MI with Nondiagnostic first ECG Dr Vinod Sharma
![The use of sensitive or high-sensitivity cardiac troponin [(h)s-c. Tn] allows more rapid rule-out The use of sensitive or high-sensitivity cardiac troponin [(h)s-c. Tn] allows more rapid rule-out](https://slidetodoc.com/presentation_image_h/23281574161caaa98a51646b5558302e/image-28.jpg)
- Slides: 49
MI with Non-diagnostic first ECG Dr. Vinod Sharma National Heart Institute New Delhi 1
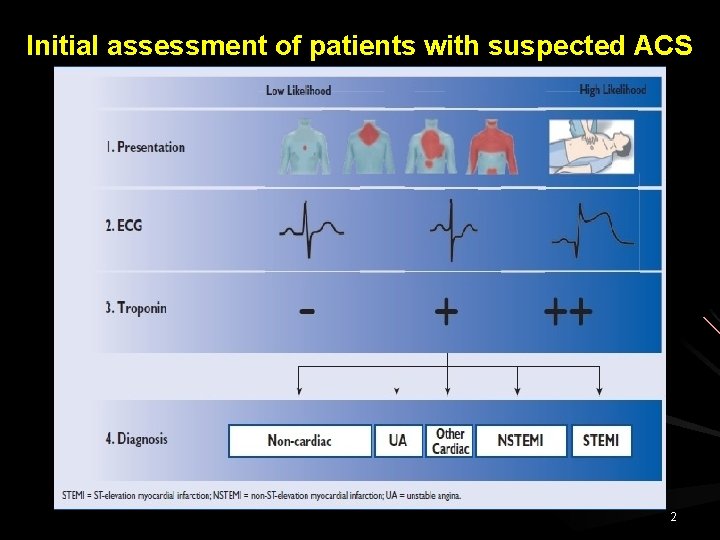
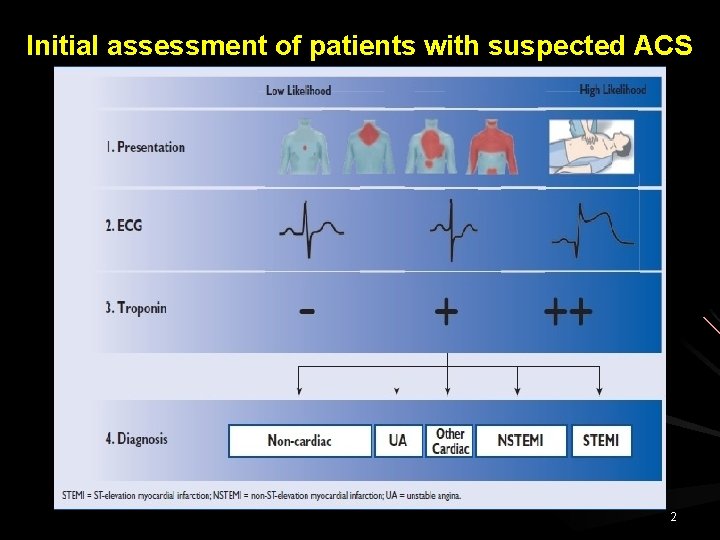
Initial assessment of patients with suspected ACS 2
MI with Non-diagnostic EKG 20% of AMI & 40% of UA have normal EKG in emergency room. Only about one in four of those with significant ST depression prove to have ACS. Only 5% with T wave changes meeting ACS criteria have AMI. 3
