LeggCalve Perthes Disease FIRM 1 GRANDROUND PRESENTERS DR


- Slides: 44
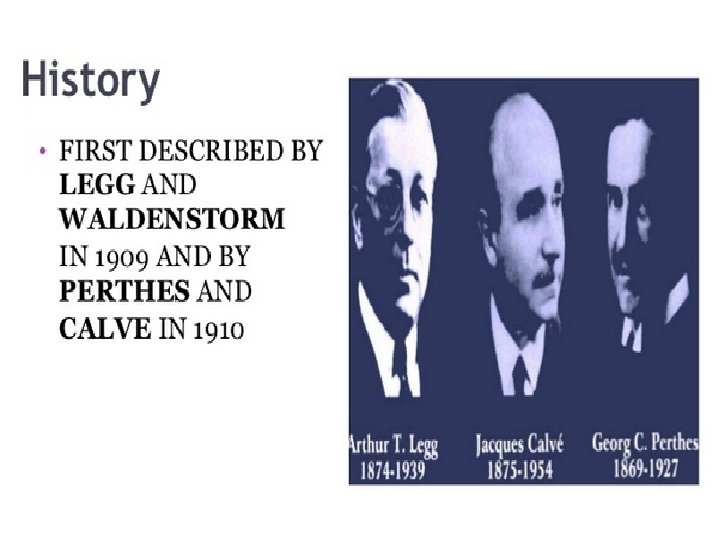
Legg-Calve. Perthes Disease FIRM 1 GRANDROUND PRESENTERS: DR. MAINA/DR. ONDARI FACILITATOR: DR. T. MOGIRE 01/08/2013
Georg Perthes (1869 -1927)
First described by Karel Maydl
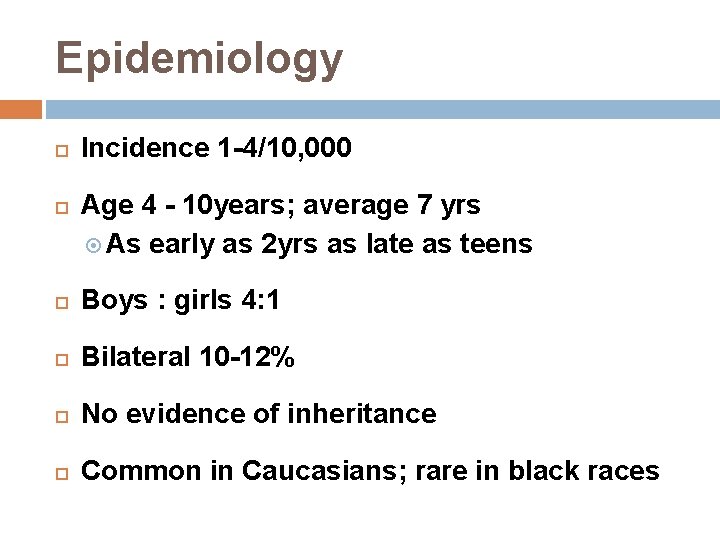
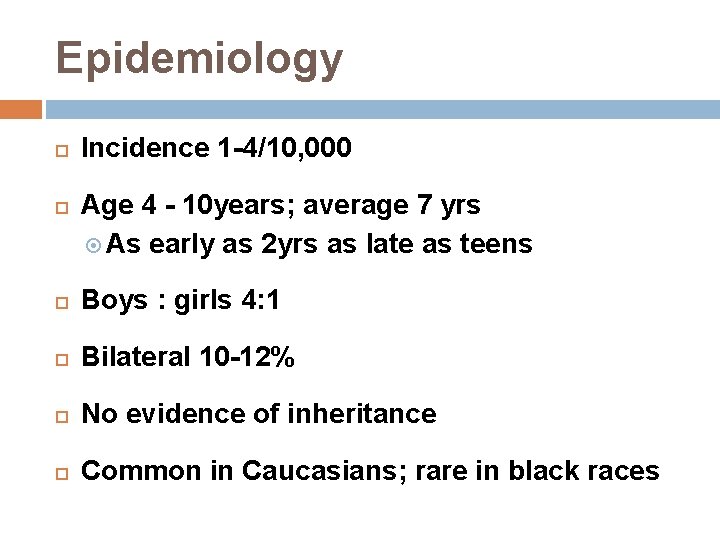
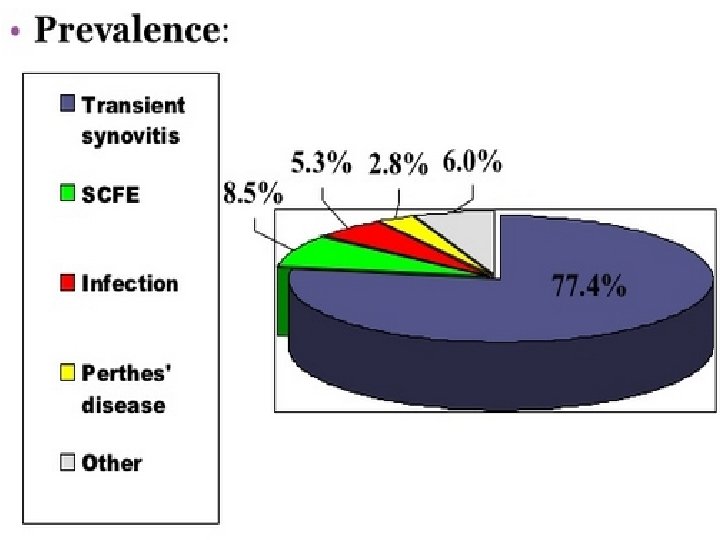
Epidemiology Incidence 1 -4/10, 000 Age 4 - 10 years; average 7 yrs As early as 2 yrs as late as teens Boys : girls 4: 1 Bilateral 10 -12% No evidence of inheritance Common in Caucasians; rare in black races
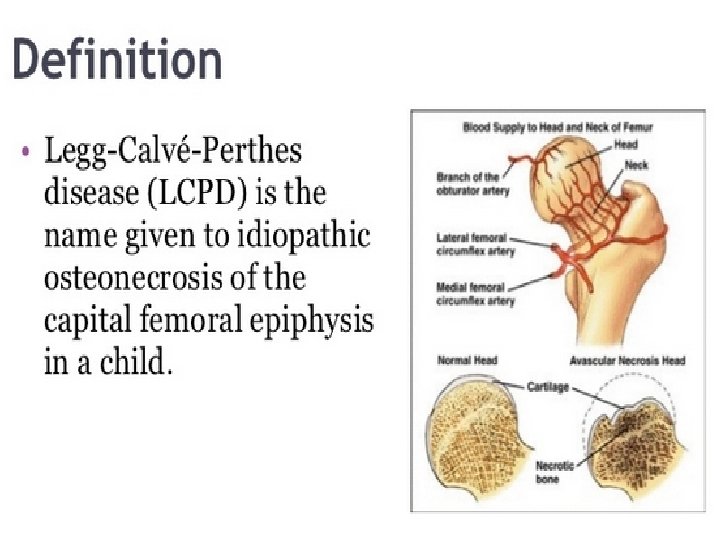
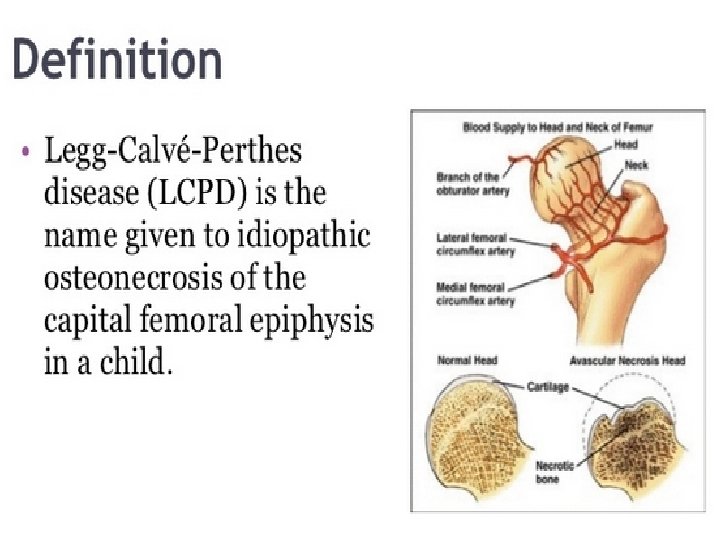
Etiology Idiopathic Past theories Infection, inflammation, trauma, congenital Most theories involve vascular compromise
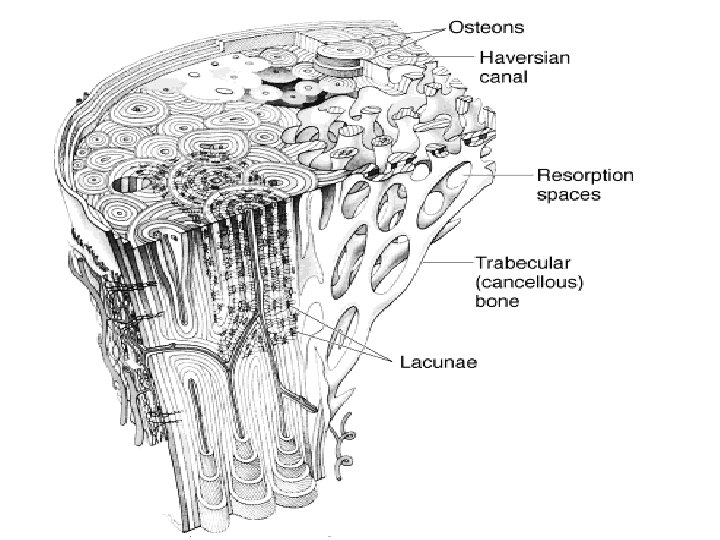
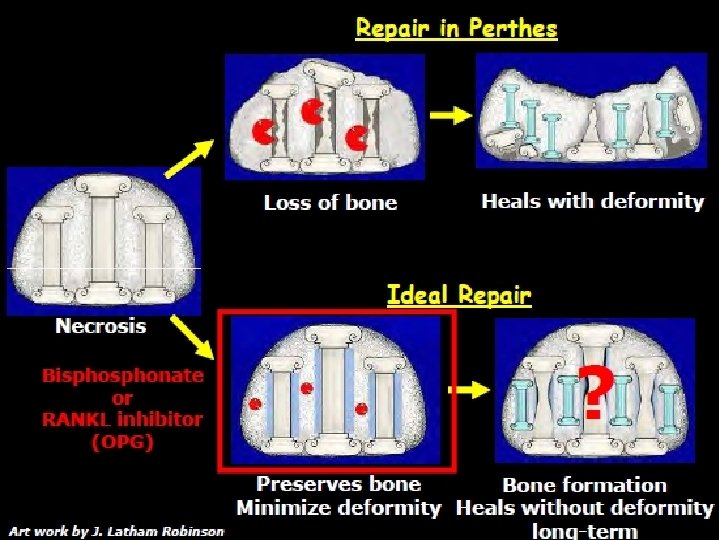
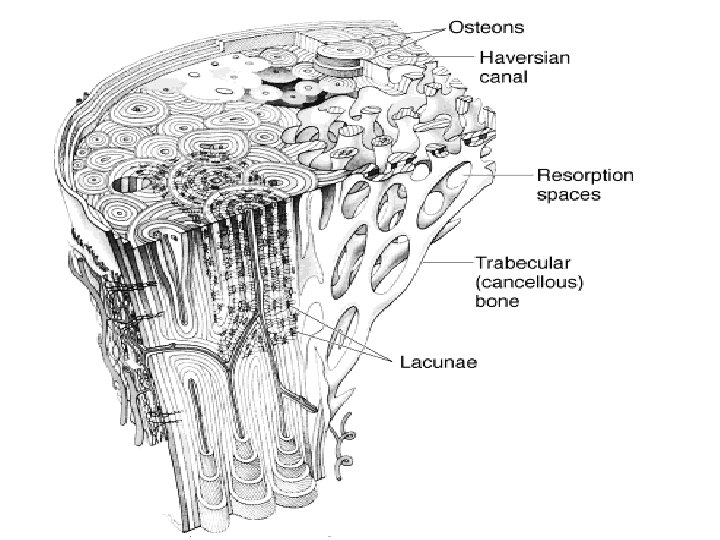
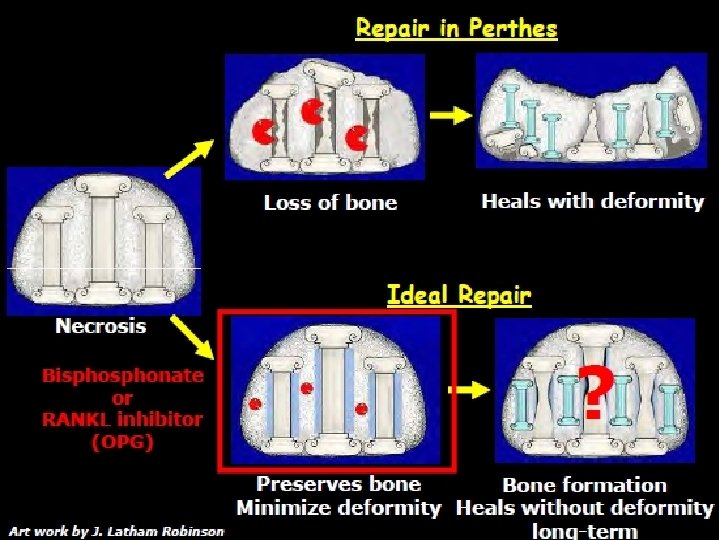
Pathophysiology Rapid growth occurs in relation to devt of blood supply Interruption of blood supply results in necrosis, removal of necrotic tissue, and its replacement with new bone. Bone replacement may be so complete and perfect that completely normal bone may result The adequacy of bone replacement depends on
