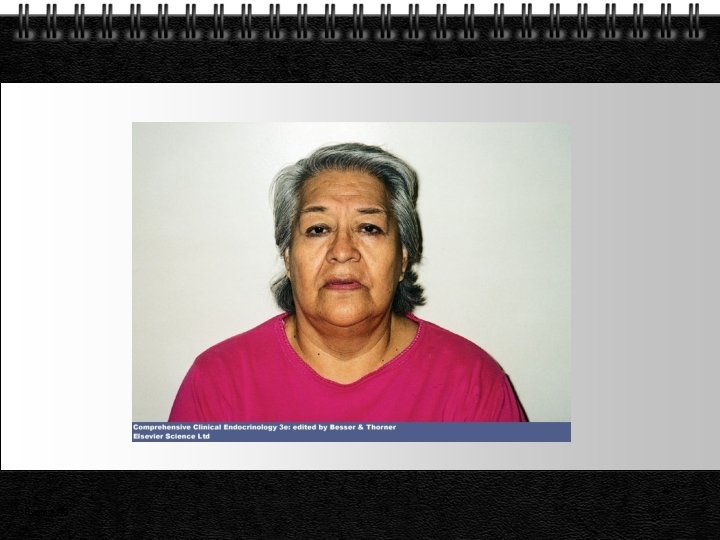
Page 16
Cardiovascular System – Decreased cardiac output (stroke volume + heart rate) – Increased peripheral vascular resistance – Narrow pulse pressure – Pericardial effusion, dilated myocardium – Coronary atherosclerosis (HT, HL) – ECG changes (bradycardia, low amplitude QRS, prolonged PR, ST alterations) Page 17

Respiratory System – Pleural effusions – Decreased ventilatory drive (hypercapnia, hypoxemia) – Involvement of respiratory muscles – Obstructive sleep apnea Page 18
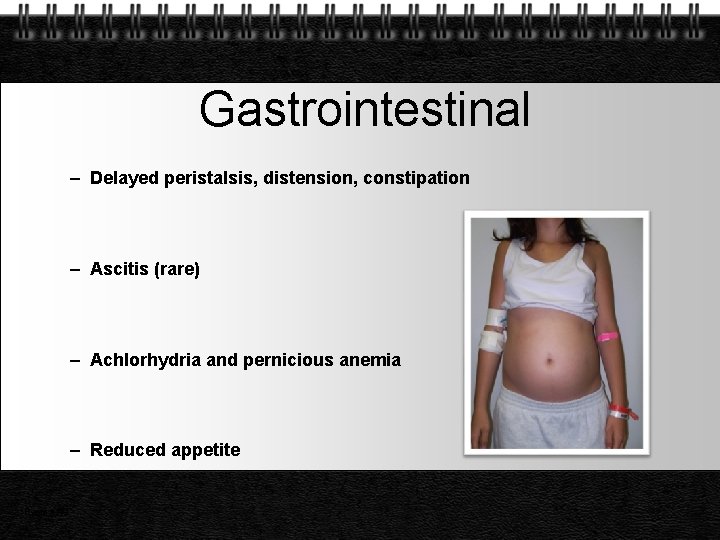
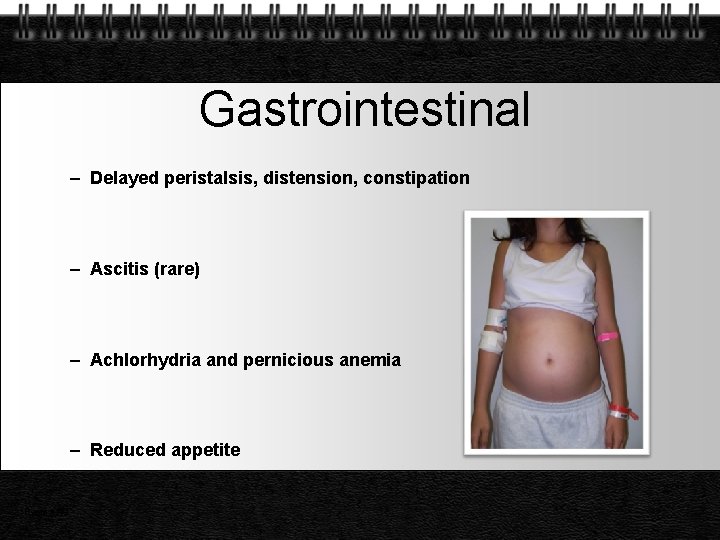
Gastrointestinal – Delayed peristalsis, distension, constipation – Ascitis (rare) – Achlorhydria and pernicious anemia – Reduced appetite Page 19

Musculoskletal – Delayed, abnormal epiphyseal ossification – Impaired linear growth (short limbs) and bone age – Myalgias (inflamation, infiltration) – Joint effusions Page 20
Neuropsychiatric – Decreased cerebral perfusion, myelination, and cortical development- retardation – Slow speech, lack of concentration and memory, depression, paranoia – Delay in the relaxation phase of DTR – Delayed nerve conduction, carpal tunnel syndrome – Perceptive hearing loss (Pendred Synd. ) Page 21

Reproductive System – Delayed puberty – Oligomenorrhea and menorrhagia – Reduced fertility – Oligospermia and erectile dysfunction – Hyperprolactinemia Page 22
Other – Decreased erythropoetin (anemia) – Decreased Factor 8 and 9 – Low basal metabolic rate – Increased cholesterol, TG, LDL and decreased HDL Page 23
