Colorectal MCQs TNM Staging of colorectal cancer yp

- Slides: 46
Colorectal MCQs
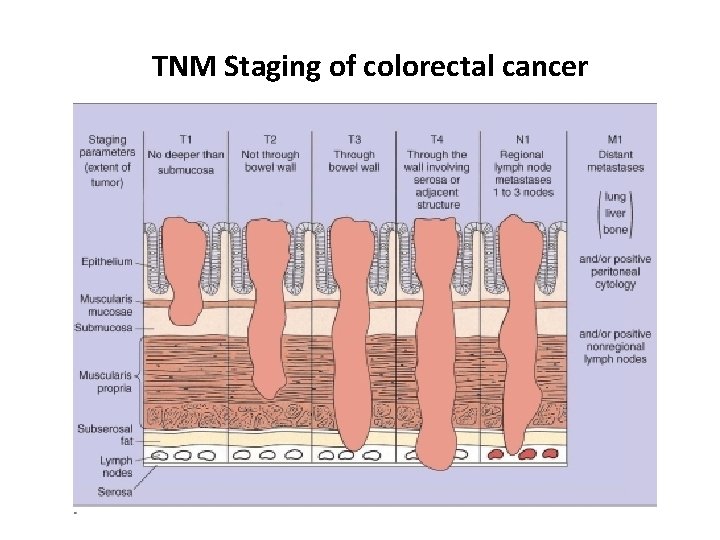
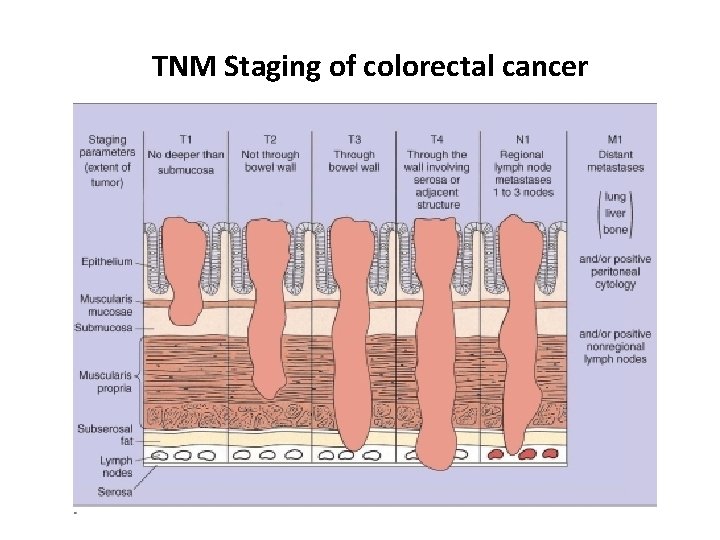
TNM Staging of colorectal cancer
yp. T 3 N 1 M 0 yp. T 4 N 2 M 0 R 0 p. T 3 N 3 M 1 yp. T 2 N 1 M 0 R 0 V 0
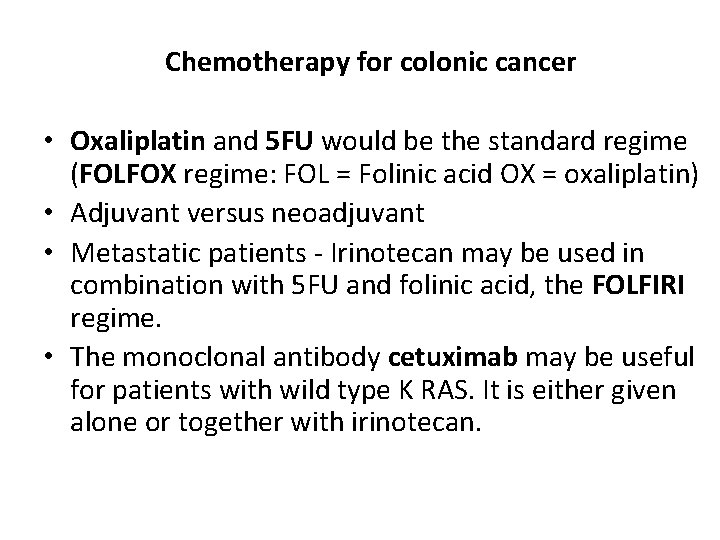
Chemotherapy for colonic cancer • Oxaliplatin and 5 FU would be the standard regime (FOLFOX regime: FOL = Folinic acid OX = oxaliplatin) • Adjuvant versus neoadjuvant • Metastatic patients - Irinotecan may be used in combination with 5 FU and folinic acid, the FOLFIRI regime. • The monoclonal antibody cetuximab may be useful for patients with wild type K RAS. It is either given alone or together with irinotecan.
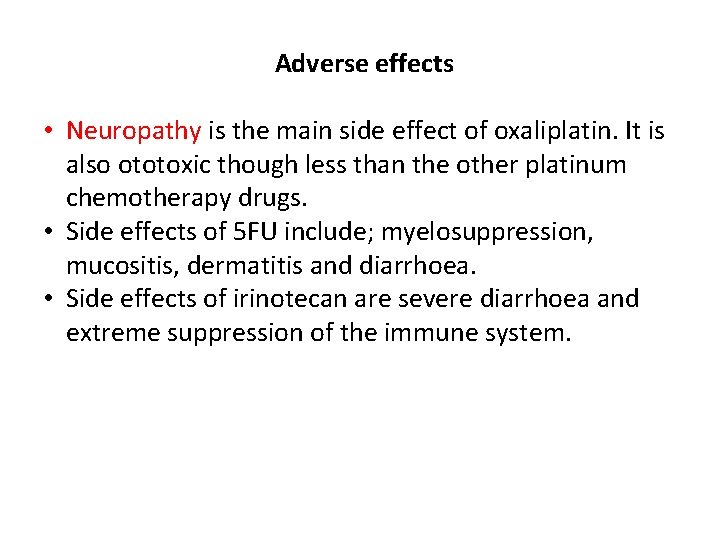
Adverse effects • Neuropathy is the main side effect of oxaliplatin. It is also ototoxic though less than the other platinum chemotherapy drugs. • Side effects of 5 FU include; myelosuppression, mucositis, dermatitis and diarrhoea. • Side effects of irinotecan are severe diarrhoea and extreme suppression of the immune system.
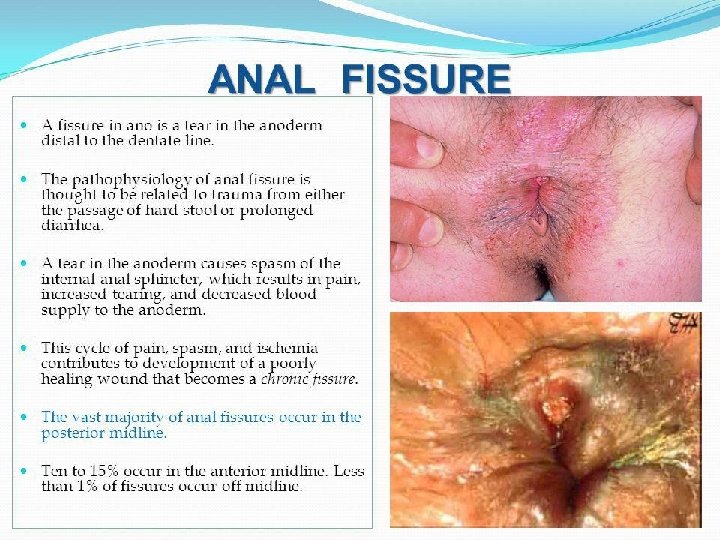
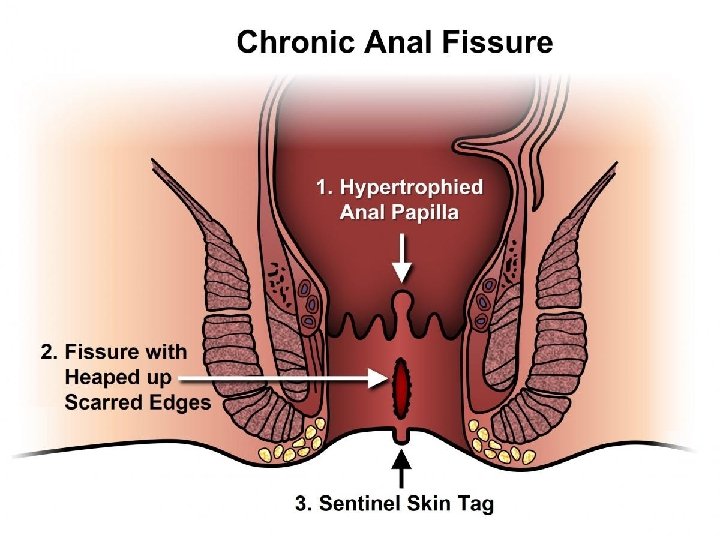
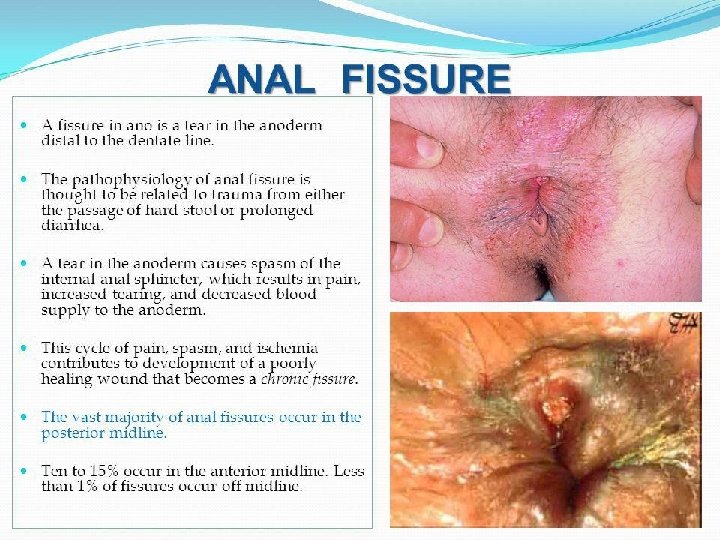
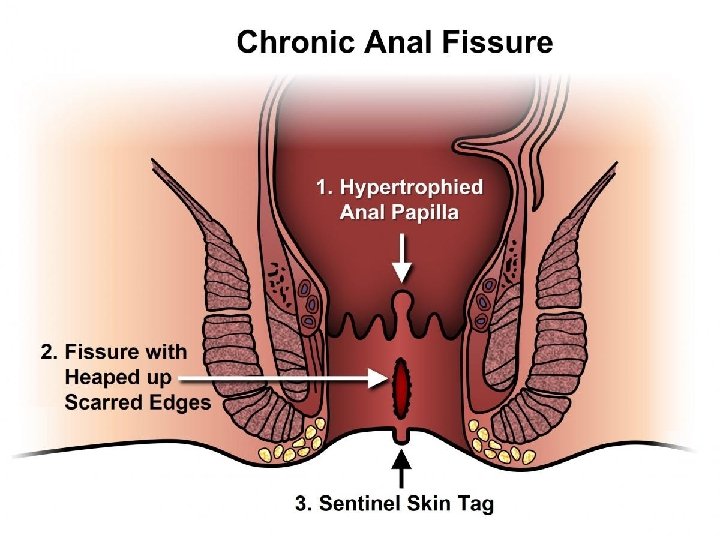
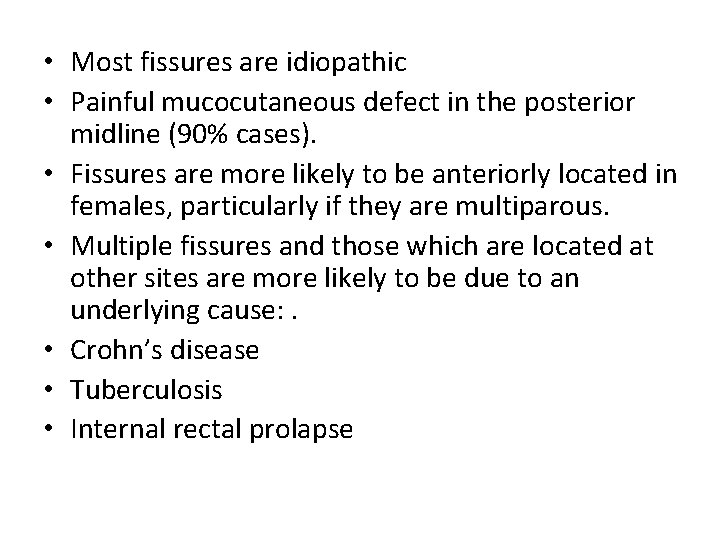
• Most fissures are idiopathic • Painful mucocutaneous defect in the posterior midline (90% cases). • Fissures are more likely to be anteriorly located in females, particularly if they are multiparous. • Multiple fissures and those which are located at other sites are more likely to be due to an underlying cause: . • Crohn’s disease • Tuberculosis • Internal rectal prolapse
