SPINAL CORD INJURY Presenter moderator Dr venkat raman















































- Slides: 89

SPINAL CORD INJURY Presenter moderator Dr venkat raman Dr BSK prusty
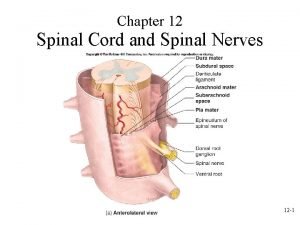
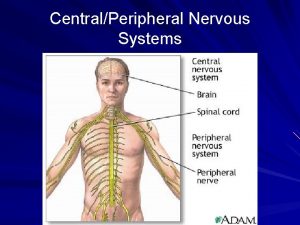
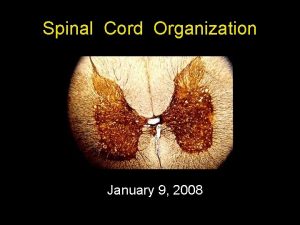
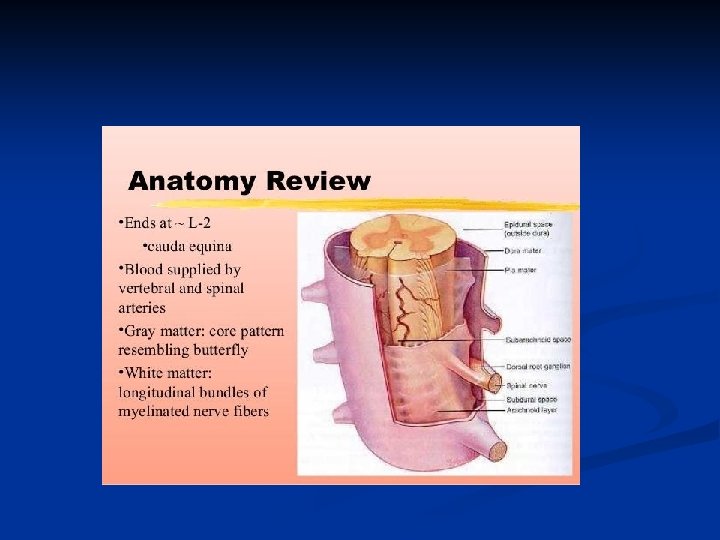
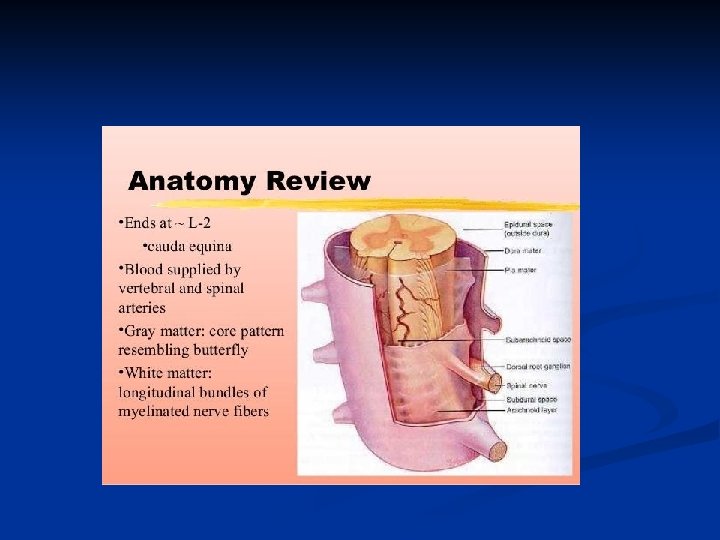
SPINAL CORD INJURY SCI is damage to the spinal cord that results in loss of functions such as mobility and feeling. n Spinalcord is the major bundle of the nerves that carry impulses to/from brain to rest of body n Spinalcord is surrounded by rings of bone vertebra and function to protect spinalcord n Most common vertebra include C 5, C 6, T 12 and L 1 because they have greatest ROM n
n n n SCI is insult to spinalcord resulting in achange in normal motor, sensory or autonomic function. This change is either temporary or permanent. TETRAPLEGIA: impairment or loss of motor and / or sensory function in the cervical segments of spinalcord due to damage of neural elements with in the spinal canal PARAPLEGIA : impairment or loss of motor and / or sensory function in the thoracic , lumbar or sacral segments of spinal cord due to damage of neural elements with in the spinalcanal
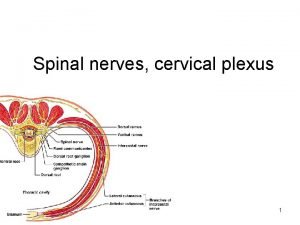
n n DERMATOME : area of the skin innervated by one sensory nerve root MYOTOME : collection of muscles innervated by one motor nerve root NEUROLOGICAL LEVEL OF INJURY : most caudal segment of spinal cord with normal motor and sensory function on bothsides SKELETAL LEVEL : radiographic level of greatest vertebral damage
MOTOR LEVEL : most caudal key muscle group that is graded 3/5 or greater with the segments cephalad to that level graded normal 5/5 strength. n SENSORY LEVEL : most caudal dermatome to have nomal sensation for both pinprick and light touch on both sides. n
NLOI The most caudal cord segment with normal motor and sensory function bilaterally. n Normal motor function refers to a motor grade of 3. . with all cephalad motor levels being grade 5. n This is distinct from skeletal or radiological level of injury n
COMPLETE INJURY : the absence of sensory and motor function in the lowest sacral segments n INCOMPLETE INJURY : preservation of motor or sensory function below the neurologic level of injury that includes lowest sacral segments n
SACRAL SPARING : presence of motor function or sensory function in the lowest sacral segments n ZONE OF PARTIAL PRESERVATON : all segments below the neurologic level of injury that have preserved motor or sensory findings ; used only in complete SCI n
SPINAL SHOCK : the period of flaccid paresis and areflexia following a spinal injury, lasting from 48 hours to weeks , and ending with return of reflexes such as bulbocavernosus reflexes. n NEUROGENIC SHOCK : form of distributive ( cardiovascular ) shock following SCI due to loss of sympathetic tone in peripheral vasculature n

























