The ICS CSS Frailty Review What you said

- Slides: 31
The ICS CSS Frailty Review What you said overview! Samantha Gamble ICS CSS Programme Lead November 2019
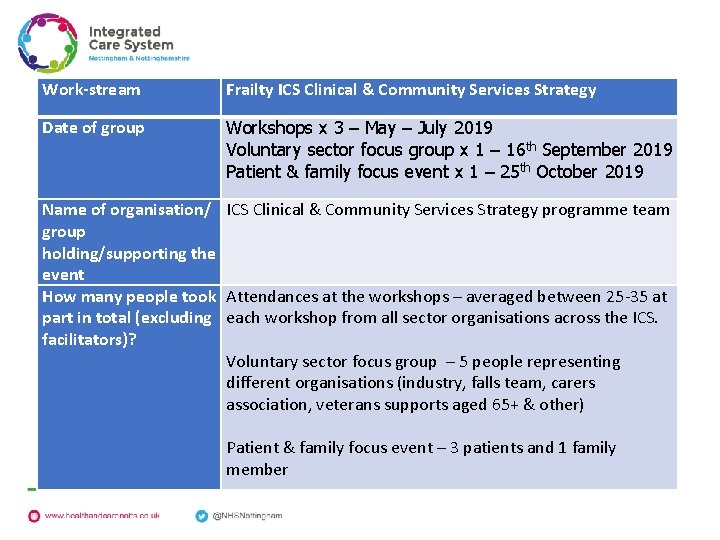
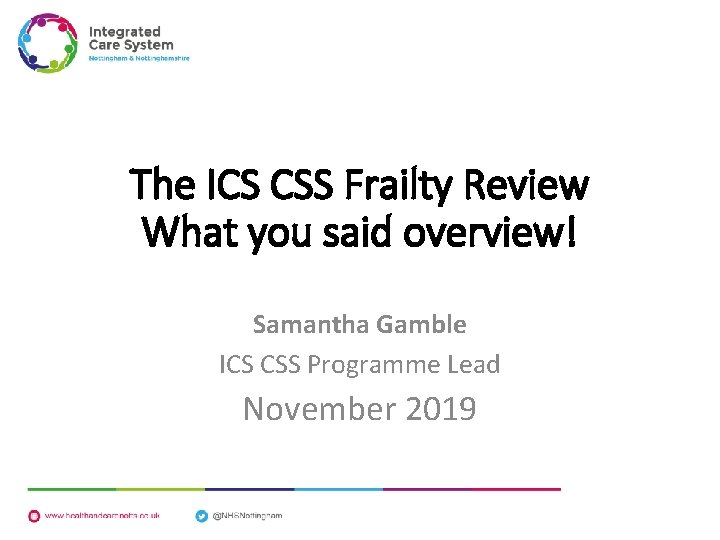
Work-stream Frailty ICS Clinical & Community Services Strategy Date of group Workshops x 3 – May – July 2019 Voluntary sector focus group x 1 – 16 th September 2019 Patient & family focus event x 1 – 25 th October 2019 Name of organisation/ group holding/supporting the event How many people took part in total (excluding facilitators)? ICS Clinical & Community Services Strategy programme team Attendances at the workshops – averaged between 25 -35 at each workshop from all sector organisations across the ICS. Voluntary sector focus group – 5 people representing different organisations (industry, falls team, carers association, veterans supports aged 65+ & other) Patient & family focus event – 3 patients and 1 family member
Frailty ICS CCSS Work stream Workshop 1 23 rd May 2019 Stakeholder Feedback
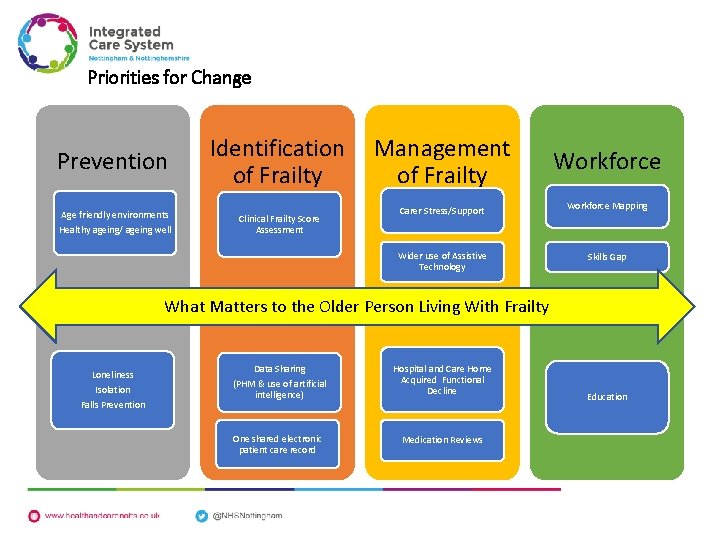
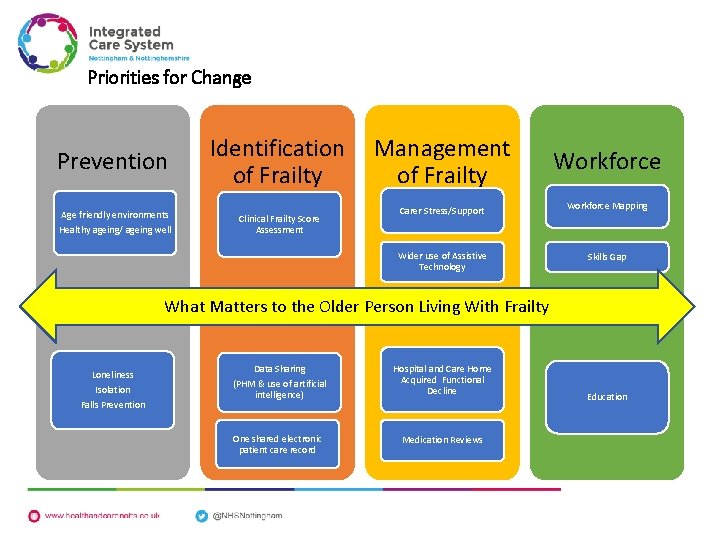
Priorities for Change Prevention Age friendly environments Healthy ageing/ ageing well Identification Management of Frailty Clinical Frailty Score Assessment Workforce Carer Stress/Support Workforce Mapping Wider use of Assistive Technology Skills Gap What Matters to the Older Person Living With Frailty Loneliness Isolation Falls Prevention Data Sharing (PHM & use of artificial intelligence) Hospital and Care Home Acquired Functional Decline One shared electronic patient care record Medication Reviews Education
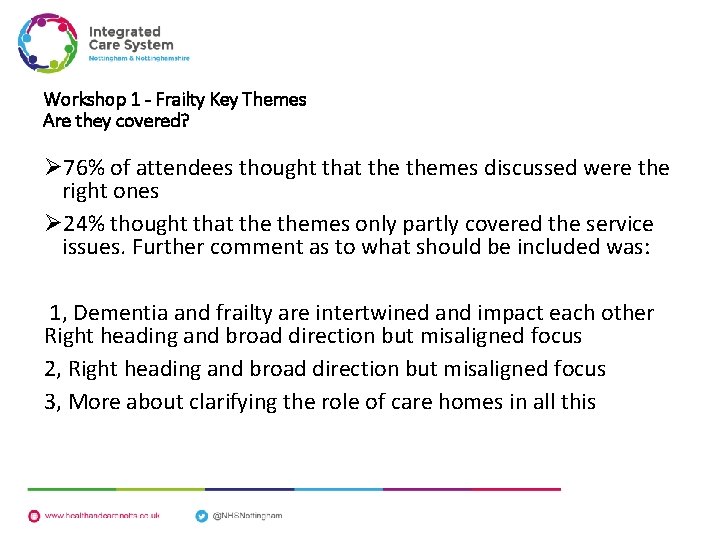
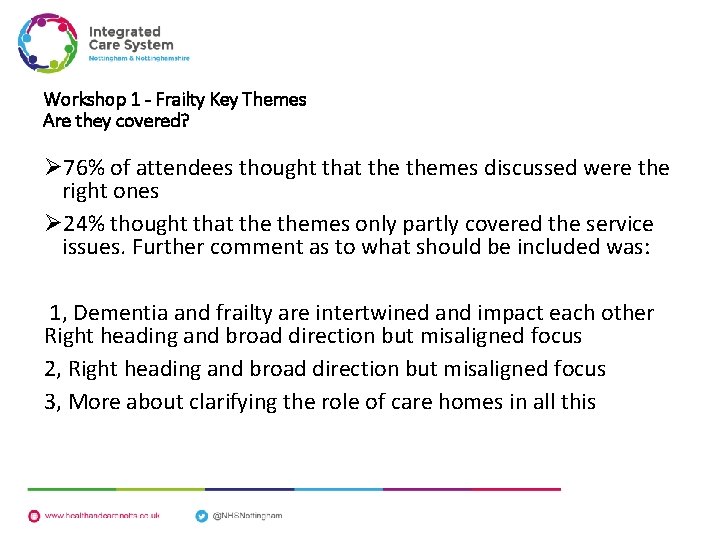
Workshop 1 - Frailty Key Themes Are they covered? Ø 76% of attendees thought that themes discussed were the right ones Ø 24% thought that themes only partly covered the service issues. Further comment as to what should be included was: 1, Dementia and frailty are intertwined and impact each other Right heading and broad direction but misaligned focus 2, Right heading and broad direction but misaligned focus 3, More about clarifying the role of care homes in all this
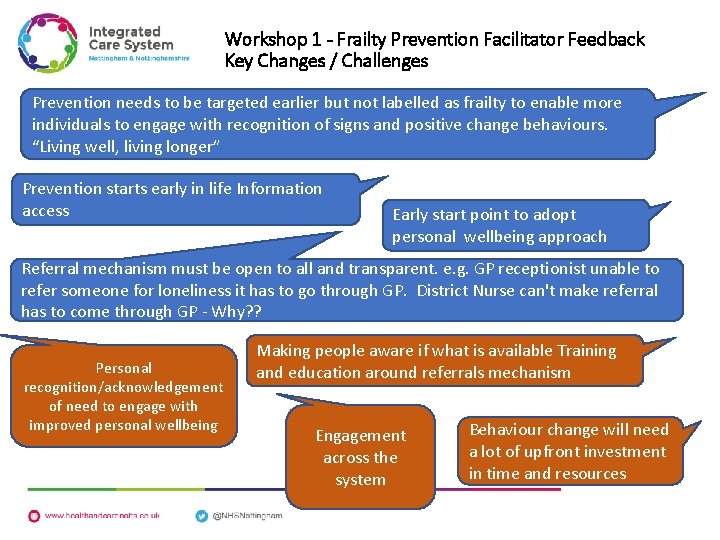
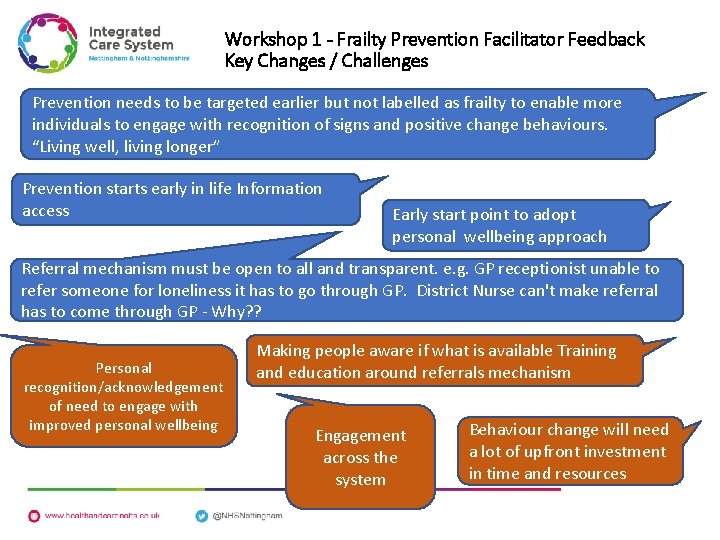