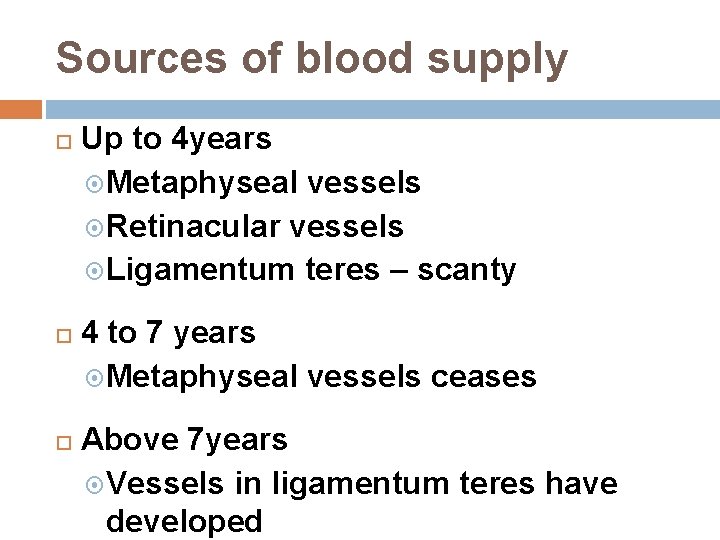
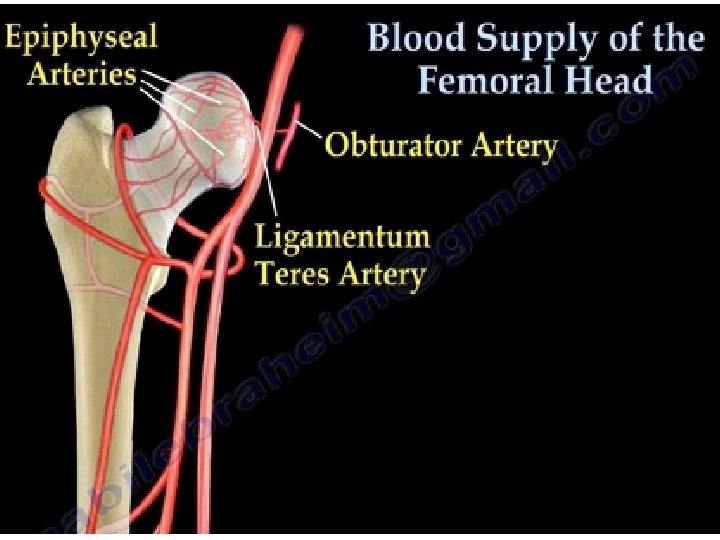
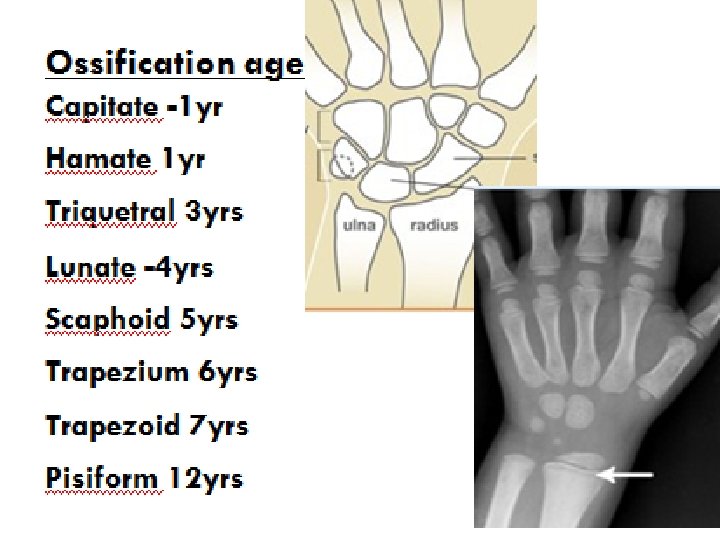
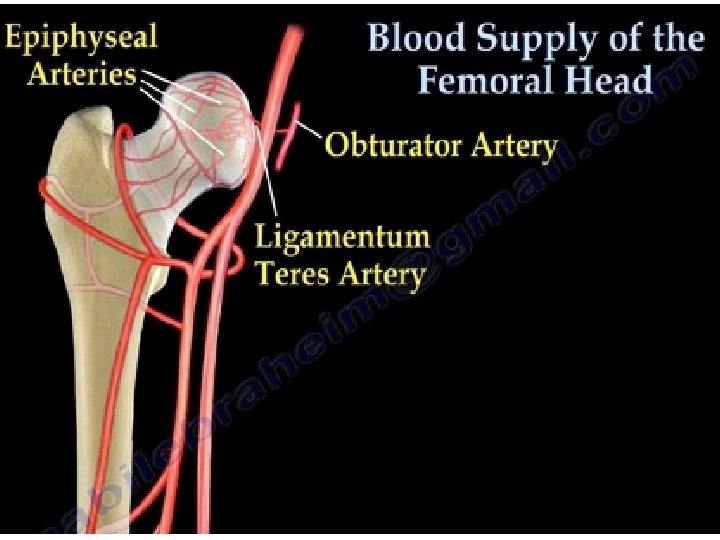
Sources of blood supply Up to 4 years Metaphyseal vessels Retinacular vessels Ligamentum teres – scanty 4 to 7 years Metaphyseal vessels ceases Above 7 years Vessels in ligamentum teres have developed
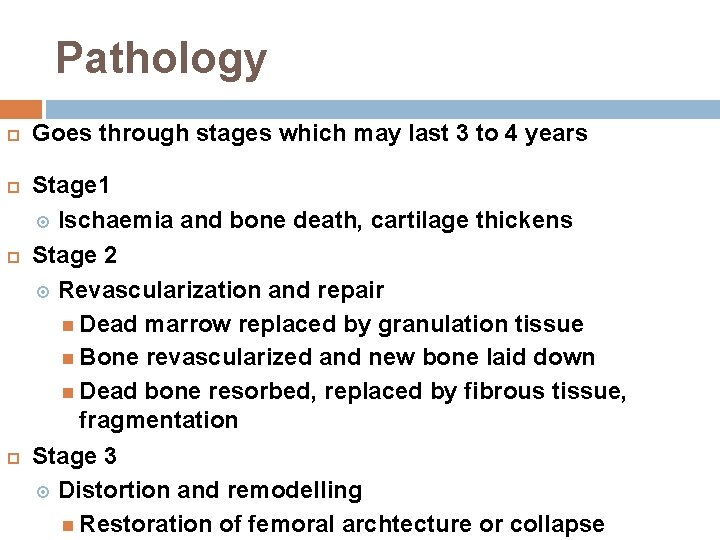
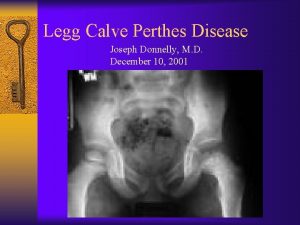
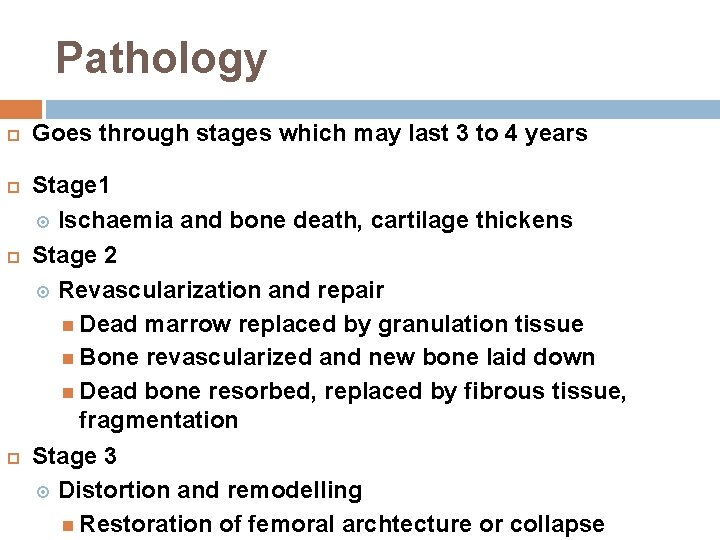
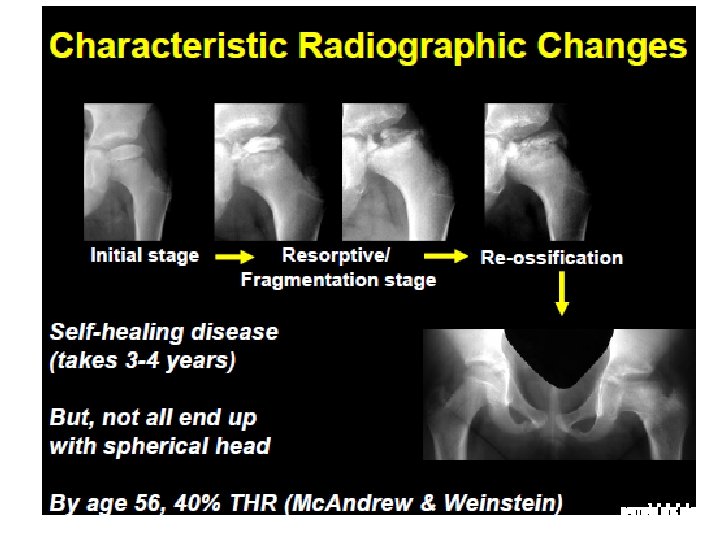
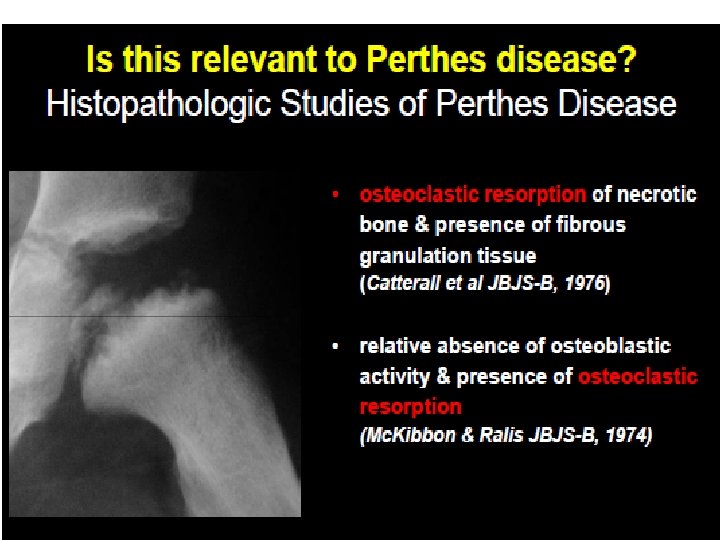
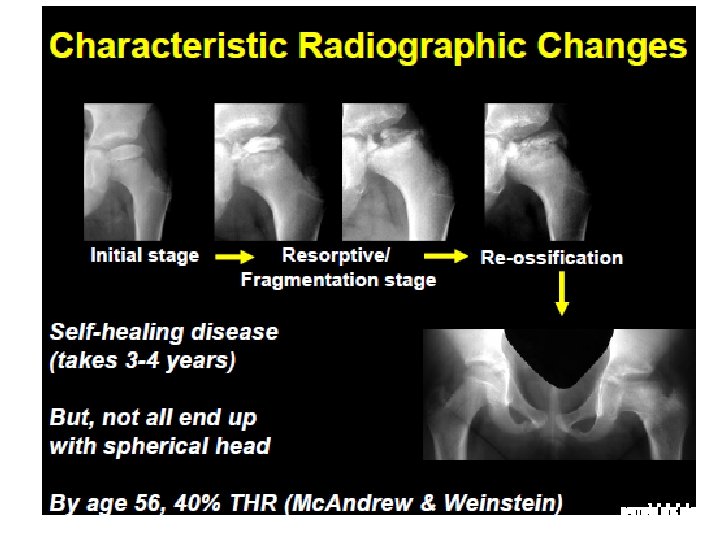
Pathology Goes through stages which may last 3 to 4 years Stage 1 Ischaemia and bone death, cartilage thickens Stage 2 Revascularization and repair Dead marrow replaced by granulation tissue Bone revascularized and new bone laid down Dead bone resorbed, replaced by fibrous tissue, fragmentation Stage 3 Distortion and remodelling Restoration of femoral archtecture or collapse
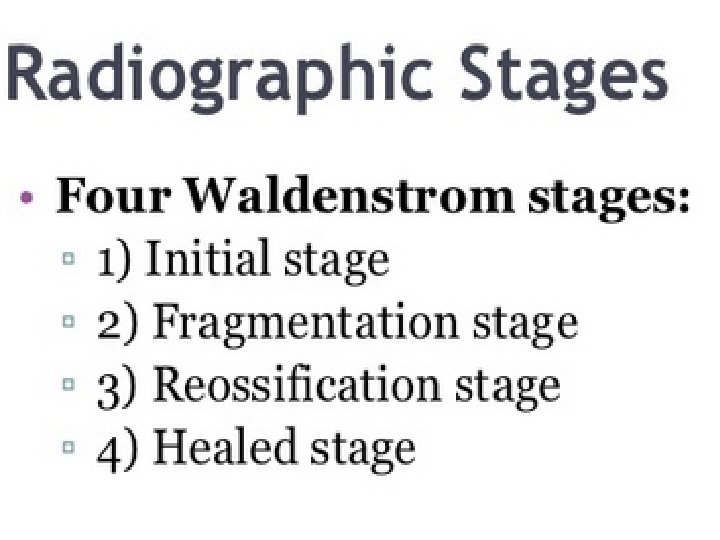
