EMERGENCY SEVERITY INDEX DEFINITION OF TRIAGE Classification of

- Slides: 44

EMERGENCY SEVERITY INDEX
DEFINITION OF TRIAGE Classification of patient acuity that characterizes the degree to which the patient’s condition is life or limb threatening and whether immediate treatment is needed to alleviate symptoms
ENA-ACEP JOINT STATEMENT Joint ENA-ACEP Task Force convened in 2003 to study the evidence on 5 level triage systems and issued the following statement: �ACEP and ENA believe that quality of patient care would benefit from implementing a standardized ED triage scale and acuity categorization process. Based expert consensus of currently available evidence, ACEP and ENA support the adoption of a reliable, valid 5 level triage scale
WHAT CONSTITUTES A GOOD TRIAGE INSTRUMENT? • Facilitates the prioritization of patients based on the urgency of the patient’s condition ▫ “Who should be seen first? ” ▫ “How long can everybody wait? ” ▫ “Which resources are needed? ” • Patient streaming: ▫ Getting the right patient to the right resources at the right place and at the right time
INTRODUCTION TO ESI (EMERGENCY SEVERITY INDEX) • Simple to use • 5 levels of triage • Categorizes patients by evaluating patient acuity and resources • Acuity is determined by the stability of vital functions and potential for life, limb, or organ threat
Comprehensive Eyeball
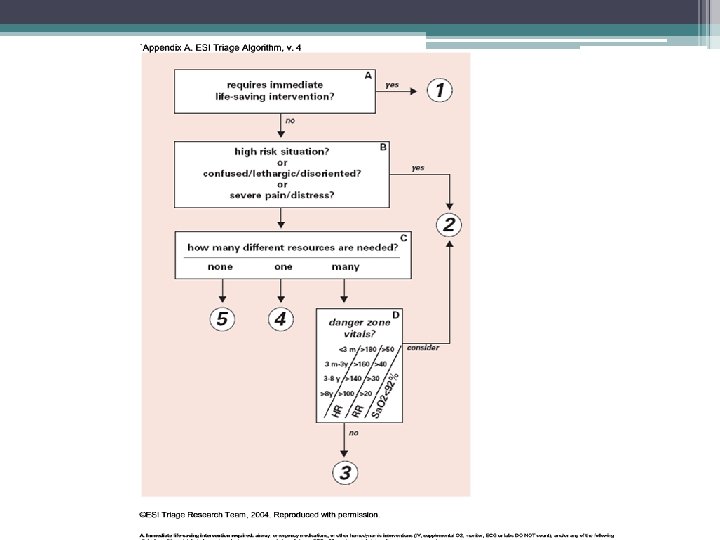
ALGORITHM DECISION POINT A • Does the patient require immediate life-saving intervention? ▫ Level 1 patients are seen immediately because timeliness of interventions can affect morbidity and mortality �Immediate physician involvement in the care of the patient is a key difference between level 1 and level 2 • UNRESPONSIVENESS ▫ Goal is to identify the patient who has an acute change in LOC—compare with baseline �AVPU
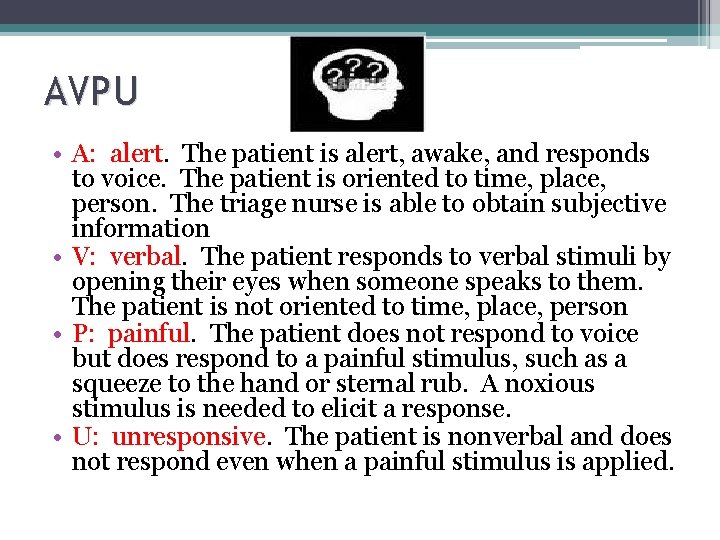
AVPU • A: alert. The patient is alert, awake, and responds to voice. The patient is oriented to time, place, person. The triage nurse is able to obtain subjective information • V: verbal. The patient responds to verbal stimuli by opening their eyes when someone speaks to them. The patient is not oriented to time, place, person • P: painful. The patient does not respond to voice but does respond to a painful stimulus, such as a squeeze to the hand or sternal rub. A noxious stimulus is needed to elicit a response. • U: unresponsive. The patient is nonverbal and does not respond even when a painful stimulus is applied.
