Sequelae of wearing complete dentures Contents n n


- Slides: 80
Sequelae of wearing complete dentures
Contents n n n n Introduction Soft tissues consideration Denture stomatitis Commisural chelitis Flabby ridge Traumatic ulcers Denture irritation hyperplasia Clicking Gagging Burning mouth syndrome Residual ridge reduction Overdenture abutments: caries &periodontal disease Indirect sequelae Conclusion References
Introduction n Placement of removable prosthesis in the oral cavity produces profound changes of the oral environment that may have an adverse effect on the integrity of oral tissues. n Mucosal reactions could result from a mechanical irritation by the dentures, an accumulation of microbial plaque on dentures or occasionally a toxic or allergic reaction to denture base material. n The continuous wearing of denture have a negative effect on residual ridges form because of bone resorption. Furthermore wearing dentures that function poorly and that impair masticatory function could be a negative factor with regard to maintenance of adequate muscle function and nutritional status
Interaction of prosthetic materials and oral environment n Surface properties of denture base affect plaque formation on the prosthesis. Irregularities or microporosities promote plaque accumulation. n Different materials in oral cavity may give rise to electrochemical corrosion. Corrosive galvanic currents is seen in B. M. S , oral lichen planus & in altered taste perception.
n Certain microorganism (yeast) are able to use methyl methacrylate as a carbon source thereby causing chemical degradation of denture resin. n Local irritation of mucosa by dentures may increase mucosal permeability to allergens or microbial antigen thereby capable of eliciting an allergic response
Soft tissue considerations n 1. Soft tissues supporting the dentures can be divided into 3 types Mucosa with a tightly attached submucosa : masticatory mucosa covering the crest and slopes of residual ridges & anterior third of palate in rugae area. They resist pressure and frictional impact of dentures.
2. Mucosa with loosely attached submucosa : located in vestibular fornix &soft palate distal to the palatine bones. They form a seal with the borders of dentures 3. Mucosa with differentiated submucosa : located in posterior third of hard palate , except for palatine raphae &in retromolar pad.
n 1. 2. The soft tissues that contact but do not support the dentures may be classified into 2 types: Lining mucosa : covering the cheeks, lips, undersurface of tongue, floor of mouth. Specialized mucosa : covers the dorsal surface of tongue.
1. Injuries to oral tissues occur principally in 3 areas: Tissues that support and resists stress. 2. Tissues that act to form a seal with denture borders. 3. Tissues that contact the polished surfaces and the teeth. n
Stress bearing mucosa n 1. 2. Signs and symptoms of traumatic injury to this area is as follows : Lesions occurring in the mucosa that covers the palate and the crest of residual ridges are small, well circumscribed and indurated. The presence of excessive keratin often causes the area to be white. Lesions that appear punched out & the surrounding mucosa hyperemic are a result of imperfections of denture base, trauma from food particles or an injury produced when the dentures were not in mouth.
3. Lesions that are hyperemic & painful to the pressure of closure are usually the result of pressure directed toward an area of exostosis , spur of bone or a foreign body. 4. Severe irritation and detaching of overlying mucosa occurs occasionally over mylohyoid ridge, cuspid eminences, alveolar tubercles &areas of exostosis. caused by denture flanges during insertion or removal of denture or from excessive friction during function. 5. Hyperemic , painful and detached areas of epithelium that develop on the slope of residual ridges due to occlusal disharmony.
Basal seat mucosa n n 1. 2 problems associated are hypertrophy and inflammation. Inflammatory reactions covering the basal seat are the result of the following: Continuous wear of dentures Generalized hyperemia of crest and slopes of the ridges accompanied by pain in the muscles attached to mandible, the production of hyperkeratin, looseness of dentures as a result of insufficient inter occlusal distance
3. 4. 5. 6. 7. 8. Presence of loosely attached submucosa results in friction of underlying bone against the undersurface of the mucosa when the dentures glide on mucosa thereby producing inflammation. Complete denture opposite natural dentition or partial denture causes localized hyperemia and edema. Poor oral hygiene Unbalanced diet and avitaminosis Endocrine gland disturbances, systemic diseases Allergic reactions to denture base materials
Transitional submucosa n Hypertrophy occur in area of transitional submucosa such as border extensions. results due to unpolished or sharp borders. n Lesions appear as slit like fissures, varying length and depth , painful and often become ulcerated.
Lining mucosa n Abrasions appear on mucosa of cheeks and lips are frequently the result of : 1. cheek biting. 2. Rough margins on the teeth. 3. Unpolished denture bases.
Specialized mucosa n 1. 2. 3. Ulcerations and other lesions appearing on the margins and apex of tongue are results of: Tongue biting often caused by improper placement of teeth either in horizontal or vertical position. An unpolished denture base or a too pronounced rugae area. Rough margins on teeth.
