Quality and Safety Education for Nurses 2007 Jowers

- Slides: 54
Quality and Safety Education for Nurses 2007 Jowers Lecture Linda Cronenwett, Ph. D, RN, FAAN December 5, 2007
Greetings from the University of North Carolina - Chapel Hill School of Nursing Quality and Safety Education for Nurses (QSEN) Linda Cronenwett Principal Investigator, Professor and Dean Gwen Sherwood Co-Investigator, Professor and Associate Dean for Academic Affairs
U. S. Institute of Medicine Quality Chasm Reports n To Err Is Human: Building a Safer Health System (2000) n Crossing the Quality Chasm: A New Health System for the 21 st Century (2001) n Health Professions Education: A Bridge to Quality (2003) n Patient Safety: Achieving a New Standard for Care (2004) n Identifying and Preventing Medication Errors (2007)
Development of Safety Sciences n Worldwide, scientists in other industries uncovering knowledge about the interventions that produced safe systems Lean, zero defect production systems n Aviation n Nuclear energy n n Health care remains committed to the ideal of the individual professional as source of quality and safety
Impetus for Change n Variations in outcomes shown to be related to systems of care rather than individual patient characteristics n U. S. hospitals adopt quality improvement and safety science methods in the late 1990’s n Health care professionals in hospitals taught, one by one, about quality and safety n Yet -n No health professions education on QI/safety
Impetus for Change in Nursing n People become nurses in order to relieve suffering and contribute to the overall health of communities and individuals n Quality care is an essential value n As nurses work in systems where quality is eroded, joy in work diminishes n Less joy in work leads to work force shortages n Health professionals run our systems -- they can improve our systems if they possess the competencies required to make improvement a part of daily work
Health Professions Education: A Bridge to Quality (2003) All health professionals should be educated to deliver patient-centered care as members of an interdisciplinary team, emphasizing evidencebased practice, quality improvement approaches, and informatics.
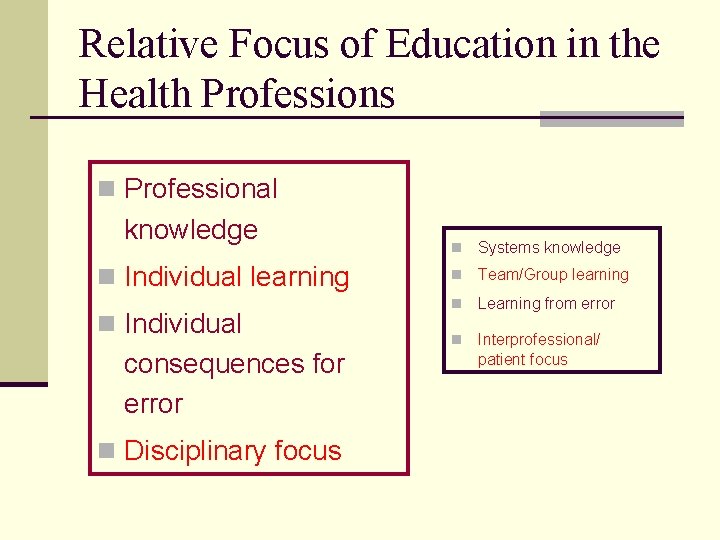
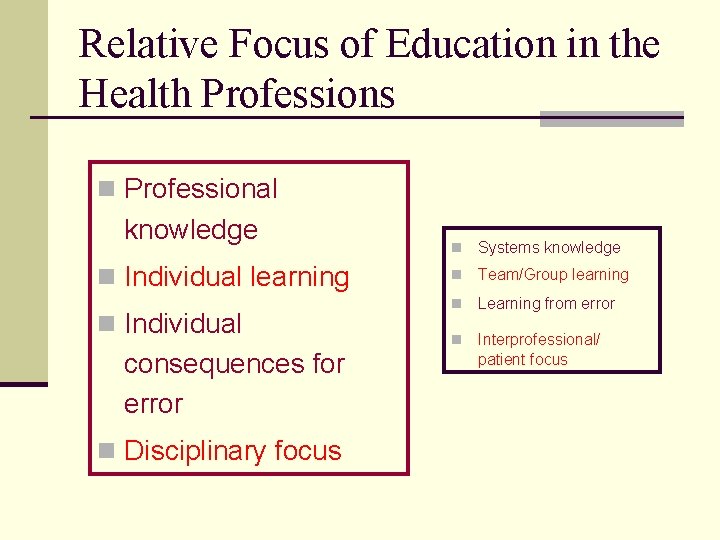
Relative Focus of Education in the Health Professions n Professional knowledge n Individual learning n Individual consequences for error n Disciplinary focus n Systems knowledge n Team/Group learning n Learning from error n Interprofessional/ patient focus
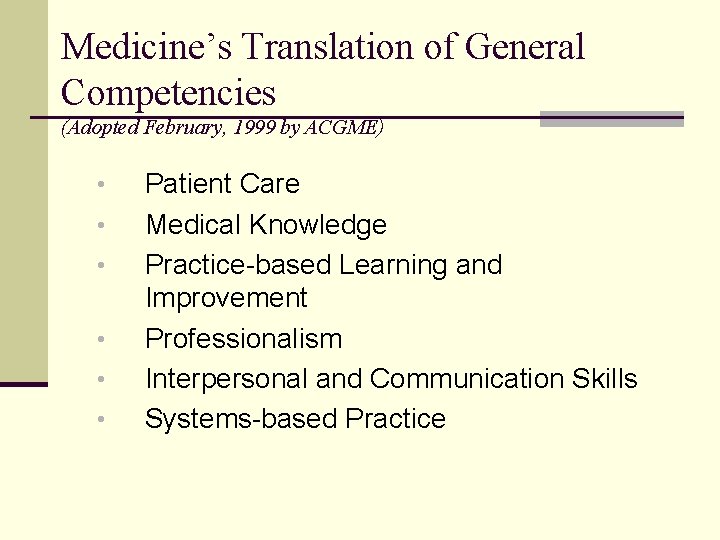
Medicine’s Translation of General Competencies (Adopted February, 1999 by ACGME) • • • Patient Care Medical Knowledge Practice-based Learning and Improvement Professionalism Interpersonal and Communication Skills Systems-based Practice
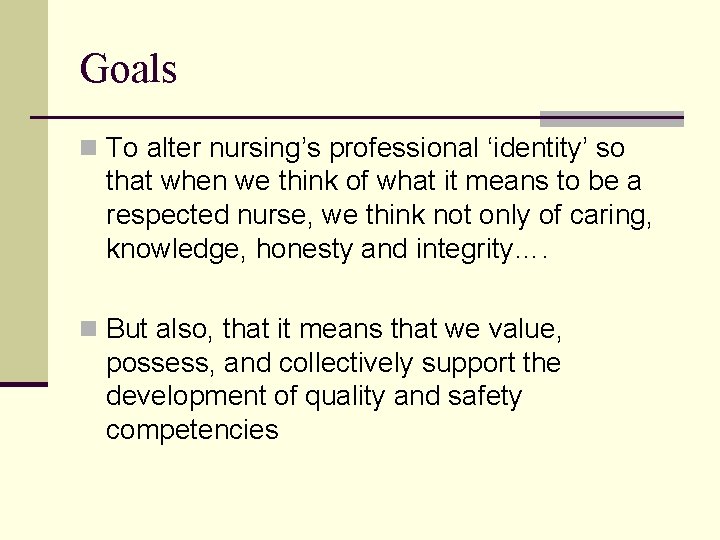
Goals n To alter nursing’s professional ‘identity’ so that when we think of what it means to be a respected nurse, we think not only of caring, knowledge, honesty and integrity…. n But also, that it means that we value, possess, and collectively support the development of quality and safety competencies
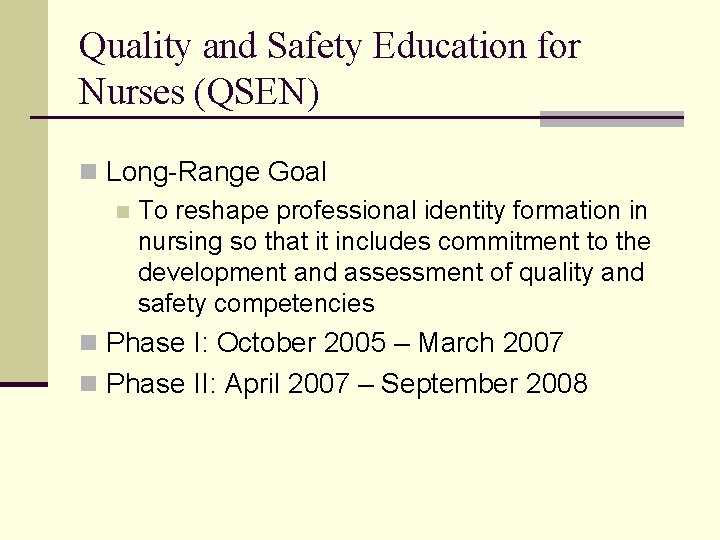
Quality and Safety Education for Nurses (QSEN) n Long-Range Goal n To reshape professional identity formation in nursing so that it includes commitment to the development and assessment of quality and safety competencies n Phase I: October 2005 – March 2007 n Phase II: April 2007 – September 2008