MI with Non-diagnostic EKG Small MI At least 3% of LV must be involved for EKG changes to develop. A normal EKG in face of AMI may relate to its location. - Infarct in lateral & post segment of LV are not directly interrogated by EKG. - 50% of infarct in LCx territory may be electrocardiography silent. Patient presenting with ischemic chest pain & normal EKG are actually pre-infarctional at that instant. 4
MI with Non-diagnostic EKG often does not detect: Transient myocardial ischemia. Ischemia in patients with prior MI. Vein graft occlusion. 5
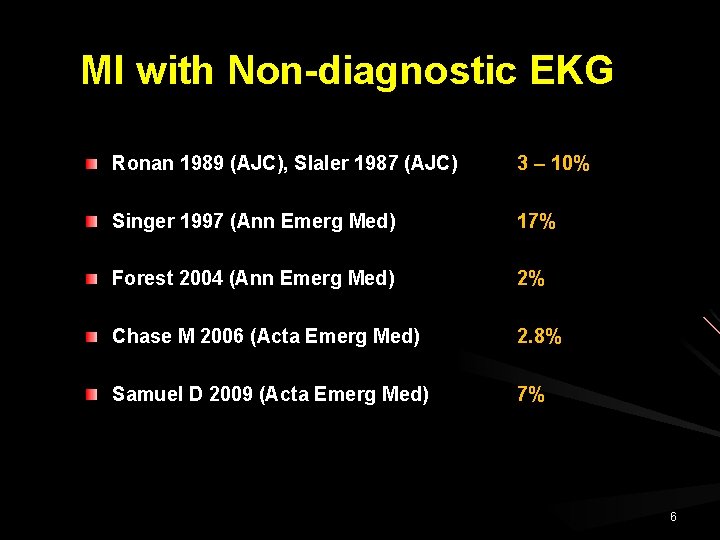
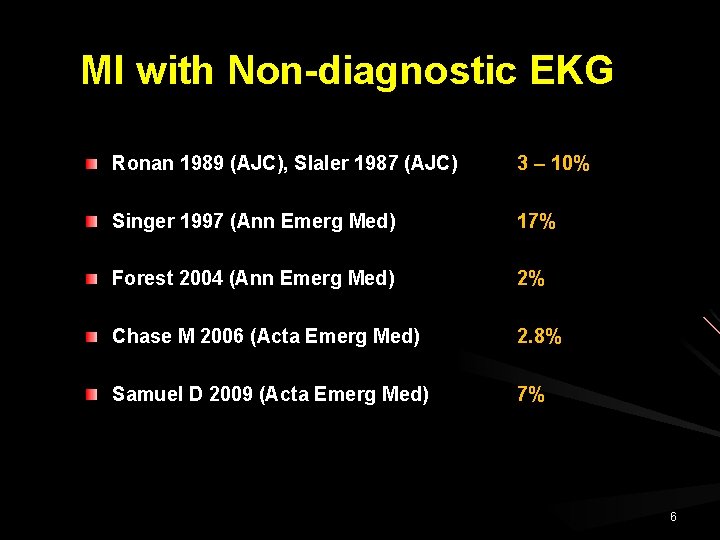
MI with Non-diagnostic EKG Ronan 1989 (AJC), Slaler 1987 (AJC) 3 – 10% Singer 1997 (Ann Emerg Med) 17% Forest 2004 (Ann Emerg Med) 2% Chase M 2006 (Acta Emerg Med) 2. 8% Samuel D 2009 (Acta Emerg Med) 7% 6
AMI with Non-diagnostic EKG Majority of patients presenting with an MI & initially normal EKG developed changes within the first 48 