n THE PATHOPHYSIOLOGY OF - SCI - IS DESCRIBED AS BIPHASIC CONSISTING OF PRIMARY AND SECONDARY PHASES
PRIMARY INJURY Direct mechanical injury may produce focal compression , laceration or traction injury to cord n Ischemic injury may result from interference to the segmental spinal arterial supply n Initial pathological changes include the traumatic severing of axons, blood vessels and cell membranes. n
SECONDARY INJURY Local hypoperfusion and ischemia begin at the site of injury , extending progressively over hours from the site of injury in both directions n There is loss of spinalcord autoregulation , often comlicated by arterial hypotension in high SCI n Other mechanisms include release of free radicals, reactive oxygen species , eicosanoids , proteases, calcium , phospolipases and excitotoxic neurotransmitters. n
Petechial haemorrhages begin in greymatter and may result in significant hemorrhage in to cord. n There is edema, cellular chromatolysis and vacuolation and neuronal necrosis. n In white matter vasogenic edema , axonal degeneration and demyelination follows. n Later coagulative necrosis and cavitation subsequently takes place. n
INITIAL ASSESSMENT AND MANAGEMENT n n 1. 2. 3. 4. Main principles in the early management of spinal injury relate to prevention of secondary injury and provision of optimum conditions for neurological recovery. This includes IMMOBILISATION PREVENTION OF HYPOXIA DEFENDING BLOOD PRESSURE AVOIDING METABOLIC ABNORMALITIES.

