Personality Disorders Dr Andrea Williams Consultant Psychiatrist in






- Slides: 54
Personality Disorders Dr Andrea Williams Consultant Psychiatrist in Psychotherapy Personality Disorder and Homelessness Team NHS Greater Glasgow and Clyde
What we will cover • • Overview Definitions Prevalence and course Types of personality disorder – Dissocial – Borderline • Attachment basis • Treatment/ management • PD and Legislation

Overview
Personality Disorder: What’s in a name? Stigma Untreatable? Excluded from Services
Stigma People with a PD can be seen as troublesome patients in medical terms/ troublesome people in society. They do not improve rapidly; offer few rewards to those treating them; can make us feel impotent/ guilty/ angry and many other things.
Stigma – changing? All of this improves if more effort to UNDERSTAND and ADDRESS the nature of the difficulty Requires attention to how services delivered User groups claiming the diagnosis as a useful tool for accessing services
Untreatable? not true Emerging evidence that a number of psychological approaches can help – particularly in BORDERLINE PD • Mentalisation Based Therapy • DBT(Dialectical behavioural therapy)
Excluded from Services ? shouldn’t be • “Personality Disorder – no longer a diagnosis of exclusion” document in England • NICE guidelines for treatment • Scotland – “Personality Disorder – Demanding patients or Deserving People? ” (CCI, 2005)
Excluded from Services ? • Scottish Personality Disorder Network (SPDN) co-ordinates regular conferences to share expertise and good practice • More recently- Borderline PD included as one of categories in Integrated Care Pathways being implemented across all Health Boards in Scotland.

Definitions
What Do we mean by Personality Disorder? • Deeply ingrained maladaptive patterns of behaviour • Extreme/ significant deviation from the way the average person in that culture perceives/ thinks/ feels and relates to others. (MAKES THEM DIFFERENT) • Recognisable from adolescence
