QUALITY AND SAFETY EDUCATION FOR NURSES QSEN CASSIE


- Slides: 41
QUALITY AND SAFETY EDUCATION FOR NURSES (QSEN) CASSIE MOFFITT, BSN, RN NURS 5327 FEBRUARY 27, 2017
OBJECTIVE • TO UNDERSTAND THE ROLE OF QSEN IN NURSING PRACTICE • TO PROVIDE INFORMATION IN ORDER TO PROMOTE SAFETY • PROVIDE STRATEGIES TO PROMOTE SAFETY • IMPROVE QUALITY OF CARE
WHAT IS QSEN? • DEVELOPED IN 2005 IN RESPONSE TO INSTITUTE OF MEDICINE REPORT TITLED, “TO ERR IS HUMAN: BUILDING A SAFER HEALTHCARE SYSTEM”. • REPORT CREATED AWARENESS IN REGARD TO HEALTHCARE SAFETY • COMPREHENSIVE, COMPETENCY-BASED RESOURCES • QSEN FOUNDERS BELIEVED IN ORDER TO SUCCEED, COMPETENCIES MUST BE WIDELY SHARED • LAUNCHED ACTIVE WEBSITE TO PROVIDE THESE COMPETENCIES FREE OF CHARGE (PATRICIAN, 2016)
PURPOSE • FOUNDERS OF QSEN RECOGNIZED THAT SCHOOLS OF NURSING NEEDED TO BETTER PREPARE NURSES FOR CHALLENGES CREATED BY HAZARDS OF HEALTH CARE. • TO INTEGRATE ACADEMIA AND ACTUAL NURSING PRACTICE • NOT LIMITED TO NURSING SCHOOLS AND INPATIENT UNITS • ORIENTATION PROGRAMS • CLINICAL LADDER ACTIVITIES • PERFORMANCE EVALUATIONS • RESIDENCY PROGRAMS (PATRICIAN, 2016)
PATIENT CENTERED CARE • DEMONSTRATED THROUGH CLEAR AND THOROUGH COMMUNICATION, RESPONSE, AND RESPECT. • LISTENING TO THE PATIENT’S INPUT, RECOGNIZING THEM AS PART OF CARE TEAM • CAN BE ALLIES IN THEIR OWN SAFETY • BASED ON RESPECT FOR PATIENT’S PREFERENCES, NEEDS, VALUES, AND CULTURE (SHERWOOD AND ZOMORODI, 2014)
STRATEGIES 1. COMPLETION OF ADMISSION PROFILE ON ARRIVAL TO UNIT 2. ASSESSMENT OF PAIN AND GENERAL WELL-BEING IN THE PATIENT’S SUBJECTIVE VIEW 3. CONTINUOUSLY PROVIDE COMMUNICATION CONCERNING CARE PLAN IN LANGUAGE AND TERMS APPLICABLE TO THE PATIENT’S PREFERENCES AND ABILITIES
Video 1. Hospital Admission Excerpt. (Providence Holy Cross Medical Center, 2010)
PAIN ASSESSMENT CONSIDERATIONS • KNOW THE UNIT POLICY ON FREQUENCY—PARTICULARLY IF OPIOIDS ARE IN USE. • BE AWARE OF ANY POSSIBLE MEDICATION REACTIONS. EX. : SEDATING MEDICATIONS, SUCH AS MIND-ALTERING MEDICATIONS IN COMBINATION WITH SEDATING OPIOIDS • USE AGE-APPROPRIATE SCALE AND BE AWARE OF ANY LANGUAGE, LEARNING, VERBAL DIFFICULTIES, AND MENTAL STATUS
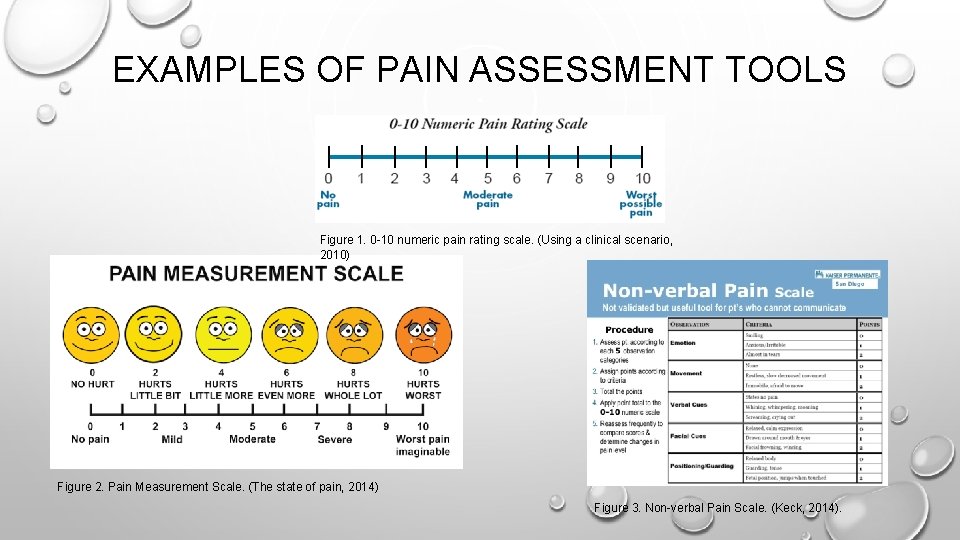
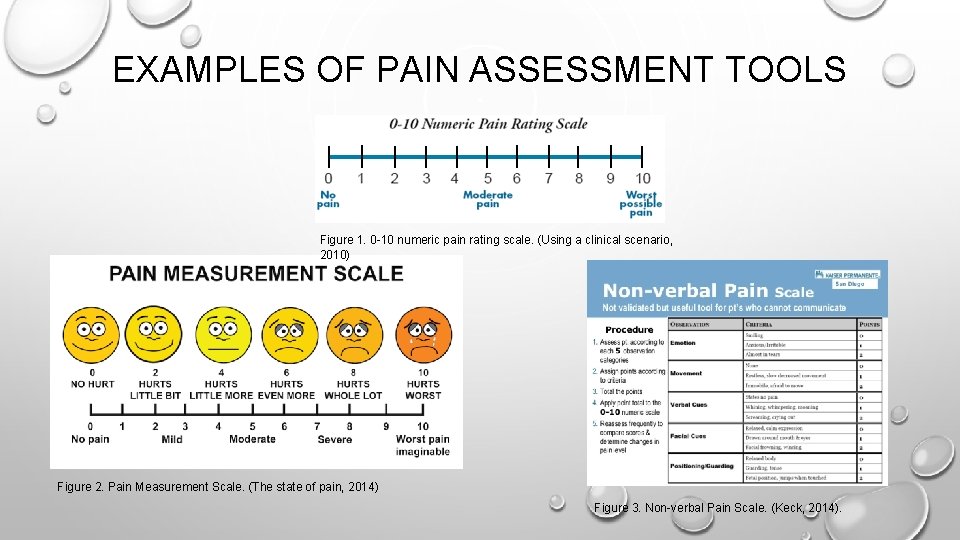
EXAMPLES OF PAIN ASSESSMENT TOOLS Figure 1. 0 -10 numeric pain rating scale. (Using a clinical scenario, 2010) Figure 2. Pain Measurement Scale. (The state of pain, 2014) Figure 3. Non-verbal Pain Scale. (Keck, 2014).
