Addressing the Demand for Pediatric Mental Health Services

- Slides: 54
Addressing the Demand for Pediatric Mental Health Services A Systems of Care Approach David Axelson, M. D. Chief of Psychiatry and Medical Director of Behavioral Health, Nationwide Children’s Hospital Clinical Professor of Psychiatry, The Ohio State University School of Medicine Chief of Child & Adolescent Psychiatry, The Ohio State University Wexner Medical Center ………………. . …………………………………………………………………. .
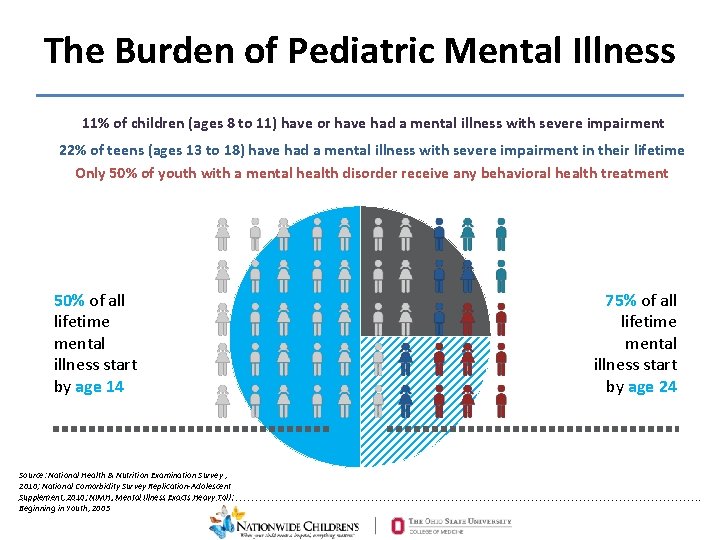
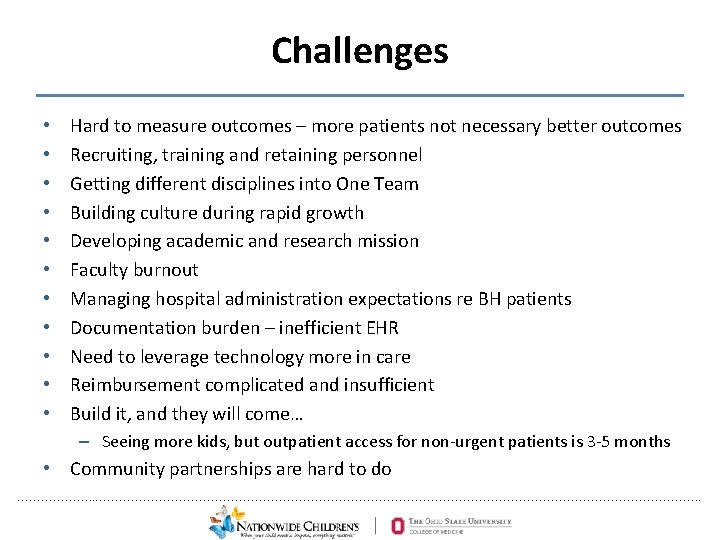
The Burden of Pediatric Mental Illness 11% of children (ages 8 to 11) have or have had a mental illness with severe impairment 22% of teens (ages 13 to 18) have had a mental illness with severe impairment in their lifetime Only 50% of youth with a mental health disorder receive any behavioral health treatment 50% of all lifetime mental illness start by age 14 75% of all lifetime mental illness start by age 24 Source: National Health & Nutrition Examination Survey , 2010; National Comorbidity Survey Replication-Adolescent Supplement, 2010; NIMH, Mental Illness Exacts Heavy Toll: ………………. . …………………………………………………………………. . Beginning in Youth, 2005
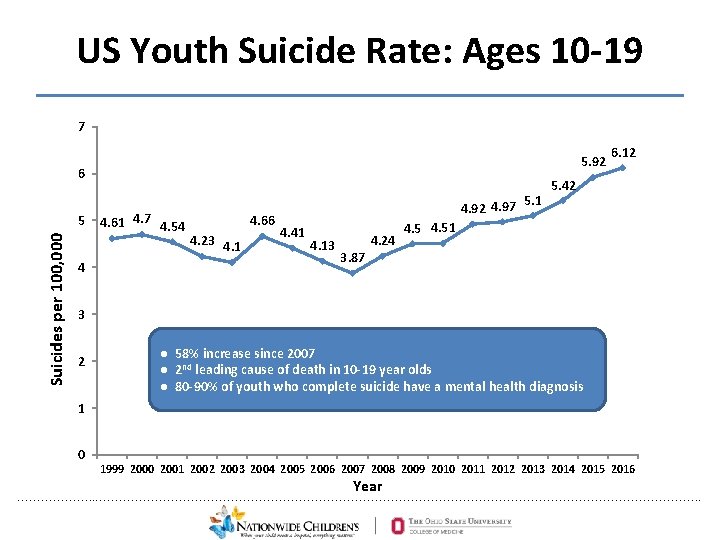
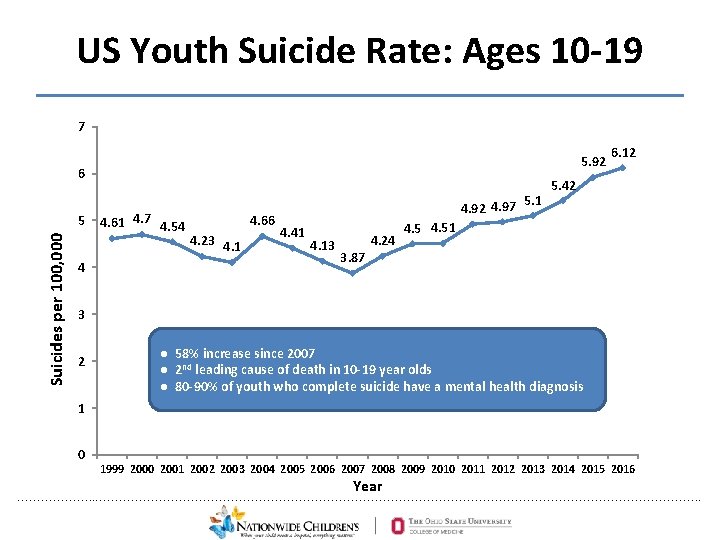
US Youth Suicide Rate: Ages 10 -19 7 5. 92 6 Suicides per 100, 000 5 4 4. 61 4. 7 4. 54 4. 66 4. 23 4. 1 5. 1 4. 92 4. 97 4. 41 4. 13 4. 24 6. 12 5. 42 4. 51 3. 87 3 2 ● 58% increase since 2007 ● 2 nd leading cause of death in 10 -19 year olds ● 80 -90% of youth who complete suicide have a mental health diagnosis 1 0 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 Year ………………. . …………………………………………………………………. .
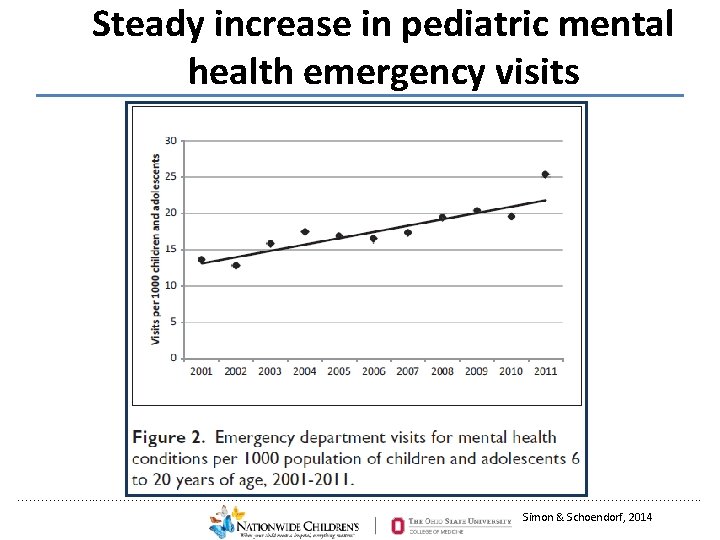
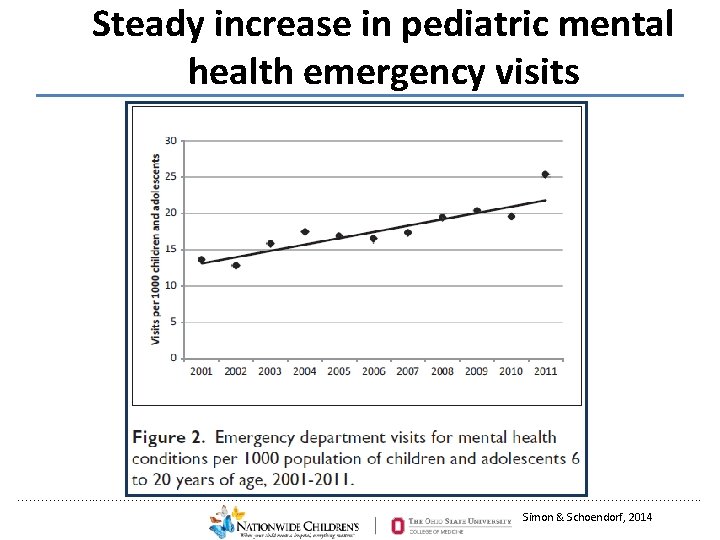
Steady increase in pediatric mental health emergency visits ………………. . …………………………………………………………………. . Simon & Schoendorf, 2014
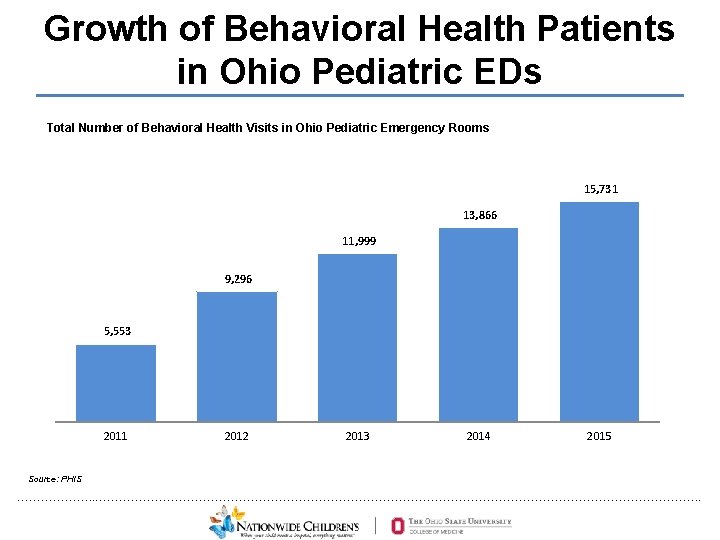
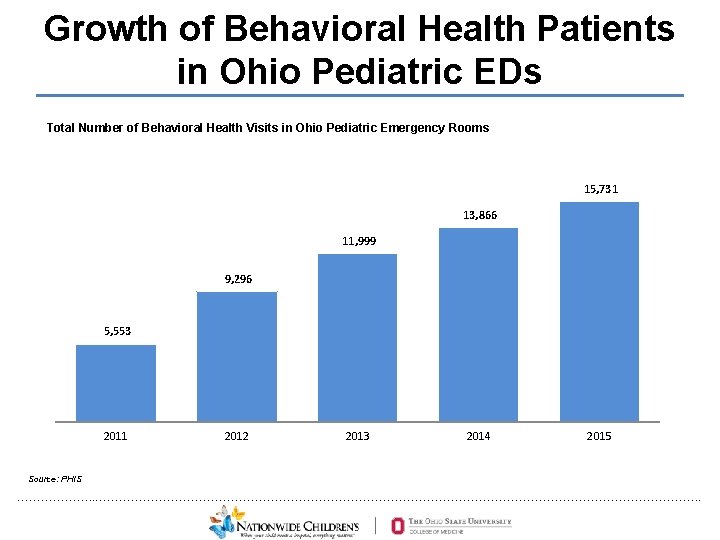
Growth of Behavioral Health Patients in Ohio Pediatric EDs Total Number of Behavioral Health Visits in Ohio Pediatric Emergency Rooms 15, 731 13, 866 11, 999 9, 296 5, 553 2011 2012 2013 2014 2015 Source: PHIS ………………. . …………………………………………………………………. .
