Eric Lazar MD Pediatric Surgery for the Pediatric


- Slides: 61
Eric Lazar, MD Pediatric Surgery for the Pediatric Board Review
Common versus uncommon conditions
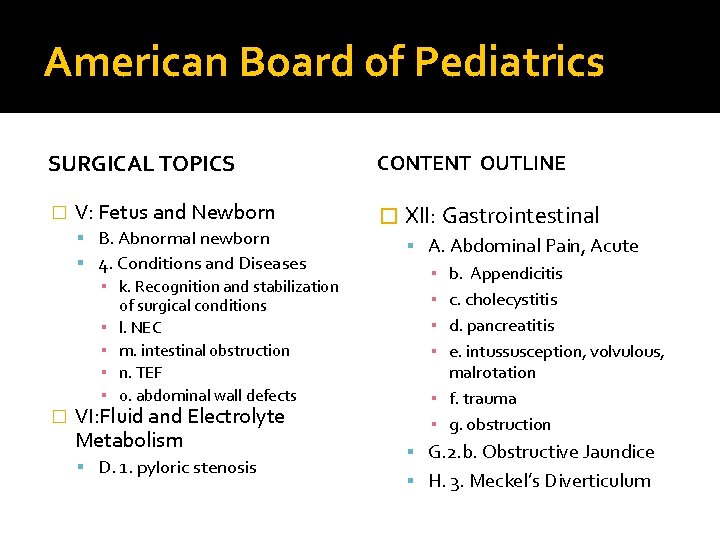
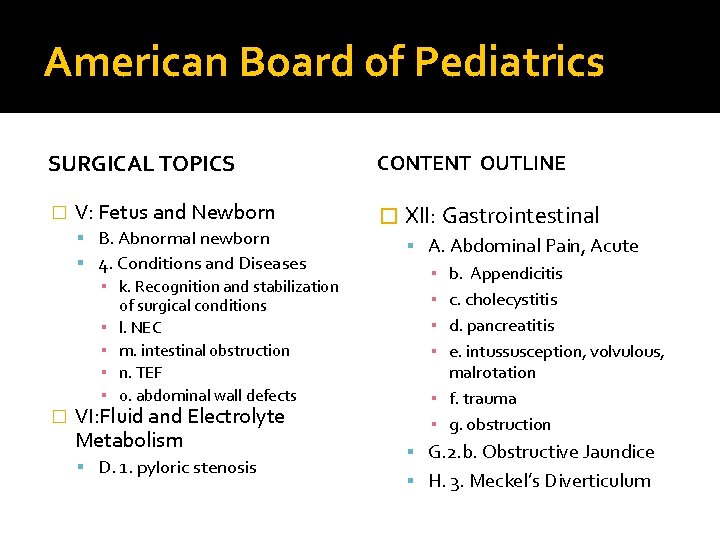
American Board of Pediatrics SURGICAL TOPICS � V: Fetus and Newborn B. Abnormal newborn 4. Conditions and Diseases ▪ k. Recognition and stabilization of surgical conditions ▪ l. NEC ▪ m. intestinal obstruction ▪ n. TEF ▪ o. abdominal wall defects � VI: Fluid and Electrolyte Metabolism D. 1. pyloric stenosis CONTENT OUTLINE � XII: Gastrointestinal A. Abdominal Pain, Acute ▪ b. Appendicitis ▪ c. cholecystitis ▪ d. pancreatitis ▪ e. intussusception, volvulous, malrotation ▪ f. trauma ▪ g. obstruction G. 2. b. Obstructive Jaundice H. 3. Meckel’s Diverticulum
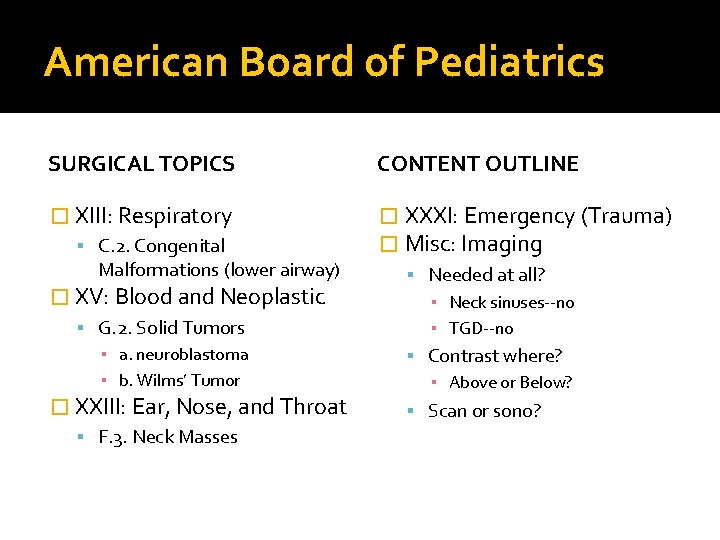
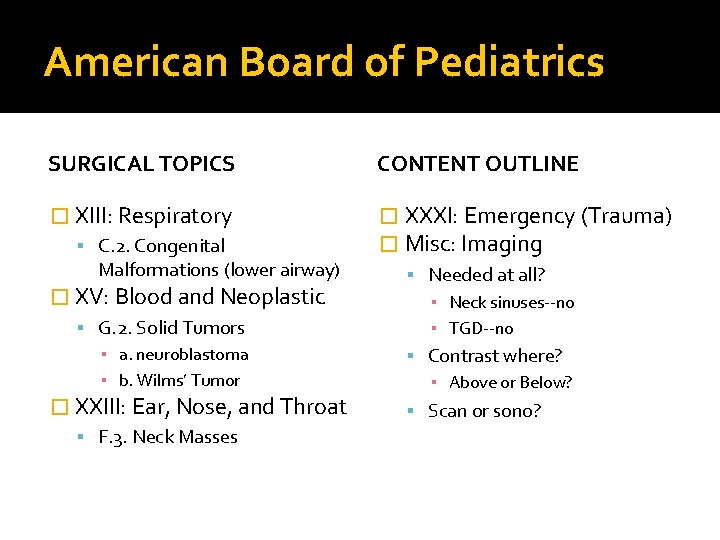
American Board of Pediatrics SURGICAL TOPICS CONTENT OUTLINE � XIII: Respiratory � XXXI: Emergency (Trauma) � Misc: Imaging C. 2. Congenital Malformations (lower airway) � XV: Blood and Neoplastic G. 2. Solid Tumors ▪ a. neuroblastoma ▪ b. Wilms’ Tumor � XXIII: Ear, Nose, and Throat F. 3. Neck Masses Needed at all? ▪ Neck sinuses--no ▪ TGD--no Contrast where? ▪ Above or Below? Scan or sono?
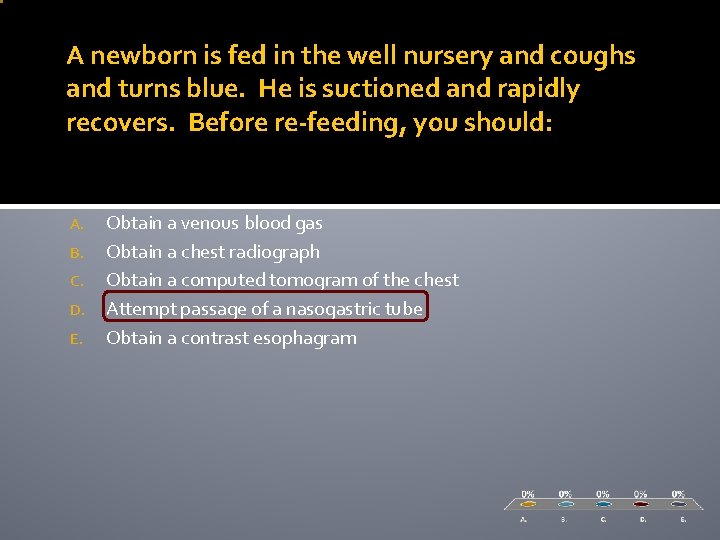
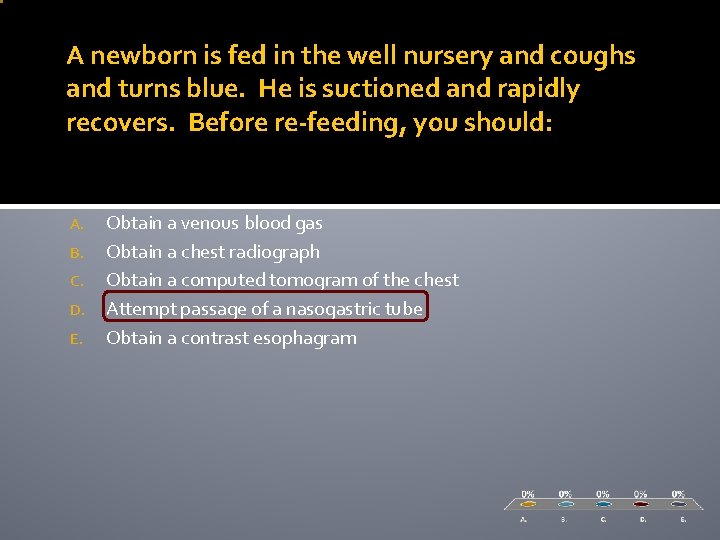
A newborn is fed in the well nursery and coughs and turns blue. He is suctioned and rapidly recovers. Before re-feeding, you should: A. B. C. D. E. Obtain a venous blood gas Obtain a chest radiograph Obtain a computed tomogram of the chest Attempt passage of a nasogastric tube Obtain a contrast esophagram
Surgical Causes of Newborn Respiratory Distress (V. b. 4. k; XIII. c. a) � Virtually no anatomic cause of newborn respiratory distress requires emergent surgery. (exception: airway lesions) � A period of resuscitation and investigation is almost always mandated and usually reveals the nature of the defect.
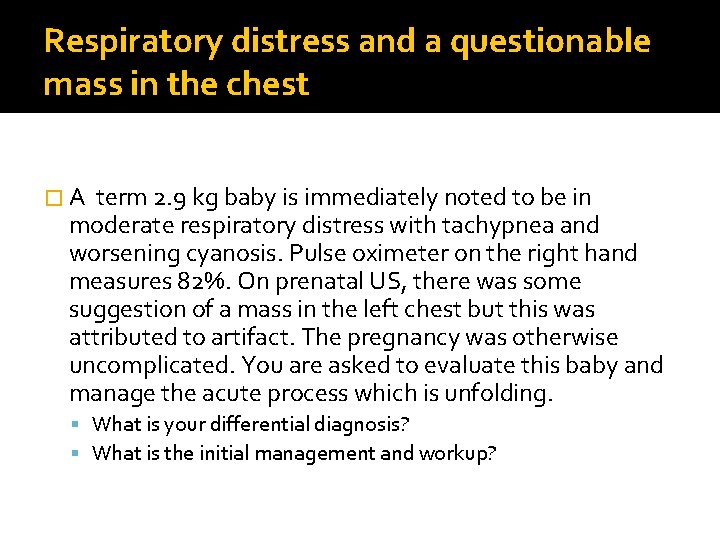
Respiratory distress and a questionable mass in the chest �A term 2. 9 kg baby is immediately noted to be in moderate respiratory distress with tachypnea and worsening cyanosis. Pulse oximeter on the right hand measures 82%. On prenatal US, there was some suggestion of a mass in the left chest but this was attributed to artifact. The pregnancy was otherwise uncomplicated. You are asked to evaluate this baby and manage the acute process which is unfolding. What is your differential diagnosis? What is the initial management and workup?
