S E H C A D A E





- Slides: 31
S E H C A D A E H T H O O T A K E C O N T R O L W Presented by Nancy Smith Beste, MPAS, PA-C Registered Psychotherapiist

S E D U L C IN INE IAL F N C E I O I D EN T E A M B T N SE LY E S A AL E B OT R P CE D. S N EC S I TH IDE AN ENT EV D TM AN EA TAR If you tried it…and it worked…. We want to hear about it !!!
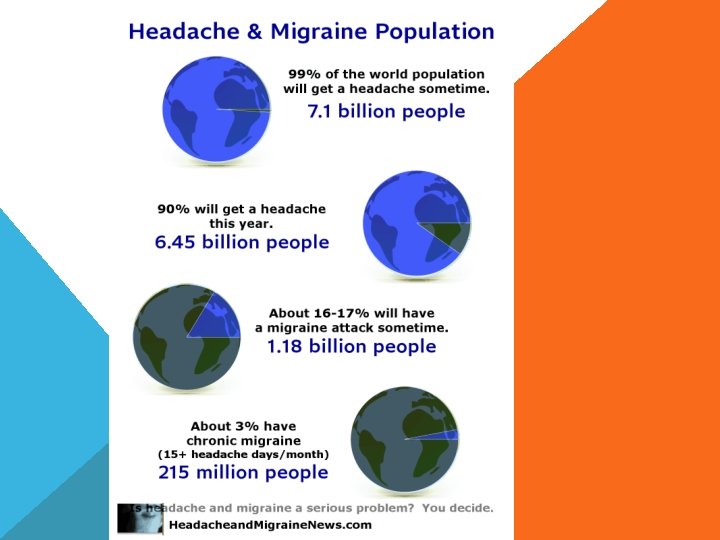
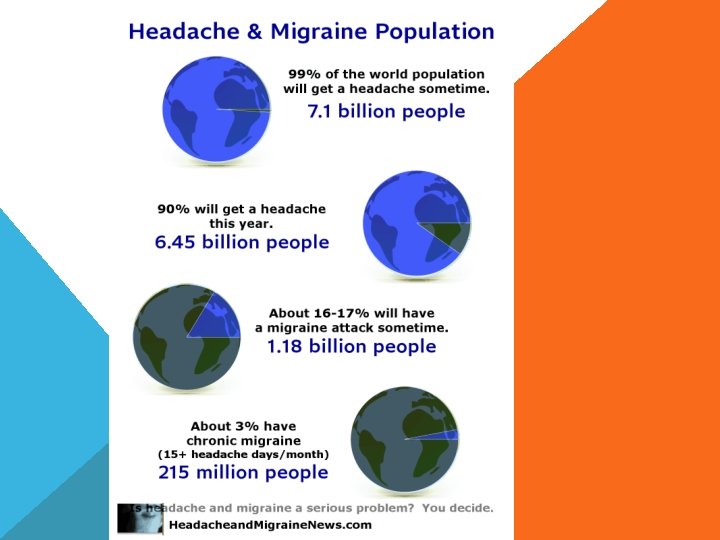
WHO SUFFERS HEADACHE? 1 IN 4 PEOPLE SUFFER HEADACHE. 3 X MORE WOMEN
HEADACHES ARE THE 7 TH MOST COMMON CAUSE OF DISABILITY IN THE U. S. EACH YEAR HEADACHE SUFFERS LOSE ABOUT 4. 2 DAYS OF WORK DUE TO HEADACHE SYMPTOMS SCHWARTZ BS, ET AL. J OCCUP ENVIRON MED. 1197
NOT TONIGHT DEAR… I HAVE A HEADACHE.
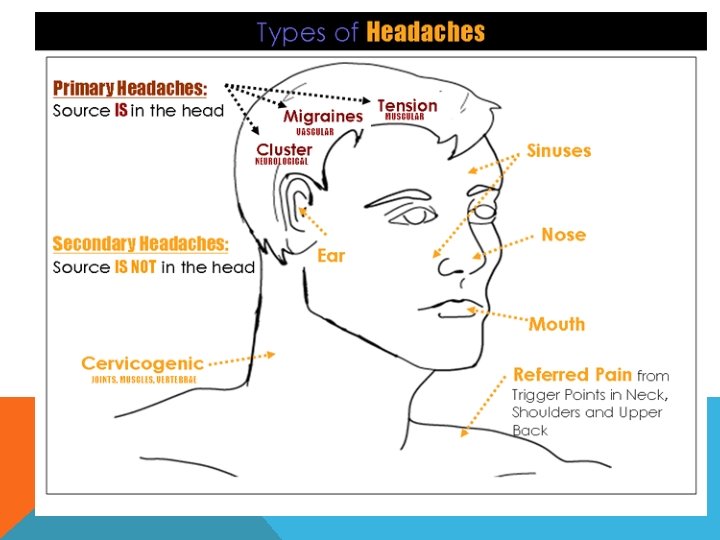
WHAT KIND OF A HEADACHE IS IT? E H T W O N O K T T E S P U Y M T IN WE ACHE A P E D H A T E H L O R ONT
G IN N I , : F G E PE IN , D Y S M I R T T O E , T G Y E T G I I S H R R E C E ND T V U A E , A NG L S D I , C Y A D TY VIT LU E I L E C TS H A G IN N U N I Q O A S N, , L TIE PL Y LI M O I C T N A CO A E U C U Q ED O Q L E UE T FR IQ CIA UN SO AS
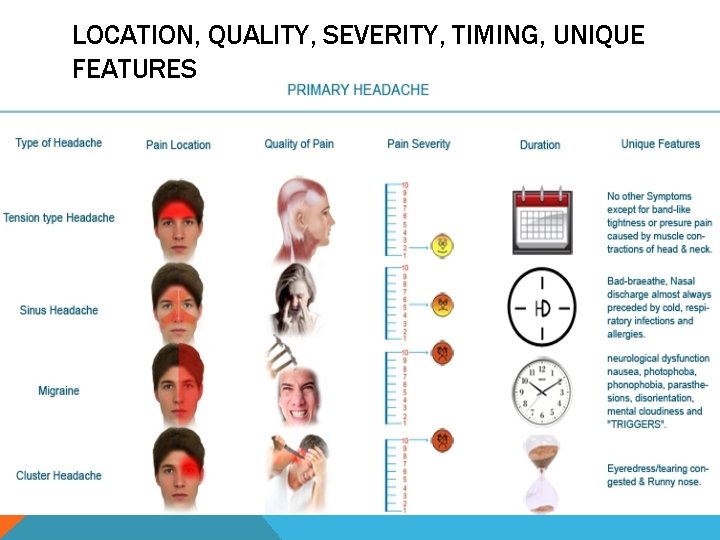
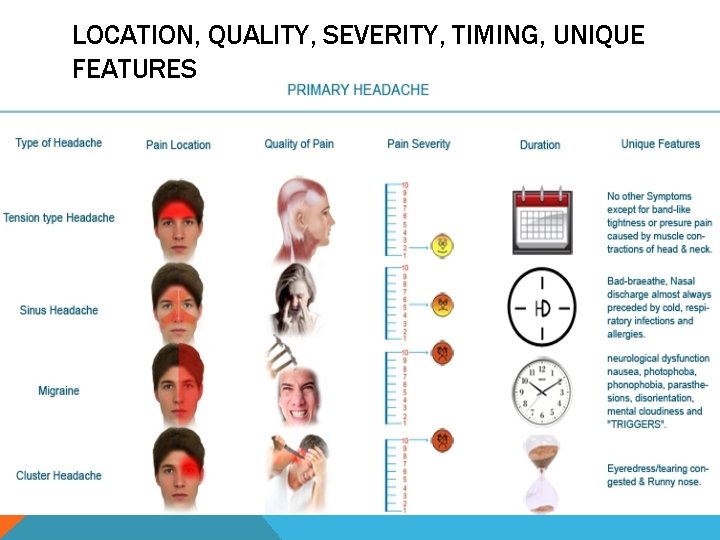
LOCATION, QUALITY, SEVERITY, TIMING, UNIQUE FEATURES