How to meet the demand? Expand improve the system of care? • Population Health Approach • Systems of Care that will have the maximum impact on the overall health of youth given the available resources ………………. . …………………………………………………………………. .
Justification • It is the right thing to do – Public health need • Good economics (harder to quantify) – May improve efficiency of overall hospital operations (Psych patients clogging ED and Hospital Beds) – Accountable Care Organization / At-risk ………………. . …………………………………………………………………. .
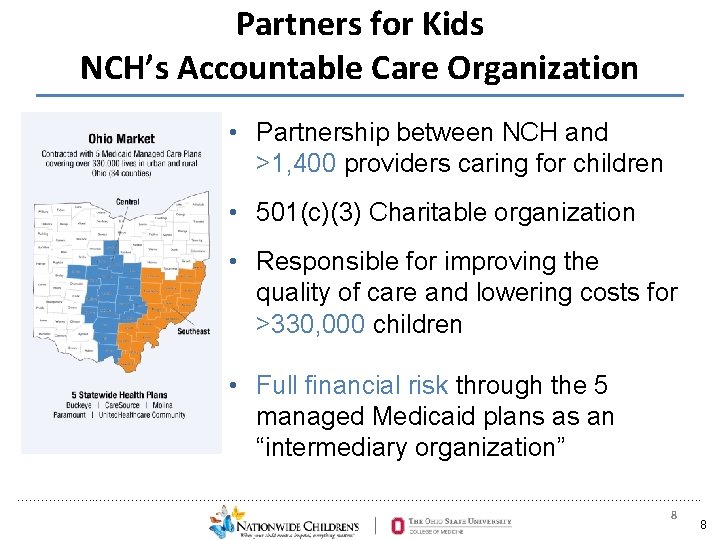
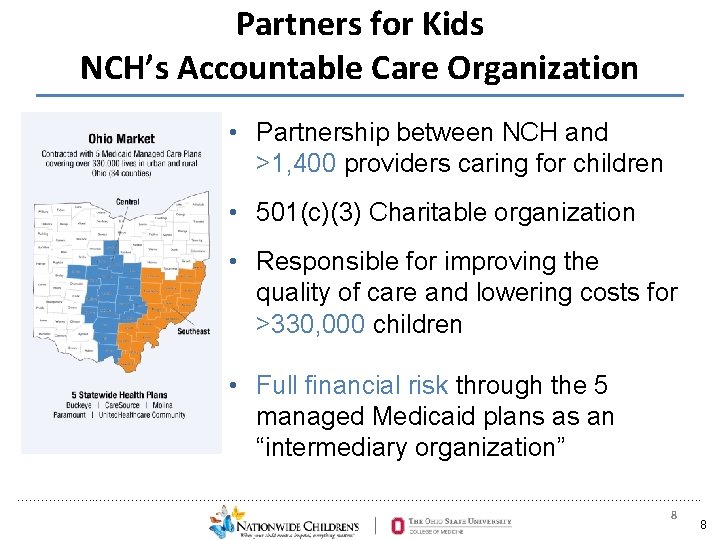
Partners for Kids NCH’s Accountable Care Organization • Partnership between NCH and >1, 400 providers caring for children • 501(c)(3) Charitable organization • Responsible for improving the quality of care and lowering costs for >330, 000 children • Full financial risk through the 5 managed Medicaid plans as an “intermediary organization” ………………. . …………………………………………………………………. . 8 8
How to expand pediatric behavioral health services? • What will give the most “bang for the buck”? • What will address the need at the “front door” (ED, Intake Department)? • ? Evidence base for effective system of pediatric mental health care ………………. . …………………………………………………………………. .
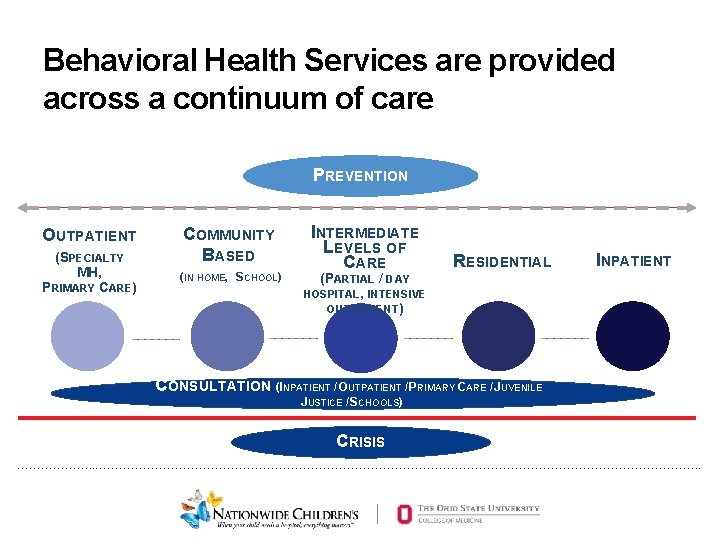
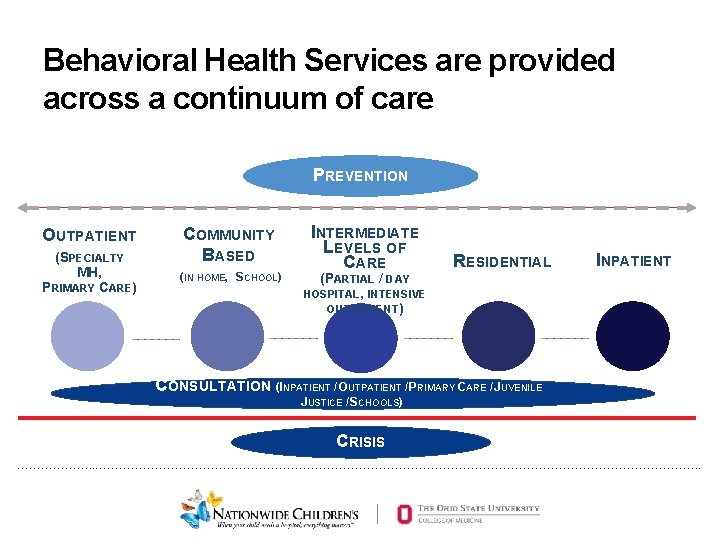
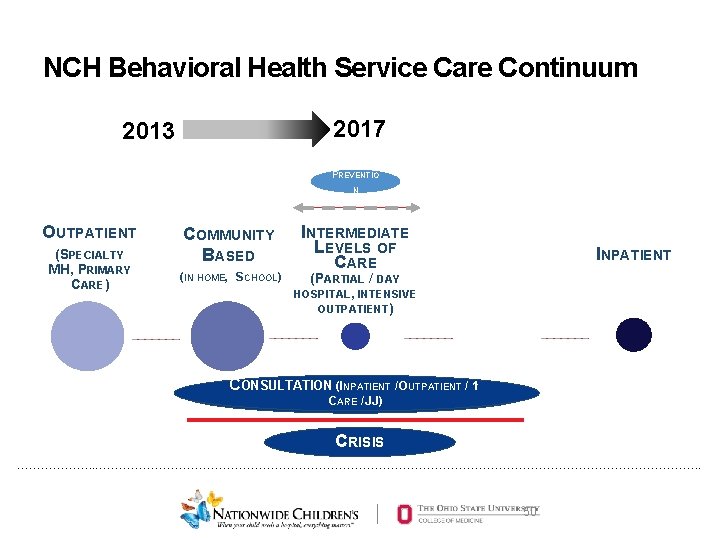
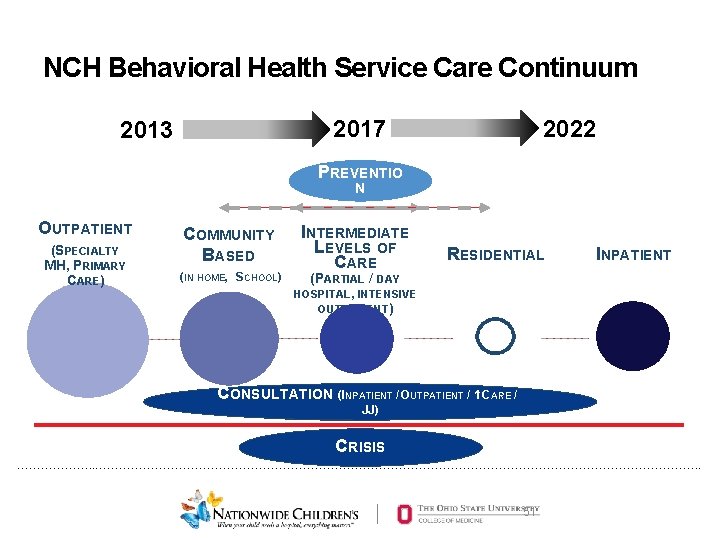
Behavioral Health Services are provided across a continuum of care PREVENTION OUTPATIENT (SPECIALTY MH, PRIMARY CARE) COMMUNITY BASED (IN HOME, SCHOOL) INTERMEDIATE LEVELS OF CARE (PARTIAL / DAY HOSPITAL, INTENSIVE OUTPATIENT) RESIDENTIAL INPATIENT CONSULTATION (INPATIENT / OUTPATIENT / PRIMARY CARE / JUVENILE JUSTICE / SCHOOLS) CRISIS ………………. . …………………………………………………………………. .
Hypothesis • Ensure that there are sufficient quality services at each point of the care continuum • Remove barriers to accessing appropriate services • Improve coordination among levels of care • Outcomes will improve ………………. . …………………………………………………………………. .
