OFFICE OF THE CHIEF PSYCHIATRIST Mental Health Act


- Slides: 93
OFFICE OF THE CHIEF PSYCHIATRIST Mental Health Act 2014 Authorised Mental Health Practitioner Training This is a self-learning presentation for current AMHPs who wish to continue in the role Slide 1
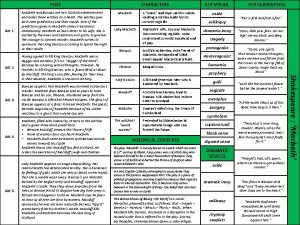
AMHP Program Expectations: • All AMHP participants must have completed the Clinicians ELearning Package (CELP); • All AMHP participants must have a working knowledge of the Clinician’s Practice Guide Edition 3(CPG); • All AMHP participants must have a working knowledge of the Chief Psychiatrist’s Standards (Addendum 1 CPG) • All AMHP participants must have a working knowledge of the Mental Health Act 1996 (MHA 96) • Completed minimum 2 hour F 2 F training or TTTP Slide 2
Background to the Mental Health Act 2014 • • • The MHA 14 received Royal Assent in November 2014 and commenced on 30 November 2015 The MHA 14 and the Regulations can be accessed on State Law Publishers website For consumers and carers there will are a number of resources including pamphlets developed by the Mental Health Commission.
This AMHP presentation will reinforce & highlight: What is in the MHA 14 specific to AMHPs Consider the power of referral Specifically look at the issue of capacity to consent to treatment Consider the powers of detention, revoking referrals and changing destinations The completion of legal Forms The role of AMHPs in relation to voluntary patients detained in authorised hospitals for assessment The role of AMHPs in confirming a Community Treatment Order Reporting to the Chief Psychiatrist What next?
Definitions AMHP- authorised mental health practitioner means a mental health practitioner designated as such by an order in force under section 539; Mental health practitioners A mental health practitioner is a person who, as one of the following, has at least 3 years’ experience in the management of people who have a mental illness — (a) a psychologist; (b) a nurse whose name is entered on Division 1 of the Register of Nurses kept under the Health Practitioner Regulation National Law (Western Australia) as a registered nurse; (c) an occupational therapist; (d) a social worker. (MHA 14 s. 538)
Definitions Authorised hospitals- a public hospital, or part of a public hospital, in respect of which an order is in force under section 542 or a private hospital the licence of which is endorsed under the Hospitals and Health Services Act 1927 (s. 541). Other placesa) an ED; b) a general hospital; c) a non-authorised mental health hospital including private hospitals; d) a community mental health or general health clinic; e) a nursing post particularly in remote areas of the state; and f) in appropriate circumstances a place of residence such as a residential home, hostel or where a person is living. (ref: CPG Addendum 2(b))
Police powers to apprehend Under MHA 96 the police can apprehend a person they suspect has a mental illness and take them to a place to be assessed by a medical practitioner or authorised mental health practitioner (AMHP) In addition under the MHA 14 - • If the person apprehended or arrested by police is not referred to be examined by a psychiatrist or cannot continue to be detained the practitioner must as soon as practicable inform the police. So details of the police officers who apprehended the person needs to be gathered • There is a need to document who informed the police, the name, rank and location of the police officer who was informed and the date & time they were informed. (s. 158) Slide 7
Referring a person for an examination by a psychiatrist at an authorised hospital or other place Referral Orders Form 1 A can be made by medical practitioners including psychiatrists and AMHPs if the practitioner reasonably suspects that a person is in need of an involuntary treatment order, or the person is on a CTO but is in need of an inpatient treatment order The term ‘reasonably suspects’ is a lower threshold than certainty so even if there are doubts as to whether the patient should be referred the practitioner may still, in the best interests of the patient, refer them for a psychiatric examination. Slide 8
Assessment: An assessment must be conducted in the least restrictive way and in the least restrictive environment The assessment must be conducted when the AMHP and the person are in one another’s physical presence; or if that is not practicable must be able to hear one another without using a communication device (for example, by being able to hear one another through a door); or when the person is in a non-metropolitan area and a face to face assessment is not practicable then the assessment can be conducted using Audio-Visual (AV) means (s. 48)
Assessments by AV means. That the person being assessed is in a non-metropolitan area but the AMHP need not be That a health professional- medical practitioner/ nurse/ social worker/ psychologist/ occupational therapist- or when assessing a person of Aboriginal or Torres Strait Islander (ATSI) an ATSI mental health worker or health professional is with the patient Guidance on use of AV is provided in Addendum 7 of the Clinician’s Practice Guide.
Assessment In making an assessment, information can be gathered directly from the person, their medical record or from a carer or family member. However, a referral cannot be made only on information obtained from another person or from the medical record. There needs to be some information obtained from an assessment made by the practitioner. Information provided in confidence and which should not be released to the referred person should be recorded in the attachment to the Form 1 A
Aboriginal or Torres Strait Islander (ATSI) If the person being assessed is of ATSI descent then, to the extent that it is practicable and appropriate, any assessment should be conducted in collaboration with an ATSI mental health worker and significant members of the person’s community, such as important family members, traditional healers or elders (CPG Addendum 5) For additional assistance State-Wide Aboriginal Mental Health Service can be contacted
Referrals The referral must be done within 48 hours of conducting an assessment (except when subject to Form 2) (s. 40) Referral orders last 72 hours and in non-metropolitan areas can be extended by a further 72 hours to a maximum of 144 hours (Form 1 B) The request for an extension can be made by the person transporting the referred person if the referral order will expire before the destination is reached If the practitioner who made the order cannot be contacted then the extension could be made by another medical practitioner or AMHP An extension of the Transport Order automatically occurs when a Referral Order is extended (s. 151) An AMHP cannot refer a person who is a relative, a person on a Guardianship Order to the referrer, or a person with whom the referrer is in partnership (for example in a business, or is an employer or employee of the person, for example their superior or subordinate in a work situation).