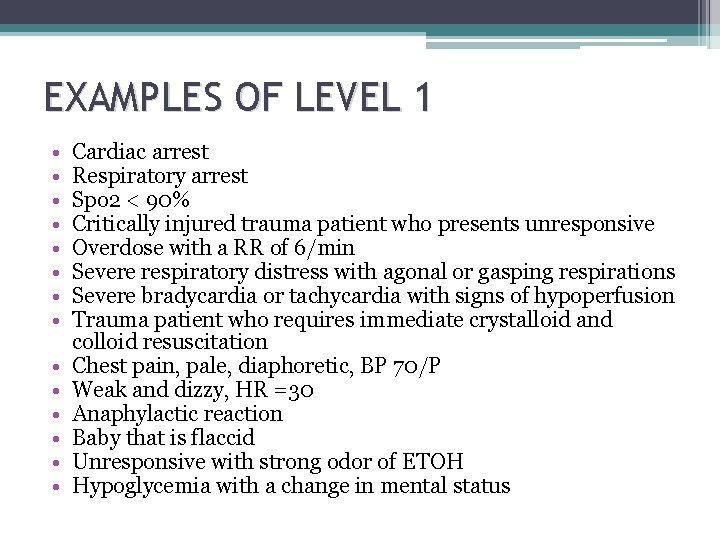
EXAMPLES OF LEVEL 1 • • • • Cardiac arrest Respiratory arrest Spo 2 < 90% Critically injured trauma patient who presents unresponsive Overdose with a RR of 6/min Severe respiratory distress with agonal or gasping respirations Severe bradycardia or tachycardia with signs of hypoperfusion Trauma patient who requires immediate crystalloid and colloid resuscitation Chest pain, pale, diaphoretic, BP 70/P Weak and dizzy, HR =30 Anaphylactic reaction Baby that is flaccid Unresponsive with strong odor of ETOH Hypoglycemia with a change in mental status
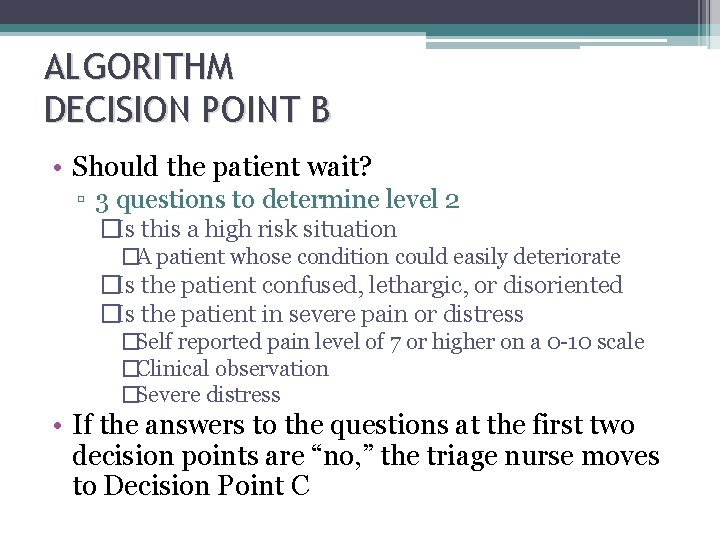
ALGORITHM DECISION POINT B • Should the patient wait? ▫ 3 questions to determine level 2 �Is this a high risk situation �A patient whose condition could easily deteriorate �Is the patient confused, lethargic, or disoriented �Is the patient in severe pain or distress �Self reported pain level of 7 or higher on a 0 -10 scale �Clinical observation �Severe distress • If the answers to the questions at the first two decision points are “no, ” the triage nurse moves to Decision Point C
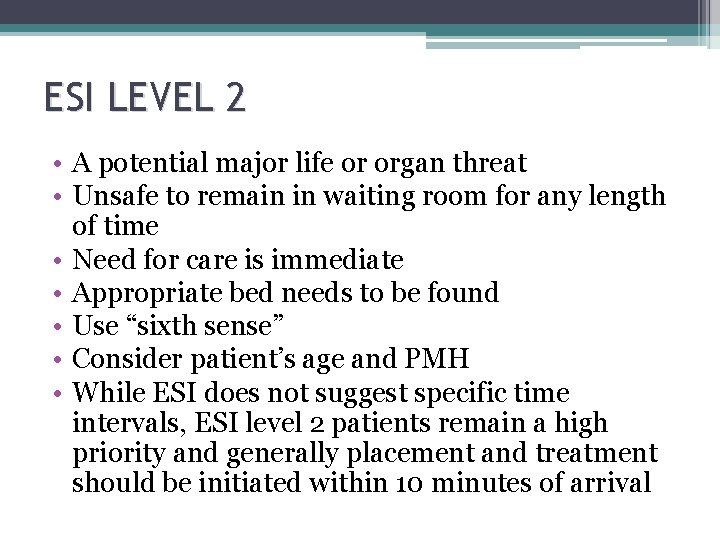
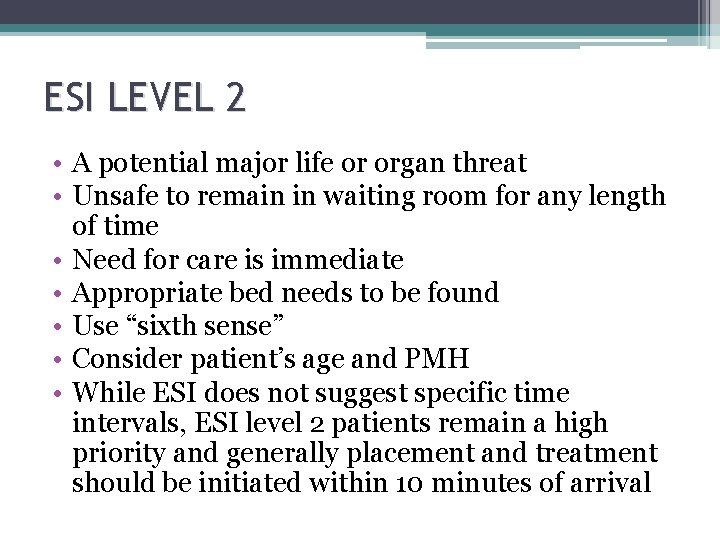
ESI LEVEL 2 • A potential major life or organ threat • Unsafe to remain in waiting room for any length of time • Need for care is immediate • Appropriate bed needs to be found • Use “sixth sense” • Consider patient’s age and PMH • While ESI does not suggest specific time intervals, ESI level 2 patients remain a high priority and generally placement and treatment should be initiated within 10 minutes of arrival
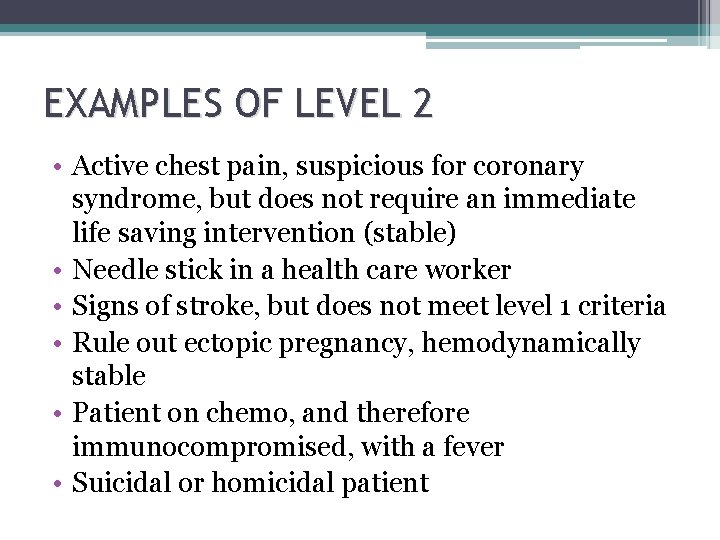
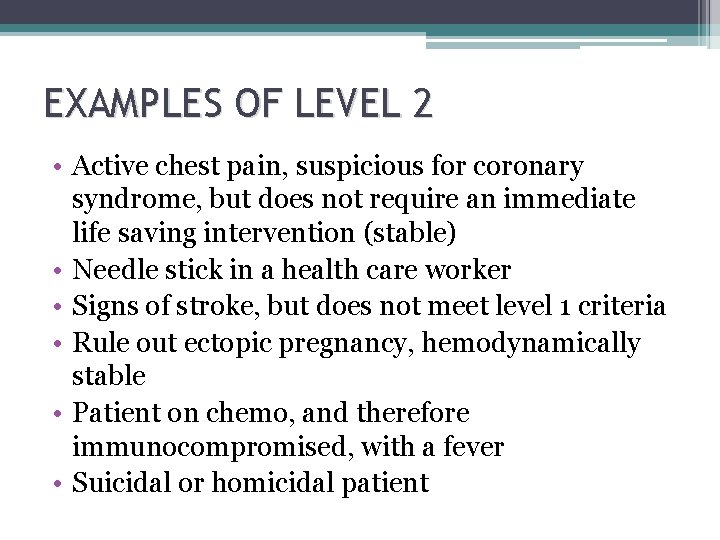
EXAMPLES OF LEVEL 2 • Active chest pain, suspicious for coronary syndrome, but does not require an immediate life saving intervention (stable) • Needle stick in a health care worker • Signs of stroke, but does not meet level 1 criteria • Rule out ectopic pregnancy, hemodynamically stable • Patient on chemo, and therefore immunocompromised, with a fever • Suicidal or homicidal patient
