Grow Healthy Pakistan Prof Dr Saira Afzal Dean





- Slides: 19
Grow Healthy Pakistan • Prof Dr Saira Afzal • Dean of Public Health and Preventive Medicine, KEMU
Grow Healthy Pakistan • Current Situation • Epidemiology • Clinical features of kwashiorkor and Marasmus and their Differences • Biochemical and Metabolic Changes • Prevention • A way forward

Stunted Growth • Children are defined as stunted if their height-for-age is more than two standard deviations below the WHO Child Growth Standards median.
• Stunting is the impaired growth and development that children experience from: • poor nutrition, repeated infection, and poor sanitation condition.
• Among Children 6 -23 months of age, only 12% are fed according to the criteria of minimum acceptable diet
• More than one in every three children born in Pakistan today is stunted. • 240 Million Children have growth retardation (https: //www. thenews. com. pk/print/361890 -number-of-stuntedand-wasted-children-in-pakistan)
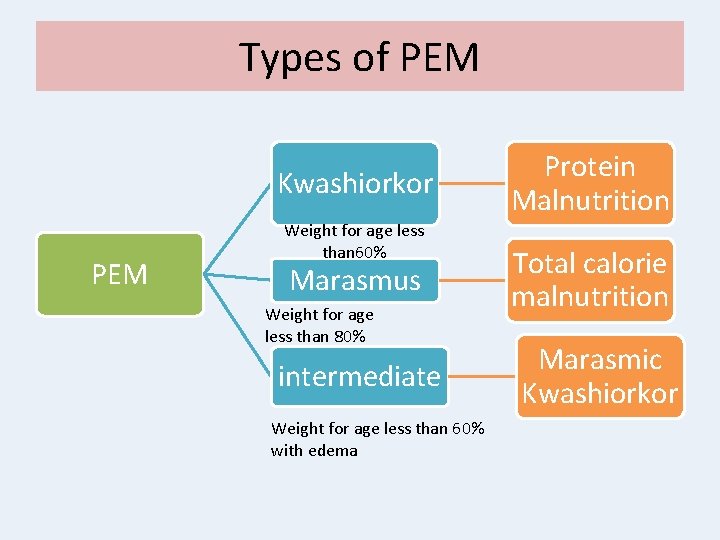
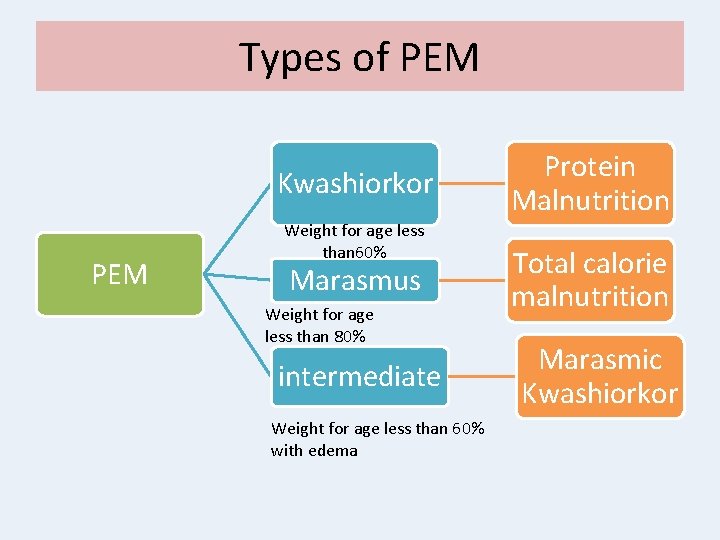
Types of PEM Kwashiorkor PEM Weight for age less than 60% Marasmus Weight for age less than 80% intermediate Weight for age less than 60% with edema Protein Malnutrition Total calorie malnutrition Marasmic Kwashiorkor
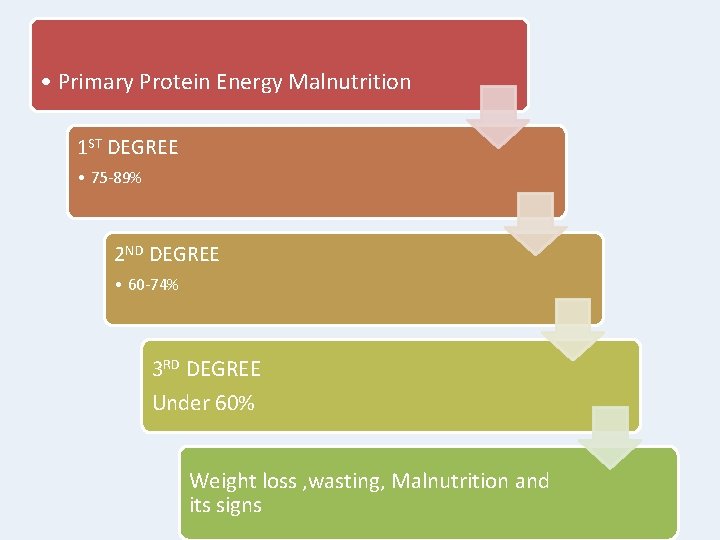
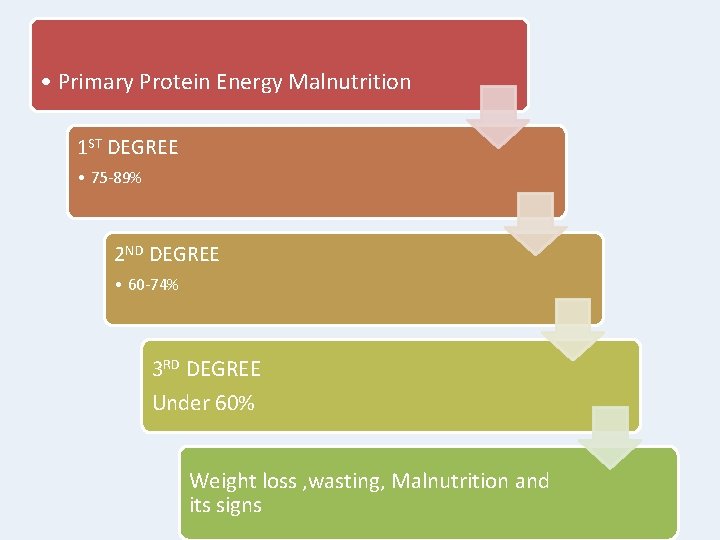
• Primary Protein Energy Malnutrition 1 ST DEGREE • 75 -89% 2 ND DEGREE • 60 -74% 3 RD DEGREE Under 60% Weight loss , wasting, Malnutrition and its signs