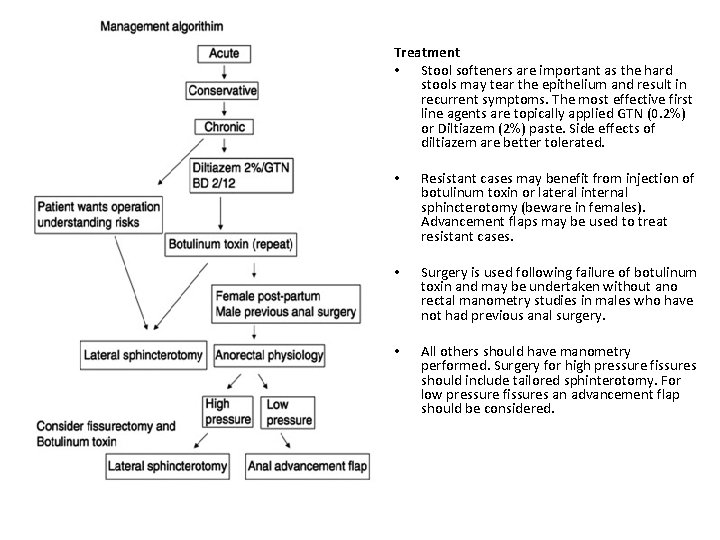
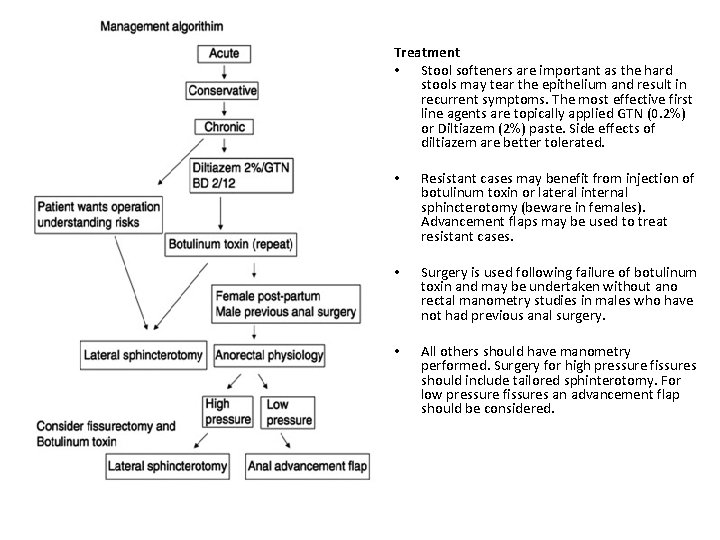
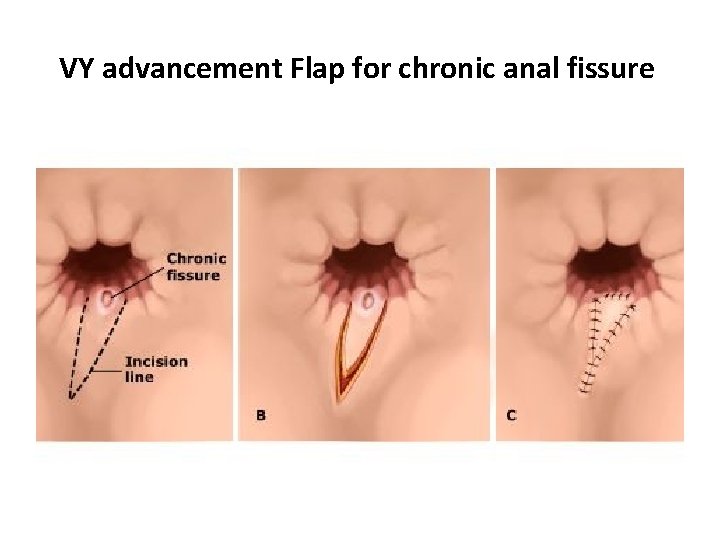
Treatment • Stool softeners are important as the hard stools may tear the epithelium and result in recurrent symptoms. The most effective first line agents are topically applied GTN (0. 2%) or Diltiazem (2%) paste. Side effects of diltiazem are better tolerated. • Resistant cases may benefit from injection of botulinum toxin or lateral internal sphincterotomy (beware in females). Advancement flaps may be used to treat resistant cases. • Surgery is used following failure of botulinum toxin and may be undertaken without ano rectal manometry studies in males who have not had previous anal surgery. • All others should have manometry performed. Surgery for high pressure fissures should include tailored sphinterotomy. For low pressure fissures an advancement flap should be considered.
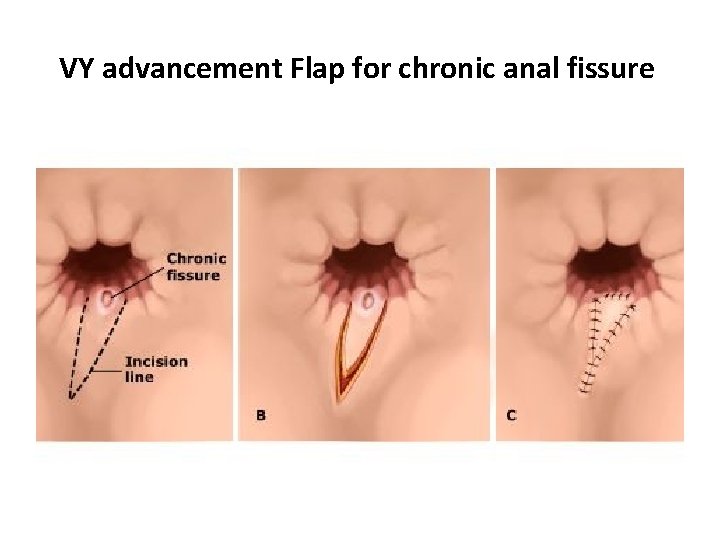
VY advancement Flap for chronic anal fissure
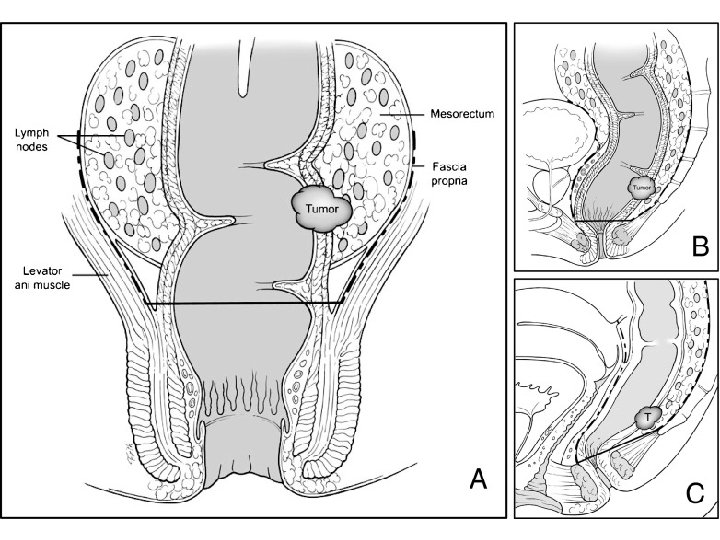
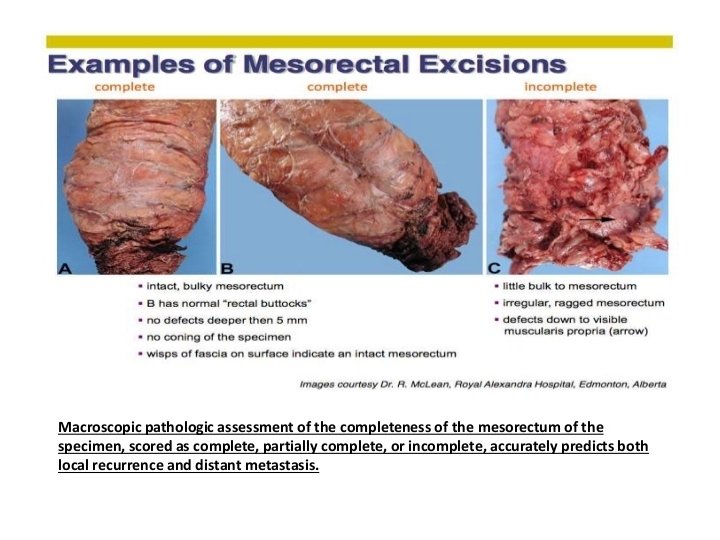
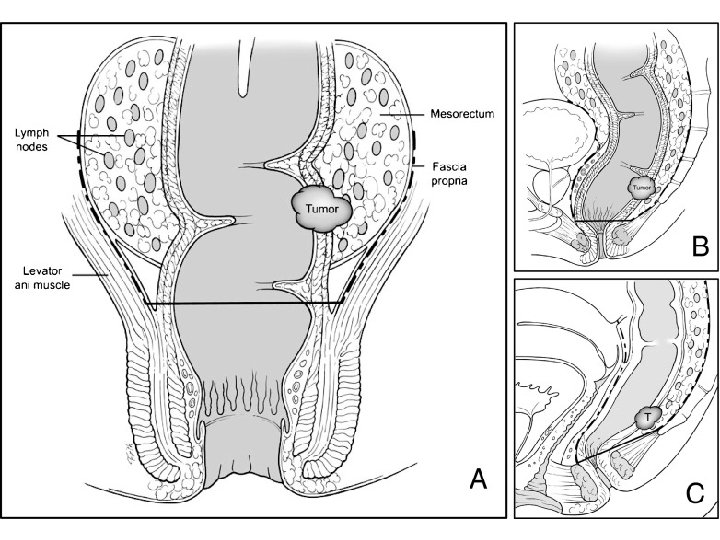
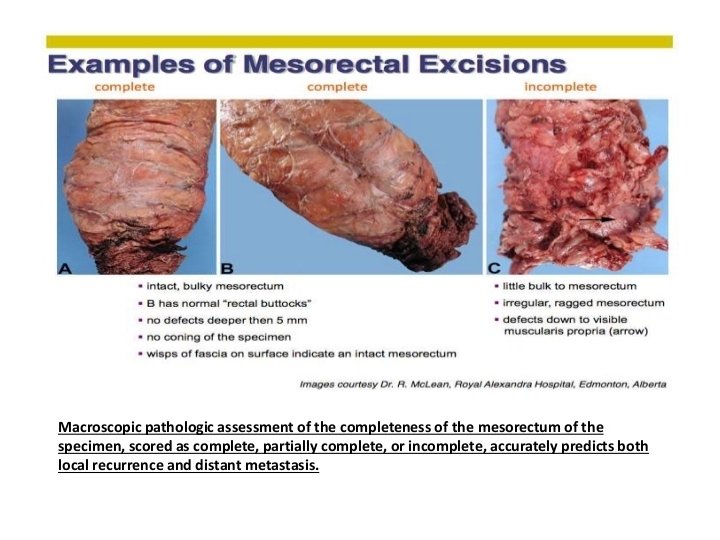
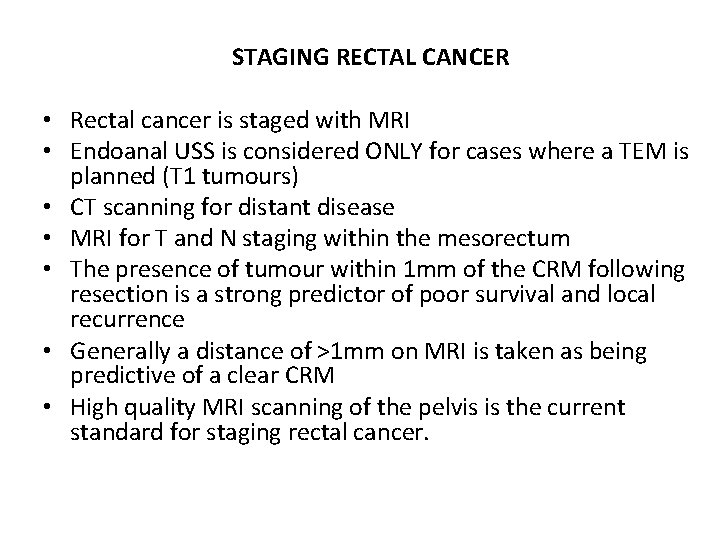
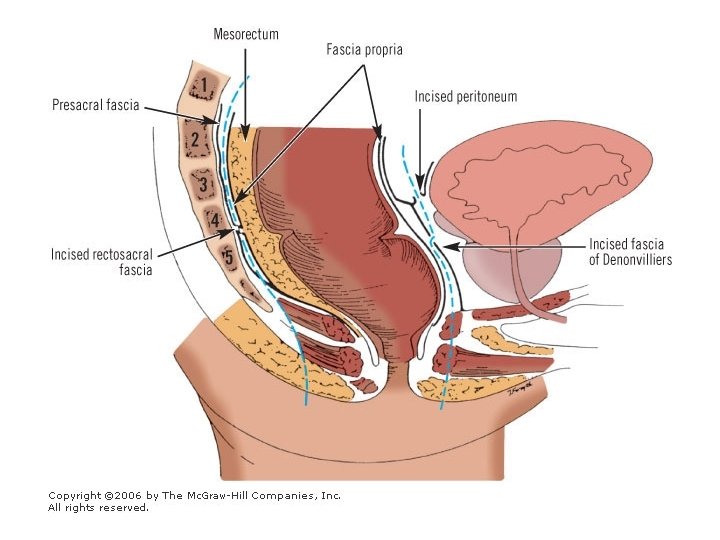
STAGING RECTAL CANCER • Rectal cancer is staged with MRI • Endoanal USS is considered ONLY for cases where a TEM is planned (T 1 tumours) • CT scanning for distant disease • MRI for T and N staging within the mesorectum • The presence of tumour within 1 mm of the CRM following resection is a strong predictor of poor survival and local recurrence • Generally a distance of >1 mm on MRI is taken as being predictive of a clear CRM • High quality MRI scanning of the pelvis is the current standard for staging rectal cancer.
