SPINAL CORD INJURY SPINAL CORD INJURY Definition Insult

- Slides: 40
SPINAL CORD INJURY

SPINAL CORD INJURY
Definition Insult to spinal cord resulting in a change, in the normal motor, sensory or autonomic function. This change is either temporary or permanent.
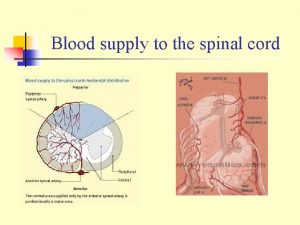
Mechanisms: Direct trauma ii) Compression by bone fragments / haematoma / disc material iii) Ischemia from damage / impingement on the spinal arteries i)
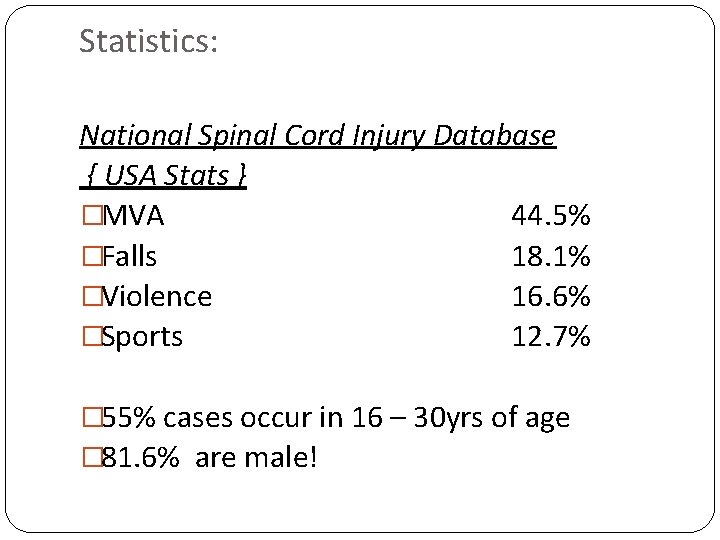
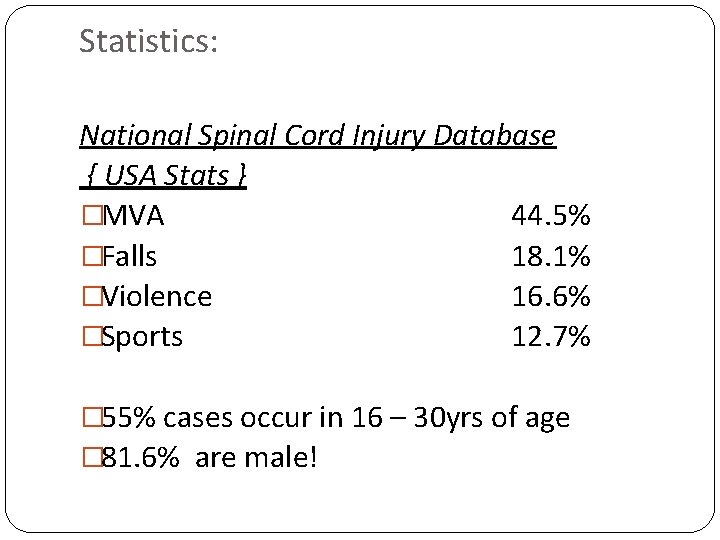
Statistics: National Spinal Cord Injury Database { USA Stats } �MVA 44. 5% �Falls 18. 1% �Violence 16. 6% �Sports 12. 7% � 55% cases occur in 16 – 30 yrs of age � 81. 6% are male!
Other causes: �Vascular disorders �Tumours �Infectious conditions �Spondylosis �Iatrogenic �Vertebral fractures secondary to osteoporosis �Development disorders
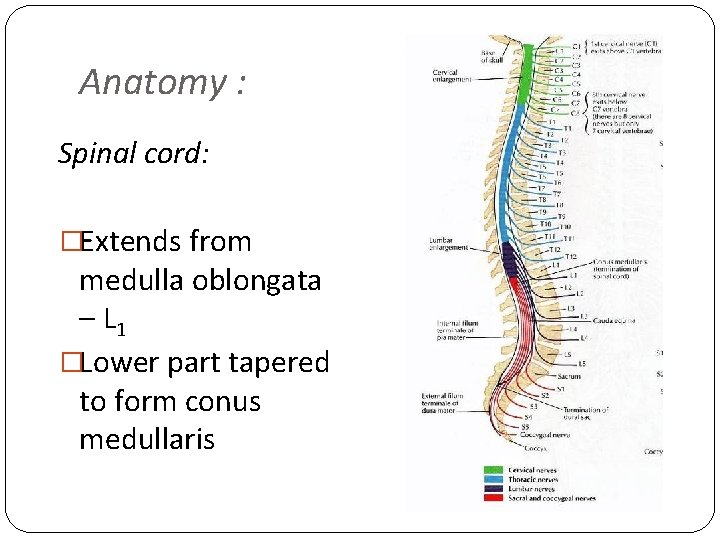
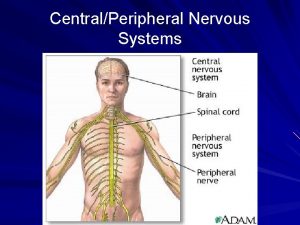
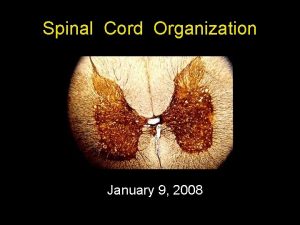
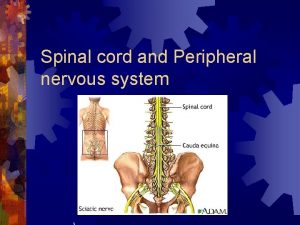
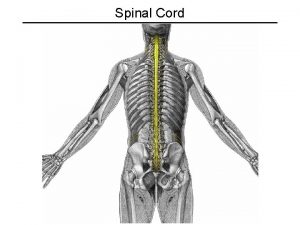
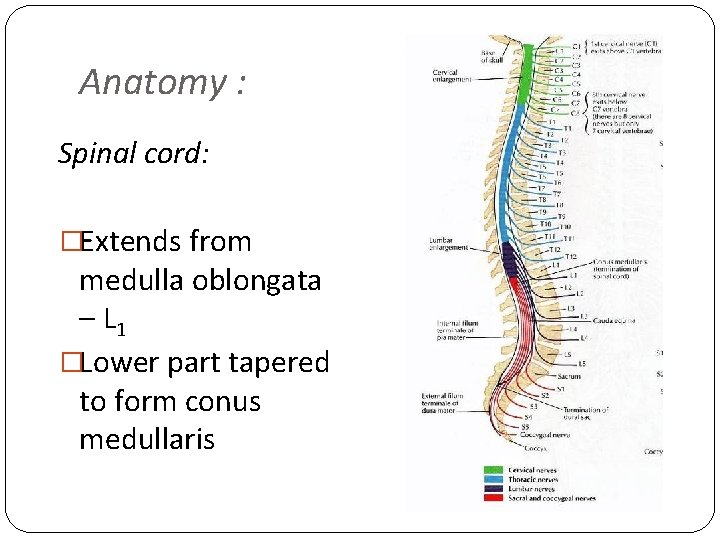
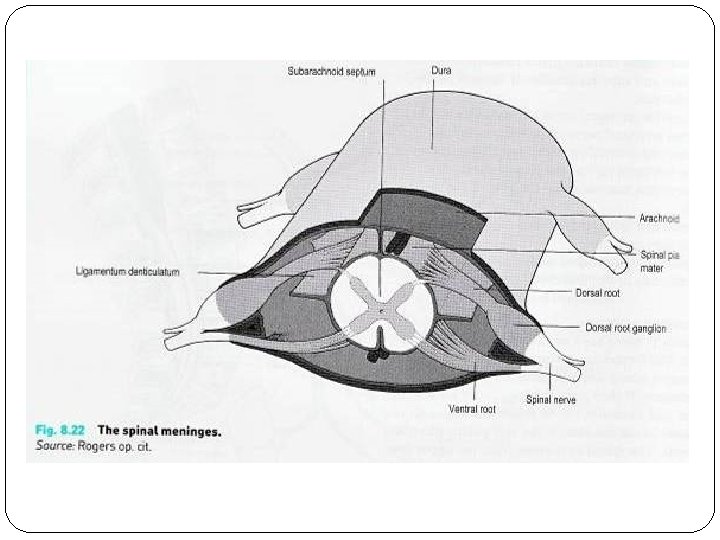
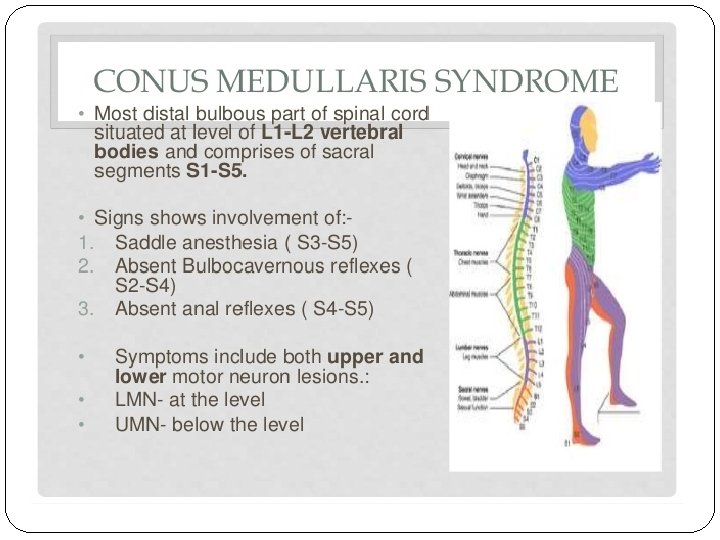
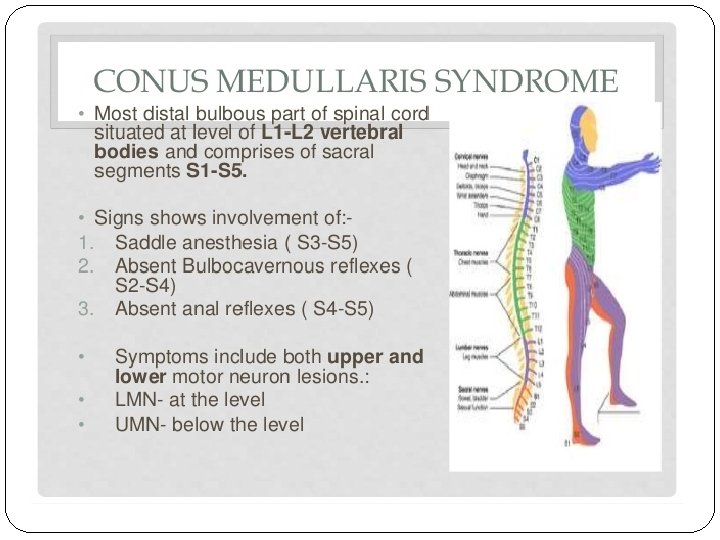
