COLORECTAL CANCER Ozlem UysalSonmez MD Yeditepe University Hospital






- Slides: 40
COLORECTAL CANCER Ozlem Uysal-Sonmez, MD Yeditepe University Hospital Department of Medical Oncology
Anatomy of the Colon and Rectum • The colon + rectum = the large intestine • Colon makes upto first 150 -180 cm of large intestine • Rectum makes up the last 12 -15 cm ending at the anus
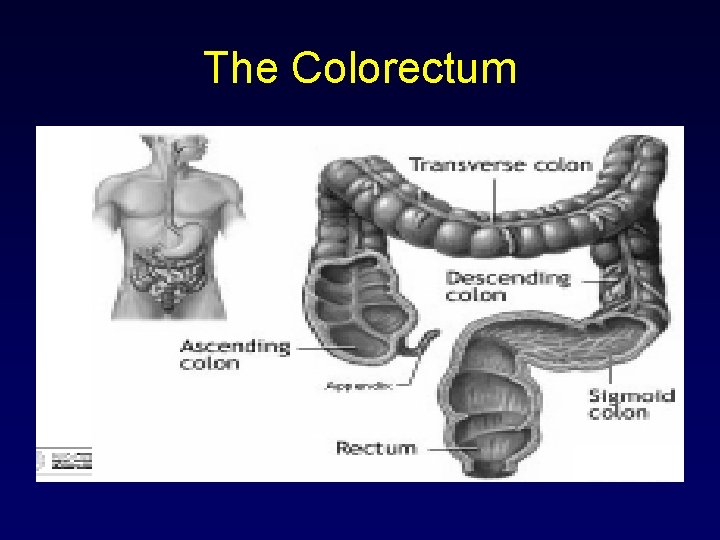
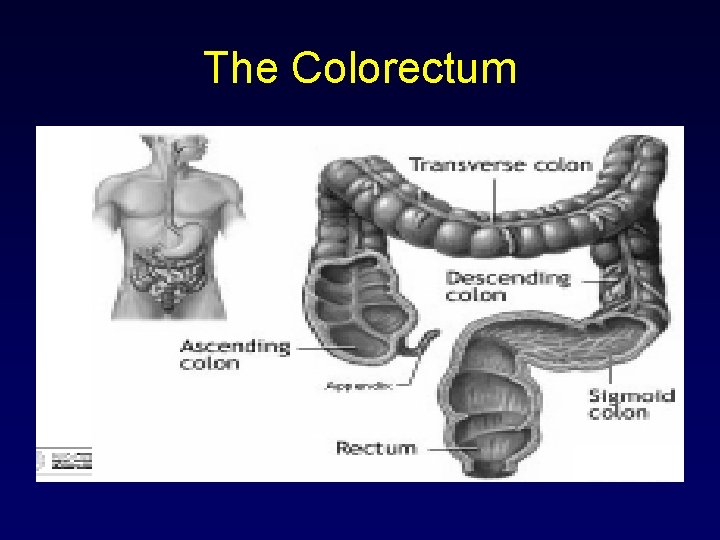
The Colorectum


Epidemiology • Third most common cancer • Second most common cause of cancer death • Male = Female • Lifetime probability of 6% (1 in 17) • Very curable if detected in early stages
Epidemiology • Males=Females • Risk increases with age – Average at diagnosis is 67 -70 yrs • Highest in industrialized nations: – Canada, US, N/W Europe • Most cancers start as polyps precancerous growths that develop on the inner wall of the colon and rectum
Most of the colon and Rectum cancers are diagnosed at: 1) Routine physical to evaluate anemia 2) Screening colonoscopy recommended for age 50 and over
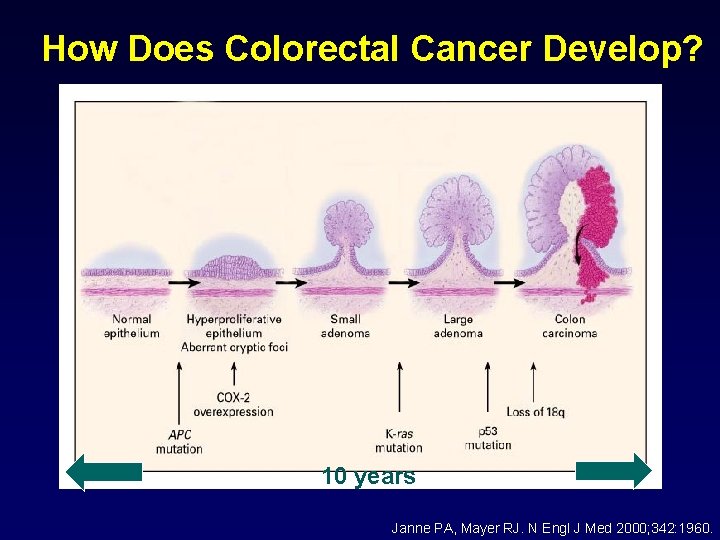
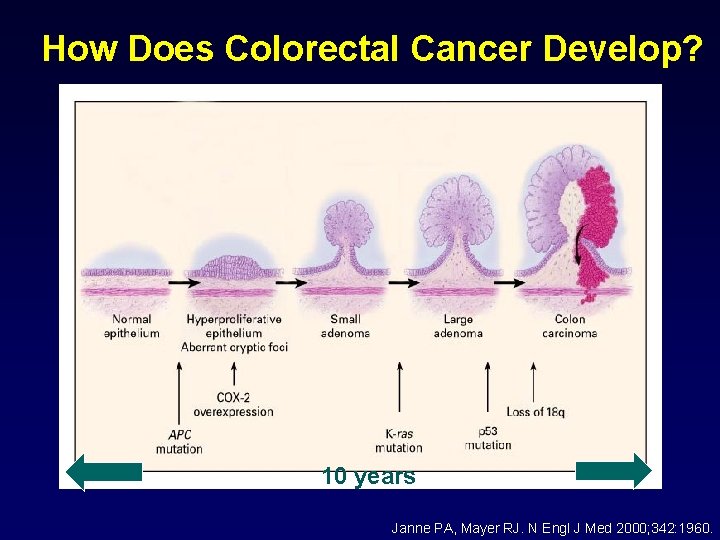
How Does Colorectal Cancer Develop? 10 years Janne PA, Mayer RJ. N Engl J Med 2000; 342: 1960.