What is your differential diagnosis �Congenital diaphragmatic hernia �Congenital cystic adenomatoid malformation (CCAM) now CPAM �Pulmonary sequestration Intralobar Extralobar �Congenital Lobar Emphysema �Bronchogenic Cyst
How would you manage this patient �ABC’s- don’t hesitate to intubate this patient. Excessive bagging for most of these infant is not a good idea �PE: scaphoid abdomen; bowel sounds in chest; decreased breath sounds �Labs and lines �Pre and post ductal saturation probes �NGT is critical �CXR stat
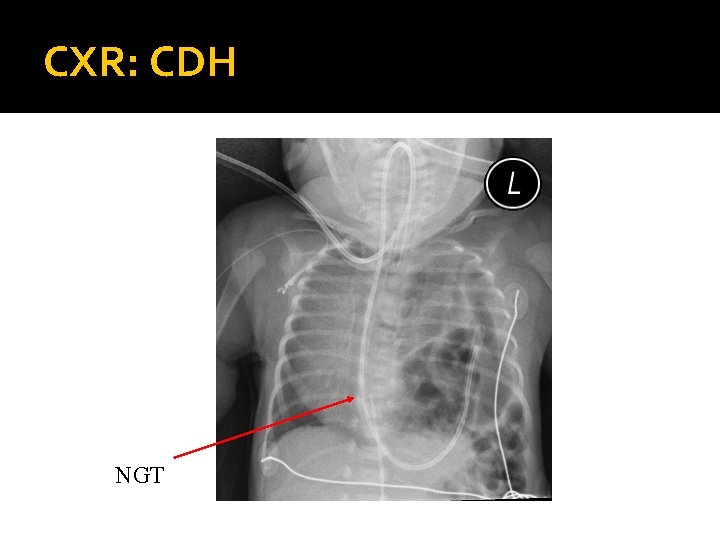
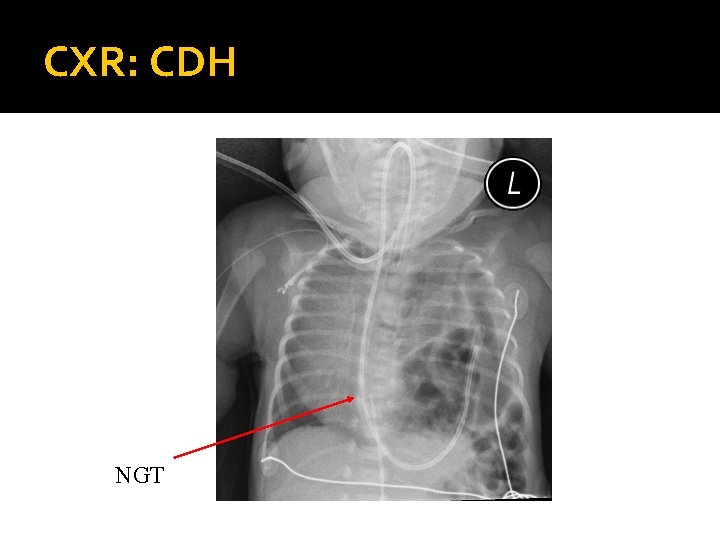
CXR: CDH NGT
Treatment: CDH � Delayed surgical approach; not a surgical emergency � Conventional Vent, Oscillator, “gentle ventilation”, possible ECMO (10 -15%) � Primary repair; patch sometimes needed � Overall survival 50 -80 %

Pearls: CDH � Bochdalek: posterolateral defect; usually on left � Morgagni: retrosternal (anterior); presents late � Lung hypoplasia affects both sides. � Pulmonary HTN / persistent fetal circulation are the greatest challenges. � Most repairs do not necessitate a postoperative chest tube. � Honeymoon period can end very quickly!
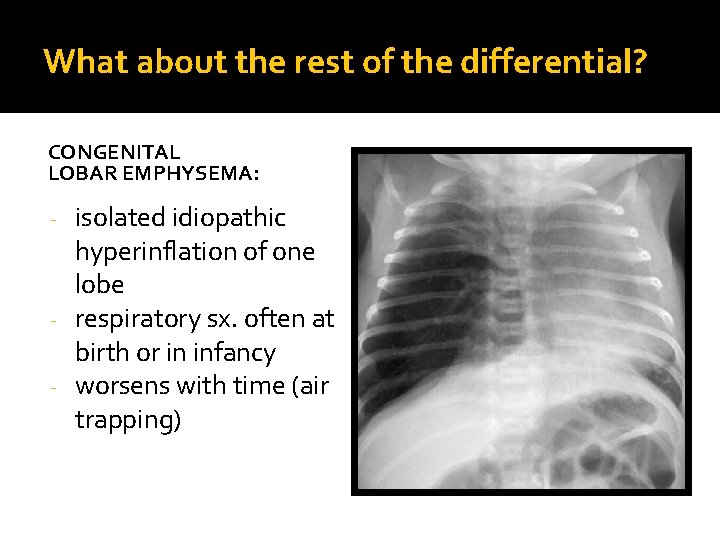
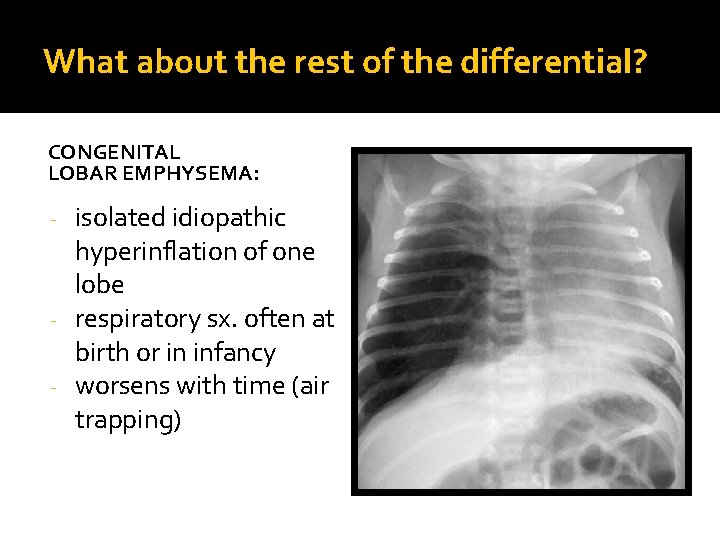
What about the rest of the differential? CONGENITAL LOBAR EMPHYSEMA: isolated idiopathic hyperinflation of one lobe - respiratory sx. often at birth or in infancy - worsens with time (air trapping) -
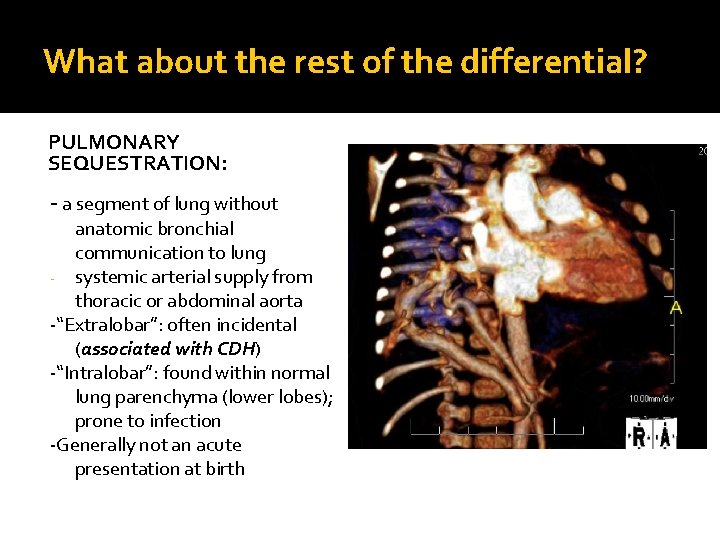
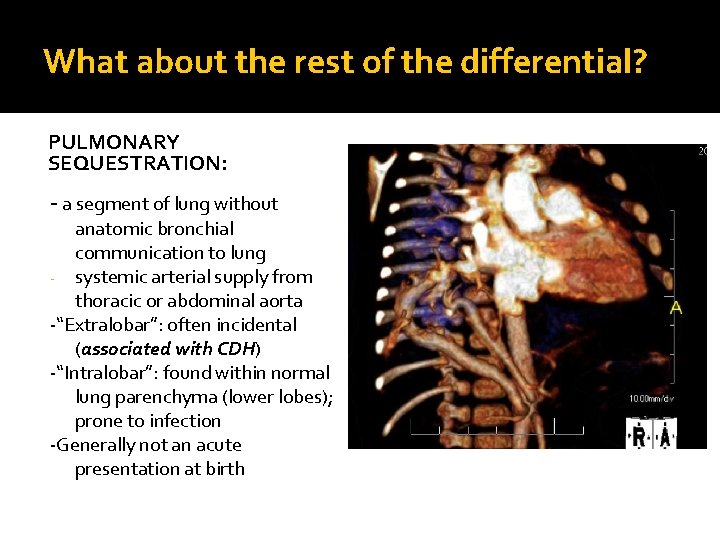
What about the rest of the differential? PULMONARY SEQUESTRATION: - a segment of lung without anatomic bronchial communication to lung - systemic arterial supply from thoracic or abdominal aorta -“Extralobar”: often incidental (associated with CDH) -“Intralobar”: found within normal lung parenchyma (lower lobes); prone to infection -Generally not an acute presentation at birth
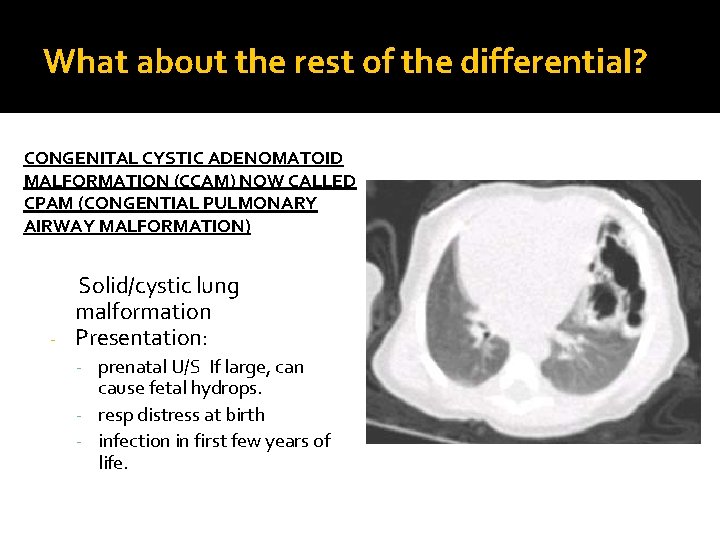
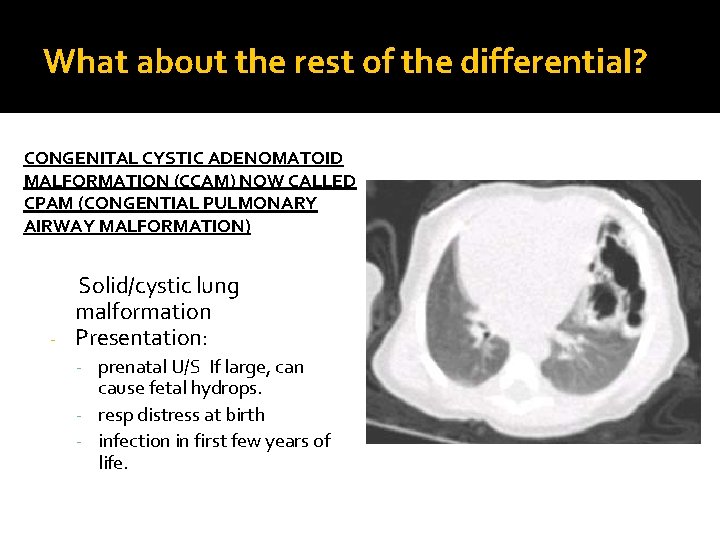
What about the rest of the differential? CONGENITAL CYSTIC ADENOMATOID MALFORMATION (CCAM) NOW CALLED CPAM (CONGENTIAL PULMONARY AIRWAY MALFORMATION) Solid/cystic lung malformation - Presentation: - prenatal U/S If large, can cause fetal hydrops. - resp distress at birth - infection in first few years of life.