What Does it Mean? • Disturbed ways of RELATING • Difficulties with MOOD CONTROL and IMPULSIVITY • Disturbed ways of THINKING
What Does it Mean? • Enduring – long lasting • Pervasive – affects all areas of person’s life • Considerable personal distress
Prevalence and Course
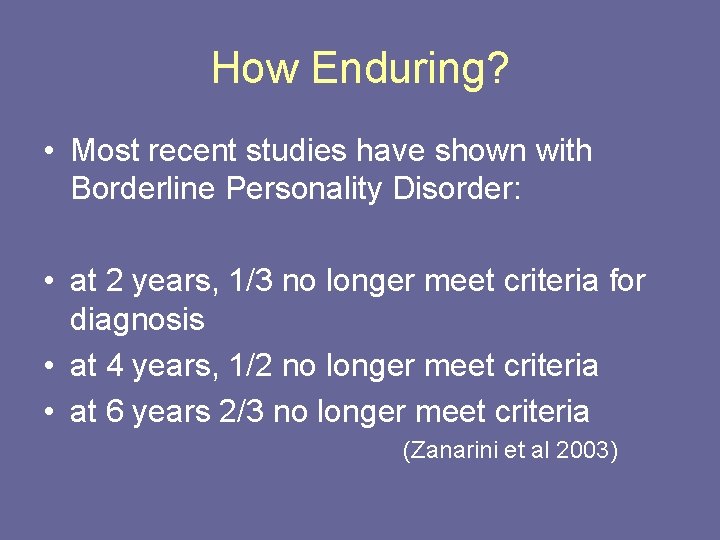
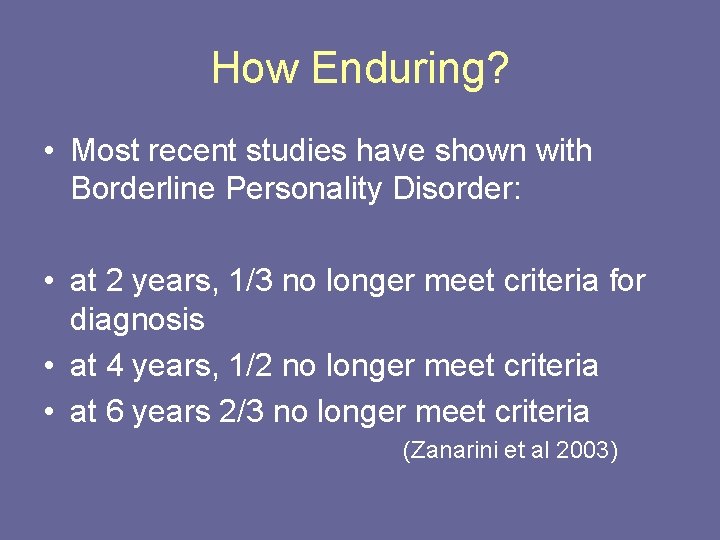
How Enduring? • Most recent studies have shown with Borderline Personality Disorder: • at 2 years, 1/3 no longer meet criteria for diagnosis • at 4 years, 1/2 no longer meet criteria • at 6 years 2/3 no longer meet criteria (Zanarini et al 2003)
How enduring? (cont) Older wisdom was that personality mellowed with age, but this had limited support from long-term follow up Studies show that marked disturbance continues, although some of the more noticable behaviours became less frequent i. e. TRAITS are enduring, but expression of these may modify with age/ experience
How Common Is It? • 5 -10% of general adult population (zimmerman and coryell, 1990) • 35% + of those in Psychiatric Hospital • 50% of female prisoners • 60 -80% of male prisoners
Types of Personality Disorder
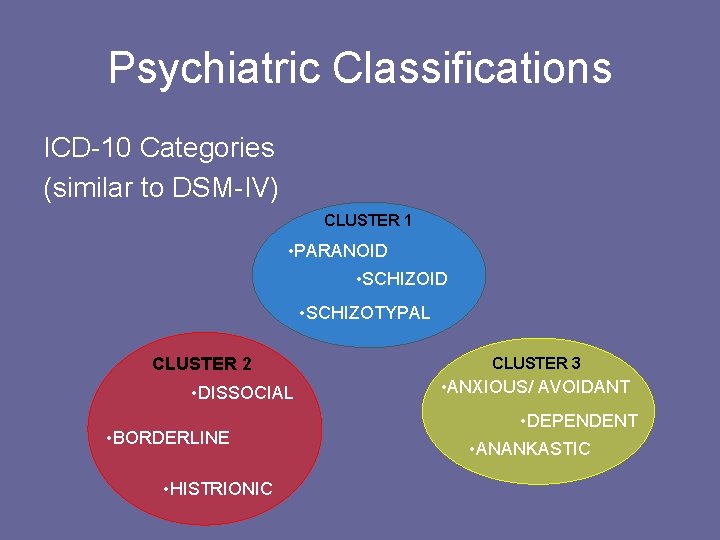
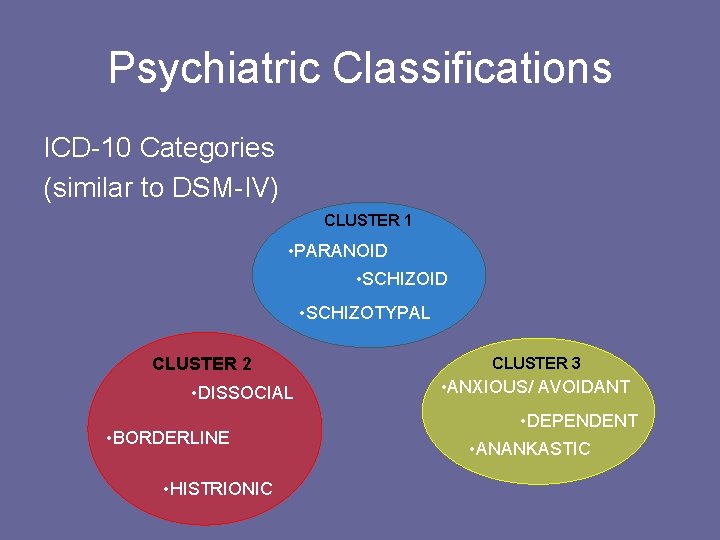
Psychiatric Classifications ICD-10 Categories (similar to DSM-IV) CLUSTER 1 • PARANOID • SCHIZOTYPAL CLUSTER 2 • DISSOCIAL • BORDERLINE • HISTRIONIC CLUSTER 3 • ANXIOUS/ AVOIDANT • DEPENDENT • ANANKASTIC
• New DSM – V due May 2013 After much debate – little change to classifications • New ICD – 11 due 2015 Likely to move to Dimensions (how badly affected is the person) rather than Categories (what type)
Dissocial Personality Disorder • Callous unconcern for the feelings of others • Irresponsible. No regard for social norms, rules and obligations. • Unable to maintain lasting relationships, though having no difficulty in starting them.
