Review of START and Jump Start Triage Condell


















- Slides: 70
Review of START and Jump. Start Triage Condell Medical Center EMS System ECRN Disaster Training Module March 2009 Material development by Illinois EMSC and children’s Memorial Hospital. Modified for CMC staff by Sharon Hopkins, RN, BSN, EMT-P
Rationale for the Packet § Without training you will be ill-prepared to respond to a disaster/multiple patient incident § START and Jump. START triage is the triage process in the Region X Multiple Patient Plan for disaster management § This training is to review the triage processes referred to as START for the adult and Jump. Start for the pediatric patient § This triage is usually performed in the field but can be adapted to be performed in the ED
Pediatric Disaster Triage Utilizing the Jump. START Method March 2009 Development of this educational program was sponsored by Illinois EMSC and Children’s Memorial Hospital and supported in part by an Assistant Secretary for Preparedness and Response (ASPR) grant. This program was adapted from a module developed through HRSA funding by the Chicago Department of Public Health. Program adapted to Condell ECRN CE by Sharon Hopkins, RN, BSN 3. 09
Disclaimer NOTE: This slide set and all related training information provided in this session is in accordance with current practice at the time that this program was developed. This program was developed utilizing federal grant funding, therefore all training materials are considered under public domain and can be utilized by others in the conduction of similar educational programs, provided there is acknowledgement of the source of these materials. When using these training materials, please include appropriate acknowledgements which can be found on the last slide in this presentation. These training materials are available on the Illinois EMSC website http: //www. luhs. org/emsc
Objectives § Review unique pediatric issues in a disaster situation § Review incorporating pediatrics into your disaster planning § Review triage and the pediatric patient § Review START and Jump. START triage § Complete triage scenario exercises in the packet § Complete the quiz with a score of 80% or better
“That Won’t Happen in My Backyard”

Disaster “A medical disaster occurs when the destructive effects of natural or man made forces overwhelm the ability of a given area or community to meet the demand for health care. ” ACEP Policy Statement June 2000
Mass Casualty Incident Any incident in which there are more patients than rescuers with inadequate resources to immediately care for them
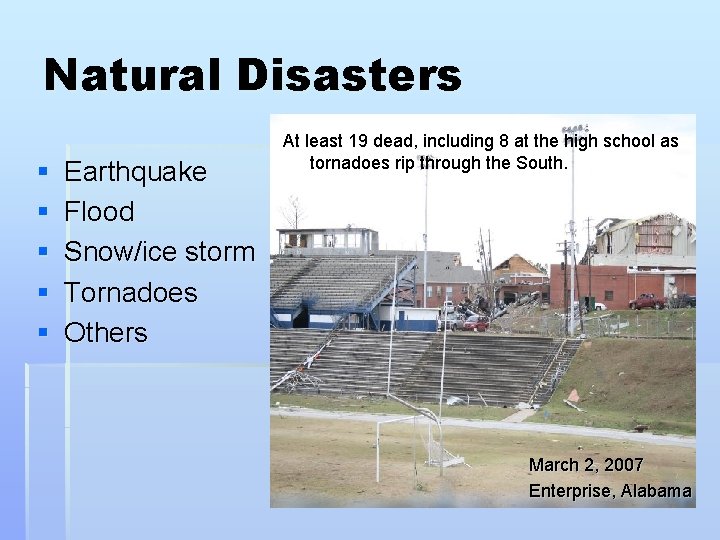
Natural Disasters § § § Earthquake Flood Snow/ice storm Tornadoes Others At least 19 dead, including 8 at the high school as tornadoes rip through the South. March 2, 2007 Enterprise, Alabama

Natural Disasters can involve pediatric patients

Terrorist events § § Arson Bombings Shootings Use of chemical, biological or nuclear agents
The Old Way of Thinking… Kids were secondary victims of terrorism and inadvertently targeted
The new way of thinking … Children may be intentionally targeted Photo courtesy of Charles H Porter IV