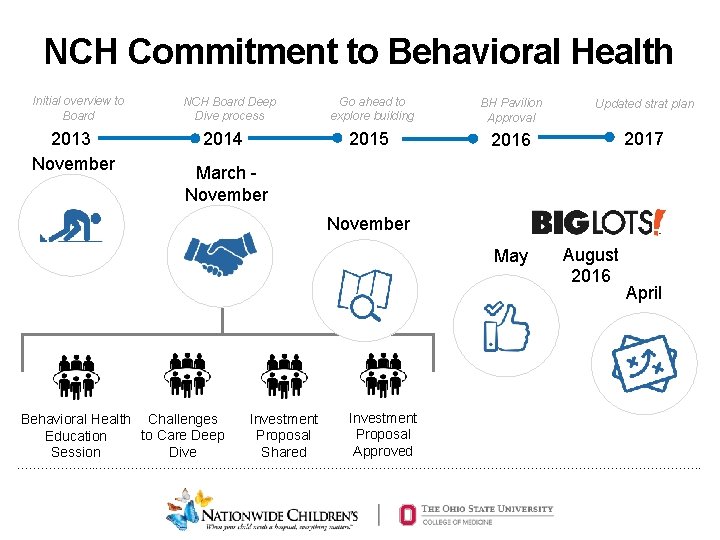
NCH Commitment to Behavioral Health Initial overview to NCH Board 2013 November ………………. . …………………………………………………………………. . 12
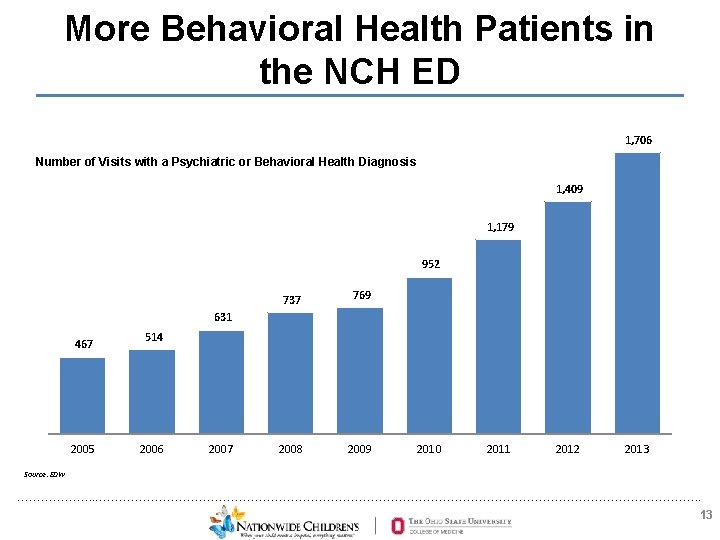
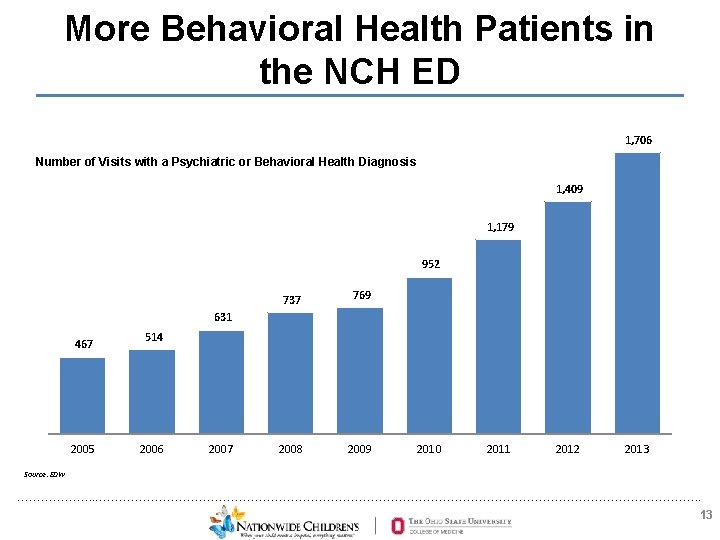
More Behavioral Health Patients in the NCH ED 1, 706 Number of Visits with a Psychiatric or Behavioral Health Diagnosis 1, 409 1, 179 952 737 769 2008 2009 631 467 2005 514 2006 2007 2010 2011 2012 2013 Source: EDW ………………. . …………………………………………………………………. . 13
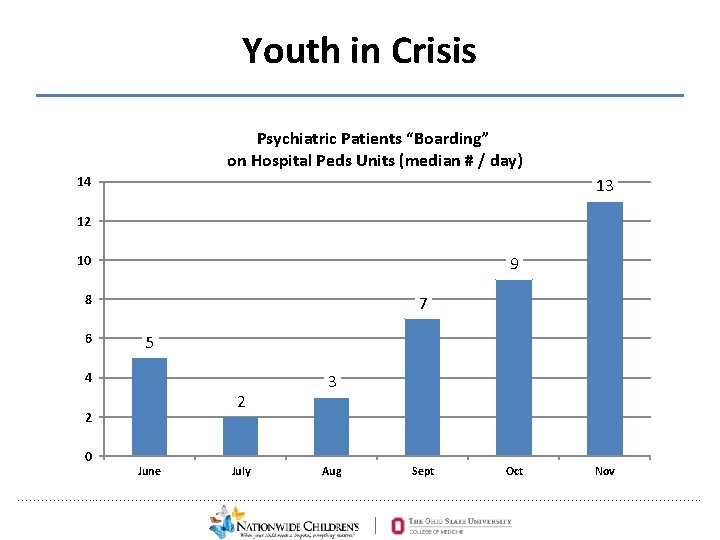
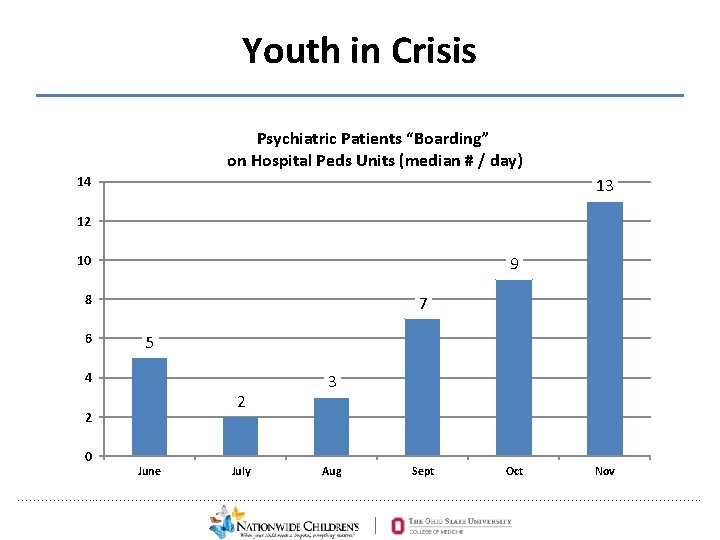
Youth in Crisis Psychiatric Patients “Boarding” on Hospital Peds Units (median # / day) 14 13 12 10 9 8 6 7 5 4 2 2 0 June July 3 Aug Sept Oct Nov ………………. . …………………………………………………………………. .
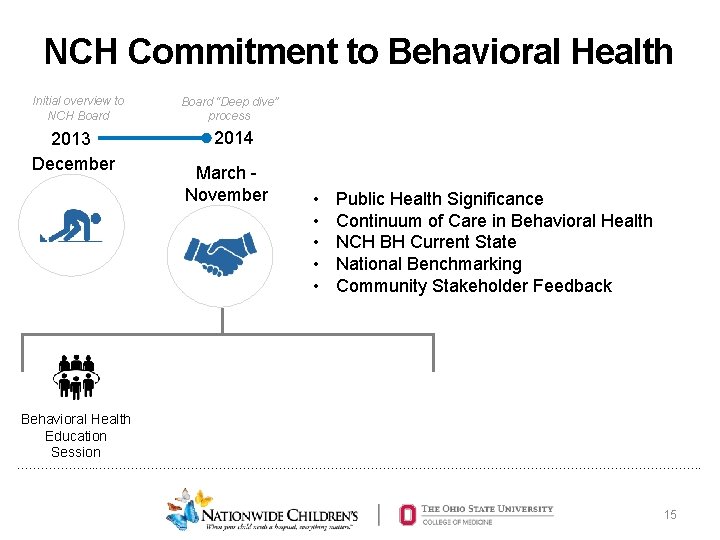
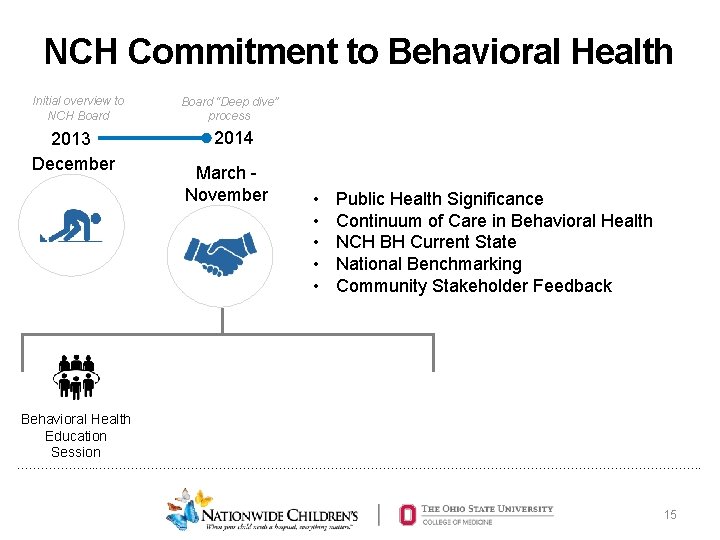
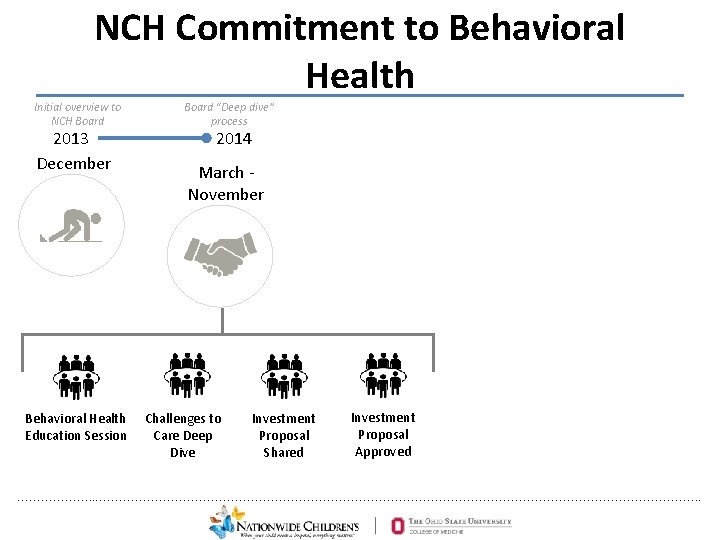
NCH Commitment to Behavioral Health Initial overview to NCH Board 2013 December Board “Deep dive” process 2014 March November • • • Public Health Significance Continuum of Care in Behavioral Health NCH BH Current State National Benchmarking Community Stakeholder Feedback Behavioral Health Education Session ………………. . …………………………………………………………………. . 15
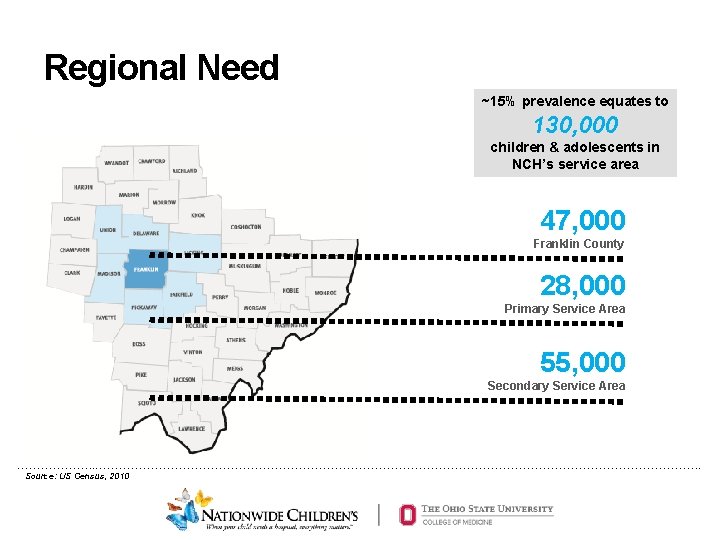
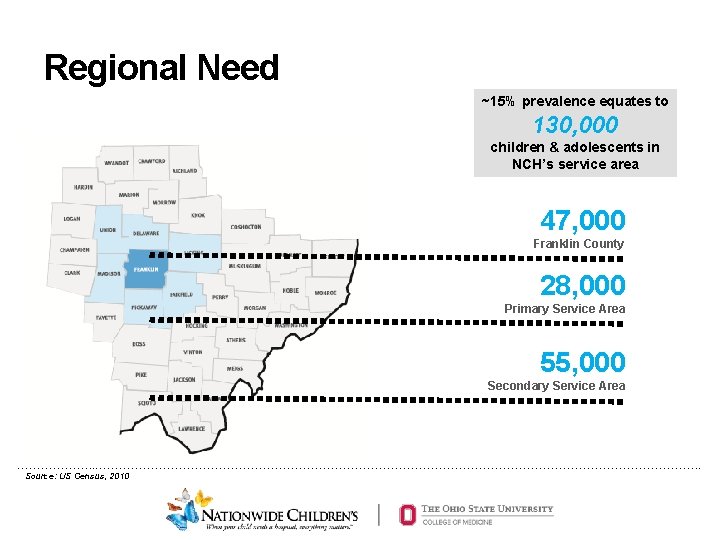
Regional Need ~15% prevalence equates to 130, 000 children & adolescents in NCH’s service area 47, 000 Franklin County 28, 000 Primary Service Area 55, 000 Secondary Service Area ………………. . …………………………………………………………………. . Source: US Census, 2010
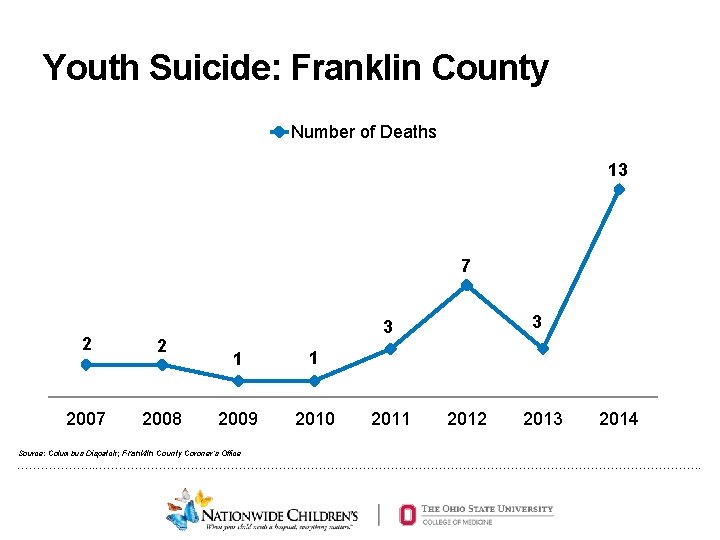
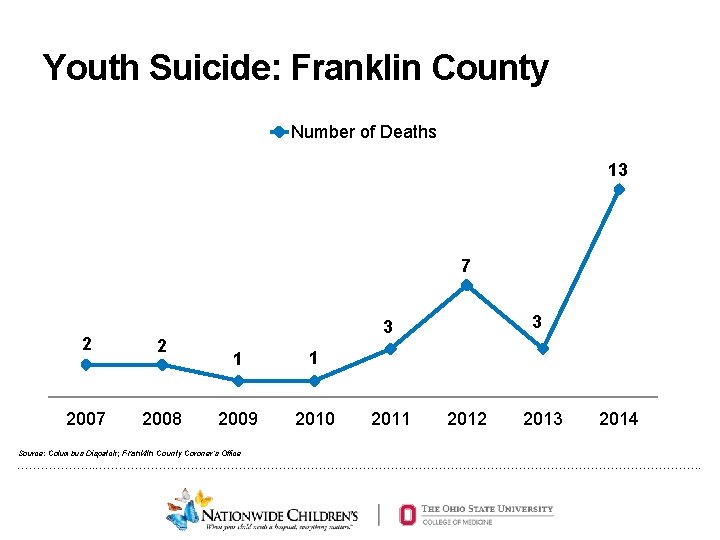
Youth Suicide: Franklin County Number of Deaths 13 7 2 2 2007 2008 3 3 1 1 2009 2010 Source: Columbus Dispatch; Franklin County Coroner’s Office 2011 2012 2013 2014 ………………. . …………………………………………………………………. .
