Migraine and other headaches Dr David Kernick Exeter






















- Slides: 101
Migraine and other headaches Dr David Kernick Exeter Headache clinic
Outline n Where does headache come from? n Epidemiology n Classification n Management

HEADACHE – pain from cranium that can be reffered to or from the neck and face
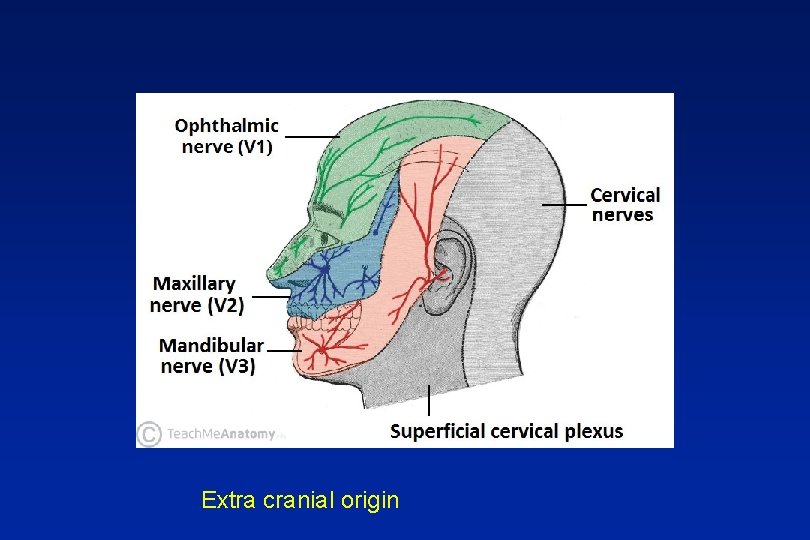
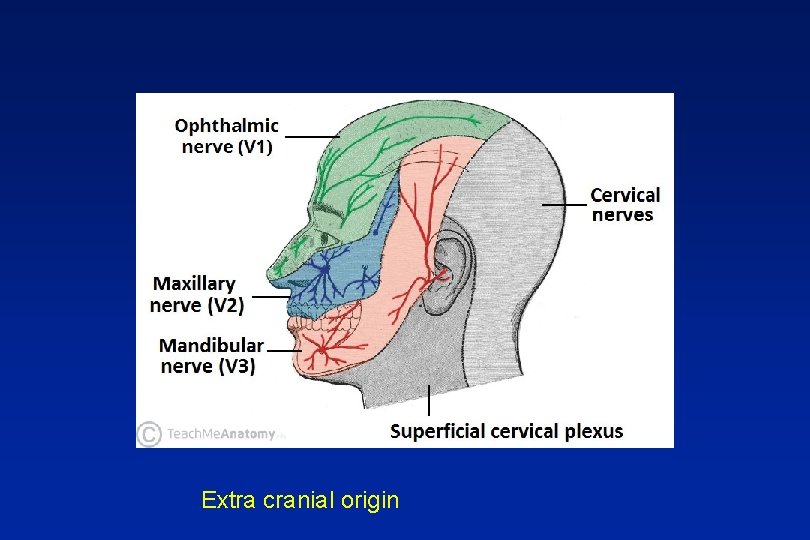
Extra cranial origin
Where does the pain come from? Extra - cranial n Arteritis n Neuralgia n Muscle tension n Facial structures
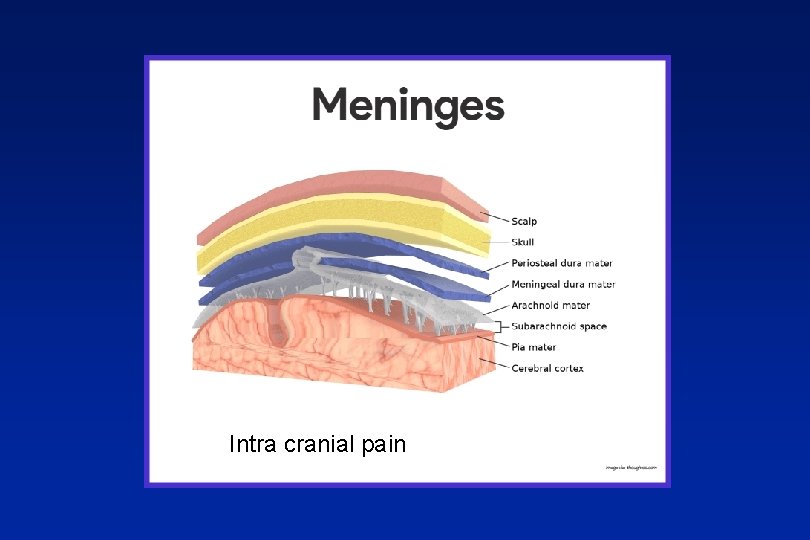
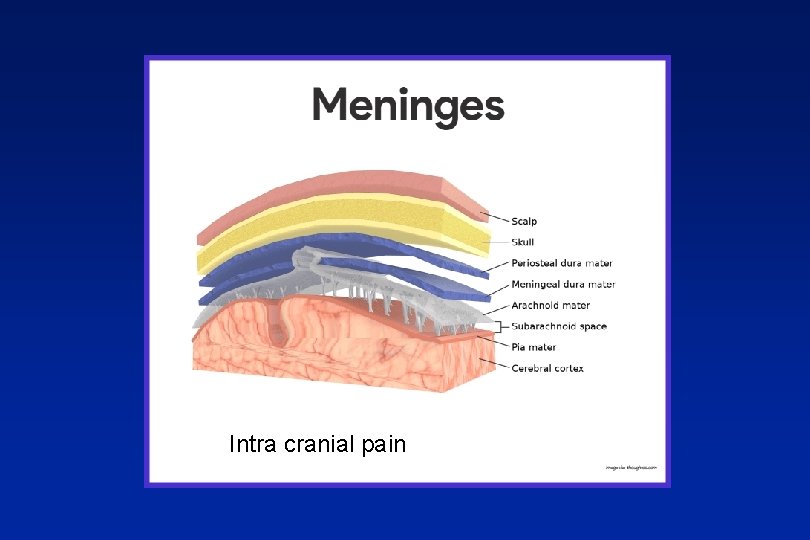
Intra cranial pain
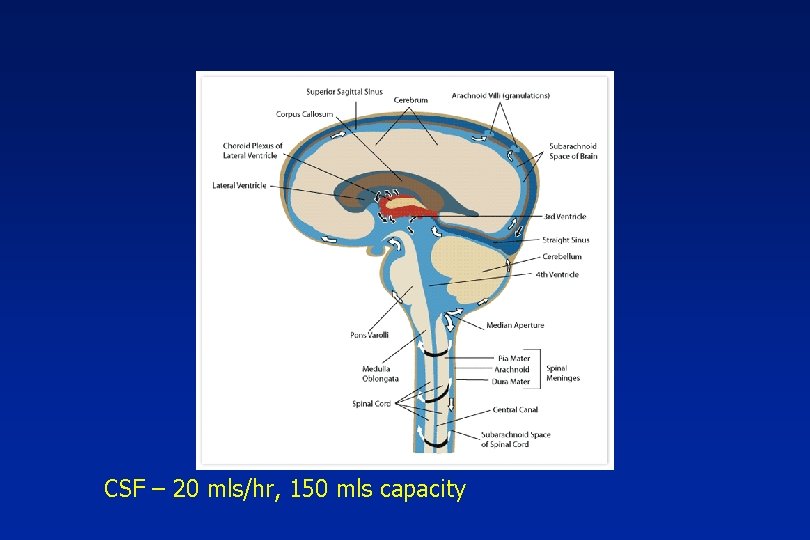
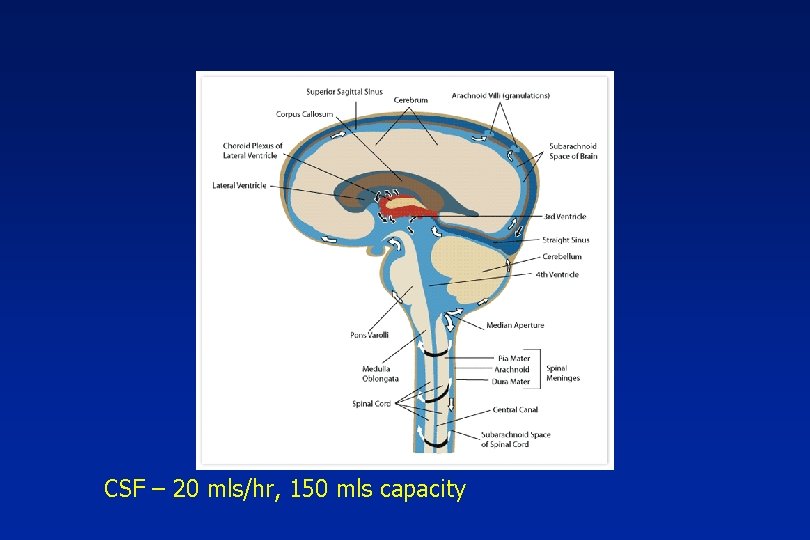
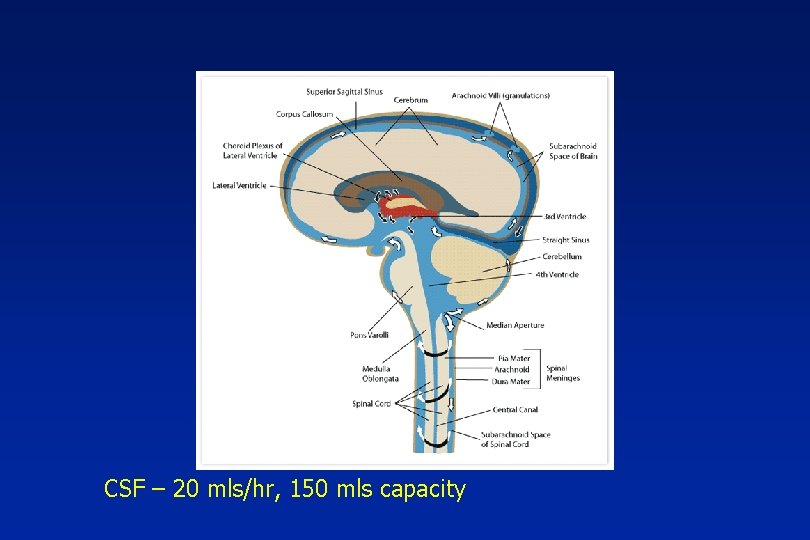
CSF – 20 mls/hr, 150 mls capacity
Where does the pain come from? Intra – cranial (dural pain fibres) n Tension – raised intracranial pressure n Compression – tumour n Inflammation - migraine, meningitis, blood
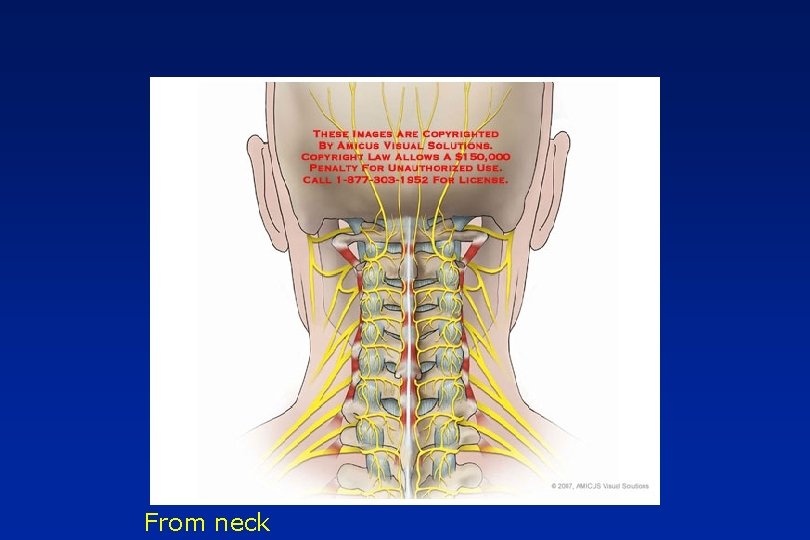
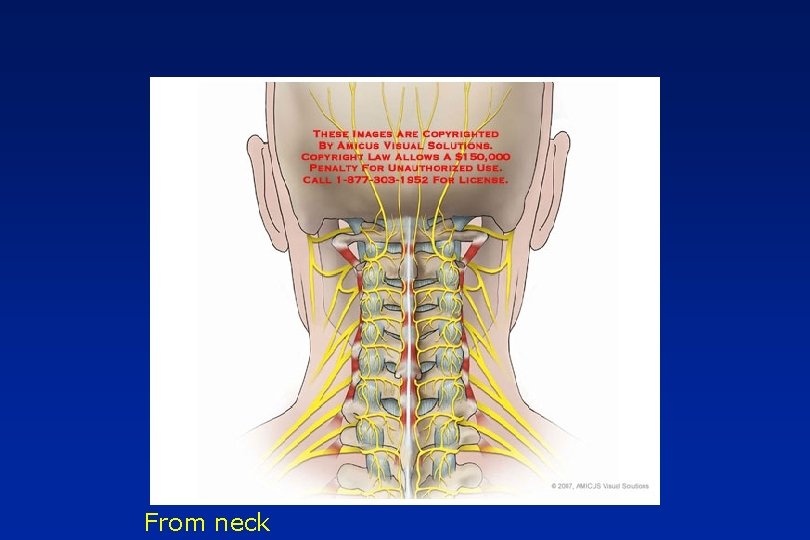
From neck
Migraineur on metopralol. Uses salbutamol inh 5 times a week.