hours of hospitalization. In these cases in hospital complications are common. Lack of EKG evidence over the first 48 hours identifies a subgroup of patients that have smaller infarction & fewer in hospital complication. 7
MI with Non-diagnostic EKG Patient with AMI who demonstrates an initial normal EKG do not always have a favourable prognosis. High in hospital mortality rate 5. 7%. Serious cardiac event rate 19. 2%. Welch et al JAMA 2001 8
Approach in patients with suspected AMI & Nondiagnostic EKG 9
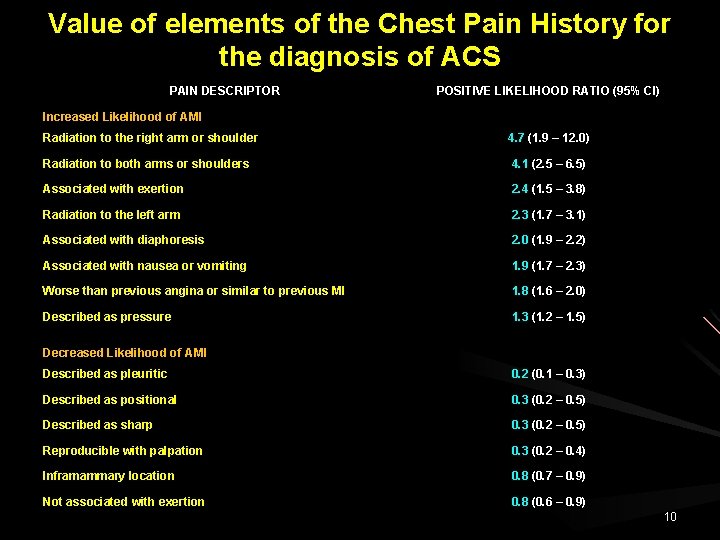
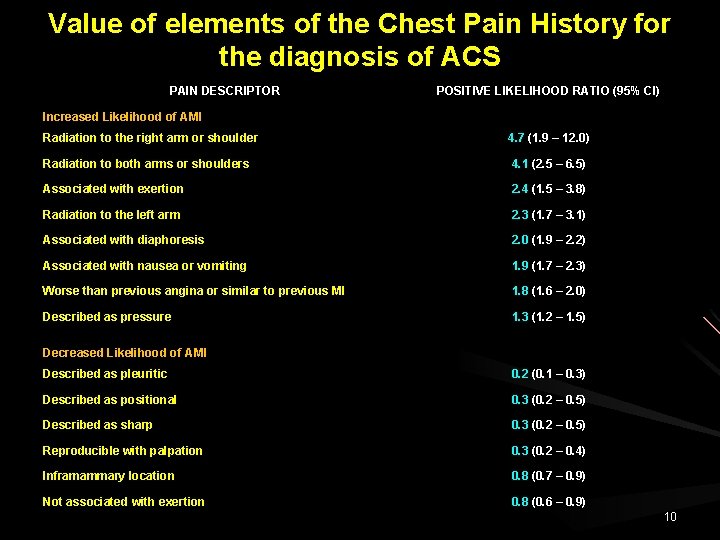
Value of elements of the Chest Pain History for the diagnosis of ACS PAIN DESCRIPTOR POSITIVE LIKELIHOOD RATIO (95% CI) Increased Likelihood of AMI Radiation to the right arm or shoulder 4. 7 (1. 9 – 12. 0) Radiation to both arms or shoulders 4. 1 (2. 5 – 6. 5) Associated with exertion 2. 4 (1. 