Anatomy : Spinal cord: �Extends from medulla oblongata – L 1 �Lower part tapered to form conus medullaris
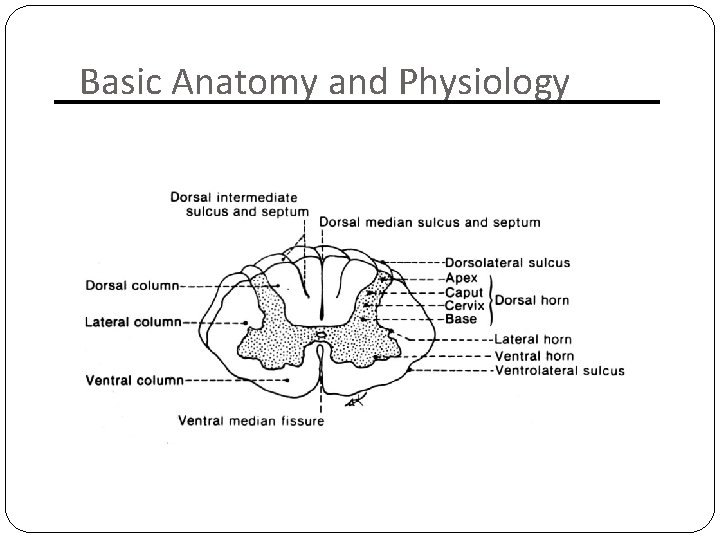
On the surface : �Deep anterior median fissure �Shallower posterior median sulcus Spinal cord segment : �Section of the cord from which a pair of spinal nerves are given off
Hence: 31 pairs of spinal nerves: 8 cervical 12 thoracic 5 lumbar 5 sacral 1 coccygeal
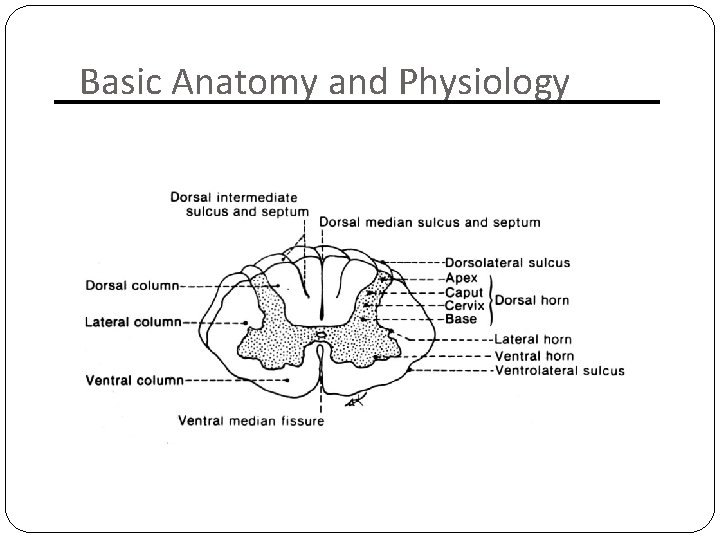
Basic Anatomy and Physiology
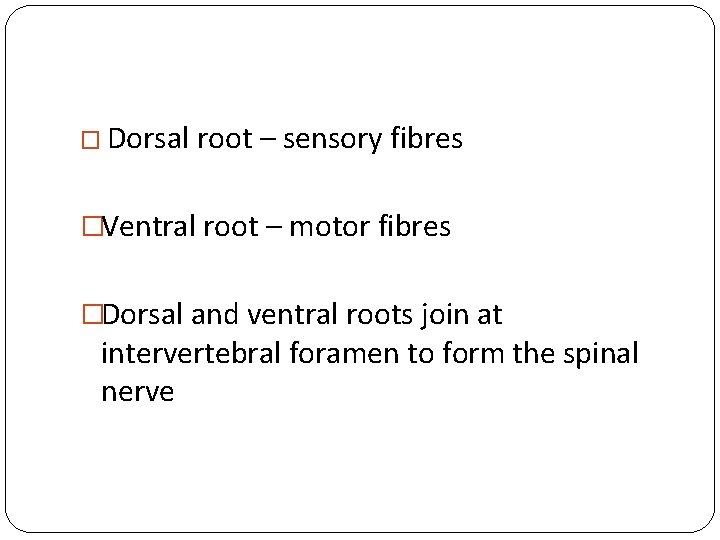
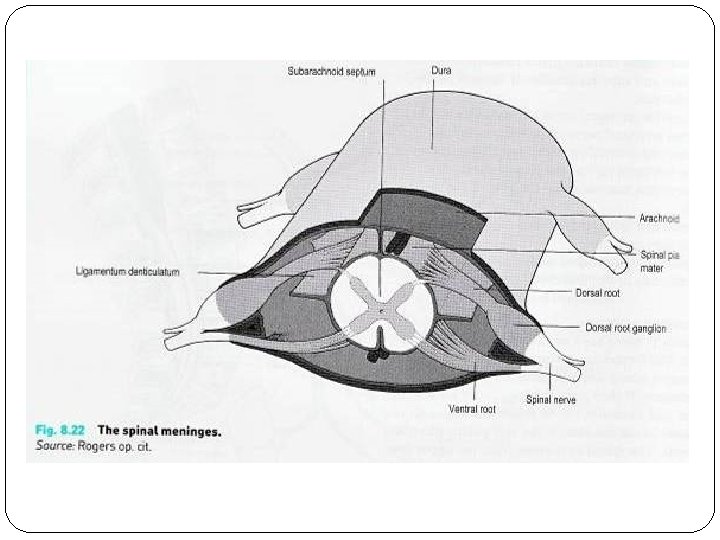
� Dorsal root – sensory fibres �Ventral root – motor fibres �Dorsal and ventral roots join at intervertebral foramen to form the spinal nerve
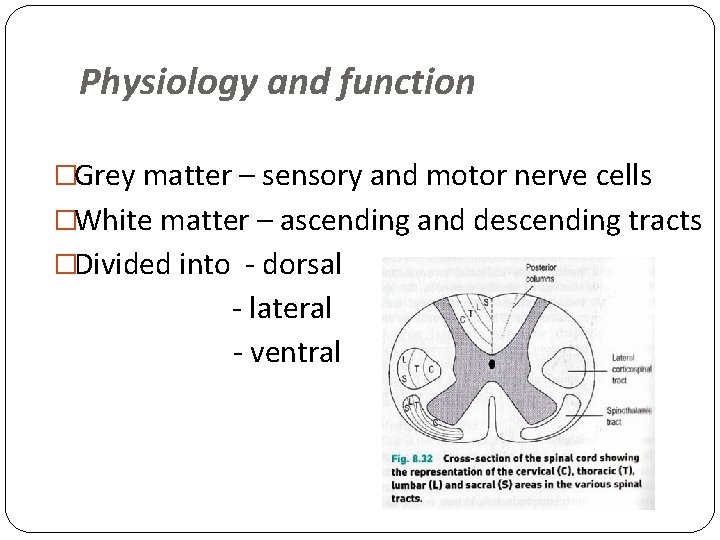
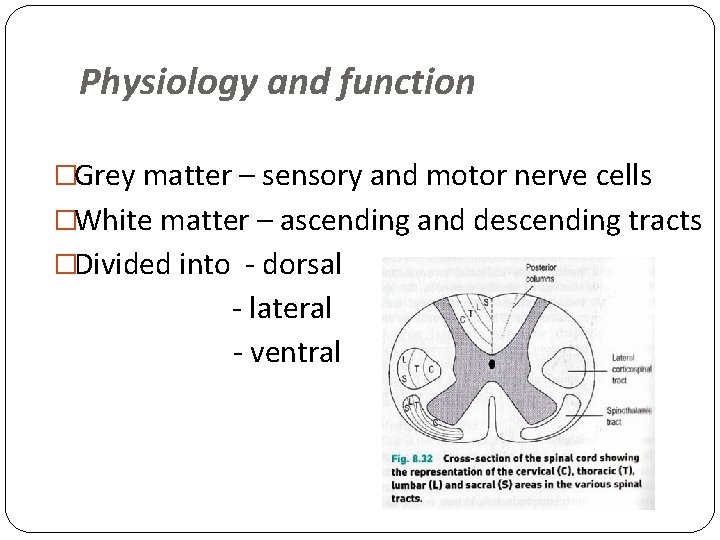
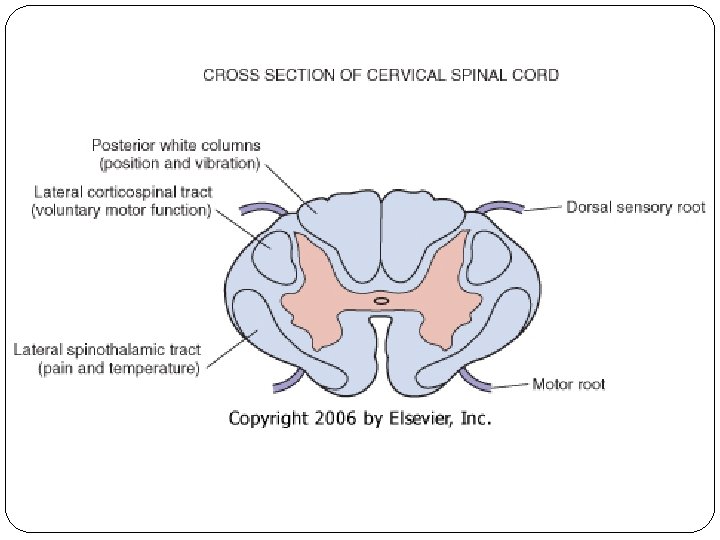
Physiology and function �Grey matter – sensory and motor nerve cells �White matter – ascending and descending tracts �Divided into - dorsal - lateral - ventral
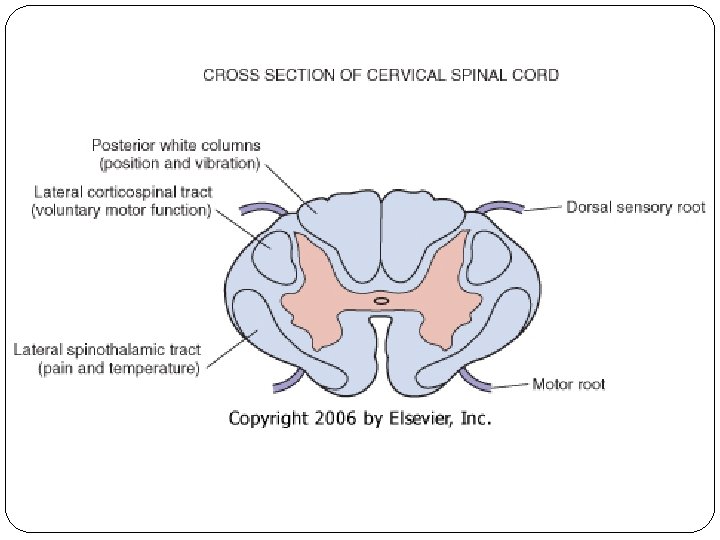
Tracts : 1) Posterior column: �Fine touch �Light pressure �Proprioception
2) Lateral corticospinal tract : �Skilled voluntary movement 3) Lateral spinothalamic tract : �Pain & temperature sensation
