PEDIATRIC HISTORY TAKING Dr Pourmirzaiee History Taking Definition




- Slides: 40

PEDIATRIC HISTORY TAKING Dr. Pourmirzaiee
History Taking - Definition • History taking can be defined as a systematic inquiry into the patient’s condition. • It is the process of obtaining relevant information from the patient or patient’s caretaker (such as the mother or father) for the purpose of making a diagnosis. • The pediatric history is the foundation upon which the future physician/ patient/ parent relationship is built.
Objectives • To understand the content differences in obtaining a medical history on a pediatric patient compared to an adult. • To understand how the age of the child has an impact on obtaining an appropriate medical history. • To highlight the role of parents during taking pediatric history.
Objectives • To highlight the fact that modern technology must be used when appropriate only to enhance the clinical assessment of the patient, not to replace it. • Understand the appropriate wording of questions in taking a pediatric history, and appropriate use of questions. • Children are not just small adults!
Goals of the history • To determine why the patient/parent came to see the physician. • To determine what the patient/parent is worried about most and why. • Direct appropriate examination and investigation • Reach a correct diagnosis (or form a differential diagnosis)
Differences of a Pediatric History Compared to an Adult History II. Parent as Historian • Parent’s interpretation of signs, symptoms o Children above the age of 4 may be able to provide some of their own history o Reliability of parents’ observations varies o Adjust wording of questions - “When did you first notice Majid was limping”? instead of “When did Majid’s hip pain start”? • Observation of parent-child interactions • Parental behaviors/emotions are important
Listening to Mothers
Listening to Mothers • A good doctor is a good listener. • Mothers are excellent observers of their children and do know when they are sick. • She may not know what’s wrong but she certainly knows something is wrong. • No one can replace the mother in providing an accurate and thorough description of the child and his complaints.
Listening to Mothers • Ask her to define her terms (What do you mean by. . . ? ). • A good opening is, ‘Tell me about your baby’, and then simply let the mother talk. • Learn through history taking to be a good listener.
Listening to Mothers • Always ask the parents to relate the sequence of events leading to the present complaints. • A suitable start ‘When was he last well? ’ • Patients appreciate a doctor who gives them individual attention and devoted time. • Mothers may, of course, unintentionally deceive. • A common complaint is: ‘I can’t get him to eat anything’ and a strong overweight toddler!
Listening to Mothers • Always ask the parents to relate the sequence of events leading to the present complaints. • A suitable start ‘When was he last well? ’ • Patients appreciate a doctor who gives them individual attention and devoted time. • Mothers may, of course, unintentionally deceive. • A common complaint is: ‘I can’t get him to eat anything’ and a strong overweight toddler!
Outline of the Pediatric History
History – General, Personal • • • Date Patient's name Birth date……. . Age Gender, be careful to use the correct gender Residence The person giving the history (relationship to patient and perceived reliability)