5 – 3. 8) Radiation to the left arm 2. 3 (1. 7 – 3. 1) Associated with diaphoresis 2. 0 (1. 9 – 2. 2) Associated with nausea or vomiting 1. 9 (1. 7 – 2. 3) Worse than previous angina or similar to previous MI 1. 8 (1. 6 – 2. 0) Described as pressure 1. 3 (1. 2 – 1. 5) Decreased Likelihood of AMI Described as pleuritic 0. 2 (0. 1 – 0. 3) Described as positional 0. 3 (0. 2 – 0. 5) Described as sharp 0. 3 (0. 2 – 0. 5) Reproducible with palpation 0. 3 (0. 2 – 0. 4) Inframammary location 0. 8 (0. 7 – 0. 9) Not associated with exertion 0. 8 (0. 6 – 0. 9) 10
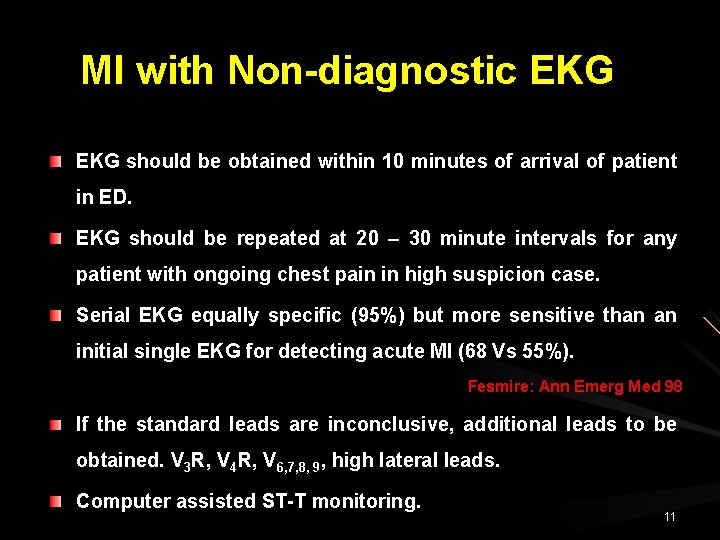
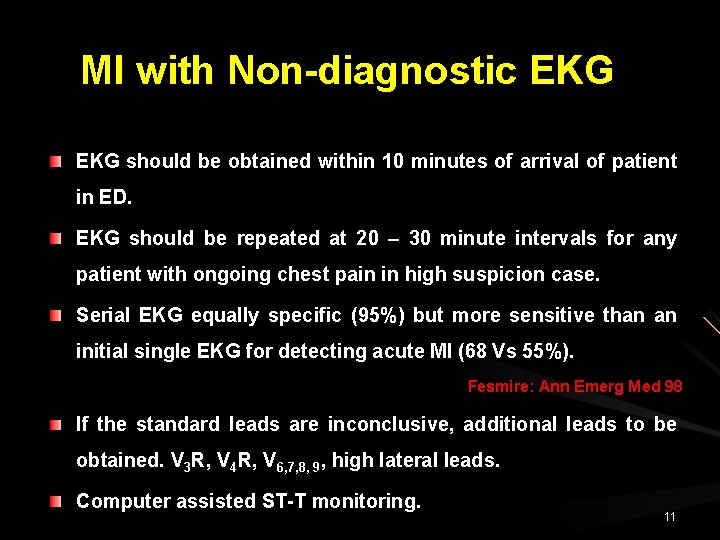
MI with Non-diagnostic EKG should be obtained within 10 minutes of arrival of patient in ED. EKG should be repeated at 20 – 30 minute intervals for any patient with ongoing chest pain in high suspicion case. Serial EKG equally specific (95%) but