The child with respiratory Alteration Lecture 3 Part
- Slides: 40
The child with respiratory Alteration Lecture 3, Part one
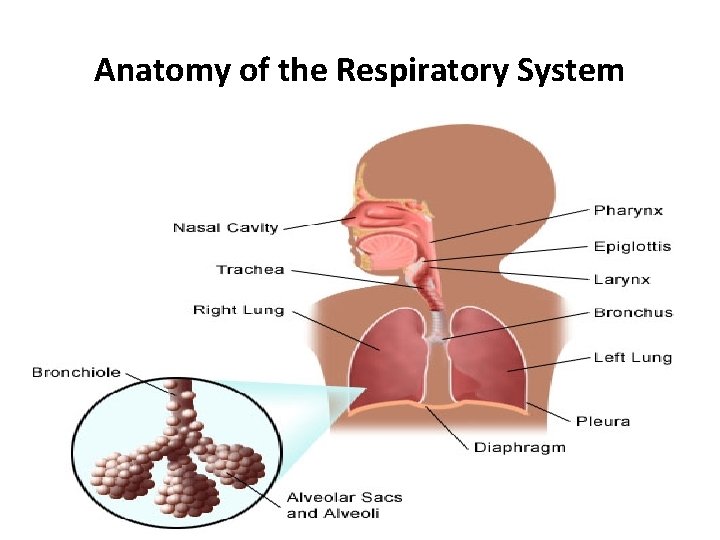
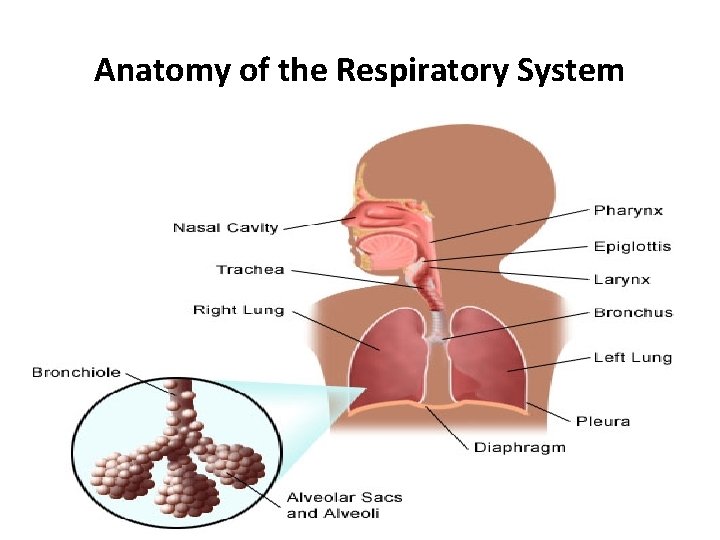
Anatomy of the Respiratory System 04/12/2020 2
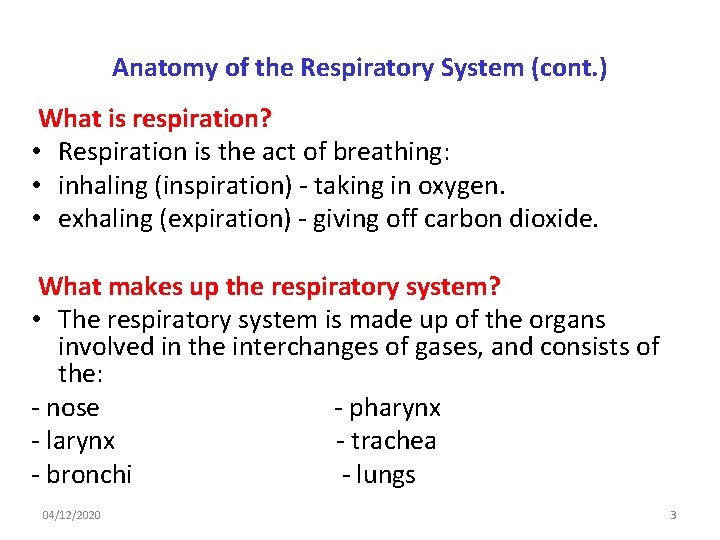
Anatomy of the Respiratory System (cont. ) What is respiration? • Respiration is the act of breathing: • inhaling (inspiration) - taking in oxygen. • exhaling (expiration) - giving off carbon dioxide. What makes up the respiratory system? • The respiratory system is made up of the organs involved in the interchanges of gases, and consists of the: - nose - pharynx - larynx - trachea - bronchi - lungs 04/12/2020 3
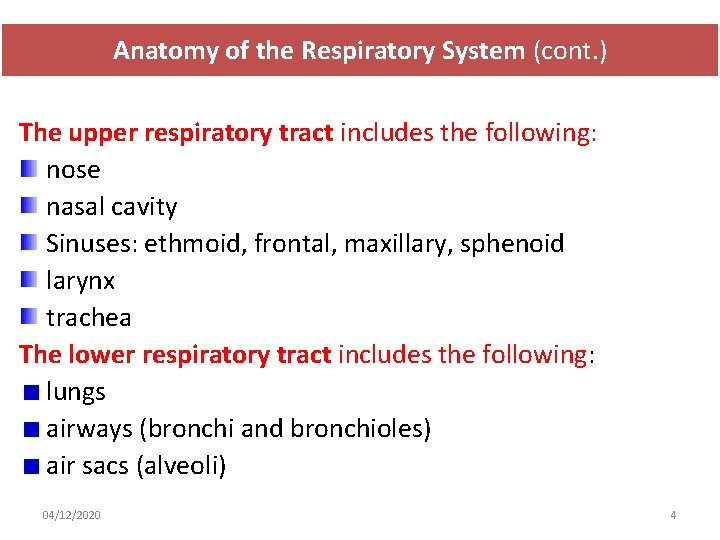
Anatomy of the Respiratory System (cont. ) The upper respiratory tract includes the following: nose nasal cavity Sinuses: ethmoid, frontal, maxillary, sphenoid larynx trachea The lower respiratory tract includes the following: lungs airways (bronchi and bronchioles) air sacs (alveoli) 04/12/2020 4
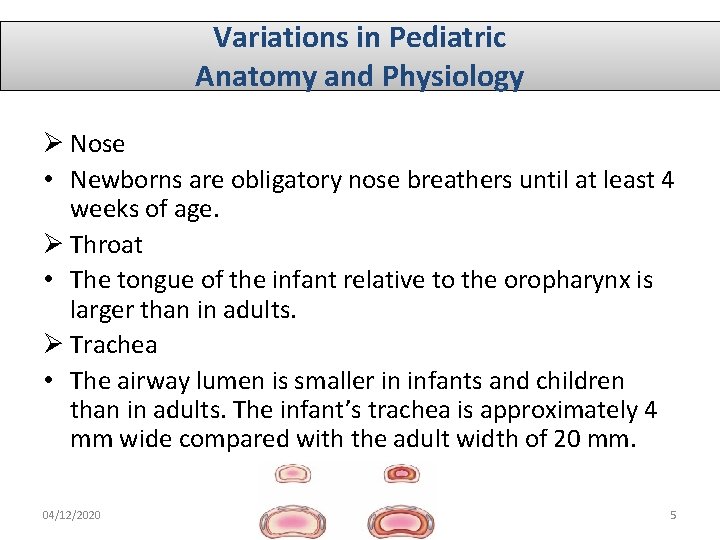
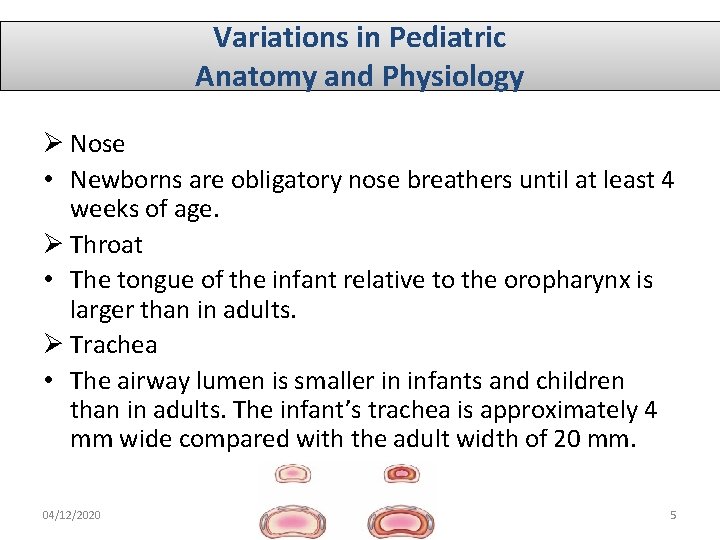
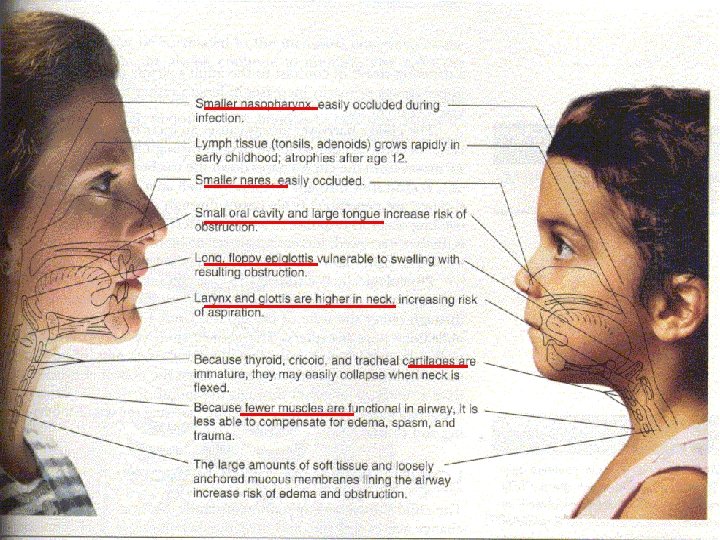
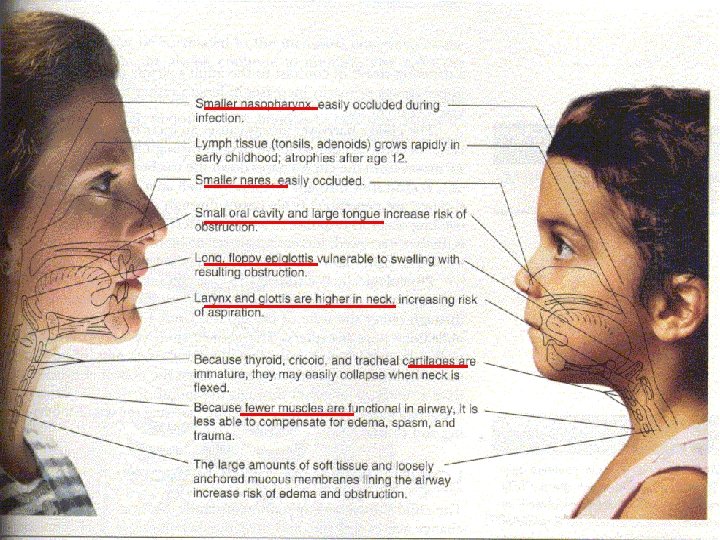
Variations in Pediatric Anatomy and Physiology Ø Nose • Newborns are obligatory nose breathers until at least 4 weeks of age. Ø Throat • The tongue of the infant relative to the oropharynx is larger than in adults. Ø Trachea • The airway lumen is smaller in infants and children than in adults. The infant’s trachea is approximately 4 mm wide compared with the adult width of 20 mm. 04/12/2020 5