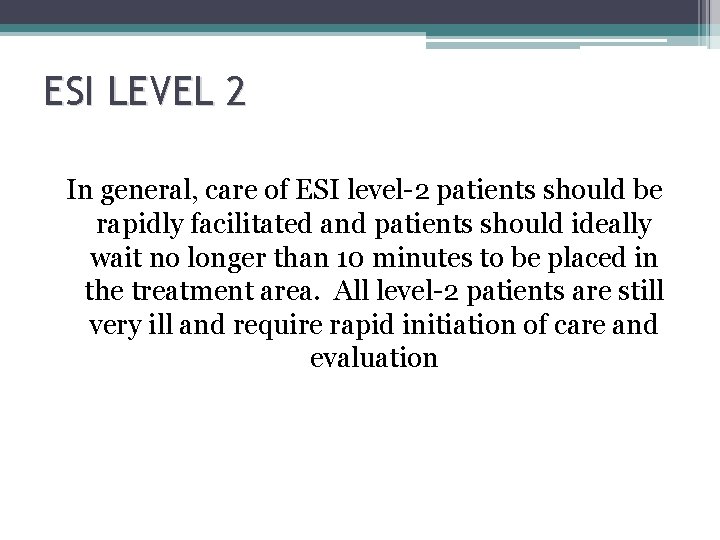
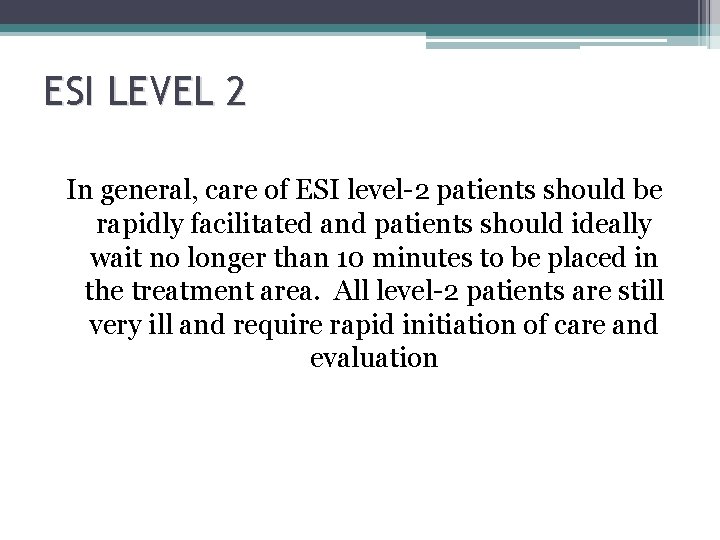
ESI LEVEL 2 In general, care of ESI level-2 patients should be rapidly facilitated and patients should ideally wait no longer than 10 minutes to be placed in the treatment area. All level-2 patients are still very ill and require rapid initiation of care and evaluation
ALGORITHM DECISION POINT C • “How many different resources are needed? ” • Be familiar with the ED standards of care to identify resource needs • Resource prediction is only used for less acute patients and is an integral part of the ESI levels 3, 4, or 5
ESI LEVEL 3 • Patients who are expected to need two or more resources are designated an ESI level-3. Once the triage nurse has identified two probable resources, there is no need to continue to estimate resources • The triage nurse should count the number of different types of resources needed to determine the patient’s disposition, not the number of individual tests • Usually, a patient requires either no resources, one, or two or more resources
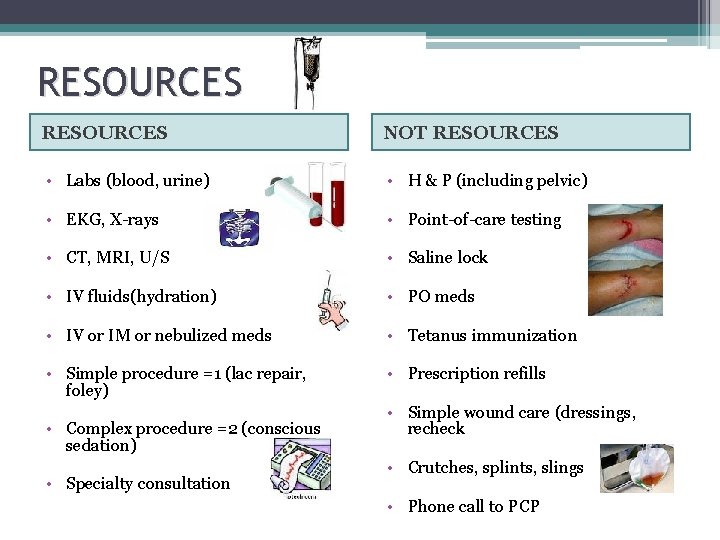
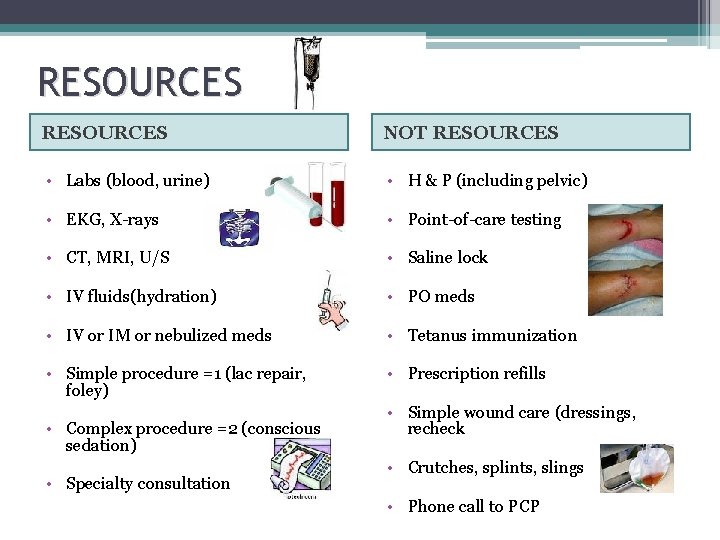
RESOURCES NOT RESOURCES • Labs (blood, urine) • H & P (including pelvic) • EKG, X-rays • Point-of-care testing • CT, MRI, U/S • Saline lock • IV fluids(hydration) • PO meds • IV or IM or nebulized meds • Tetanus immunization • Simple procedure =1 (lac repair, foley) • Prescription refills • Complex procedure =2 (conscious sedation) • Specialty consultation • Simple wound care (dressings, recheck • Crutches, splints, slings • Phone call to PCP
ESI LEVEL 4 AND 5 If your patient does not need two resources, you must determine how many resources if any to decide on an ESI Level 4 or 5 ▫ Level 4 – One resource ▫ Level 5 – No resources
SCENARIO 1 • 22 year old male with RLQ pain since early this morning, also c/o nausea and no appetite • PREDICTED RESOURCES: � 2 or more: lab studies, IV fluids, Abdominal CT, possible surgery consult • ESI TRIAGE CATEGORY: � 3