RECTAL CANCER: TREATMENT • Short course radiotherapy is shown to increase sexual dysfunction in males following surgery • The Swedish cancer trial was the largest trial to be undertaken • Demonstrated a reduction in local recurrence with the addition of short course radiotherapy • Other, large, multicentre trials have demonstrated similar benefits from short course radiotherapy • The main group to benefit from pre operative radiotherapy are those patients with a threatened or involved CRM (usually by T 4 tumours). • Radiotherapy in this setting is given as long course and the addition of chemotherapy to the regime produces improved downstaging (at the cost of increased toxicity • Indeed, in some patients complete regression of the tumour is seen.
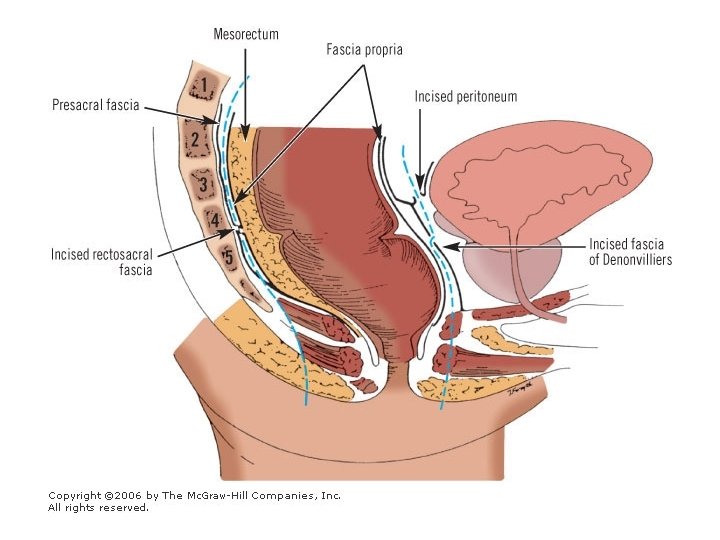
• Rectal cancer = tumours with distal margin 15 cm or less from the anal verge as measured with rigid sigmoidoscopy. • All patients with rectal cancer should have rectal MRI scanning to assess nodal disease, T and N stages. • The addition of chemoradiotherapy is of proven benefit in downstaging and reducing local recurrence rates in patients with a threatened CRM or suspicion of bulky nodal disease in the mesorectum. • The evidence for short course radiotherapy stems primarily from the Swedish Rectal cancer trial where local recurrence rates decreased from 27% to 11%. Such benefits were also seen in the Dutch TME trial 8. 2% to 2. 4%.