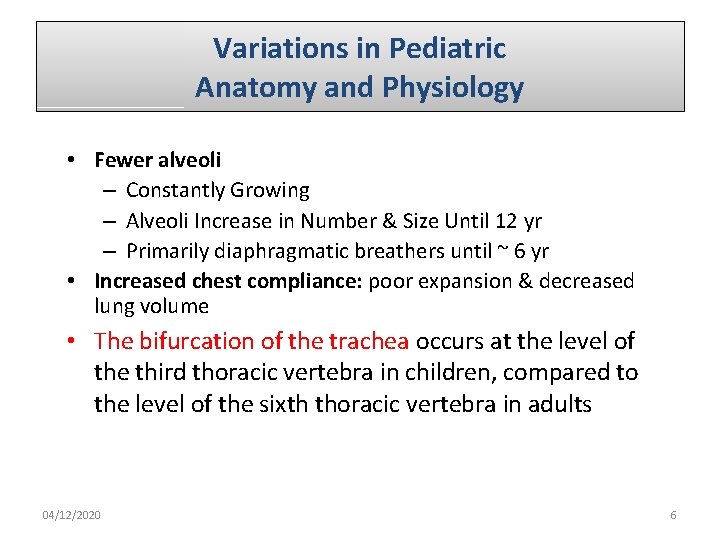
Variations in Pediatric Anatomy and Physiology • Fewer alveoli – Constantly Growing – Alveoli Increase in Number & Size Until 12 yr – Primarily diaphragmatic breathers until ~ 6 yr • Increased chest compliance: poor expansion & decreased lung volume • The bifurcation of the trachea occurs at the level of the third thoracic vertebra in children, compared to the level of the sixth thoracic vertebra in adults 04/12/2020 6
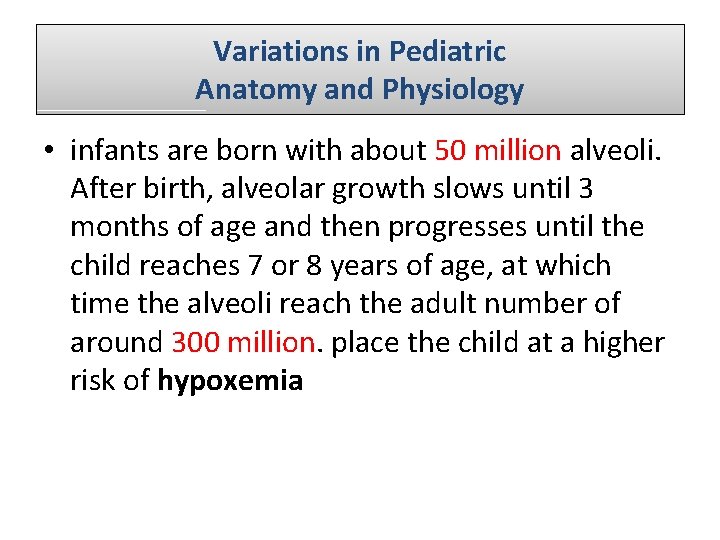
Variations in Pediatric Anatomy and Physiology • infants are born with about 50 million alveoli. After birth, alveolar growth slows until 3 months of age and then progresses until the child reaches 7 or 8 years of age, at which time the alveoli reach the adult number of around 300 million. place the child at a higher risk of hypoxemia
04/12/2020 8
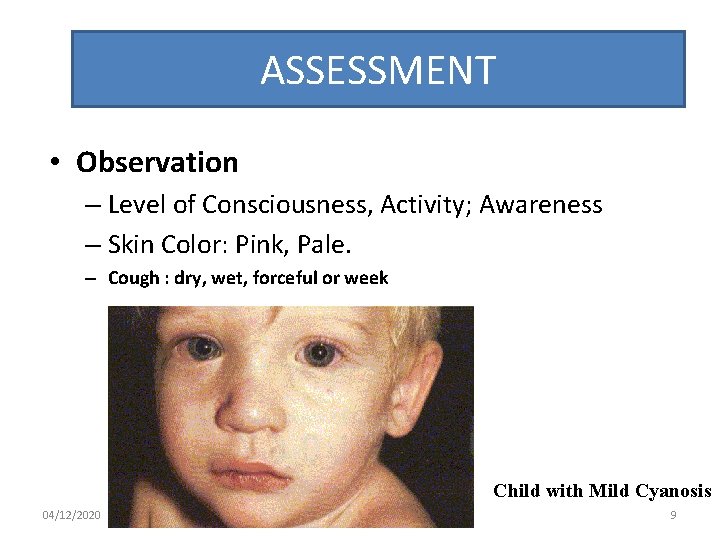
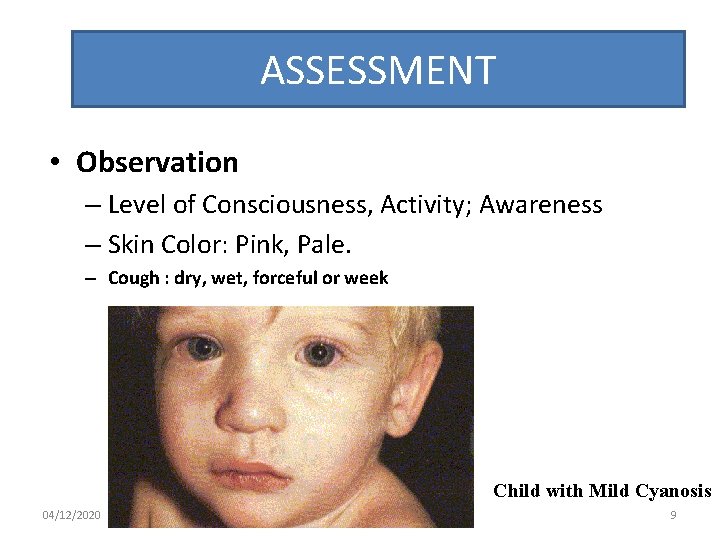
ASSESSMENT • Observation – Level of Consciousness, Activity; Awareness – Skin Color: Pink, Pale. – Cough : dry, wet, forceful or week Child with Mild Cyanosis 04/12/2020 9
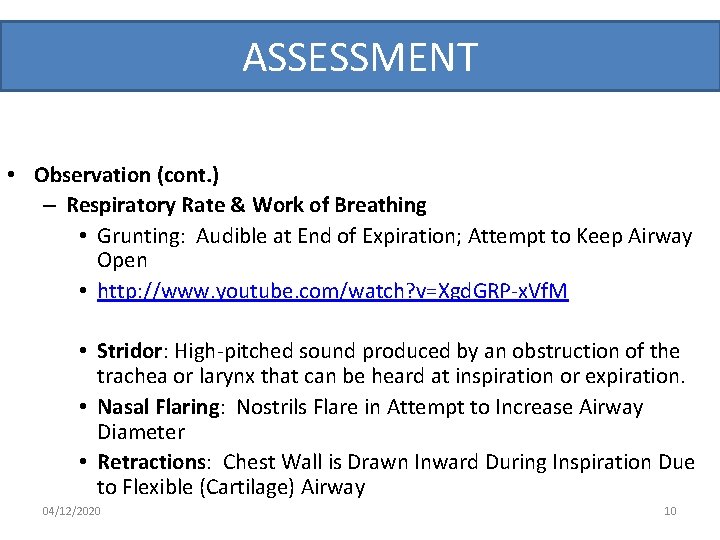
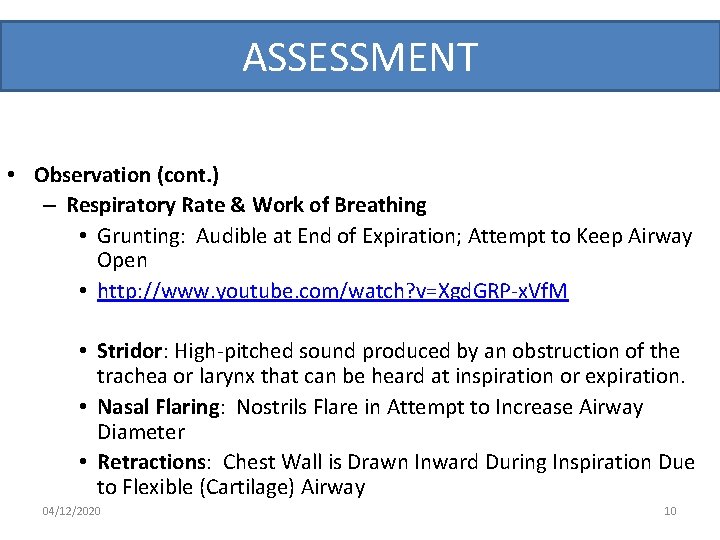
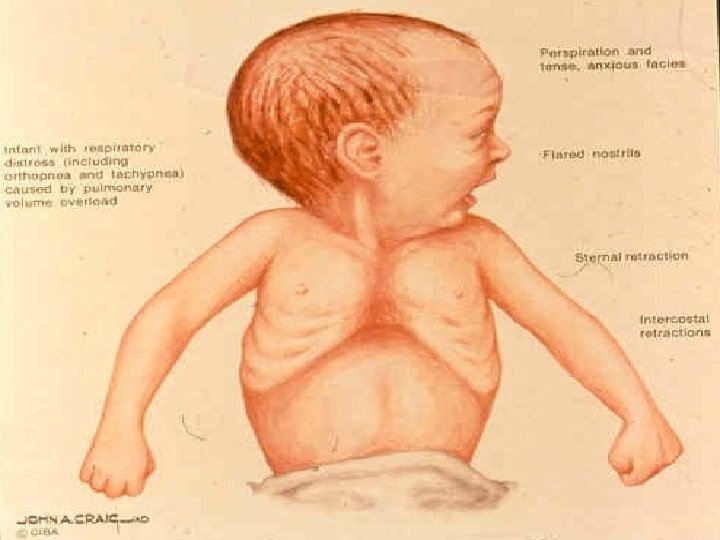
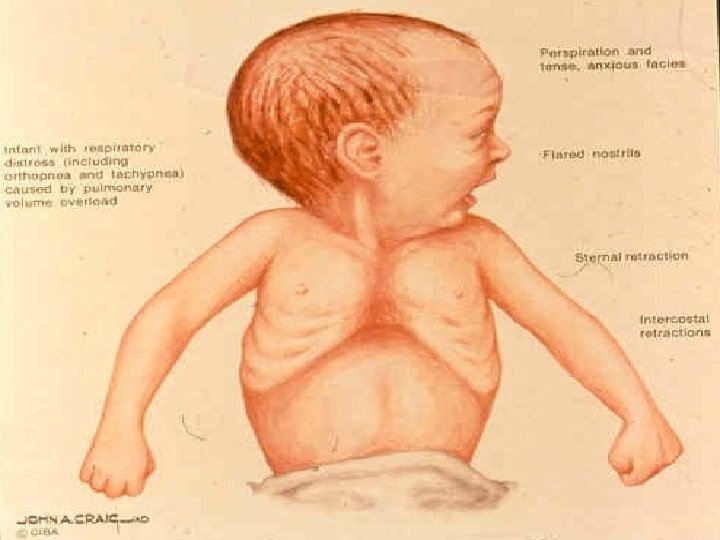
