Personality Disorders Dr Sean Fernandez Consultant Psychiatrist in
- Slides: 30
Personality Disorders Dr Sean Fernandez Consultant Psychiatrist in Psychotherapy Mid and East Surrey Psychotherapy Service
Aims of talk What is a personality disorder? What treatments are available at SABP? Some Do’s and Don'ts in working with personality disordered patients
ICD-11 -definition Personality disorder is characterized by Problems with the self (e. g. , identity, self-worth, accuracy of self-view, self-direction), Problems with others (e. g. , inability to develop and maintain close and mutually satisfying relationships, inability to understand others’ perspectives and to manage conflict in relationships) Persist over an extended period of time (e. g. , 2 years or more). The disturbance is manifest in patterns of cognition, emotional experience, emotional expression, and behaviour that are maladaptive (e. g. , inflexible or poorly regulated) and is manifest across a range of personal and social situations (i. e. , is not limited to specific relationships or social roles). The patterns of behaviour characterizing the disturbance are not developmentally appropriate and cannot be explained primarily by social or cultural factors, including socio-political conflict. The disturbance is associated with substantial distress or significant impairment in personal, family, social, educational, occupational or other important areas of functioning.
Personality disorders definition Problems in relation to self and others which are persistent, pervasive, outside of the developmental, social and cultural norms are distressing to both self and others and give rise to significant impairment in function in most if not all areas of life. Prevalence Adult Psychiatric Morbidity Survey 2014 for People aged 18 -64 General Population 13. 9 -17. 3 % ASPD 3. 3% Men 4. 9% Women 1. 8% BPD 2. 4 % Men and Women no statistically significant differences Approx prevalence 12: 25: 50 population : primary care : secondary care
