Opioid Use Disorder and Treatment Farinaz Khan Paul
















- Slides: 52
Opioid Use Disorder and Treatment Farinaz Khan, Paul Romo, MD
Disclosure • None
Outline • • Opioids and the Neuroendocrine system Misuse and Addiction Treatment Special Populations- forensics
Objective • • By the end of this didactic, you will be able to: Connect endogenous mechanisms to clinical observations Understand OUD as a disease state Discuss treatment options for MOUD including adverse effects and contraindications.
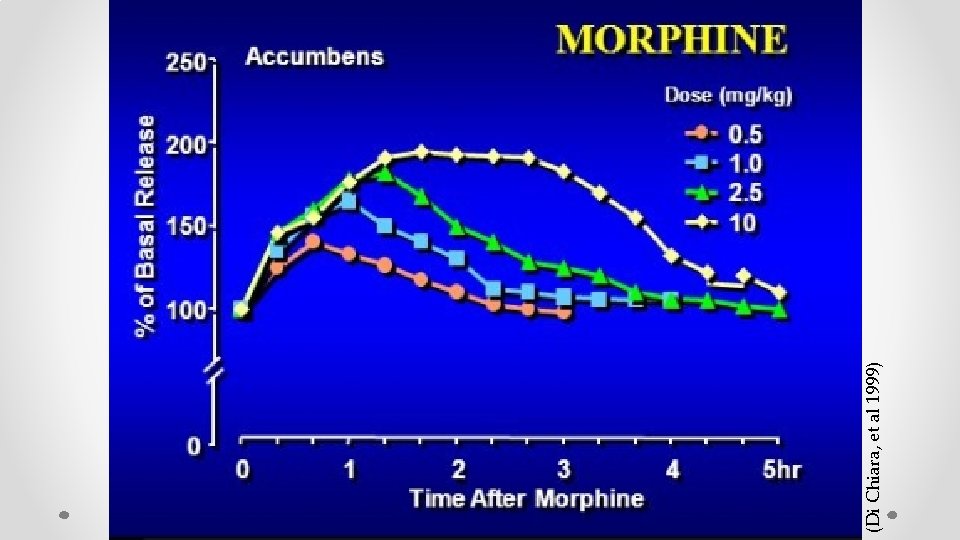
Opioid effects on DA and NE systems • • Peptide families: endorphin, enkephalin, dynorphins Receptors: Mu, Delta, Kappa Mu most robust