Triage Priority Wang TzongLuen MD Ph D FESC










- Slides: 65
Triage Priority Wang, Tzong-Luen, MD, Ph. D, FESC, FACC
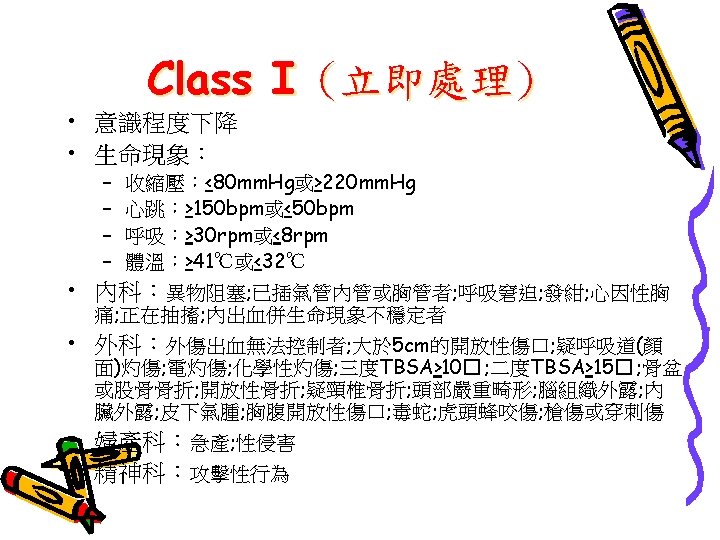








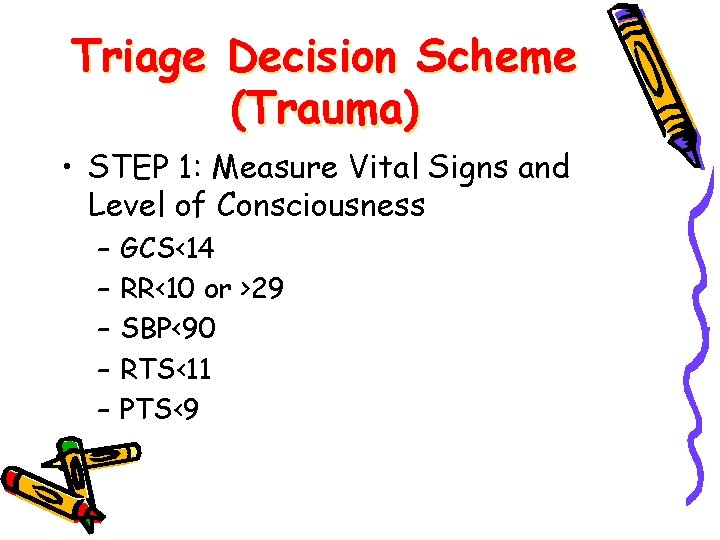
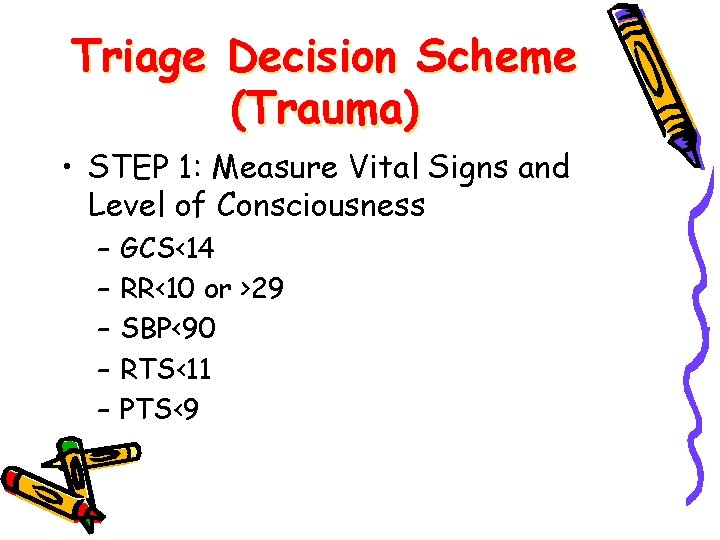
Triage Decision Scheme (Trauma) • STEP 1: Measure Vital Signs and Level of Consciousness – – – GCS<14 RR<10 or >29 SBP<90 RTS<11 PTS<9
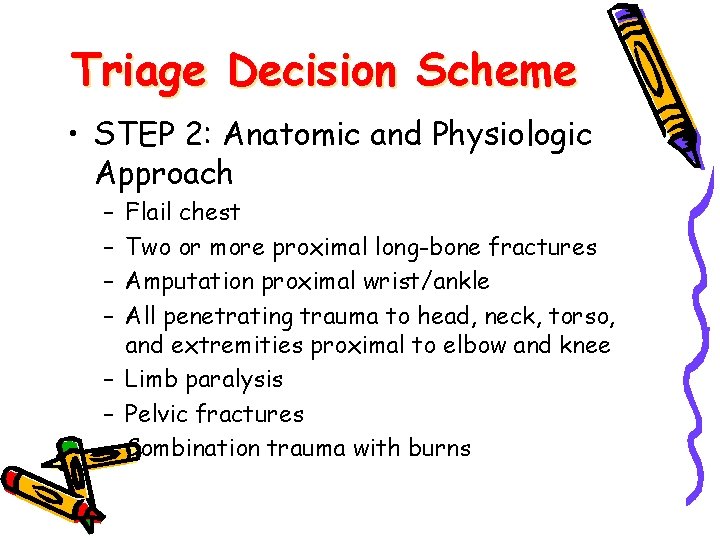
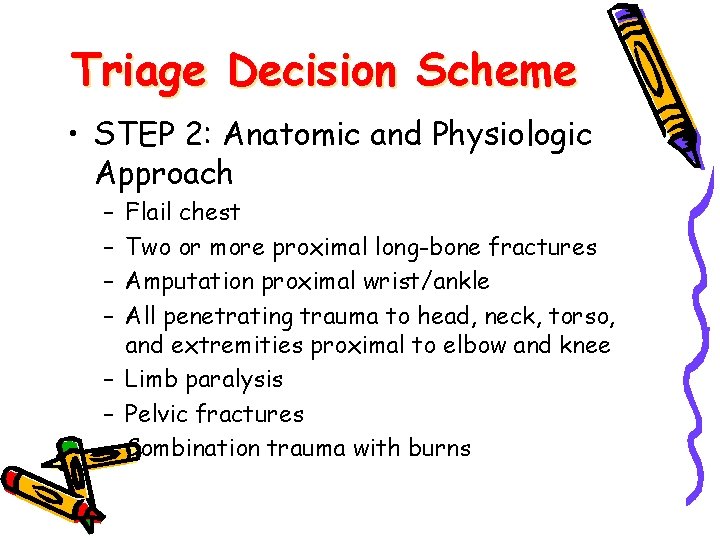
Triage Decision Scheme • STEP 2: Anatomic and Physiologic Approach – – Flail chest Two or more proximal long-bone fractures Amputation proximal wrist/ankle All penetrating trauma to head, neck, torso, and extremities proximal to elbow and knee – Limb paralysis – Pelvic fractures – Combination trauma with burns
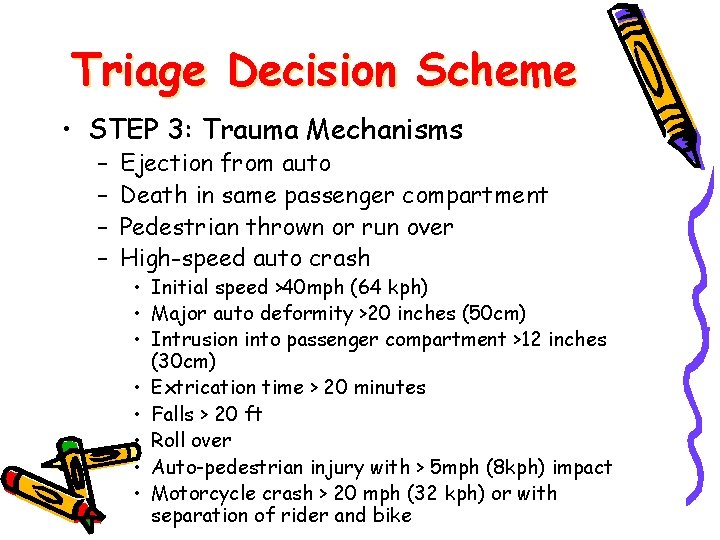
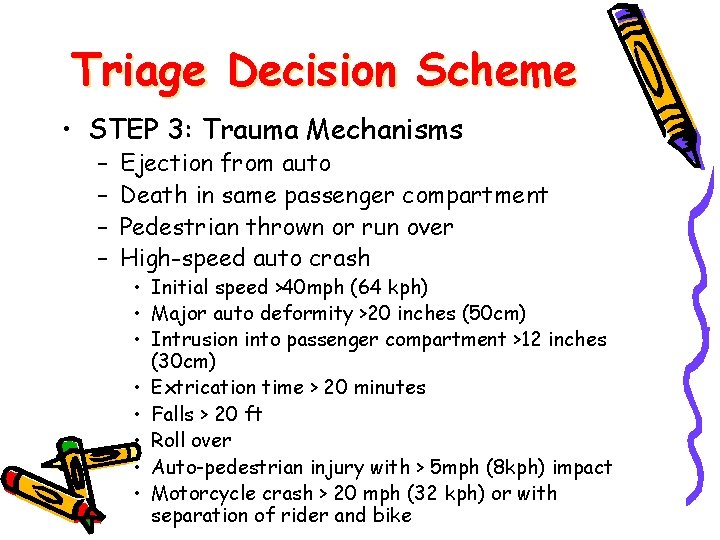
Triage Decision Scheme • STEP 3: Trauma Mechanisms – – Ejection from auto Death in same passenger compartment Pedestrian thrown or run over High-speed auto crash • Initial speed >40 mph (64 kph) • Major auto deformity >20 inches (50 cm) • Intrusion into passenger compartment >12 inches (30 cm) • Extrication time > 20 minutes • Falls > 20 ft • Roll over • Auto-pedestrian injury with > 5 mph (8 kph) impact • Motorcycle crash > 20 mph (32 kph) or with separation of rider and bike
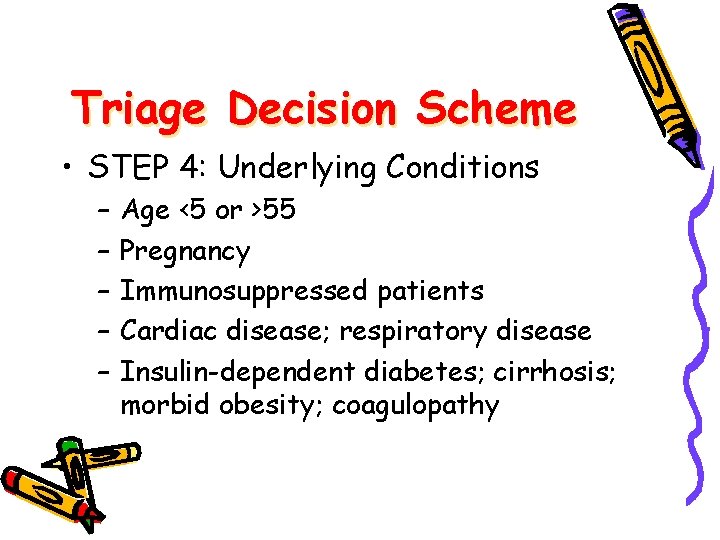
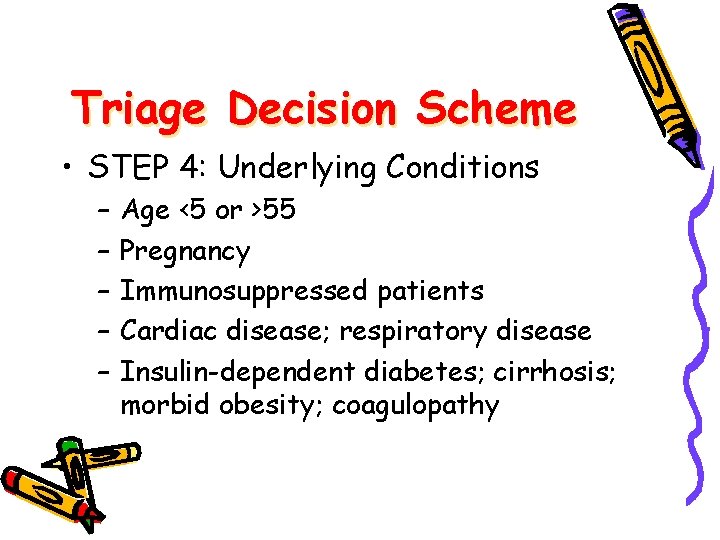
Triage Decision Scheme • STEP 4: Underlying Conditions – – – Age <5 or >55 Pregnancy Immunosuppressed patients Cardiac disease; respiratory disease Insulin-dependent diabetes; cirrhosis; morbid obesity; coagulopathy
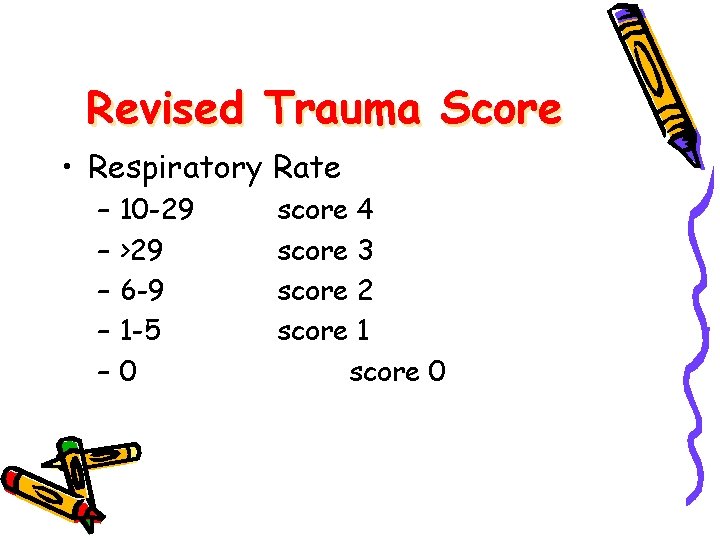
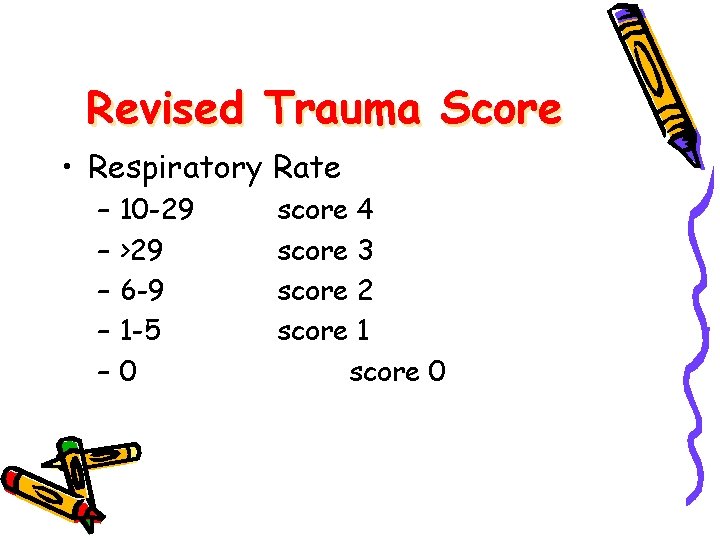
Revised Trauma Score • Respiratory Rate – – – 10 -29 >29 6 -9 1 -5 0 score 4 score 3 score 2 score 1 score 0
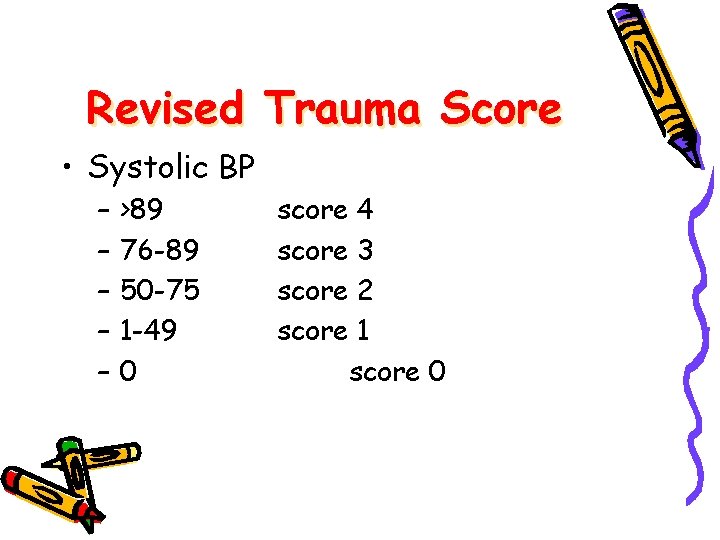
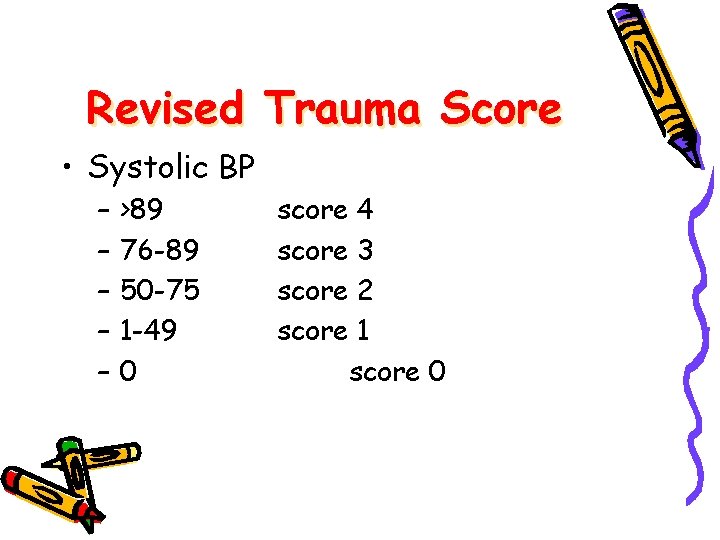