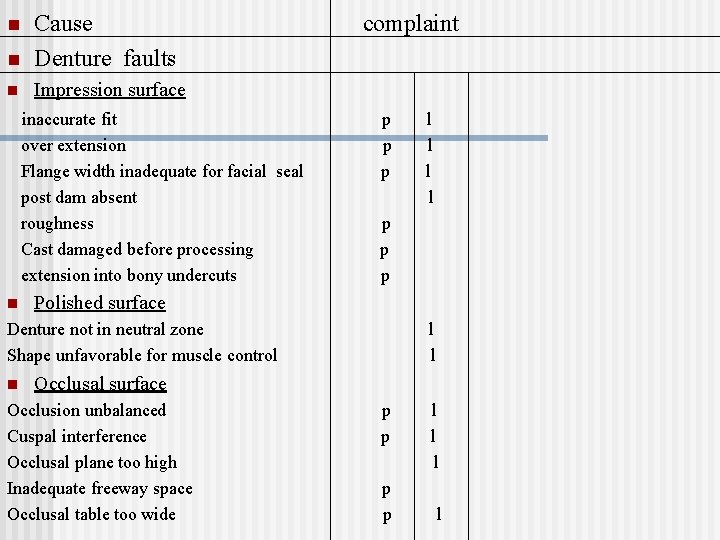
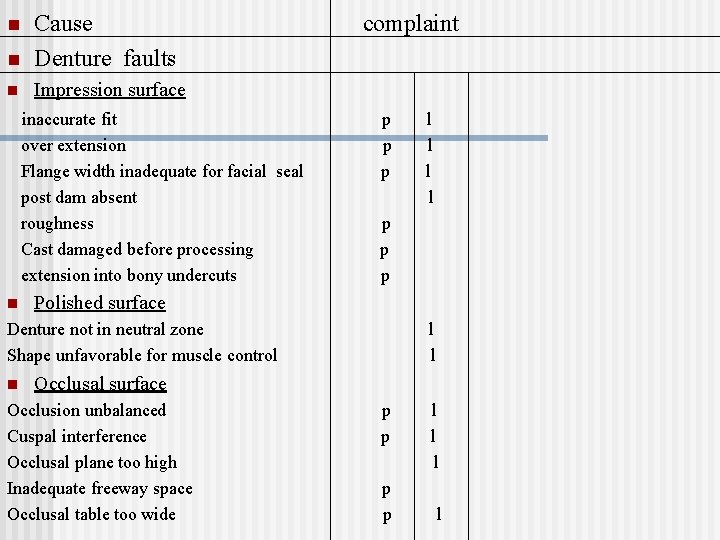
n Cause Denture faults n Impression surface n inaccurate fit over extension Flange width inadequate for facial seal post dam absent roughness Cast damaged before processing extension into bony undercuts n complaint p p p Polished surface Denture not in neutral zone Shape unfavorable for muscle control n l l l Occlusal surface Occlusion unbalanced Cuspal interference Occlusal plane too high Inadequate freeway space Occlusal table too wide p p l l
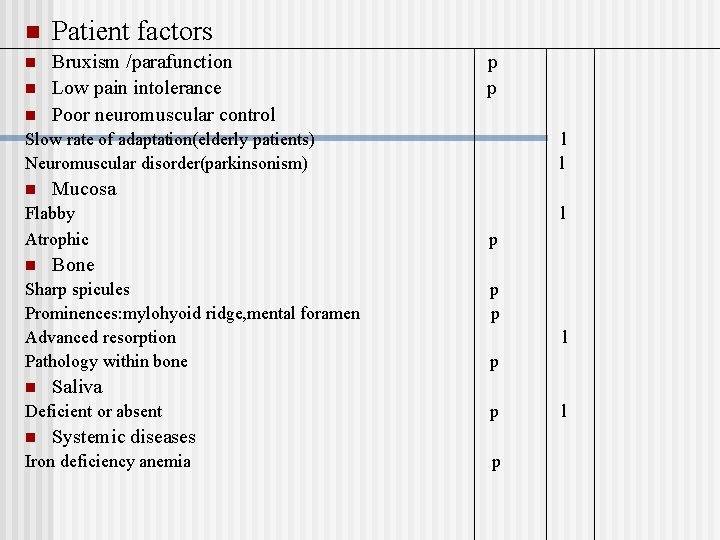
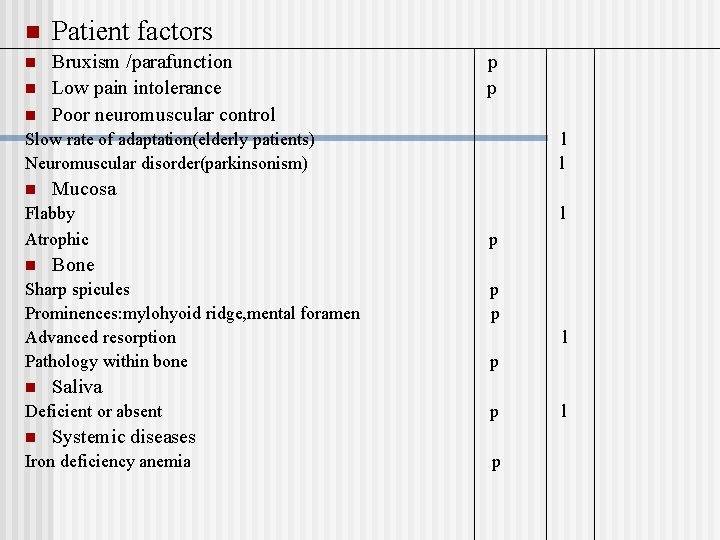
n Patient factors n Bruxism /parafunction Low pain intolerance Poor neuromuscular control n n p p Slow rate of adaptation(elderly patients) Neuromuscular disorder(parkinsonism) n Mucosa Flabby Atrophic n p p p l p Saliva Deficient or absent n l Bone Sharp spicules Prominences: mylohyoid ridge, mental foramen Advanced resorption Pathology within bone n l l p Systemic diseases Iron deficiency anemia p l
Direct sequelae Mucosal reactions n Oral galvanic currents n Altered taste perception n Burning mouth syndrome n Gagging n Residual ridge reduction n Periodontal disease & caries of abutments n
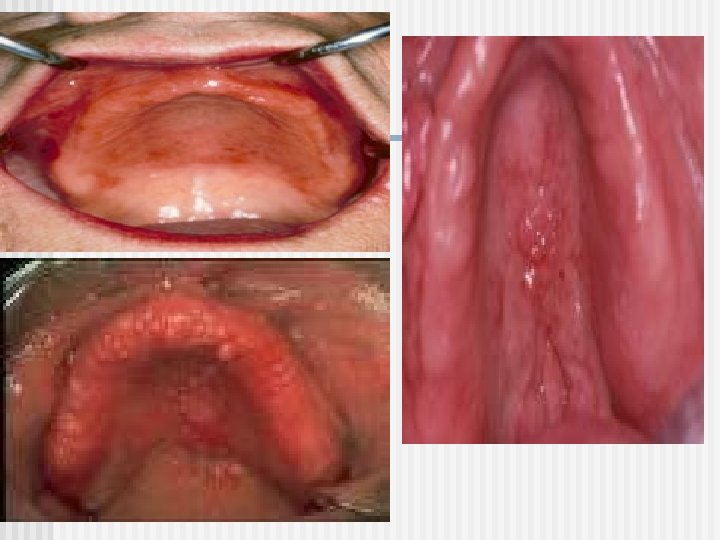
Denture stomatitis Newton’s classification Type I: localized simple inflammation or pinpoint hyperemia Type II: An erythematus or generalized simple type seen as more diffuse erythema involving a part or entire denture covered mucosa Type III: granular type involving central part of hard palate and alveolar ridges
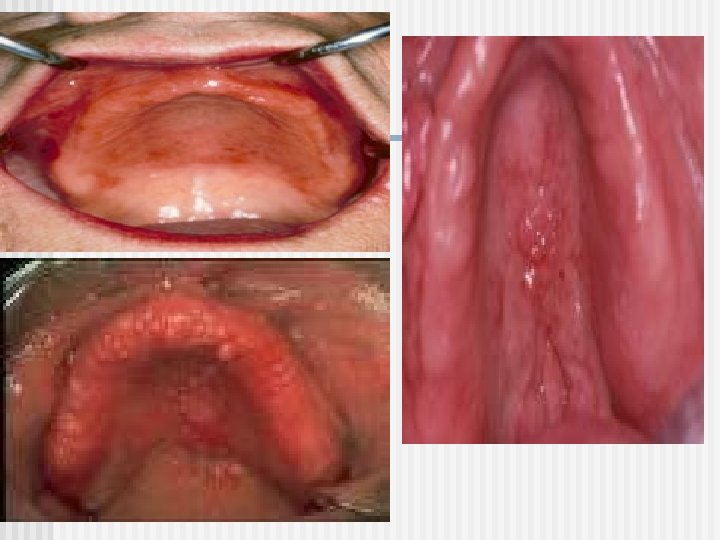
Etiology n Type I is trauma induced whereas types II & III are caused by presence of microbial plaque accumulation(bacteria or yeast) on the fitting denture surface & the underlying mucosa n The direct predisposing factor for candida associated denture stomatitis is presence of dentures in oral cavity. n Kulak Y, Arikan A(1993) found that there was a statistically significant relationship between denture stomatitis and denture hygiene, smoking habits, candidal formation and colonization.