ASSESSMENT • Observation (cont. ) – Respiratory Rate & Work of Breathing • Grunting: Audible at End of Expiration; Attempt to Keep Airway Open • http: //www. youtube. com/watch? v=Xgd. GRP-x. Vf. M • Stridor: High-pitched sound produced by an obstruction of the trachea or larynx that can be heard at inspiration or expiration. • Nasal Flaring: Nostrils Flare in Attempt to Increase Airway Diameter • Retractions: Chest Wall is Drawn Inward During Inspiration Due to Flexible (Cartilage) Airway 04/12/2020 10
04/12/2020 11
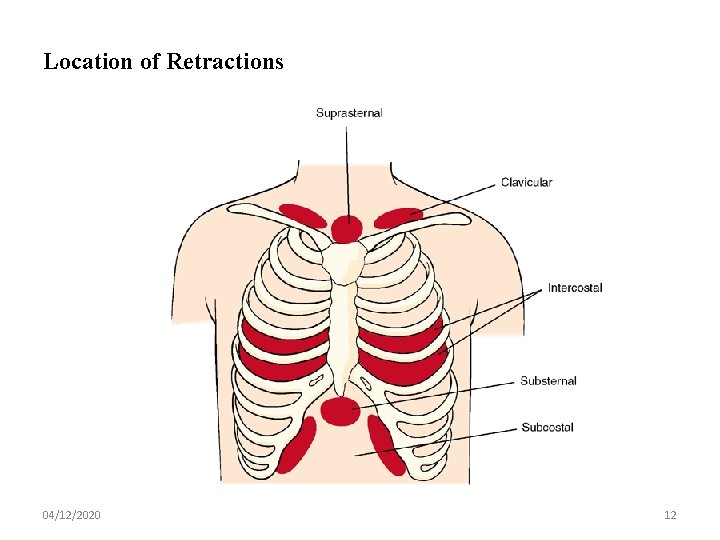
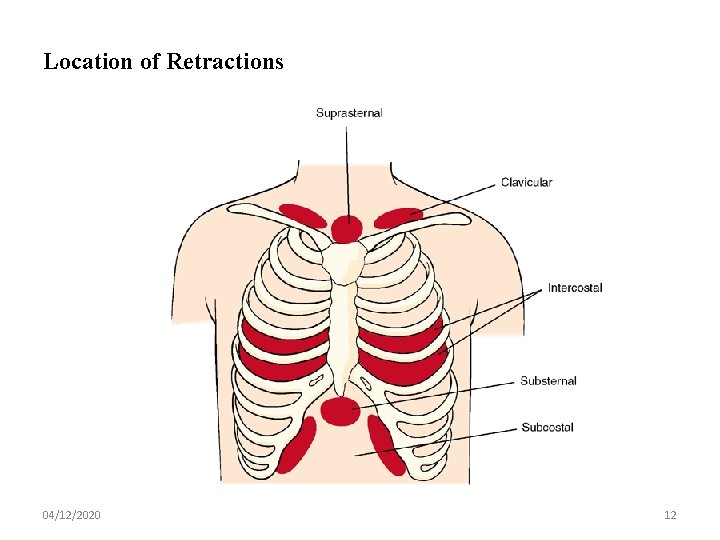
Location of Retractions 04/12/2020 12
ASSESSMENT • Auscultation – CRACKLES: Coarse or Fine; Related to Fluid in Airway (Pneumonia, CHF) – WHEEZES: Musical Sound Related to Turbulent Airflow in Constricted Airway (Asthma) • DESCRIBE Location of Retractions & Adventitious Airway Sounds; Use LANDMARKS 04/12/2020 13
UPPER RESPIRATORY TRACT INFECTION 04/12/2020 14
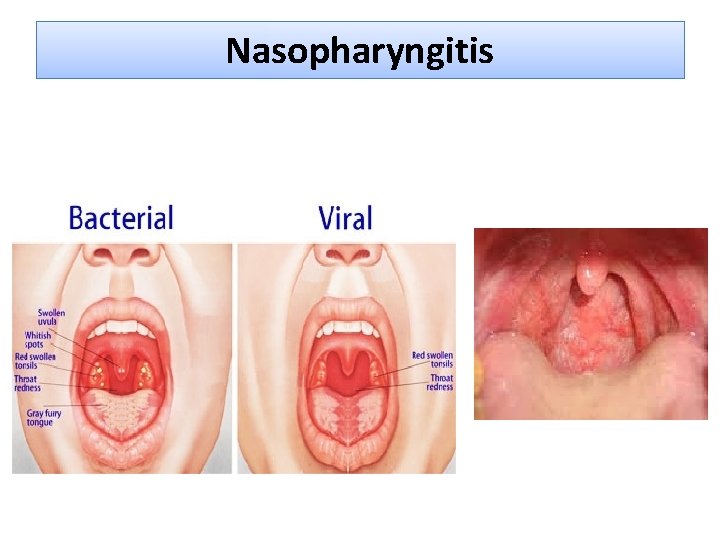
Nasopharyngitis Ø Nasopharyngitis: Common cold. Ø Causes: rhinovirus, adenovirus, influenza virus, Resp. syncytial virus (RSV), Para influenza virus. Ø Clinical manifestations: fever, irritability, restlessness, sneezing, vomiting, diarrhea. dryness, irritation of nose, & Throat, cough, sneezing , chilly sensation, muscular aches. Physical signs: edema& vasodilatation of mucosa. 04/12/2020 15
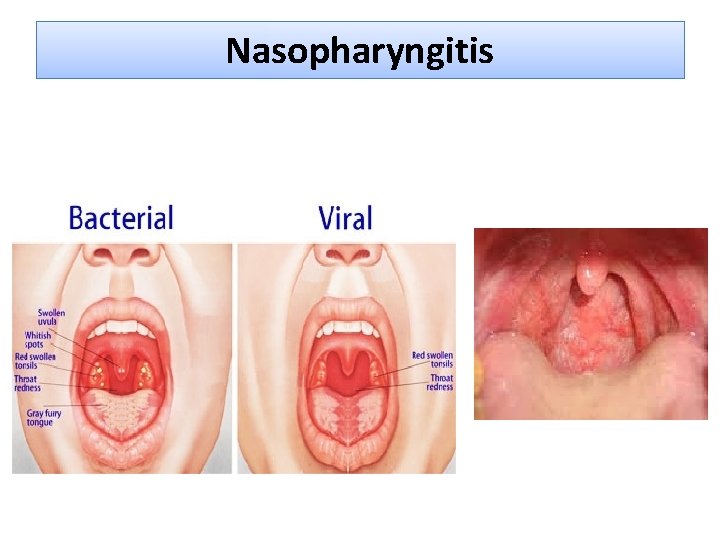
Nasopharyngitis
Nasopharyngitis (cont. ) q Therapeutic management: § Mostly treated at home , no vaccine, antipyretics for fever. § Decongestants: nose drops more effective than orally. § Cough: suppressant. § Antihistamine are ineffective. § Antibiotic: usually not indication. Nursing consideration: • For nasal obstruction: elevate head of bed, suctioning and vaporization, saline nasal drops. • Maintain adequate fluid intake to prevent dehydration. • Avoiding spread the virus. 04/12/2020 17