�Posterior column and lateral corticospinal tract crosses over at medulla oblongata �Spinothalamic tract crosses in the spinal cord and ascends on the opposite side NB to understand this as it helps to understand the clinical features of injury patterns and the neurological deficit
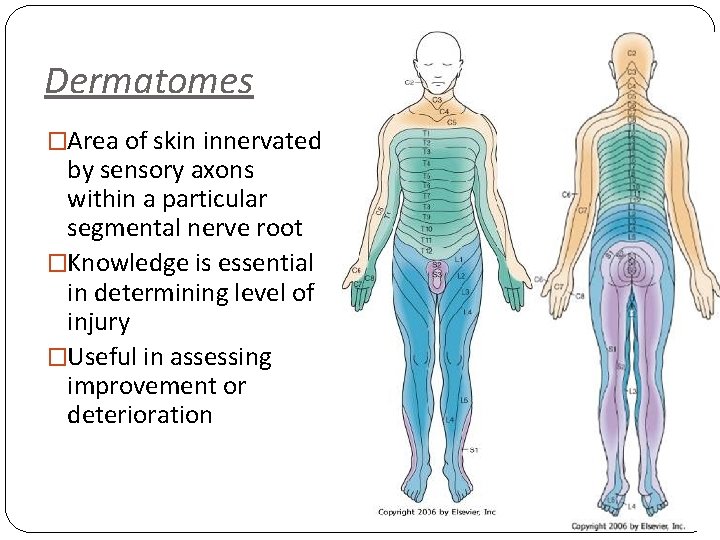
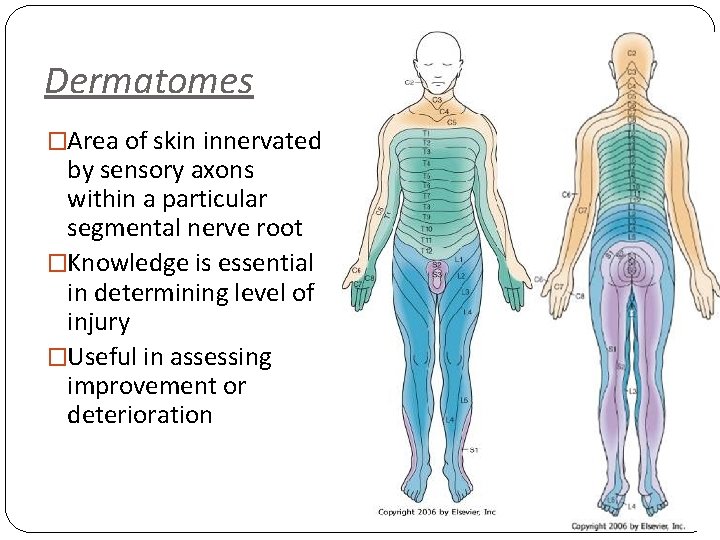
Dermatomes �Area of skin innervated by sensory axons within a particular segmental nerve root �Knowledge is essential in determining level of injury �Useful in assessing improvement or deterioration
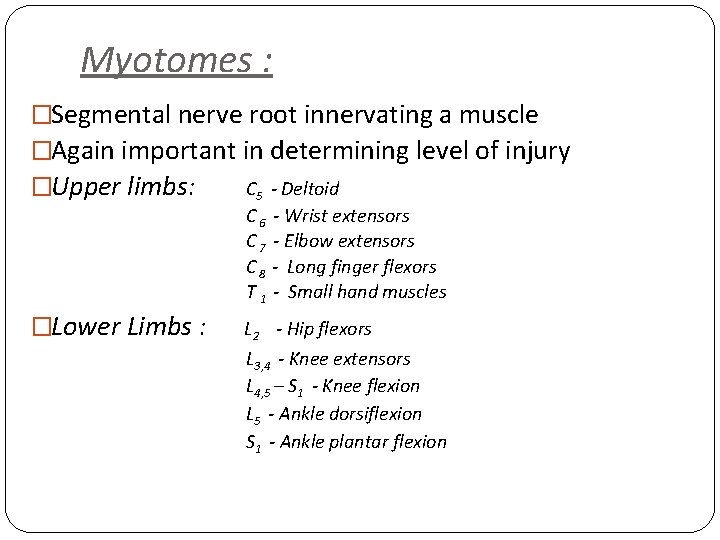
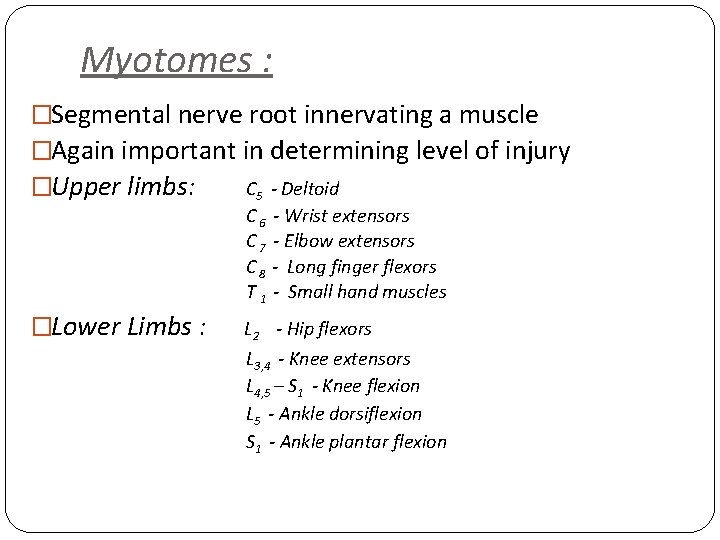
Myotomes : �Segmental nerve root innervating a muscle �Again important in determining level of injury �Upper limbs: C 5 - Deltoid C 6 - Wrist extensors C 7 - Elbow extensors C 8 - Long finger flexors T 1 - Small hand muscles �Lower Limbs : L 2 - Hip flexors L 3, 4 - Knee extensors L 4, 5 – S 1 - Knee flexion L 5 - Ankle dorsiflexion S 1 - Ankle plantar flexion
Spinal Cord Injury Classification �Quadriplegia : injury in cervical region all 4 extremities affected �Paraplegia : injury in thoracic, lumbar or sacral segments 2 extremities affected
Injury either: 1) Complete i) iii) 2) Loss of voluntary movement of parts innervated by segment, this is irreversible Loss of sensation Spinal shock Incomplete i) iii) Some function is present below site of injury More favourable prognosis overall Are recognisable patterns of injury, although they are rarely pure and variations occur