LANGUAGE SERVICES • PAGE TRANSLATOR-ON-CALL FOR SPECIFIC LANGUAGE • ACCESS HOSPITAL-WIDE LIST OF SPEAKERS OF VARIOUS LANGUAGES (EX. : URDU, FARSI, SPANISH, SWAHILI, ETC. ) • PHONE/TABLET APPS (FREE) • TRANSLATOR • GOOGLE TRANSLATE (BE CAREFUL: THIS IS NOT ALWAYS ACCURATE) • DUOLINGO • SPANISH DICT
COMMUNICATION • COMMUNICATION DIFFICULTIES ARE NOT LIMITED TO LANGUAGE • MUST GIVE CONSIDERATION TO • AGE • HEARING CAPABILITIES • LEARNING/COMPREHENSION DELAYS • ASSESS COMPREHENSION AND PROVIDE DETAILED INSTRUCTIONS IN FORMAT APPROPRIATE TO LEARNING/COMPREHENSION ABILITIES • EX. : PICTURES OF PROCEDURES FOR PATIENTS TO ILLUSTRATE CARE • LETTING PATIENTS HOLD OR TOUCH INSTRUMENTS/EQUIPMENT THAT WILL BE USED IN THEIR CARE
TEAMWORK AND COLLABORATION • ROLE IN FUNCTIONING BETWEEN TEAMS OF VARIOUS TYPES • WITHIN NURSING • MULTIDISCIPLINARY • WITH PATIENTS AND FAMILIES/LOVED ONES • MUTUAL RESPECT • OPEN COMMUNICATION • SHARED DECISION-MAKING (SHERWOOD AND ZOMORODI, 2014)
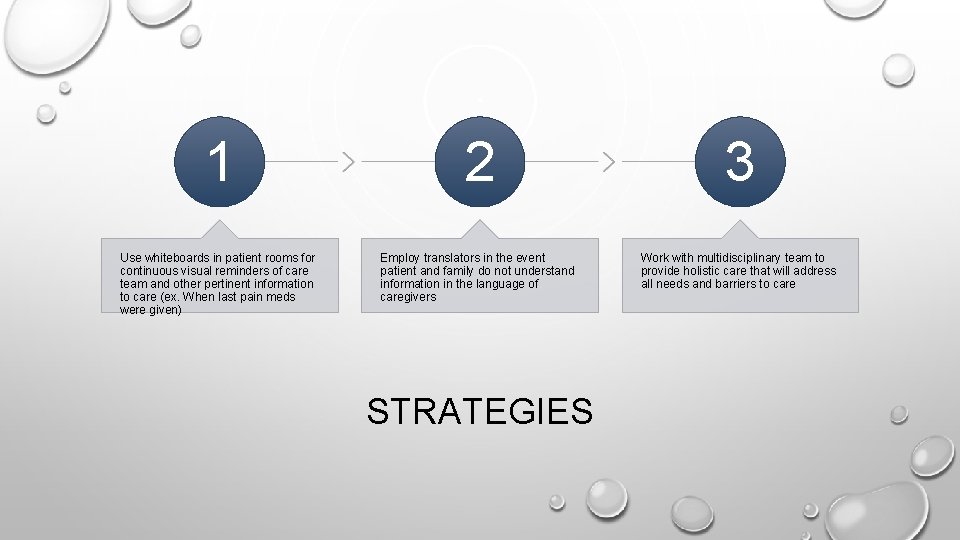
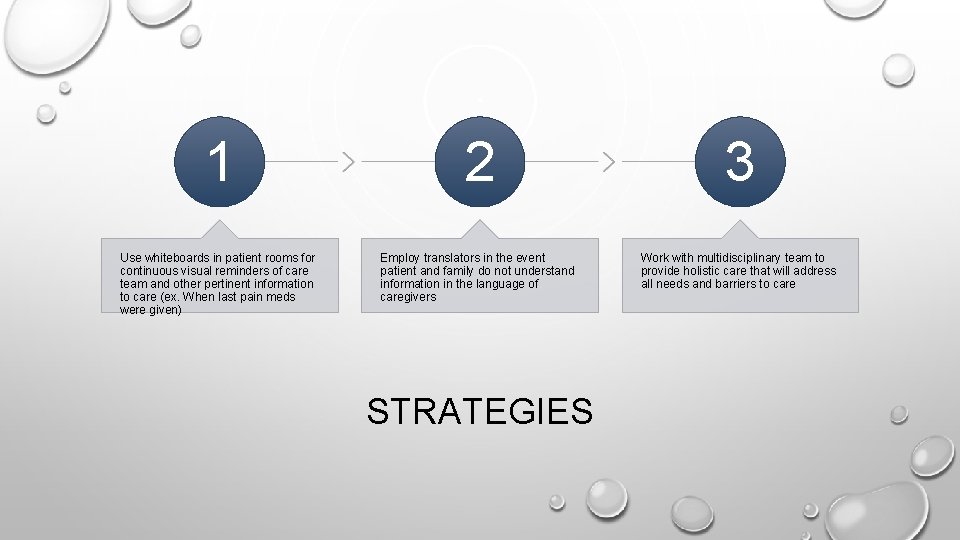
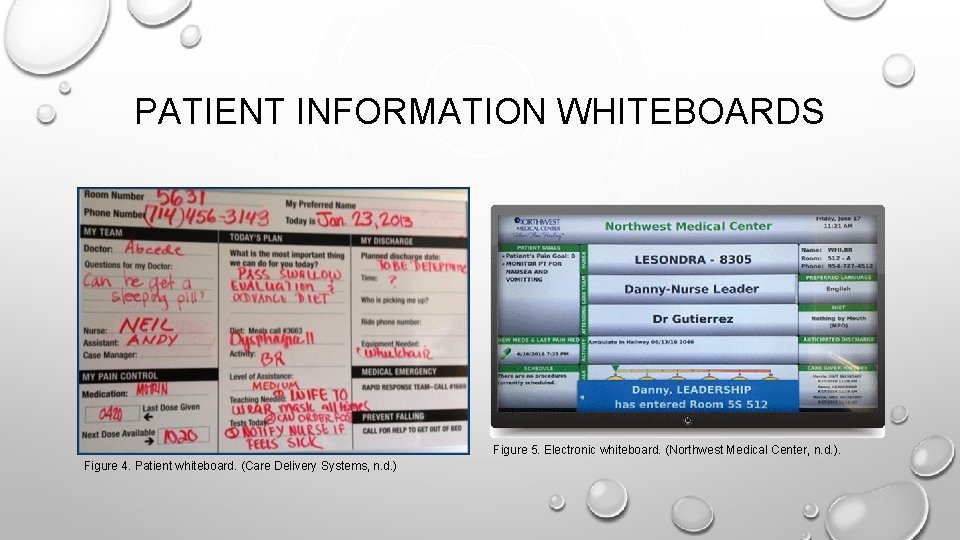
1 2 3 Use whiteboards in patient rooms for continuous visual reminders of care team and other pertinent information to care (ex. When last pain meds were given) Employ translators in the event patient and family do not understand information in the language of caregivers Work with multidisciplinary team to provide holistic care that will address all needs and barriers to care STRATEGIES
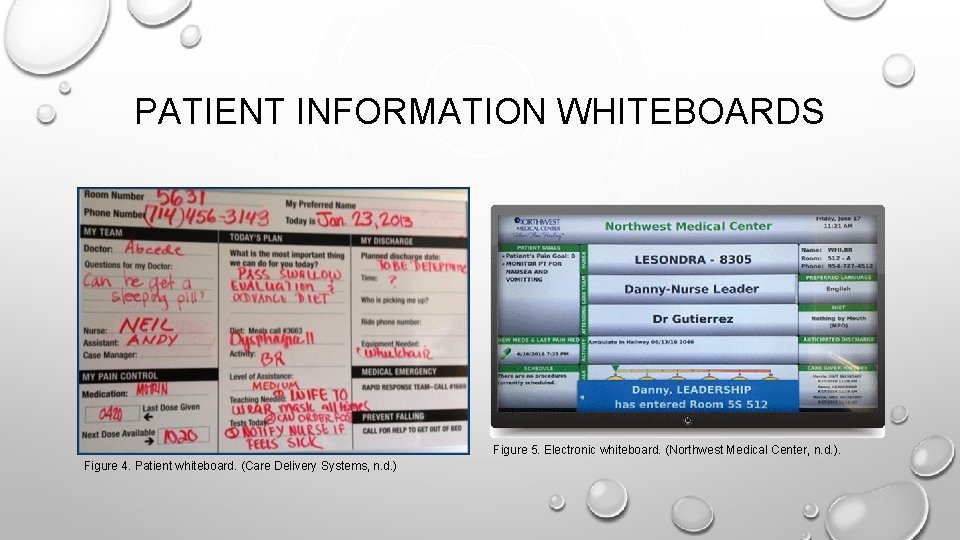
PATIENT INFORMATION WHITEBOARDS Figure 5. Electronic whiteboard. (Northwest Medical Center, n. d. ). Figure 4. Patient whiteboard. (Care Delivery Systems, n. d. )
Video 2. Interdisciplinary Team Care: Case One (Reynolds, 2014)
LANGUAGE LINES • COMMUNICATION FOR THE DEAF • HAVE PATIENT DIAL DIRECTLY FIRST (MANY HAVE SERVICE SET UP ALREADY) • IF NO ANSWER, HAVE PATIENT’S PHONE NUMBER AND UNIT COST CENTER READY • CALL COMMUNICATION FOR THE DEAF AT 888 -225 -6056 • SPEAK AS THOUGH YOU WERE TALKING DIRECTLY TO THE PARTY YOU ARE TRYING TO REACH. PARTY WILL RECEIVE MESSAGE VIA VIDEO TRANSLATION