Pharyngitis • Causes : 80 -90%of cases are viral cause , other is group A and B hemolytic streptococci • Clinical manifestation: - May be mild so no symptoms. - Headache, fever, abdominal pain exudates on pharynx& tonsils, 3 -5 days usually symptoms are subside • Complication if not treated : - Acute glumerulonephritis syndrome in about 10 days. 04/12/2020 18
Pharyngitis (cont. ) • Diagnostic evaluation: throat culture should be performed to rule out. • Therapeutic management: - If streptococcal sore throat infection: oral Penicillin for 10 days , or IM Benzathine penicillin G. - Oral Erythromycin if the child has allergy to penicillin. • Nursing consideration: - Obtain throat swab for culture. - Administer penicillin & analgesic. - Cold or warm compresses to the neck may provide relief. - 04/12/2020 Warm saline gargles. 19
Pharyngitis (cont. ) • Nursing consideration (cont. ) - Soft liquid food are more acceptable than solid. - Continue oral medication to complete the course. - IM injection applied in deep muscle as vastus lateralis or ventrogluteal muscle, use Emla cream before IM around 2 hours. - Nurse role to prevent the spread of disease. - Children are considered non infectious to other 24 hours after initiation of antibiotics therapy. 04/12/2020 20
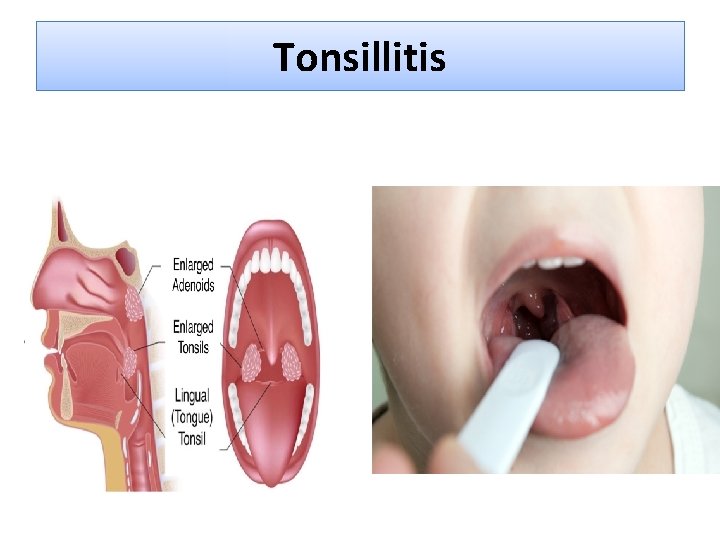