n It is seen the major part of microorganisms of denture plaque are also involved. In addition trauma could stimulate turnover of palatal epithelial cells thereby reducing the degree of keratinization and barrier function of epithelium thus the penetration of fungal and bacterial antigens takes place more easily
Colonization of fitting denture surface by candida species depends on : n Adherence of yeast cells Interaction with oral commensal bacteria Surface properties of acrylic resins Poor oral hygeine High carbohydrate intake Reduced salivary flow Continous denture wear
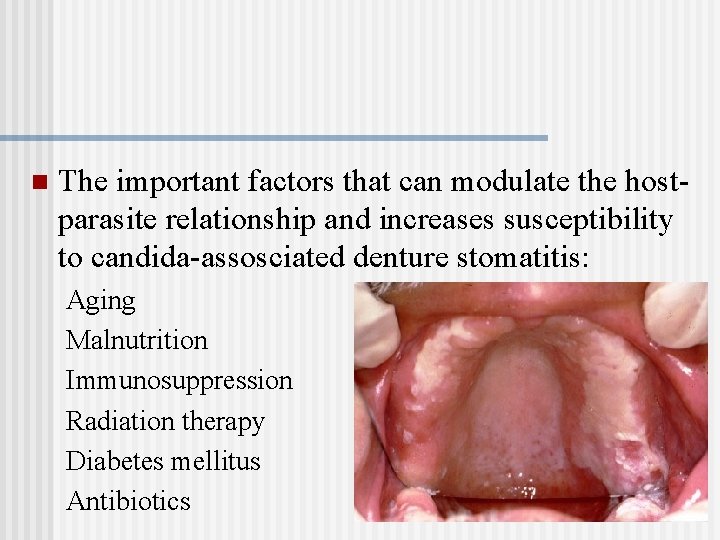
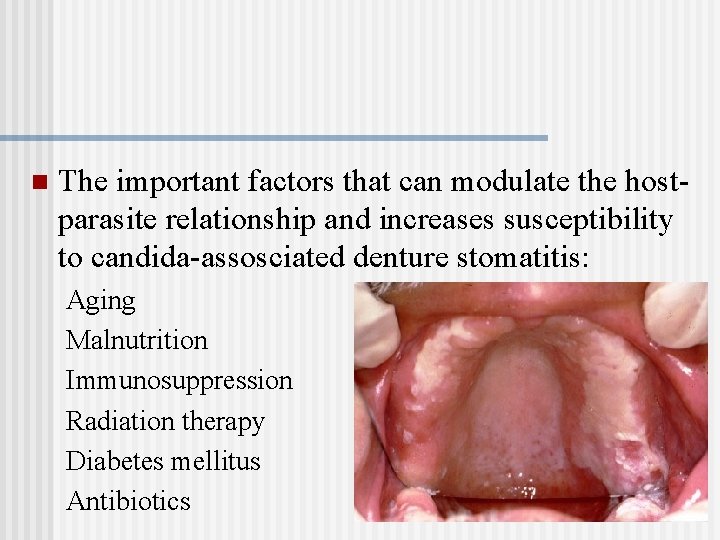
n The important factors that can modulate the hostparasite relationship and increases susceptibility to candida-assosciated denture stomatitis: Aging Malnutrition Immunosuppression Radiation therapy Diabetes mellitus Antibiotics
Diagnosis n Confirmed by finding of mycelia or pseudohyphae in a direct smear of isolation of candida species in high numbers(>50 colonies)
Management and preventive measures Institution of efficient oral and denture hygiene and correction of denture wearing habits n Patient instructed to remove dentures after meal and scrub them vigorously with soap before reinserting them n
The mucosa in contact with denture should be kept clean and massaged with a soft toothbrush. n Patients with recurrent infections should be persuaded not to use the dentures at night but rather leave them exposed to air. n
Rough areas on the fitting surface should be smoothened or relined with a soft tissue conditioner n About 1 mm of internal surface being penetrated by microorganisms should be removed and relined n Polishing or glazing of tissue surface of denture should be done n
