Ulcers of the oral Cavity Dr Arshad M





- Slides: 45
Ulcers of the oral Cavity Dr: Arshad M. Malik Associate Professor Surgery LUMHS
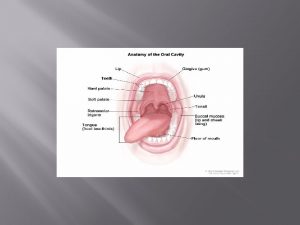
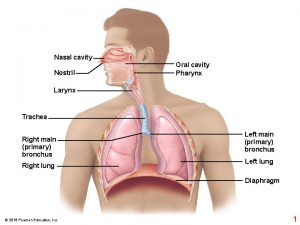
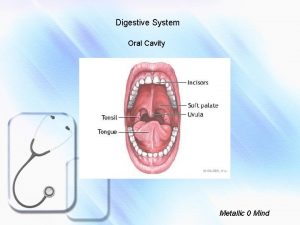
ORAL CAVITY • • LIPS TEETH GINGIVA ORAL MUCOUS MEMBRANES PALATE TONGUE ORAL LYMPHOID TISSUES
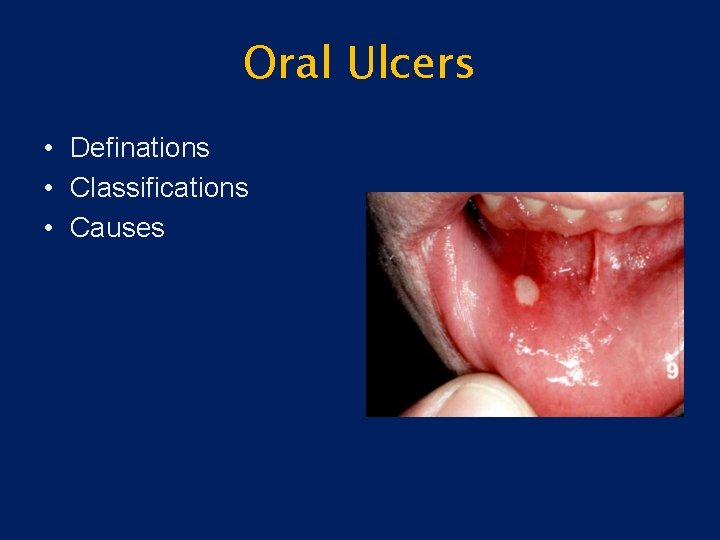
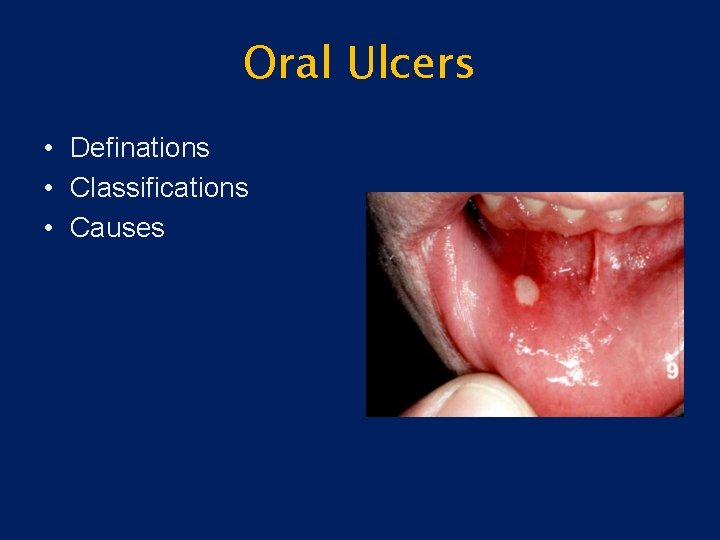
Oral Ulcers • Definations • Classifications • Causes
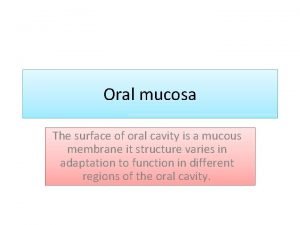
Definition • Injury to the oral mucosa may result in a localized defect of the surface in which the covering epithelium is destroyed leaving an inflammed area of exposed connective tissue. Such defects or erosions are called Ulcers.
Classification • Traumatic • Recurrent apthous stomatitis (RAS). • Ulcers associated with systemic diseases and vesicolobulous disease(Pemphigus, pemphigoid, erythema multiform) • (Dermatitis herpetiformis epidermolysis bullosa)
Causes of Oral ulceration 1. Infective, viral, bacterial, fungal. 2. Traumatic. • Mechanical • Thermal • Chemical • Factitious injury • Radiation • Eosinophilic ulcer or traumatic granuloma 3. Idiopathic • Recurrent apthous stomatitis (RAS) • Minor apthous ulcers • Major apthous ulcers • Herpitiform ulcers