Tonsillitis • Tonsils are masses of lymphoid tissue, first immune defense. • Tonsillitis often occur with pharyngitis, viral or bacterial causes. • S& S: - enlarge tonsils, difficult breathing & swallow. - Enlargement of adenoid, blocked postnasal space &mouth breathing. 04/12/2020 21
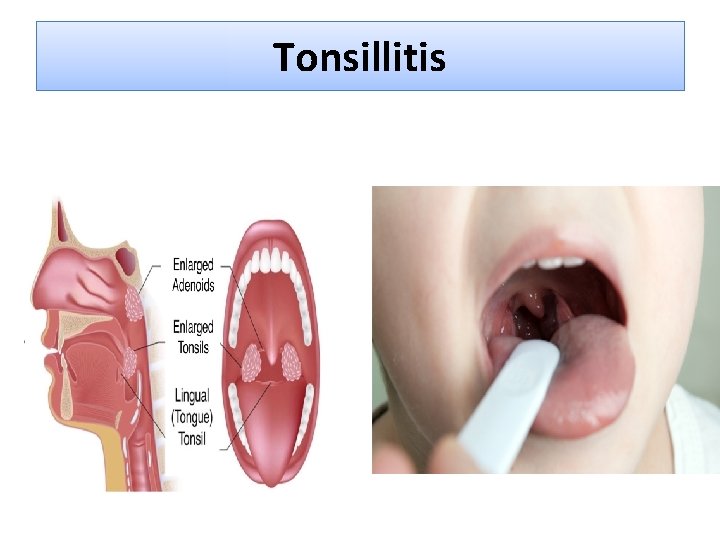
Tonsillitis
Tonsillitis • Therapeutic management: - throat culture to determine the causative agent , viral or bacterial - Tonsillectomy & adenoidectomy (T&S) - Contraindicating for Ts &As: cleft palate, tonsillitis, blood disorder. • Nursing consideration: Ø Providing comfort & maintain minimize activities. Ø A soft or liquid diet is prescribed. Ø Warm salt water gargles Ø Analgesic, antipyretic. 04/12/2020 23
Tonsillitis • Post operative care: Ø Position (place child on abdomen or side). Ø Discourage child from coughing frequency. Ø Some secretion are common as dried blood. Ø Crushed ice& ice water to relief pain. Ø Analgesic may be rectally or IV, avoid oral route. 04/12/2020 24
Tonsillitis • Post operative care (cont. ): Ø Soft food, milk or ice cream Ø Check post operative signs of Hemorrhage: - Increase pulse more than 120 b/min. Pallor. Frequent swallowing. Vomiting of bright blood Decrease blood pressure is late sign of shock. Note: use good light to look direct on site of operation. 04/12/2020 25
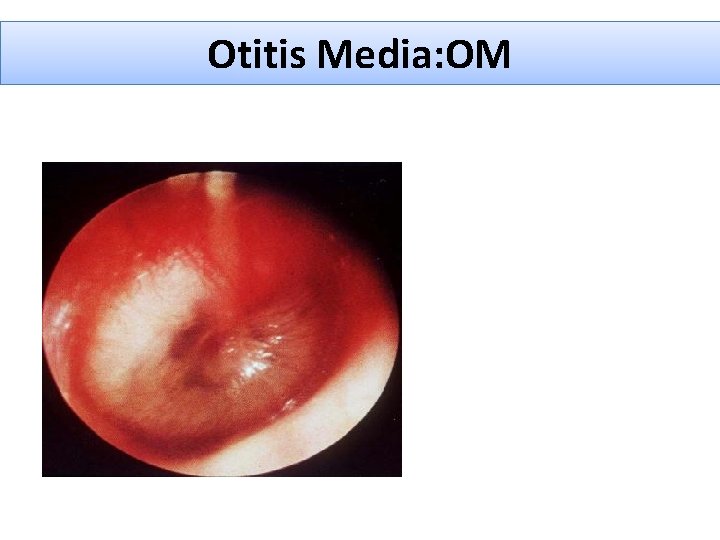
Otitis Media: OM • OM is inflammation of middle ear. • Episode of acute OM occur in the first 24 month, decrease at 5 years, r/to drainage through the Eustachian tube & inflammatory of Resp. system. • Etiology: - Acute (AOM): streptococcus, Haemophilus influenza, moraxella catarrhlis, are the most common bacteria. - OM: blocked Eustachian tube from edema of URTI , allergic hypertrophy adenoid. - Chronic (COM): extension of AOM. 04/12/2020 26