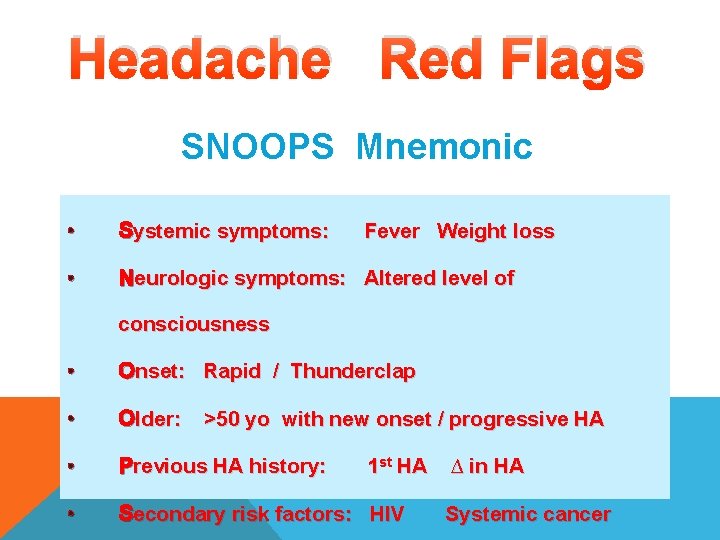
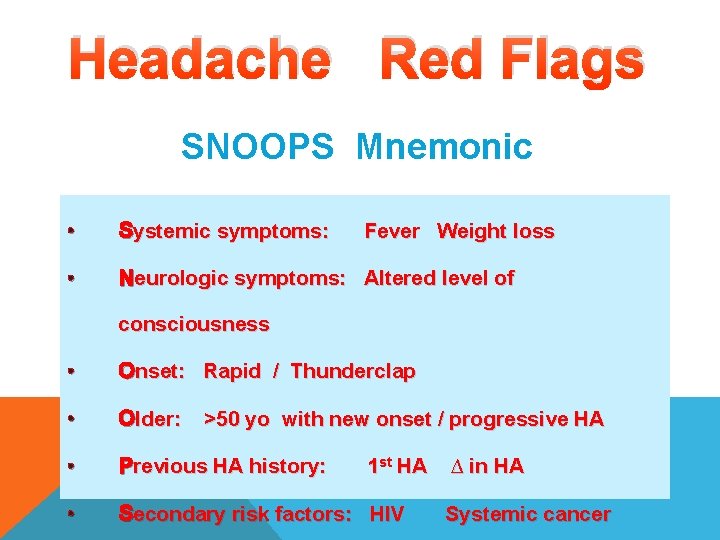
Headache Red Flags SNOOPS Mnemonic • Systemic symptoms: • Neurologic symptoms: Altered level of Fever Weight loss consciousness • Onset: Rapid / Thunderclap • Older: • Previous HA history: • Secondary risk factors: HIV >50 yo with new onset / progressive HA 1 st HA ∆ in HA Systemic cancer
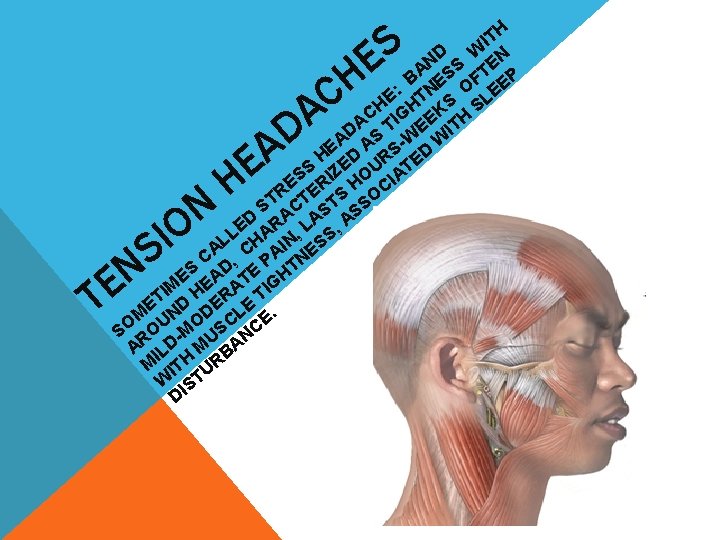
S E H IT D W N N S TE A S F EP B E O : TN E E L S H H K S C G H I E A T E IT D A AS -W W E H ED RS ED S IZ OU AT S E ER H CI R S O ST CT ST SS D RA LA , A E L HA N, S L I ES A C , P TN D S E E EA T GH M I H RA TI T E D E E M UN OD CL E. SO RO -M US NC A ILD M BA M ITH UR W IST D H C N TE I S N O H A E A D
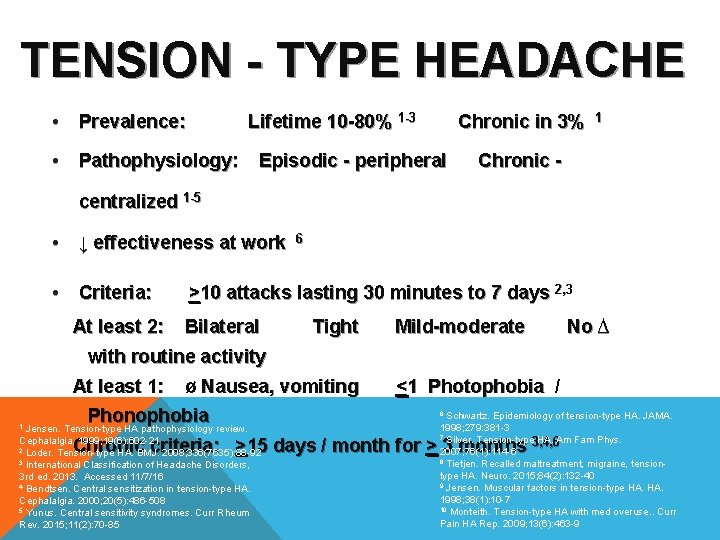
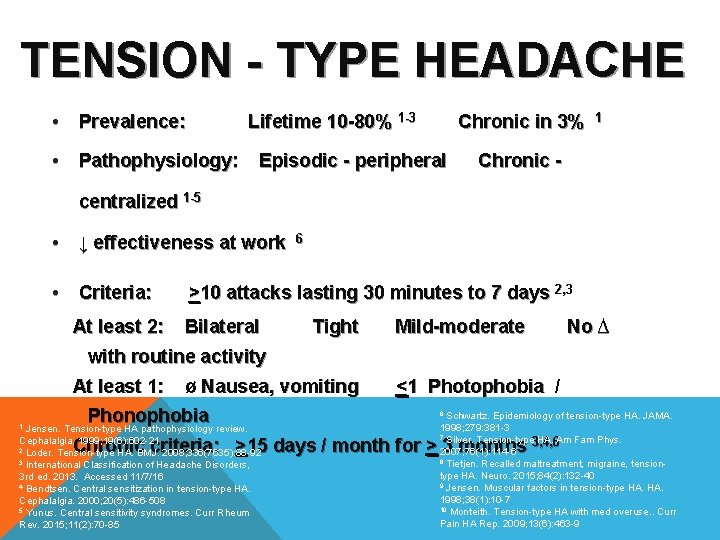
TENSION - TYPE HEADACHE • Prevalence: Lifetime 10 -80% 1 -3 • Pathophysiology: Chronic in 3% Episodic - peripheral 1 Chronic - centralized 1 -5 • ↓ effectiveness at work • Criteria: At least 2: 6 >10 attacks lasting 30 minutes to 7 days 2, 3 Bilateral Tight Mild-moderate No ∆ with routine activity At least 1: ø Nausea, vomiting Phonophobia Jensen. Tension-type HA pathophysiology review. Cephalalgia. 