Transforming the Pathway in Prostate Cancer Manit Arya






- Slides: 42
Transforming the Pathway in Prostate Cancer Manit Arya Consultant Urological Surgeon UCLH and PAH
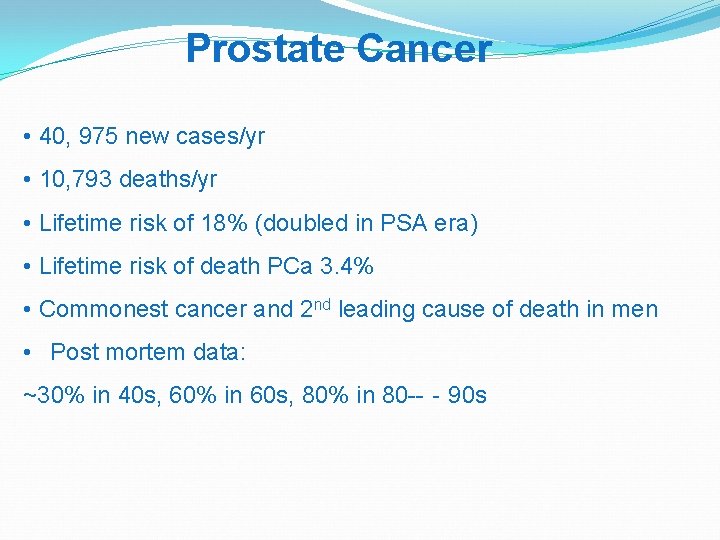
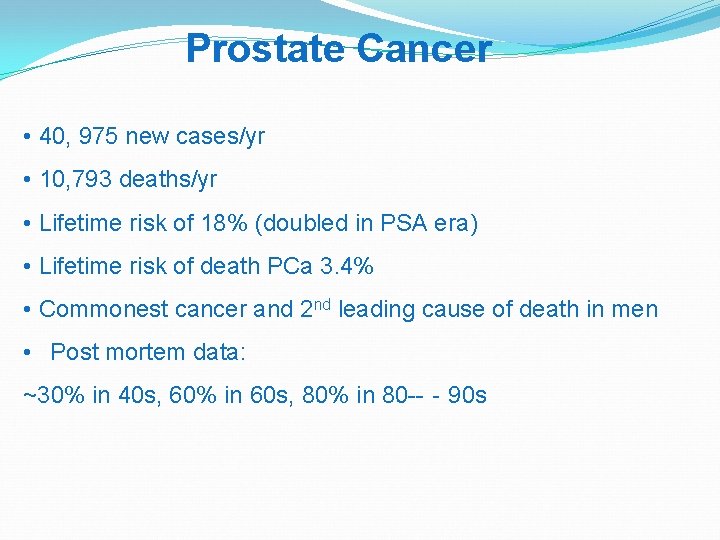
Prostate Cancer • 40, 975 new cases/yr • 10, 793 deaths/yr • Lifetime risk of 18% (doubled in PSA era) • Lifetime risk of death PCa 3. 4% • Commonest cancer and 2 nd leading cause of death in men • Post mortem data: ~30% in 40 s, 60% in 60 s, 80% in 80 --‐ 90 s
Diagnosis

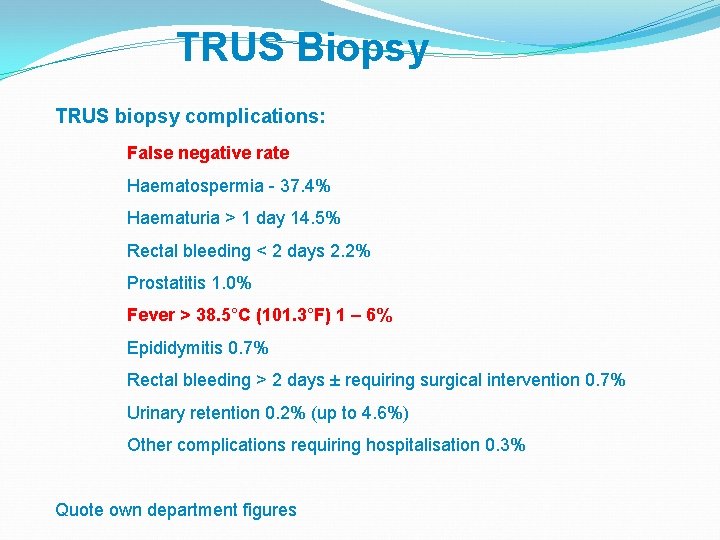
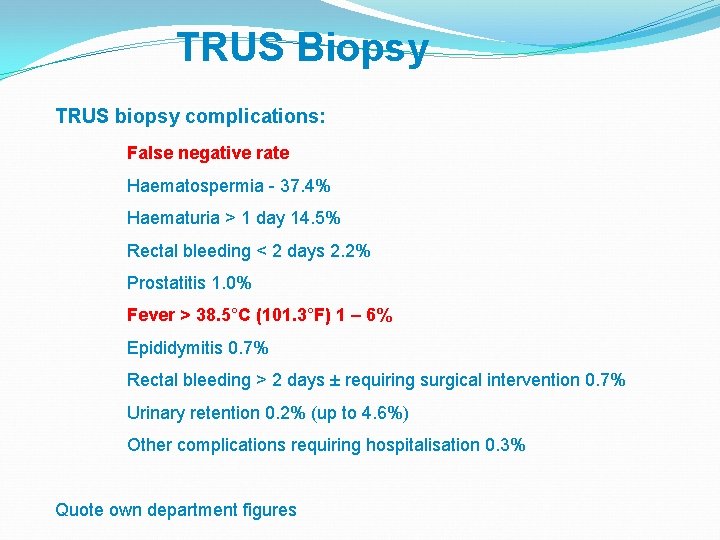
TRUS Biopsy TRUS biopsy complications: False negative rate Haematospermia - 37. 4% Haematuria > 1 day 14. 5% Rectal bleeding < 2 days 2. 2% Prostatitis 1. 0% Fever > 38. 5°C (101. 3°F) 1 – 6% Epididymitis 0. 7% Rectal bleeding > 2 days ± requiring surgical intervention 0. 7% Urinary retention 0. 2% (up to 4. 6%) Other complications requiring hospitalisation 0. 3% Quote own department figures
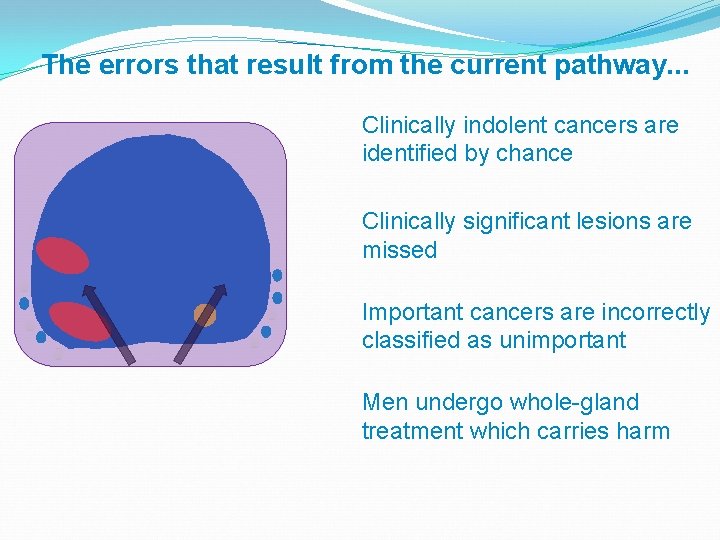
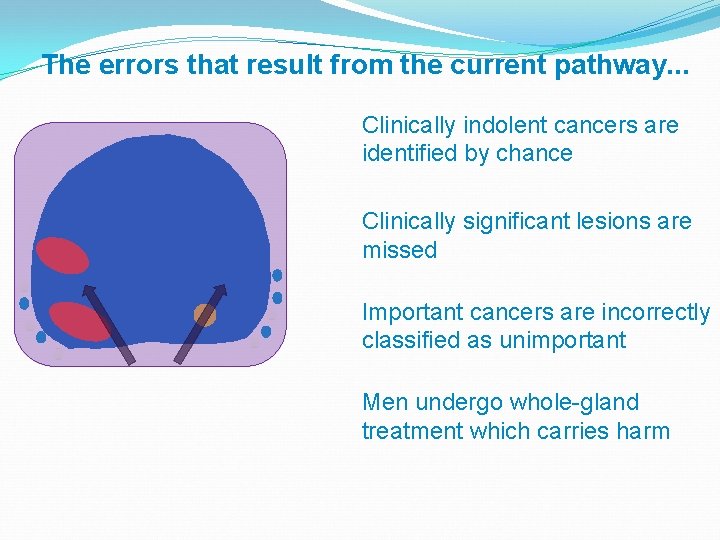
