Interdisciplinary Treatment for Opioid Use Disorder in the
- Slides: 21
Interdisciplinary Treatment for Opioid Use Disorder in the UAMS Women’s Mental Health Program – A Case Study Michael A. Cucciare, Ph. D and Shona Ray-Griffith, MD Women’s Mental Health Program University of Arkansas for Medical Sciences Text MCUCCIARE 737 to 22333 join 1
Disclosures • Dr. Cucciare has no disclosures. • Dr. Ray-Griffith receives clinical trial support from Neuronetics and has received clinical trial support from Sage Therapeutics. Neither will be discussed today.
Today’s Goals • Briefly describe the UAMS Women’s Mental Health Program (WMHP) • Describe an interdisciplinary approach to treating opioid use disorder • Talk about patient’s outcomes and lessons learned 3
Women’s Mental Health Program (WMHP) • Outpatient psychiatric practice focused on pregnant and postpartum women with neuropsychiatric illnesses, including substance use disorders. 4
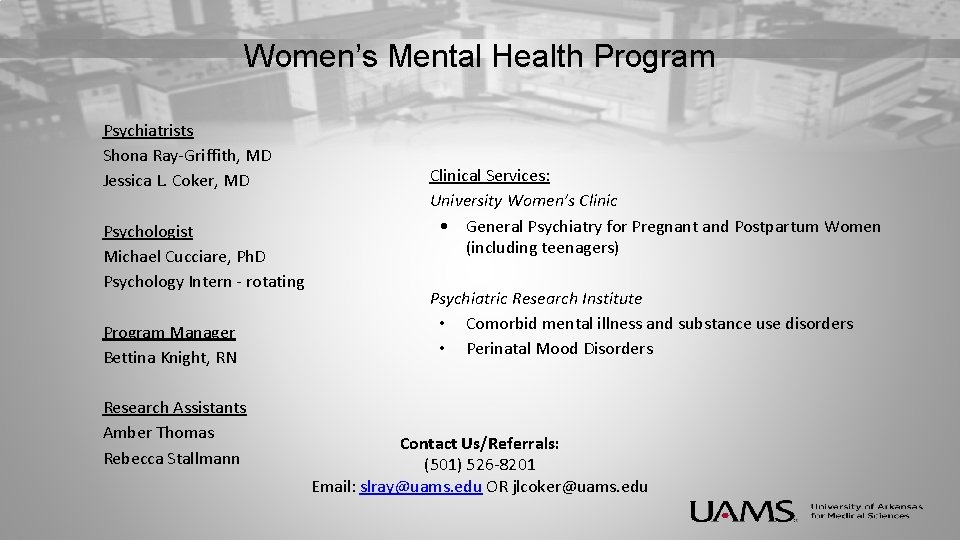
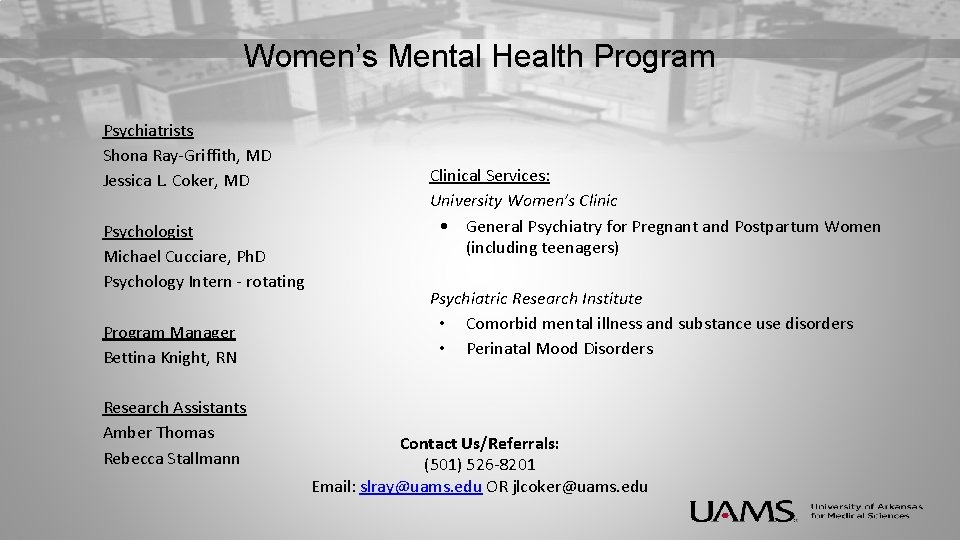
Women’s Mental Health Program Psychiatrists Shona Ray-Griffith, MD Jessica L. Coker, MD Psychologist Michael Cucciare, Ph. D Psychology Intern - rotating Program Manager Bettina Knight, RN Research Assistants Amber Thomas Rebecca Stallmann Clinical Services: University Women’s Clinic • General Psychiatry for Pregnant and Postpartum Women (including teenagers) Psychiatric Research Institute • Comorbid mental illness and substance use disorders • Perinatal Mood Disorders Contact Us/Referrals: (501) 526 -8201 Email: slray@uams. edu OR jlcoker@uams. edu
Case Study • • • 22 year old woman, Caucasian 19 weeks pregnant (unplanned, wanted) Not currently employed; some college No pregnancy complications reported at time of intake Referred by Maternal-Fetal Medicine (high risk) Hepatitis C 6