1999; 19(6): 602 -21 2 Loder. Tension-type HA. BMJ. 2008; 336(7635): 88 -92 3 International Classification of Headache Disorders, 3 rd ed. 2013. Accessed 11/7/16 4 Bendtsen. Central sensitization in tension-type HA. Cephalalgia. 2000; 20(5): 486 -508 5 Yunus. Central sensitivity syndromes. Curr Rheum Rev. 2015; 11(2): 70 -85 1 <1 Photophobia / Schwartz. Epidemiology of tension-type HA. JAMA. 1998; 279: 381 -3 7 Silver. Tension-type HA. Am Fam Phys. 3, 4, 6 2007; 76(1): 114 -6 8 Tietjen. Recalled maltreatment, migraine, tensiontype HA. Neuro. 2015; 84(2): 132 -40 9 Jensen. Muscular factors in tension-type HA. 1998; 38(1): 10 -7 10 Monteith. Tension-type HA with med overuse. . Curr Pain HA Rep. 2009; 13(6): 463 -9 6 Chronic criteria: >15 days / month for > 3 months
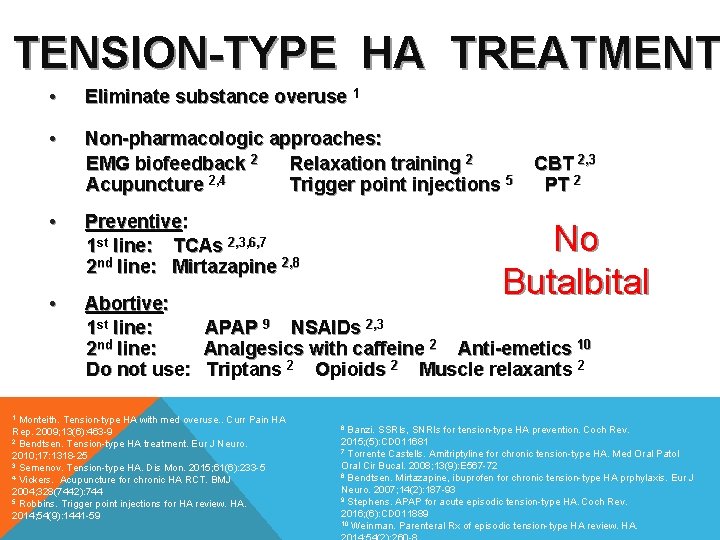
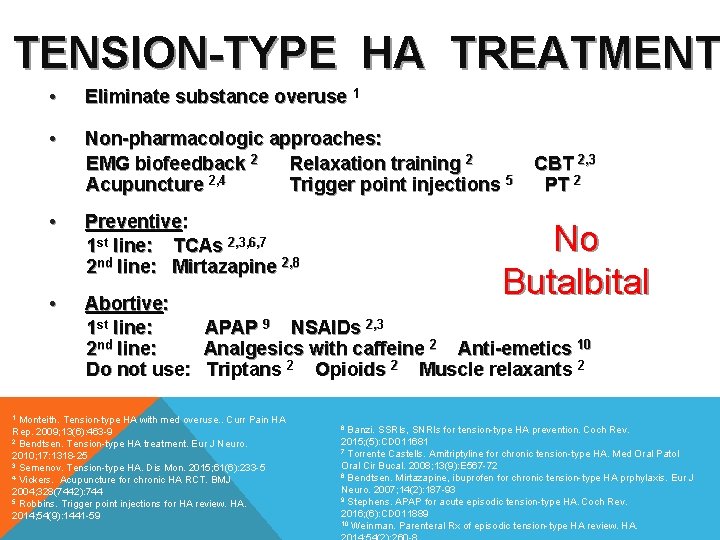
TENSION-TYPE HA TREATMENT • Eliminate substance overuse 1 • Non-pharmacologic approaches: EMG biofeedback 2 Relaxation training 2 Acupuncture 2, 4 Trigger point injections 5 • Preventive: 1 st line: TCAs 2, 3, 6, 7 2 nd line: Mirtazapine 2, 8 • Abortive: 1 st line: 2 nd line: Do not use: CBT 2, 3 PT 2 No Butalbital APAP 9 NSAIDs 2, 3 Analgesics with caffeine 2 Anti-emetics 10 Triptans 2 Opioids 2 Muscle relaxants 2 Monteith. Tension-type HA with med overuse. . Curr Pain HA Rep. 2009; 13(6): 463 -9 2 Bendtsen. Tension-type HA treatment. Eur J Neuro. 