Causes contd; 4. Associated with systemic diseases • Hematological diseases • Gastrointestinal diseases • Behcet syndrome • HIV infection • Other diseases 5. Associated with dermatological conditions • Lichen Plannus • Chronic discoid lupus erythromatous • Vesiculobullous dseases 6. Neoplastic • Squamous cell carcinoma • Other malignant tumors
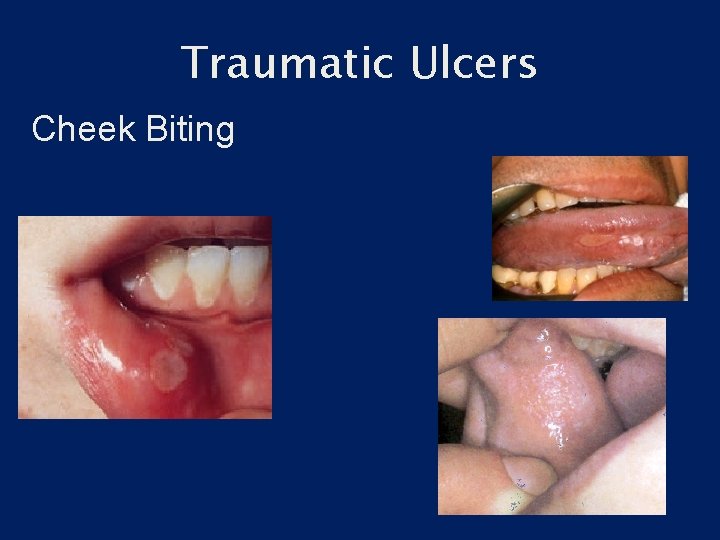
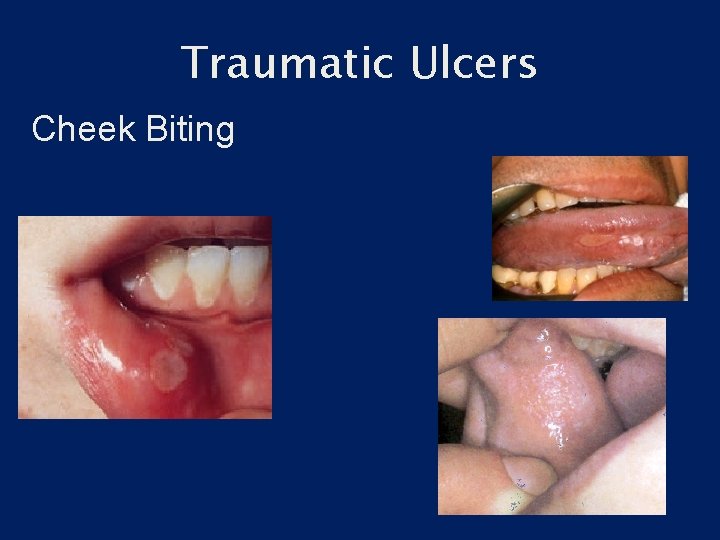
Traumatic Ulcers Cheek Biting
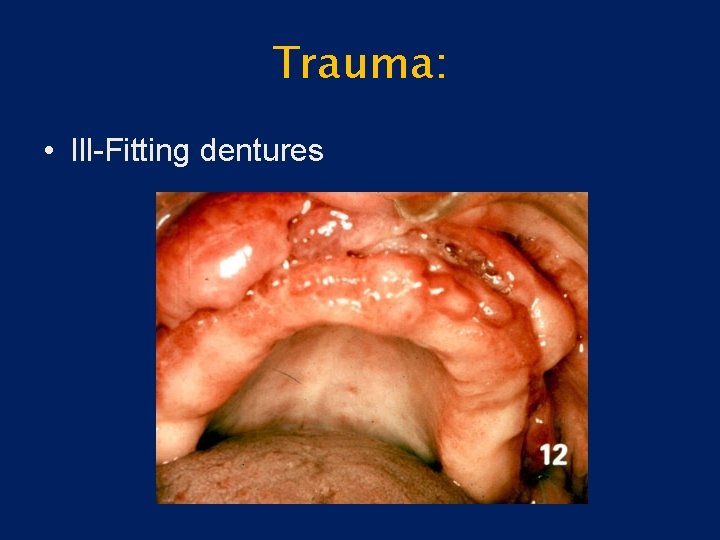
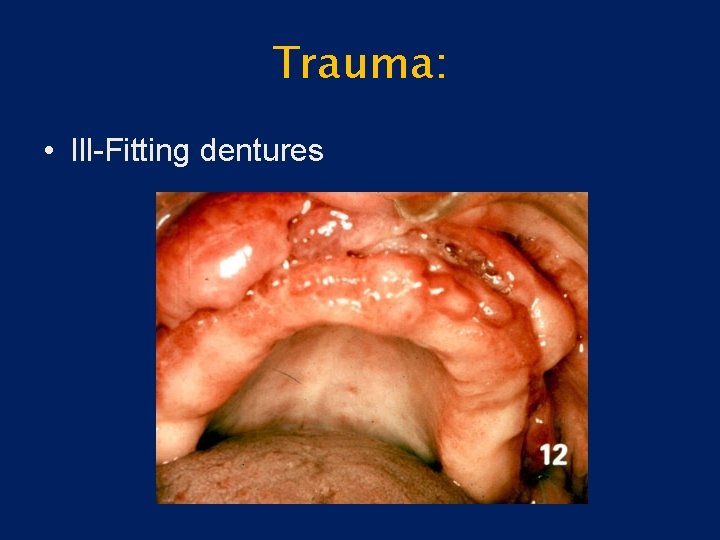
Trauma: • Ill-Fitting dentures
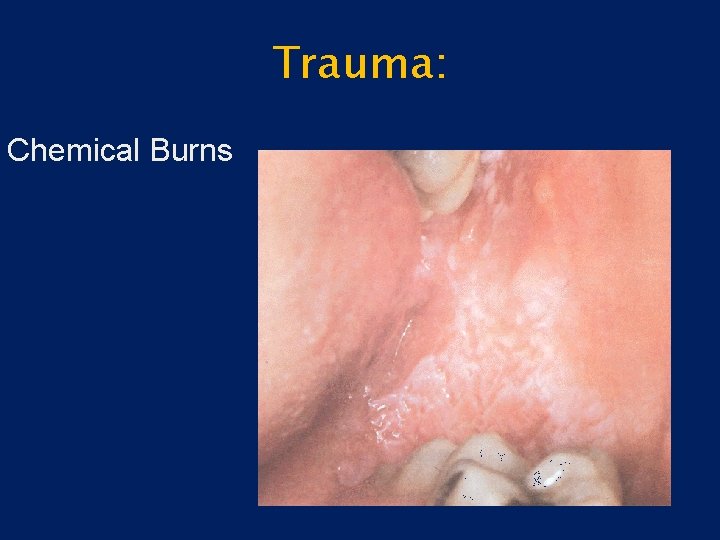
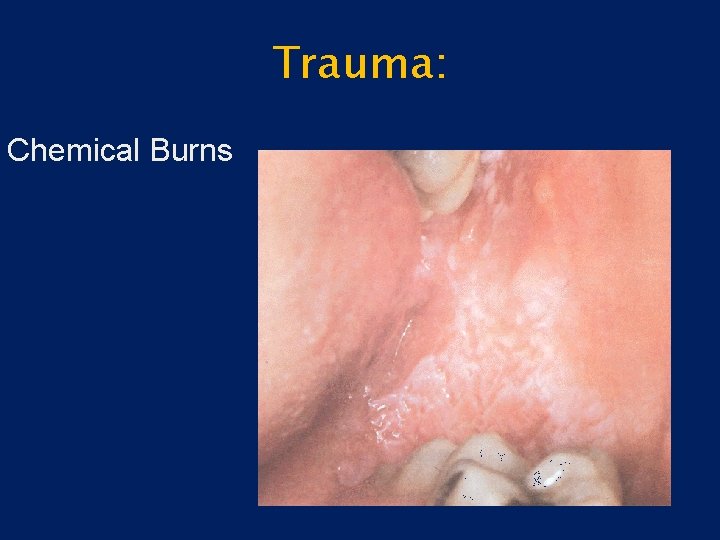
Trauma: Chemical Burns
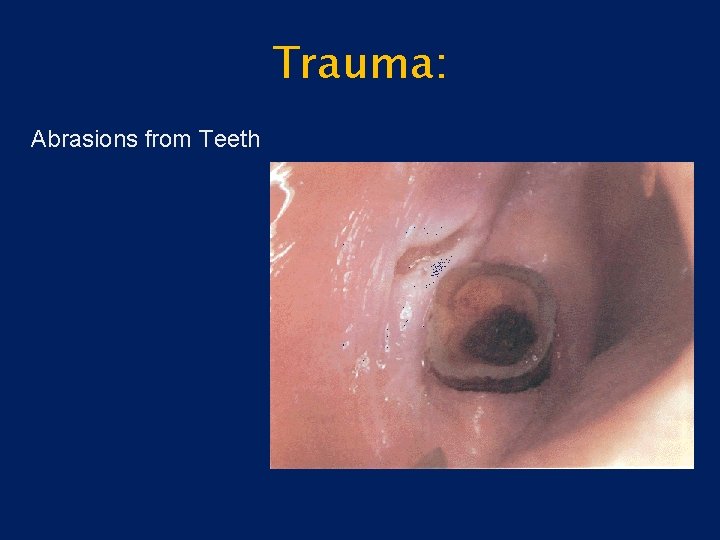
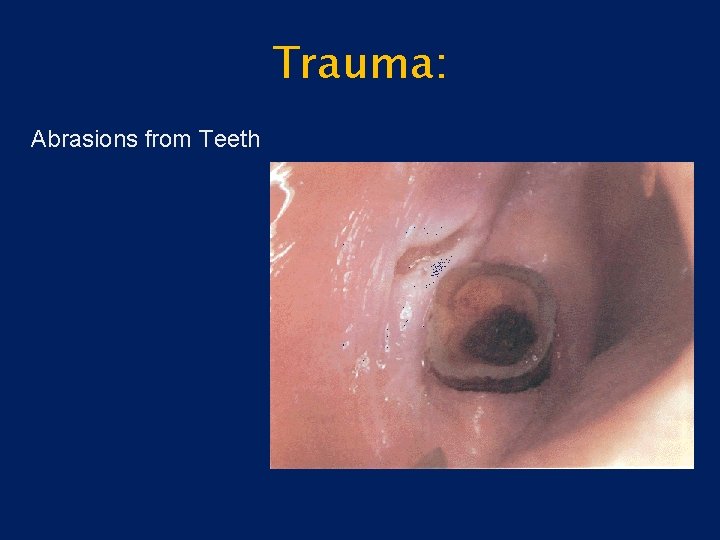
Trauma: Abrasions from Teeth
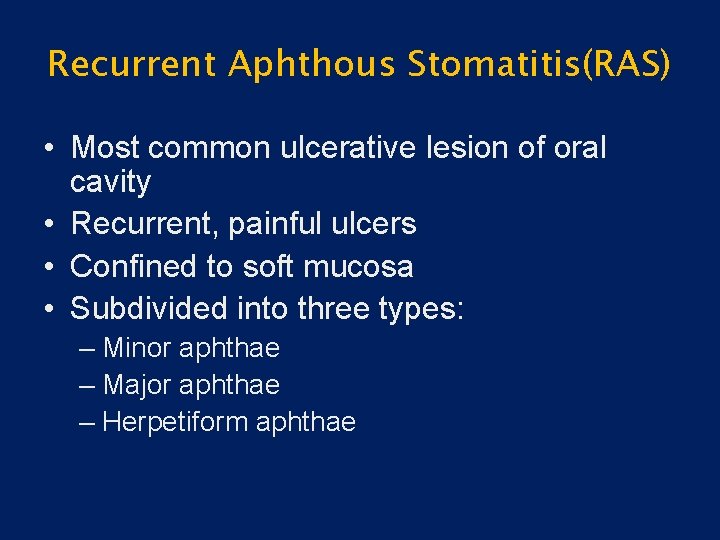
Recurrent Aphthous Stomatitis(RAS) • Most common ulcerative lesion of oral cavity • Recurrent, painful ulcers • Confined to soft mucosa • Subdivided into three types: – Minor aphthae – Major aphthae – Herpetiform aphthae
Apthous ulcers contd: • Etiology • A. Not understood but damaging immune response in increasingly implicated. Some of the factors are related to the cause 1. Immunological factors 2. Heredity factors 3. Microbiological factors 4. Emotional stress 5. Nutritional deficiencies 6. Allergic disorders 7. Hematological factors 8. Gastrointestinal factors.