When referring a person for examination the AMHP must have regard to the criterion for involuntary status. Criterion 1 That the AMHP suspects the person has a mental illness requiring treatment. Section 6 provides a definition of mental illness(1) A person has a mental illness if the person has a condition that — (a) is characterised by a disturbance of thought, mood, volition, perception, orientation or memory; and (b) significantly impairs (temporarily or permanently) the person’s judgement or behaviour.
This definition is similar to the MHA 96 and reflects a decision based on the observations of identified behaviours rather than on a specific diagnosis. A decision whether or not a person has a mental illness must be made in accordance with internationally accepted standards prescribed by the Regulations – ICD 10 and DSM V The definition describes conditions characterised by a number of different types of disturbance which all indicate the presence of a possible mental illness. Ø Disturbance of thought or perception may indicate a type of psychotic illness such as schizophrenia. Ø Disturbance of mood and volition may indicate a mood disorder such as depression or mania. Ø Disturbance of orientation or memory may indicate an organic disorder such as dementia. In addition that the condition significantly impairs either temporarily or permanently the person’s judgement or behaviour.
The MHA 14 provides for a number of behaviours which in themselves or combined with other behaviours in the list would not indicate a mental illness. The list is similar to the list under the MHA 96. One major change is that ‘taking alcohol or drugs’ changes to ‘the person uses alcohol or other drugs’ but thatdoes not prevent the serious or permanent physiological, biochemical or psychological effects of the use of alcohol or other drugs from being regarded as an indication that a person has a mental illness. This recognises that some of the serious or permanent symptoms of alcohol and drug use such as depression, mania or dementia may all indicate that the person may also have a mental illness and may need to be referred even though they are exhibiting intoxication
Criterion 2 that, because of the mental illness, there is — (i) a significant risk to the health or safety of the person or to the safety of another person; or (ii) a significant risk of serious harm to the person or to another person; While the specific risks -financial, risk to reputation and risk to relationships have been removed the ‘catch-all’ “significant risk to health and safety significant risk of serious harm” will allow referral when risk is evident However the addition of the word ‘significant’ is significant and needs to be considered when assessing the person The Chief Psychiatrist’s standards & guidelines in the addendum to the CPG explores issues of risk (Standard 5 & Guideline 2 (a))
Criterion 3 that the person does not demonstrate the capacity required by section 18 to make a treatment decision about the provision of the treatment to himself or herself. Section 18. Determining capacity to make treatment decision A person has the capacity to make a treatment decision about the provision of treatment to themselves they must:
(a) understand the things that are required under section 19 to be communicated to the person about the treatment; and (b) understand the matters involved in making the treatment decision; and (c) understand the effect of the treatment decision; and (d) weigh up the factors referred to in paragraphs (a), (b) and (c) for the purpose of making the treatment decision; and (e) communicate the treatment decision in some way. If another person (substitute decision maker) is making that decision the above provisions also apply
What is Capacity? A person’s capacity is their mental ability to make a decision for themselves. Slightly different from ‘competence’ which is more of a legal term A person who has capacity can make decisions about things that affect their lives. This includes lifestyle decisions such as where to live, what to eat and what to buy. A person who has capacity can also make decisions about things that have legal consequences. This includes making a will, getting married or signing a contract. It also includes providing, or refusing to provide, consent to treatment for a mental illness.
Why is Capacity Important? Capacity is important for ethical, clinical and legal reasons. The concept of capacity reflects society’s strong ethical position for maintaining a person’s decisional autonomy and recognition that competence is essential for autonomy. Capacity is clinically important because it involves evaluating a person’s mental functioning. This requires obtaining a psychiatric history and mental status examination focusing specifically on functions relevant to decision making including attention, mood, thinking (form and structure), memory and cognitive function.
Capacity is legally Important A person with legal capacity has the right to make decisions for themselves and to have their decisions respected. A person with legal capacity also has the power to stop others from making decisions for him or her. Failure to respect a person’s legal capacity can also have legal consequences. Consent to treatment will be invalid if it has been given by a person who lacks decision making capacity, and provision of treatment to a person without consent or other lawful authority may give rise to civil and/or criminal sanctions. In the MHA 14 a person can only be made an involuntary patient if the person does not demonstrate decision making capacity.
Key Features of Capacity is not something solid that you can hold and measure. Neither is it something that is the same all the time. Rather, capacity is affected by a person’s abilities and by what’s happening around them. It varies from person to person, from situation to situation. It can also vary depending on the person’s mental or physical health.
An Adult’s Capacity must be Presumed At law, adults must be presumed to have decision making capacity. This includes adults with mental illness or with any other disability. Generally a person’s lack of capacity to make a decision must be positively established, and there must be good reasons for making a determination that a person lacks decision making capacity. Under MHA 14 a person is required to demonstrate they have the capacity to make treatment decisions. (s. 25(1)(c)) A person’s age, appearance, disability, behaviour, language skills or other conditions or characteristics should not lead to an assumption that the person lacks decision making capacity.
Capacity is Decision Specific Capacity is specific to the decision being made, and a person may have capacity to make some types of decisions but not others. A person’s capacity may depend on the type of decision being made, whether the decision is simple or complicated and the person’s familiarity with the particular matter. This means that a person’s capacity should be reassessed when a key decision needs to be made.
A Person’s Capacity may Fluctuate A person’s capacity may change over time and be affected by environmental and other factors. Inability to make a decision in the past does not determine inability to make decisions in the future It also depend on environmental factors such as the physical environment, the time of day, location, noise levels and who is present with the person. Capacity may be affected by personal stress or anxiety levels, medication, infection, drugs or alcohol, and by mental and physical health. The amount and type of information that has been given to the person and how well they understand the information may also be relevant. (s. 19)
A Person with Capacity has the Right to Make “Bad” Decisions A person’s decision doesn’t always have to be a good one, and not everyone will agree with the decisions that a person makes. There are however times when the decision that a person makes may prompt the need to assess the person’s capacity to make the decision. This includes where the decision puts the person at significant risk of harm or mistreatment. It also includes times when the person’s decision is different from the decisions that they would usually make. Deciding whether to assess capacity in these circumstances involves carefully balancing the person’s right to make a decision and the extent to which their health or safety, or the safety of others, might be in danger if they make that decision.
