Multinodular goiter Agenda Definition and gross pathology Epidemiology














- Slides: 46

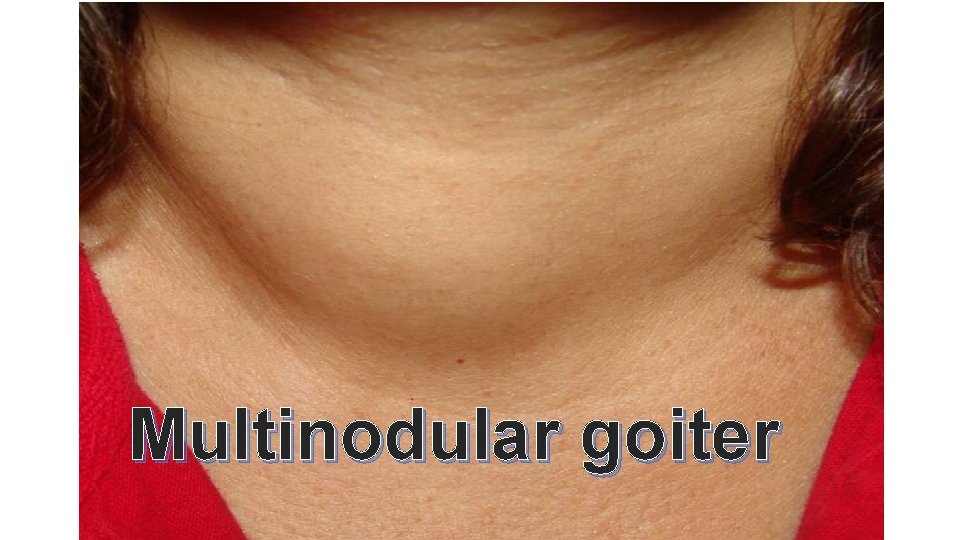
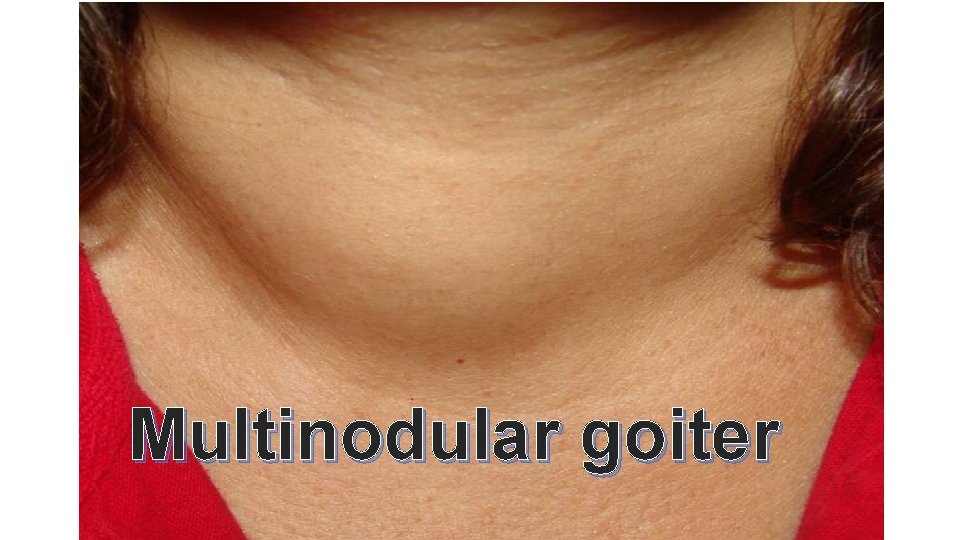
Multinodular goiter
Agenda Definition and gross pathology Epidemiology Pathogenesis Clinical presentation Clinical evaluation & investigation Treatment Conclusion
Definition Clinicopathological entity characterized by an increased volume of the thyroid gland with formation of nodules Goiter is defined as a thyroid gland w. t > 20 -25 g or a volume of over 19 ml in women and 25 ml in men Grossly nodules are discrete lesions: solid and/or cystic A solid nodule can be adenoma, containing capsule, or more commonly a hyperplastic nodule, without capsule Cystic lesions can be colloid cysts or hemorrhagic cyst Not associated with overt hypo or hyperthyroidism & not Resulted from inflammation or neoplasia
Agenda Definition and gross pathology Epidemiology Pathogenesis Clinical presentation Clinical evaluation & investigation Treatment Conclusion
Epidemiology • Prevalence is 5% by palpation • Prevalence is 50% by US • Annual incidence is 0. 1% which means 350, 000 new nodules in U. S. in 2014 • >600, 000 FNAs per yr • More common in women, in elderly, with I-deficiency and after radiation • 95% are benign

Agenda Definition and gross pathology Epidemiology Pathogenesis Clinical presentation Clinical evaluation & investigation Treatment Conclusion
Pathogenesis Diffuse follicular hyperplasia, focal nodular proliferation & Finally Functional automaticity Long-term exposure of the thyroid gland to proliferative Stimuli (iodine deficiency, goitrogens and inborn error of thyroid Hormone synthesis) results in insufficient thyroid Hormone Production and Stimulate TSH secretion which Results in enlargement of thyroid Gland, increased radio-Iodine uptake and increased T 4 and T 3 levels Nodule formation result of inherent & acquired heterogeneity in proliferative and functional upregulation of The follicular cells Follicular cells acquiring activating somatic mutations in the Cell proliferation can expand clonally to form a nodule.