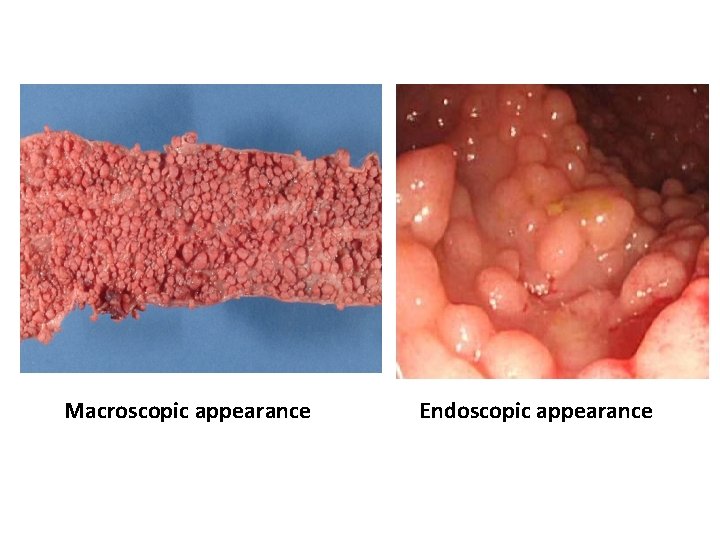
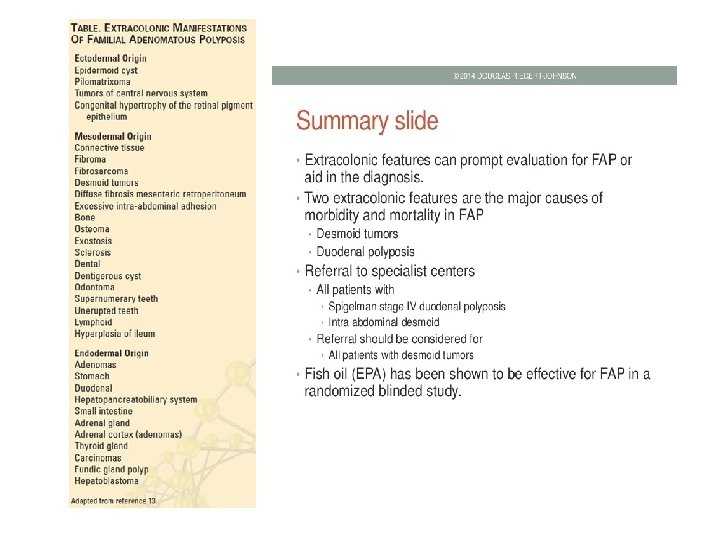
Familial adenomatous polyposis coli (FAP) • Hundreds of colonic polyps - as a result of mutation of APC gene on chromosome 5 q • Autosomal dominant inheritance • Risk of malignancy nearly 100% • Duodenal adenomatous polyps • 20% occur as a new mutation and not be part of an FAP family • 80% of cases with FAP will be familial
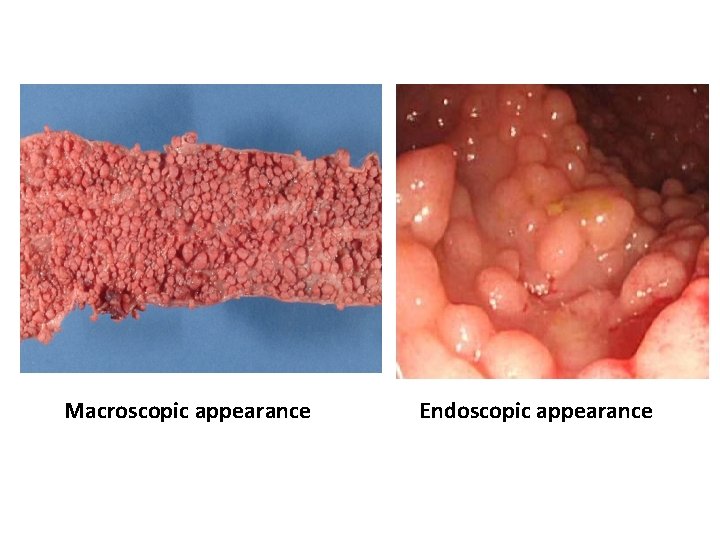
Macroscopic appearance Endoscopic appearance
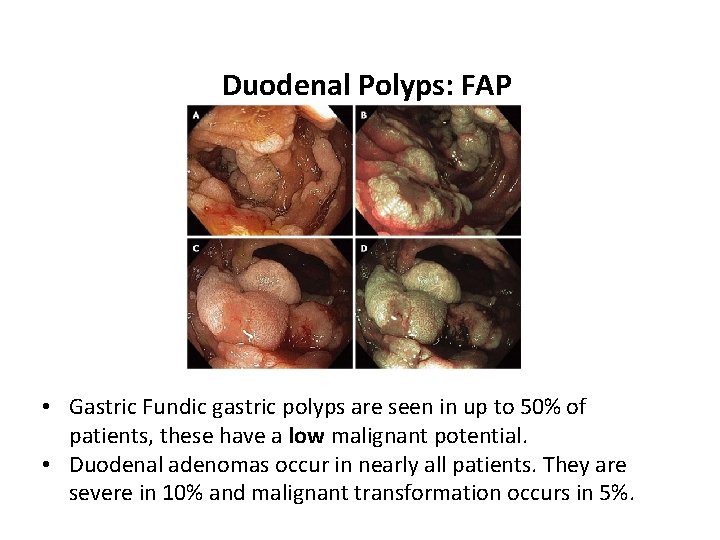
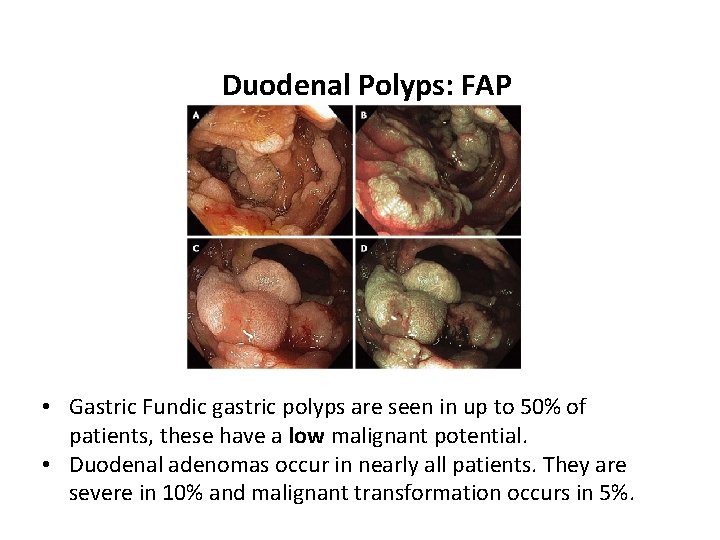
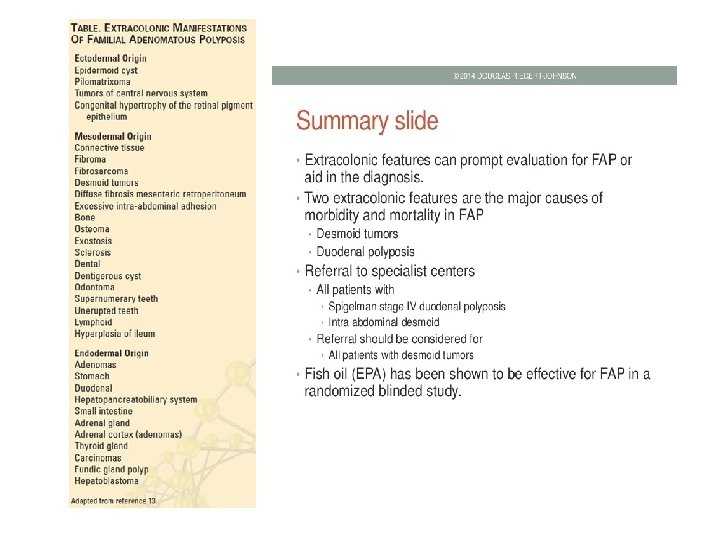
Duodenal Polyps: FAP • Gastric Fundic gastric polyps are seen in up to 50% of patients, these have a low malignant potential. • Duodenal adenomas occur in nearly all patients. They are severe in 10% and malignant transformation occurs in 5%.
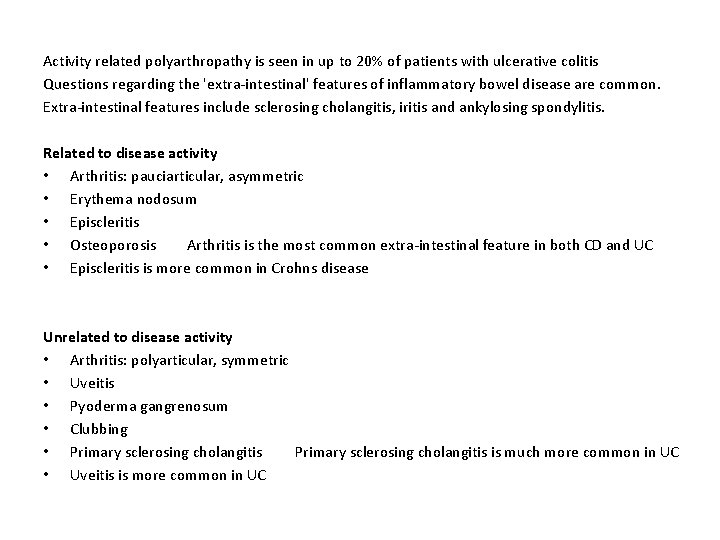
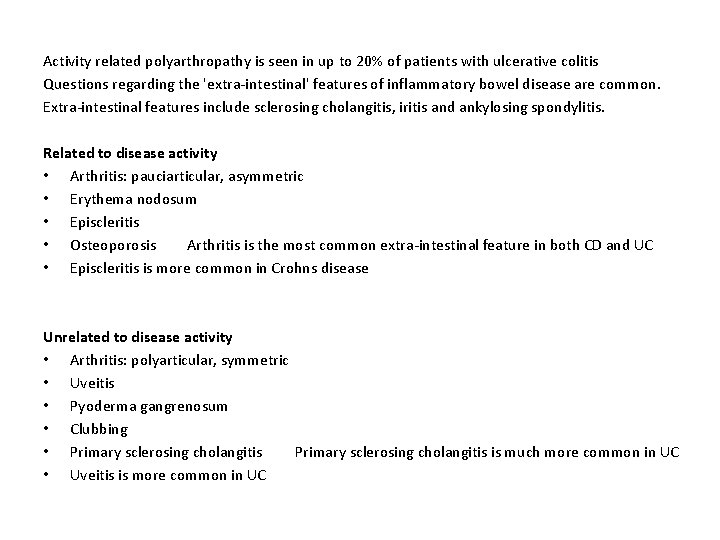
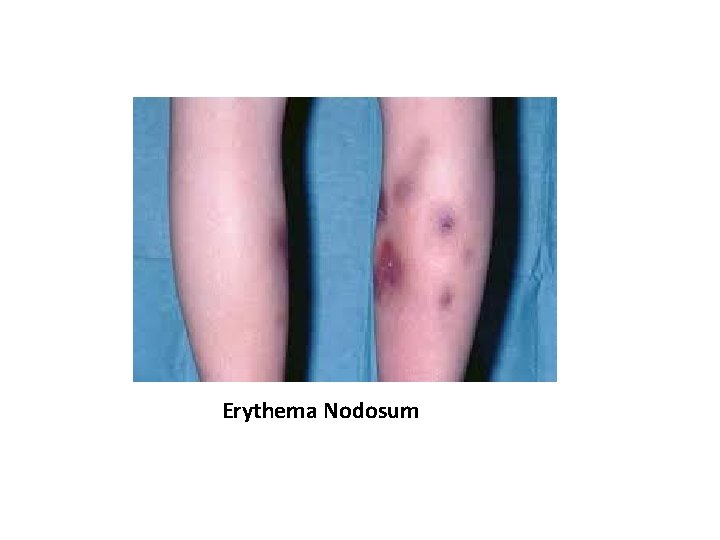
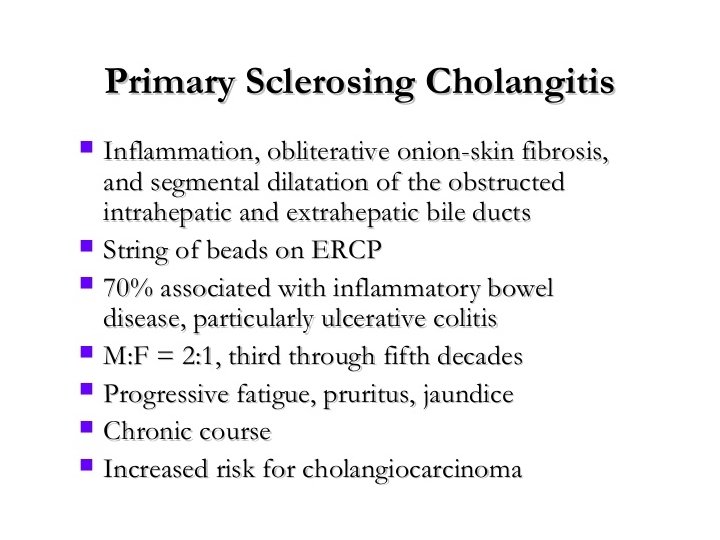
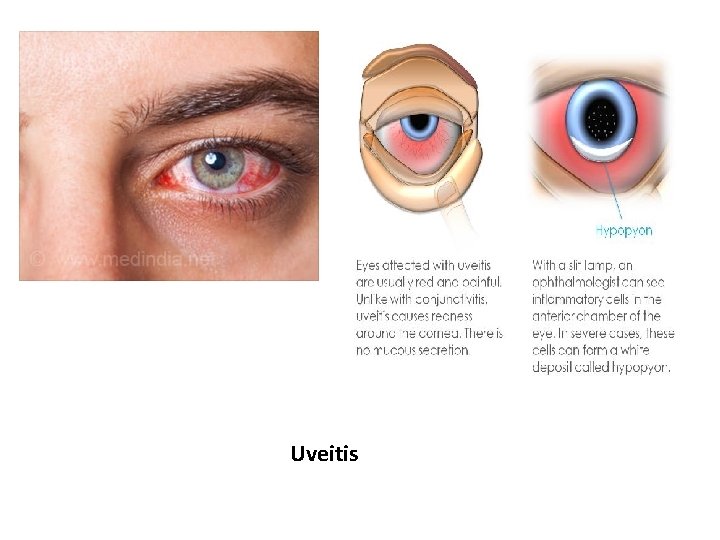
Activity related polyarthropathy is seen in up to 20% of patients with ulcerative colitis Questions regarding the 'extra-intestinal' features of inflammatory bowel disease are common. Extra-intestinal features