Are you prepared?
Illinois Demographics § Illinois is the 5 th most populous state with a population of 12. 7 million § Over 3 million children <18 years of age § 900, 000 are age five and younger. § Percent of Illinois children <18 y/o increased 10% between 1990 - 2000 § In the event of a disaster or terrorist event, children would be one of our most vulnerable populations
Basic Pediatric Differences Airway § Mouth and nose are smaller § More easily obstructed § Infants are nose breathers so secretions can be a major issue § Trachea is much shorter § ETT can be displaced easier § Narrow Airways § Easily obstructed § Diaphragm § Infants depend on diaphragm to breathe so abdominal distention can be problematic Oral explorers § Germs with feet
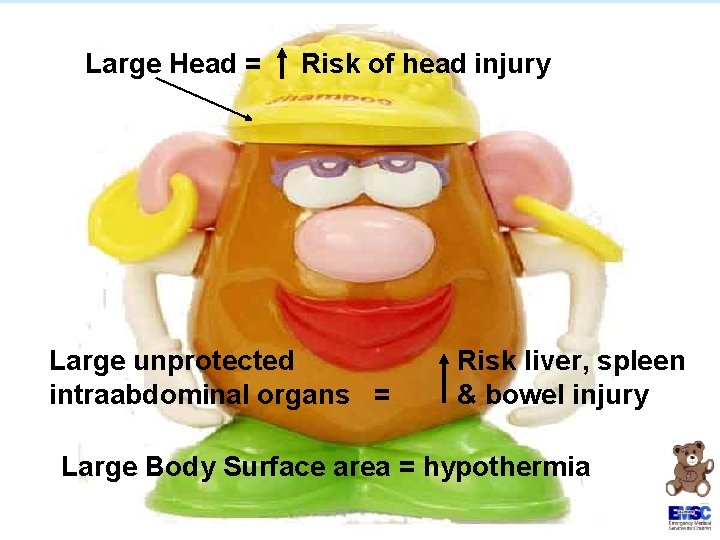
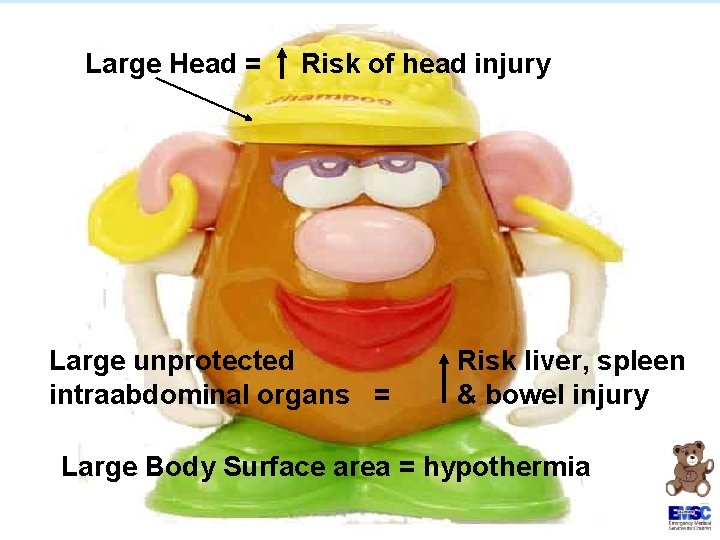
Large Head = Risk of head injury Large unprotected intraabdominal organs = Risk liver, spleen & bowel injury Large Body Surface area = hypothermia
Vulnerability of Children: Anatomic & Physiologic Issues § Children are particularly vulnerable to aerosolized biological or chemical agents and radiation § Some agents (e. g. , Sarin and Chlorine and radiation) are heavier than air and accumulate close to the ground—in breathing zone of children. § Children have faster ventilatory rates than adults § Inhale larger doses of the substance in the same period of time.
Vulnerability of Children: Anatomic & Physiologic Issues § Thinner skin and proportionately greater Body Surface Area (BSA) § Increased risk for hypothermia during field decontamination and treatment § Increased susceptibility to chemical agents § Vesicating agents (Nitrogen/Sulfur Mustard, Lewisite) § Nerve agents (Sarin, VX, Tabun, Soman) § Irritants and corrosives (chlorine, ammonia, phosgene) § Increased susceptibility to infections § Newborns § Children with chronic illnesses
Vulnerability of Children: Anatomic & Physiologic Issues A child’s condition can rapidly go from stable to life-threatening § Children have smaller circulating blood volumes than adults. § They have less blood and fluid reserves § § § More vulnerable to the effects of agents that produce vomiting and/or diarrhea -- can become dehydrated faster § Blood/fluid loss can lead to irreversible shock or death More sensitive to changes in body temperature Higher basal metabolic and cellular growth rates § Increased susceptibility to radiation, chemical agents § Increased leukemia and cancer risk to radiation exposed children age < 5 y/o
Vulnerability of Children : Developmental Considerations § Can’t anticipate, recognize or flee from dangerous situations § Fear of strangers – inability to cooperate or communicate with officials/providers § Family separation – unaccompanied minors § Sensitive to emotional state of parents § Children, Terrorism & Disasters Toolkit (AAP) at www. aap. org further identifies these vulnerabilities
Decon Considerations § Unlikely to be cooperative § Will be frightened of process and staff in protective gear § § § Hypothermia risk Slippery when wet How best to get them through the decon shower system § Laundry baskets § Car seats with padding removed. Strap them in. § Hospital plastic bassinettes § Stretcher or conveyor system § Strip them, including the diaper!
“Hello. Come with me. I’m going to take you thru this shower over here”
Decon Considerations § Warm Water § High Volume/Low Pressure § Keeping the family unit together as much as possible § How will they hear you? § Showering process will take more time with children § Identification issues

Lessons learned § Decontamination of kids is “not a fun time” § Decon brushes can be rough on skin § Blankets, booties and towels work well § Age specific decision tree § Use ink markers to write directly on skin to identify
EMS systems need plans to establish communication and restore unity of families
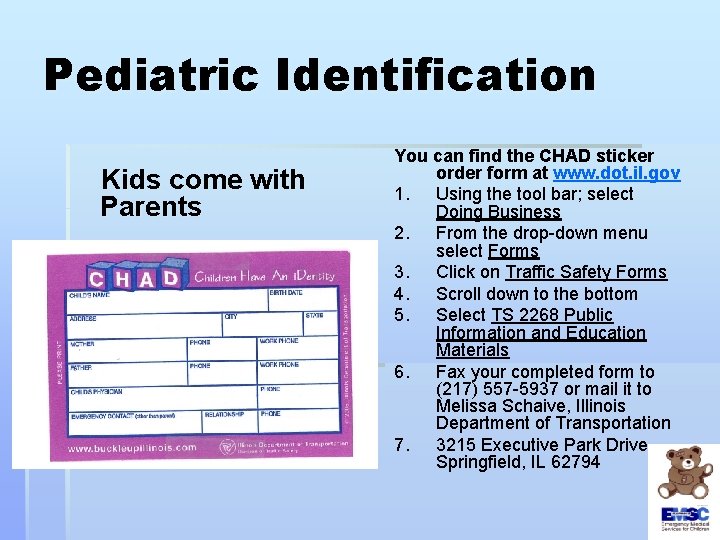
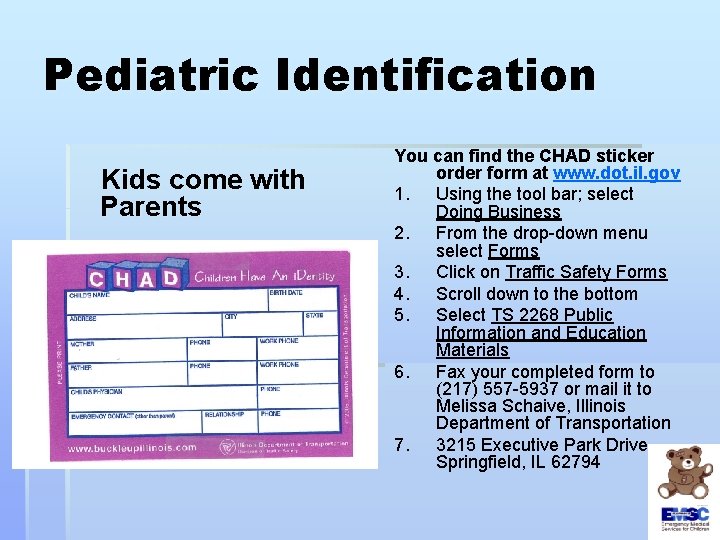
Pediatric Identification Kids come with Parents You can find the CHAD sticker order form at www. dot. il. gov 1. Using the tool bar; select Doing Business 2. From the drop-down menu select Forms 3. Click on Traffic Safety Forms 4. Scroll down to the bottom 5. Select TS 2268 Public Information and Education Materials 6. Fax your completed form to (217) 557 -5937 or mail it to Melissa Schaive, Illinois Department of Transportation 7. 3215 Executive Park Drive, Springfield, IL 62794