Agenda Definition and gross pathology Epidemiology Pathogenesis Clinical presentation Clinical evaluation & investigation Treatment Conclusion
Clinical Presentation variable depends on the size, location, and thyroid function Asymptomatic long-standing visible goiter Hyperthyroidism(25% ) substernal goiter obstruction or pressure exertional or positional dyspnea dysphagia , cough, choking sensation, or hoarseness
Agenda Definition and gross pathology Epidemiology Pathogenesis Clinical presentation Clinical evaluation & investigation Treatment Conclusion
Clinical evaluation & investigation History & physical examination Serum TSH Ultrasonography Thyroid scintigraphy FNA
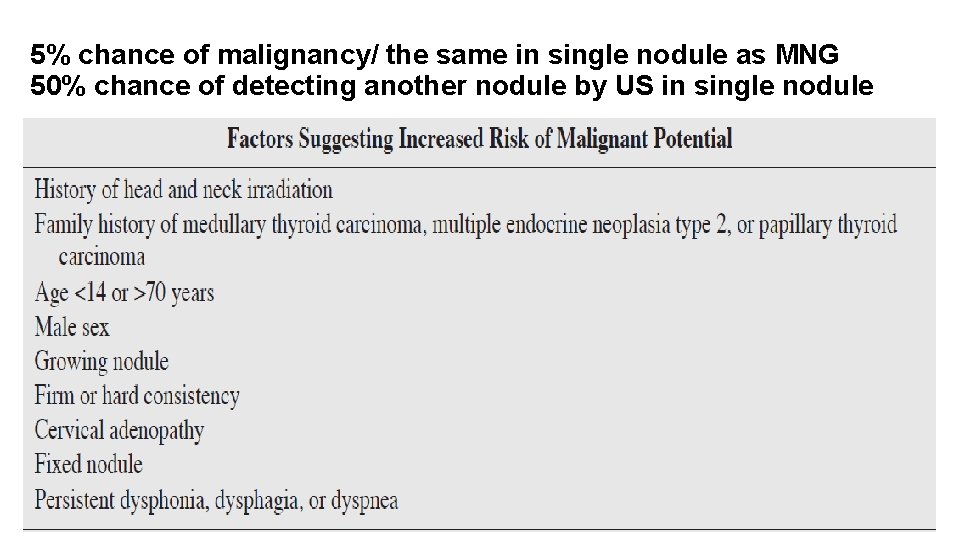
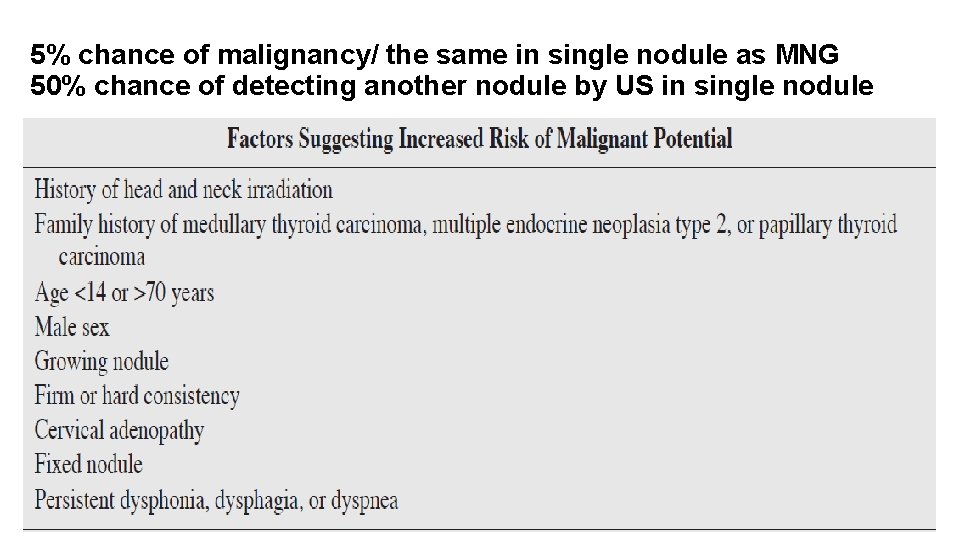
5% chance of malignancy/ the same in single nodule as MNG 50% chance of detecting another nodule by US in single nodule
Serum TSH Patients with nodular goiter should have a complete history and Physical exam, and serum TSH levels should be measured (Rec. 1 -A) If low, a thyroid scintigraphy (using either technetium 99 m. Tc Pertechnetate or 123 I) should be performed Low serum levels of TSH suggest overt or subclinical hyperthyroidism And presence of hyperfunctioning (“hot”) nodules(Rec. 1 -A) “Hot” nodules need not FNA Serum TSH levels are an independent predictor of malignancy Associated with a more advanced stage of the disease
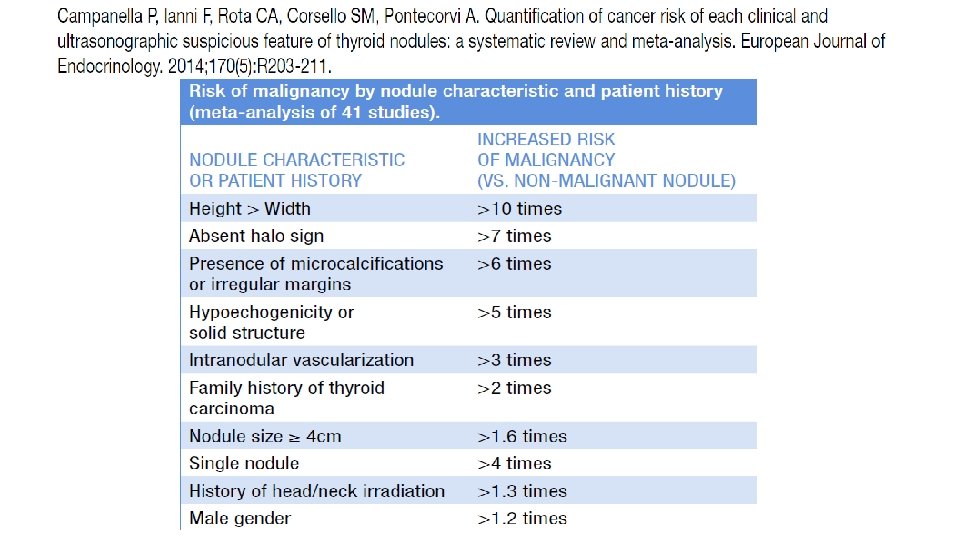
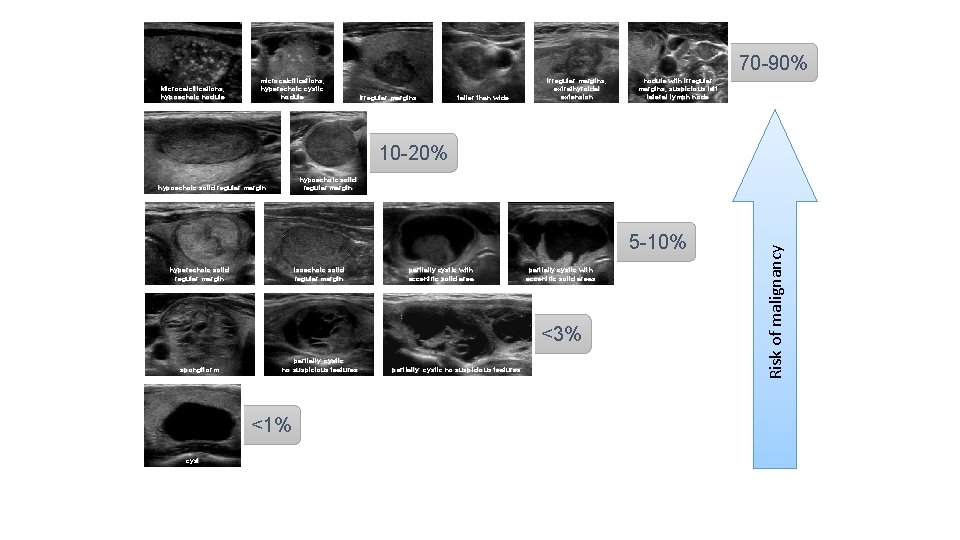
Sonography Current US technology using high resolution transducers is the most Sensitive method available (approaching 95%) and is capable of Detecting nodules as small as 1– 2 mm All pts with thyroid nodules should be evaluated with US (Rec. 2 -A) To confirm the presence of a mass, assess whether the lesion is