include sclerosing cholangitis, iritis and ankylosing spondylitis. Related to disease activity • Arthritis: pauciarticular, asymmetric • Erythema nodosum • Episcleritis • Osteoporosis Arthritis is the most common extra-intestinal feature in both CD and UC • Episcleritis is more common in Crohns disease Unrelated to disease activity • Arthritis: polyarticular, symmetric • Uveitis • Pyoderma gangrenosum • Clubbing • Primary sclerosing cholangitis is much more common in UC • Uveitis is more common in UC
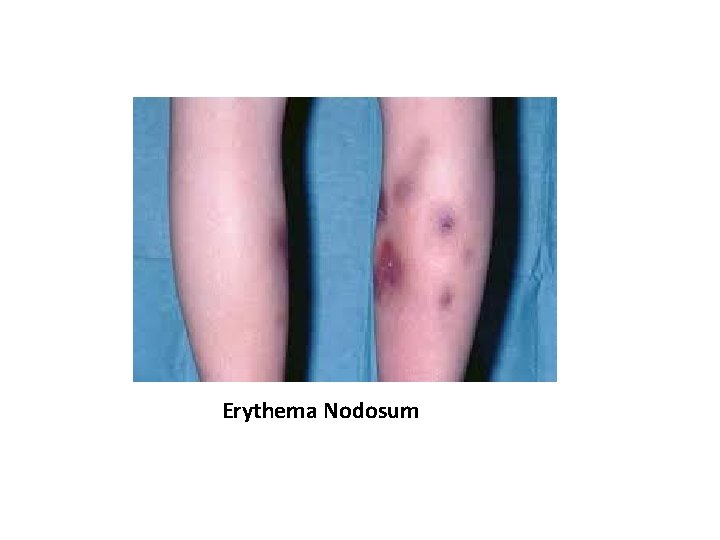
Erythema Nodosum

Pyoderma gangreonosum
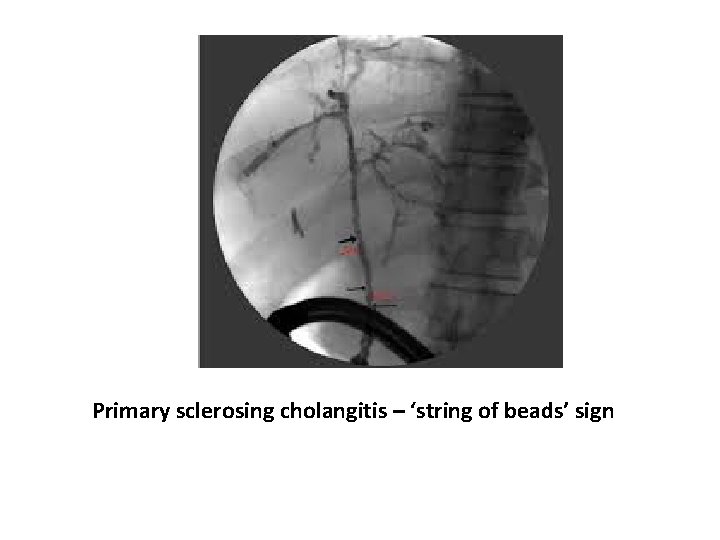
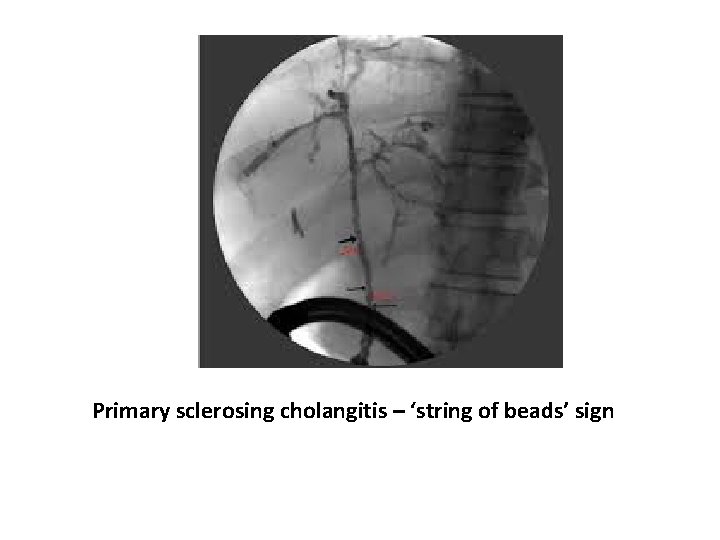
Primary sclerosing cholangitis – ‘string of beads’ sign
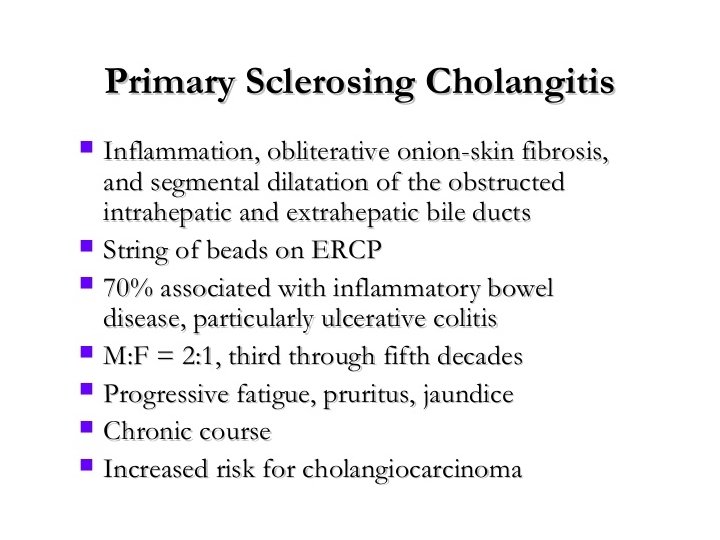
Primary sclerosing cholangitis – ‘string of beads’ sign
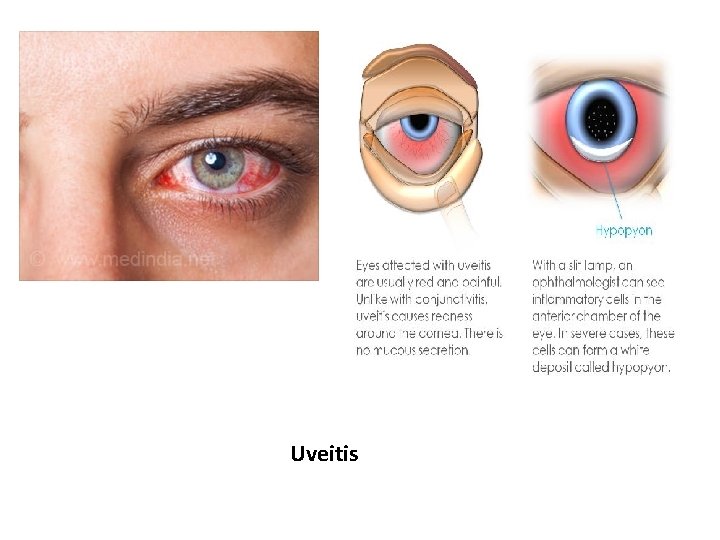
Uveitis
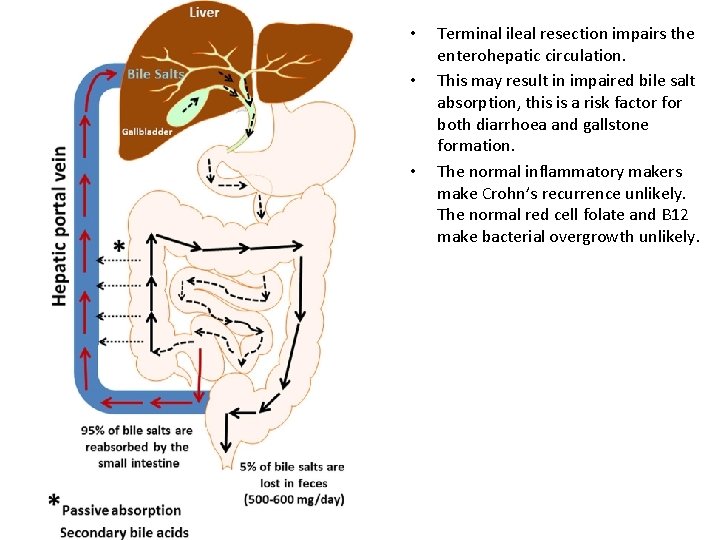
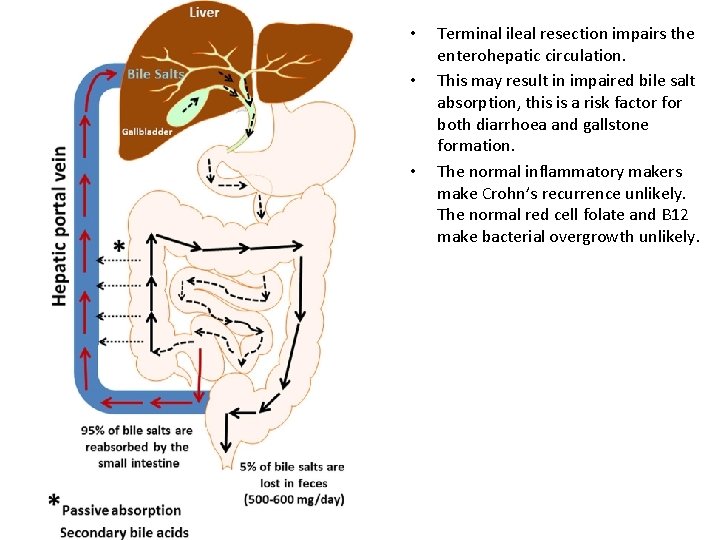
• • • Terminal ileal resection impairs the enterohepatic circulation. This may result in impaired bile salt absorption, this is a risk factor for both diarrhoea and gallstone formation. The normal inflammatory makers make Crohn’s recurrence unlikely. The normal red cell folate and B 12 make bacterial overgrowth unlikely.