QSEN Personnel QSEN Leaders based in UNC-Chapel Hill n QSEN Faculty – Experts in quality and safety from throughout the U. S. n QSEN Advisory Board – Leaders of organizations that set standards for nursing regulation, certification, and accreditation of nursing programs n
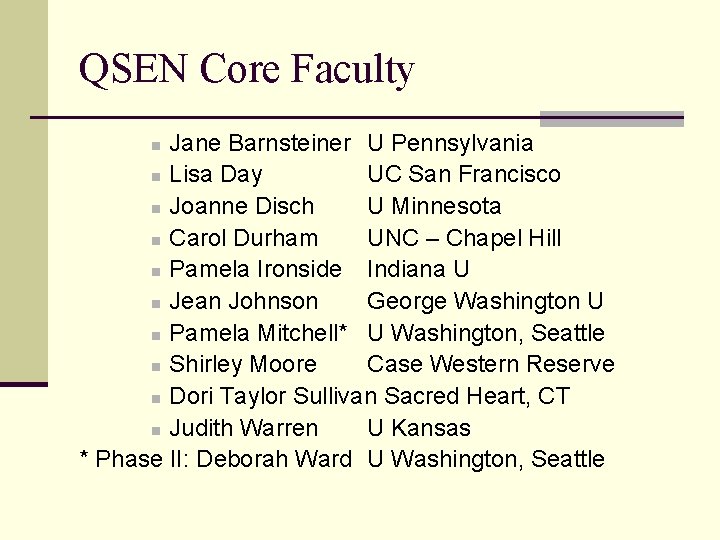
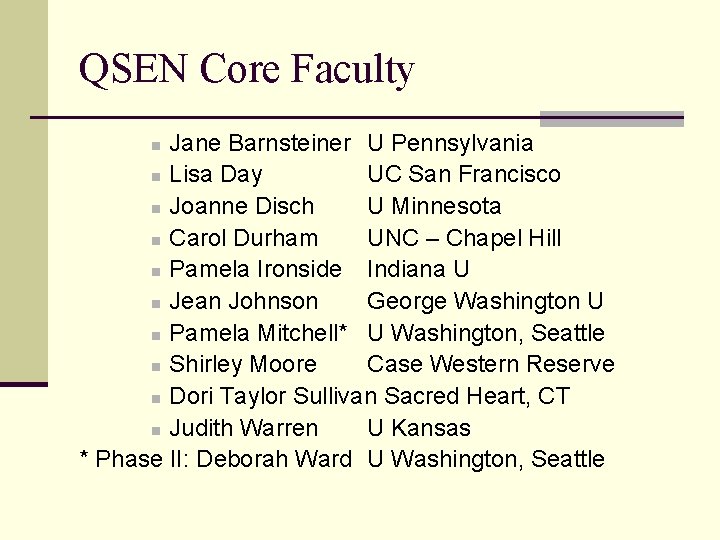
QSEN Core Faculty Jane Barnsteiner U Pennsylvania n Lisa Day UC San Francisco n Joanne Disch U Minnesota n Carol Durham UNC – Chapel Hill n Pamela Ironside Indiana U n Jean Johnson George Washington U n Pamela Mitchell* U Washington, Seattle n Shirley Moore Case Western Reserve n Dori Taylor Sullivan Sacred Heart, CT n Judith Warren U Kansas * Phase II: Deborah Ward U Washington, Seattle n
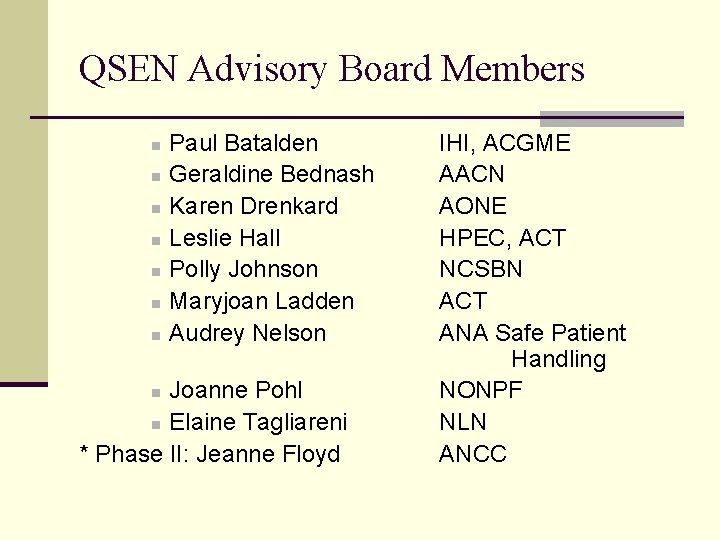
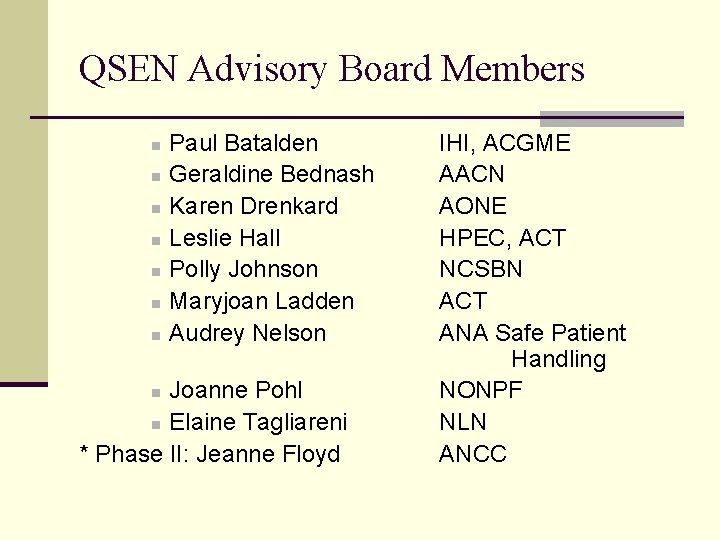
QSEN Advisory Board Members n n n n Paul Batalden Geraldine Bednash Karen Drenkard Leslie Hall Polly Johnson Maryjoan Ladden Audrey Nelson Joanne Pohl n Elaine Tagliareni * Phase II: Jeanne Floyd n IHI, ACGME AACN AONE HPEC, ACT NCSBN ACT ANA Safe Patient Handling NONPF NLN ANCC
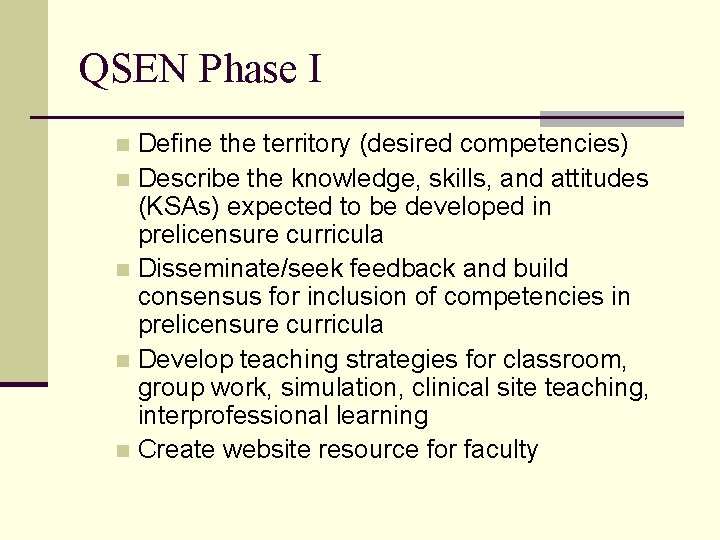
QSEN Phase I Define the territory (desired competencies) n Describe the knowledge, skills, and attitudes (KSAs) expected to be developed in prelicensure curricula n Disseminate/seek feedback and build consensus for inclusion of competencies in prelicensure curricula n Develop teaching strategies for classroom, group work, simulation, clinical site teaching, interprofessional learning n Create website resource for faculty n
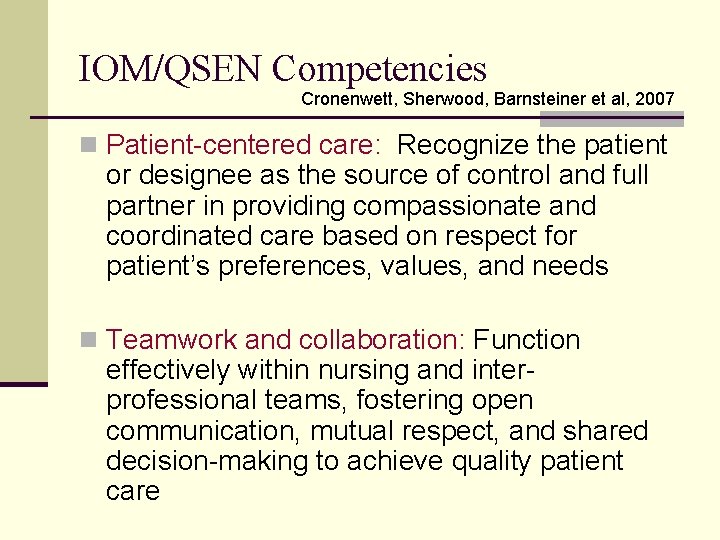
IOM/QSEN Competencies Cronenwett, Sherwood, Barnsteiner et al, 2007 n Patient-centered care: Recognize the patient or designee as the source of control and full partner in providing compassionate and coordinated care based on respect for patient’s preferences, values, and needs n Teamwork and collaboration: Function effectively within nursing and interprofessional teams, fostering open communication, mutual respect, and shared decision-making to achieve quality patient care
IOM/QSEN Competencies Cronenwett, Sherwood, Barnsteiner et al, 2007 n Evidence-based practice: Integrate best current evidence with clinical expertise and patient/family preferences and values for delivery of optimal health care n Quality improvement: Use data to monitor the outcomes of care processes and use improvement methods to design and test changes to continuously improve the quality and safety of health care systems
IOM/QSEN Competencies Cronenwett, Sherwood, Barnsteiner et al, 2007 n Safety: Minimize risk of harm to patients and providers through both system effectiveness and individual performance n Informatics: Use information and technology to communicate, manage knowledge, mitigate error, and support decision making
QSEN Assumptions n Competency definitions could serve the profession as: n n n Curricular threads Foci of accreditation of nursing programs Foci of licensure or certification exams Foci of transition to work (residency) program development Foci of criteria for recertification or relicensure
Current Assessments of Quality and Safety Education Smith, E. L. , Cronenwett, L. , & Sherwood, G. (2007). Current assessments of quality and safety education in nursing. Nursing Outlook, 55 (3), 132 -137.