Single or multiple, determine thyroidal origin, and guide FNA biopsy Up to 50% of patients with a single palpable thyroid nodule Will demonstrate additional nodules when US exam is performed Certain ultrasonographic features associated with increased risk of Malignancy include nodule hypoechogenicity, microcalcifications, Increased vascular flow, irregular borders, and the absence of a halo When present, nodules should be preferentially aspirated(Rec. 12 a-B)
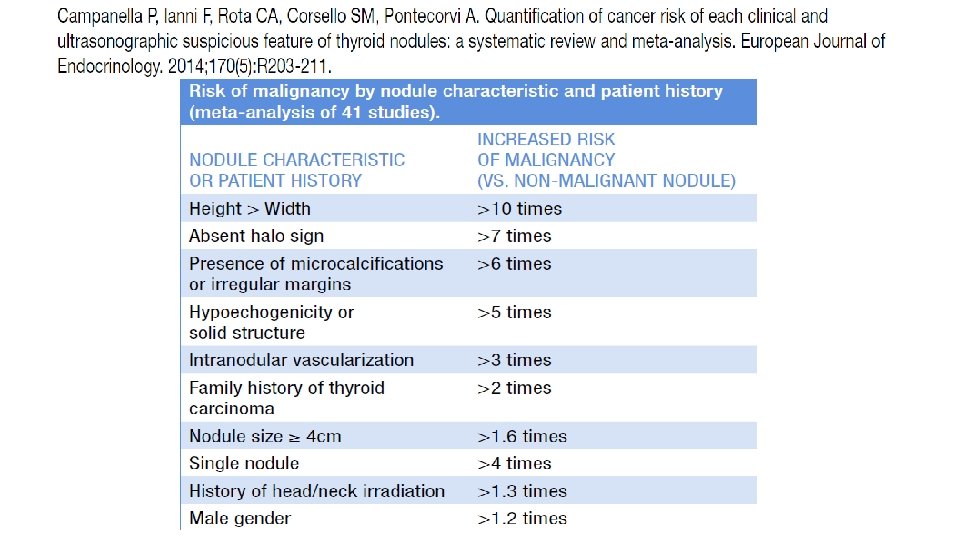
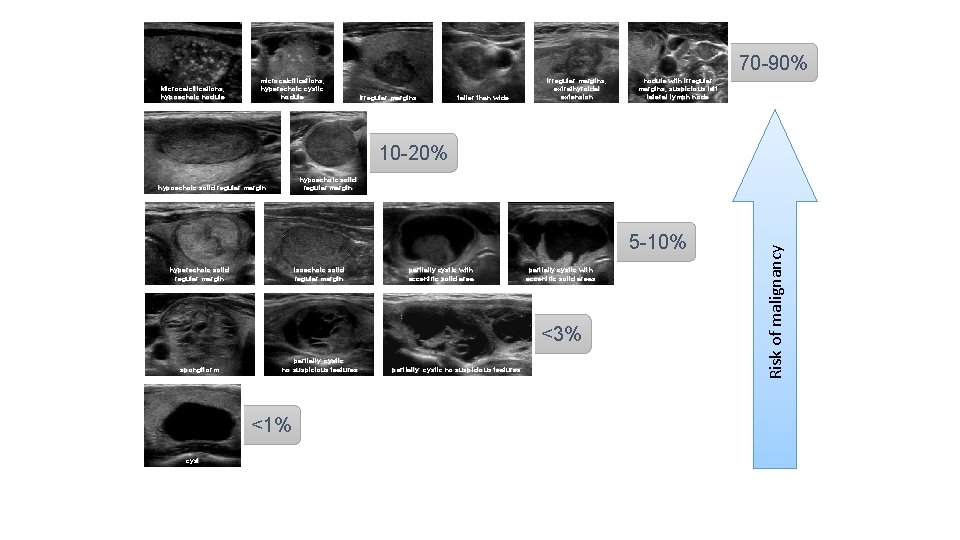
70 -90% Microcalcifications, hypoechoic nodule microcalcifications, hyperechoic cystic nodule irregular margins taller than wide irregular margins, extrathyroidal extension nodule with irregular margins, suspicious left lateral lymph node 10 -20% 5 -10% hyperechoic solid regular margin isoechoic solid regular margin partially cystic with eccentric solid areas <3% spongiform partially cystic no suspicious features <1% cyst partially cystic no suspicious features Risk of malignancy hypoechoic solid regular margin
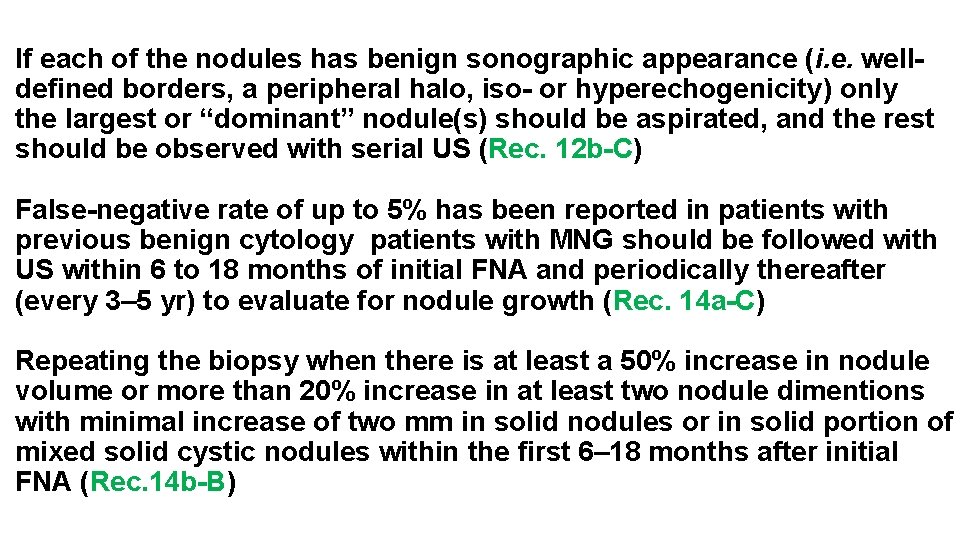
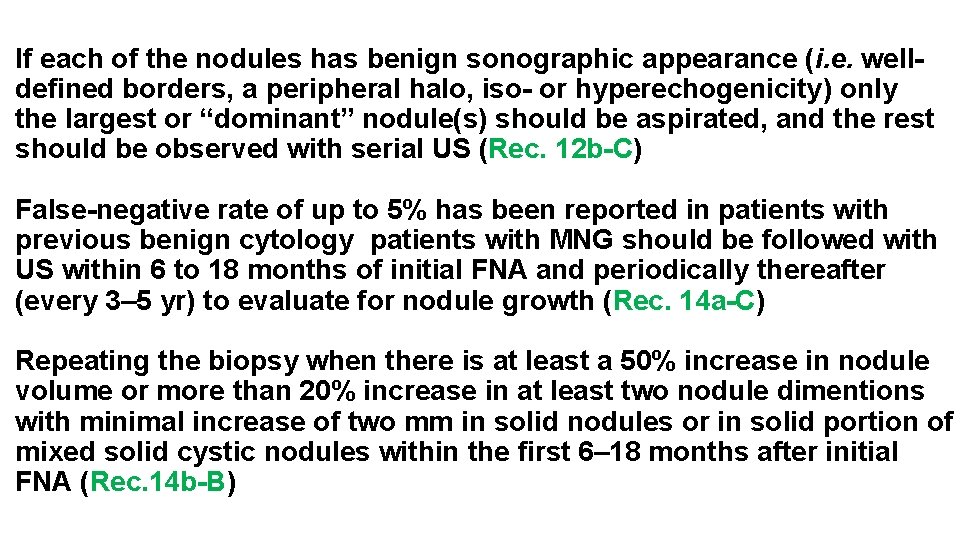
If each of the nodules has benign sonographic appearance (i. e. welldefined borders, a peripheral halo, iso- or hyperechogenicity) only the largest or “dominant” nodule(s) should be aspirated, and the rest should be observed with serial US (Rec. 12 b-C) False-negative rate of up to 5% has been reported in patients with previous benign cytology patients with MNG should be followed with US within 6 to 18 months of initial FNA and periodically thereafter (every 3– 5 yr) to evaluate for nodule growth (Rec. 14 a-C) Repeating the biopsy when there is at least a 50% increase in nodule volume or more than 20% increase in at least two nodule dimentions with minimal increase of two mm in solid nodules or in solid portion of mixed solid cystic nodules within the first 6– 18 months after initial FNA (Rec. 14 b-B)