The errors that result from the current pathway. . . Clinically indolent cancers are identified by chance Clinically significant lesions are missed Important cancers are incorrectly classified as unimportant Men undergo whole-gland treatment which carries harm
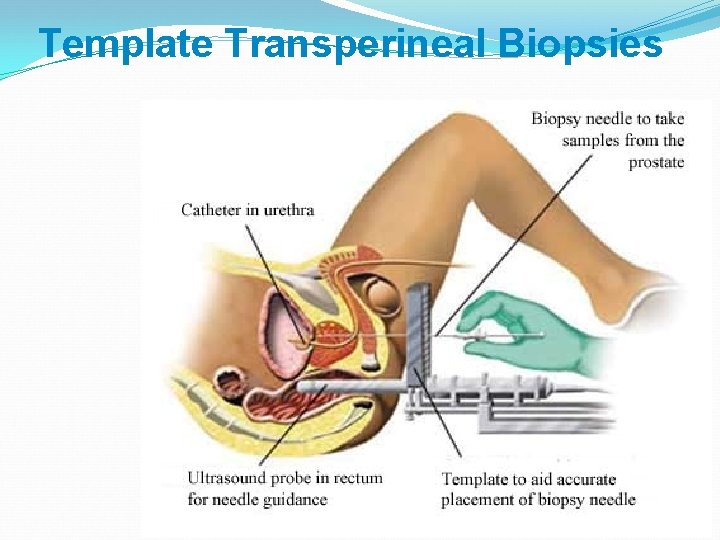
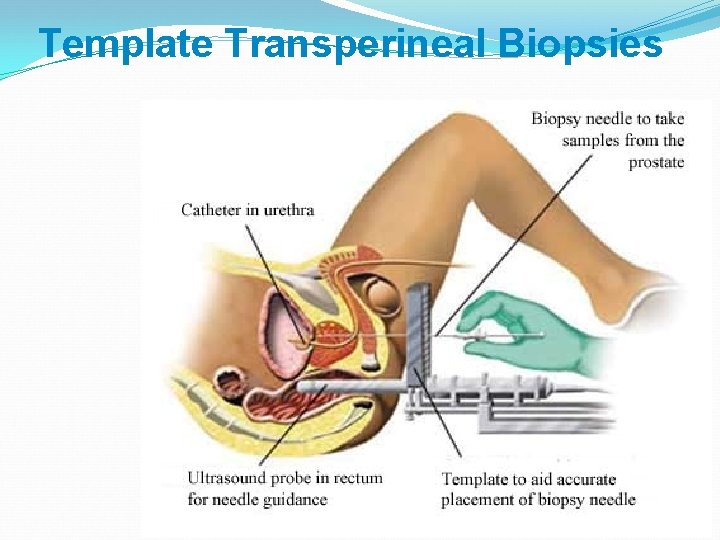
Template Transperineal Biopsies
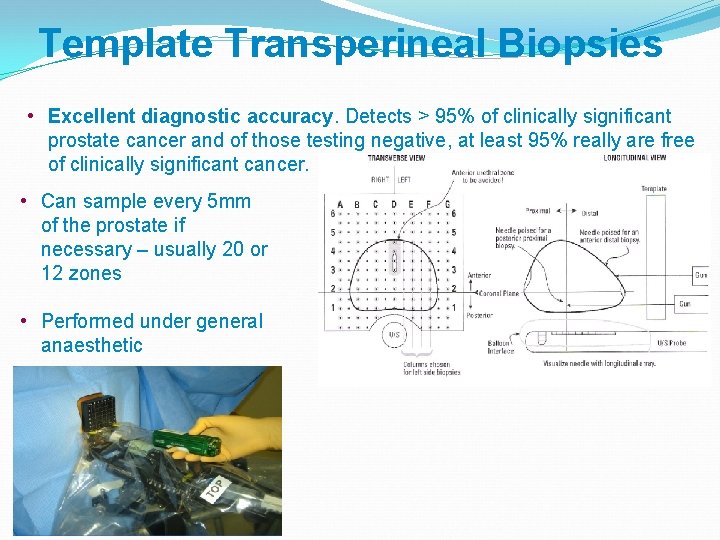
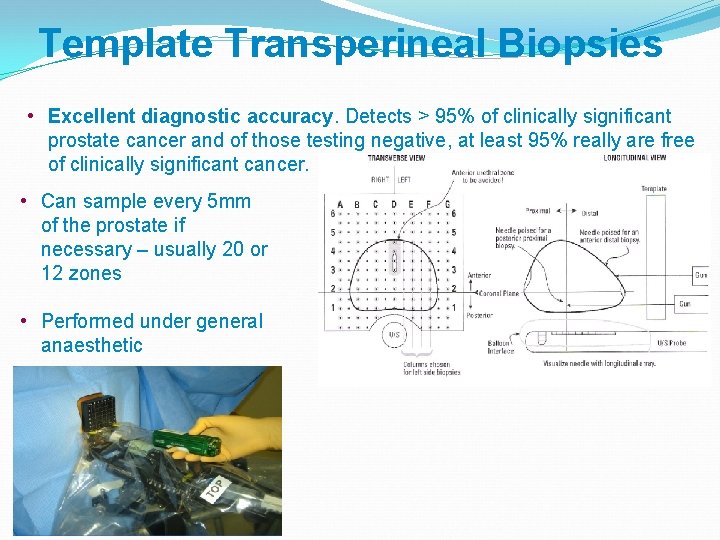
Template Transperineal Biopsies • Excellent diagnostic accuracy. Detects > 95% of clinically significant prostate cancer and of those testing negative, at least 95% really are free of clinically significant cancer. • Can sample every 5 mm of the prostate if necessary – usually 20 or 12 zones • Performed under general anaesthetic
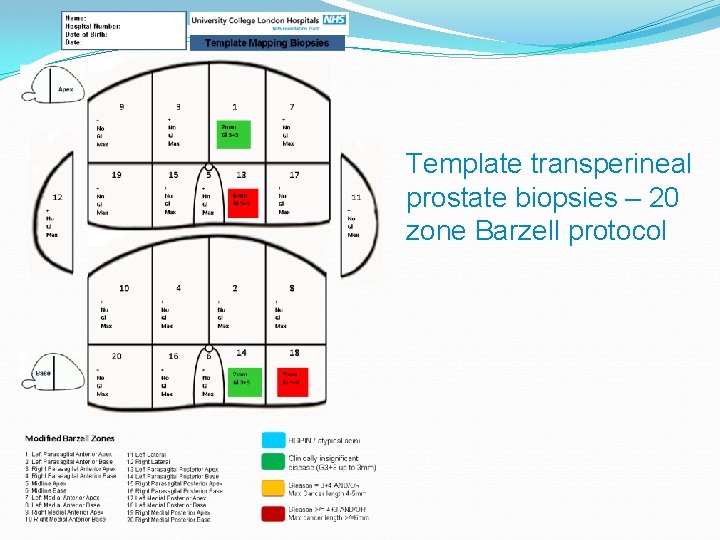
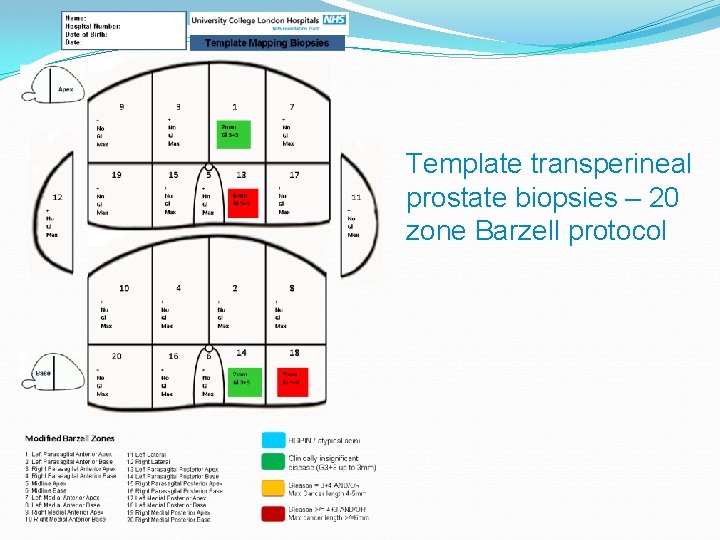
Template transperineal prostate biopsies – 20 zone Barzell protocol
BUT New kid on the block as a diagnostic test
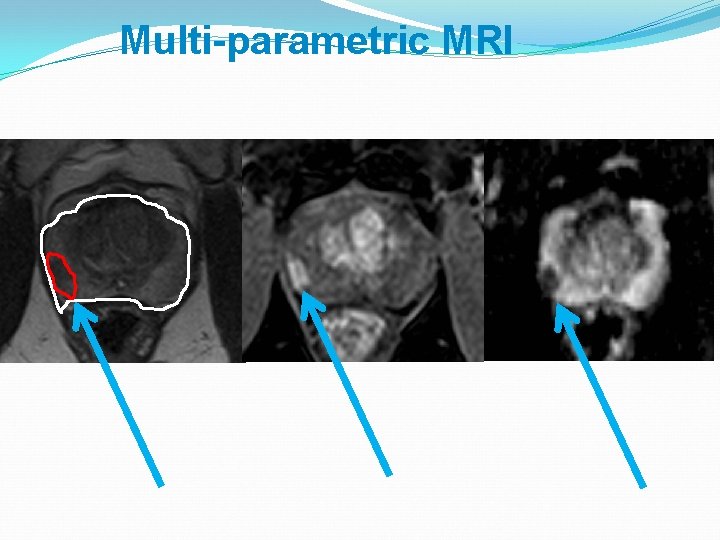
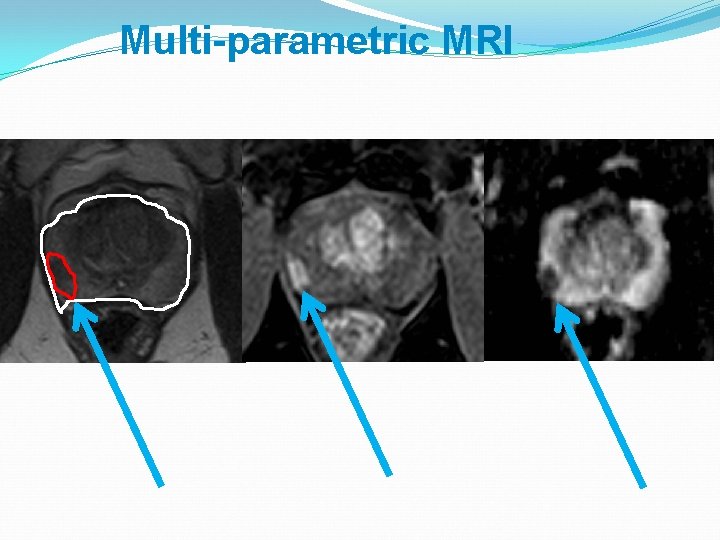
Multi-parametric MRI
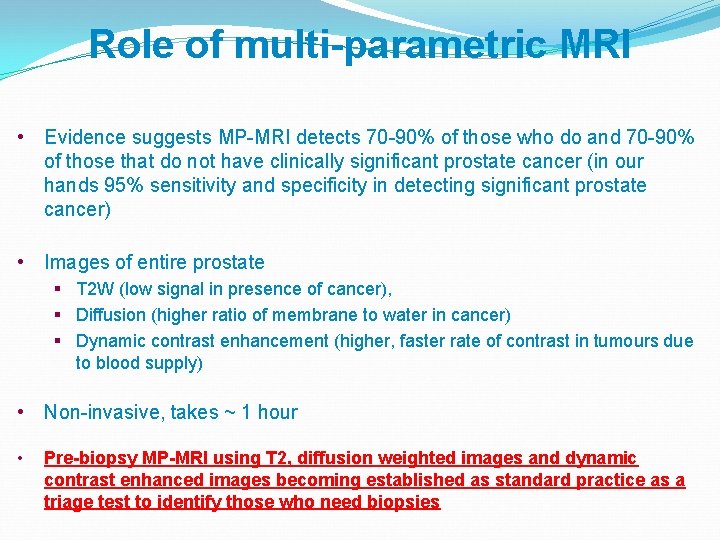
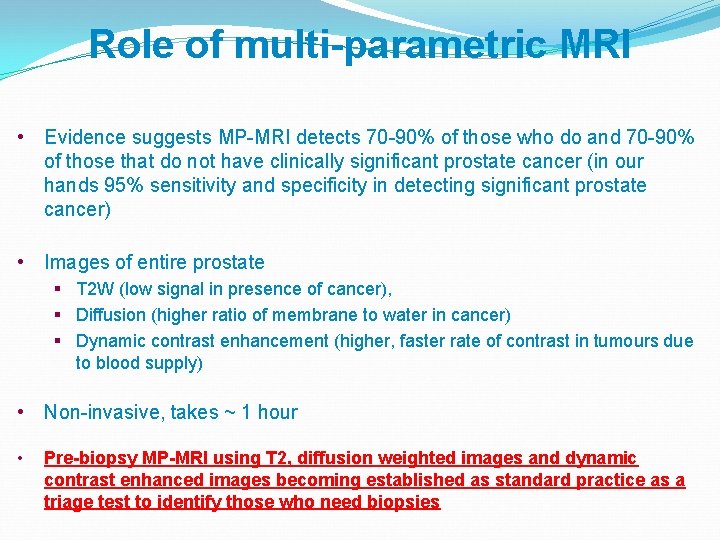