Otitis Media: OM (cont. ) • Diagnostic evaluation: assessment of tympanic membrane with otoscope: AOM: purulent discolored effusion, bulging • S&S: otalgia (earache), fever, purulent discharge, infant rolls his head from side to side, loss of appetite, crying or verbalized feeling of discomfort (older child). • COM: hearing loss, feeling of fullness, vertigo, tinnitus. 04/12/2020 27
Otitis Media: OM (cont. ) • - Therapeutic management: Antibiotic for 10 -14 days e. g. Amoxicillin. Myringotomy: surgical incision of eardrum& grommets. Hear test after 3 month of AOM. • Nursing consideration: Ø Relieving pain. analgesic drug +ice bag on ear. Ø Facilitate drainage & topical A. Biotics. Ø Preventing complication. Ø Instruct family to be careful when deal with child. With temporary hearing loss. Ø Preventing OM during infant feeding and setting after that. 28
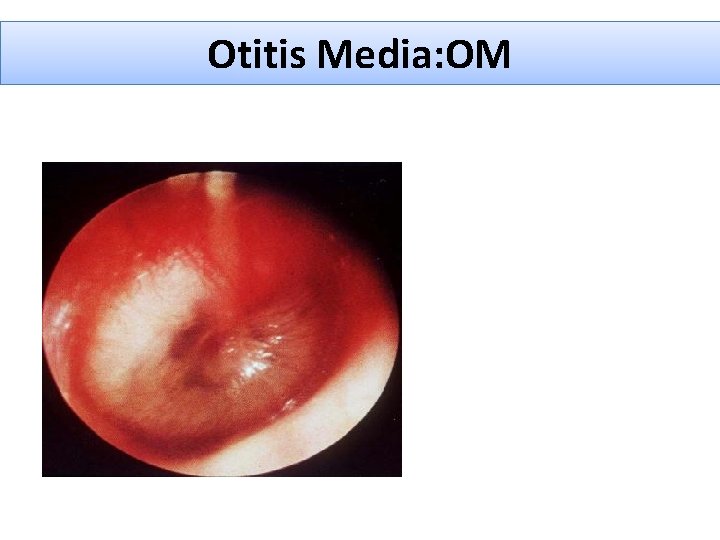
Otitis Media: OM
Lower Respiratory Tract Infections 04/12/2020 30
Infection of the Lower Air ways • Cartilaginous support of the air ways is not fully developed until adolescence, consequently the smooth muscle in these structures represents a major factor in the constriction of the airway. 04/12/2020 31