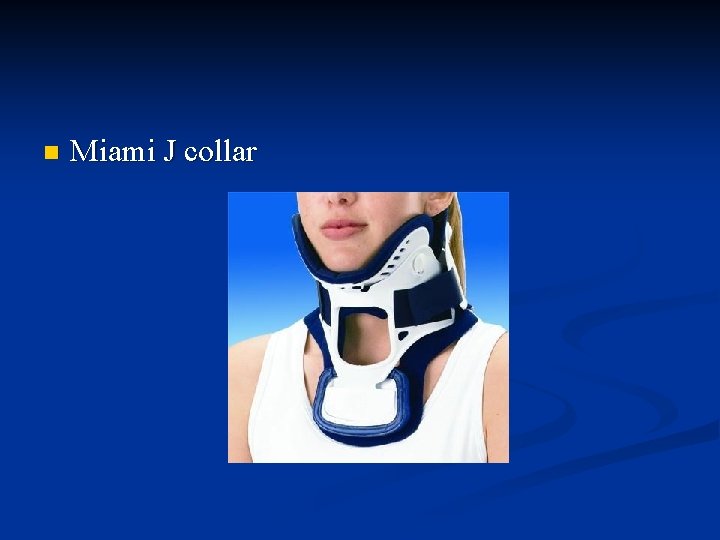
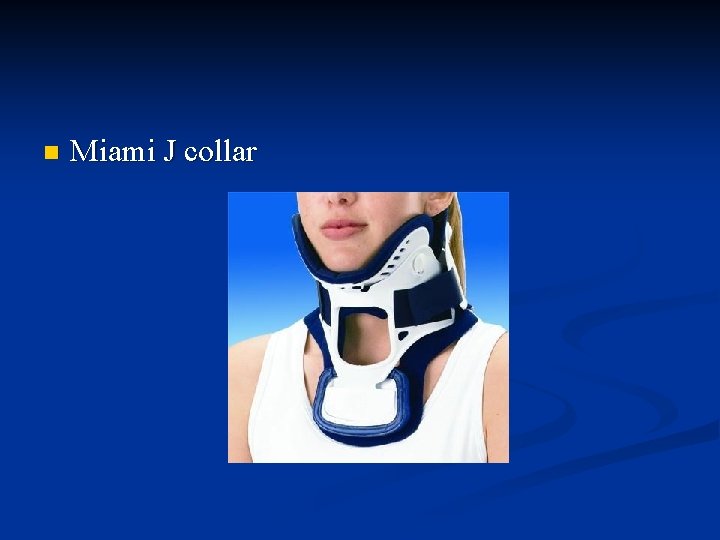
n Miami J collar

n Philadelphia collar
With a suspected thoracolumbar spinal injury , the patient is again lifted as a single unit. n Rigid collars and hard spinal boards cause rapid development of pressure areas. n This risk can be minimised by transfering the patient off a hard board , safely rolling the patient every 2 hours. n

Complications of immobilisation Complications include : cutaneous pressure ulceration difficulties with the airway and intubation potential venous obstruction high risk of VTE high risk of respiratory infections gastrostasis and inablity to provide oral care








SPINAL CORD INJURIES Cord concussion and cord contusion – temporary loss of cord mediated function. n Cord compression – decompression required to minimise permanent injury. n Laceration –permanent injury dependent on degree of damage. n Hemorrhage – may results in local ischemia n
n 1. Cord transection: Complete : all tracts disrupted cord mediated function below transections are permanently lost possible results QUADRIPLEGIA : C SPINE INJURY PARAPLEGIA : T L SPINE INJURY

CORD TRANSECTION : INCOMPLETE : some tracts and cord mediated functions remain intact. potential for recovery of function possible syndromes : BROWN SEQUARD SYNDROME ANTERIOR CORD SYNDROME CENTRAL CORD SYNDROME CONUS MEDULLARIS SYNDROME CAUDA EQUINA SYNDROME n
n BROWN SEQUARD : ipsilateral loss of motor, propioception and fine touch, with contralateral loss of pain and temperature sensation below the NLOI. it usually follows a penetrating SCI damaging only one half of spinal cord

n ANTERIOR CORD : loss of motor function and pain and temperature sensation below the NLOI , with preservation of fine touch and proprioception it is less common typically following interruption of blood supply to anterior spinal cord

n CENTRAL CORD SYNDROME : weakness and sensory loss, greater in the arms than the legs typically followed by hyperextension injury with pre existing canal stenosis ischemia or hematoma in the centre of cord effects the cervical segments more due to the pattern of lamination of the corticospinal and spinothalamic tracts

n n CONUS MEDULLARIS : sudden onset, symmetrical paraplegia with mixed and lower motor neuron findings caused by injury at T 12/L 1 CAUDA EQUINA : often asymmetrical, lower motor neuron lower limb weakness with saddle area hypoaesthesia , with bladder and bowel areflexia caused by injury below L 1 damaging the lumbosacral nerve roots


n 1. 2. 3. 4. 5. NEXUS ( national emergency x-radiography utilization study ) suggests cervical spining indicated for patients with trauma unless they meet all following criteria : No posterior midline cervical spine tenderness No evidence of intoxication Normal level of alertness No focal neurological deficit No painful distracting injuries.