Role of multi-parametric MRI • Evidence suggests MP-MRI detects 70 -90% of those who do and 70 -90% of those that do not have clinically significant prostate cancer (in our hands 95% sensitivity and specificity in detecting significant prostate cancer) • Images of entire prostate § T 2 W (low signal in presence of cancer), § Diffusion (higher ratio of membrane to water in cancer) § Dynamic contrast enhancement (higher, faster rate of contrast in tumours due to blood supply) • Non-invasive, takes ~ 1 hour • Pre-biopsy MP-MRI using T 2, diffusion weighted images and dynamic contrast enhanced images becoming established as standard practice as a triage test to identify those who need biopsies
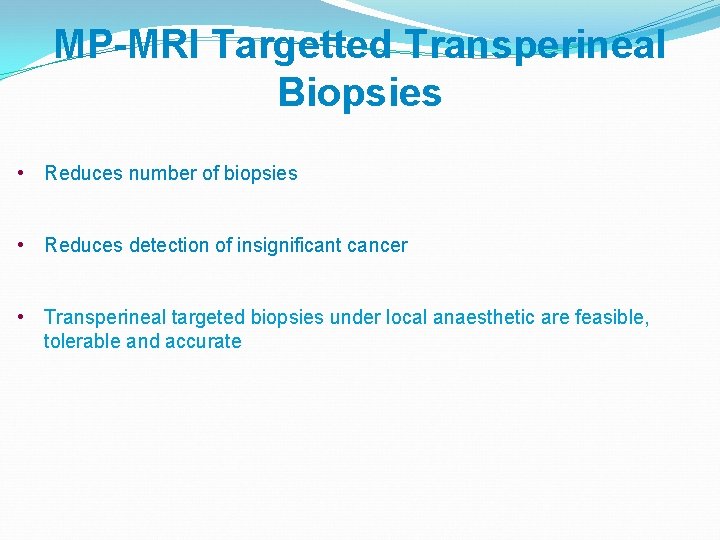
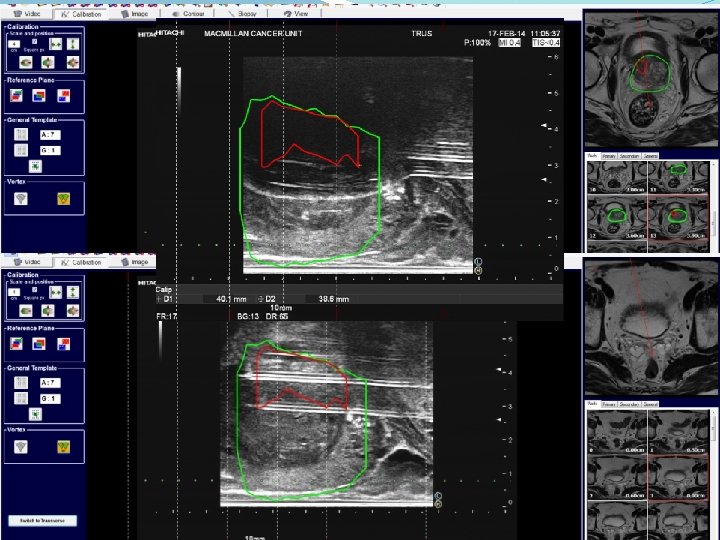
MP-MRI Targetted Transperineal Biopsies • Reduces number of biopsies • Reduces detection of insignificant cancer • Transperineal targeted biopsies under local anaesthetic are feasible, tolerable and accurate
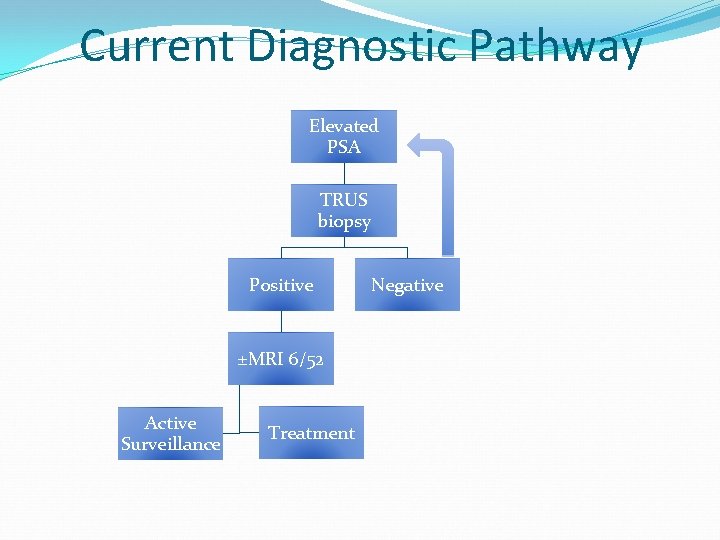
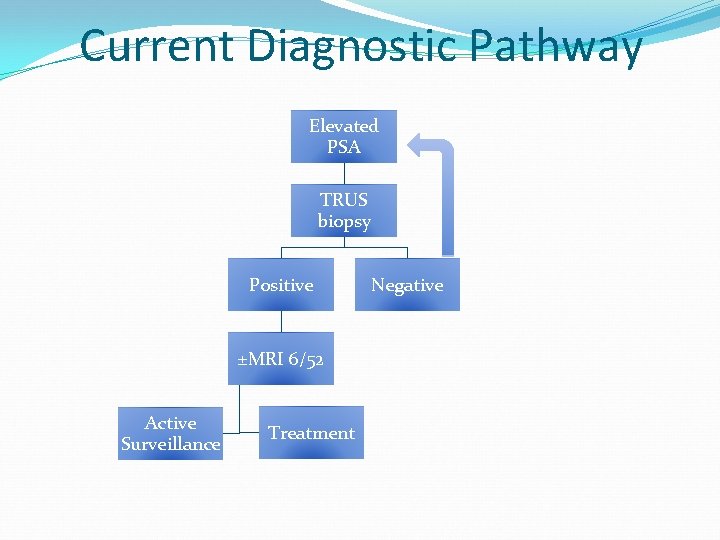
Current Diagnostic Pathway Elevated PSA TRUS biopsy Positive ±MRI 6/52 Active Surveillance Treatment Negative
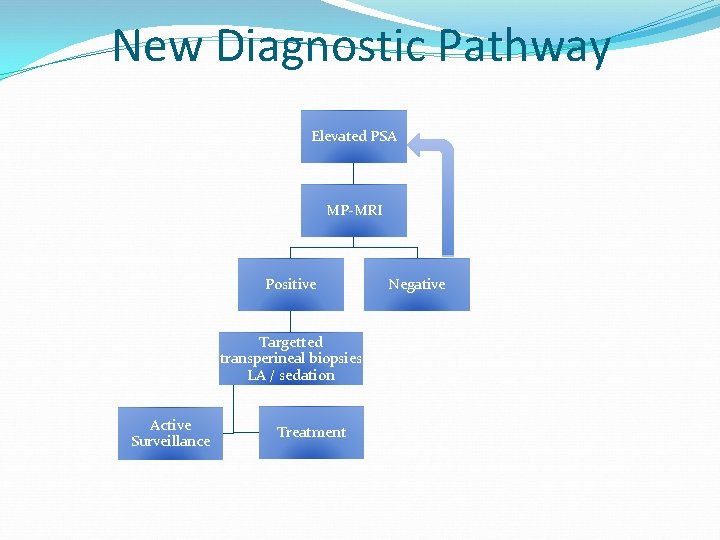
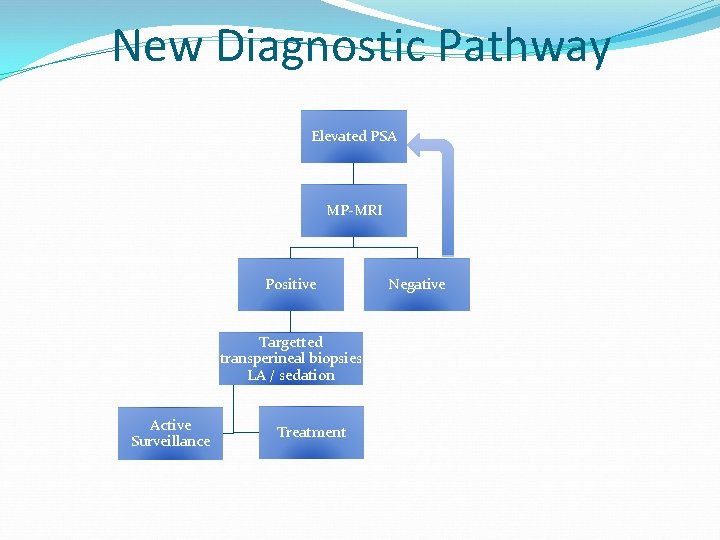