Bronchitis • Bronchitis or tracheobronchitis is inflammation of larger air way (trachea and bronchi). • Causative agents: viruses or mycoplasma pneumonia. • Ch-ch & symptoms: dry, nonproductive cough that worsens at night then become productive in 2 -3 days. • Bronchitis is a mild disease required symptomatic treatment as antipyretic, analgesic and humidity, cough suppressants may be useful at night. 04/12/2020 32
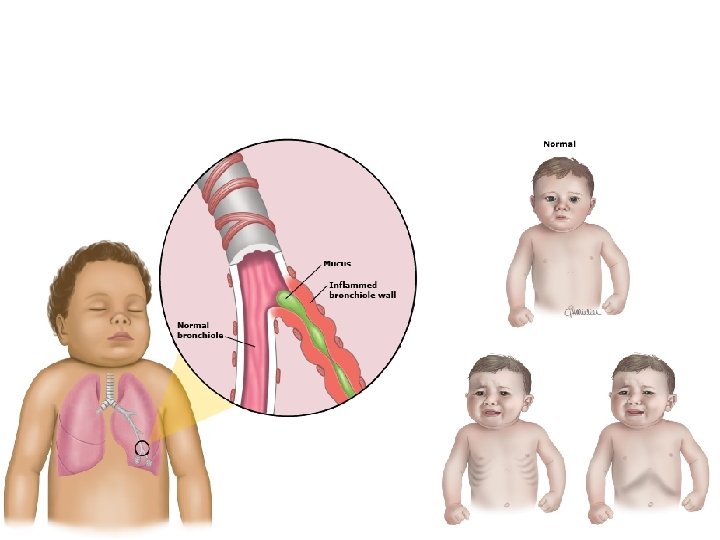
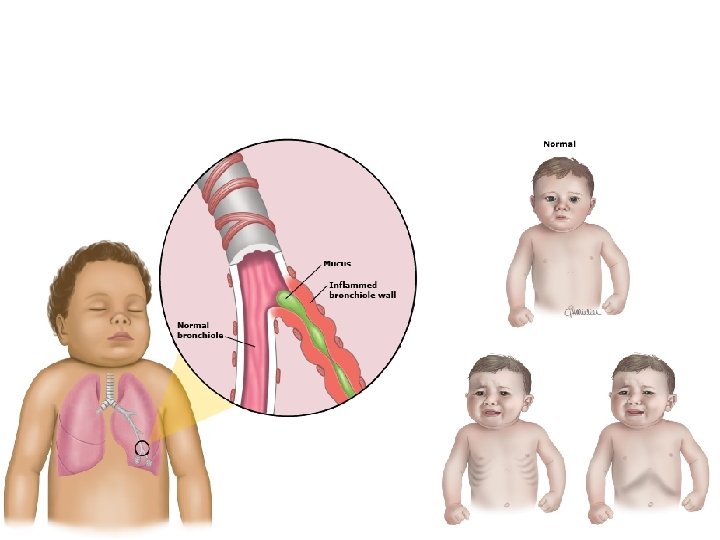
Bronchiolitis & Resp. Syncytial Virus RSV • Bronchiolitis: is an acute viral infection with maximum effect at the bronchiolar level, and rare in children older of 2 years. § One of the Most Frequent Cause of Hospitalization in Infants § Virus or Bacteria Causes Inflammatory Response & Obstruction of Small Airways From Edema • RSV is responsible of 80% of cases during epidemic periods. 04/12/2020 34
Pneumonia • Pneumonia: is inflammation of the pulmonary parenchyma. • Common in children but more frequently occur in infancy & early childhood. • Types of pneumonia (depend on place): Ø Lobar- Pneumonia: one-lobe or more (bilateral or double Pneumonia). Ø Broncho Pneumonia: begins in the terminal bronchioles form consolidated patches in nearly lobules, also called lobular Pneumonia. Ø Interstitial Pneumonia: inflammatory process is confined within the alveolar walls and peribronchial and interlobular tissues. 35 04/12/2020
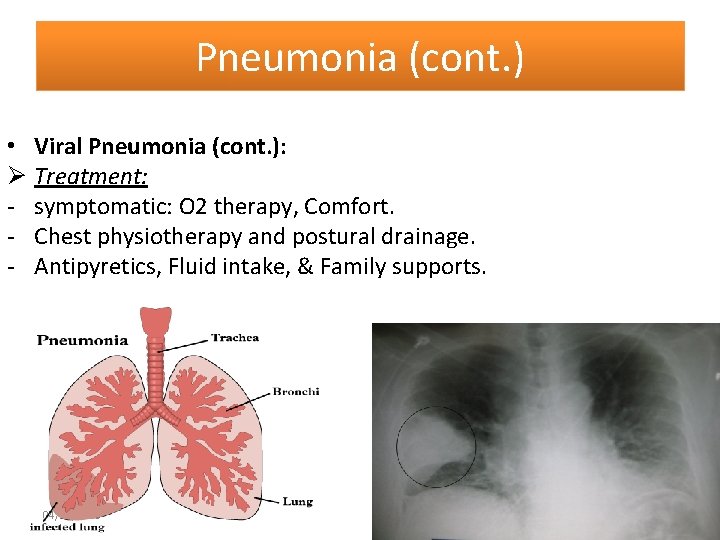
Pneumonia (cont. ) • Morphology classification: viral, bacterial, mycoplasma , aspiration of foreign body, fungal. • Viral Pneumonia: Ø Occurs more than bacterial. Ø Causes: RSV, parainfluenza, adenovirus. Ø Clinical symptoms: fever, cough, abnormal breath sound; whitish sputum, nasal flaring, retraction, chest pain, pallor to cyanosis, irritable, restless, anorexia, vomiting, diarrhea, abdominal pain. 04/12/2020 36
