LeggCalvePerthes Assoc Prof Melih Gven Yeditepe University Hospital
- Slides: 31
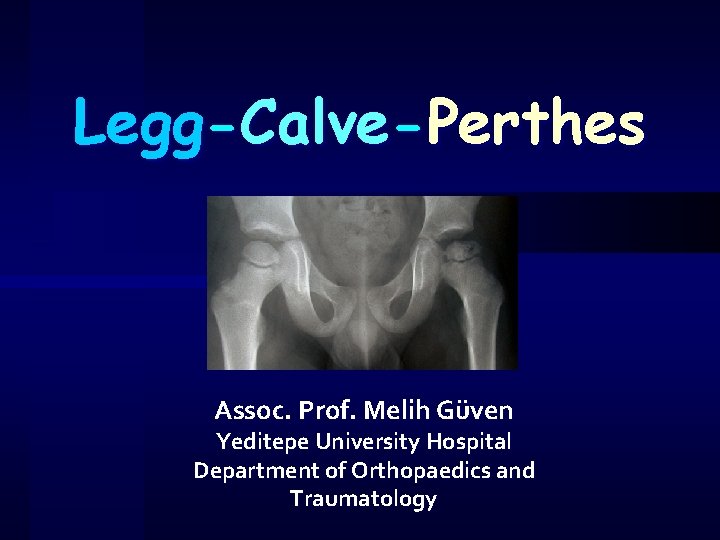
Legg-Calve-Perthes Assoc. Prof. Melih Güven Yeditepe University Hospital Department of Orthopaedics and Traumatology
Learning Objectives ü ü ü ü Should be able to explain the etiopathogenesis of osteonecrosis of the femoral head in children. Should be able to list the stages and clinical, radiographic features of the stages. Should be able to define the risk factors of Perthes’ disease. Should be able to list the radiographic features of the femoral head under risk. Should be able to make differential diagnosis of Perthes’ disease. Should be able to explain the clinical findings of Perthes’ disease. Should be able to list conservative and surgical treatment methods of Perthes’ disease.
Perthes disease Idiopathic juvenile avascular necrosis of the femoral head ü Waldenström disease ü 1/1200 ü E/K = 7 -8/1 ü Most commonly is seen in children aged 4 -8 (2 -12) years, with an average of 7 years ü %10 -15 bilateral ü
