Joint Hospital Surgical Grandround Management of Toxic Multinodular
- Slides: 25
Joint Hospital Surgical Grandround Management of Toxic Multinodular Goiter - Role of surgery Shi LAM Queen Mary Hospital
“. . two distinct types of thyroid intoxication…” – H. S Plummer 1913 n Hyperplastic (Grave’s) n Non-hyperplastic (Plummer’s) n n Solitary toxic nodule n Toxic multinodular goiter Two major causes (> 80%) of hyperthyroidism worldwide
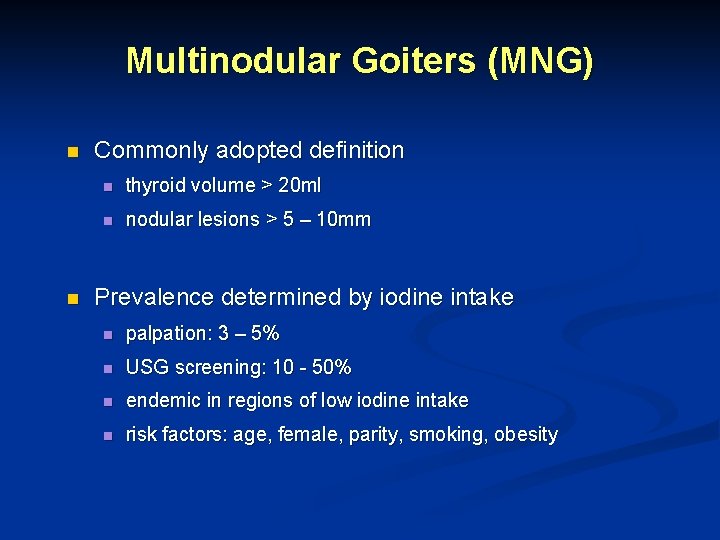
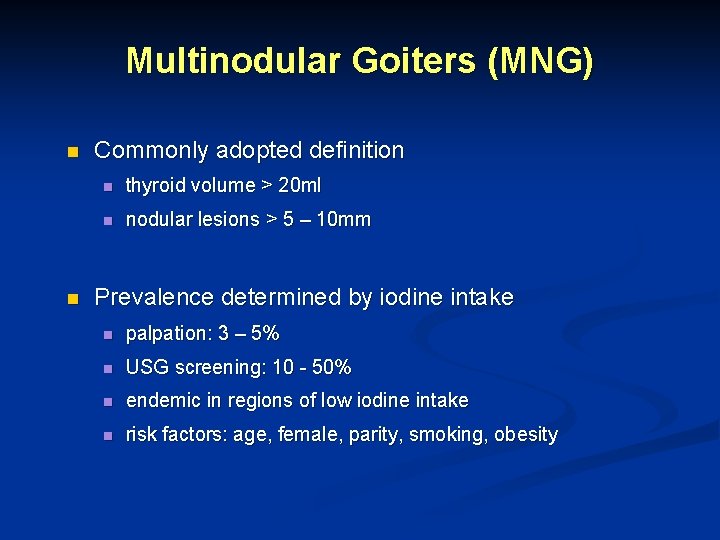
Multinodular Goiters (MNG) n n Commonly adopted definition n thyroid volume > 20 ml n nodular lesions > 5 – 10 mm Prevalence determined by iodine intake n palpation: 3 – 5% n USG screening: 10 - 50% n endemic in regions of low iodine intake n risk factors: age, female, parity, smoking, obesity
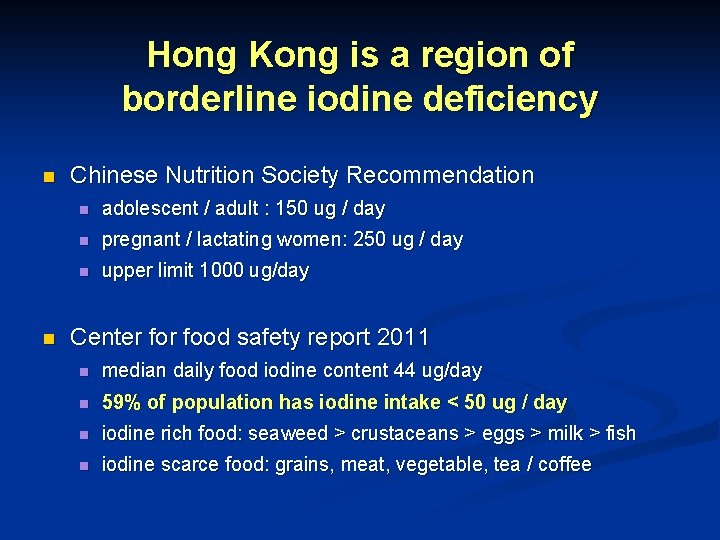
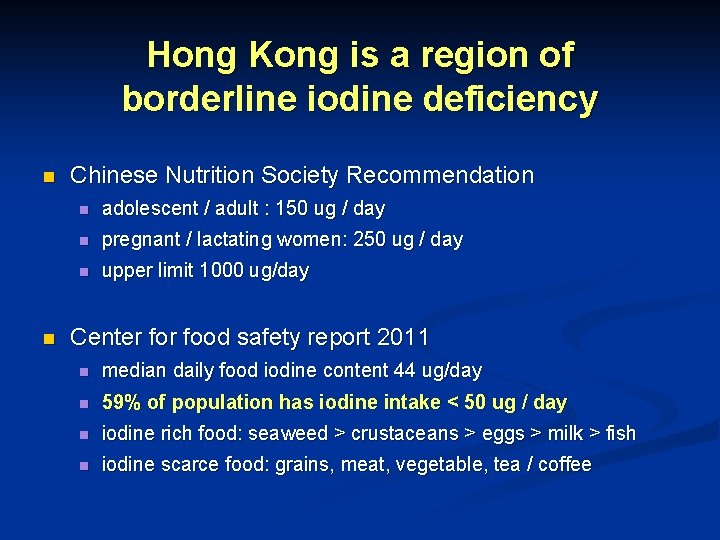
Hong Kong is a region of borderline iodine deficiency n n Chinese Nutrition Society Recommendation n adolescent / adult : 150 ug / day n pregnant / lactating women: 250 ug / day n upper limit 1000 ug/day Center food safety report 2011 n median daily food