LANGUAGE LINES (CONT’D) • AT&T LANGUAGE LINE • BE PREPARED WITH PATIENT’S MEDICAL RECORD NUMBER, DATE OF BIRTH, AND UNIT COST CENTER • DIAL 77777 TO ACCESS LANGUAGE LINE • SPEAK AS THOUGH YOU ARE TALKING DIRECTLY TO THE PARTY AND TRANSLATOR WILL TRANSLATE YOUR MESSAGE. • IF YOU NEED TO LEAVE A VOICEMAIL, AGAIN SPEAK DIRECTLY TO THE PARTY AND THE TRANSLATOR WILL LEAVE THE MESSAGE IN THE PATIENT’S PREFERRED LANGUAGE
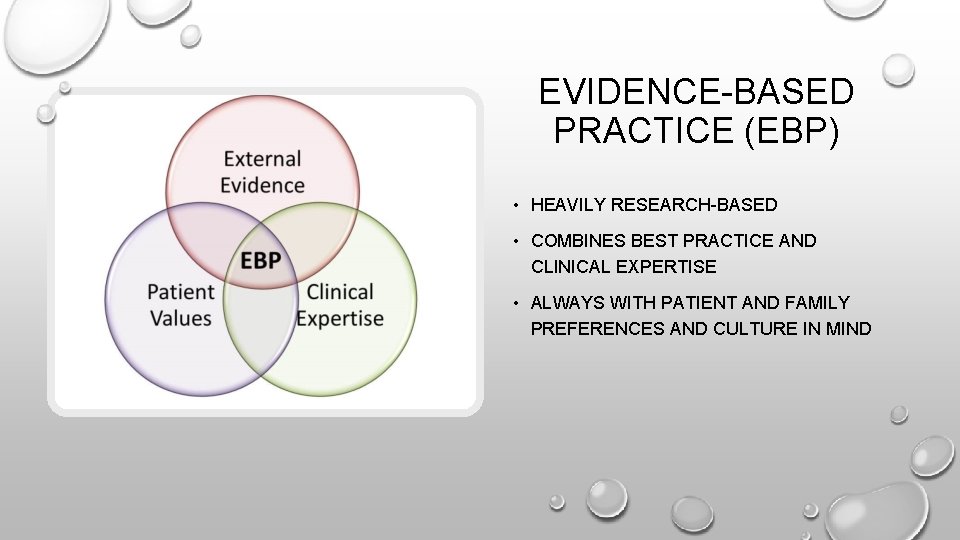
EVIDENCE-BASED PRACTICE (EBP) • HEAVILY RESEARCH-BASED • COMBINES BEST PRACTICE AND CLINICAL EXPERTISE • ALWAYS WITH PATIENT AND FAMILY PREFERENCES AND CULTURE IN MIND
STRATEGIES 1. ASSESS FALL RISK 2. REPOSITION PATIENT EVERY TWO HOURS TO PREVENT SKIN BREAKDOWN (TASHMAN AND LOW, 2016) 3. ASSESSMENT AND ROTATION OF PERIPHERAL IVS BASED ON CLINICAL ASSESSMENT VS. LENGTH OF TIME SINCE INSERTION (HELTON, HINES, AND BEST, 2016)
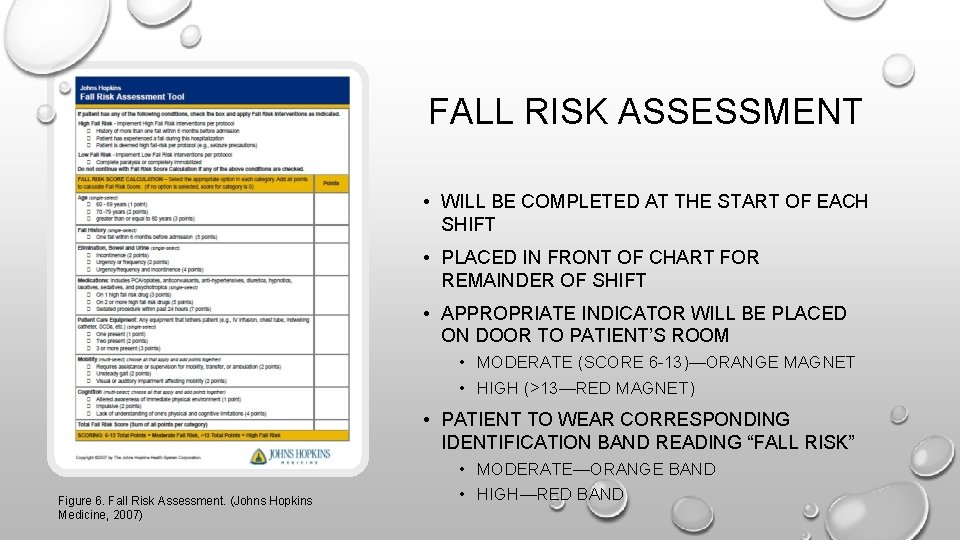
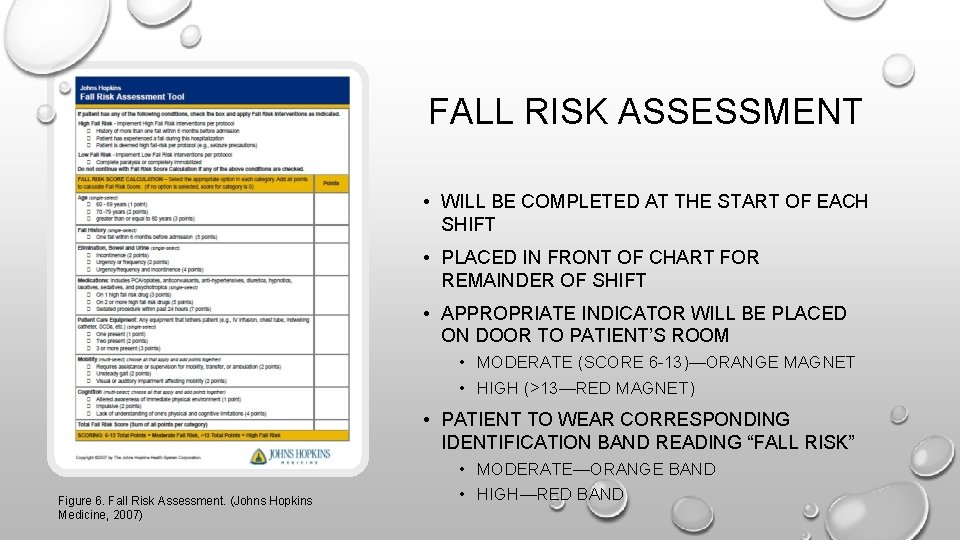
FALL RISK ASSESSMENT • WILL BE COMPLETED AT THE START OF EACH SHIFT • PLACED IN FRONT OF CHART FOR REMAINDER OF SHIFT • APPROPRIATE INDICATOR WILL BE PLACED ON DOOR TO PATIENT’S ROOM • MODERATE (SCORE 6 -13)—ORANGE MAGNET • HIGH (>13—RED MAGNET) • PATIENT TO WEAR CORRESPONDING IDENTIFICATION BAND READING “FALL RISK” Figure 6. Fall Risk Assessment. (Johns Hopkins Medicine, 2007) • MODERATE—ORANGE BAND • HIGH—RED BAND
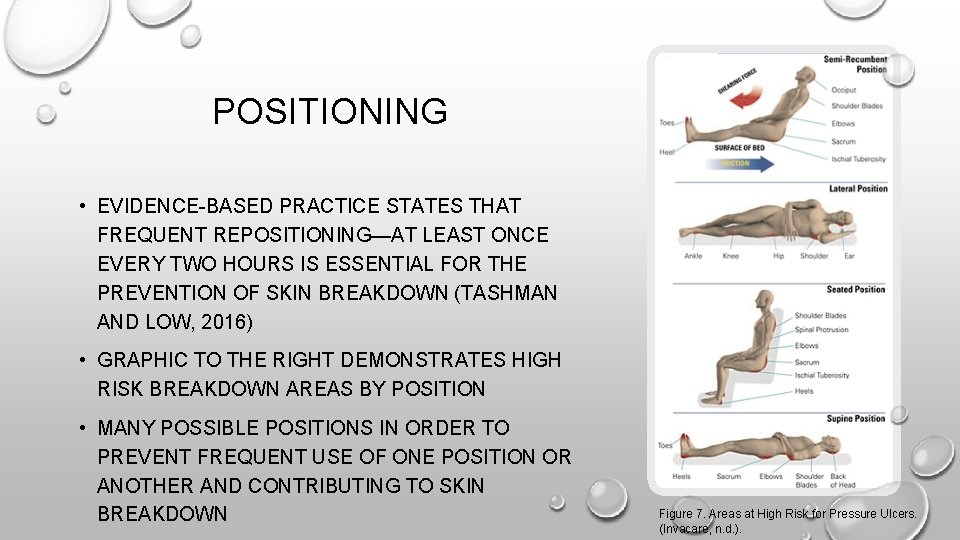
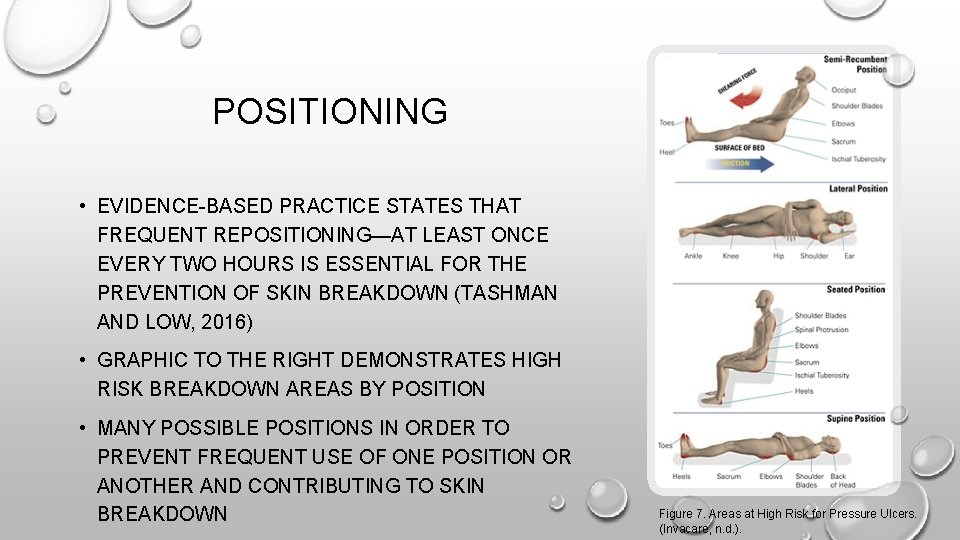
POSITIONING • EVIDENCE-BASED PRACTICE STATES THAT FREQUENT REPOSITIONING—AT LEAST ONCE EVERY TWO HOURS IS ESSENTIAL FOR THE PREVENTION OF SKIN BREAKDOWN (TASHMAN AND LOW, 2016) • GRAPHIC TO THE RIGHT DEMONSTRATES HIGH RISK BREAKDOWN AREAS BY POSITION • MANY POSSIBLE POSITIONS IN ORDER TO PREVENT FREQUENT USE OF ONE POSITION OR ANOTHER AND CONTRIBUTING TO SKIN BREAKDOWN Figure 7. Areas at High Risk for Pressure Ulcers. (Invacare, n. d. ).