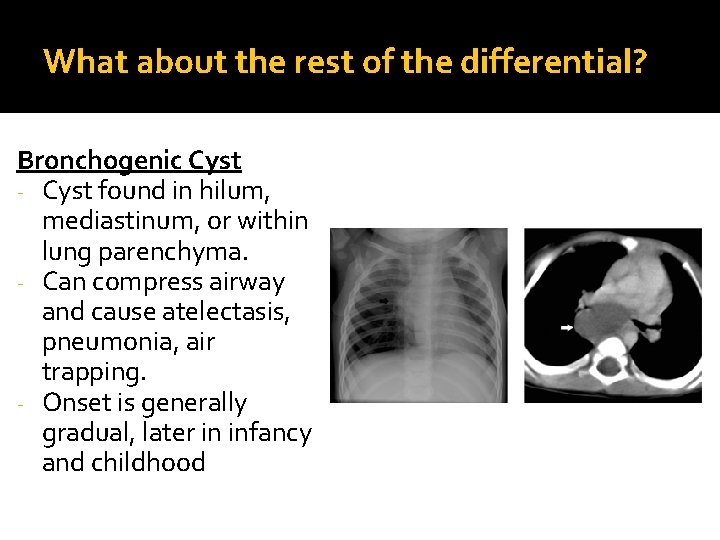
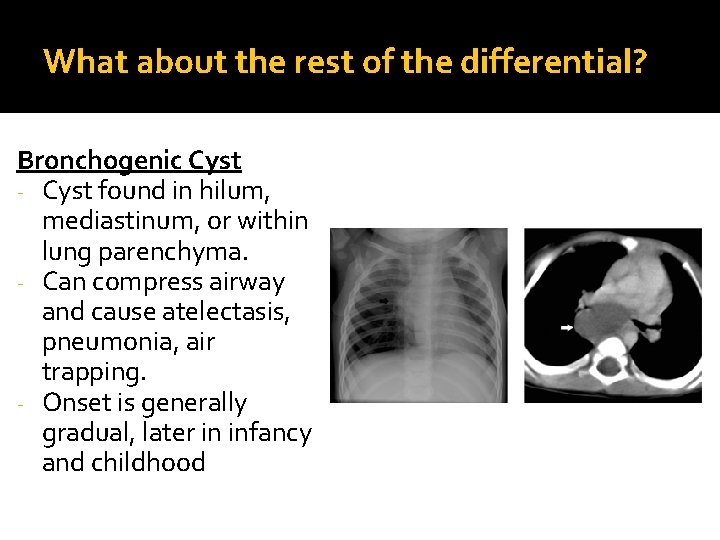
What about the rest of the differential? Bronchogenic Cyst - Cyst found in hilum, mediastinum, or within lung parenchyma. - Can compress airway and cause atelectasis, pneumonia, air trapping. - Onset is generally gradual, later in infancy and childhood
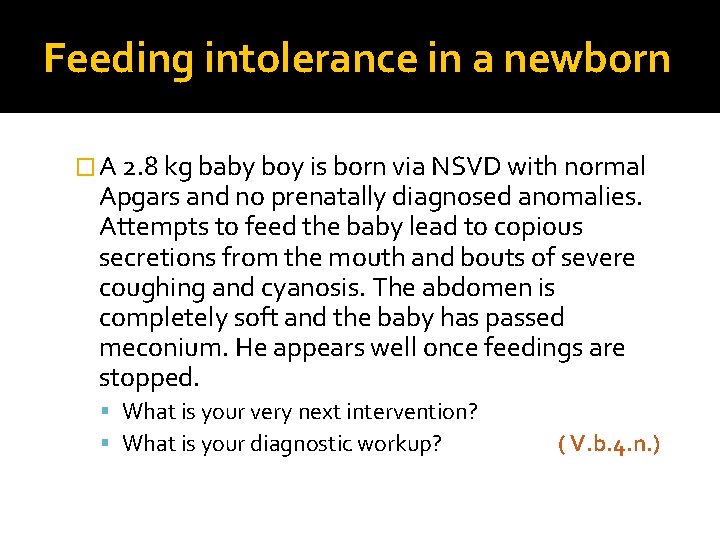
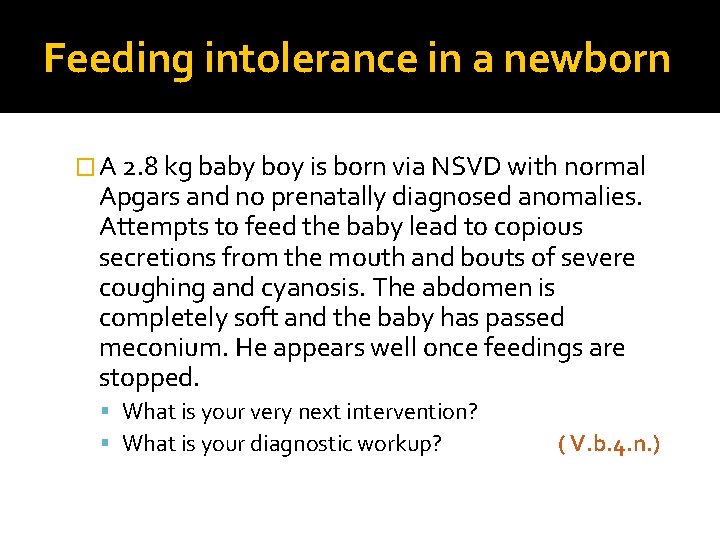
Feeding intolerance in a newborn � A 2. 8 kg baby boy is born via NSVD with normal Apgars and no prenatally diagnosed anomalies. Attempts to feed the baby lead to copious secretions from the mouth and bouts of severe coughing and cyanosis. The abdomen is completely soft and the baby has passed meconium. He appears well once feedings are stopped. What is your very next intervention? What is your diagnostic workup? ( V. b. 4. n. )
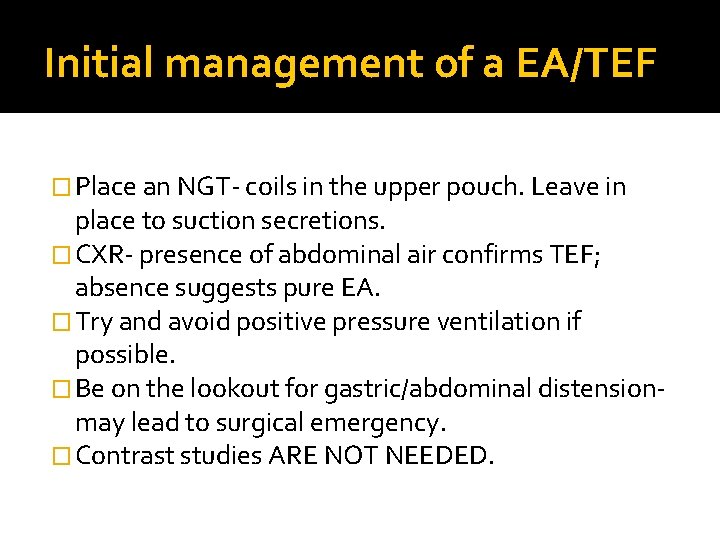
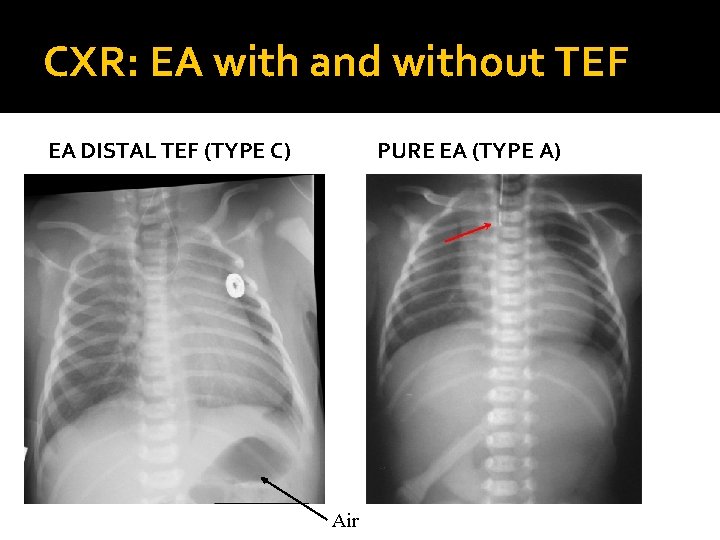
Initial management of a EA/TEF � Place an NGT- coils in the upper pouch. Leave in place to suction secretions. � CXR- presence of abdominal air confirms TEF; absence suggests pure EA. � Try and avoid positive pressure ventilation if possible. � Be on the lookout for gastric/abdominal distensionmay lead to surgical emergency. � Contrast studies ARE NOT NEEDED.
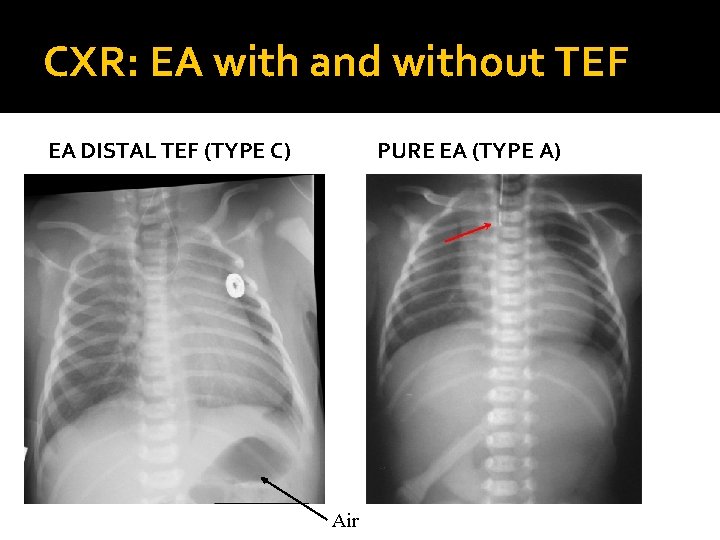
CXR: EA with and without TEF EA DISTAL TEF (TYPE C) PURE EA (TYPE A) Air
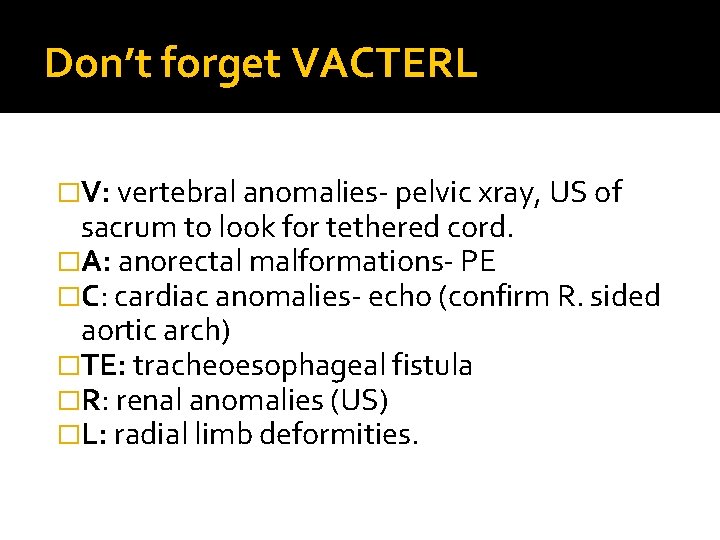
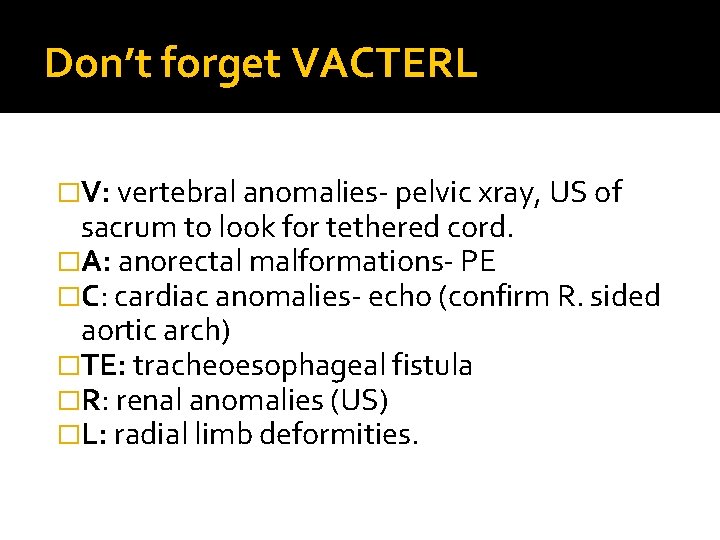
Don’t forget VACTERL �V: vertebral anomalies- pelvic xray, US of sacrum to look for tethered cord. �A: anorectal malformations- PE �C: cardiac anomalies- echo (confirm R. sided aortic arch) �TE: tracheoesophageal fistula �R: renal anomalies (US) �L: radial limb deformities.