SCENARIO 2 • 45 year old obese female with left lower leg pain and swelling which started 2 days ago, after driving in a car for 12 hours • PREDICTED RESOURCES: • Labs, ultrasound, possible anticoagulant therapy • ESI TRIAGE CATEGORY: • 3
SCENARIO 3 • Healthy, 19 year old female who twisted her ankle playing soccer. Edema at lateral malleolus; hurts to bear weight • PREDICTED RESOURCES: • Ankle x-ray • ESI TRIAGE CATEGORY: • 4
SCENARIO 4 • Healthy 29 year old female with UTI symptoms, appears well; afebrile; denies vaginal discharge • PREDICTED RESOURCES: • Urine and urine culture, possible urine h. CG • ESI TRIAGE CATEGORY: • 4
SCENARIO 5 • Healthy 10 year old child with poison ivy on extremities • PREDICTED RESOURCES: • None • ESI TRIAGE CATEGORY: ▫ 5
SCENARIO 6 • Healthy 52 year old man ran out of BP medication yesterday. BP 150/84. No acute complaints • PREDICTED RESOURCES: • None • ESI TRIAGE CATEGORY: • 5
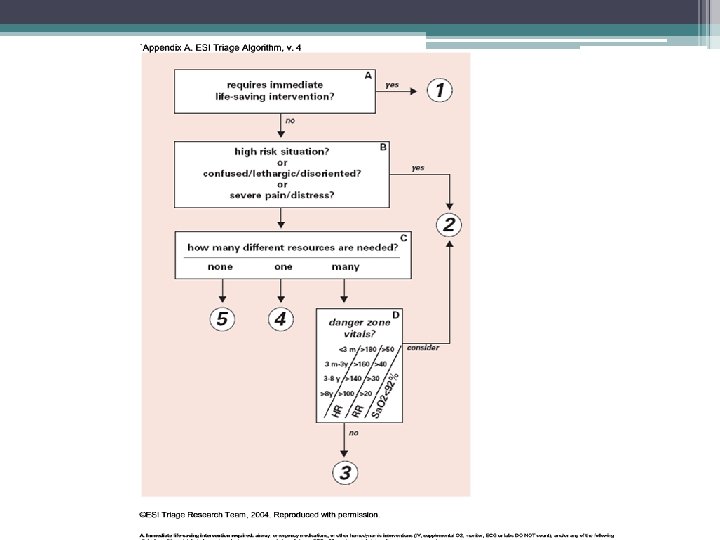
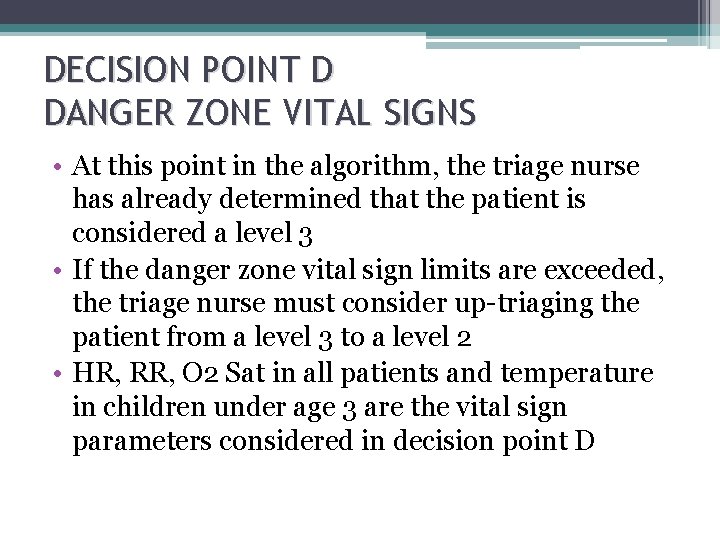
DECISION POINT D DANGER ZONE VITAL SIGNS • At this point in the algorithm, the triage nurse has already determined that the patient is considered a level 3 • If the danger zone vital sign limits are exceeded, the triage nurse must consider up-triaging the patient from a level 3 to a level 2 • HR, RR, O 2 Sat in all patients and temperature in children under age 3 are the vital sign parameters considered in decision point D
ARE VITAL SIGNS NECESSARY AT TRIAGE? • Vital signs may not always be the most appropriate tool to determine triage acuity • Age, PMH, and social history should be considered in trying to determine acuity level • The only absolute requirement for vital signs assessment is for patients who don’t initially meet level 1 or 2 criteria, but who are predicted to need two or more resources (level 3)