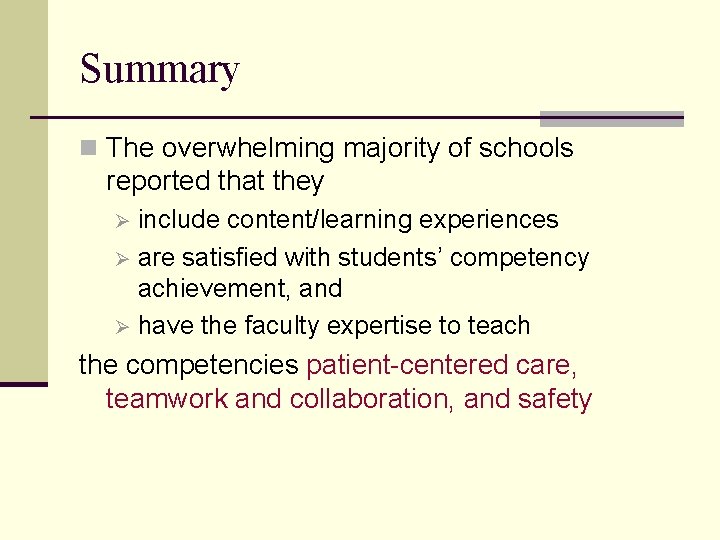
Summary n The overwhelming majority of schools reported that they include content/learning experiences Ø are satisfied with students’ competency achievement, and Ø have the faculty expertise to teach Ø the competencies patient-centered care, teamwork and collaboration, and safety
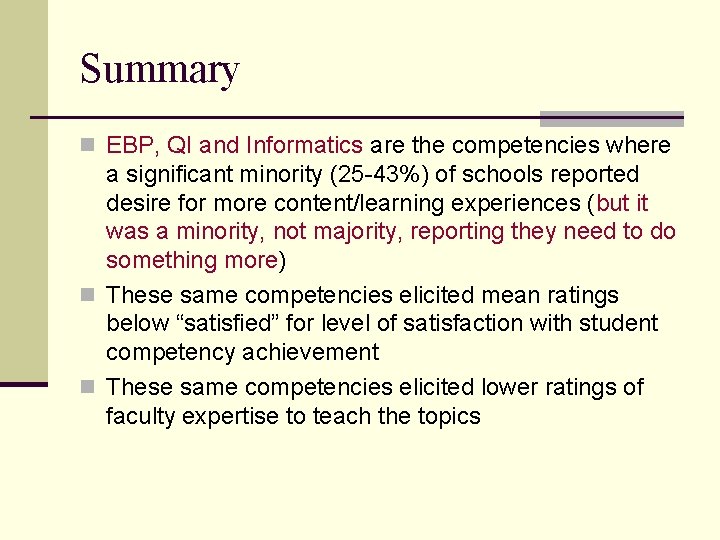
Summary n EBP, QI and Informatics are the competencies where a significant minority (25 -43%) of schools reported desire for more content/learning experiences (but it was a minority, not majority, reporting they need to do something more) n These same competencies elicited mean ratings below “satisfied” for level of satisfaction with student competency achievement n These same competencies elicited lower ratings of faculty expertise to teach the topics
Prelicensure Knowledge, Skills and Attitudes (KSAs) by Competency Cronenwett, L. , Sherwood, G. , Barnsteiner, J. , Disch, J. , Johnson, J. , Mitchell, P, & Warren, J. (2007). Quality and safety education for nurses. Nursing Outlook, 55(3), 122 -131.
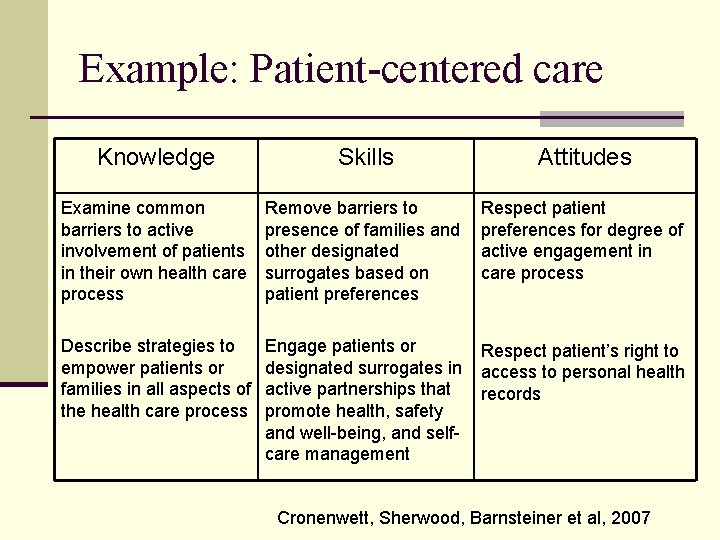
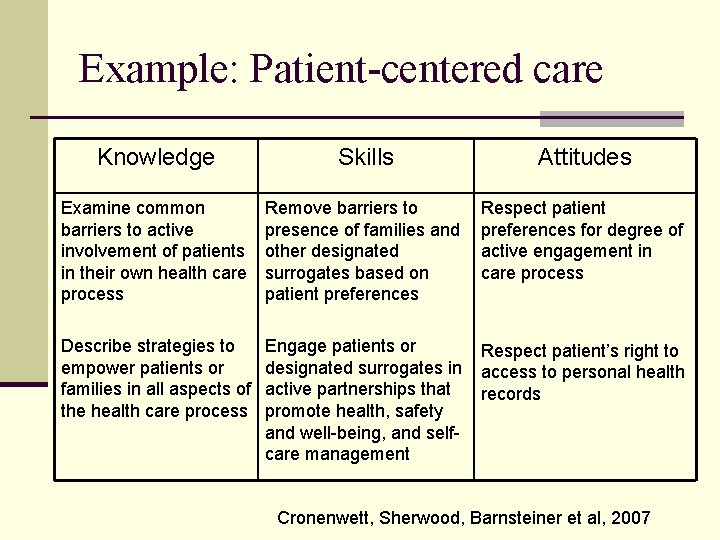
Example: Patient-centered care Knowledge Skills Attitudes Examine common barriers to active involvement of patients in their own health care process Remove barriers to presence of families and other designated surrogates based on patient preferences Respect patient preferences for degree of active engagement in care process Describe strategies to empower patients or families in all aspects of the health care process Engage patients or designated surrogates in active partnerships that promote health, safety and well-being, and selfcare management Respect patient’s right to access to personal health records Cronenwett, Sherwood, Barnsteiner et al, 2007
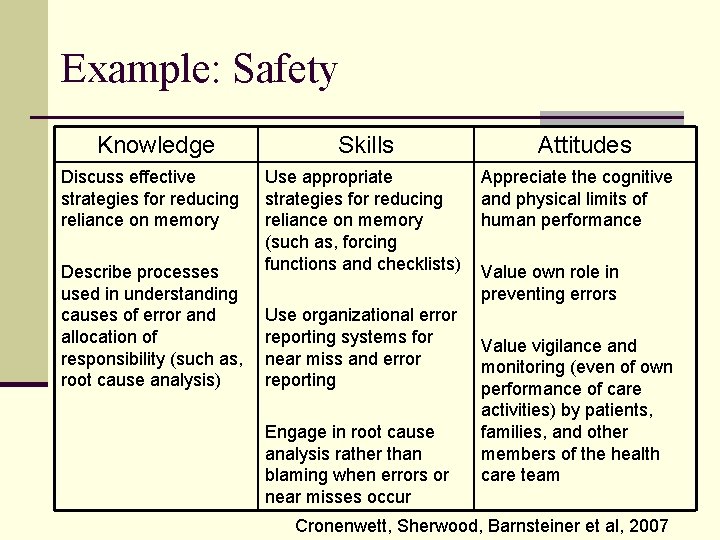
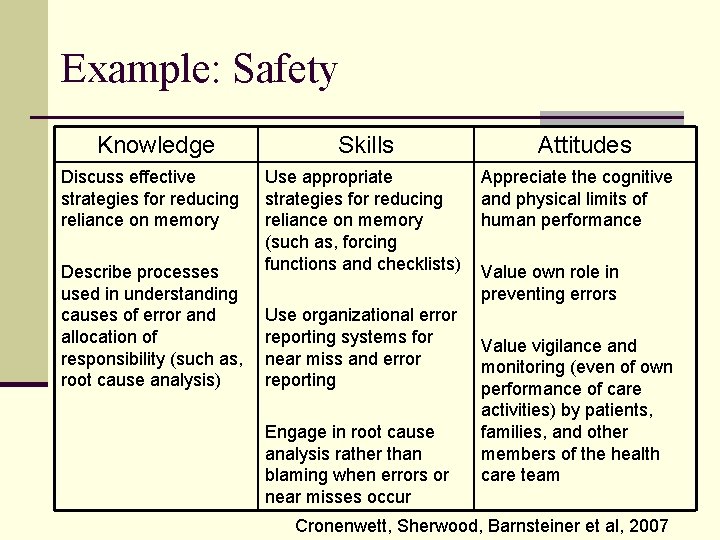
Example: Safety Knowledge Discuss effective strategies for reducing reliance on memory Describe processes used in understanding causes of error and allocation of responsibility (such as, root cause analysis) Skills Use appropriate strategies for reducing reliance on memory (such as, forcing functions and checklists) Use organizational error reporting systems for near miss and error reporting Engage in root cause analysis rather than blaming when errors or near misses occur Attitudes Appreciate the cognitive and physical limits of human performance Value own role in preventing errors Value vigilance and monitoring (even of own performance of care activities) by patients, families, and other members of the health care team Cronenwett, Sherwood, Barnsteiner et al, 2007
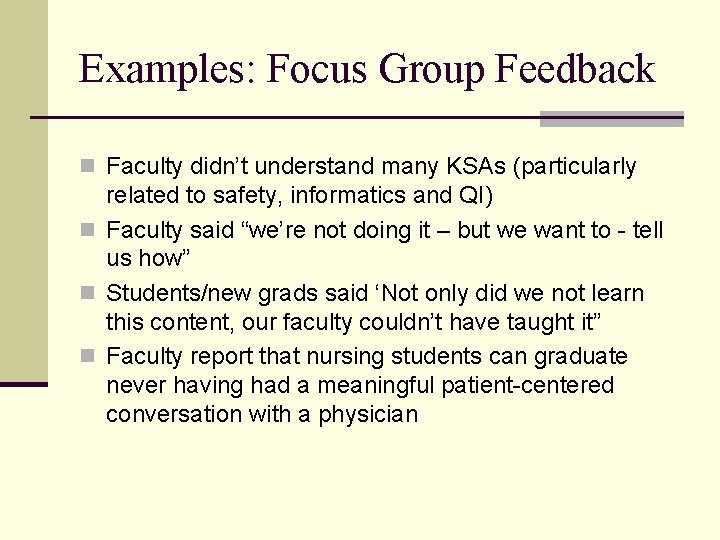
Examples: Focus Group Feedback n Faculty didn’t understand many KSAs (particularly related to safety, informatics and QI) n Faculty said “we’re not doing it – but we want to - tell us how” n Students/new grads said ‘Not only did we not learn this content, our faculty couldn’t have taught it” n Faculty report that nursing students can graduate never having had a meaningful patient-centered conversation with a physician