more sensitive than an initial single EKG for detecting acute MI (68 Vs 55%). Fesmire: Ann Emerg Med 98 If the standard leads are inconclusive, additional leads to be obtained. V 3 R, V 4 R, V 6, 7, 8, 9, high lateral leads. Computer assisted ST-T monitoring. 11
The 80 -Lead ECG and Body Surface Mapping More leads investigate more areas of the heart. Mapping allows computer generated pictures of ischemic areas. Computerized readings for more accurate interpretation. allow
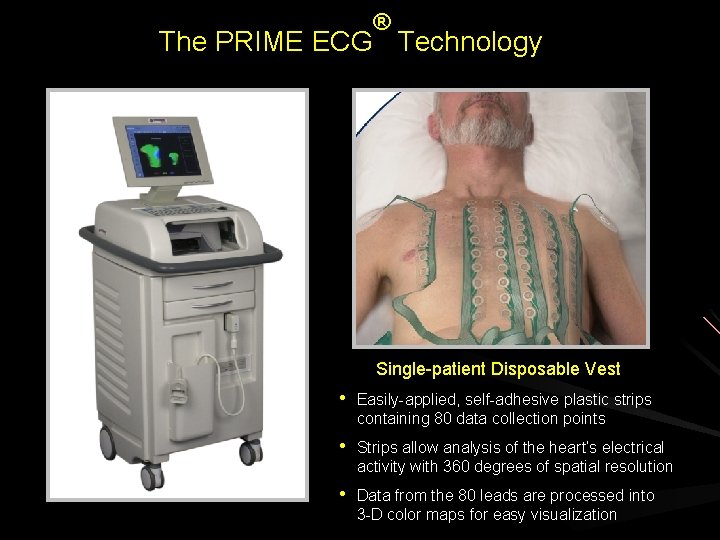
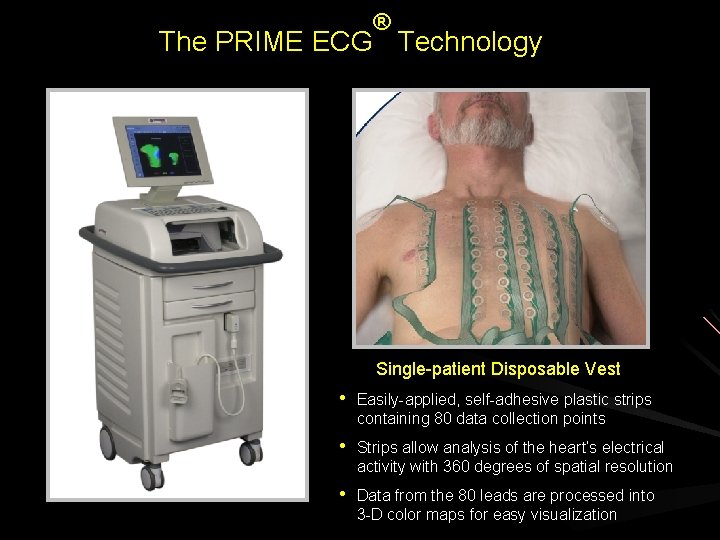
® The PRIME ECG Technology Single-patient Disposable Vest • Easily-applied, self-adhesive plastic strips containing 80 data collection points • Strips allow analysis of the heart’s electrical activity with 360 degrees of spatial resolution • Data from the 80 leads are processed into 3 -D color maps for easy visualization