Pediatric Identification School Identification Medical History School identification
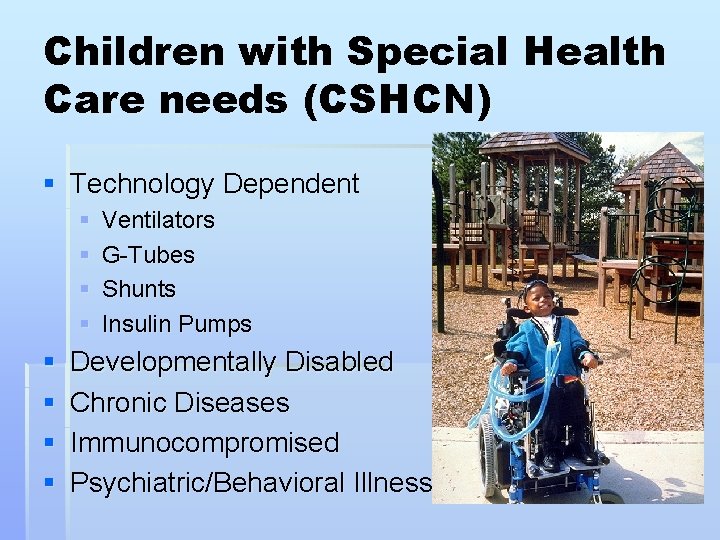
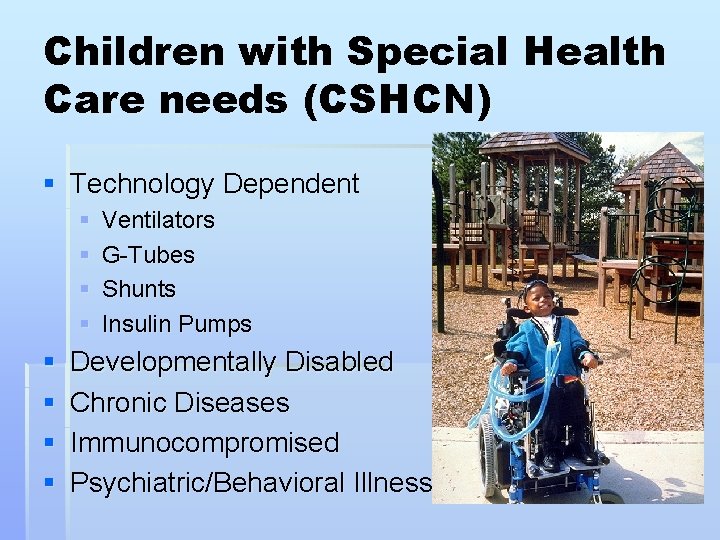
Children with Special Health Care needs (CSHCN) § Technology Dependent § § § § Ventilators G-Tubes Shunts Insulin Pumps Developmentally Disabled Chronic Diseases Immunocompromised Psychiatric/Behavioral Illnesses
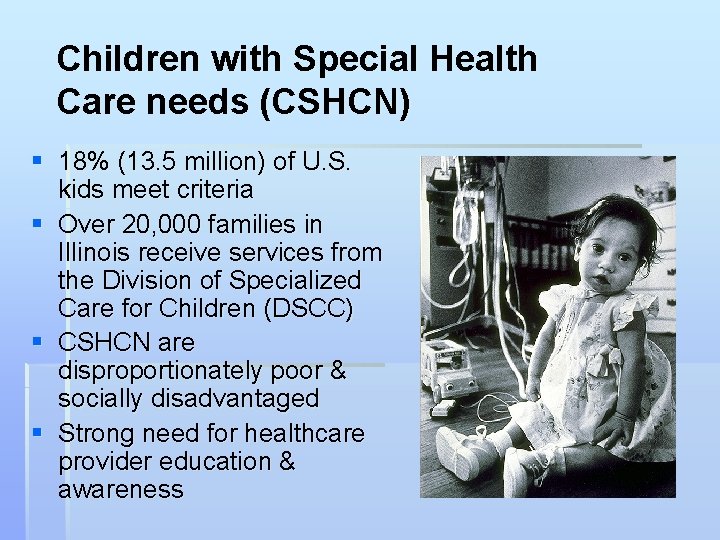
Children with Special Health Care needs (CSHCN) § 18% (13. 5 million) of U. S. kids meet criteria § Over 20, 000 families in Illinois receive services from the Division of Specialized Care for Children (DSCC) § CSHCN are disproportionately poor & socially disadvantaged § Strong need for healthcare provider education & awareness
Key Principles of Medical Care Conventional Medical Care The objective of conventional medical care is to… Do the greatest good for the individual patient. Disaster Medical Care The key principle of disaster medical care is to… Do the greatest good for the greatest number of patients. Briggs, S and Brinsfield, K (eds), Advanced Disaster Medical Response for Providers. Harvard Medical International, 2003.

Triage § “To Sort” § Look at medical needs and urgency of each individual patient § Triage in Daily Emergencies § Do the best for each individual § Disaster Triage § Do the greatest good for the greatest number § Make an impossible task manageable
Triage § Primary Triage § Triage that is performed at the scene or point of first contact with patients. § Secondary Triage § Triage that is performed after further intervention is provided. Usually done in a medical sector.

80% of casualties self or buddy transport to the closest hospital
Important Triage Concepts § Helps to prioritize patients in a systematic and organized fashion § Helps in resource allocation § Provides an objective framework for stressful and emotional decisions § MCI (mass casualty incident) triage is different than daily triage, in both field and ED settings
MCI (Mass Casualty Incident) Triage § In order for MCI triage to work effectively, all victims must have equal importance at the time of primary triage. § No patient group can receive special consideration other than that dictated by their physiologic state. This includes children! Adapted from the Dr. Lou Romig slide set available at www. jumpstarttriage. com/
Triage Categories § RED - Immediate/emergent § YELLOW - Urgent § GREEN - Nonurgent § BLACK- Dead/little to no hope of survival BLACK RED YELLOW GREEN

RED - Immediate § Severely injured but treatable injuries and able to be saved with relatively quick treatment and transport § Examples § Severe bleeding § Shock § Open chest or abdominal wounds § Emotionally out of control
Yellow - Delayed Injured and unable to walk on their own. Potentially serious injuries but stable enough to wait a short while for medical treatment § Examples § Burns with no respiratory distress § Spinal injuries § Moderate blood loss § Conscious with head injuries

Green – Non-Urgent § Minor injuries that can wait for a longer period of time for treatment. § May or may not be able to ambulate § Examples § Minor fractures § Minor bleeding § Minor lacerations

Black - Deceased § Dead or obviously dying. May have signs of life but injuries are incompatible with survival. § Handle based on local protocols § Examples § Cardiac arrest § Respiratory arrest with a pulse § Massive head injury § Can be psychologically difficult to tag a child as black

Review of START and Jump. START MCI Triage Tools Photo courtesy of Miami Dade Fire Rescue © Lou Romig MD, 2006. Used with permission.