Respiratory effect of beta-blockers in people with asthma and cardiovascular disease: population-based nested case control study Daniel R. 2017
35, 502 with active asthma and CVD 14. 1% and 1. 2% were prescribed cardioselective and non-selective beta-blockers Results Beta-blocker use was not associated with a significantly increased risk of moderate or severe asthma exacerbations. Conclusion Cardioselective beta-blockers in asthma and CVD were not associated with a significantly increased risk of moderate or severe asthma exacerbations and potentially could be used more widely when strongly indicated.
Outline n Where does headache come from? n Epidemiology n Classification n Management
Epidemiology n Prevalence n Incidence n Impact – Qo. L, Economic n Health seeking behaviour
Headache annual prevalence n Population: n Tension type 70% n Migraine 12%, n Cluster 0. 1%

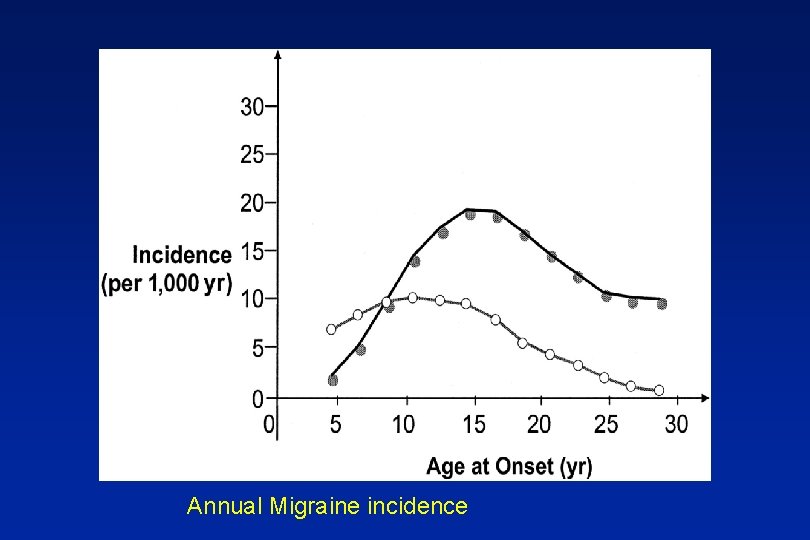
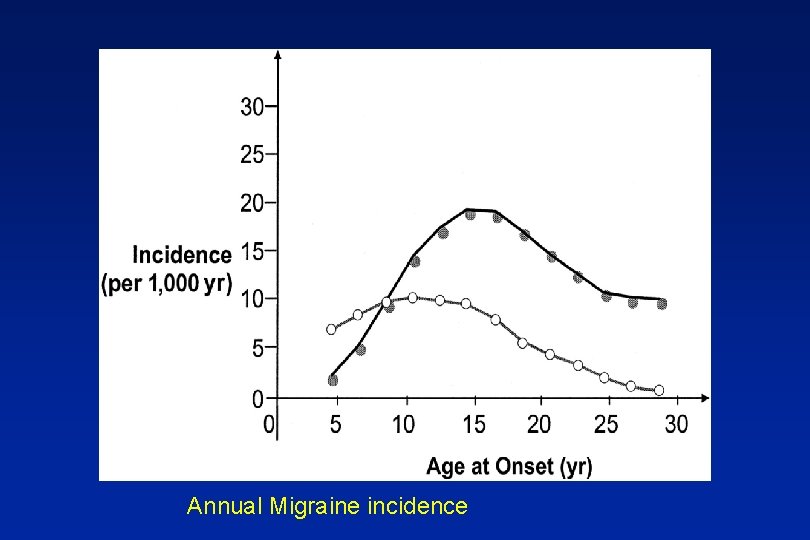
Annual Migraine incidence
Epidemiology n Prevalence n Incidence n Impact – Qo. L, Economic n Health seeking behaviour

National Challenge Reference Approximately 9 million people live with migraine in the UK Migraine: the seventh disabler (Steiner et al 2013) Migraine is the second leading cause of years lived with disability Global Burden of Disease (The Lancet 2016) 25 million days lost from work or school each year in England because of migraine alone The prevalence and disability burden of adult migraine in England their relationships to age, gender and ethnicity. (Steiner et al 2003)
Headache impact n 20% adult population – headache impacts on their quality of life Kernick 2001
Impact upon children Kernick BJGP 2009 n 20% - 1 or more headaches each week, significant impact home or school
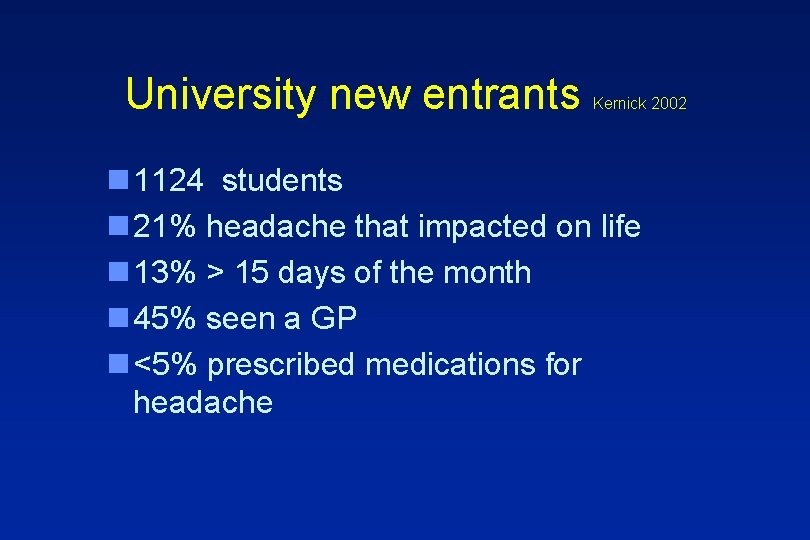
University new entrants Kernick 2002 n 1124 students n 21% headache that impacted on life n 13% > 15 days of the month n 45% seen a GP n <5% prescribed medications for headache
Epidemiology n Prevalence n Incidence n Impact – Qo. L, Economic n Health seeking behaviour
When people develop headache what do they think they have? What do GPs think they have? What do they actually have?
When people come to see you what do they think they have? n Need glasses n Blood pressure n Brain tumour
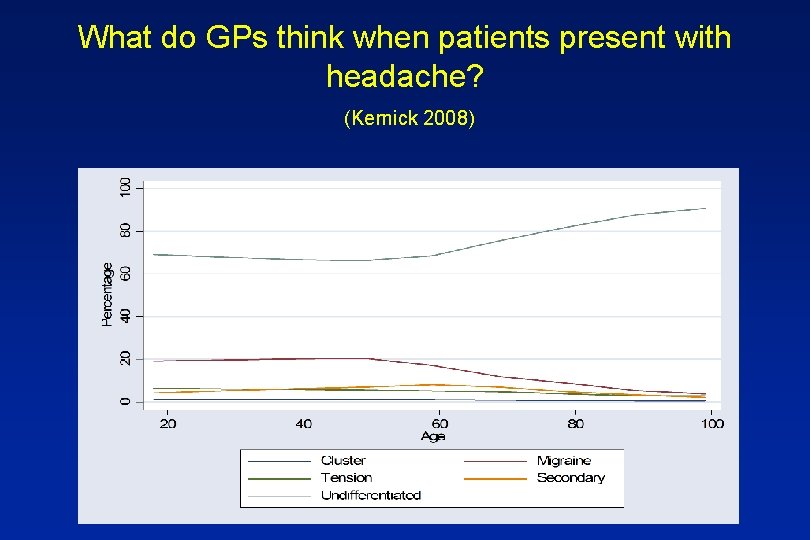
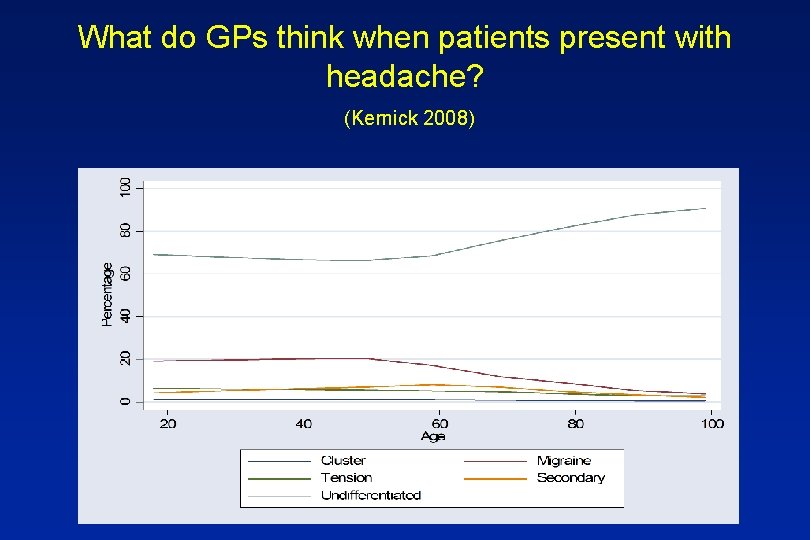
What do GPs think when patients present with headache? (Kernick 2008)
What do patients have when they present to GP with headache? Landmark Study n 85% migraine n 10% Tension type headache n 5% secondary headache n <1% other types of headache
What happens? n Less than 50% migraineurs will see GP n Less than 10% will receive Triptan Walling 2006 n 10% of those who would benefit from prevention receive it Rahimtoola 2005
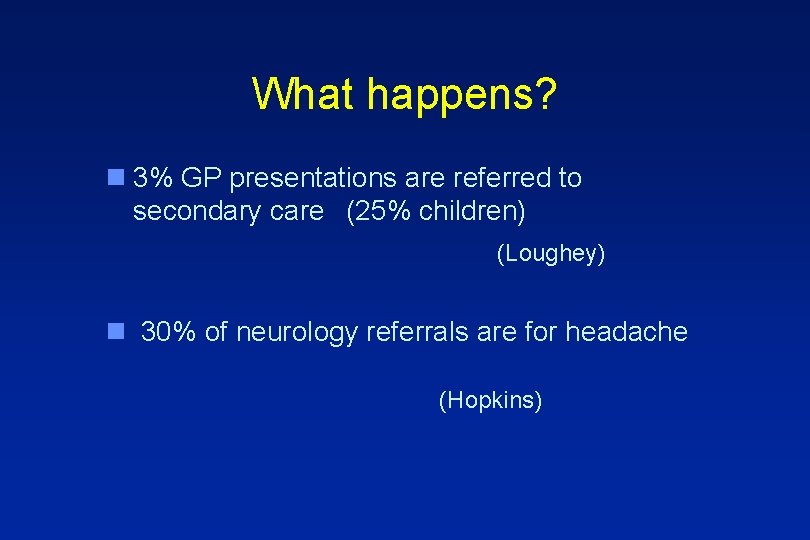
What happens? n 3% GP presentations are referred to secondary care (25% children) (Loughey) n 30% of neurology referrals are for headache (Hopkins)
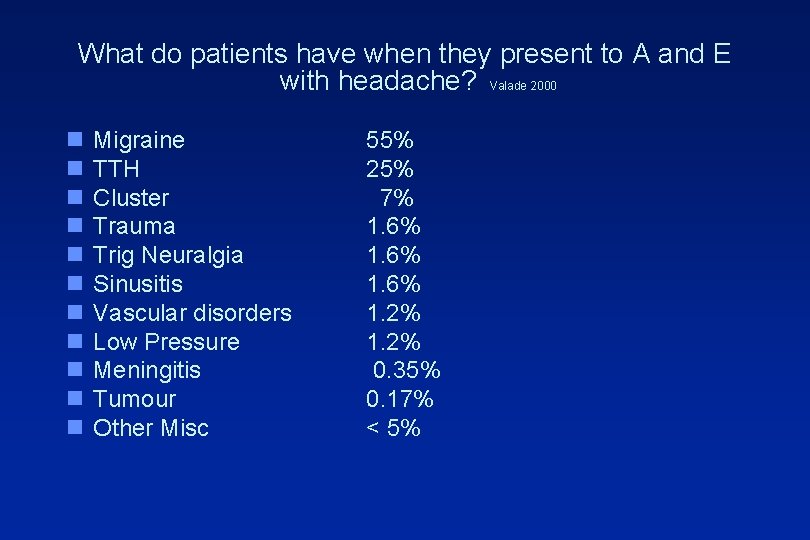
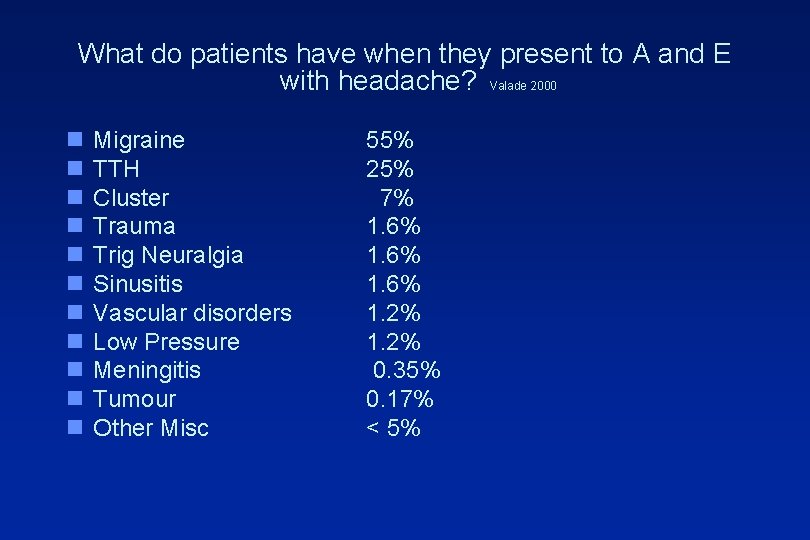
What do patients have when they present to A and E with headache? Valade 2000 n n n Migraine TTH Cluster Trauma Trig Neuralgia Sinusitis Vascular disorders Low Pressure Meningitis Tumour Other Misc 55% 25% 7% 1. 6% 1. 2% 0. 35% 0. 17% < 5%