Epidemiology of Malnutrition • Global Burden- Starts In Womb And Ends In Tomb • Affects every 4 th Child worldwide • More than 50% deaths are associated with Malnutrition • Median Case fatality rate is 23. 5% in severe malnutrition and 50% in edematous Malnutrition
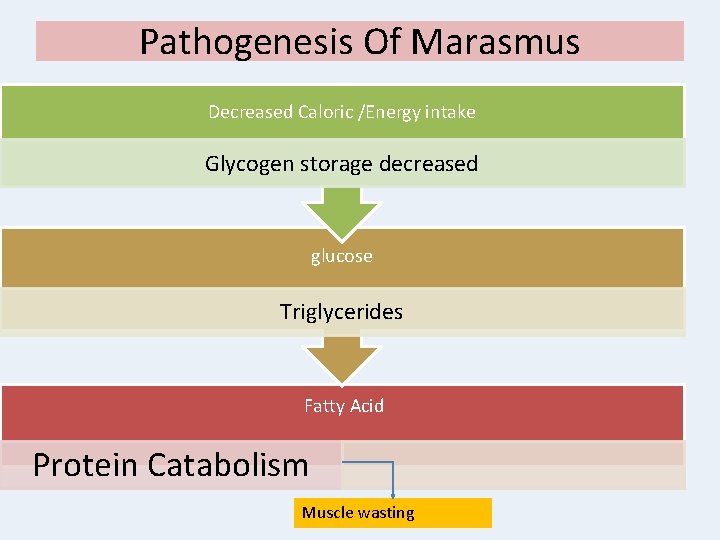
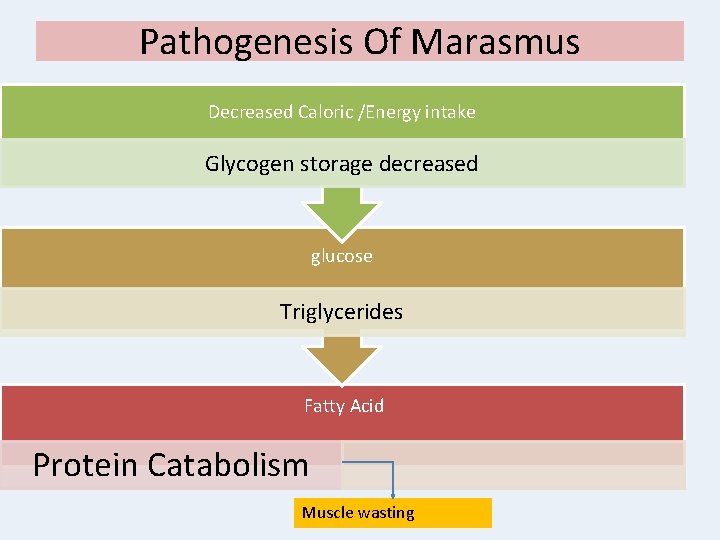
Pathogenesis Of Marasmus Decreased Caloric /Energy intake Glycogen storage decreased glucose Triglycerides Fatty Acid Protein Catabolism Muscle wasting
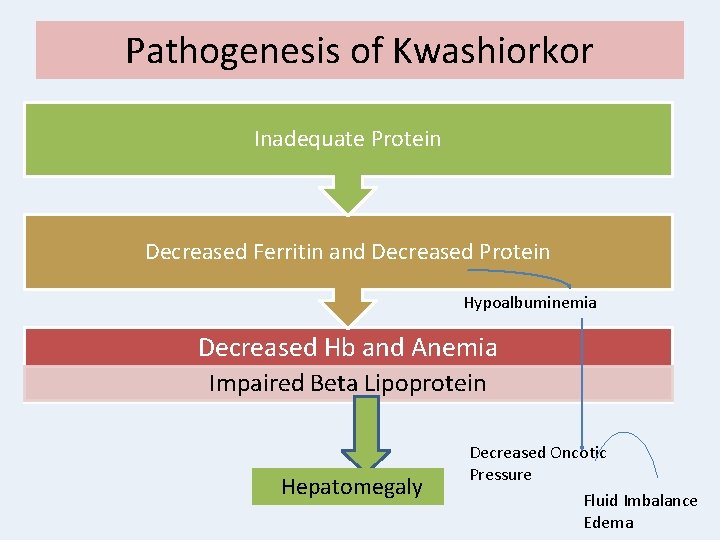
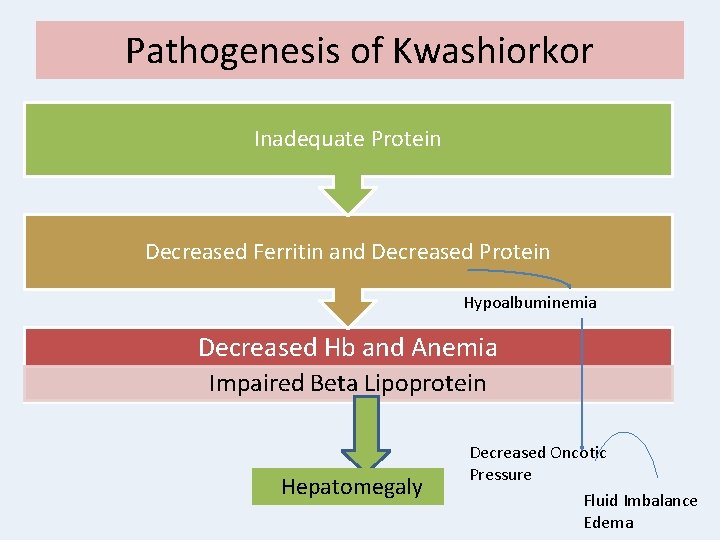
Pathogenesis of Kwashiorkor Inadequate Protein Decreased Ferritin and Decreased Protein Hypoalbuminemia Decreased Hb and Anemia Impaired Beta Lipoprotein Hepatomegaly Decreased Oncotic Pressure Fluid Imbalance Edema

Kwashiorkor Condition of Protein Malnutrition Moon Face with little interest in surroundings Edema of legs Swollen Abdomen Protein Intake deficient Generalised Muscle Wasting Hyponatremia