Dissocial Personality Disorder • Easily becomes frustrated, angry or violent. • Not able to feel guilt or to profit from experience or punishment. • Tends to blame others, or to offer explanations, for the behaviours that has brought the patient into conflict with society.
“Psychopathy” • Extreme form of antisocial/ dissocial personality disorder • Psychopathy Check-List – Revised – Cold, callous self-centred, predatory individuals – Strongly correlated with risk of future violence • Narrower group than dissocial category – often also fulfil antisocial/ narcissistic/ histrionic and paranoid
Borderline Personality Disorder • Does NOT mean the person may or may not have a PD • Historical terminology designating a condition on the “borderline” between Neurotic (anxiety/ phobias/ depression) and Psychotic (schizophrenia) conditions
Borderline Personality Disorder • BPD is called Emotionally Unstable Personality Disorder in the ICD-10 classification • It is sub-divided into – Impulsive Type And – Borderline Type
Borderline Personality Disorder • Emotionally unstable. • Person’s self-image, aims and internal preferences (including sexual) are often unclear or disturbed. • Chronic feelings of emptiness.
Borderline Personality Disorder • Becomes involved in intense and unstable relationships, with repeated emotional crisis. • Extreme efforts to avoid real or imagined abandonment. • Recurrent suicidal threats, gestures and behaviours or self-harming behaviours.
Borderline Personality Disorder • Tend to act without considering consequences • Lack of Impulse control • Transient stress-related paranoid ideas or severe dissociative symptoms.
Psychiatric Model of Personality Disorder • Not very accurate, despite all efforts to pin categories down • Looked at again for ICD-11 and DSM-V • People often fit more than one category • 2 people with BPD might have very different symptoms • Types have been shown to alter and change
PSYCHODYNAMIC APPROACH WHAT DOES IT OFFER? • Theory of Unconscious motivations – not all “manipulative” behaviour is consciously under the person’s control • Takes a developmental view • Defence mechanisms – the way people have to act at times to protect themselves from overwhelming emotional states
What does it offer? (cont) • The way the person’s internal state impacts emotionally on others • The importance of Attachment • THESE ARE ALL TOOLS TO INCREASE UNDERSTANDING
ATTACHMENT

Healthy development The caregiver’s emotionally attuned responses to the infant’s states becomes a source of information to the infant about his internal states
When things go wrong Still face experiment