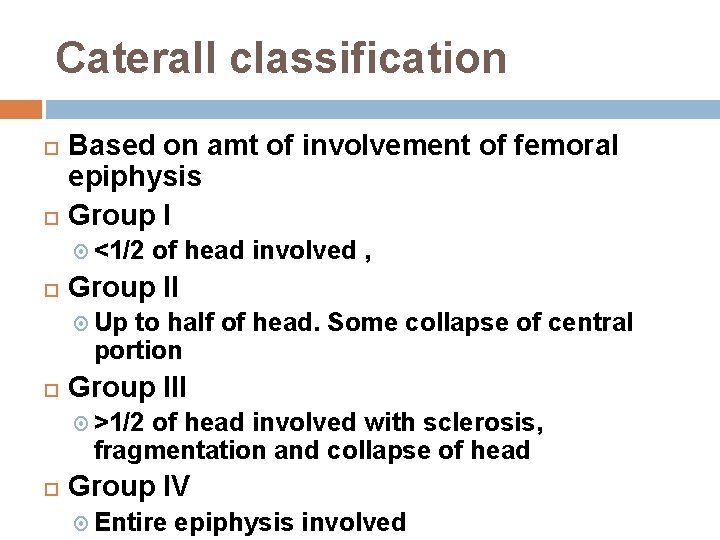
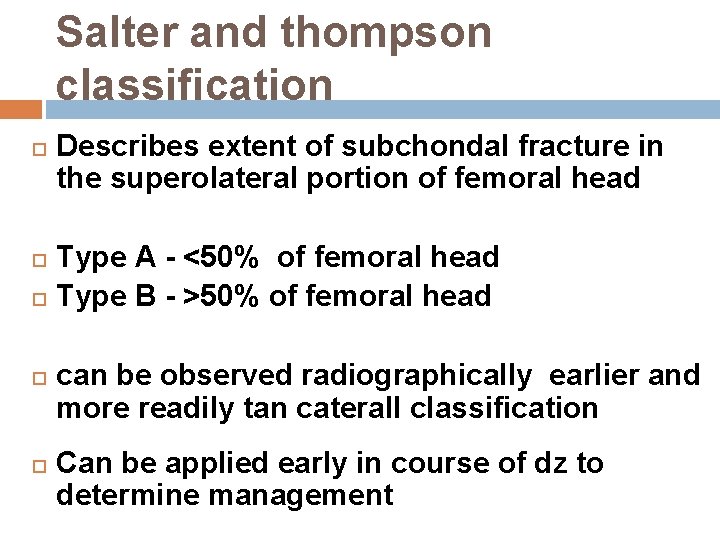
Classification Waldenstrom classification Catterall classification Salter and thompson classification Herring classification
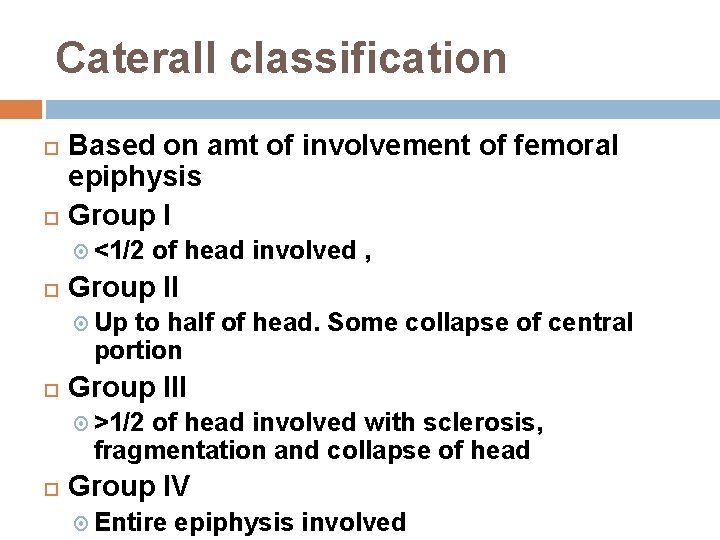
Caterall classification Based on amt of involvement of femoral epiphysis Group I <1/2 of head involved , Group II Up to half of head. Some collapse of central portion Group III >1/2 of head involved with sclerosis, fragmentation and collapse of head Group IV Entire epiphysis involved
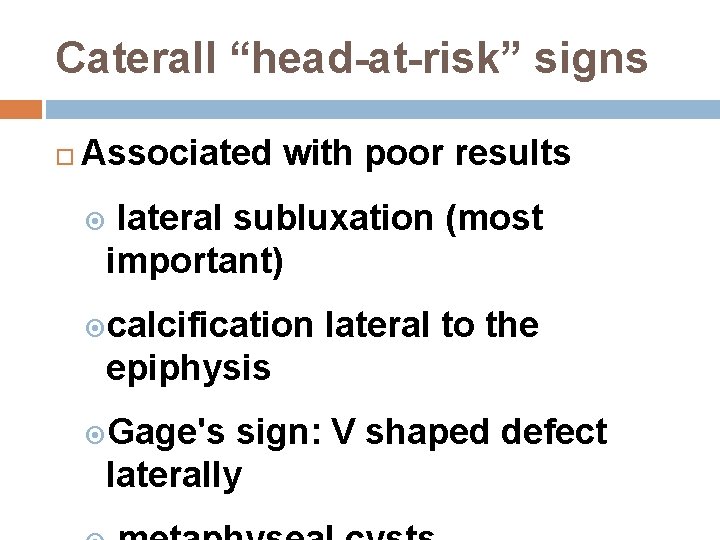
Caterall “head-at-risk” signs Associated with poor results lateral subluxation (most important) calcification lateral to the epiphysis Gage's sign: V shaped defect laterally

Caterall “head-at-risk” sign metaphyseal cysts

Gage's sign
Salter and thompson classification Describes extent of subchondal fracture in the superolateral portion of femoral head Type A - <50% of femoral head Type B - >50% of femoral head can be observed radiographically earlier and more readily tan caterall classification Can be applied early in course of dz to determine management
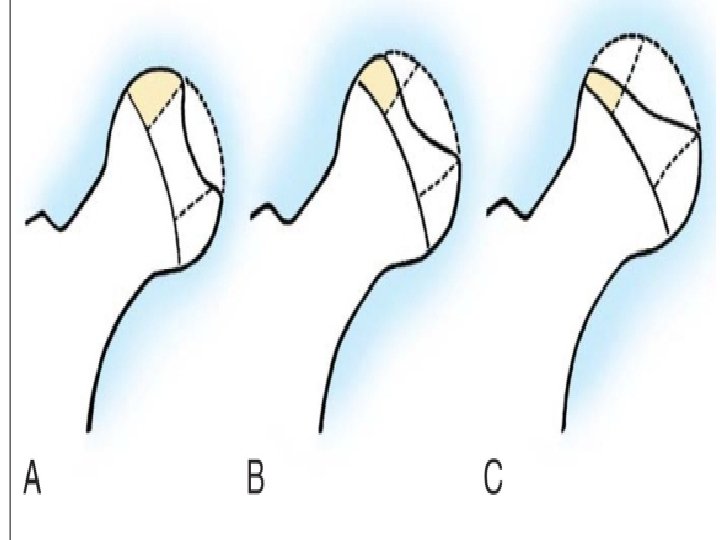