iodine content 44 ug/day n 59% of population has iodine intake < 50 ug / day n iodine rich food: seaweed > crustaceans > eggs > milk > fish n iodine scarce food: grains, meat, vegetable, tea / coffee
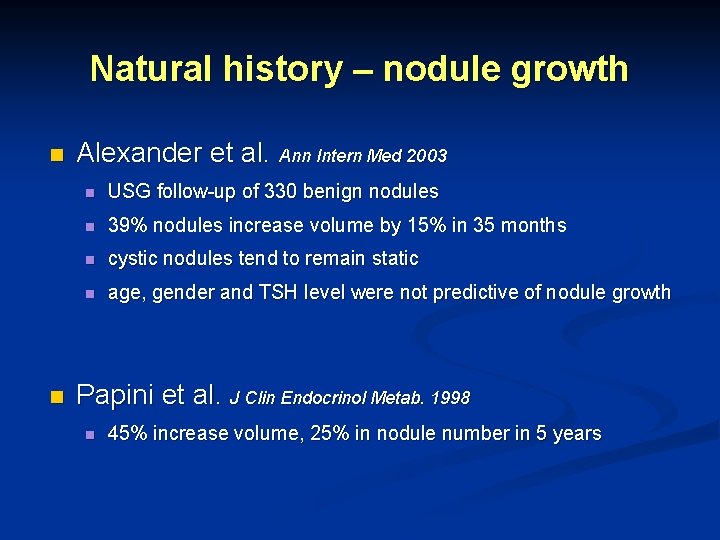
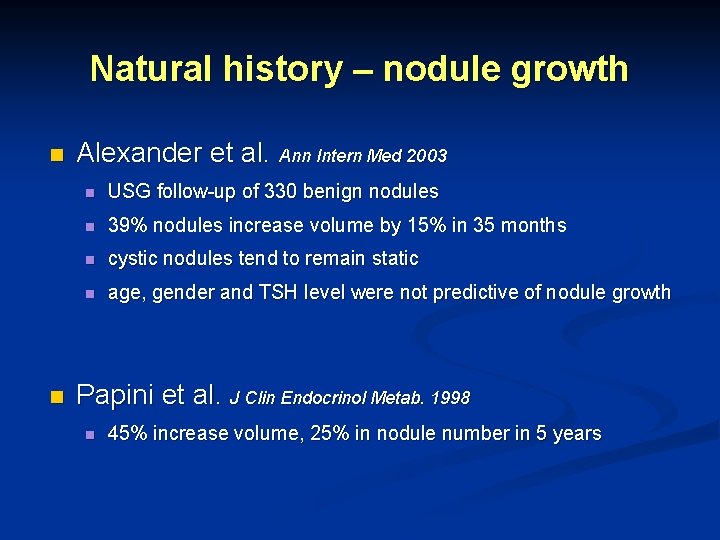
Natural history – nodule growth n n Alexander et al. Ann Intern Med 2003 n USG follow-up of 330 benign nodules n 39% nodules increase volume by 15% in 35 months n cystic nodules tend to remain static n age, gender and TSH level were not predictive of nodule growth Papini et al. J Clin Endocrinol Metab. 1998 n 45% increase volume, 25% in nodule number in 5 years
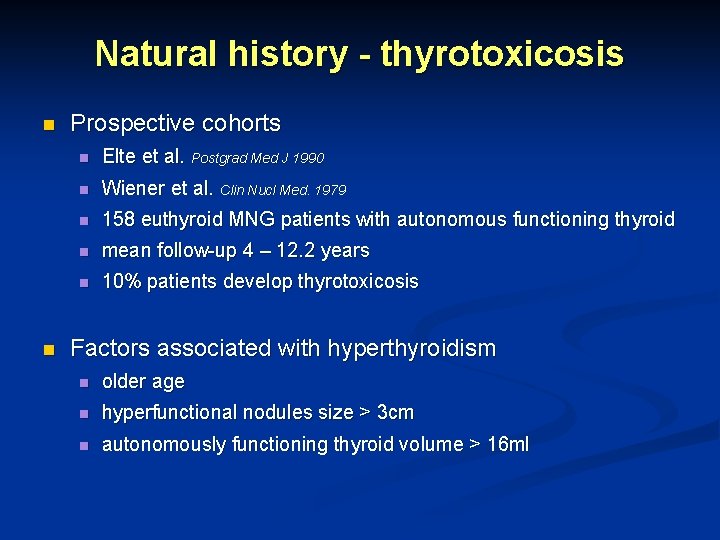
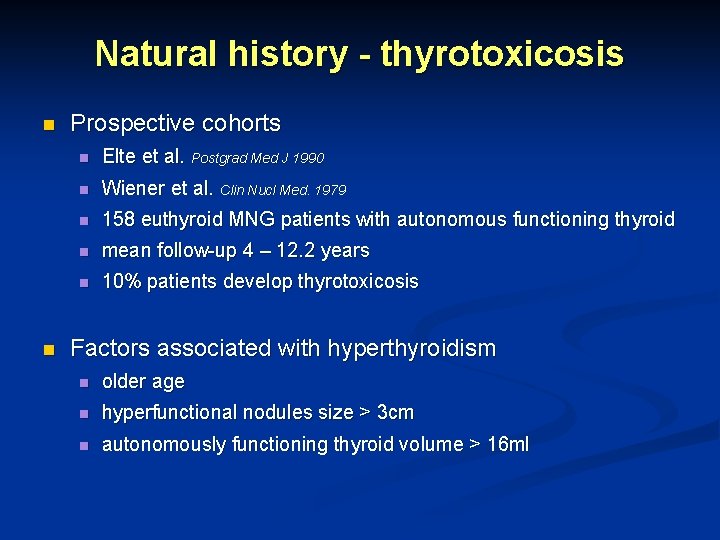
Natural history - thyrotoxicosis n n Prospective cohorts n Elte et al. Postgrad Med J 1990 n Wiener et al. Clin Nucl Med. 1979 n 158 euthyroid MNG patients with autonomous functioning thyroid n mean follow-up 4 – 12. 2 years n 10% patients develop thyrotoxicosis Factors associated with hyperthyroidism n older age n hyperfunctional nodules size > 3 cm n autonomously functioning thyroid volume > 16 ml