ICD 11 classification Personality difficulty Mild Personality Disorder Moderate Personality Disorder Severe Personality Disorder Borderline constellation Dimensional and Trait based
ICD 11 -Personality traits Negative affectivity- low self esteem, anxiety, anger/irritability Detachment-social/emotional Dissociality Disinhibition- impulsivity, Anankastia- obsessionality, rigidity
DSM V Cluster A- Odd/Eccentric- Paranoid, Schizoid and Schizotypal Cluster B- Dramatic/Emotional /Erratic- Antisocial, Borderline, Histrionic, Narcissistic Cluster C-Anxious/Fearful- Obsessive compulsive, Avoidant and Dependant Categorical Moved into Axis I also alternative systerm of classification in appendix which is hybrid categorical and dimensional
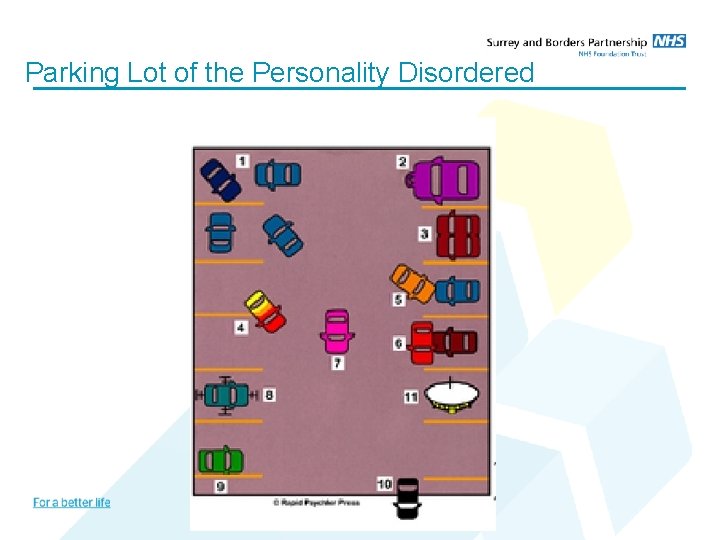
Parking Lot of the Personality Disordered
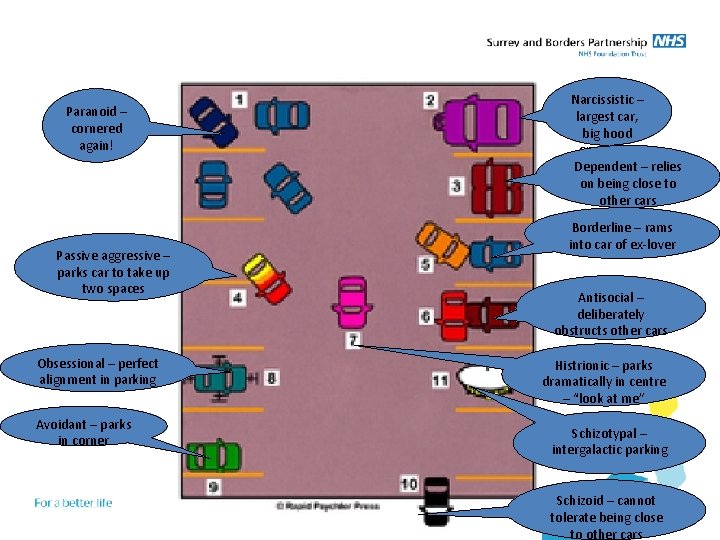
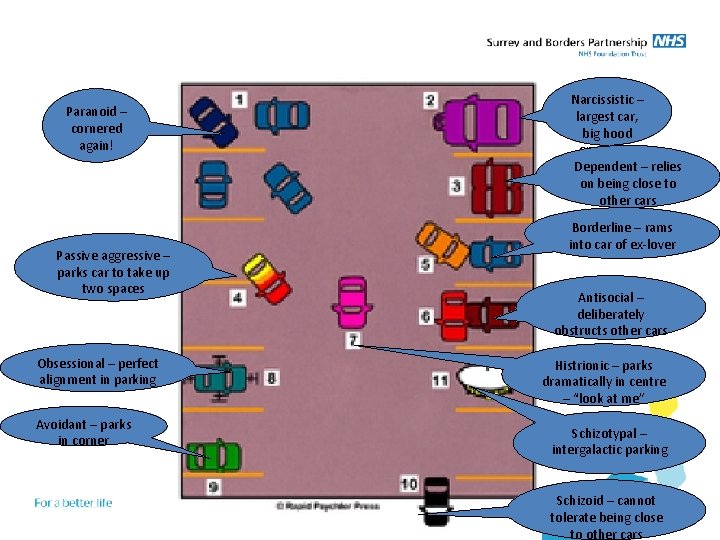
Paranoid – cornered again! Passive aggressive – parks car to take up two spaces Obsessional – perfect alignment in parking Avoidant – parks in corner Narcissistic – largest car, big hood ornament Dependent – relies on being close to other cars Borderline – rams into car of ex-lover Antisocial – deliberately obstructs other cars Histrionic – parks dramatically in centre – “look at me” Schizotypal – intergalactic parking Schizoid – cannot tolerate being close to other cars
Personality Organisation Reality testing Aggression Defence mechanisms Identity integration Object relatedness Superego functioning (internalised values)
