PERTHES DISEASE LeggCalvePerthes Disease Coxa Plana PROFESSORAYMAN SOLIMAN




















- Slides: 50
PERTHES DISEASE (Legg-Calve-Perthes Disease, Coxa Plana) PROFESSORAYMAN SOLIMAN ISMAIL
PERTHES DISEASE (Legg-Calve-Perthes Disease. Coxa Plana) Perthes disease is a condition of the immature hip caused by necrosis of the femoral epiphysis; the femoral head subsequently deforms as necrotic bone is replaced by living bone.
Incidence Age: 4 -8 years Sex: Males are affected more than females 4 – 1 Bilateral affection in 15% of cases.
Etiology The etiology of necrosis is UNKNOWN. The most popular theory is interruption of the arterial supply to the hip, with possible multiple episodes of infarction. Transient synovitis of the hip has been thought to be associated with Perthes disease (12% of cases will develop Perthes disease)
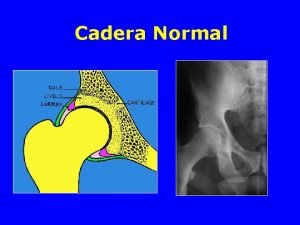
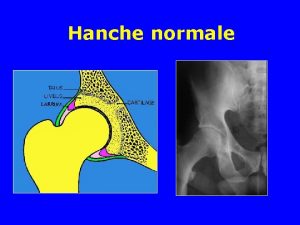
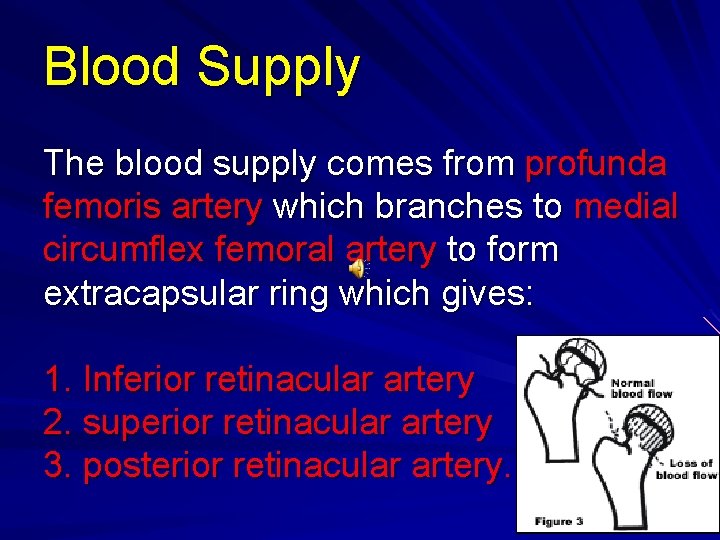
Blood Supply The blood supply comes from profunda femoris artery which branches to medial circumflex femoral artery to form extracapsular ring which gives: 1. Inferior retinacular artery 2. superior retinacular artery 3. posterior retinacular artery.
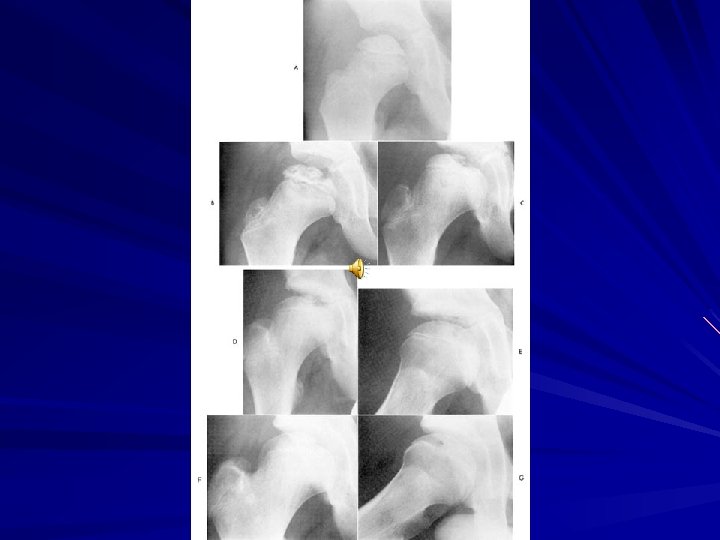
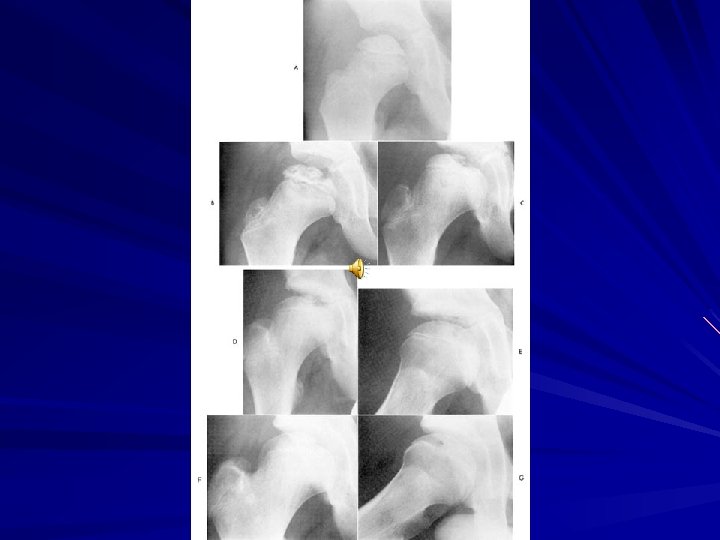
Natural History of Perthes disease 4 stages 1. Necrosis 2. Fragmentation 3. Re-ossification 4. Remodeling average 5 months average 7 months average 20 -40 months until skeletal maturity
1. Necrotic Stage There is necrosis of the epiphysis due to vascular occlusion The necrotic epiphysis becomes radiologically dense. This is due to relative osteoporosis of the viable bone, increases calcification of necrotic bone and deposition of new bone on necrotic trabeculae.