Revised Trauma Score • Systolic BP – – – >89 76 -89 50 -75 1 -49 0 score 4 score 3 score 2 score 1 score 0
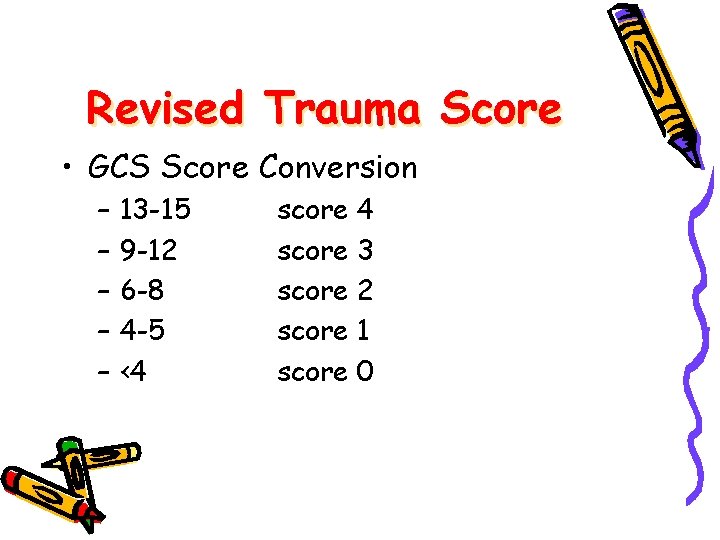
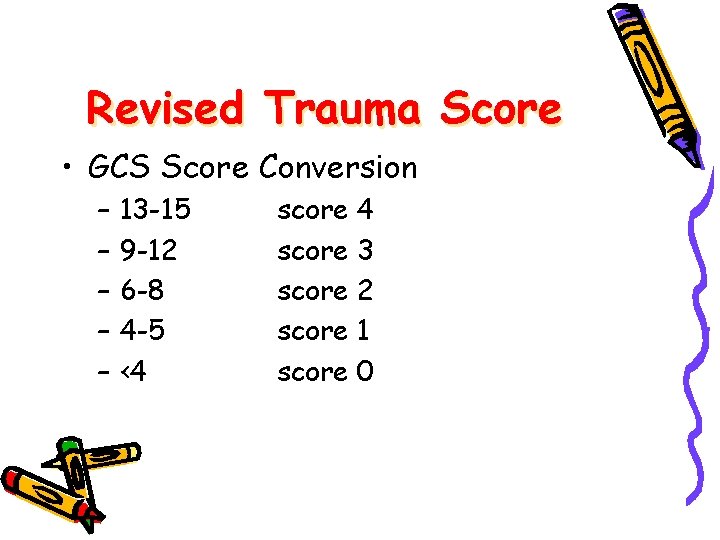
Revised Trauma Score • GCS Score Conversion – – – 13 -15 9 -12 6 -8 4 -5 <4 score 3 score 2 score 1 score 0
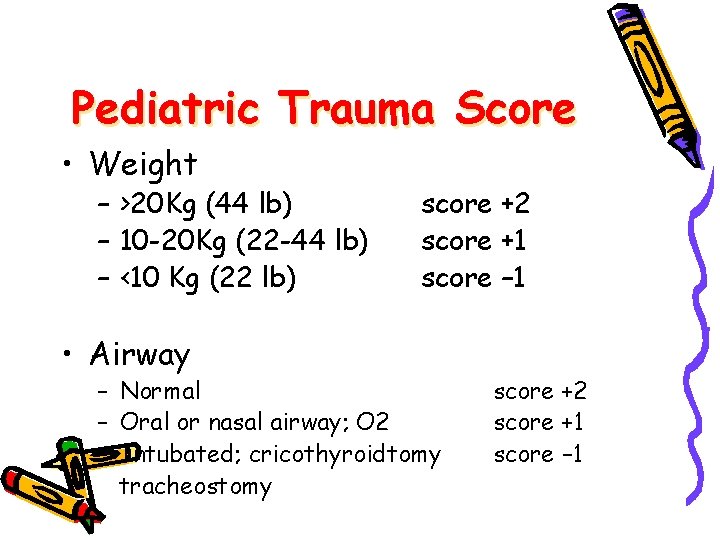
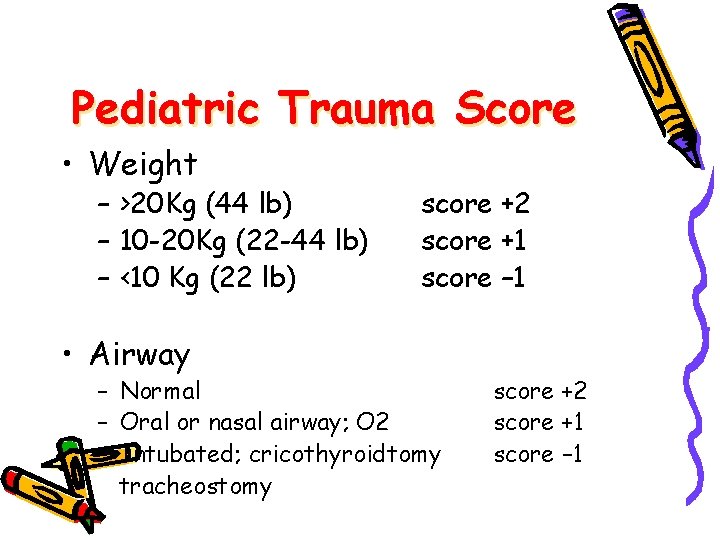
Pediatric Trauma Score • Weight – >20 Kg (44 lb) – 10 -20 Kg (22 -44 lb) – <10 Kg (22 lb) • Airway score +2 score +1 score – 1 – Normal – Oral or nasal airway; O 2 – Intubated; cricothyroidtomy tracheostomy score +2 score +1 score – 1
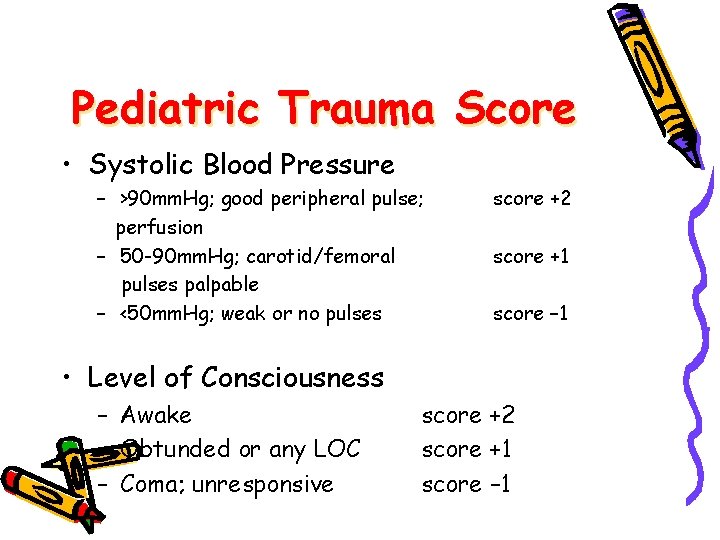
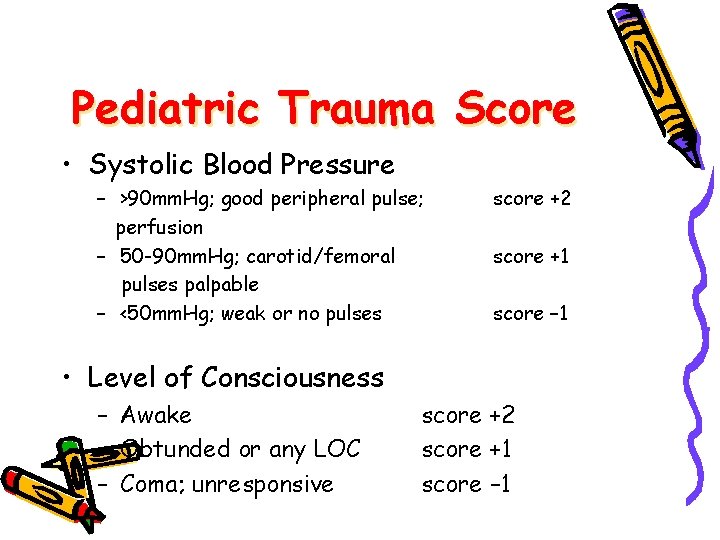
Pediatric Trauma Score • Systolic Blood Pressure – >90 mm. Hg; good peripheral pulse; perfusion – 50 -90 mm. Hg; carotid/femoral pulses palpable – <50 mm. Hg; weak or no pulses score +2 score +1 score – 1 • Level of Consciousness – Awake – Obtunded or any LOC – Coma; unresponsive score +2 score +1 score – 1
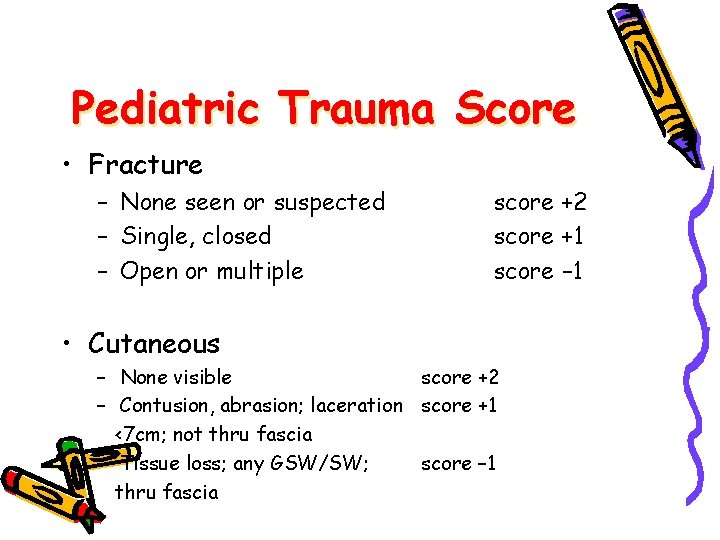
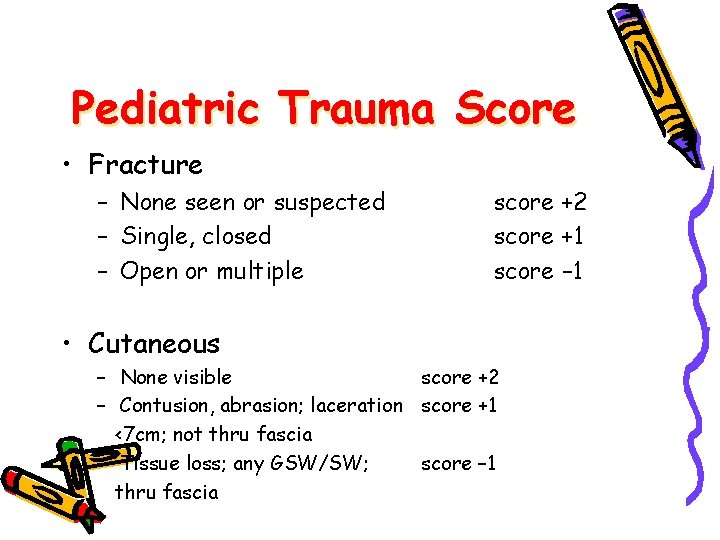
Pediatric Trauma Score • Fracture – None seen or suspected – Single, closed – Open or multiple • Cutaneous score +2 score +1 score – 1 – None visible score +2 – Contusion, abrasion; laceration score +1 <7 cm; not thru fascia – Tissue loss; any GSW/SW; score – 1 thru fascia
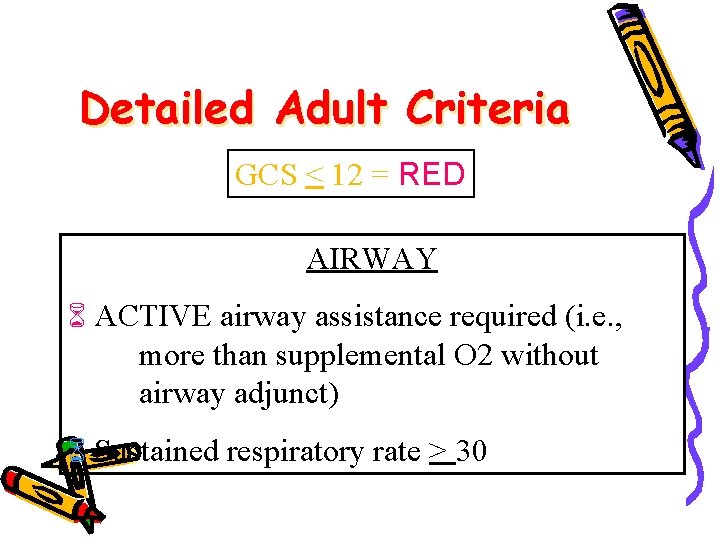
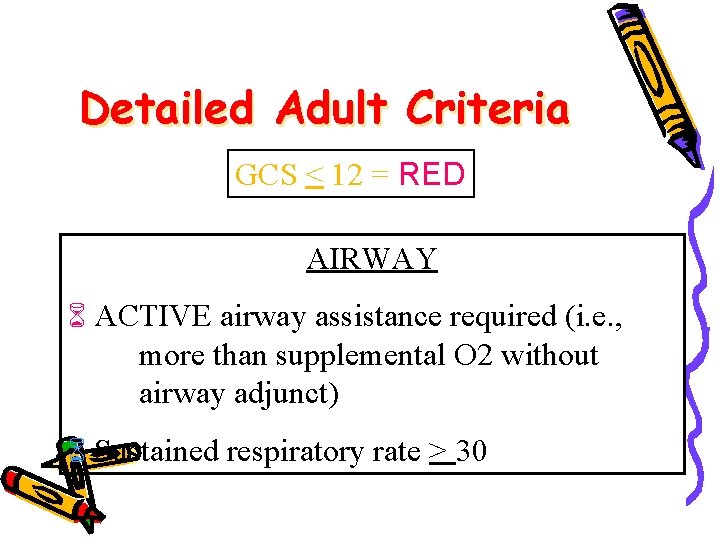
Detailed Adult Criteria GCS < 12 = RED AIRWAY ACTIVE airway assistance required (i. e. , more than supplemental O 2 without airway adjunct) Sustained respiratory rate > 30
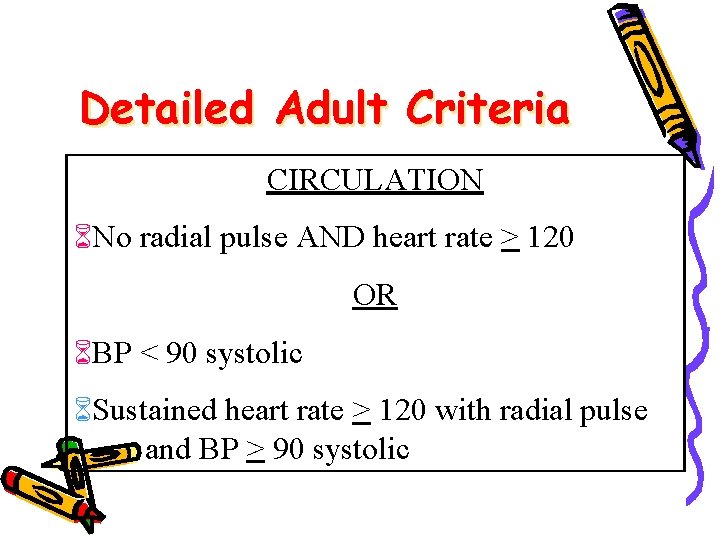
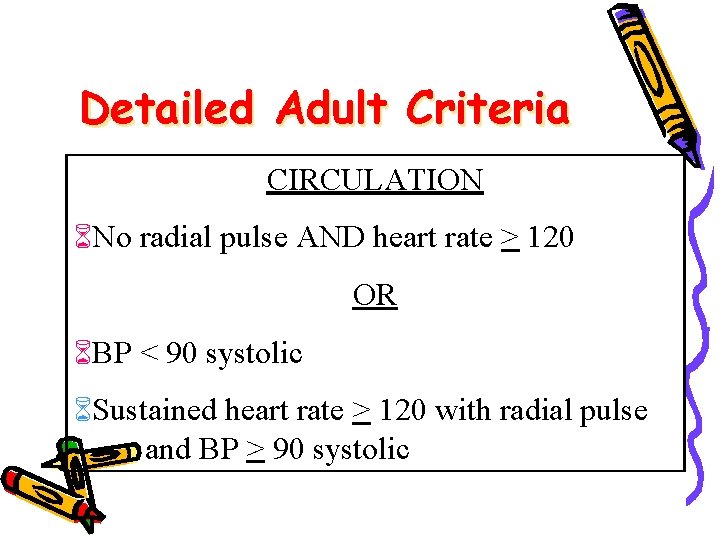
Detailed Adult Criteria CIRCULATION No radial pulse AND heart rate > 120 OR BP < 90 systolic Sustained heart rate > 120 with radial pulse and BP > 90 systolic
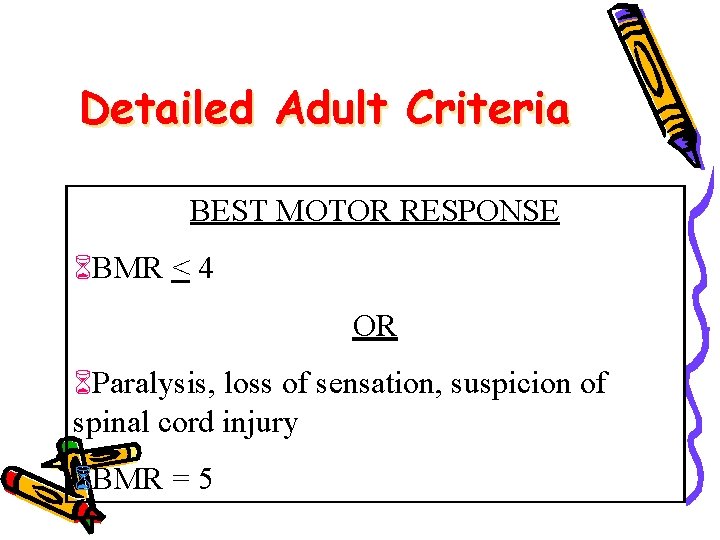