n Treatment with antifungal agents is used in the following patients: 1. In patients after the clinical diagnosis is confirmed by mycological examination In patients with associated burning sensation of oral mucosa In patients in whom the infection has spread to other sites of oral cavity or pharynx Patients with increased risk of systemic mycotic infections due to debilitating diseases, drugs or radiation therapy 2. 3. 4.
n Local therapy with nystatin, amphotercin B, miconazole or clotrimazole is preferred to systemic therapy with ketoconazole or fluconnazole because resistance of candida species to latter drugs occurs regularly
n Treatment with antifungals should continue for 4 weeks n When lozenges are prescribed, the patient should be instructed to take out dentures during sucking n The patient should be instructed meticulous oral and denture hygiene; the patient should be told to wear denture as seldom as possible & to keep them dry or in disinfectant solution of 0. 2%-2% chlorhexidine during nights
n Surgical elimination of deep crypt formations in type III denture stomatitis is a prerequisite for effective mucosal hygiene. Achieved with cryosurgery
Commisural cheilitis n Inflammation of the angles of mouth. n Attributed to excessive interocclusal distance. n It usually develops when occlusal plane of the lower teeth is too high. This prevents the regular action of the cheek from eliminating the saliva from the lower buccal vestibule, so saliva will exit through the corners of mouth indicating spread of infection to the angles of mouth. n Advisable to construct new dentures

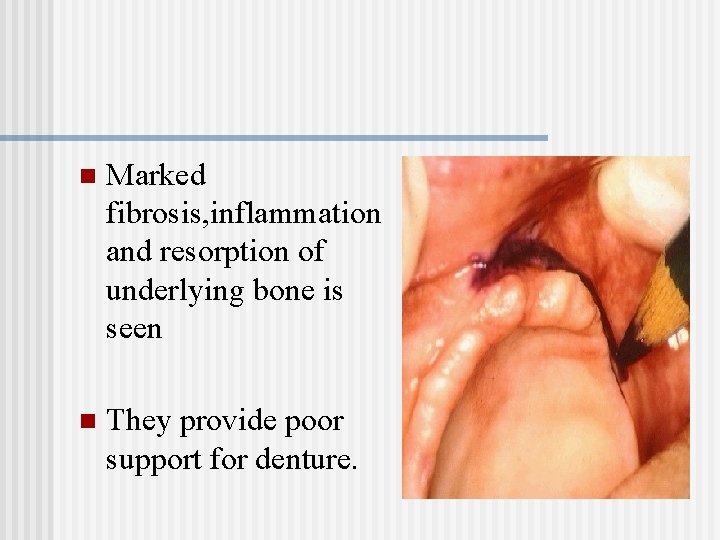
Flabby ridge n Flabby ridge(mobile or extremely resilient alveolar ridge) is due replacement of bone by fibrous tissue. n Seen in anterior part of maxilla, probably sequelae of excessive load of residual ridge and unstable occlusal conditions.