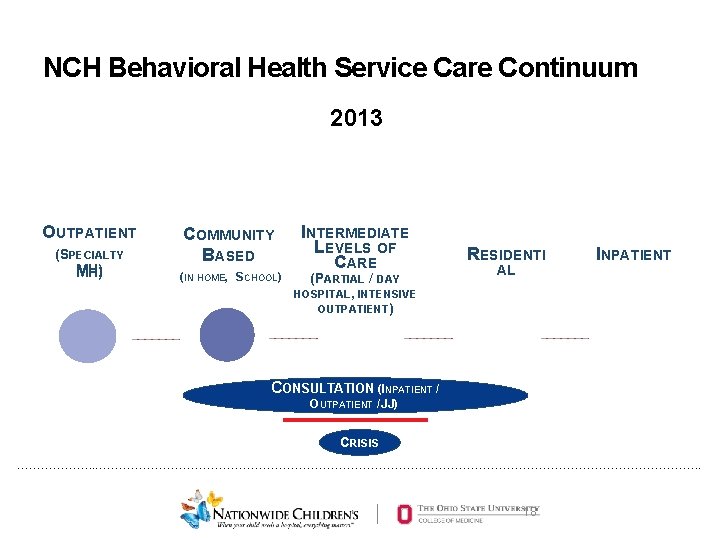
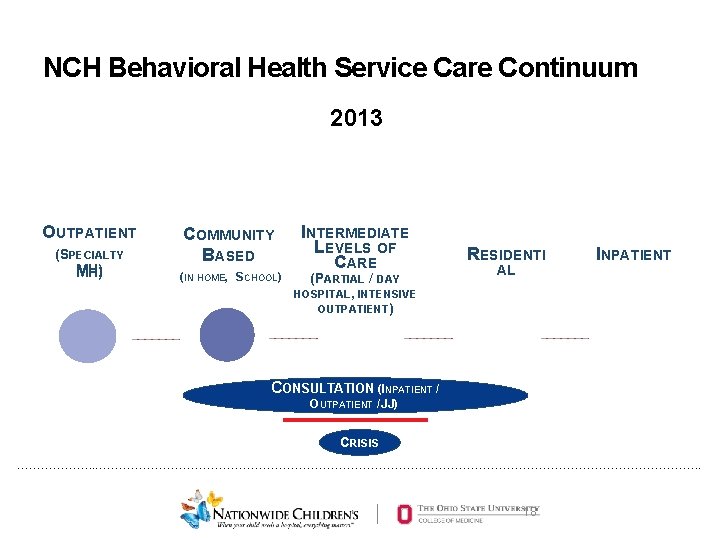
NCH Behavioral Health Service Care Continuum 2013 OUTPATIENT (S (SPECIALTY MH) COMMUNITY BASED (IN HOME, SCHOOL) INTERMEDIATE LEVELS OF CARE (PARTIAL / DAY HOSPITAL, INTENSIVE OUTPATIENT) RESIDENTI AL INPATIENT ONSULTATION (I(I NPATIENT CCONSULTATION NPATIENT // OUTPATIENT / JJ)) CRISIS ………………. . …………………………………………………………………. . 18
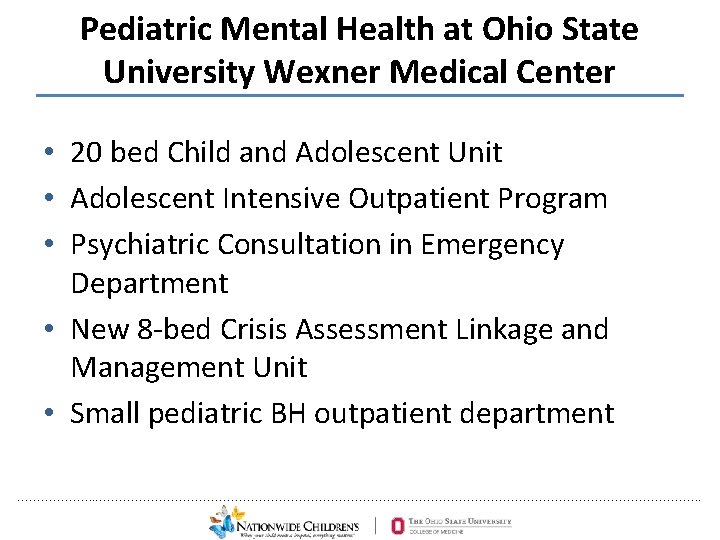
Pediatric Mental Health at Ohio State University Wexner Medical Center • 20 bed Child and Adolescent Unit • Adolescent Intensive Outpatient Program • Psychiatric Consultation in Emergency Department • New 8 -bed Crisis Assessment Linkage and Management Unit • Small pediatric BH outpatient department ………………. . …………………………………………………………………. .
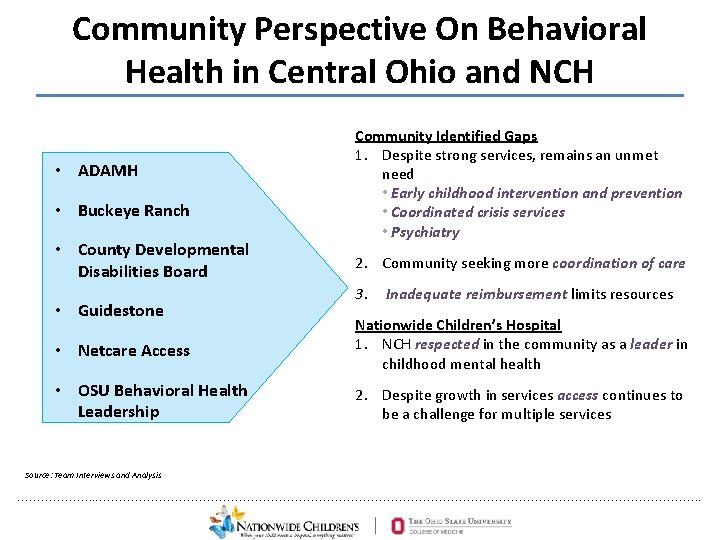
Community Perspective On Behavioral Health in Central Ohio and NCH • ADAMH • Buckeye Ranch • County Developmental Disabilities Board • Guidestone Community Identified Gaps 1. Despite strong services, remains an unmet need • Early childhood intervention and prevention • Coordinated crisis services • Psychiatry 2. Community seeking more coordination of care 3. Inadequate reimbursement limits resources • Netcare Access Nationwide Children’s Hospital 1. NCH respected in the community as a leader in childhood mental health • OSU Behavioral Health Leadership 2. Despite growth in services access continues to be a challenge for multiple services Source: Team Interviews and Analysis ………………. . …………………………………………………………………. .
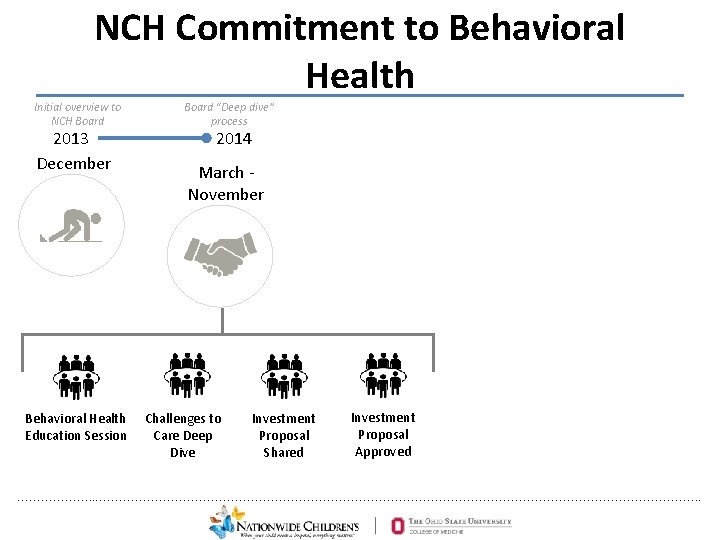
NCH Commitment to Behavioral Health Initial overview to NCH Board 2013 December Behavioral Health Education Session Board “Deep dive” process 2014 March - November Challenges to Care Deep Dive Investment Proposal Shared Investment Proposal Approved ………………. . …………………………………………………………………. .

Behavioral Health Strategic Plan Expanding clinical § Crisis Services access to pediatric § Inpatient Services mental health care § Youth Crisis Stabilization Unit Our Aspiration: To develop a national model for pediatric mental health care Developing targeted § Intermediate prevention efforts Levels of Care § Integrated & Multi-specialty Programs § Primary Care Integration § ↑ Existing consult, outpatient & community-based Leading a coordinated, services collaborative system § Recruitment / Retention Researching the causes § Infrastructure and §treatment behavioral Quality &of. Process Improvement: Operational & Clinical Services health Systems conditions ………………. . …………………………………………………………………………. 22
Emergency Crisis Services - 2013 • Netcare (County Supported Crisis Center and Crisis Hotline) • NCH Emergency Department – Social Work consulted for all psychiatric concerns – Sporadic phone support from Child Psychiatry • Admit as Psychiatric Boarder or to Youth Crisis Stabilization Unit ………………. . …………………………………………………………………. .
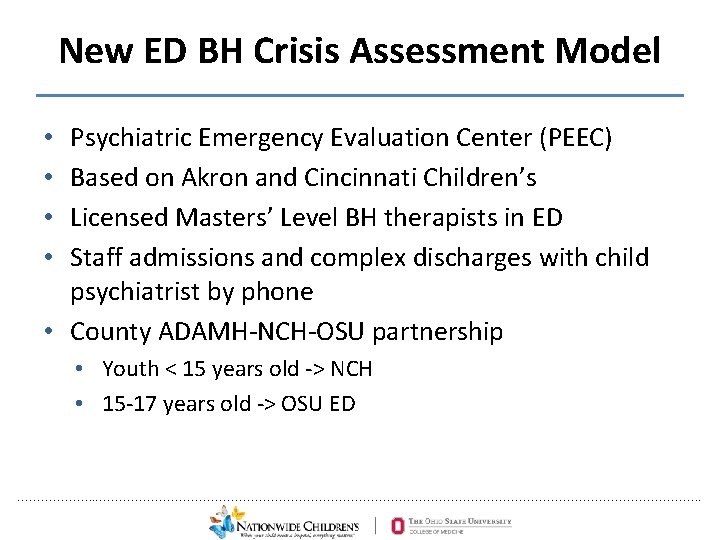
New ED BH Crisis Assessment Model Psychiatric Emergency Evaluation Center (PEEC) Based on Akron and Cincinnati Children’s Licensed Masters’ Level BH therapists in ED Staff admissions and complex discharges with child psychiatrist by phone • County ADAMH-NCH-OSU partnership • • • Youth < 15 years old -> NCH • 15 -17 years old -> OSU ED ………………. . …………………………………………………………………. .