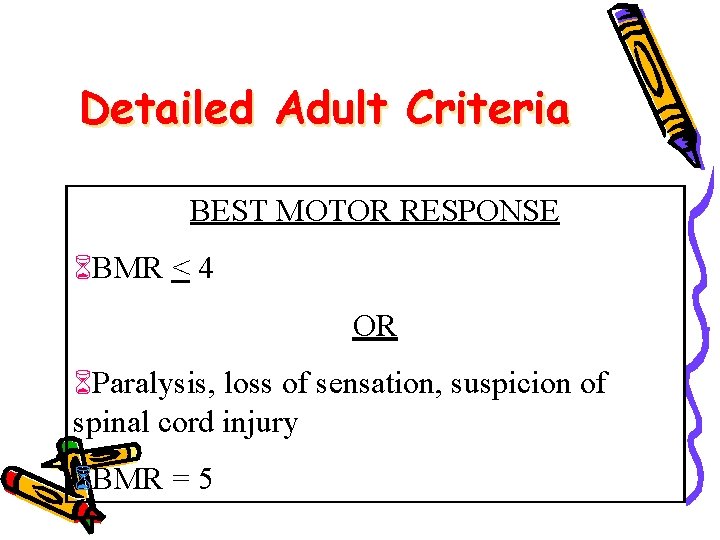
Detailed Adult Criteria BEST MOTOR RESPONSE BMR < 4 OR Paralysis, loss of sensation, suspicion of spinal cord injury BMR = 5
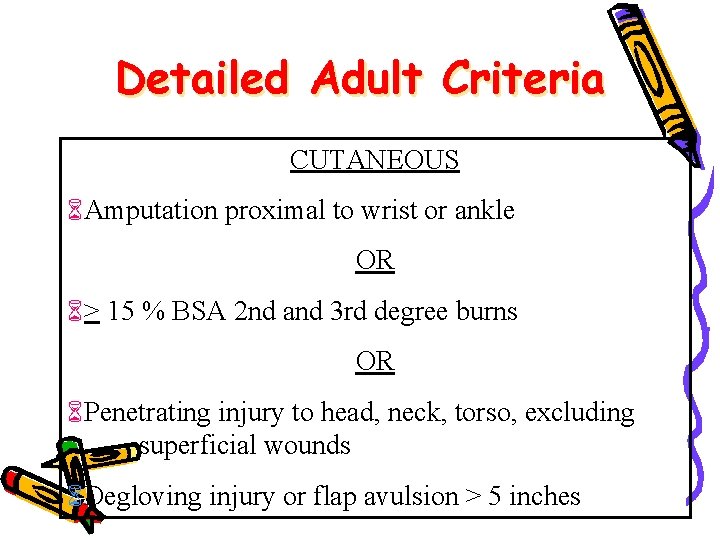
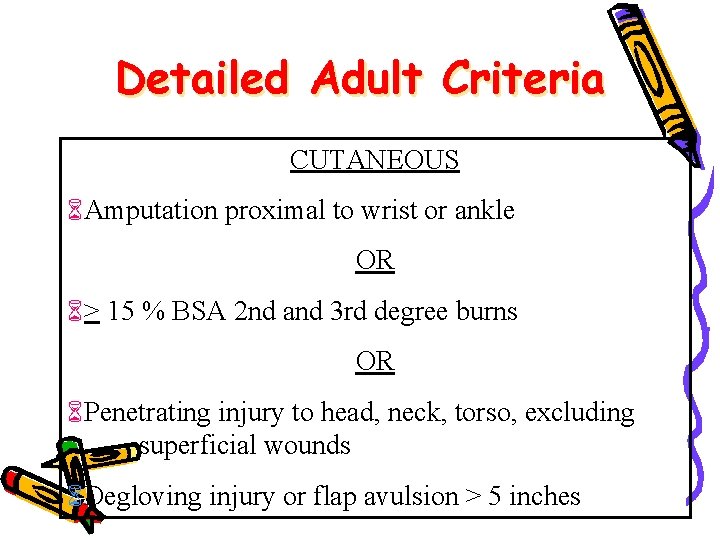
Detailed Adult Criteria CUTANEOUS Amputation proximal to wrist or ankle OR > 15 % BSA 2 nd and 3 rd degree burns OR Penetrating injury to head, neck, torso, excluding superficial wounds Degloving injury or flap avulsion > 5 inches
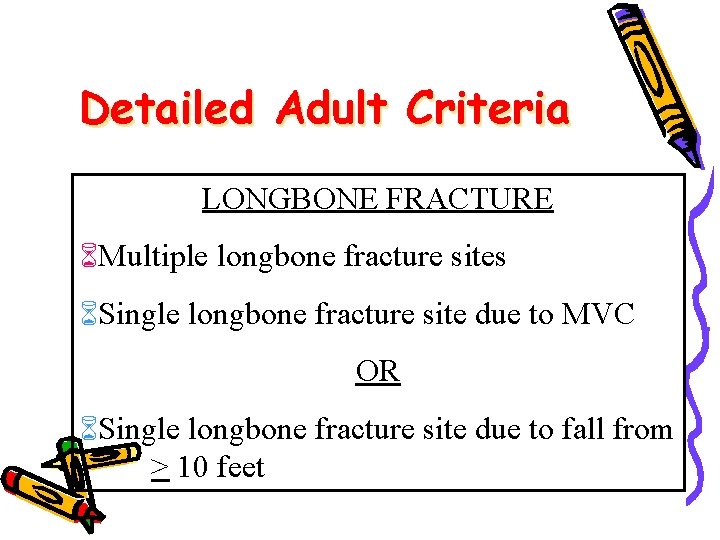
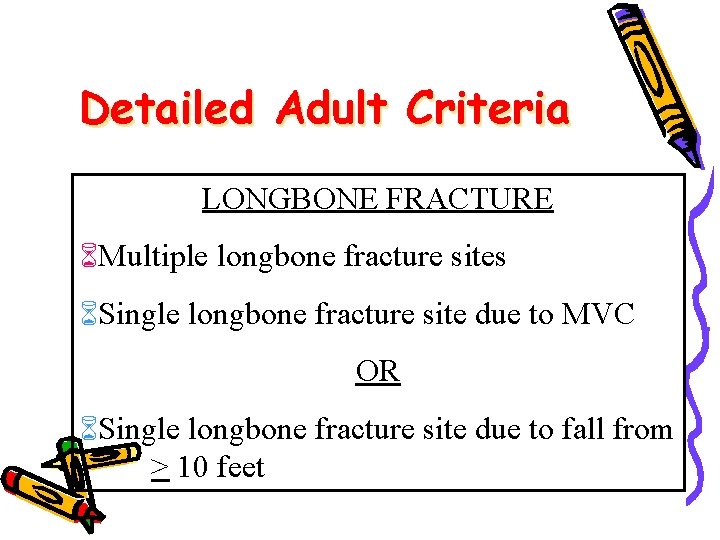
Detailed Adult Criteria LONGBONE FRACTURE Multiple longbone fracture sites Single longbone fracture site due to MVC OR Single longbone fracture site due to fall from > 10 feet
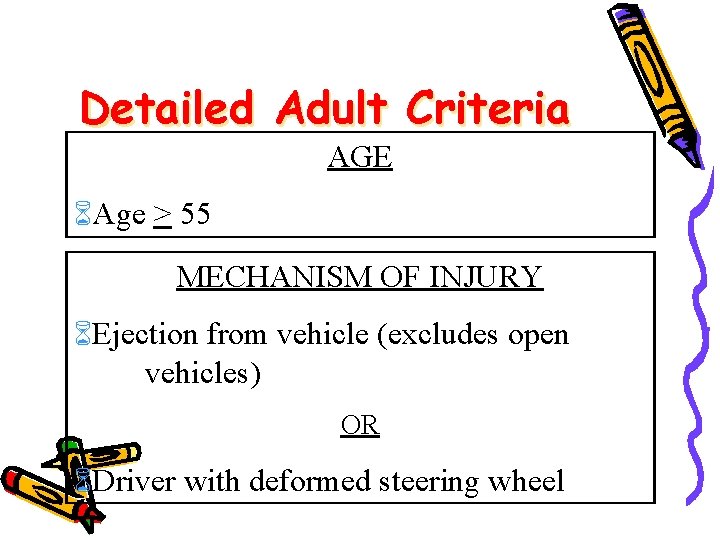
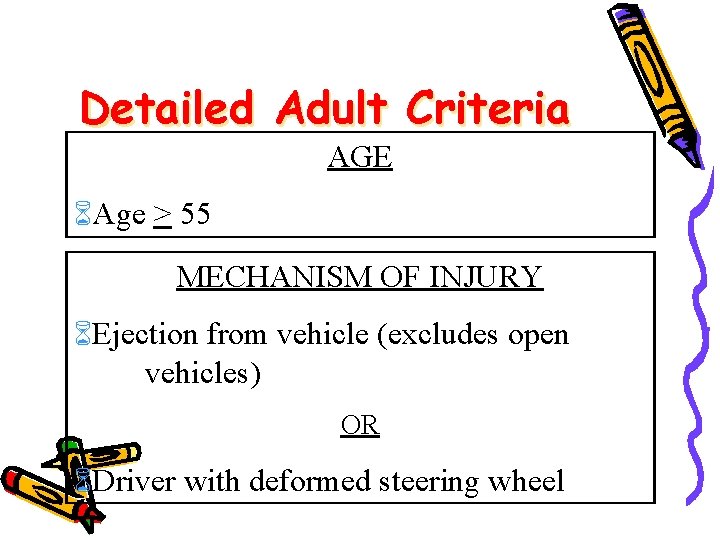
Detailed Adult Criteria AGE Age > 55 MECHANISM OF INJURY Ejection from vehicle (excludes open vehicles) OR Driver with deformed steering wheel
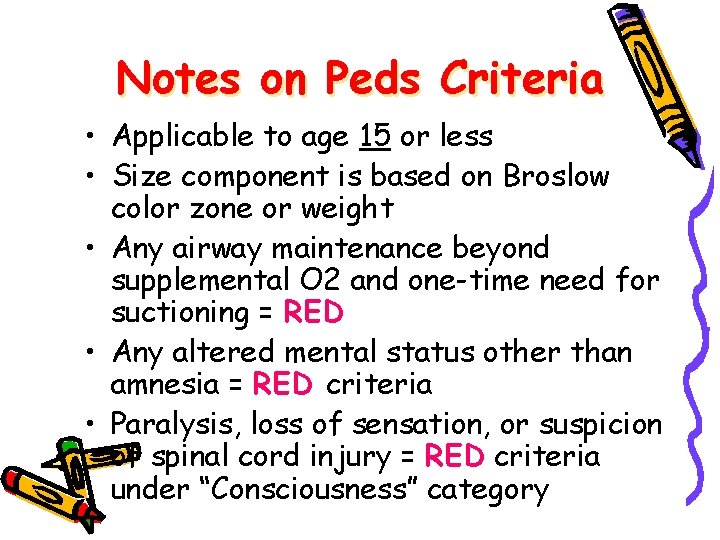
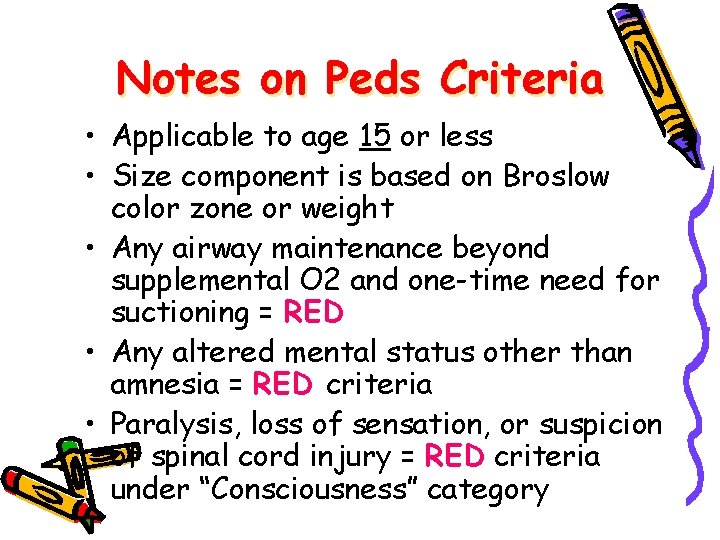
Notes on Peds Criteria • Applicable to age 15 or less • Size component is based on Broslow color zone or weight • Any airway maintenance beyond supplemental O 2 and one-time need for suctioning = RED • Any altered mental status other than amnesia = RED criteria • Paralysis, loss of sensation, or suspicion of spinal cord injury = RED criteria under “Consciousness” category
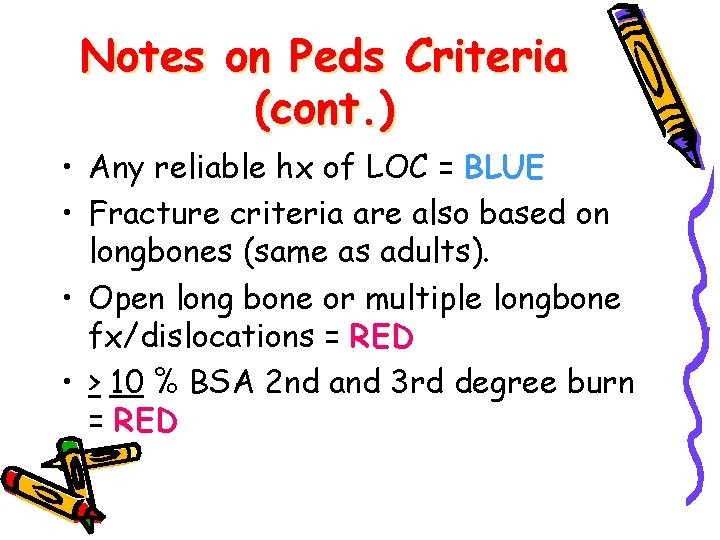
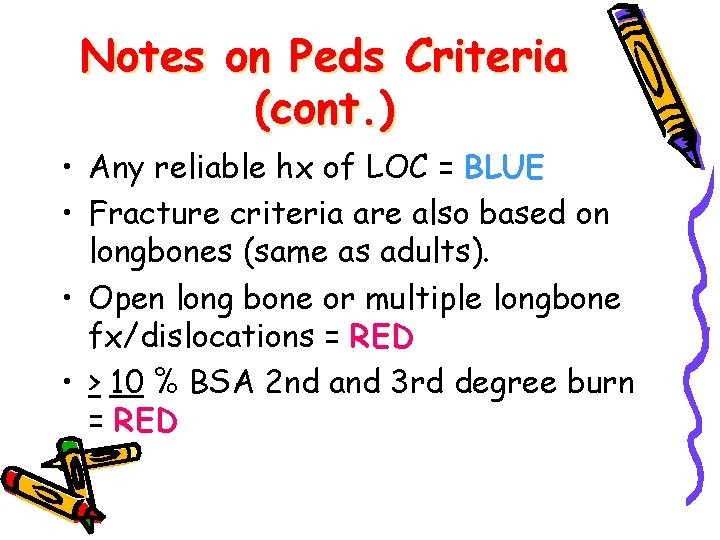
Notes on Peds Criteria (cont. ) • Any reliable hx of LOC = BLUE • Fracture criteria are also based on longbones (same as adults). • Open long bone or multiple longbone fx/dislocations = RED • > 10 % BSA 2 nd and 3 rd degree burn = RED
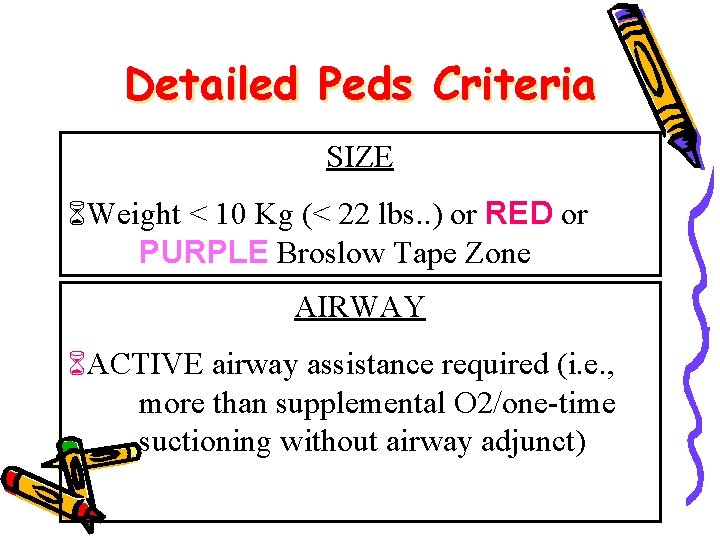
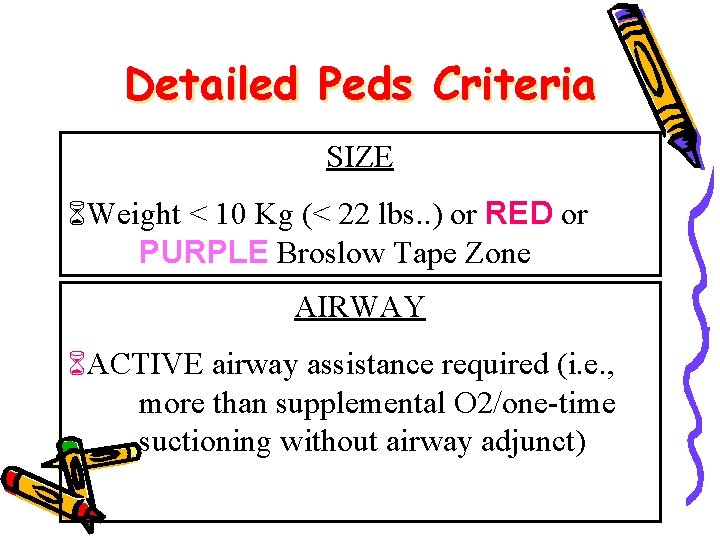