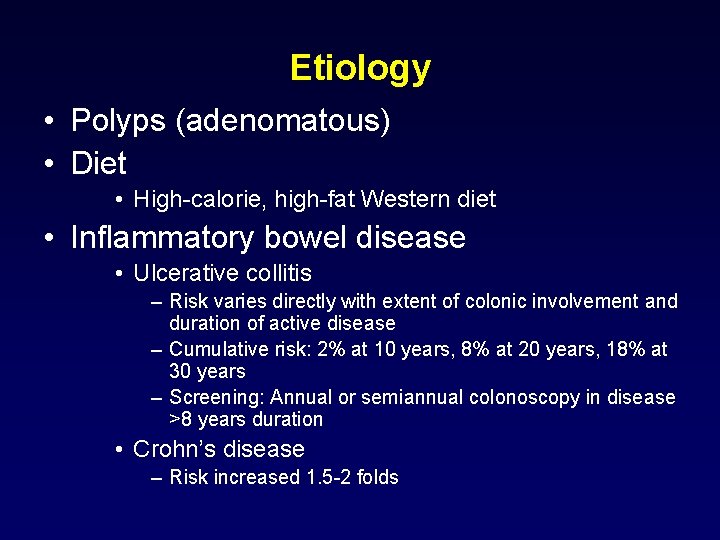
Etiology • Polyps (adenomatous) • Diet • High-calorie, high-fat Western diet • Inflammatory bowel disease • Ulcerative collitis – Risk varies directly with extent of colonic involvement and duration of active disease – Cumulative risk: 2% at 10 years, 8% at 20 years, 18% at 30 years – Screening: Annual or semiannual colonoscopy in disease >8 years duration • Crohn’s disease – Risk increased 1. 5 -2 folds
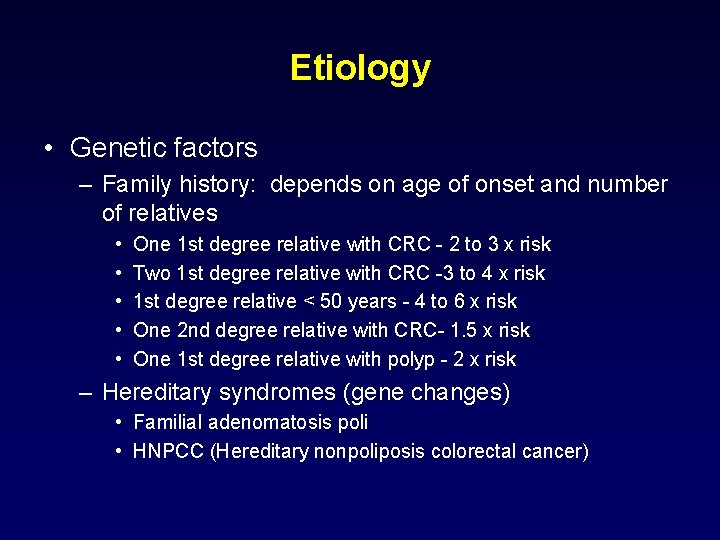
Etiology • Genetic factors – Family history: depends on age of onset and number of relatives • • • One 1 st degree relative with CRC - 2 to 3 x risk Two 1 st degree relative with CRC -3 to 4 x risk 1 st degree relative < 50 years - 4 to 6 x risk One 2 nd degree relative with CRC- 1. 5 x risk One 1 st degree relative with polyp - 2 x risk – Hereditary syndromes (gene changes) • Familial adenomatosis poli • HNPCC (Hereditary nonpoliposis colorectal cancer)
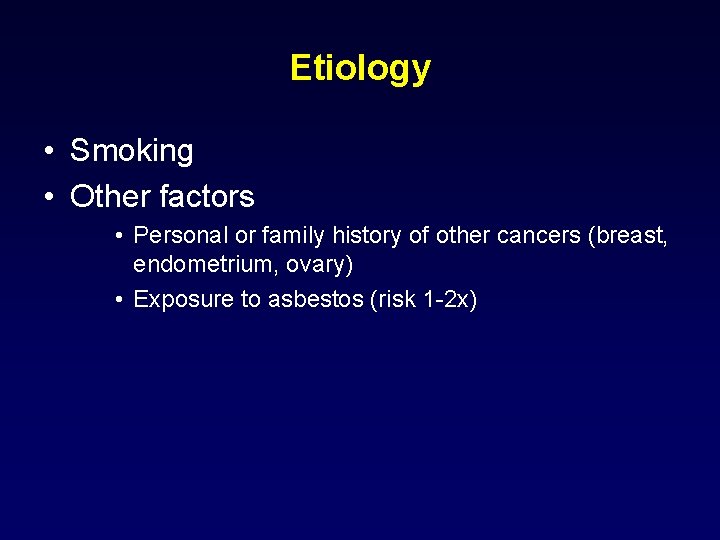
Etiology • Smoking • Other factors • Personal or family history of other cancers (breast, endometrium, ovary) • Exposure to asbestos (risk 1 -2 x)
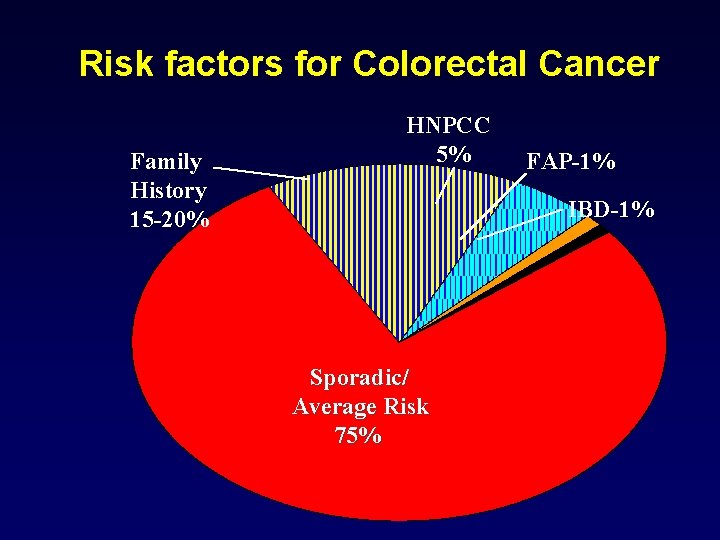
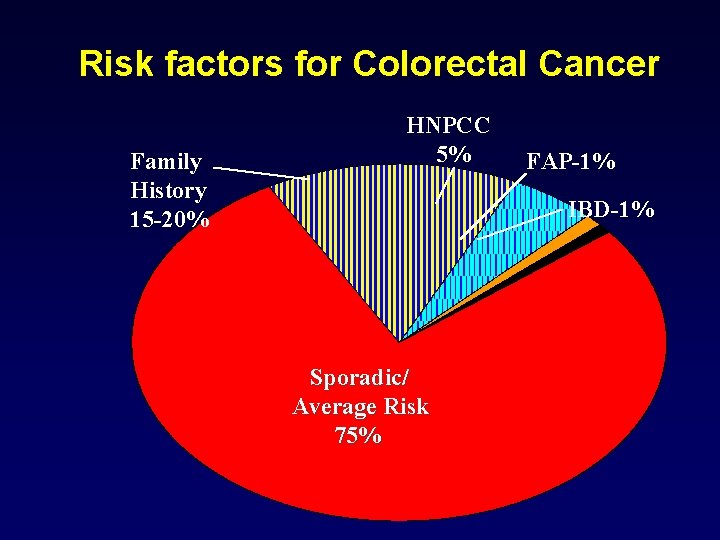
Risk factors for Colorectal Cancer Family History 15 -20% HNPCC 5% FAP-1% IBD-1% Sporadic/ Average Risk 75%
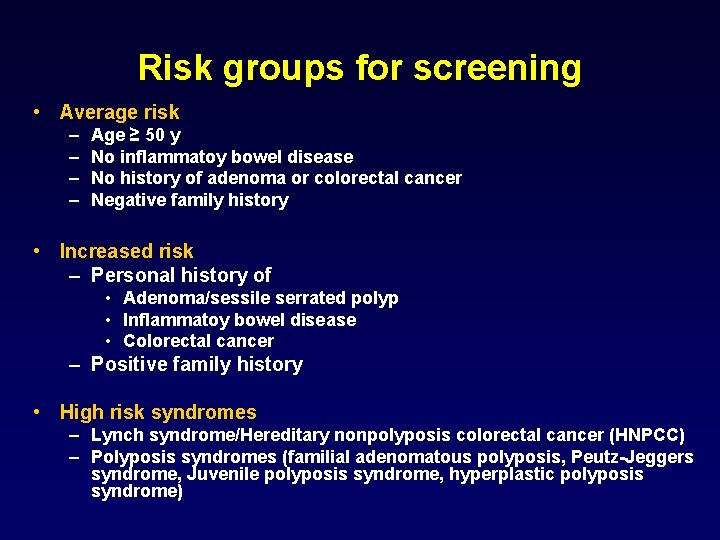
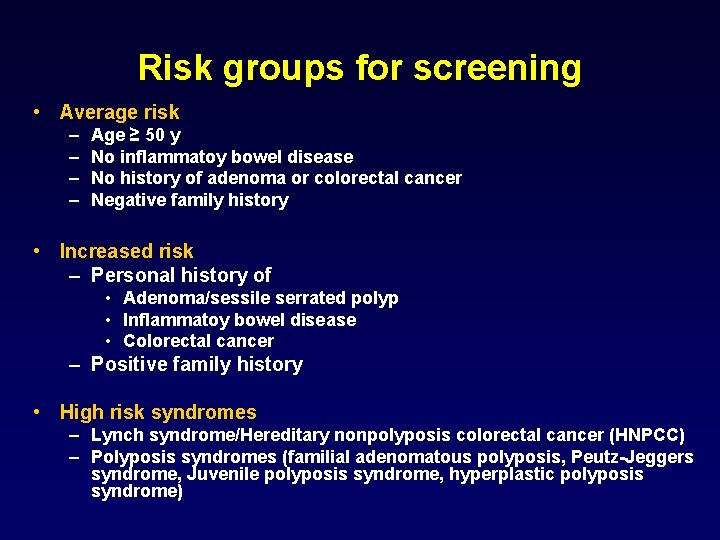