Workshop 1 - Frailty Prevention Facilitator Feedback Key Changes / Challenges Prevention needs to be targeted earlier but not labelled as frailty to enable more individuals to engage with recognition of signs and positive change behaviours. “Living well, living longer” Prevention starts early in life Information access Early start point to adopt personal wellbeing approach Referral mechanism must be open to all and transparent. e. g. GP receptionist unable to refer someone for loneliness it has to go through GP. District Nurse can't make referral has to come through GP - Why? ? Personal recognition/acknowledgement of need to engage with improved personal wellbeing Making people aware if what is available Training and education around referrals mechanism Engagement across the system Behaviour change will need a lot of upfront investment in time and resources
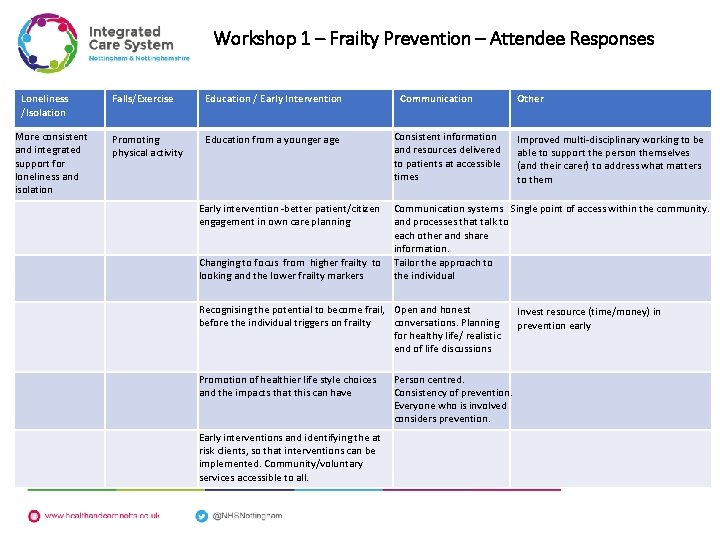
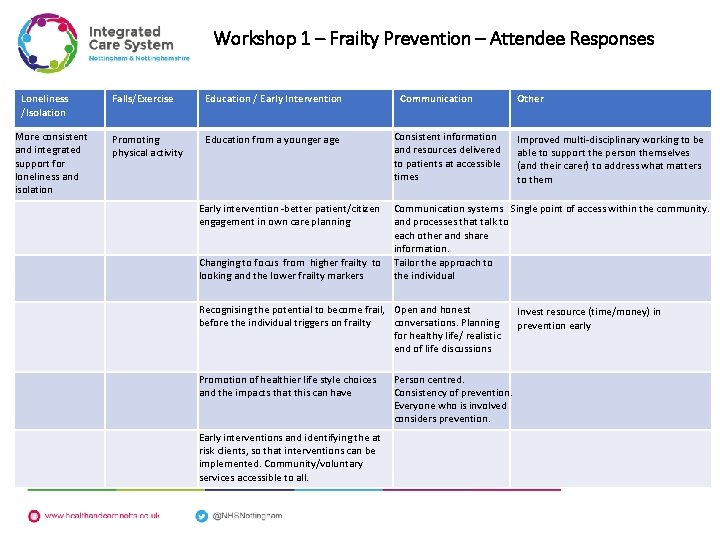
Workshop 1 – Frailty Prevention – Attendee Responses Loneliness /Isolation More consistent and integrated support for loneliness and isolation Falls/Exercise Education / Early Intervention Promoting physical activity Education from a younger age Communication Consistent information and resources delivered to patients at accessible times Other Improved multi-disciplinary working to be able to support the person themselves (and their carer) to address what matters to them Early intervention -better patient/citizen engagement in own care planning Communication systems Single point of access within the community. and processes that talk to each other and share information. Changing to focus from higher frailty to Tailor the approach to looking and the lower frailty markers the individual Recognising the potential to become frail, Open and honest before the individual triggers on frailty conversations. Planning for healthy life/ realistic end of life discussions Promotion of healthier life style choices and the impacts that this can have Early interventions and identifying the at risk clients, so that interventions can be implemented. Community/voluntary services accessible to all. Person centred. Consistency of prevention. Everyone who is involved considers prevention. Invest resource (time/money) in prevention early
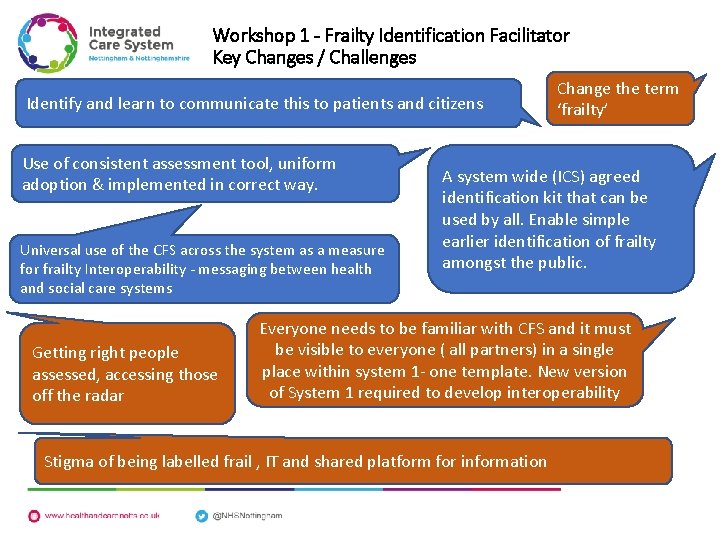
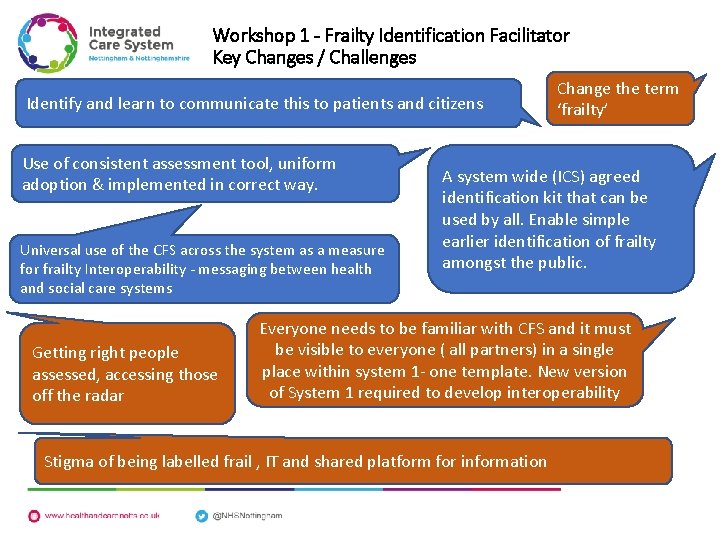