New Diagnostic Pathway Elevated PSA MP-MRI Positive Targetted transperineal biopsies LA / sedation Active Surveillance Treatment Negative
Treatment
So, …we have a target… … can we treat just that target… … as opposed to the whole prostate i. e. radical prostatectomy or radiotherapy?
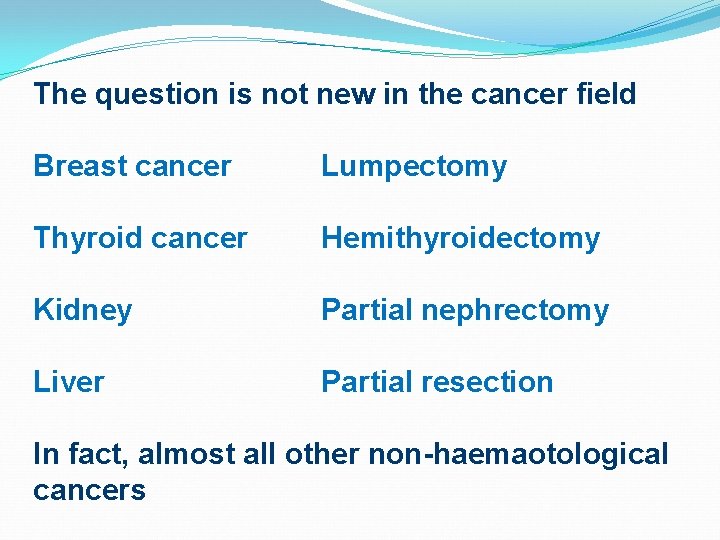
The question is not new in the cancer field Breast cancer Lumpectomy Thyroid cancer Hemithyroidectomy Kidney Partial nephrectomy Liver Partial resection In fact, almost all other non-haemaotological cancers
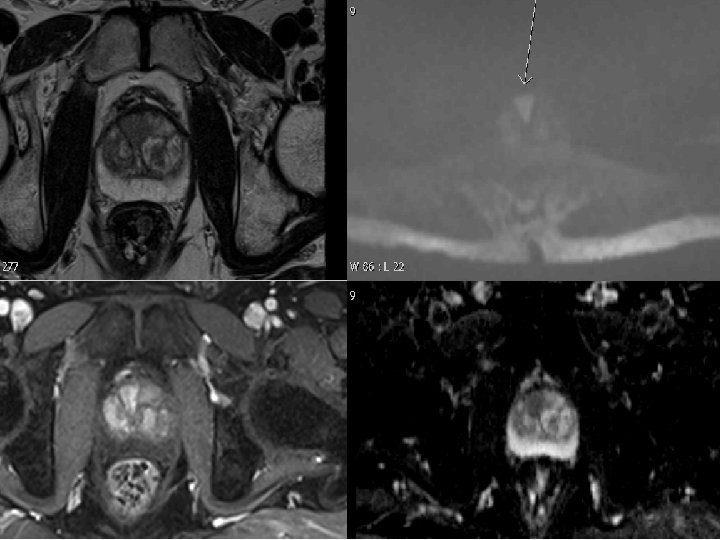
We can accurately localise prostate cancers
We now have the tools to treat just the tumour and not the whole prostate…
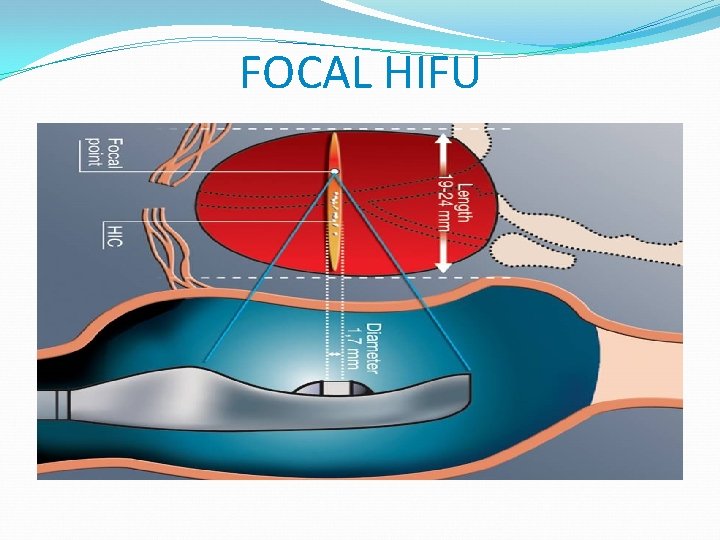
Difficult to surgically remove only part of the prostate Need energy source that will result in cancer cell death and that can be accurately targetted/ focused to affected areas - HIFU / cryotherapy
Cryotherapy High Intensity Focused Ultrasound Brachytherapy Interstitial Photothermal Laser Irreversible Electroporation Photodynamic Therapy Radiofrequency Ablation
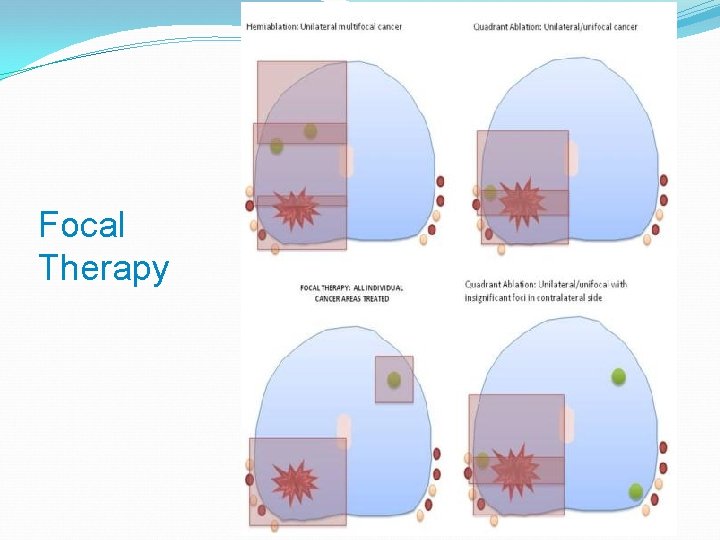
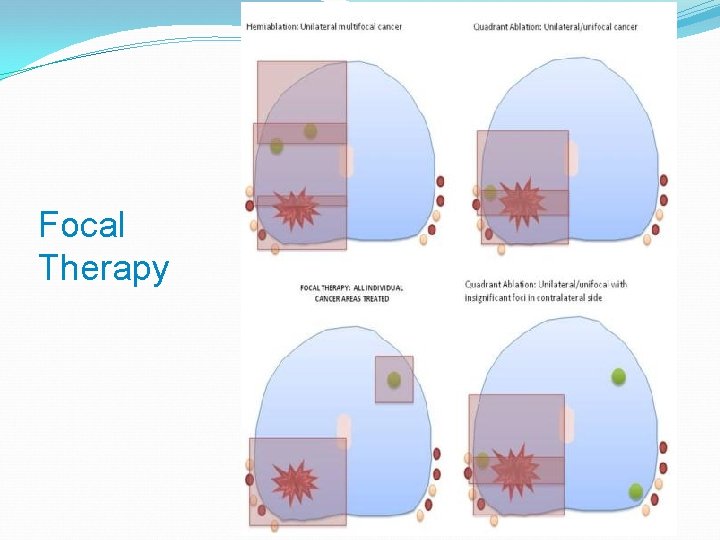