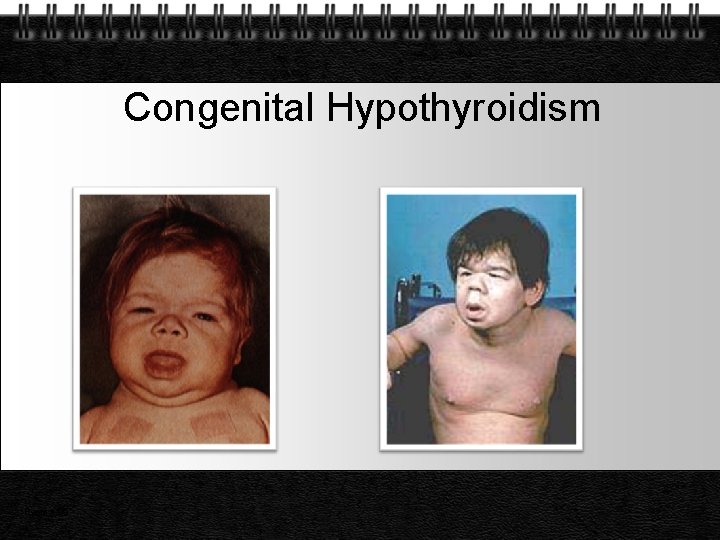
Infantile Hypothyroidism (Cretinism) Retardation of mental development and growth Protuberant abdomen, umblical hernia, dry skin, poor hair and nail growth, delayed teeth eruption, waddling gait Epiphysial dysgenesis Page 24
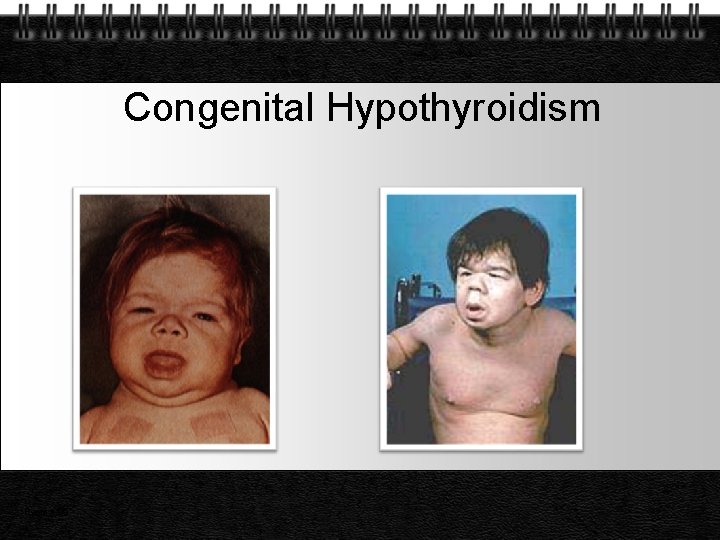
Congenital Hypothyroidism Page 25
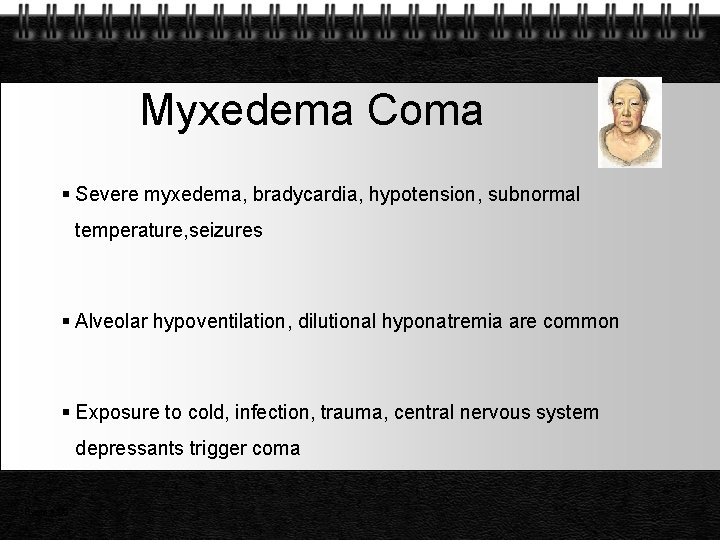
Myxedema Coma Severe myxedema, bradycardia, hypotension, subnormal temperature, seizures Alveolar hypoventilation, dilutional hyponatremia are common Exposure to cold, infection, trauma, central nervous system depressants trigger coma Page 26
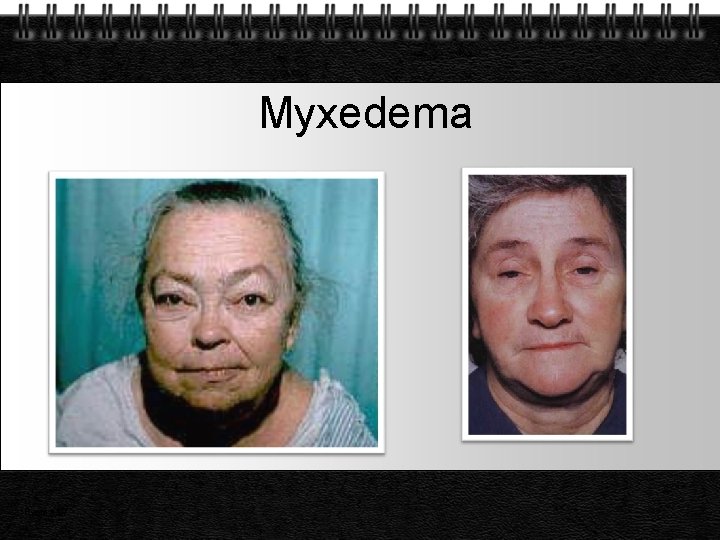
Myxedema Page 27
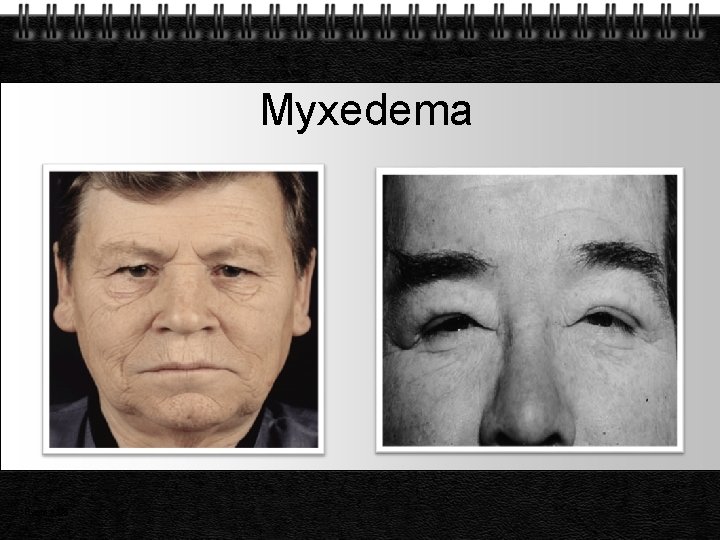
Myxedema Page 28

Solid Oedema Page 29 Xanthomata
Diagnosis Page
Laboratory Tests TSH T 3 and T 4 Thyroid antibodies RAIU Serum lipids CK, SGOT, LDH Hemogram Page 31
Differential Diagnosis Elderly patients Chronic renal failure Nephrotic states Pernicious anemia Euthyroid Sick Syndrome Down Syndrome Page 32
Co-morbidity Hypercholesterolemia Depression Infertility – Menstrual Irregularities Diabetes mellitus Page 33
Hypothyroidism and Hypercholesterolemia 14% of patients with elevated cholesterol have hypothyroidism Approximately 90% of patients with overt hypothyroidism have increased cholesterol and / or triglycerides Page 34

Lipids in Patient with Hypothyroidism Hypercholesterolemi a (>200 mg/d. L) Hypertriglyceridemia (>150 mg/d. L) N= 268 Hypercholesterolemi a and mild Hyper TG Normal Lipids Page 35