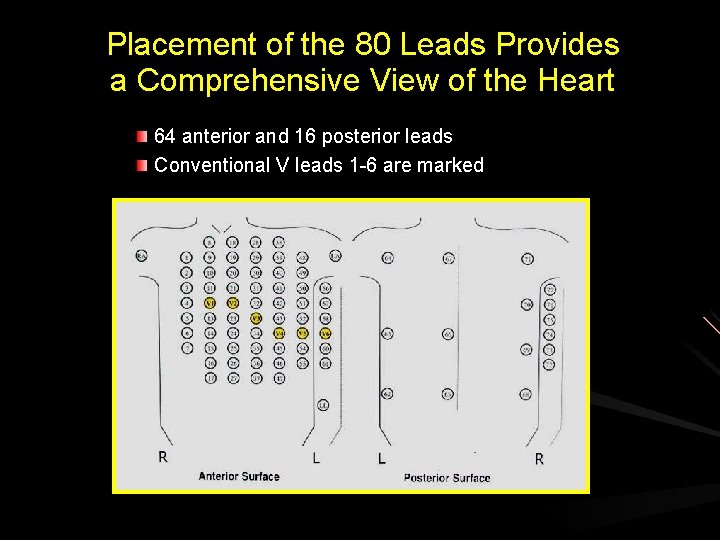
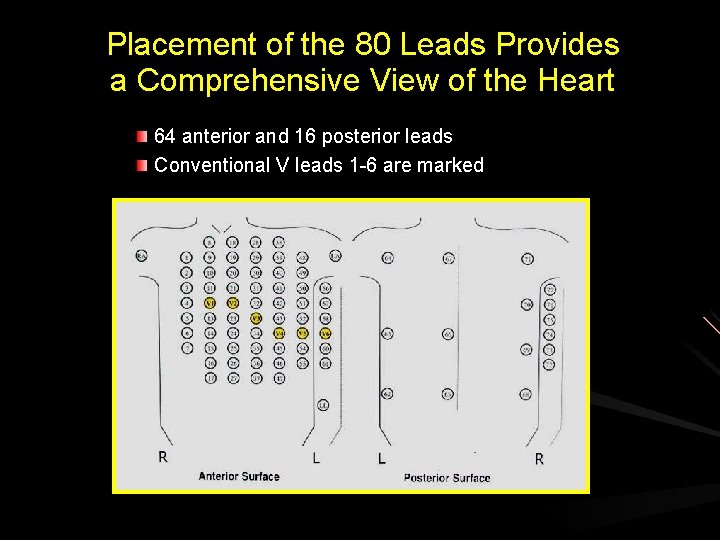
Placement of the 80 Leads Provides a Comprehensive View of the Heart 64 anterior and 16 posterior leads Conventional V leads 1 -6 are marked
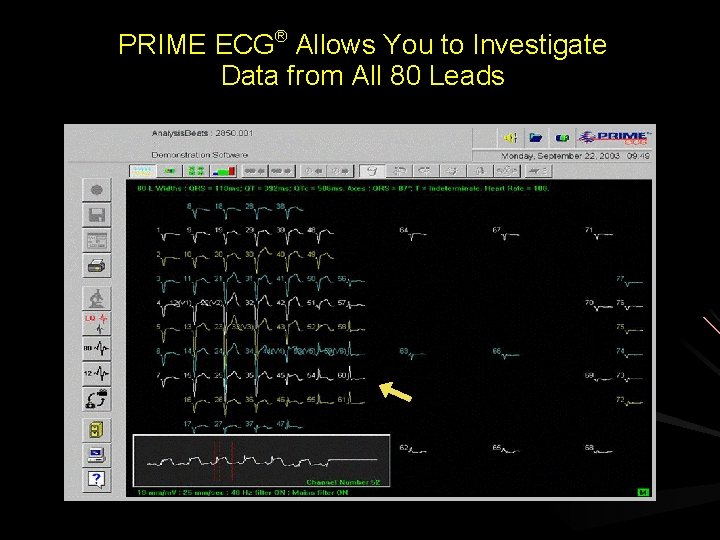
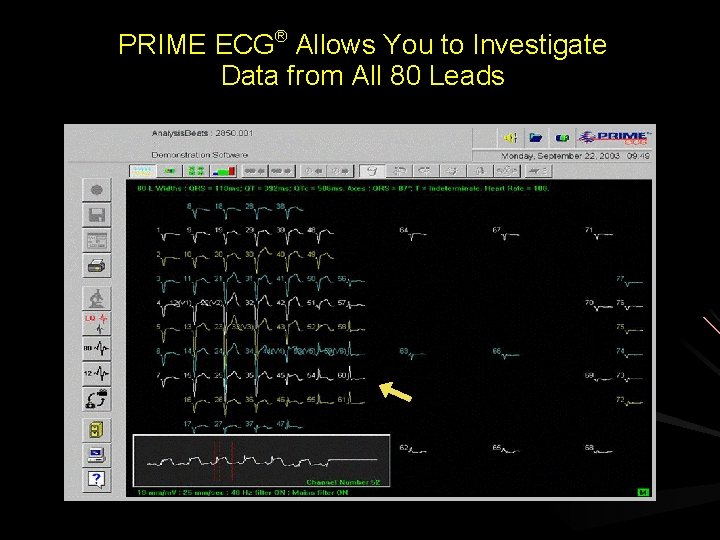
PRIME ECG® Allows You to Investigate Data from All 80 Leads View a single 10 -second recording for leads of interest
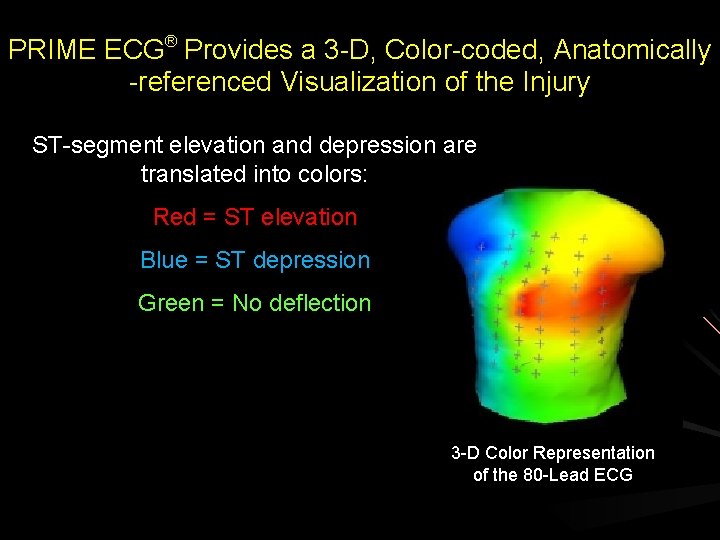
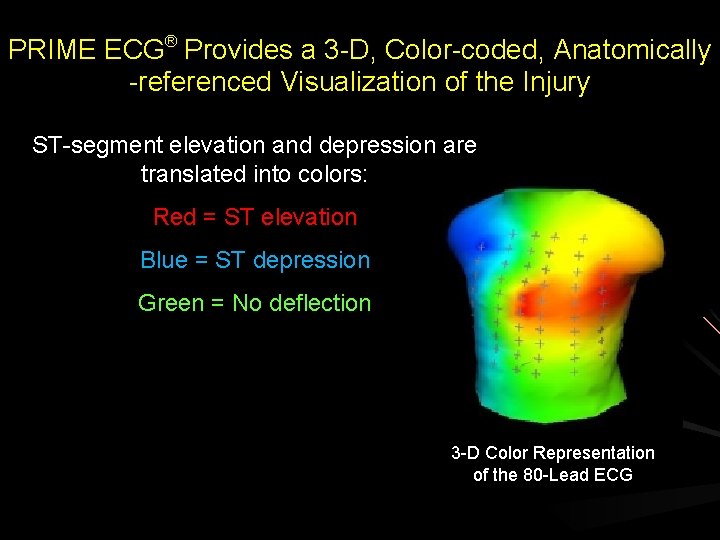
PRIME ECG® Provides a 3 -D, Color-coded, Anatomically -referenced Visualization of the Injury ST-segment elevation and depression are translated into colors: Red = ST elevation Blue = ST depression Green = No deflection 3 -D Color Representation of the 80 -Lead ECG
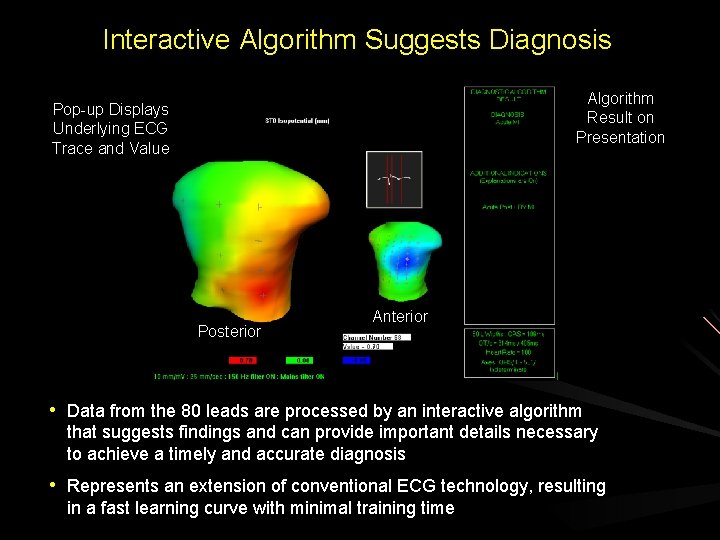
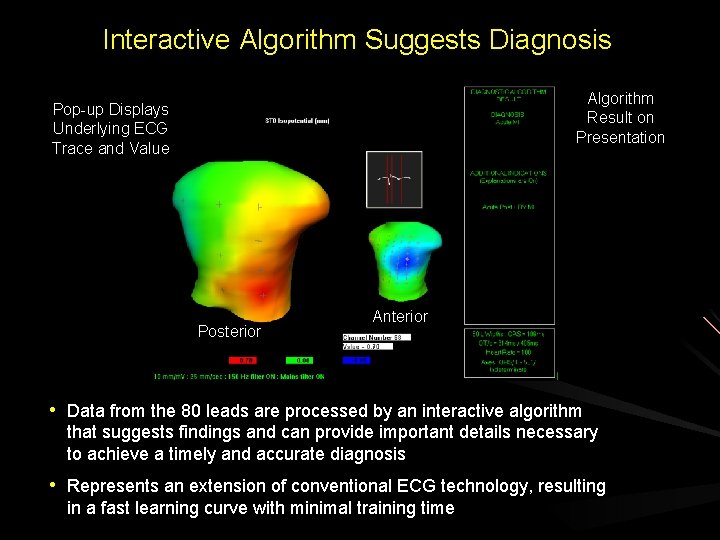