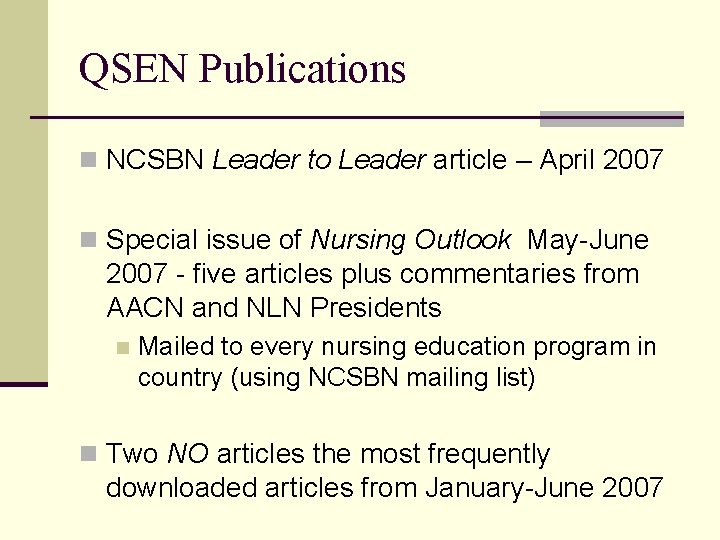
QSEN Publications n NCSBN Leader to Leader article – April 2007 n Special issue of Nursing Outlook May-June 2007 - five articles plus commentaries from AACN and NLN Presidents n Mailed to every nursing education program in country (using NCSBN mailing list) n Two NO articles the most frequently downloaded articles from January-June 2007
Policy Strategies n Shared products with professional organizations involved in licensure and certification or in accreditation of prelicensure programs
What and How Do We Guide Student Learning? www. qsen. org and Pilot School Learning Collaborative
QSEN Assumptions n Faculty and students are committed to quality and safety in all they do n Learning experiences aimed only at knowledge acquisition will be insufficient for development of competencies n Invitations to select from and experiment with a variety of curricular strategies will yield greater long-term gains than being highly prescriptive
Teaching Resource: QSEN Website n www. qsen. org Competency definitions and KSAs n Annotated references by competency n Teaching strategies for classroom, clinical, skills/simulation labs, and interprofessional learning n Opportunity for all faculty to upload ideas and evaluations of teaching strategies n
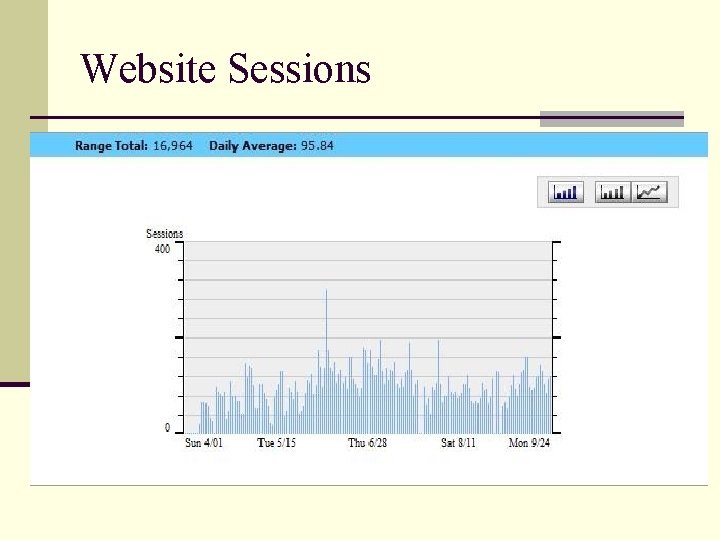
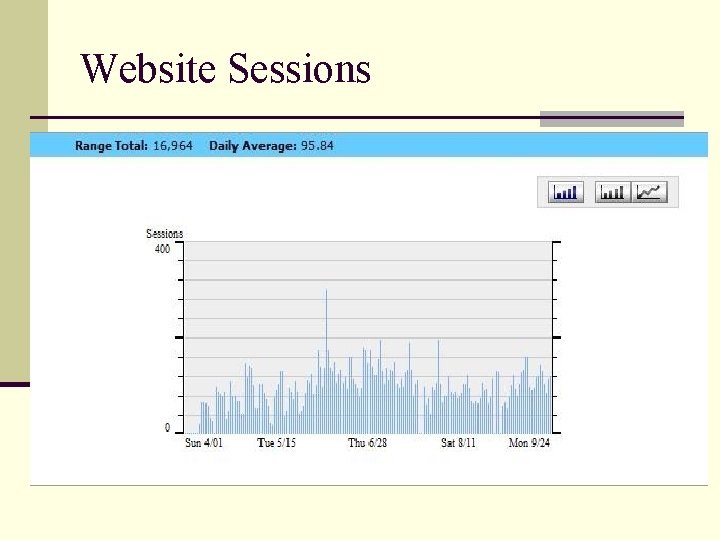
Website Sessions
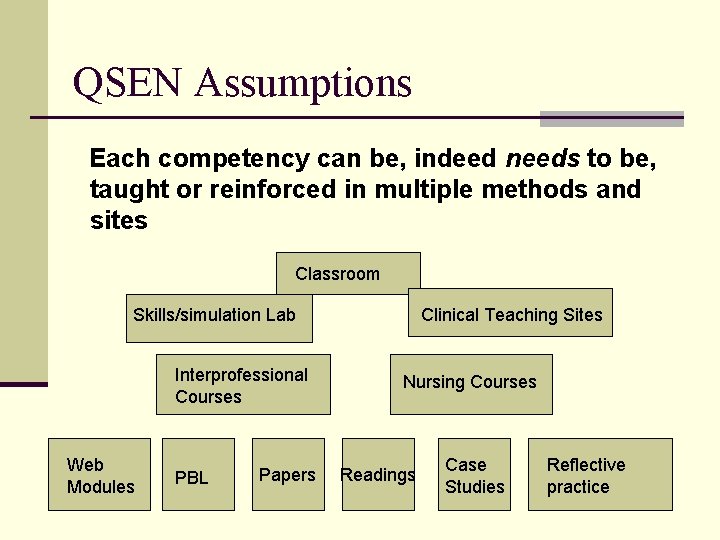
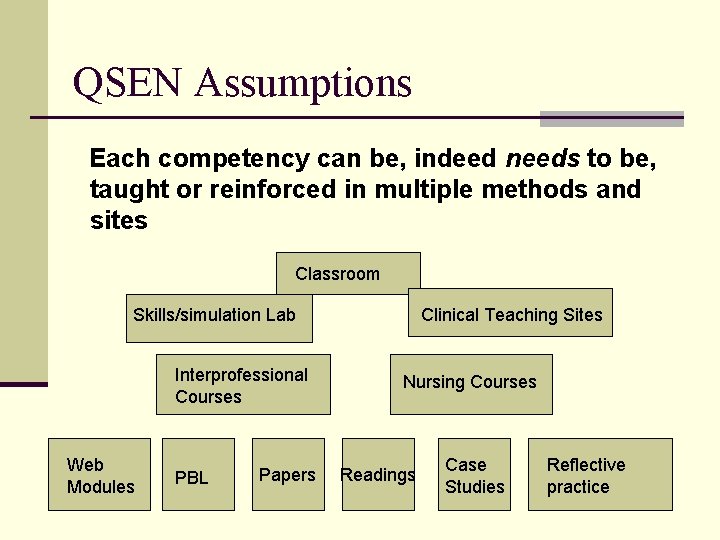
QSEN Assumptions Each competency can be, indeed needs to be, taught or reinforced in multiple methods and sites Classroom Skills/simulation Lab Interprofessional Courses Web Modules PBL Papers Clinical Teaching Sites Nursing Courses Readings Case Studies Reflective practice
QSEN Phase II: Prelicensure Education n Pilot School Learning Collaborative n Goal: Engage prelicensure faculty members in developing and testing teaching strategies for the QSEN competencies n Call for proposals mailed to all nursing education programs in March, 2007 n 15 schools selected July 2007 from 53 applications
QSEN Learning Collaborative n Augustana College (SD) n Catholic University (DC) n Charleston Southern University of Nebraska n n n n (SC) Curry College (MA) Emory University (GA) Lasalle University (PA) St. John’s College of Nursing/Southwest Baptist (MO) University of Colorado at Denver University of Massachusetts. Boston n n Medical Center University of South Dakota, Sioux Falls University of Tennessee Health Science Center, Memphis University of Wisconsin. Madison University of Pittsburgh Medical Center-Shadyside School of Nursing (PA) Wright State University (OH)
QSEN Learning Collaborative n All have committed practice partners n Associate degree, diploma, BSN programs in schools without graduate programs, and BSN programs in universities n Our “edgerunners” Some focusing on simulation n Some focusing on innovations in clinical teaching n Some focusing on curriculum as a whole n
