History taking mental state examination Dr Shahid Hussain








- Slides: 32
History taking & mental state examination Dr: Shahid Hussain ST 6 Psychiatry of Acute Care
Lets revise • To assess the patient to identify any mental health difficulties. • Can be therapeutic. • Strongly variable on the basis of time, place & patient.

Set the scene • • Privacy & Confidentiality Try to avoid interruptions Safety- Seating arrangement Note taking
General principles • Put the patient at ease • Introduce yourself & anyone accompanying you & explain the role • Length of interview
Interview style • Keep relax & in control even in difficult situation • Appropriate eye contact, appear interested • Begin with a general question eg “tell me about your problem” • Have a systematic but flexible approach • May need to interrupt

Interview techniques • Open questions where possible • Closed questions can be helpful • Avoid leading questions eg “You have a poor appetite, don’t you? ”
Interview techniques • May need to explain the rationale of certain questions, eg abuse, criminal record etc. • Summarise to check understanding • Don’t take words at face value eg “paranoid” • Pick up non-verbal cues • Encourage patient by leaning forward, nodding, saying “go on” “tell me more about…. . ”
Collateral information • Always useful particularly if patient is cognitively impaired, patient is concealing information etc • Often best to see patient alone first and then with informant • Ascertain informants concerns as well as gather information. • Interview patients in first language where possible. May need interpreter • Symptomatology, cultural beliefs & treatment expectations may vary
History • Presenting Complaint • History of presenting complaint • Family History • Personal History • Past Psychiatric History • Past Medical History • Substance Use • Drug History • Forensic History • Personality • Current Social Situation
Presenting Complaint(s) • • Mode of referral Where is patient being seen. Presentation status eg informal etc What is their problem, in their own words
History of presenting complaint • Nature of problem • Chronology of each symptom • Onset & duration • Severity of symptoms & Degree of functional impairment Precipitating factors • Perpetuating factors Protective factors • Factors worsening or improving • Treatments trialled
Past psychiatric history • Similar or other symptoms in the past • Psychiatric diagnosis • Psychiatric admission • Any treatments (drugs, psychotherapy, psychosocial interventions, from primary care, counselling, CAMHS etc ) • ECT • Outcomes of treatment, any recovery, remission etc • Suicide, DSH attempts

Past medical history • Full medical history • Endocrine, CNS, systemic illness • Chronic medical conditions: diabetes, ischemic heart disease, epilepsy, asthma (use of steroids), CCF, stroke • Chronology of illnesses, hospitalizations • Recovery
Medications history • Current medications • All drugs taken for psychiatric or medical illness: dose, duration and outcome • Drugs that may precipitate psychiatric disorders • Side effects of psychiatric medication • Allergies • May need to check with the GP
Family history • Family tree to include patient’s siblings and parents eg adoptees, biological etc, separation, divorce, steps • Pt’s nature of relationship with the family & among family • Nature of death if any one not alive • Known or suspected Hx of mental illness • Suicides, suicidal behaviours or Hx of DSH in relatives • Hx of substance misuse

Personal history • Mother’s pregnancy • Neuro-developmental milestones – birth, walking, talking, sitting & socializing age • Childhood separation or emotional problems • Home & school environment (Bullying, school refusal, shyness, conduct disorders) • Schooling and academic achievements • Relationships with friends and family
Social history • Profession and employment record, Current employment • Financial situation in general • Current and past debt problems, spending etc • Marital status – single, married, divorced, widowed • Children – ages if dependent, parental responsibility • Housing situation, past and present-living alone • Stressors • Social supports • Typical day
Forensic history • Past and present charges, penalties, arrests and convictions (Violence/Anger, sexual offences etc) • Pending court cases • Unrecorded offences • Relationship to symptoms & substance misuse
Pre morbid personality • Life long persistent characteristics prior to illness • Moral and religious beliefs • Leisure activities and hobbies • How would others eg relatives/friends describe them
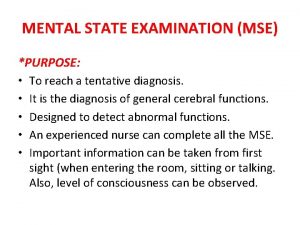
Mental state examination • Here and now • Hx- Symptoms • More reliant on observation & skilful exploration • History suggest relevant cluster of pathologies.