Workshop 1 - Frailty Identification Facilitator Key Changes / Challenges Identify and learn to communicate this to patients and citizens Use of consistent assessment tool, uniform adoption & implemented in correct way. Universal use of the CFS across the system as a measure for frailty Interoperability - messaging between health and social care systems Getting right people assessed, accessing those off the radar Change the term ‘frailty’ A system wide (ICS) agreed identification kit that can be used by all. Enable simple earlier identification of frailty amongst the public. Everyone needs to be familiar with CFS and it must be visible to everyone ( all partners) in a single place within system 1 - one template. New version of System 1 required to develop interoperability Stigma of being labelled frail , IT and shared platform for information
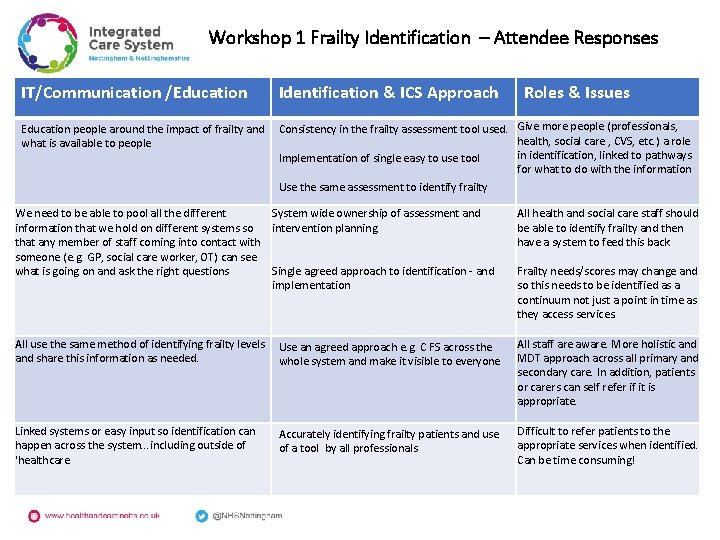
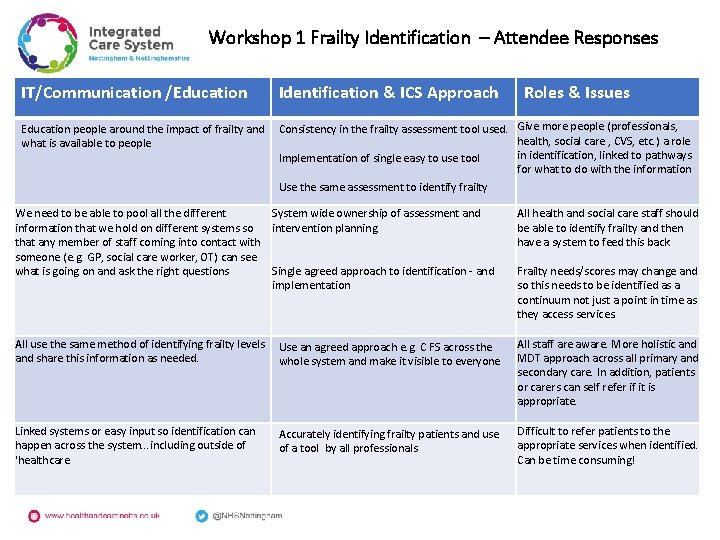
Workshop 1 Frailty Identification – Attendee Responses IT/Communication /Education Identification & ICS Approach Roles & Issues Education people around the impact of frailty and Consistency in the frailty assessment tool used. Give more people (professionals, health, social care , CVS, etc. ) a role what is available to people in identification, linked to pathways Implementation of single easy to use tool for what to do with the information Use the same assessment to identify frailty We need to be able to pool all the different System wide ownership of assessment and information that we hold on different systems so intervention planning that any member of staff coming into contact with someone (e. g. GP, social care worker, OT) can see what is going on and ask the right questions Single agreed approach to identification - and implementation All health and social care staff should be able to identify frailty and then have a system to feed this back. All use the same method of identifying frailty levels Use an agreed approach e. g. C FS across the and share this information as needed. whole system and make it visible to everyone All staff are aware. More holistic and MDT approach across all primary and secondary care. In addition, patients or carers can self refer if it is appropriate. Linked systems or easy input so identification can happen across the system. . . including outside of 'healthcare Difficult to refer patients to the appropriate services when identified. Can be time consuming! Accurately identifying frailty patients and use of a tool by all professionals Frailty needs/scores may change and so this needs to be identified as a continuum not just a point in time as they access services.