START § Simple Triage and Rapid Transport § Joint development by the Fire & Marine Department and Hoag Hospital in New Port Beach, California § Gold standard for field adult MCI triage in U. S. and numerous other countries § Utilizes the standard four color triage categories § Used for primary triage § More information at www. start-triage. com
START vs Jump. START Triage § START triage § Used for the adult population (non-pediatric) § Jump. START § Used when the victim appears to be a child § Adult and pediatric patients do not share the same normal values for vital signs hence the need for 2 different tools § At approximately age 8, the pediatric patient is similar anatomically with the adult airway
ED Triage § Primary START or Jump. START triage does not have to be repeated at the point of entry to the ED when patients are transported by EMS § But, not all patients will come by EMS § Historically, we know patients will selftransport § Triage will be a valuable tool to perform quick sorting when dealing with multiple patients at one time
Understanding Field Triage § The ED staff need to understand the triage performed in the field § Helps with the flow of continuity of care § If ED staff understand START and Jump. START triage, they will understand how EMS made the decisions they did § START and Jump. START triage is a process that can be duplicated and performed in the ED as needed – not all patients come by EMS!!!
START Triage § This is just the 1 st process of triage § It is meant to quickly and initially separate those with life threatening injuries from the less seriously wounded/ill § Secondary triage will allow retriage of a patient § Patient may be placed into a different triage category § Decision will be based on physiological criteria § START triage attempts to remove the emotional reaction from the decision process
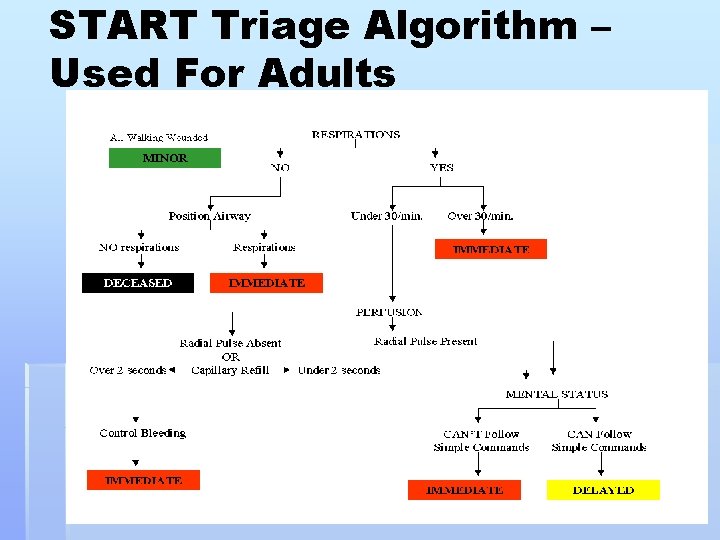
START Triage § Start at the top of the algorithm § As soon as patient has been categorized, stop assessment and move onto the next patient § Triage proceeds through a process üCan patient get up and walk to triage area? üEvaluate respirations (presence & rate) üEvaluate circulation (capillary refill) üEvaluate neurological status (obeys simple commands)
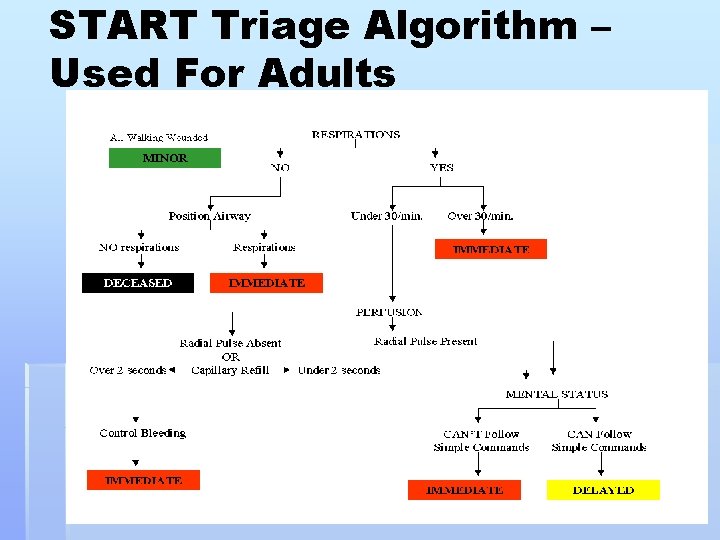
START Triage Algorithm – Used For Adults
Jump. START Triage § Pediatric patients do not fit the START triage criteria § The youngest of our patients don’t walk yet § Respiratory rates are different § Circulation assessment is altered § Ability to follow directions changes with age § START triage has been modified to be able to be applied to this unique population
Jump. START Triage § § § Tool for pediatric mass casualty triage Provides objective framework Based primarily on physiologic differences between children and adults § Designed for use in Disaster/MCI (mass casualty incident) events Adapted from the Dr. Lou Romig slide set available at www. jumpstarttriage. com
Differences Between START and Jump. START § If positioning airway does not restart breathing, a ventilatory trial is administered in Jump. START (pediatrics) § Capillary refill is used to assess perfusion in START (adult) while peripheral pulse is used in Jump. START (pediatrics) § The ability to follow command is used to assess mental status in START (adult) while the AVPU scale is used in Jump. START (pediatrics)
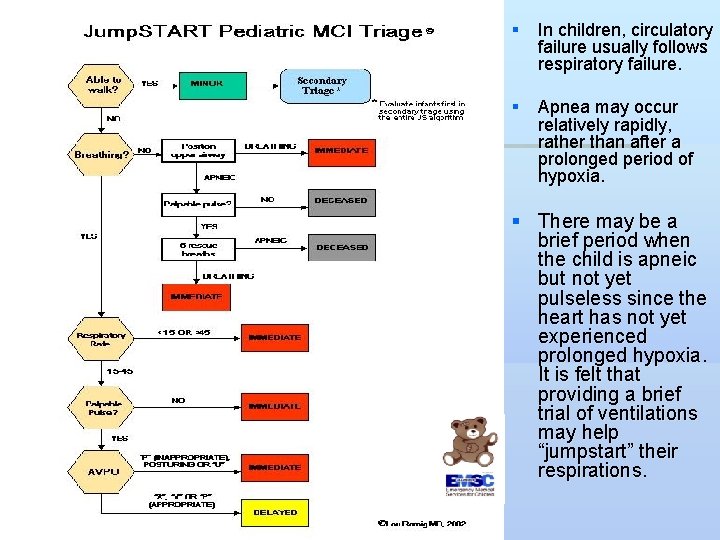
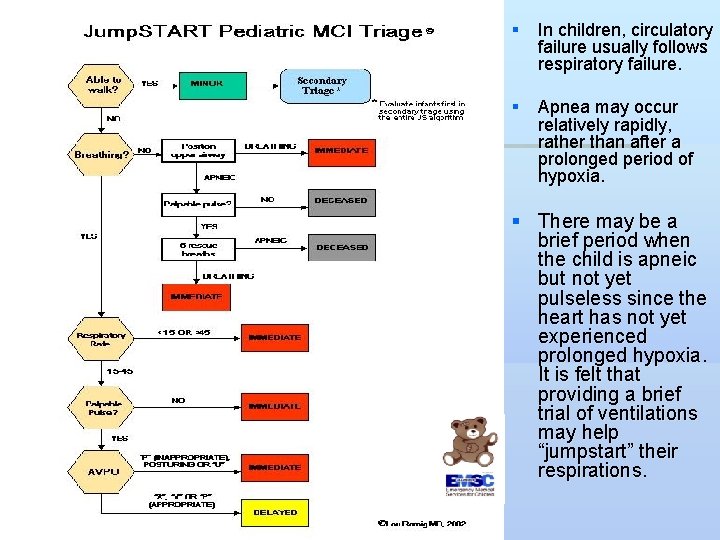
Jump. Start § In children, circulatory failure usually follows respiratory failure. § Apnea may occur relatively rapidly, rather than after a prolonged period of hypoxia. § There may be a brief period when the child is apneic but not yet pulseless since the heart has not yet experienced prolonged hypoxia. It is felt that providing a brief trial of ventilations may help “jumpstart” their respirations.
The Pediatric Patient § What age? What age defines peds?
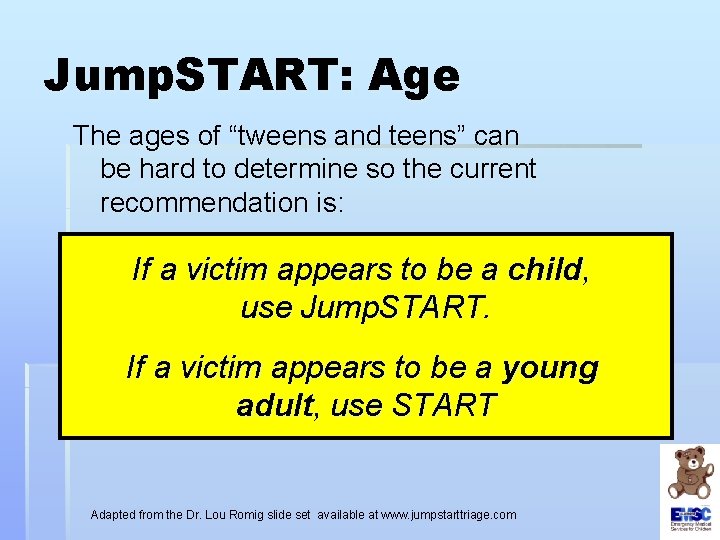
Jump. START: Age The ages of “tweens and teens” can be hard to determine so the current recommendation is: . to be a child, If a victim appears use Jump. START. If a victim appears to be a young adult, use START Adapted from the Dr. Lou Romig slide set available at www. jumpstarttriage. com