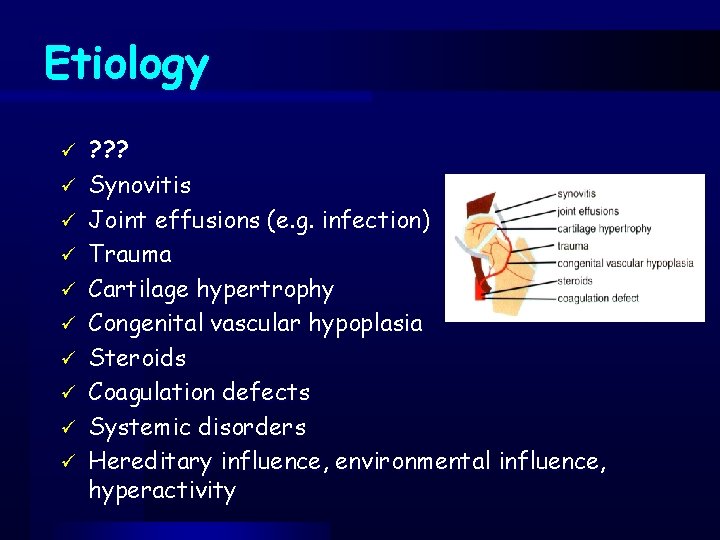
Etiology ü ü ü ü ü ? ? ? Synovitis Joint effusions (e. g. infection) Trauma Cartilage hypertrophy Congenital vascular hypoplasia Steroids Coagulation defects Systemic disorders Hereditary influence, environmental influence, hyperactivity
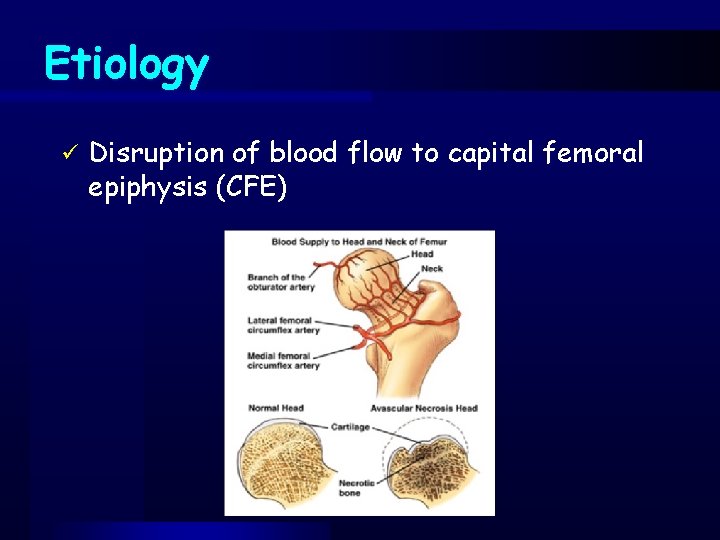
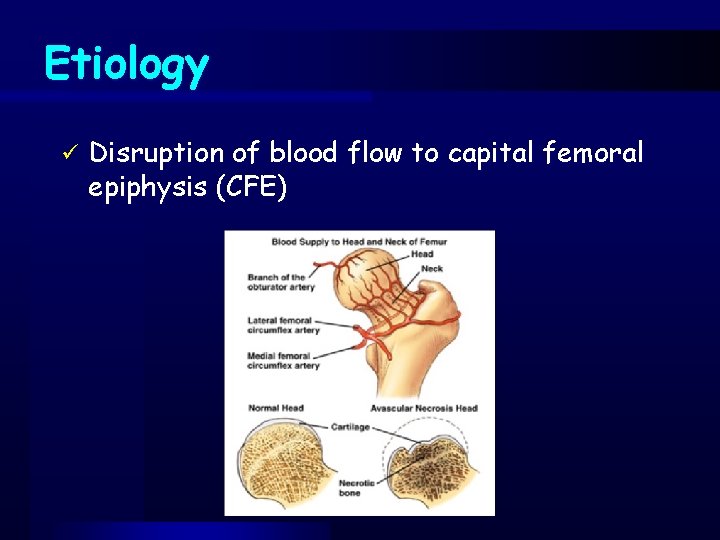
Etiology ü Disruption of blood flow to capital femoral epiphysis (CFE)
Pathology The blood supply to the capital femoral epiphysis is interrupted (arteries and veins) ü Bone infarction occurs, especially in the subchondral cortical bone, while articular cartilage continues to grow. (Articular cartilage grows because its nutrients come from the synovial fluid) ü Revascularization occurs, and new bone ossification starts ü Changes to the epiphyseal growth plate occur secondary to the subchondral fracture ü