• • COLONIC INJURIES Colonic injuries usually arise as a result of penetrating trauma, typically 75% occur as a result of gunshot injuries. Historically, the typical treatment for most types of colonic injury was resection and formation of stoma/ exteriorisation. Non destructive colonic injuries in a stable patient can be managed by primary repair. More significant injuries can be managed by resection and primary anastomosis. In the damage control setting, attempts to anastomose are associated with leak rates of 20% or more.
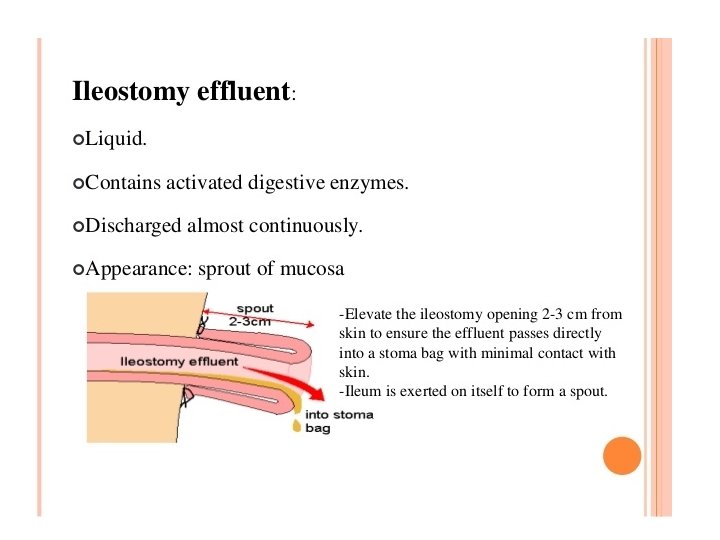
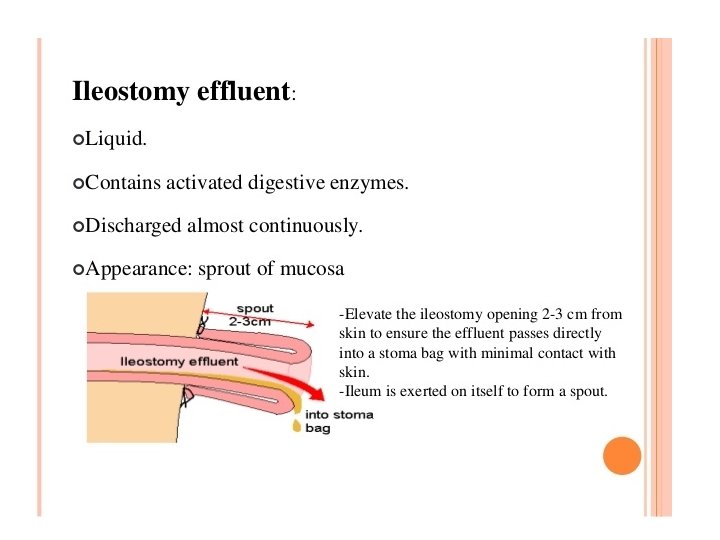
• Ileostomy output is roughly in the range of 510 ml/Kg/ 24 hours. • Output in excess requires supplementary intravenous fluids. • Early high output is not uncommon • AKI risk with high output • Excessive fluid losses are generally managed by administration of oral loperamide (up to 4 mg QDS) to try and slow the output. • Codeine Phosphate / PPI
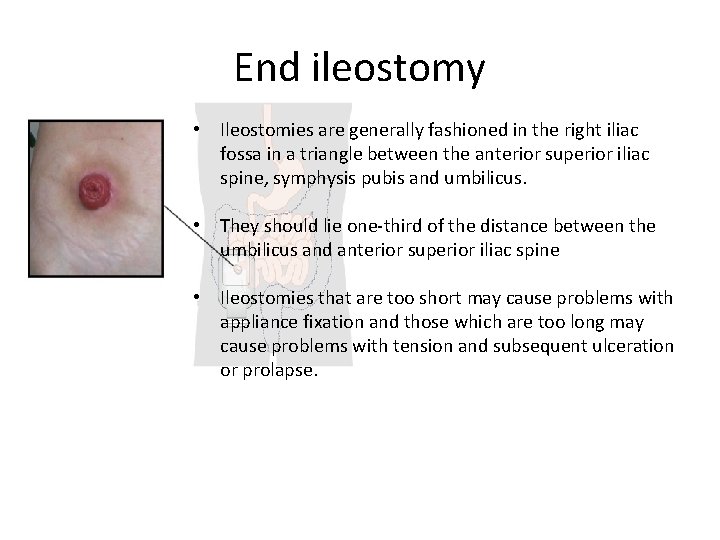
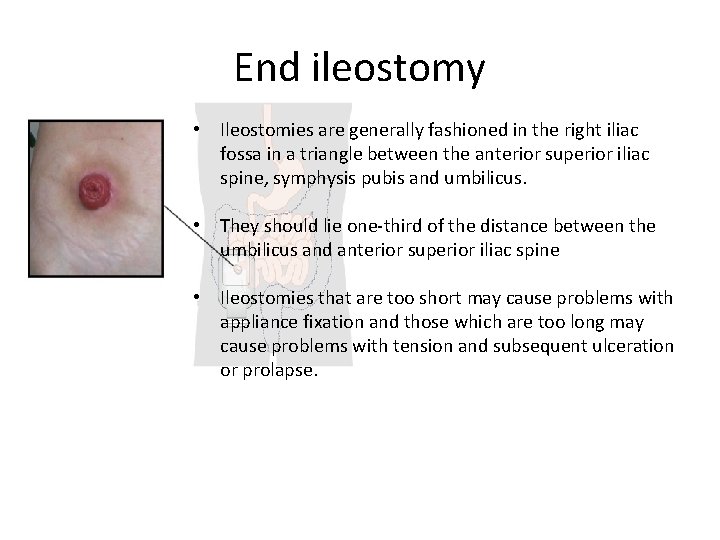
End ileostomy • Ileostomies are generally fashioned in the right iliac fossa in a triangle between the anterior superior iliac spine, symphysis pubis and umbilicus. • They should lie one-third of the distance between the umbilicus and anterior superior iliac spine • Ileostomies that are too short may cause problems with appliance fixation and those which are too long may cause problems with tension and subsequent ulceration or prolapse.