Triage – First Step § At a MCI there is panic and people are looking for someone to “take charge” § The initial sorting is to determine who can follow directions and walk § Helpful is to call out for patients to selfsegregate (“if you can walk go over to …”) sending patients to a close but alternate site (ie: the tree, the fence, the desk) § Patients will be triaged and sorted again at this next site § There is NO treatment at triage

Using Jump. START Triage Kids are good at following directions Anyone that can hear me, get up and walk if you can and come to… The big tree

START & Jump. START: Step 1 Patients who are able to walk are assumed to have stable, well compensated physiology, regardless of the nature of their injuries or illness. Tag these patients GREEN
Walking & Carried Patients § These patients need to be triaged immediately in the new area § Think, no-one has really looked at or evaluated these patients § This group of patients were able to walk to an alternate site as a process to “thin” the group of patients that are potentially more critically injured/ill § Start with the secondary triage process to determine the color category (GCS, RR, systolic B/P to get RTS)
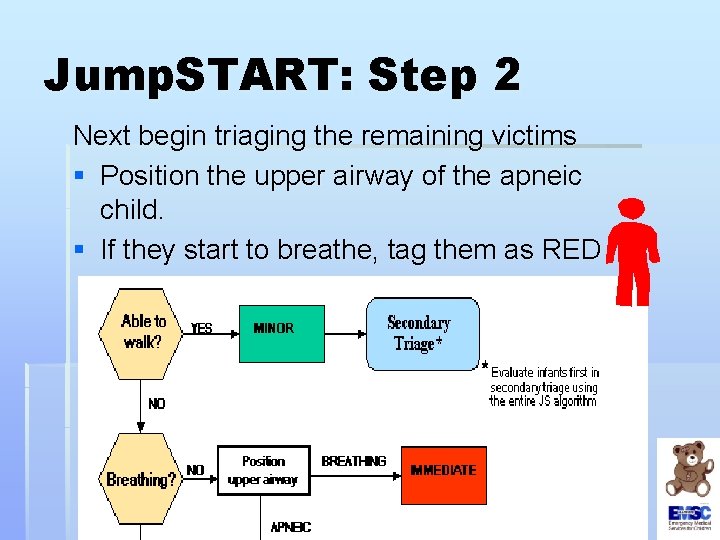
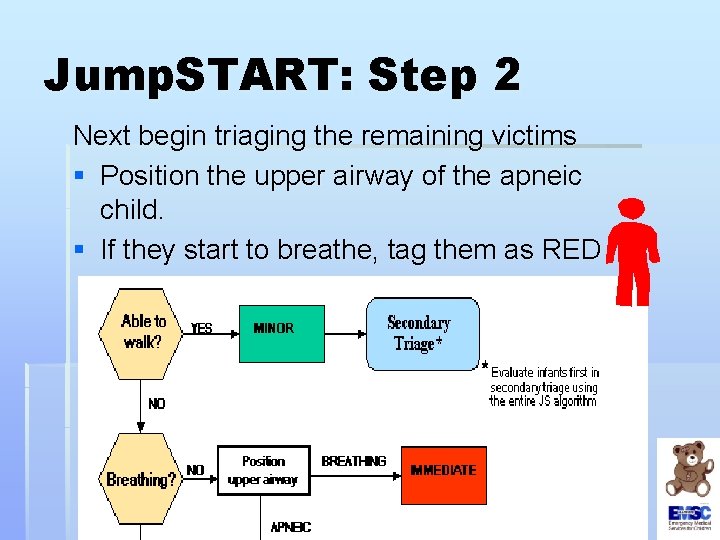
Jump. START: Step 2 Next begin triaging the remaining victims § Position the upper airway of the apneic child. § If they start to breathe, tag them as RED
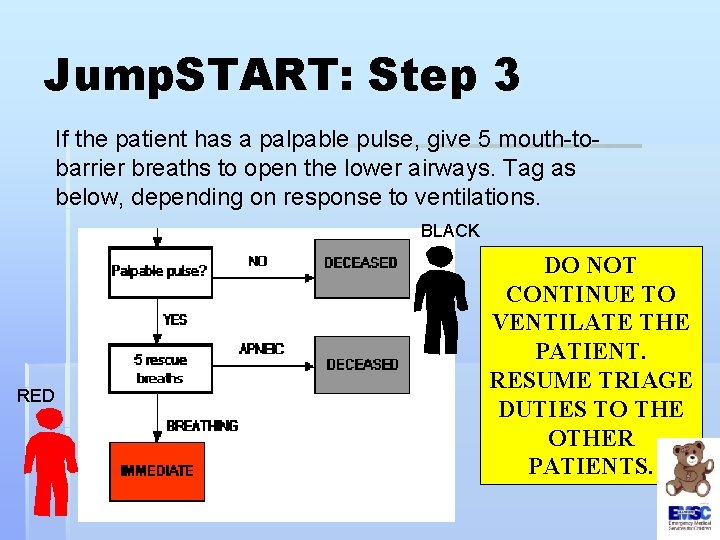
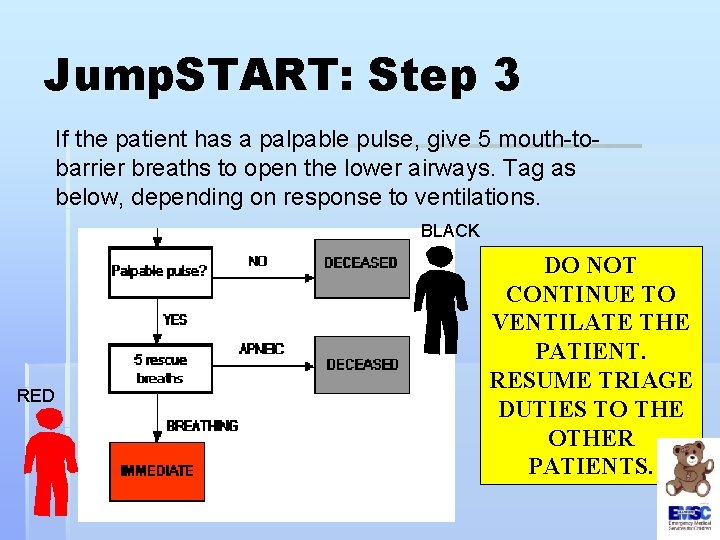
Jump. START: Step 3 If the patient has a palpable pulse, give 5 mouth-tobarrier breaths to open the lower airways. Tag as below, depending on response to ventilations. BLACK RED DO NOT CONTINUE TO VENTILATE THE PATIENT. RESUME TRIAGE DUTIES TO THE OTHER PATIENTS.
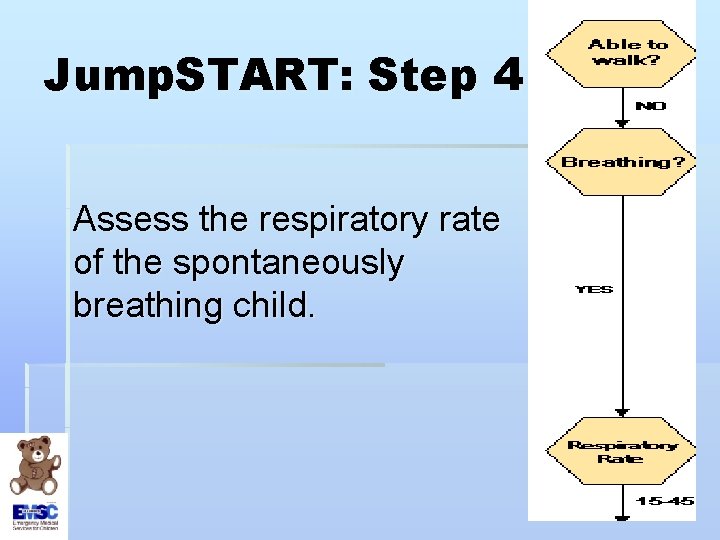
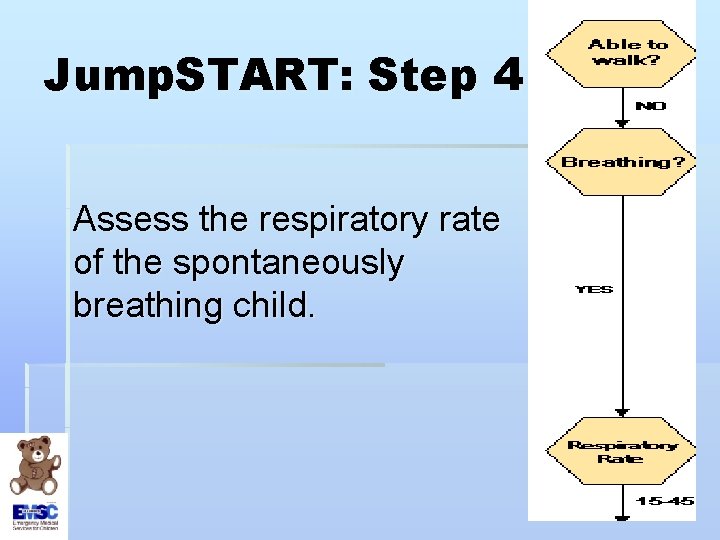
Jump. START: Step 4 Assess the respiratory rate of the spontaneously breathing child.