Focal Therapy

HIFU with the Sonablate® System The Sonablate® 500 is a medical device that uses HIFU to thermally ablate the prostate.
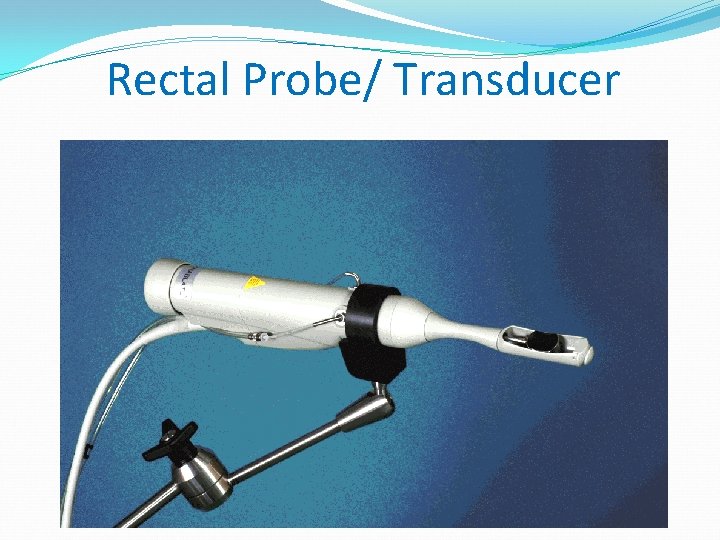
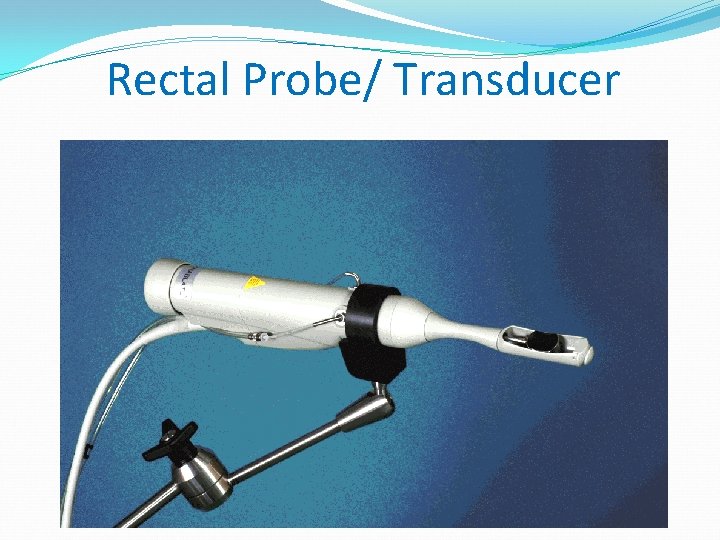
Rectal Probe/ Transducer
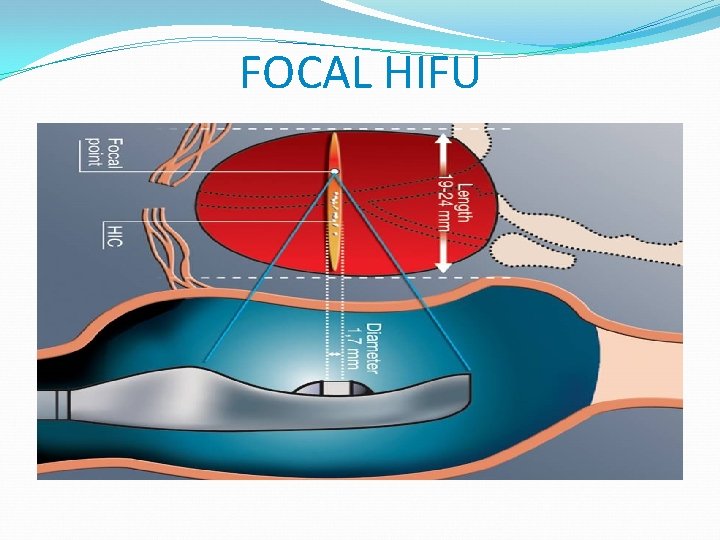
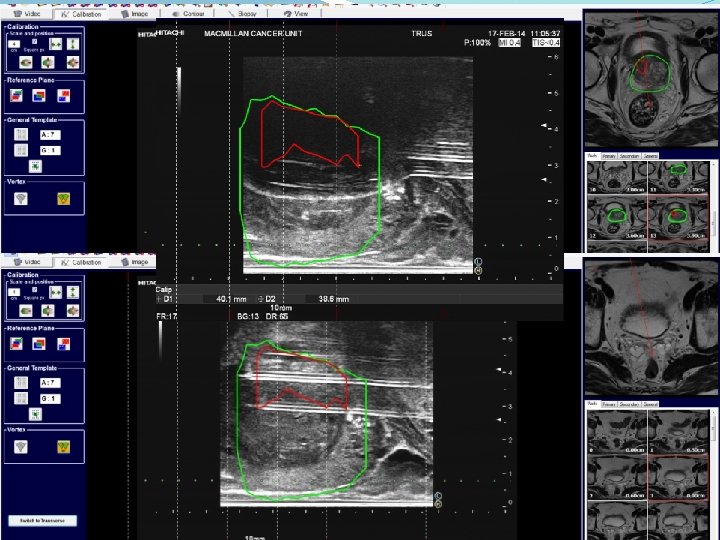
FOCAL HIFU
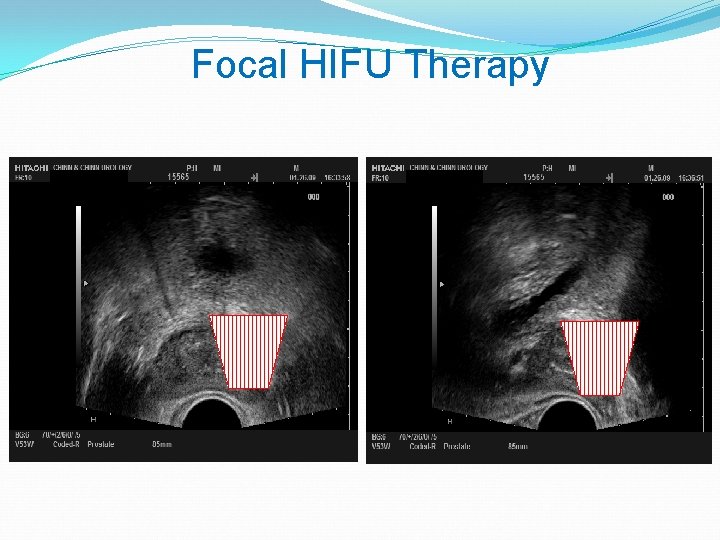
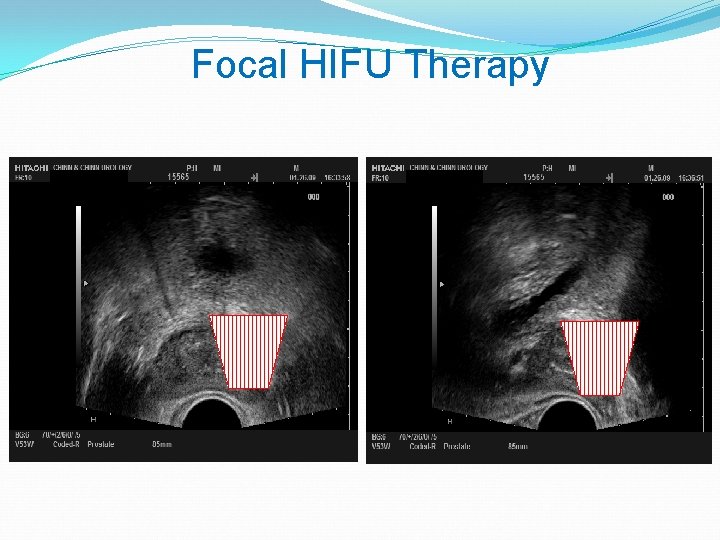
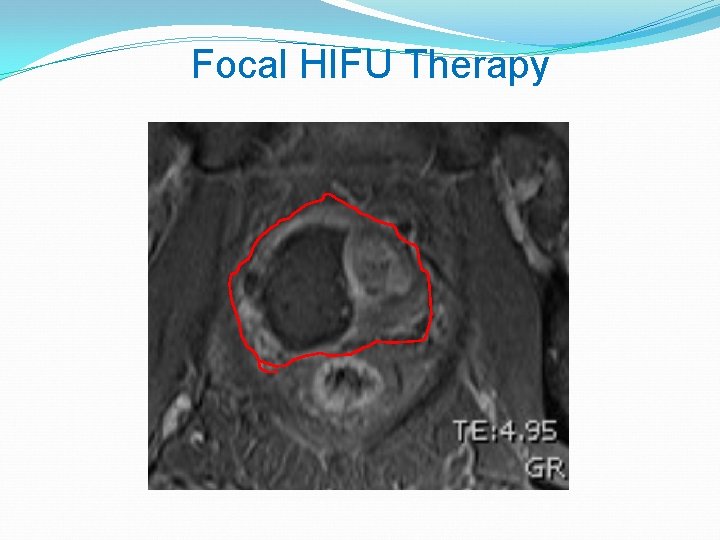
Focal HIFU Therapy
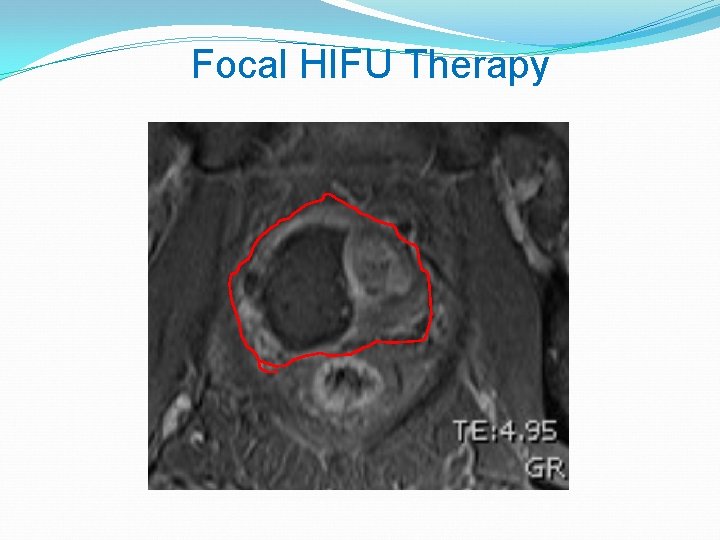
Focal HIFU Therapy

Focal HIFU Therapy
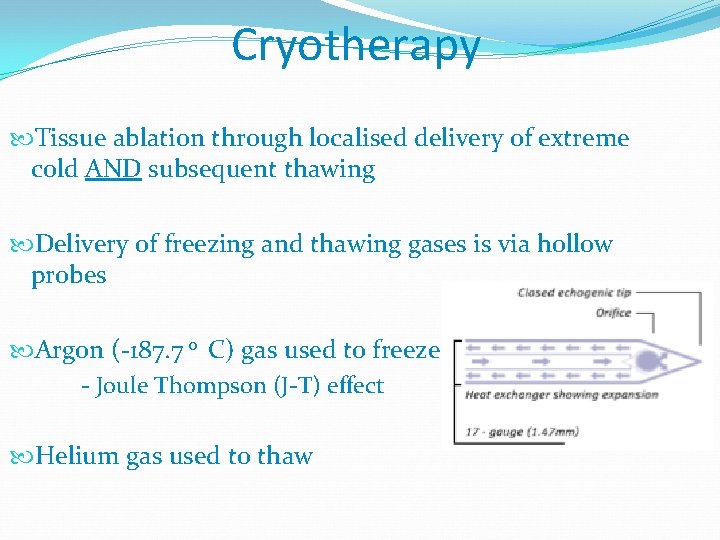
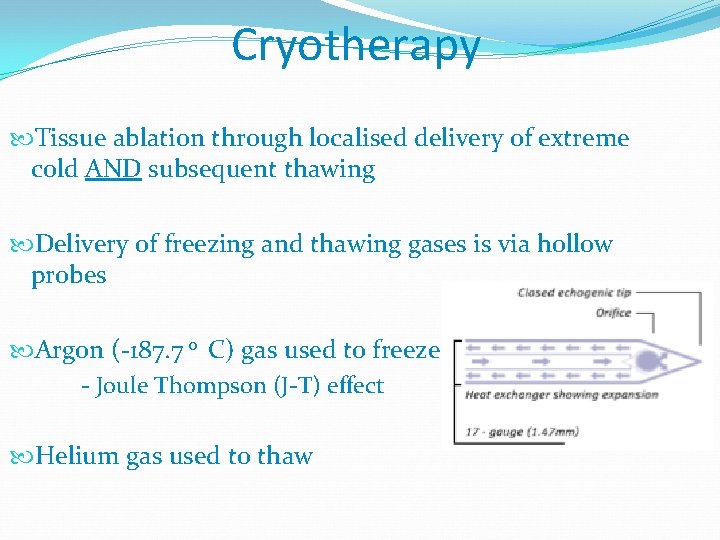
Cryotherapy Tissue ablation through localised delivery of extreme cold AND subsequent thawing Delivery of freezing and thawing gases is via hollow probes Argon (-187. 7 0 C) gas used to freeze - Joule Thompson (J-T) effect Helium gas used to thaw
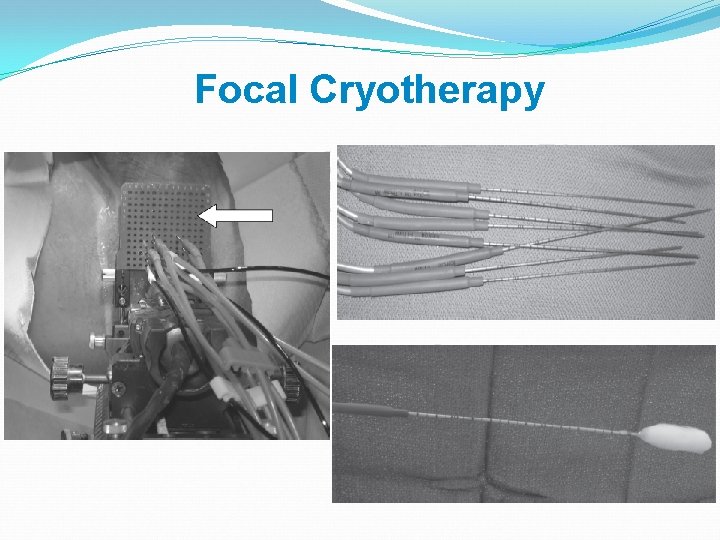
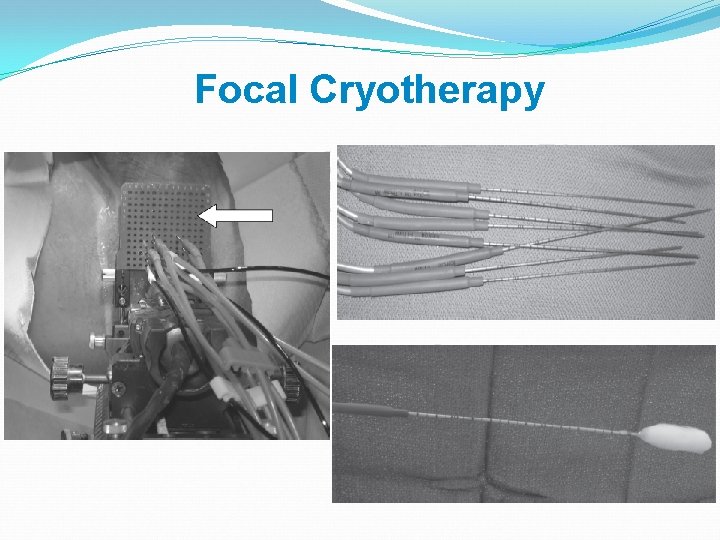
Focal Cryotherapy
Example from the Cohort Mr GM, 64 years, Gl 3+3 on AS since 2008, PSA 8
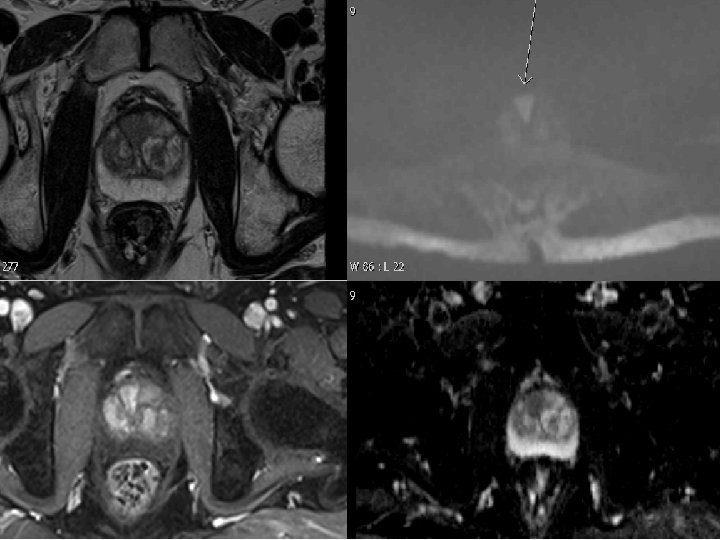
Example from the Cohort


Mr Markham

Post-operative MP-MRI