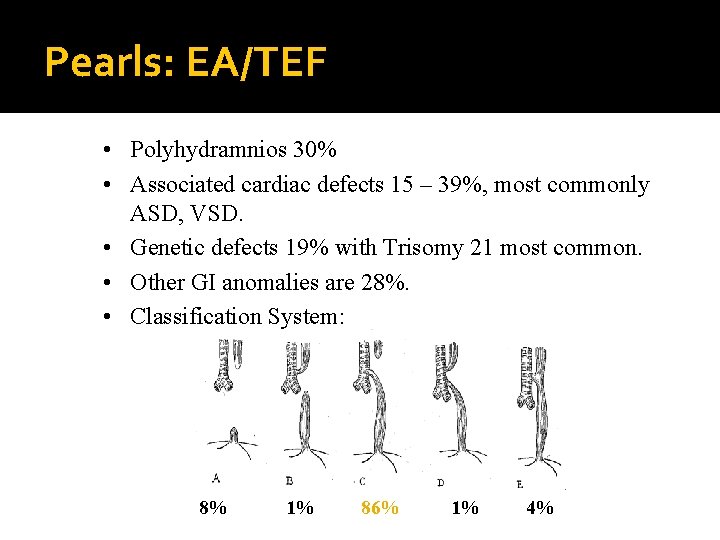
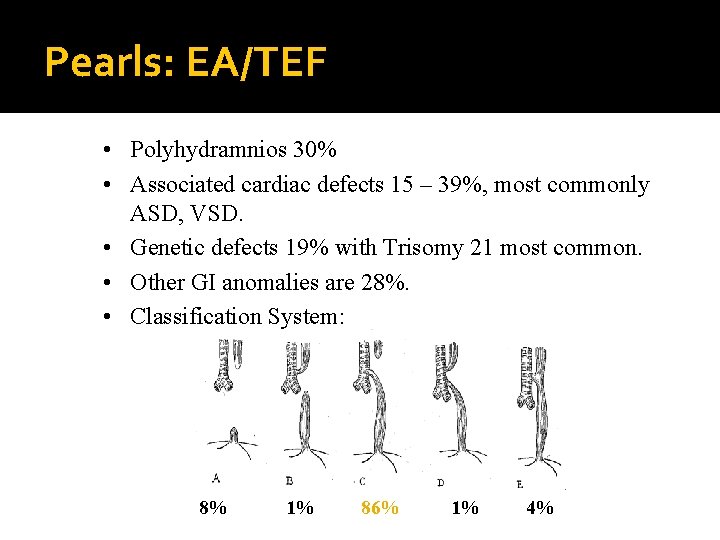
Pearls: EA/TEF • Polyhydramnios 30% • Associated cardiac defects 15 – 39%, most commonly ASD, VSD. • Genetic defects 19% with Trisomy 21 most common. • Other GI anomalies are 28%. • Classification System: 8% 1% 86% 1% 4%
Treatment: EA/TEF �Right thoracotomy, retropleural dissection and primary esophagostomy. �Chest drain for possible leak. �Transanastomotic feeding tube controversial. �Contrast study on POD #7.
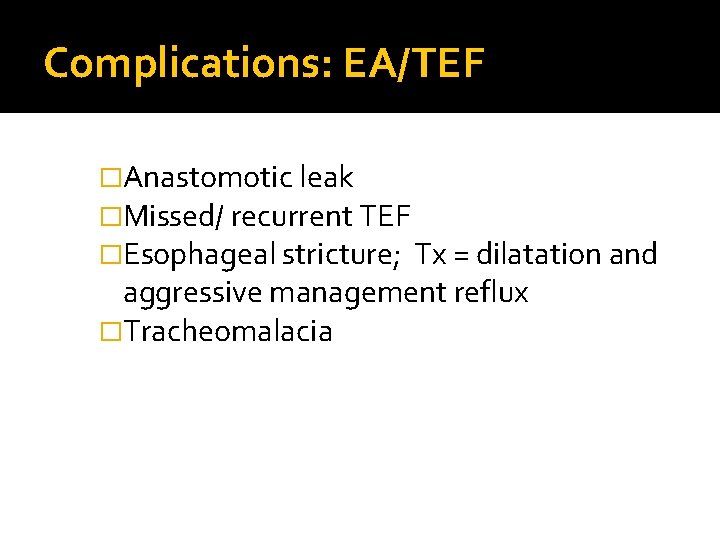
Complications: EA/TEF �Anastomotic leak �Missed/ recurrent TEF �Esophageal stricture; Tx = dilatation and aggressive management reflux �Tracheomalacia
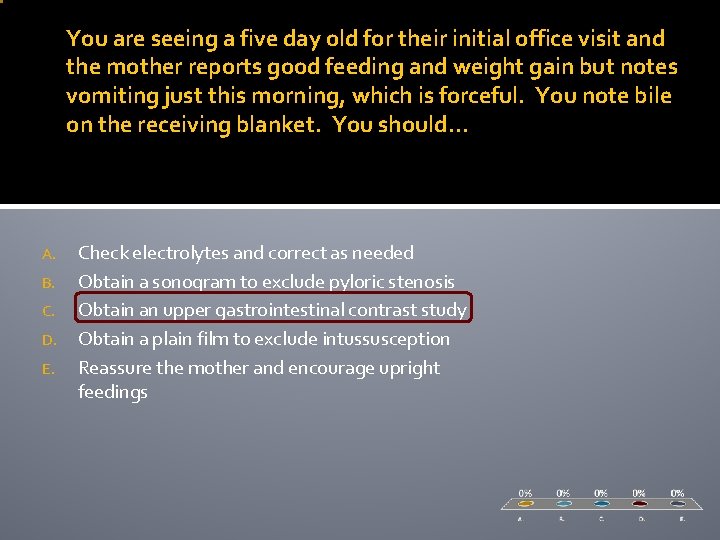
You are seeing a five day old for their initial office visit and the mother reports good feeding and weight gain but notes vomiting just this morning, which is forceful. You note bile on the receiving blanket. You should… A. B. C. D. E. Check electrolytes and correct as needed Obtain a sonogram to exclude pyloric stenosis Obtain an upper gastrointestinal contrast study Obtain a plain film to exclude intussusception Reassure the mother and encourage upright feedings
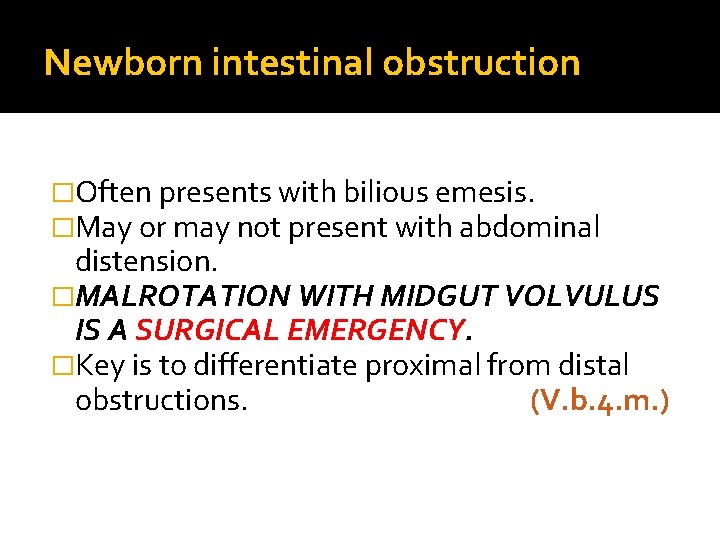
Newborn intestinal obstruction �Often presents with bilious emesis. �May or may not present with abdominal distension. �MALROTATION WITH MIDGUT VOLVULUS IS A SURGICAL EMERGENCY. �Key is to differentiate proximal from distal obstructions. (V. b. 4. m. )
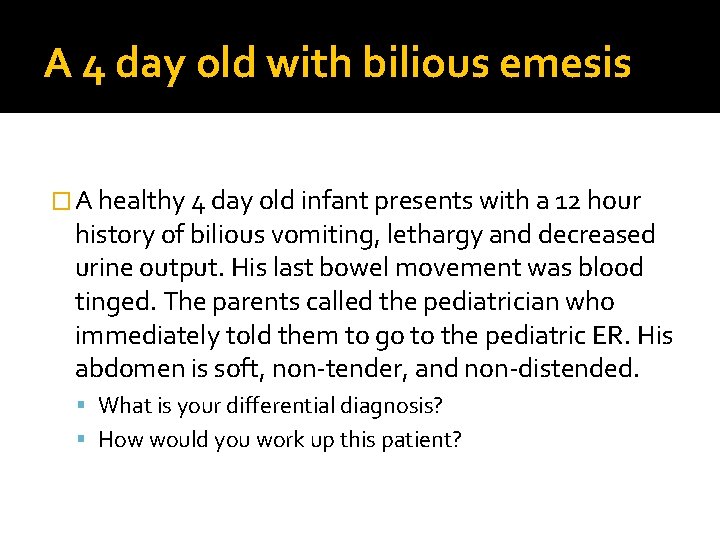
A 4 day old with bilious emesis � A healthy 4 day old infant presents with a 12 hour history of bilious vomiting, lethargy and decreased urine output. His last bowel movement was blood tinged. The parents called the pediatrician who immediately told them to go to the pediatric ER. His abdomen is soft, non-tender, and non-distended. What is your differential diagnosis? How would you work up this patient?