2010; 17: 1318 -25 3 Semenov. Tension-type HA. Dis Mon. 2015; 61(6): 233 -5 4 Vickers. Acupuncture for chronic HA RCT. BMJ 2004; 328(7442): 744 5 Robbins. Trigger point injections for HA review. HA. 2014; 54(9): 1441 -59 1 Banzi. SSRIs, SNRIs for tension-type HA prevention. Coch Rev. 2015; (5): CD 011681 7 Torrente Castells. Amitriptyline for chronic tension-type HA. Med Oral Patol Oral Cir Bucal. 2008; 13(9): E 567 -72 8 Bendtsen. Mirtazapine, ibuprofen for chronic tension-type HA prphylaxis. Eur J Neuro. 2007; 14(2): 187 -93 9 Stephens. APAP for acute episodic tension-type HA. Coch Rev. 2016; (6): CD 011889 10 Weinman. Parenteral Rx of episodic tension-type HA review. HA. 6
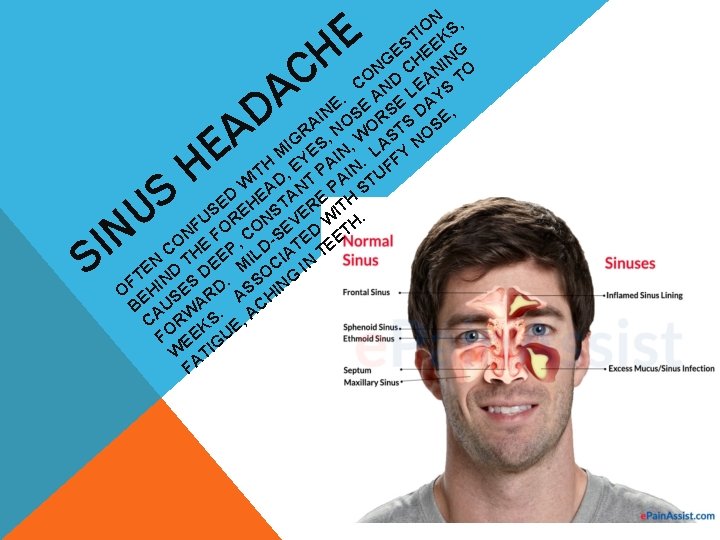
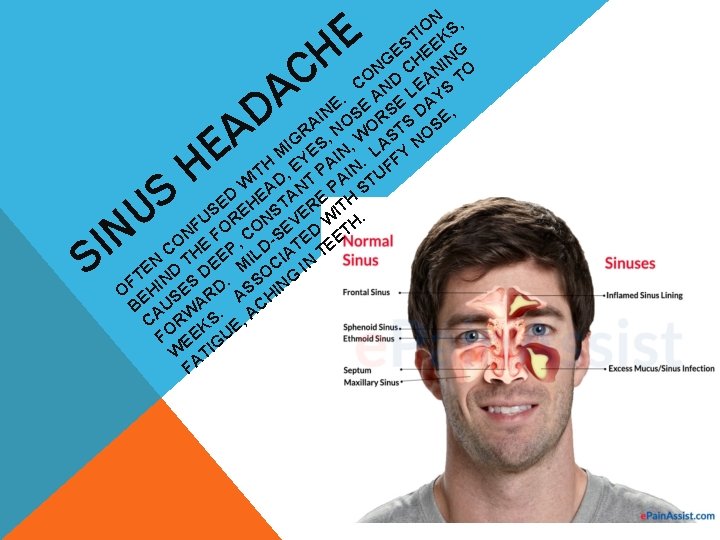
E H N O S, I T K S E EE NG NG CH NI O CO ND LEA S T A E AY. E E IN OS RS S D E, A R , N WO ST OS N IG S , M YE IN. LA FY A H IT D, E T P AIN TUF W A N P S D E TA E H S E NS ER IT. U R O EV W H F O N F , C -S ED ET O C HE EP ILD IAT TE N T E M C IN E D D O FT IN ES D. SS ING O EH S R A H C B AU WA. A C R KS E, FO EE GU W TI FA C A I S S U N E H D A