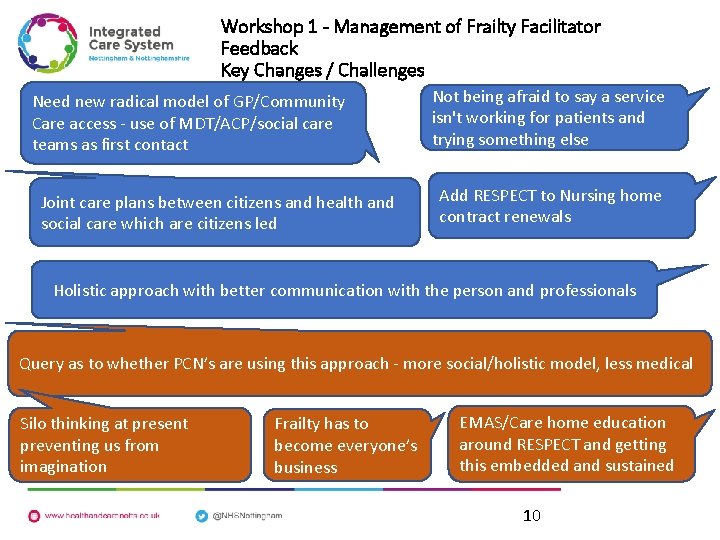
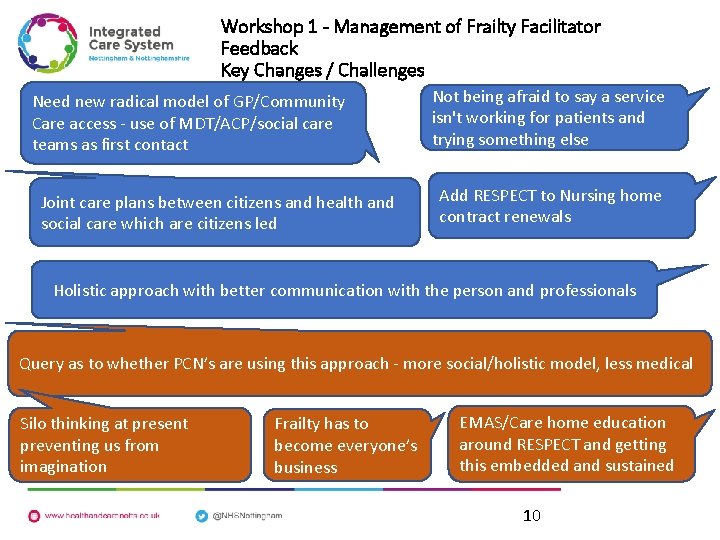
Workshop 1 - Management of Frailty Facilitator Feedback Key Changes / Challenges Need new radical model of GP/Community Care access - use of MDT/ACP/social care teams as first contact Joint care plans between citizens and health and social care which are citizens led Not being afraid to say a service isn't working for patients and trying something else Add RESPECT to Nursing home contract renewals Holistic approach with better communication with the person and professionals Query as to whether PCN’s are using this approach - more social/holistic model, less medical Silo thinking at present preventing us from imagination Frailty has to become everyone’s business EMAS/Care home education around RESPECT and getting this embedded and sustained 10
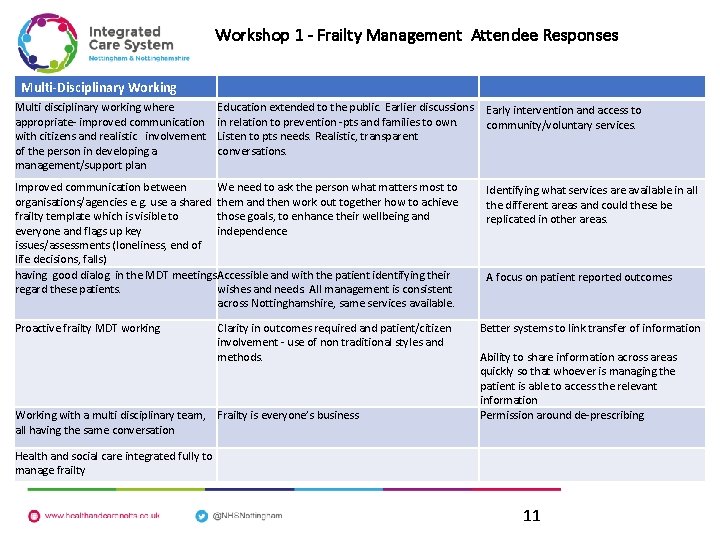
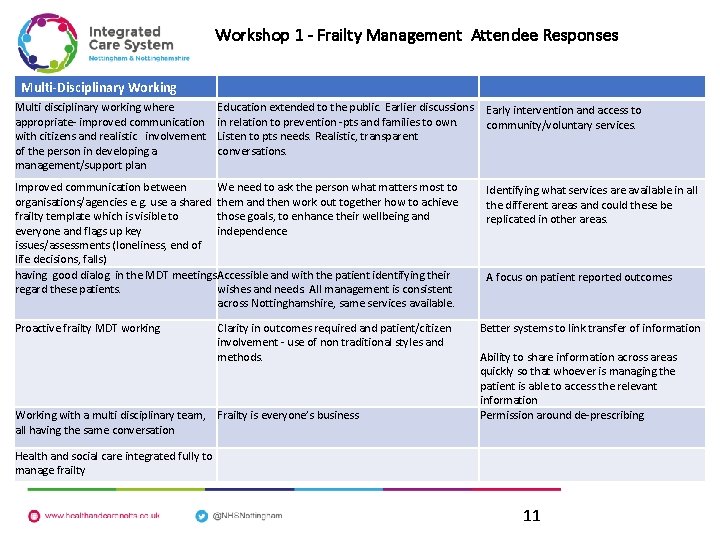
Workshop 1 - Frailty Management Attendee Responses Multi-Disciplinary Working Multi disciplinary working where appropriate- improved communication with citizens and realistic involvement of the person in developing a management/support plan Education extended to the public. Earlier discussions Early intervention and access to in relation to prevention -pts and families to own. community/voluntary services. Listen to pts needs. Realistic, transparent conversations. Improved communication between We need to ask the person what matters most to organisations/agencies e. g. use a shared them and then work out together how to achieve frailty template which is visible to those goals, to enhance their wellbeing and everyone and flags up key independence issues/assessments (loneliness, end of life decisions, falls) having good dialog in the MDT meetings Accessible and with the patient identifying their regard these patients. wishes and needs. All management is consistent across Nottinghamshire, same services available. Proactive frailty MDT working Clarity in outcomes required and patient/citizen involvement - use of non traditional styles and methods. Working with a multi disciplinary team, Frailty is everyone’s business all having the same conversation Identifying what services are available in all the different areas and could these be replicated in other areas. A focus on patient reported outcomes Better systems to link transfer of information Ability to share information across areas quickly so that whoever is managing the patient is able to access the relevant information Permission around de-prescribing Health and social care integrated fully to manage frailty 11
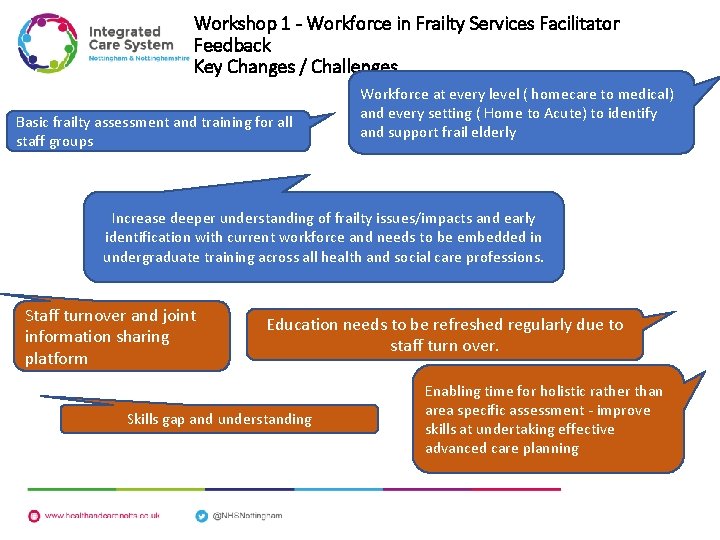
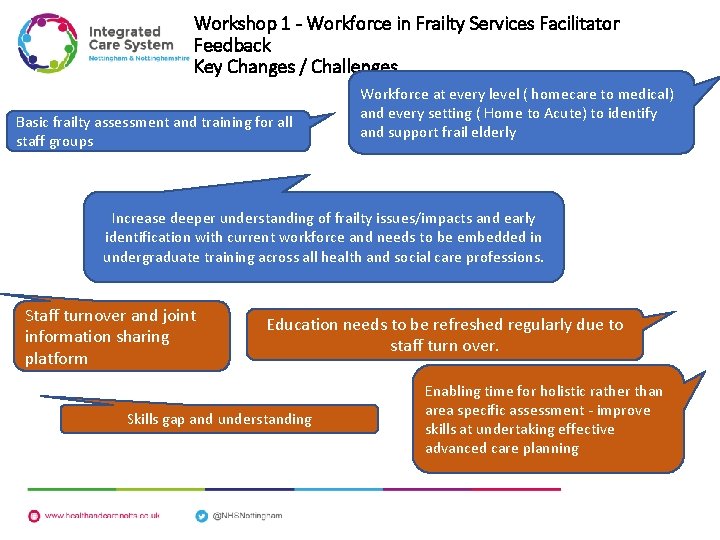