Risk groups for screening • Average risk – – Age ≥ 50 y No inflammatoy bowel disease No history of adenoma or colorectal cancer Negative family history • Increased risk – Personal history of • Adenoma/sessile serrated polyp • Inflammatoy bowel disease • Colorectal cancer – Positive family history • High risk syndromes – Lynch syndrome/Hereditary nonpolyposis colorectal cancer (HNPCC) – Polyposis syndromes (familial adenomatous polyposis, Peutz-Jeggers syndrome, Juvenile polyposis syndrome, hyperplastic polyposis syndrome)
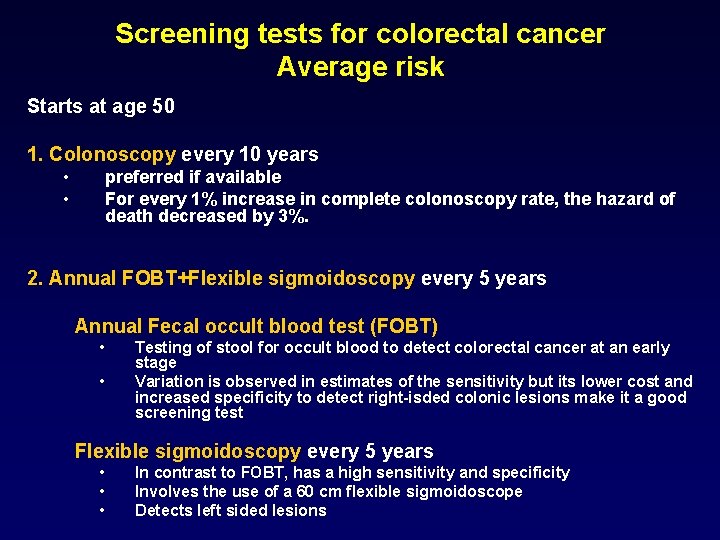
Screening tests for colorectal cancer Average risk Starts at age 50 1. Colonoscopy every 10 years • • preferred if available For every 1% increase in complete colonoscopy rate, the hazard of death decreased by 3%. 2. Annual FOBT+Flexible sigmoidoscopy every 5 years Annual Fecal occult blood test (FOBT) • • Testing of stool for occult blood to detect colorectal cancer at an early stage Variation is observed in estimates of the sensitivity but its lower cost and increased specificity to detect right-isded colonic lesions make it a good screening test Flexible sigmoidoscopy every 5 years • • • In contrast to FOBT, has a high sensitivity and specificity Involves the use of a 60 cm flexible sigmoidoscope Detects left sided lesions
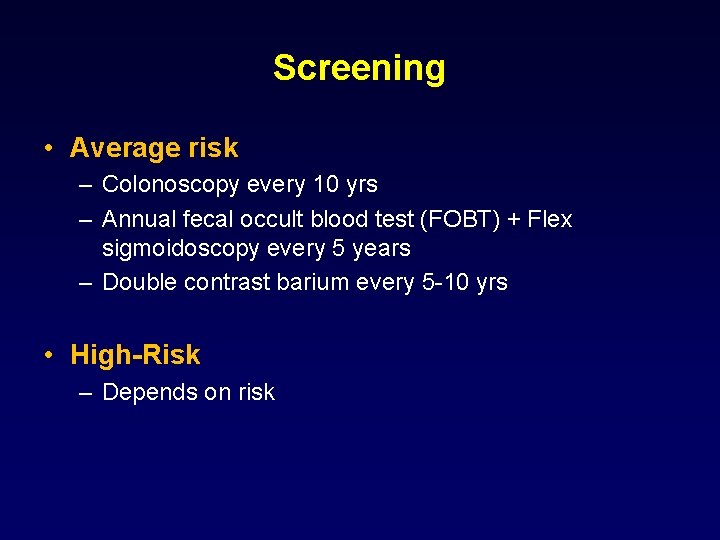
Screening • Average risk – Colonoscopy every 10 yrs – Annual fecal occult blood test (FOBT) + Flex sigmoidoscopy every 5 years – Double contrast barium every 5 -10 yrs • High-Risk – Depends on risk