Clinical symptoms ü Hip and groin pain, which may be referred to the thigh ü± knee pain !!! ü Limp – with or without pain üEspecially Trendelenburg test (+) ü Limitation in abduction and internal rotation (decreased range of motion) ü Atrophy of thigh muscles ü Flexion contracture
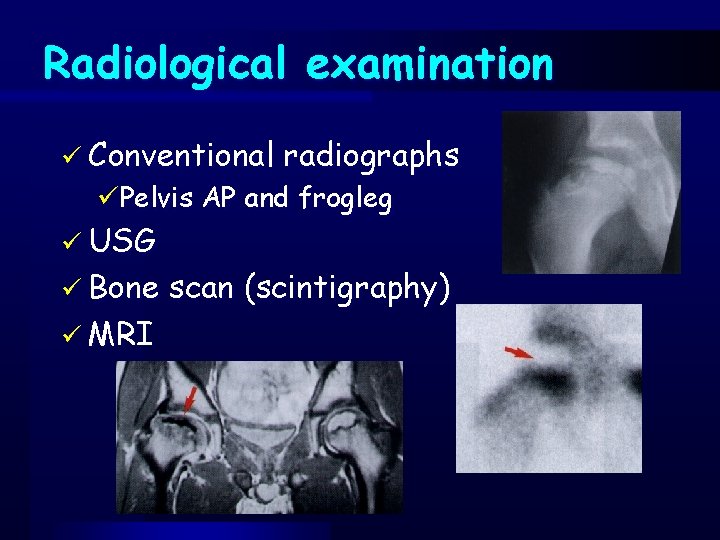
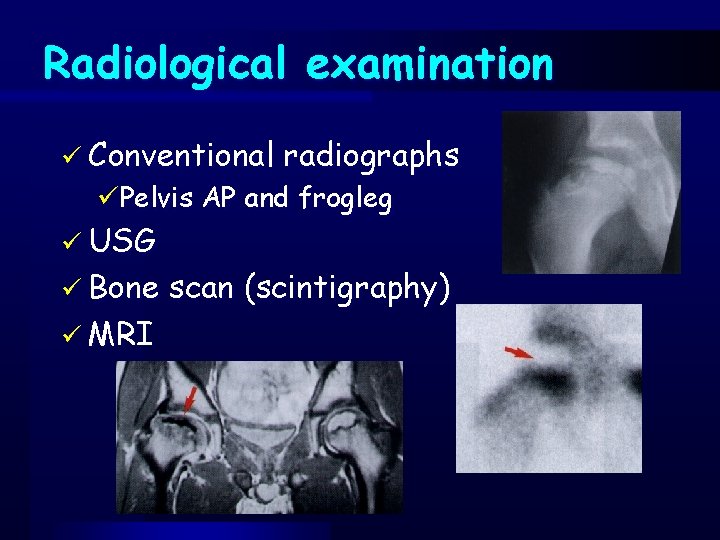
Radiological examination ü Conventional radiographs üPelvis AP and frogleg ü USG ü Bone ü MRI scan (scintigraphy)
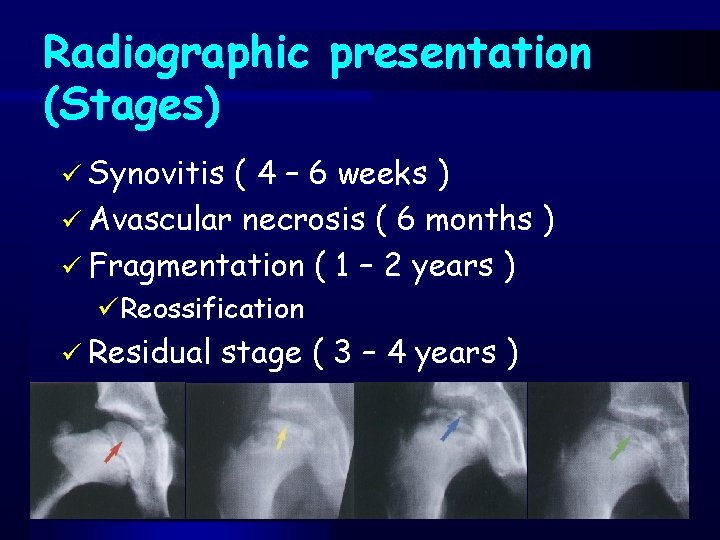
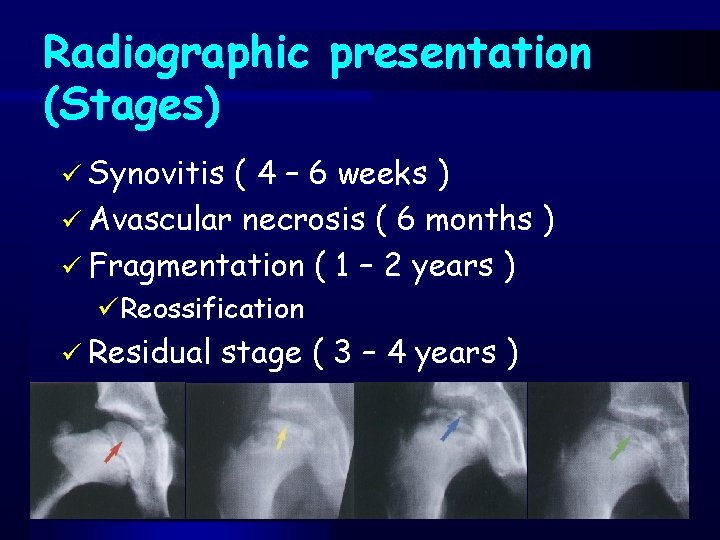
Radiographic presentation (Stages) ü Synovitis ( 4 – 6 weeks ) ü Avascular necrosis ( 6 months ) ü Fragmentation ( 1 – 2 years ) üReossification ü Residual stage ( 3 – 4 years )
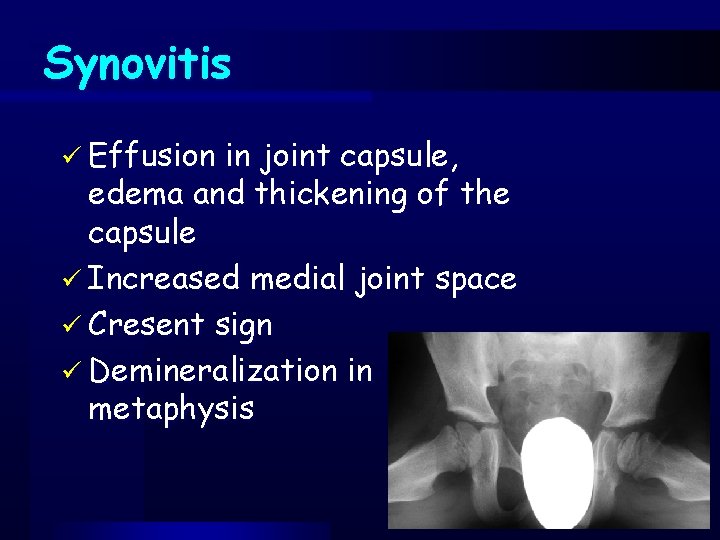
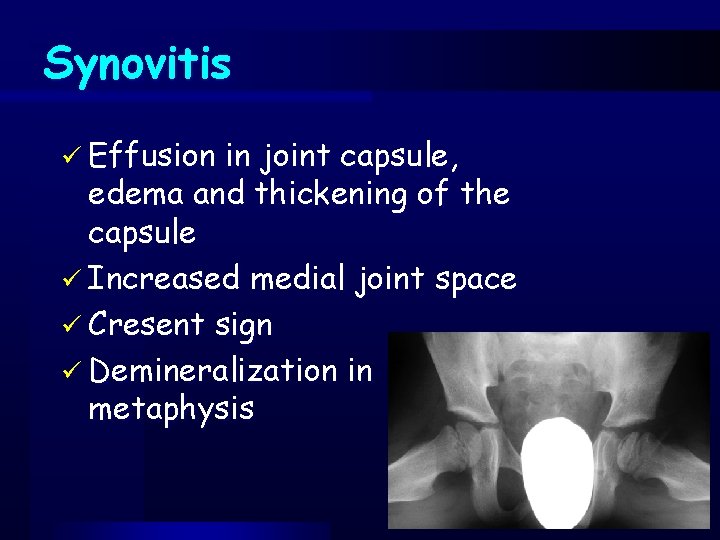
Synovitis ü Effusion in joint capsule, edema and thickening of the capsule ü Increased medial joint space ü Cresent sign ü Demineralization in metaphysis
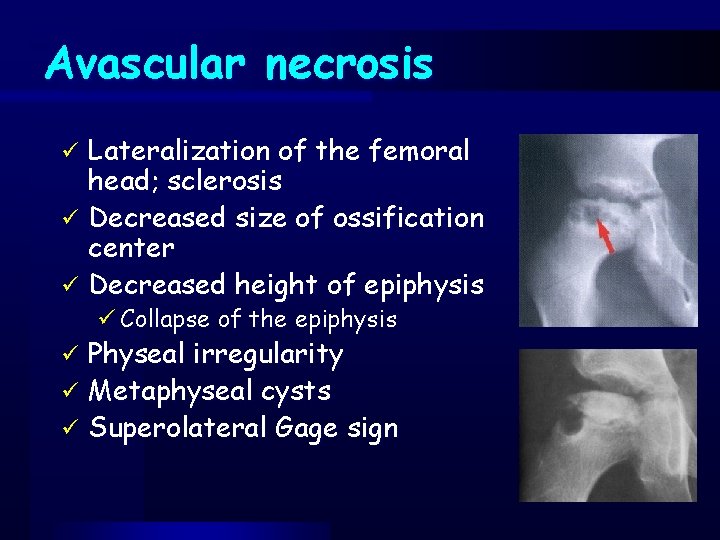
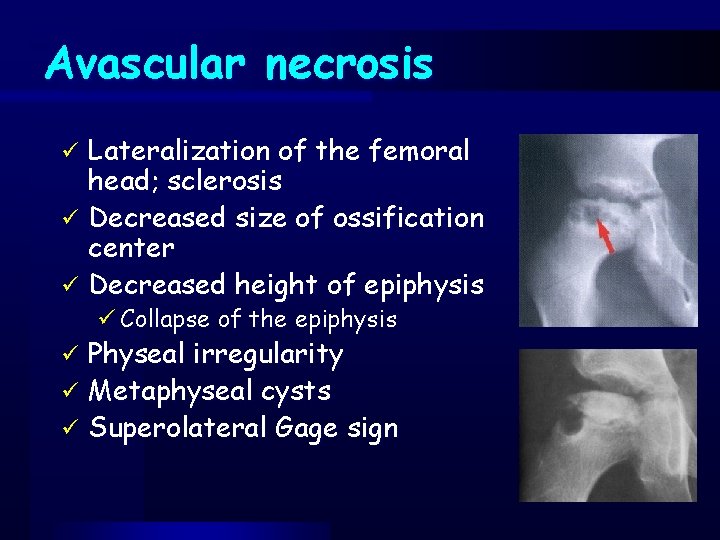