Jump. START: Step 4 § If respiratory rate is 15 -45 breaths/minute, move to perfusion assessment. § If respiratory rate is <15 or >45, tag the patient as RED
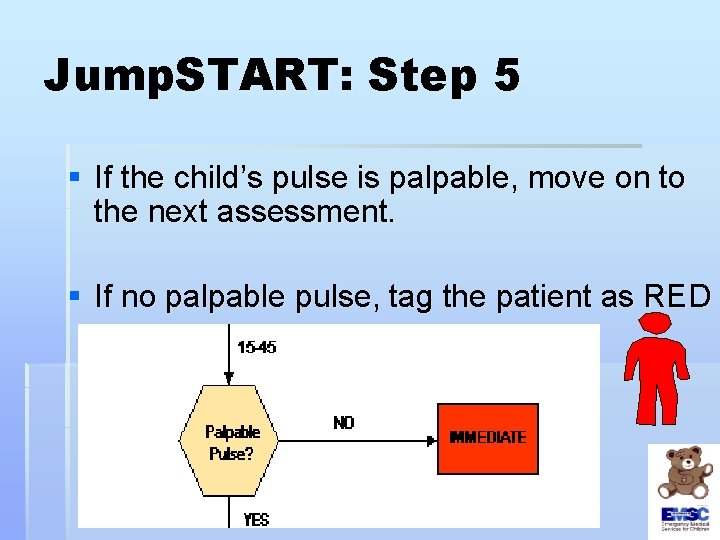
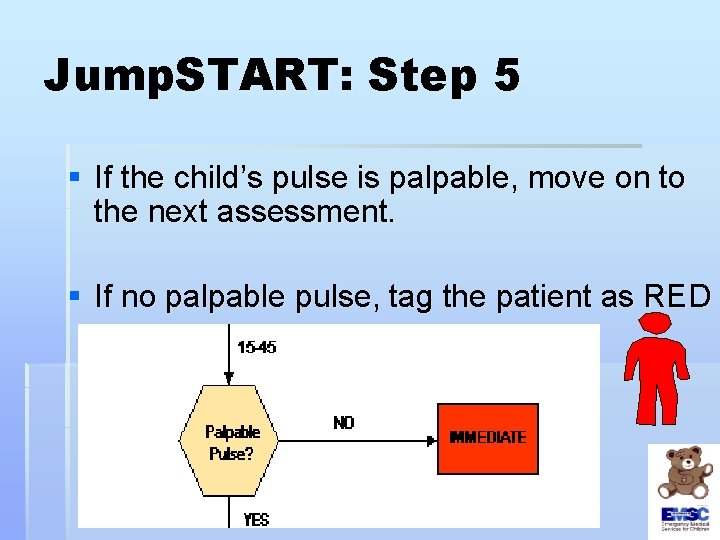
Jump. START: Step 5 § If the child’s pulse is palpable, move on to the next assessment. § If no palpable pulse, tag the patient as RED