Neurotic organisation Reality testing-intact Aggression-inhibited, angry outburst followed by guilt Defences-intermediate to mature, repression based Identity integration- relatively integrated and stable sense of self Object relatedness- more integrated view of others but specific areas of conflict Superego- excessive guilt , inflexibility/rigidity
Personality Disorder (Borderline)Organization Reality testing-generally intact but can breakdown with stress Aggression- significant self and other directed aggression Defence mechanisms- primitive and splitting based Identity integration- identity diffusion Object relatedness- confused/contradictory internal working modelsmarked interpersonal difficulties Superego- inconsistent value set , at times major gaps in value system
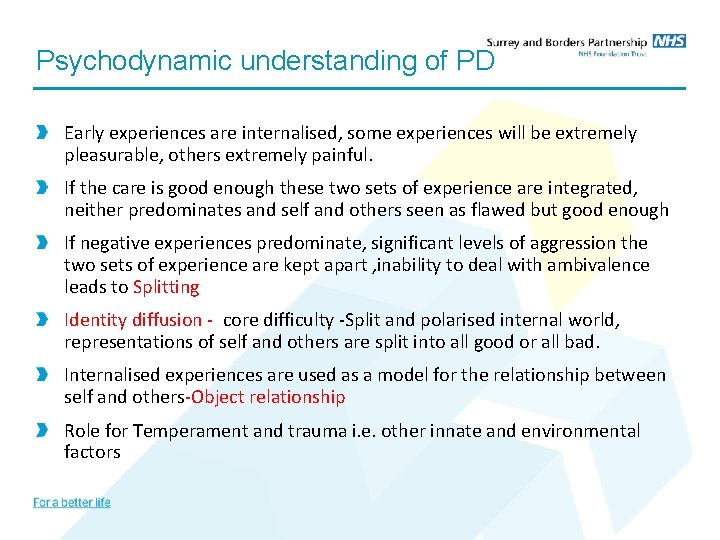
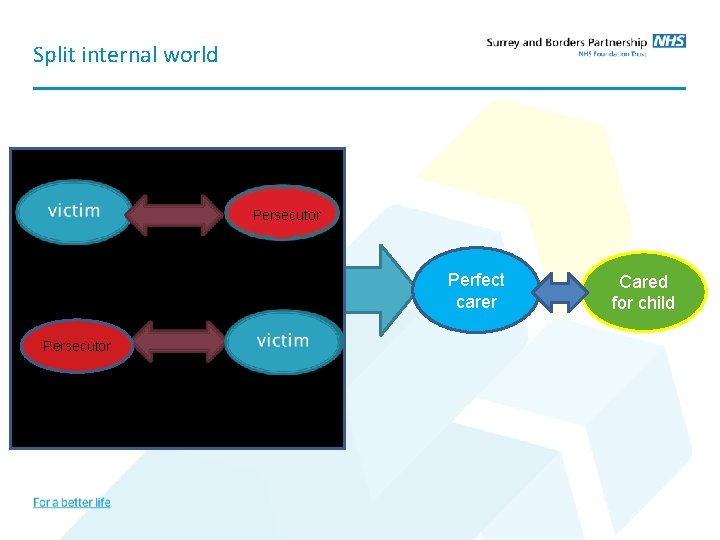
Psychodynamic understanding of PD Early experiences are internalised, some experiences will be extremely pleasurable, others extremely painful. If the care is good enough these two sets of experience are integrated, neither predominates and self and others seen as flawed but good enough If negative experiences predominate, significant levels of aggression the two sets of experience are kept apart , inability to deal with ambivalence leads to Splitting Identity diffusion - core difficulty -Split and polarised internal world, representations of self and others are split into all good or all bad. Internalised experiences are used as a model for the relationship between self and others-Object relationship Role for Temperament and trauma i. e. other innate and environmental factors
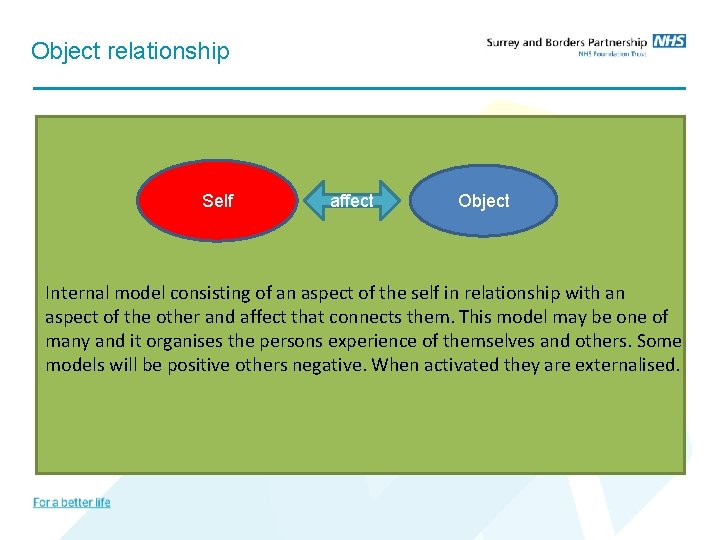
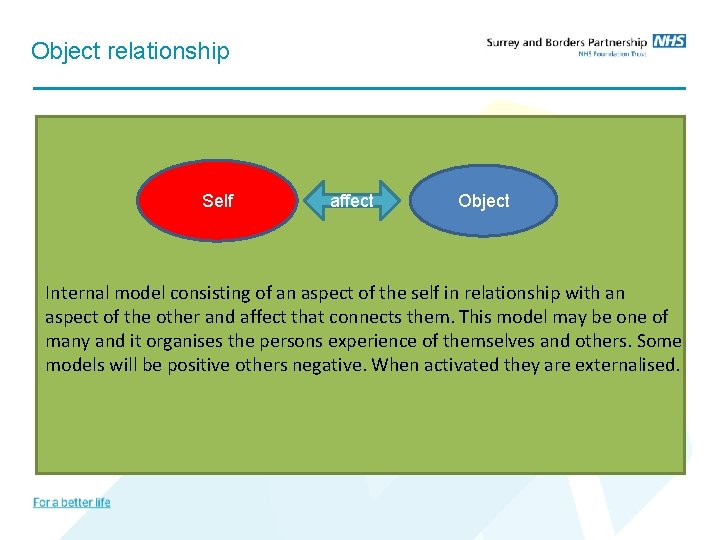
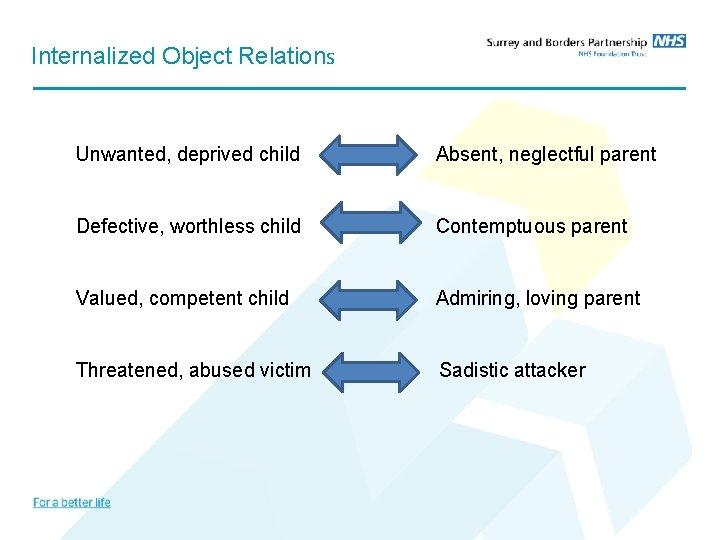