Detailed Peds Criteria SIZE Weight < 10 Kg (< 22 lbs. . ) or RED or PURPLE Broslow Tape Zone AIRWAY ACTIVE airway assistance required (i. e. , more than supplemental O 2/one-time suctioning without airway adjunct)
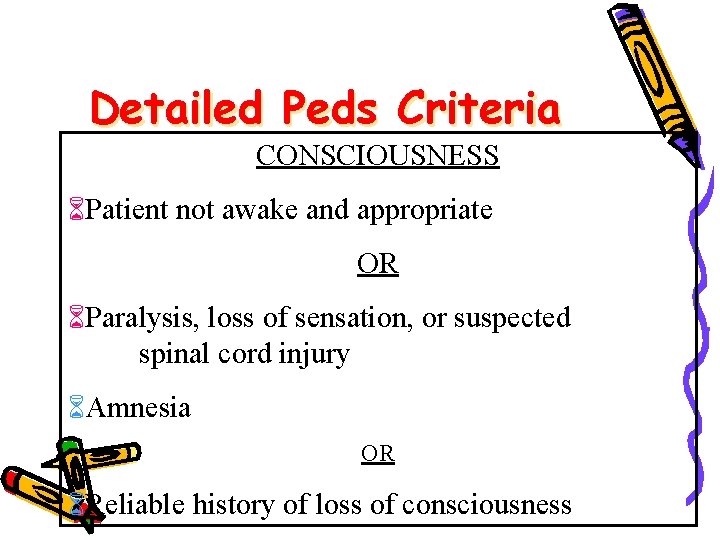
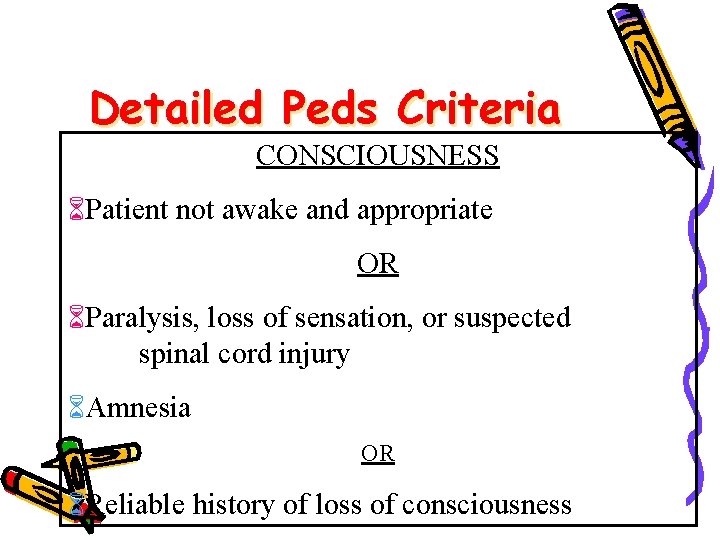
Detailed Peds Criteria CONSCIOUSNESS Patient not awake and appropriate OR Paralysis, loss of sensation, or suspected spinal cord injury Amnesia OR Reliable history of loss of consciousness
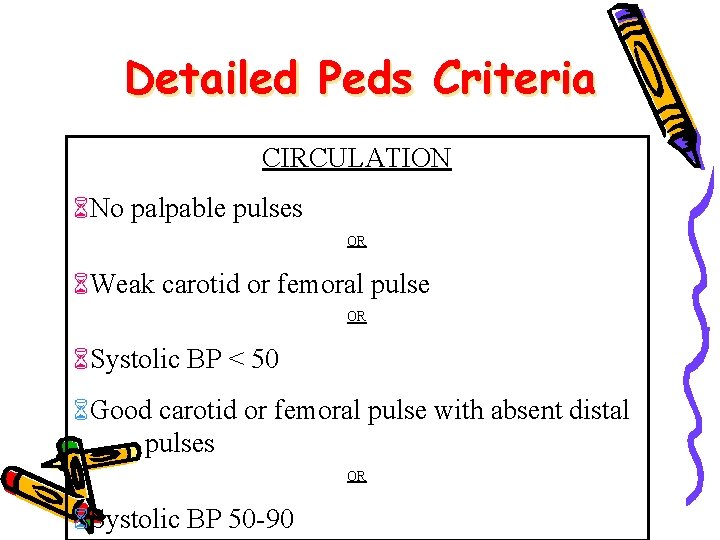
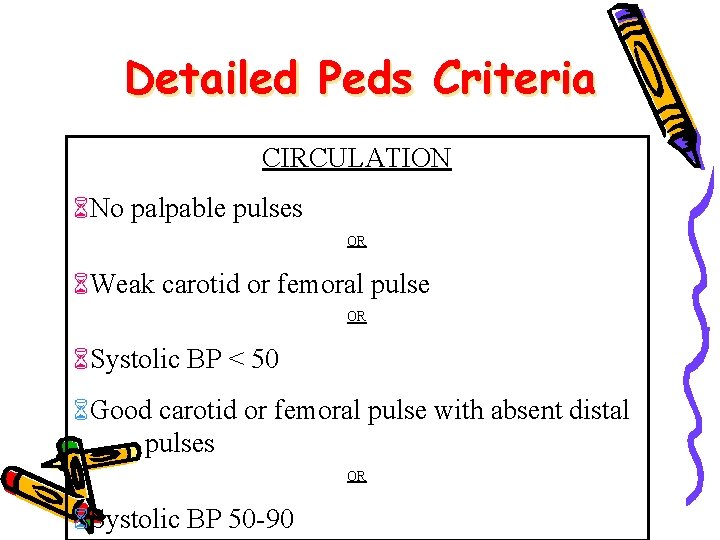
Detailed Peds Criteria CIRCULATION No palpable pulses OR Weak carotid or femoral pulse OR Systolic BP < 50 Good carotid or femoral pulse with absent distal pulses OR Systolic BP 50 -90
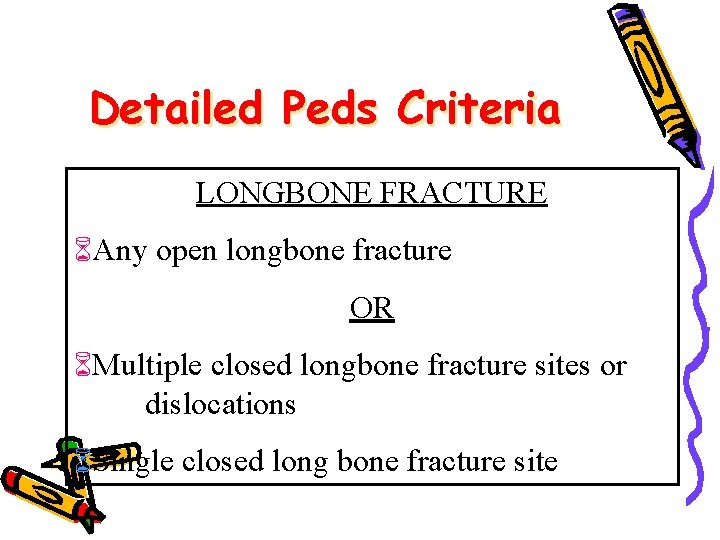
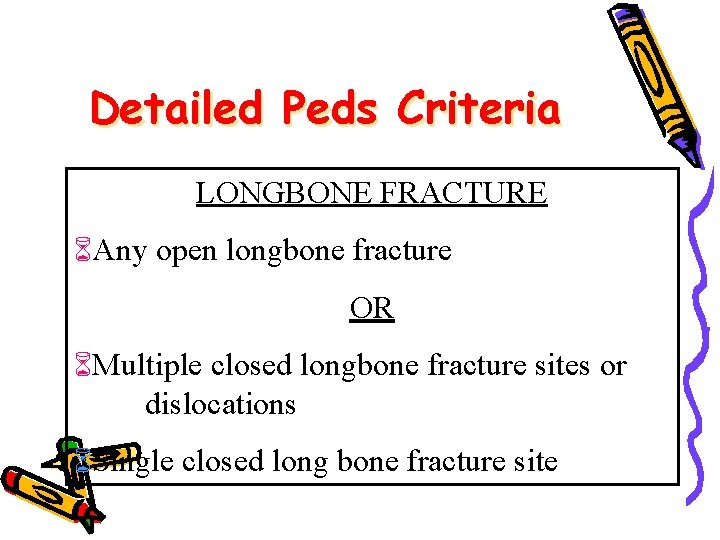
Detailed Peds Criteria LONGBONE FRACTURE Any open longbone fracture OR Multiple closed longbone fracture sites or dislocations Single closed long bone fracture site
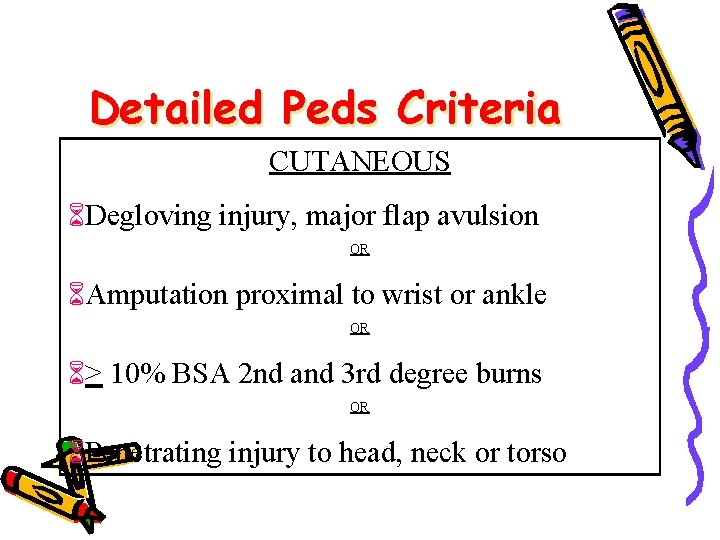
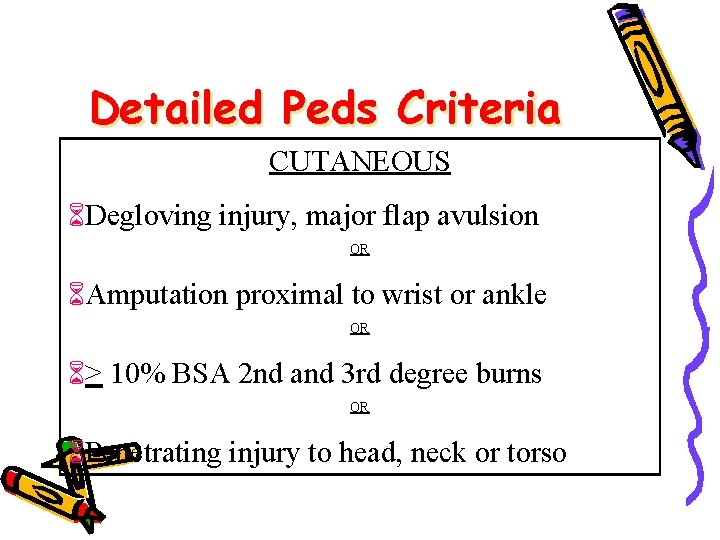
Detailed Peds Criteria CUTANEOUS Degloving injury, major flap avulsion OR Amputation proximal to wrist or ankle OR > 10% BSA 2 nd and 3 rd degree burns OR Penetrating injury to head, neck or torso
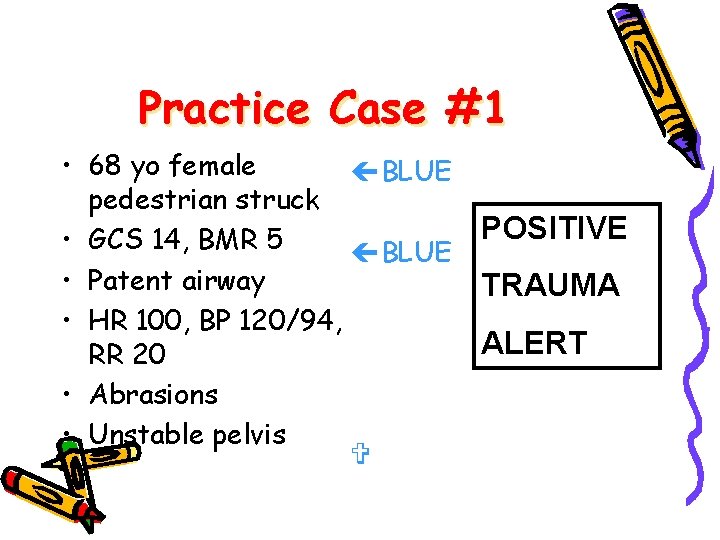
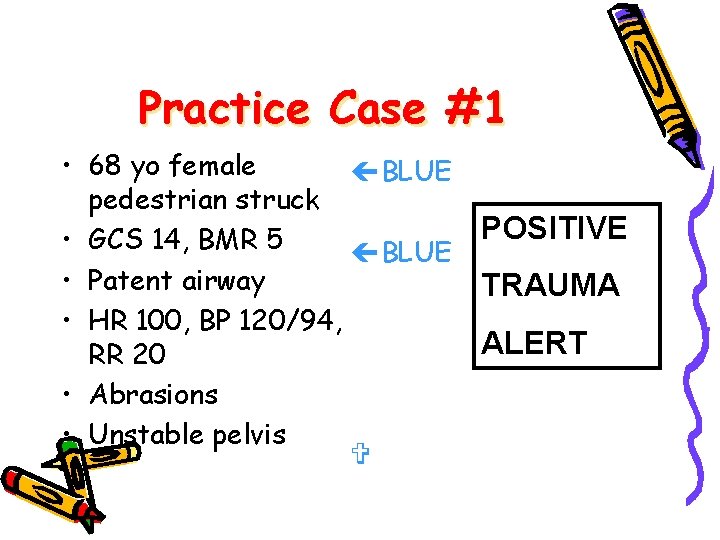
Practice Case #1 • 68 yo female çBLUE pedestrian struck • GCS 14, BMR 5 çBLUE • Patent airway • HR 100, BP 120/94, RR 20 • Abrasions • Unstable pelvis POSITIVE TRAUMA ALERT
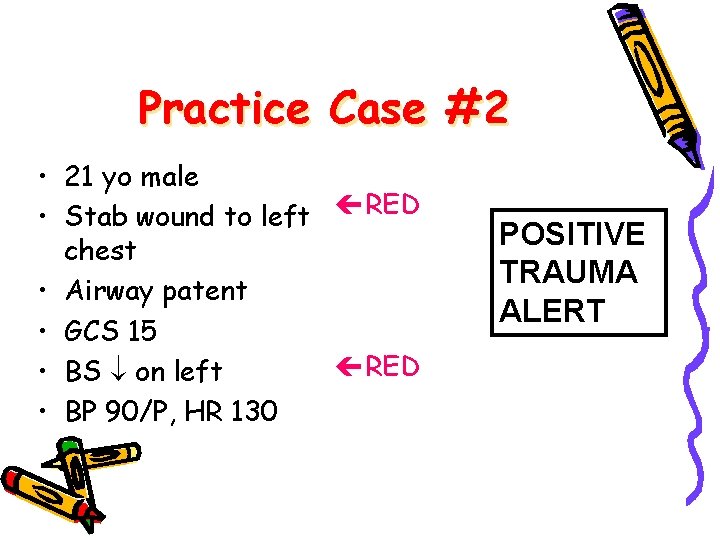
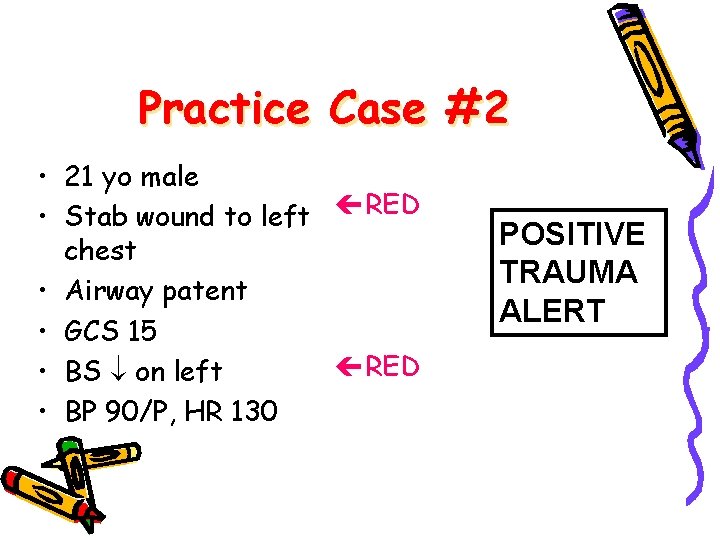
Practice Case #2 • 21 yo male • Stab wound to left çRED chest • Airway patent • GCS 15 çRED • BS on left • BP 90/P, HR 130 POSITIVE TRAUMA ALERT

Practice Case #3 • 4 year old neardrowning in pool • No signs of trauma • Intubated • Normal skin signs • Normal brachial pulse • Responsive to deep pain Drowning is not considered trauma unless injury accompanies it!