What is the unmet need in primary care? Kernick Journal of Headache and Pain 2008 n < 50 % adults, <10% children see GP
Why don’t people seek help?
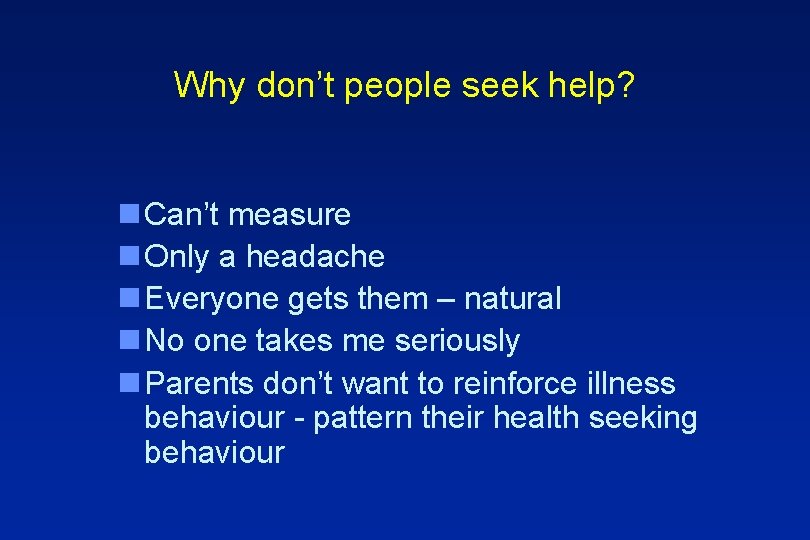
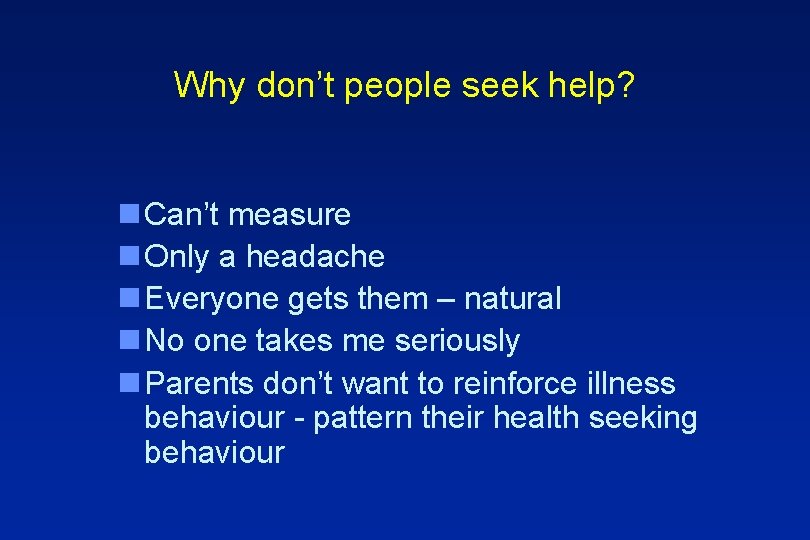
Why don’t people seek help? n Can’t measure n Only a headache n Everyone gets them – natural n No one takes me seriously n Parents don’t want to reinforce illness behaviour - pattern their health seeking behaviour

How should we deliver headache services n Self management n GPs first line management n GPSI support n Tertiary headache centres
Outline n Where does headache come from? n Epidemiology n Classification n Management
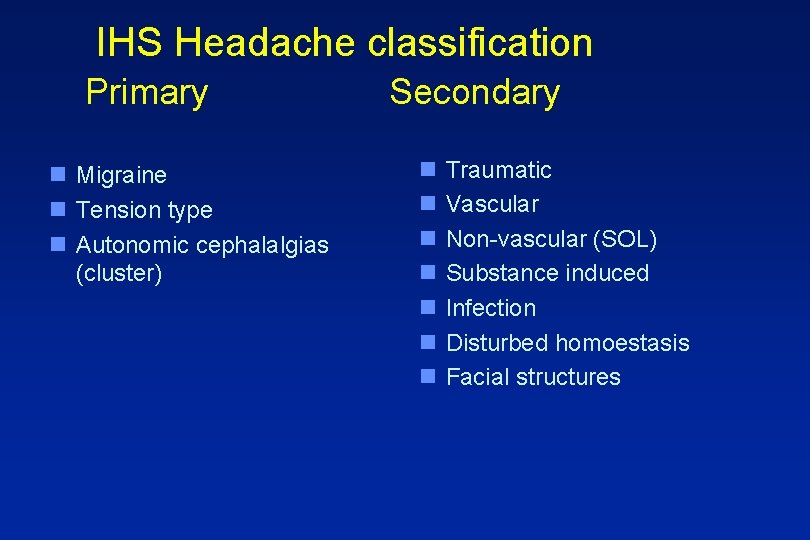
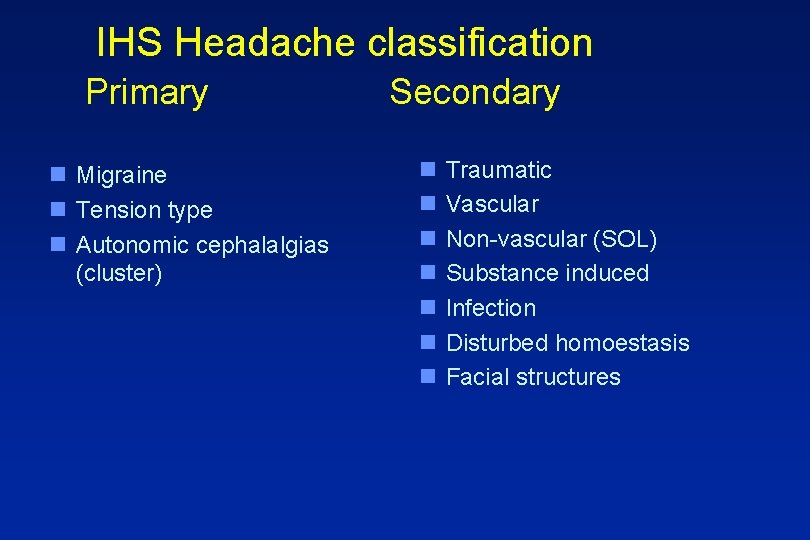
IHS Headache classification Primary n Migraine n Tension type n Autonomic cephalalgias (cluster) Secondary n n n n Traumatic Vascular Non-vascular (SOL) Substance induced Infection Disturbed homoestasis Facial structures
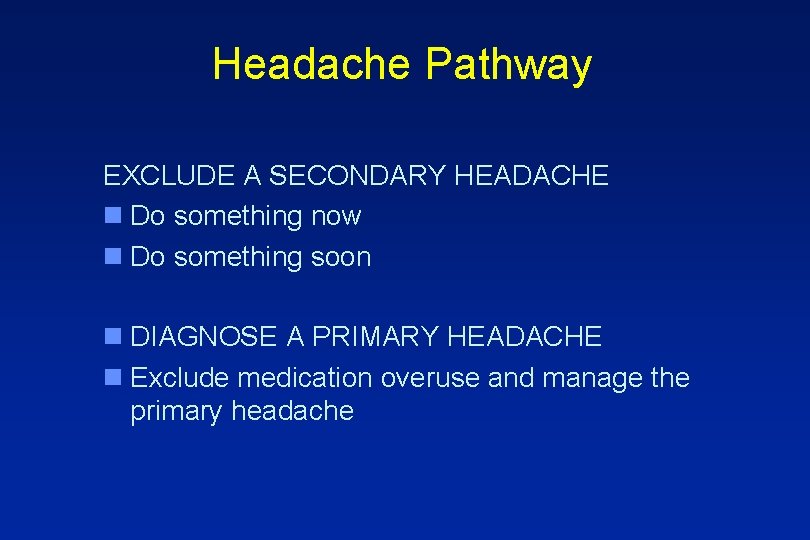
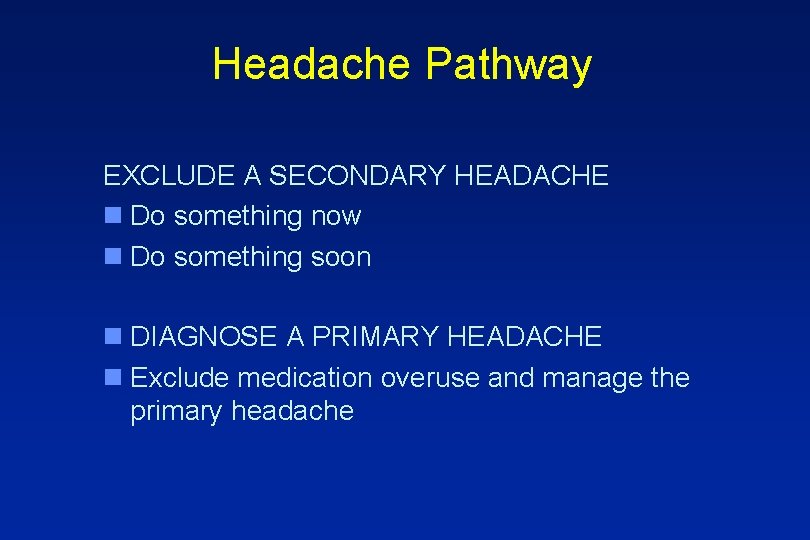
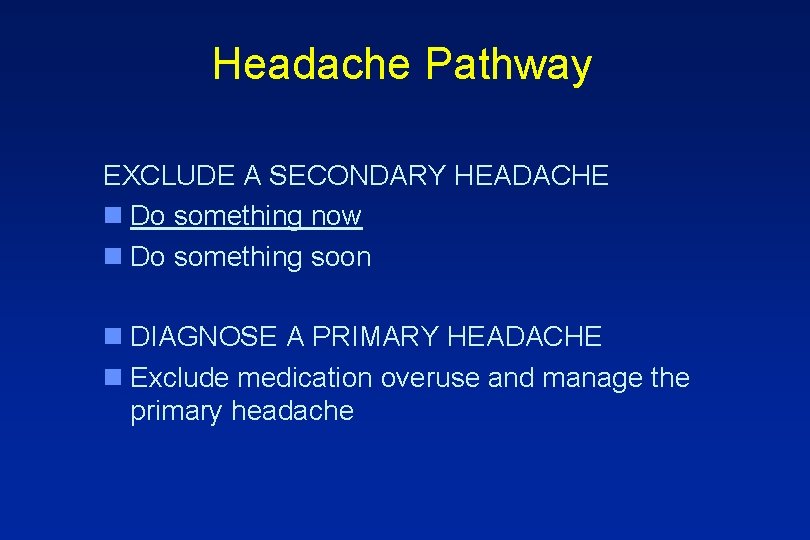
Headache Pathway EXCLUDE A SECONDARY HEADACHE n Do something now n Do something soon n DIAGNOSE A PRIMARY HEADACHE n Exclude medication overuse and manage the primary headache
Headache Pathway EXCLUDE A SECONDARY HEADACHE n Do something now n Do something soon n DIAGNOSE A PRIMARY HEADACHE n Exclude medication overuse and manage the primary headache
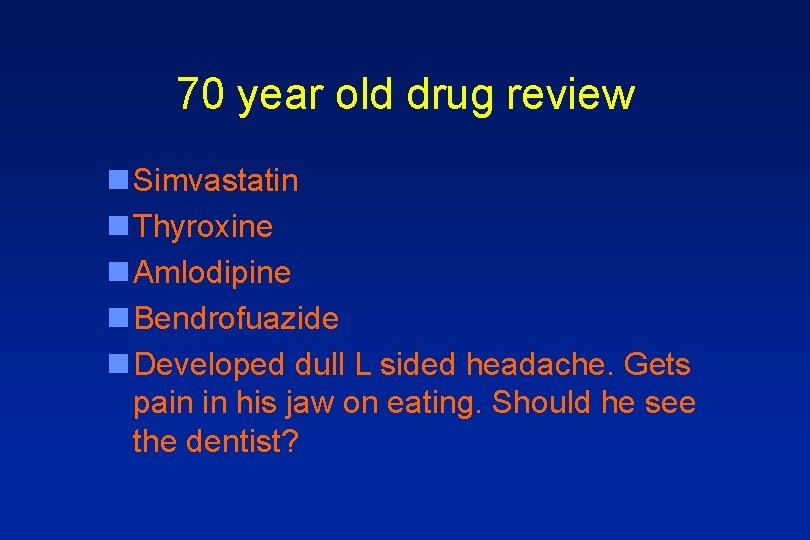
70 year old drug review n Simvastatin n Thyroxine n Amlodipine n Bendrofuazide n Developed dull L sided headache. Gets pain in his jaw on eating. Should he see the dentist?
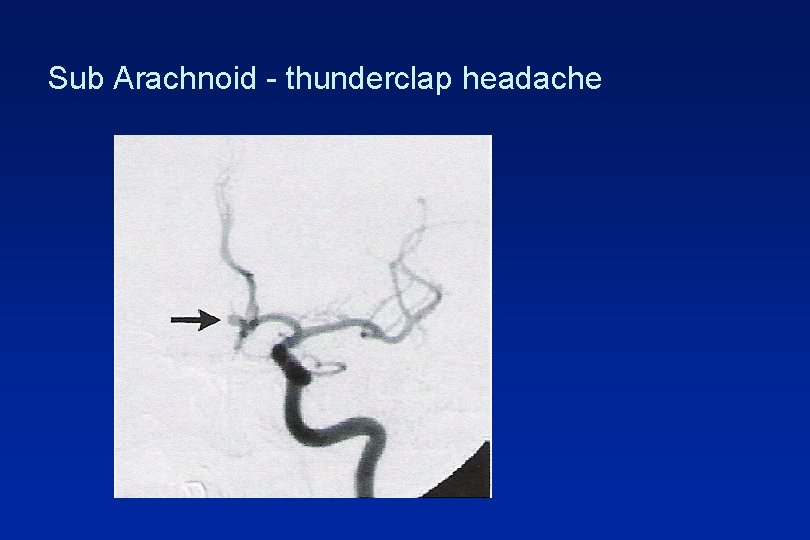
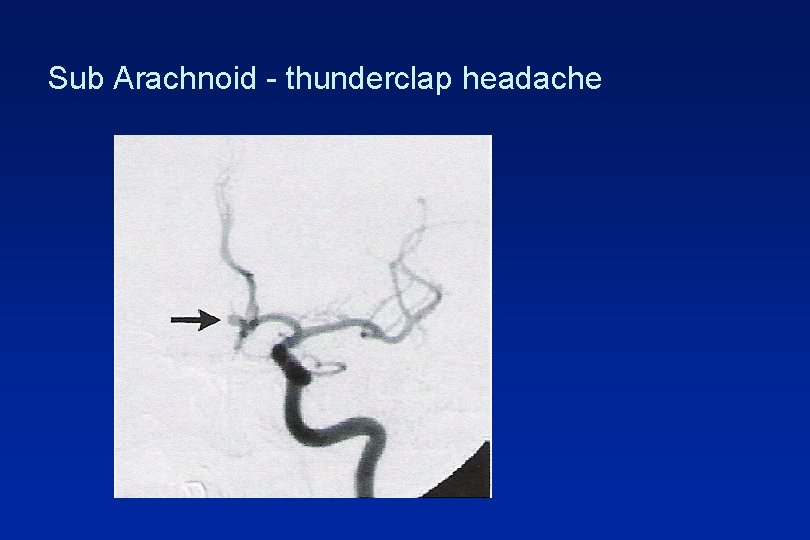
Sub Arachnoid - thunderclap headache