Object relationship Self affect Object Internal model consisting of an aspect of the self in relationship with an aspect of the other and affect that connects them. This model may be one of many and it organises the persons experience of themselves and others. Some models will be positive others negative. When activated they are externalised.
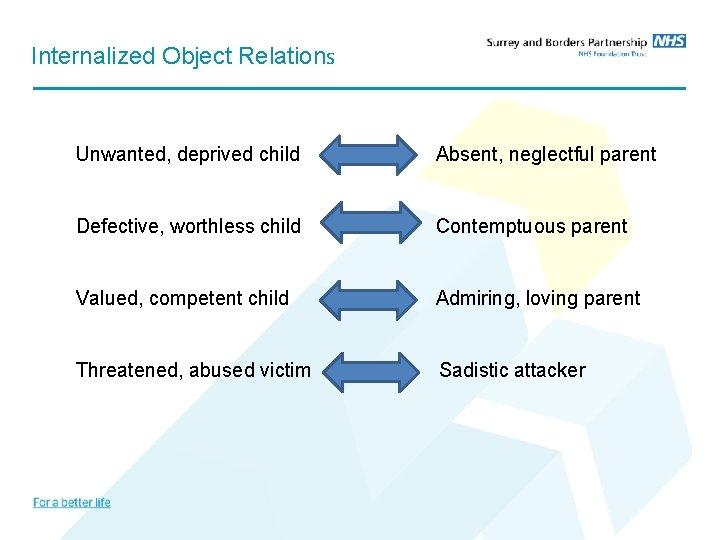
Internalized Object Relations Unwanted, deprived child Absent, neglectful parent Defective, worthless child Contemptuous parent Valued, competent child Admiring, loving parent Threatened, abused victim Sadistic attacker
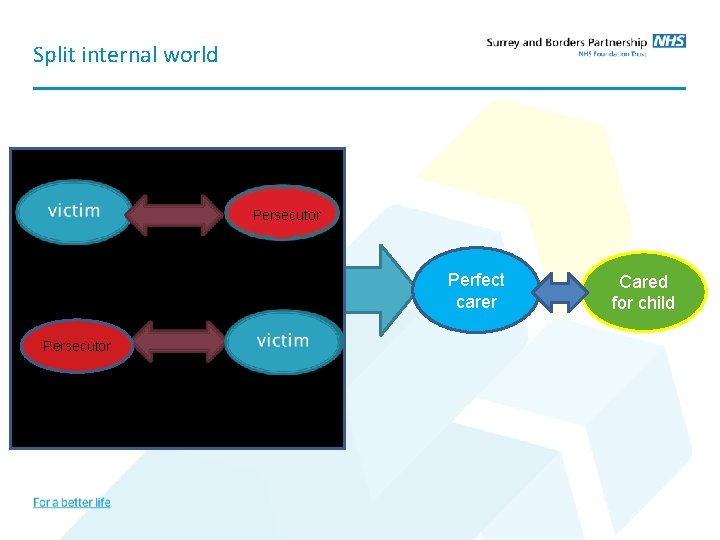
Split internal world Oscillation of roles Persecutor Perfect carer Persecutor Cared for child
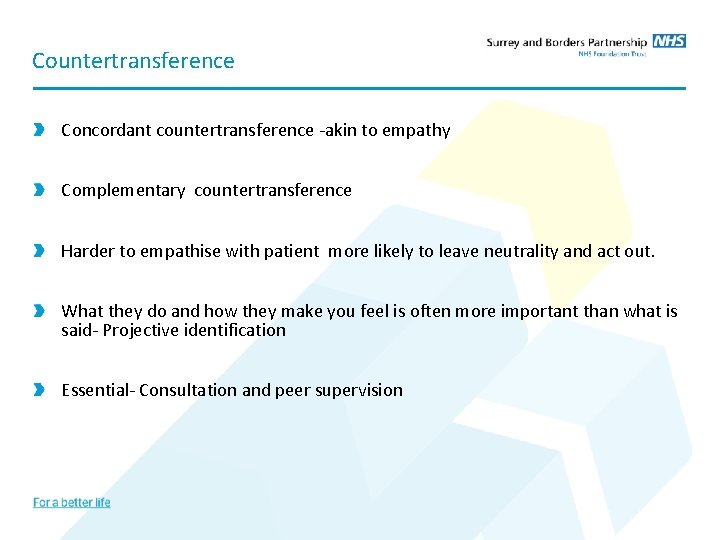
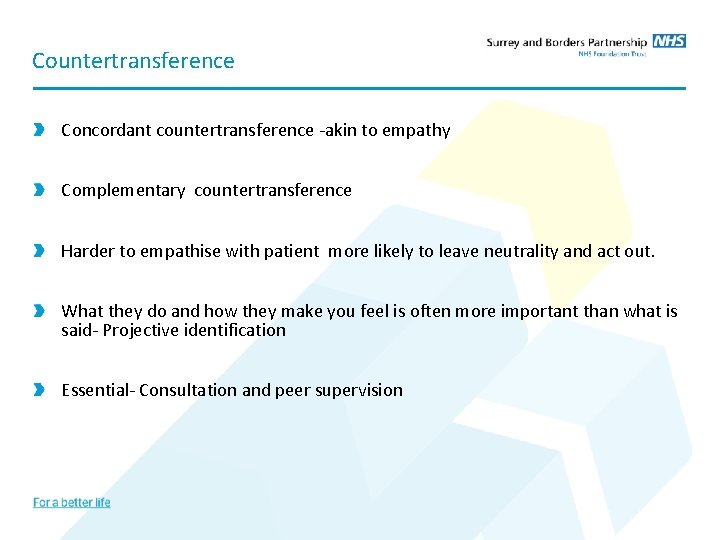
Countertransference Concordant countertransference -akin to empathy Complementary countertransference Harder to empathise with patient more likely to leave neutrality and act out. What they do and how they make you feel is often more important than what is said- Projective identification Essential- Consultation and peer supervision
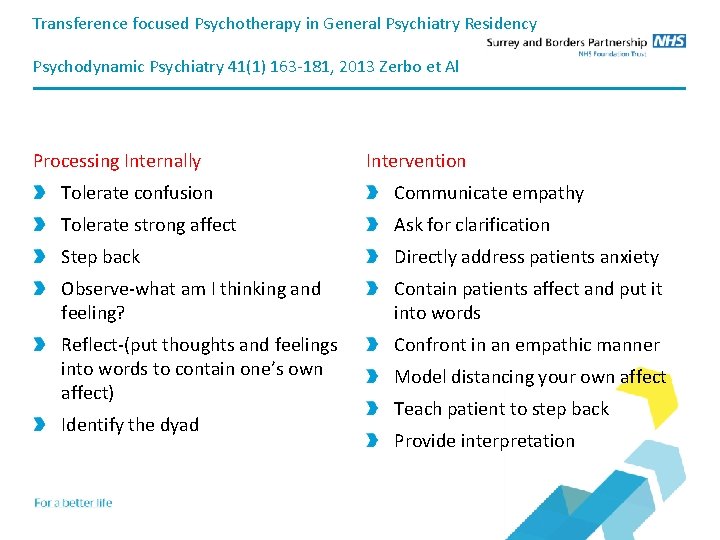
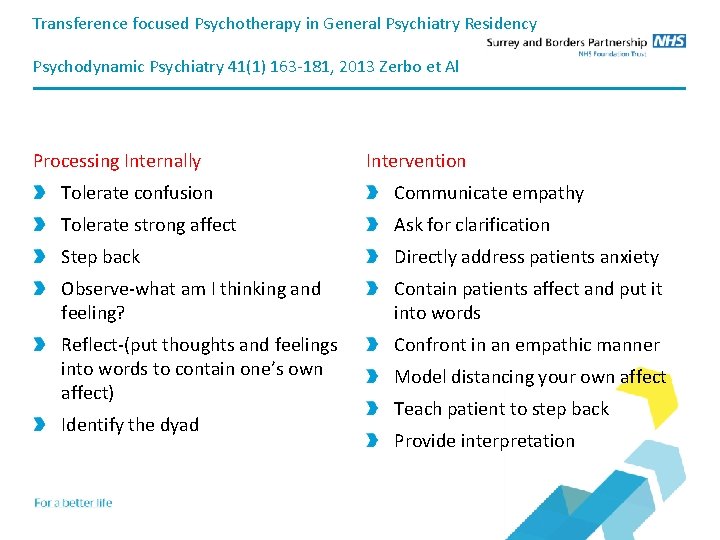
Transference focused Psychotherapy in General Psychiatry Residency Psychodynamic Psychiatry 41(1) 163 -181, 2013 Zerbo et Al Processing Internally Intervention Tolerate confusion Communicate empathy Tolerate strong affect Ask for clarification Step back Directly address patients anxiety Observe-what am I thinking and feeling? Contain patients affect and put it into words Reflect-(put thoughts and feelings into words to contain one’s own affect) Confront in an empathic manner Identify the dyad Model distancing your own affect Teach patient to step back Provide interpretation