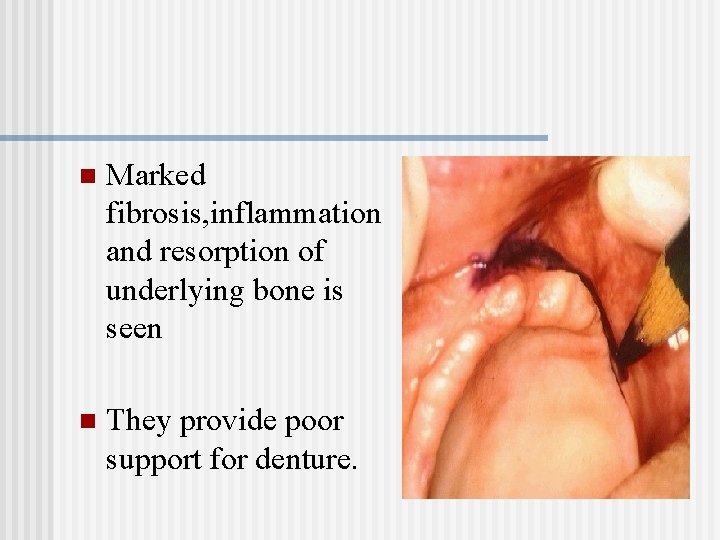
n Marked fibrosis, inflammation and resorption of underlying bone is seen n They provide poor support for denture.
n To improve stability of denture and minimize ridge resorption , the tissue should be surgically removed. n In situation of extreme atrophy of maxillary alveolar ridge, flabby ridges should not be totally removed because the vestibular area would be eliminated
Traumatic ulcers n Develop within 1 -2 days after placement of new dentures. n Small painful lesions, covered by a gray necrotic membrane and surrounded by an inflammatory halo with firm , elevated borders. n Caused due to overextended denture flanges or unbalanced occlusion.
n Conditions that suppress resistance of mucosa to mechanical irritation are predisposing factors. e. g, diabetes mellitus, nutritional deficiences, radiation therapy or xerostomia. n In a non –compromised host ulcers will heal after correction of dentures. When left untreated, it subsequently develops into denture irritation hyperplasia.
Denture Irritation Hyperplasia n Common sequelae of wearing ill-fitting dentures is occurrence of tissue hyperplasia of mucosa in contact with denture border n Lesions are a result of chronic injury by unstable dentures or by thin , overextended denture flanges. n Lesions may be single or quite numerous and are composed of flaps of hyperplastic connective tissue.
n Inflammation is variable; however in bottom of deep fissures, severe inflammation may occur. n Treatment is adjustment or replacement of denture. surgical excision of hyperplastic tissues n If lymphadenopathy is present, the denture irritation hperplasia may simulate a neoplastic process.
Clicking n A clicking noise when teeth contact during functional movements is a result of insufficient interocclusal distance, vertical displacement of mandibular denture.
n 1. 2. 3. Treatment : Correct stability and retention by rebasing or remaking the dentures. If dentures are not loose, if sufficent interocclusal distance exists, and if teeth are porcelain, replace the porcelain teeth with acrylic resin teeth. When interocclusal distance is not sufficient, alter the occlusal surfaces of teeth with remount procedures to provide adequate space
Gagging n Stimulation of sensitive areas in posterior pharyngeal wall, soft palate, uvula, fauces or the posterior surface of tongue results in series of uncoordinated and spasmodic movements of swallowing muscles. This is referred to as gagging
n 1. 2. 3. 4. Complete denture patient may develop gagging as a result of: Loose dentures Poor occluion Incorrect extension or contour of dentures particularly in posterior area of palate and retromylohyoid space. Under extended denture borders.
5. 6. 7. Placing the maxillary teeth too far in a palatal direction and the mandibular teeth too far in lingual direction so that the dorsum of tongue is forced into pharynx during the act of swallowing Increased vertical dimension of occlusion Psychogenic factors
Treatment n n n Determine the cause Eliminate the biological and mechanical factors that contribute to the problem. Prescribe a combination of hyoscine, hyoscyamine and atropine with a sedative during initial period of denture use.
Burning mouth syndrome n Characterized by a burning sensation in one or several oral structures in contact with dentures. n Symptoms often appear for first time in association with placement of new dentures. n Common sites are tongue and upper denture bearing tissues. Less common sites are the lips and lower denture bearing tissues. Oral mucosa appears normal.
Classification n 1. 3 types of BMS have been described by Lamey & Lewis 1989 Type I: There are no symptoms on waking. A burning sensation then commences and becomes worse as the day progresses. This pattern occurs everyday. 33% of patients fall into this category and are likely to include those haematinic deficiencies and defects in denture designs.
2. Type II : Burning is present on waking and persists throughout the day. Occurs everyday. About 55% of patients are placed in this category, a high proportion of whom have chronic anxiety and are most difficult to treat successfully. 3. Type III : Patients have symptom – free days. Burning occurs in less usual sites such as floor of mouth, throat & buccal mucosa. Main causative factors are allergy & emotional instability (Lamey et al. 1994). They make up for the remaining 12% of patients.
Causes n Local factors: mechanical irritation , allergy due to residual monomer , infection , oral habits and parafunction , myofascial pain. n Errors in denture design which cause a denture to move excessively over the mucosa which increase the functional stress on the mucosa or which interfere with the freedom of movement of the surrounding muscles may initiate a complaint of burning rather than soreness. Seen in 50% of BMS patients
n Systemic factors: vitamin deficiency , iron deficiency anemia , xerostomia , menopause, diabetes, parkinson’s diseases, medication. n Psychogenic factors: depression, anxiety and psychosocial stressors.