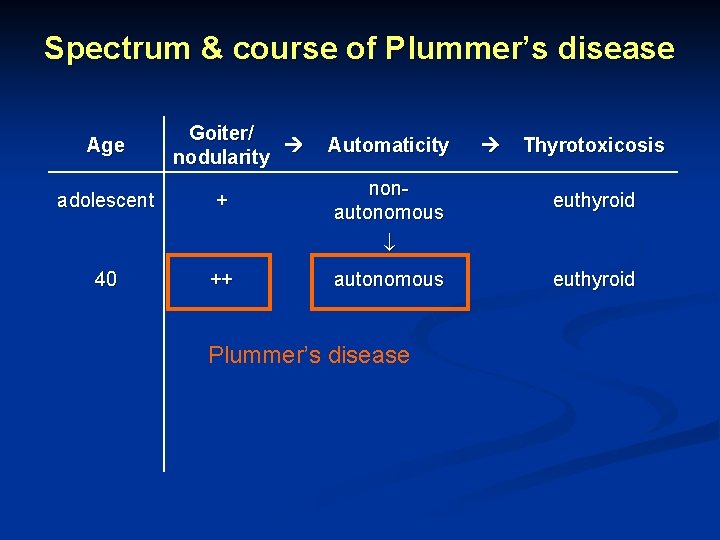
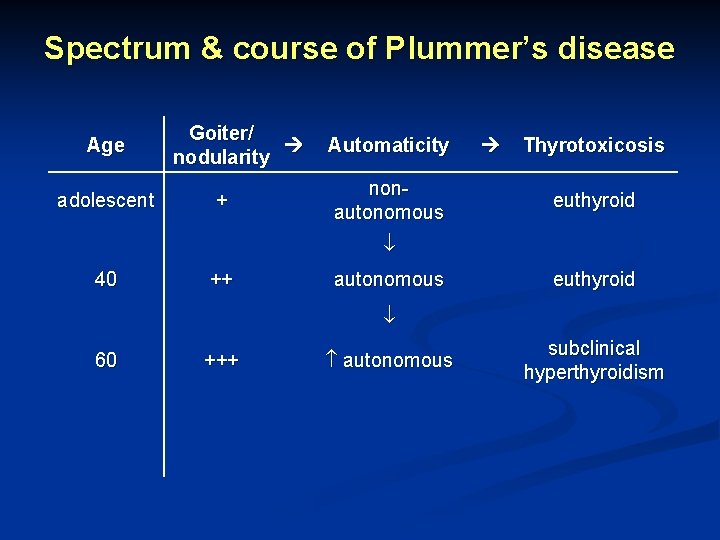
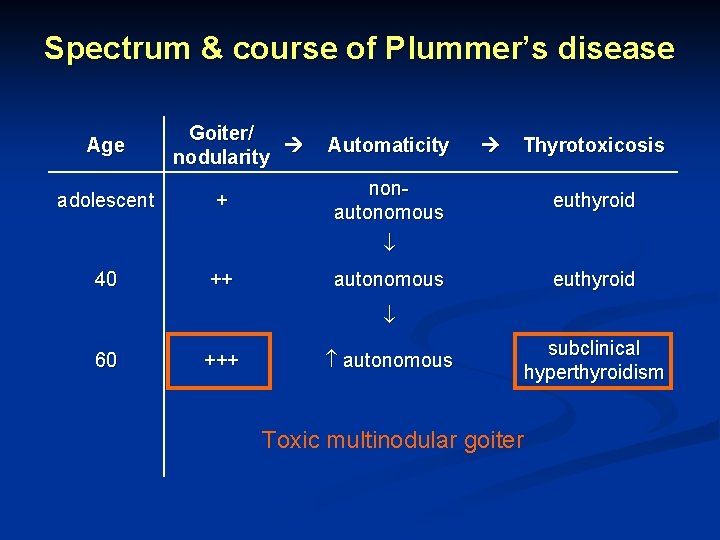
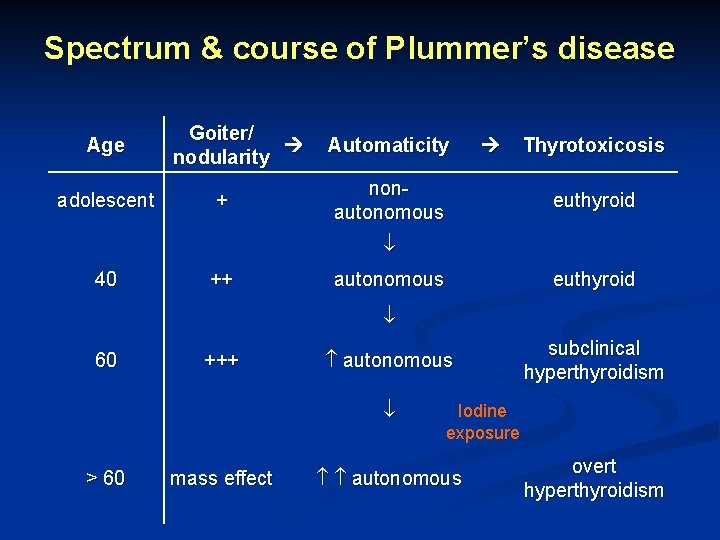
Spectrum & course of Plummer’s disease Age Goiter/ nodularity
Spectrum & course of Plummer’s disease Age Goiter/ nodularity Automaticity
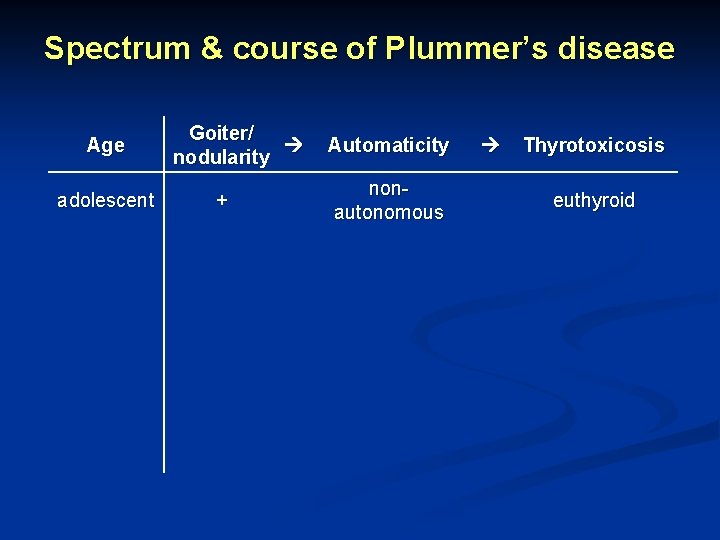
Spectrum & course of Plummer’s disease Age Goiter/ nodularity Automaticity Thyrotoxicosis
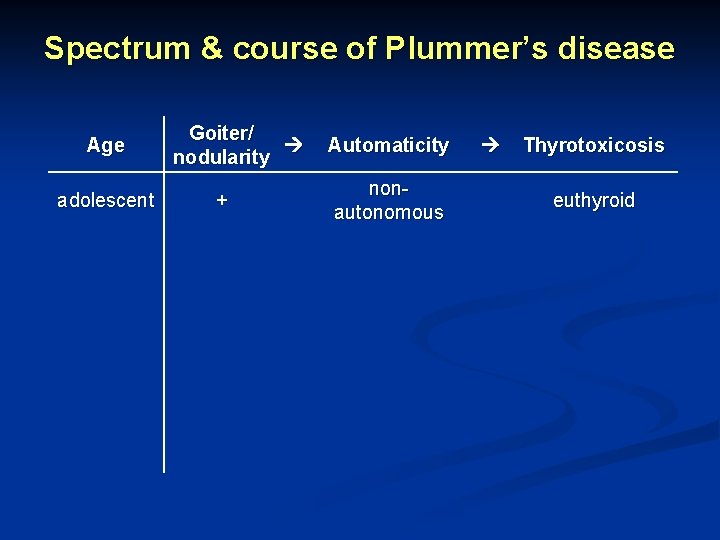
Spectrum & course of Plummer’s disease Age adolescent Goiter/ nodularity + Automaticity nonautonomous Thyrotoxicosis euthyroid
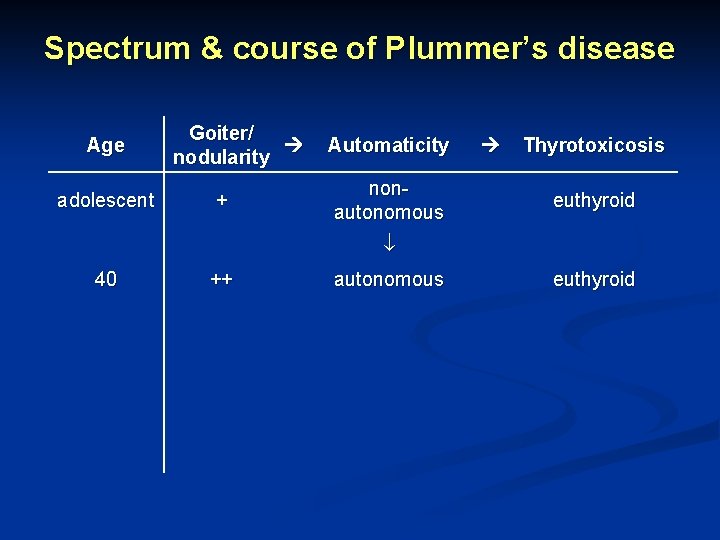
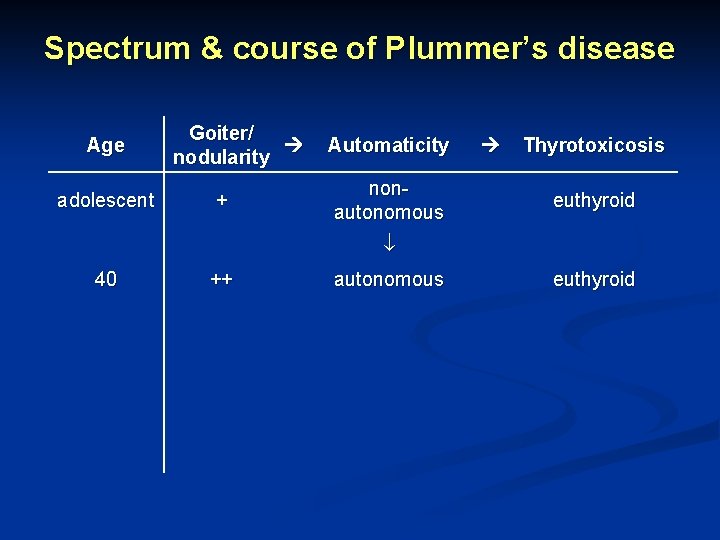
Spectrum & course of Plummer’s disease Age adolescent Goiter/ nodularity + Automaticity nonautonomous Thyrotoxicosis euthyroid 40 ++ autonomous euthyroid
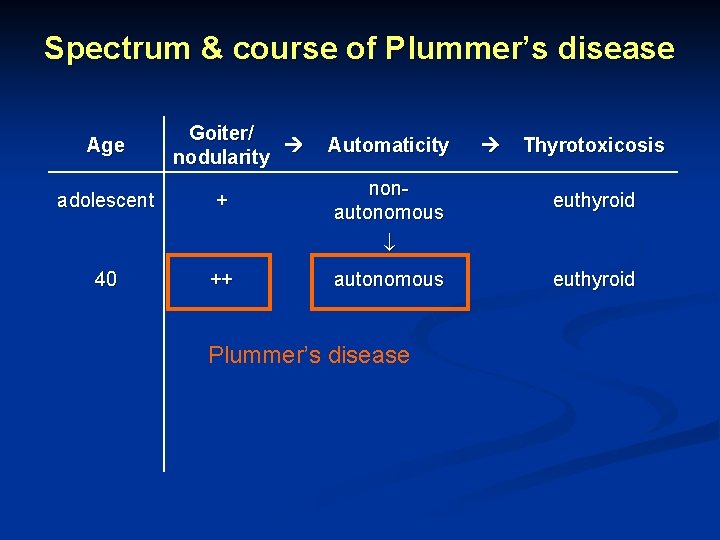
Spectrum & course of Plummer’s disease Age adolescent Goiter/ nodularity + Automaticity nonautonomous Thyrotoxicosis euthyroid 40 ++ autonomous Plummer’s disease euthyroid
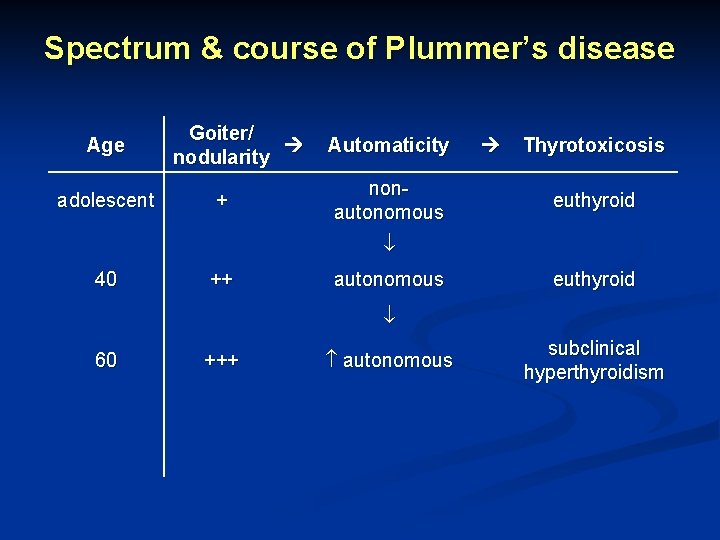