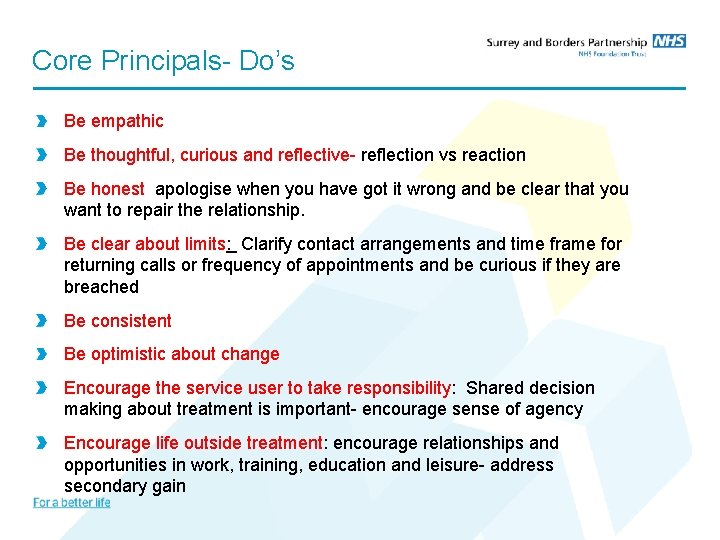
Core Principals- Do’s Be empathic Be thoughtful, curious and reflective- reflection vs reaction Be honest apologise when you have got it wrong and be clear that you want to repair the relationship. Be clear about limits: Clarify contact arrangements and time frame for returning calls or frequency of appointments and be curious if they are breached Be consistent Be optimistic about change Encourage the service user to take responsibility: Shared decision making about treatment is important- encourage sense of agency Encourage life outside treatment: encourage relationships and opportunities in work, training, education and leisure- address secondary gain
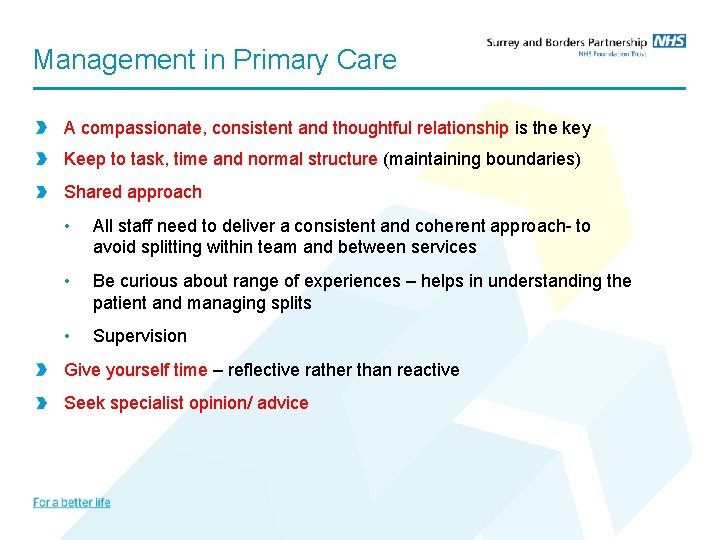
Management in Primary Care A compassionate, consistent and thoughtful relationship is the key Keep to task, time and normal structure (maintaining boundaries) Shared approach • All staff need to deliver a consistent and coherent approach- to avoid splitting within team and between services • Be curious about range of experiences – helps in understanding the patient and managing splits • Supervision Give yourself time – reflective rather than reactive Seek specialist opinion/ advice
Making the Diagnosis Don’t avoid the diagnosis GP well placed to obtain longitudinal perspective / corroborating history Often better able to distinguish between new, transient and enduring patterns of behavior GP less likely to make specific PD diagnosis Other than borderline (BPD) and antisocial (ASPD) Consider Co-morbid conditions