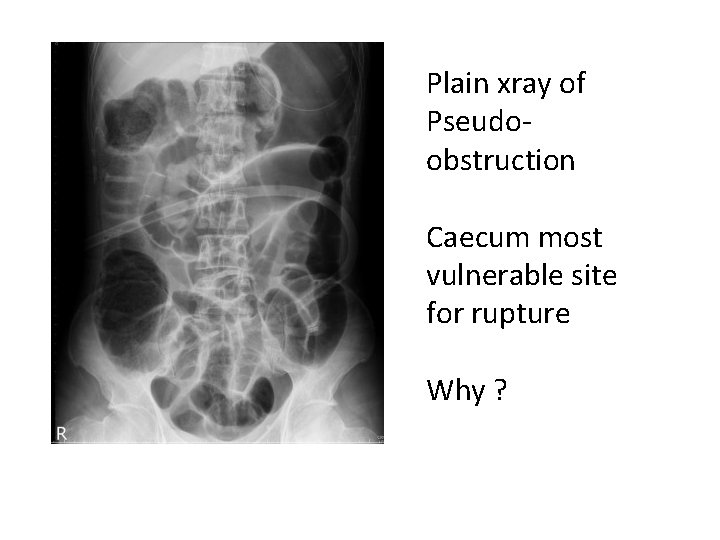
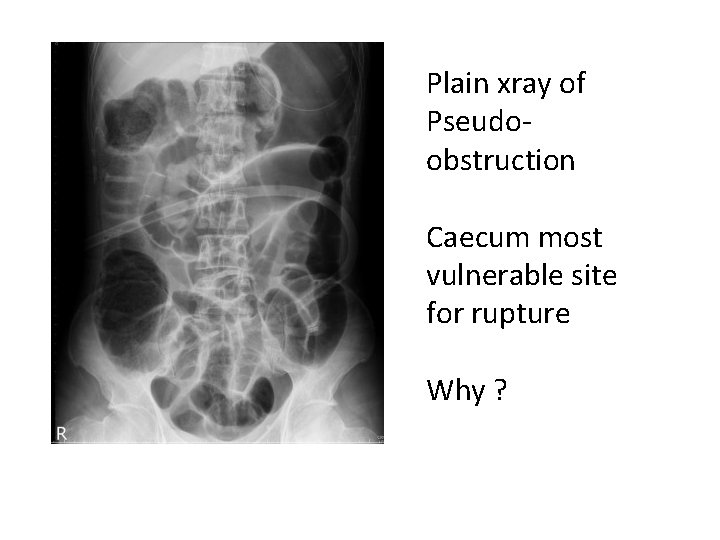
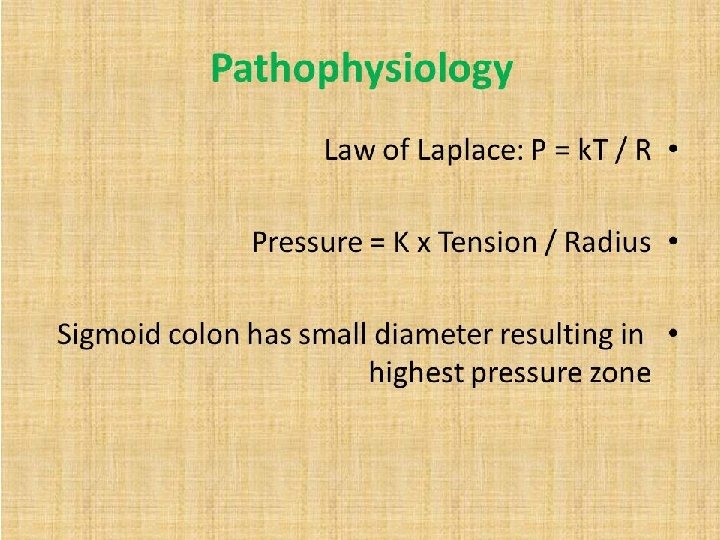
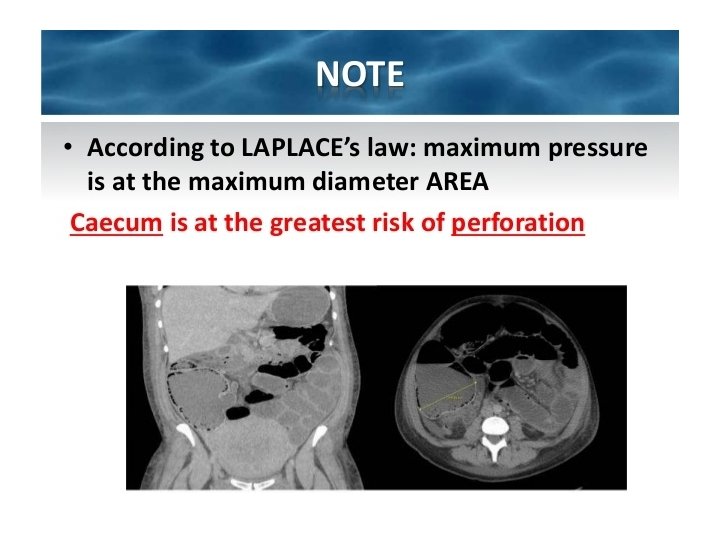
Plain xray of Pseudoobstruction Caecum most vulnerable site for rupture Why ?
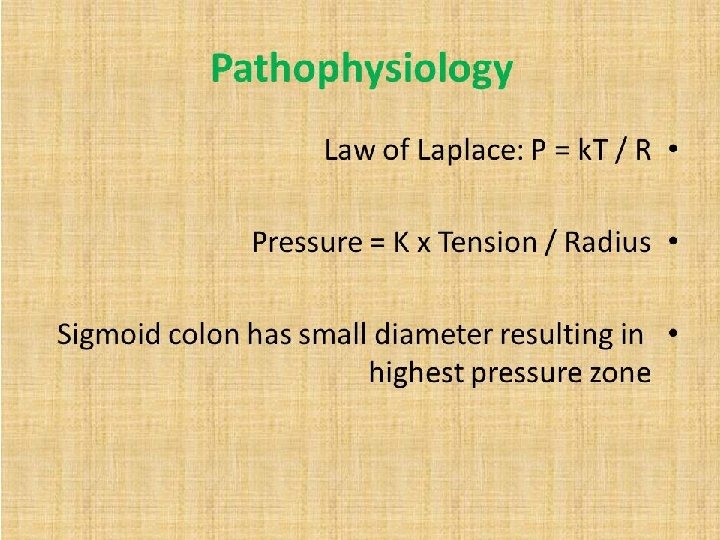
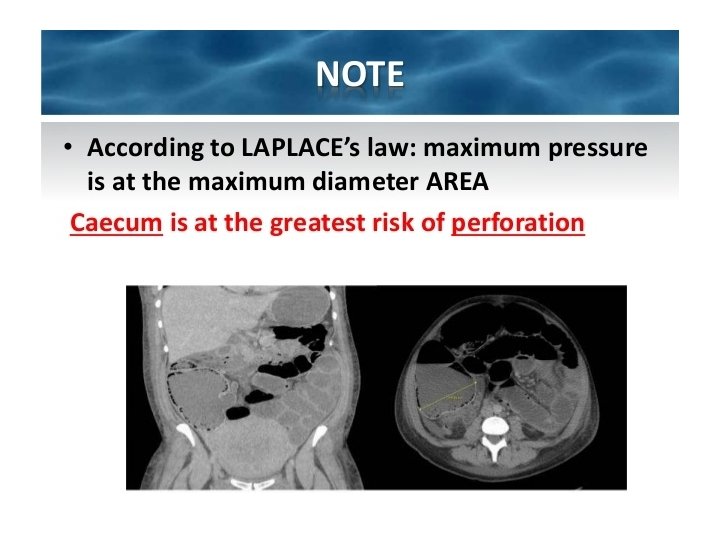
• Neostigmine affects the degradation of acetylcholine and will therefore stimulate both nicotinic and muscarinic receptors. • It may produce symptomatic bradycardia and should therefore only be administered in a monitored environment. • In colonic pseudo-obstruction it produces generalised colonic contractions and its onset is usually rapid.
Anal sphincter • Internal anal sphincter composed of smooth muscle continuous with the circular muscle of the rectum. It surrounds the upper two- thirds of the anal canal and is supplied by sympathetic nerves. • External anal sphincter is composed of striated muscle which surrounds the internal sphincter but extends more distally. • The nerve supply of the external anal sphincter is from the inferior rectal branch of the pudendal nerve (S 2 and S 3) and the perineal branch of the S 4 nerve roots. • The external anal sphincter is innervated by the inferior rectal branch of the pudendal nerve, this has root values of S 2, 3 and the perineal branch of S 4
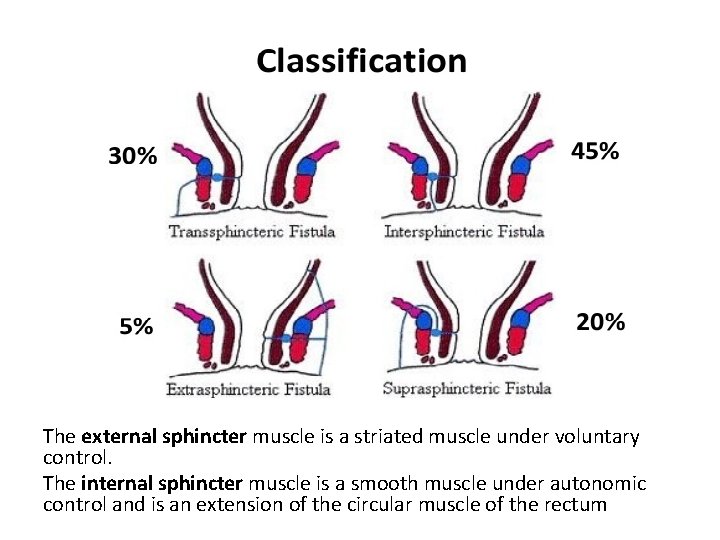
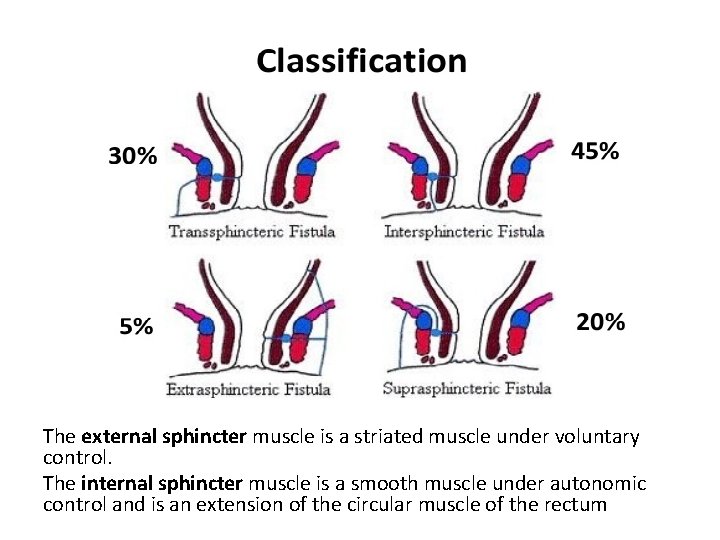
The external sphincter muscle is a striated muscle under voluntary control. The internal sphincter muscle is a smooth muscle under autonomic control and is an extension of the circular muscle of the rectum
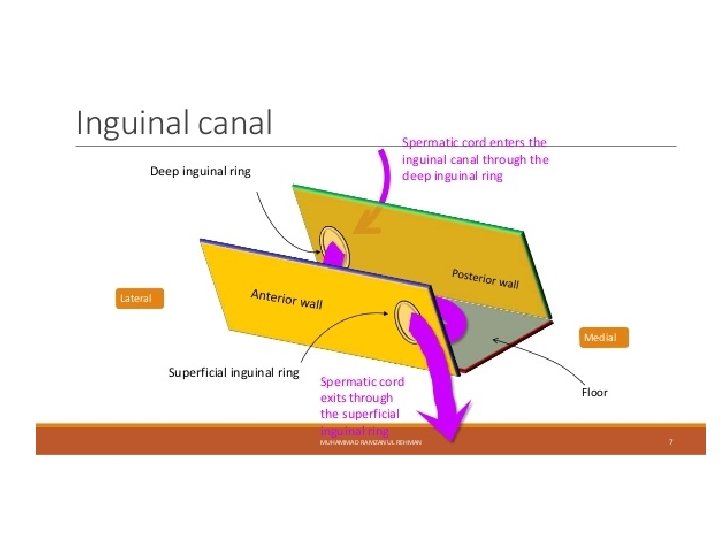
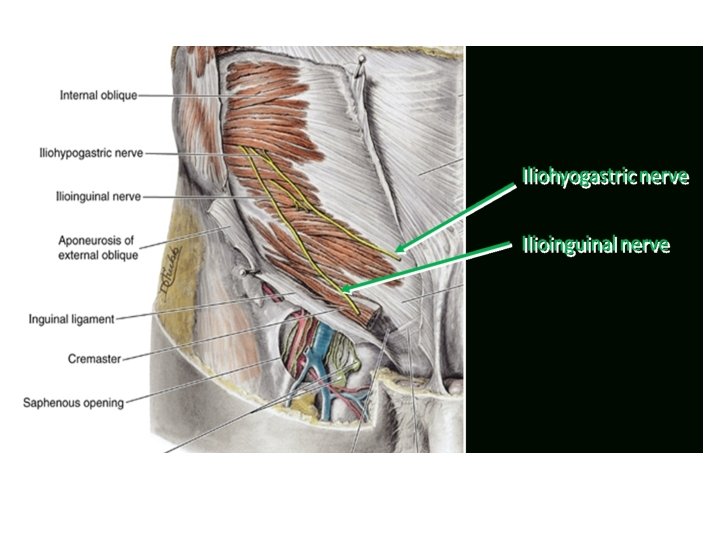
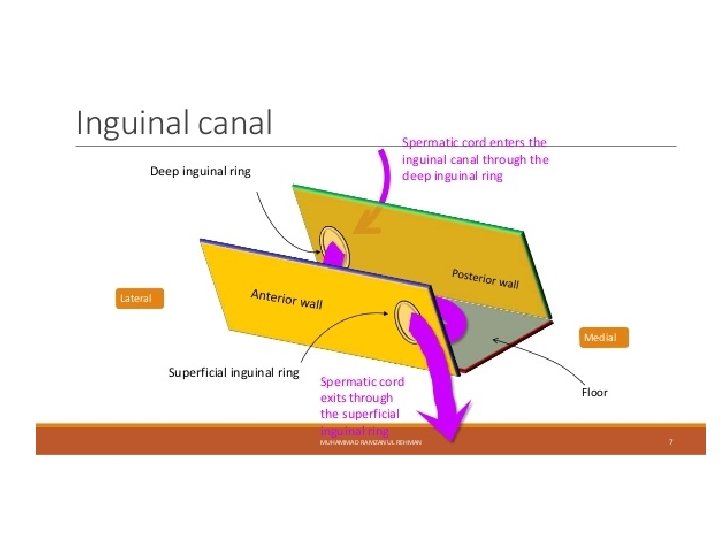
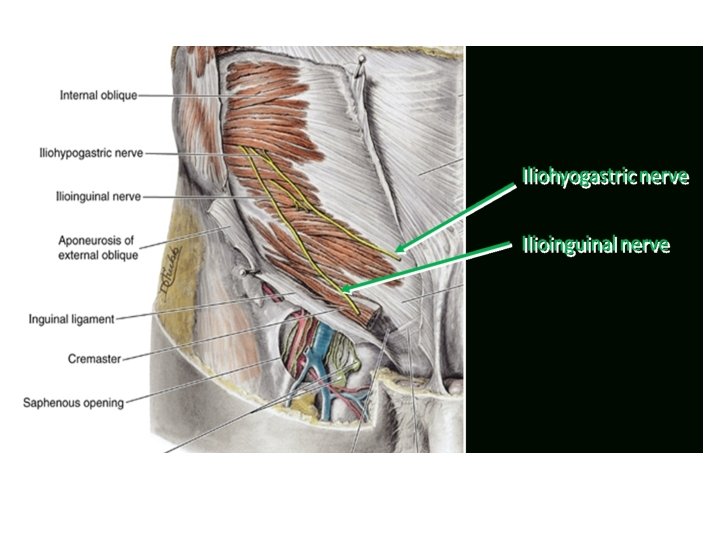
Contents Males • Spermatic cord and ilioinguinal nerve As it passes through the canal the spermatic cord has 3 coverings: • External spermatic fascia from external oblique aponeurosis Cremasteric fascia Internal spermatic fascia Females Round ligament of uterus and ilioinguinal nerve
Contents • The genitofemoral nerve divides into two branches as it approaches the inguinal ligament. • The genital branch passes anterior to the external iliac artery through the deep inguinal ring into the inguinal canal. • It communicates with the ilioinguinal nerve in the inguinal canal.
Genitofemoral nerve Supplies • Small area of the upper medial thigh Path • Arises from the first and second lumbar nerves • Passes obliquely through Psoas major, and emerges from its medial border opposite the fibrocartilage between the third and fourth lumbar vertebrae. • It then descends on the surface of Psoas major, under cover of the peritoneum • Divides into genital and femoral branches. • The genital branch passes through the inguinal canal, within the spermatic cord, to supply the skin overlying the skin and fascia of the scrotum. The femoral branch enters the thigh posterior to the inguinal ligament, lateral to the femoral artery. It supplies an area of skin and fascia over the femoral triangle. • It may be injured during abdominal or pelvic surgery, or during inguinal hernia repairs.