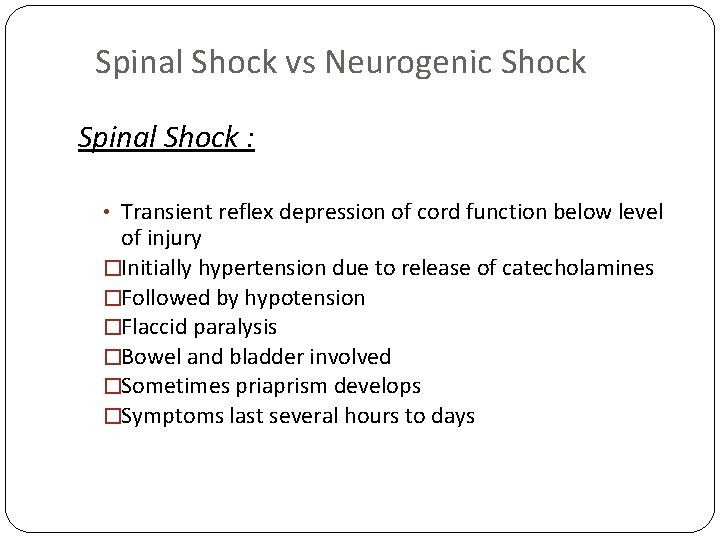
Spinal Shock vs Neurogenic Shock Spinal Shock : • Transient reflex depression of cord function below level of injury �Initially hypertension due to release of catecholamines �Followed by hypotension �Flaccid paralysis �Bowel and bladder involved �Sometimes priaprism develops �Symptoms last several hours to days
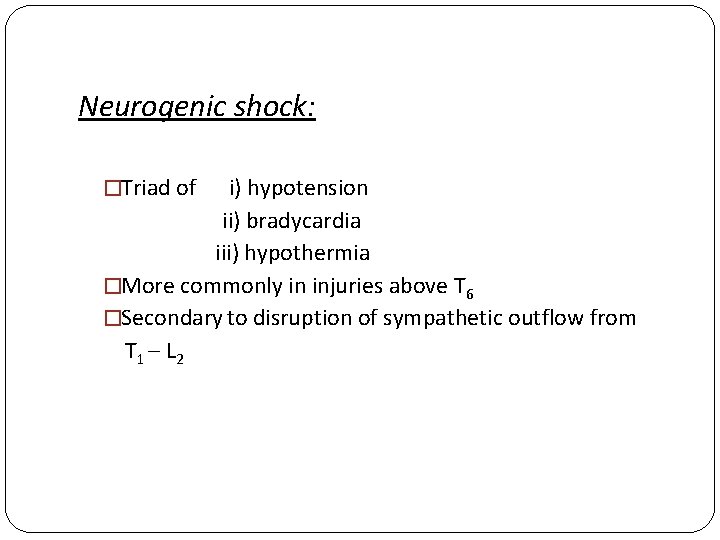
Neurogenic shock: �Triad of i) hypotension ii) bradycardia iii) hypothermia �More commonly in injuries above T 6 �Secondary to disruption of sympathetic outflow from T 1 – L 2
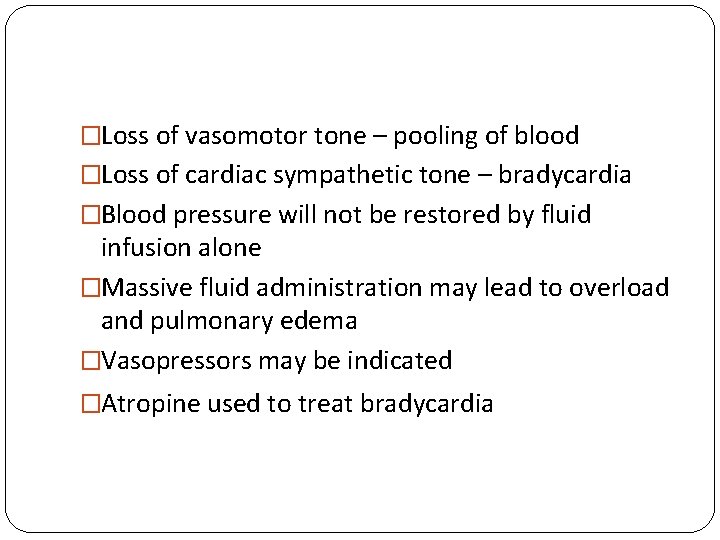
�Loss of vasomotor tone – pooling of blood �Loss of cardiac sympathetic tone – bradycardia �Blood pressure will not be restored by fluid infusion alone �Massive fluid administration may lead to overload and pulmonary edema �Vasopressors may be indicated �Atropine used to treat bradycardia
What is the difference between spinal shock and neurogenic shock? �Spinal shock is mainly a loss of reflexes (flaccid paralysis) �Neurogenic shock is mainly hypotension and bradycardia due to loss of sympathetic tone