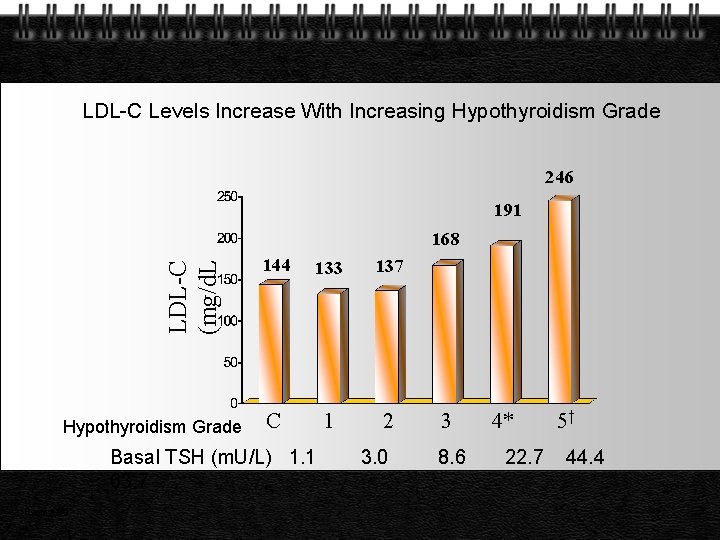
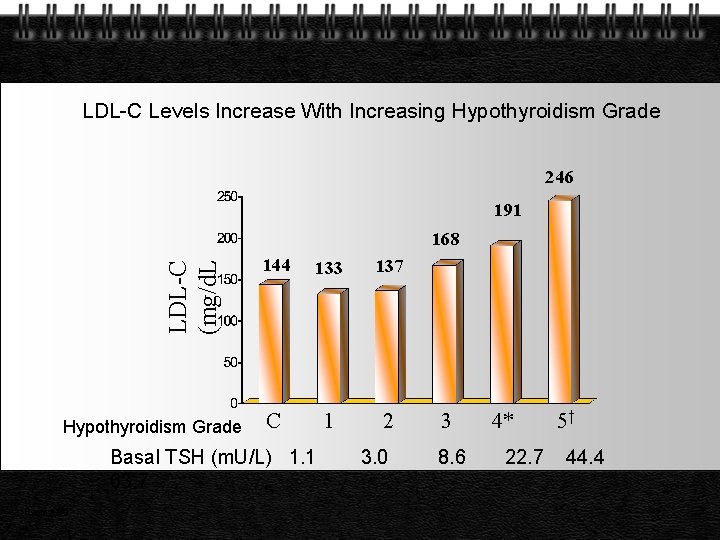
LDL-C Levels Increase With Increasing Hypothyroidism Grade 246 191 LDL-C (mg/d. L 168 Hypothyroidism Grade 144 133 137 C 1 2 Basal TSH (m. U/L) 1. 1 63. 7 Page 36 3. 0 3 8. 6 4* 22. 7 5† 44. 4
Hypothyroidism and Depression Depressive symptoms are common in hypothyroidism Many hypothyroid patients fulfill DSM-IV criteria for a depressive disorder Depressed patients may be more likely than normal individuals to be hypothyroid All depressed patients should be evaluated for thyroid dysfunction Page 37
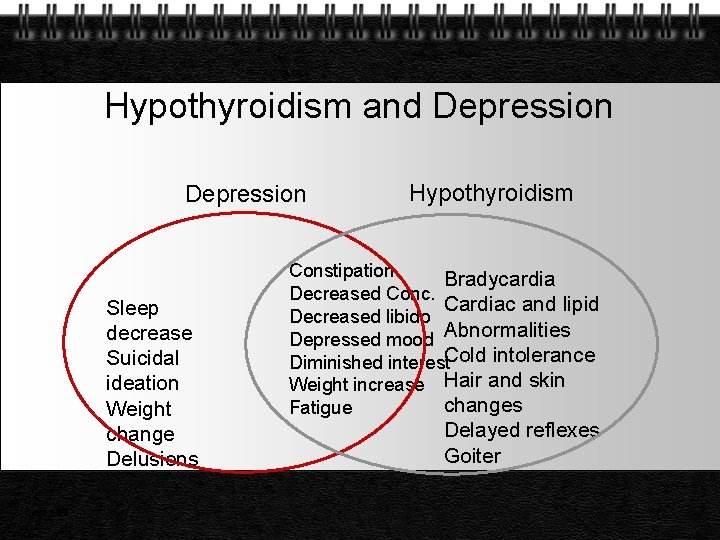
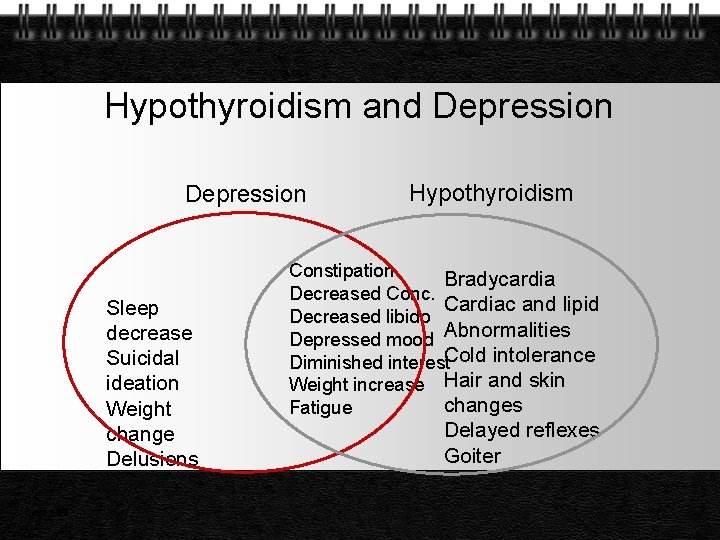
Hypothyroidism and Depression Sleep decrease Suicidal ideation Weight change Delusions Page 38 Hypothyroidism Constipation Bradycardia Decreased Conc. Cardiac and lipid Decreased libido Depressed mood Abnormalities Diminished interest. Cold intolerance Weight increase Hair and skin changes Fatigue Delayed reflexes Goiter
Hypothyroidism and Infertility 1. Hypothyroidism associated with infertility, miscarriage, stillbirth 2. Infertility : Evaluate thyroid function, treat hypothyroidism 3. Equivocal results: Begin therapy; discontinue if no pregnancy for several months. Page 39
Suspect Hypothyroidism 1. Amenorrhea 2. Oligomenorrhea 3. Menorrhogia 4. Galactorrhea 5. Premature ovarian failure 6. Infertility 7. Decreased libido 8. Precocious / delayed puberty Page 40