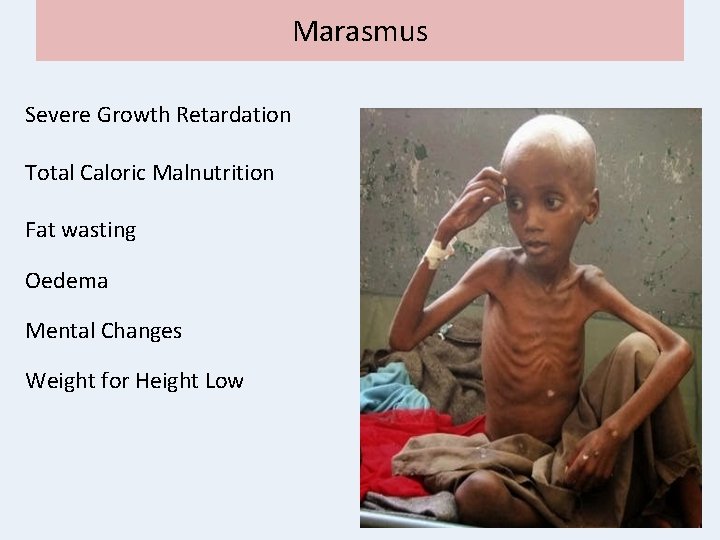
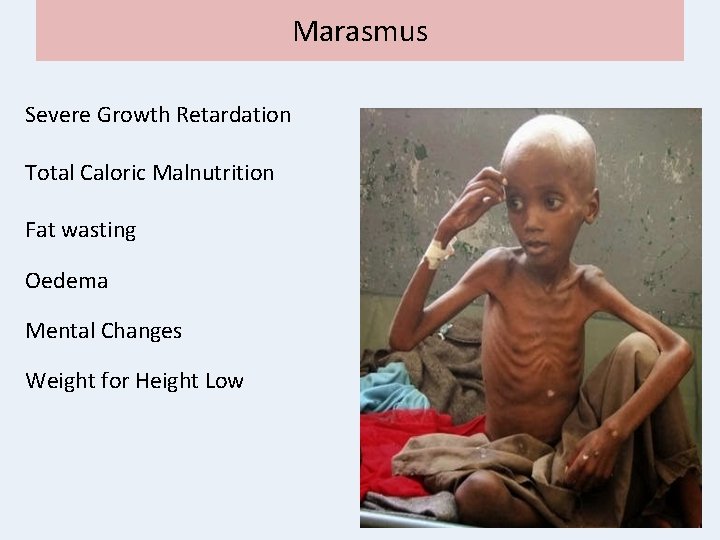
Marasmus Severe Growth Retardation Total Caloric Malnutrition Fat wasting Oedema Mental Changes Weight for Height Low
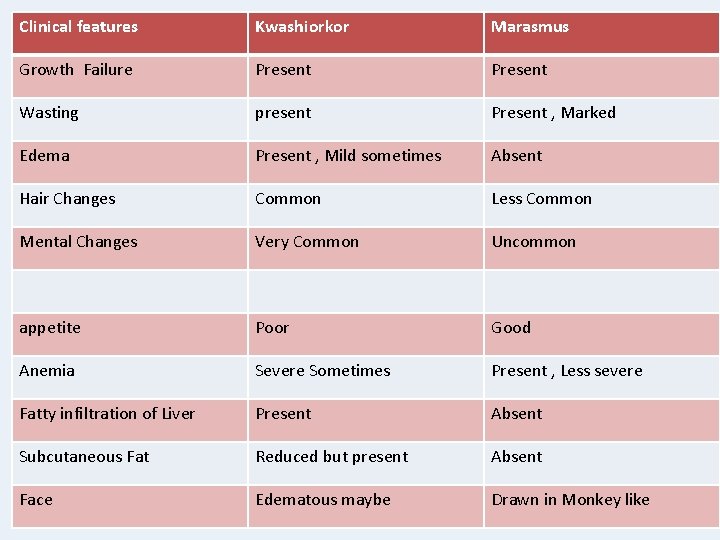
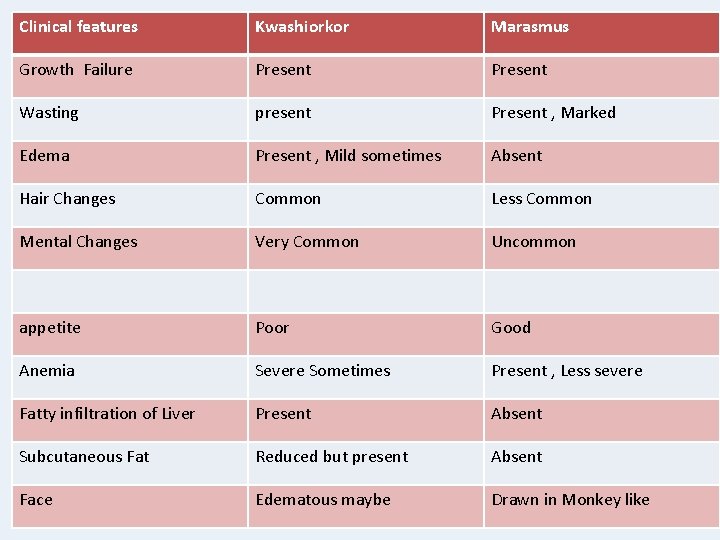
Clinical features Kwashiorkor Marasmus Growth Failure Present Wasting present Present , Marked Edema Present , Mild sometimes Absent Hair Changes Common Less Common Mental Changes Very Common Uncommon appetite Poor Good Anemia Severe Sometimes Present , Less severe Fatty infiltration of Liver Present Absent Subcutaneous Fat Reduced but present Absent Face Edematous maybe Drawn in Monkey like
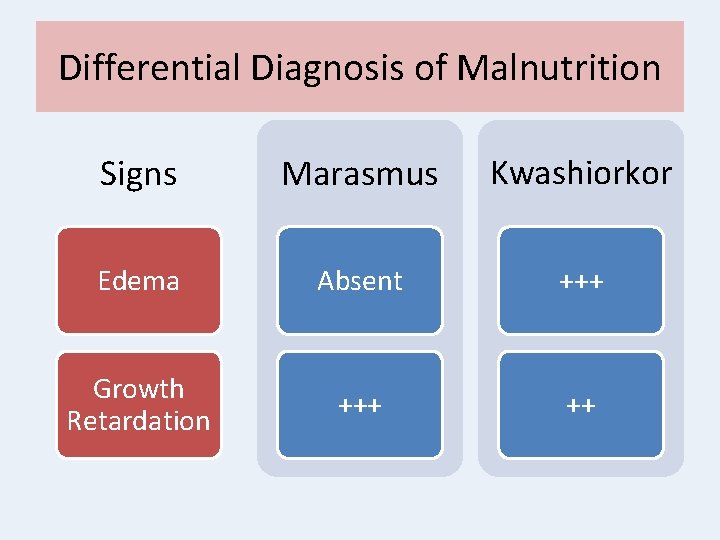
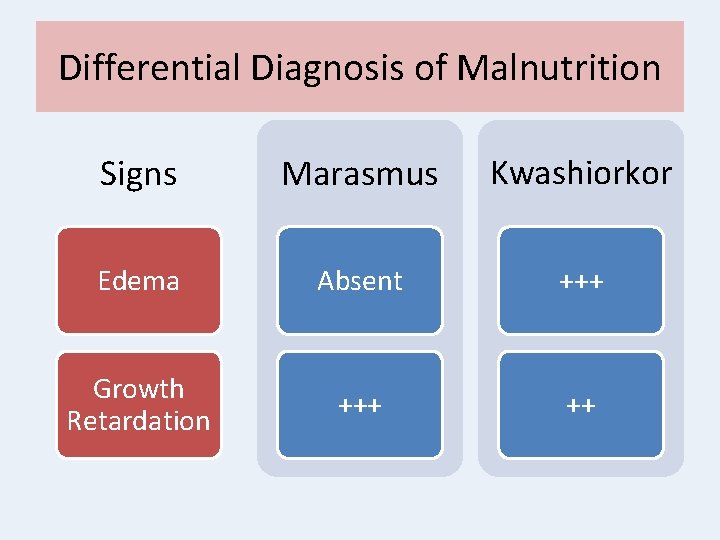