ARE VITAL SIGNS NECESSARY AT TRIAGE? • Optional at triage and at the discretion of the nurse for patients triaged at level 1, 2, 4, or 5 • It is never WRONG to obtain a set of vital signs. Only REQUIRED for patients considered level-3 • It is important to note that when considering abnormal vital signs, BP is not included in the ESI algorithm. ▫ This does not mean that the triage nurse should not take a BP or a temperature on older children or adults but that these vital signs are not necessarily used to assist in selecting the appropriate triage acuity level.
PEDIATRIC VITAL SIGNS • The ESI Research Team recommends that vital signs in patients under age 3 be assessed at triage. ▫ Vital sign evaluation is essential to the overall assessment of a known febrile infant under age 36 months. ▫ This helps to differentiate ESI level-2 and 3 patients and minimize the risk that potentially bacteremic children will be sent to the waiting area and experience an inappropriate wait. • When triaging a child between 3 and 36 months of age who is highly febrile, it is important to assess the child’s immunization status and whethere is an identifiable source for the fever
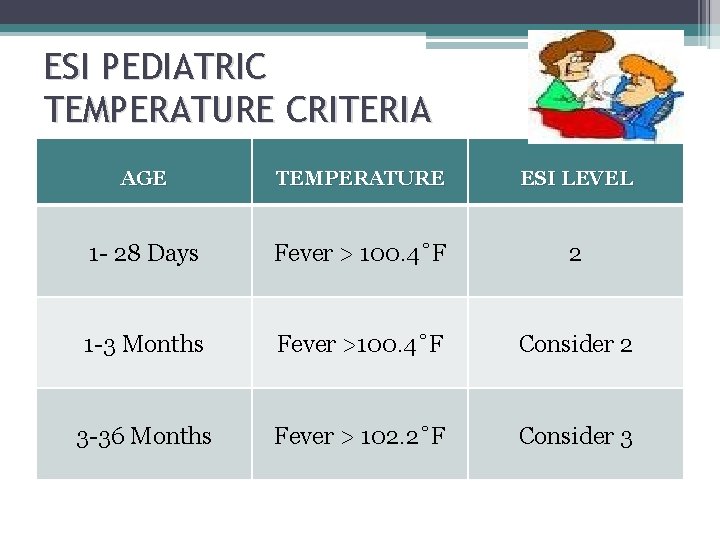
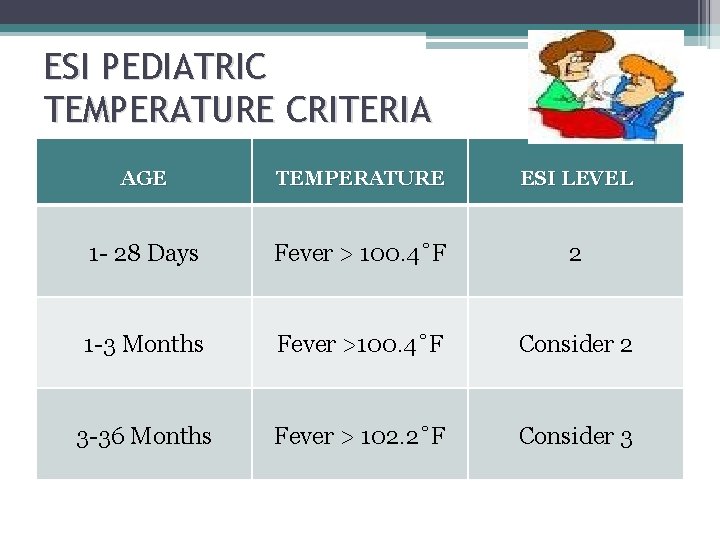
ESI PEDIATRIC TEMPERATURE CRITERIA AGE TEMPERATURE ESI LEVEL 1 - 28 Days Fever > 100. 4˚F 2 1 -3 Months Fever >100. 4˚F Consider 2 3 -36 Months Fever > 102. 2˚F Consider 3
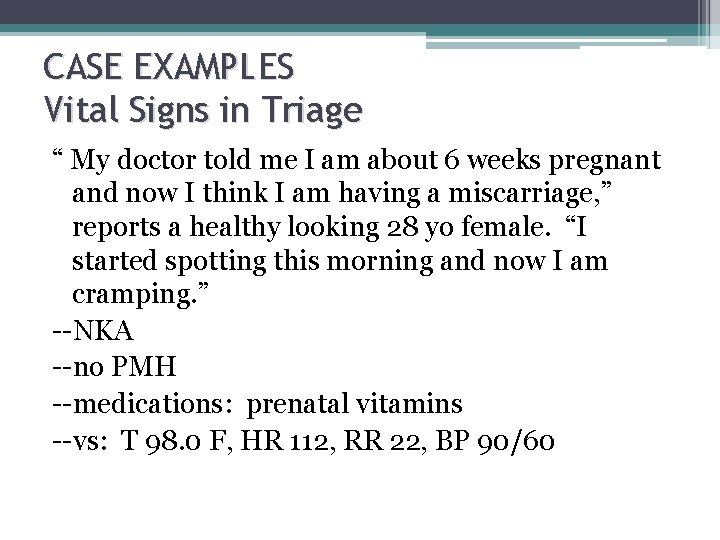
CASE EXAMPLES Vital Signs in Triage “ My doctor told me I am about 6 weeks pregnant and now I think I am having a miscarriage, ” reports a healthy looking 28 yo female. “I started spotting this morning and now I am cramping. ” --NKA --no PMH --medications: prenatal vitamins --vs: T 98. 0 F, HR 112, RR 22, BP 90/60
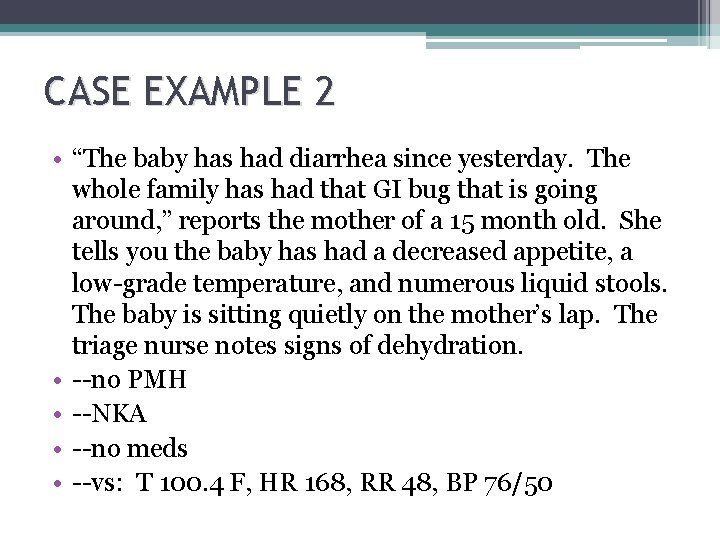
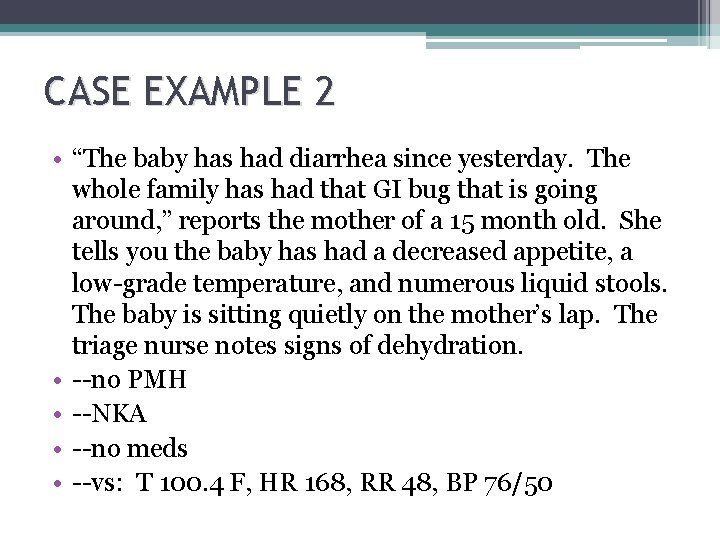
CASE EXAMPLE 2 • “The baby has had diarrhea since yesterday. The whole family has had that GI bug that is going around, ” reports the mother of a 15 month old. She tells you the baby has had a decreased appetite, a low-grade temperature, and numerous liquid stools. The baby is sitting quietly on the mother’s lap. The triage nurse notes signs of dehydration. • --no PMH • --NKA • --no meds • --vs: T 100. 4 F, HR 168, RR 48, BP 76/50