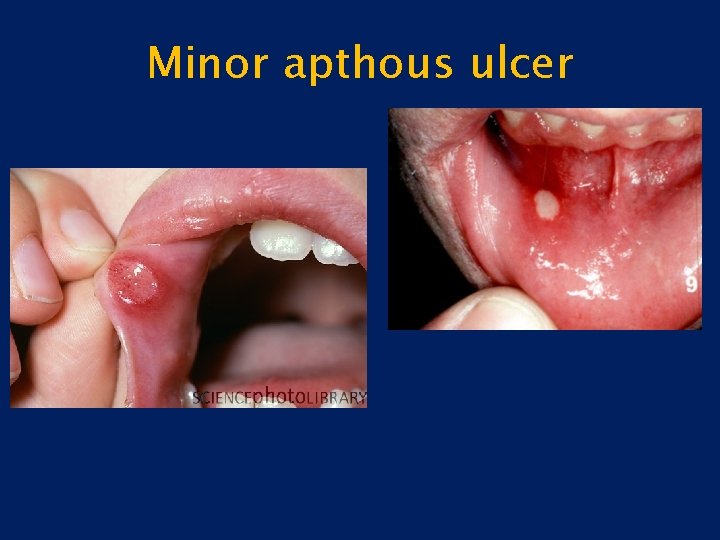
Recurrent apthous ulcer stomatitis contd: • C/F Minor apthous ulcers 1. Prodromal signs appear hours before with burning and itching. 2. Comprise more than 80% 3. May be shallow and round affecting the 4. Non-keratinized part of the oral epithelium. 5. Diameter of ulcer is less than 10 mm with red margin. 6. Heal without scarring within 7 -10 days. 7. Tend to recur with in 1 -4 months. 8. Site is usually the tongue, buccal mucosa, soft palate.
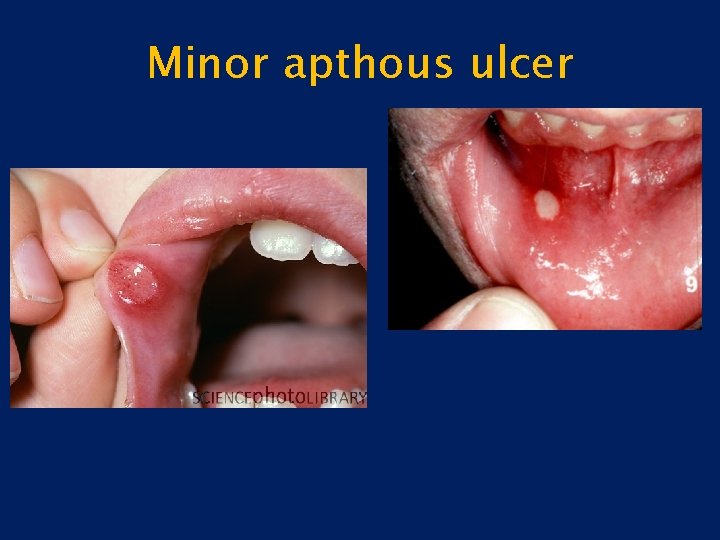
Minor apthous ulcer
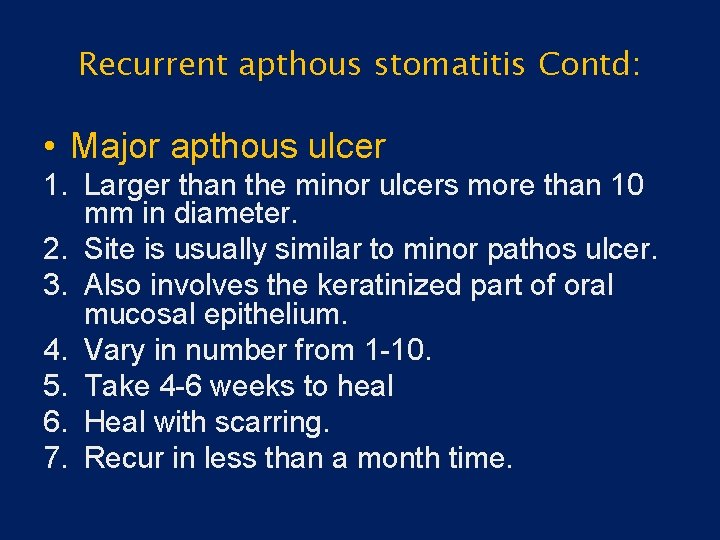
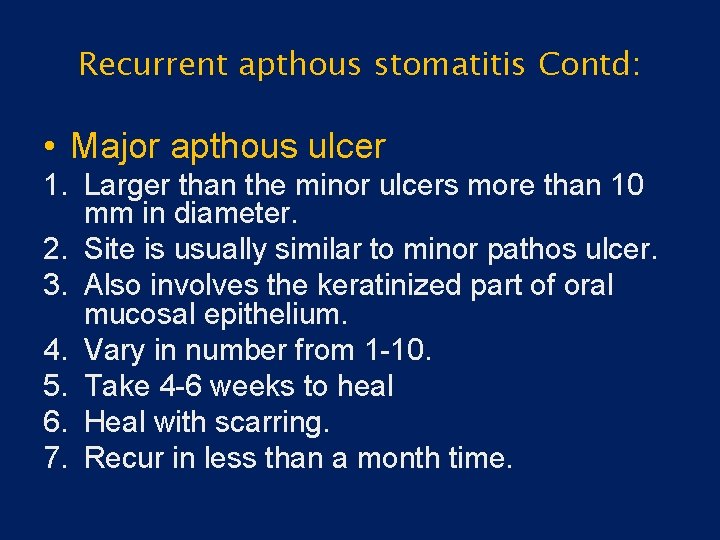
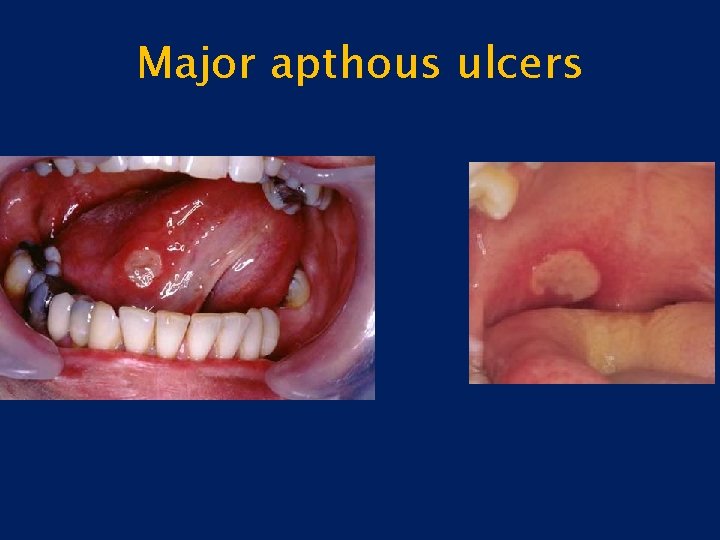
Recurrent apthous stomatitis Contd: • Major apthous ulcer 1. Larger than the minor ulcers more than 10 mm in diameter. 2. Site is usually similar to minor pathos ulcer. 3. Also involves the keratinized part of oral mucosal epithelium. 4. Vary in number from 1 -10. 5. Take 4 -6 weeks to heal 6. Heal with scarring. 7. Recur in less than a month time.