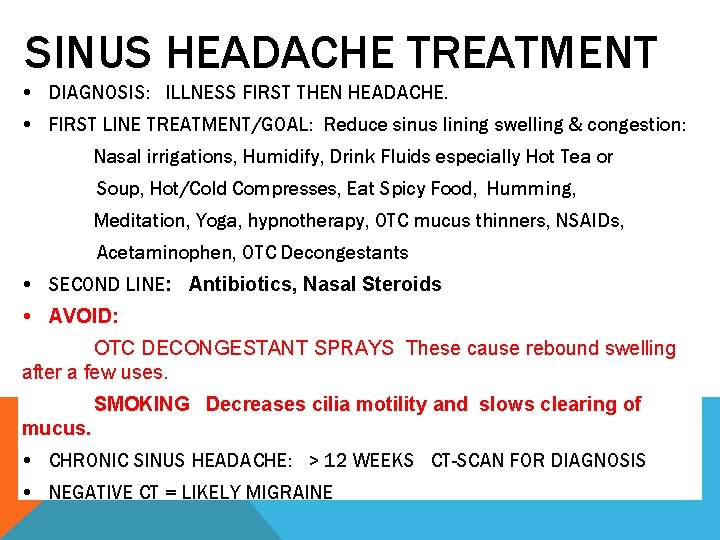
SINUS HEADACHE TREATMENT DIAGNOSIS: ILLNESS FIRST THEN HEADACHE. FIRST LINE TREATMENT/GOAL: Reduce sinus lining swelling & congestion: Nasal irrigations, Humidify, Drink Fluids especially Hot Tea or Soup, Hot/Cold Compresses, Eat Spicy Food, Humming, Meditation, Yoga, hypnotherapy, OTC mucus thinners, NSAIDs, Acetaminophen, OTC Decongestants SECOND LINE: Antibiotics, Nasal Steroids AVOID: OTC DECONGESTANT SPRAYS These cause rebound swelling after a few uses. SMOKING Decreases cilia motility and slows clearing of mucus. CHRONIC SINUS HEADACHE: > 12 WEEKS CT-SCAN FOR DIAGNOSIS NEGATIVE CT = LIKELY MIGRAINE
S E V O M , S D AN IN. D SIA D PA TE HE A A T L HE NT CI AS UA E TA SO R IS H T S S A V F ON. A A, P S, O C S I S E E D NG AY OB IN ERS I S TI D PH UD G E N A O O O IG O TR S T ON CL TR N E R O EN OU PHTAL LE LY. P H NDEN AB L E TS O A , M CK A D U I S T A USO S LA HO ION TR IN T E. , P AT ND A P IDE ER EA NT , A S EV S IE ES S AU OR G N IS N D HA C E N I A M R IG
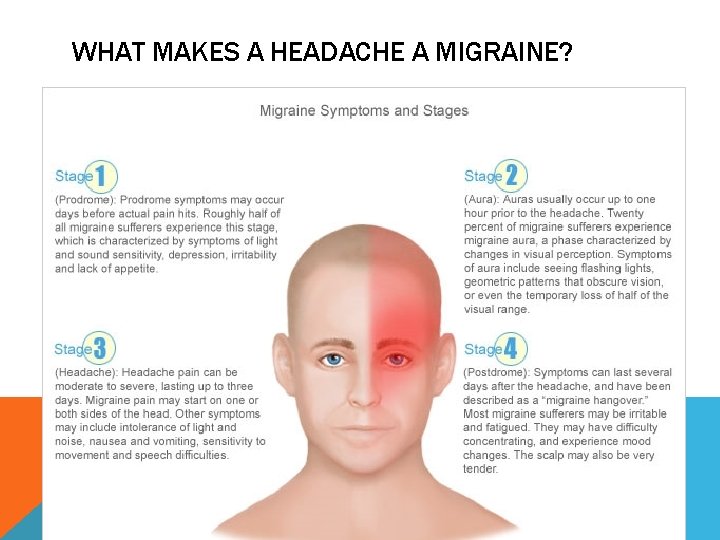
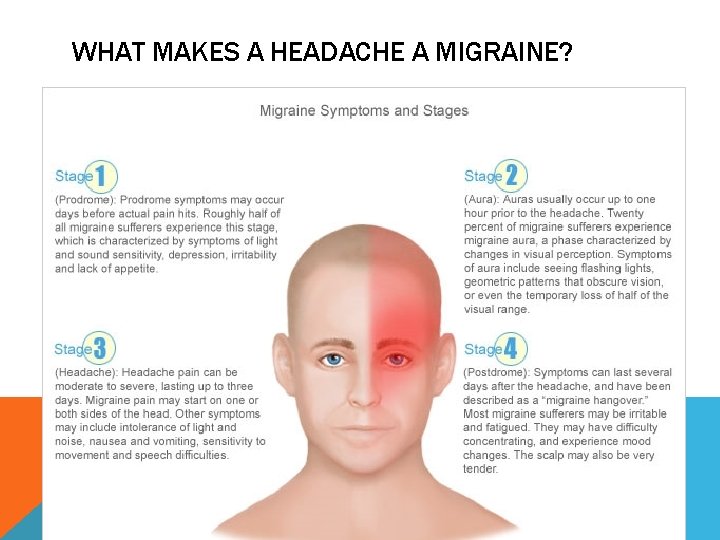
WHAT MAKES A HEADACHE A MIGRAINE?
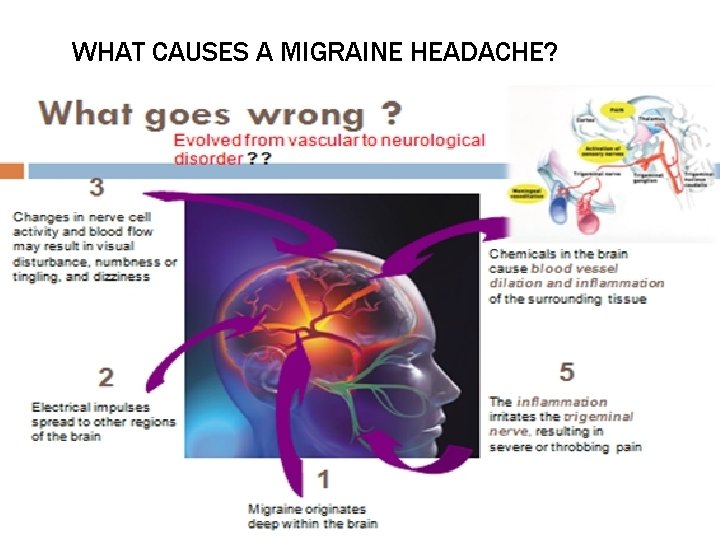
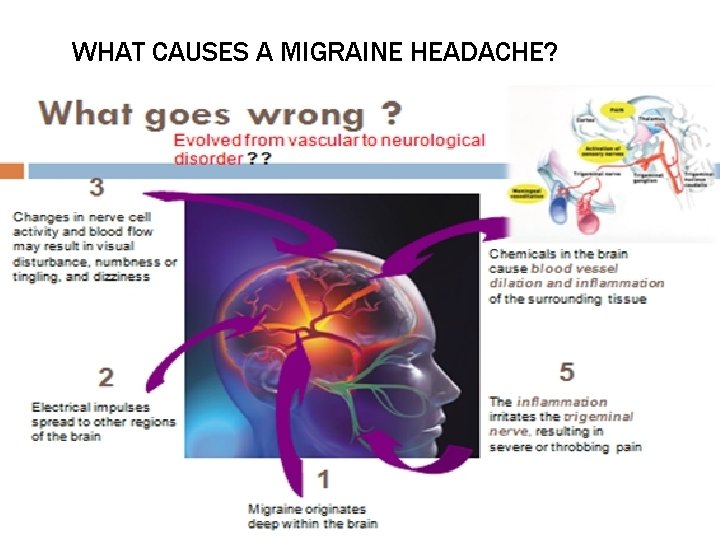
WHAT CAUSES A MIGRAINE HEADACHE?