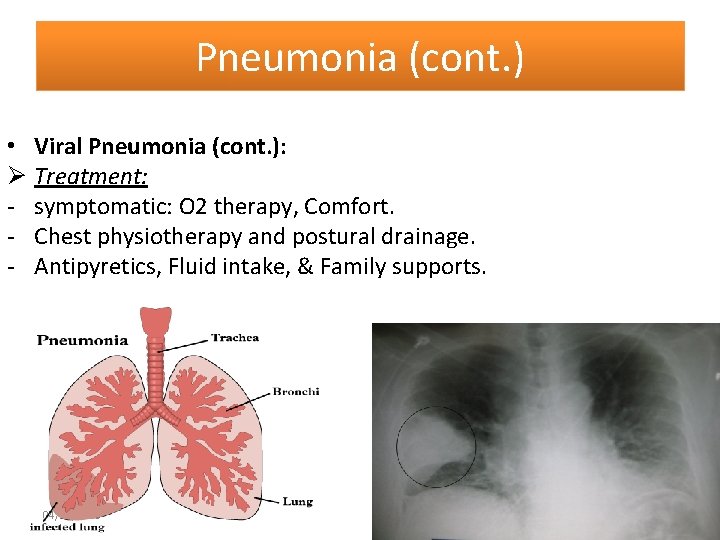
Pneumonia (cont. ) • Viral Pneumonia (cont. ): Ø Treatment: - symptomatic: O 2 therapy, Comfort. - Chest physiotherapy and postural drainage. - Antipyretics, Fluid intake, & Family supports. 04/12/2020 37
Bacterial Pneumonia • Streptococcus Pneumonia is the most common cause in children and adult • In infant mainly followed viral infection. • Symptoms: fever, malaise, rapid& shallow respiration, cough, chest pain, abdominal pain? ? Appendicitis, meningeal symptoms. • Treatment: bed rest, antipyretic, fluid intake, need hospitalization when pleural effusion or empyema, I. V fluid, O 2 therapy. 04/12/2020 38
Bacterial Pneumonia (cont. ) • Complication: - Tension pneumothorax and empyema if the causative agent is staphelococcus auoraus, - lung abscess if pnumococcal pneumonia. • Prognosis: is generally good if recognize the disease early & treat early. • Prevention: pnumococcal poysaetheride vaccine for 04/12/2020 children older than 2 years who is risk. 39
Bacterial Pneumonia (cont. ) • Nursing consideration: Ø Administer of O 2 therapy , rest, humidity. Ø Assess Resp. status frequently. Ø I. V fluid intake. Ø Antipyretic. Ø Lying the child on affected side. Ø Suctioning by bulb syringe for infant. Ø Chest physiotherapy & postural drainage. Ø Family support & reassurance. 04/12/2020 40