Workshop 1 - Workforce in Frailty Services Facilitator Feedback Key Changes / Challenges Basic frailty assessment and training for all staff groups Workforce at every level ( homecare to medical) and every setting ( Home to Acute) to identify and support frail elderly Increase deeper understanding of frailty issues/impacts and early identification with current workforce and needs to be embedded in undergraduate training across all health and social care professions. Staff turnover and joint information sharing platform Education needs to be refreshed regularly due to staff turn over. Skills gap and understanding Enabling time for holistic rather than area specific assessment - improve skills at undertaking effective advanced care planning
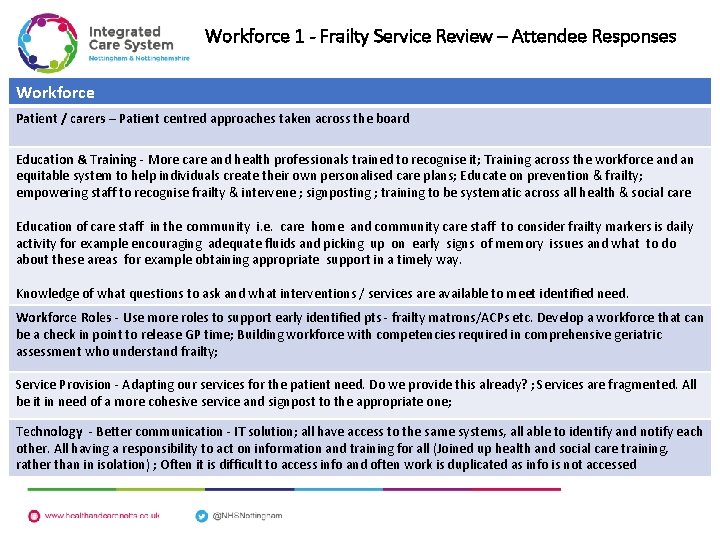
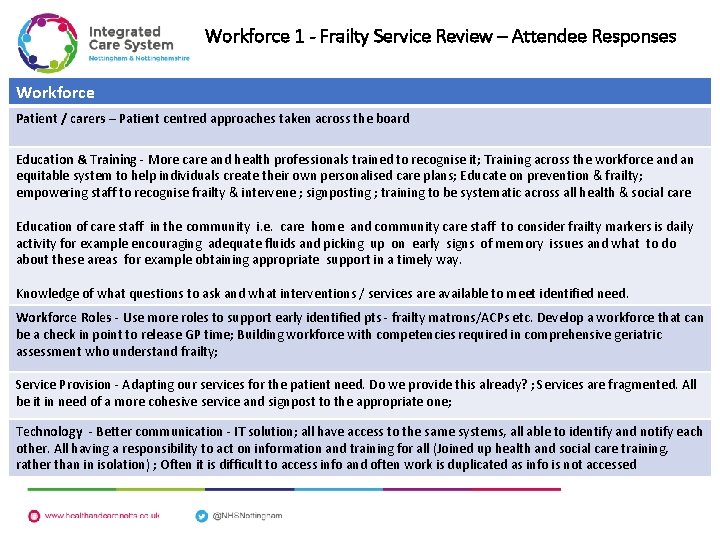
Workforce 1 - Frailty Service Review – Attendee Responses Workforce Patient / carers – Patient centred approaches taken across the board Education & Training - More care and health professionals trained to recognise it; Training across the workforce and an equitable system to help individuals create their own personalised care plans; Educate on prevention & frailty; empowering staff to recognise frailty & intervene ; signposting ; training to be systematic across all health & social care Education of care staff in the community i. e. care home and community care staff to consider frailty markers is daily activity for example encouraging adequate fluids and picking up on early signs of memory issues and what to do about these areas for example obtaining appropriate support in a timely way. Knowledge of what questions to ask and what interventions / services are available to meet identified need. Workforce Roles - Use more roles to support early identified pts - frailty matrons/ACPs etc. Develop a workforce that can be a check in point to release GP time; Building workforce with competencies required in comprehensive geriatric assessment who understand frailty; Service Provision - Adapting our services for the patient need. Do we provide this already? ; Services are fragmented. All be it in need of a more cohesive service and signpost to the appropriate one; Technology - Better communication - IT solution; all have access to the same systems, all able to identify and notify each other. All having a responsibility to act on information and training for all (Joined up health and social care training, rather than in isolation) ; Often it is difficult to access info and often work is duplicated as info is not accessed
Frailty ICS CCSS Work stream Workshop 2 10 th July 2019 Stakeholder Feedback
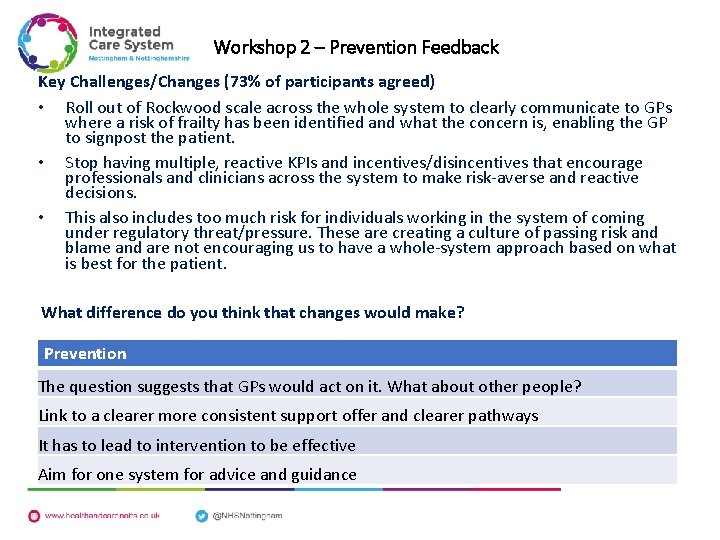
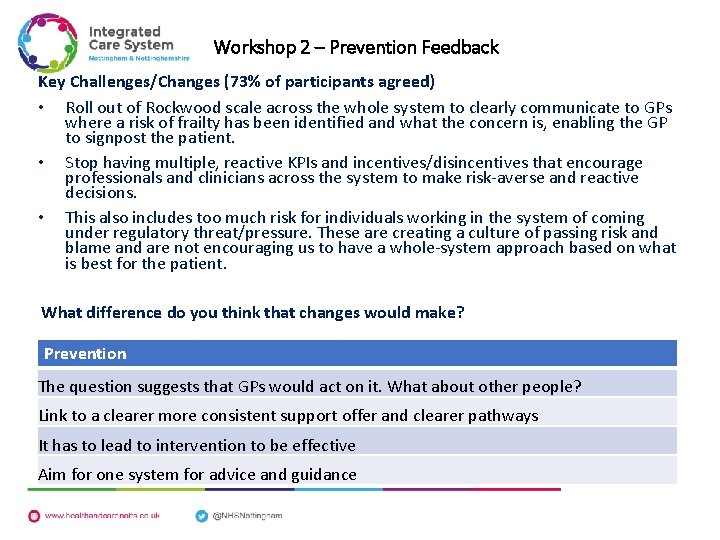