MANAGEMENT 1. 2. 3. 4. 5. 6. 7. 8. 9. Initial assessment Secondary assessment ICU care BP management Avoid steriods DVT prophylaxis Closed reduction and traction Maintain nutrition Operative intervention.
Initial assessment : apply cervical collar and check airway , breathing and circulation n Secondary assessment : assess GCS and pupillary reaction and localising signs n ICU care : management of patients with acute spinal cord injury is recommended in ICU n
BP monitoring : maintain arterial BP at 85 -90 mm of Hg for the first 7 days following acute SCI as it improves spinal cord perfusion if CVP exceeds 10 cm of water , dopamine or noradrenaline infusion may be given to maintain BP. n Avoid steriods : not recommended n
DVT prophylaxis : low dose heparin in combination with PC stockings for a minimum period of 3 months. venacava filters who fail anticoagulation. n Closed reduction / traction : early closed reduction of spinal fracture dislocation with craniocervical traction is recommended for restoration of anatomic alignment n
Maintain nutrition: nitrogen requirements. calorie requirements may be lower due to muscle paralysis and flaccidity. n Operative intervention : decompression and fusion n
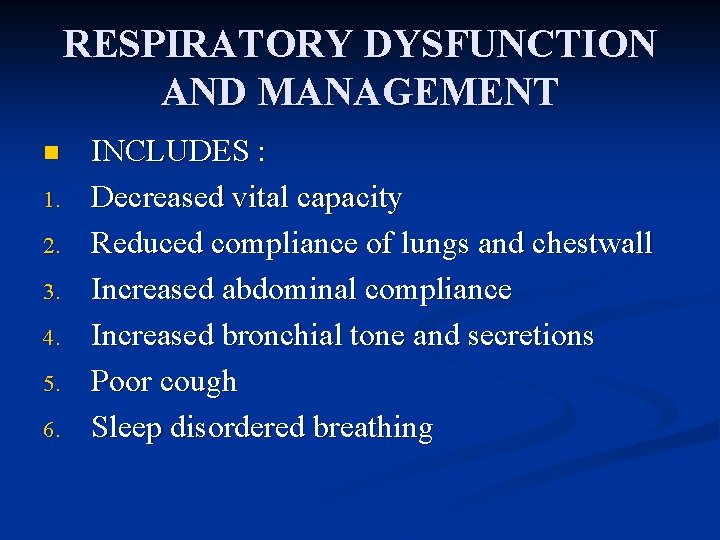
RESPIRATORY DYSFUNCTION AND MANAGEMENT n 1. 2. 3. 4. 5. 6. INCLUDES : Decreased vital capacity Reduced compliance of lungs and chestwall Increased abdominal compliance Increased bronchial tone and secretions Poor cough Sleep disordered breathing
75% of patients with cervical SCI require intubation and mechanical ventilation n Tidal volumes in excess of 10 ml/kg are used – to prevent atlelectasis and air hunger. n Another approach is use of more conventional tidal volumes and higher PEEP to prevent atelectasis n
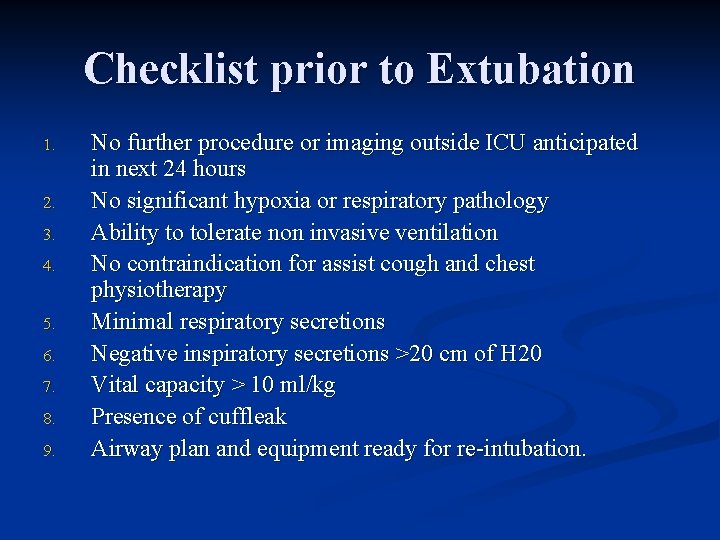
Checklist prior to Extubation 1. 2. 3. 4. 5. 6. 7. 8. 9. No further procedure or imaging outside ICU anticipated in next 24 hours No significant hypoxia or respiratory pathology Ability to tolerate non invasive ventilation No contraindication for assist cough and chest physiotherapy Minimal respiratory secretions Negative inspiratory secretions >20 cm of H 20 Vital capacity > 10 ml/kg Presence of cuffleak Airway plan and equipment ready for re-intubation.