for clinically active opioids Exogenous opioids impact the same system(s) • Down stream effects on dopamine (DA) and Norepinephrine (NE)




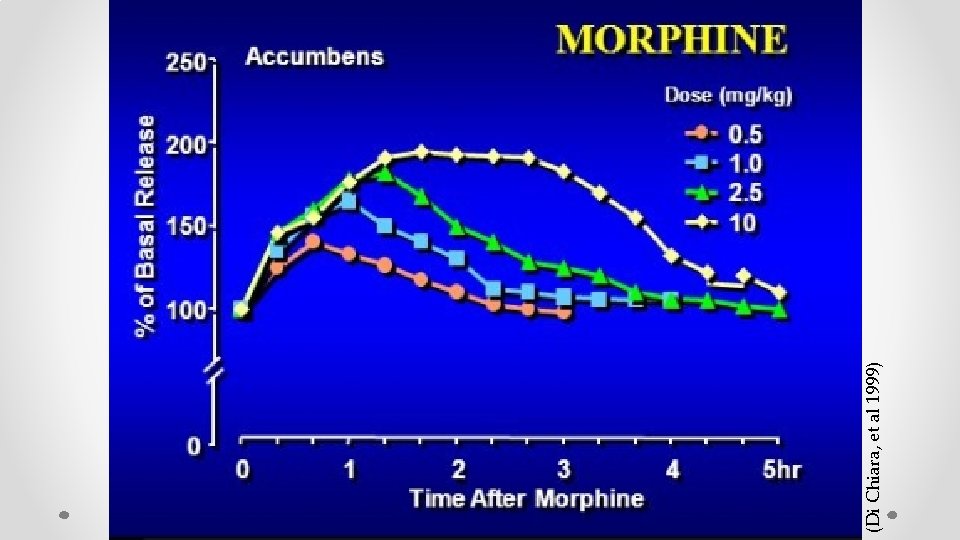
(Di Chiara, et al 1999)


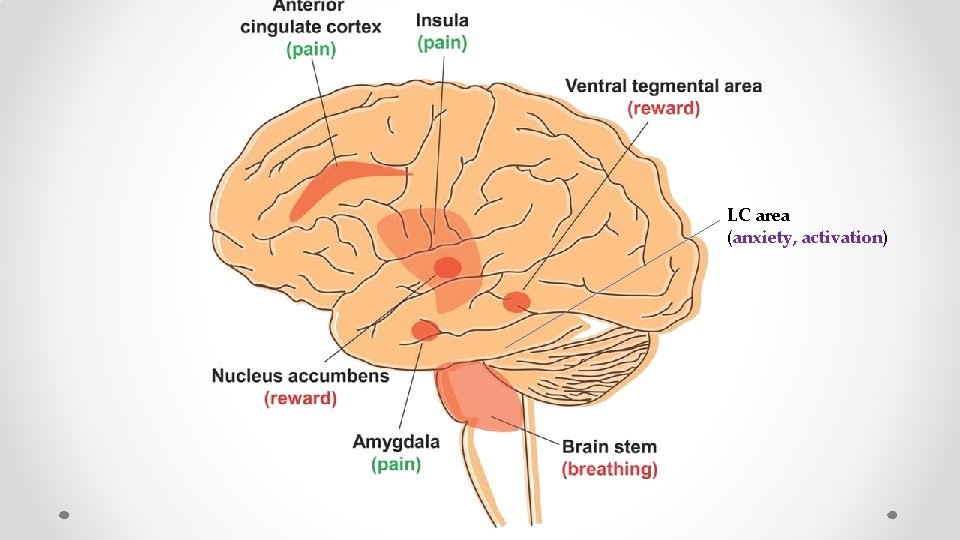
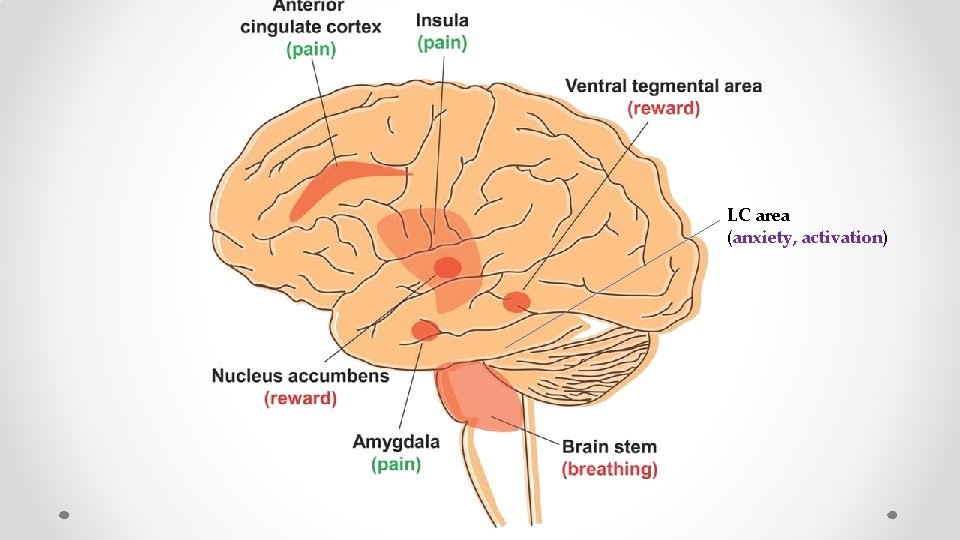
LC area (anxiety, activation)
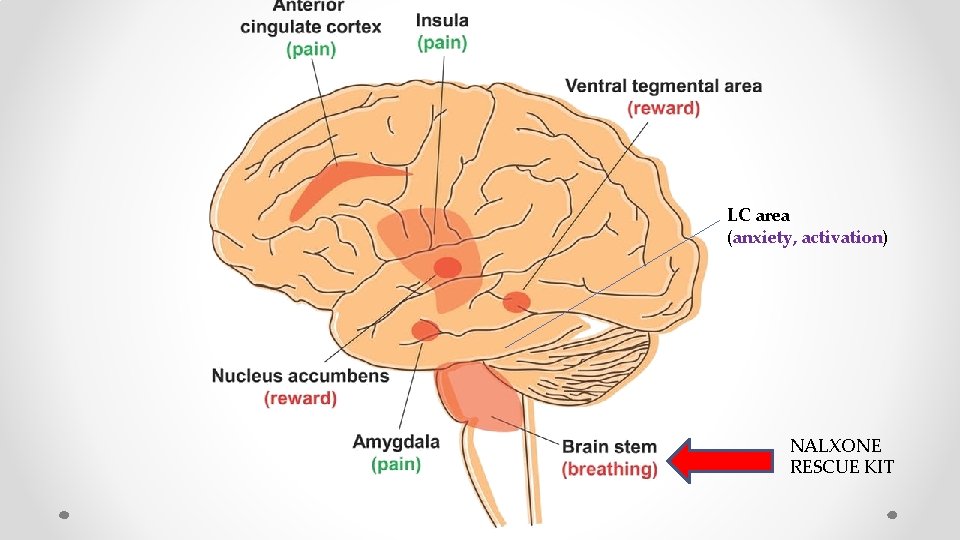
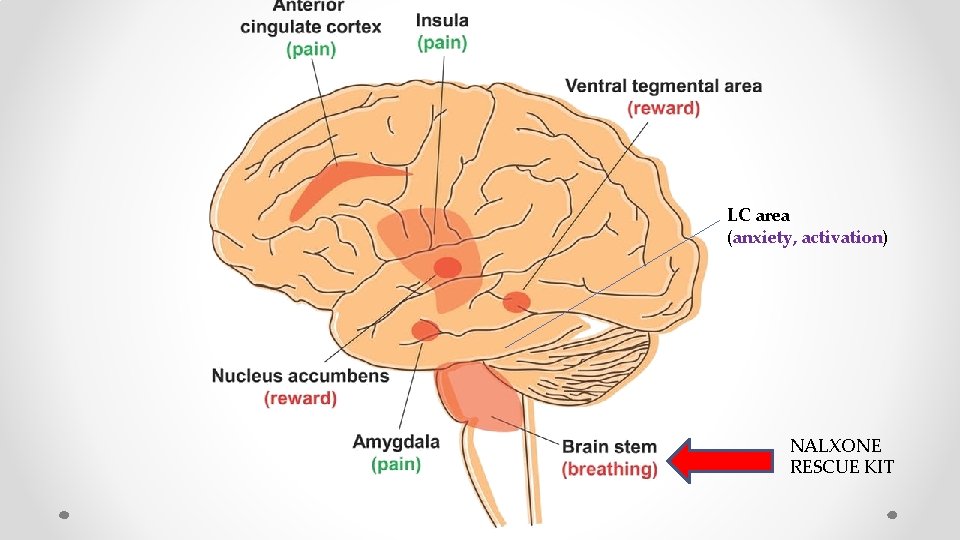
LC area (anxiety, activation) NALXONE RESCUE KIT
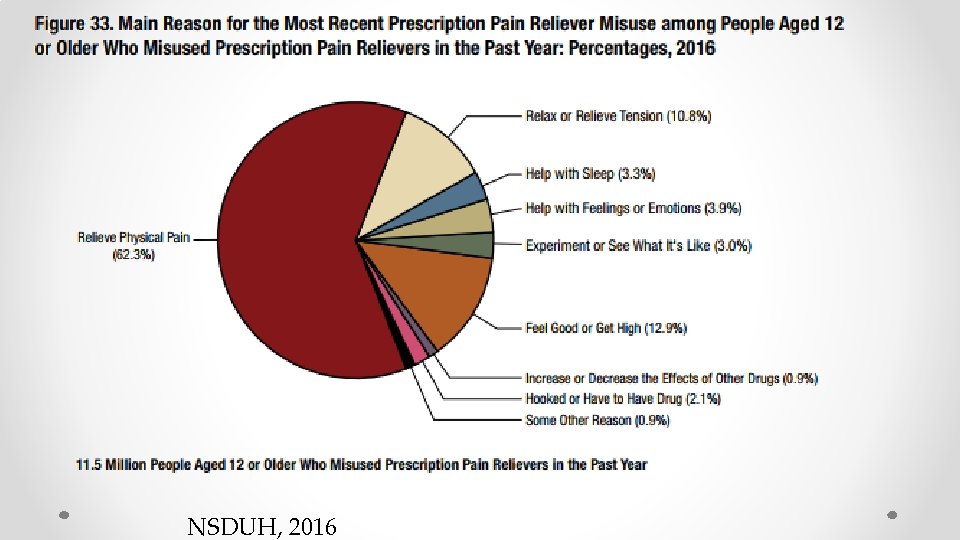
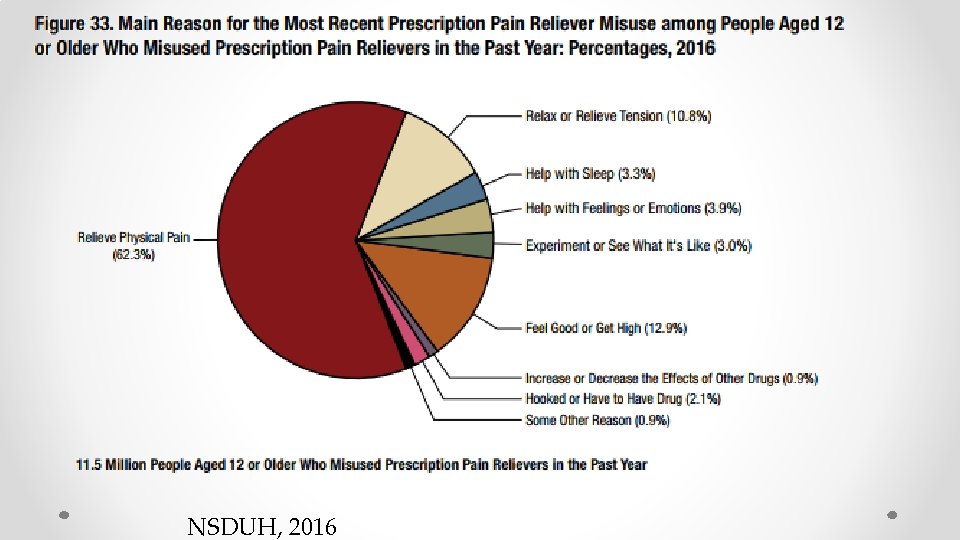
NSDUH, 2016
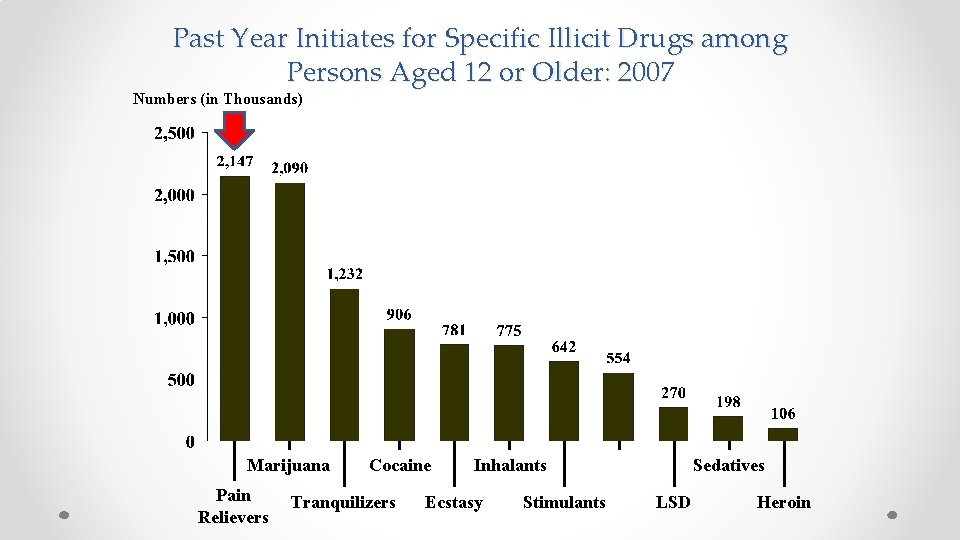
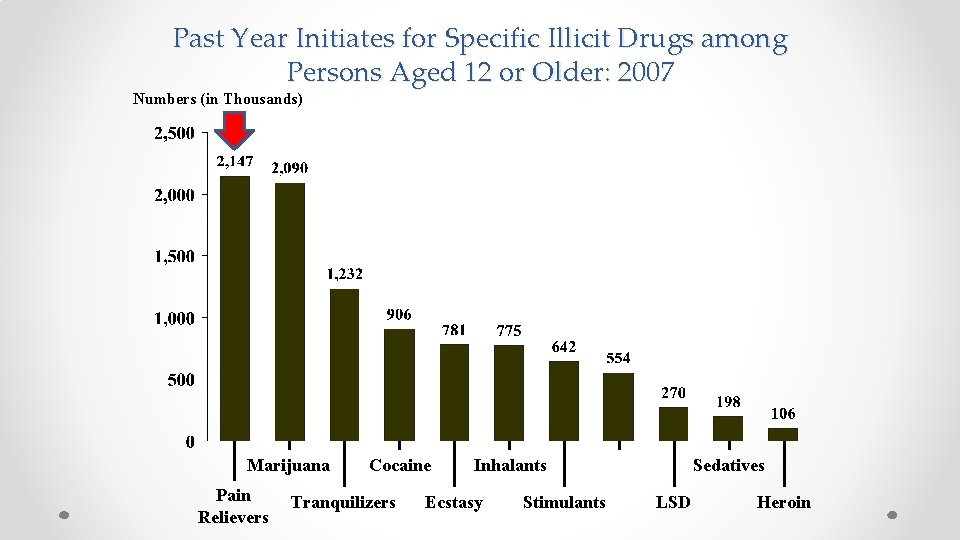