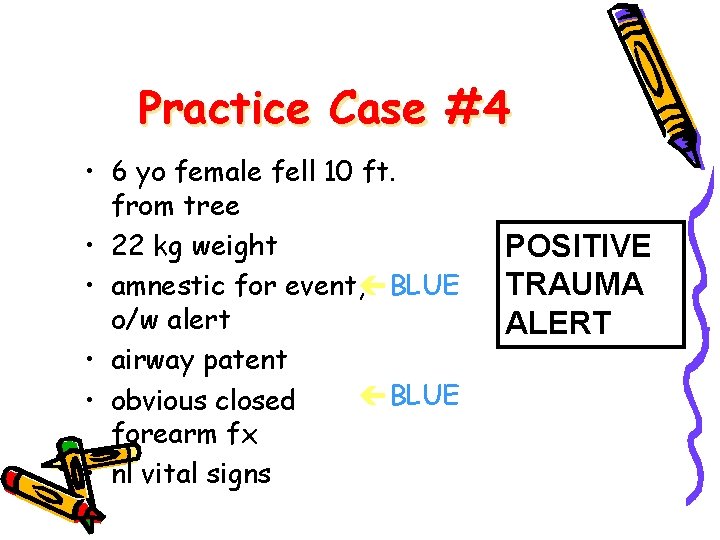
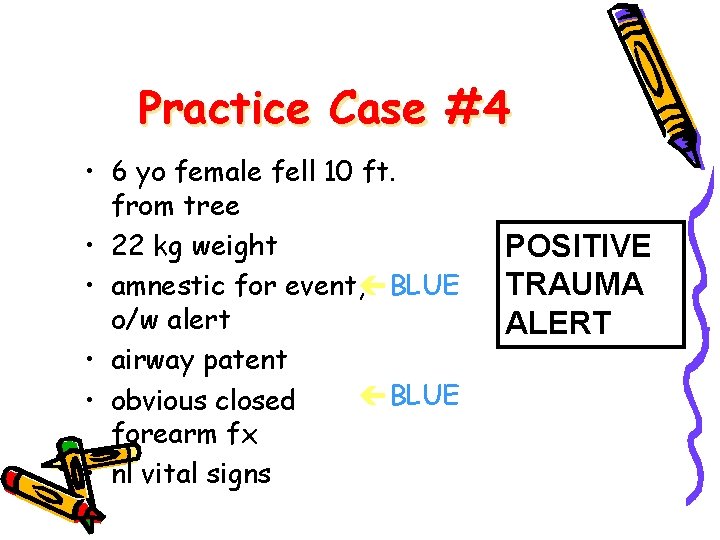
Practice Case #4 • 6 yo female fell 10 ft. from tree • 22 kg weight • amnestic for event, çBLUE o/w alert • airway patent çBLUE • obvious closed forearm fx • nl vital signs POSITIVE TRAUMA ALERT
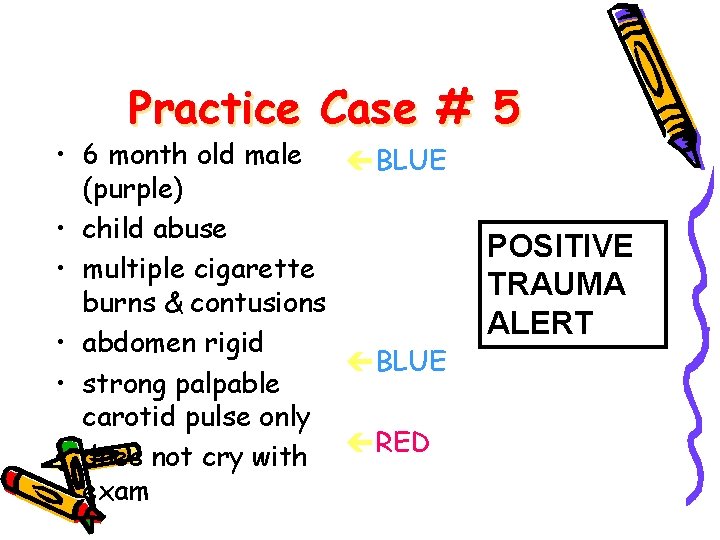
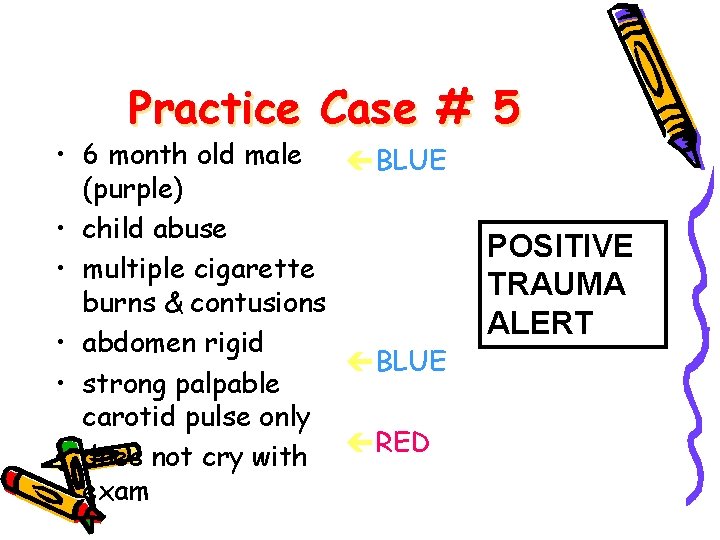
Practice Case # 5 • 6 month old male çBLUE (purple) • child abuse • multiple cigarette burns & contusions • abdomen rigid çBLUE • strong palpable carotid pulse only çRED • does not cry with exam POSITIVE TRAUMA ALERT
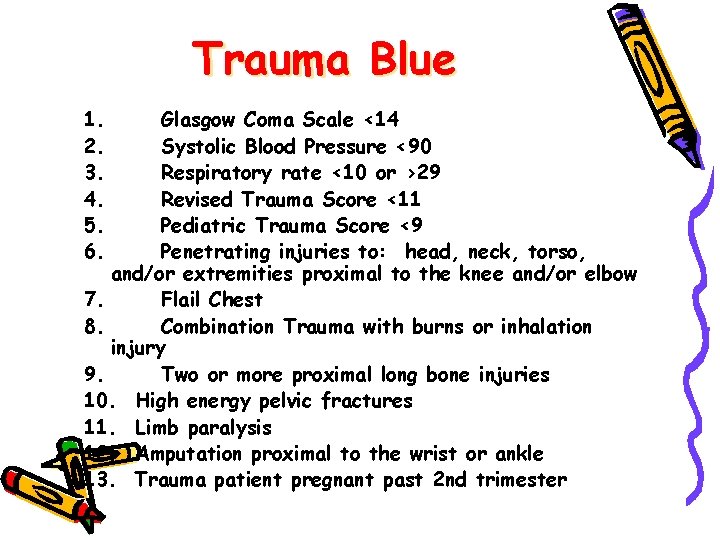
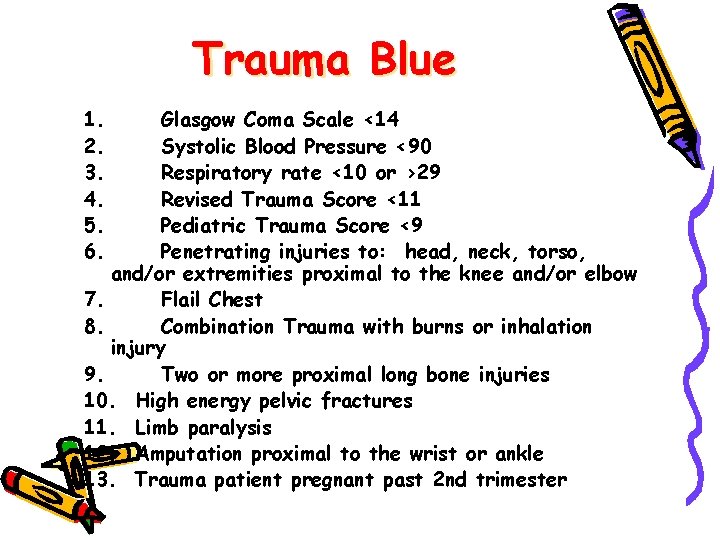
Trauma Blue 1. Glasgow Coma Scale <14 2. Systolic Blood Pressure <90 3. Respiratory rate <10 or >29 4. Revised Trauma Score <11 5. Pediatric Trauma Score <9 6. Penetrating injuries to: head, neck, torso, and/or extremities proximal to the knee and/or elbow 7. Flail Chest 8. Combination Trauma with burns or inhalation injury 9. Two or more proximal long bone injuries 10. High energy pelvic fractures 11. Limb paralysis 12. Amputation proximal to the wrist or ankle 13. Trauma patient pregnant past 2 nd trimester Another Example
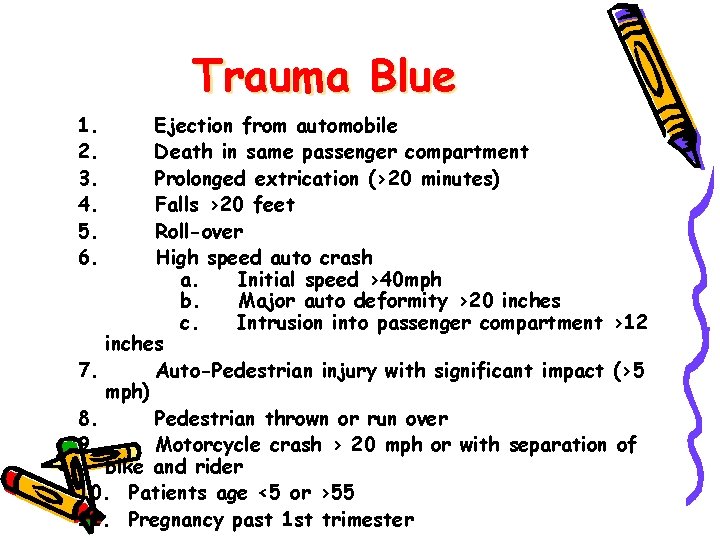
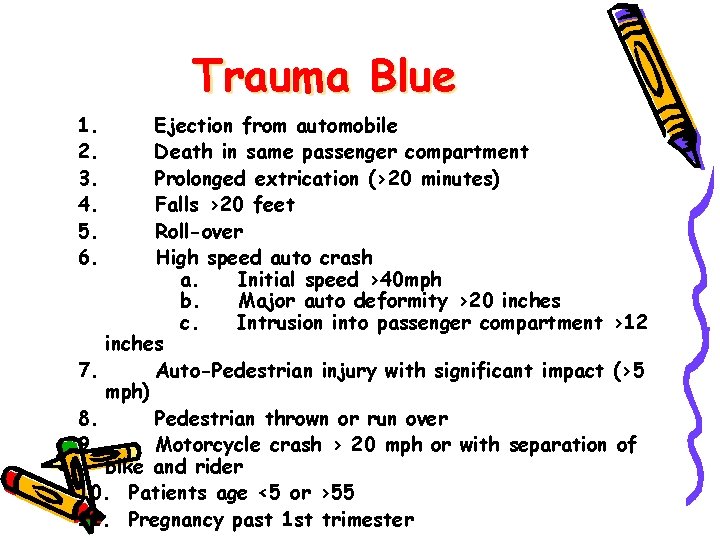
Trauma Blue 1. Ejection from automobile 2. Death in same passenger compartment 3. Prolonged extrication (>20 minutes) 4. Falls >20 feet 5. Roll-over 6. High speed auto crash a. Initial speed >40 mph b. Major auto deformity >20 inches c. Intrusion into passenger compartment >12 inches 7. Auto-Pedestrian injury with significant impact (>5 mph) 8. Pedestrian thrown or run over 9. Motorcycle crash > 20 mph or with separation of bike and rider 10. Patients age <5 or >55 11. Pregnancy past 1 st trimester
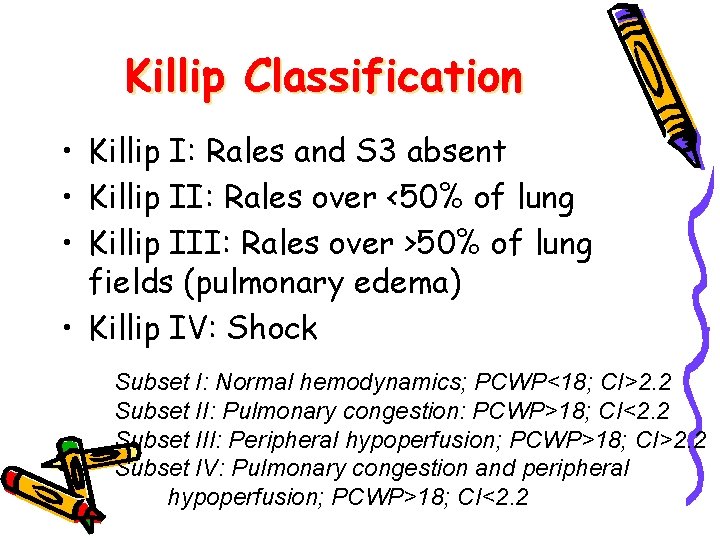
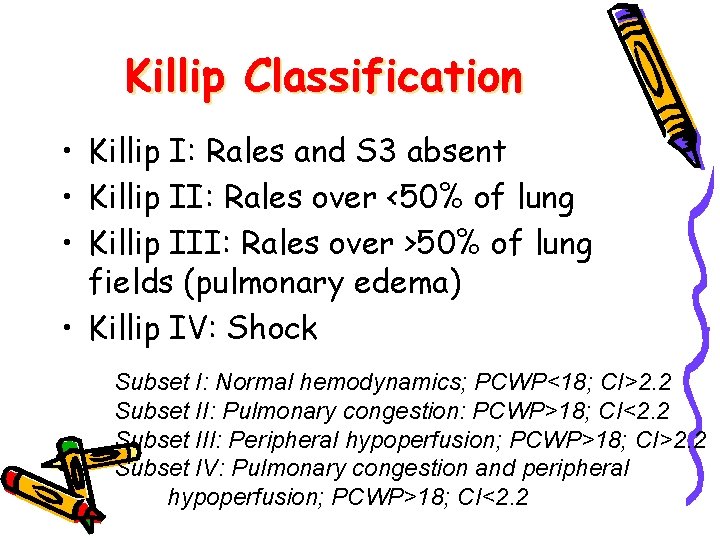
Killip Classification • Killip I: Rales and S 3 absent • Killip II: Rales over <50% of lung • Killip III: Rales over >50% of lung fields (pulmonary edema) • Killip IV: Shock Subset I: Normal hemodynamics; PCWP<18; CI>2. 2 Subset II: Pulmonary congestion: PCWP>18; CI<2. 2 Subset III: Peripheral hypoperfusion; PCWP>18; CI>2. 2 Subset IV: Pulmonary congestion and peripheral hypoperfusion; PCWP>18; CI<2. 2
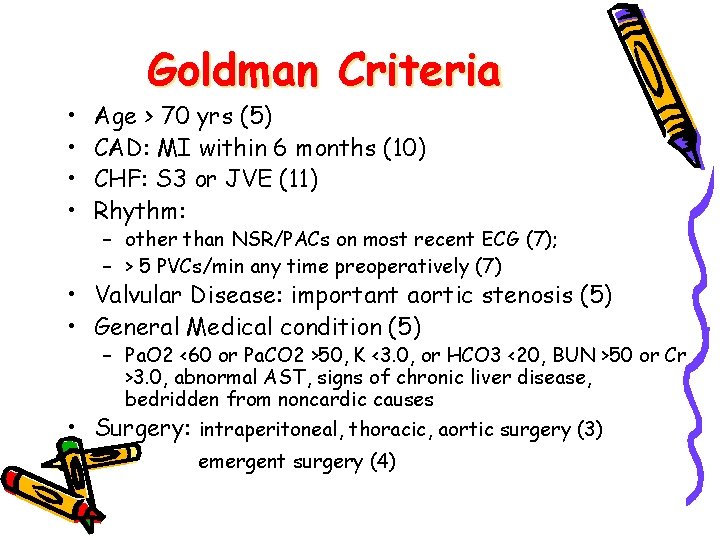
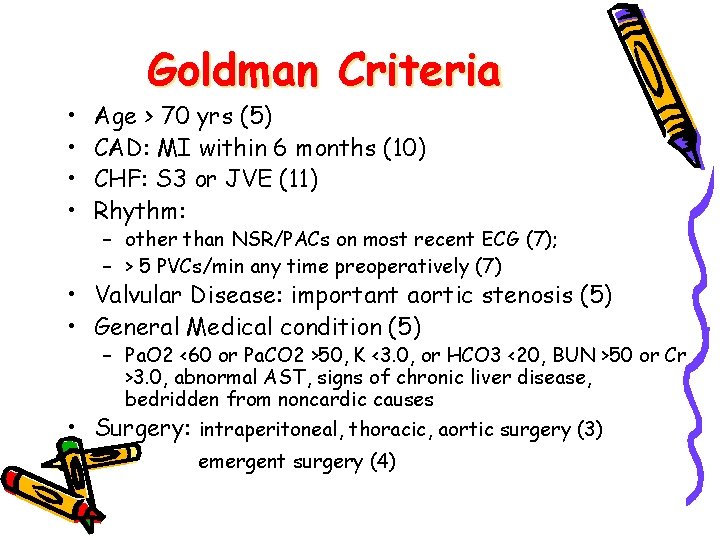
• • Goldman Criteria Age > 70 yrs (5) CAD: MI within 6 months (10) CHF: S 3 or JVE (11) Rhythm: – other than NSR/PACs on most recent ECG (7); – > 5 PVCs/min any time preoperatively (7) • Valvular Disease: important aortic stenosis (5) • General Medical condition (5) – Pa. O 2 <60 or Pa. CO 2 >50, K <3. 0, or HCO 3 <20, BUN >50 or Cr >3. 0, abnormal AST, signs of chronic liver disease, bedridden from noncardic causes • Surgery: intraperitoneal, thoracic, aortic surgery (3) emergent surgery (4)