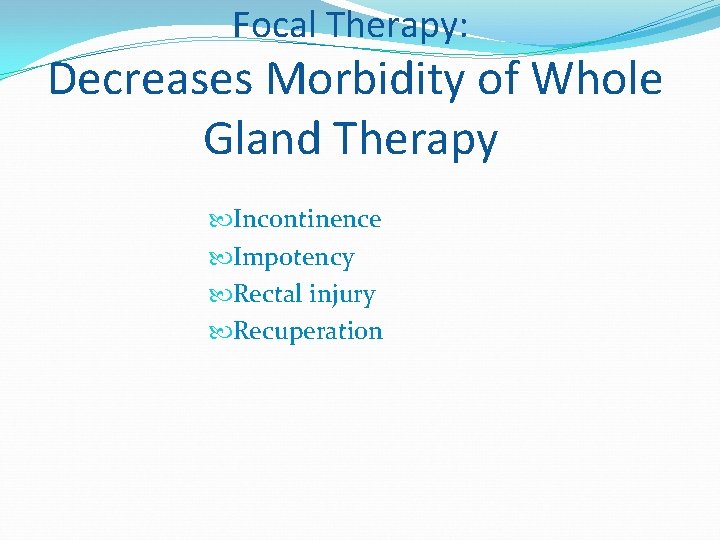
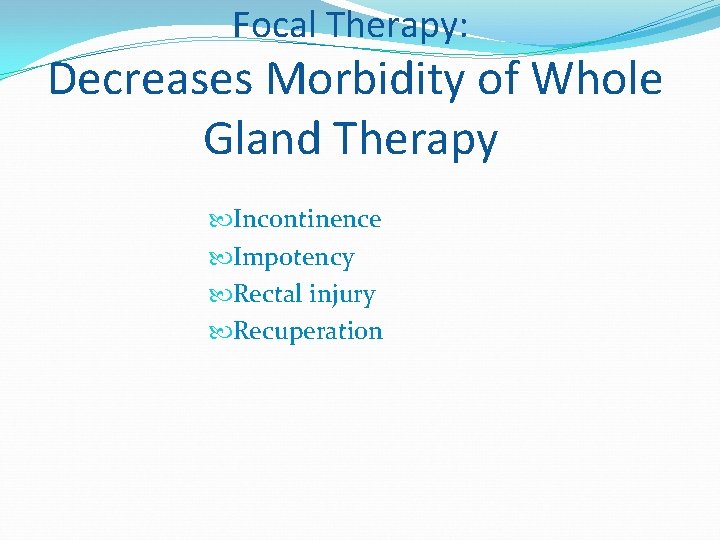
Focal Therapy: Decreases Morbidity of Whole Gland Therapy Incontinence Impotency Rectal injury Recuperation
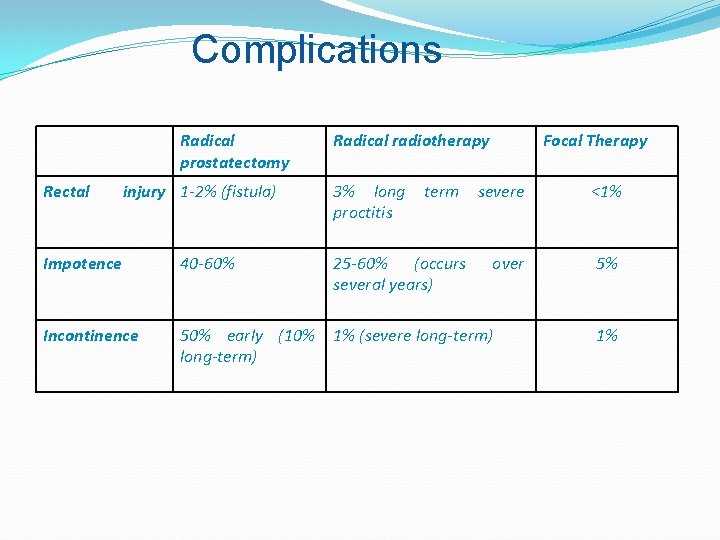
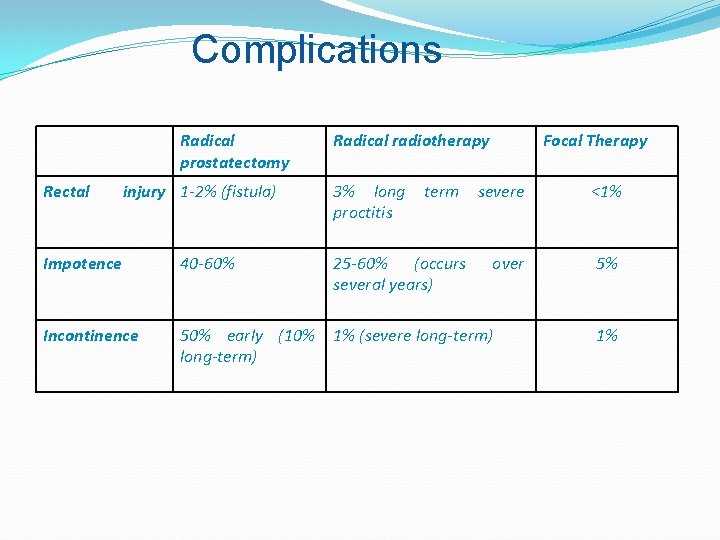
Complications Radical prostatectomy Rectal injury 1 -2% (fistula) Radical radiotherapy 3% long proctitis term Focal Therapy severe <1% over 5% Impotence 40 -60% 25 -60% (occurs several years) Incontinence 50% early (10% long-term) 1% (severe long-term) 1%
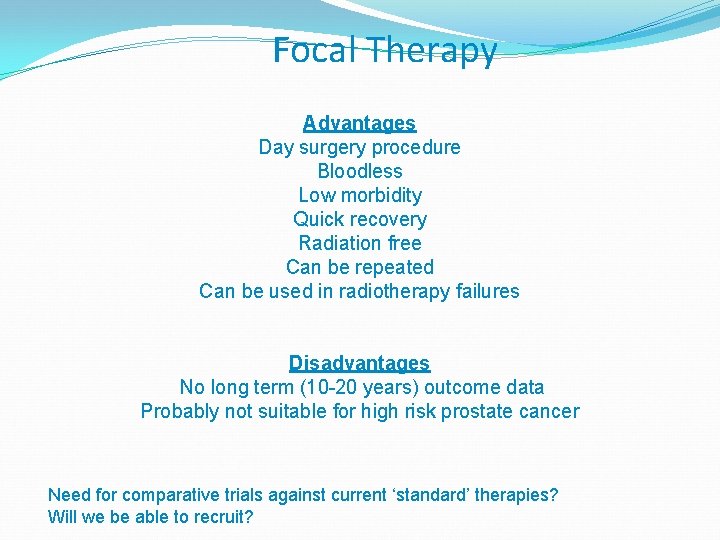
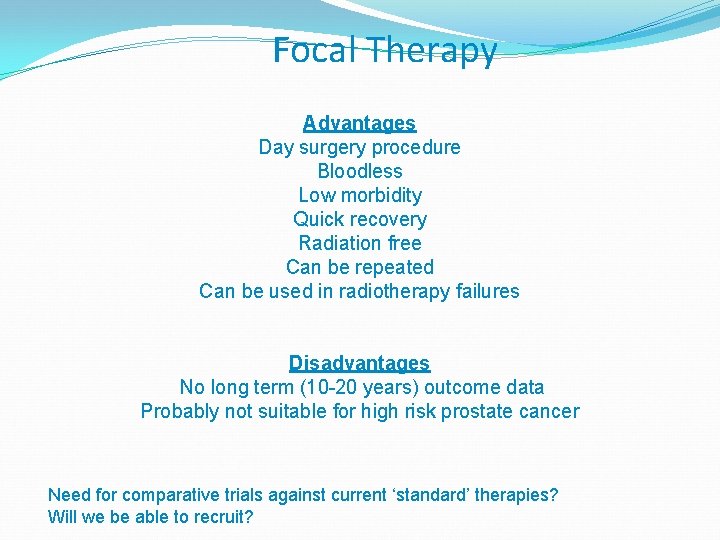
Focal Therapy Advantages Day surgery procedure Bloodless Low morbidity Quick recovery Radiation free Can be repeated Can be used in radiotherapy failures Disadvantages No long term (10 -20 years) outcome data Probably not suitable for high risk prostate cancer Need for comparative trials against current ‘standard’ therapies? Will we be able to recruit?
Prediction Four Prostate cancer is the last cancer in which we insist upon treating the whole organ harbouring the cancer… …Tissue preservation, both active surveillance and focal therapy, will reduce the over-treatment burden of localised disease