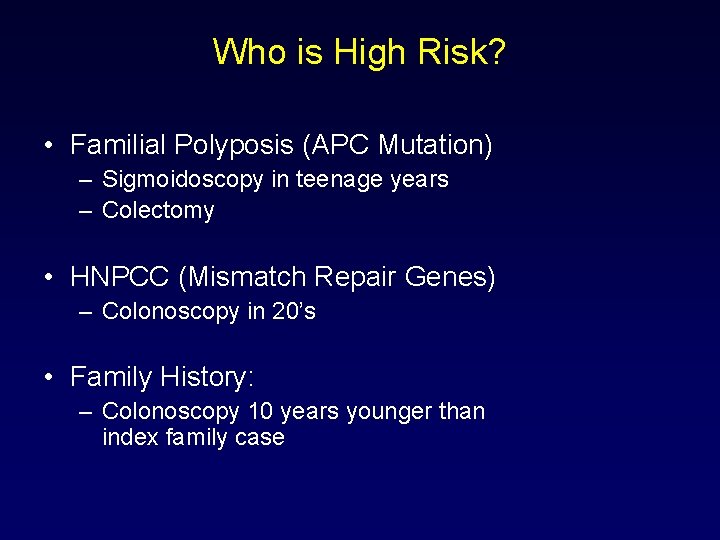
Who is High Risk? • Familial Polyposis (APC Mutation) – Sigmoidoscopy in teenage years – Colectomy • HNPCC (Mismatch Repair Genes) – Colonoscopy in 20’s • Family History: – Colonoscopy 10 years younger than index family case
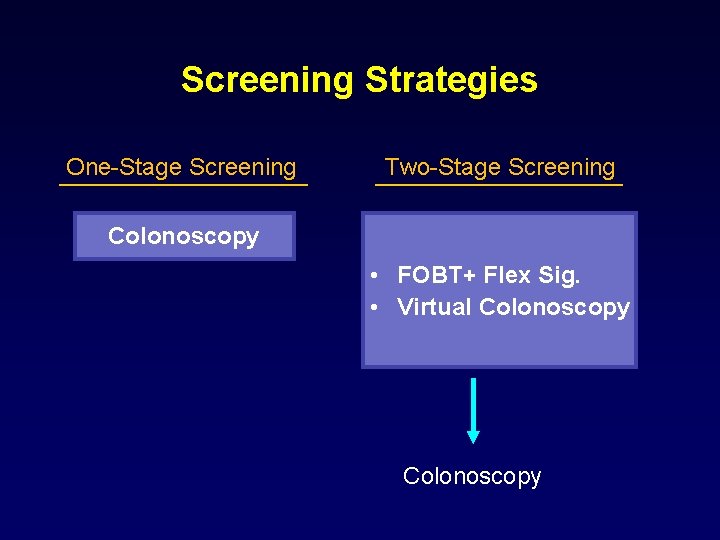
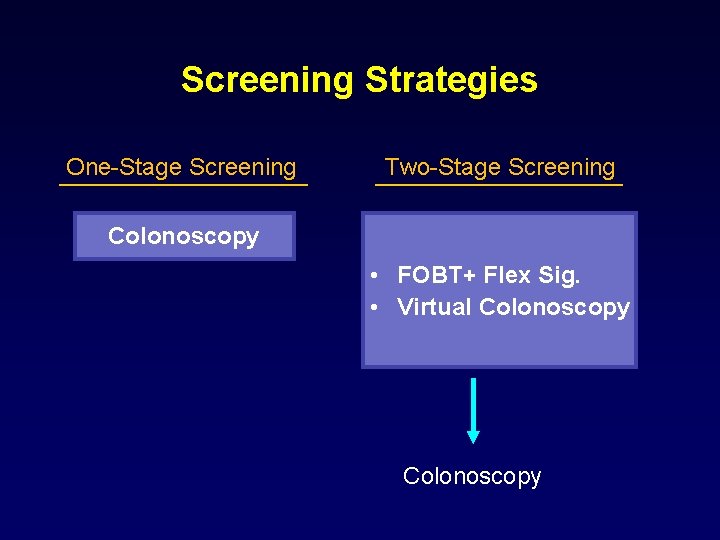
Screening Strategies One-Stage Screening Two-Stage Screening Colonoscopy • FOBT+ Flex Sig. • Virtual Colonoscopy
Prevention • Periodic sigmoidoscopy+FOB or colonoscopy • Diet • NSAID: Sulindac, aspirin
Pathology and natural history • Pathology – Adenocarcinoma is most common type – Cancers of anal verge: Most often squamous cell or basaloid carcinomas • Most arise from adenomatous polyps
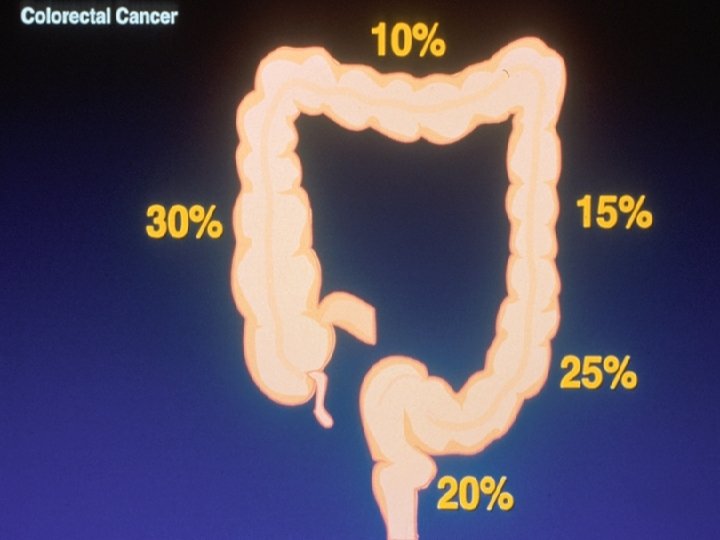
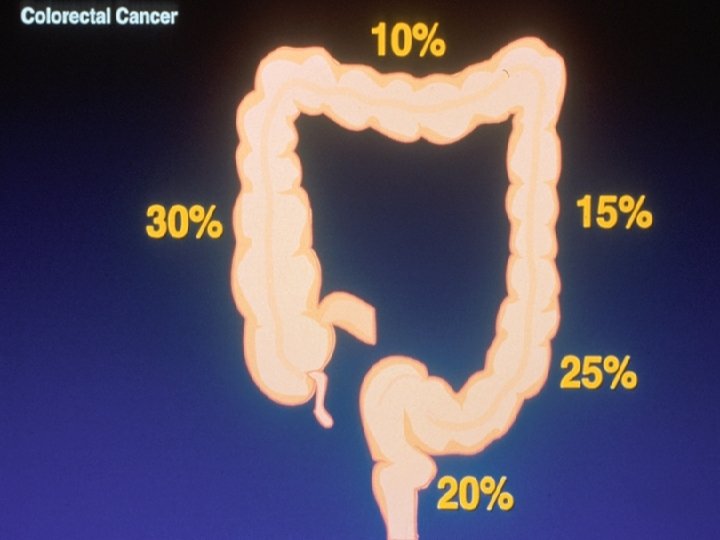
Site Distribution
Pathology and natural history • Proximal tumors – More genetically unstable – May arise through same mechanisms underlying HNPCC • Distal tumors – greater genetic stability – May develop through same mechanisms underlying polyposis-associated colorectal cancer
Natural history • Tumors spread through the walls of the intestine and into the lymphatic system • Metastases to lymph nodes in 40%-70% • Tumors most commonly spread to the liver because venous blood flow from the colorectal tumor is through the portal vein • Most common: Liver, peritoneal cavity, lung • Rectum cancers are 3 times more likely to recur locally, because most of rectum lacks serosal layer • Because of venous and lymphatic drainage of rectum to inferior vena cava, rectum cancers often recur first in lung