Jump. START: Step 6 § If patient is alert, responds to voice or appropriately responds to pain/touch, tag as YELLOW § If patient is inappropriately responsive to pain, posturing, or unresponsive, tag as RED
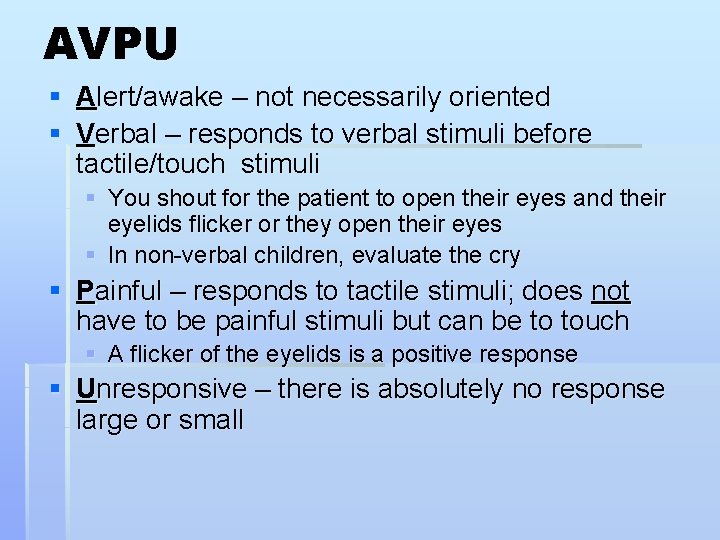
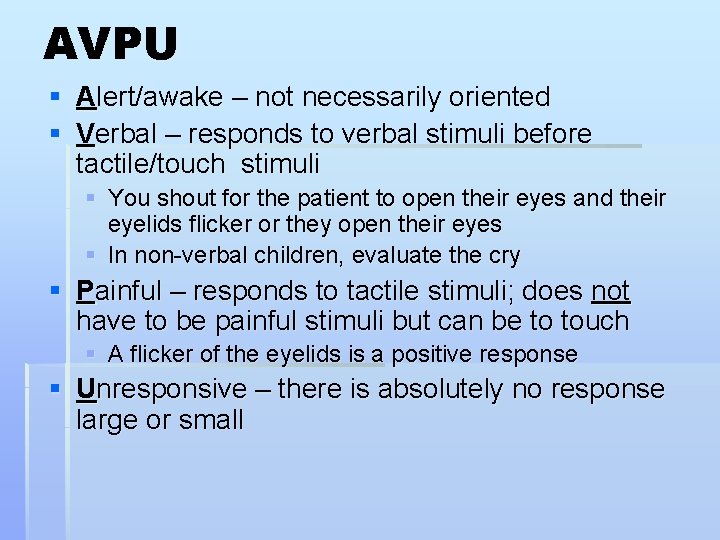
AVPU § Alert/awake – not necessarily oriented § Verbal – responds to verbal stimuli before tactile/touch stimuli § You shout for the patient to open their eyes and their eyelids flicker or they open their eyes § In non-verbal children, evaluate the cry § Painful – responds to tactile stimuli; does not have to be painful stimuli but can be to touch § A flicker of the eyelids is a positive response § Unresponsive – there is absolutely no response large or small
Children who classify as “non-ambulatory” § Infants who normally can’t walk yet § Children with developmental delay § Children with acute injuries which prevented them from walking before the incident occurred § Children with chronic disabilities CHILDREN MEETING THIS CRITERIA SHOULD BE EVALUATED USING THE Jump. START ALGORITHM BEGINNING WITH STEP 2 - BREATHING
Modification for Nonambulatory Children (and used for adults) All children carried to the GREEN area by other ambulatory victims must be the first assessed by medical personnel in that area. If patient meets any red criteria tag as RED If patient meets yellow criteria and has significant external signs of injury, tag as YELLOW If patient has no significant external signs of injury, tag as GREEN
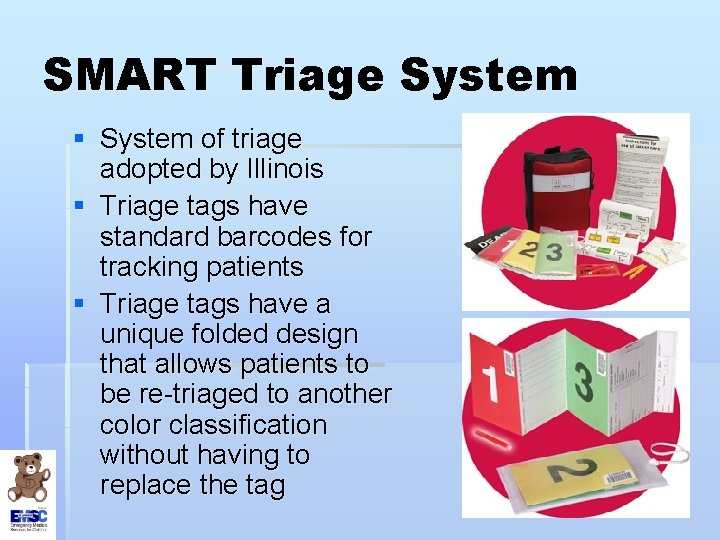
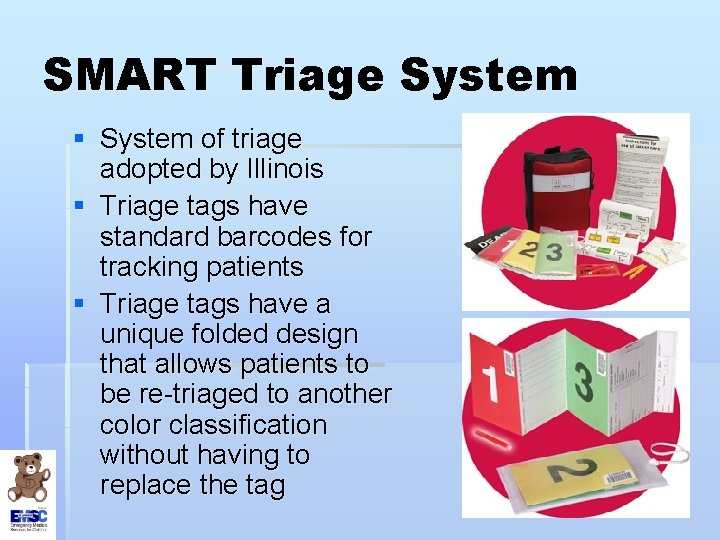
SMART Triage System § System of triage adopted by Illinois § Triage tags have standard barcodes for tracking patients § Triage tags have a unique folded design that allows patients to be re-triaged to another color classification without having to replace the tag
Folding Triage Tags § Tags will only show one color at a time § If the triage category changes, refold the card to reflect the new color status and replace into the plastic sleeve § Triage cards are dynamic – they can change if the patient changes § Space provided to write notes, record vital signs, GCS, tally RTS (revised trauma score), treatments
 Triage start
Triage start We're gonna jump jump jump in the river
We're gonna jump jump jump in the river Jump start in field traige assessment
Jump start in field traige assessment Jump triage
Jump triage Jump start triage
Jump start triage Escala rts de trauma
Escala rts de trauma Disaster triage
Disaster triage Jump triage
Jump triage Difference between conditional jump and unconditional jump