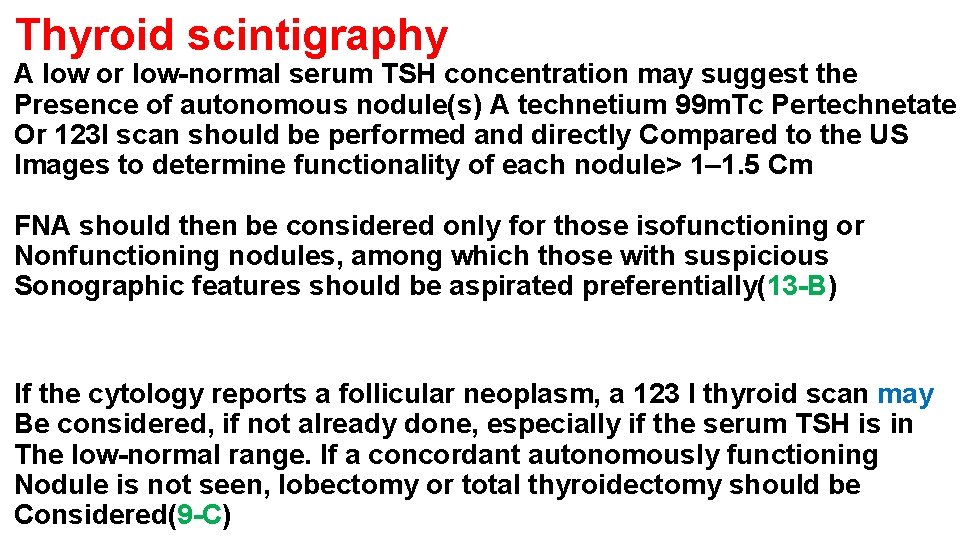
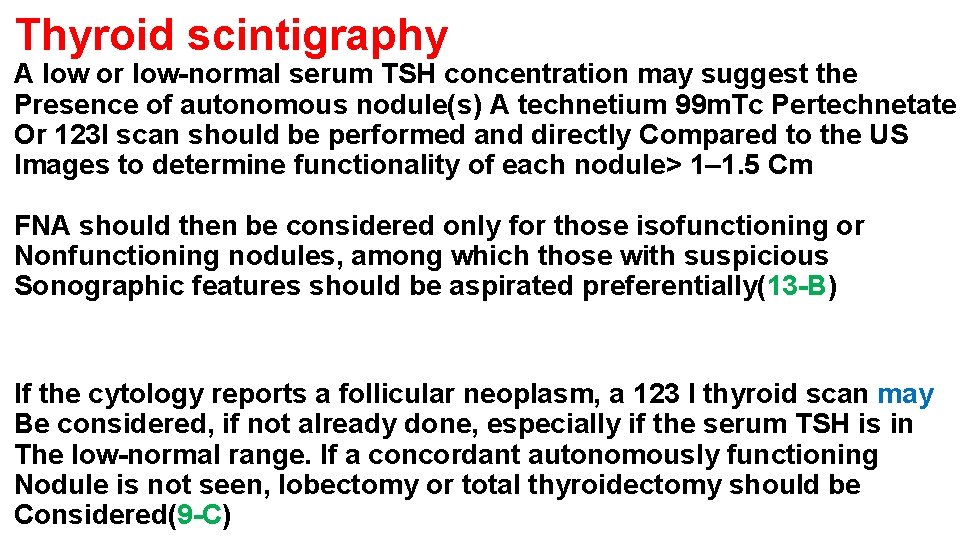
Thyroid scintigraphy A low or low-normal serum TSH concentration may suggest the Presence of autonomous nodule(s) A technetium 99 m. Tc Pertechnetate Or 123 I scan should be performed and directly Compared to the US Images to determine functionality of each nodule> 1– 1. 5 Cm FNA should then be considered only for those isofunctioning or Nonfunctioning nodules, among which those with suspicious Sonographic features should be aspirated preferentially(13 -B) If the cytology reports a follicular neoplasm, a 123 I thyroid scan may Be considered, if not already done, especially if the serum TSH is in The low-normal range. If a concordant autonomously functioning Nodule is not seen, lobectomy or total thyroidectomy should be Considered(9 -C)
Thyroid FNA biopsy Single most valuable, cost effective, and accurate method in the Evaluation of a patient with a nodular goiter 35 to 75%reduction in the number of patients requiring surgery, while Still doubling or tripling the malignancy yield at thyroidectomy Biopsy of only the “dominant” nodule may not detect an existing Thyroid cancer. US guidance extremely helpful in selecting the best Targets for FNA and is most helpful in small (1. 5 cm), partly cystic, And nonpalpable nodules (Rec. 5 b-B) In the hands of experienced operators, adequate samples can be Obtained from solid nodules in 90– 97% of aspirations For suspicious” cytology in the absence of autonomous function, surgical excision of these nodules is recommended (Rec. 9 -C)