Overview of Brain Development • How does a brain become a brain? – Adult brain weighs 3 lb – Quadruples in size between birth and 6 years – White matter increases throughout childhood; increasing speed of communication The Anatomy of Mentalization: A view from developmental neuroimaging (Giedd 2003)
Overview of Brain Development (2) • • • Overproduction of cells Competitive elimination – “survival of the fittest” Arborisation and pruning Sensitive periods of development Enormous plasticity of developing brain
This means that brain pathway development is affected by environmental (particularly Attachment) factors. People with Personality disorder have problems with how their brain functions, particularly under stress

Treatment/ Management
Treatment/ Management • Growing evidence for psychotherapy approaches – MBT, DBT – Long-term, fairly intensive treatment – Not widely available • Growing consensus on general principles for good management – NICE guidelines, Integrated Care Pathway (ICP) • Above mainly for BPD
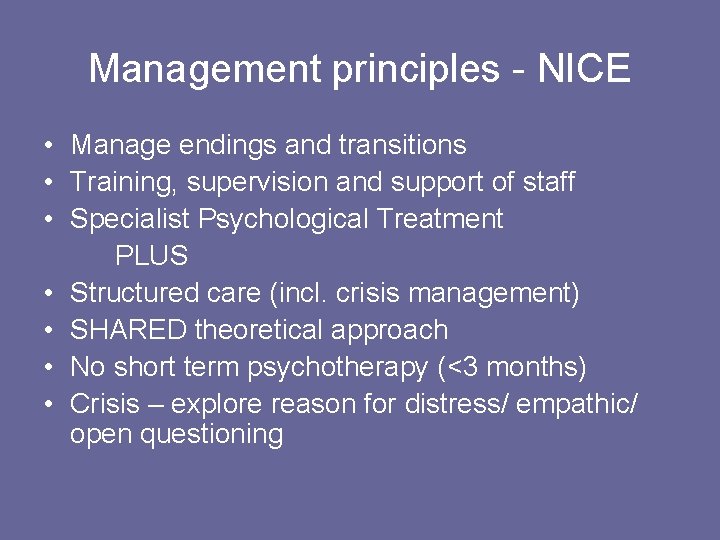
Management principles - NICE • Manage endings and transitions • Training, supervision and support of staff • Specialist Psychological Treatment PLUS • Structured care (incl. crisis management) • SHARED theoretical approach • No short term psychotherapy (<3 months) • Crisis – explore reason for distress/ empathic/ open questioning
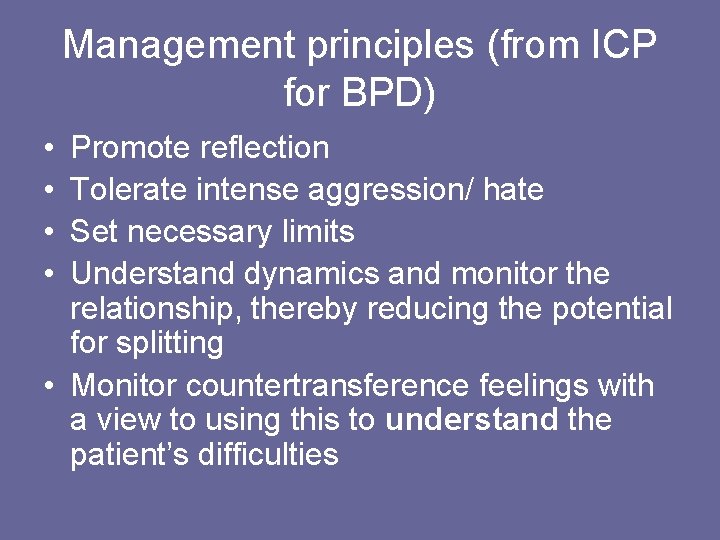
Management principles (from ICP for BPD) • • Promote reflection Tolerate intense aggression/ hate Set necessary limits Understand dynamics and monitor the relationship, thereby reducing the potential for splitting • Monitor countertransference feelings with a view to using this to understand the patient’s difficulties

Treatment/ Management • Little evidence that standard psychiatric inpatient care is helpful – may be harmful • Limited role for medication – poor evidence base – Important to treat co-morbid conditions – May be groups of symptoms that respond to some medications

Legislation
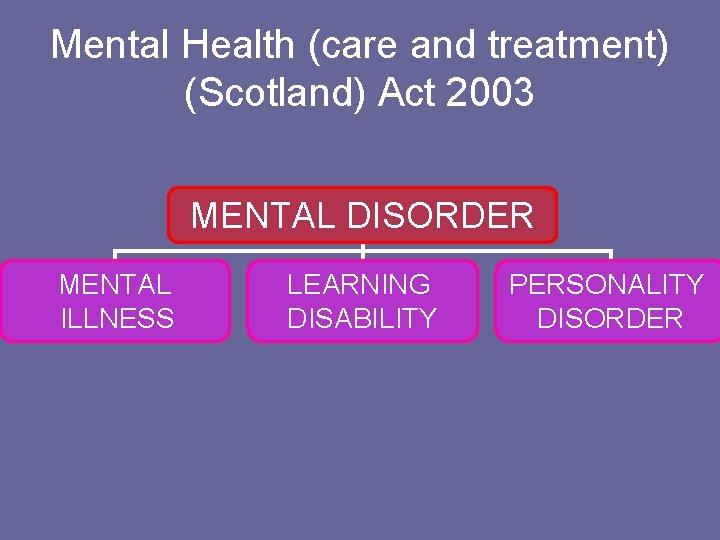
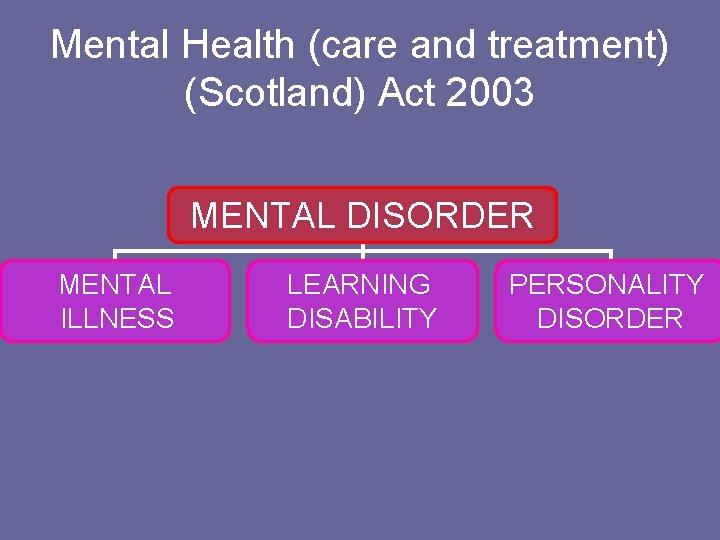
Mental Health (care and treatment) (Scotland) Act 2003 MENTAL DISORDER MENTAL ILLNESS LEARNING DISABILITY PERSONALITY DISORDER
Use of Compulsory Measures and Personality Disorder • PD is included in 2003 Mental Health Act, but people with PD often not thought to meet criteria for compulsory measures • Requires that – “person has a mental disorder which causes their ability to make decisions about treatment to be significantly impaired” – ? Impaired decision making