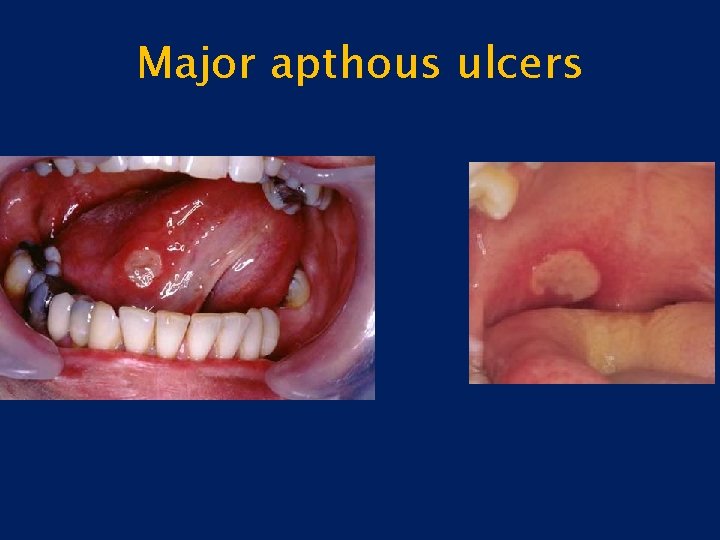
Major apthous ulcers
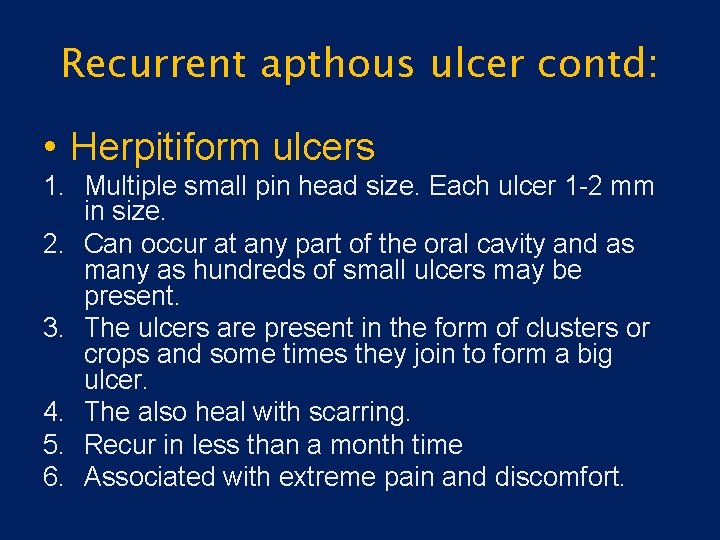
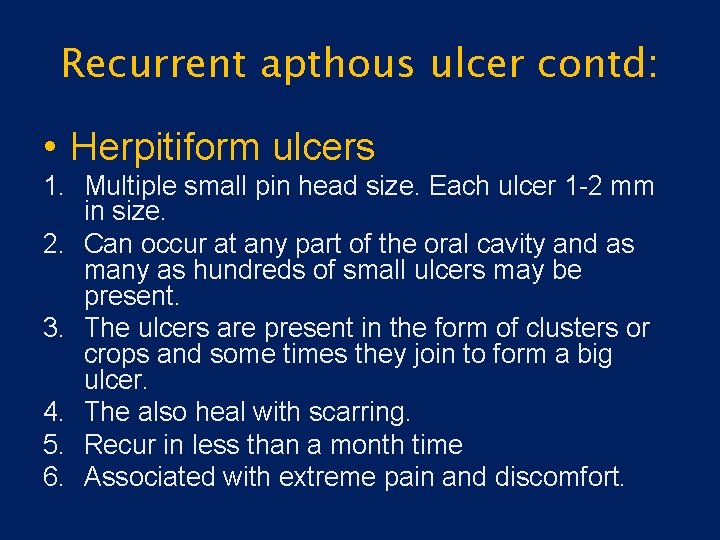
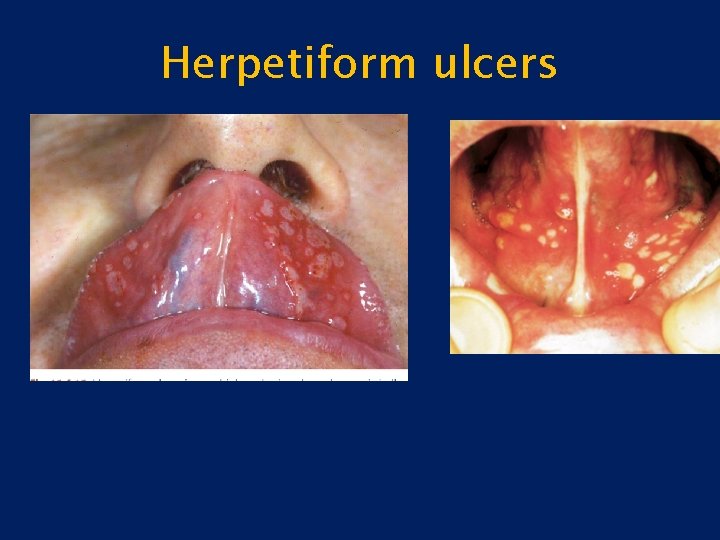
Recurrent apthous ulcer contd: • Herpitiform ulcers 1. Multiple small pin head size. Each ulcer 1 -2 mm in size. 2. Can occur at any part of the oral cavity and as many as hundreds of small ulcers may be present. 3. The ulcers are present in the form of clusters or crops and some times they join to form a big ulcer. 4. The also heal with scarring. 5. Recur in less than a month time 6. Associated with extreme pain and discomfort.
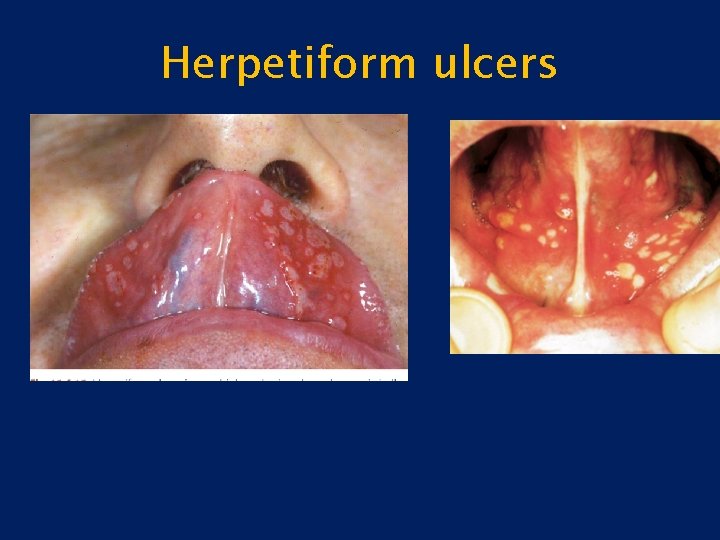
Herpetiform ulcers
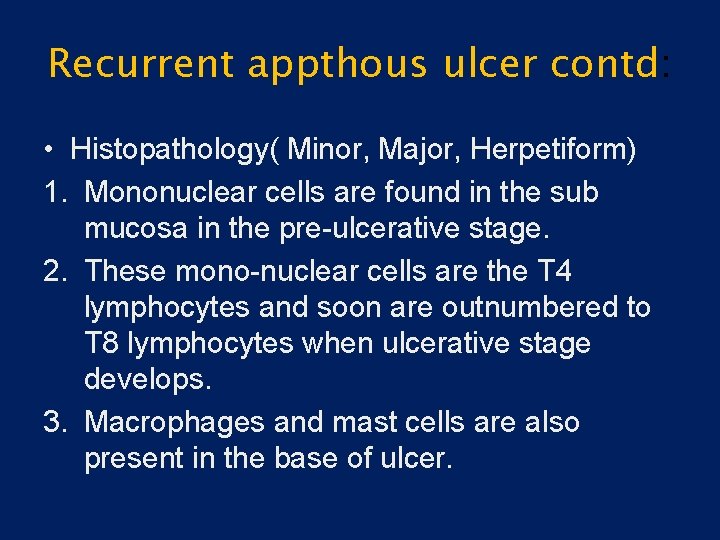
Recurrent appthous ulcer contd: • Histopathology( Minor, Major, Herpetiform) 1. Mononuclear cells are found in the sub mucosa in the pre-ulcerative stage. 2. These mono-nuclear cells are the T 4 lymphocytes and soon are outnumbered to T 8 lymphocytes when ulcerative stage develops. 3. Macrophages and mast cells are also present in the base of ulcer.