Presenting complaint - Chief complaint • In the patient's or parent's words. • A brief statement of the primary problem (including duration). • It is important to establish the duration of each complaint.
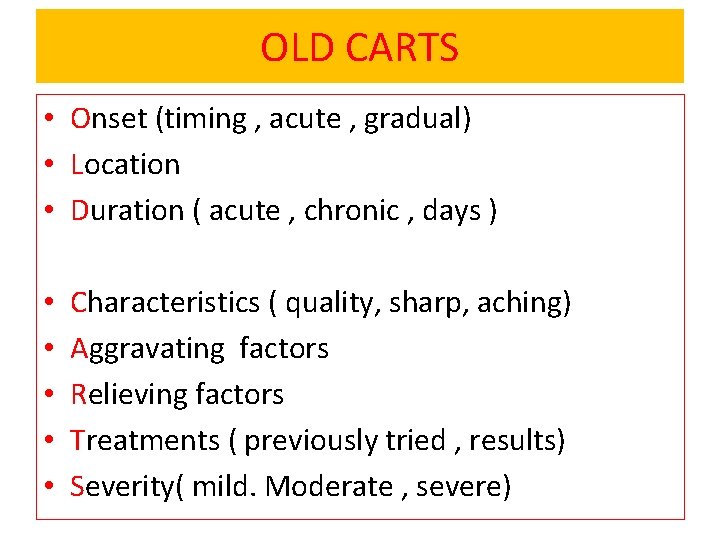
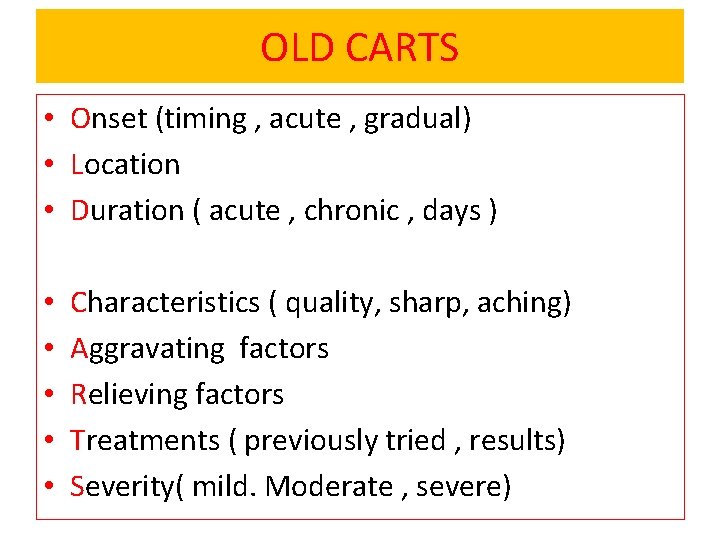
OLD CARTS • Onset (timing , acute , gradual) • Location • Duration ( acute , chronic , days ) • • • Characteristics ( quality, sharp, aching) Aggravating factors Relieving factors Treatments ( previously tried , results) Severity( mild. Moderate , severe)
History of the Present Illness • Any significant prior laboratory or radiology studies should be noted here. • Child maltreatment or abuse should be considered if the history and physical exam are not consistent with one another or if there is a delay in seeking care.
Past Medical History • • • Hospitalizations Surgeries Drug allergies Vaccinations Recent travel Recent exposure
Past Medical History • The relative importance of these items depends on: – the age of the patient and – the reason for the visit • In general, the birth history is not significant for an acute minor trauma visit for an adolescent!
Perinatal history • Prenatal: o Length of gestation. Age of mother at delivery o Any maternal insults [alcohol, smoking] or illnesses during gestation. • Natal: o Where born: hospital, clinic, home. o Birth weight, mode of delivery, difficulties in delivery. o Resuscitation, Apgar score • Postnatal: o Cyanosis, pallor, jaundice, convulsions, malformations, feeding or respiratory difficulties. o How baby was fed in first few days. o Whether the child went home with mother
Developmental history • Age when able to… – Hold head erect when in sitting position – Roll from front to back; back to front – Sit alone; unsupported – Stand with support; without – Use words – Talk in sentences – Dress self – Age when toilet trained