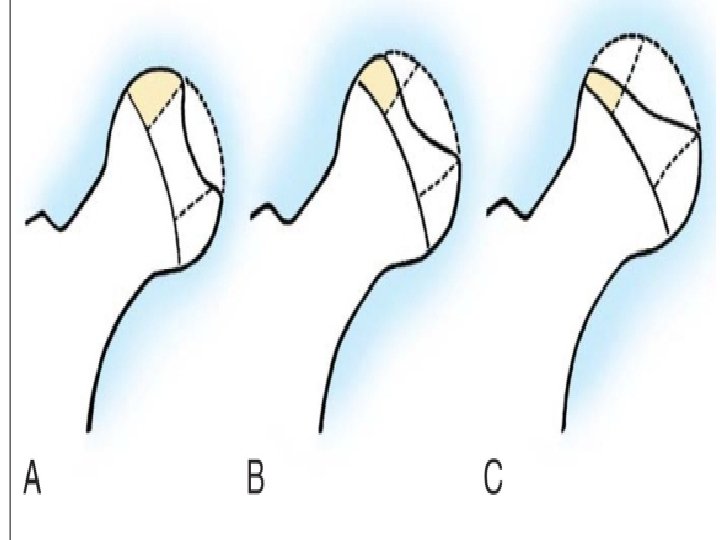
Herring classificatin/lateral pillar Based on degree of collapse of lateral pillar during fragmentation stage Goup A No collapse, no progressive flattening Group B <50% collapse Group C >50% collapse Ritterbusch 1993 Has the highest predictive value and interobserver reliability
Bilateral involvement More severe dz than unilateral Boys and girls equally affected Independent event Bone age delayed in perthes disease
Examination Short stature Delayed bone age Early Decreased ROM Antalgic gait Late Decreased ROM of motion from acetabular impingement Disuse atrophy of thigh muscles Leg lenght descrepancy Trendelenburg gait
Investigations Blood tests haemogram, ESR, CRP Imaging Plain X-rays Hip U/S Bone scintigrpahy MRI Dynamic arthrography Assess spherity of femoral head Hinge abduction Bilateral perthes Skeleta survey as part of work-up
Song et al MRI findings on widened medial joint space Initial stage Overgrowth of cartilage Fragmentation stage Overgrown cartilage with widened true medial joint space Healing stage Widened true medial joint space