Treatment • Major, Minor, Herpetiform ulcers. 1. Minor apthous ulcers require no treatment only topical gels are used to minimize the pain, as the ulcer is self limiting and heals with in 7 -10 days. 2. Anti inflammatory gels and mouth washes are also used to prevent any further infection and to control the inflammation caused by the ulcer. 3. For major apthos ulcers topical steroids may be used. 4. In extreme severe cases systemic steroids such as prednisolone in doses 20 -40 mg daily have giving promising results.
Behcet’s • Symptom complex of: – Recurrent aphthous ulcers of the mouth – Painful genital ulcers – Uveitis or conjuctivitis

Herpesvirus Infection • HSV-1 and/or HSV-2 – Primary Infection – Secondary Infection • Varicella zoster virus (HHV-3)
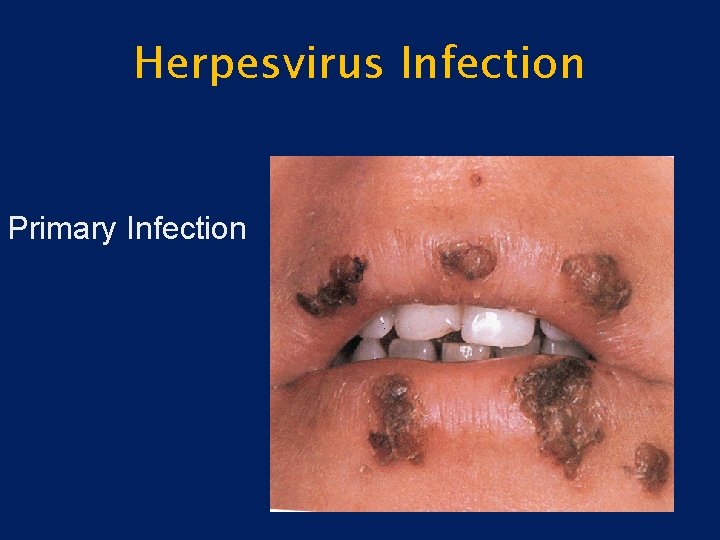
Herpesvirus Infection • Primary Infection – Herpetic gingivostomatitis – Younger patients – Often asymptomatic – May be associated with fever, chills, malaise – Vesicles-ulcers-crusting – Anywhere in the oral cavity
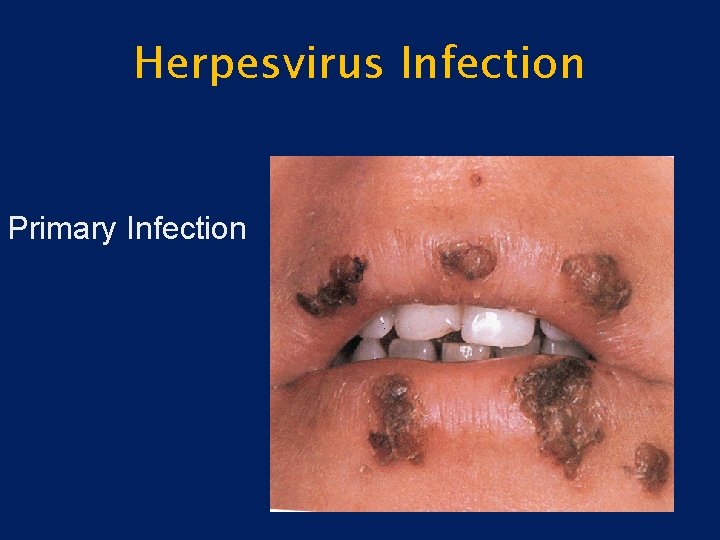
Herpesvirus Infection Primary Infection
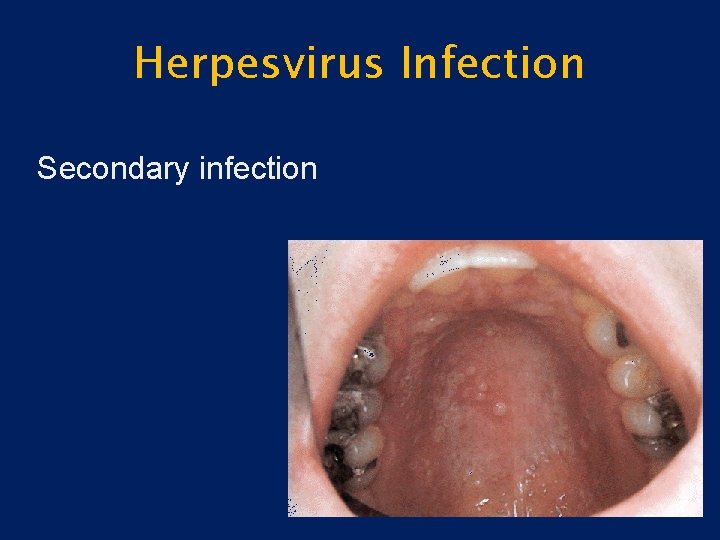
Herpesvirus Infection • Secondary Infection – Reactivation of latent virus – Not associated with systemic symptoms – Small vesicles – Occur only on the hard palate and gingiva – Prodromal signs
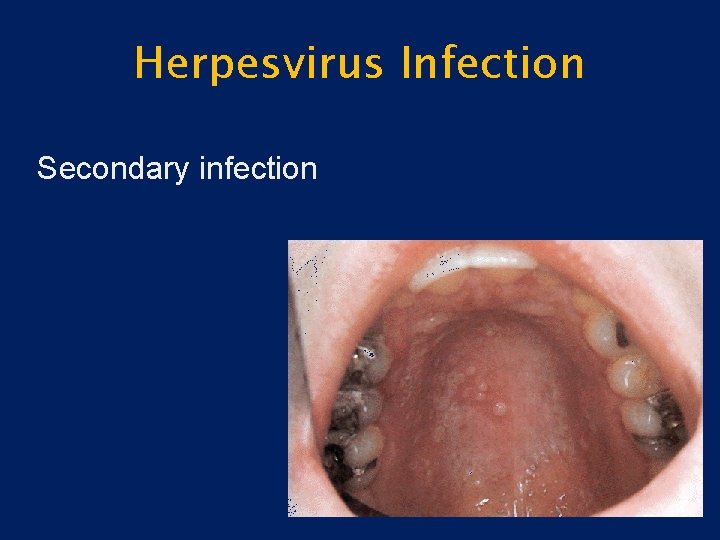
Herpesvirus Infection Secondary infection
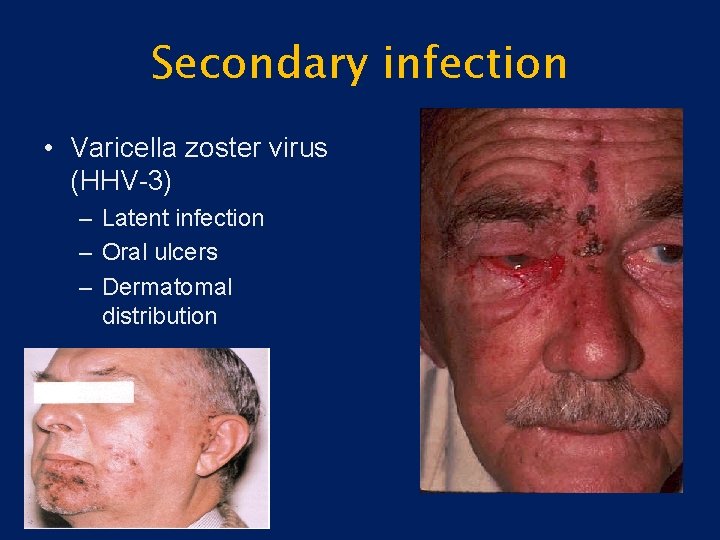
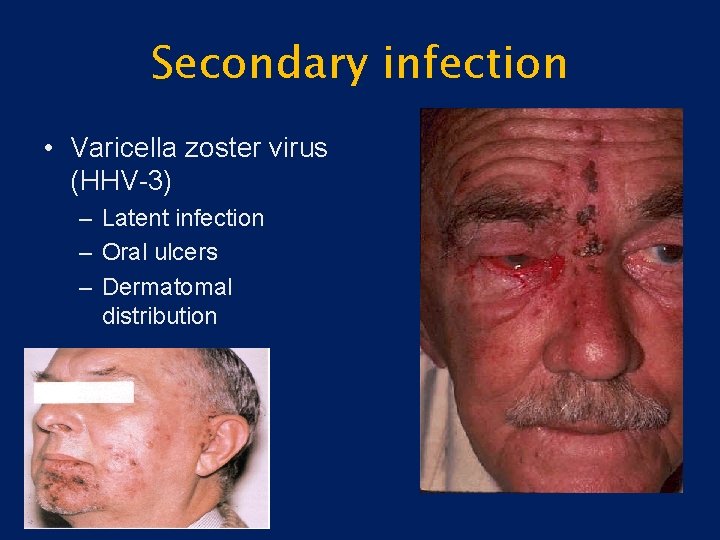