Clinical Manifestations • Many colorectal cancers cause no symptoms in the early stages. • Goal of screening is to detect cancers in the early stages, before symptoms develop. • Symptoms in the later stages include: – – – – Change in bowel habits Blood in stool Fatigue Loss of appetite Abdominal pain Nausea Weight loss Anemia.
Clinical Manifestations • Cancer on the right side gives rise to manifestations that are different from those on the left side of the colon • Left-sided lesions • Rectal bleeding • Alternating constipation and diarrhea • Narrow, ribbonlike stools • Right-sided lesions • • Usually asymptomatic Vague abdominal discomfort Iron deficiency anemia Occult bleeding
Diagnosis & Staging • General evaluation – History, Physical examination with digital rectal examination – CBC, liver function tests – Chest x-ray • Carcinoembryonic antigen (CEA) screening • Colonoscopy or sigmoidoscopy or barium enema • Imaging tests – CT scan or MRI – Ultrasound, Endorectal ultrasonography


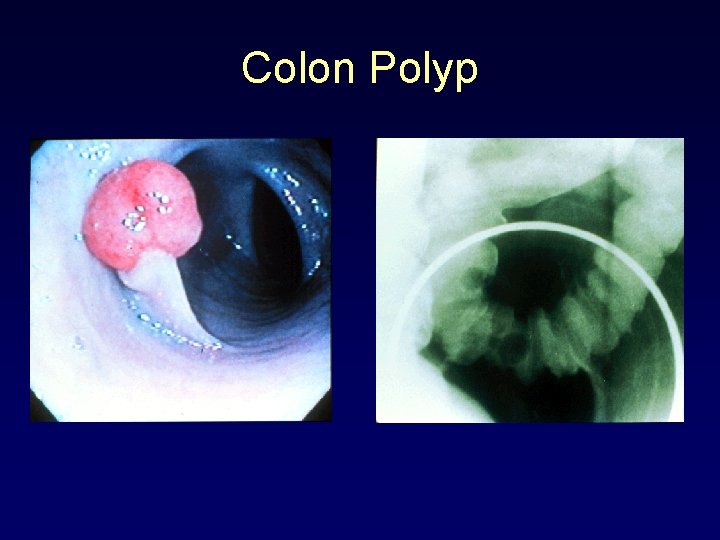
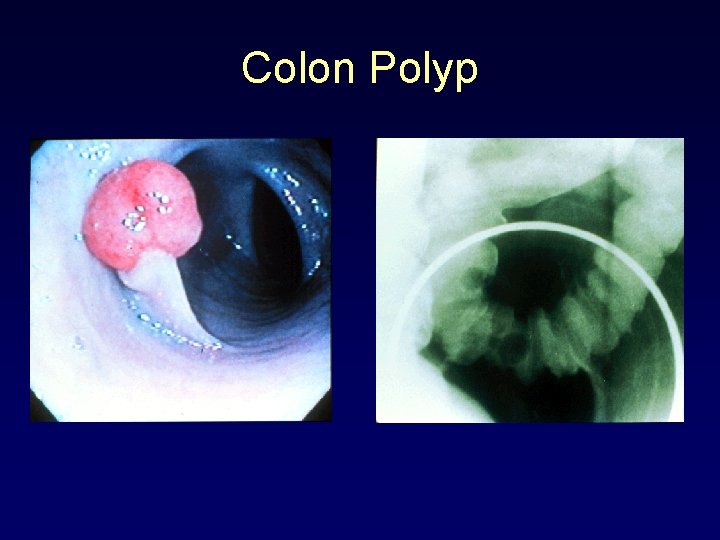
Colon Polyp
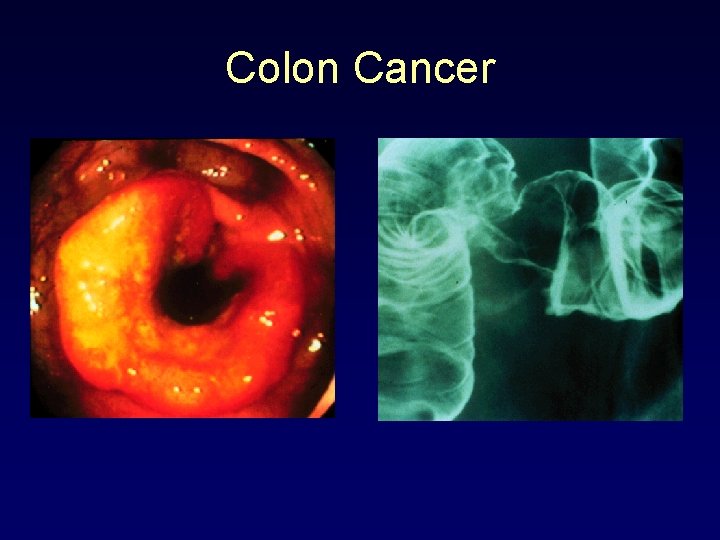
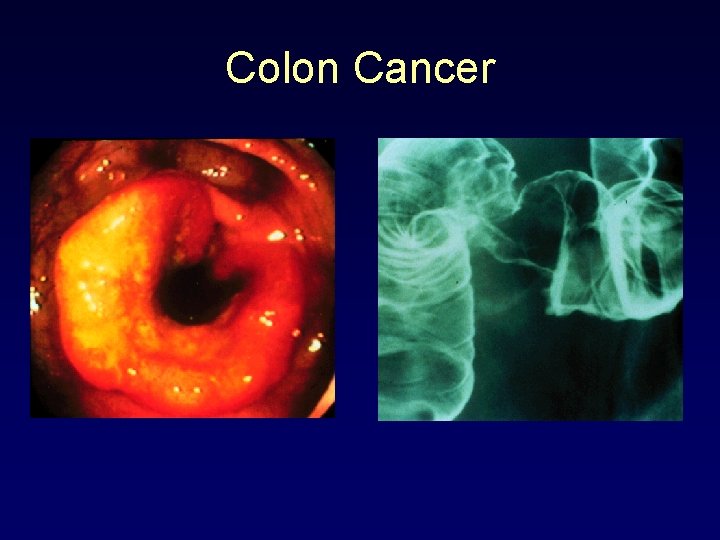
Colon Cancer
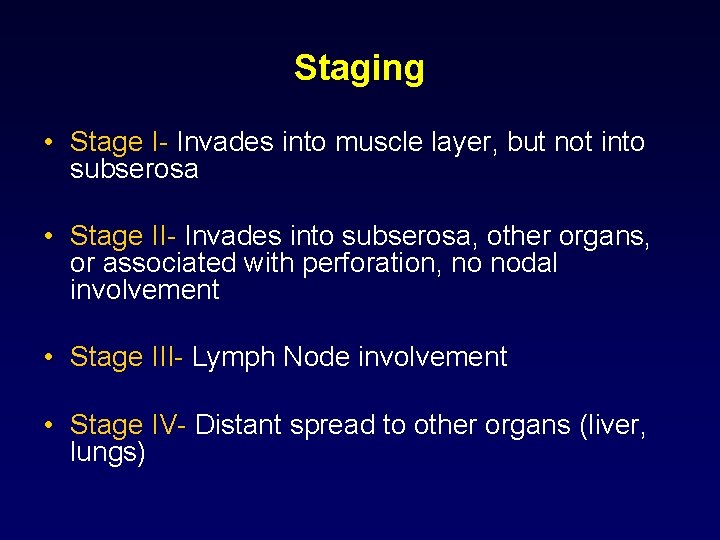