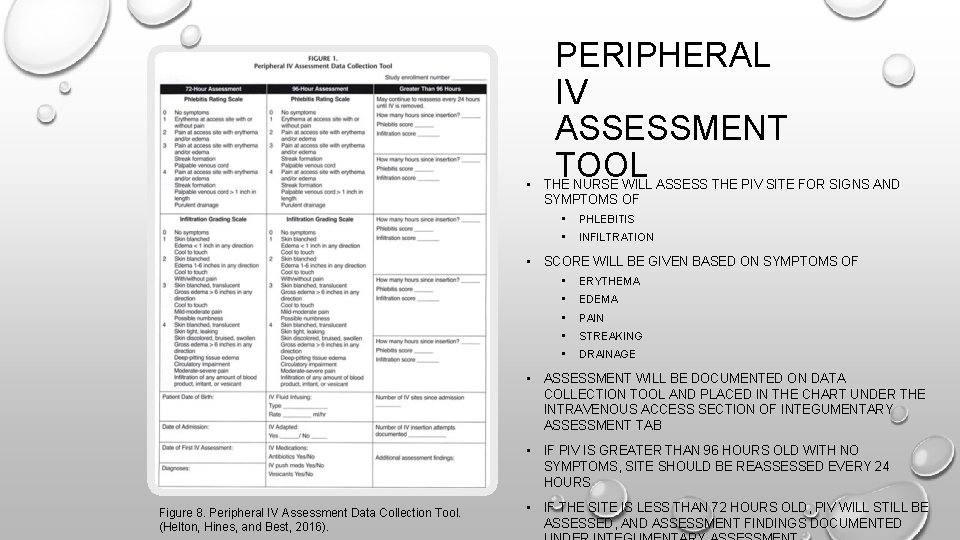
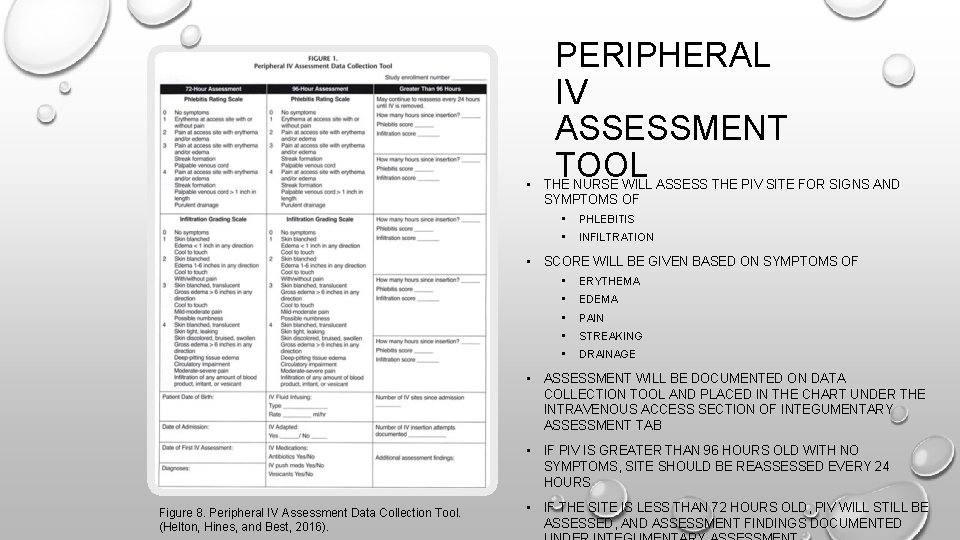
PERIPHERAL IV ASSESSMENT TOOL • THE NURSE WILL ASSESS THE PIV SITE FOR SIGNS AND SYMPTOMS OF • PHLEBITIS • INFILTRATION • SCORE WILL BE GIVEN BASED ON SYMPTOMS OF • ERYTHEMA • EDEMA • PAIN • STREAKING • DRAINAGE • ASSESSMENT WILL BE DOCUMENTED ON DATA COLLECTION TOOL AND PLACED IN THE CHART UNDER THE INTRAVENOUS ACCESS SECTION OF INTEGUMENTARY ASSESSMENT TAB • IF PIV IS GREATER THAN 96 HOURS OLD WITH NO SYMPTOMS, SITE SHOULD BE REASSESSED EVERY 24 HOURS Figure 8. Peripheral IV Assessment Data Collection Tool. (Helton, Hines, and Best, 2016). • IF THE SITE IS LESS THAN 72 HOURS OLD, PIV WILL STILL BE ASSESSED, AND ASSESSMENT FINDINGS DOCUMENTED
QUALITY IMPROVEMENT (QI) • APPRAISES DATA INVOLVING • PATIENT OUTCOMES • PROCESSES LEADING TO THOSE OUTCOMES • WORKS TO CONTINUOUSLY IMPROVE BY • IMPLEMENTING CHANGES • CONTINUOUSLY TESTING CHANGES • CREATING NEW ITERATIONS AS NECESSARY TO FURTHER IMPROVE PATIENT CARE OUTCOMES (SHERWOOD AND ZOMORODI, 2014)

STRATEGIES 1. HOURLY ROUNDING 2. DAILY MEDICATION COUNT TO REDUCE ERRORS 3. DAILY OBSERVATION OF FLUID BALANCE
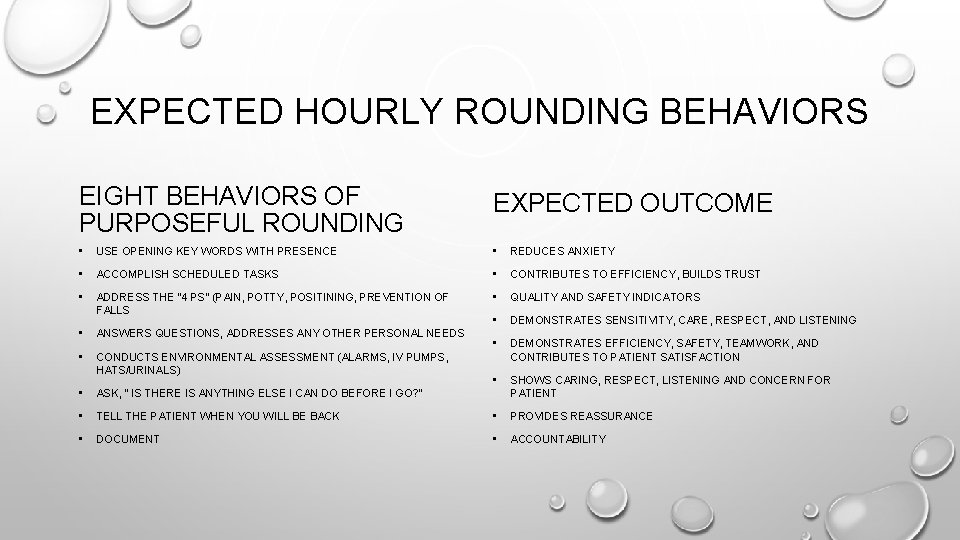
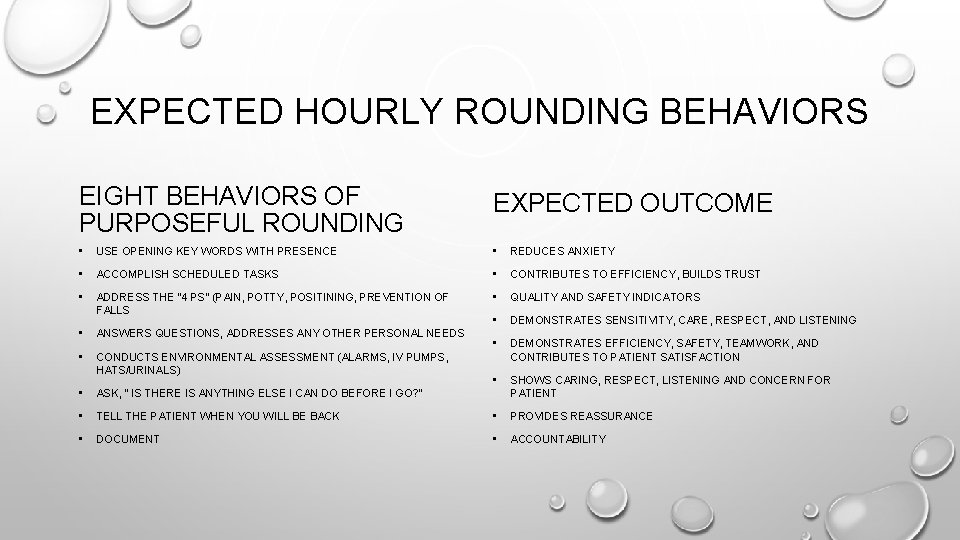
EXPECTED HOURLY ROUNDING BEHAVIORS EIGHT BEHAVIORS OF PURPOSEFUL ROUNDING EXPECTED OUTCOME • USE OPENING KEY WORDS WITH PRESENCE • REDUCES ANXIETY • ACCOMPLISH SCHEDULED TASKS • CONTRIBUTES TO EFFICIENCY, BUILDS TRUST • ADDRESS THE “ 4 PS” (PAIN, POTTY, POSITINING, PREVENTION OF FALLS • QUALITY AND SAFETY INDICATORS • DEMONSTRATES SENSITIVITY, CARE, RESPECT, AND LISTENING • ANSWERS QUESTIONS, ADDRESSES ANY OTHER PERSONAL NEEDS • • CONDUCTS