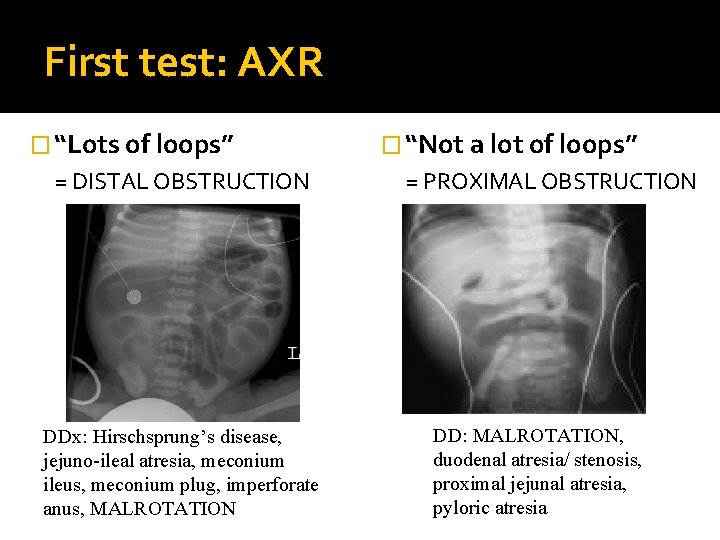
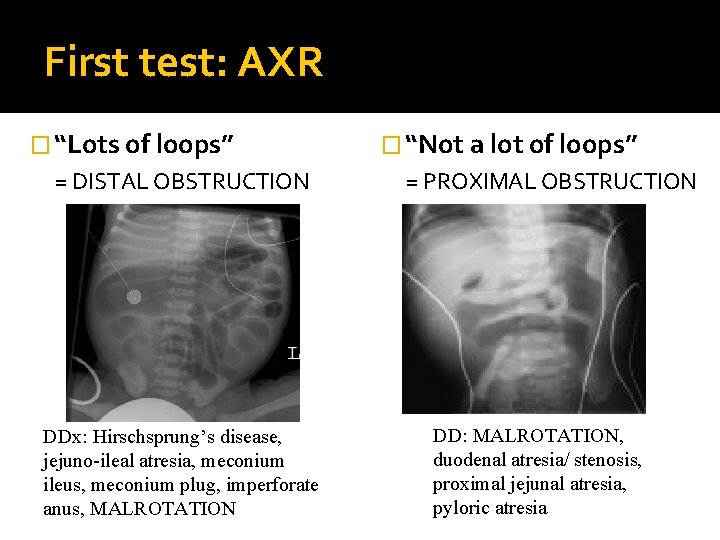
First test: AXR � “Lots of loops” = DISTAL OBSTRUCTION DDx: Hirschsprung’s disease, jejuno-ileal atresia, meconium ileus, meconium plug, imperforate anus, MALROTATION � “Not a lot of loops” = PROXIMAL OBSTRUCTION DD: MALROTATION, duodenal atresia/ stenosis, proximal jejunal atresia, pyloric atresia
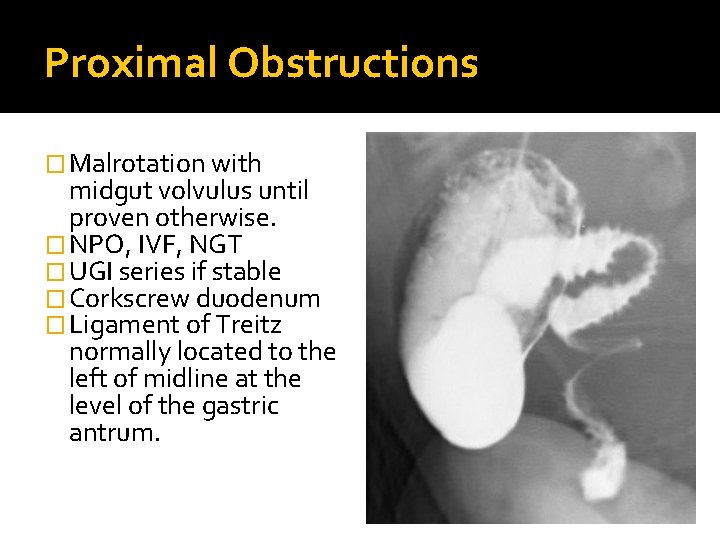
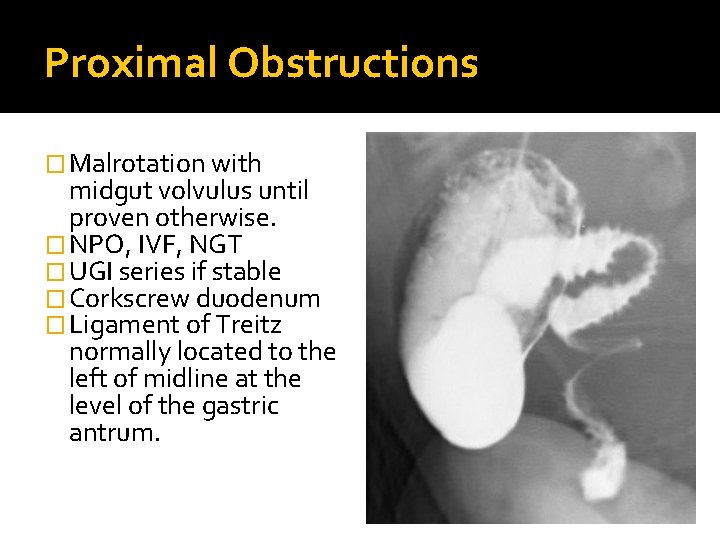
Proximal Obstructions � Malrotation with midgut volvulus until proven otherwise. � NPO, IVF, NGT � UGI series if stable � Corkscrew duodenum � Ligament of Treitz normally located to the left of midline at the level of the gastric antrum.
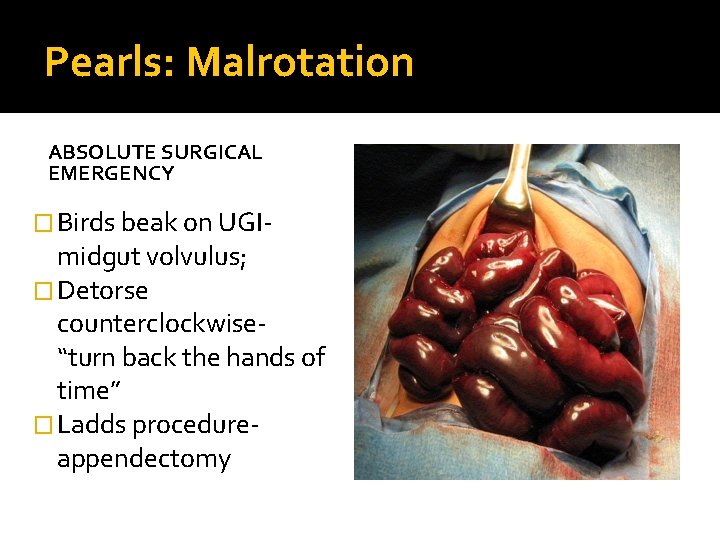
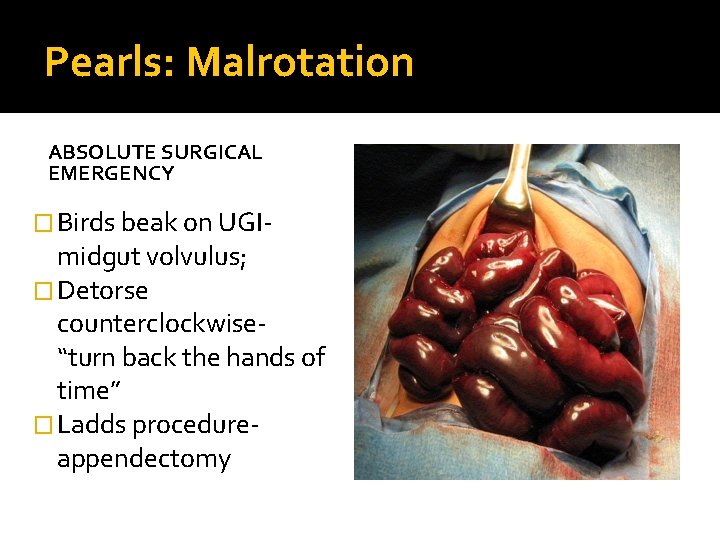
Pearls: Malrotation ABSOLUTE SURGICAL EMERGENCY � Birds beak on UGI- midgut volvulus; � Detorse counterclockwise“turn back the hands of time” � Ladds procedureappendectomy
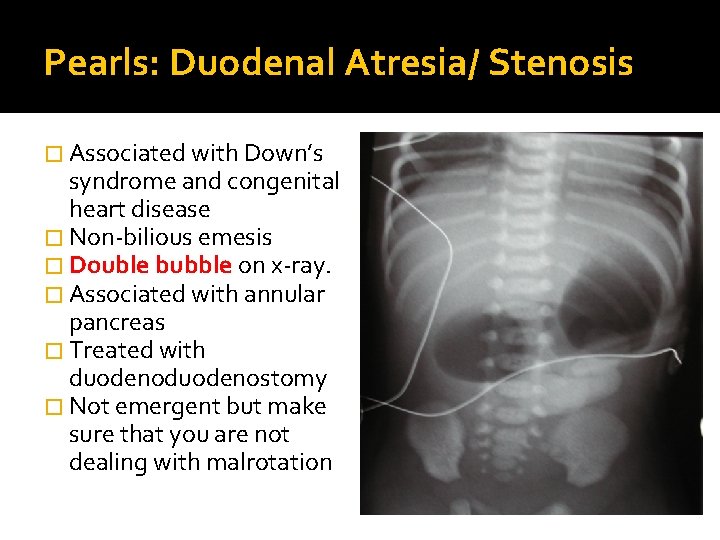
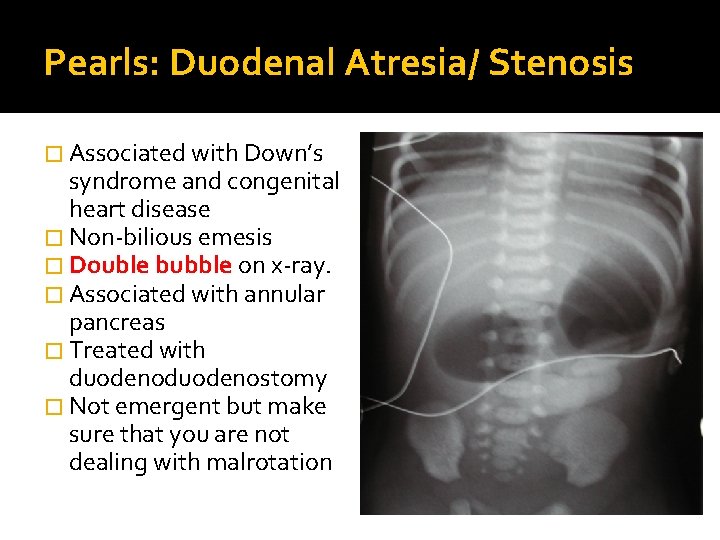
Pearls: Duodenal Atresia/ Stenosis � Associated with Down’s syndrome and congenital heart disease � Non-bilious emesis � Double bubble on x-ray. � Associated with annular pancreas � Treated with duodenostomy � Not emergent but make sure that you are not dealing with malrotation
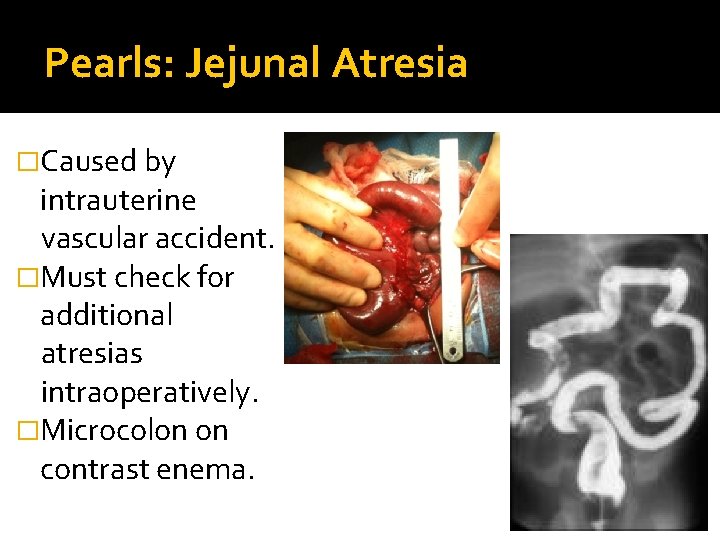
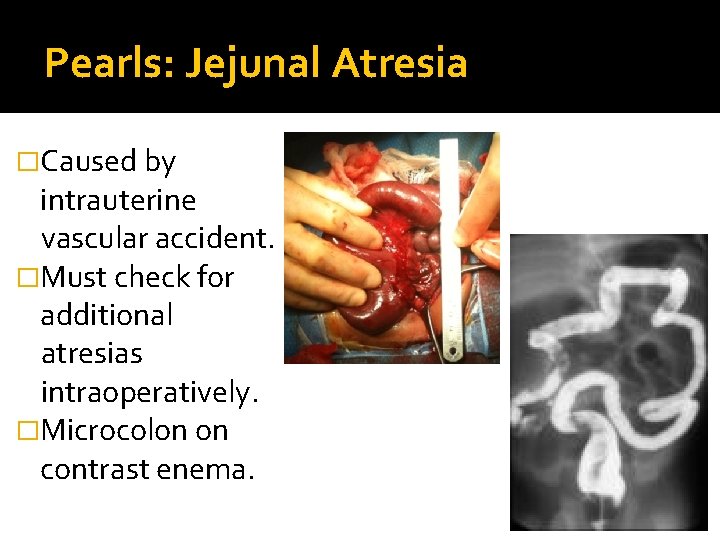
Pearls: Jejunal Atresia �Caused by intrauterine vascular accident. �Must check for additional atresias intraoperatively. �Microcolon on contrast enema.