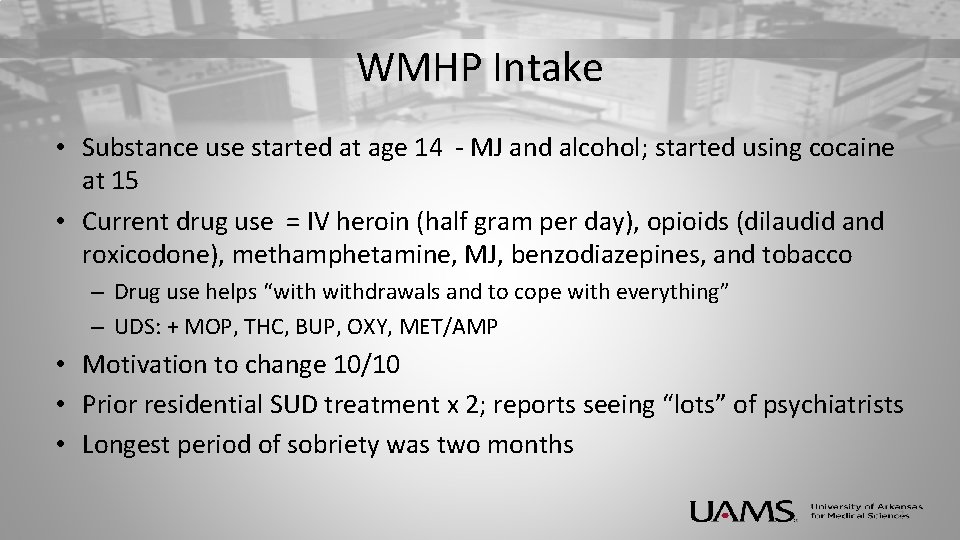
WMHP Intake • Substance use started at age 14 - MJ and alcohol; started using cocaine at 15 • Current drug use = IV heroin (half gram per day), opioids (dilaudid and roxicodone), methamphetamine, MJ, benzodiazepines, and tobacco – Drug use helps “withdrawals and to cope with everything” – UDS: + MOP, THC, BUP, OXY, MET/AMP • Motivation to change 10/10 • Prior residential SUD treatment x 2; reports seeing “lots” of psychiatrists • Longest period of sobriety was two months 7
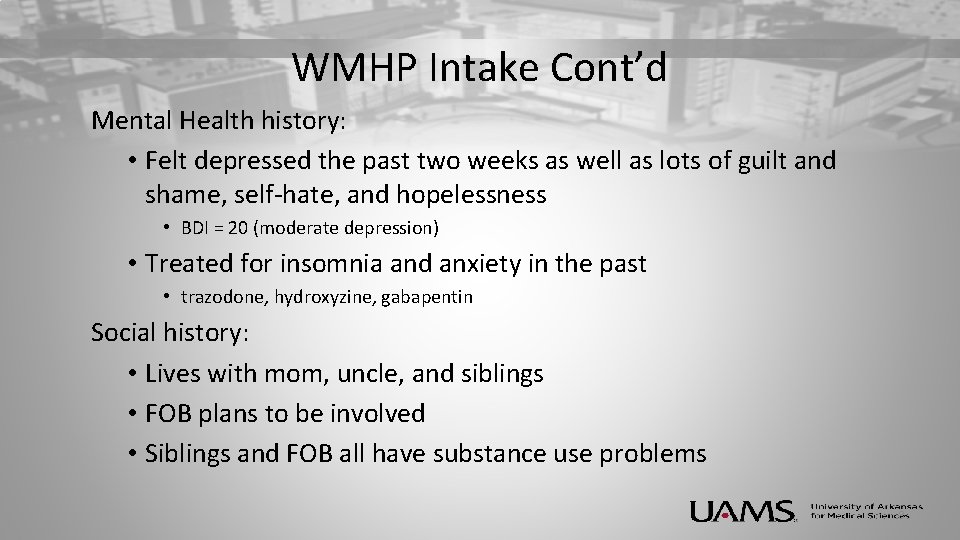
WMHP Intake Cont’d Mental Health history: • Felt depressed the past two weeks as well as lots of guilt and shame, self-hate, and hopelessness • BDI = 20 (moderate depression) • Treated for insomnia and anxiety in the past • trazodone, hydroxyzine, gabapentin Social history: • Lives with mom, uncle, and siblings • FOB plans to be involved • Siblings and FOB all have substance use problems 8
9
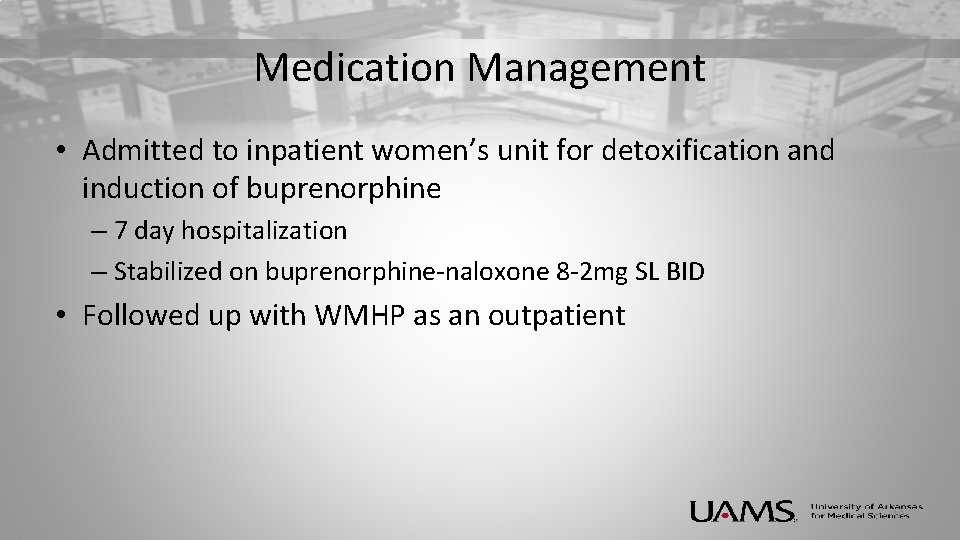
Medication Management • Admitted to inpatient women’s unit for detoxification and induction of buprenorphine – 7 day hospitalization – Stabilized on buprenorphine-naloxone 8 -2 mg SL BID • Followed up with WMHP as an outpatient 10
Behavioral Intervention • Skills-based group treatment: learning about, identifying, and avoiding “triggers”; coping with stress and uncomfortable emotions • Individual counseling: – Relapse Prevention: identify high risk situations that can trigger drug use and enhancing skills for coping, managing lapses – Cognitive Behavioral Therapy for anxiety: identify negative thinking and beliefs, helping patients change unhelpful thinking and behavior to improve mood and functioning 11