Staging • Stage I- Invades into muscle layer, but not into subserosa • Stage II- Invades into subserosa, other organs, or associated with perforation, no nodal involvement • Stage III- Lymph Node involvement • Stage IV- Distant spread to other organs (liver, lungs)
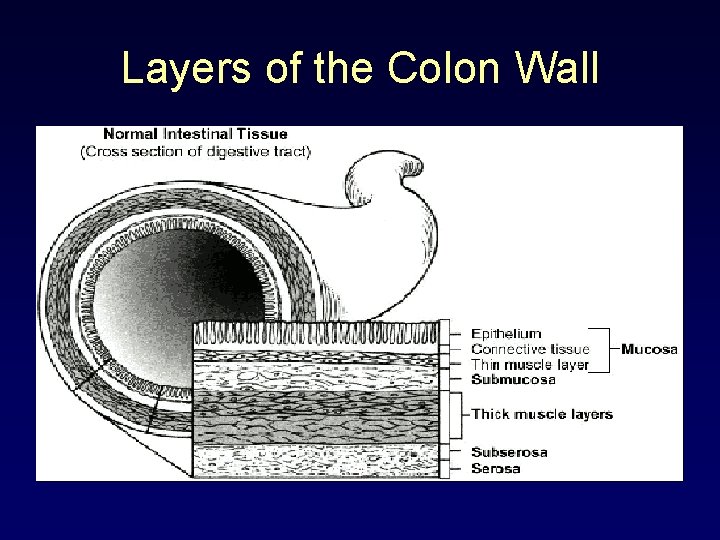
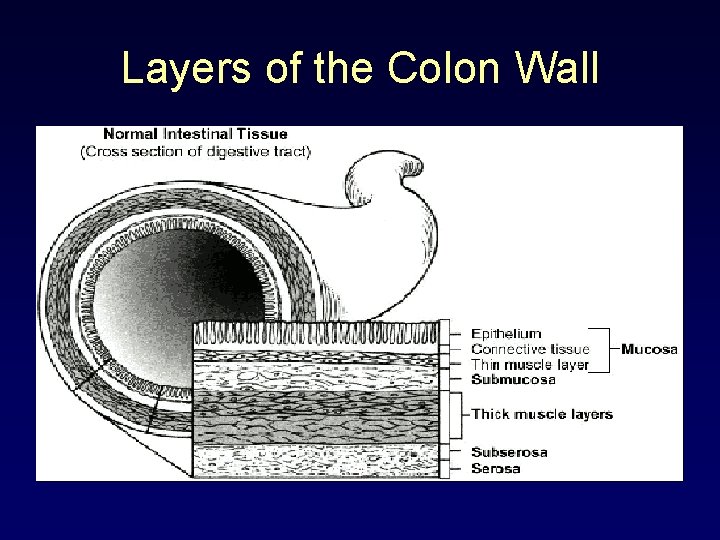
Layers of the Colon Wall

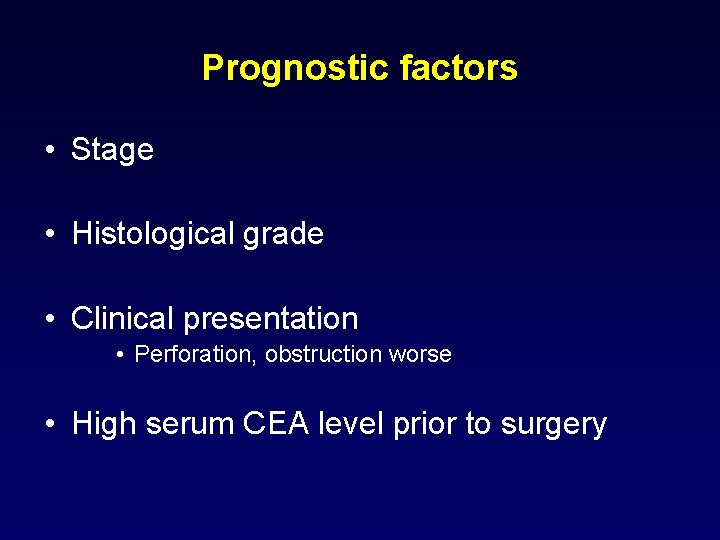
Prognostic factors • Stage • Histological grade • Clinical presentation • Perforation, obstruction worse • High serum CEA level prior to surgery
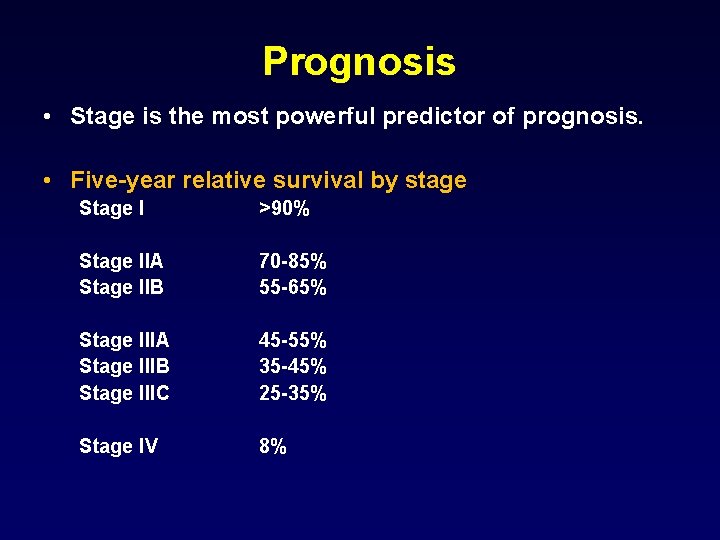
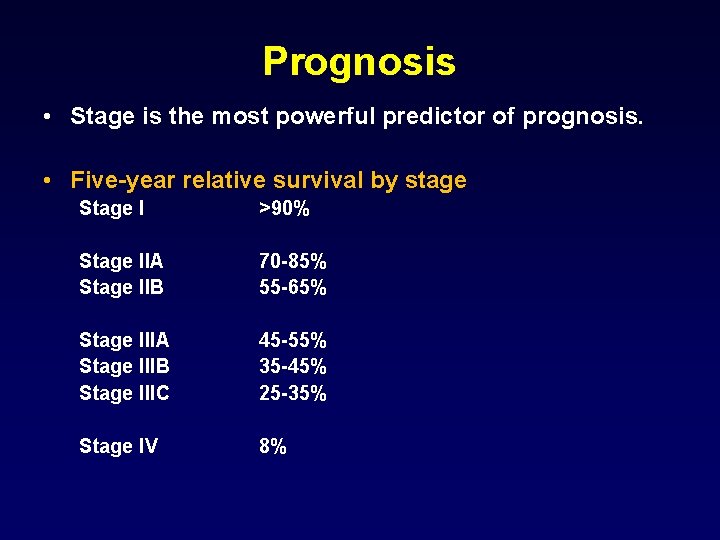
Prognosis • Stage is the most powerful predictor of prognosis. • Five-year relative survival by stage Stage I >90% Stage IIA Stage IIB 70 -85% 55 -65% Stage IIIA Stage IIIB Stage IIIC 45 -55% 35 -45% 25 -35% Stage IV 8%
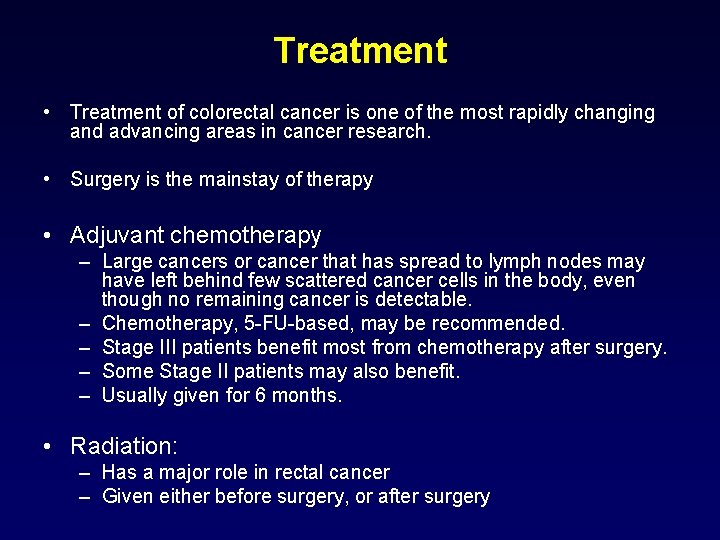
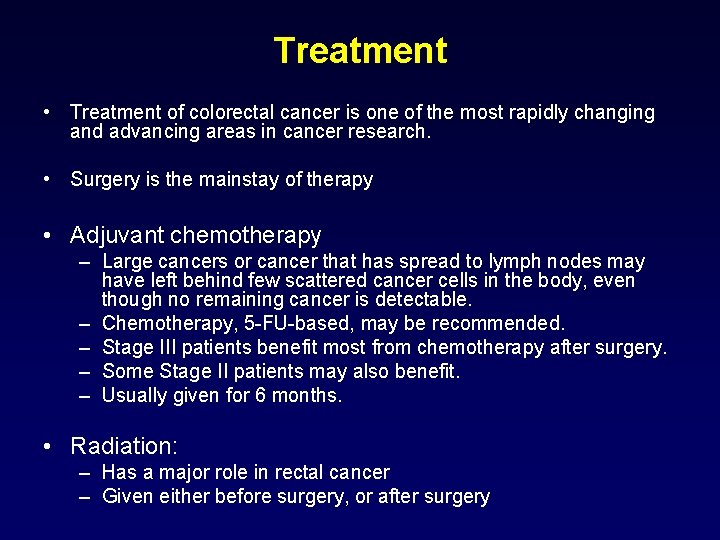
Treatment • Treatment of colorectal cancer is one of the most rapidly changing and advancing areas in cancer research. • Surgery is the mainstay of therapy • Adjuvant chemotherapy – Large cancers or cancer that has spread to lymph nodes may have left behind few scattered cancer cells in the body, even though no remaining cancer is detectable. – Chemotherapy, 5 -FU-based, may be recommended. – Stage III patients benefit most from chemotherapy after surgery. – Some Stage II patients may also benefit. – Usually given for 6 months. • Radiation: – Has a major role in rectal cancer – Given either before surgery, or after surgery