Medication Most randomised trials in the last 20 years are of BPD Most trials are judged to be of low quality by NICE (2009) “antipsychotic drugs should not be used for the medium and long term treatment of borderline personality disorder” “in general drug treatment should be avoided except in an emergency” Lieb et al (2010): British Journal of Psychiatry 196, 4 -12 Pharmacotherapy for BPD : Cochrane systematic review of randomised trials. Suggested that mood stabilisers and second generation antipsychotics may be effective for treating a number of core symptoms Evidence does not support effectiveness for overall severity of Borderline PD “Pharmacotherapy should be targeted at specific symptoms”
When to refer Significant Risk to Self or Others • Assessment of level of risk • Diagnosis and Formulation • Risk management plan • Treatment Pathway • Evidence based treatments Co-morbidity • Depression, Anxiety, Somatization, Substance Misuse, Trauma Marked impairment of psychosocial functioning
Secondary care services Referral via Single Point of Access CMHRS – Good General Psychiatric Care Psychology- STEPPS and DBT Psychotherapy- Psychoanalytic Psychotherapy, Group Analytic Psychotherapy, MBT PD forum Risk Management Panels Community Forensic Services Crisis Beds / Safe Havens/ Crisis lines and HTT Tier 4 services
Areas for discussion Crisis management Admission to hospital Medication Affect storms Team dynamics
STEPPS Systems Training for Emotional Predictability and Problem Solving (STEPPS) Programme This is a twenty week programme for people with a confirmed diagnosis of Borderline Personality Disorder. The programme is a manual-based group treatment programme involving psycho education and emotion and behaviour management skills training. The programme also includes education for friends, relatives or care teams as nominated by each member. The STEPPS Programme is offered as a standalone therapy as well as a step up into more intense therapies