Secondary infection • Varicella zoster virus (HHV-3) – Latent infection – Oral ulcers – Dermatomal distribution
Infection • • • Rare HIV/AIDS patients Bacterial Deep mycotic infection Candida
Infection • Bacterial – Usually secondary infection – Primary infection: syphilis, tuberculous, or actinomycosis

Infection Bacterial-Syphilis
Infection • Mycotic – Blastomycosis – Histoplasmosis
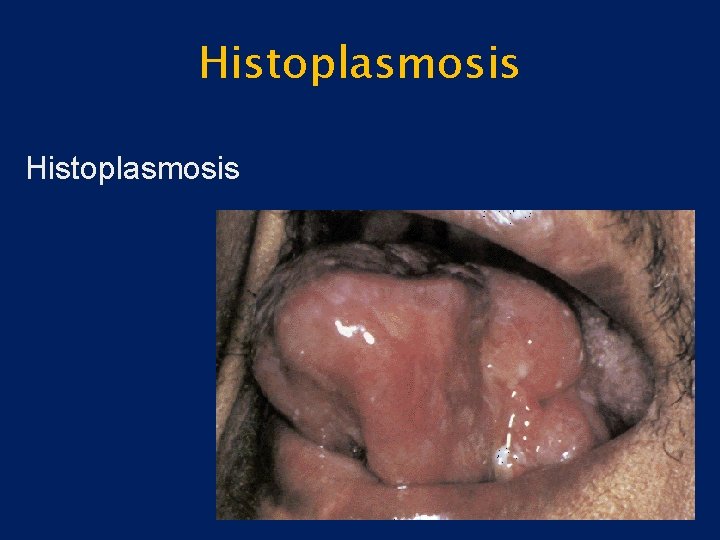
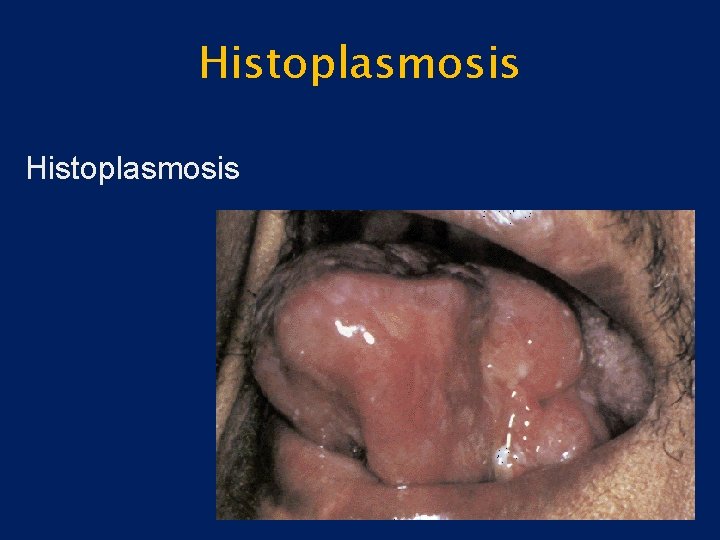
Histoplasmosis
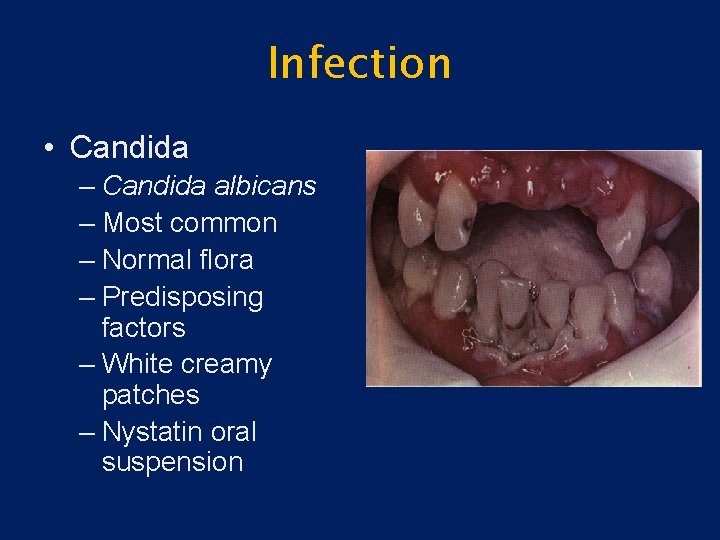
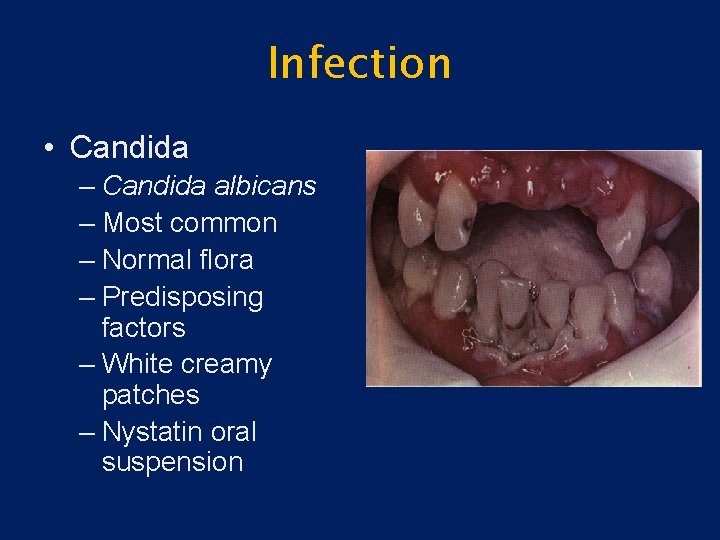
Infection • Candida – Candida albicans – Most common – Normal flora – Predisposing factors – White creamy patches – Nystatin oral suspension

Infection • Candida
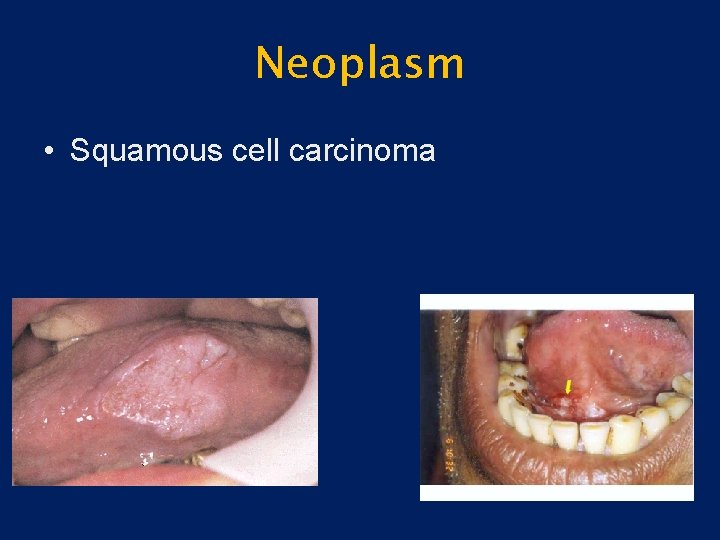
Neoplasm • Squamous cell carcinoma (SCC) – Most common – Irregular ulcers with raised margins – May be exophytic, infiltrative or verrucoid – Mimic benign lesions grossly
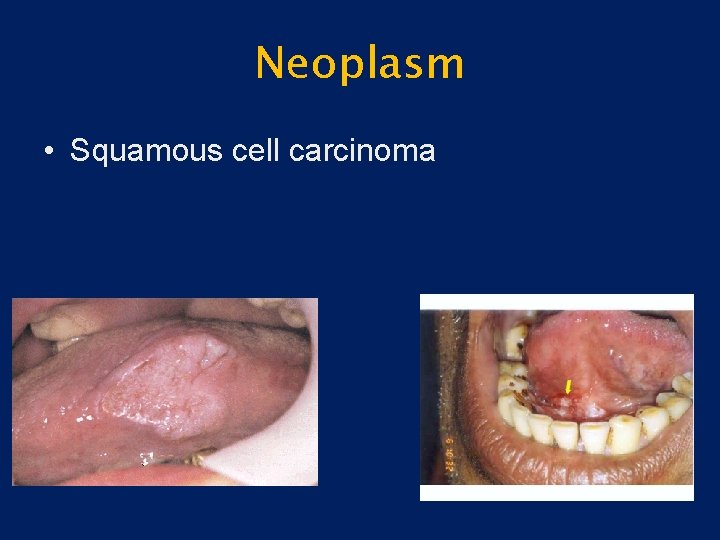
Neoplasm • Squamous cell carcinoma
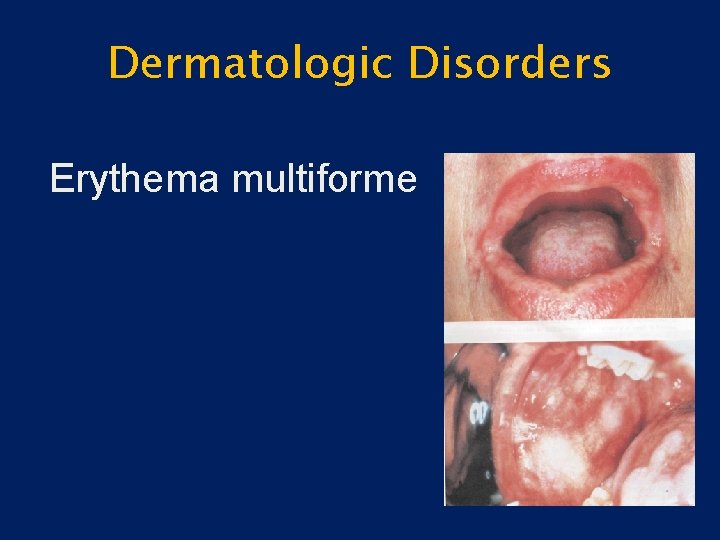
Dermatologic Disorders • Erythema multiforme – Rapidly progressive – Antigen-antibody complex deposition in vessels of the dermis – Target lesions of the skin – Diffuse ulceration, crusting of lips, tongue, buccal mucosa – Self-limited, heal without scarring
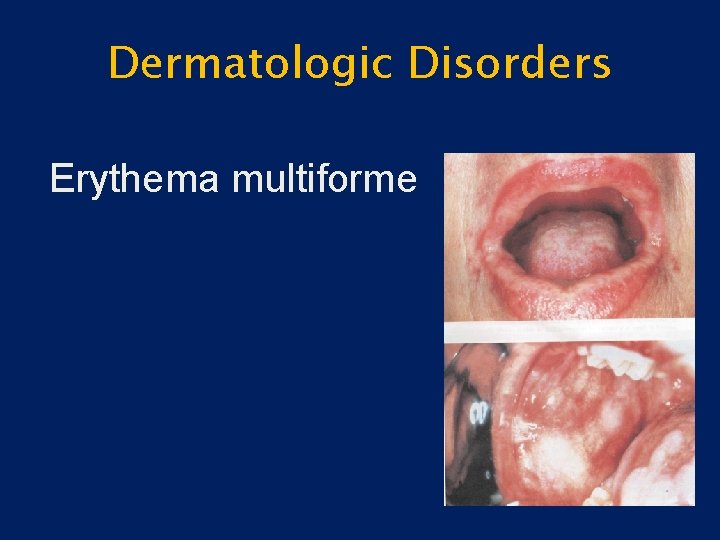
Dermatologic Disorders Erythema multiforme
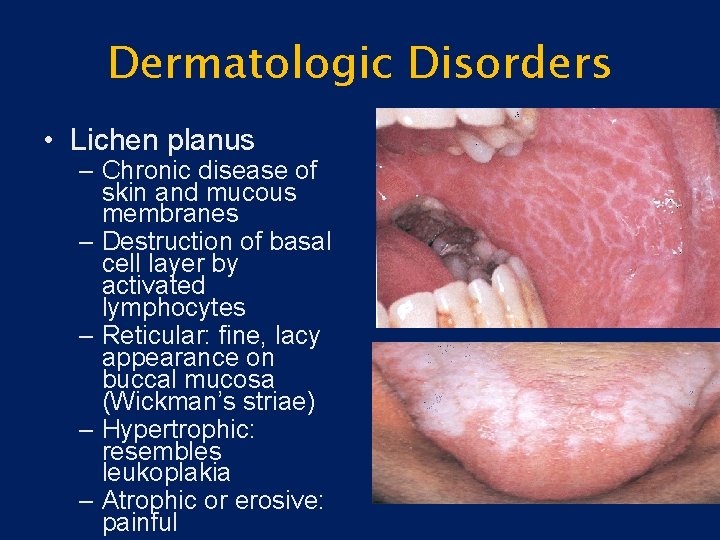
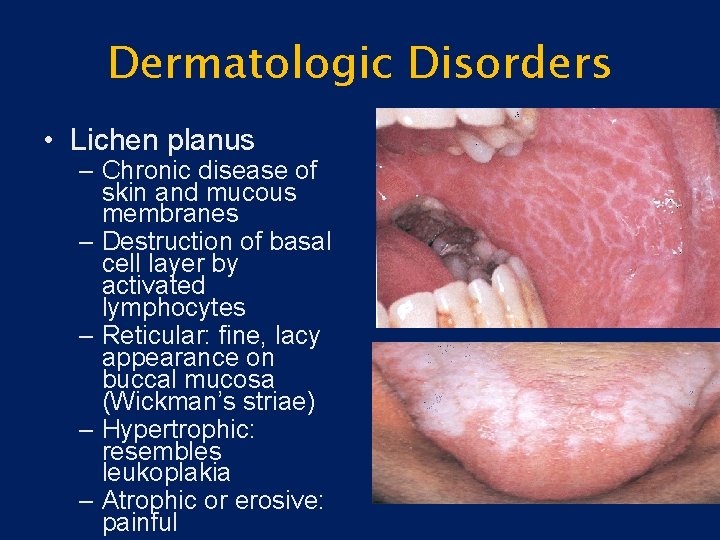