Appearance and behaviour • Body language & appropriateness of dress • Evidence of self neglect • Under or over psychomotor activity – excitation or retardation • Facial expression – dilated pupils, rigidity • Abnormal movements or posture • Rapport & eye contact • Distractibility • Disinhibition Preoccupation
Speech • Rate, tone & volume • Level of coherence • Rate: slow in depression; pressured in mania. • Quantity: poverty in depression & chronic schiz: • Pattern: spontaneous, coherence, circumstantial, trivial details eg obsessional traits, perseveration • Neologisms, word salad, FTD: loosening of associations
Mood • Subjective description-Sad, happy, top of the world, worried, up & down. • Objective • Range: depression – euthymic – euphoria • Inability to enjoy activities (anhedonia) • Inability to describe one’s emotion (alexithymia)
Affect • Your objective description of emotion • Depressed, anxious, fearful, irritable, suspicious, perplexed, elated, angry • Fluctuations: reactivity, lability (mania), blunting (chronic schizophrenia) • Congruent with thoughts/behaviour?

Thought • Pre-occupations: thoughts that recur frequently but can be put of mind eg obsessions, phobias & rituals • Form & content • Obsessions- ideas, images, doubts & images • Delusion. . out of keeping with the patient’s social & cultural background. • Primary & secondary delusions • Delusional perception: eg traffic light change means chosen to be Messiah.
• Content: persecution, infidelity, grandiose, hypochondriacal, love, guilt, nihilistic, poverty, reference, infestation. • Derealisation & depersonalization • First rank symptoms • Thought insertion, withdrawal, broadcast • Voices- echo, running commentary & 3 rd PAH • Passivity affect, action & impulse
Perceptions • Illusions • Hallucinations • Auditory (2 nd, 3 rd) visual gustatory, olfactory (organic, TLE), tactile (cocaine addiction, drug withdrawals) Pseudo-hallucinations Hypnopompic/hypnogogic hallucinations Functional/Reflex hallucinations Extracampine

Cognition • Orientation to time, place & person • Test short term and long term memory • Determine subjective and objective concentration levels • Carry out a MMSE • Separate poor concentration from memory problems
Insight • Awareness of abnormal state of mind • Insight rests on a continuum from being partially insightful to having insight • Ask the patient if they think they are ill • Mentally or physically • Ask the patient if they are willing to accept help • Ask the patient if they will take treatment

Multiaxial System • Axis I: Clinical Disorders and Other Conditions That May Be a Focus of Clinical Attention • Axis II: Personality Disorders and Mental Retardation • Axis III: General Medical Conditions • Axis IV: Psychosocial and Environmental Problems • Axis V: Global Assessment of Functioning
Useful Reading • Lecture notes- Psychiatry • Shorter Oxford Textbook of Psychiatry (ed) Gelder, Harrison & Cowen • Fish’s Clinical Psychopathology, Casey & Kelly • Sims’ Symptoms in the Mind, Femi Oyebode • Psychiatric Inteviewing and Assessment, Poole & Higgo
This is to certify that: . . Has reviewed/completed. . . History Taking & Mental State Examination. . Date. . . . .
 Shahid hussain psychiatrist
Shahid hussain psychiatrist Valori mmse
Valori mmse Mental status exam example
Mental status exam example Shahid ghori
Shahid ghori Shahid arju moni secondary barisal
Shahid arju moni secondary barisal Sohaib shahid
Sohaib shahid Shahid sattar aptma
Shahid sattar aptma Soill
Soill Nabil shahid
Nabil shahid Shahid sattar aptma
Shahid sattar aptma Anjum asim shahid rahman
Anjum asim shahid rahman Jordan fox passif
Jordan fox passif Dr shahid aziz
Dr shahid aziz Mse in psychology
Mse in psychology Types of thought process
Types of thought process A full mental status examination example
A full mental status examination example Mental status examination purpose
Mental status examination purpose Vamc slums
Vamc slums Hussain manawer poems
Hussain manawer poems Dr azhar hussain
Dr azhar hussain Mohamed father in law
Mohamed father in law Hussain mujhko maaf karna
Hussain mujhko maaf karna Hanin hussain
Hanin hussain Rosie hussain
Rosie hussain Mam sehrish
Mam sehrish Waris husain
Waris husain Zahin hussain
Zahin hussain Maria hussain leeds
Maria hussain leeds Journey of imam hussain
Journey of imam hussain Tarif-i-hussain shahi
Tarif-i-hussain shahi Maria hussain leeds
Maria hussain leeds Asaad hussain
Asaad hussain Hussain
Hussain