QSEN Learning Collaborative n Collaborative meetings (October, 2007 and June, 2008) n Evaluate one class of graduating students’ perceptions of n n n competency achievement Produce a curricular map with the quality and safety KSAs integrated into their pre-licensure curriculum Develop and evaluate teaching strategies for classroom, clinical, and simulation/skills laboratories Share teaching strategies through submissions to the QSEN website Document specific challenges encountered in the process of curricular change Share successful strategies for overcoming challenges with others in collaborative conferences and conference calls
QSEN Assumptions n Nurses in practice settings are critical partners in accomplishing competency development n Examples: n n n Staff are role models for how these competencies define what it means to be a respected and qualified nurse Students and faculty know the safety and QI initiatives – always know the ‘next likely error’ in the setting Students learn from staff what “good care” is and how “local care” compares to that standard
QSEN Assumptions n n n Students use information technology during clinical practice Students see team skills in action in communications between nurses and other health professionals Students see patients and families involved as partners in care Health professions students in a setting interact with each other in improvement work Transition to practice programs build on the competency development from pre-licensure programs
Quality and Safety Education for Nurses Graduate Education
Phase I: Graduate Education n Sought feedback from major APN organizations about KSAs: Can they represent all of nursing? n Added NONPF representative to Advisory Board
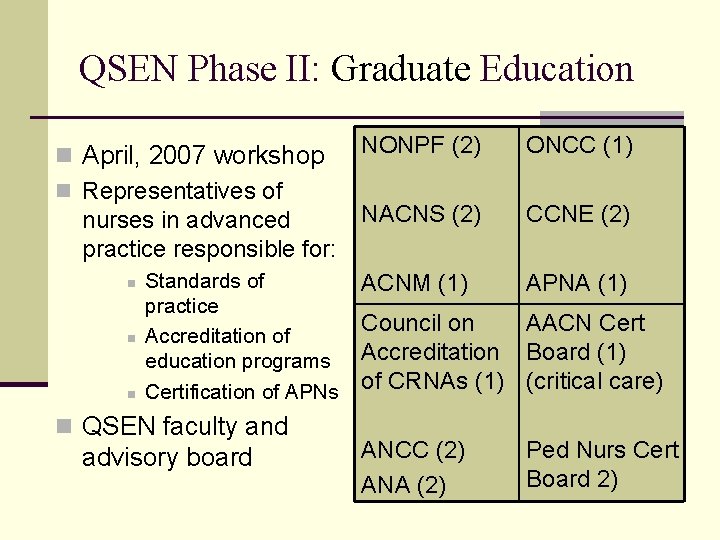
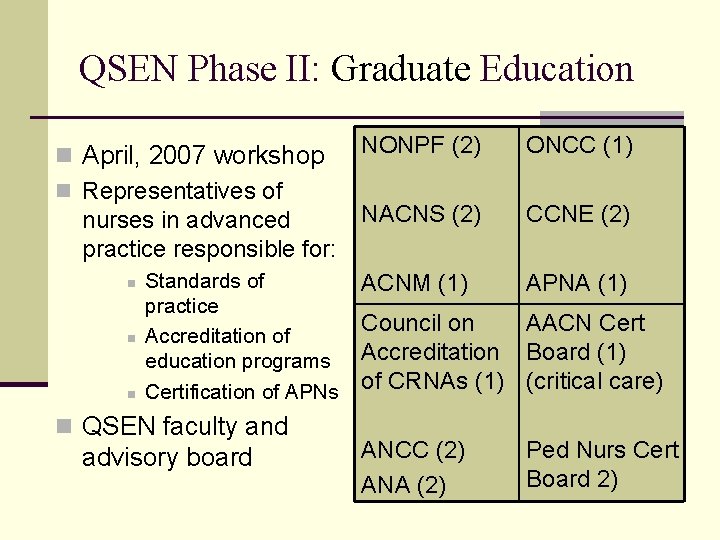
QSEN Phase II: Graduate Education n April, 2007 workshop n Representatives of nurses in advanced practice responsible for: n n n Standards of practice Accreditation of education programs Certification of APNs n QSEN faculty and advisory board NONPF (2) ONCC (1) NACNS (2) CCNE (2) ACNM (1) APNA (1) Council on AACN Cert Accreditation Board (1) of CRNAs (1) (critical care) ANCC (2) ANA (2) Ped Nurs Cert Board 2)
Graduate Education Initial conversation: Focus on advanced practice rather than all advanced roles n Focus on advanced practice rather than the type of program in which the graduate student is prepared n Focus on goal of assisting faculty who wish to develop quality and safety competencies already identified as essential elements n
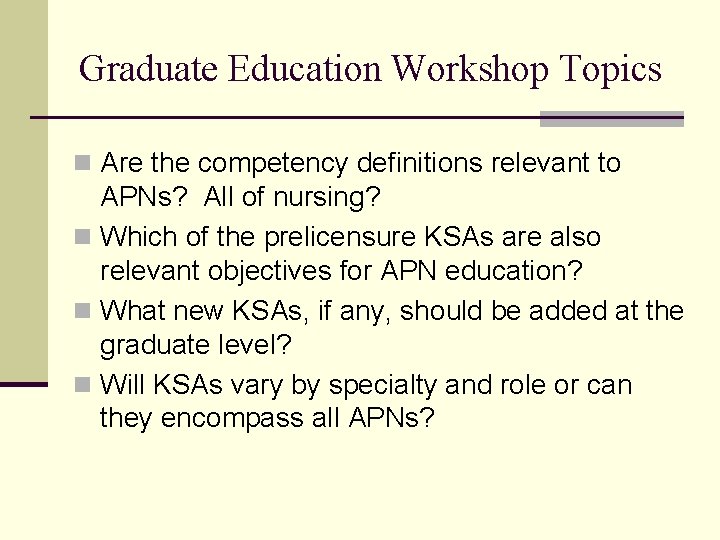
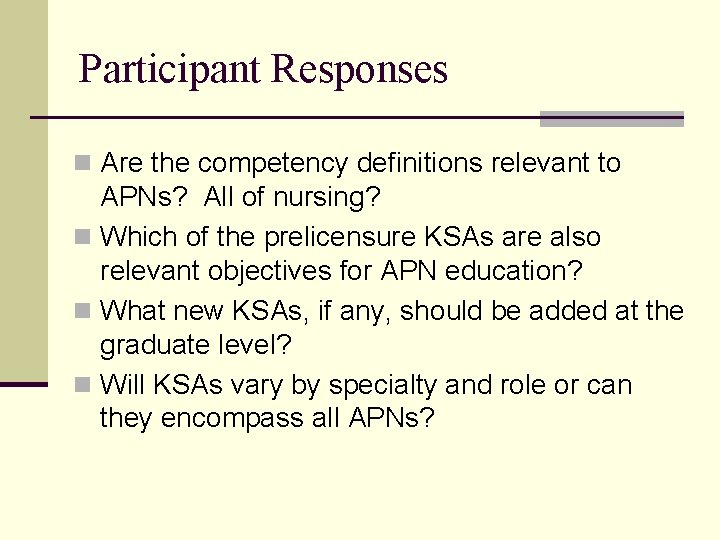
Graduate Education Workshop Topics n Are the competency definitions relevant to APNs? All of nursing? n Which of the prelicensure KSAs are also relevant objectives for APN education? n What new KSAs, if any, should be added at the graduate level? n Will KSAs vary by specialty and role or can they encompass all APNs?
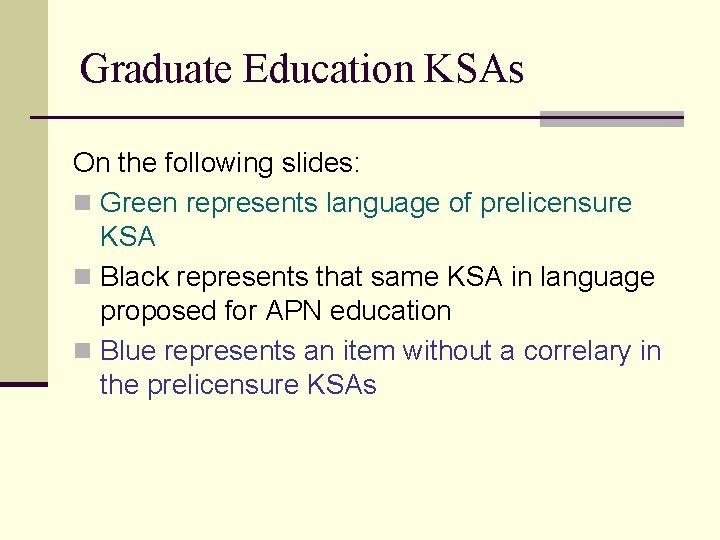