Workshop 2 – Prevention Feedback Key Challenges/Changes (73% of participants agreed) • Roll out of Rockwood scale across the whole system to clearly communicate to GPs where a risk of frailty has been identified and what the concern is, enabling the GP to signpost the patient. • Stop having multiple, reactive KPIs and incentives/disincentives that encourage professionals and clinicians across the system to make risk-averse and reactive decisions. • This also includes too much risk for individuals working in the system of coming under regulatory threat/pressure. These are creating a culture of passing risk and blame and are not encouraging us to have a whole-system approach based on what is best for the patient. What difference do you think that changes would make? Prevention The question suggests that GPs would act on it. What about other people? Link to a clearer more consistent support offer and clearer pathways It has to lead to intervention to be effective Aim for one system for advice and guidance
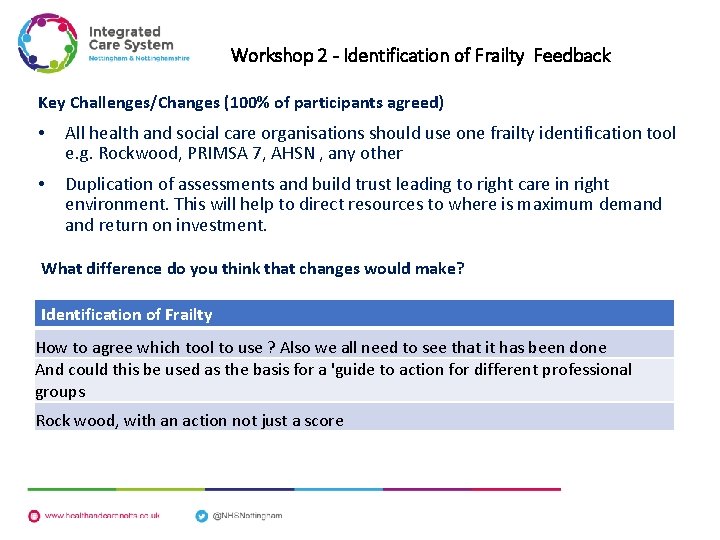
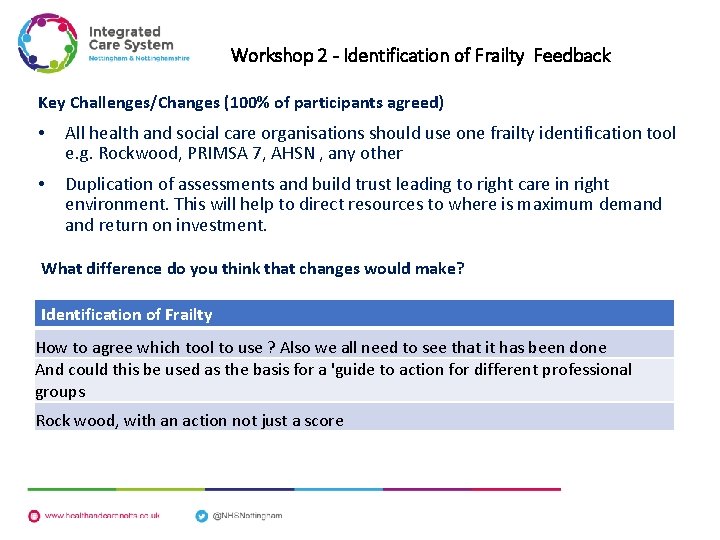
Workshop 2 - Identification of Frailty Feedback Key Challenges/Changes (100% of participants agreed) • All health and social care organisations should use one frailty identification tool e. g. Rockwood, PRIMSA 7, AHSN , any other • Duplication of assessments and build trust leading to right care in right environment. This will help to direct resources to where is maximum demand return on investment. What difference do you think that changes would make? Identification of Frailty How to agree which tool to use ? Also we all need to see that it has been done And could this be used as the basis for a 'guide to action for different professional groups Rock wood, with an action not just a score
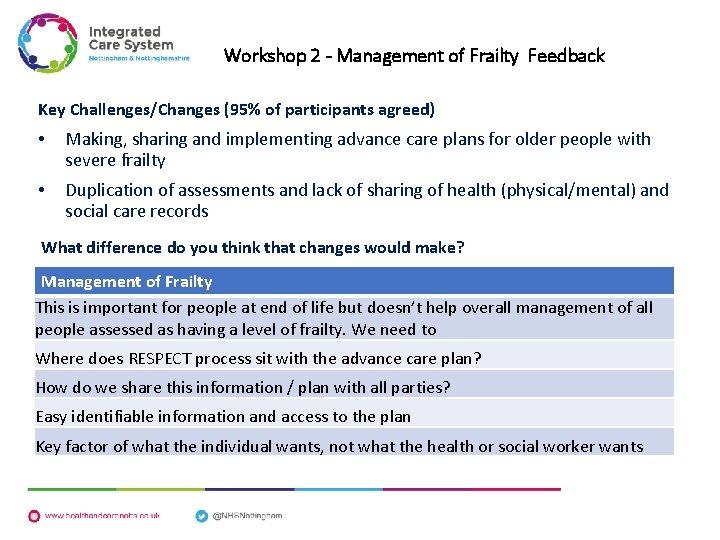
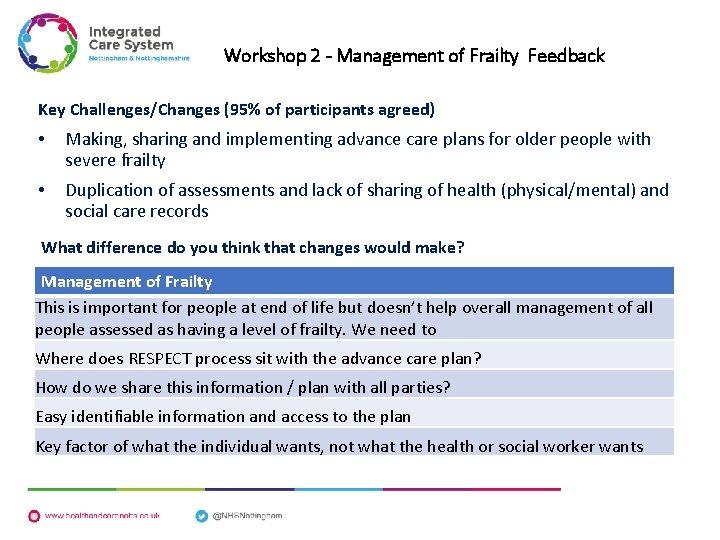
Workshop 2 - Management of Frailty Feedback Key Challenges/Changes (95% of participants agreed) • Making, sharing and implementing advance care plans for older people with severe frailty • Duplication of assessments and lack of sharing of health (physical/mental) and social care records What difference do you think that changes would make? Management of Frailty This is important for people at end of life but doesn’t help overall management of all people assessed as having a level of frailty. We need to Where does RESPECT process sit with the advance care plan? How do we share this information / plan with all parties? Easy identifiable information and access to the plan Key factor of what the individual wants, not what the health or social worker wants
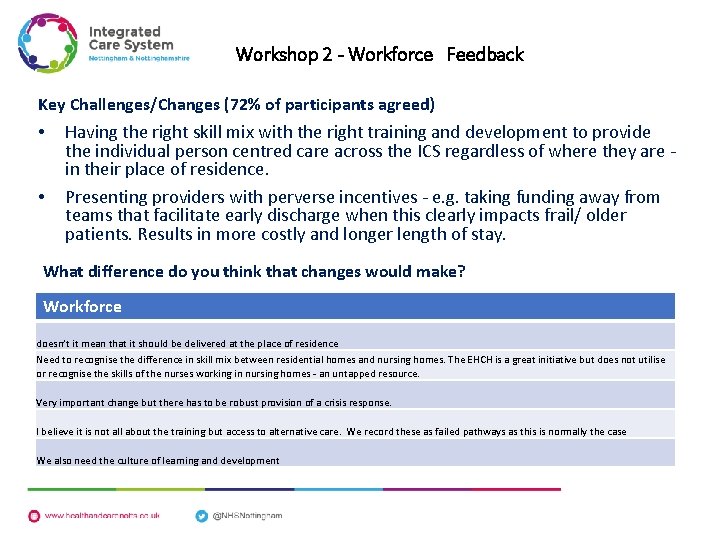
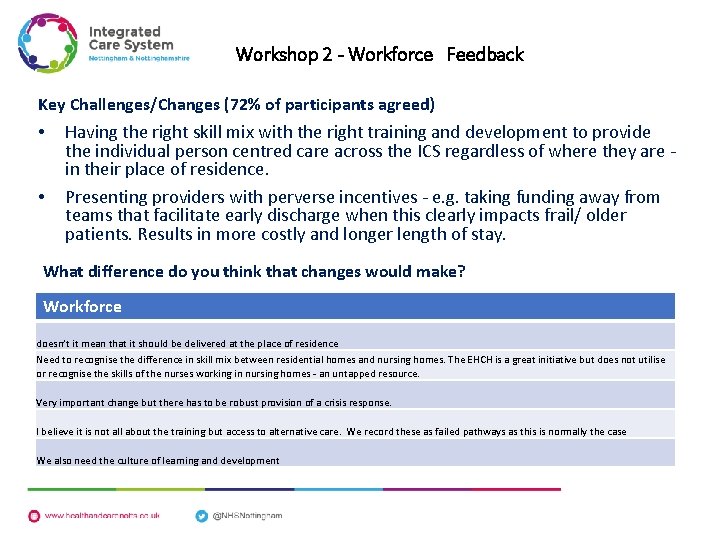