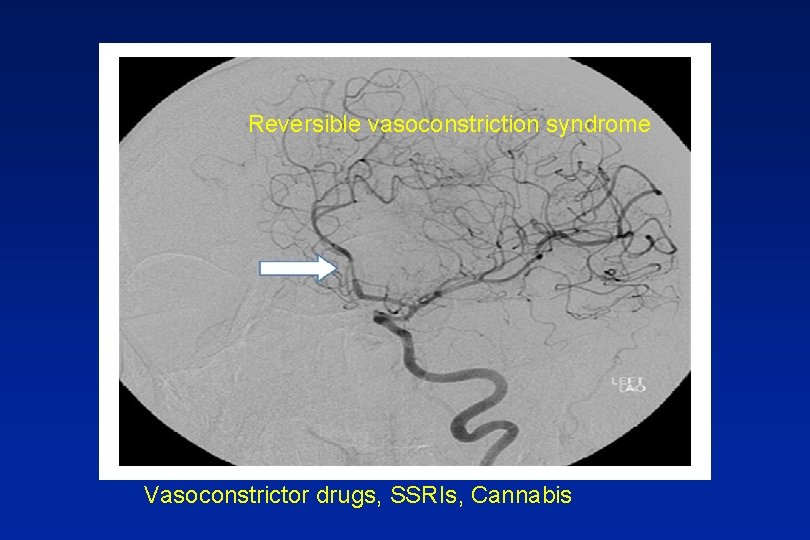
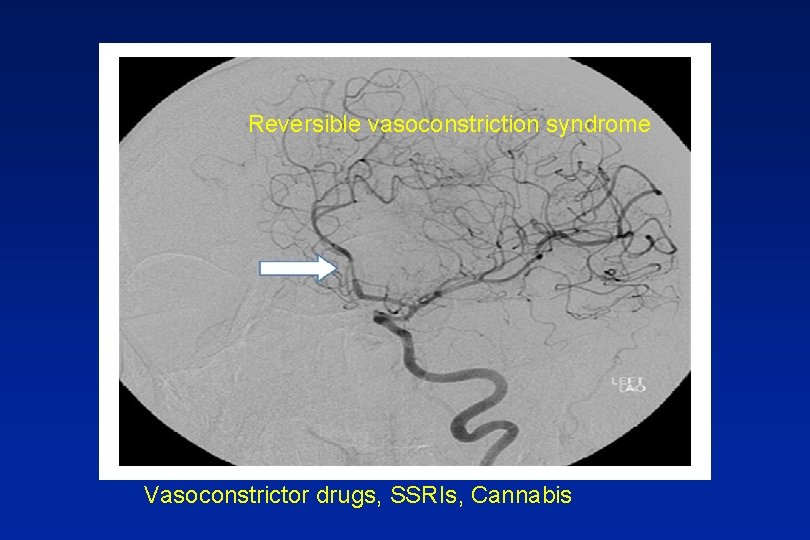
Reversible vasoconstriction syndrome Vasoconstrictor drugs, SSRIs, Cannabis

Thrombophilia

Meningitis

Malignant hypertension
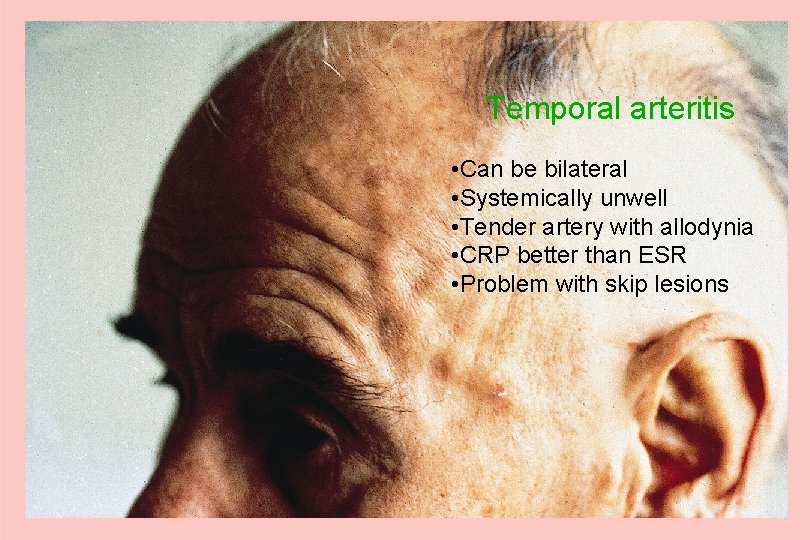
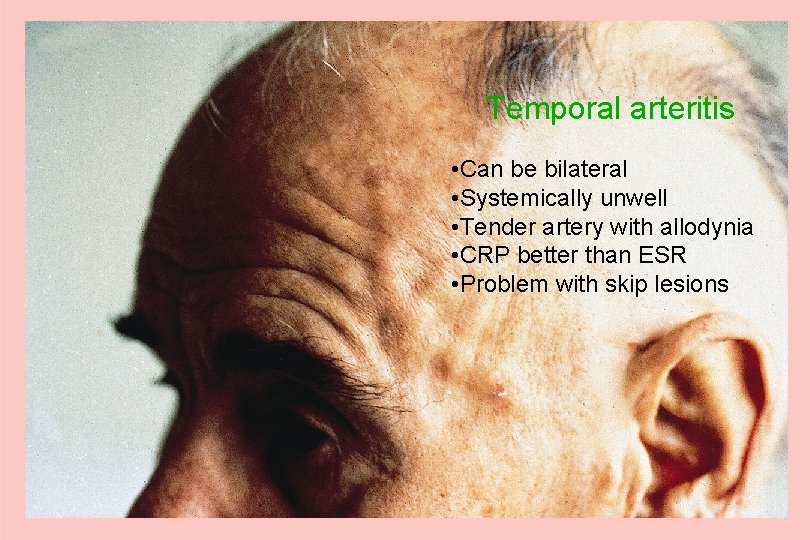
Temporal arteritis • Can be bilateral • Systemically unwell • Tender artery with allodynia • CRP better than ESR • Problem with skip lesions
Headache Pathway EXCLUDE A SECONDARY HEADACHE n Do something now n Do something soon n DIAGNOSE A PRIMARY HEADACHE n Exclude medication overuse and manage the primary headache
Exercise headache 1/3
Pressure – too high. Idiopathic intracranial hypertension n Non specific headache n Tinnitus n Visual field/acuity defect n Papilloedema
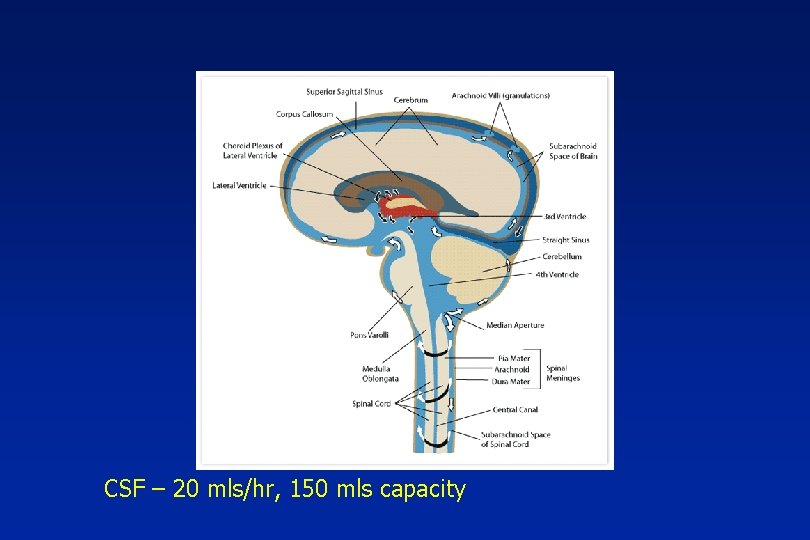
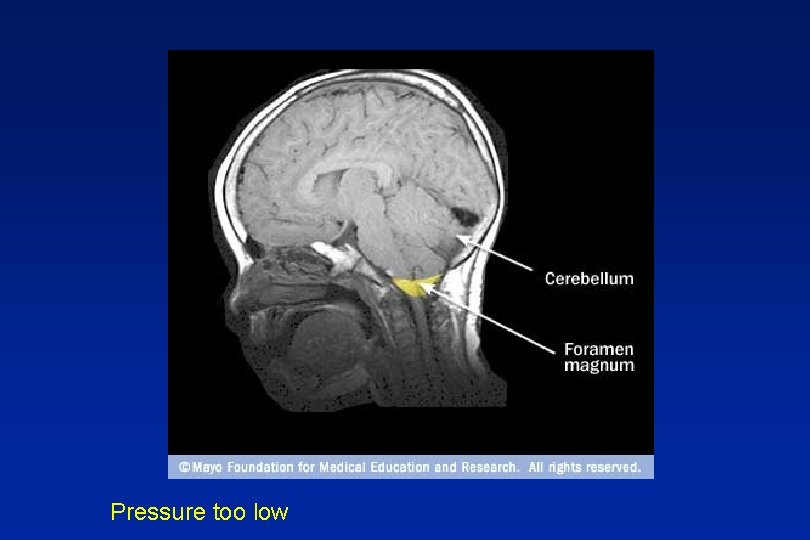
CSF – 20 mls/hr, 150 mls capacity
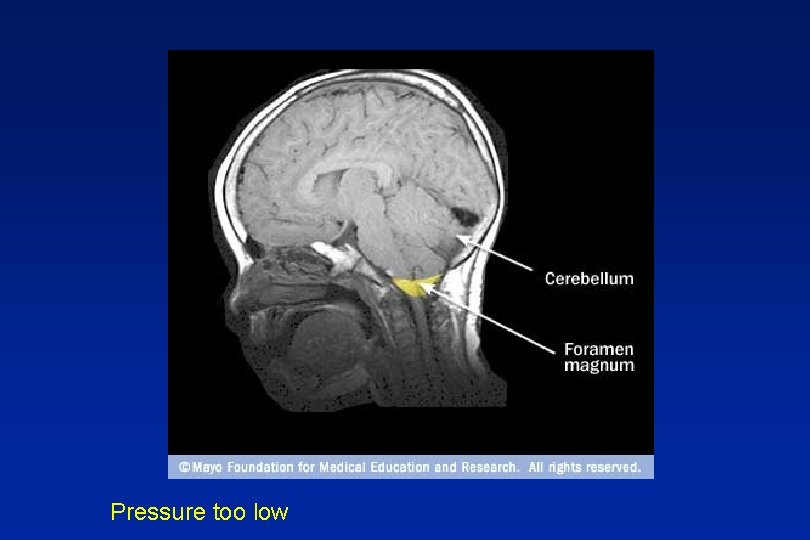
Pressure too low
Space occupying lesions Stretch, compression, blockage n Benign – cysts, A-V malformations n Malignant – primary secondary