Past Year Initiates for Specific Illicit Drugs among Persons Aged 12 or Older: 2007 Numbers (in Thousands) Marijuana Pain Relievers Cocaine Tranquilizers Inhalants Ecstasy Stimulants Sedatives LSD Heroin
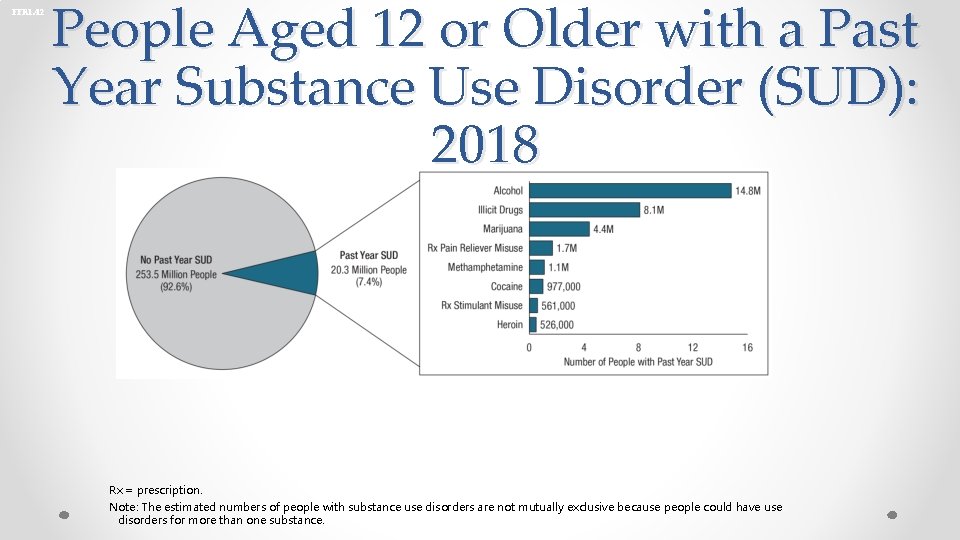
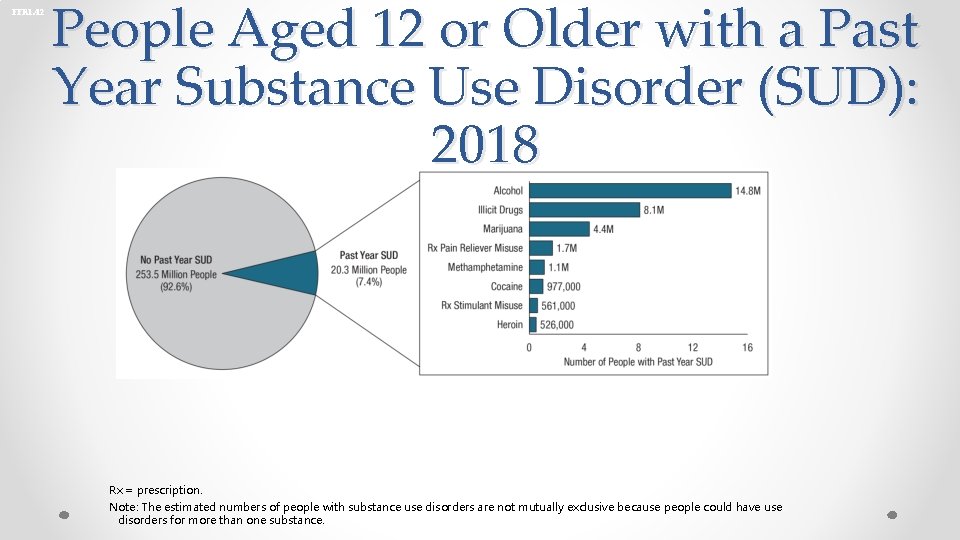
FFR 1. 42 People Aged 12 or Older with a Past Year Substance Use Disorder (SUD): 2018 Rx = prescription. Note: The estimated numbers of people with substance use disorders are not mutually exclusive because people could have use disorders for more than one substance.
ADDICTION AS A DISEASE MODEL


ASAM Definition of Addiction • A primary, chronic disease of brain reward, motivation, memory and related circuitry. • Dysfunction in these circuits leads to