Difference between conditional jump and unconditional jump Pediatric start triage
Pediatric start triage Joan condell
Joan condell Disaster triage tag system
Disaster triage tag system Triage chart
Triage chart Triage basico
Triage basico Start triage
Start triage Rpm triage
Rpm triage Start adult triage
Start adult triage Jump start triaj
Jump start triaj Forevers gotta start tonight
Forevers gotta start tonight Er acuity scale
Er acuity scale Naru triage
Naru triage Chapter review motion part a vocabulary review answer key
Chapter review motion part a vocabulary review answer key Ap gov final review
Ap gov final review Narrative review vs systematic review
Narrative review vs systematic review Narrative review vs systematic review
Narrative review vs systematic review Narrative review vs systematic review
Narrative review vs systematic review Jump vs branch
Jump vs branch Chuckles can jump and run
Chuckles can jump and run High jump recording sheet
High jump recording sheet Jnz instruction in 8086
Jnz instruction in 8086 Long and triple jump workouts
Long and triple jump workouts What are the outputs of the sign-extend and the jump
What are the outputs of the sign-extend and the jump Example of past present and future tense
Example of past present and future tense Psystart
Psystart Ciampeds data
Ciampeds data Objectives of triage
Objectives of triage Triage forensik adalah
Triage forensik adalah Esi triage minsal
Esi triage minsal Ramp triage protocol
Ramp triage protocol Os triage
Os triage Oncology haematology helpline triage tool
Oncology haematology helpline triage tool Triage verb
Triage verb Education triage
Education triage Triage esi chart
Triage esi chart Atls triage scenarios answers 10th edition
Atls triage scenarios answers 10th edition Atls ample
Atls ample Tackykard
Tackykard Traffic director triage
Traffic director triage Global sorting triage
Global sorting triage Rapid triage
Rapid triage Oncology triage tool
Oncology triage tool Rit work order
Rit work order Dayton mmrs
Dayton mmrs Function of triage
Function of triage Peec triage
Peec triage Emergency care system framework
Emergency care system framework Ukons
Ukons Bug triage programs
Bug triage programs Triase bencana
Triase bencana A&ox1 shirt
A&ox1 shirt Triage van waddell
Triage van waddell Telephone techniques medical assistant
Telephone techniques medical assistant Soreu significato
Soreu significato Draw d wildland
Draw d wildland Triage sort
Triage sort Triage sort
Triage sort Dr wuyts tienen
Dr wuyts tienen Ob triage unm
Ob triage unm Uriticarial
Uriticarial Yow3
Yow3 Salvation army triage
Salvation army triage