Avascular necrosis Lateralization of the femoral head; sclerosis ü Decreased size of ossification center ü Decreased height of epiphysis ü ü Collapse of the epiphysis Physeal irregularity ü Metaphyseal cysts ü Superolateral Gage sign ü
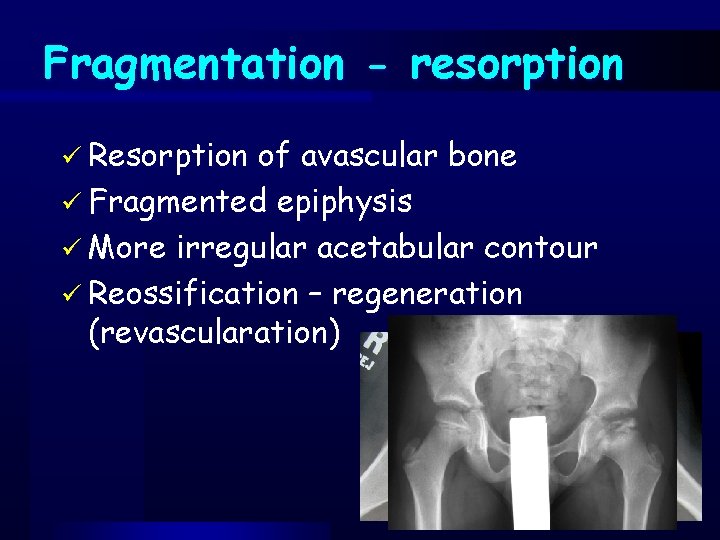
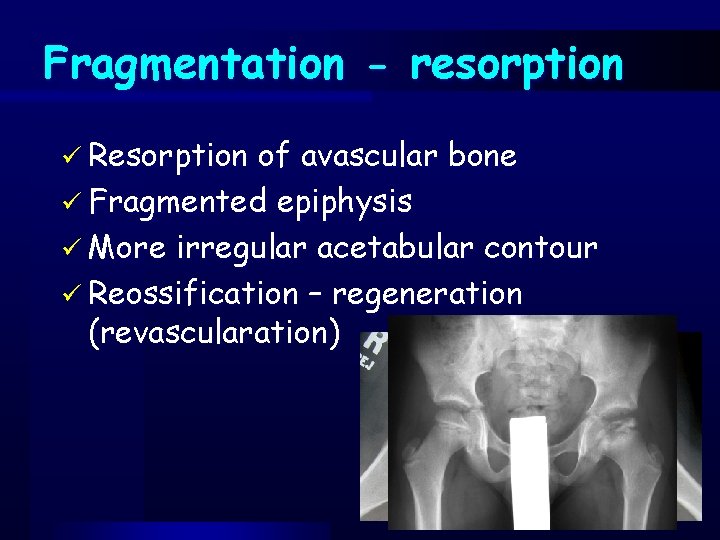
Fragmentation - resorption ü Resorption of avascular bone ü Fragmented epiphysis ü More irregular acetabular contour ü Reossification – regeneration (revascularation)
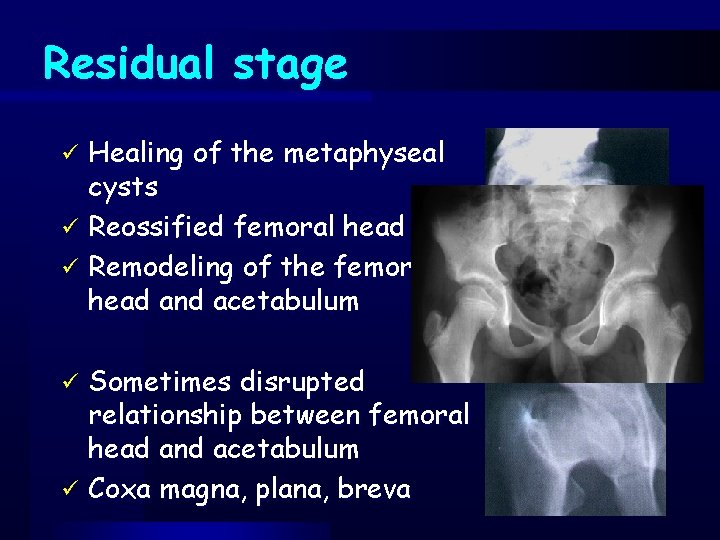
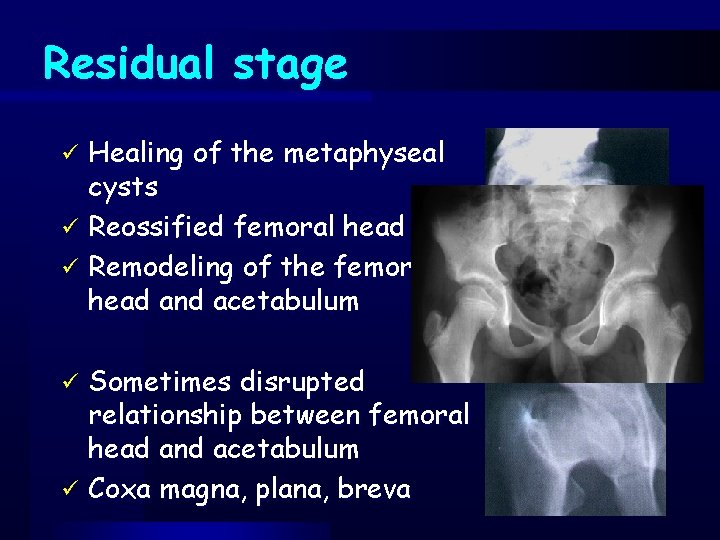
Residual stage Healing of the metaphyseal cysts ü Reossified femoral head ü Remodeling of the femoral head and acetabulum ü Sometimes disrupted relationship between femoral head and acetabulum ü Coxa magna, plana, breva ü
Differential diagnosis ü Synovitis üToxic synovitis üSeptic arthritis üAcute rheumatic fever üJuvenile arthritis üTbc arthritis üOsteoid osteoma
Differential diagnosis ü Avascular necrosis üSickle cell anemia üGaucher disease üTraumatic avascular necrosis