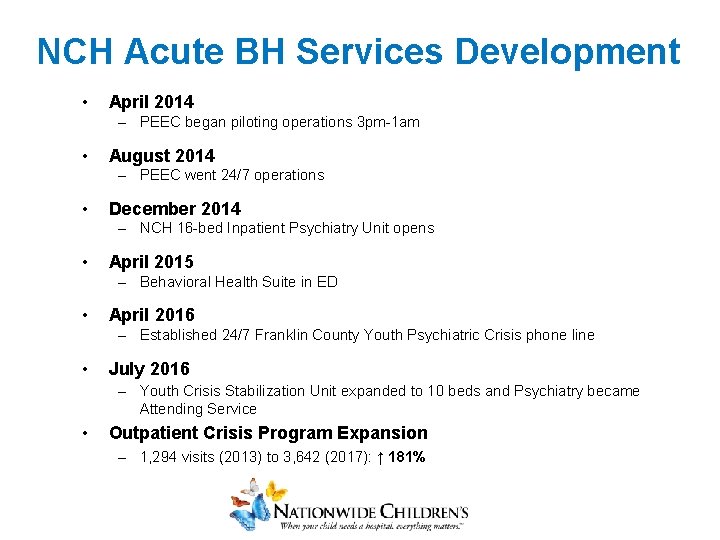
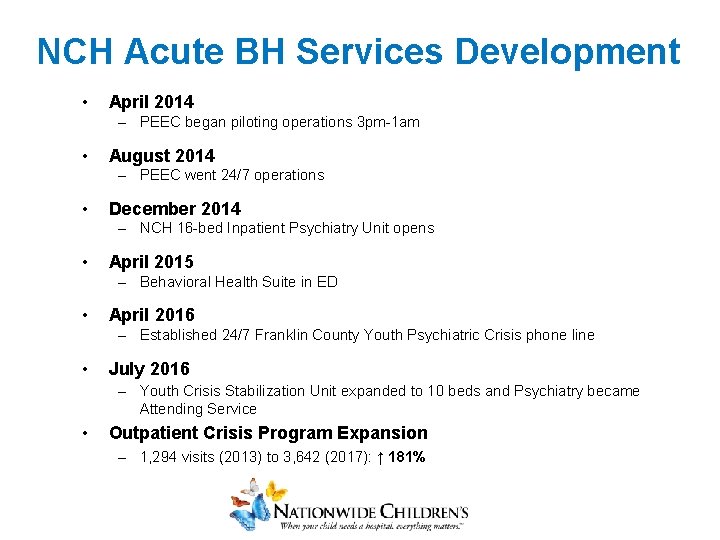
NCH Acute BH Services Development • April 2014 – PEEC began piloting operations 3 pm-1 am • August 2014 – PEEC went 24/7 operations • December 2014 – NCH 16 -bed Inpatient Psychiatry Unit opens • April 2015 – Behavioral Health Suite in ED • April 2016 – Established 24/7 Franklin County Youth Psychiatric Crisis phone line • July 2016 – Youth Crisis Stabilization Unit expanded to 10 beds and Psychiatry became Attending Service • Outpatient Crisis Program Expansion – 1, 294 visits (2013) to 3, 642 (2017): ↑ 181%
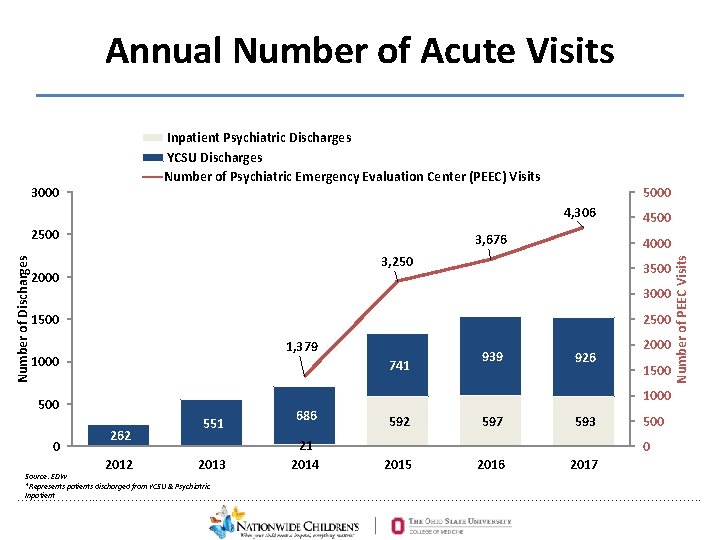
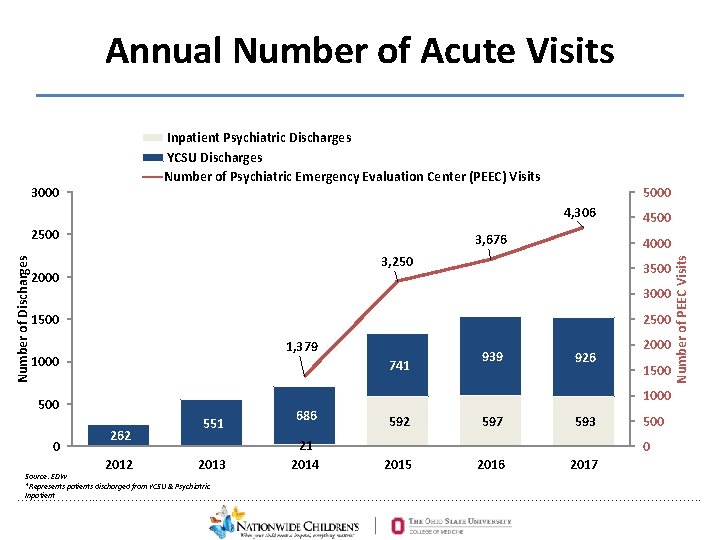
Annual Number of Acute Visits Inpatient Psychiatric Discharges YCSU Discharges Number of Psychiatric Emergency Evaluation Center (PEEC) Visits 5000 4, 306 Number of Discharges 2500 3, 676 4000 3, 250 2000 3500 3000 1500 2500 1, 379 1000 741 939 926 2000 1500 1000 500 0 4500 Number of PEEC Visits 3000 262 2012 551 2013 686 21 2014 592 597 593 500 0 2015 2016 2017 Source: EDW *Represents patients discharged from YCSU & Psychiatric Inpatient ………………. . …………………………………………………………………. .
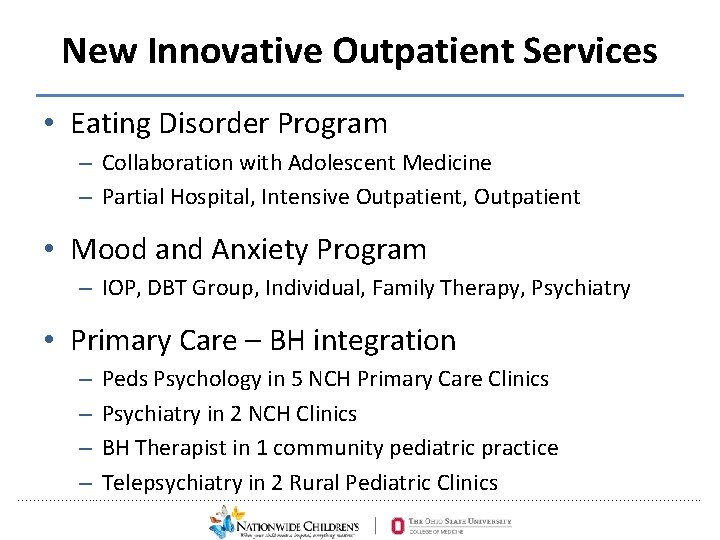
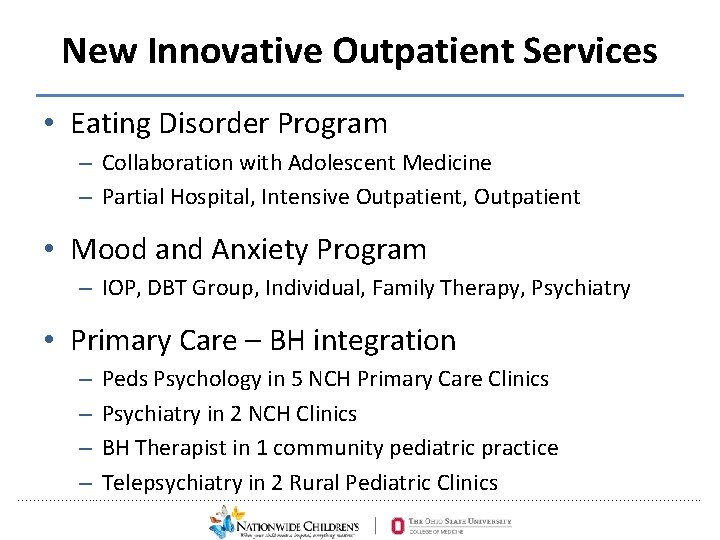
New Innovative Outpatient Services • Eating Disorder Program – Collaboration with Adolescent Medicine – Partial Hospital, Intensive Outpatient, Outpatient • Mood and Anxiety Program – IOP, DBT Group, Individual, Family Therapy, Psychiatry • Primary Care – BH integration – Peds Psychology in 5 NCH Primary Care Clinics – Psychiatry in 2 NCH Clinics – BH Therapist in 1 community pediatric practice – Telepsychiatry in 2 Rural Pediatric Clinics ………………. . …………………………………………………………………. .
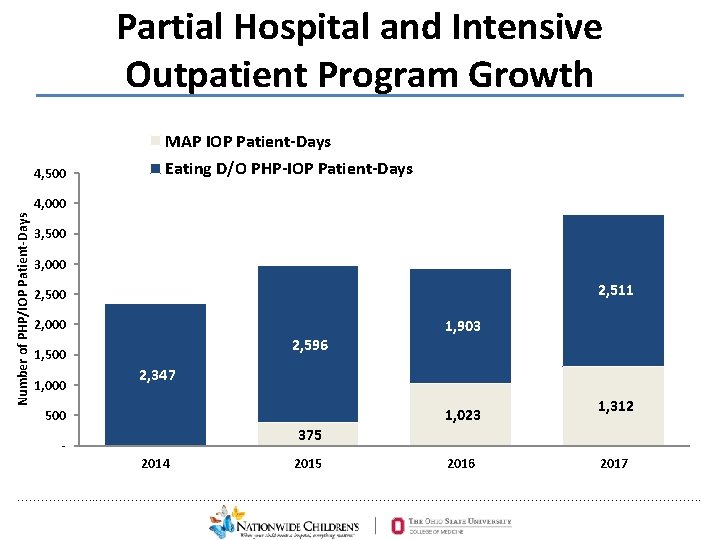
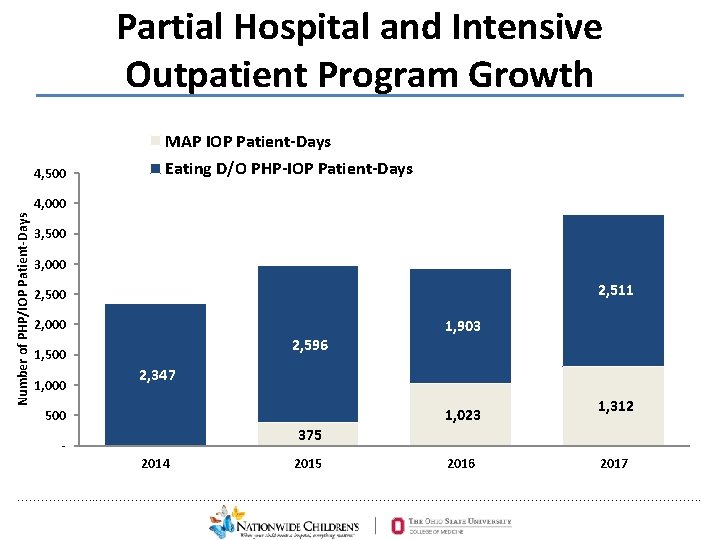
Partial Hospital and Intensive Outpatient Program Growth MAP IOP Patient-Days 4, 500 Eating D/O PHP-IOP Patient-Days Number of PHP/IOP Patient-Days 4, 000 3, 500 3, 000 2, 511 2, 500 2, 000 2, 596 1, 500 1, 000 1, 903 2, 347 1, 023 500 1, 312 375 2014 2015 2016 2017 ………………. . …………………………………………………………………. .