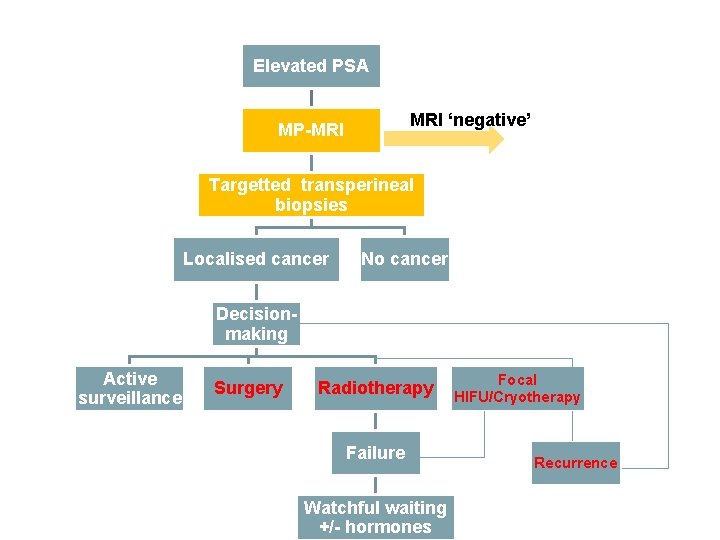
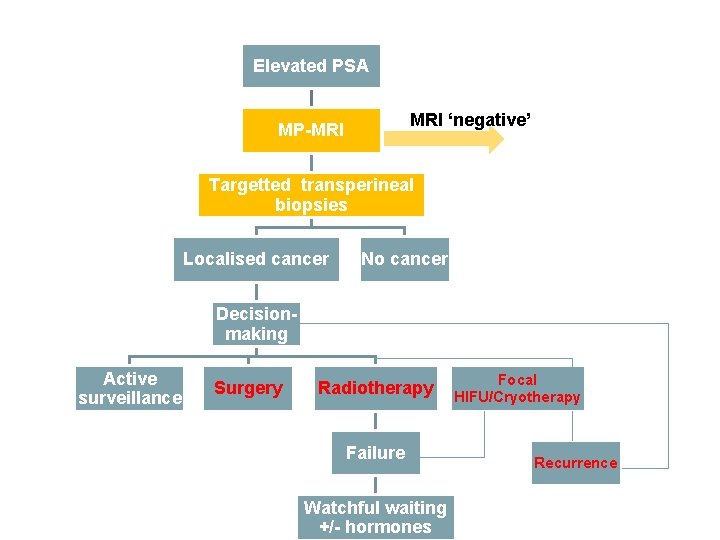
The new pathway…? Elevated PSA MRI ‘negative’ MP-MRI Targetted transperineal biopsies Localised cancer No cancer Decisionmaking Active surveillance Surgery Radiotherapy Failure Watchful waiting +/- hormones Focal HIFU/Cryotherapy Recurrence
 Stephen ko md
Stephen ko md The new prostate cancer infolink
The new prostate cancer infolink Prostate cancer staging
Prostate cancer staging Prostate cancer tnm classification
Prostate cancer tnm classification Mdv3100 prostate cancer
Mdv3100 prostate cancer Espérance de vie après récidive cancer prostate
Espérance de vie après récidive cancer prostate Single cancer pathway
Single cancer pathway Dr. amy ford
Dr. amy ford Optimal lung cancer pathway
Optimal lung cancer pathway Colon cancer pathway
Colon cancer pathway Kitab suci agama hindu
Kitab suci agama hindu Eoss obesity
Eoss obesity @arya ia:http://work4unity.in/haicantik.html
@arya ia:http://work4unity.in/haicantik.html Arya eden
Arya eden Amita arya
Amita arya Arya overweight
Arya overweight Arya kimia
Arya kimia Labial bar indications