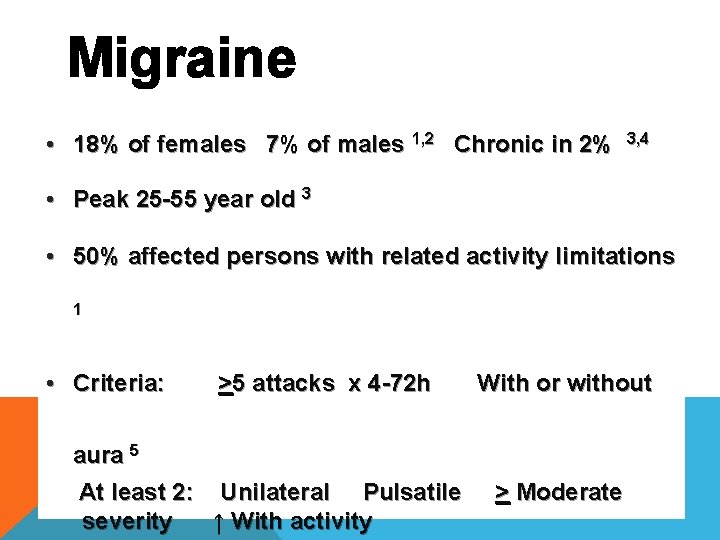
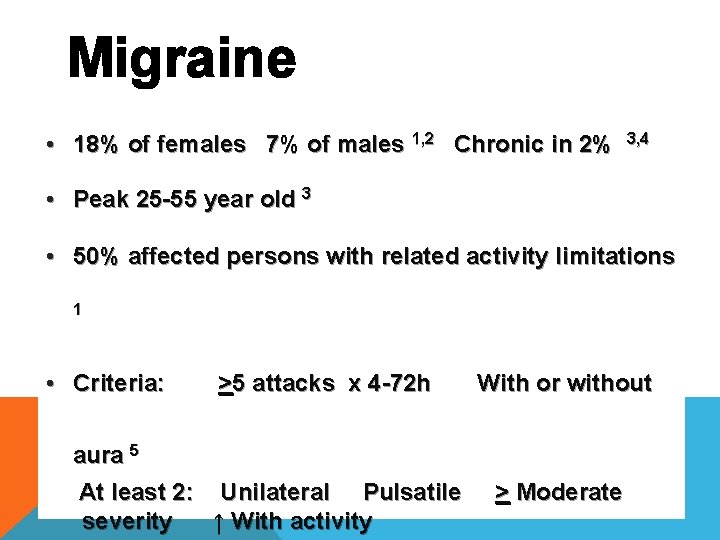
Migraine • 18% of females 7% of males 1, 2 Chronic in 2% 3, 4 • Peak 25 -55 year old 3 • 50% affected persons with related activity limitations 1 • Criteria: >5 attacks x 4 -72 h With or without aura 5 At least 2: Unilateral Pulsatile severity ↑ With activity > Moderate
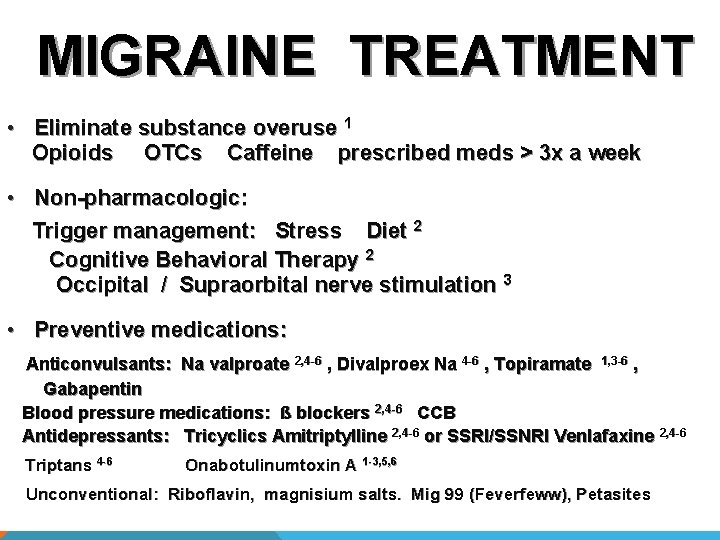
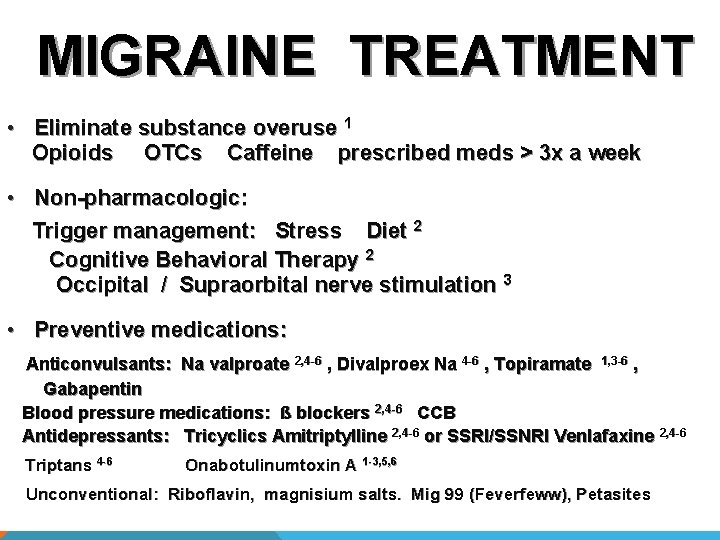
MIGRAINE TREATMENT • Eliminate substance overuse 1 Opioids OTCs Caffeine prescribed meds > 3 x a week • Non-pharmacologic: Trigger management: Stress Diet 2 Cognitive Behavioral Therapy 2 Occipital / Supraorbital nerve stimulation 3 • Preventive medications: Anticonvulsants: Na valproate 2, 4 -6 , Divalproex Na 4 -6 , Topiramate 1, 3 -6 , Gabapentin Blood pressure medications: ß blockers 2, 4 -6 CCB 2, 4 -6 Antidepressants: Tricyclics Amitriptylline 2, 4 -6 or SSRI/SSNRI Venlafaxine 2, 4 -6 Triptans 4 -6 Onabotulinumtoxin A 1 -3, 5, 6 Unconventional: Riboflavin, magnisium salts. Mig 99 (Feverfeww), Petasites
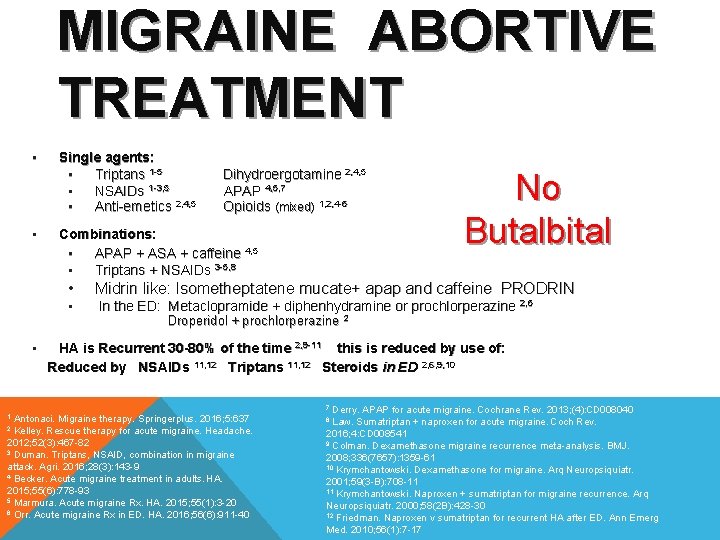
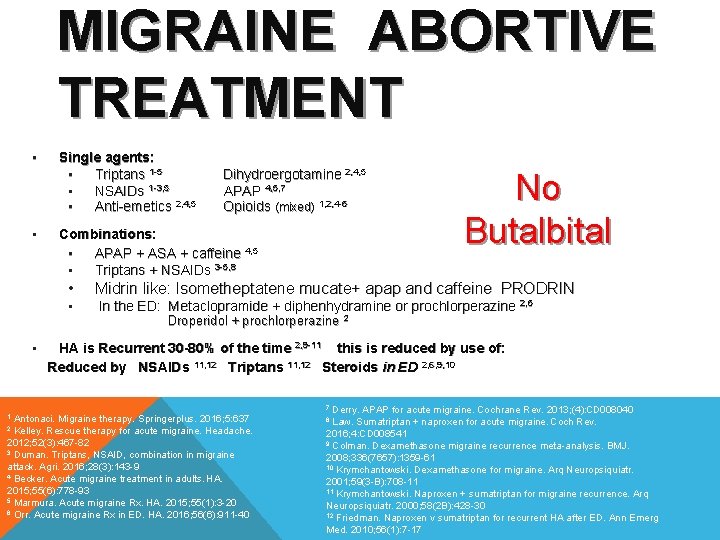
MIGRAINE ABORTIVE TREATMENT • • Single agents: • Triptans 1 -5 • NSAIDs 1 -3, 5 • Anti-emetics 2, 4, 5 Combinations: • APAP + ASA + caffeine 4, 5 • Triptans + NSAIDs 3 -5, 8 • • • Dihydroergotamine 2, 4, 5 APAP 4, 5, 7 Opioids (mixed) 1, 2, 4 -6 Midrin like: Isometheptatene mucate+ apap and caffeine PRODRIN In the ED: Metaclopramide + diphenhydramine or prochlorperazine 2, 6 Droperidol + prochlorperazine 2 HA is Recurrent 30 -80% of the time 2, 9 -11 this is reduced by use of: Reduced by NSAIDs 11, 12 Triptans 11, 12 Steroids in ED 2, 6, 9, 10 Derry. APAP for acute migraine. Cochrane Rev. 2013; (4): CD 008040 Law. Sumatriptan + naproxen for acute migraine. Coch Rev. 2016; 4: CD 008541 9 Colman. Dexamethasone migraine recurrence meta-analysis. BMJ. 2008; 336(7657): 1359 -61 10 Krymchantowski. Dexamethasone for migraine. Arq Neuropsiquiatr. 