ENVIRONMENTAL ASSESSMENT (ALARMS, IV PUMPS, HATS/URINALS) DEMONSTRATES EFFICIENCY, SAFETY, TEAMWORK, AND CONTRIBUTES TO PATIENT SATISFACTION • SHOWS CARING, RESPECT, LISTENING AND CONCERN FOR PATIENT • ASK, “ IS THERE IS ANYTHING ELSE I CAN DO BEFORE I GO? ” • TELL THE PATIENT WHEN YOU WILL BE BACK • PROVIDES REASSURANCE • DOCUMENT • ACCOUNTABILITY
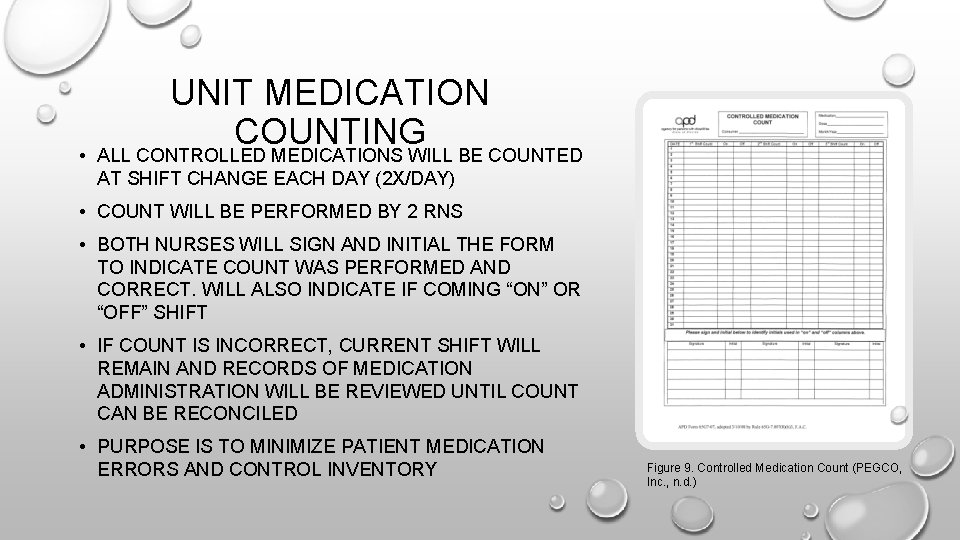
UNIT MEDICATION COUNTING • ALL CONTROLLED MEDICATIONS WILL BE COUNTED AT SHIFT CHANGE EACH DAY (2 X/DAY) • COUNT WILL BE PERFORMED BY 2 RNS • BOTH NURSES WILL SIGN AND INITIAL THE FORM TO INDICATE COUNT WAS PERFORMED AND CORRECT. WILL ALSO INDICATE IF COMING “ON” OR “OFF” SHIFT • IF COUNT IS INCORRECT, CURRENT SHIFT WILL REMAIN AND RECORDS OF MEDICATION ADMINISTRATION WILL BE REVIEWED UNTIL COUNT CAN BE RECONCILED • PURPOSE IS TO MINIMIZE PATIENT MEDICATION ERRORS AND CONTROL INVENTORY Figure 9. Controlled Medication Count (PEGCO, Inc. , n. d. )
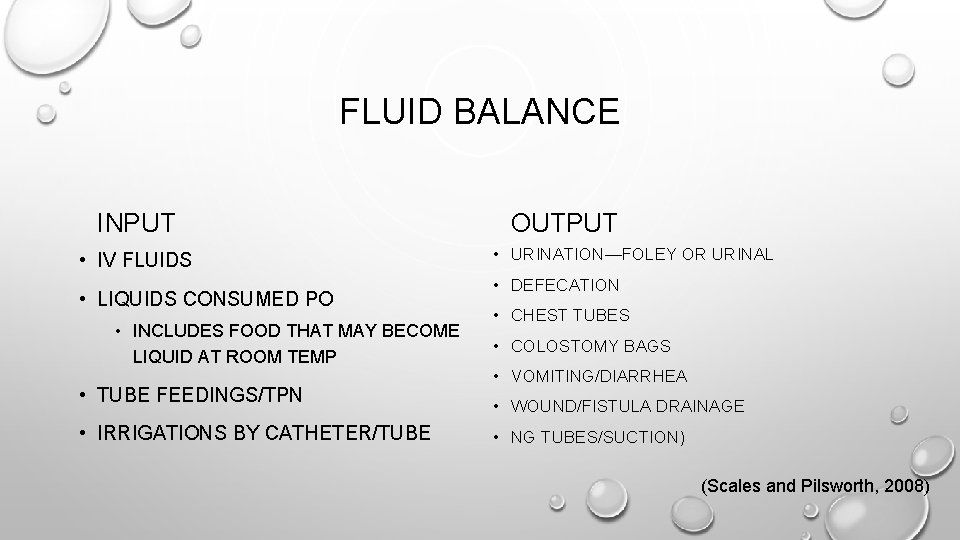
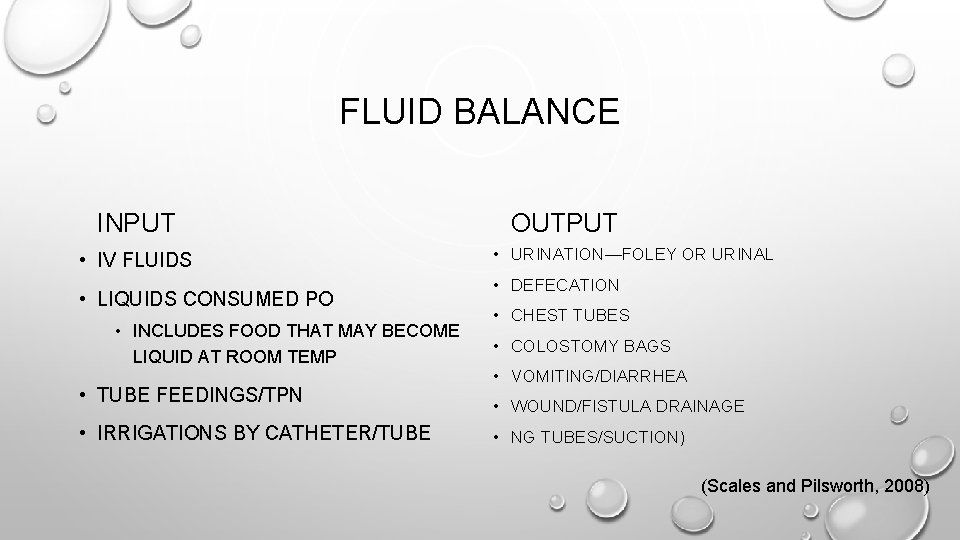
FLUID BALANCE INPUT • IV FLUIDS • LIQUIDS CONSUMED PO • INCLUDES FOOD THAT MAY BECOME LIQUID AT ROOM TEMP • TUBE FEEDINGS/TPN • IRRIGATIONS BY CATHETER/TUBE OUTPUT • URINATION—FOLEY OR URINAL • DEFECATION • CHEST TUBES • COLOSTOMY BAGS • VOMITING/DIARRHEA • WOUND/FISTULA DRAINAGE • NG TUBES/SUCTION) (Scales and Pilsworth, 2008)
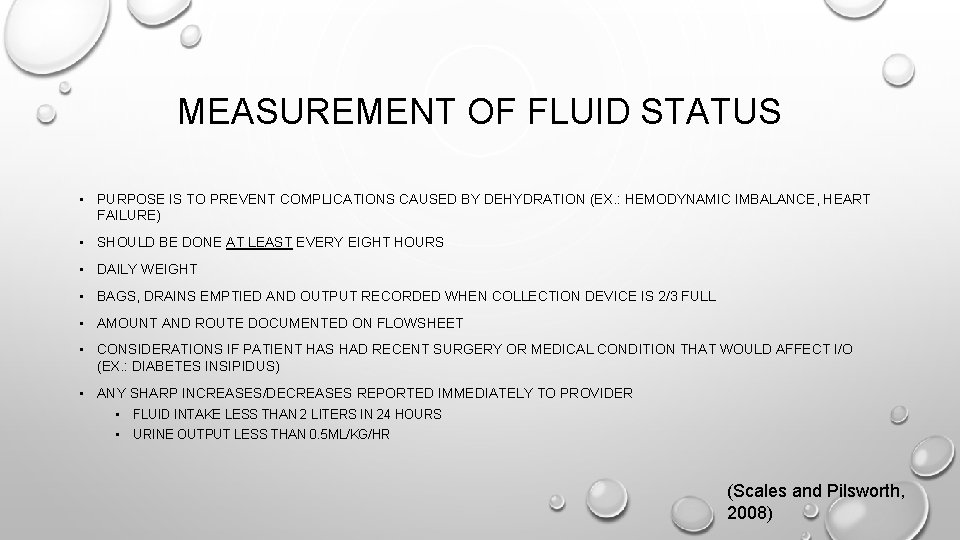
MEASUREMENT OF FLUID STATUS • PURPOSE IS TO PREVENT COMPLICATIONS CAUSED BY DEHYDRATION (EX. : HEMODYNAMIC IMBALANCE, HEART FAILURE) • SHOULD BE DONE AT LEAST EVERY EIGHT HOURS • DAILY WEIGHT • BAGS, DRAINS EMPTIED AND OUTPUT RECORDED WHEN COLLECTION DEVICE IS 2/3 FULL • AMOUNT