2. Fragmentation stage as continued stress is applied across the hip, the necrotic bone will be crushed. Osteoclasts will replace the distorted trabeculae and fibrocartilage will fill the defect. The femoral epiphysis will deform.

Re-ossification stage: Following fragmentation, re-ossification of the fibrovascular tissue will occur. It starts at the margin of the epiphysis and progresses until the entire epiphysis is reossified.
Remodeling stage The femoral head continues to remodel until the patient reaches maturity.


CLINICAL FEATURES * EARLY in the course of Perthes disease (Necrosis, Fragmentation), the presentation is that of synovitis. There is pain and limp of insidious onset. . Pain is usually in the groin area, radiating to thigh or knee. . Limp is typically antalgic gait. * If the patient presents LATE (re-ossification – remodeling), there is limp (antalgic, short-leg or stiff hip). . Pain is mild and usually in the hip area.

PROGNOSIS. More than 50% of all patients with Perthes disease will do well without treatment. . But 85% will develop osteoarthritis before 65 years of age. . Children less than 6 years of age at onset of symptoms have a good prognosis, whereas those older than 9 years have a poor prognosis.

TREATMENT. The goal f treatment in Perthes disease is the prevention of deformity of the femoral head. . The treatment involves maintaining a full range of motion of the hip and by containing the femoral head in the acetabulum. . In containment treatment, the normally shaped acetabulum is used as a mold to prevent deformity of the femoral head.
The femoral head can be directed into the depth of the acetabulum in one of the following ways: 1. Positioning of the leg in abduction and internal rotation. 2. Positioning the leg in abduction and flexion. 1. and 2. can be achieved by plaster cast or braces. 3. Performing a varus femoral osteotomy to redirect the femoral head into the acetabulum. 4. Performing a pelvic osteotomy to redirect the acetabulum over the femoral head.




SLIPPED UPPER (CAPITAL) FEMORAL EPIPHYSIS = SCFE = ADOLESCENT COXA VARA
This is an affection of late childhood in which the upper femoral epiphysis is displaced from its normal position upon the femoral neck. The displacement occurs at the growth plate (epiphyseal line).



INCIDENCE. 2 cases per 100, 000. More common in boys than girls. Peak age is in early puberty, range 10 -16 ys. Bilateral affection in 25% of cases
CAUSE UNKNOWN. The condition is associated with overweight in about 50% of cases: a. mechanical shear forces on the physis associated with obesity has been thought to cause SCFE. b. Endocrine reasons such as growth hormone deficiency, hypothyroidism and hypogonadism have been implicated. . In 50% of cases, the patient is of normal build.
CLINICAL PRESENTATION 1. PRESLIP 2. ACUTE SLIP 3. CHRONIC SLIP 4. ACUTE ON TOP OF CHRONIC 10% 60% 20%
PRESLIP 10% This is essentially an x-ray finding There is irregularity and widening of the epiphyseal plate. The most constant positive finding in preslip is lack of medial rotation in patients who complain of pain and weakness in the leg.