Treatment Goals of tratment Maintain femoral head spherity – containment Avoid severe degenerative arthritis Guided by Age Severity Limitation in ROM
Treatment cont. Initial Mx determined by sympts severity Analgesia Modification of activities Bedrest and short period of traction Wheelchair/crutch walking discouraged
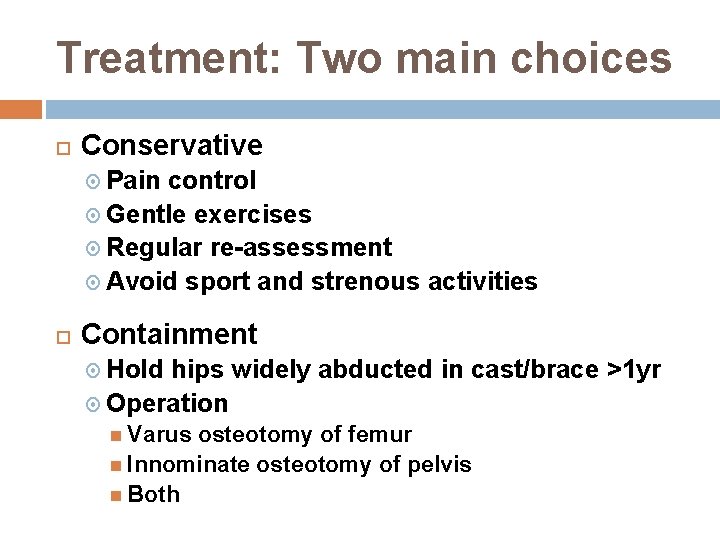
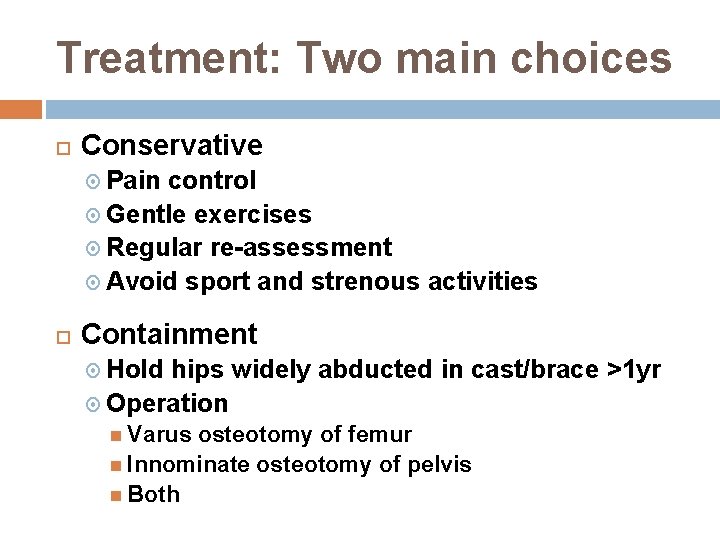
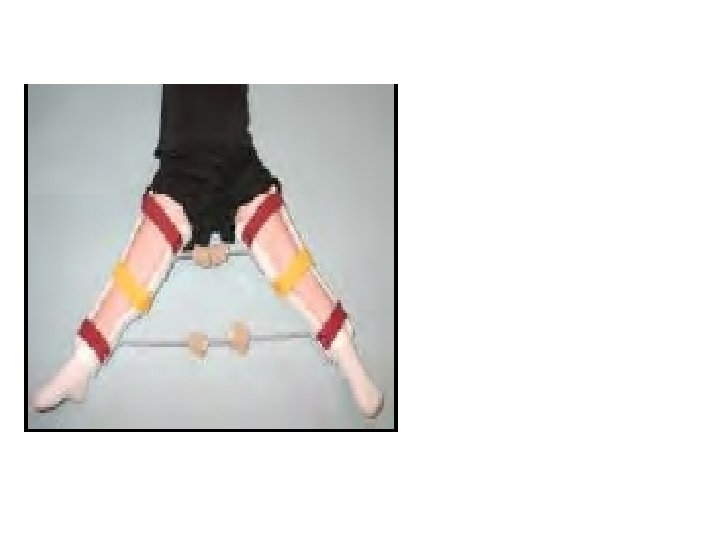
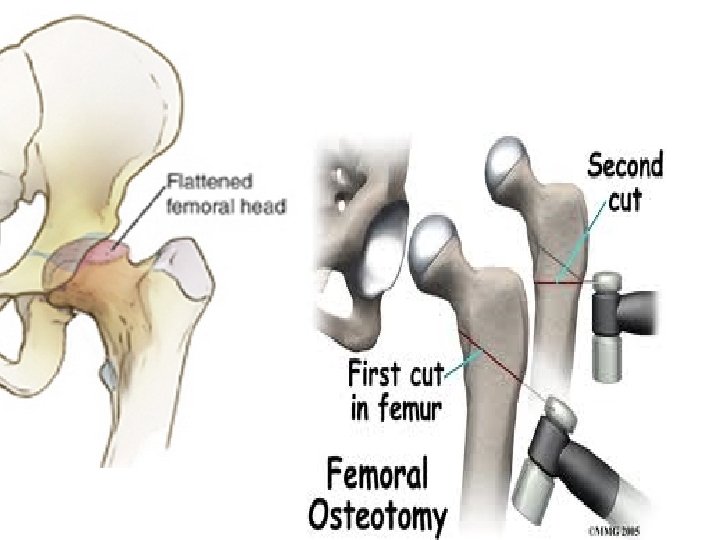
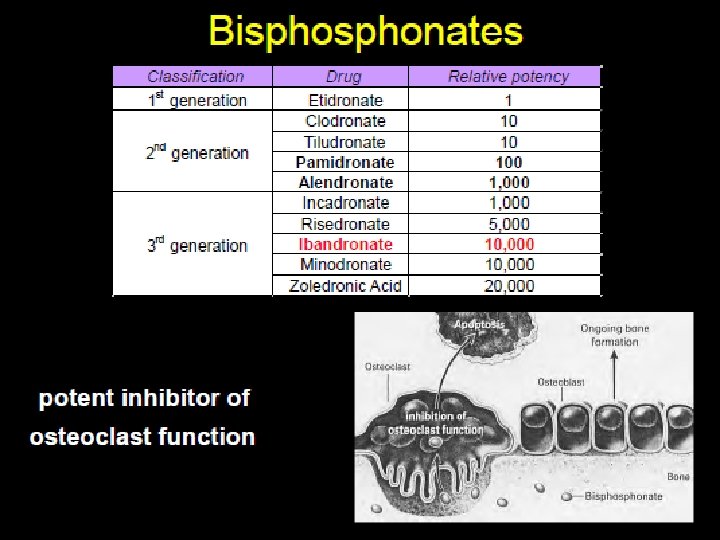
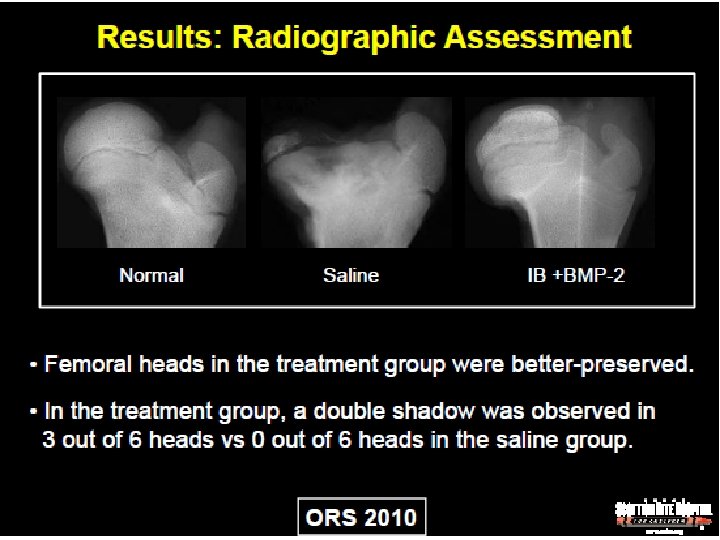
Treatment: Two main choices Conservative Pain control Gentle exercises Regular re-assessment Avoid sport and strenous activities Containment Hold hips widely abducted in cast/brace >1 yr Operation Varus osteotomy of femur Innominate osteotomy of pelvis Both
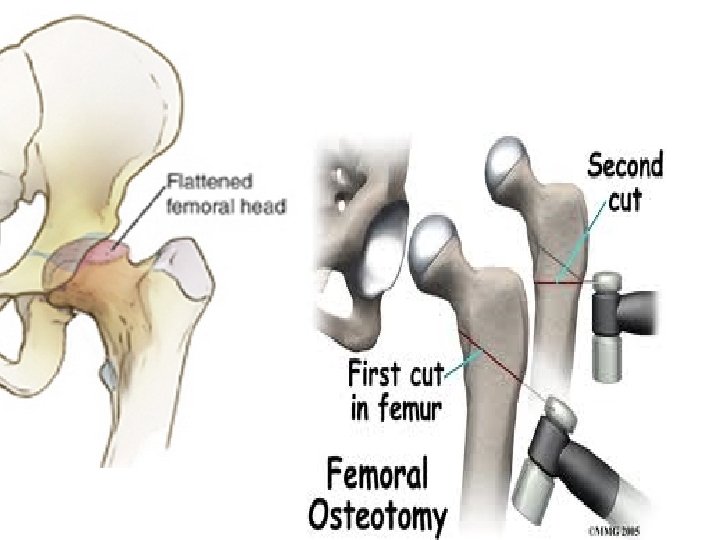
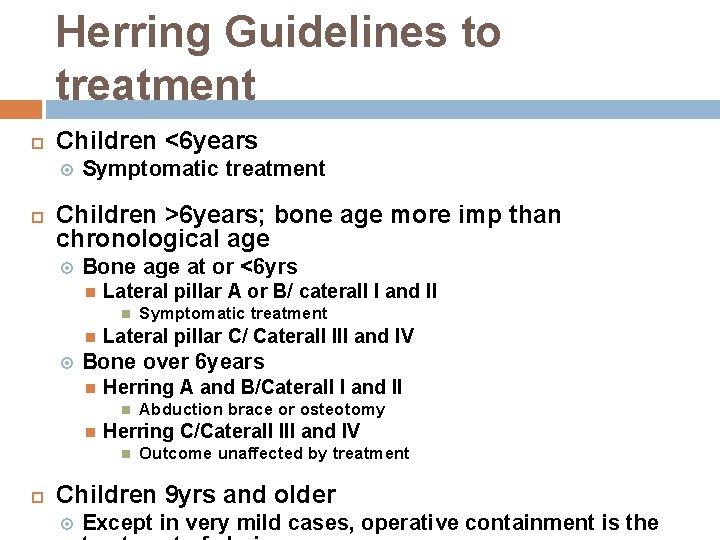
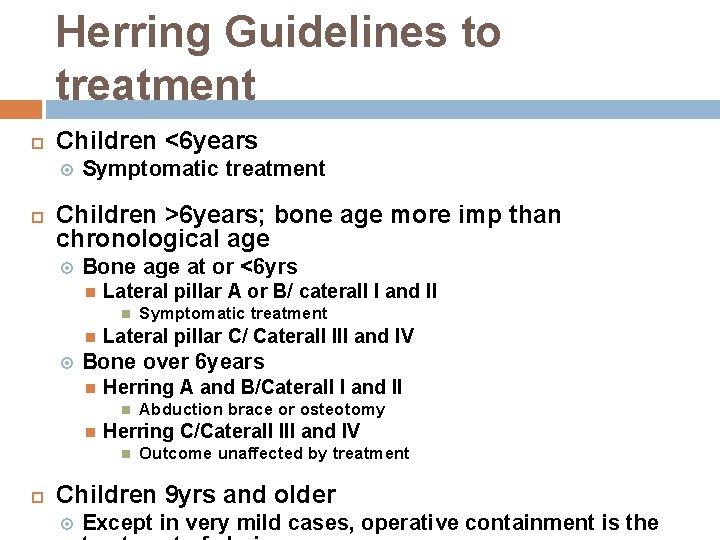
Herring Guidelines to treatment Children <6 years Symptomatic treatment Children >6 years; bone age more imp than chronological age Bone age at or <6 yrs Lateral pillar A or B/ caterall I and II Lateral pillar C/ Caterall III and IV Bone over 6 years Herring A and B/Caterall