A 3 day old who fails to pass meconium � A 3 day old infant has been vomiting bilious material all day. His abdomen is now markedly distended although he does not seem have any abdominal pain. Of note, he has failed to pass any meconium since birth. A rectal exam is met with explosive foul smelling green stool which hits another isolette across the room. What is your differential diagnosis? How does this case differ from the malrotation case earlier? How would you proceed with your workup?
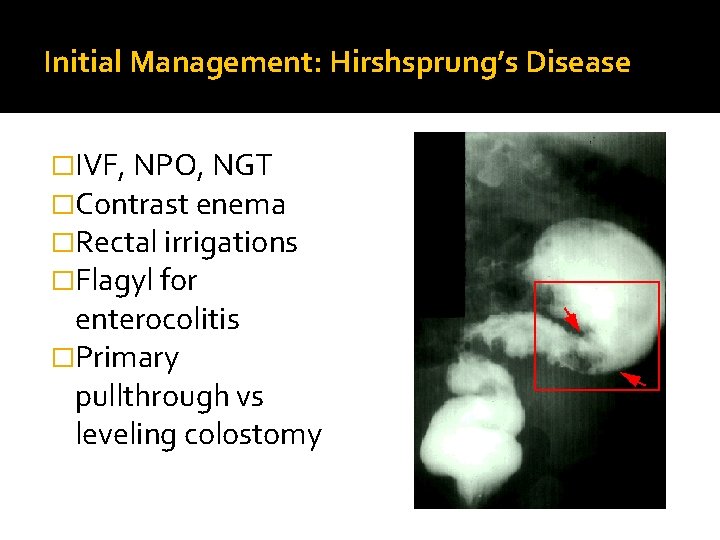
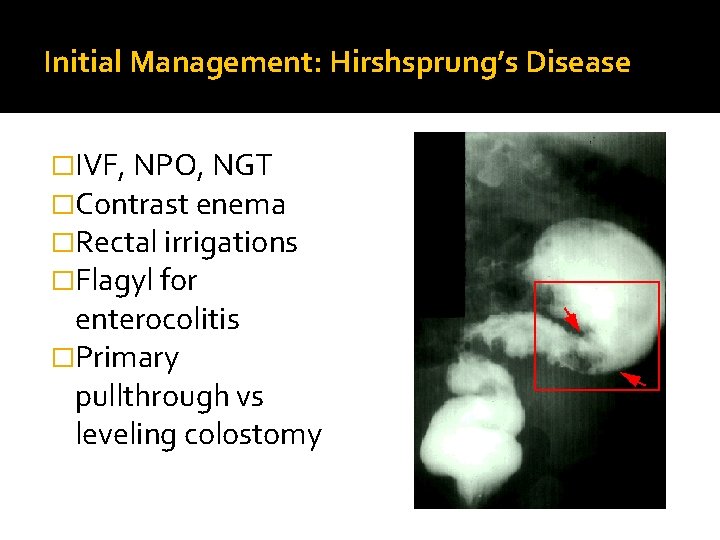
Initial Management: Hirshsprung’s Disease �IVF, NPO, NGT �Contrast enema �Rectal irrigations �Flagyl for enterocolitis �Primary pullthrough vs leveling colostomy
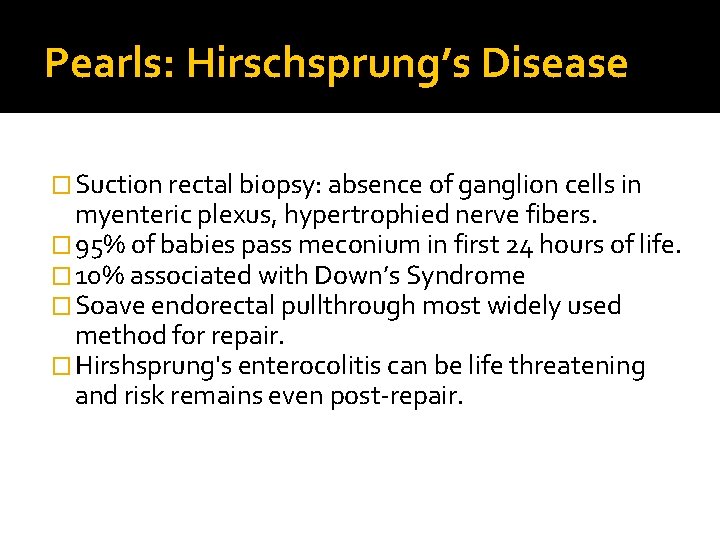
Pearls: Hirschsprung’s Disease � Suction rectal biopsy: absence of ganglion cells in myenteric plexus, hypertrophied nerve fibers. � 95% of babies pass meconium in first 24 hours of life. � 10% associated with Down’s Syndrome � Soave endorectal pullthrough most widely used method for repair. � Hirshsprung's enterocolitis can be life threatening and risk remains even post-repair.
Pearls: Meconium Ileus � 95 % associated with cystic fibrosis; often the first manifestation of disease. �Can be treated with hyperosmolar contrast enema which loosens meconium and allows it to pass. Microcolon seen on xray �Surgery if enema unsuccessful �Differentiate from SLC, meconium obstruction of colon (not assoc with CF)
Pearls: Imperforate Anus � Most common types: boy= rectourethral fistula; girls= rectovestibular fistula � VACTERL workup. � Usually a colostomy at birth; PSARP later. � Most common long term complication= fecal incontinence. � Cloaca: common channel connects genitourinary tracts and gastrointestinal tracts.
Pearls: Hypertrophic Pyloric Stenosis � Non-bilious projectile vomiting; 3 -8 week old � Most common: first born males � Hypokalemic, hypochloremic, metabolic alkalosis with paradoxical aciduria. � Not a surgical emergency- fix electrolytes with NS boluses, D 5 0. 5 NS maintenance. Add K+ once baby is urinating. � OR when Chloride > 98; HCO 3 <26 � Treatment: pyloromyotomy; babies often vomit postop- just keep feeding! � ( VI. d. 1)
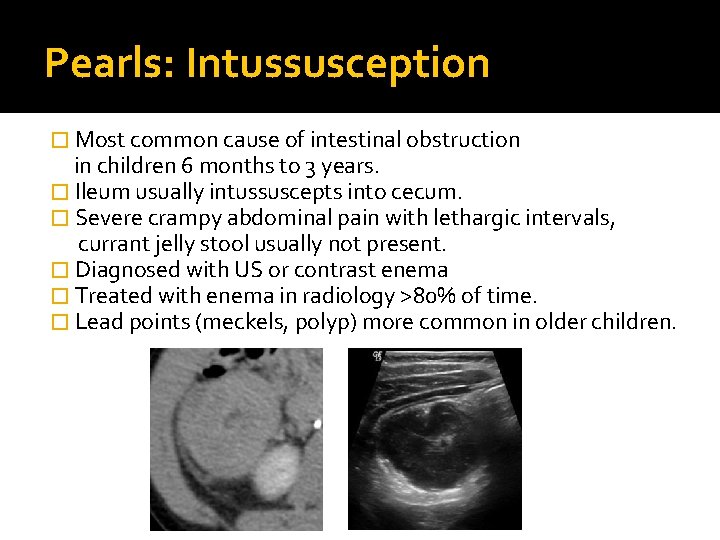
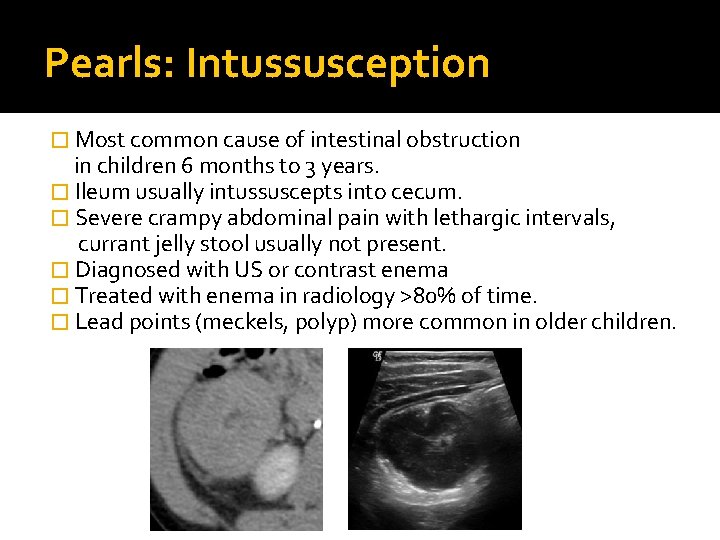
Pearls: Intussusception � Most common cause of intestinal obstruction in children 6 months to 3 years. � Ileum usually intussuscepts into cecum. � Severe crampy abdominal pain with lethargic intervals, currant jelly stool usually not present. � Diagnosed with US or contrast enema � Treated with enema in radiology >80% of time. � Lead points (meckels, polyp) more common in older children.
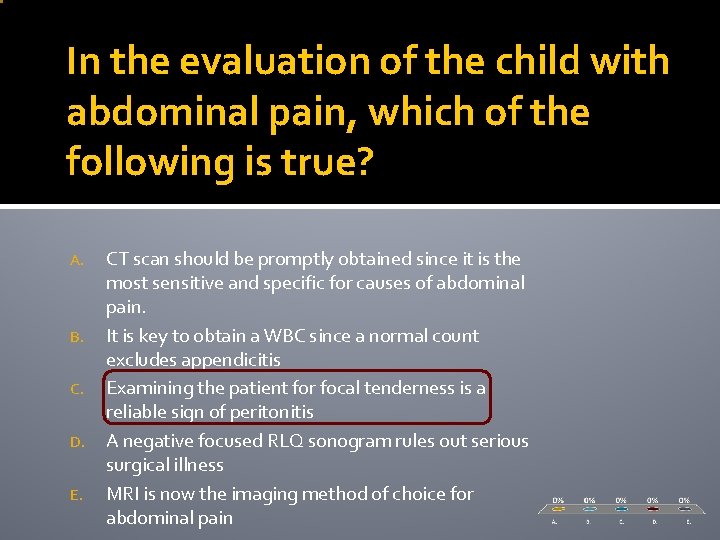
In the evaluation of the child with abdominal pain, which of the following is true? A. B. C. D. E. CT scan should be promptly obtained since it is the most sensitive and specific for causes of abdominal pain. It is key to obtain a WBC since a normal count excludes appendicitis Examining the patient for focal tenderness is a reliable sign of peritonitis A negative focused RLQ sonogram rules out serious surgical illness MRI is now the imaging method of choice for abdominal pain
3. Abdominal Pain Perhaps the most common reason for urgent consultation with a surgeon is the child with acute abdominal pain. While in theory, there are many possible causes for abdominal pain, most are self-limited and short-lived. While viral illness, UTI, intussusception, Meckel’s, pneumonia, pancreatitis, and a variety of other conditions can lead to abdominal pain, persistent acute abdominal pain in the childhood years must raise consideration of appendicitis. Missed appendicitis is a major source of liability claims against pediatricians and family physicians.
Abdominal Pain You are seeing a 7 year old boy who has been in your practice since birth and has only had well visits. He complains of constant pain in his abdomen that started in school yesterday. He ate dinner but threw up and went to bed. He has had no fever. He describes the pain as everywhere but on examination he is guarding in the right lower quadrant. You send a CBC from the office which is normal, he has no fever, and the urine dip is (+) for WBCs. A. What is your important differential? B. What are your plans?