Dermatologic Disorders • Lichen planus – Chronic disease of skin and mucous membranes – Destruction of basal cell layer by activated lymphocytes – Reticular: fine, lacy appearance on buccal mucosa (Wickman’s striae) – Hypertrophic: resembles leukoplakia – Atrophic or erosive: painful

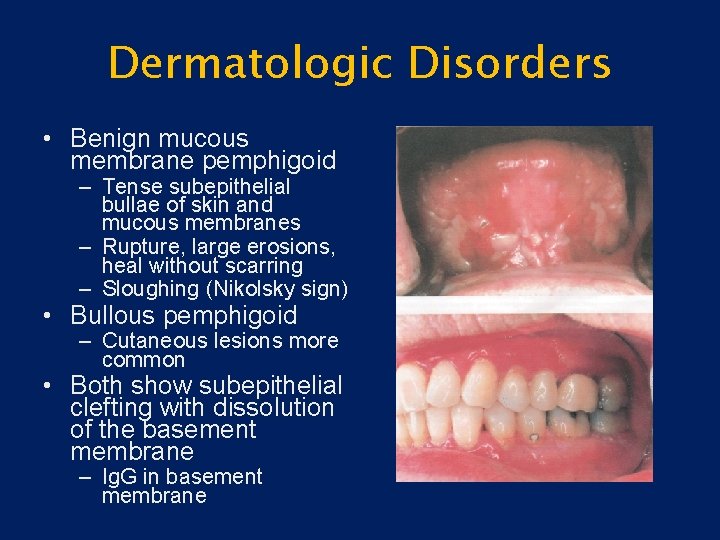
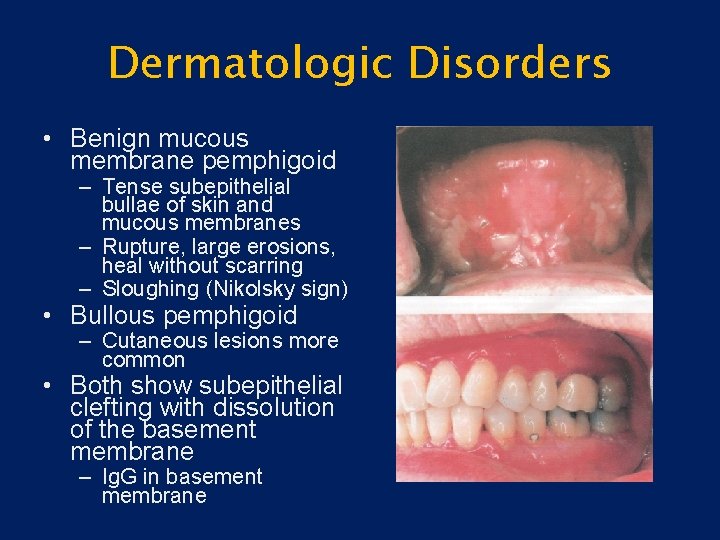
Dermatologic Disorders • Benign mucous membrane pemphigoid – Tense subepithelial bullae of skin and mucous membranes – Rupture, large erosions, heal without scarring – Sloughing (Nikolsky sign) • Bullous pemphigoid – Cutaneous lesions more common • Both show subepithelial clefting with dissolution of the basement membrane – Ig. G in basement membrane
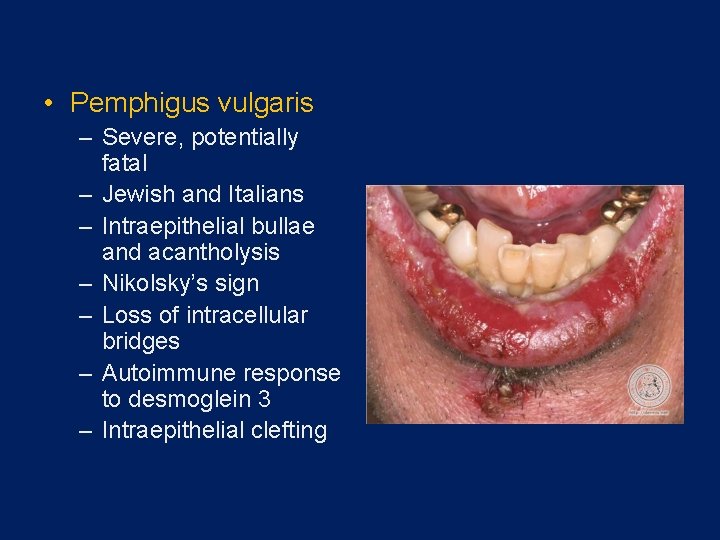
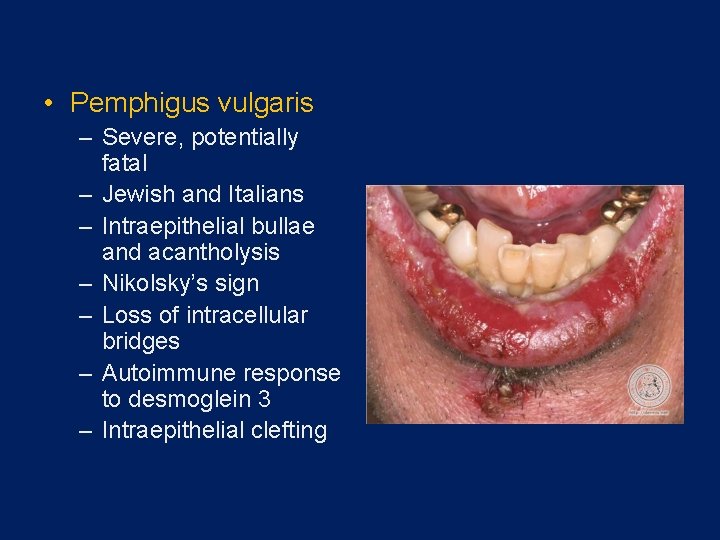
• Pemphigus vulgaris – Severe, potentially fatal – Jewish and Italians – Intraepithelial bullae and acantholysis – Nikolsky’s sign – Loss of intracellular bridges – Autoimmune response to desmoglein 3 – Intraepithelial clefting

Thanks for your attention
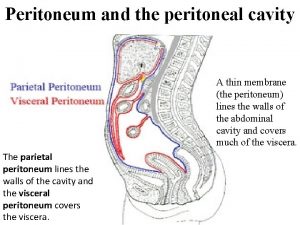
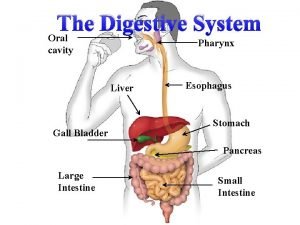
 Body cavity
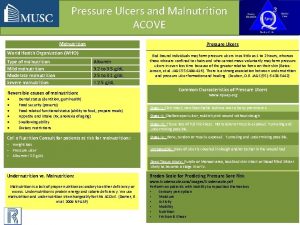
Body cavity Types of ulcer edge
Types of ulcer edge Continuous bedside pressure mapping
Continuous bedside pressure mapping Anorexia and stomach ulcers
Anorexia and stomach ulcers Acute gastritis
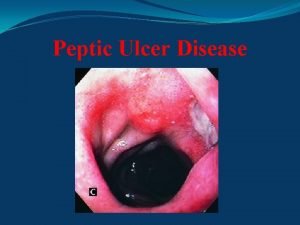
Acute gastritis Stomach ulcer definition
Stomach ulcer definition May and kuster perforator
May and kuster perforator Typhoid ulcer and tuberculous ulcer
Typhoid ulcer and tuberculous ulcer What causes ulcers