Red Flags n Abnormal neurological symptoms or signs n History of cancer elsewhere
Orange Flags n Aggregated by Valsalva manoeuvre n Headache with significant change in character n Awakes from sleep n New headache over 50 years n Memory loss n Personality change
Headache Pathway EXCLUDE A SECONDARY HEADACHE n Do something now n Do something soon n DIAGNOSE A PRIMARY HEADACHE n Exclude medication overuse and manage the primary headache
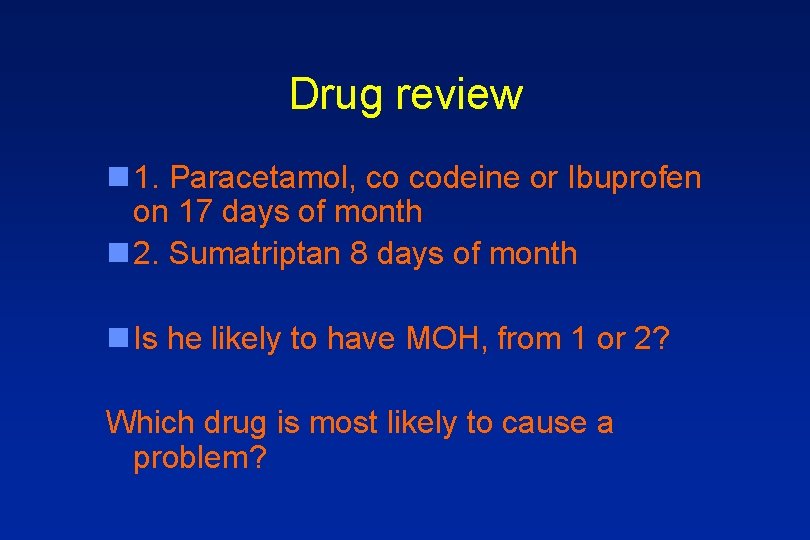
Drug review n 1. Paracetamol, co codeine or Ibuprofen on 17 days of month n 2. Sumatriptan 8 days of month n Is he likely to have MOH, from 1 or 2? Which drug is most likely to cause a problem?
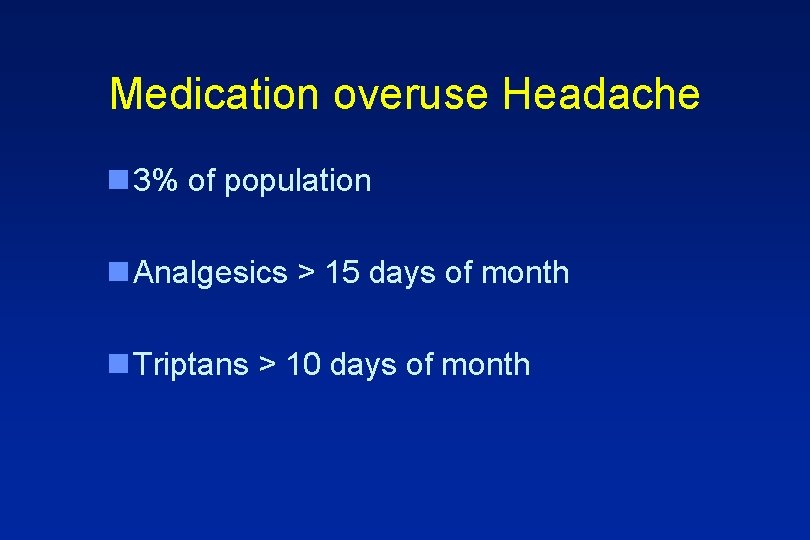
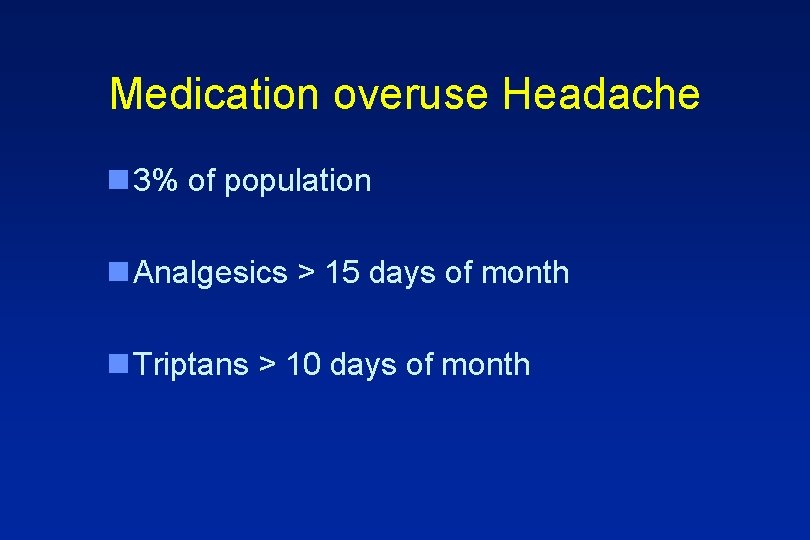
Medication overuse Headache n 3% of population n Analgesics > 15 days of month n Triptans > 10 days of month
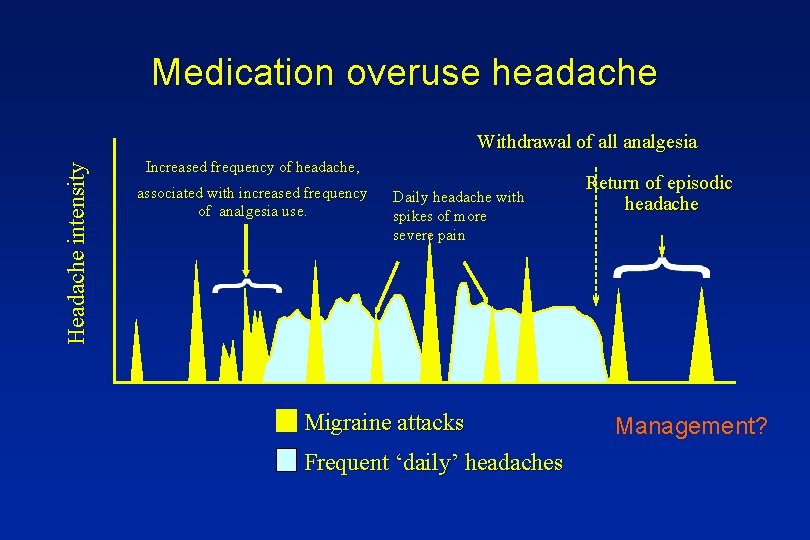
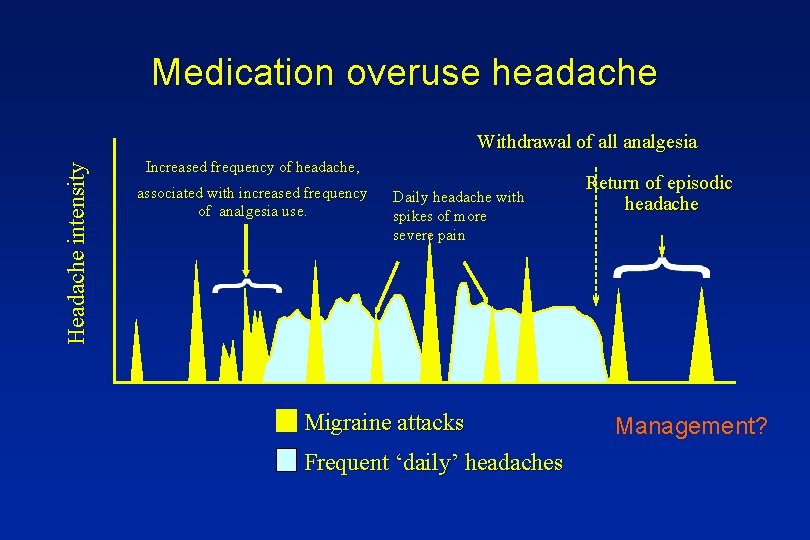
Medication overuse headache Headache intensity Withdrawal of all analgesia Increased frequency of headache, associated with increased frequency of analgesia use. Daily headache with spikes of more severe pain Migraine attacks Frequent ‘daily’ headaches Return of episodic headache Management?
Headache Pathway EXCLUDE A SECONDARY HEADACHE n Do something now n Do something soon n DIAGNOSE A PRIMARY HEADACHE n Exclude medication overuse and manage the primary headache
Primary Headaches n Migraine n Tension Type n Cluster n n n Paroxysmal hemicrania Hemicrania continua SUNCT Primary cough headache NPDH ect
A 30 year old male n Pain in L eye n Lasts 30 minutes, 5 times a day n GP diagnosed migraine given oral sumatriptan 100 mg and propanolol 160 MR but not working?

Cluster - Autonomic Cephalopathy n High impact ++ n Peri-orbital clusters 15 mins - 3 hours n Cluster attacks and periods n Unilateral autonomic features n Acute or chronic
Cluster treatment n Injectable Sumatriptan n Nasal Zolmitriptan n Short term steroids n Oxygen 100% n Verapamil
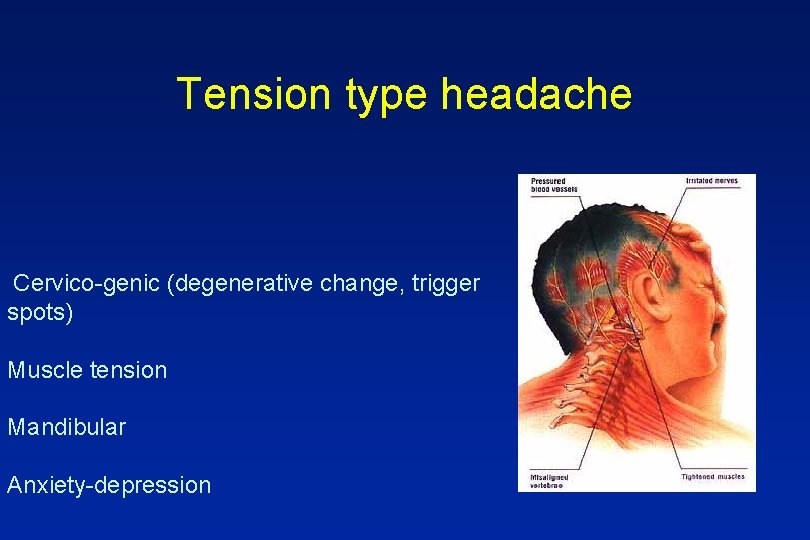
Tension type headache Cervico-genic (degenerative change, trigger spots) Muscle tension Mandibular Anxiety-depression