Capacity can be Regained A person may regain and/or increase their capacity. A person can learn new skills that will enable them to make decisions for themselves. For example learn to cook so they can live independently. A person with mental illness may have capacity to make decisions when well but not during periods of mental ill health.

When Should Capacity be Assessed? The presence of mental illness, or refusal to consent to treatment, are not generally enough, on their own, to trigger a capacity assessment. Capacity should however be assessed if mental illness is present and the person’s decision is very different from their usual decisions, conflicts with the person’s usual preferences, is at odds with the person’s best interests, or is different to the decision that most people would make in the circumstances. Capacity should particularly be assessed if the person’s decision puts themselves, or others, at risk of harm or mistreatment – that is, if the decision is “high stakes” and has potentially severe consequences.
When Should Capacity be Assessed? MHA 2014 When. A MP or AMHP is assessing a person and considering a Referral • A psychiatrist makes a decision about an Inpatient Treatment Order • A psychiatrist reviewing or making a decision about an Community Treatment Order • A patient is involved in decision about the level of involvement of personal support persons • Persons aged less than 18 years when any decision is required (as capacity is not assumed)
When Should Capacity be Assessed in a child? The Gillick Case: “the parental right to determine whether or not their minor child below the age of sixteen will have medical treatment terminates if and when the child achieves sufficient understanding and intelligence to understand fully what is proposed” Most adolescents by that age of 14 (and some as young as 12) when given adult-level information present as competent as adults in making treatment decisions. For this reason it is important to assess if a child has capacity to make a decision and include them in decision making processes (regardless of capacity) to provide templates for future decision making.
“Freely and voluntarily” In determining capacity to make decision it is stated that “a decision made by a person about a matter relating to himself or herself must be made freely and voluntarily” 15(2) When assessing capacity it is important to ensure that a decision is not made under duress or because of undue influence of other persons.
Information, advice and understanding Any communication “must be given in a language, form of communication and terms that the person is likely to understand using any means of communication that is practicable and using an interpreter if necessary and practicable” (s. 9(2) ) This means that care must be taken to ensure that the person has been given relevant information relevant appropriate to his or her circumstances. This includes ensuring that the information is in plain English, free of jargon and delivered in a way that is appropriate to the person’s age. It should also be given when appropriate in the person’s language if they are not English speaking.
“Understand any information or advice about the decision ” s 15 a, s 18 a Section 19 outlines the explanation that is required to be given when informed consent to a treatment decision is required: sufficient information to make a balanced judgement identifying and explaining any alternative Rx warnings of any risks Attention, concentration and ability to retain the information for a sufficient time period to come to a decision is required Reasonable person test A person’s ability to understand information given to them may be evaluated by asking the patient to paraphrase back information that is given; and a person’s ability to understand may be doubted if he or she gives an incongruent response
“Understand the matters involved in the decision” s 15 b, s 18 b Understand why the treatment is being offered and how it will impact on the person’s life. Understand the factors relevant to the risk and benefits of treatment. The inclusion of this criteria also ensures that the assessment of capacity takes into account the persons capacity to appreciate the impact of any treatment effects (positive and negative) on all aspects of their life (not just their physical and mental health).
“Understand the effect of the decision” s 15 c, s 18 c The person must be able to understand information on: v the consequences of making the decision one way or the other; v deferring the making of the decision; v failing to make the decision
“Weigh up Factors involved in decision” s 15 d, s 18 d All treatment decisions have a positive and negative effect. A person’s ability to use or weigh information in coming to a decision can be tested by considering. Has the person made the decision in a way that makes sense to us? Is the way that the person has made the decision the way that we would expect people generally to make decisions of this kind?
“Communicate the Decision” s 15 e, s 18 e Being able to communicate the decision indicates that the person has understood and weighed up the factors This element of the test is of relevance for people with communication difficulties, catatonia, or people who are otherwise extremely agitated and who are unable to communicate their decision by speech, by gesture, or by any other means, because of their disability or condition. The person considering if a person demonstrates capacity may not be able to determine this if the person is unable or unwilling to communicate.
Time for consideration s 20 The person making a decision should be be given time and support to make a the decision. A person cannot be asked to make a treatment decision unless the person is given – Sufficient time to consider the matters involved – A reasonable opportunity to discuss those matters with a health professional who is proposing treatment – A reasonable opportunity to obtain any other advice or assistance in relation to the treatment decisions that the person wishes
“Substitute” Decision Making For the purposes of Mental Health Act 2014 if a person does not have capacity to make decisions about a matter relating to himself or herself, the person authorised by law may make a decision on that person’s behalf The Act enables the transfer of responsibility for care decisions from the person, to a substitute decision maker, for the time that they are lacking in capacity, should the substitute decision maker be willing and available to make decisions including treatment decisions. • A parent or guardian of a child can make decisions on a child’s behalf. • The Guardianship and Administration Act 1990 outlines a hierarchy of substitute decision makers for adults that are lacking in decision making capacity
Supported decision making- Substitute Decision Making is a Last Resort Everything possible should be done to support a person to make a decision before the person is assessed as lacking decision making capacity. Such as • Communicating in a way that is appropriate for the person (using Plain English, non-verbal communication, or an interpreter if needed) • Giving the person sufficient information about the decision and its consequences • Choosing a time and place that puts the person at ease • Helping the person to get treatment for any medical condition that may be affecting their capacity • Helping the person to find someone to support them (such as a family member, friend or advocate)
Tips for Assessing Decision Making Capacity • • • Tell the person about the process. Explain that there are some concerns about their ability to make a particular decision, explain why they should participate in the process, and outline the likely outcome or outcomes. If possible, be flexible about when, where and how the assessment is conducted. If the decision can wait and the person’s capacity is fluctuating, consider delaying the capacity assessment process until the person is at their best. Take the person’s individual needs into account wherever possible. v In particular, consider the person’s language, communication and other needs and provide the person with assistance (an interpreter, support person, advocate or family member) if needed.