Dialectical Behaviour Therapy DBT suggests that in order to overcome these problems you need to learn how to control your emotions, and that the first step in doing so is to experience, recognise and accept your emotions. You can then start to reduce their intensity and let them go quicker. Marsha Linehan developed DBT from CBT and Mindfulness for use in BPD CBT traditionally focuses on helping change unhelpful ways of thinking and behaving DBT also helps change but focuses on accepting who you are at the same time DBT uses a balance of change techniques and acceptance techniques Uses individual and group sessions, out of hours contact, and a team approach Evidence in particular in women with BPD who self harm
Mentalization Based therapy (MBT) People with BPD may have a poor capacity to mentalize. Mentalization is the ability to think about thinking. • Examining thoughts and beliefs • Assessing whether they are useful, realistic and based on reality • Recognising that others have thoughts, emotions etc. and that your interpretation of these may not necessarily be correct • Being aware of the potential impact your actions will have on other people’s mental states MBT aims to improve ability to recognise your own and others’ mental states, and learn to ‘step back’ from your thoughts about yourself and others and examine them to see if they are valid. Individual and groups sessions; usually up to 18 months
Transference Focused Psychotherapy Manualised evidence based treatment Developed from the work of Prof Otto Kernberg drawing on object relations theory Not just for BPD but for range of personality disorders Aim of TFP is integration of the self. Move from split view of self and others to a more integrated, realistic and nuanced view of oneself and others Paranoid/schizoid to depressive position functioning Mastery and sublimation of aggressive feelings