2001; 59(3 -B): 708 -11 11 Krymchantowski. Naproxen + sumatriptan for migraine recurrence. Arq Neuropsiquiatr. 2000; 58(2 B): 428 -30 12 Friedman. Naproxen v sumatriptan for recurrent HA after ED. Ann Emerg Med. 2010; 56(1): 7 -17 7 Antonaci. Migraine therapy. Springerplus. 2016; 5: 637 2 Kelley. Rescue therapy for acute migraine. Headache. 2012; 52(3): 467 -82 3 Duman. Triptans, NSAID, combination in migraine attack. Agri. 2016; 28(3): 143 -9 4 Becker. Acute migraine treatment in adults. HA. 2015; 55(6): 778 -93 5 Marmura. Acute migraine Rx. HA. 2015; 55(1): 3 -20 6 Orr. Acute migraine Rx in ED. HA. 2016; 56(6): 911 -40 1 No Butalbital 8


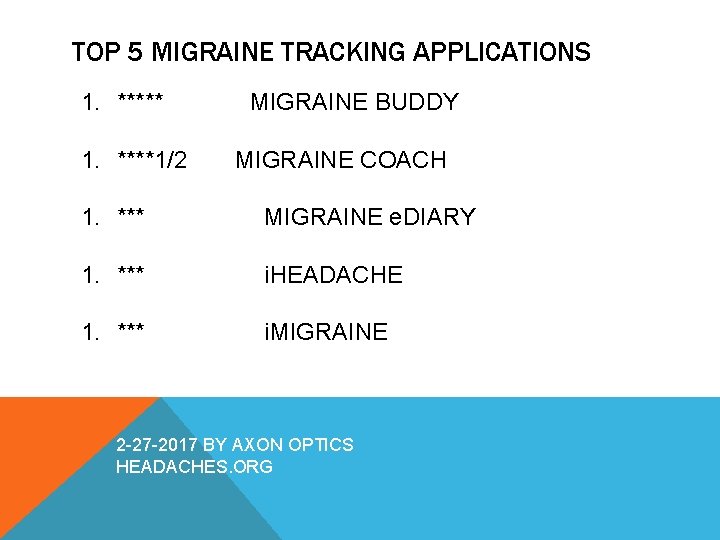
TOP 5 MIGRAINE TRACKING APPLICATIONS 1. ***** 1. ****1/2 MIGRAINE BUDDY MIGRAINE COACH 1. *** MIGRAINE e. DIARY 1. *** i. HEADACHE 1. *** i. MIGRAINE 2 -27 -2017 BY AXON OPTICS HEADACHES. ORG

MIGRAINE TRIGGERS Changes in Routine Too Much or Too Little Sleep Stress Changes in Caffeine Environmental Factors Computer Drinks Food and Food Additives Missing Meals Aged Cheese, Salty Food, Processed Food Dehydration Hormonal Changes. ESTROGEN Teeth Grinding CANNIBAS MAKES IT DIFFICULT TO TREAT MIGRAINE Migrainetrust. org

E G G I R T A E T VE A L O O C O HO CH SE W W IS O NO TH K TO R? E T LA W T N A CO O H C L Lippi G et al. Chocolate and migraine: the hisory of an ambiguous asociation. Acta Biomed. 201 Dec 17; 85(3): 216 -21
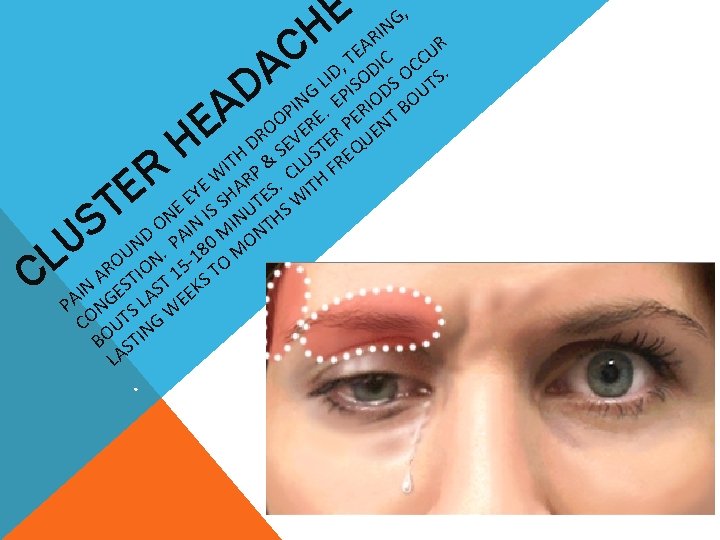
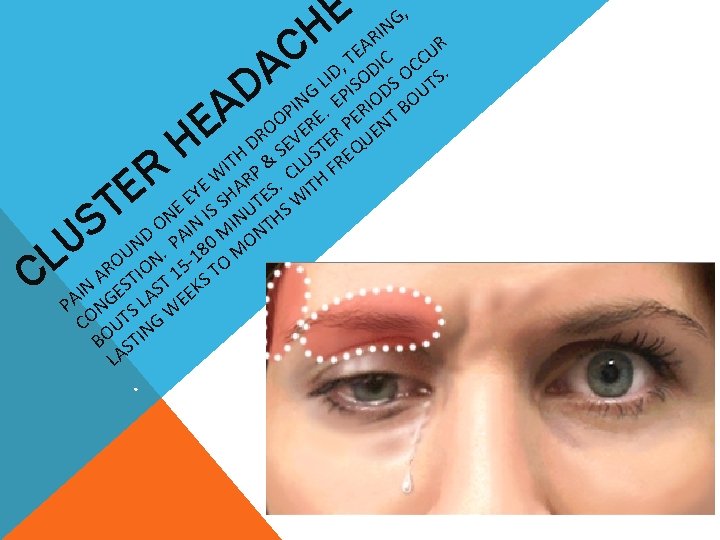
D A IS DS UT G P IN. E RIO BO P O RE PE NT O E E DR SEV STER QU ITH P & CLU FRE W R. TH E Y SHA TES WI E E IS U S N O IN MIN NTH D PA 0 N 8 MO. U 1 O ON 5 - TO R A STI T 1 S IN GE AS EEK A P N SL W CO UT NG BO STI LA. R E T S U L C , G E IN R H R A E U C T IC CC , A LID OD O S. E H