Management n n n n Initial assesment (history/examination/special test) Provisional diagnosis Initial treatment(elimination of local irritants & investigating &treating haematinic deficiencies) Assessment of initial treatment Definitive diagnosis Definitive treatment (local/systemic/psychological therapy) Follow -up
Residual ridge reduction Residual ridge resorption (GPT 7): A term used for the diminishing quantity and quality of the residual ridge after teeth are removed. Continous bone loss after tooth extraction and placement of complete denture is seen. Reduction is a sequel of alveolar remodeling due to altered functional stimulus of bone tissue. It is a progressive and irreversible course that results in impairment of prosthesis and oral function
The process of resorption is important in areas with thin cortical bone(e. gbuccal and labial plates of maxilla and lingual plate of mandible). The annual rate of reduction in height in mandible is about 0. 1 -0. 2 and in general four times less in edentulous maxilla.
CLASSIFICATIONS OF RESIDUAL RIDGE RESORPTION According to Brånemark et al in 1985, ridges were classified on the basis of bone quantity and bone quality by radiographic means. BONE QUANTITY: (Brånemark) Class A: Most of the alveolar bone is present Class B: Moderate Residual Ridge Resorption occurs Class C: Advance residual ridge resorption occurs Class D: Moderate resorption of the basal bone is present Class E: Extreme resorption of the basal bone
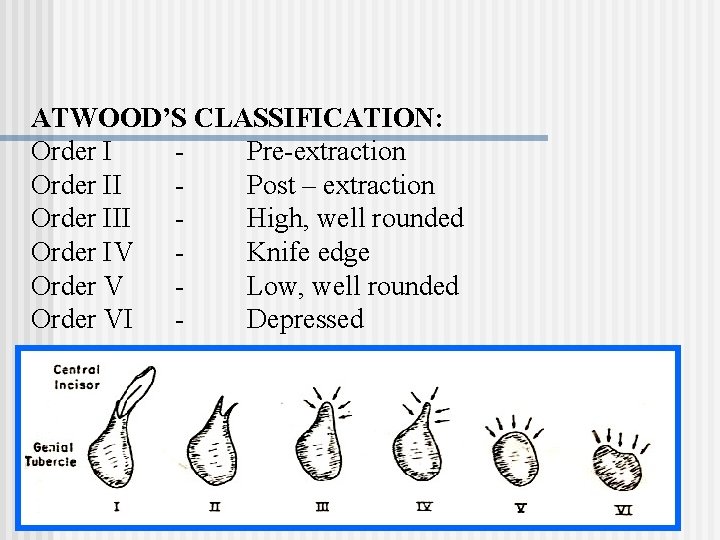
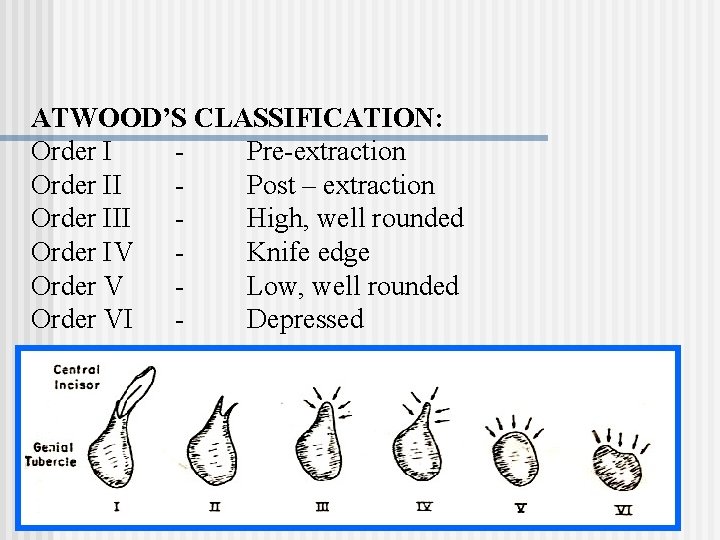
ATWOOD’S CLASSIFICATION: Order I Pre-extraction Order II Post – extraction Order III High, well rounded Order IV Knife edge Order V Low, well rounded Order VI Depressed
Etiological factors of residual ridge reduction n n Anatomical factors Important in mandible versus maxilla Short and square face associated with elevated masticatory forces Alveoloplasty Prosthodontic factors Intensive denture wearing Unstable occlusal conditions
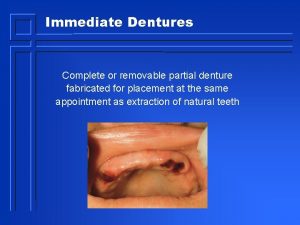
Immediate denture treatment n n Metabolic and systemic factors Osteoporosis Mechanical factors transmitted by dentures or tongue to the residual ridges results in remodeling process.
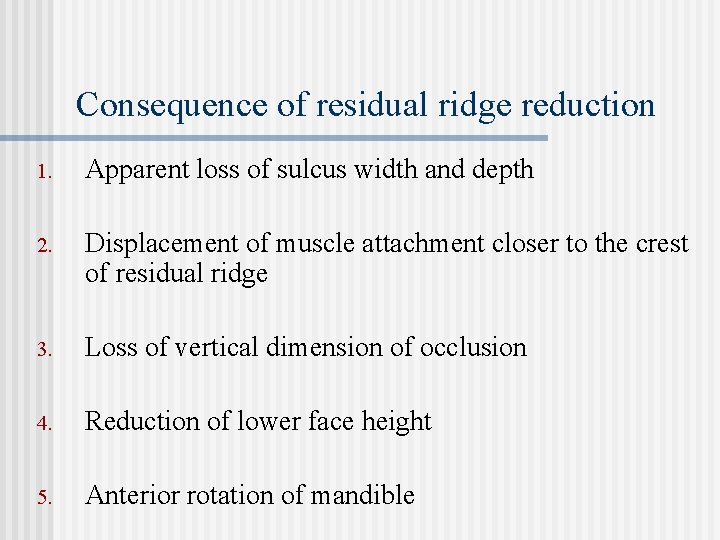
Consequence of residual ridge reduction 1. Apparent loss of sulcus width and depth 2. Displacement of muscle attachment closer to the crest of residual ridge 3. Loss of vertical dimension of occlusion 4. Reduction of lower face height 5. Anterior rotation of mandible
6. Increase in relative prognathia. 7. Changes in interalveolar ridge relationship after progression of residual ridge reduction. 8. Morphological changes of alveolar bone such as sharp, spiny, uneven residual ridges and location of mental foramen to the top of residual ridge.