Types of incomplete injuries i) iii) iv) v) Central Cord Syndrome Anterior Cord Syndrome Posterior Cord Syndrome Brown – Sequard Syndrome Cauda Equina Syndrome
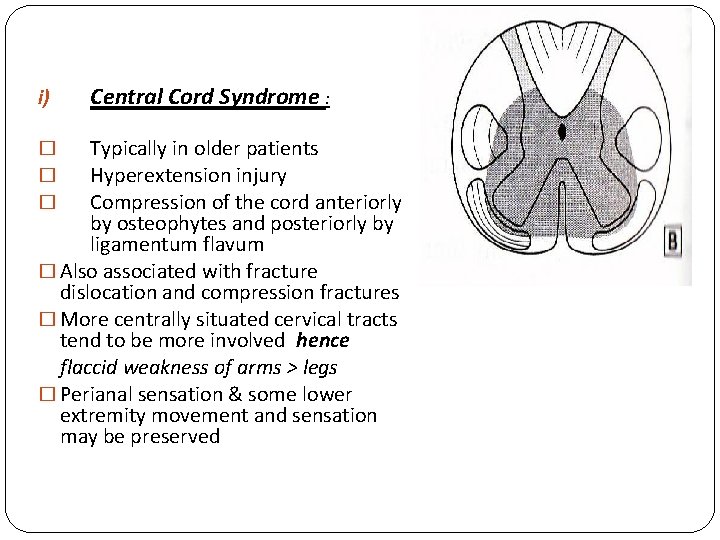
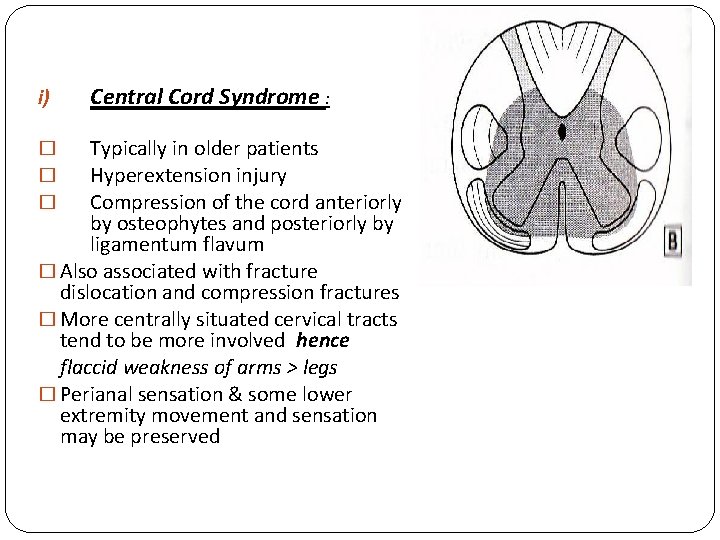
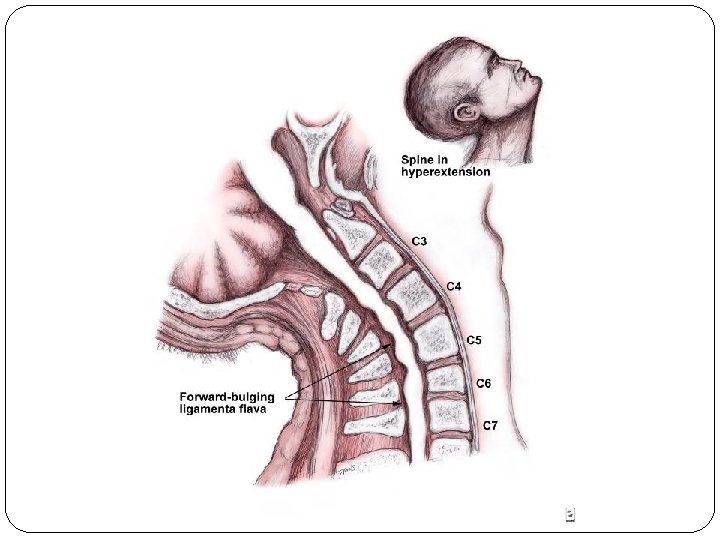
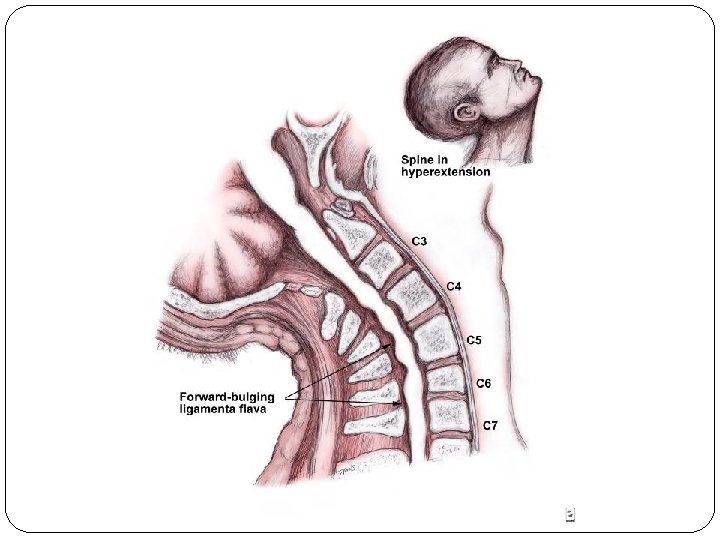
i) Central Cord Syndrome : Typically in older patients Hyperextension injury Compression of the cord anteriorly by osteophytes and posteriorly by ligamentum flavum � Also associated with fracture dislocation and compression fractures � More centrally situated cervical tracts tend to be more involved hence flaccid weakness of arms > legs � Perianal sensation & some lower extremity movement and sensation may be preserved � � �
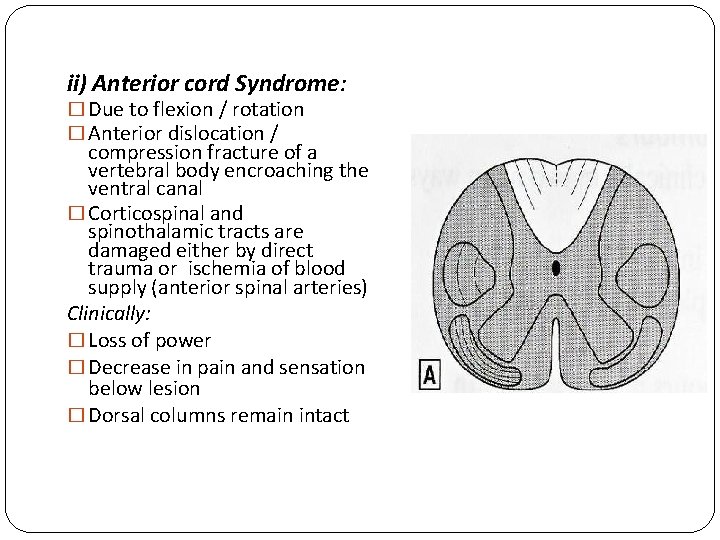
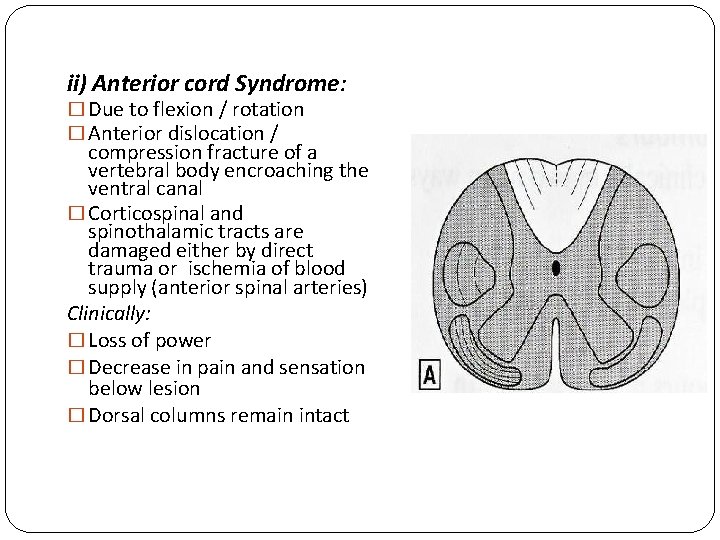
ii) Anterior cord Syndrome: � Due to flexion / rotation � Anterior dislocation / compression fracture of a vertebral body encroaching the ventral canal � Corticospinal and spinothalamic tracts are damaged either by direct trauma or ischemia of blood supply (anterior spinal arteries) Clinically: � Loss of power � Decrease in pain and sensation below lesion � Dorsal columns remain intact
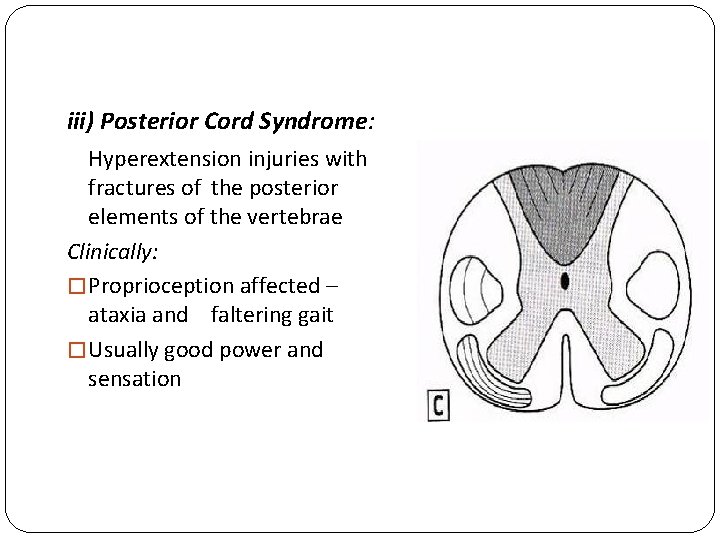
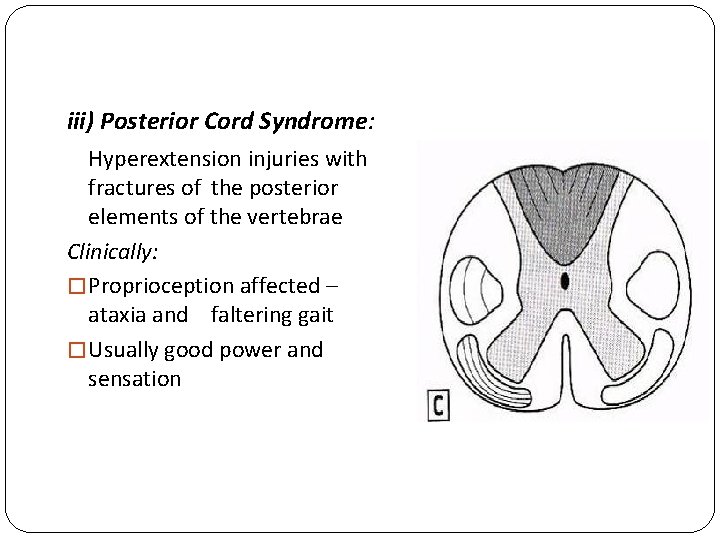