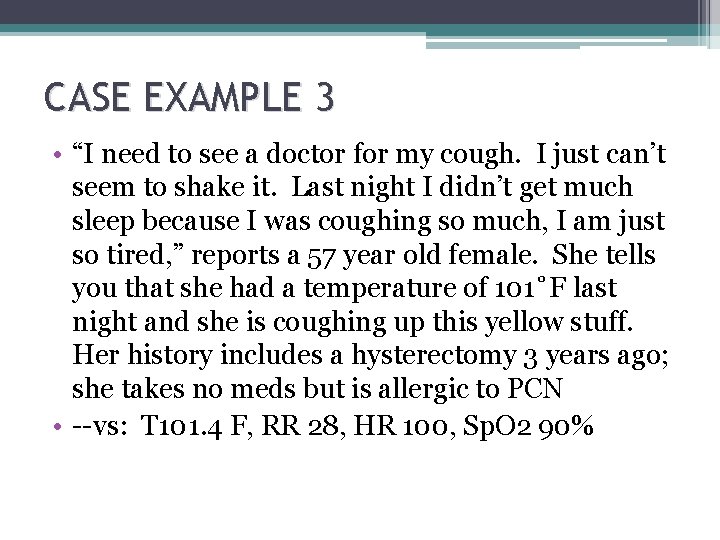
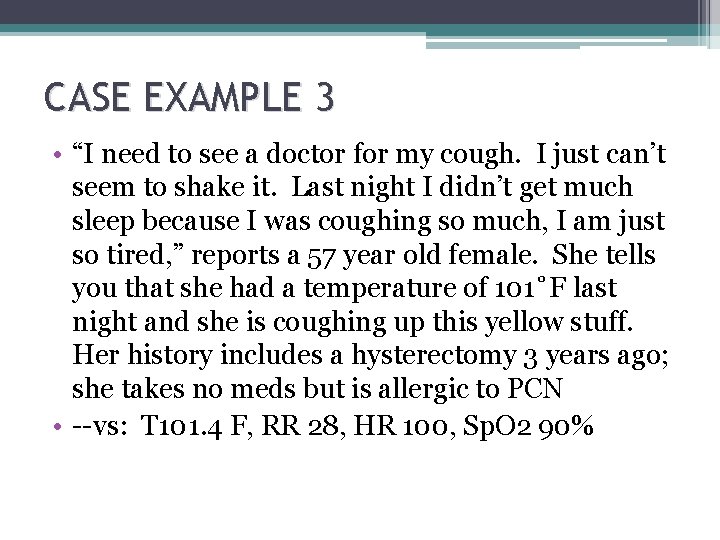
CASE EXAMPLE 3 • “I need to see a doctor for my cough. I just can’t seem to shake it. Last night I didn’t get much sleep because I was coughing so much, I am just so tired, ” reports a 57 year old female. She tells you that she had a temperature of 101˚F last night and she is coughing up this yellow stuff. Her history includes a hysterectomy 3 years ago; she takes no meds but is allergic to PCN • --vs: T 101. 4 F, RR 28, HR 100, Sp. O 2 90%
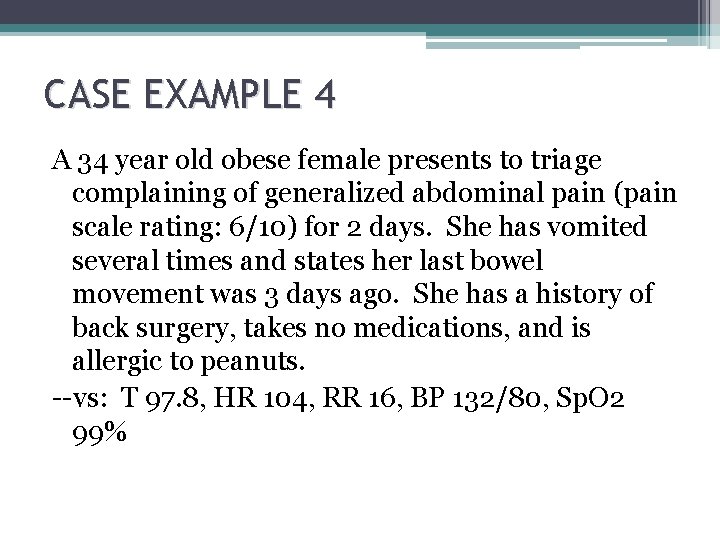
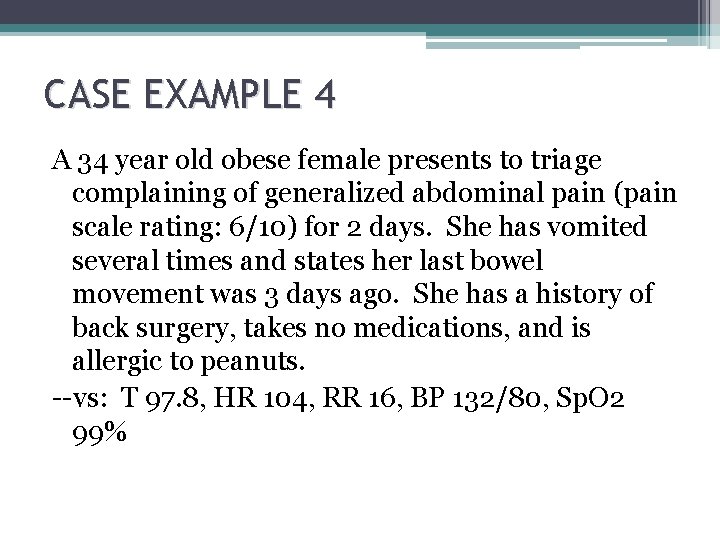
CASE EXAMPLE 4 A 34 year old obese female presents to triage complaining of generalized abdominal pain (pain scale rating: 6/10) for 2 days. She has vomited several times and states her last bowel movement was 3 days ago. She has a history of back surgery, takes no medications, and is allergic to peanuts. --vs: T 97. 8, HR 104, RR 16, BP 132/80, Sp. O 2 99%
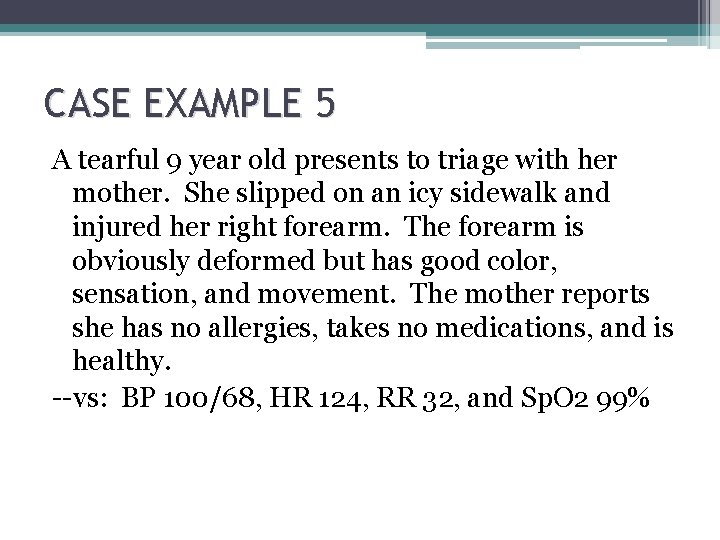
CASE EXAMPLE 5 A tearful 9 year old presents to triage with her mother. She slipped on an icy sidewalk and injured her right forearm. The forearm is obviously deformed but has good color, sensation, and movement. The mother reports she has no allergies, takes no medications, and is healthy. --vs: BP 100/68, HR 124, RR 32, and Sp. O 2 99%
CASE EXAMPLE 6 A 72 y/o patient presents to the ED with her oxygen via NC for her advanced COPD. She informs the triage nurse that she has an infected cat bite on her left hand. The hand is red, tender, and swollen. The patient has no other medical problems, uses albuterol prn, and takes an ASA daily, NKDA --vs: T 99. 6 F, HR 88, RR 22, BP 138/80, Sp. O 2 91%. She denies respiratory distress
SCENARIOS IN WHICH FLOW AND TRIAGE CATEGORY MAY CONFLICT TRAUMA The patient presents to triage with localized right upper quadrant pain with stable vital signs. This patient is physiologically stable, walked into the ED and does not meet ESI level-1. However, the patient is at high risk for a liver laceration and other significant trauma, so should be triaged as ESI level 2.