Migraine – the default diagnosis
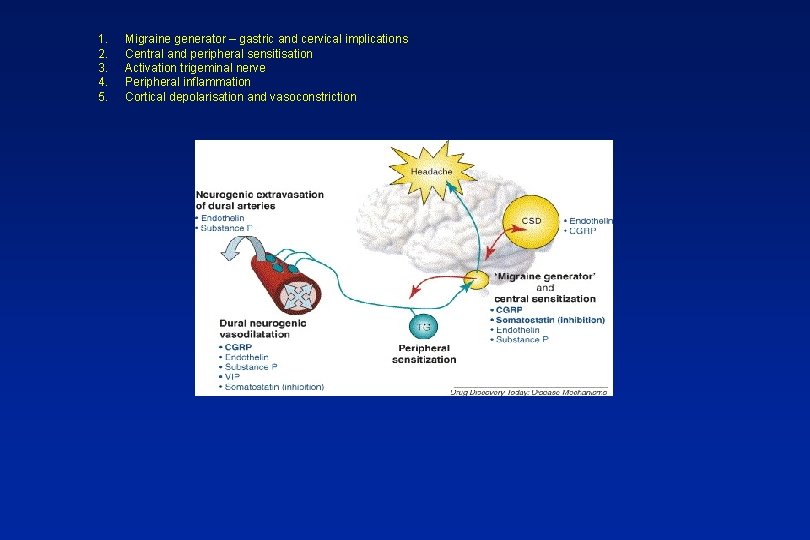
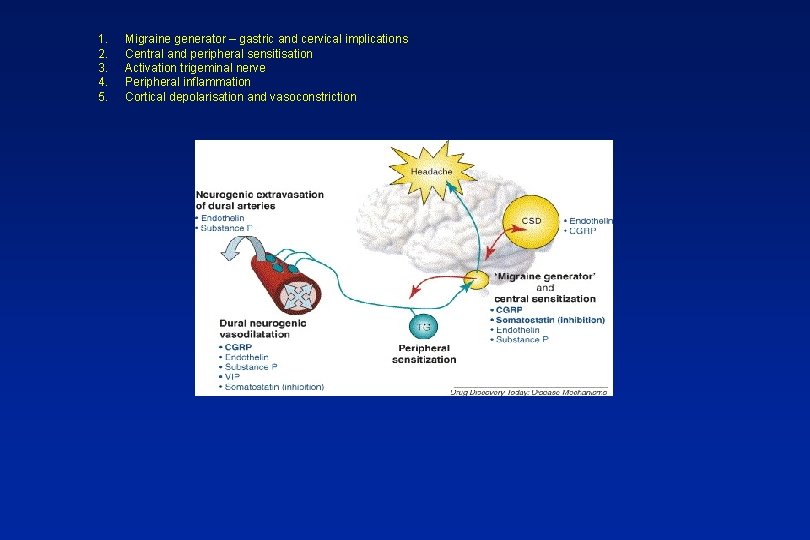
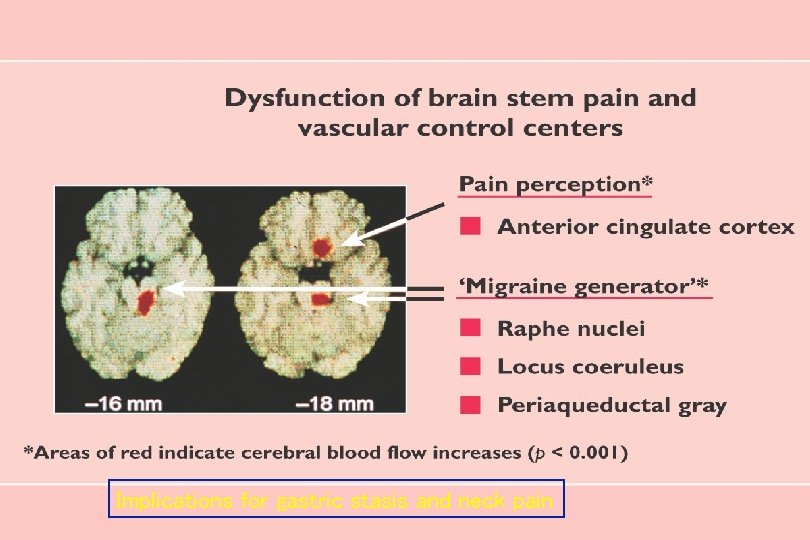
1. 2. 3. 4. 5. Migraine generator – gastric and cervical implications Central and peripheral sensitisation Activation trigeminal nerve Peripheral inflammation Cortical depolarisation and vasoconstriction Classifying headache 2
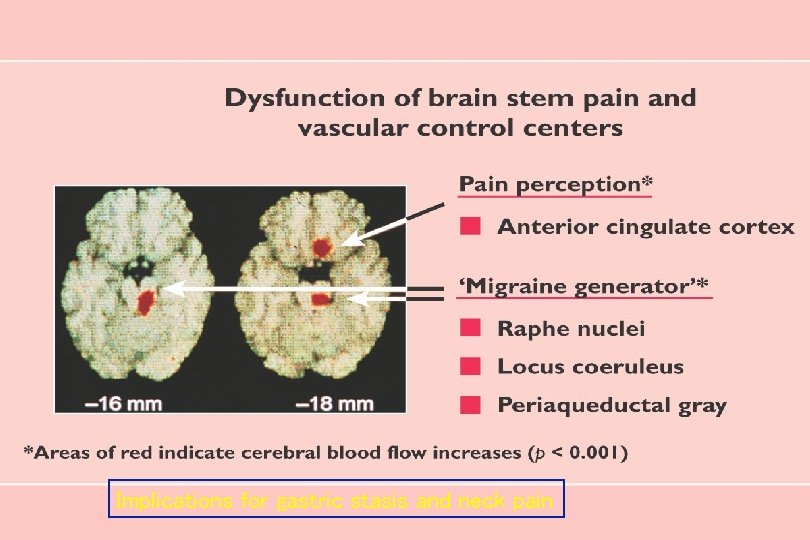
Implications for gastric stasis and neck pain
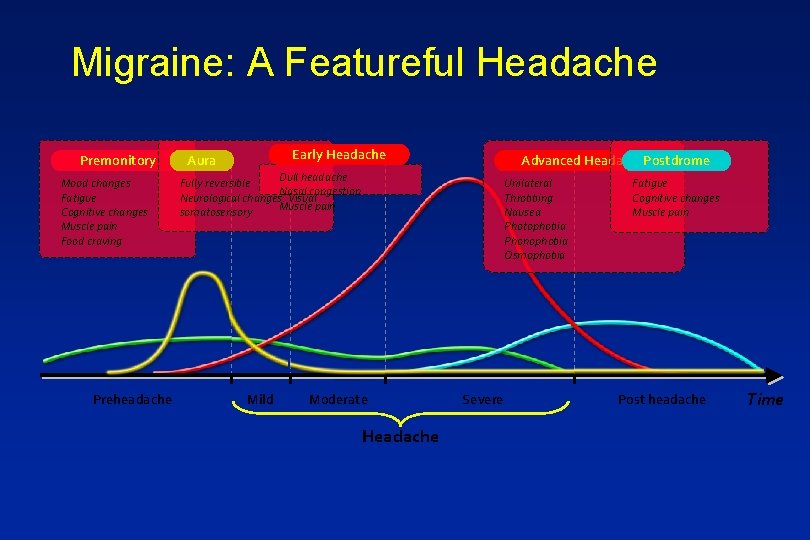
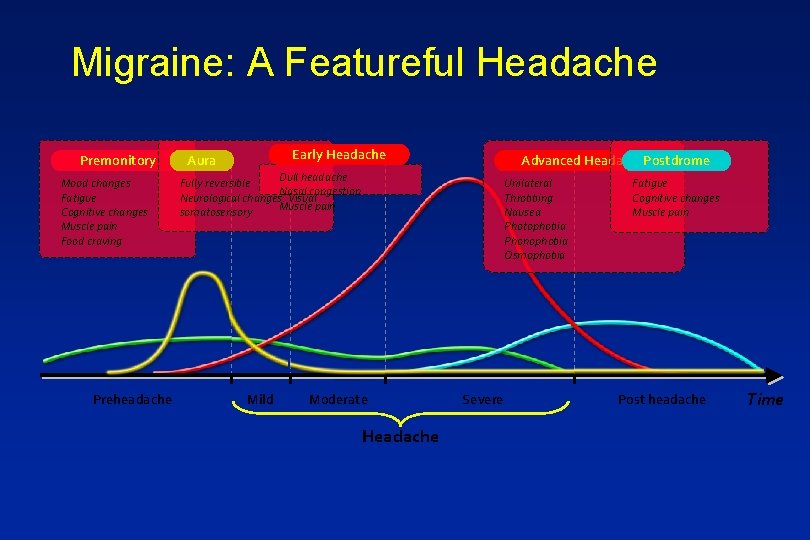
Migraine: A Featureful Headache Premonitory Mood changes Fatigue Cognitive changes Muscle pain Food craving Preheadache Early Headache Aura Advanced Headache. Postdrome Dull headache Fully reversible Nasal congestion Neurological changes: Visual Muscle pain somatosensory Mild Unilateral Throbbing Nausea Photophobia Phonophobia Osmophobia Moderate Headache Severe Fatigue Cognitive changes Muscle pain Post headache Time
In practice n Recurrent headache that bothers n Nausea with headache n Light or sound bothers n Invariably a family history
Migraine co-morbidities n Anxiety n Depression n IBS n Asthma n Epilepsy
Migraine Acute treatment n Paracetamol, Aspirin, Prokinetic (Domperidone/metochlorpropramide). n Triptan n Not opiates

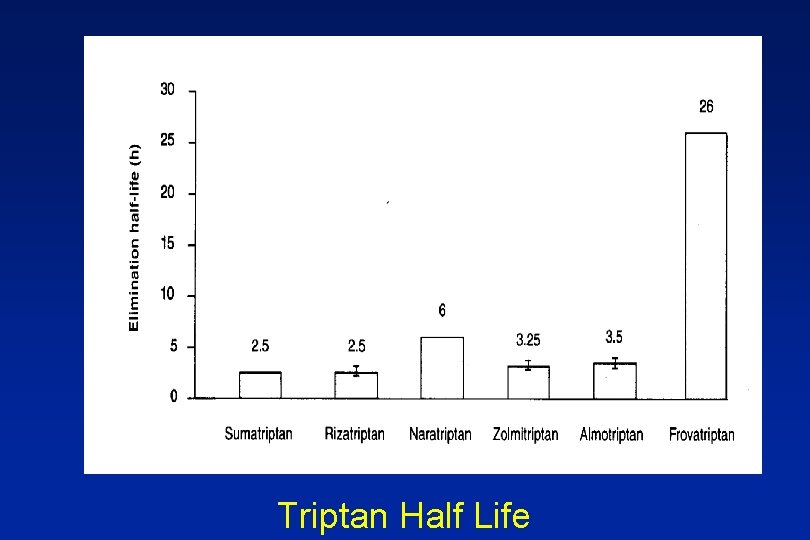
Triptans
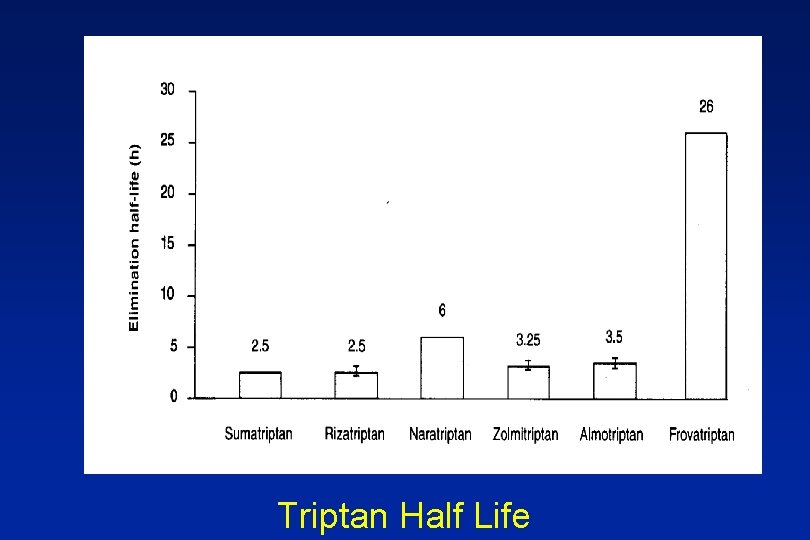
Triptan Half Life
n Severe nausea, often vomits n Sumatriptan 50 mg only partially effective

Options n Anti emetic n Take early n Change the dose n Change formulation (nasal, wafer, inj) n Change the Triptan (failure not a class effect)
Taking Sumatriptan 100 mg Which cause you concern? n On COC pill n Age 69 n Past history TIA n Started SSRI