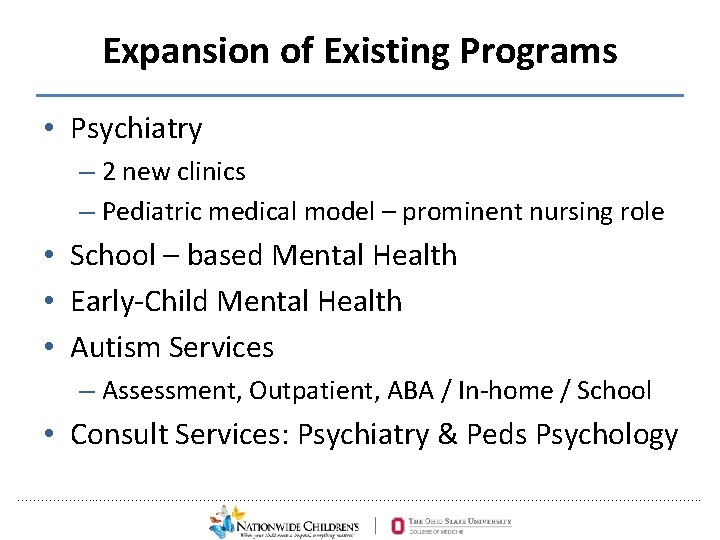
Expansion of Existing Programs • Psychiatry – 2 new clinics – Pediatric medical model – prominent nursing role • School – based Mental Health • Early-Child Mental Health • Autism Services – Assessment, Outpatient, ABA / In-home / School • Consult Services: Psychiatry & Peds Psychology ………………. . …………………………………………………………………. .
Evidence-based Psychosocial Treatments • All community behavioral health outpatient therapists trained in CBT • Added 2 Intensive Home-Based Treatment programs ………………. . …………………………………………………………………. .
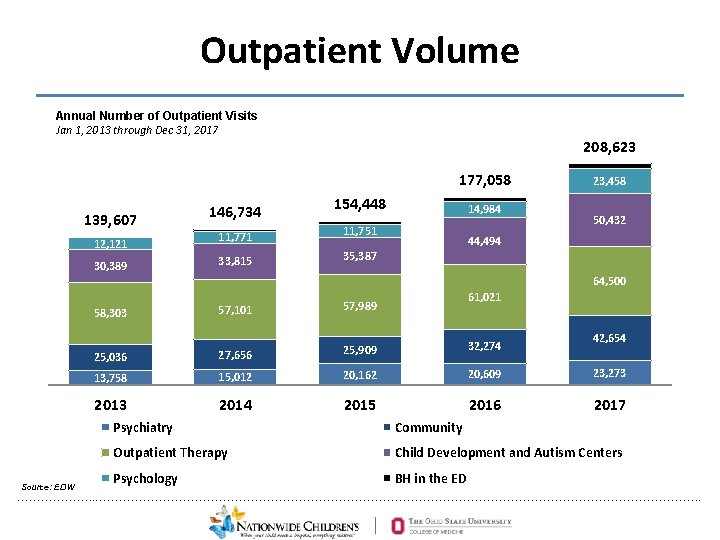
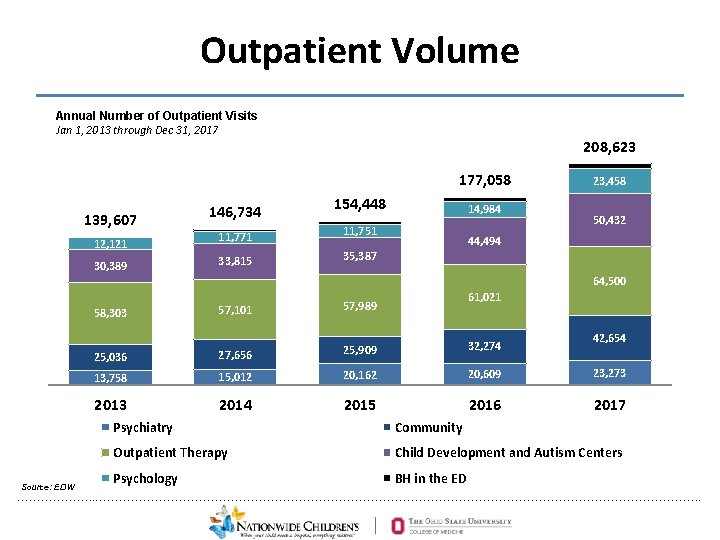
Outpatient Volume Annual Number of Outpatient Visits Jan 1, 2013 through Dec 31, 2017 208, 623 177, 058 139, 607 12, 121 30, 389 146, 734 11, 771 33, 815 154, 448 14, 984 11, 751 23, 458 50, 432 44, 494 35, 387 64, 500 57, 989 25, 036 27, 656 25, 909 32, 274 13, 758 15, 012 20, 162 20, 609 23, 273 2014 2015 2016 2017 58, 303 Source: EDW 61, 021 57, 101 42, 654 Psychiatry Community Outpatient Therapy Child Development and Autism Centers Psychology BH in the ED ………………. . …………………………………………………………………. .
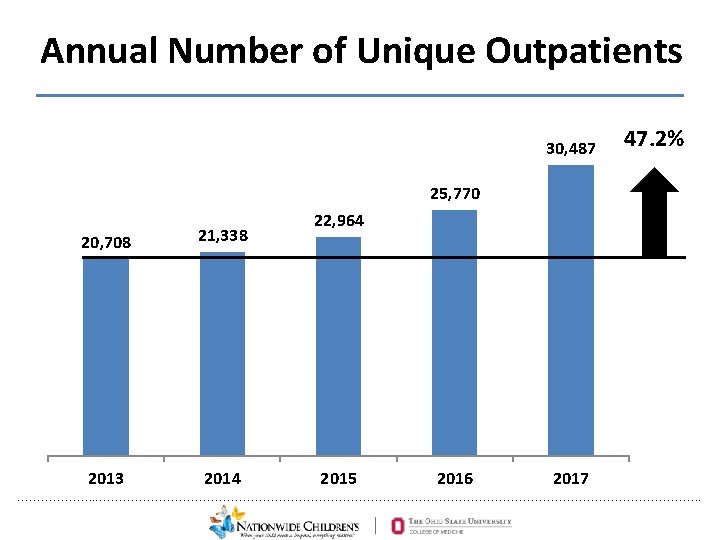
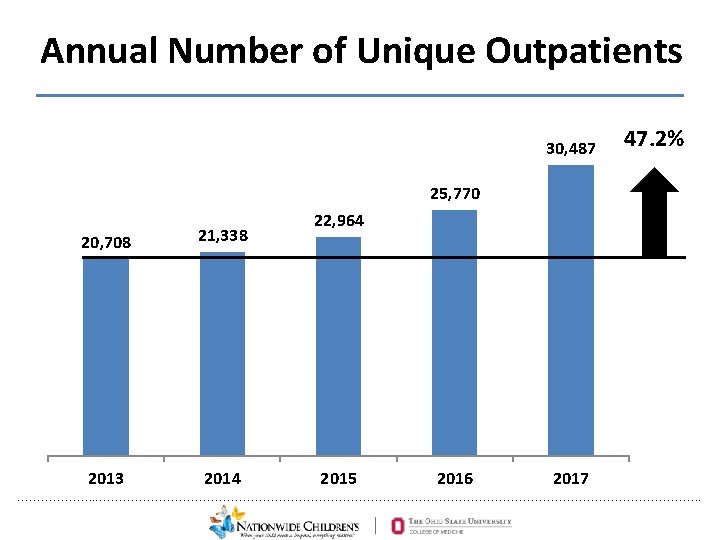
Annual Number of Unique Outpatients 30, 487 47. 2% 25, 770 20, 708 21, 338 2013 2014 22, 964 2015 2016 2017 ………………. . …………………………………………………………………. .
Prevention Expanding clinical access to pediatric mental health care § Center for Suicide Prevention and Research Developing targeted prevention efforts § PAX Good Behavior Game Leading a coordinated, collaborative system § Preschool Consultation / Early-Child Mental Health Researching the causes and treatment of behavioral health conditions ………………. . …………………………………………………………………. . 33
How and why does NCH sustain suicide prevention? • Consistent with our values & mission • Reduced risk of suicide clusters and contagion • Reduced individual, family and community suffering • Decreased costs • For every 1, 000 children, 5 fewer suicide attempts • For every $1 spent, estimated $4. 50 ROI Garraza et al. , 2016; Walrath et al. , 2015 • Reduction in ED visits • Strong interest from donors & community leaders ………………. . …………………………………………………………………. .
Signs of Suicide (SOS) • Evidence-based universal suicide prevention • Three RCTs show 40 -64% reduction in self-reported suicide attempts (Aseltine & De. Martino, 2004; Aseltine, 2007; Schilling et al. , 2016) at 3 -month follow-up • Greater pre-post knowledge and attitudes about depression • Increase in help-seeking behaviors not significant (Aseltine, 2007) ………………. . …………………………………………………………………. .
Signs of Suicide (SOS) • Train all adults to identify depression symptoms and warning signs for suicide • Teach action steps to students and adults when encountering suicidal behavior • Increase student awareness and help-seeking • Acronym (ACT) • Acknowledge • Care - show that you care • Tell a trusted adult ………………. . …………………………………………………………………. .
Advantages of SOS • Implemented by school staff • Engages existing supports including school staff, parents, peers, community • Incorporates many best practice elements • Increases dialogue around mental health • Reduces stigma • Sustainable ………………. . …………………………………………………………………. .
How the CSPR stages SOS training • • • Step 1: Meet with school staff to plan logistics (60 min) Step 2: Provide SOS training to all school staff (60 -90 min) Step 3: Host parent educational evening (60 min) Step 4: School staff trained to present SOS (90 min) Step 5: School staff who collect screening data and follow up with students receive training (90 min) • Step 6: Deliver the SOS curriculum over two days to a specified grade or set of classes • Step 7: Students screened and assessed if indicated • Step 8: Review disposition with school and parent ………………. . …………………………………………………………………. .
Screening and Risk Assessment • School personnel implement the screening and first phase of risk assessment • Student response card • BSAD depression and suicide screening questionnaire • NCH clinician available for consultation ………………. . …………………………………………………………………. .
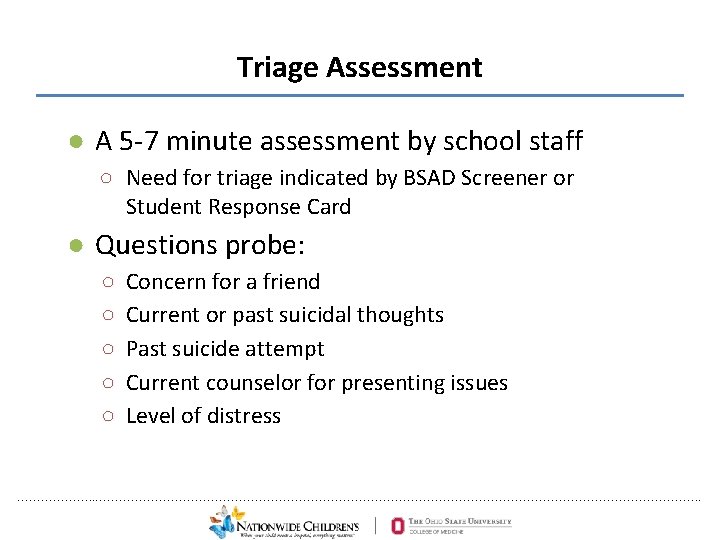
Triage Assessment ● A 5 -7 minute assessment by school staff ○ Need for triage indicated by BSAD Screener or Student Response Card ● Questions probe: ○ ○ ○ Concern for a friend Current or past suicidal thoughts Past suicide attempt Current counselor for presenting issues Level of distress ………………. . …………………………………………………………………. .