n Rogers and Applebaum (1941) concluded from measurements made in cadavers with dentulous and edentulous jaws that in the maxillae the vertical height of the ridges had decreased and the crest of the edentulous ridges had shifted palatally after tooth extraction. They felt that in the mandible the most extensive resorption of the alveolar bone occurred on the superior surface of the ridge and on the lingual surface of the posterior part of the ridge.
n Tylman and Tylman (1960) found that in the maxillae, the labial and the buccal alveolar plates resorb much faster than the palatal plates, while in the mandible the amount of bone resorbed in the lingual and labial are approximately the same
Treatment Pre-prosthetic surgery includes the following: § Ridge preservation procedure as a preventive measure. § Corrective or recontouring procedures of the defects and abnormalities. § Ridge extension procedures: Relative methods Eg. sulcus extension (vestibuloplasty) Absolute methods Eg. Ridge augmentation methods.
§ § § Reconstruction methods like correction of abnormal ridge relationship. Provision of accessory undercuts. Creating favorable undercuts Dental implants. Onlay denture. Modified denture construction procedure Eg. Immediate denture where construction of the denture proceeds surgery
The Ø Ø prosthetic factors to be considered include broad area coverage (to reduce the force per unit area decreased number of dental units, decreased buccolingual width of teeth, and Ø improved tooth form (to decrease the amount of force required to penetrate a bolus of food); Ø avoidance of inclined planes (to minimize dislodgement of dentures and shear forces); Ø centralization of occlusal contacts (to increase stability of dentures and to maximize compressive forces); Ø provision of adequate tongue room (to improve stability of denture in speech and mastication); Ø adequate inter-occlusal distance during rest jaw relation (to decrease the frequency and duration of tooth contacts)
Overdenture abutments: caries and periodontal disease n Wearing of overdentures is often associated with a high risk of caries and progression of periodontal disease of abutment teeth. n This is due to bacterial colonization beneath a close fitting denture is enhanced, and good plaque control of fitting denture surface is difficult to obtain. n Predominant micro organisms are streptococcus, lactobacilli and actinomyces.
n n These species initiate gingivitis after 1 -3 days of plaque accumulation when oral hygiene is discontinued. Presence of streptococcus mutans and lactobacilli in dental plaque flora in high proportions results in caries.
Management n Abstain from wearing dentures in the night. n Application of flouride-chlorhexidine gel and polishing, mechanical & chemical plaque control. n Placement of copings that cover the exposed dentin and root surface is indicated where caries is more deeply penetrating. This is to reduce risk of new or recurrent caries. n Periodontal pockets greater than 4 -5 mm should be surgically eliminated
Indirect sequelae: atrophy of masticatory muscles n n n Masticatory function depends on the skeletal muscular force and the facility with which the patient is able to coordinate oral functional movements during mastication In complete denture wearers, particularly in women atrophy of masseter and medial pterygoid muscle is seen The decrease in bite force and chewing efficiency results in impaired masticatory function.
Preventive measures & management n Retention of a small number of teeth used as overdenture abutments helps in maintenance of oral functions. n In completely edentulous patients , placement of implants is usually followed by an improvement of masticatory function & an increase of maximal occlusal forces.
Nutritional status and masticatory functions 1. 4 factors are related to dietary selection and nutritional status of wearers of complete dentures: Masticatory function and oral health 2. General health 3. Socio-economic status 4. Dietary habits n
Management 1. Re-education of elderly denture wearers regarding dietary habits. 2. Replacement of ill-fitting dentures. 3. Mechanical preparation of food before eating will help mastication and reduce its influence on food selection.
Conclusion n The essential consequences of wearing complete dentures are reduction of residual ridges and pathological changes of oral mucosae. This results in poor patient comfort, destabilization of occlusion , insufficient masticatory function and esthetic problems.
n Effort should be made to retain some teeth in strategically good positions to serve as overdenture abutments. The maintenance of tooth roots in mandible is important. n The patient should follow a regular follow - up schedule at yearly interval so that an acceptable fit and stable occlusion can be maintained
n Patients should be aware of implant supported prosthesis. In young patients, advantage would be reduced residual ridge reduction. In elderly patients , the main advantage are improved comfort and maintenance of masticatory function. n Patient should be motivated to practice proper denture wearing habits and maintenance of oral hygiene and follow a program of recall and maintenance for continuous monitoring of dentures and oral tissues.