ACUTE SLIP 10%. Sudden onset of symptoms for 2 weeks or less. . It seems that acute slips occur as a traumatic event in patients who have preslip without displacement.

Acute, severe slip
CHRONIC SLIP 60% . Symptoms existing for more than 2 weeks. . Pain in groin and thigh, OR pain in the region of the knee. . Clinically, there is characteristic limitation of internal rotation. . A constant clinical sign is external rotation of the leg when the hip is flexed.
Chronic slip
ACUTE ON TOP OF CHRONIC SLIP 20% a. Symptoms for longer than 2 weeks and recent sudden exacerbation of pain following trivial injury. b. Patients may initially – on clinical grounds – thought to have an acute slip, but radiological results show that there has been a chronic process going on for some time, with superimposed acute slip.
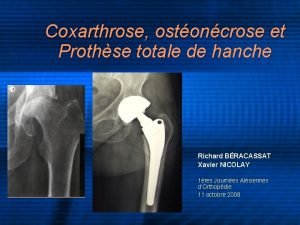
RADIOLOGIC ASSESSMENT On anteroposterior view, SCFE can be divided into mild, moderate or severe according to the amount of displacement of the femoral neck.
1. MILD: The neck is displaced less than 1/3 rd of the diameter of the head. 2. MODERATE: The neck is displaced between 1/3 rd and ½ of the diameter of the head. 3. SEVERE: The neck is displaced more than ½ the diameter of the head.