iii) Posterior Cord Syndrome: Hyperextension injuries with fractures of the posterior elements of the vertebrae Clinically: � Proprioception affected – ataxia and faltering gait � Usually good power and sensation
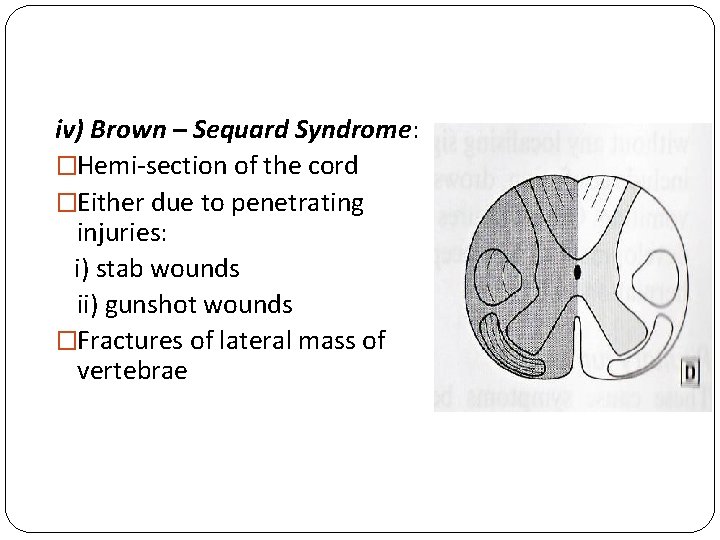
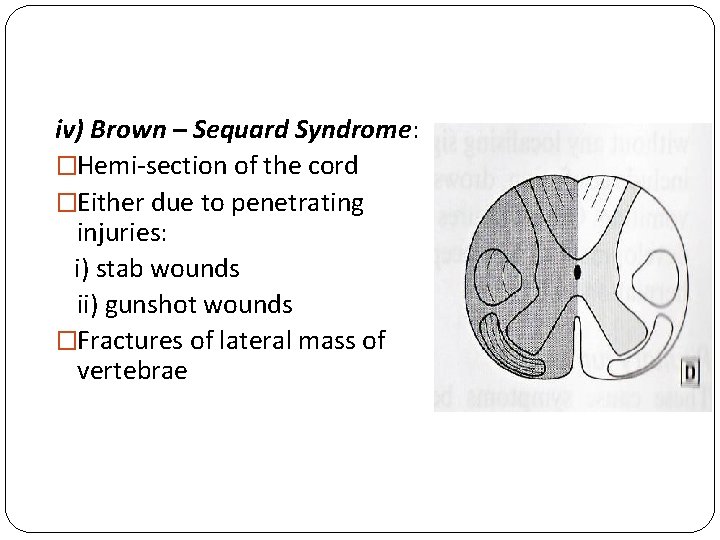
iv) Brown – Sequard Syndrome: �Hemi-section of the cord �Either due to penetrating injuries: i) stab wounds ii) gunshot wounds �Fractures of lateral mass of vertebrae
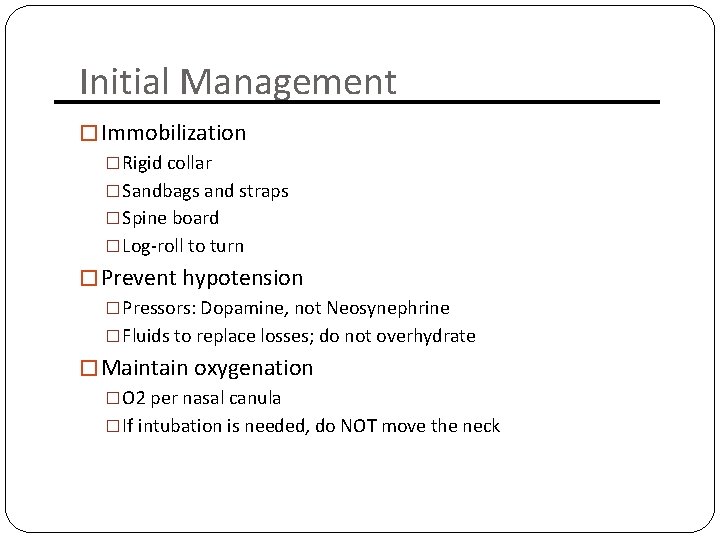
Initial Management � Immobilization �Rigid collar �Sandbags and straps �Spine board �Log-roll to turn � Prevent hypotension �Pressors: Dopamine, not Neosynephrine �Fluids to replace losses; do not overhydrate � Maintain oxygenation �O 2 per nasal canula �If intubation is needed, do NOT move the neck
Management in the hospital � NGT to suction �Prevents aspiration �Decompresses the abdomen (paralytic ileus is common in the first days) � Foley �Urinary retention is common � Methylprednisolone (Solu-Medrol) �Only if started within 8 hours of injury �Exclusion criteria � Cauda equina syndrome � GSW � Pregnancy � Age <13 years � Patient on maintenance steroids
CT scan �Good in acute situations �Shows bone very well �Sagittal reconstruction is mandatory �Soft tissues (discs, spinal cord) are poorly visualized �Do NOT give contrast in trauma patients (contrast is bright, mimicking blood)