Workshop 2 - Workforce Feedback Key Challenges/Changes (72% of participants agreed) • • Having the right skill mix with the right training and development to provide the individual person centred care across the ICS regardless of where they are - in their place of residence. Presenting providers with perverse incentives - e. g. taking funding away from teams that facilitate early discharge when this clearly impacts frail/ older patients. Results in more costly and longer length of stay. What difference do you think that changes would make? Workforce doesn’t it mean that it should be delivered at the place of residence Need to recognise the difference in skill mix between residential homes and nursing homes. The EHCH is a great initiative but does not utilise or recognise the skills of the nurses working in nursing homes - an untapped resource. Very important change but there has to be robust provision of a crisis response. I believe it is not all about the training but access to alternative care. We record these as failed pathways as this is normally the case We also need the culture of learning and development
Frailty ICS CCSS Work stream Voluntary Sector Focus Group Feedback 16 th September 2019
Question: What works best in identifying and engaging people who are frail or at risk of becoming frail? Individuals/ patients : • Being supported to having self-motivation to change their behaviours in reducing frailty • Being supported to self-identify their own loss of ability. • Being supported to see frailty prevention as an issue of promoting wellbeing rather than of treating illness. • The fear around acknowledging loss of ability for individuals is linked to concern for their independence : being encouraged to see that discussing, planning and following measures for maintaining and improving physical ability can help retain their independence is a vital part of gaining their “buy – in. ”
Question: What works best in identifying and engaging people who are frail or at risk of becoming frail? Health Professionals : • Being aware of the impact of becoming frail on individuals’ self-esteem and selfimage • Understanding individual motivation to change behaviours ( which varies between individuals) • Taking a person-centred approach to supporting individuals • Being aware of the sensitivity for individuals of acknowledging that their level of ability is declining: having the skills to facilitate sometimes difficult conversations • Checking individuals’ understanding of terms used in frailty risk reduction (e. g. , “improved muscle strength”) • Education and training around recognising the early indicators of declining physical ability (this for non-health personnel too – e. g. delivery workers, meals at home staff etc. ) • Effective communication between all agencies working in the community: ensuring that staff know where to refer a concern about a person showing signs of frailty.