Any Questions ?
 Parking lot of the personality disordered
Parking lot of the personality disordered Expert in consultant liaison psychiatrist
Expert in consultant liaison psychiatrist Psychiatrist leicester
Psychiatrist leicester Paranoia disorder
Paranoia disorder Diathesis stress model
Diathesis stress model Weird wild wacky personality disorders
Weird wild wacky personality disorders Cluster b personality disorders
Cluster b personality disorders Psychological disorders characterized by inflexible
Psychological disorders characterized by inflexible Antisocial personality disorder ελληνικα
Antisocial personality disorder ελληνικα Cluster b disorder
Cluster b disorder Personality disorder
Personality disorder Cluster c personality disorders
Cluster c personality disorders Cluster c
Cluster c Dramatic personality disorders
Dramatic personality disorders Cluster c personality disorders
Cluster c personality disorders Cluster b traits
Cluster b traits Sadistic personality
Sadistic personality Dsm v personality disorders
Dsm v personality disorders Dr rebecca lawrence psychiatrist
Dr rebecca lawrence psychiatrist Uuuu0
Uuuu0 Donna grant psychiatrist
Donna grant psychiatrist Dr shahid hussain psychiatrist
Dr shahid hussain psychiatrist Dr hoosen psychiatrist
Dr hoosen psychiatrist Dr moghul psychiatrist
Dr moghul psychiatrist Psychiatrist vs psychologist
Psychiatrist vs psychologist Dr derek lovell psychiatrist
Dr derek lovell psychiatrist Dr joubert psychiatrist
Dr joubert psychiatrist David ash psychiatrist
David ash psychiatrist Dr fionnuala o'loughlin psychiatrist
Dr fionnuala o'loughlin psychiatrist Dr peter byrne
Dr peter byrne Dr simon howard psychiatrist
Dr simon howard psychiatrist