characteristic biological, psychological, social, and spiritual manifestations. • This is reflected in an individual pathologically pursuing reward and/or relief by substance use and other behaviors. http: //www. asam. org/Definitionof. Addiction-Long. Version. html
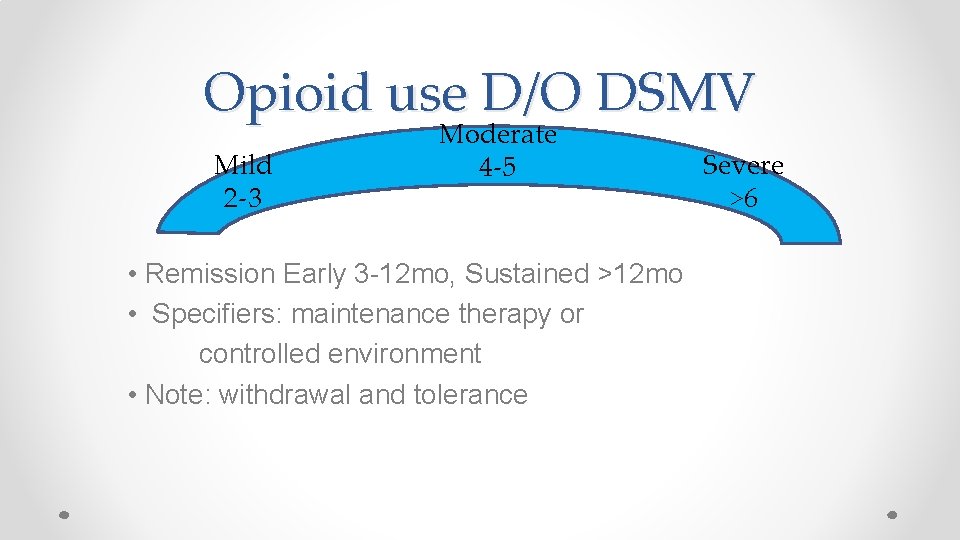
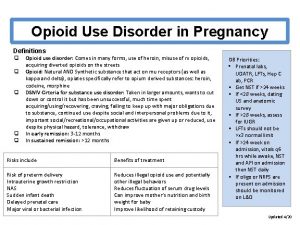
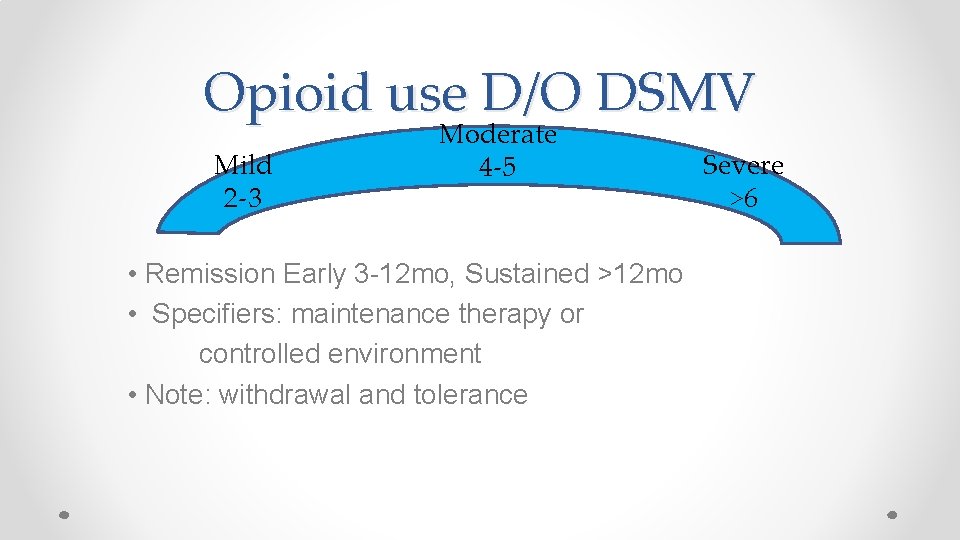
Opioid use D/O DSMV Mild 2 -3 Moderate 4 -5 • Remission Early 3 -12 mo, Sustained >12 mo • Specifiers: maintenance therapy or controlled environment • Note: withdrawal and tolerance Severe >6
SUD Criteria • Substance is often taken in larger amounts or over a longer period than was intended. • There is a persistent desire or unsuccessful efforts to cut down or control use. • A great deal of time is spent in activities necessary to obtain, use, or recover from its effects. • Craving, or a strong desire or urge to use substance. • Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home. • Withdrawal • Tolerance
SUD Criteria • Continued substance use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of the substance. • Important social, occupational, or recreational activities are given up or reduced because of substance use. • Recurrent substance use in situations in which it is physically hazardous. • Substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance.