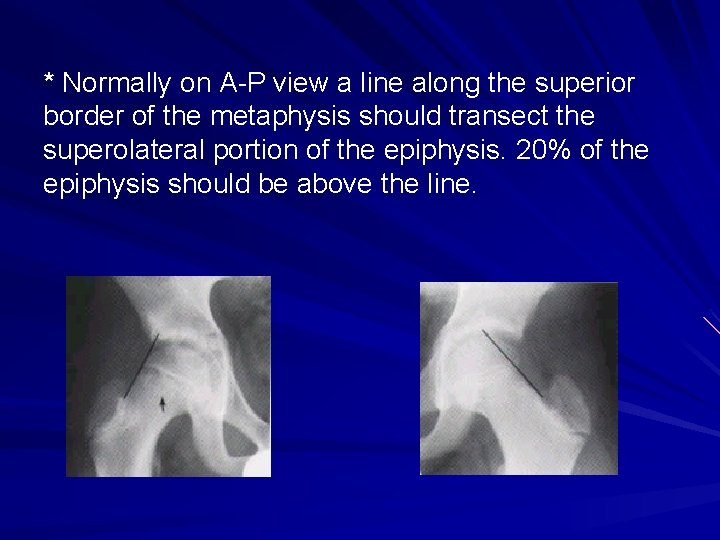
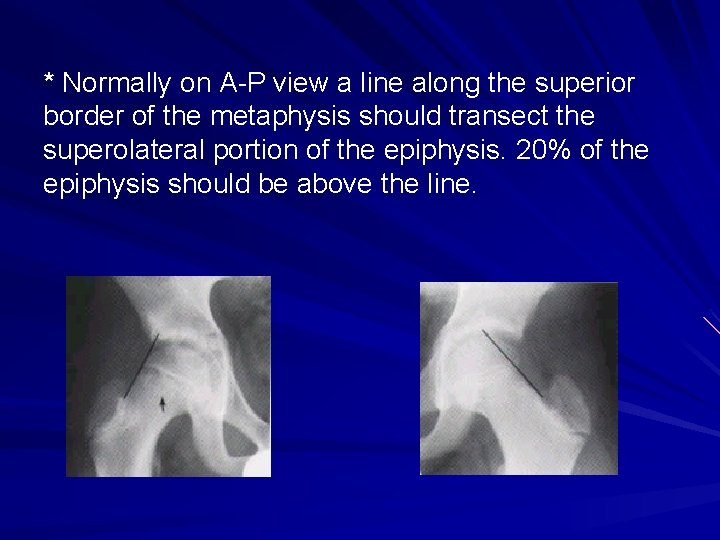
* Normally on A-P view a line along the superior border of the metaphysis should transect the superolateral portion of the epiphysis. 20% of the epiphysis should be above the line.
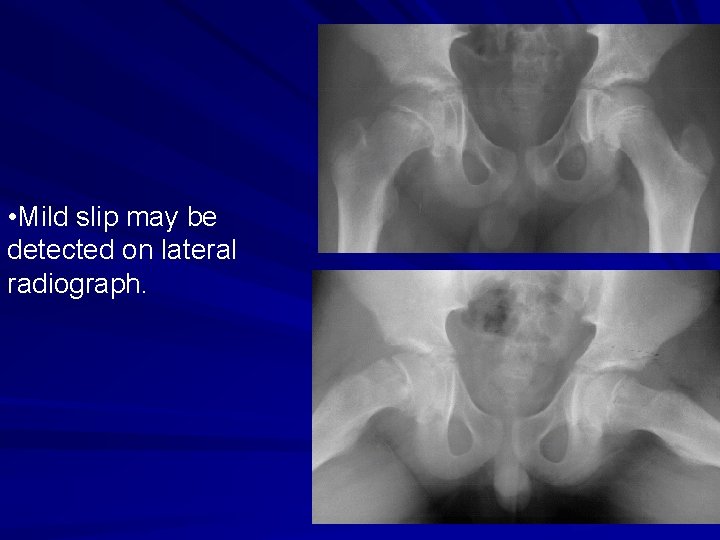
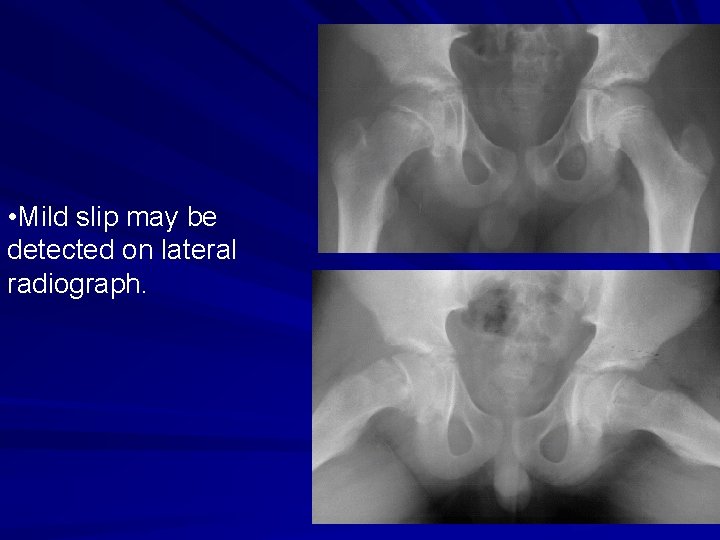
• Mild slip may be detected on lateral radiograph.
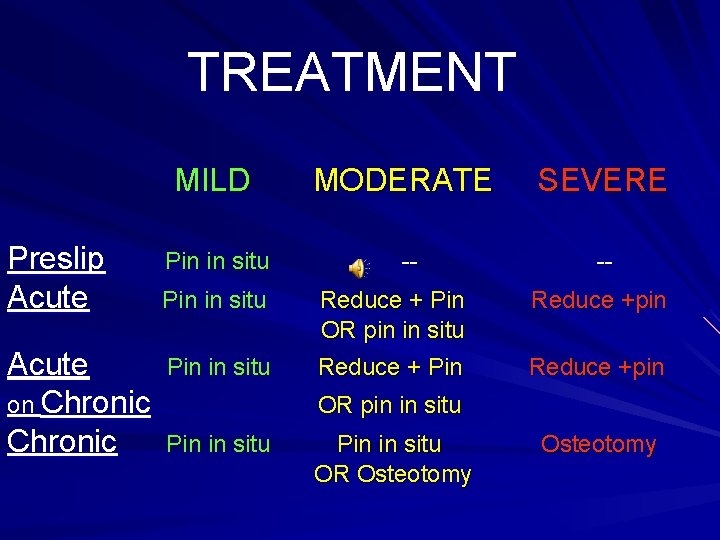
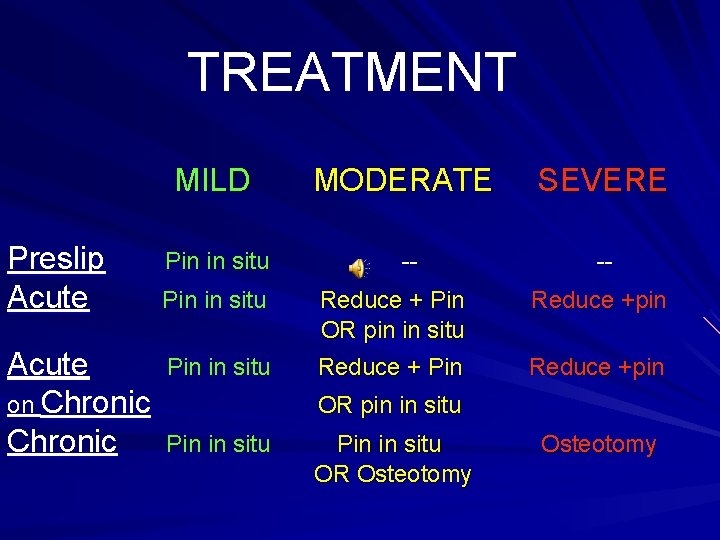
TREATMENT Preslip Acute on Chronic MILD MODERATE SEVERE Pin in situ -- -- Pin in situ Reduce + Pin OR pin in situ Reduce + Pin Reduce +pin OR pin in situ Pin in situ OR Osteotomy