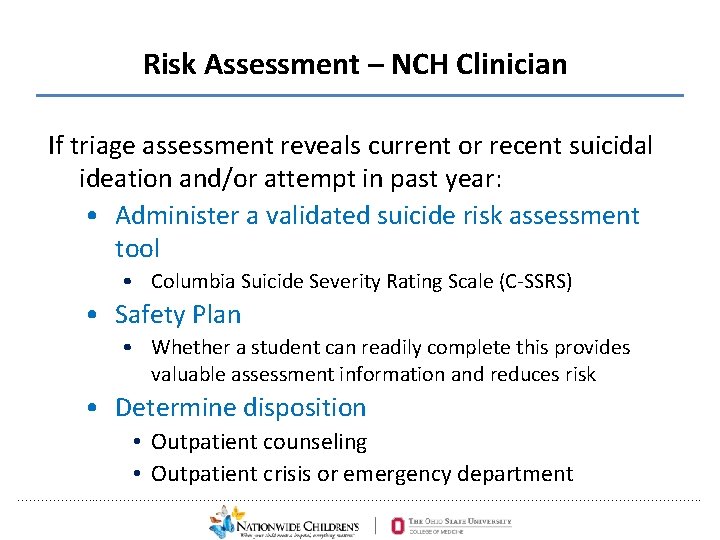
Risk Assessment – NCH Clinician If triage assessment reveals current or recent suicidal ideation and/or attempt in past year: • Administer a validated suicide risk assessment tool • Columbia Suicide Severity Rating Scale (C-SSRS) • Safety Plan • Whether a student can readily complete this provides valuable assessment information and reduces risk • Determine disposition • Outpatient counseling • Outpatient crisis or emergency department ………………. . …………………………………………………………………. .
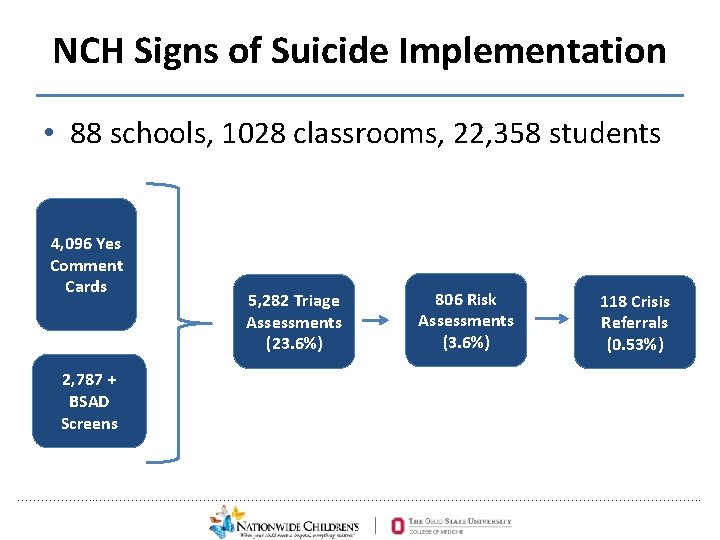
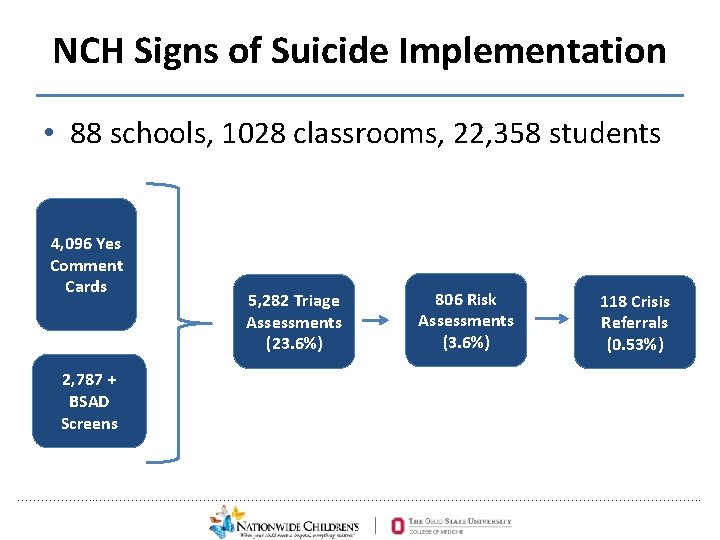
NCH Signs of Suicide Implementation • 88 schools, 1028 classrooms, 22, 358 students 4, 096 Yes Comment Cards 5, 282 Triage Assessments (23. 6%) 806 Risk Assessments (3. 6%) 118 Crisis Referrals (0. 53%) 2, 787 + BSAD Screens ………………. . …………………………………………………………………. .
PAX Good Behavior Game • Evidence-based universal prevention model for elementary school students • Teacher-driven, implemented in the classroom • Applies basic behavioral core principles • Game-like reward system • Encourages development of self-management skills, emotional regulation and pro-social behavior ………………. . …………………………………………………………………. . 43
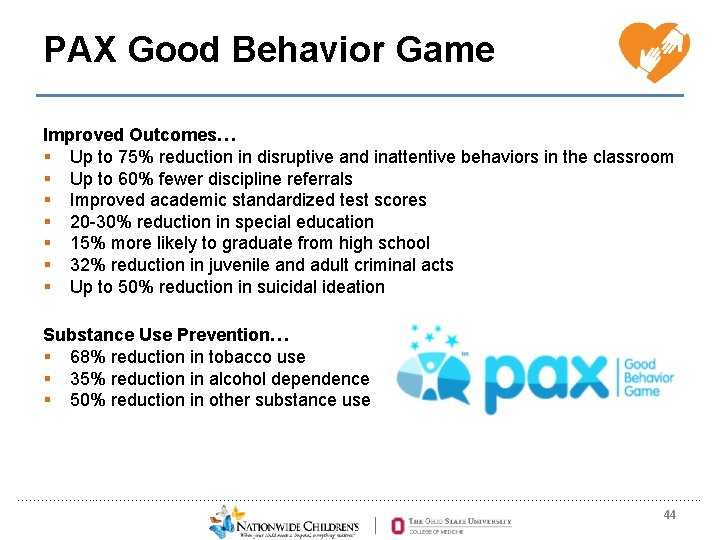
PAX Good Behavior Game Improved Outcomes… § Up to 75% reduction in disruptive and inattentive behaviors in the classroom § Up to 60% fewer discipline referrals § Improved academic standardized test scores § 20 -30% reduction in special education § 15% more likely to graduate from high school § 32% reduction in juvenile and adult criminal acts § Up to 50% reduction in suicidal ideation Substance Use Prevention… § 68% reduction in tobacco use § 35% reduction in alcohol dependence § 50% reduction in other substance use ………………. . …………………………………………………………………. . 44
Implementation • Classroom teachers trained in 1 -day session • NCH therapist available for coaching – Masters’ level therapists – 1 -day initial training; 3 -day PAX partner training ………………. . …………………………………………………………………. . 45
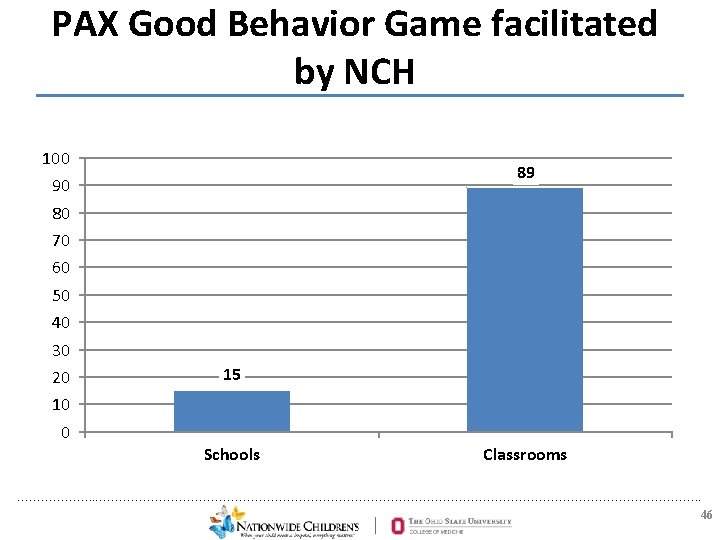
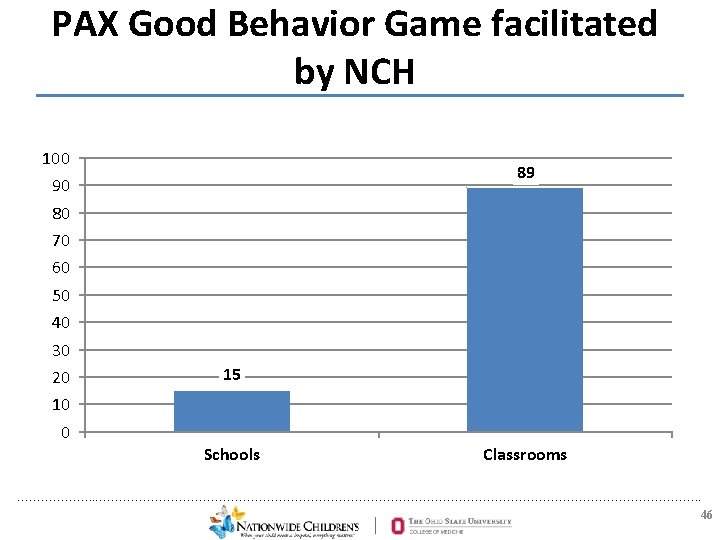
PAX Good Behavior Game facilitated by NCH 100 89 90 80 70 60 50 40 30 20 15 10 0 Schools Classrooms ………………. . …………………………………………………………………. . 46
Importance of School Administration Support 2015 -16 school year vs. 2016 -17: • Strong support for PAX-GBG: – 54. 1 % reduction in the rate of suspension days/student (1. 12 to 0. 51 days/student) – 39% reduction in infractions resulting in suspensions • Weak support for PAX-GBG: – 12. 6% increase in the rate of suspension days/student (1. 23 to 1. 38 days/student) – 5% increase in infractions resulting in suspensions ………………. . …………………………………………………………………. .
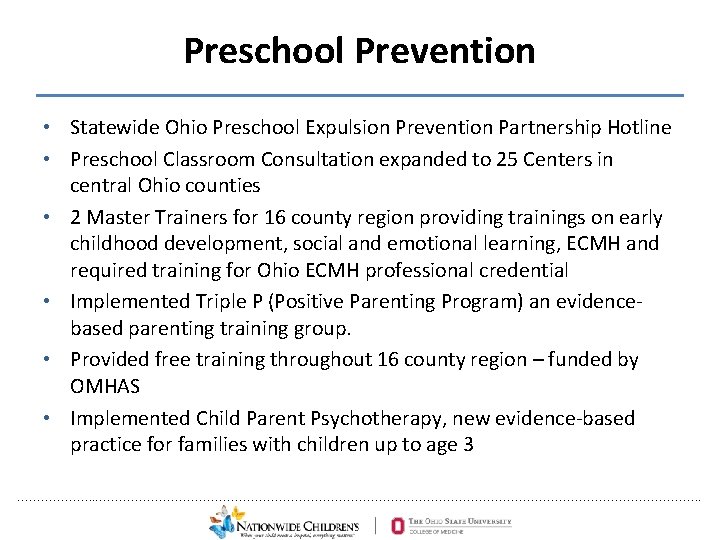
Preschool Prevention • Statewide Ohio Preschool Expulsion Prevention Partnership Hotline • Preschool Classroom Consultation expanded to 25 Centers in central Ohio counties • 2 Master Trainers for 16 county region providing trainings on early childhood development, social and emotional learning, ECMH and required training for Ohio ECMH professional credential • Implemented Triple P (Positive Parenting Program) an evidencebased parenting training group. • Provided free training throughout 16 county region – funded by OMHAS • Implemented Child Parent Psychotherapy, new evidence-based practice for families with children up to age 3 ………………. . …………………………………………………………………. .