CHEST PAIN If a patient is physiologically stable but experiencing chest pain that is potentially an acute coronary syndrome, the patient meets level -2 criteria. They do not require immediate life saving interventions but they are a high risk patient. Their care is time-sensitive, an EKG should be performed within 10 minutes of patient arrival. But the patient with chest pain who presents to triage diaphoretic, with a BP of 80/palp would meet level-1 criteria.
STROKE A patient who present with signs of an acute stroke. Again, if physiologically stable, a 10 minute wait to initiate care will probably not further compromise the patient. However, the patient with signs of stroke that is unable to maintain an airway meets ESI level-1 criteria.
CONSIDER PAIN An elderly patient fell, may have a fractured hip, arrives by private car with family, and is in pain. The patient does not really meet ESI level-2 criteria but is very uncomfortable. The triage nurse would categorize the patient as ESI level 3 and probably place the patient in an available bed before other ESI level-3 patients
ARRIVING BY AMBULANCE Ambulance patients may also present with a similar scenario. Arriving by ambulance is not a criterion to assign a patient ESI level 1 or 2. The ESI criteria should always be used to determine triage level without regard to method of arrival
IMPLEMENTATION OF ESI TRIAGE • A well thought out implementation plan is critical to successful integration of the ESI into the emergency department • Application of Kurt Lewin’s theory of planned change ▫ 3 phases of change �Unfreezing �Movement �Refreezing • Triage committee It is well established that without adequate planning, implementation will fail
 Esi triage examples
Esi triage examples Avpu
Avpu Ctas triage
Ctas triage Dust storm severity index
Dust storm severity index Pneumonia severity index