Aspirates with insufficient number of cells are considered Nondiagnostic or unsatisfactory 50% of cases initially classified as nondiagnostic will produce a Satisfactory specimen when FNA is repeated under US guidance ATA guidelines recommended repeat biopsy in this setting (Rec. 5 a-A) Incidence of malignancy in the subset (5– 10%) of patients with Nodules remaining nondiagnostic has been found to be between 2 & 9% such nodules should be followed closely or surgery considered, Particularly if the nodule is solid (Rec. 6 b-B)

Agenda Definition and gross pathology Epidemiology Pathogenesis Clinical presentation Clinical evaluation & investigation Treatment Conclusion
Treatment In the absence of clinical, sonographic, or cytological findings Suggestive of malignancy, the selection of the best therapeutic Option depend on several factors, including size and location of The goiter, the presence and severity of compressive symptoms, And the presence or absence of thyrotoxicosis Including: 1 -Expectant therapy 2 -levothyroxine suppression therapy 3 -Minimally invasive therapy 4 -Radioiodine therapy +/- rh. TSH 5 -Surgery
Expectant therapy proper for small asymptomatic nonsuspicious MNG Levothyroxine suppression therapy TSH regarded as a growth factor for thyroid epithelial cells Levothyroxine in doses sufficient to suppress TSH has long been Used to prevent or reduce growth of thyroid nodules Effectiveness of this practice remains controversial Although some studies have shown efficacy others have failed to Show a clear benefit likely owing to differences in study design, the Population being evaluated, and epidemiological factors such as Prevalence of iodine insufficiency, nature of the nodular goiter (single vs. multinodular) adequacy of TSH suppression, duration of treatment