Social History
Social history - Items • Living accommodation • Who lives at home with the patient, including extended family members • Age and parents' occupation • Level of parental education • Sibling relationships • The type of discipline used
Social history - Items • School performance (Education history) • Any others at daycare/ school with the same complaint. • Travel: where, how lived when there, immunization/ prophylactic status when went. • Smokers in the home. • Pets in the home. • Nationality and migration of parents.
Social History
Family history • Families share genes and diseases. • A family tree that includes the last two generations. • Childhood diseases or adult diseases with childhood onset. • History of unexplained recurrent miscarriages or SIDS.
Family history • • Neonatal deaths. Parents/siblings: age, health, where living. Height and weight of parents. Age of parents at the birth of this child.
Let The Children Speak
Let The Children Speak • Don’t forget the child!! • Children need to be heard and to be noticed. • Children over 4 years should be asked to give their account of events with parental comments. • If he does not like to talk, or shy don’t push him.
Case study
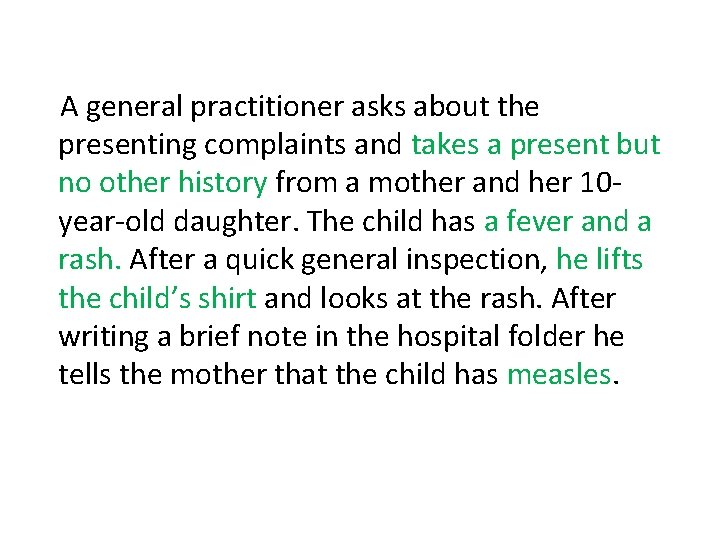
A general practitioner asks about the presenting complaints and takes a present but no other history from a mother and her 10 year-old daughter. The child has a fever and a rash. After a quick general inspection, he lifts the child’s shirt and looks at the rash. After writing a brief note in the hospital folder he tells the mother that the child has measles.
1. What mistake has the doctor made in taking a history?
1. What mistake has the doctor made in taking a history? Only a present history was taken. It is important always to take a past, social and immunization history as well.
2. Why is an immunization history important? It is important to know whether this child has been fully immunized, especially against measles and rubella.
A general practitioner asks about the presenting complaints and takes a present but no other history from a mother and her 10 year-old daughter. The child has a fever and a rash. After a quick general inspection, he lifts the child’s shirt and looks at the rash. After writing a brief note in the hospital folder he tells the mother that the child has measles.
What is a problem list? • This is a clear & simple list of the patient’s problems. • The problem list is drawn up during the assessment at the end of the complete examination. • The problem list is the most important part of summarizing the findings of the history, physical examination and investigations. • A problem list must always be made even if the diagnosis is not known.
History Taking - Summary • Personal History: Name, age, sex and address • Complaint: Main symptom(s) that necessitate medical advice • Present History: Onset, course and duration including medical care given (if any) • Past History: Perinatal, developmental, nutritional, vaccinations, …. • Social History: Home and school • Family History: siblings, similar conditions

Thank You
 Pediatric history and physical examination
Pediatric history and physical examination Pinkham pediatric dentistry
Pinkham pediatric dentistry Trends in pediatric nursing
Trends in pediatric nursing Define child health nursing
Define child health nursing Pediatric nursing definition
Pediatric nursing definition Oldcarts
Oldcarts Abcde sample
Abcde sample History taking respiratory system
History taking respiratory system Pc hpc pmh dh
Pc hpc pmh dh Polypus vesicae felleae
Polypus vesicae felleae Mse history taking
Mse history taking Crapriop
Crapriop Ros history taking
Ros history taking Physical exam for abdominal pain
Physical exam for abdominal pain Lodcraft history taking
Lodcraft history taking Principles of physical assessment
Principles of physical assessment Orthopedic history taking
Orthopedic history taking History taking paediatrics
History taking paediatrics The art of history taking
The art of history taking Components of history
Components of history Systemic review
Systemic review Socrates abdominal pain
Socrates abdominal pain Lodcraft history taking
Lodcraft history taking History taking
History taking Marcus gunn pupil
Marcus gunn pupil Acute dysphagia
Acute dysphagia Jaundice history taking
Jaundice history taking Smoking history taking
Smoking history taking Ddsep 8
Ddsep 8 Systematic review in history taking
Systematic review in history taking Lodcraft history taking
Lodcraft history taking Relevance of note making
Relevance of note making Unc chapel hill hematology oncology
Unc chapel hill hematology oncology Miami pediatric nephrology seminar
Miami pediatric nephrology seminar Headache red flags
Headache red flags Pediatric seizures
Pediatric seizures Pediatric vital signs
Pediatric vital signs Plasmlyte
Plasmlyte Pediatric vision scanner
Pediatric vision scanner Pediatric urologist atlanta
Pediatric urologist atlanta Spo2 normal range by age chart
Spo2 normal range by age chart