Graduate Education KSAs On the following slides: n Green represents language of prelicensure KSA n Black represents that same KSA in language proposed for APN education n Blue represents an item without a correlary in the prelicensure KSAs
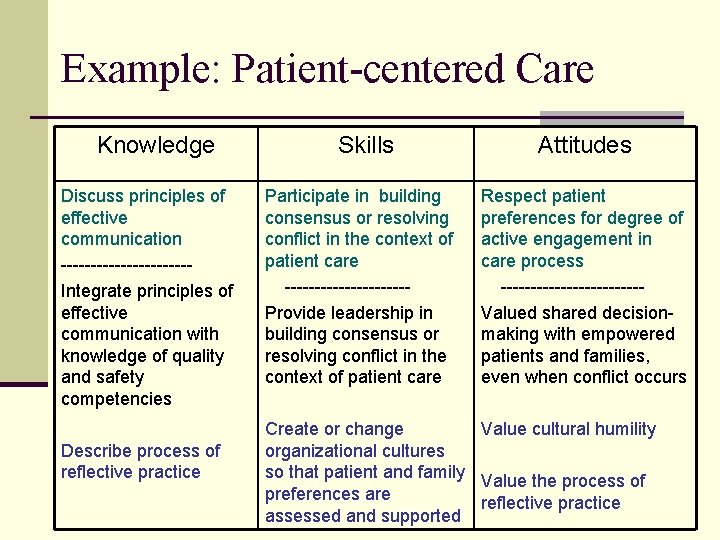
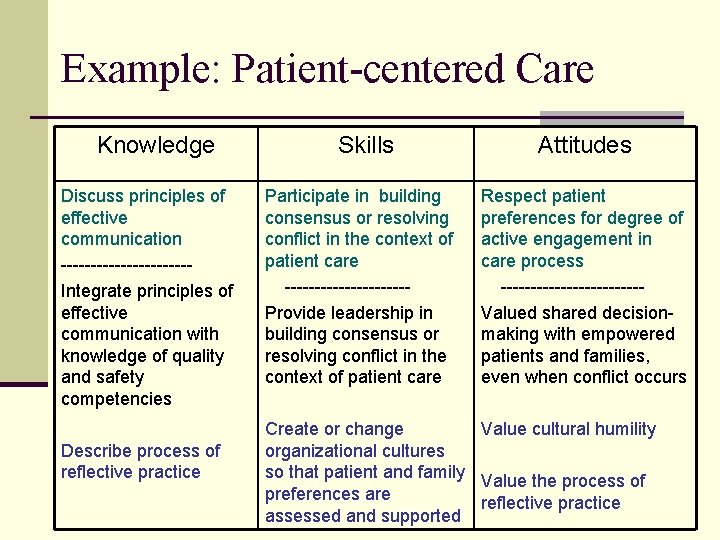
Example: Patient-centered Care Knowledge Discuss principles of effective communication -----------Integrate principles of effective communication with knowledge of quality and safety competencies Describe process of reflective practice Skills Participate in building consensus or resolving conflict in the context of patient care ----------Provide leadership in building consensus or resolving conflict in the context of patient care Attitudes Respect patient preferences for degree of active engagement in care process ------------Valued shared decisionmaking with empowered patients and families, even when conflict occurs Create or change Value cultural humility organizational cultures so that patient and family Value the process of preferences are reflective practice assessed and supported
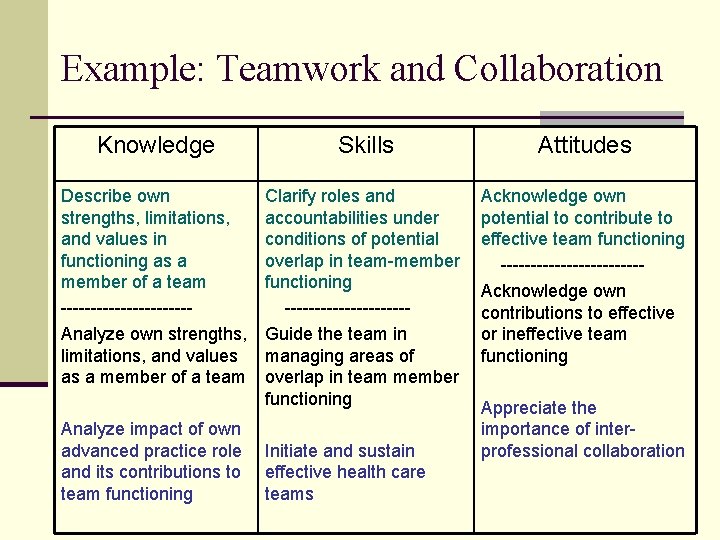
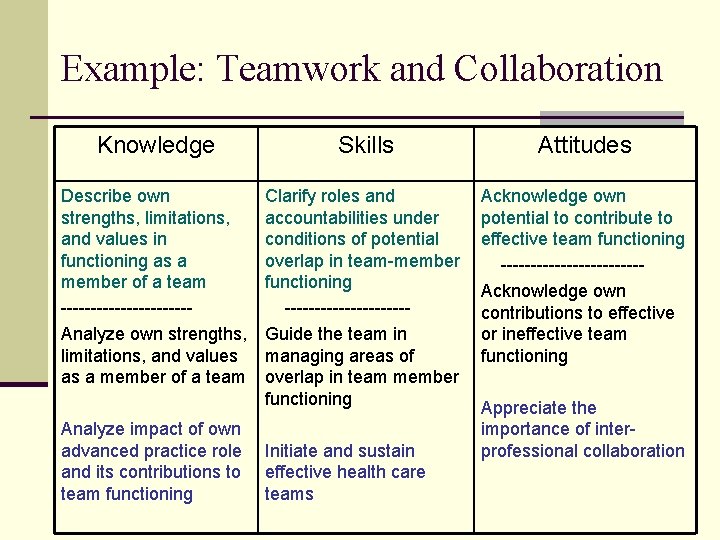
Example: Teamwork and Collaboration Knowledge Skills Attitudes Describe own strengths, limitations, and values in functioning as a member of a team -----------Analyze own strengths, limitations, and values as a member of a team Clarify roles and accountabilities under conditions of potential overlap in team-member functioning ----------Guide the team in managing areas of overlap in team member functioning Acknowledge own potential to contribute to effective team functioning ------------Acknowledge own contributions to effective or ineffective team functioning Analyze impact of own advanced practice role and its contributions to team functioning Initiate and sustain effective health care teams Appreciate the importance of interprofessional collaboration
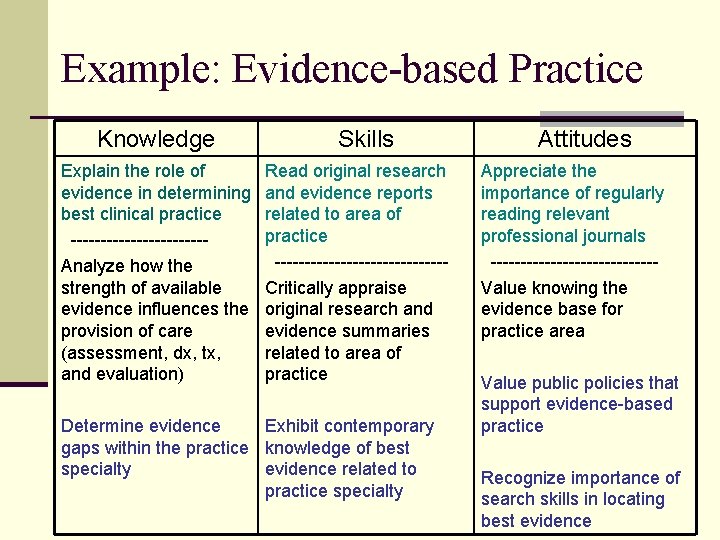
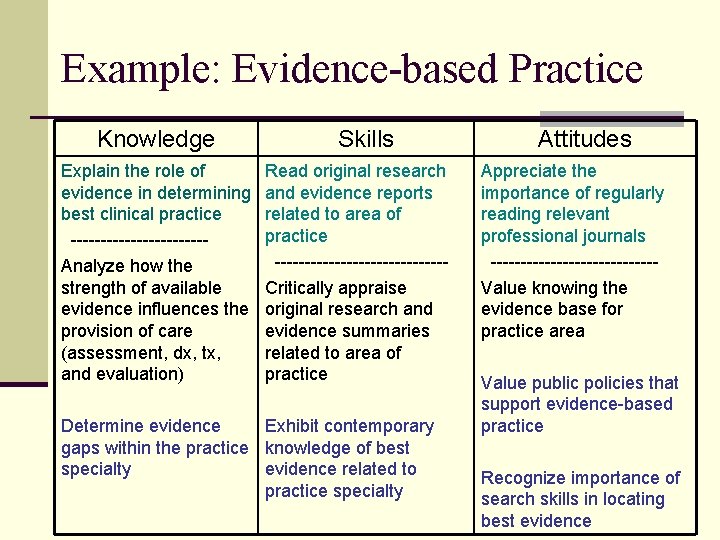
Example: Evidence-based Practice Knowledge Explain the role of evidence in determining best clinical practice -----------Analyze how the strength of available evidence influences the provision of care (assessment, dx, tx, and evaluation) Skills Read original research and evidence reports related to area of practice --------------Critically appraise original research and evidence summaries related to area of practice Determine evidence Exhibit contemporary gaps within the practice knowledge of best specialty evidence related to practice specialty Attitudes Appreciate the importance of regularly reading relevant professional journals --------------Value knowing the evidence base for practice area Value public policies that support evidence-based practice Recognize importance of search skills in locating best evidence
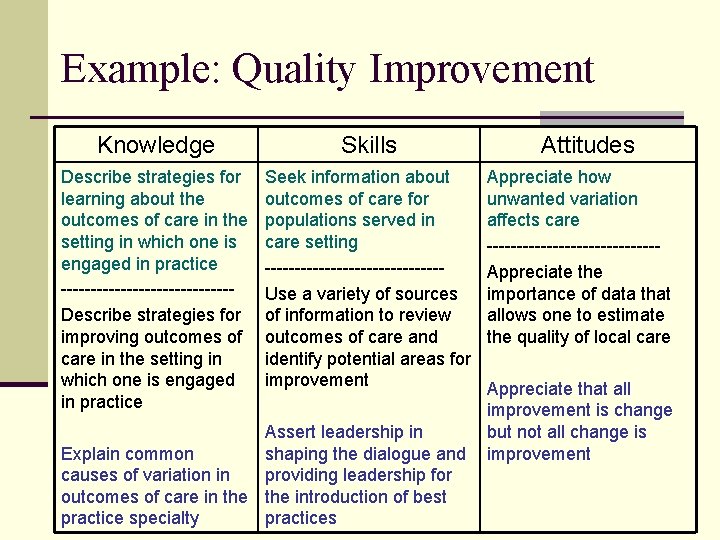
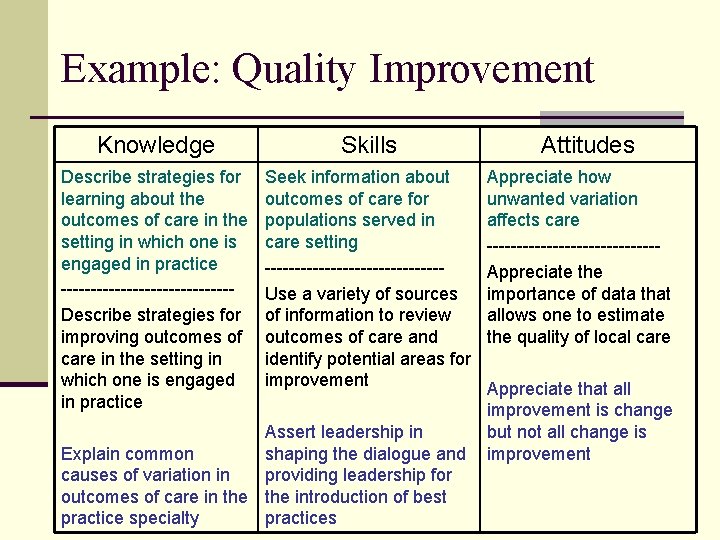