Differential Diagnosis of Malnutrition Signs Marasmus Kwashiorkor Edema Absent +++ Growth Retardation +++ ++
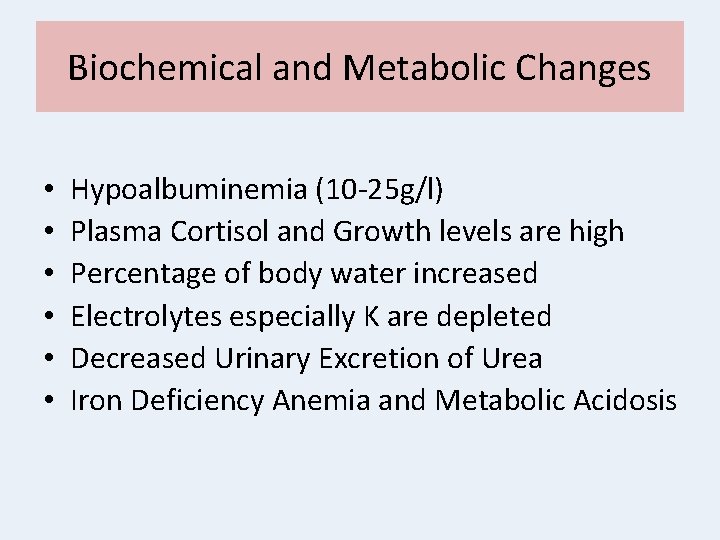
Biochemical and Metabolic Changes • Hypoalbuminemia (10 -25 g/l) • Plasma Cortisol and Growth levels are high • Percentage of body water increased • Electrolytes especially K are depleted • Decreased Urinary Excretion of Urea • Iron Deficiency Anemia and Metabolic Acidosis
Prevention • • Provision of Adequate Nutrition Provision of Protein High Energy Food during Pregnancy Education Food Supplements Better School Health Services Better Feeding Practices Awareness Campaigns

• First two years of life • Maternal Nutrition and Literacy • Better Feeding Practices • Educational and Policy Reforms • School Health Services

Thank You
 Dean d dean
Dean d dean Saira a table
Saira a table Saira has a fear of cats
Saira has a fear of cats Healthy community poster
Healthy community poster Healthy nurse healthy nation
Healthy nurse healthy nation Healthy food healthy mind journal
Healthy food healthy mind journal Healthy soil healthy life poster ideas
Healthy soil healthy life poster ideas Dr. m. tanvir afzal
Dr. m. tanvir afzal Dr. m. tanvir afzal
Dr. m. tanvir afzal Dr. afzal hossain
Dr. afzal hossain Dr. m. tanvir afzal
Dr. m. tanvir afzal Dr tanveer afzal
Dr tanveer afzal Ali afzal malik
Ali afzal malik Dr. m. tanvir afzal
Dr. m. tanvir afzal Bad boy by walter dean myers
Bad boy by walter dean myers Jessica dean attorney
Jessica dean attorney Dean sherzai wikipedia
Dean sherzai wikipedia Mark dean biography
Mark dean biography Shoe leather survey
Shoe leather survey Dean eidelman
Dean eidelman