AND ROUTE DOCUMENTED ON FLOWSHEET • CONSIDERATIONS IF PATIENT HAS HAD RECENT SURGERY OR MEDICAL CONDITION THAT WOULD AFFECT I/O (EX. : DIABETES INSIPIDUS) • ANY SHARP INCREASES/DECREASES REPORTED IMMEDIATELY TO PROVIDER • FLUID INTAKE LESS THAN 2 LITERS IN 24 HOURS • URINE OUTPUT LESS THAN 0. 5 ML/KG/HR (Scales and Pilsworth, 2008)

SAFETY • WORKS TO DECREASE ADVERSE OUTCOMES IN PATIENTS • USES EVIDENCE-BASED PRACTICE AS APPLICABLE WITH PATIENT SAFETY AT THE FOREFRONT • ACCOUNTABILITY • SYSTEMS AND PROCESSES • INDIVIDUAL PERFORMANCE (SHERWOOD AND ZOMORODI, 2014)
STRATEGIES 1. CREATION OF ”QUIET ZONE” WHEN ADMINISTERING MEDICATIONS—A DESIGNATED AREA WHICH NO ONE CAN ENTER WHILE MEDICATIONS ARE BEING DISPENSED 2. “TIME OUT” BEFORE ANY INVASIVE PROCEDURES 3. SBAR REPORTING
Video 3. Patient safety: Medication administration. (Mary Greeley Medical Center, 2013).
Video 4. Beside procedure time out. (United Memorial Medical Center, 2014).
Video 5. SBAR: Good communication basics. (Million Innovators, 2016).
INFORMATICS • INVOLVES TECHNOLOGY • MAINTAIN AND IMPROVE KNOWLEDGE • EVALUATE PATIENT OUTCOMES • MINIMIZE ERRORS • SUSTAIN DECISION-MAKING (SHERWOOD AND ZOMORODI, 2014)
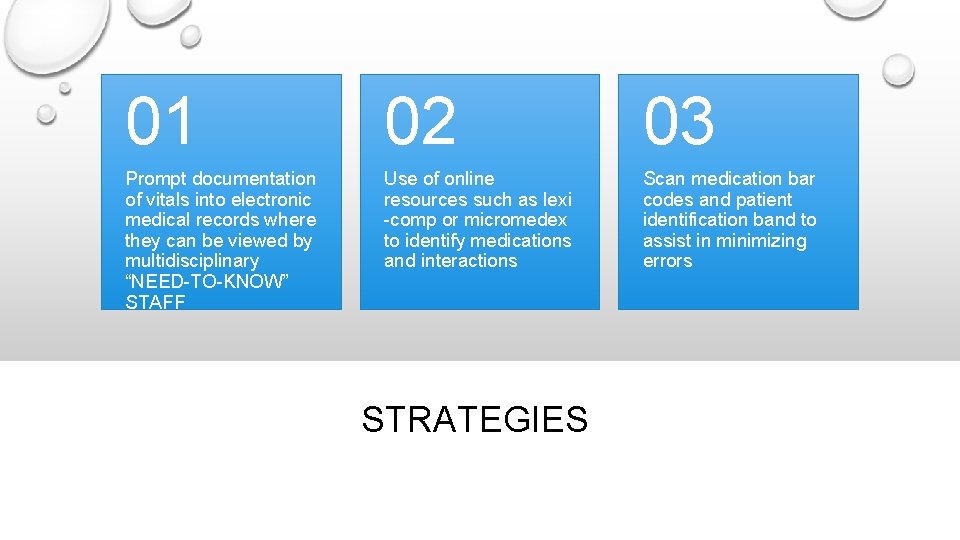
01 02 03 Prompt documentation of vitals into electronic medical records where they can be viewed by multidisciplinary “NEED-TO-KNOW” STAFF Use of online resources such as lexi -comp or micromedex to identify medications and interactions Scan medication bar codes and patient identification band to assist in minimizing errors STRATEGIES
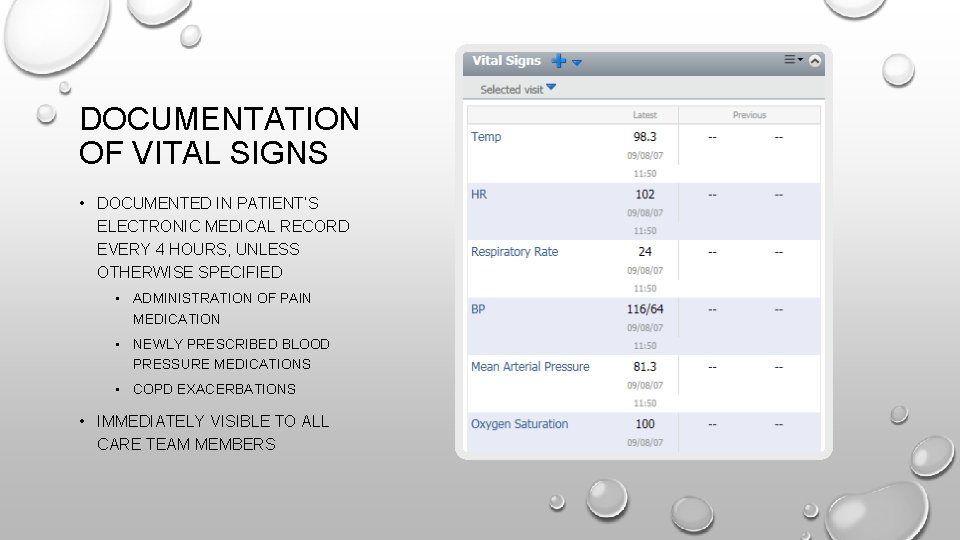
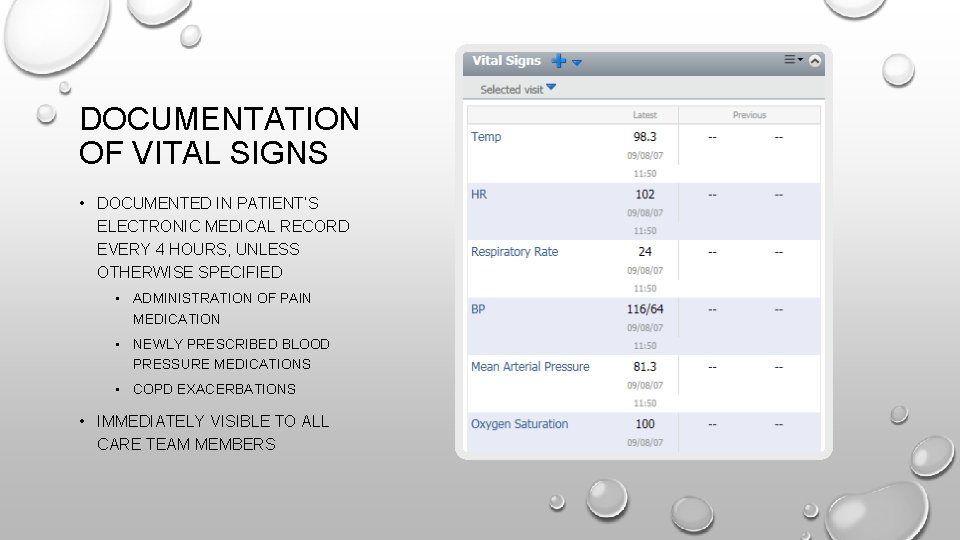