MRI �Almost never an emergency �Exception: cauda equina syndrome �Shows tumors and soft tissues (e. g. , herniated discs) much better than CT scan �May be used to clear c-spine in comatose patients
Lumbar Puncture �Sedate the patient and make your life easier �Measure opening pressure with legs straight �Always get head CT prior to LP to r/o increased ICP or brain tumor
Long term care �Rehab for maximizing motor function �Bladder/bowel training �Psychological and social support
 Magnanimous noun
Magnanimous noun Spinal cord
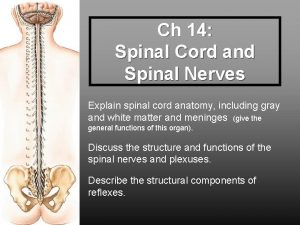
Spinal cord Figure 13-2 spinal nerves
Figure 13-2 spinal nerves Exercise 15 spinal cord and spinal nerves
Exercise 15 spinal cord and spinal nerves Cervical and brachial plexus
Cervical and brachial plexus Christopher reeve spinal cord injury level
Christopher reeve spinal cord injury level Eat well live well with spinal cord injury
Eat well live well with spinal cord injury Spinal cord injury protocol
Spinal cord injury protocol Spinal cord injury shoulder exercises
Spinal cord injury shoulder exercises Spinal cord injury rehabilitation st. louis
Spinal cord injury rehabilitation st. louis Somi brace
Somi brace How old are janie and jody now?