Differential diagnosis ü Fragmentation üTbc arthritis üMultiple epiphyseal dysplasia üHypothyroid
Prognostic factors ü Age ü Gender ü Time to diagnose and treatment ü Amount of femoral head involvement ü “Head at risk” signs
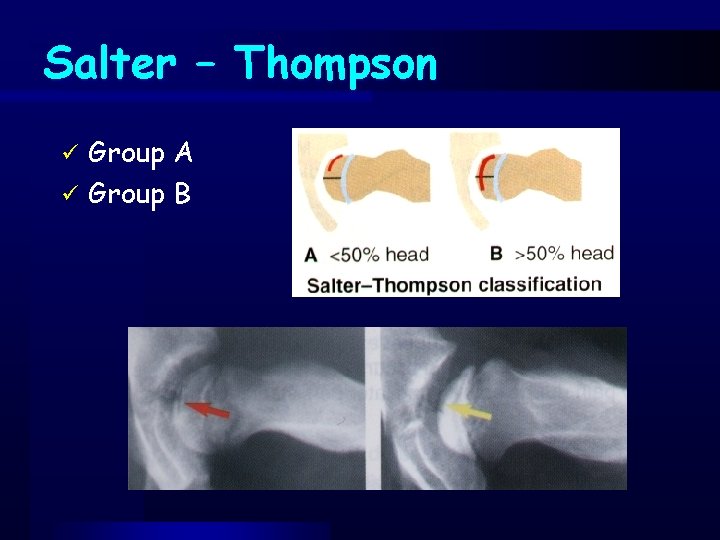
Classifications ü After occurance of subchondral cresent sign üSalter - Thompson ü At the fragmentation stage üCatterall üHerring-Lateral pillar ü After skeletal maturity üStulberg
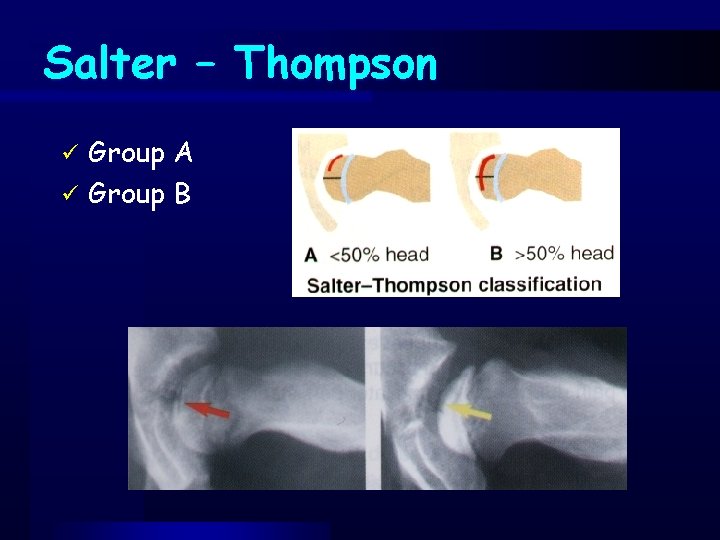
Salter – Thompson Group A ü Group B ü
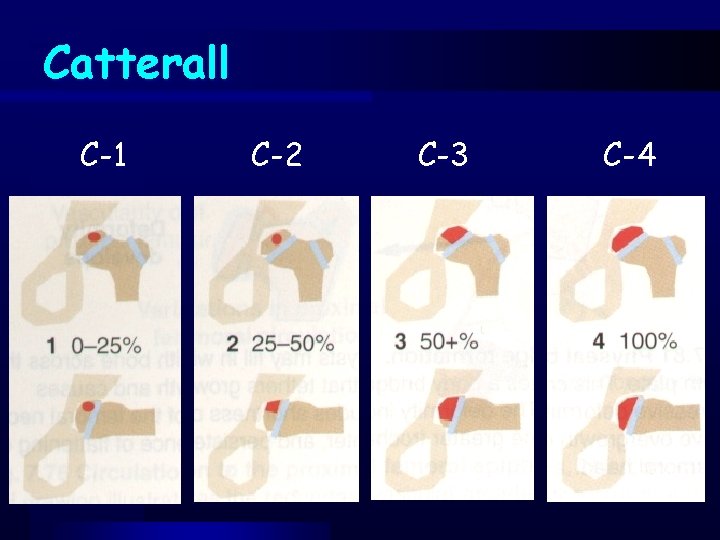
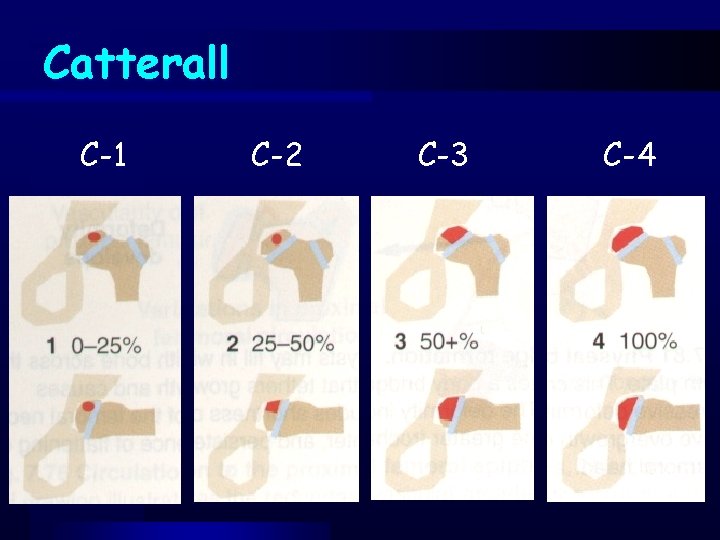
Catterall C-1 C-2 C-3 C-4
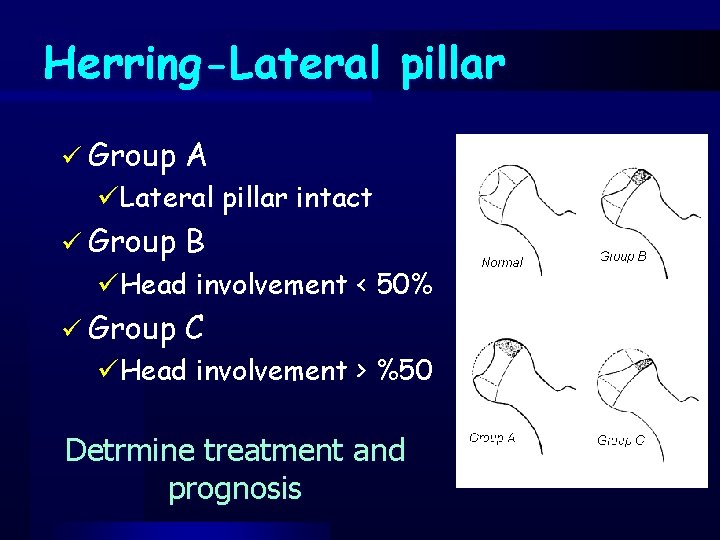
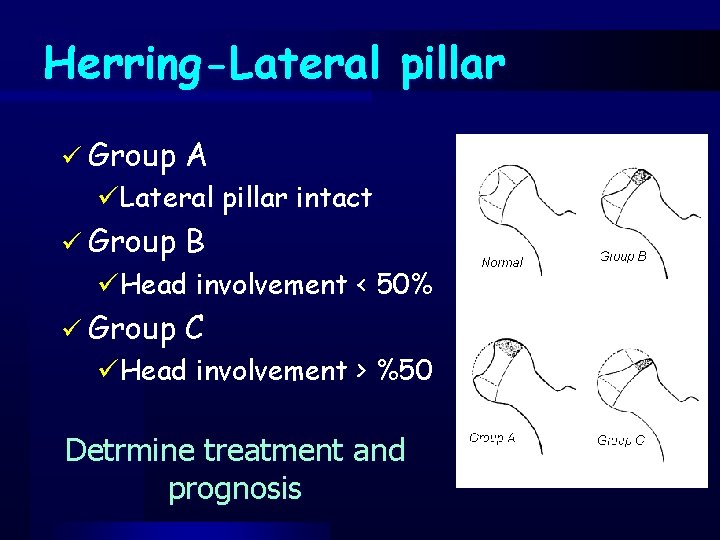
Herring-Lateral pillar ü Group A ü Group B ü Group C üLateral pillar intact üHead involvement < 50% üHead involvement > %50 Detrmine treatment and prognosis
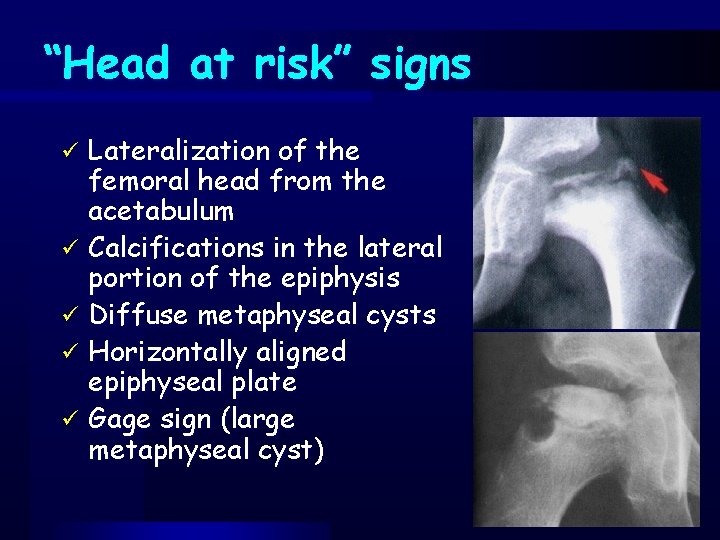
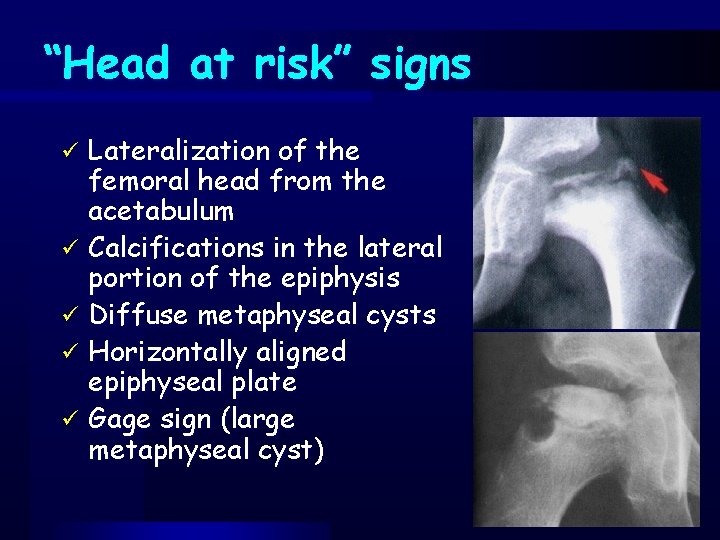