DOCUMENTATION OF VITAL SIGNS • DOCUMENTED IN PATIENT’S ELECTRONIC MEDICAL RECORD EVERY 4 HOURS, UNLESS OTHERWISE SPECIFIED • ADMINISTRATION OF PAIN MEDICATION • NEWLY PRESCRIBED BLOOD PRESSURE MEDICATIONS • COPD EXACERBATIONS • IMMEDIATELY VISIBLE TO ALL CARE TEAM MEMBERS
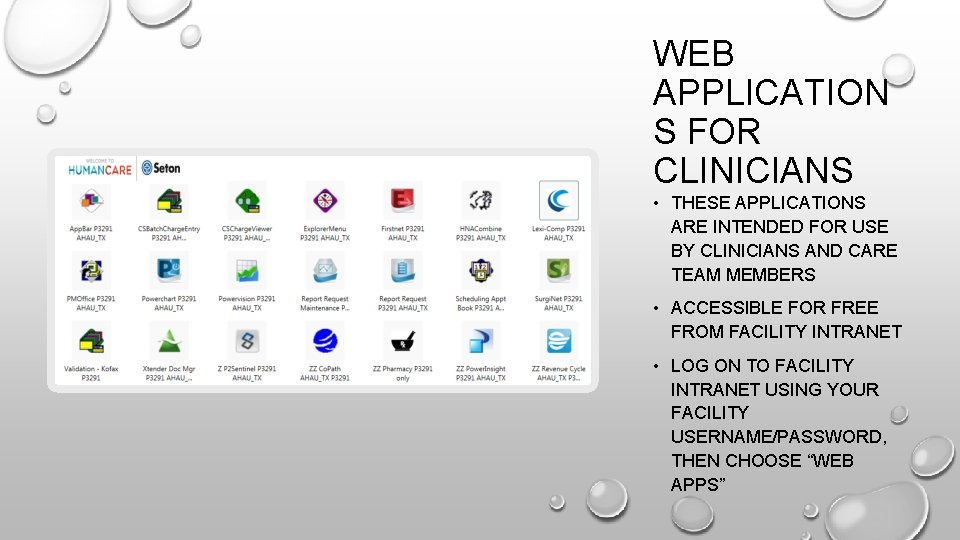
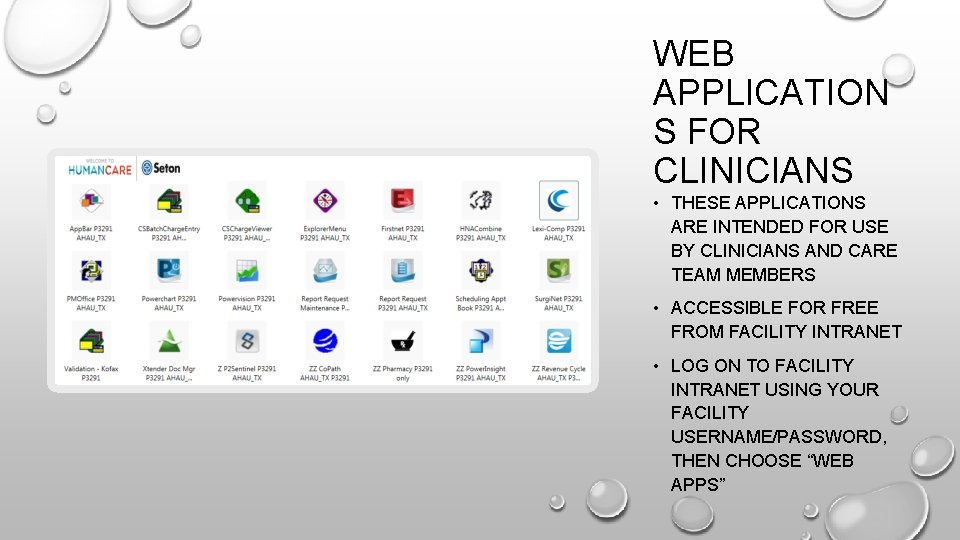
WEB APPLICATION S FOR CLINICIANS • THESE APPLICATIONS ARE INTENDED FOR USE BY CLINICIANS AND CARE TEAM MEMBERS • ACCESSIBLE FOR FREE FROM FACILITY INTRANET • LOG ON TO FACILITY INTRANET USING YOUR FACILITY USERNAME/PASSWORD, THEN CHOOSE “WEB APPS”
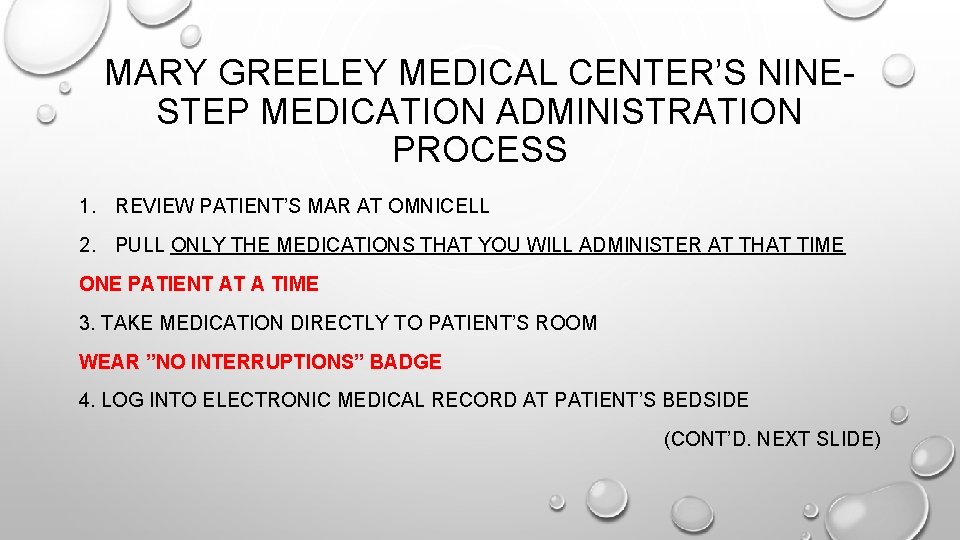
MARY GREELEY MEDICAL CENTER’S NINESTEP MEDICATION ADMINISTRATION PROCESS 1. REVIEW PATIENT’S MAR AT OMNICELL 2. PULL ONLY THE MEDICATIONS THAT YOU WILL ADMINISTER AT THAT TIME ONE PATIENT AT A TIME 3. TAKE MEDICATION DIRECTLY TO PATIENT’S ROOM WEAR ”NO INTERRUPTIONS” BADGE 4. LOG INTO ELECTRONIC MEDICAL RECORD AT PATIENT’S BEDSIDE (CONT’D. NEXT SLIDE)
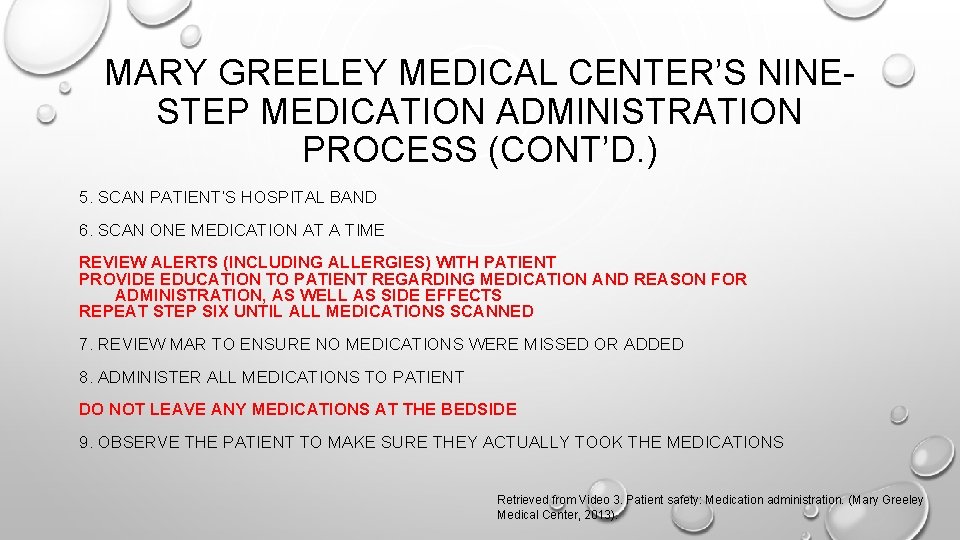
MARY GREELEY MEDICAL CENTER’S NINESTEP MEDICATION ADMINISTRATION PROCESS (CONT’D. ) 5. SCAN PATIENT’S HOSPITAL BAND 6. SCAN ONE MEDICATION AT A TIME REVIEW ALERTS (INCLUDING ALLERGIES) WITH PATIENT PROVIDE EDUCATION TO PATIENT REGARDING MEDICATION AND REASON FOR ADMINISTRATION, AS WELL AS SIDE EFFECTS REPEAT STEP SIX UNTIL ALL MEDICATIONS SCANNED 7. REVIEW MAR TO ENSURE NO MEDICATIONS WERE MISSED OR ADDED 8. ADMINISTER ALL MEDICATIONS TO PATIENT DO NOT LEAVE ANY MEDICATIONS AT THE BEDSIDE 9. OBSERVE THE PATIENT TO MAKE SURE THEY ACTUALLY TOOK THE MEDICATIONS Retrieved from Video 3. Patient safety: Medication administration. (Mary Greeley Medical Center, 2013).