Triptans – some practical points n Treat early n Formulation? n Failure not class effect n Not in CVD n SSRIs n Over 65 years
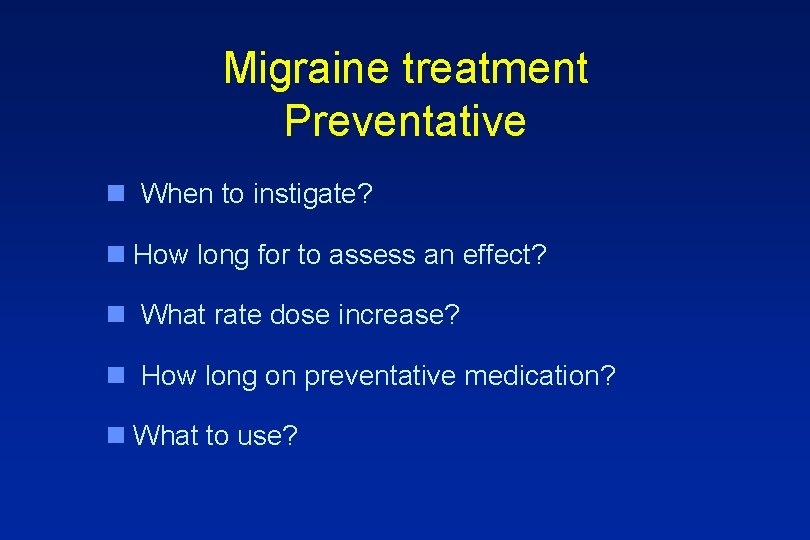
Migraine treatment Preventative n When to instigate? n How long for to assess an effect? n What rate dose increase? n How long on preventative medication? n What to use?
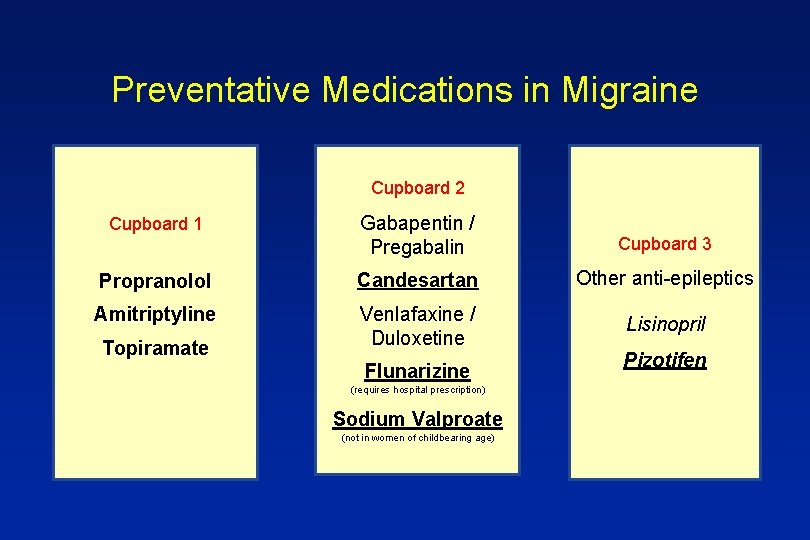
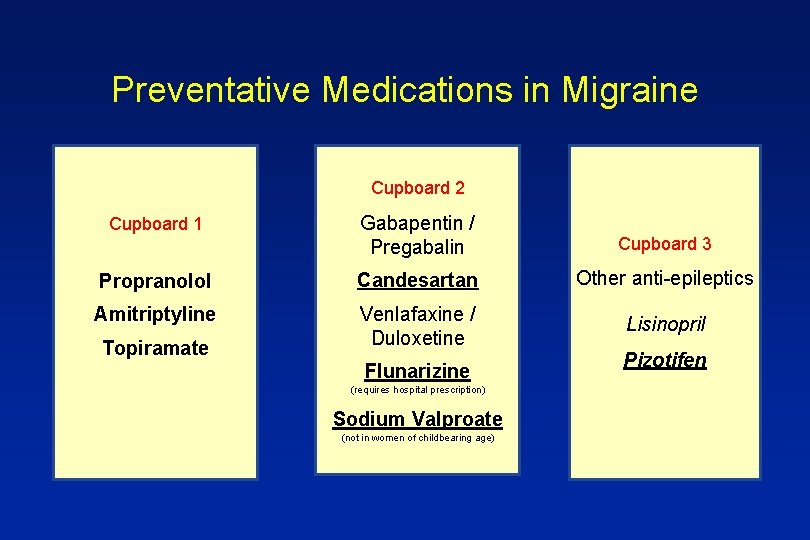
Preventative Medications in Migraine Cupboard 2 Cupboard 1 Gabapentin / Pregabalin Cupboard 3 Propranolol Candesartan Other anti-epileptics Amitriptyline Venlafaxine / Duloxetine Lisinopril Topiramate Flunarizine (requires hospital prescription) Sodium Valproate (not in women of childbearing age) Pizotifen
Migraineur on verapamil, domperidone, Triptan. Just started on Amitriptyline

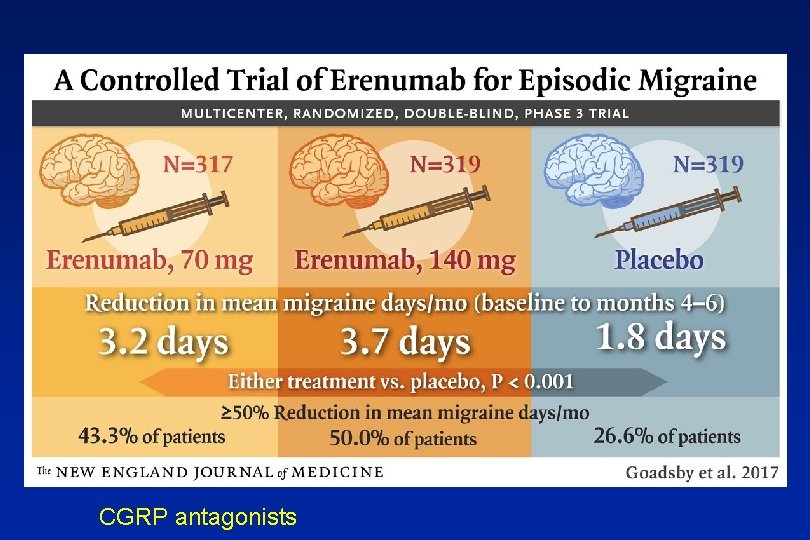
Patient read in Daily Mail about new “breakthrough” drug. How do you advise?
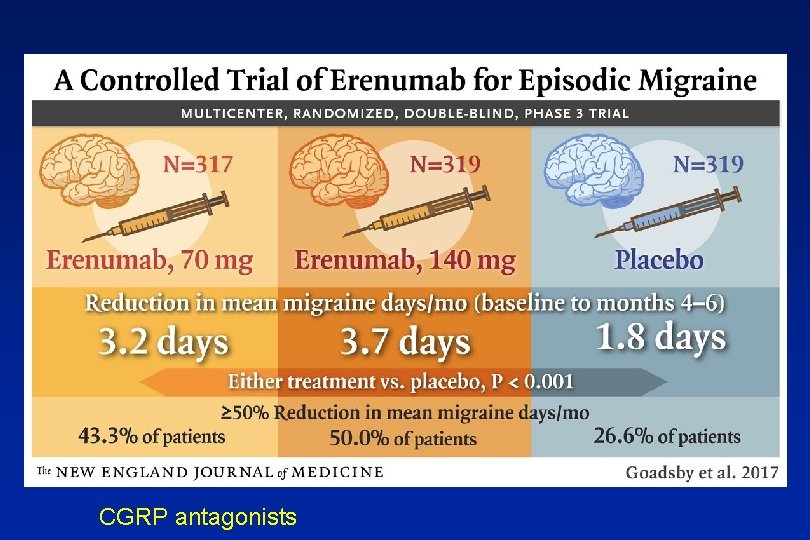
CGRP antagonists
Non – drug options

Triggers/lifestyle n Triggers – yes n Lifestyle - yes (including hormones) Keep constant n Food allergy - no
Naturally occurring drugs n Magnesium – ? yes n Co Q 10 – ? yes n Feverfew, butterbur, riboflavin – possibly
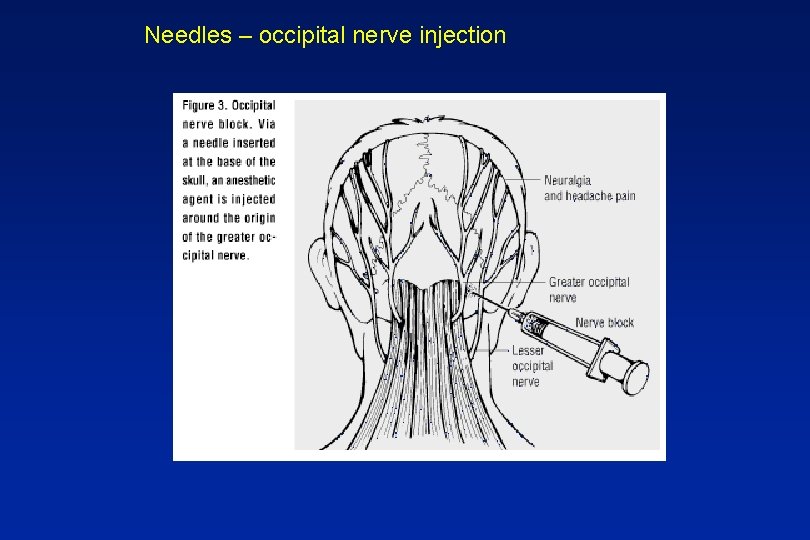
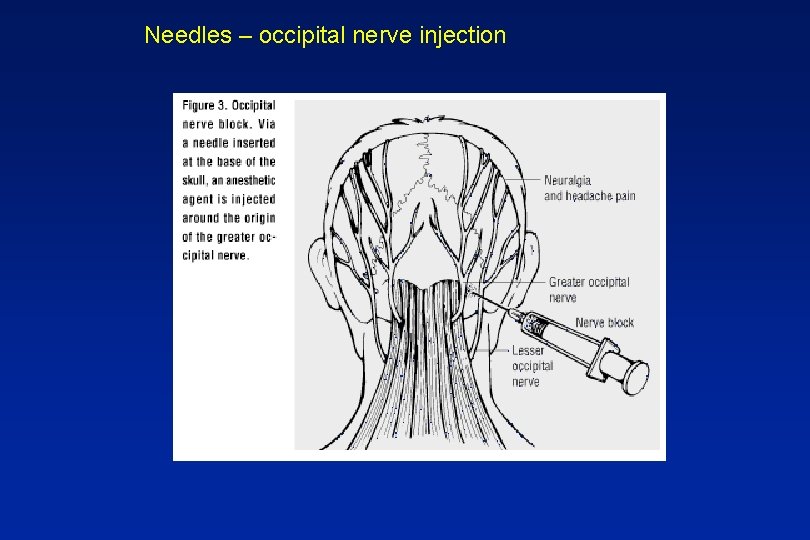
Needles – occipital nerve injection
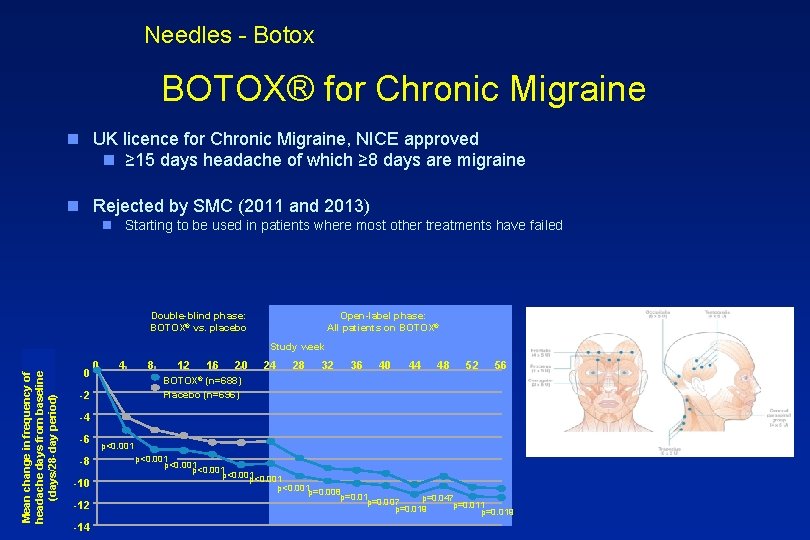
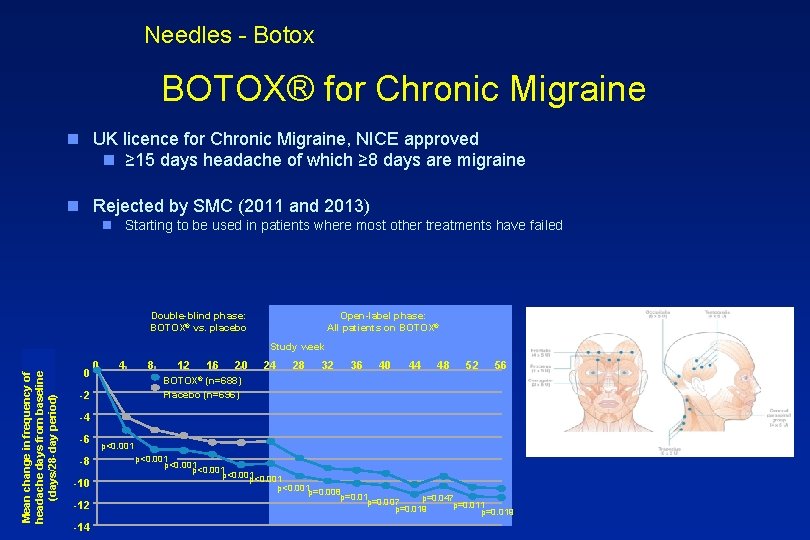
Needles - Botox BOTOX® for Chronic Migraine n UK licence for Chronic Migraine, NICE approved n ≥ 15 days headache of which ≥ 8 days are migraine n Rejected by SMC (2011 and 2013) n Starting to be used in patients where most other treatments have failed Double-blind phase: BOTOX® vs. placebo Open-label phase: All patients on BOTOX® Mean change in frequency of headache days from baseline (days/28 -day period) Study week 0 0 4 8 12 16 20 24 28 32 36 40 44 48 52 56 BOTOX® (n=688) Placebo (n=696) -2 -4 -6 -8 -10 -12 -14 p<0. 001 p<0. 001 p=0. 008 p=0. 01 p=0. 047 p=0. 007 p=0. 011 p=0. 019
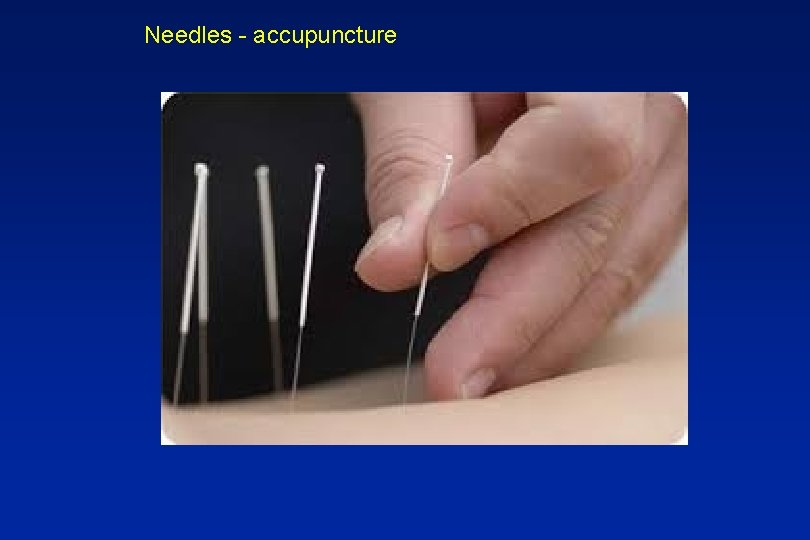
Needles - accupuncture