“Head at risk” signs Lateralization of the femoral head from the acetabulum ü Calcifications in the lateral portion of the epiphysis ü Diffuse metaphyseal cysts ü Horizontally aligned epiphyseal plate ü Gage sign (large metaphyseal cyst) ü
Goal of treatment Preservation of the roundness of the femoral head and prevention of deformity while the condition runs its course
Treatment algorithm ü< 7 years of age, C-1 and C-2 or Herring lateral pillar group A – No treatment ü> 7 years of age, C-3 and C-4, Herring lateral pillar group B and C – Treatment
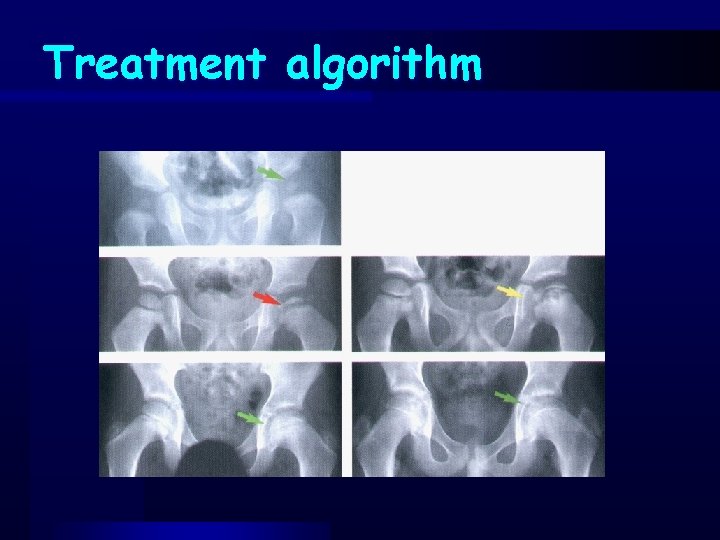
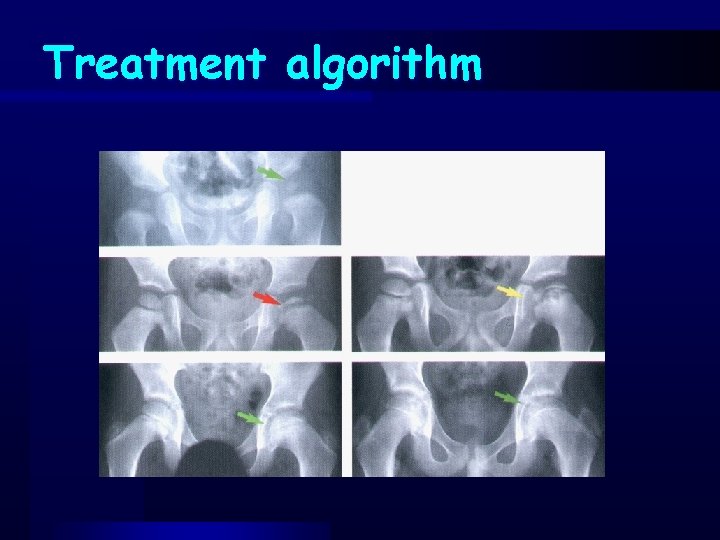
Treatment algorithm
Phases of treatment ü Initial period ü Containment provider modalities ü Reconstructive procedures (salvage methods)
Phases of treatment ü Initial period üObservation üBed rest üManual or skin traction üNSAI
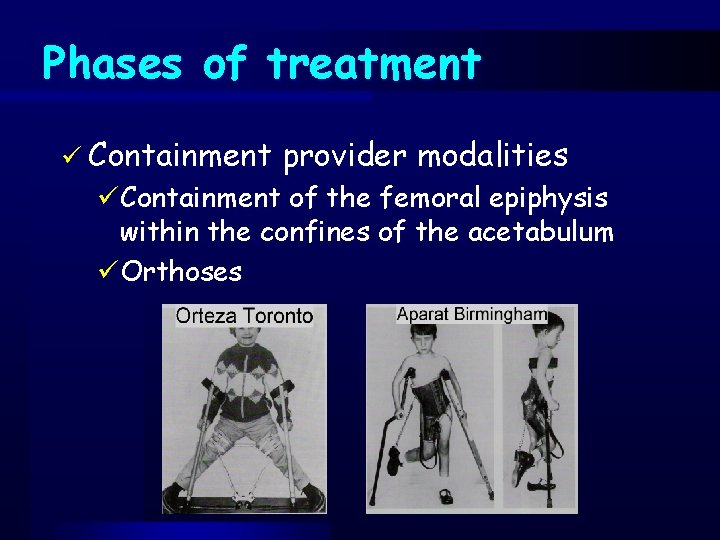
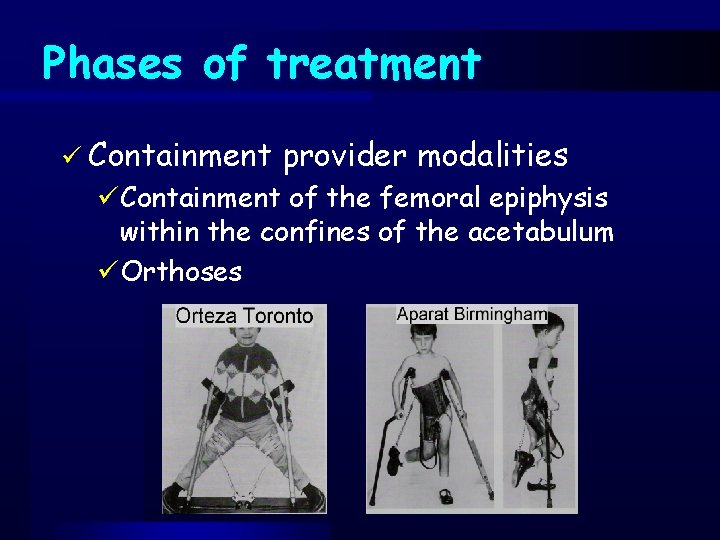
Phases of treatment ü Containment provider modalities üContainment of the femoral epiphysis within the confines of the acetabulum üOrthoses