Tips for Assessing Decision Making Capacity • • • Consider the person’s cultural and linguistic diversity and how this may influence or impact on their decision making and bear this in mind when assessing the person’s capacity. Avoid value judgements and be objective and impartial about the person’s beliefs, values, preferences, feelings and emotions. Avoid undue influence. v Ask who else has been involved in the decision making process and if you suspect undue influence, try communicating with the person making the decision without others present. Also try to ask questions that will separate the views of the person, from the views of others.
Tips for Assessing Decision Making Capacity • Communicate clearly and avoid using jargon or complicated medical terminology. • Ask lots of open ended questions (rather than questions which have a “yes” or “no” answer), • Try to generate a discussion. Avoid leading questions or questions which suggest or guide the person to a particular answer, • Ask the person to repeat back to you, in their own words, their understanding of what has been discussed.
Tips for Assessing Decision Making Capacity Generally useful questions to ask include: • Tell me about your health now and what you think is wrong with your health • Can you tell me what you’ve decided about the treatment options that we’ve discussed? • Tell me about the treatment that you are currently having – do you think that the treatment is helping you? • Tell me about the treatment that we’ve discussed – do you think that the treatment will help you? How do you think that it will help you? • Are there any bad things about the treatment that you are having now or that we’ve discussed? • Are there any other treatments that you might be able to have? How do you think that those other treatments would help you? • In your own words, which do you think is the best treatment? Why?
Tips for Assessing Decision Making Capacity Useful questions to ask to determine whether the patient can understand relevant information (s 18 a, b and c): • What did your doctor tell you about the treatment and its risks and benefits? • What did your doctor tell you about other treatments? • What did your doctor tell you about your condition? • What do you think will happen if you have the treatment? • Did your doctor tell you what may happen if you have no treatment? What do you think will happen if you have no treatment? Useful questions to ask to determine whether the patient can weigh up the factors relevant to the decision: • Why have you decided to have (or not to have) the treatment? • What things were important to you in making the decision? • How did you balance those factors?
What To Do If You Aren’t Sure If you have any doubts after having conducted a capacity assessment about whether or not a person has decision making capacity, a second opinion should be sought. It may also be useful to seek a second opinion when the person does not agree with the outcome of your assessment or where there is disagreement between family members, carers and other professionals about whether or not the person has decision making capacity. This is particularly the case where the consequences of the person’s decision are significant. In relation to Referrals for Assessment the psychiatrist may make an order for involuntary treatment. The Mental Health Tribunal will ultimately decide whether or not the person lacks decision making capacity about treatment decisions through review of these orders.
Documentation The outcome of a capacity assessment should always be documented. It is also critical for clinicians to document how they came to a conclusion that a person has, or lacks, decision-making capacity. This documentation should be in the clinical notes.
Criterion 4 that the person cannot be adequately provided with treatment in a way that would involve less restriction on the person’s freedom of choice and movement than making an involuntary treatment order. Criterion 5 for inpatient orders that, treatment in the community cannot reasonably be provided to the person Criterion 6 for CTOs a significant risk of the person suffering serious physical or mental deterioration; and that treatment in the community can reasonably be provided to the person
Form 1 A A referral must be on an approved form (Forms 1 A) and must specify the following: a) the date and time the referral form was completed b) the date and time it will expire (which is 72 hours from the time it was completed unless (i) below applies, which relates to non-metropolitan areas) c) the place where the form was completed, for example a person’s home, an ED, a GP clinic d) the name of the authorised hospital or other place where the examination by the psychiatrist will take place e) the date and time when the assessment was completed, which cannot be longer than 48 hours from when the referral order is completed (exception is voluntary inpatient in AH who is subject to a Form 2 – referral decision must be made on completion of assessment)
f) details on which the suspicion that the patient needs to be an involuntary patient are based, differentiating between information directly obtained from the person, such as answers to questions, and observations from collateral information from other people or from the medical record g) the name and qualifications of the referring practitioner h) the signature of the practitioner which certifies that having considered the criteria in section 25, the practitioner reasonably suspects that the person is in need of an involuntary treatment order i) if the referral is in or from a non-metropolitan area, whether the referral was done by AV means or was extended and if it was extended what process was used (Form 1 B) Include information on which the suspicion is based Information that is not to be provided should be done on the Attachment to Form 1 A
• The referred person must be provided with the information on the Form, best done by giving them a copy of the form • Any information in the Attachment to Form 1 A must not be given to the referred person. • No time frame is given when the information should be provided so ‘as soon as practicable’ Note- A patient or someone else with sufficient interest can apply to the Mental Health Tribunal for a Treatment Order to be found invalid on the basis that the ‘there has been a failure to comply with the requirements of the Act in relation to the conduct of any assessment or the making of any referral order that led to the making of the treatment order’.