Use of Compulsory Measures and Personality Disorder • CTO – requires that “medical treatment is available which is likely to prevent disorder worsening or likely to alleviate the symptoms or effects of the disorder” - and that there is significant risk to the patient or any other person if the patient were not provided with such treatment
“Medical treatment” is defined as : • Pharmacological or physical treatment (such as ECT) • Psychological and social interventions • Nursing • Care • Habilitation – including education and training in work, social and independent living skills • Rehabilitation
Criminal Procedures (Scot) Act 1995, amended by MH(C&Tr)(Scot) Act 2003 • PD included in 2003 Act as mental disorder • Criterion of “significantly impaired ability to make decisions about treatment” is EXCLUDED for mentally disordered offenders, therefore • Issues of treatability are prominent • Treatability harder to argue for antisocial/ psychopathic disorders
Treatability of Dissocial/ Antisocial disorders • Many treatment models thought to be useful to some degree – anger management, – CBT approaches, – therapeutic community models No great evidence base for any of these
Use of Compulsory Measures and Personality Disorder - FORENSIC • Routine practice in Scotland NOT to admit on compulsory basis, individuals with a primary diagnosis of PD to forensic units • Focus of forensic mental health services is on psychotic disorders • 1976 Carstairs incident (Darjee and Crichton 2003)
(cont) • Challenges re “treatability” – unconditional discharge of a patient from Carstairs on grounds that he was untreatable - 1999 • Led to MH(public safety and appeals)(Scotland) Act 1999 – changed legislative definition of mental illness to include PD and added a criterion of serious risk to others – so untreatable restricted pts could still be detained
Adults with Incapacity (Scotland) Act 2000 • Usually applies to people with Dementia/ Learning Disability/ Brain Injury • Can also be used in other severe and enduring mental disorders where CAPACITY shown to be impaired
AWI (Scotland) 2000 (cont. ) • For the purposes of the Act, 'incapable' means incapable of: • acting on decisions; or • making decisions; or – communicating decisions; or – understanding decisions; or – retaining the memory of decisions • in relation to any particular matter due to mental disorder
Adult Support and Protection (Scotland) Act 2007 • Adult is engaging (or is likely to engage) in conduct which causes (or is likely to cause) self-harm • Almost the definition of many personality disorders • Principles – Must provide benefit – Least restrictive
 Expert in consultant liaison psychiatrist
Expert in consultant liaison psychiatrist Psychiatrist leicester
Psychiatrist leicester Verna and sam case study answers