What causes ulcers Gastric ucler
Gastric ucler Lesser peritoneal cavity
Lesser peritoneal cavity Gastric veins
Gastric veins Dorsal cavity
Dorsal cavity The abdominal cavity is to the thoracic cavity
The abdominal cavity is to the thoracic cavity Arshad usmani
Arshad usmani New kuwait
New kuwait Dr arshad ali khan
Dr arshad ali khan Arshad mansoor
Arshad mansoor Reactive airways dysfunction syndrome
Reactive airways dysfunction syndrome Dr arshad ejazi
Dr arshad ejazi Arshad habib
Arshad habib Naveed arshad lums
Naveed arshad lums Normal flora of oral cavity
Normal flora of oral cavity The vestibule
The vestibule Mouth landmarks
Mouth landmarks Monophasic and biphasic liquid dosage forms
Monophasic and biphasic liquid dosage forms Epithelial component
Epithelial component Classification of white lesions of oral cavity
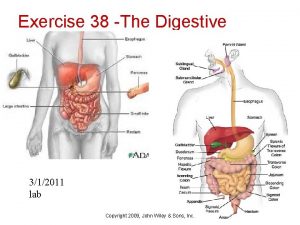
Classification of white lesions of oral cavity Exercise 38
Exercise 38 Roof of buccal cavity
Roof of buccal cavity Pharynx digestion
Pharynx digestion Pharynx to esophagus
Pharynx to esophagus ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Tư thế ngồi viết
Tư thế ngồi viết Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Bổ thể
Bổ thể Tư thế ngồi viết
Tư thế ngồi viết Ví dụ về giọng cùng tên
Ví dụ về giọng cùng tên Thể thơ truyền thống
Thể thơ truyền thống Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Hổ sinh sản vào mùa nào
Hổ sinh sản vào mùa nào đại từ thay thế
đại từ thay thế Diễn thế sinh thái là
Diễn thế sinh thái là