Hypothyroidism and Diabetes 1. Approximately 10% of patients with type 1 diabetes mellitus develop sub-clinical hypothyroidism 2. In diabetic patients - examine for goitre 3. TSH measurement at regular intervals Page 41
Hormone Replacement Page
Many Causes, One Treatment Goal : Normalize TSH level regardless of cause of hypothyroidism Treatment : Once daily dosing with Levothyroxine sodium (1. 6 µg/kg/day) Monitor TSH levels at 6 to 8 weeks, after initiation of therapy or dosage change Page 43
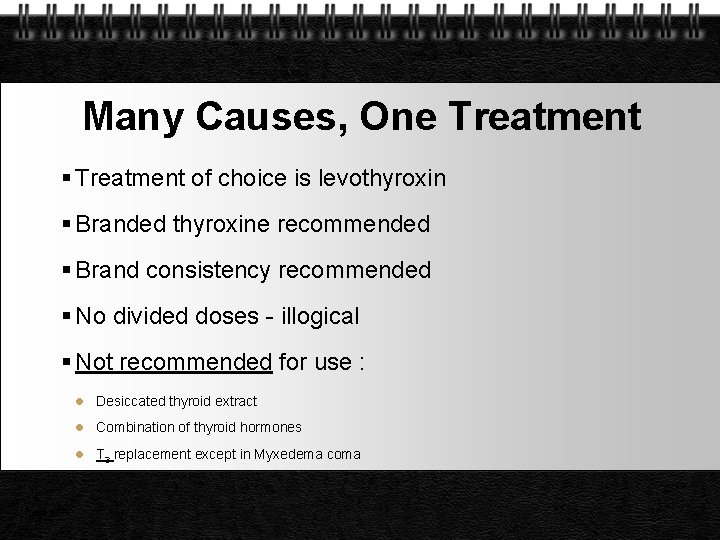
Many Causes, One Treatment of choice is levothyroxin Branded thyroxine recommended Brand consistency recommended No divided doses - illogical Not recommended for use : Page 44 l Desiccated thyroid extract l Combination of thyroid hormones l T 3 replacement except in Myxedema coma

Dosage Adjustments Age (in elderly start with half dose) Severity and duration of hypothyroidism (↑ dose) Weight (0. 5µg/kg/day ↑ upto 3. 0µg/kg/day) Malabsorption (requires ↑ dose) Concomitant drug therapy (only on empty stomach) Pregnancy ( 25% ↑ in dose), safe in lactating mother Presence of cardiac disease (start alt. day Rx) Page 45
Start Low and Go Slow Starting dose for healthy patients < 50 years at 1. 0 µg/kg/day Starting dose for healthy patients > 50 years should be < 0, 50 µg/day. Dose ↑ by 25 µg, if needed, at 6 to 8 weeks intervals. Starting dose for patients with heart disease should be Page 46 12. 5 to 25 µg/day and increase by 12. 5 to 25 µg/day, if