Question: What works best in identifying and engaging people who are frail or at risk of becoming frail? The Public Health Structure: • Having a national Frailty Ambassador and Frailty Champions • Predictive prevention/analytics to identify trends and target campaign messages • Accessing the insights from existing initiatives and research (e. g. a pilot in • • • Nottingham involving CPSOs and the Carers Federation): do ROSPA, Age UK, the Osteoporosis Society etc. have any relevant data? Addressing issues of capacity for responding to referrals (e. g. GPs now hold a significantly larger caseload than a decade ago). Recognising that the return on measures implemented to reduce frailty is something to be measured over the longer term (rather than expecting short – term gains) Prevention through investing to save in community services. Understanding the strong link between the risk of frailty and being socially isolated: measures to reduce the risk of frailty should be targeted to individuals who are socially isolated. Taking a more holistic approach to approaches promoting the reduction of frailty risk: using flu clinics or “well man/ women” as an opportunity to assess for signs of frailty (e. g. grip strength test)
Question: What works best in identifying and engaging people who are frail or at risk of becoming frail? Society: • Being able to discuss frailty (which is an inevitable aspect of the ageing process) more openly: there is a similar taboo around having conversations about it as there around death and dying • Changing the expectations many individuals have that the NHS can and will “fix” everything: promoting a greater emphasis on self-care and self-management.
Question: How can services best support people who are frail and those at risk of becoming frail? Individuals/ patients: • Being encouraged to talk about their levels of ability on and in their own terms • More likely to engage with frailty services where they have had an input • Being given an overview of how services fit together (areas of responsibility etc. ) • Being aware of a wider focus on frailty prevention might encourage them to initiate conversations about their own ability levels (or to be more amenable to health professionals doing so). • Having a local culture of knowing and talking to neighbours in a local community.
Question: How can services best support people who are frail and those at risk of becoming frail? Health Professionals : • Linking with social care domiciliary services to provide advice on healthy eating, hydration and nutrition. • Tailoring the frailty prevention message to meet the communication needs of different groups and individuals • Having a single portal to coordinate the response to frailty concerns. • Encouraging younger people to access health checks for muscle mass
How can services best support people who are frail and those at risk of becoming frail? The Public Health Structure: • The focus of measures which address the risk of frailty should be centred around nutrition as well as exercise • Early intervention is vital to frailty prevention • Encouraging employers to promote a healthier lifestyle would be effective: activities and sessions offered in the workplace would be easier / more convenient for people to attend. • Using workplace redundancy/ retirement information events at work as a forum for promoting frailty awareness. • Recognising frailty awareness and prevention as a prime potential of the new, more formalised approach to social prescribing (Link Worker role etc. ) • Including Link Workers in training for making frailty assessments. • Clarifying the part the PCNs will have in frailty services: recognising the importance of detailed local knowledge. • Ensuring that any new initiative is aligned with existing delivery systems (e. g. Making Every Contact Count).
Question: How can services best support people who are frail and those at risk of becoming frail? Society: • Identifying frailty is everyone’s business
Frailty ICS CCSS Work stream Patient & Family Focus Group Feedback 11 th October 2019
Patient & Family Focus Group Feedback Citizen experience 1: • Lady reliant on buses which aren’t regular enough – transport is key • Felt that she was not in the right independent living care facilities to meet her needs • Frequently had days where she sees no one ‘felt very lonely’ • Used to have a friend that worked in the home that visited each day for a short time and this made the world of difference to her • The home have previously put on activities but there was only her and another lady that would go to them as there was a lack of interest from other residents • Unaware of all the homes available in the area it was felt that when there was a need to move into a home following a crisis that a quick decision is made without necessarily being aware of the facilities in the area – lack of information • Family support was really important but they were unable to visit every day.

Patient & Family Focus Group Feedback Citizen experience 2: • A Gentleman looking at various independent living facilities as he has lost his wife and his health is deteriorating and he ‘feels very lonely’ and found it hard to engage with others • Support was provided by a named council placement officer to visit different living facilities and help with finances– this was viewed as very positive as he had did not know what financial support he was entitled to claim • He could still drive he felt that this offered him more independence and was less concerned with bus routes. • Since the death of his wife he became very lonely to the point that he’s visited his GP with suicidal feelings due to loneliness • He had tried computer clubs to learn how to use a computer which has helped him engage with his family • Family support was intermittent and he felt that this contributed to his feelings of loneliness • He wished to access independent living facilities knowing he could access support as he needed to e. g. support manager, group sessions , trips out and increased daily interactions
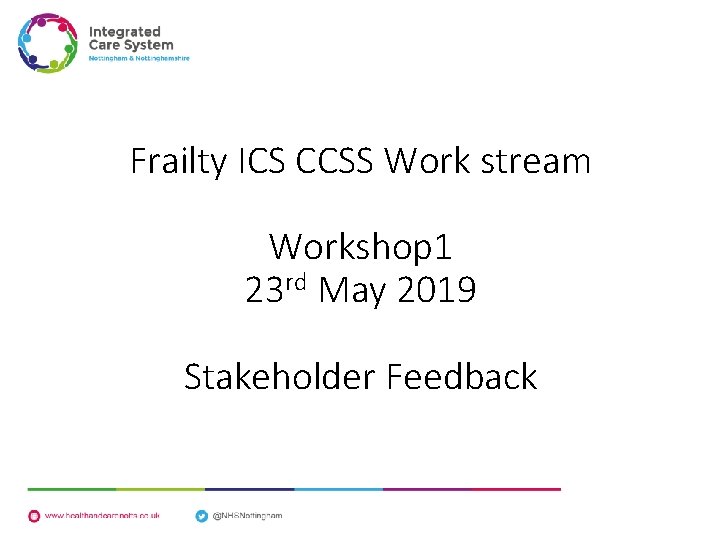
Support Manager Experience There was a frustration regarding the facilities provided for people to promote independent living such as : • Mobility scooters not being allowed in the corridors of the independent living area’s as they are deemed to be a trip hazard to other residents or the corridors were deemed as too narrow • There was no provision to charge scooters in or outside of the building • The gradient of the slope from the facilities to the local shops, GP practice etc. and a lack of use of scooters left unoccupied flats. • There were two floors of flats available but many on the second floor were unoccupied as there was no lift available. • There was no WI FI available for residents to use (no future proof for future generations) • There was no communal TV as a licence needed to be paid
 Complex incident
Complex incident Frailty thy name is woman
Frailty thy name is woman Hamlet baroque
Hamlet baroque Geriatric syndrome
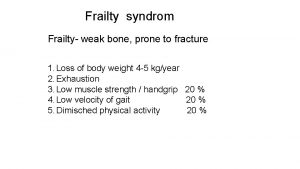
Geriatric syndrome Fried score frailty
Fried score frailty Rockwood frailty index
Rockwood frailty index Frailty score
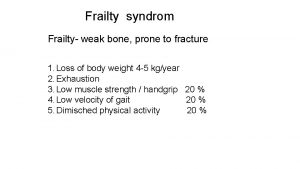
Frailty score Frailty syndrom
Frailty syndrom Think said the robin
Think said the robin Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Slidetodoc
Slidetodoc Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Thang điểm glasgow
Thang điểm glasgow Chúa yêu trần thế
Chúa yêu trần thế Các môn thể thao bắt đầu bằng tiếng nhảy
Các môn thể thao bắt đầu bằng tiếng nhảy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Phép trừ bù
Phép trừ bù Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng xinh xinh thế chỉ nói điều hay thôi
Cái miệng xinh xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