I and II Abduction brace or osteotomy Herring C/Caterall III and IV Symptomatic treatment Outcome unaffected by treatment Children 9 yrs and older Except in very mild cases, operative containment is the
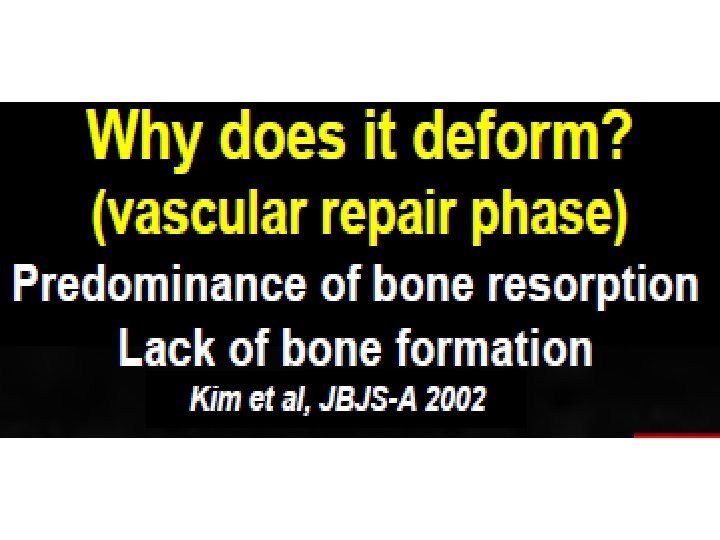
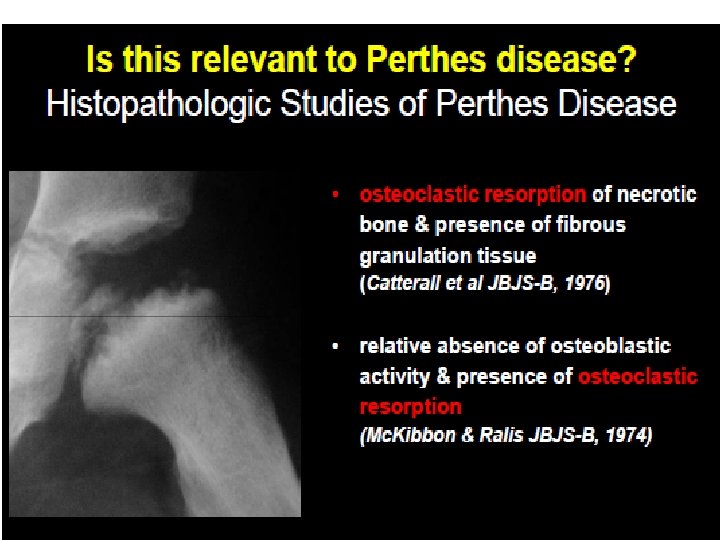
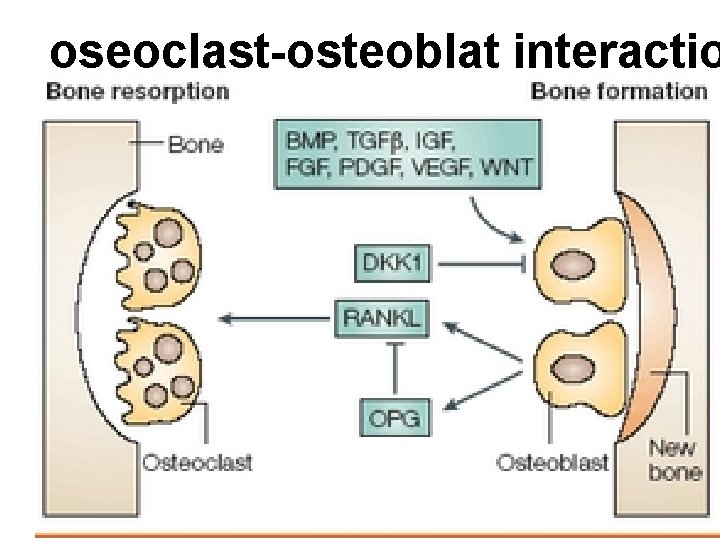
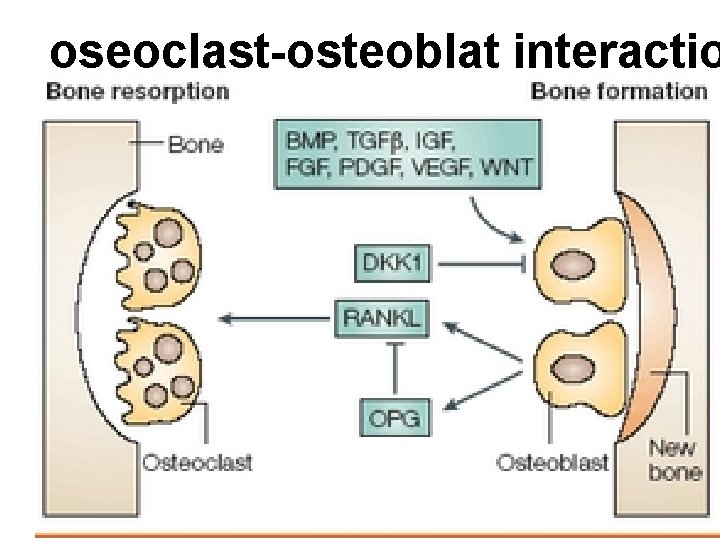
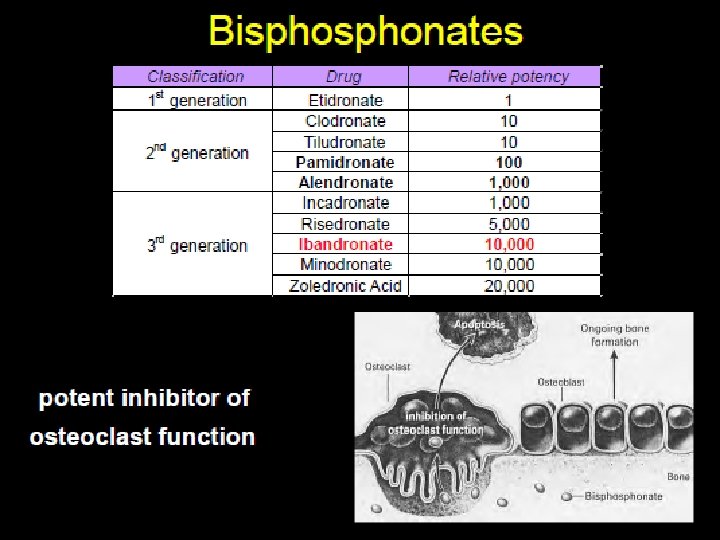
oseoclast-osteoblat interactio
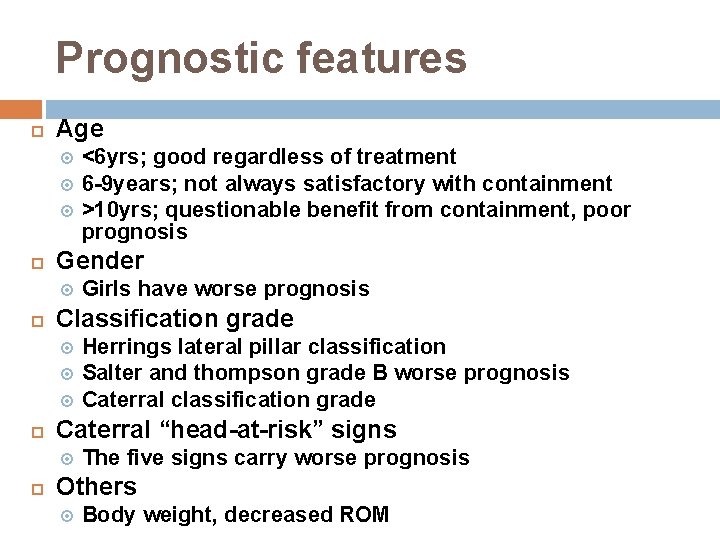
Prognostic features Age Gender Herrings lateral pillar classification Salter and thompson grade B worse prognosis Caterral classification grade Caterral “head-at-risk” signs Girls have worse prognosis Classification grade <6 yrs; good regardless of treatment 6 -9 years; not always satisfactory with containment >10 yrs; questionable benefit from containment, poor prognosis The five signs carry worse prognosis Others Body weight, decreased ROM
 Legg calve perthes disease vs scfe
Legg calve perthes disease vs scfe Osteoblat
Osteoblat Perthes disease
Perthes disease Perthes vs sufe
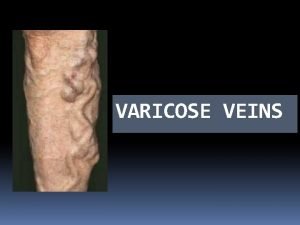
Perthes vs sufe Sindrome di cockett
Sindrome di cockett Perthes vs sufe