Under the MHA 96 revocation was not an option. Under the MHA 14 Referral Order can be revoked before receival Form 1 A • Can be revoked if a medical practitioner or AMHP is satisfied that the person is no longer in need of an involuntary treatment order. • The revocation can be done by another practitioner, but only if he or she has consulted with the referring practitioner as to why the order should be revoked • If the referring practitioner cannot be contacted despite reasonable efforts being made, then the other practitioner can decide whether to revoke the order without consulting the referring practitioner. • Any Transport Order Form 4 A attached to the Referral Order is automatically revoke
Detention of referred persons Detention of a referred person under the MHA 96 was under duty of care Under the MHA 14 Referred persons can be detained to enable them to be taken to the place of examination Form 3 A • • A Detention Order can only follow a Referral Order • Further periods of 24 hours of detention can be authorised following a further assessment to a maximum of 72 hours or in non-metropolitan areas where the referral has been extended to 144 hours • While reasonable force in the MHA 14 can be used in a number of situations, it can only be used for referred persons under the provisions of ‘duty of care’. A medical practitioner or AMHP, and not necessarily the medical practitioner or AMHP who made the referral, may make an order authorising the referred person’s detention for up to 24 hours from the time the detaining order is made Slide 54
Personal support person When a Detention Order is made ‘Notify personal support person’ A patient being admitted must be asked for contact details of their personal support person and if they would like that person to be involved in their care A personal support person is either a Ø Ø Ø Enduring guardian or guardian Child’s parent or guardian Nominated person Carer, or Close family member
• If a patient has more than one carer or close family member then it is sufficient compliance if at least one carer and one family member is involved. • If despite reasonable efforts the person cannot be contacted then it is reasonable for the person responsible to conclude that no carer or close family member can be provided with information • The practitioner could decide it is not in the person’s best interest to notify the personal support person • If a decision is made not to notify a personal support person a record of the decision and the reasons must be recorded and a copy given to the Chief Mental Health Advocate
• The practitioner must ensure that the referred person is given the opportunity, if they wish, to contact any personal support person, a current health professional or the Advocacy Service as soon as practicable after the order is made and at all reasonable times while the person is detained • • The referred person must be given a copy of the Form 3 A. Referred persons can be searched by a police officer or authorised person and certain articles seized – powers also apply to persons being admitted and returning from leave. Slide 57
Search and seizure Under the MHA 96 the police may search a person and seize certain articles. Additionally under the MHA 14 - • Police and authorised persons (person in charge of the ward/ staff member authorised by person in charge of the ward/ staff member of a mental health service/ health professional in a place that is not a mental health service) may search voluntary patients, referred persons, involuntary patients and MIAs in authorised hospitals • • • They may use reasonable force when conducting a search and ask another person to assist • • Other articles seized need to be stored or managed by the health service responsible Certain items can be seized if found during a search Form 8 A Anything seized which is thought to be illegal (guns or drugs) must be dealt with according to other laws If the person is released then anything seized must be returned to them Form 8 B Slide 58
Absence without leave (CPG 4. 10) (MHA 14 ss. 97 -101) If a detained person leaves without permission (absent without leave) every effort should be made to return the person. However if this is unsuccessful an Apprehension and Return Order Form 7 D can be made • • An Apprehension and Return Order authorises a police officer or person authorised by the Regulations (staff member)to apprehend and return a detained person who has left without permission Form 7 D A Form 7 D lasts for 14 days and cannot be extended The order can also be revoked if not required and the police officer or authorised person informed ‘Notify personal support person’ of the person being absent without leave Slide 59
Changing the place where the examination will be conducted (CPG 3. 11) Under the MHA 96 changing the place of examination was not an option. Under the MHA 14 changing the place is an option- • Following a medical practitioner or AMHP consulting with clinicians at the new destination, where the psychiatric examination will take place Form 1 B. (s. 46) • The patient, personal support person as well as those involved in transporting the person need to be informed of the new destination and a copy of the form given to the patient and placed in the patient’s medical record Slide 60
Emergency Psychiatric Treatment (EPT Form 9 A) Ø Under the MHA 96 EPT could be provided and that continues under the MHA 14 with the exception of ECT which can only be given in an emergency to adult involuntary patients with the Chief Psychiatrist’s approval. Ø A copy of the EPT form must be given to the person and a copy forwarded to the Chief Psychiatrist Ø The Chief Psychiatrist recognises that medical practitioner may prefer to use duty of care under the doctrine of necessity instead of EPT Slide 61
Transport Orders Form 4 A (s. 149) A Transport Order should only be made if assistance is needed from either a police officer or a transport officer to take the referred person to an authorised hospital or other place for examination by a psychiatrist, because of the referred person’s condition and where no other safe means of transport is reasonably available A transport order should never be automatically completed just because a referral order or detention order is made. An independent judgement needs to be made by the referrer as to whether a police officer or transport officer is needed.
Transport Orders continued If transport can be safely provided by the hospital or community staff, perhaps with the assistance of a relative or ambulance service then that is the preferred, less restrictive process for transporting a referred person. There is no requirement for a transport order if the person can be safely transported by the ambulance service without assistance from the police or transport officer. Similarly there is no requirement under the Act for transport by the Royal Flying Doctor Service (RFDS) to always include a transport order.
Transport Officers • Transport officers are a new role for people authorised to carry out a Transport Order and have similar powers to police to apprehend, detain, restrain and transport • Using transport officers are the preferred method when a Transport Order Form 4 A is completed.
Transport Officers • Authorising a police officer to assist with transport should only be done if there isØ A significant risk of serious harm to the person being transported or another person, or Ø A transport officer is not available to carry out the transport within a reasonable time and Ø Any delay is likely to pose a significant risk to the person or another person. • Police officers and transport officers are authorised to use reasonable force when apprehending and transporting a referred person
Transport Orders for referred persons • If a transport order is needed a medical practitioner or AMHP (and not necessarily the referring practitioner) must complete a Transport Order Form 4 A • Transport Orders last 72 hours or expires at the time the Referral Order expires. • If the referral is from a non-metropolitan area and the police officer or transport officer thinks that the referral order will expire before getting to the destination, then he or she may verbally request an extension of the referral order from a medical practitioner or AMHP (up to 144 hours) • If this occurs the Transport Order is automatically extended Slide 66
• If a Referral Order is revoked or expires then the Transport Order also expires. • A Transport Order can also be revoked, even though the referral continues, when assistance by a police officer or transport officer is no longer needed. • A medical practitioner, AMHP or mental health practitioner can revoke a Transport Order by making a Revocation Order Form 4 A and the police or transport officer informed. • Inform Personal Support person’ Slide 67
Transport Orders for referred persons continued • If a Transport Order is revoked or expires while the person is being transported, the police officer or transport officer must take reasonable steps to make sure that the person is taken at their request to either the place where the person was transported from or to another place reasonably nominated by the person • The practitioner must give a copy of the Transport Order to the patient and the police or transport officer who is carrying out the transport • If a Transport order is made or revoked-‘Notify personal support
Making a Community Treatment Order The MHA 96 introduced Community Treatment Orders (CTOs) as an option for community care. The MHA 14 makes the following changes- • CTOs can be made following an examination, with or without a referral, by AV means in a non-metropolitan area (s. 79) • If it was made without a referral order the CTO must be confirmed by a medical practitioner or AMHP (s. 76) Slide 69
Confirming a CTO Should be an independent review of the decision to place the person on a CTO. Although not legislated for it would be best practice for the confirming practitioner to examine the person, discuss the issues with significant others such as carers and relatives and reach a conclusion that the patient meets the criteria for being on a CTO. The AMHP needs to complete the Confirming a CTO section on the Form 5 A Deviation from best practice may be appropriate in extenuating circumstances but would require clear documentation as to why this has occurred. A confirming examination can be done via AV means in non-metropolitan areas. If the confirming practitioner does not believe that the criteria are met, he or she should not confirm the CTO and if an order is not confirmed the CTO immediately ceases to be in force. (s. 76) It would not be acceptable for the psychiatrist to then request another practitioner to confirm the order.