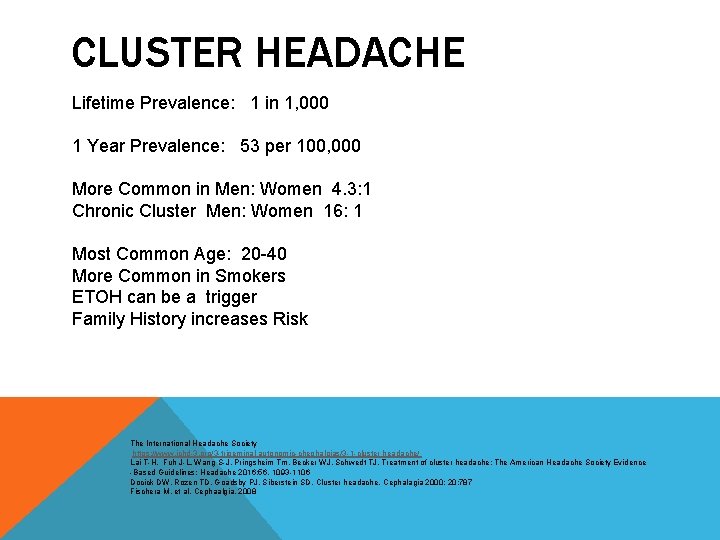
CLUSTER HEADACHE Lifetime Prevalence: 1 in 1, 000 1 Year Prevalence: 53 per 100, 000 More Common in Men: Women 4. 3: 1 Chronic Cluster Men: Women 16: 1 Most Common Age: 20 -40 More Common in Smokers ETOH can be a trigger Family History increases Risk The International Headache Society https: //www. ichd-3. org/3 -trigeminal-autonomic-chephalgias/3 -1 -cluster headache/ Lai T-H, Fuh J-L, Wang S-J, Pringsheim Tm, Becker WJ, Schwedt TJ. Treatment of cluster headache: The American Headache Society Evidence -Based Guidelines: Headache 2016; 56. 1093 -1106 Docick DW, Rozen TD, Goadsby PJ, Siberstein SD, Cluster headache. Cephalagia 2000; 20: 787 Fischera M, et al. Cephaalgia. 2008
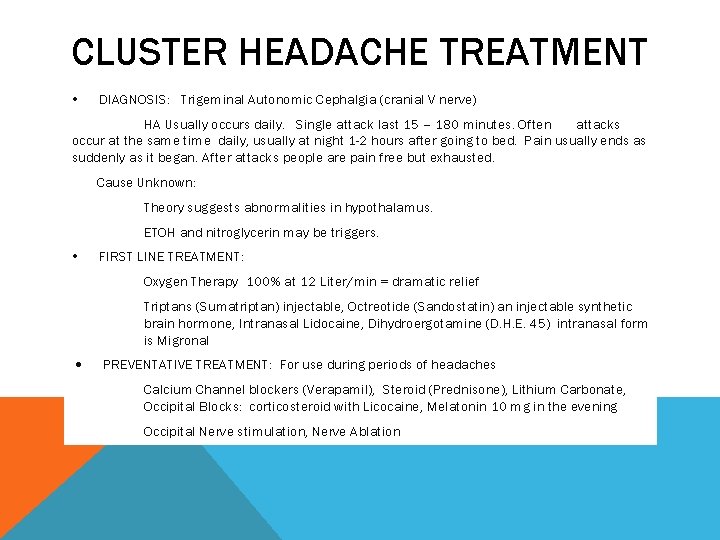
CLUSTER HEADACHE TREATMENT DIAGNOSIS: Trigeminal Autonomic Cephalgia (cranial V nerve) HA Usually occurs daily. Single attack last 15 – 180 minutes. Often attacks occur at the same time daily, usually at night 1 -2 hours after going to bed. Pain usually ends as suddenly as it began. After attacks people are pain free but exhausted. Cause Unknown: Theory suggests abnormalities in hypothalamus. ETOH and nitroglycerin may be triggers. FIRST LINE TREATMENT: Oxygen Therapy 100% at 12 Liter/min = dramatic relief Triptans (Sumatriptan) injectable, Octreotide (Sandostatin) an injectable synthetic brain hormone, Intranasal Lidocaine, Dihydroergotamine (D. H. E. 45) intranasal form is Migronal PREVENTATIVE TREATMENT: For use during periods of headaches Calcium Channel blockers (Verapamil), Steroid (Prednisone), Lithium Carbonate, Occipital Blocks: corticosteroid with Licocaine, Melatonin 10 mg in the evening Occipital Nerve stimulation, Nerve Ablation