Opioid Use D/O Treatment • Behavioral interventions have poor outcomes • Controlled environment • Medication assisted detoxification poor outcomes • N. A. • These forms of treatment or lack of, have higher associated risk or relapse, OD, recidivism, crime, infection, death • (Bart, 2012)
Opioid Withdrawal • • Nausea Vomiting Abdominal cramping Diarrhea Muscle aches Runny nose Sweating Tachycardia • • Increased tearing Insomnia Yawning Dilated pupils Goose bumps Agitation Anxiety
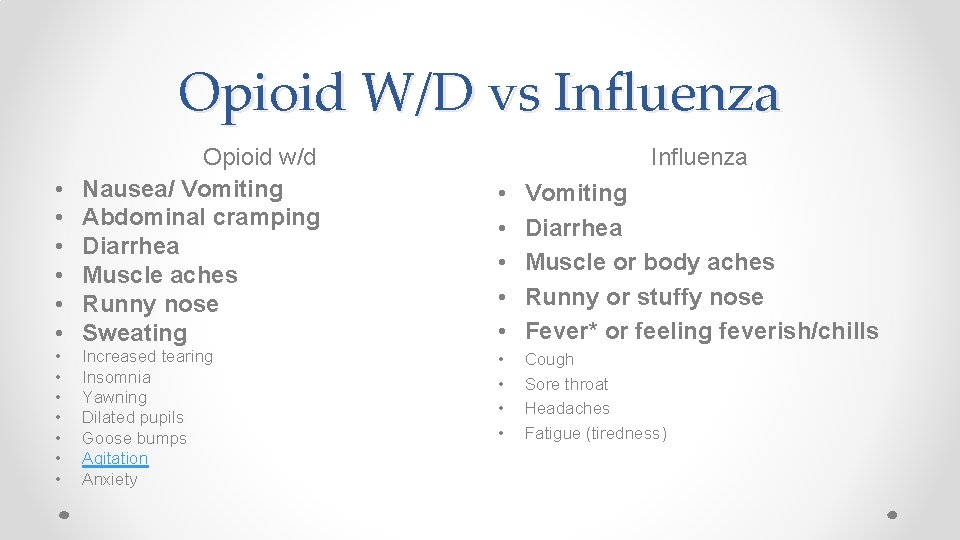
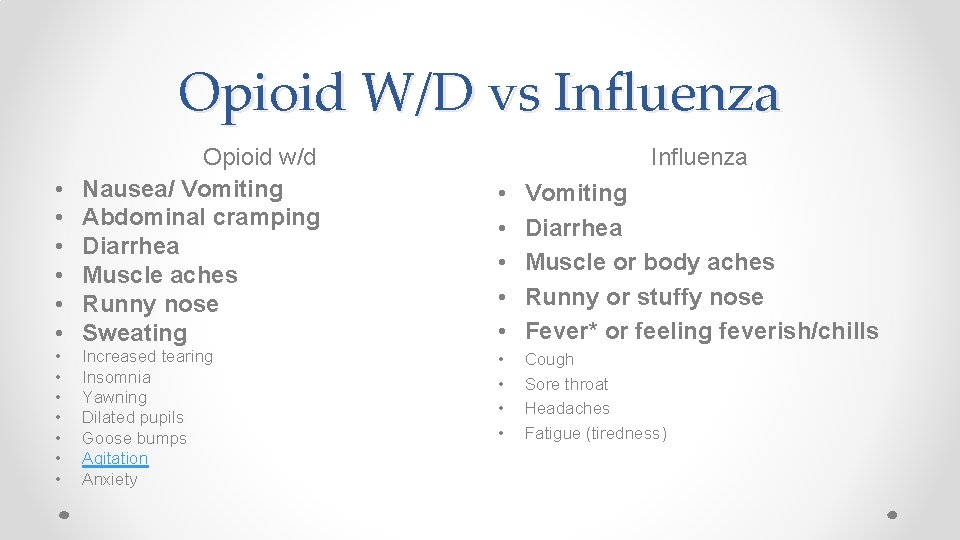
Opioid W/D vs Influenza • • • Opioid w/d Nausea/ Vomiting Abdominal cramping Diarrhea Muscle aches Runny nose Sweating • • Increased tearing Insomnia Yawning Dilated pupils Goose bumps Agitation Anxiety Influenza • • • Vomiting Diarrhea Muscle or body aches Runny or stuffy nose Fever* or feeling feverish/chills • • Cough Sore throat Headaches Fatigue (tiredness)
Opioid W/D kick kit • • • NSAIDS Clonidine Muscle relaxant Antiemetic Imodium
Maintenance Medications • FDA approved for long term treatment: • Methadone (MTD)-opioid agonist • Buprenorphine (BUP)-partial agonist • Naltrexone (NTX)-opioid antagonist • Office based and clinic based
MAT as Detox Agent • >90% of patients relapse within 2 months of taper • 95% of methadone patients will relapse within 1 year after d/c • Nosyk, 2013, Weiss, 2011

Adverse Effects and Contraindications • • Hepatic-Hepatitis and Decreased Function (monitor LFTS) Cardiac- QTC prolongation CNS-sedative effects or paradoxical effects GI- constipation and secondary morbidity
Side Effects and Contraindications • • Drug-Drug interactions (i. e. benzodiazepines) QTC prolongation (i. e. antihistamines, antidepressants, antibiotics, antifungals) Inhibition (i. e. Seroquel) Induction (i. e. Dilantin)

Switching Classes of FDA approved treatments • Naltrexone Buprenorphine Methadone (reduced efficacy initially) • No risk of precipitating withdrawal

Switching Classes of FDA approved treatments • Methadone Buprenorphine Naltrexone • Risk of precipitating withdrawal • Wash out period is longer for bup and methadone
Special Populations • • • Adolescents Geriatrics Pregnant Women LBGTQ Forensics
Forensic Population