Example: Quality Improvement Knowledge Skills Describe strategies for learning about the outcomes of care in the setting in which one is engaged in practice --------------Describe strategies for improving outcomes of care in the setting in which one is engaged in practice Seek information about outcomes of care for populations served in care setting ---------------Use a variety of sources of information to review outcomes of care and identify potential areas for improvement Assert leadership in Explain common shaping the dialogue and causes of variation in providing leadership for outcomes of care in the introduction of best practice specialty practices Attitudes Appreciate how unwanted variation affects care --------------Appreciate the importance of data that allows one to estimate the quality of local care Appreciate that all improvement is change but not all change is improvement
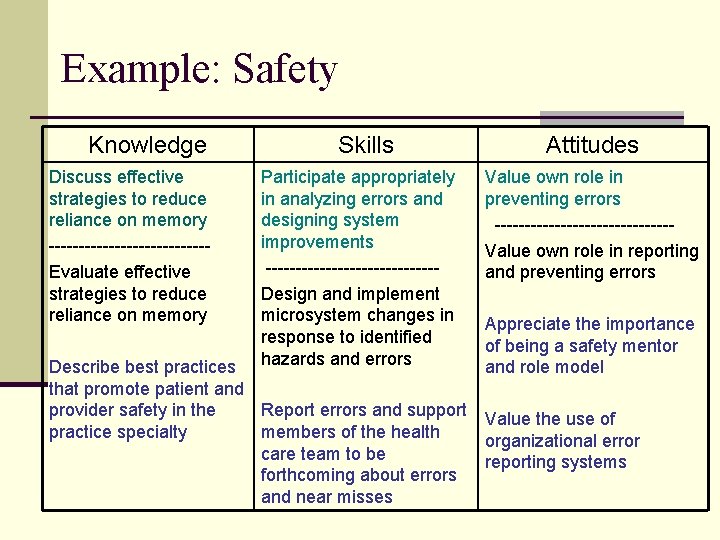
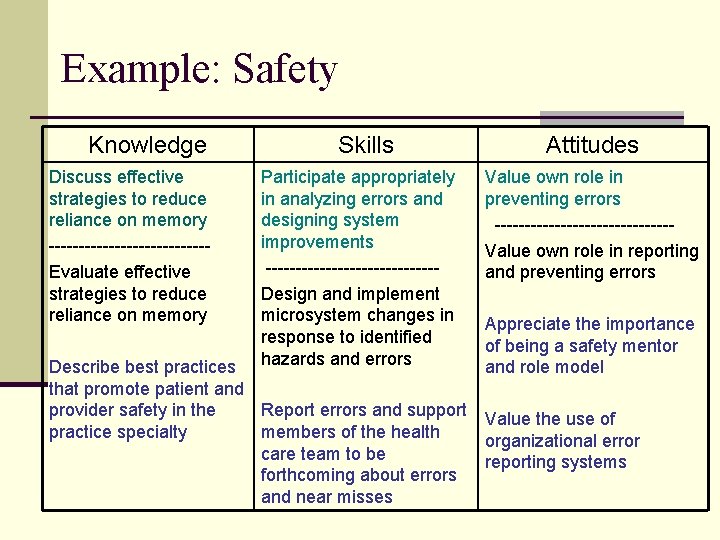
Example: Safety Knowledge Discuss effective strategies to reduce reliance on memory -------------Evaluate effective strategies to reduce reliance on memory Skills Participate appropriately in analyzing errors and designing system improvements --------------Design and implement microsystem changes in response to identified hazards and errors Describe best practices that promote patient and provider safety in the Report errors and support practice specialty members of the health care team to be forthcoming about errors and near misses Attitudes Value own role in preventing errors ---------------Value own role in reporting and preventing errors Appreciate the importance of being a safety mentor and role model Value the use of organizational error reporting systems
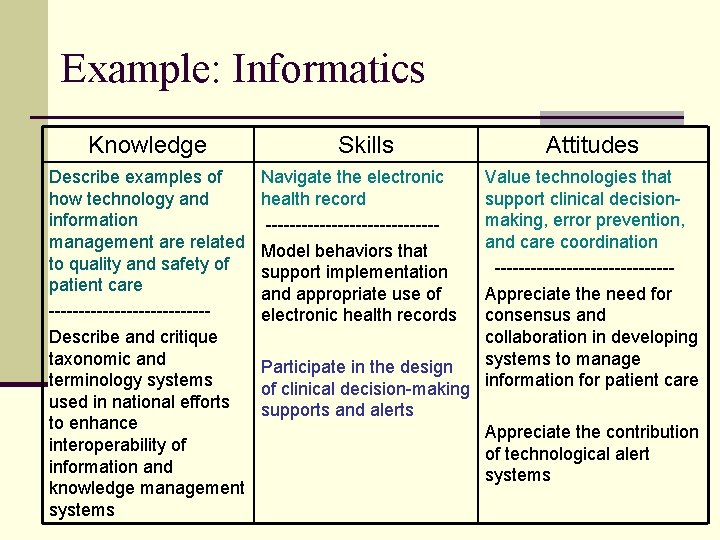
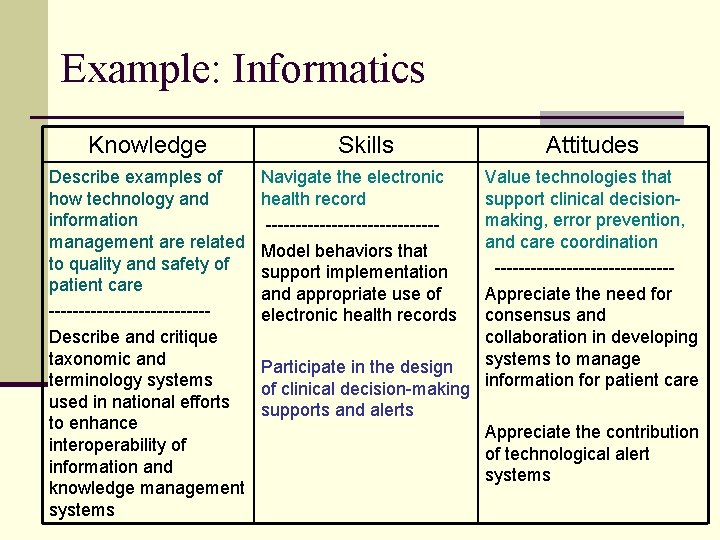
Example: Informatics Knowledge Describe examples of how technology and information management are related to quality and safety of patient care -------------Describe and critique taxonomic and terminology systems used in national efforts to enhance interoperability of information and knowledge management systems Skills Navigate the electronic health record --------------Model behaviors that support implementation and appropriate use of electronic health records Attitudes Value technologies that support clinical decisionmaking, error prevention, and care coordination ---------------Appreciate the need for consensus and collaboration in developing systems to manage Participate in the design of clinical decision-making information for patient care supports and alerts Appreciate the contribution of technological alert systems
Participant Responses n Are the competency definitions relevant to APNs? All of nursing? n Which of the prelicensure KSAs are also relevant objectives for APN education? n What new KSAs, if any, should be added at the graduate level? n Will KSAs vary by specialty and role or can they encompass all APNs?
Graduate Education: Next Steps n Draft 2 under review by all participants and their organizations n Feedback received in November, awaiting full analysis n Dissemination