Interactive Algorithm Suggests Diagnosis Algorithm Result on Presentation Pop-up Displays Underlying ECG Trace and Value Posterior Anterior • Data from the 80 leads are processed by an interactive algorithm that suggests findings and can provide important details necessary to achieve a timely and accurate diagnosis • Represents an extension of conventional ECG technology, resulting in a fast learning curve with minimal training time
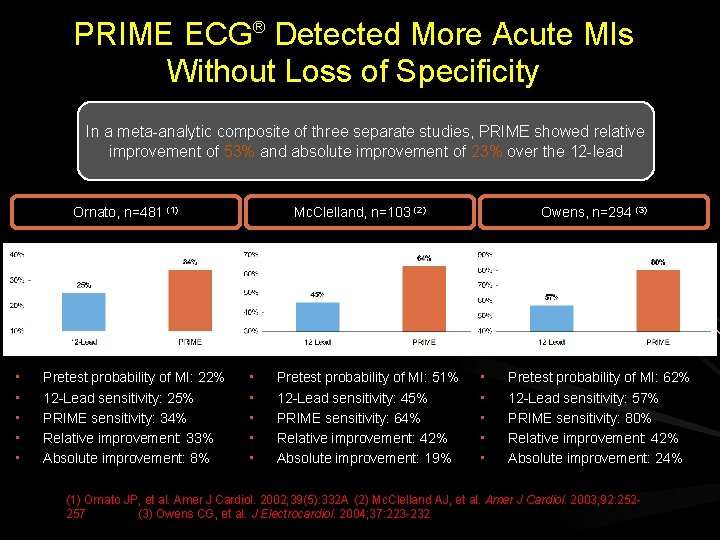
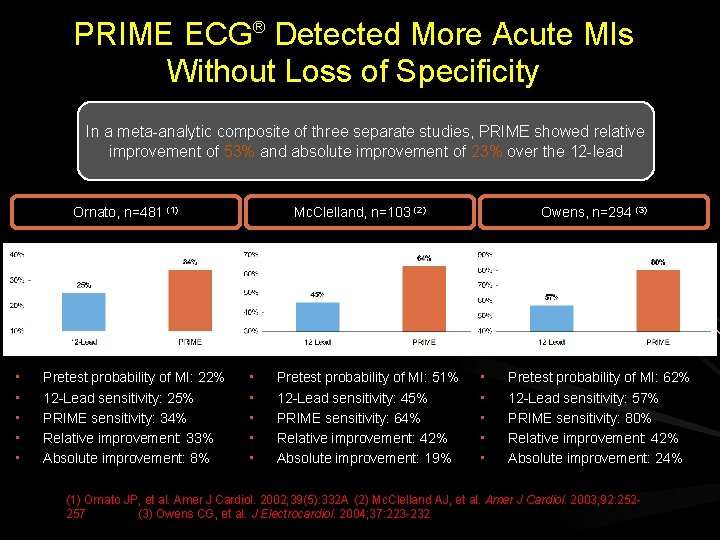
PRIME ECG® Detected More Acute MIs Without Loss of Specificity In a meta-analytic composite of three separate studies, PRIME showed relative improvement of 53% and absolute improvement of 23% over the 12 -lead Ornato, n=481 (1) • • • Pretest probability of MI: 22% 12 -Lead sensitivity: 25% PRIME sensitivity: 34% Relative improvement: 33% Absolute improvement: 8% Mc. Clelland, n=103 (2) • • • Pretest