Perthes vs sufe Morrissey cough impulse
Morrissey cough impulse Kalça abduksiyonu
Kalça abduksiyonu Calve legg perthes hund
Calve legg perthes hund Presenters name
Presenters name Calender presenters
Calender presenters Job title example
Job title example Presenters name
Presenters name Name of presenter
Name of presenter Atv presenters
Atv presenters Famous british tv presenters
Famous british tv presenters Presenters name
Presenters name Thank you to all presenters
Thank you to all presenters Michael henderson monash
Michael henderson monash Communicable disease and non communicable disease
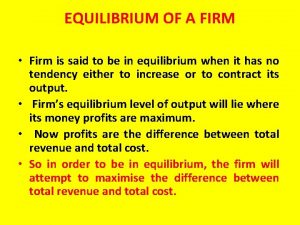
Communicable disease and non communicable disease Money management decisions attempt to manage a firm's
Money management decisions attempt to manage a firm's Best milk a typical profit-maximizing dairy firm
Best milk a typical profit-maximizing dairy firm Why this firm
Why this firm 4 firm concentration ratio
4 firm concentration ratio Kreowanie wizerunku przedsiębiorstwa w otoczeniu
Kreowanie wizerunku przedsiębiorstwa w otoczeniu Dominant firm with a competitive fringe
Dominant firm with a competitive fringe Fs law
Fs law International trade theory
International trade theory Evaluating a firm’s internal capabilities
Evaluating a firm’s internal capabilities Valuation and capital budgeting for the levered firm
Valuation and capital budgeting for the levered firm Therefore my dear brothers stand firm
Therefore my dear brothers stand firm Konto direct
Konto direct Theory of the firm managerial behavior
Theory of the firm managerial behavior Moral overconfidence
Moral overconfidence Explicit costs are payments the firm makes for
Explicit costs are payments the firm makes for Chip cosse law firm
Chip cosse law firm Law firm risk management manual
Law firm risk management manual Value centric appraisals
Value centric appraisals Minder grinder finder
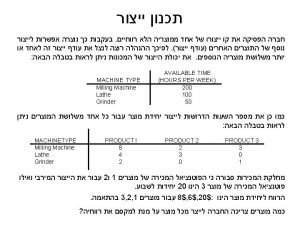
Minder grinder finder A firm is planning to manufacture a new product
A firm is planning to manufacture a new product Vertical boundaries of the firm
Vertical boundaries of the firm The firm author
The firm author Exemplifies the complexity of relationships
Exemplifies the complexity of relationships Duopoly
Duopoly Best law firm websites 2013
Best law firm websites 2013