 Quality and safety education for nurses
Quality and safety education for nurses Quality and safety education for nurses
Quality and safety education for nurses Quality and safety education for nurses
Quality and safety education for nurses Quality and safety education for nurses (qsen)
Quality and safety education for nurses (qsen) Perform quality assurance
Perform quality assurance Basic quality concepts
Basic quality concepts Mitochondria
Mitochondria Simply misplaced
Simply misplaced A nurse floats to a busy surgical unit
A nurse floats to a busy surgical unit Relationship between safety, quality and productivity
Relationship between safety, quality and productivity Ndis orientation module
Ndis orientation module Importance of food quality and safety
Importance of food quality and safety Patient safety and quality care movement
Patient safety and quality care movement Blood safety and quality regulations
Blood safety and quality regulations Tamilnadu nursing council registration status
Tamilnadu nursing council registration status Safe staffing ratios benefiting nurses and patients
Safe staffing ratios benefiting nurses and patients Education quality and accountability office
Education quality and accountability office Project quality management pmp
Project quality management pmp Pmbok quality assurance vs quality control
Pmbok quality assurance vs quality control Define quality assurance in nursing
Define quality assurance in nursing Compliance vs quality
Compliance vs quality Two quality gurus
Two quality gurus Quality is free: the art of making quality certain
Quality is free: the art of making quality certain Old quality vs new quality
Old quality vs new quality Formuö
Formuö Typiska drag för en novell
Typiska drag för en novell Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Vad står k.r.å.k.a.n för
Vad står k.r.å.k.a.n för Shingelfrisyren
Shingelfrisyren En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Personalliggare bygg undantag
Personalliggare bygg undantag Tidbok yrkesförare
Tidbok yrkesförare A gastrica
A gastrica Vad är densitet
Vad är densitet Datorkunskap för nybörjare
Datorkunskap för nybörjare Boverket ka
Boverket ka Debattinlägg mall
Debattinlägg mall För och nackdelar med firo
För och nackdelar med firo Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Tryck formel
Tryck formel Svenskt ramverk för digital samverkan
Svenskt ramverk för digital samverkan Lyckans minut erik lindorm analys
Lyckans minut erik lindorm analys Presentera för publik crossboss
Presentera för publik crossboss Teckenspråk minoritetsspråk argument
Teckenspråk minoritetsspråk argument Kanaans land
Kanaans land Treserva lathund
Treserva lathund Epiteltyper
Epiteltyper Claes martinsson
Claes martinsson Cks
Cks Verifikationsplan
Verifikationsplan Mat för unga idrottare
Mat för unga idrottare Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Rutin för avvikelsehantering
Rutin för avvikelsehantering Smärtskolan kunskap för livet
Smärtskolan kunskap för livet