Efficacy of levothyroxine suppressive therapy in preventing recurrenc of goiter growth after partial thyroidectomy is less clear Randomized trials have failed to confirm benefit Because of deleterious effects on the skeleton due to suppressive therapy and the increased risk of AF and other cardiovascular complications, this treatment modality is not recommended by the ATA(Rec. 16 -F) Should be particularly avoided in postmenopausal women with Evidence of low bone mass, in the elderly, and in those with cardiac Disease, in whom the risk of this therapy generally outweighs its Uncertain benefits

Radioiodine therapy Cure the hyperthyroidism shrink thyroid gland Used for symptomatic nontoxic goiter as a non-Surgical option Out-patient treatment in most countries Probably superior to surgery as regards cost-effectiveness No trial has yet compared 131 I-therapy and surgery head-to-head bellows are good candidates for RAI Small or moderate goiter volume Previous thyroidectomy Co-existing hyperthyroidism due to nodular autonomy Advanced physiological age and/or co-morbidity associated with an increased surgical risk
131 I-therapy reduces the goiter volume by about *40% after 1 year 50– 60% after 2 years, without further significant reduction Also substernal goiters have been treated with beneficial results Generally, 131 I doses of 3. 7 MBq per gram of thyroid Tissue corrected for the thyroid 131 I uptake (RAIU), have been given Symptoms most often improve and patient satisfaction is high Treatment can be repeated if further goiter reduction is required Risk of permanent hypothyroidism in MNG range from 11% to 58% After 1 to 8 year follow up Secondary goiter growth following 131 I-therapy should always raise Suspicion of malignancy and lead to re-evaluation