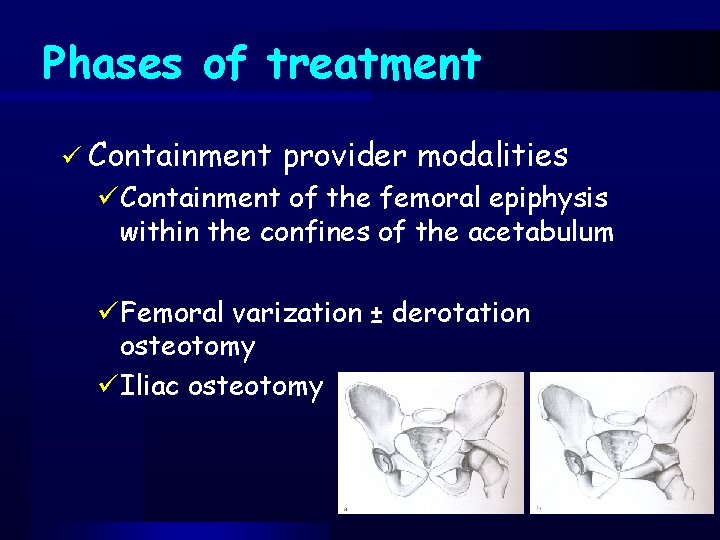
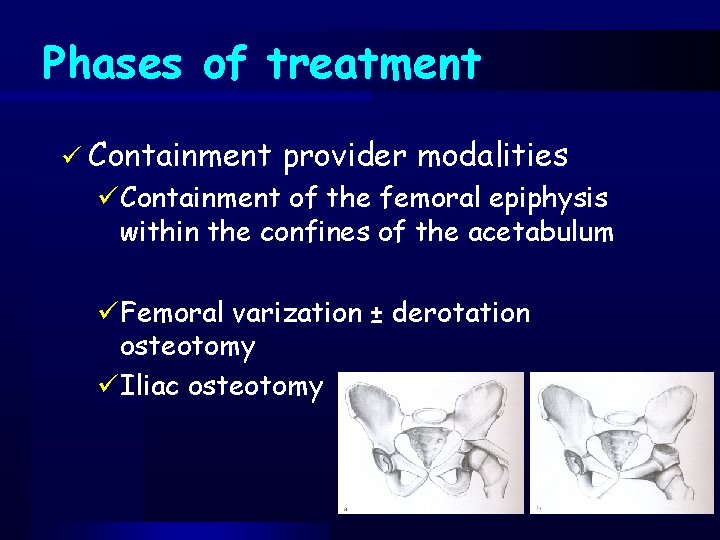
Phases of treatment ü Containment provider modalities üContainment of the femoral epiphysis within the confines of the acetabulum üFemoral varization ± derotation osteotomy üIliac osteotomy
Phases of treatment ü Reconstructive methods) procedures (salvage üShelf acetabuloplasty üDouble or triple iliaca osteotomies ü± femoral osteotomies
Thanks !
 Common lisp assoc
Common lisp assoc Angus gestation calculator
Angus gestation calculator Iyi dokunuş nedir
Iyi dokunuş nedir Gven
Gven Superior vertebral notch
Superior vertebral notch Yeditepe tıp
Yeditepe tıp Coadsys exam yeditepe
Coadsys exam yeditepe Coadsys exam
Coadsys exam Melih kaan can
Melih kaan can Elastik manşonlu kavrama
Elastik manşonlu kavrama Site:slidetodoc.com
Site:slidetodoc.com University hospital of pisa
University hospital of pisa Brendan rauw
Brendan rauw Benha university hospital
Benha university hospital Kyorin university hospital
Kyorin university hospital University hospital tuebingen
University hospital tuebingen University hospital of pisa
University hospital of pisa Patras university hospital
Patras university hospital Pisa university hospital
Pisa university hospital Hanifin rajka atopic dermatitis
Hanifin rajka atopic dermatitis Portsmouth hospital trust values
Portsmouth hospital trust values Kyung hee university hospital at gangdong
Kyung hee university hospital at gangdong Kaohsiung medical university hospital
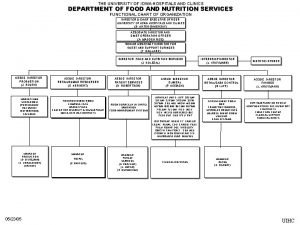
Kaohsiung medical university hospital University of iowa hospital and clinics departments
University of iowa hospital and clinics departments King saud university hospital nurse salary
King saud university hospital nurse salary 詹景裕
詹景裕 Prof. dr. marcus eckert
Prof. dr. marcus eckert Agamenon quimica
Agamenon quimica Prof david toback
Prof david toback What is this in english
What is this in english Dr suganda
Dr suganda Th
Th