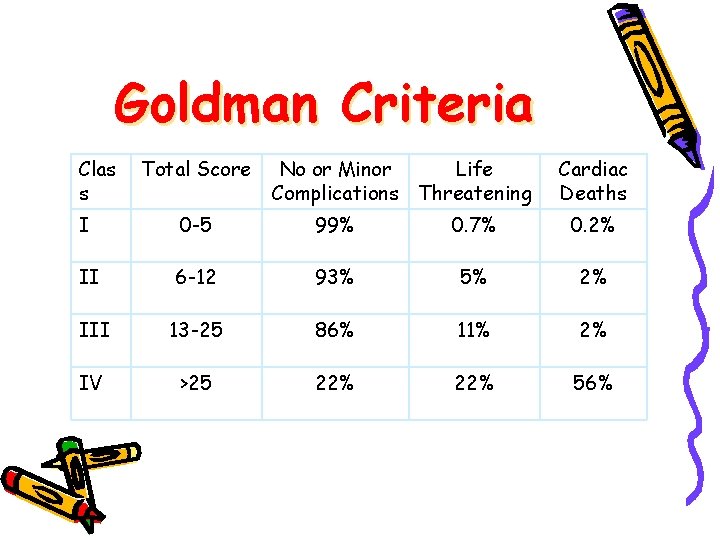
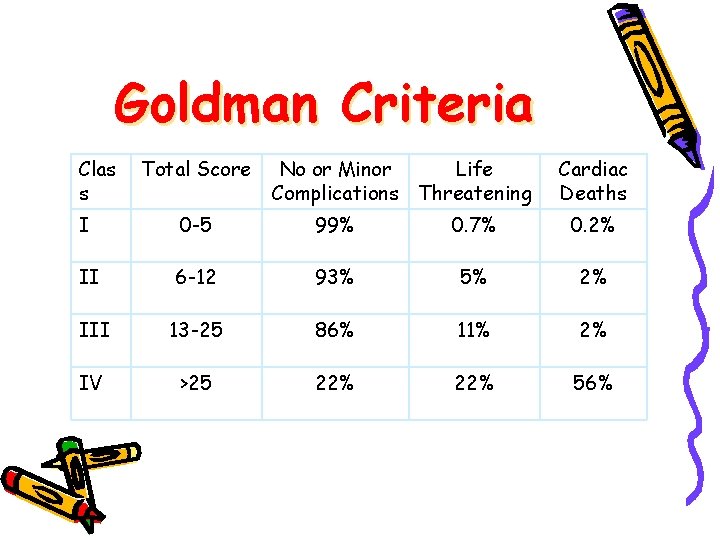
Goldman Criteria Clas s Total Score No or Minor Life Complications Threatening Cardiac Deaths I 0 -5 99% 0. 7% 0. 2% II 6 -12 93% 5% 2% III 13 -25 86% 11% 2% IV >25 22% 56%
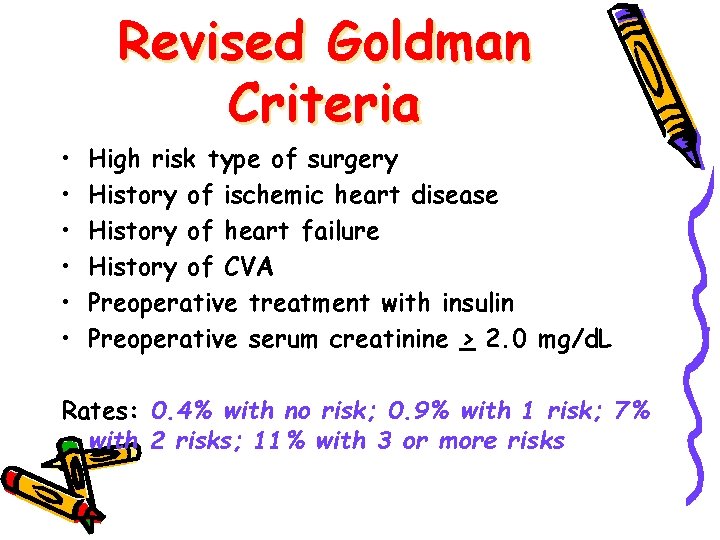
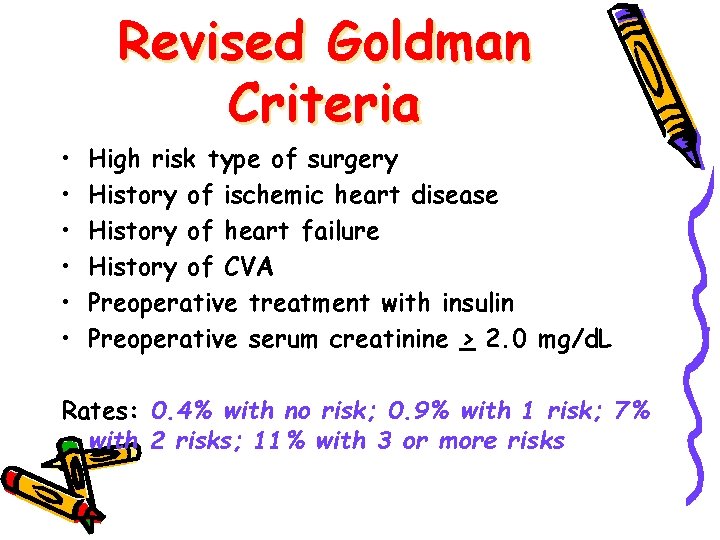
• • • Revised Goldman Criteria High risk type of surgery History of ischemic heart disease History of heart failure History of CVA Preoperative treatment with insulin Preoperative serum creatinine > 2. 0 mg/d. L Rates: 0. 4% with no risk; 0. 9% with 1 risk; 7% with 2 risks; 11% with 3 or more risks
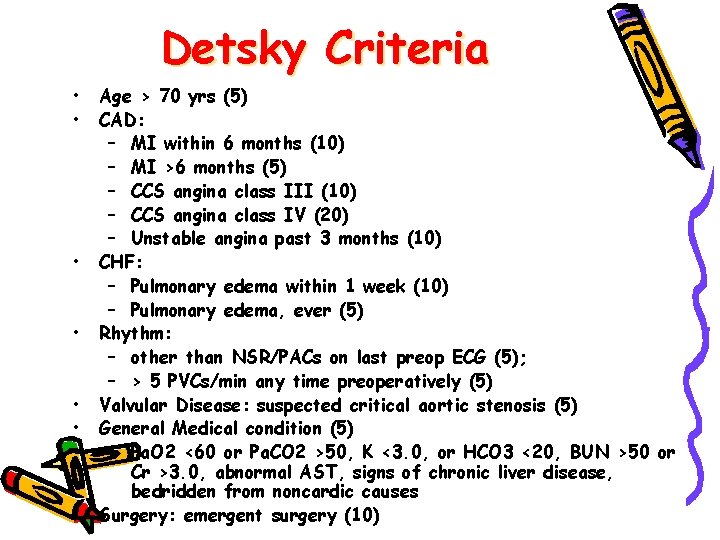
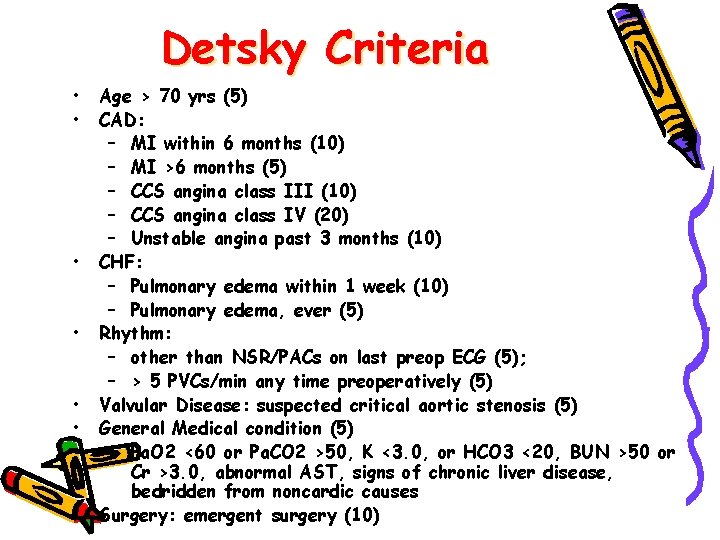
Detsky Criteria • • Age > 70 yrs (5) CAD: – MI within 6 months (10) – MI >6 months (5) – CCS angina class III (10) – CCS angina class IV (20) – Unstable angina past 3 months (10) CHF: – Pulmonary edema within 1 week (10) – Pulmonary edema, ever (5) Rhythm: – other than NSR/PACs on last preop ECG (5); – > 5 PVCs/min any time preoperatively (5) Valvular Disease: suspected critical aortic stenosis (5) General Medical condition (5) – Pa. O 2 <60 or Pa. CO 2 >50, K <3. 0, or HCO 3 <20, BUN >50 or Cr >3. 0, abnormal AST, signs of chronic liver disease, bedridden from noncardic causes Surgery: emergent surgery (10)
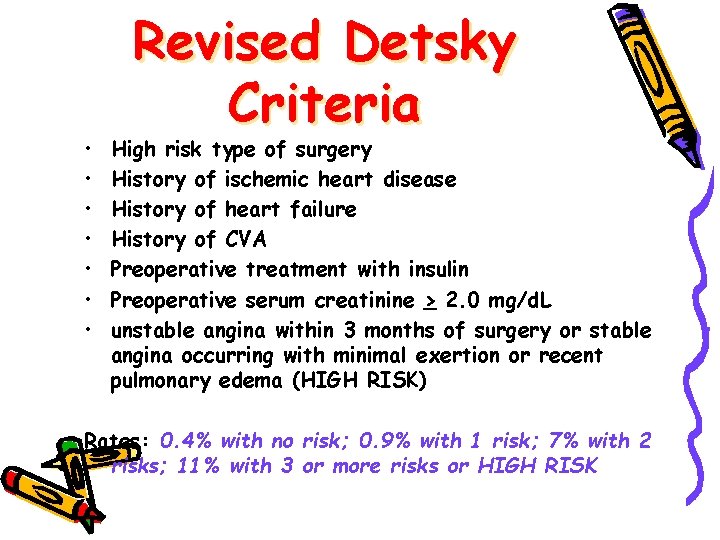
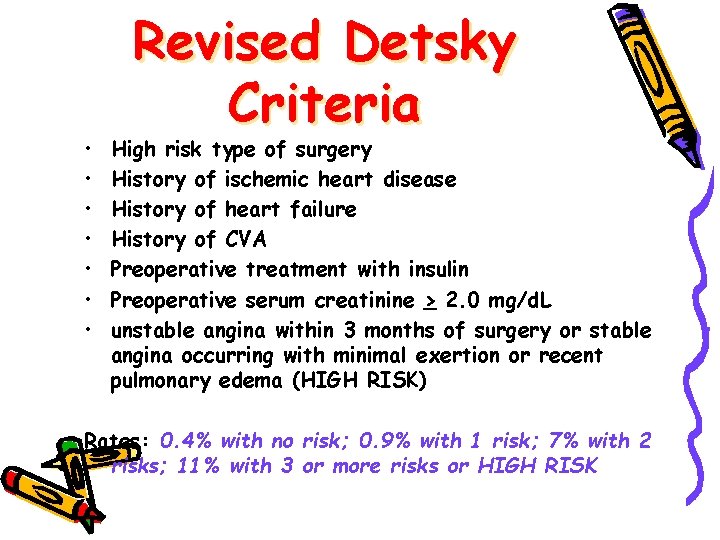
• • Revised Detsky Criteria High risk type of surgery History of ischemic heart disease History of heart failure History of CVA Preoperative treatment with insulin Preoperative serum creatinine > 2. 0 mg/d. L unstable angina within 3 months of surgery or stable angina occurring with minimal exertion or recent pulmonary edema (HIGH RISK) Rates: 0. 4% with no risk; 0. 9% with 1 risk; 7% with 2 risks; 11% with 3 or more risks or HIGH RISK
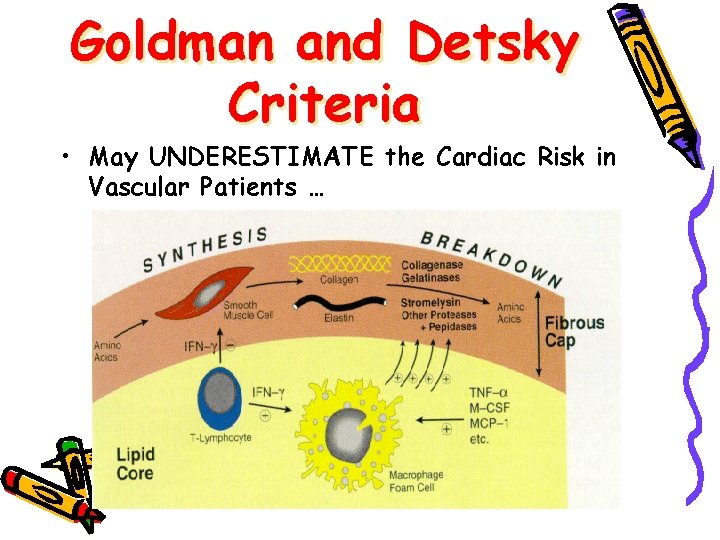
Goldman and Detsky Criteria • May UNDERESTIMATE the Cardiac Risk in Vascular Patients …
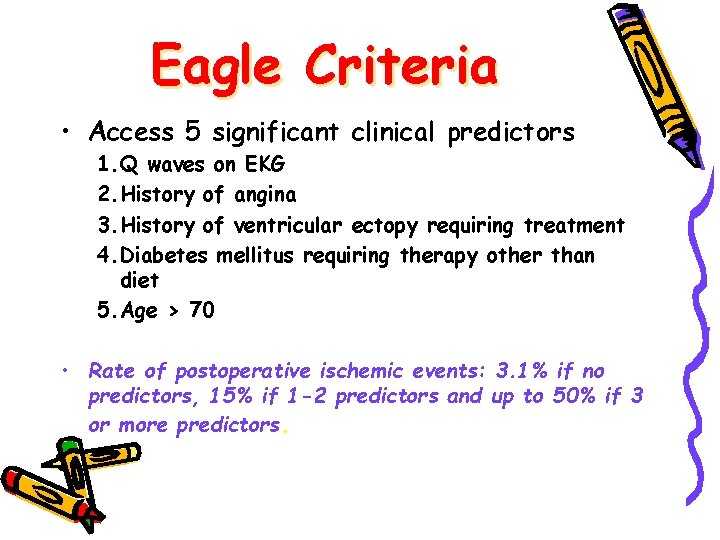
Eagle Criteria • Access 5 significant clinical predictors 1. Q waves on EKG 2. History of angina 3. History of ventricular ectopy requiring treatment 4. Diabetes mellitus requiring therapy other than diet 5. Age > 70 • Rate of postoperative ischemic events: 3. 1% if no predictors, 15% if 1 -2 predictors and up to 50% if 3 or more predictors.