Verna and sam case study answers Andy williams robert williams
Andy williams robert williams Robbie williams janet williams
Robbie williams janet williams Weird wild wacky personality disorders
Weird wild wacky personality disorders Inflexible personality
Inflexible personality Class a personality disorders
Class a personality disorders Paranoid personality disorder
Paranoid personality disorder Type c personality disorder
Type c personality disorder Cluster c personality disorders
Cluster c personality disorders Cluster b disorder
Cluster b disorder Cluster b personality disorder
Cluster b personality disorder Dramatic personality disorders
Dramatic personality disorders Personality disorder types
Personality disorder types Shebani sethi
Shebani sethi Cluster b personality disorders
Cluster b personality disorders Dsm v personality disorders
Dsm v personality disorders Schizoid
Schizoid Diathesis stress model
Diathesis stress model Dr john hillery
Dr john hillery Banshee psychiatrist
Banshee psychiatrist Dr hoosen psychiatrist
Dr hoosen psychiatrist Uuuu0
Uuuu0 Psychiatrist vs psychologist
Psychiatrist vs psychologist Shahid hussain psychiatrist
Shahid hussain psychiatrist Dr rebecca lawrence psychiatrist
Dr rebecca lawrence psychiatrist David ash psychiatrist
David ash psychiatrist Dr moghul psychiatrist
Dr moghul psychiatrist Dr peter byrne
Dr peter byrne Dr derek lovell psychiatrist
Dr derek lovell psychiatrist Dr shanaya rathod
Dr shanaya rathod Dr fionnuala o'loughlin psychiatrist
Dr fionnuala o'loughlin psychiatrist Dr joubert psychiatrist
Dr joubert psychiatrist Sean fernandez
Sean fernandez Steve pearce psychiatrist
Steve pearce psychiatrist Dr simon howard psychiatrist
Dr simon howard psychiatrist Donna grant psychiatrist
Donna grant psychiatrist Epicor configurator demo
Epicor configurator demo Sustainable tourism consultant jobs
Sustainable tourism consultant jobs What is a consultant radiographer
What is a consultant radiographer Chloe ashford
Chloe ashford Modern data architecture consulting
Modern data architecture consulting Pcnse certificate
Pcnse certificate New consultant training
New consultant training Multiple consultant report
Multiple consultant report Assertivel
Assertivel Nous hospital consultant
Nous hospital consultant Consultant knowledge management
Consultant knowledge management Dan rogers it consultant
Dan rogers it consultant Behavioral genetics consultant
Behavioral genetics consultant Dr gupta stepping hill hospital
Dr gupta stepping hill hospital Associate consultant in capgemini
Associate consultant in capgemini Diagnosis
Diagnosis Nutra metrix
Nutra metrix