Psychological approaches n Cognitive therapy, mindfulness
Electrics

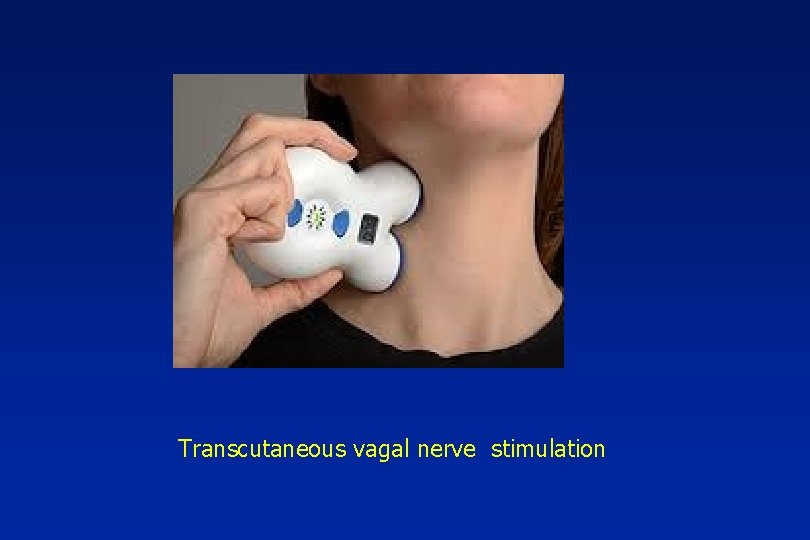
Transcutaneous vagal nerve stimulation
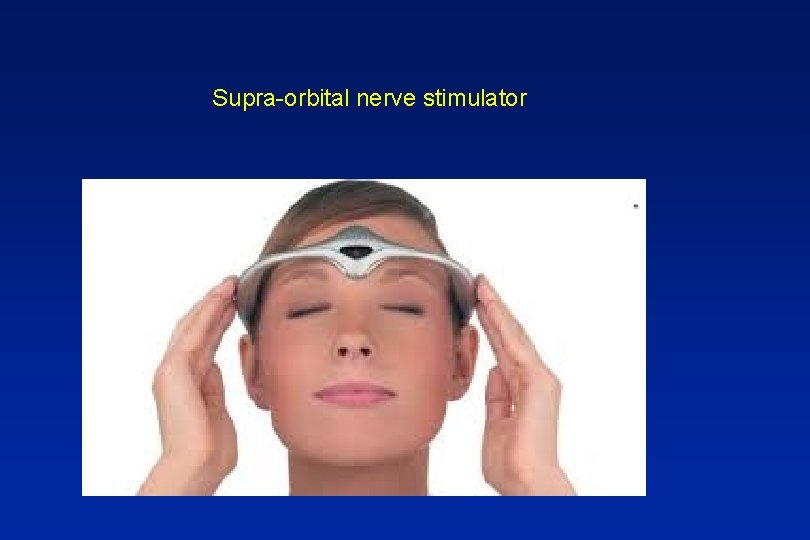
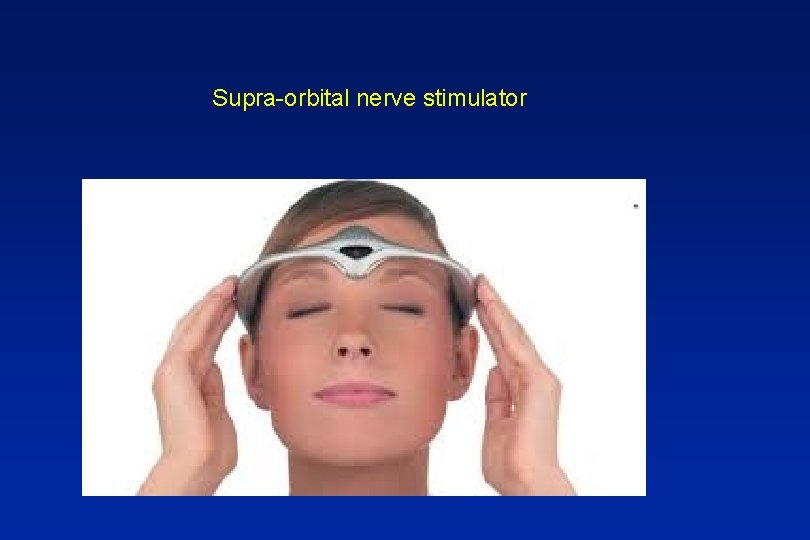
Supra-orbital nerve stimulator
In summary n Lot of it out there n Significant impact n Needs unmet

 Apsasia
Apsasia Headache chart
Headache chart Migraine avec aura définition
Migraine avec aura définition Ichd 3 vestibular migraine
Ichd 3 vestibular migraine Ocular migraine
Ocular migraine Migraine vs epilepsy
Migraine vs epilepsy Migraine triggers
Migraine triggers Symptoms of love analysis
Symptoms of love analysis Dr abdul
Dr abdul Trigeminal migraine
Trigeminal migraine Does emgality need to be refrigerated
Does emgality need to be refrigerated Migraine
Migraine Osteopern
Osteopern Postdrome
Postdrome Prodrome migraine
Prodrome migraine Pathophysiology of migraine
Pathophysiology of migraine Paroxysmal hemicrania
Paroxysmal hemicrania Vestibular migraine
Vestibular migraine Vertebrobasilaire tia
Vertebrobasilaire tia Esd flooring exeter
Esd flooring exeter Richard mansell exeter
Richard mansell exeter Math 3-4 exeter
Math 3-4 exeter Bart submissions exeter
Bart submissions exeter Truro to heathrow
Truro to heathrow Andrew connolly exeter
Andrew connolly exeter Exeter scholars year 12
Exeter scholars year 12 Todd kaplan exeter
Todd kaplan exeter Penryn info point
Penryn info point Feele exeter
Feele exeter Wendy robinson exeter
Wendy robinson exeter Exeter radar
Exeter radar Exeter circular economy
Exeter circular economy Types of repair
Types of repair Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders What is literary present
What is literary present Root of an equation
Root of an equation Sociology and social science
Sociology and social science Rule 4 respect other people's time and bandwidth example
Rule 4 respect other people's time and bandwidth example Goes back to vedic period times around 1000 bc
Goes back to vedic period times around 1000 bc Internet etiquette or netiquette
Internet etiquette or netiquette Symbiotic relationship between ostrich and gazelle
Symbiotic relationship between ostrich and gazelle Intertextuality
Intertextuality Explain how currents and magnets exert forces on each other
Explain how currents and magnets exert forces on each other A depressant drug drivers ed
A depressant drug drivers ed Plans used for work that has to do with construction
Plans used for work that has to do with construction Process of removing food
Process of removing food Net present value and other investment criteria
Net present value and other investment criteria Chapter 31 schizophrenia and other psychoses
Chapter 31 schizophrenia and other psychoses Licensing franchising and other contractual strategies
Licensing franchising and other contractual strategies Free enterprise and other economic systems
Free enterprise and other economic systems Water soluble vitamins characteristics
Water soluble vitamins characteristics Solipsism and the problem of other minds
Solipsism and the problem of other minds Solving square root and other radical equations
Solving square root and other radical equations Taste and other tales a swim summary
Taste and other tales a swim summary Relationship of social work with other social sciences
Relationship of social work with other social sciences Article xi code of ethics
Article xi code of ethics Advantages and disadvantages of payback method
Advantages and disadvantages of payback method Topic 6 quadrilaterals and other polygons answers
Topic 6 quadrilaterals and other polygons answers Snmp uses two other protocols
Snmp uses two other protocols Solving square root and other radical equations
Solving square root and other radical equations Lightly drawn lines to guide drawing other lines and shapes
Lightly drawn lines to guide drawing other lines and shapes Louie his cousin and his other cousin
Louie his cousin and his other cousin Kinds of intertextuality
Kinds of intertextuality My family and other animals characters
My family and other animals characters Bandwagon persuasive technique example
Bandwagon persuasive technique example Chapter 15 alcohol other drugs and driving
Chapter 15 alcohol other drugs and driving Technology and other operational risks
Technology and other operational risks Written and other recorded events of people
Written and other recorded events of people Options, futures, and other derivatives
Options, futures, and other derivatives Acts 11:19
Acts 11:19 Be form verbs
Be form verbs Names in romeo and juliet
Names in romeo and juliet Maps and plans
Maps and plans Mathematical literacy grade 11 maps and scales
Mathematical literacy grade 11 maps and scales Maps plans and other representations of the physical world
Maps plans and other representations of the physical world Respect other people's time and bandwidth
Respect other people's time and bandwidth Generates fresh produce and other farm products
Generates fresh produce and other farm products Generates fresh produce and other farm products
Generates fresh produce and other farm products Science class five
Science class five Respect other people's time and bandwidth
Respect other people's time and bandwidth Providing support services facilities and other amenities
Providing support services facilities and other amenities Advantage and disadvantage of npv
Advantage and disadvantage of npv Chapter 9 net present value and other investment criteria
Chapter 9 net present value and other investment criteria Chapter 24 milady review questions
Chapter 24 milady review questions Chapter 15 alcohol other drugs and driving
Chapter 15 alcohol other drugs and driving Generates fresh produce and other farm products
Generates fresh produce and other farm products Unit 24 cutting with oxyfuels and other gases
Unit 24 cutting with oxyfuels and other gases Sprint tokenizer
Sprint tokenizer Topic 6 quadrilaterals and other polygons answers
Topic 6 quadrilaterals and other polygons answers Air 78 nitrogen
Air 78 nitrogen Fungi prokaryote
Fungi prokaryote Strip map mathematical literacy
Strip map mathematical literacy Why do states cooperate with each other
Why do states cooperate with each other Is music speech and other sounds represented in binary
Is music speech and other sounds represented in binary Bandwagon and other persuasive techniques
Bandwagon and other persuasive techniques Burger king propaganda technique used
Burger king propaganda technique used Transcendental functions examples with solutions
Transcendental functions examples with solutions Existence of inverse function
Existence of inverse function Exponential integration
Exponential integration And other stories quality
And other stories quality Chapter 11 real estate and other investments
Chapter 11 real estate and other investments