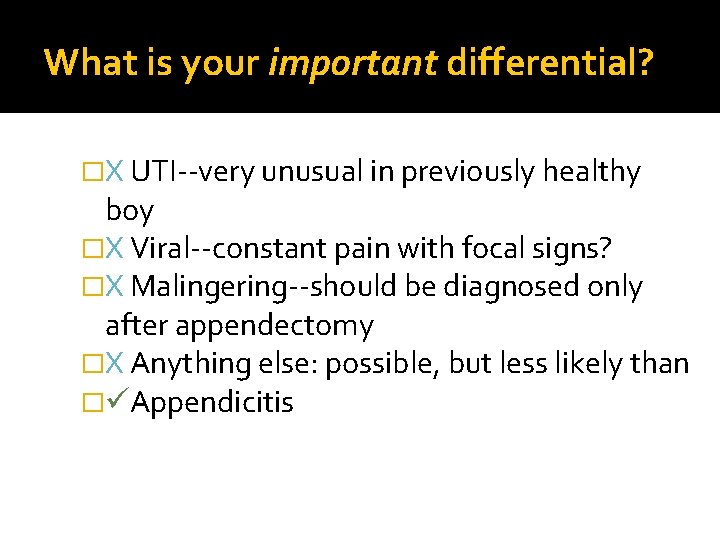
What is your important differential? �X UTI--very unusual in previously healthy boy �X Viral--constant pain with focal signs? �X Malingering--should be diagnosed only after appendectomy �X Anything else: possible, but less likely than � Appendicitis
Points to consider �The urine findings, of blood or + leuks, can occur from ureteral irritation from appy �Appendicitis is more common than… � Classic appendicitis is not necessary…focal findings can compensate for lack of fever, WBC, etc.
Plan of action? �Surgical Consultation/Contact �ER for hydration �Imaging may be needed but should be after a surgical consultation, not instead of… �CT can be harmful and can be wrong and can waste tremendous amount of time �Remain involved
Pearls �Letting surgeon know before referring patient to ER can expedite process �Do not tell patient/family you are referring to the ER for a CT…it may not be needed �Observation is a reasonable course in the short term �CT should be reserved for the difficult diagnosis
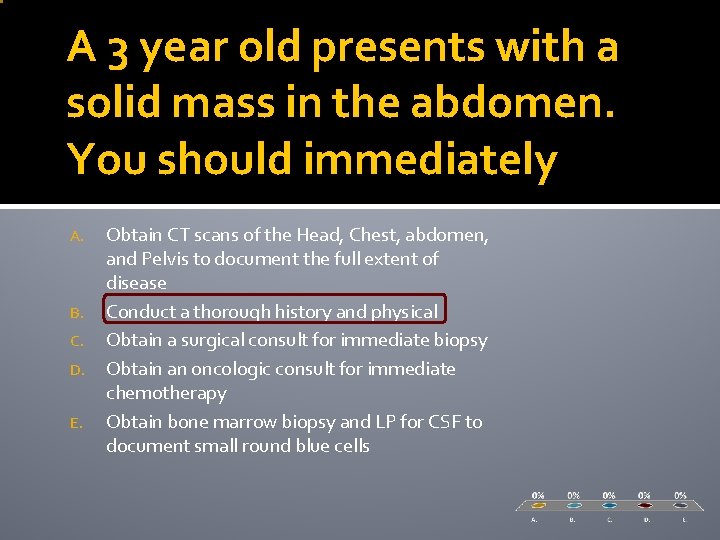
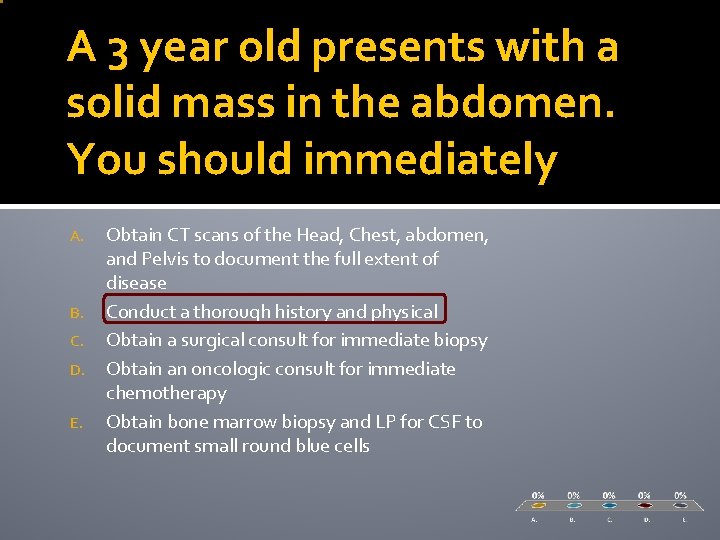
A 3 year old presents with a solid mass in the abdomen. You should immediately A. B. C. D. E. Obtain CT scans of the Head, Chest, abdomen, and Pelvis to document the full extent of disease Conduct a thorough history and physical Obtain a surgical consult for immediate biopsy Obtain an oncologic consult for immediate chemotherapy Obtain bone marrow biopsy and LP for CSF to document small round blue cells
4. Abdominal Masses �Abdominal masses are uncommon �Most are asymptomatic and are found by either a caregiver, usually during a bath, or the physician, during routine examination �Some can be quite benign (distended bladder, fecaloma) but we always consider and seek to exclude tumor
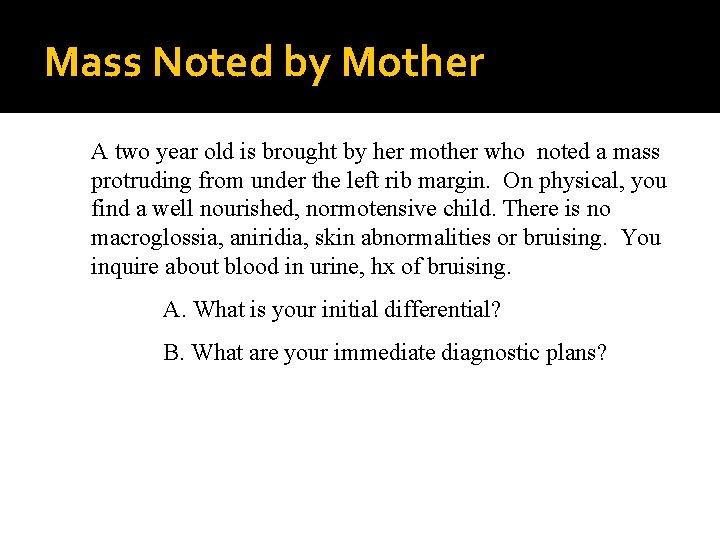
Mass Noted by Mother A two year old is brought by her mother who noted a mass protruding from under the left rib margin. On physical, you find a well nourished, normotensive child. There is no macroglossia, aniridia, skin abnormalities or bruising. You inquire about blood in urine, hx of bruising. A. What is your initial differential? B. What are your immediate diagnostic plans?
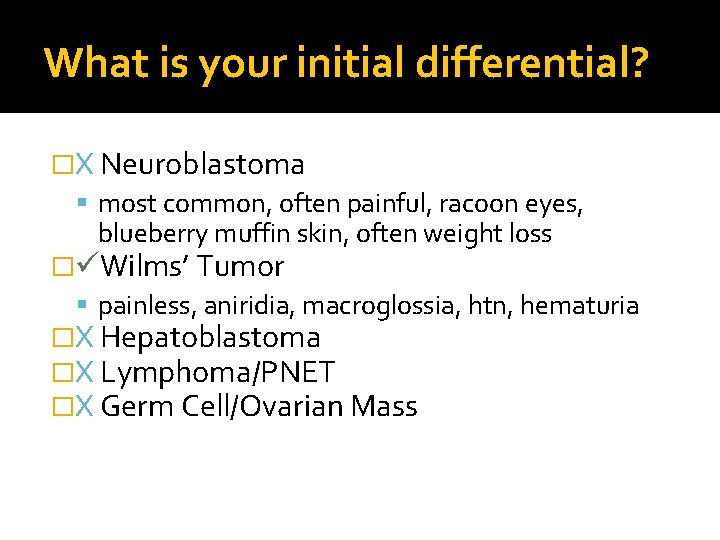
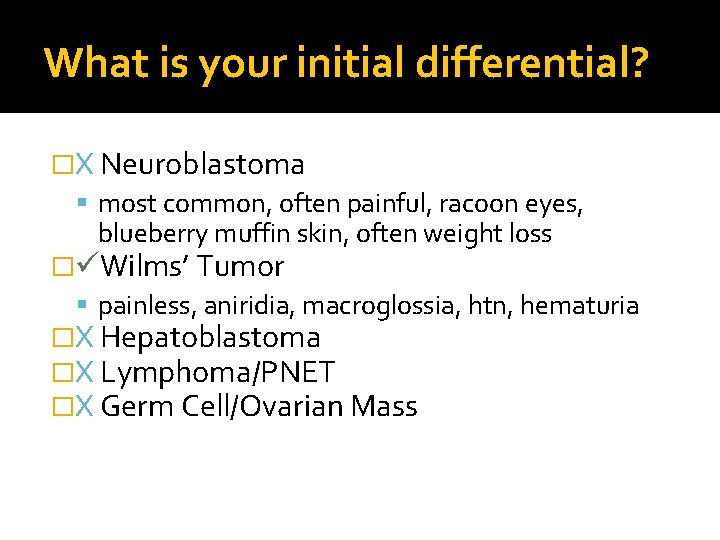
What is your initial differential? �X Neuroblastoma most common, often painful, racoon eyes, blueberry muffin skin, often weight loss � Wilms’ Tumor painless, aniridia, macroglossia, htn, hematuria �X Hepatoblastoma �X Lymphoma/PNET �X Germ Cell/Ovarian Mass
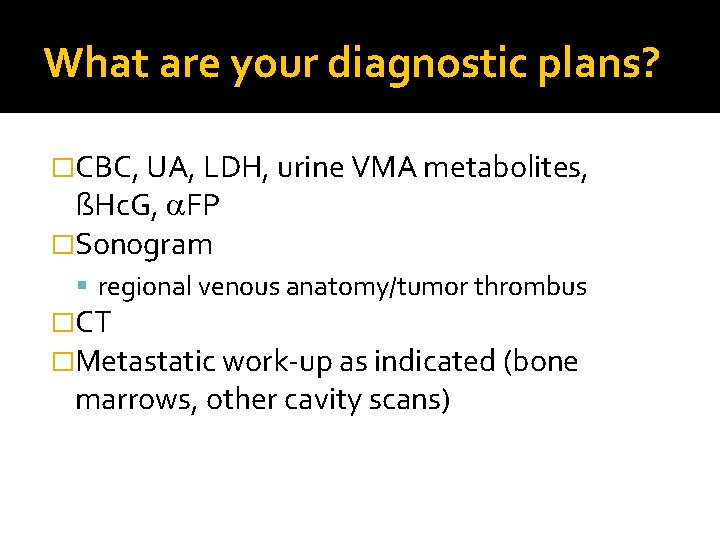
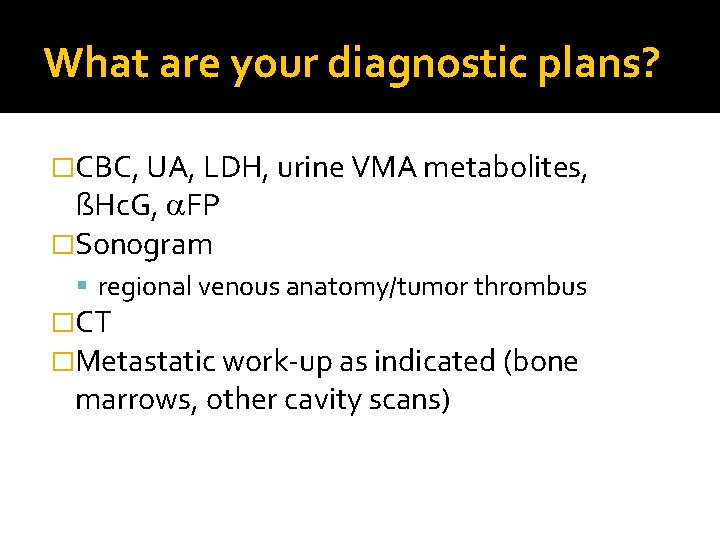
What are your diagnostic plans? �CBC, UA, LDH, urine VMA metabolites, ßHc. G, FP �Sonogram regional venous anatomy/tumor thrombus �CT �Metastatic work-up as indicated (bone marrows, other cavity scans)

Pearls �Accessory signs are helpful when present but most tumors present without �Neuroblastoma demonstrates calcifications on plain film, Wilms’ does not �Work up should be thorough but logical-head to toe scanning is not the approach �Diagnosis should await tissue confirmation �Try to minimize palpation