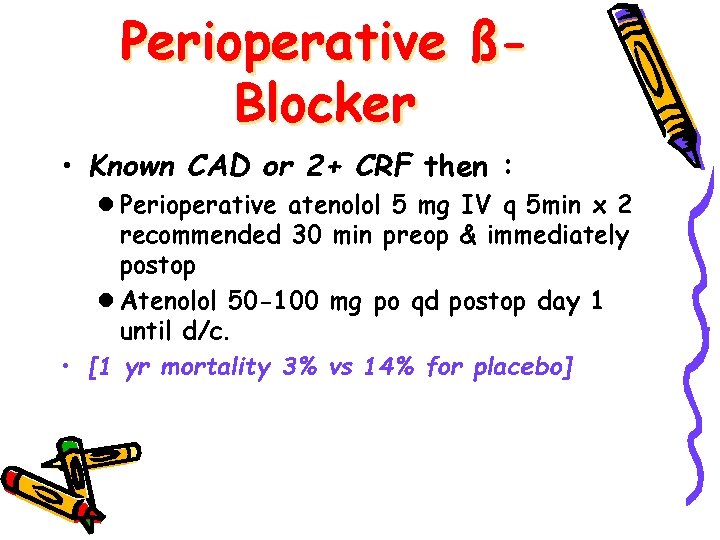
Perioperative ßBlocker • Known CAD or 2+ CRF then : l Perioperative atenolol 5 mg IV q 5 min x 2 recommended 30 min preop & immediately postop l Atenolol 50 -100 mg po qd postop day 1 until d/c. • [1 yr mortality 3% vs 14% for placebo]
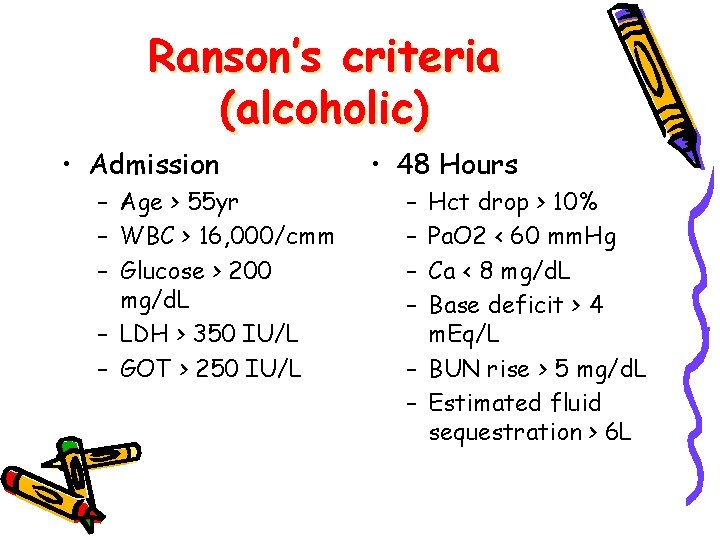
Ranson’s criteria (alcoholic) • Admission – Age > 55 yr – WBC > 16, 000/cmm – Glucose > 200 mg/d. L – LDH > 350 IU/L – GOT > 250 IU/L • 48 Hours – – Hct drop > 10% Pa. O 2 < 60 mm. Hg Ca < 8 mg/d. L Base deficit > 4 m. Eq/L – BUN rise > 5 mg/d. L – Estimated fluid sequestration > 6 L
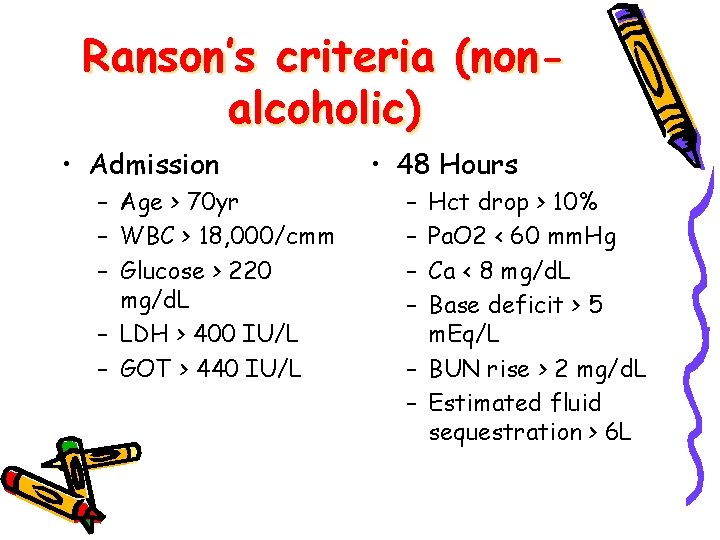
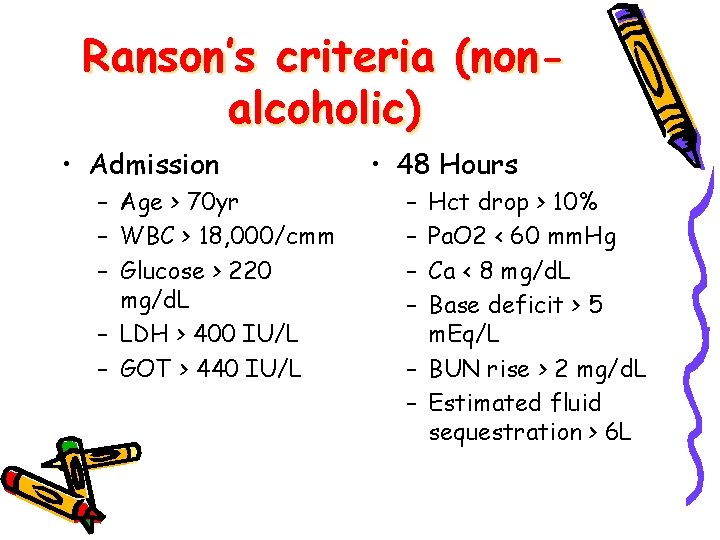
Ranson’s criteria (nonalcoholic) • Admission – Age > 70 yr – WBC > 18, 000/cmm – Glucose > 220 mg/d. L – LDH > 400 IU/L – GOT > 440 IU/L • 48 Hours – – Hct drop > 10% Pa. O 2 < 60 mm. Hg Ca < 8 mg/d. L Base deficit > 5 m. Eq/L – BUN rise > 2 mg/d. L – Estimated fluid sequestration > 6 L
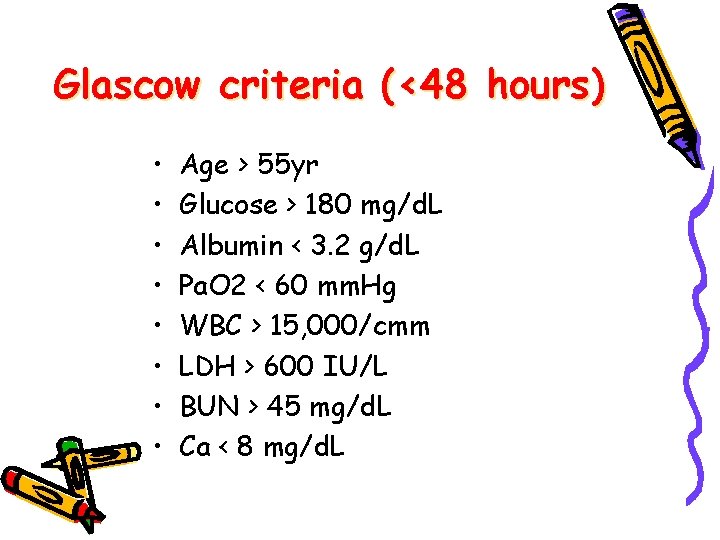
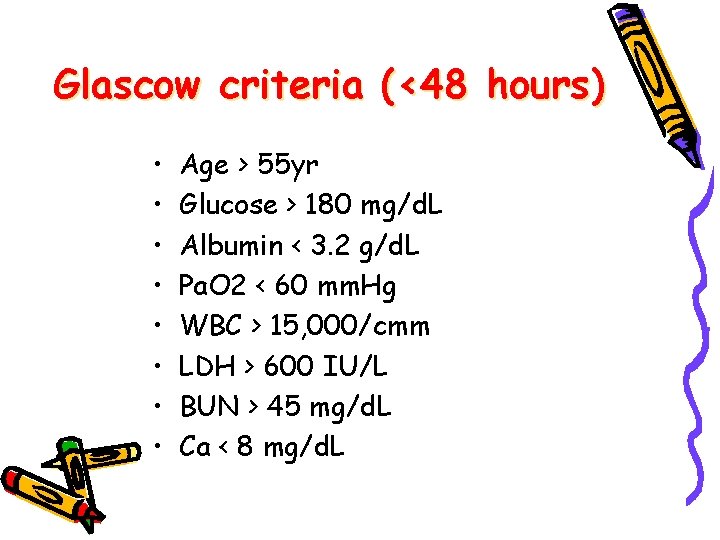
Glascow criteria (<48 hours) • • Age > 55 yr Glucose > 180 mg/d. L Albumin < 3. 2 g/d. L Pa. O 2 < 60 mm. Hg WBC > 15, 000/cmm LDH > 600 IU/L BUN > 45 mg/d. L Ca < 8 mg/d. L
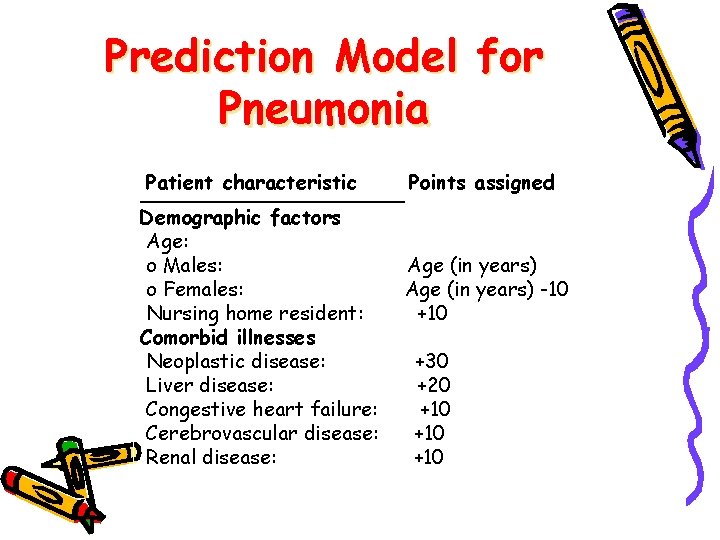
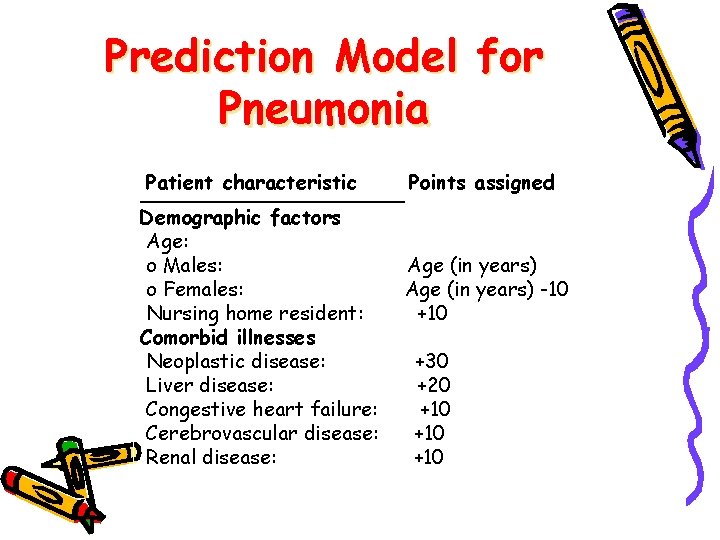
Prediction Model for Pneumonia Patient characteristic Points ________ Demographic factors Age: o Males: o Females: Nursing home resident: Comorbid illnesses Neoplastic disease: Liver disease: Congestive heart failure: Cerebrovascular disease: Renal disease: assigned Age (in years) -10 +30 +20 +10 +10
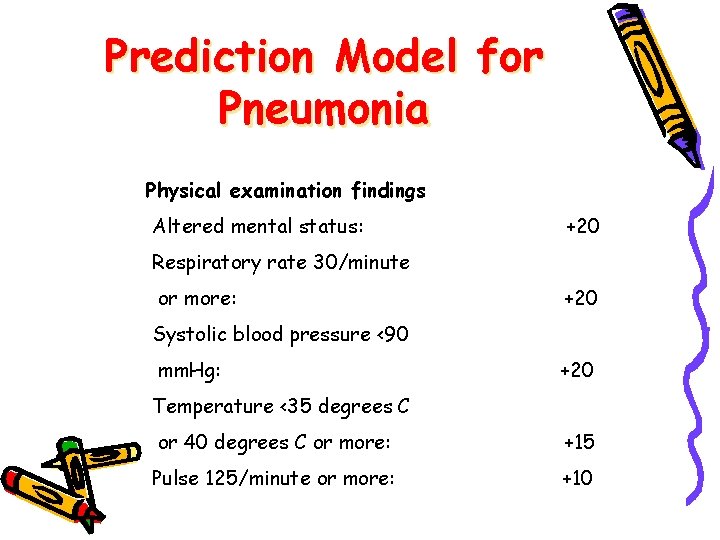
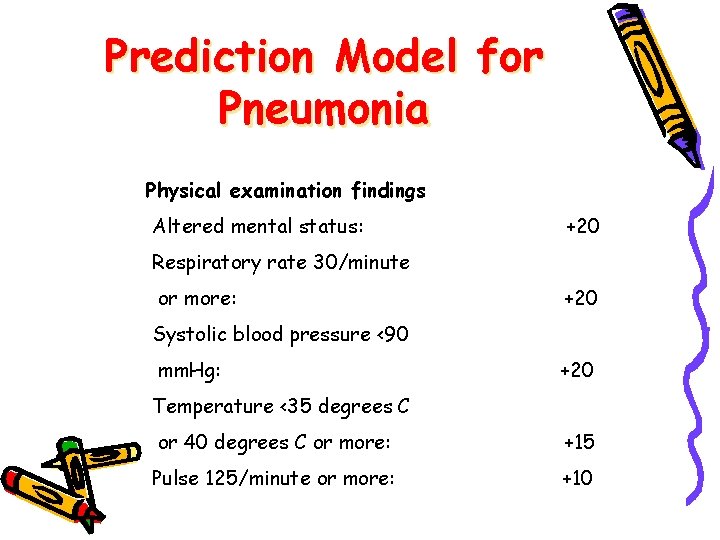
Prediction Model for Pneumonia Physical examination findings Altered mental status: +20 Respiratory rate 30/minute or more: +20 Systolic blood pressure <90 mm. Hg: +20 Temperature <35 degrees C or 40 degrees C or more: +15 Pulse 125/minute or more: +10
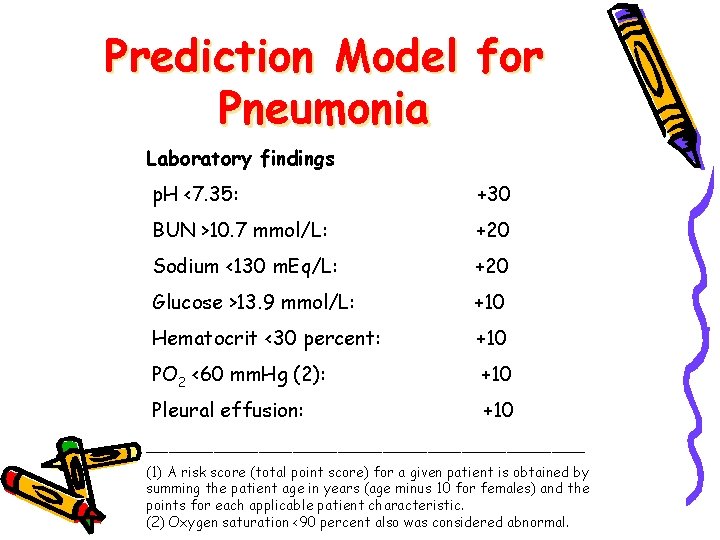
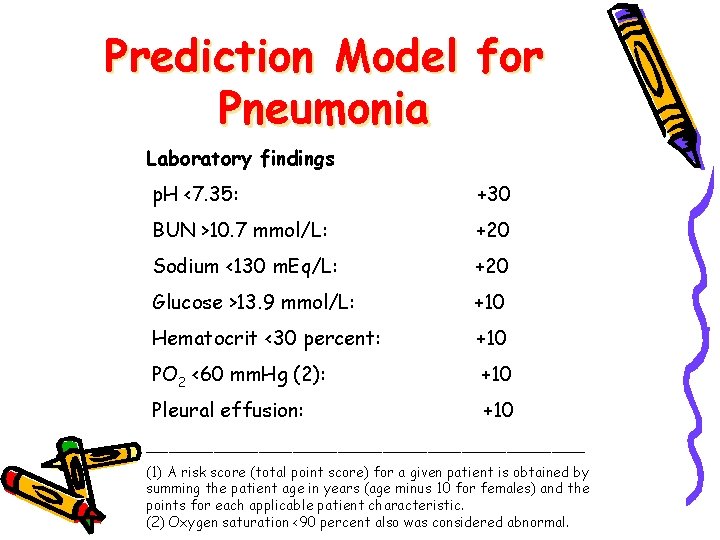
Prediction Model for Pneumonia Laboratory findings p. H <7. 35: +30 BUN >10. 7 mmol/L: +20 Sodium <130 m. Eq/L: +20 Glucose >13. 9 mmol/L: +10 Hematocrit <30 percent: +10 PO 2 <60 mm. Hg (2): +10 Pleural effusion: +10 ____________________ (1) A risk score (total point score) for a given patient is obtained by summing the patient age in years (age minus 10 for females) and the points for each applicable patient characteristic. (2) Oxygen saturation <90 percent also was considered abnormal.
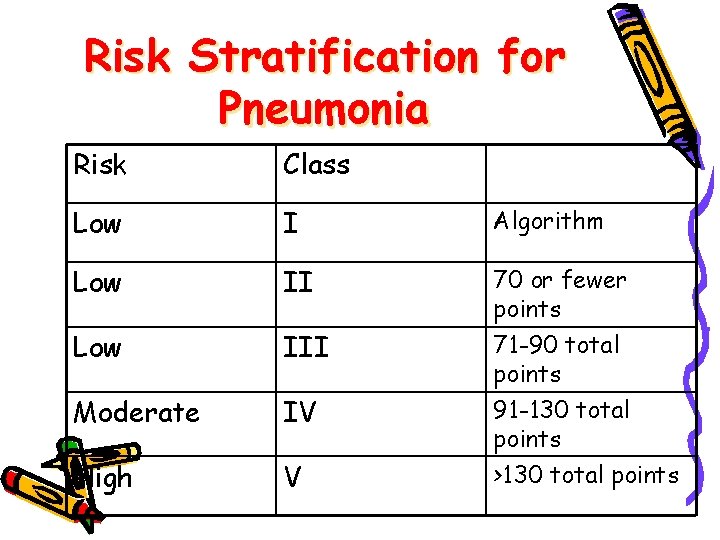
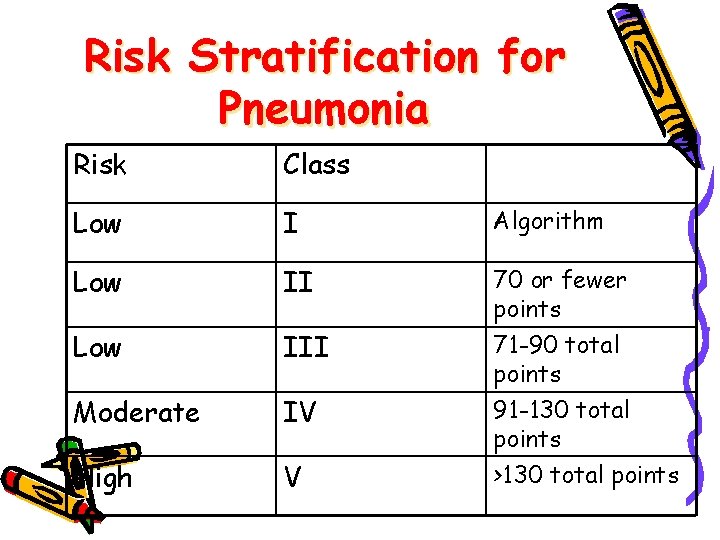
Risk Stratification for Pneumonia Risk Class Low I Algorithm Low II 70 or fewer points Low III Moderate IV High V 71 -90 total points 91 -130 total points >130 total points
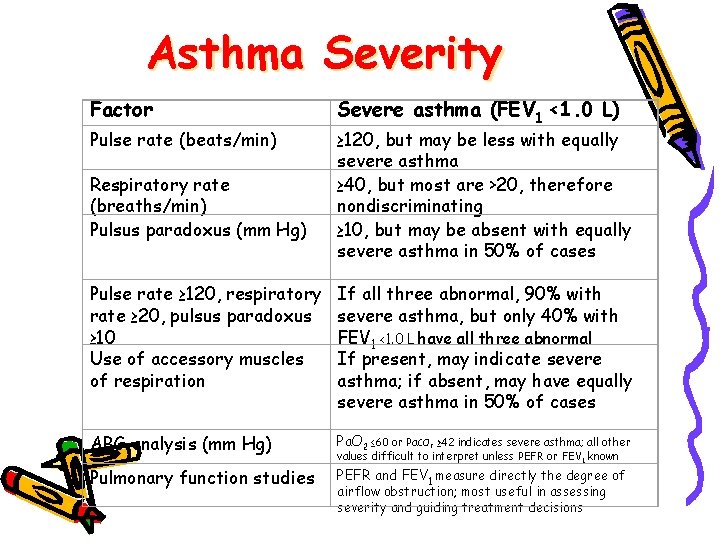
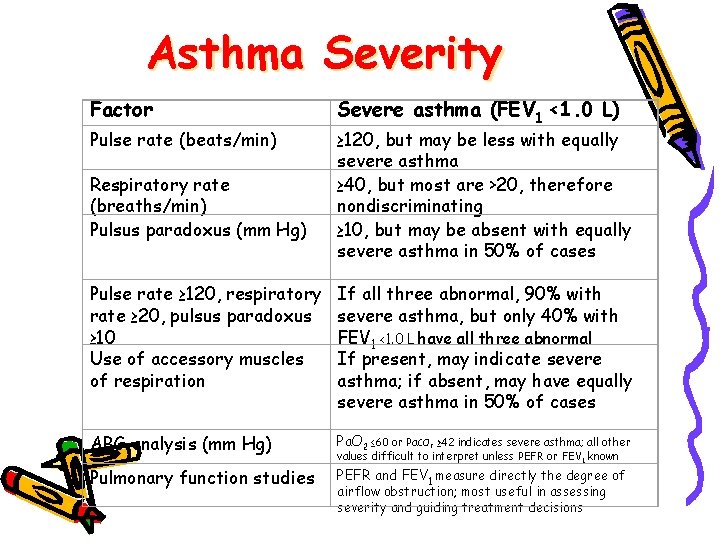
Asthma Severity Factor Pulse rate (beats/min) Respiratory rate (breaths/min) Pulsus paradoxus (mm Hg) Severe asthma (FEV 1 <1. 0 L) ≥ 120, but may be less with equally severe asthma ≥ 40, but most are >20, therefore nondiscriminating ≥ 10, but may be absent with equally severe asthma in 50% of cases Pulse rate ≥ 120, respiratory rate ≥ 20, pulsus paradoxus ≥ 10 Use of accessory muscles of respiration If all three abnormal, 90% with severe asthma, but only 40% with FEV 1 <1. 0 L have all three abnormal If present, may indicate severe asthma; if absent, may have equally severe asthma in 50% of cases ABG analysis (mm Hg) Pa. O 2 ≤ 60 or Pa. CO Pulmonary function studies PEFR and FEV 1 measure directly the degree of ≥ 42 indicates severe asthma; all other values difficult to interpret unless PEFR or FEV 1 known 2 airflow obstruction; most useful in assessing severity and guiding treatment decisions