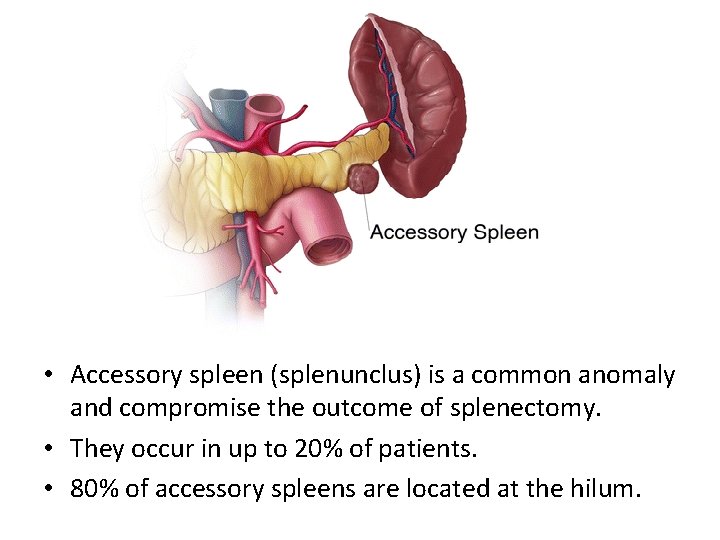
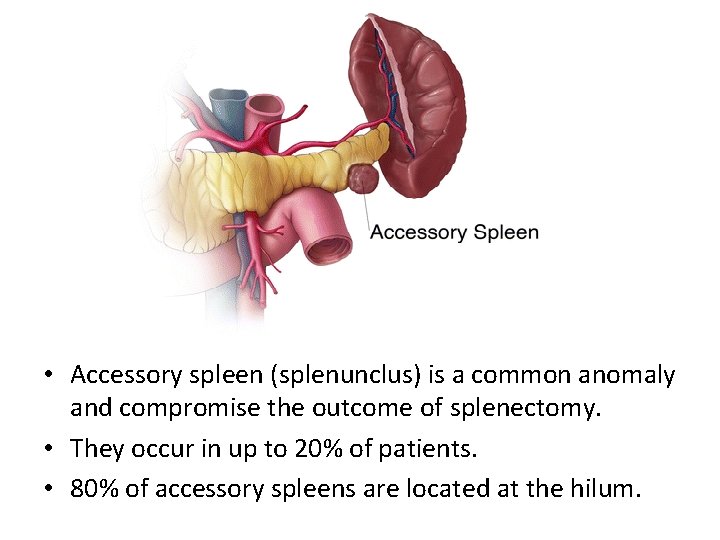
• Accessory spleen (splenunclus) is a common anomaly and compromise the outcome of splenectomy. • They occur in up to 20% of patients. • 80% of accessory spleens are located at the hilum.
 Breast lump differential diagnosis
Breast lump differential diagnosis Tnm stage lung cancer
Tnm stage lung cancer Ajcc breast cancer staging
Ajcc breast cancer staging Gulf university
Gulf university Amsterdam criteria
Amsterdam criteria Colorectal cancer drug trial
Colorectal cancer drug trial Sorunun cevabını bul
Sorunun cevabını bul Pl
Pl Breast tnm staging
Breast tnm staging Yp tnm staging
Yp tnm staging Carcinoma bronquioloalveolar
Carcinoma bronquioloalveolar Prostate cancer tnm classification
Prostate cancer tnm classification Prostate cancer staging
Prostate cancer staging Mammoprint
Mammoprint Glottic cancer staging
Glottic cancer staging Patho
Patho Ann lyons colorectal surgeon
Ann lyons colorectal surgeon Tnm ovario
Tnm ovario Mammadensiteit c
Mammadensiteit c Tnm crc
Tnm crc Colonografía
Colonografía Manuel alejandro martinez vazquez
Manuel alejandro martinez vazquez Tnm ovario
Tnm ovario Tnm colangiocarcinoma
Tnm colangiocarcinoma Tnm tiroide
Tnm tiroide Tnm 8 head and neck
Tnm 8 head and neck Classificazione di bormann
Classificazione di bormann Tnm yp
Tnm yp What is the main purpose of the persuasive paragraph mcq
What is the main purpose of the persuasive paragraph mcq Systemic pathology mcqs
Systemic pathology mcqs Mcq on university wits
Mcq on university wits Hyaline cartilage
Hyaline cartilage Subroto's father consider subroto and his sibling with___.
Subroto's father consider subroto and his sibling with___. Therapeutic exercise chapter 1 mcqs
Therapeutic exercise chapter 1 mcqs Protein metabolism mcqs
Protein metabolism mcqs Ozymandias alliteration
Ozymandias alliteration Concept of stress and coping mcqs
Concept of stress and coping mcqs Two races of man by charles lamb analysis
Two races of man by charles lamb analysis Positive psychology mcqs
Positive psychology mcqs Xbreast
Xbreast Mcq on memory in psychology
Mcq on memory in psychology University wits mcqs
University wits mcqs Vignette style multiple choice
Vignette style multiple choice Building blocks of data warehouse
Building blocks of data warehouse Sacroilitis radiopedia
Sacroilitis radiopedia Enneking classification
Enneking classification Arena stage theatre definition
Arena stage theatre definition