Pneumonia severity index Dr fawad ahmad randhawa
Dr fawad ahmad randhawa Nsap 腹痛
Nsap 腹痛 Asthma classifications
Asthma classifications Wash severity classification
Wash severity classification Jagsync
Jagsync Netlogo dictionary
Netlogo dictionary Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Autism range severity
Autism range severity Normal ankle brachial index
Normal ankle brachial index Injury severity score
Injury severity score Severity assessment adalah
Severity assessment adalah Asthma control
Asthma control Hiradc sample
Hiradc sample Severity of hemophilia
Severity of hemophilia Rvsp calculation
Rvsp calculation John conrad otto
John conrad otto Pcc severity rating scale
Pcc severity rating scale Symptom assessment scale palliative care
Symptom assessment scale palliative care Low priority high severity example
Low priority high severity example Asam ladder
Asam ladder How to write a letter in afrikaans
How to write a letter in afrikaans Sql server agent alerts for severity 16 through 25
Sql server agent alerts for severity 16 through 25 Venous clinical severity score
Venous clinical severity score Sp_redirect_publisher
Sp_redirect_publisher Safe t score formula
Safe t score formula Memory architecture in sql server
Memory architecture in sql server Fmea exercise
Fmea exercise Optical fibre
Optical fibre Primary index is dense or sparse
Primary index is dense or sparse Mycobacterium leprae
Mycobacterium leprae Pqli advantages and disadvantages
Pqli advantages and disadvantages Diff between step index and graded index fiber
Diff between step index and graded index fiber How to calculate simpsons diversity index
How to calculate simpsons diversity index Consistency index and liquidity index
Consistency index and liquidity index Clustered index và non clustered index
Clustered index và non clustered index Smart triage kit
Smart triage kit Ocular emergency definition
Ocular emergency definition Nutrition emergency definition
Nutrition emergency definition Gagandeep singh bedi
Gagandeep singh bedi Psystart
Psystart