Mental Health Advocacy Service (CPG Chapter 8) The Advocacy Service replaces the MHA 96 Council of Official Visitors The term ‘Affected person’ such as involuntary patients and residents of private psychiatric hostels is replaced by the term ‘identified person’ In addition identified persons include a person referred under the MHA 14 to be examined by a psychiatrist at an authorised hospital or other place The referred person should be given the opportunity and means to contact an advocate as soon as practicable after being referred and at reasonable intervals If the referred person is detained they can request contact from the MHAS within 72 hours Slide 71
Mental Health Tribunal Under the MHA 14 the Tribunal replaces the Mental Health Review Board In addition to reviewing involuntary status the Tribunal can review- • • • The validity of Involuntary Treatment Orders Decisions affecting rights Applications for compliance notices Slide 72
Compliance notices for non-clinical matters (CPG 9. 10) • A patient, personal support person, an advocate, or another person who in has an interest can apply to the Tribunal for a compliance notice regarding: Ø The giving of a document to a patient or another person; Ø Include a document in the patient’s medical record; Ø Comply with a request made by a patient or other person; Ø Preparing, reviewing or revising the treatment, support and discharge plan • Compliance notices are not about treatment decisions • At a review the Tribunal can hear from the patient, or the person to whom the compliance notice relates, the service provider or any other person • Having reviewed the matter, the Tribunal can decide to take no action, or direct the service provider to take specific action within a time period and report back on the action taken Slide 73
Chief Psychiatrist (CPG 11. 1 & Addendum 1) Under the MHA 96 the Chief Psychiatrist has a number of responsibilities and duties. Under the MHA 14 the Chief Psychiatrist is responsible for involuntary patients, MIAs in authorised hospitals and residents of private psychiatric hostels. Additionally the Chief Psychiatrist is responsible for overseeing the treatment and care of voluntary patients
Chief Psychiatrist As required by the MHA 14 the Chief Psychiatrist has published standards & guidelines for the treatment and care of patients as well as monitoring compliance with the standards through a review processes (s. 190) The standards & guidelines specifically relevant to AMHPs include: • • Assessment Standard • Making decisions about whether authorised hospital or other place is appropriate for examination (Addendum 2 Guideline (c)) • Compliance with approved forms (Addendum 2 Guideline (g)) (ref: CPG addendum) Risk Assessment and Management Standard Aboriginal Practice Standard Making decisions about whether or not a person is in need of an ITO (Addendum 2 Guideline (a)) Where there is no specific Chief Psychiatrist Standard the Standards from the National Standards for Mental Health Services (2010) apply
• all voluntary patients of a mental health service. This includes patients at a hospital (general or psychiatric) who have or may have a mental illness or patients of a community mental health service • all voluntary patients who have been referred under the MHA 14 for an examination by a psychiatrist at an authorised hospital or other place. The Chief Psychiatrist will publish standards for the treatment and care of patients as well as monitoring compliance with those standards through a review processes.
Responsibilities for the Chief Psychiatrist for AMHPs includes: Designate a mental health practitioner as an AMHP if satisfied that the practitioner has the qualifications, training and experience to perform the functions of an AMHP under this Act by order published in the Government Gazette By mutual agreement a mental health service and a mental health practitioner may apply to the Chief Psychiatrist for the practitioner, if they meet the criteria, to be designated as an AMHP.
The Chief Psychiatrist may specify any limits or any conditions subject to which those functions can be performed by the AMHP. For example, the Chief Psychiatrist may limit the role so the person can only function as an AMHP while working for a particular service or in a particular clinical role. The decision to authorise or revoke a mental health practitioner is the responsibility of the Chief Psychiatrist.
The Chief Psychiatrist must keep a register of AMHPs to be determined by the Chief Psychiatrist. The register must include: a) the AMHP’s name b) the date on which the order designating the person as an AMHP was published in the Government Gazette c) any limits within which, or any conditions subject to which, the person can perform the functions of an AMHP that were specified in the order d) the date on which any order was amended and published in the Gazette with details of the amendments e) the date on which any AMHP status was revoked and published in the Gazette.
Duties of an AMHP The Chief Psychiatrist can designate a mental health practitioner as an AMHP if satisfied that the practitioner has the qualifications, training and experience to perform the functions of an AMHP under this Act by order published in the Government Gazette A mental health practitioner may apply to the Chief Psychiatrist for the practitioner, if they meet the criteria, to be designated as an AMHP, however an application requires the approval of the Executive Director or Clinical lead.
The Chief Psychiatrist may specify any limits or any conditions subject to which those functions can be performed by the AMHP. For example, the Chief Psychiatrist may limit the role so the person can only function as an AMHP while working for a particular service or in a particular clinical role. The Chief Psychiatrist will not authorise a mental health practitioner who works for an agency such as Nurse. West The decision to authorise or revoke a mental health practitioner is the responsibility of the Chief Psychiatrist.