131 I-therapy amplification by rh. TSH stimulation Some limitations with conventional RAI-therapy This treatment is unlikely to succeed if the thyroid RAIU is low (less than 15% at 24 hour) or the dominant nodule is scintigraphically ‘cold’ Relative goiter reduction is inversely correlated with the initial goiter size probably because large goiters harbor a higher amount of degenerated and fibrous tissue This problem could be overcome by increasing the administered 131 I activity and thereby the absorbed thyroid dose, but the concomitant increase in the whole-body radiation burden is a clear disadvantage
rh. TSH increases the thyroid 24 -h RAIU by 100% or even more Without compromising the 131 I half-life to any greater extent Causes more homogeneous distribution of 131 I within the goiter Increase in the thyroid RAIU inversely correlated to the initial RAIU Most beneficial in patients with MNG with low thyroid RAIU Use of rh. TSH is restricted to thyroid cancer patients Off-label drug for patients with benign thyroid diseases Unknown long-term effect of rh. TSH stimulated 131 I therapy With a ‘superiority strategy’ the goiter reduction is on Average enhanced by 35– 56% 1 year after 131 I-therapy The gain is most pronounced in large goiters Randomized trials have failed to demonstrate a positive impact on Patient satisfaction and quality of life
Nieuwlaat et al. demonstrated pre-treatment with 0. 01 and 0. 03 mg rh. TSH allowed a 50% reduction of administered 131 I activity, while still achieving a goiter reduction of *40% after 1 year Also showed that pre-stimulation with rh. TSH resulted in a two to threefold lower absorbed dose in the bladder and the stomach compared to conventional 131 I-therapy(equality strategy) As a direct consequence, the need for hospitalization and posttherapeutic restrictions was profoundly reduced.