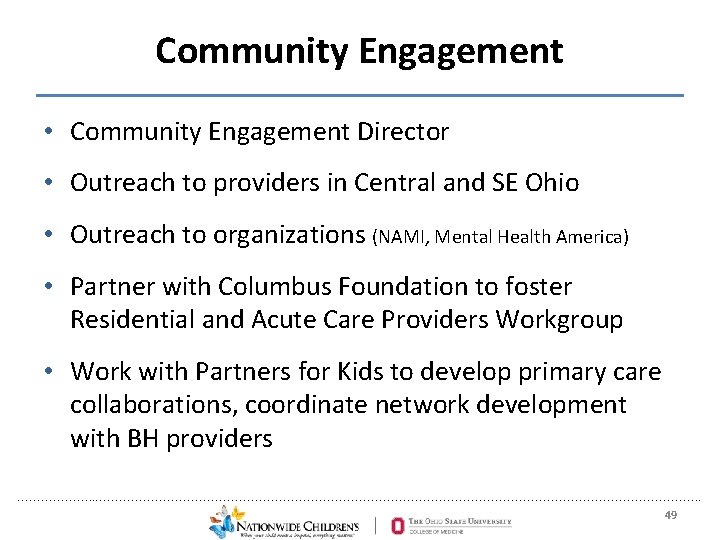
Community Engagement • Community Engagement Director • Outreach to providers in Central and SE Ohio • Outreach to organizations (NAMI, Mental Health America) • Partner with Columbus Foundation to foster Residential and Acute Care Providers Workgroup • Work with Partners for Kids to develop primary care collaborations, coordinate network development with BH providers ………………. . …………………………………………………………………. . 49
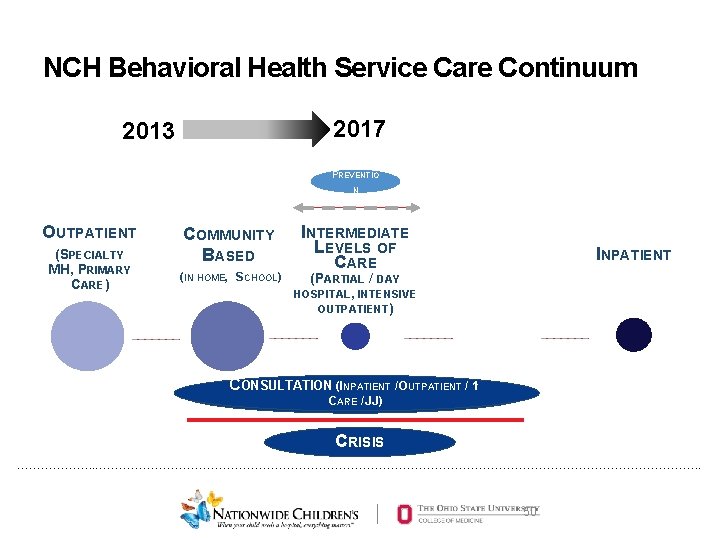
NCH Behavioral Health Service Care Continuum 2017 2013 PREVENTIO N OUTPATIENT (S (SPECIALTY MH, MH) PRIMARY CARE) COMMUNITY BASED (IN HOME, SCHOOL) INTERMEDIATE LEVELS OF CARE INPATIENT (PARTIAL / DAY HOSPITAL, INTENSIVE OUTPATIENT) CONSULTATION (INPATIENT / OUTPATIENT / 1◦ ONSULTATION (I(I NPATIENT CCONSULTATION NPATIENT // ARE / JJ) OCUTPATIENT OUTPATIENT / JJ)) CCRISIS ………………. . …………………………………………………………………. . 50
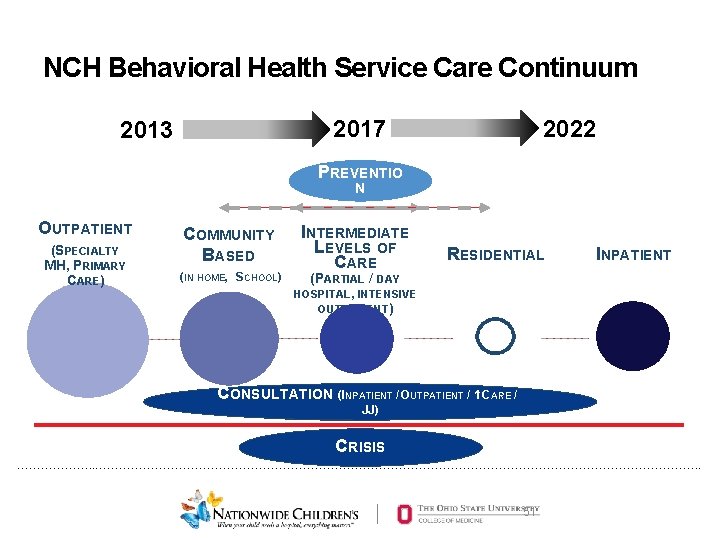
NCH Behavioral Health Service Care Continuum 2022 2017 2013 PREVENTIO N N OUTPATIENT (SPECIALTY MH, PRIMARY CARE) COMMUNITY BASED (IN HOME, SCHOOL) INTERMEDIATE LEVELS OF CARE RESIDENTIAL INPATIENT (PARTIAL / DAY HOSPITAL, INTENSIVE OUTPATIENT) CCONSULTATION NPATIENT OUTPATIENT CONSULTATION (INPATIENT / ONSULTATION (I(INPATIENT //O // 11◦◦ CARE / OCUTPATIENT ARE /JJ) ) CCRISIS ………………. . …………………………………………………………………. . 51
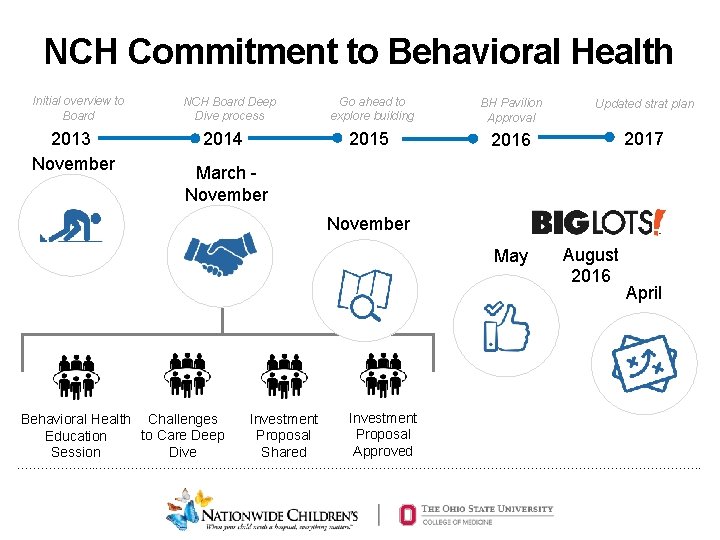
NCH Commitment to Behavioral Health Initial overview to Board 2013 November NCH Board Deep Dive process 2014 Go ahead to explore building BH Pavilion Approval Updated strat plan 2015 2016 2017 March November May Behavioral Health Challenges to Care Deep Education Dive Session Investment Proposal Shared Investment Proposal Approved August 2016 April ………………. . …………………………………………………………………. .
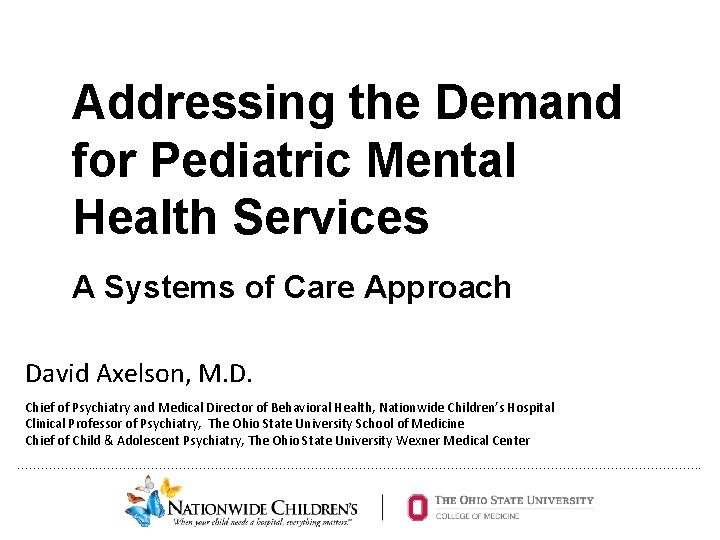
Key Principles • Burning platform: pediatric mental health crisis and youth suicide • Engage board, hospital administration, donors, community leaders, governmental agencies • Think systemically and build care continuum • Prevention as part of care continuum • Interdisciplinary teams are required • Coordination with other providers (BH, primary care, pediatric subspecialists) ………………. . …………………………………………………………………. .
Challenges • • • Hard to measure outcomes – more patients not necessary better outcomes Recruiting, training and retaining personnel Getting different disciplines into One Team Building culture during rapid growth Developing academic and research mission Faculty burnout Managing hospital administration expectations re BH patients Documentation burden – inefficient EHR Need to leverage technology more in care Reimbursement complicated and insufficient Build it, and they will come… – Seeing more kids, but outpatient access for non-urgent patients is 3 -5 months • Community partnerships are hard to do ………………. . …………………………………………………………………. .
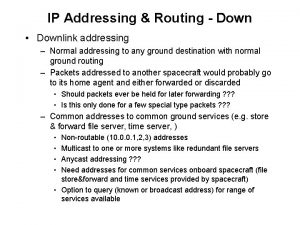
 Flat addressing vs hierarchical addressing
Flat addressing vs hierarchical addressing Mental health and mental illness chapter 20
Mental health and mental illness chapter 20 Mental health jeopardy questions
Mental health jeopardy questions Bexar county mental health services
Bexar county mental health services Discharge letter from mental health services
Discharge letter from mental health services West cork mental health services bantry
West cork mental health services bantry California mental health services authority
California mental health services authority Inventory modeling
Inventory modeling Measures to correct excess and deficient demand
Measures to correct excess and deficient demand Individual demand vs market demand
Individual demand vs market demand Dependent demand operations management
Dependent demand operations management Halimbawa ng demand curve
Halimbawa ng demand curve Dependent demand vs independent demand
Dependent demand vs independent demand Module 5 supply and demand introduction and demand
Module 5 supply and demand introduction and demand Demand forecasting methods in managerial economics
Demand forecasting methods in managerial economics Distinguish between individual demand and market demand
Distinguish between individual demand and market demand Dependent and independent demand in inventory management
Dependent and independent demand in inventory management Fspos vägledning för kontinuitetshantering
Fspos vägledning för kontinuitetshantering Typiska drag för en novell
Typiska drag för en novell Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Ekologiskt fotavtryck
Ekologiskt fotavtryck Varför kallas perioden 1918-1939 för mellankrigstiden
Varför kallas perioden 1918-1939 för mellankrigstiden En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Underlag för särskild löneskatt på pensionskostnader
Underlag för särskild löneskatt på pensionskostnader Personlig tidbok
Personlig tidbok Anatomi organ reproduksi
Anatomi organ reproduksi Förklara densitet för barn
Förklara densitet för barn Datorkunskap för nybörjare
Datorkunskap för nybörjare Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Debatt artikel mall
Debatt artikel mall För och nackdelar med firo
För och nackdelar med firo Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Lufttryck formel
Lufttryck formel Offentlig förvaltning
Offentlig förvaltning Jag har nigit för nymånens skära
Jag har nigit för nymånens skära Presentera för publik crossboss
Presentera för publik crossboss Vad är ett minoritetsspråk
Vad är ett minoritetsspråk Kanaans land
Kanaans land Klassificeringsstruktur för kommunala verksamheter
Klassificeringsstruktur för kommunala verksamheter Fimbrietratt
Fimbrietratt Claes martinsson
Claes martinsson Cks
Cks Byggprocessen steg för steg
Byggprocessen steg för steg Mat för unga idrottare
Mat för unga idrottare Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Rutin för avvikelsehantering
Rutin för avvikelsehantering Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Tack för att ni har lyssnat
Tack för att ni har lyssnat Referat mall
Referat mall Redogör för vad psykologi är
Redogör för vad psykologi är Matematisk modellering eksempel
Matematisk modellering eksempel Tack för att ni har lyssnat
Tack för att ni har lyssnat Borra hål för knoppar
Borra hål för knoppar