Addiction and Crime • US has highest incarceration rate • Costly 1. 7 trillion (Anderson, 2011) • 1/100 adults may be incarcerated in life time, higher for minorities (Warren, 2008)
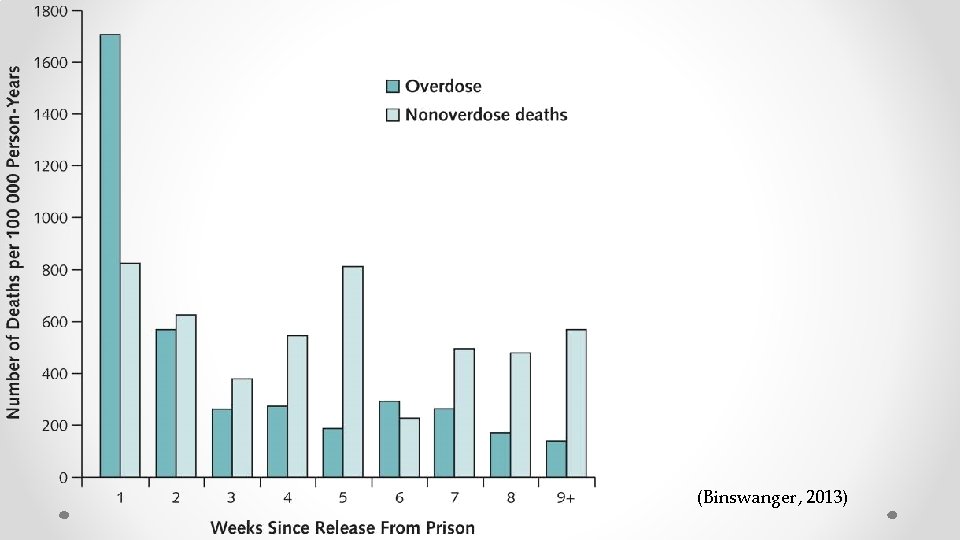
• SUD and crime highly correlated 50% cases (Nunn 2009) • Nearly 1/4 of inmates in DOC report heroin use (Karberg 2016) • OUD correlated with other poor outcomes such as HIV transmission, crime, recidivism, opioid toxicities and deaths (Rudd 2016) • Risk of OD 13 x greater for parolees within first 2 weeks after release • In England, risk documented 29 x higher than those without OUD (Binswanger, 2013, (Merrall, 2010)
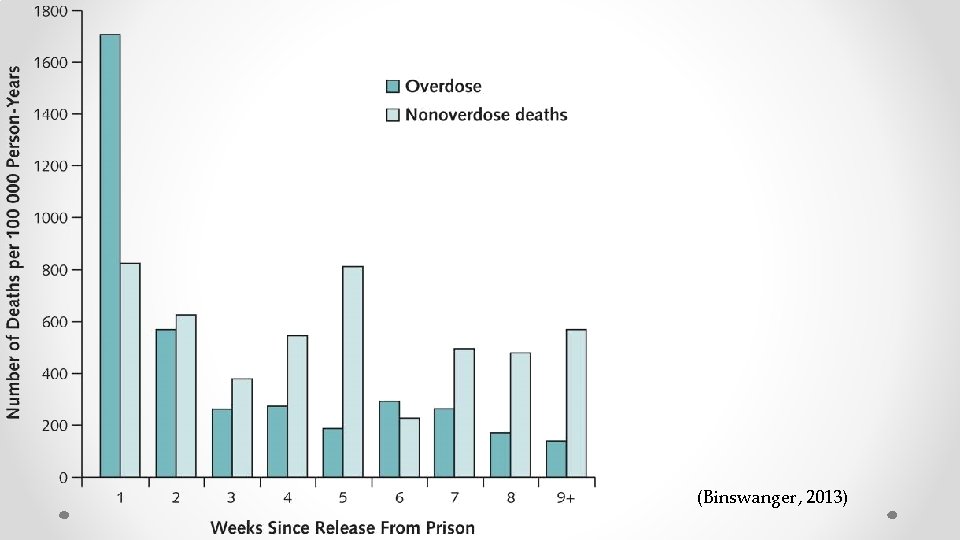
(Binswanger, 2013)
Intervention Points • Contact with EMS services including Law Enforcement • Drug Court • Pretrial Services
Intervention Points • Intra system programs and treatment • Release and post incarceration services • UNM Jail Diversion Services, JDS
Treatment • MOUDs reduce drug use and criminality (Perry 2014) • MOUDs reduce post release drug use and crime (Schwartz 2017) Benefits extend out 12 months following release after incarceration according to RCT (Kinlock 2009) Despite data, MOUDs are rarely implemented in the criminal justice system

Other treatment modalities • • • Naloxone rescue kit distribution upon d/c Naltrexone and Vivitrol Suboxone 12 step groups Individual and Group Counseling ATP, mimics an IOP
Outline • • Opioids and the Neuroendocrine system Misuse and Addiction Treatment Special Populations- forensics
Questions
Objective • • By the end of this didactic, you will be able to: Connect endogenous mechanisms to clinical observations Understand OUD as a disease state Discuss treatment options for MOUD including adverse effects and contraindications.
 Farinaz edalat
Farinaz edalat Treatment of substance use disorder
Treatment of substance use disorder Conversion vs somatic symptom disorder
Conversion vs somatic symptom disorder Impulse control disorder treatment
Impulse control disorder treatment Impulse control disorder treatment
Impulse control disorder treatment Integrated dual disorder treatment
Integrated dual disorder treatment Loose association speech
Loose association speech Poss scale
Poss scale Opioid reseptörleri
Opioid reseptörleri Alprazolam äquivalenzdosis
Alprazolam äquivalenzdosis Opioid overdose
Opioid overdose Opioid overdose