The Chief Psychiatrist must keep a register of AMHPs to be determined by the Chief Psychiatrist. The register must include: a) the AMHP’s name b) the date on which the order designating the person as an AMHP was published in the Government Gazette c) any limits within which, or any conditions subject to which, the person can perform the functions of an AMHP that were specified in the order d) the date on which any order was amended and published in the Gazette with details of the amendments e) the date on which any AMHP status was revoked and published in the Gazette. The Chief Psychiatrist must ensure that the register of AMHPs is available for inspection by members of the public free of charge from the Office of the Chief Psychiatrist during business hours and on the Chief Psychiatrist’s website. (s. 540) There is an AMHP page on the OCP website with all the names of AMHPs which is updated regularly
The AMHP role is voluntary and you can resign at any time. Please discuss resignation with your Manager so they are aware you will not be continuing in the role You can resign by completing the Request for Revocation Form on the OCP website and sending it to the Consultant, Statutory Authorisations and Approvals (Cate Wray) You can stop operating as an AMHP immediately however taking you off the register usually takes a few weeks. If you are changing your workplace complete the Change of Workplace Form on the OCP website and send it to the Consultant, Statutory Authorisations and Approvals (Cate Wray).
If you are changing your name complete the Change of Name Form on the OCP website and send it to the Consultant, Statutory Authorisations and Approvals (Cate Wray) If you are taking extended leave (maternity) contact Cate Wray by telephone or email to discuss whether you should resign or stay on the Register. The OCP has NOTHING to do with the remuneration provided to some AMHPs. Need to discuss those issues with your manager
Expectations for continuation of AMHP authorisation Annual continuing professional development (CPD) approved by the Chief Psychiatrist: AMHP are expected to undertake regular Continuing Professional Development (CPD) hours which will maintain, improve and broaden knowledge, expertise and competence required to maintain registration.
CPD records may include participation in the following activities: • Tertiary, vocational and other accredited courses including distance education (needs to relate to context of practice) • Conferences, forums, seminars and symposia • Short courses, workshops, seminars and discussion groups through a professional group or organisation who may issue a certificate of compliance/completion. • Mandatory learning activities in the workplace in the area of practice • Self-directed learning, i. e. A report on the literature searches with references to the articles that you have read;

If you are selected for audit you will be required to submit a document similar to the example in Table 1 below, which provides evidence of completing your CPD. Available on OCP website Date Provider Details Title of Activity Evidence Provided CPD Hours / / Agency name Education session Certificate 2
Annual Clinical Supervision approved by the Chief Psychiatrist: Clinical Supervision is recognised by the Chief Psychiatrist as having a focus on professional growth and practice improvement of the AMHP. It is recommended that supervision meetings are facilitated on a regular monthly basis for at least one hour. There a number of different clinical supervision formats of which two are outlined below; • Individual supervision: one-on-one clinical supervision meeting which may be held face-to-face or using media such as telephone or videoconferencing. • Peer group supervision: more than two clinicians are included in the clinical supervision process for the discussion of key clinical issues in order to provide solutions for difficult clinical scenarios. The participants learn better/alternative ways to manage professional problems and reduce stress.
Required expectations for continuation of AMHP authorisation Annual Clinical Supervision approved by the Chief Psychiatrist: All mental health clinicians have a responsibility to seek clinical supervision as outlined in the Professional Code of Conduct of their employer and by their professional group. Please refer to your relevant college or board regarding these standards. Documentation that relates to confidential information shared by clinicians during clinical supervision may be accessed by third parties in some circumstances. Third parties may access confidential information pursuant to a subpoena, a search warrant, in disclosure requirements of a criminal case, Freedom of Information Act 1992 or under the Coroner’s Act 1996.
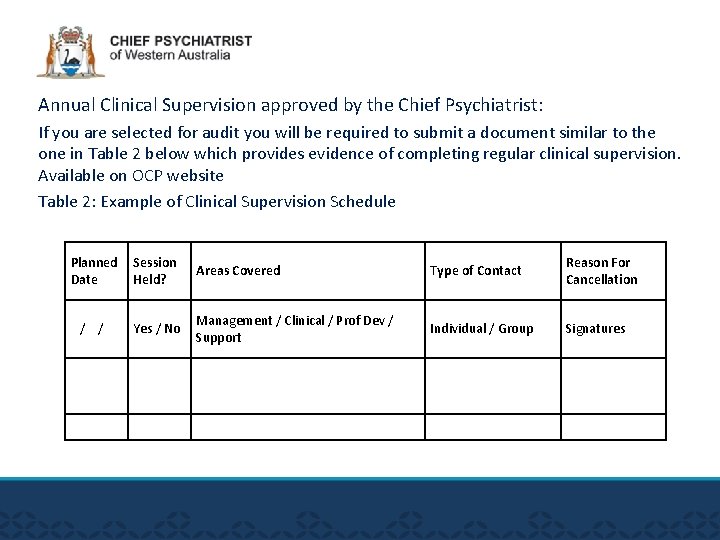
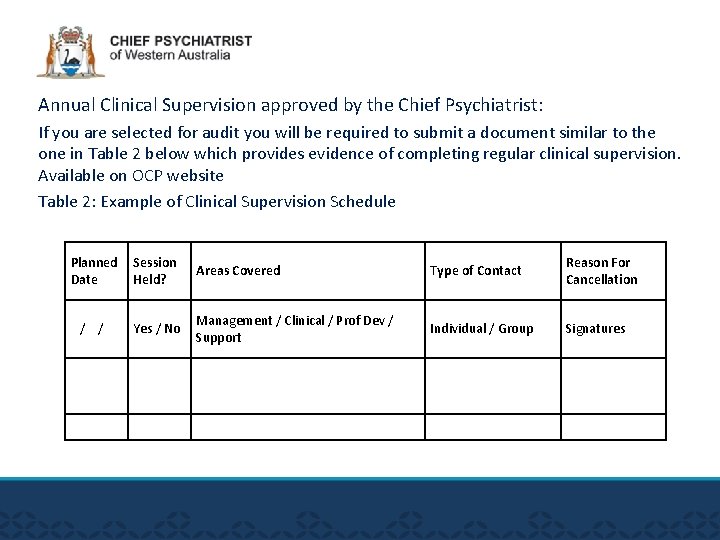
Annual Clinical Supervision approved by the Chief Psychiatrist: If you are selected for audit you will be required to submit a document similar to the one in Table 2 below which provides evidence of completing regular clinical supervision. Available on OCP website Table 2: Example of Clinical Supervision Schedule Planned Date Session Held? Areas Covered Type of Contact Reason For Cancellation / / Yes / No Management / Clinical / Prof Dev / Support Individual / Group Signatures
• Grounds on which the designation must be revoked • The AMHP has requested revocation in writing • No longer registered AHPRA or eligible for AASW membership • If the person is no longer a mental health practitioner because they have taken up a management or project officer position. • CP is notified in writing that AMHP has resigned, retired, died • Grounds on which the designation may be revoked • failure to complete CS, CPE, CP approved training; submit reports • AMHP is incapable, is mentally or physically impaired or incompetent in performing the functions, or has engaged in misconduct