Spectrum & course of Plummer’s disease Age adolescent Goiter/ nodularity + Automaticity nonautonomous Thyrotoxicosis euthyroid 40 ++ autonomous euthyroid 60 +++ autonomous subclinical hyperthyroidism
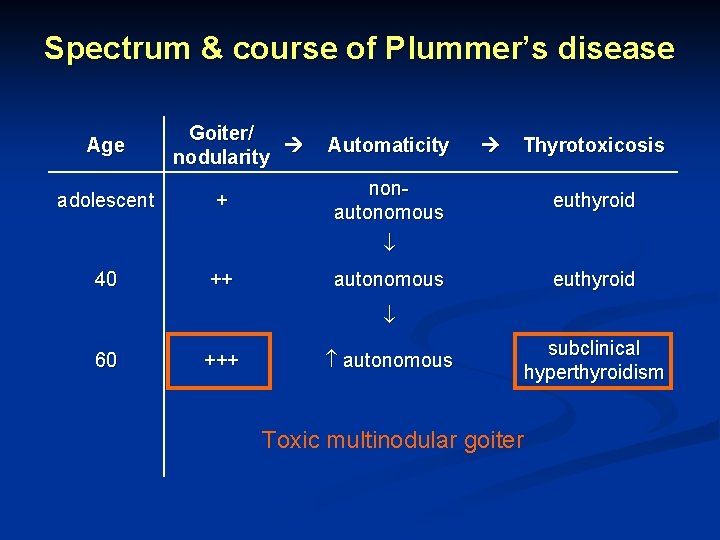
Spectrum & course of Plummer’s disease Age adolescent Goiter/ nodularity + Automaticity Thyrotoxicosis nonautonomous euthyroid 40 ++ autonomous euthyroid 60 +++ autonomous subclinical hyperthyroidism Toxic multinodular goiter
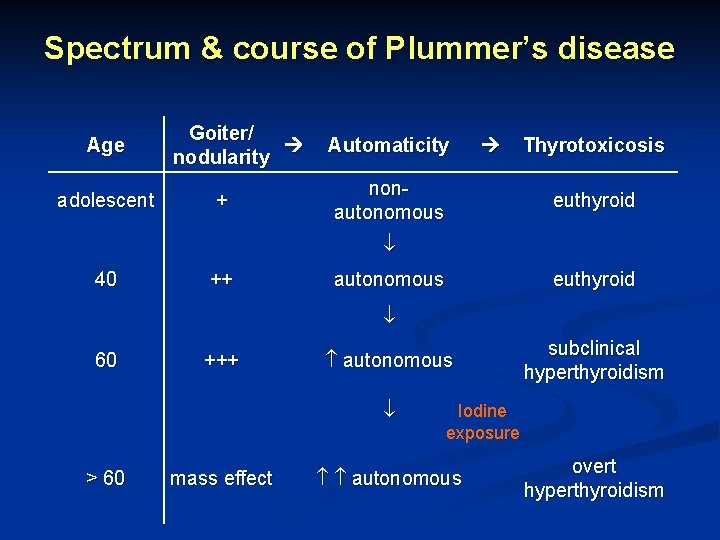
Spectrum & course of Plummer’s disease Age adolescent Goiter/ nodularity + Automaticity nonautonomous Thyrotoxicosis euthyroid 40 ++ autonomous euthyroid 60 +++ autonomous > 60 mass effect subclinical hyperthyroidism Iodine exposure autonomous overt hyperthyroidism
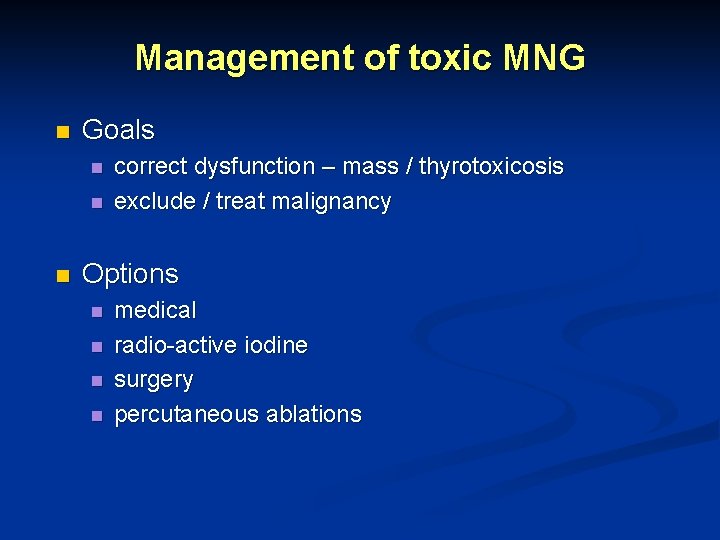
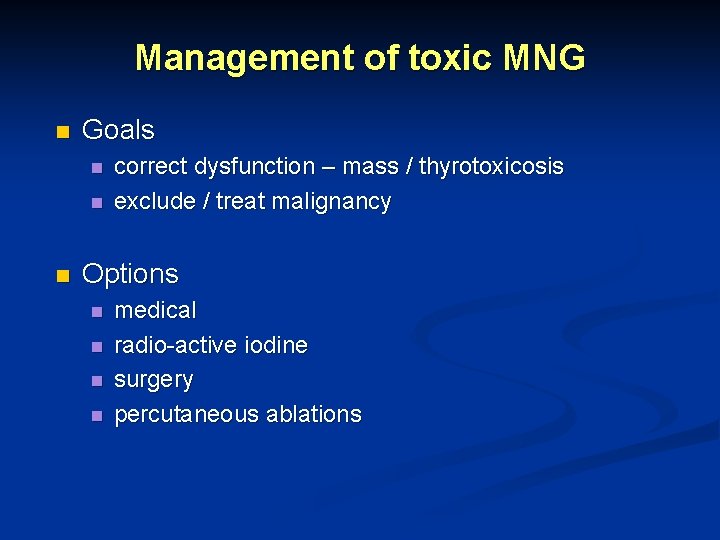
Management of toxic MNG n Goals n n n correct dysfunction – mass / thyrotoxicosis exclude / treat malignancy Options n n medical radio-active iodine surgery percutaneous ablations
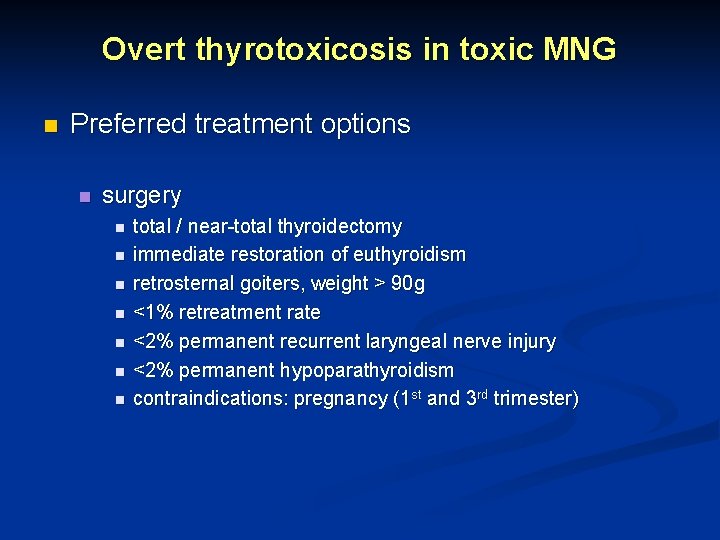
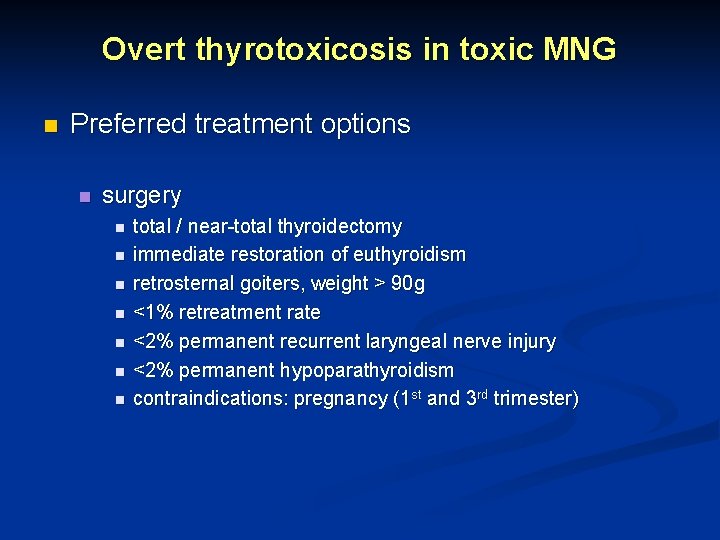