Surgery is the preferred treatment modality for patients with Euthyroid large, obstructive, and substernal nontoxic MNG and those With continued growth, if they have an acceptable surgical risk Near-total or total thyroidectomy procedure of choice Complications of surgery such as injury to the recurrent laryngeal Nerve, trachea, and parathyroid glands are more common in patients With large and substernal goiters To minimize the risk of such complications, all patients requiring Surgery, especially those with substernal goiter, should be referred to Experienced thyroid surgeons in high-volume centers
Grade B recommendation can be made that subtotal Thyroidectomy is associated with significant recurrence of Goiter, leaves a small number of incidentally detected thyroid Cancers inadequately treated, and provides little significant Safety advantage over total thyroidectomy Grade C recommendations can also be made about total Thyroidectomy being a safe and effective procedure for benign Multinodular goiters in the hands of expert surgeons


Agenda Definition and gross pathology Epidemiology Pathogenesis Clinical presentation Clinical evaluation & investigation Treatment Conclusion
Conclusion The evaluation and management of a patient with a MNG is generally More difficult than that of a patient with a solitary thyroid nodule Serum TSH measurement should be the initial step US examination +/- FNA biopsy (preferably under US guidance) When suspicious nodules are seen essential to exclude Malignancy Continued follow-up with periodic US can detect clinically Significant growth of nodules that may warrant reaspiration Selection of nodules requiring FNA biopsy should be guided by Sonographic features, clinical history, and rate of growth Euthyroid patients with asymptomatic, benign nodular goiters Can be safely observed and followed with periodic neck exam & US Patients with confirmed malignant nodules & those with benign Symptomatic MNG(pressure, dysphagia) should referred for surgery





 Mixoedema
Mixoedema Multinodular goiter pathophysiology
Multinodular goiter pathophysiology Thyroid defintion
Thyroid defintion Multinodular goiter
Multinodular goiter Dr peter lakatos
Dr peter lakatos Gross pathology definition
Gross pathology definition Pathology
Pathology Chronic pyelonephritis gross pathology
Chronic pyelonephritis gross pathology Gross pathology
Gross pathology Osteochondroma gross pathology
Osteochondroma gross pathology Rumus gross b/c
Rumus gross b/c Iodine deficiency goiter
Iodine deficiency goiter Goiter classification
Goiter classification Hashimoto thyroiditis
Hashimoto thyroiditis Nodular goiter
Nodular goiter Goiter
Goiter Thyroid gland cells
Thyroid gland cells Define nutritional epidemiology
Define nutritional epidemiology Meaning of epidermiology
Meaning of epidermiology Prevalence
Prevalence Epidemiology definition
Epidemiology definition Agenda sistemica y agenda institucional
Agenda sistemica y agenda institucional Difference between descriptive and analytic epidemiology
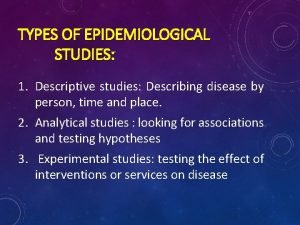
Difference between descriptive and analytic epidemiology Descriptive vs analytical epidemiology
Descriptive vs analytical epidemiology Descriptive vs analytic epidemiology examples
Descriptive vs analytic epidemiology examples Certification board of infection control and epidemiology
Certification board of infection control and epidemiology Descriptive epidemiology
Descriptive epidemiology Ukuran asosiasi statistika
Ukuran asosiasi statistika Logistic regression epidemiology
Logistic regression epidemiology Point and period prevalence
Point and period prevalence Cross sectional study advantages and disadvantages
Cross sectional study advantages and disadvantages Attack rate formula
Attack rate formula Bibliography of epidemiology
Bibliography of epidemiology Association vs causality
Association vs causality Formula for attack rate
Formula for attack rate Ramboman analysis
Ramboman analysis Epidemiological wheel
Epidemiological wheel Proportion defination
Proportion defination Defination of epidemiology
Defination of epidemiology Epornithic
Epornithic What is descriptive study in epidemiology
What is descriptive study in epidemiology Spurious association
Spurious association Field epidemiology ppt
Field epidemiology ppt Aims of epidemiology
Aims of epidemiology Gordon nichols
Gordon nichols Epidemiology kept simple
Epidemiology kept simple Diabetic ketoacidosis epidemiology
Diabetic ketoacidosis epidemiology