• If you have now completed all the components required to be gazetted please contact Cate Wray on cate. wray@ocp. wa. gov. au
Clinical Helpdesk P: (08)65530000 Email: mha 2014@ocp. wa. gov. au Or amhp@ocp. wa. gov. au
 Lesson 3 commander in chief and chief diplomat
Lesson 3 commander in chief and chief diplomat Chapter 20 mental health and mental illness
Chapter 20 mental health and mental illness Stress management jeopardy
Stress management jeopardy The mental health act 2007
The mental health act 2007 Law enforcement mental health and wellness act
Law enforcement mental health and wellness act Office of the government chief information officer
Office of the government chief information officer Usda office of the chief financial officer
Usda office of the chief financial officer Chief scientist office scotland
Chief scientist office scotland Dr steve pearce oxford
Dr steve pearce oxford Dr hoosen psychiatrist
Dr hoosen psychiatrist David ash psychiatrist
David ash psychiatrist Professor shanaya rathod
Professor shanaya rathod Donna grant psychiatrist
Donna grant psychiatrist Psychiatrist vs psychologist
Psychiatrist vs psychologist Peter byrne psychiatrist
Peter byrne psychiatrist Dr fernandez psychiatrist
Dr fernandez psychiatrist John hillery psychiatrist
John hillery psychiatrist Expert in consultant liaison psychiatrist
Expert in consultant liaison psychiatrist Shahid hussain psychiatrist
Shahid hussain psychiatrist Dr marinda joubert
Dr marinda joubert Broadmoor hospital inmates
Broadmoor hospital inmates Dr rebecca lawrence psychiatrist
Dr rebecca lawrence psychiatrist Psychiatrist leicester
Psychiatrist leicester Dr derek lovell psychiatrist
Dr derek lovell psychiatrist Dr simon howard psychiatrist
Dr simon howard psychiatrist Uuuu0
Uuuu0 Dr moghul
Dr moghul Dr fionnuala o'loughlin psychiatrist
Dr fionnuala o'loughlin psychiatrist Macbeth summary
Macbeth summary 5 mca principles
5 mca principles The vulnerable persons living with a mental disability act
The vulnerable persons living with a mental disability act Mental capacity act 2005 easy read
Mental capacity act 2005 easy read Mental capacity act 2005 summary
Mental capacity act 2005 summary Fair housing act mental illness
Fair housing act mental illness 5 principles of the mental capacity act
5 principles of the mental capacity act Statutory principles of the mca
Statutory principles of the mca 5 principles of the mental capacity act
5 principles of the mental capacity act Mental capacity act assessment
Mental capacity act assessment Macbeth's mental state in act 3
Macbeth's mental state in act 3 What is a met call
What is a met call Lenawee county cmh
Lenawee county cmh Van buren cmh
Van buren cmh Chapter 3 lesson 3 expressing emotions in healthful ways
Chapter 3 lesson 3 expressing emotions in healthful ways Together for mental health
Together for mental health Mental health triangle examples
Mental health triangle examples Mental health presentation titles
Mental health presentation titles Health committee introduction
Health committee introduction Public mental health
Public mental health Mental health nursing definition
Mental health nursing definition Definition of nursing diagnosis
Definition of nursing diagnosis Mental health programme
Mental health programme Objectives of national mental health programme
Objectives of national mental health programme Benefits of phr
Benefits of phr How to make a mind map in photoshop
How to make a mind map in photoshop 2016494500
2016494500 Mental health toolbox talk
Mental health toolbox talk Mental health documentation training
Mental health documentation training Mental health equity
Mental health equity Mental health ordinance
Mental health ordinance Schizophrenia def
Schizophrenia def Learning outcomes definition
Learning outcomes definition Mental health and older adults
Mental health and older adults Mental health problems examples
Mental health problems examples Objective for mental health awareness
Objective for mental health awareness Poem on mental health awareness day
Poem on mental health awareness day Health and wellness trivia
Health and wellness trivia Billy corgan mental health
Billy corgan mental health Mental health america of san diego county
Mental health america of san diego county Individual service plan mental health example
Individual service plan mental health example How sports affect mental health
How sports affect mental health Mobile crisis outreach team houston
Mobile crisis outreach team houston Mental health and older adults
Mental health and older adults Influence of culture on mental health
Influence of culture on mental health Mental health and citizenship
Mental health and citizenship Chapter 3 achieving mental and emotional health
Chapter 3 achieving mental and emotional health Chapter 21 mental health diseases and disorders
Chapter 21 mental health diseases and disorders Bexar county mental health services
Bexar county mental health services Thomas snyder mental health
Thomas snyder mental health Example of emotional health
Example of emotional health Chapter 3 mental and emotional health
Chapter 3 mental and emotional health Mental health equity
Mental health equity Reach institute mental health
Reach institute mental health Mental health connection of tarrant county
Mental health connection of tarrant county Traffic light safety plan mental health
Traffic light safety plan mental health Sparks police report
Sparks police report Steps to mental health recovery
Steps to mental health recovery Psychology, mental health and distress
Psychology, mental health and distress Pet therapy mental health
Pet therapy mental health Oklahoma department of mental health
Oklahoma department of mental health Nymhca
Nymhca Primary mental health northumberland
Primary mental health northumberland Mental health policy, plans and programmes michelle funk
Mental health policy, plans and programmes michelle funk Mental health lawyers association
Mental health lawyers association Mental health continuum mhfa
Mental health continuum mhfa