Overt thyrotoxicosis in toxic MNG n Preferred treatment options n surgery n n n n total / near-total thyroidectomy immediate restoration of euthyroidism retrosternal goiters, weight > 90 g <1% retreatment rate <2% permanent recurrent laryngeal nerve injury <2% permanent hypoparathyroidism contraindications: pregnancy (1 st and 3 rd trimester)
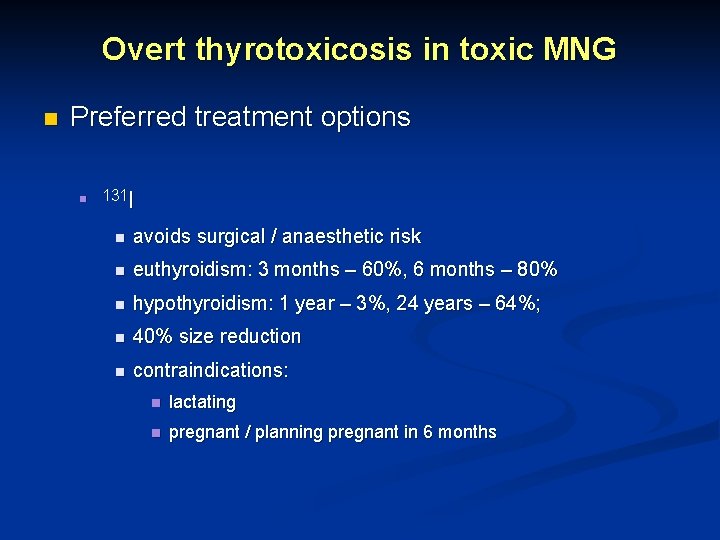
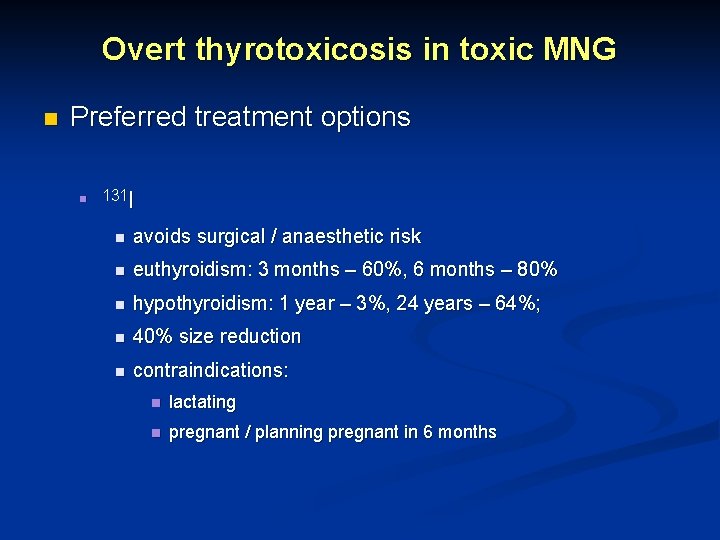
Overt thyrotoxicosis in toxic MNG n Preferred treatment options n 131 I n avoids surgical / anaesthetic risk n euthyroidism: 3 months – 60%, 6 months – 80% n hypothyroidism: 1 year – 3%, 24 years – 64%; n 40% size reduction n contraindications: n lactating n pregnant / planning pregnant in 6 months
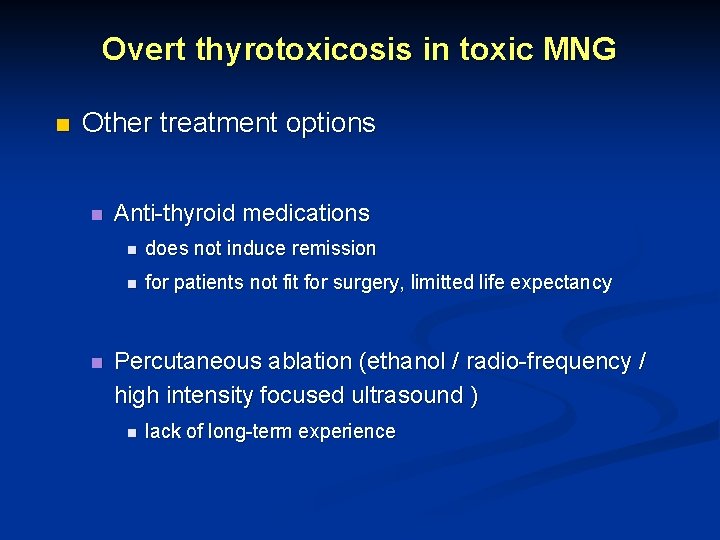
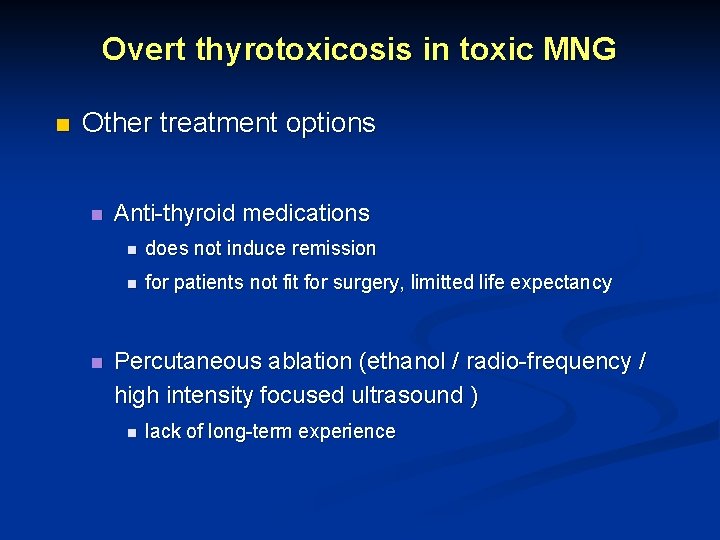
Overt thyrotoxicosis in toxic MNG n Other treatment options n n Anti-thyroid medications n does not induce remission n for patients not fit for surgery, limitted life expectancy Percutaneous ablation (ethanol / radio-frequency / high intensity focused ultrasound ) n lack of long-term experience
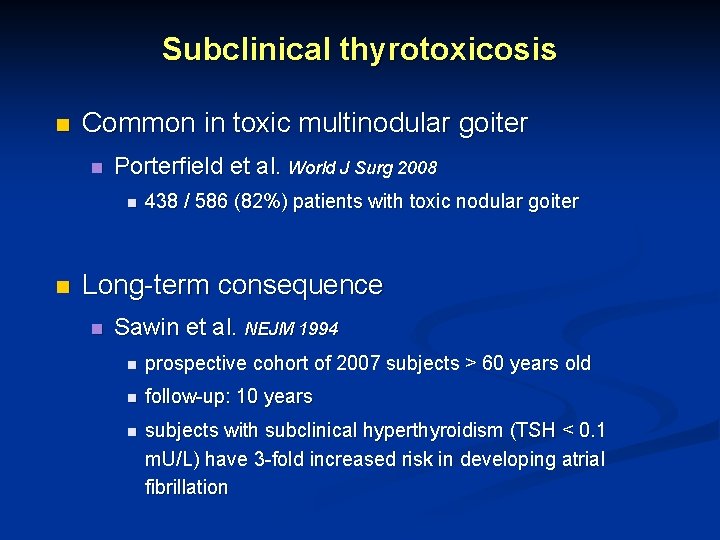
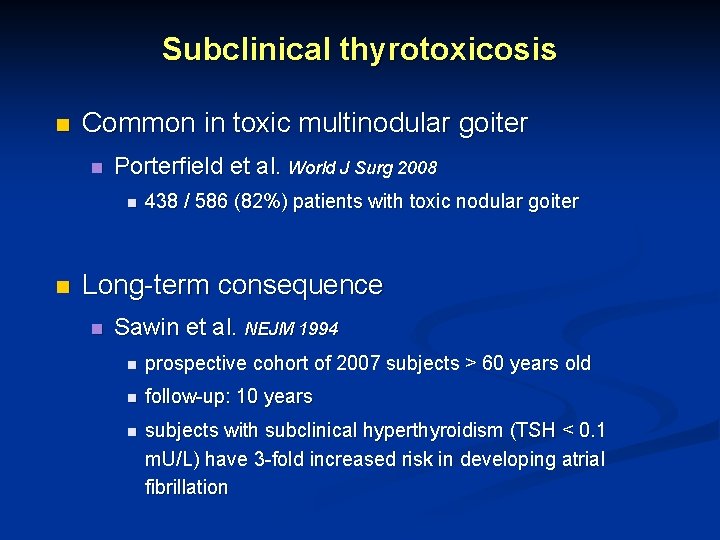