Treatment • Stage I-III: Goal is cure – Surgery – Adjuvant chemotehrapy: Stage III, some stage II • 5 -Fluorouracil based • Oxaliplatin – Adjuvant radiotherapy: Rectal cancers

Treatment • Stage IV: – Goals of therapy: palliation • To improve cancer-related symptoms • To control cancers by delaying further growth and spread • To shrink cancers • To improve survival (ie. to live longer with cancer) – Chemotherapy: not curative – Palliative surgery and radiotherapy
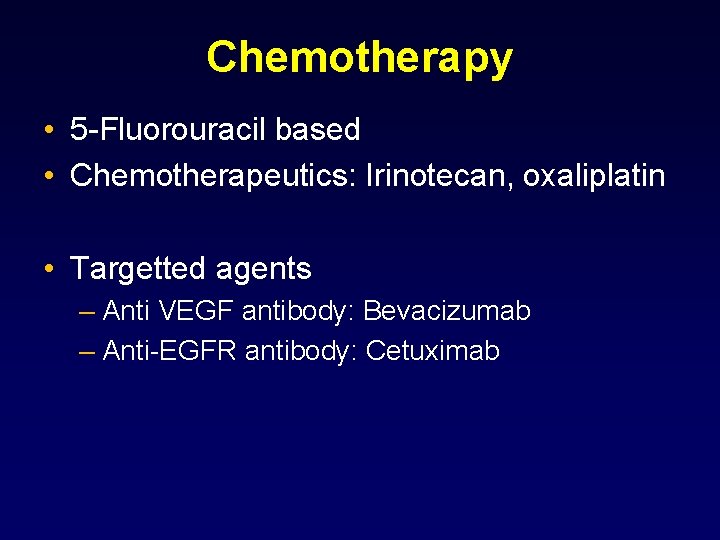
Chemotherapy • 5 -Fluorouracil based • Chemotherapeutics: Irinotecan, oxaliplatin • Targetted agents – Anti VEGF antibody: Bevacizumab – Anti-EGFR antibody: Cetuximab
Summary • Early detection is crucial • The development of new drugs and new drug combinations will continue to improve the outcome for cancer patients.
 Colorectal cancer drug trial
Colorectal cancer drug trial Sorunun cevabını bul
Sorunun cevabını bul Amsterdam criteria
Amsterdam criteria Ann lyons colorectal surgeon
Ann lyons colorectal surgeon Yeditepe tıp
Yeditepe tıp Patho
Patho Coadsys exam
Coadsys exam Coadsys exam
Coadsys exam Kuaini
Kuaini özlem pakkan
özlem pakkan Munisemetin
Munisemetin özlem alioğlu türker
özlem alioğlu türker Ozlem gurses
Ozlem gurses Insanın temel duyguları
Insanın temel duyguları Evraklar kurye ve dağıtıcılarla gönderilmelidir
Evraklar kurye ve dağıtıcılarla gönderilmelidir özlem topcan
özlem topcan Shaukat khanum memorial cancer hospital and research centre