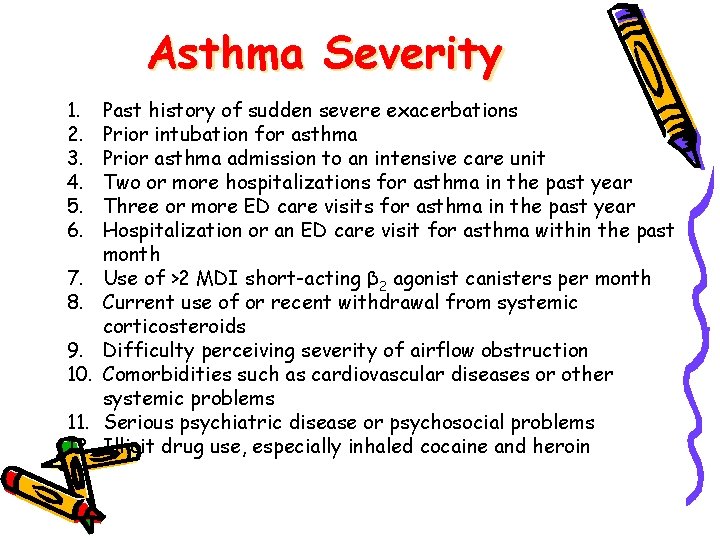
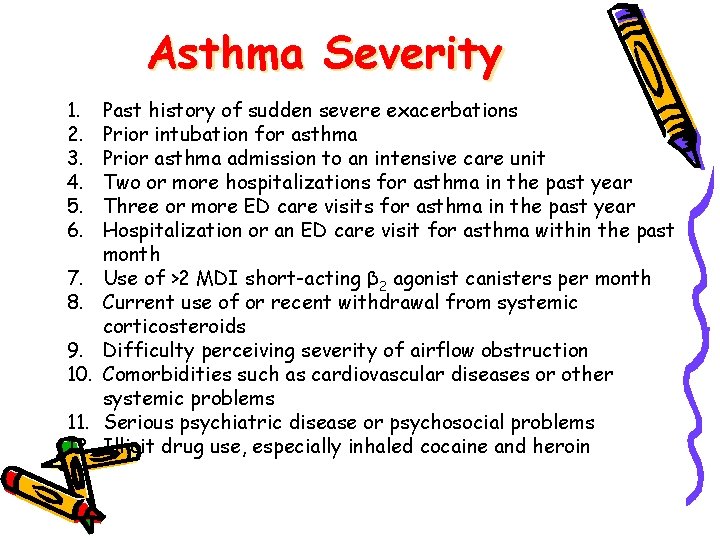
Asthma Severity 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Past history of sudden severe exacerbations Prior intubation for asthma Prior asthma admission to an intensive care unit Two or more hospitalizations for asthma in the past year Three or more ED care visits for asthma in the past year Hospitalization or an ED care visit for asthma within the past month Use of >2 MDI short-acting β 2 agonist canisters per month Current use of or recent withdrawal from systemic corticosteroids Difficulty perceiving severity of airflow obstruction Comorbidities such as cardiovascular diseases or other systemic problems Serious psychiatric disease or psychosocial problems Illicit drug use, especially inhaled cocaine and heroin
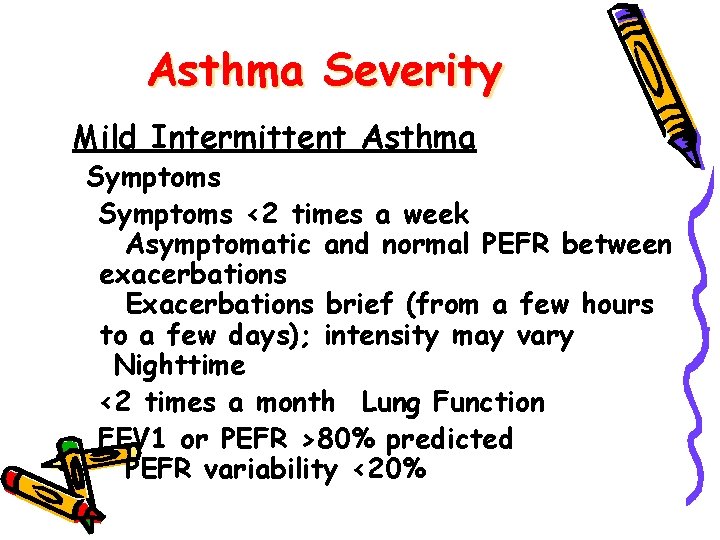
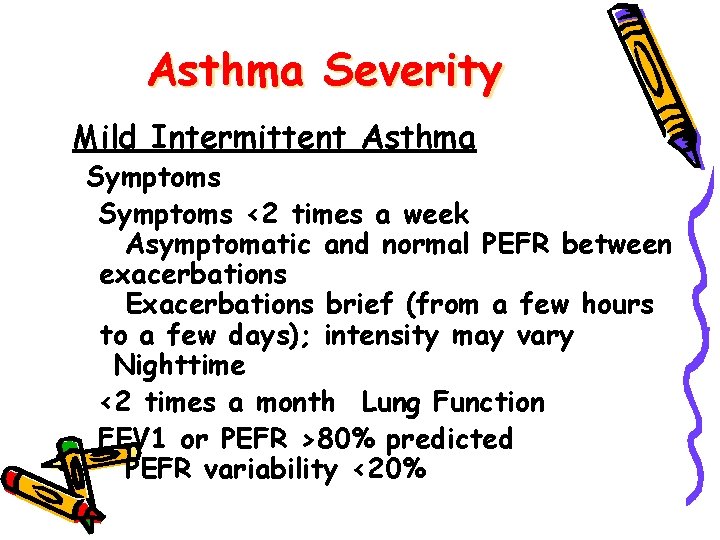
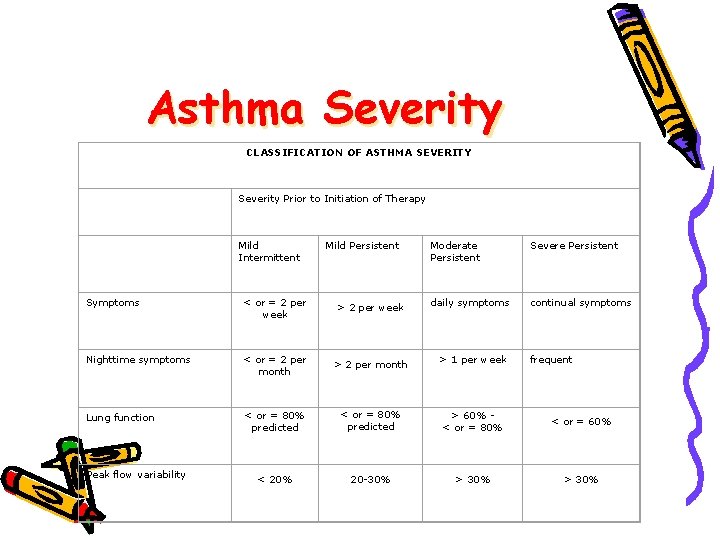
Asthma Severity Mild Intermittent Asthma Symptoms <2 times a week Asymptomatic and normal PEFR between exacerbations Exacerbations brief (from a few hours to a few days); intensity may vary Nighttime <2 times a month Lung Function FEV 1 or PEFR >80% predicted PEFR variability <20%
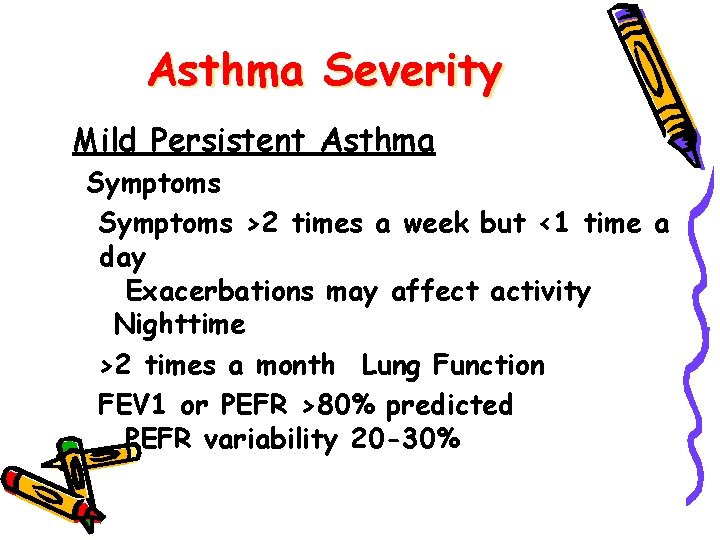
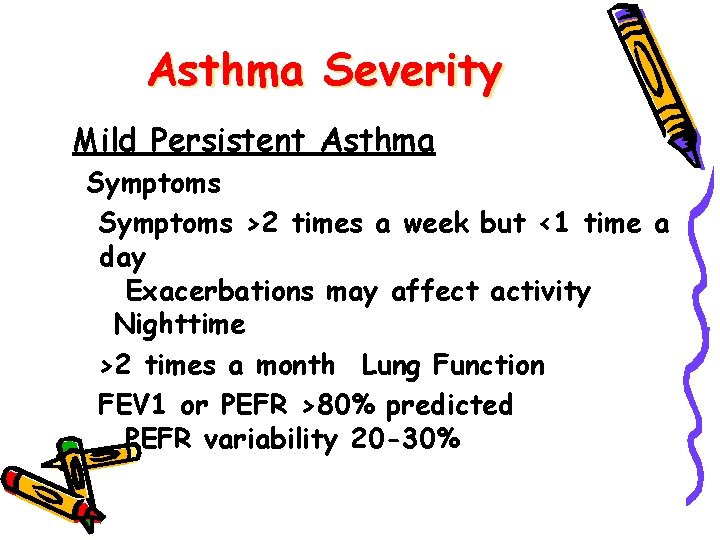
Asthma Severity Mild Persistent Asthma Symptoms >2 times a week but <1 time a day Exacerbations may affect activity Nighttime >2 times a month Lung Function FEV 1 or PEFR >80% predicted PEFR variability 20 -30%
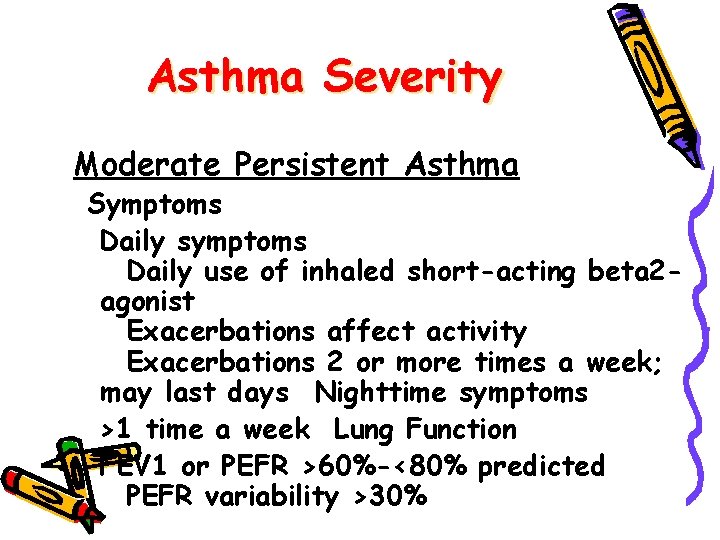
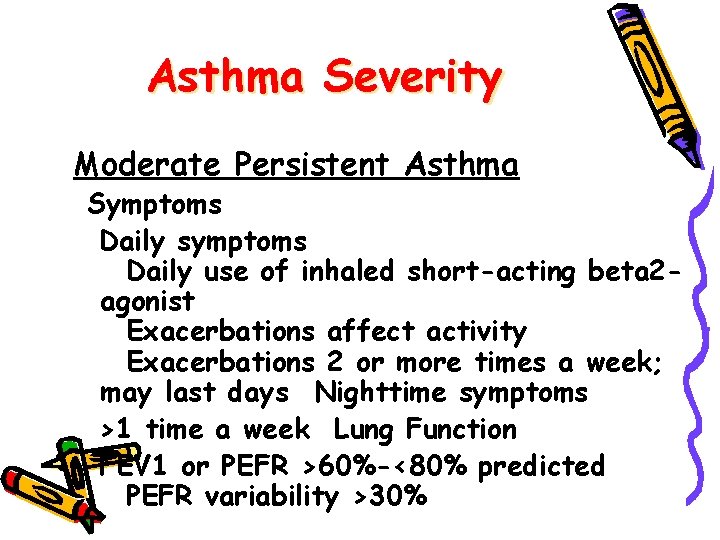
Asthma Severity Moderate Persistent Asthma Symptoms Daily symptoms Daily use of inhaled short-acting beta 2 agonist Exacerbations affect activity Exacerbations 2 or more times a week; may last days Nighttime symptoms >1 time a week Lung Function FEV 1 or PEFR >60%-<80% predicted PEFR variability >30%
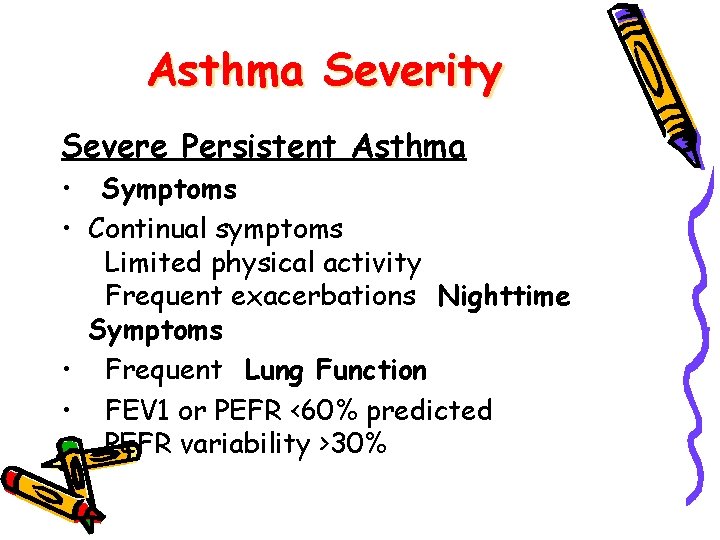
Asthma Severity Severe Persistent Asthma • Symptoms • Continual symptoms Limited physical activity Frequent exacerbations Nighttime Symptoms • Frequent Lung Function • FEV 1 or PEFR <60% predicted PEFR variability >30%
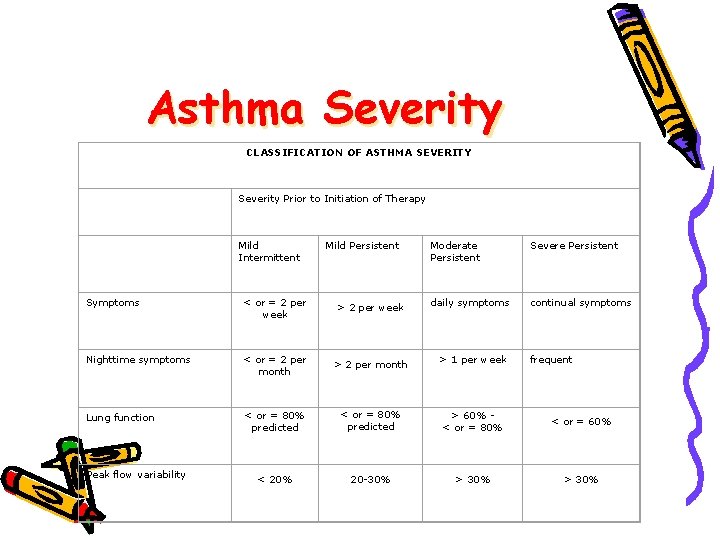
Asthma Severity CLASSIFICATION OF ASTHMA SEVERITY Severity Prior to Initiation of Therapy Mild Intermittent Mild Persistent Moderate Persistent Severe Persistent daily symptoms continual symptoms Symptoms < or = 2 per week > 2 per week Nighttime symptoms < or = 2 per month > 1 per week Lung function < or = 80% predicted > 60% < or = 80% < or = 60% < 20% 20 -30% > 30% Peak flow variability frequent
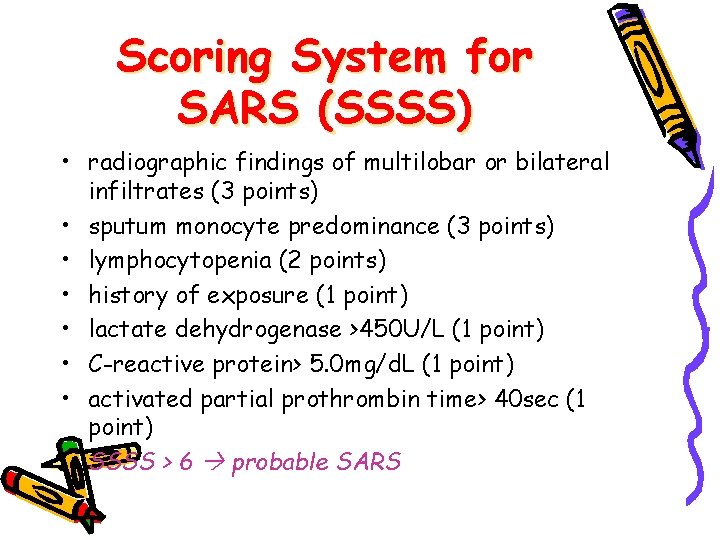
Scoring System for SARS (SSSS) • radiographic findings of multilobar or bilateral infiltrates (3 points) • sputum monocyte predominance (3 points) • lymphocytopenia (2 points) • history of exposure (1 point) • lactate dehydrogenase >450 U/L (1 point) • C-reactive protein> 5. 0 mg/d. L (1 point) • activated partial prothrombin time> 40 sec (1 point) SSSS > 6 probable SARS