Subclinical thyrotoxicosis n Common in toxic multinodular goiter n Porterfield et al. World J Surg 2008 n n 438 / 586 (82%) patients with toxic nodular goiter Long-term consequence n Sawin et al. NEJM 1994 n prospective cohort of 2007 subjects > 60 years old n follow-up: 10 years n subjects with subclinical hyperthyroidism (TSH < 0. 1 m. U/L) have 3 -fold increased risk in developing atrial fibrillation
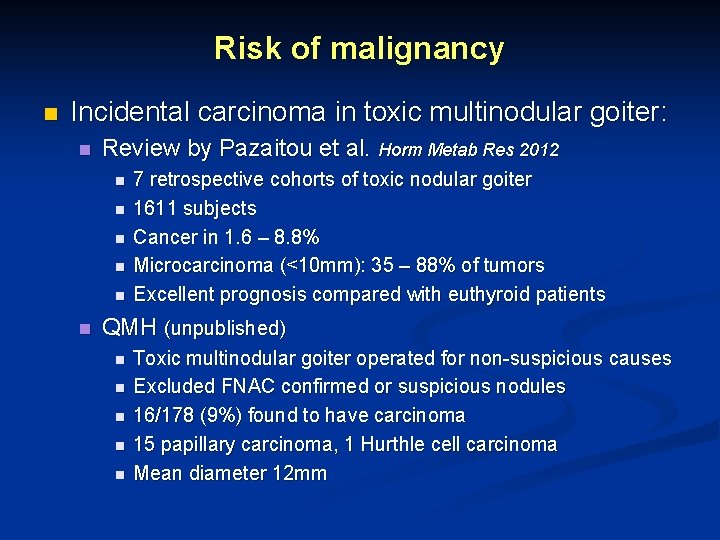
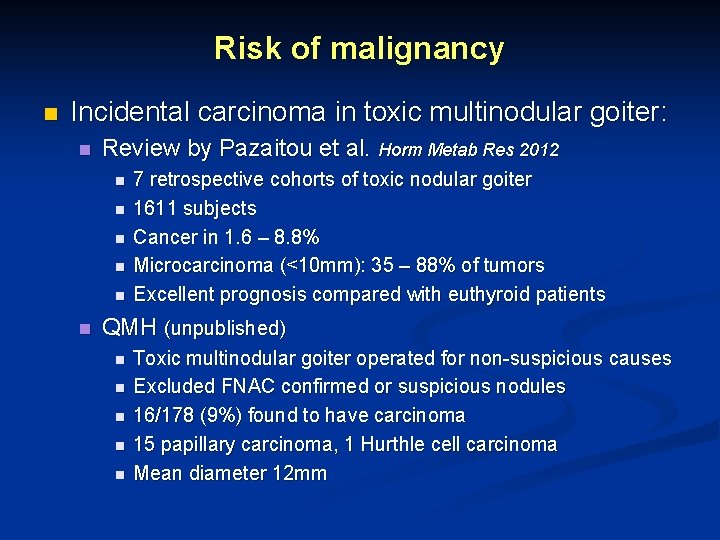
Risk of malignancy n Incidental carcinoma in toxic multinodular goiter: n Review by Pazaitou et al. Horm Metab Res 2012 n n n 7 retrospective cohorts of toxic nodular goiter 1611 subjects Cancer in 1. 6 – 8. 8% Microcarcinoma (<10 mm): 35 – 88% of tumors Excellent prognosis compared with euthyroid patients QMH (unpublished) n n n Toxic multinodular goiter operated for non-suspicious causes Excluded FNAC confirmed or suspicious nodules 16/178 (9%) found to have carcinoma 15 papillary carcinoma, 1 Hurthle cell carcinoma Mean diameter 12 mm
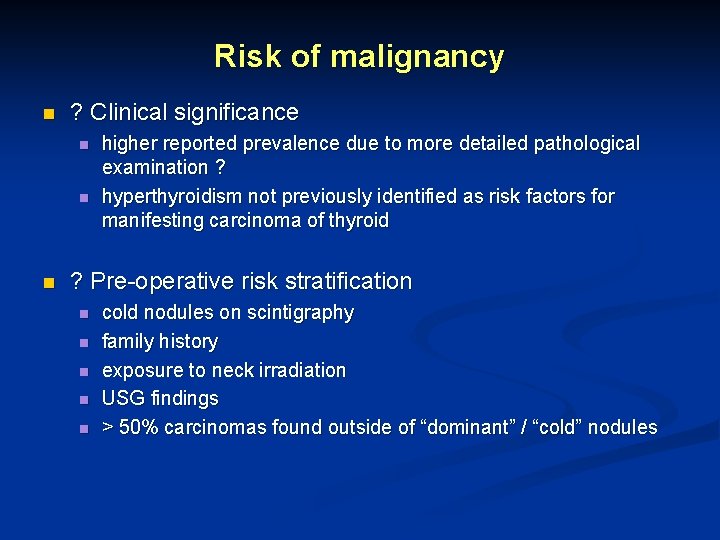
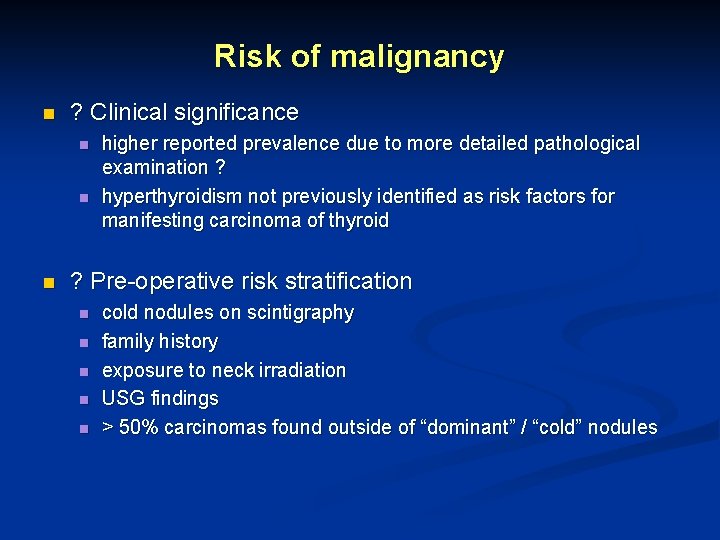