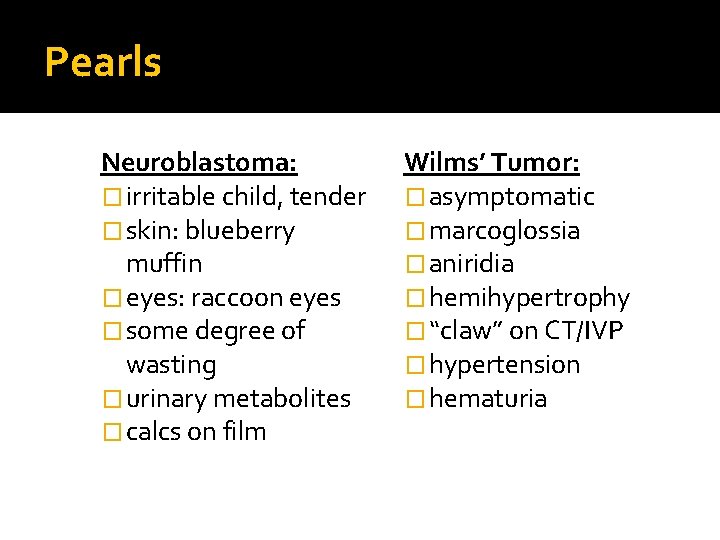
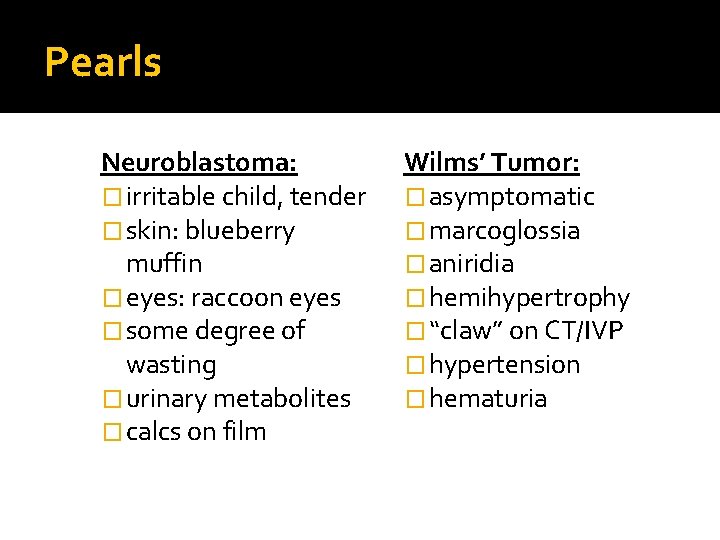
Pearls Neuroblastoma: � irritable child, tender � skin: blueberry muffin � eyes: raccoon eyes � some degree of wasting � urinary metabolites � calcs on film Wilms’ Tumor: � asymptomatic � marcoglossia � aniridia � hemihypertrophy � “claw” on CT/IVP � hypertension � hematuria
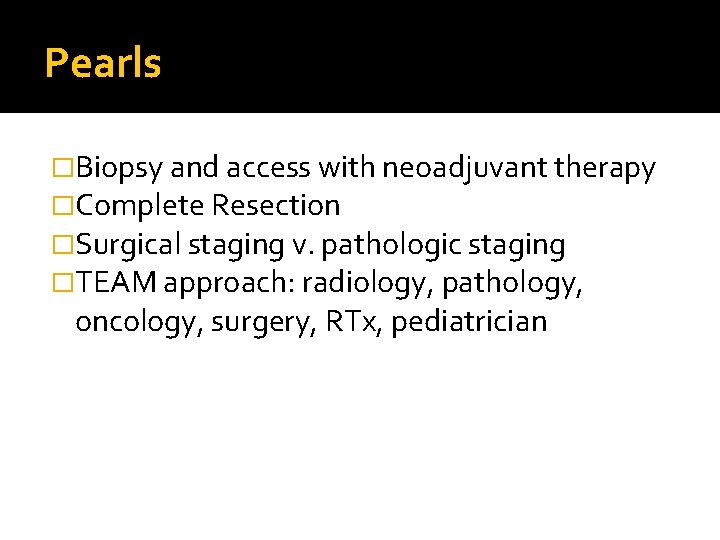
Pearls �Biopsy and access with neoadjuvant therapy �Complete Resection �Surgical staging v. pathologic staging �TEAM approach: radiology, pathology, oncology, surgery, RTx, pediatrician
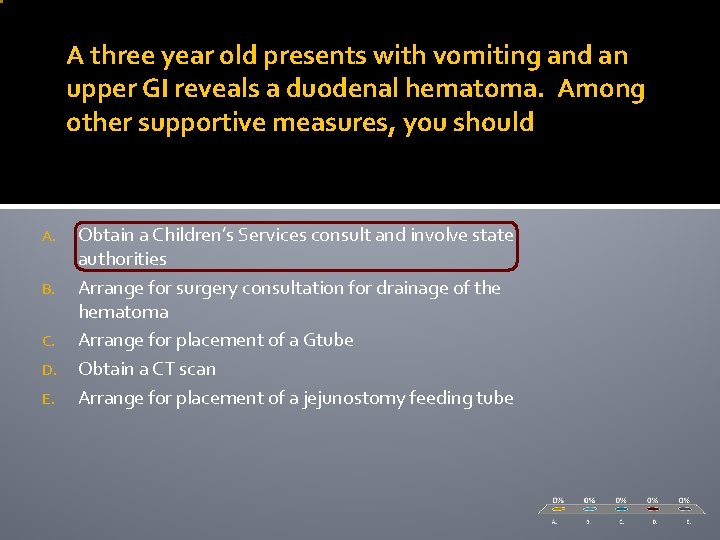
A three year old presents with vomiting and an upper GI reveals a duodenal hematoma. Among other supportive measures, you should A. B. C. D. E. Obtain a Children’s Services consult and involve state authorities Arrange for surgery consultation for drainage of the hematoma Arrange for placement of a Gtube Obtain a CT scan Arrange for placement of a jejunostomy feeding tube
5. Trauma �Accounts for more injuries and deaths in children than any other entity discussed today �Injury prevention is cost effective �Recognition of injury patterns is crucial to mitigating morbidity and mortality
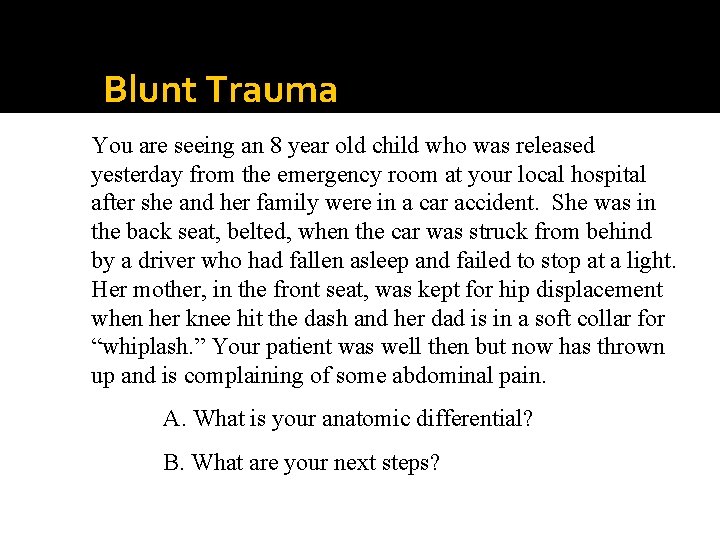
Blunt Trauma You are seeing an 8 year old child who was released yesterday from the emergency room at your local hospital after she and her family were in a car accident. She was in the back seat, belted, when the car was struck from behind by a driver who had fallen asleep and failed to stop at a light. Her mother, in the front seat, was kept for hip displacement when her knee hit the dash and her dad is in a soft collar for “whiplash. ” Your patient was well then but now has thrown up and is complaining of some abdominal pain. A. What is your anatomic differential? B. What are your next steps?
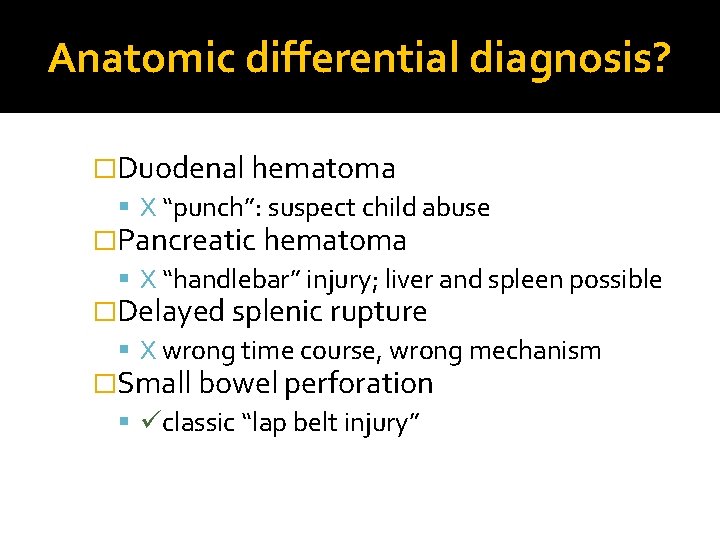
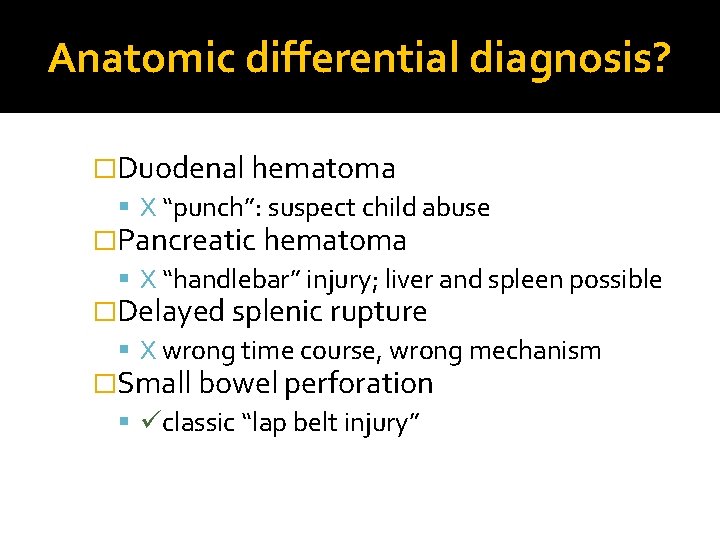
Anatomic differential diagnosis? �Duodenal hematoma X “punch”: suspect child abuse �Pancreatic hematoma X “handlebar” injury; liver and spleen possible �Delayed splenic rupture X wrong time course, wrong mechanism �Small bowel perforation classic “lap belt injury”
What are your next steps? �Examination �Arrange for admission �Surgical consultation �IV Fluids �Imaging �Operation
Pearls �Degree of trauma sustained by others must raise your level of concern. �Mechanism of injury and the pattern of injury is highly correlative. �Early surgical involvement. �Continued pediatric involvement.
Pearls �Most blunt abdominal trauma can be managed non-operatively in the stable patient �Regardless of the injury, the same principles of resuscitation apply. �The injured child has an injured family
Pearls �Infants and small children are top heavy and “lead” with their head when thrown �Cervical spine injury can occur with only subtle radiographic evidence so images must be interpreted properly �Blunt trauma to the chest can injure organs without fracturing ribs