Shaukat khanum memorial cancer hospital and research centre Howard university cancer center
Howard university cancer center Hospital pharmacy objectives and functions
Hospital pharmacy objectives and functions University hospital of pisa
University hospital of pisa Bezmialem vakıf university hospital
Bezmialem vakıf university hospital Benha university hospital
Benha university hospital Kyorin university hospital
Kyorin university hospital University hospital tuebingen
University hospital tuebingen Pisa university hospital
Pisa university hospital Patras university hospital
Patras university hospital Pisa university hospital
Pisa university hospital Hanifin rajka atopic dermatitis
Hanifin rajka atopic dermatitis Portsmouth hospitals nhs trust values
Portsmouth hospitals nhs trust values Kyung hee university hospital at gangdong
Kyung hee university hospital at gangdong Kaohsiung medical university hospital
Kaohsiung medical university hospital University of iowa hospital and clinics departments
University of iowa hospital and clinics departments King saud university hospital nurse salary
King saud university hospital nurse salary 沈榮麟
沈榮麟 Symptoms of metal fume fever
Symptoms of metal fume fever Tnm stage lung cancer
Tnm stage lung cancer Guttering definition ww1
Guttering definition ww1 The genetic basis of cancer
The genetic basis of cancer Cancer scn
Cancer scn Vida media benzodiacepinas
Vida media benzodiacepinas Cerebral salt wasting vs diabetes insipidus
Cerebral salt wasting vs diabetes insipidus