Risk of malignancy n ? Clinical significance n n n higher reported prevalence due to more detailed pathological examination ? hyperthyroidism not previously identified as risk factors for manifesting carcinoma of thyroid ? Pre-operative risk stratification n n cold nodules on scintigraphy family history exposure to neck irradiation USG findings > 50% carcinomas found outside of “dominant” / “cold” nodules
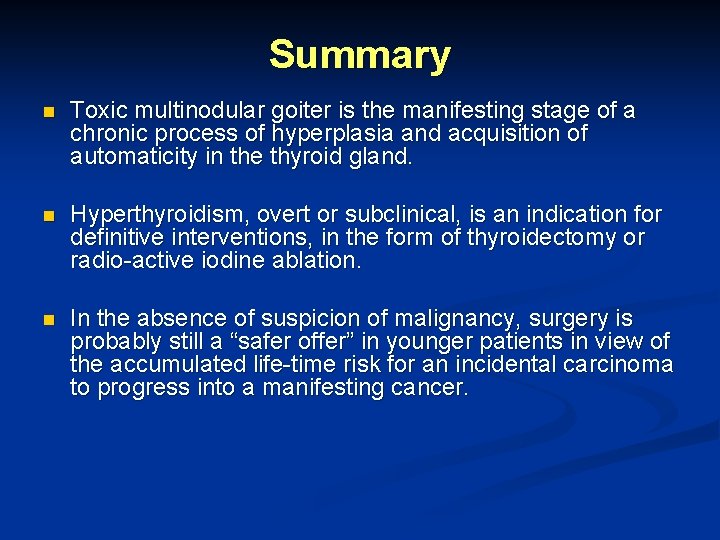
Summary n Toxic multinodular goiter is the manifesting stage of a chronic process of hyperplasia and acquisition of automaticity in the thyroid gland. n Hyperthyroidism, overt or subclinical, is an indication for definitive interventions, in the form of thyroidectomy or radio-active iodine ablation. n In the absence of suspicion of malignancy, surgery is probably still a “safer offer” in younger patients in view of the accumulated life-time risk for an incidental carcinoma to progress into a manifesting cancer.
Acknowledgement Dr. Brian Lang
Thank you!
 What causes central hypothyroidism
What causes central hypothyroidism Multinodular goiter pathophysiology
Multinodular goiter pathophysiology Tmh
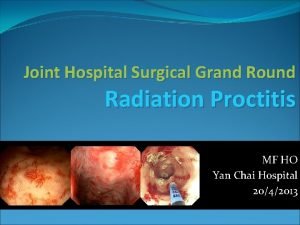
Tmh Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Joint hospital surgical grand round