Pregnancy • “Star” patient • Consistently attended all MWHP appointments • Negative urine drug screens (weekly) for many months • Expressed extreme anxiety about the following: – Potential for DHS involvement – Relapse postpartum 12
Delivery • Described as “horrible” • C-section due to failure to progress • Uncontrolled pain • Baby with no signs of NAS • + breastfeeding 13
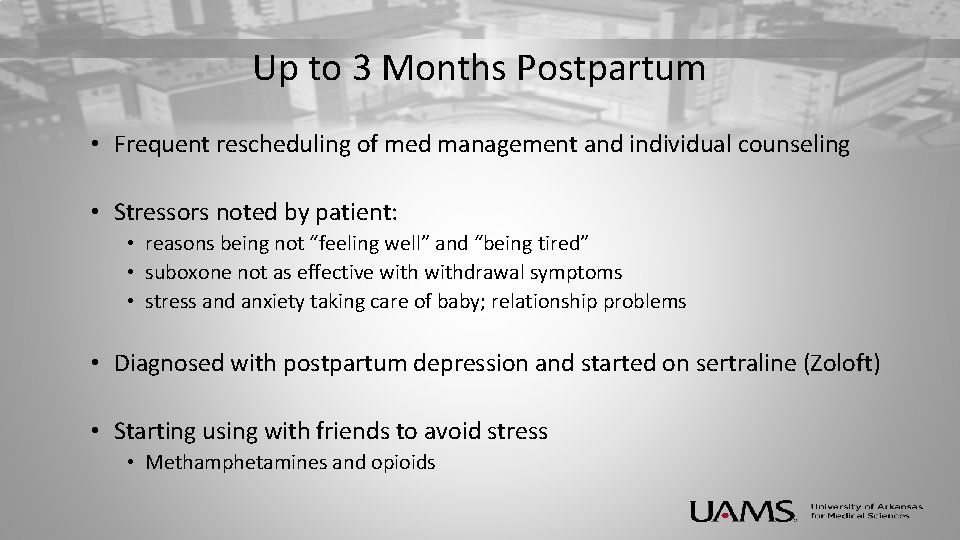
Up to 3 Months Postpartum • Frequent rescheduling of med management and individual counseling • Stressors noted by patient: • reasons being not “feeling well” and “being tired” • suboxone not as effective withdrawal symptoms • stress and anxiety taking care of baby; relationship problems • Diagnosed with postpartum depression and started on sertraline (Zoloft) • Starting using with friends to avoid stress • Methamphetamines and opioids 14
15
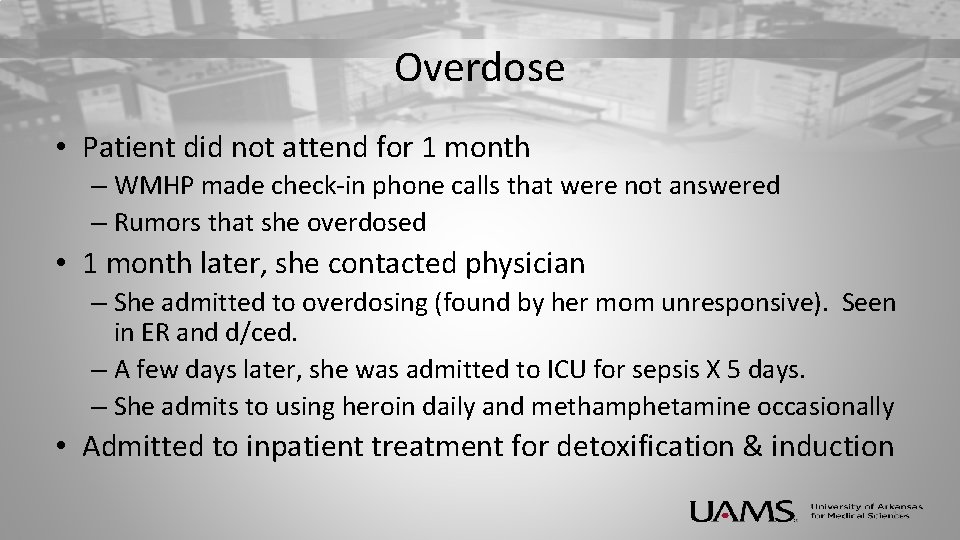
Overdose • Patient did not attend for 1 month – WMHP made check-in phone calls that were not answered – Rumors that she overdosed • 1 month later, she contacted physician – She admitted to overdosing (found by her mom unresponsive). Seen in ER and d/ced. – A few days later, she was admitted to ICU for sepsis X 5 days. – She admits to using heroin daily and methamphetamine occasionally • Admitted to inpatient treatment for detoxification & induction 16
17
Postpartum (post overdose) • Attended treatment regularly • Continued to relapse (positive UDS) • Pt reported high stress (due to caregiving, struggling with relationship with FOB and mother) as reasons for continued use. • Due to positive drug screens, patient was tapered off MAT. Discussed other options. Patient did not return to the WMHP. 18