Labial bar indications Youtube.com
Youtube.com Indo arya dan dravida
Indo arya dan dravida Arya south asia 46m series 14msinghtechcrunch
Arya south asia 46m series 14msinghtechcrunch Ttp://work4unity.in/haicantik.html
Ttp://work4unity.in/haicantik.html Tindakan menempatkan testes masuk ke scrotum disebut
Tindakan menempatkan testes masuk ke scrotum disebut Prostate pathology
Prostate pathology Prostate
Prostate Testicular artery
Testicular artery Tuip prostate
Tuip prostate Anatomie zonale de mac neal
Anatomie zonale de mac neal Function of the ductus deferens
Function of the ductus deferens Irm prostate
Irm prostate Prostate mri pi rads
Prostate mri pi rads Prostate chapman point
Prostate chapman point Prosted
Prosted Alfazusin
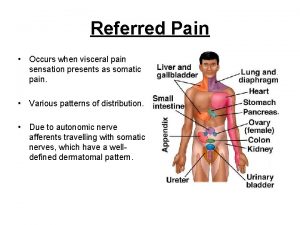
Alfazusin Prostate referred pain
Prostate referred pain Avh prostate
Avh prostate Prostate
Prostate Prostatakreft symptomer
Prostatakreft symptomer Prostate pathology
Prostate pathology Score de gleason
Score de gleason Primary sex organ of the male reproductive system? *
Primary sex organ of the male reproductive system? * Normal weight of prostate
Normal weight of prostate Prostate
Prostate