How old are janie and jody now? Spinal cord denticulate ligament
Spinal cord denticulate ligament Spinal cord structures
Spinal cord structures Hyporeflexia and hyperreflexia
Hyporeflexia and hyperreflexia Spinal cord tumors
Spinal cord tumors Pons function
Pons function Ventral root
Ventral root Scottie dog lumbar spine
Scottie dog lumbar spine Dorsal nerve cord notochord
Dorsal nerve cord notochord What covers spinal cord
What covers spinal cord Components of reflex arc
Components of reflex arc Vestibulospinal tract
Vestibulospinal tract Crossed extensor reflex
Crossed extensor reflex Osd sindrom
Osd sindrom What is the spinal cord made of
What is the spinal cord made of Spinal cord arterial supply
Spinal cord arterial supply Stretch reflex
Stretch reflex Mezgovnice
Mezgovnice Spinal cord
Spinal cord Stretch reflex
Stretch reflex Functions of spinal cord ppt
Functions of spinal cord ppt The spinebreal code
The spinebreal code Pain pathway spinal cord
Pain pathway spinal cord The spinal cord anatomy
The spinal cord anatomy Spinal cord cross section
Spinal cord cross section Spinal cord and brain
Spinal cord and brain Formation of csf
Formation of csf Spinal cord structure
Spinal cord structure Muscle spindle histology
Muscle spindle histology M supinator n radialis
M supinator n radialis