REFERENCES CARE DELIVERY SYSTEM(S) EP 4. (N. D. ). RETRIEVED FEBRUARY 26, 2017, FROM HTTP: //WWW 1. UCIRVINEHEALTH. ORG/MAGNETNURSING/CLIENTHTML/69/SUPPLEMENTAL/EP 4 UCI. HTM C 2 KMEDICAL. (2010, FEBRUARY 16). HOSPITAL ADMISSION EXCERPT. (VIDEO FILE). RETRIEVED FROM HTTPS: //YOUTU. BE/VVNEG 7 MJTP 0 HELTON, J. , HINES, A. & BEST, J. (2016). PERIPHERAL IV SITE ROTATION BASED ON CLINICAL ASSESSMENT VS. LENGTH OF TIME SINCE INSERTION. MEDSURG NURSING, 25(1), 44 -49. JOHNS HOPKINS MEDICINE. INSTITUTE FOR JOHNS HOPKINS NURSING. BALTIMORE, MD, 2007. ACCESSED FEBRUARY 26, 2017. HTTP: //WWW. HOPKINSMEDICINE. ORG/INSTITUTE_NURSING/MODELS_TOOLS/FALL_RISK. HTML. KECK, B. (2014). PAIN MANAGEMENT: SAN DIEGO SERVICE AREA. (POWERPOINT PRESENTATION). RETRIEVED FEBRUARY 26, 2017 FROM HTTPS: //WWW. SLIDESHARE. NET/BAILEYKECK/PAIN-MANAGEMENTCOMPETENCY. MARY GREELEY MEDICAL CENTER (2013, MARCH 11). PATIENT SAFETY: MEDICATION ADMINISTRATION. (VIDEO FILE). RETRIEVED FEBRUARY 26, 2017 FROM HTTPS: //YOUTU. BE/AOXWSK 3 QXDW MILLION INNOVATORS. (2016, JUNE 7). SBAR: GOOD COMMUNICATION BASICS. (VIDEO FILE). RETRIEVED FEBRUARY 26, 2017 FROM HTTPS: //YOUTU. BE/3_-KZ 3 PWFYO NORTHWEST MEDICAL CENTER. HOSPITAL OF THE FUTURE. (N. D. ). ACCESSED FEBRUARY 26, 2017. HTTP: //NORTHWESTMED. COM/CAMPAIGNS/HOSPITAL-OF-THE-FUTURE. PATRICIAN, P. A. (2016). UNITING ACADEMIA AND PRACTICE IN NURSING: USING QSEN TO IMPROVE THE QUALITY AND SAFETY OF HEALTH CARE. AMERICAN NURSE TODAY, 11(1), 33.
REFERENCES (CONT’D. ) PEGCO, INC. (N. D. ). APD 65 G-7 MEDICATION MANAGEMENT PROGRAM. RETRIEVED FEBRUARY 27, 2017, FROM HTTP: //WWW. PEGCOINC. NET/DCF_MED_MANAGEMENT 1. HTM REYNOLDS, D. (2014, JANUARY 23). INTERDISCIPLINARY CARE TEAM: CASE ONE. (VIDEO FILE). RETRIEVED FEBRUARY 26, 2017 FROM HTTPS: //YOUTU. BE/BYDUZL 5 ZUL 0 ROSARIO, E. R. , KAPLAN, S. E. , KHONSARI, S. , & PATTERSON, D. (2014). PREDICTING AND ASSESSING FALL RISK IN AN ACUTE INPATIENT REHABILITATION FACILITY. REHABILITATION NURSING, 39(2), 86 -93. DOI: 10. 1002/RNJ. 114 SCALES K, PILSWORTH J (2008) THE IMPORTANCE OF FLUID BALANCE IN CLINICAL PRACTICE. NURSING STANDARD. 22, 47, 50 -57. SHERWOOD, G. , & ZOMORODI, M. (2014). A NEW MINDSET FOR QUALITY AND SAFETY: THE QSEN COMPETENCIES REDEFINE NURSES' ROLES IN PRACTICE. NEPHROLOGY NURSING JOURNAL, 41(1), 15 -72. THE STATE OF PAIN | THE AMERICAN NURSE. (2014, JANUARY 2). RETRIEVED FEBRUARY 26, 2017, FROM HTTP: //WWW. THEAMERICANNURSE. ORG/2014/01/02/THE-STATE-OF-PAIN/ TASHMAN, N. & LOW, S. (2016). IMPROVING HOSPITAL-ACQUIRED PRESSURE ULCER PREVENTION ON AN ORTHOPEDIC UNIT. MEDSURG NURSING, 4 -7. UNITED MEMORIAL MEDICAL CENTER. (2014, MARCH 6). BEDSIDE PROCEDURE TIME OUT. (VIDEO FILE). RETRIEVED FEBRUARY 26, 2017 FROM HTTPS: //YOUTU. BE/GO 2 CV 38 VZO
 Qsen quality and safety education for nurses
Qsen quality and safety education for nurses Quality safety education for nurses
Quality safety education for nurses Megan childers
Megan childers Quality and safety education for nurses
Quality and safety education for nurses Qsen definition
Qsen definition Qsen competency safety
Qsen competency safety Qsen teamwork and collaboration definition
Qsen teamwork and collaboration definition Qsen teamwork and collaboration
Qsen teamwork and collaboration Cassie deslila
Cassie deslila Cassie edgar
Cassie edgar Structural geology practical exercises
Structural geology practical exercises Cassie delisle
Cassie delisle Uncle hammer quotes
Uncle hammer quotes What is a theme
What is a theme Cassie ostermier
Cassie ostermier Mandy e cassie
Mandy e cassie Cassie hoyt nopixel
Cassie hoyt nopixel Cassie venable
Cassie venable Cassie chisholm
Cassie chisholm Cassie crotty
Cassie crotty Georges braque (1882-1963)
Georges braque (1882-1963) Cassie brown tdi
Cassie brown tdi Cassie soeffing
Cassie soeffing Cassie baxter
Cassie baxter Properties of special right triangles
Properties of special right triangles Qsen competencies
Qsen competencies Qsen competencies
Qsen competencies Qsen
Qsen Qsen competencies examples
Qsen competencies examples Qsen simulation rubric
Qsen simulation rubric Qsen unfolding case studies
Qsen unfolding case studies Quality control and quality assurance
Quality control and quality assurance Basic concept of quality control and quality assurance pdf
Basic concept of quality control and quality assurance pdf Chapter 27 patient safety and quality
Chapter 27 patient safety and quality Safety quality and productivity
Safety quality and productivity Ndis orientation module
Ndis orientation module Importance of food quality
Importance of food quality Patient safety and quality care movement
Patient safety and quality care movement Blood safety and quality regulations
Blood safety and quality regulations Tnnmc
Tnnmc Define inadequate
Define inadequate Eagle plains public school
Eagle plains public school