Lessons Learned • Pt. indicated several months prior to delivery concern about relapse – is there something we could have done differently to prevent relapse? • Residential treatment was discussed as an option but not desired by patient – could we have done something differently to help her consider this option? • Other thoughts? 19
QUESTIONS ABOUT THE TOPIC Continuing Education Credit: TEXT: 501 -406 -0076 Event ID: 29152 -24581 20
CASE CONFERENCE AND FEEDBACK Continuing Education Credit: TEXT: 501 -406 -0076 Event ID: 29152 -24581 21
 Treatment of substance use disorder
Treatment of substance use disorder Somatic symptom disorder vs factitious disorder
Somatic symptom disorder vs factitious disorder Impulse control disorder treatment
Impulse control disorder treatment Impulse control disorder treatment
Impulse control disorder treatment Integrated dual disorder treatment
Integrated dual disorder treatment Somatic delusions
Somatic delusions Poss level
Poss level Opiyatlar grubu
Opiyatlar grubu Opiate tabelle
Opiate tabelle Opioid overdose
Opioid overdose Opioid overdose
Opioid overdose Opioid overdose
Opioid overdose Non-opioid
Non-opioid Mechanism of action of opioid analgesics
Mechanism of action of opioid analgesics Nips pain scale
Nips pain scale Opioid receptors location
Opioid receptors location Non-opioid
Non-opioid Opioid settlement calculator
Opioid settlement calculator Non-opioid
Non-opioid Kentucky opioid response effort
Kentucky opioid response effort Substance use disorder
Substance use disorder Why is environmental science considered interdisciplinary?
Why is environmental science considered interdisciplinary?