COMPLICATIONS 1. AVASCULAR NECROSIS: occurs in 1015% of cases. 2. CHONDROLYSIS: There is lysis and damage to the articular cartilage. Usually associated with pin penetration into the joint, but can occur in patients who have not been submitted to surgery.
TWO IMPORTANT CONDITIONS 1. TRAUMATIC SCFE: . Usually before 10 yrs. . Definite history of trauma (severe). 2. PATHOLOGICAL: following septic arthritis.


THANK YOU
 Hip pointer injury pictures
Hip pointer injury pictures Gage sign
Gage sign Perthes disease
Perthes disease Frog leg
Frog leg Dr nadia soleman
Dr nadia soleman Hemoglobin
Hemoglobin Added heart sounds
Added heart sounds Prophet soliman
Prophet soliman Soliman logo
Soliman logo Calve legg perthes hund
Calve legg perthes hund Perthes vs sufe
Perthes vs sufe Sindrome di cockett
Sindrome di cockett Perthes vs sufe
Perthes vs sufe Neuhof sign dvt
Neuhof sign dvt Lateral fleksiyon
Lateral fleksiyon Coxa profunda
Coxa profunda Crus varum
Crus varum Genua recurvata
Genua recurvata Metoda coxa
Metoda coxa Torsion femoral interna
Torsion femoral interna Biceps da coxa
Biceps da coxa Medidas antropométricas pdf
Medidas antropométricas pdf Clasificacion fractura de cadera
Clasificacion fractura de cadera Transverse genicular ligament
Transverse genicular ligament Coxa valga angle
Coxa valga angle Aplicação intramuscular
Aplicação intramuscular Gonalgie dex
Gonalgie dex Vis canulée hanche
Vis canulée hanche Hatanpään kantasairaala
Hatanpään kantasairaala Coxa retroversa
Coxa retroversa Coxa retrosa
Coxa retrosa Anesthesia root word
Anesthesia root word Coxa profunda traitement
Coxa profunda traitement Tekonivelinfektio
Tekonivelinfektio Polven tekonivelleikkaus hinta coxa
Polven tekonivelleikkaus hinta coxa Coxa anatomia
Coxa anatomia Coxa saltan
Coxa saltan Communicable disease and non communicable disease
Communicable disease and non communicable disease Biznis plan definicija
Biznis plan definicija Fluidodinâmica
Fluidodinâmica Ejercicios tripa plana
Ejercicios tripa plana Curva de spee concava
Curva de spee concava Modelado antrópico
Modelado antrópico Naslovna strana biznis plana
Naslovna strana biznis plana Dibujo con superficie
Dibujo con superficie Zinn halkası içinden geçenler
Zinn halkası içinden geçenler Sutura plana escamosa e serreada
Sutura plana escamosa e serreada Imaginea plastica bidimensionala plana
Imaginea plastica bidimensionala plana Polígono intruso
Polígono intruso Qumica
Qumica Placa plana
Placa plana