Opioid overdose Opioid overdose
Opioid overdose Types of pain
Types of pain Mechanism of action of opioid analgesics
Mechanism of action of opioid analgesics Nips pain scale
Nips pain scale Opioid receptors location
Opioid receptors location Non-opioid
Non-opioid Suzanne nesbit
Suzanne nesbit Poker chip pain scale
Poker chip pain scale Kentucky opioid response effort
Kentucky opioid response effort Substance use disorder
Substance use disorder How you use ict today and how you will use it tomorrow
How you use ict today and how you will use it tomorrow What is ideology of pakistan
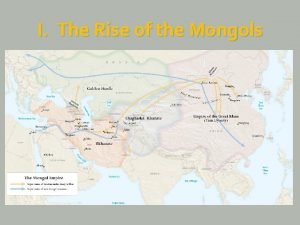
What is ideology of pakistan Genghis khan and babur
Genghis khan and babur Khan academy least common denominator
Khan academy least common denominator Khan academy active and passive voice
Khan academy active and passive voice Area of sector formula
Area of sector formula Seated boxer khan academy
Seated boxer khan academy Bpd comorbidity
Bpd comorbidity Borderline personality disorder vs adhd
Borderline personality disorder vs adhd Kode icd 10 iritasi mata
Kode icd 10 iritasi mata Thoracogenic scoliosis of thoracolumbar region
Thoracogenic scoliosis of thoracolumbar region Disorder of synovium and tendon
Disorder of synovium and tendon Thoracogenic scoliosis of thoracolumbar region
Thoracogenic scoliosis of thoracolumbar region Genghis khan dna map
Genghis khan dna map Arghun khan osman
Arghun khan osman Sir syed ahmed khan father name
Sir syed ahmed khan father name Ulugh khan
Ulugh khan Genghis real name
Genghis real name Fraternal polyandry meaning
Fraternal polyandry meaning When the united indian patriotic association was set up?
When the united indian patriotic association was set up? Electromagnetism khan academy
Electromagnetism khan academy Khan cademy
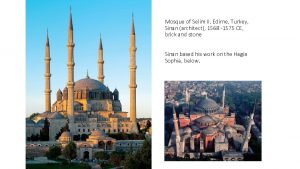
Khan cademy Mosque of selim ii khan academy
Mosque of selim ii khan academy Khan academy learn storm
Khan academy learn storm Kubla khan setting
Kubla khan setting Kubla khan shmoop
Kubla khan shmoop Khanacademy java
Khanacademy java Rational root theorem khan academy
Rational root theorem khan academy Güyük khan
Güyük khan Genghis khan name
Genghis khan name Napoleon crossing the alps neoclassical or romantic
Napoleon crossing the alps neoclassical or romantic