How the Patient Improves l Feels better in 2 – 3 weeks l Reduction in weight is the first improvement l Facial puffiness then starts coming down l Skin changes, hair changes take long time to regress l TSH starts showing decrements from the high values l TSH returns to normal eventually Page 47

Drug Interactions Reduced Absorption Page 48 l Cholestyramine resin l Sucralfate l Drugs that affect metabolism l Rifampin Ferrous sulfate l Carbamazepine l Soybean formula l Phenytoin l Aluminum hydroxide l Colestipol hydrochloride l Phenobarbitol l Amiodarone
Inappropriate Dosage Over-replacement risks Reduced bone density / osteoporosis Tachycardia, arrhythmia. atrial fibrillation In elderly or patients with heart disease, angina, arrhythmia, or myocardial infarction Under-replacement risks Continued hypothyroid state Long-term end-organ effects of hypothyroidism Increased risk of hyperlipidemia Page 49
Special Situations Page
Sub-clinical Hypothyroidism Chronic autoimmune thyroiditis Graves’ hyperthyroidism with radioiodine, surgery Inadequate replacement therapy for hypothyroidism Lithium carbonate therapy (for depressive illness) Page 51
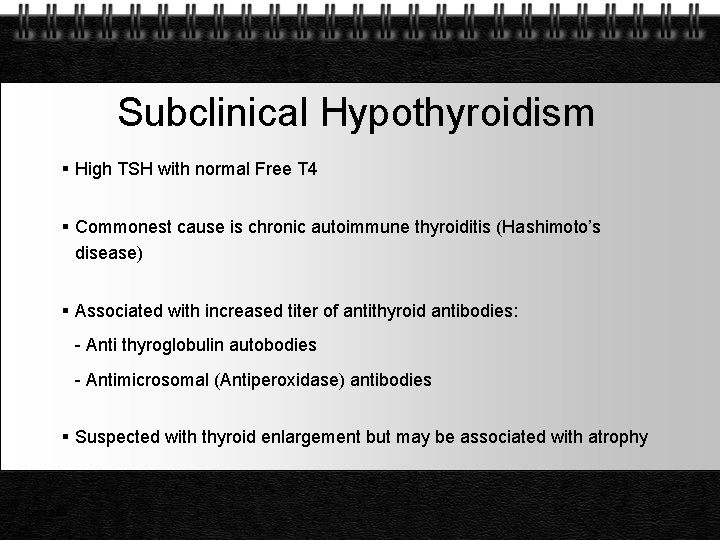
Subclinical Hypothyroidism High TSH with normal Free T 4 Commonest cause is chronic autoimmune thyroiditis (Hashimoto’s disease) Associated with increased titer of antithyroid antibodies: - Anti thyroglobulin autobodies - Antimicrosomal (Antiperoxidase) antibodies Suspected with thyroid enlargement but may be associated with atrophy Page 52