Joint hospital surgical grand round Esophgeal varices
Esophgeal varices Joint hospital surgical grand round
Joint hospital surgical grand round Conclusion of oral medication
Conclusion of oral medication Primary vs secondary thyrotoxicosis
Primary vs secondary thyrotoxicosis Multinodular goiter
Multinodular goiter Multinodular goiter causes
Multinodular goiter causes Wellspan surgical and rehab hospital
Wellspan surgical and rehab hospital Broad-based disc bulge
Broad-based disc bulge Management of toxic megacolon
Management of toxic megacolon Requirement of pharmacist in hospital
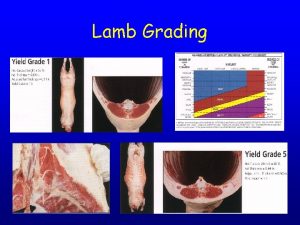
Requirement of pharmacist in hospital Spool joint vs break joint
Spool joint vs break joint Cartilage between vertebrae
Cartilage between vertebrae Semi permanent joints
Semi permanent joints Appretaite
Appretaite Lamb grading chart
Lamb grading chart Ellipsoid joint
Ellipsoid joint Padilla
Padilla Toxic waste dump problem voronoi
Toxic waste dump problem voronoi Aspartate-argininosuccinate shunt
Aspartate-argininosuccinate shunt What is the toxic trio
What is the toxic trio