References n n n Zarb –Bolender : Prosthodontic treatment for edentulous patients, 12 th edition. Arthur. Rahn. O, Charles. Heartwell. M, Jr: Textbook of complete dentures, 5 th edition. Sheldon Winkler: Essentials of complete denture prosthodontics, 2 nd edition. Basker RM & Davenport JC: Prosthetic treatment of edentulous patient, 4 th edition. Tallegren A: The continuing reduction of the residual alveolar ridges in complete denture wearers: mixed longitudinal study covering 25 yrs, J Prosthet Dent 27: 120 -132, 1972.
n n n Budtz-Jorgensen E: Oral mucosal lesions assosciated with wearing of removable dentures, J Oral Path 10: 65 -80, 1981. Conny DJ, Tedesco LA: The gagging problem in prosthodontic treatment, Part I: description & causes, J Prosthet Dent 49: 601606, 1983. Hillerup S: Preprosthetic surgery in the elderly , J Prosthet Dent 72: 551 -558, 1994.

 Indirect sequelae of wearing complete denture
Indirect sequelae of wearing complete denture Direct sequelae of wearing complete denture
Direct sequelae of wearing complete denture Dentsply denture teeth mould guide
Dentsply denture teeth mould guide Swensons technique of occlusal modification
Swensons technique of occlusal modification Protrusive relation record
Protrusive relation record Gingival approach clasp
Gingival approach clasp Direct retainer classification
Direct retainer classification Gaten matarazzo dentures
Gaten matarazzo dentures Guide planes in rpd
Guide planes in rpd Fovea palatini
Fovea palatini Retainer partial denture
Retainer partial denture Ch 52 removable prosthodontics fill in the blank
Ch 52 removable prosthodontics fill in the blank Rpd design class 3 mod 1
Rpd design class 3 mod 1 Spoon denture indication
Spoon denture indication Larell dentures
Larell dentures Hamular notch of maxilla
Hamular notch of maxilla Every denture vs spoon denture
Every denture vs spoon denture Altered cast technique indications
Altered cast technique indications Cellular events of inflammation
Cellular events of inflammation Interceptive orthodontics
Interceptive orthodontics Bacterial growth
Bacterial growth Simple subject and complete subject
Simple subject and complete subject History of wearing floral designs as personal adornment
History of wearing floral designs as personal adornment Sentence with drizzle
Sentence with drizzle Paper doll ppe
Paper doll ppe Why are you wearing
Why are you wearing Clive wearing
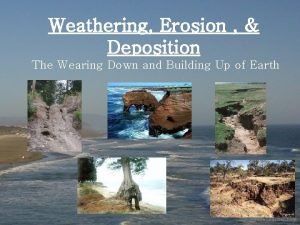
Clive wearing Compare and contrast mechanical and chemical weathering
Compare and contrast mechanical and chemical weathering Let discuss what is wearing
Let discuss what is wearing The waiter was rude. the waiter was wearing a blue shirt
The waiter was rude. the waiter was wearing a blue shirt Intrinsic plus position
Intrinsic plus position Wearing goggles
Wearing goggles History of wearing floral designs as personal adornment
History of wearing floral designs as personal adornment Pedestrian wearing reflective clothing and red light
Pedestrian wearing reflective clothing and red light Midterm break
Midterm break Old dirty flannel
Old dirty flannel Ultra thin bonded wearing course
Ultra thin bonded wearing course I am wearing song
I am wearing song Poem on importance of clothes
Poem on importance of clothes Clive wearing
Clive wearing Wearing different hats in business
Wearing different hats in business A student wearing frictionless in line skates
A student wearing frictionless in line skates Strength of the multi store model
Strength of the multi store model They are usually wearing coats in winter
They are usually wearing coats in winter Where am i wearing
Where am i wearing Bearing mcq
Bearing mcq Ambulated side
Ambulated side Family and friends 2 what are you wearing
Family and friends 2 what are you wearing Lee what are you wearing
Lee what are you wearing It was so cold i saw polar bears wearing jackets
It was so cold i saw polar bears wearing jackets Wearing a hair shirt
Wearing a hair shirt What are you wearing family and friends 2
What are you wearing family and friends 2 Contents provider
Contents provider Contents of internal capsule
Contents of internal capsule Atom table of contents
Atom table of contents Cubital fossa contents
Cubital fossa contents Ip contents
Ip contents Popliteal fossa
Popliteal fossa Contents of audit planning memorandum
Contents of audit planning memorandum Annexure to cost audit report
Annexure to cost audit report What does key characteristics mean
What does key characteristics mean Fresh frozen plasma contents
Fresh frozen plasma contents I-need-a-few-pointers-98hpou5
I-need-a-few-pointers-98hpou5 Composition notebook table of contents
Composition notebook table of contents Swot analysis event management
Swot analysis event management Iliopectineal groove
Iliopectineal groove Maudie's nutrition
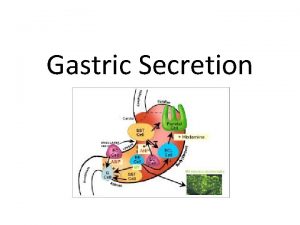
Maudie's nutrition Gastric secretion composition
Gastric secretion composition Main contents
Main contents Clipart table of contents
Clipart table of contents Anterior mediastinum contents
Anterior mediastinum contents Optab in assembler
Optab in assembler Contents background
Contents background Table of contents company profile
Table of contents company profile Importance of entrepreneurship development programme
Importance of entrepreneurship development programme Contents of inquiry
Contents of inquiry Omental tuberosity of liver
Omental tuberosity of liver Table of contents for tourism
Table of contents for tourism Brachialis
Brachialis Contents of dentinal tubules
Contents of dentinal tubules Table of contents background
Table of contents background