Prognosis May stay sub clinical May progress to clinical 5% per year with positive antibodies In elderly risk is 20%/ year Page 53
Post-Partum Thyroiditis Definition Occurrence of hyperthyroidism and / or hypothyroidism during the postpartum period in women who were euthryroid during pregnancy At Highest Risk Patients with type 1 diabetes, previous history of PPT or other autoimmune disease such as Hashimoto’s disease and Graves’ disease Page 54

Sick Euthyroid Syndrome l Total T 3 reduced l FT 3 reduced l Total T 4 reduced l FT 4 Normal l TSH Normal l Clinically Euthyroid Page 55
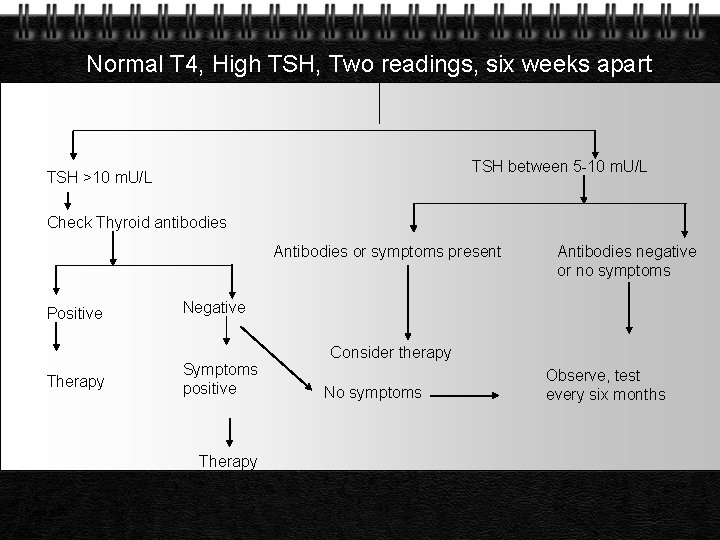
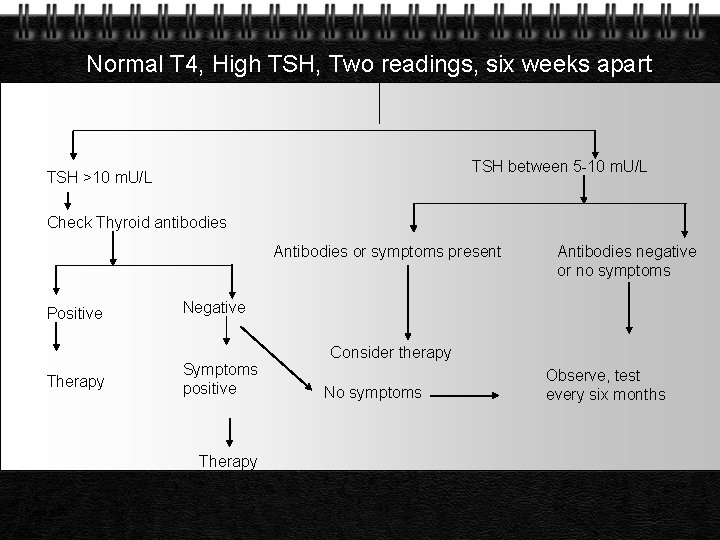
Normal T 4, High TSH, Two readings, six weeks apart TSH between 5 -10 m. U/L TSH >10 m. U/L Check Thyroid antibodies Antibodies or symptoms present Positive Therapy Negative Symptoms positive Therapy Page 56 Antibodies negative or no symptoms Consider therapy No symptoms Observe, test every six months
Thank You Page
 Ascaris lumbricoides ova
Ascaris lumbricoides ova Masaryk university medical faculty
Masaryk university medical faculty Yeditepe edu
Yeditepe edu Coadsysexam yeditepe
Coadsysexam yeditepe Yeditepe coadsys exam
Yeditepe coadsys exam Sinan aydın mali müşavir
Sinan aydın mali müşavir Nizamettin aydin
Nizamettin aydin Nizamettin aydin
Nizamettin aydin Aydın kendirci
Aydın kendirci Thede loder
Thede loder Sevil aydın
Sevil aydın Aydın bir türk kadınıyım
Aydın bir türk kadınıyım Bushra hasan
Bushra hasan Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Prof. dr. nizamettin aydin