PERCUTANEOUS TRACHEOSTOMY Extubation failure likely to necessitate a Tracheostomy n Complete injuries above C 5 usually require tracheostomy n Others include high NLOI, complete SCI , associated facial fractures , thoracic trauma and emergency intubation n
WEANING n n Weaning from MV after SCI may take considerable time It should be remembered that most patients with SCI ventilate more easily when supine compared with upright , as their abdominal contents can push the diaphragm up in to position. The NLOI is the strong predictor of successful weaning Patients with complete injuries at or above C 3 are likely need permanent ventilation.
CARDIOVASCULAR DYSFUNCTION Following SCI, loss of sympathetic supply and unopposed vagal activity may cause profound vasoplegia combined with bradycardia , resulting in hypotension and neurogenic shock. n Bradycardia and even asystole may occur during routine ICU procedures or repositioning in bed with cervical NLOI n This phenomenon occurs most commonly in first week and resolves in 2 -6 weeks after injury n
n Cardiovascular complications include Autonomic Dysreflexia venous thromboembolism
Autonomic Dysreflexia n n n Acute hypertension due to severe sympathetic stimulation with injuries above T 6 Occurs following resolution of spinal shock. Occurs due to dysregulated sympathetic activation leading to intense vasoconstriction below level of lesion. Compensatory parasympathetic activation leads to bradycardia , vasodilatation and sweating above level of NLOI. Other symptoms include headache, blurred vision nausea and nasal congestion.
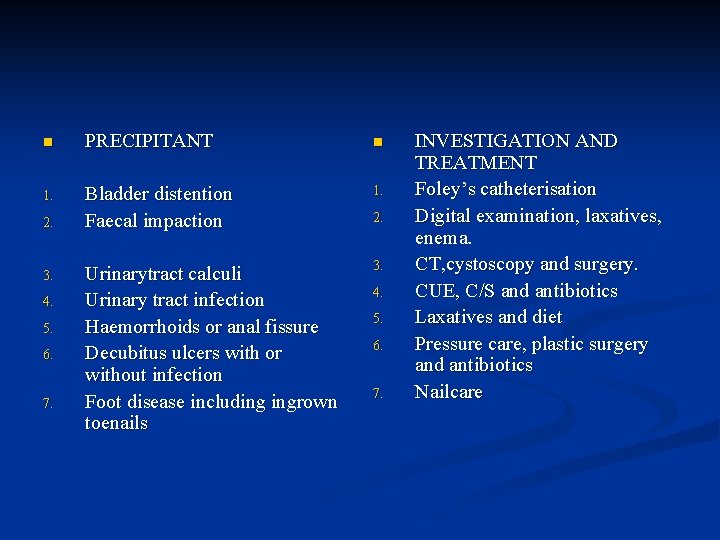
n PRECIPITANT n 1. Bladder distention Faecal impaction 1. Urinarytract calculi Urinary tract infection Haemorrhoids or anal fissure Decubitus ulcers with or without infection Foot disease including ingrown toenails 3. 2. 3. 4. 5. 6. 7. 2. 4. 5. 6. 7. INVESTIGATION AND TREATMENT Foley’s catheterisation Digital examination, laxatives, enema. CT, cystoscopy and surgery. CUE, C/S and antibiotics Laxatives and diet Pressure care, plastic surgery and antibiotics Nailcare
Sitting up – to induce orthostatic hypotensive response n Loosening tight clothing and hypertensives. n Medications include sublingual GTN , captopril or oral prazocin n IV infusion sodium nitroprusside or GTN. n Systolic BP >150 is life threatening and may lead to IC bleed , Myocardial ischemia, Retinal hemorrhage. n