Prof. dr. nizamettin aydin Coordination
Coordination Package diagram
Package diagram Aydin marine
Aydin marine Aydın başar
Aydın başar This generation of computers used transistors
This generation of computers used transistors Nazmi aydın
Nazmi aydın Aydin bal
Aydin bal Aydın kekemelik merkezi
Aydın kekemelik merkezi Medical faculty in novi sad dean
Medical faculty in novi sad dean University of split faculty of maritime studies
University of split faculty of maritime studies Bridgeport engineering department
Bridgeport engineering department University of bridgeport computer science faculty
University of bridgeport computer science faculty Hubert kairuki memorial university faculty of medicine
Hubert kairuki memorial university faculty of medicine Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Applied medical sciences
Applied medical sciences Fsu computer science
Fsu computer science Mendel university - faculty of business and economics
Mendel university - faculty of business and economics Singularity university faculty
Singularity university faculty Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Faculty of engineering university of porto
Faculty of engineering university of porto Webkredit cuni
Webkredit cuni Faculty of veterinary medicine cairo university logo
Faculty of veterinary medicine cairo university logo Faculty of law of the university of zagreb
Faculty of law of the university of zagreb University of montenegro faculty of law
University of montenegro faculty of law University of kragujevac faculty of technical sciences
University of kragujevac faculty of technical sciences University of cologne faculty of management
University of cologne faculty of management Leading university sylhet tuition fees
Leading university sylhet tuition fees Hacettepe university faculty of medicine
Hacettepe university faculty of medicine Brown university computer science
Brown university computer science Faculty of veterinary medicine - university of tehran
Faculty of veterinary medicine - university of tehran Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Lebanese university faculty of engineering
Lebanese university faculty of engineering York university concurrent education
York university concurrent education Faculty of economics and business debrecen
Faculty of economics and business debrecen Clemson electrical engineering
Clemson electrical engineering Faculty of veterinary medicine cairo university
Faculty of veterinary medicine cairo university Faculty of mechanical engineering thammasat university
Faculty of mechanical engineering thammasat university Mendel university faculty of business and economics
Mendel university faculty of business and economics Mahidol university public health
Mahidol university public health University of pecs faculty of health sciences
University of pecs faculty of health sciences Faculty of education khon kaen university
Faculty of education khon kaen university Chula communication arts
Chula communication arts