MUSCULOSKELETAL COMLICATIONS : muscle spasticity develops after resolution of spinal shock and is characterised by increased muscle tone , hyperreflexia and muscle spasms below NLOI. n Initial treatment is enteral baclofen. Side effects include sedation , fatigue , confusion and prolonged weaning. n Other medications include intrathecal baclofen, gabapenti, pregabalin and bzd. n PHYSIOTHERAPY to preserve maximum functioality. n

CHRONIC PAIN : 2 types: nociceptive pain and neuropathic pain n reports with in 6 months after injury. n Gabapentinoids , antideppresants are effective for neuropathic pain n infusion of opiates , ketamine and lidocaine for shortterm therapy n
GASTROINTESTINAL : paralytic ileus and gastric dilatation are common following SCI 1. uppermotor neuron bowel syndrome- lesions above cauda equina symptoms -constipation and faecal retention treatment- adequate fluid intake , diet , laxatives and 2. Lower motor neuron bowel syndrome is seen in cauda equina injuries symptoms – constipation and overflow incontinence treatment – proton pump inhibitors. n

 Epineurium
Epineurium Lateral pectoral nerve
Lateral pectoral nerve Inferior gluteal nerve
Inferior gluteal nerve Exercise 15 spinal cord and spinal nerves
Exercise 15 spinal cord and spinal nerves Christopher reeve spinal cord injury level
Christopher reeve spinal cord injury level Spinal cord injury rehabilitation st. louis
Spinal cord injury rehabilitation st. louis Diet for spinal cord injury patient
Diet for spinal cord injury patient Somi brace
Somi brace Spinal cord injury protocol
Spinal cord injury protocol Spinal cord injury shoulder exercises
Spinal cord injury shoulder exercises Cervical and brachial plexus
Cervical and brachial plexus Spinal cord venous drainage
Spinal cord venous drainage Spinal refleks
Spinal refleks Boston scientific spinal cord stimulator
Boston scientific spinal cord stimulator Hypothalamus
Hypothalamus Spinal cord
Spinal cord Subthalamus
Subthalamus Cerebellomedullary cistern
Cerebellomedullary cistern Nerves branching beyond the spinal cord into the body
Nerves branching beyond the spinal cord into the body Dermatome map
Dermatome map Brain and spinal cord nervous system
Brain and spinal cord nervous system What covers spinal cord
What covers spinal cord Structure of spinal cord
Structure of spinal cord Bme580
Bme580 End of spinal cord
End of spinal cord Back hurts
Back hurts Nice spinal cord compression
Nice spinal cord compression Tethered cord
Tethered cord Posterior median sulcus
Posterior median sulcus Spinal cord anatomy
Spinal cord anatomy Causes of spinal cord compression
Causes of spinal cord compression Spinal cord nerve anatomy
Spinal cord nerve anatomy Spinal cord
Spinal cord Spinal cord diagram
Spinal cord diagram Autonomic nervous system table
Autonomic nervous system table Mezgovnice
Mezgovnice Spinal cord
Spinal cord T10 spinal cord
T10 spinal cord Components of reflex arc
Components of reflex arc Objectives of nervous system
Objectives of nervous system Frog
Frog Spinal cord cross section
Spinal cord cross section Spinal cord parts
Spinal cord parts Visceral nervous system
Visceral nervous system Spinal cord
Spinal cord Spinal cord extends from
Spinal cord extends from Umbilical cord histology diagram
Umbilical cord histology diagram Spinal cord anterior
Spinal cord anterior Spinal cord
Spinal cord Tendon histology
Tendon histology Spinal cord
Spinal cord S/p laminectomy icd 10
S/p laminectomy icd 10 Vestibulospinal tract
Vestibulospinal tract Spinal cord muscles
Spinal cord muscles Neural crest cells derivatives
Neural crest cells derivatives The spinal nerves
The spinal nerves Spinal cord denticulate ligament
Spinal cord denticulate ligament Pyramidal system
Pyramidal system Spinal cord and brain
Spinal cord and brain Spinal cord spasticity
Spinal cord spasticity Spinal angiogram
Spinal angiogram Function of the pons
Function of the pons Notochord vs spinal cord
Notochord vs spinal cord Partes
Partes Gray matter
Gray matter Musculus articularis cubiti
Musculus articularis cubiti Spinal cord level
Spinal cord level Intensivis
Intensivis Example of intentional injury
Example of intentional injury Venkat subramaniam wiki
Venkat subramaniam wiki Venkat ganesan ut austin
Venkat ganesan ut austin Venkat subramaniam java
Venkat subramaniam java Rama venkat
Rama venkat Venkat subramaniam mathematician
Venkat subramaniam mathematician Venkat tummalapalli
Venkat tummalapalli Sarita venkat apple
Sarita venkat apple Cara moderator
Cara moderator Moderator vs mediator
Moderator vs mediator What is control variable in research
What is control variable in research Continuous moderator
Continuous moderator Nsnhe,f
Nsnhe,f Directe en indirecte observatie
Directe en indirecte observatie Regulator moderator war
Regulator moderator war What is a difference between the speech and the poster
What is a difference between the speech and the poster Poluarea apei brainly
Poluarea apei brainly Tugas moderator adalah
Tugas moderator adalah Good greeting for presentation
Good greeting for presentation Moderator
Moderator Mediating vs moderating variable
Mediating vs moderating variable Moderator tom
Moderator tom