probability of MI: 51% 12 -Lead sensitivity: 45% PRIME sensitivity: 64% Relative improvement: 42% Absolute improvement: 19% Owens, n=294 (3) • • • Pretest probability of MI: 62% 12 -Lead sensitivity: 57% PRIME sensitivity: 80% Relative improvement: 42% Absolute improvement: 24% (1) Ornato JP, et al. Amer J Cardiol. 2002; 39(5): 332 A (2) Mc. Clelland AJ, et al. Amer J Cardiol. 2003; 92: 252257 (3) Owens CG, et al. J Electrocardiol. 2004; 37: 223 -232
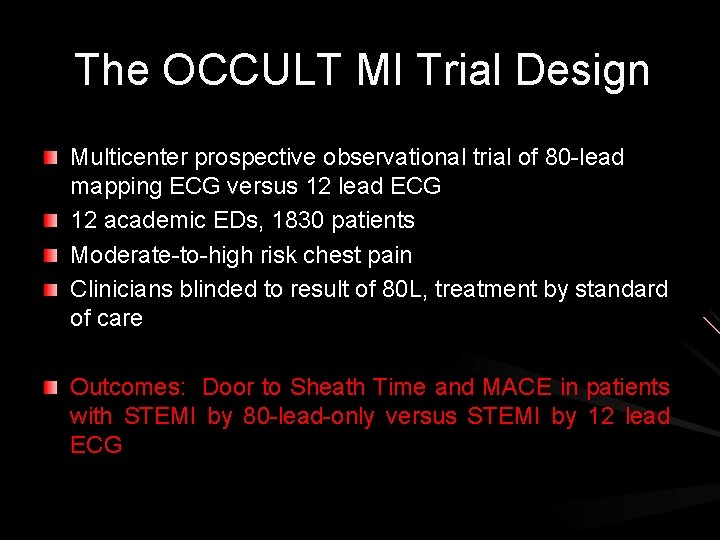
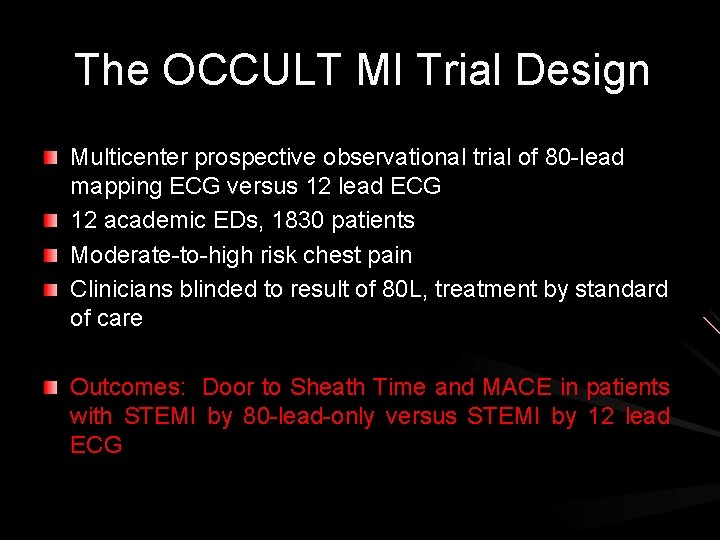
The OCCULT MI Trial Design Multicenter prospective observational trial of 80 -lead mapping ECG versus 12 lead ECG 12 academic EDs, 1830 patients Moderate-to-high risk chest pain Clinicians blinded to result of 80 L, treatment by standard of care Outcomes: Door to Sheath Time and MACE in patients with STEMI by 80 -lead-only versus STEMI by 12 lead ECG
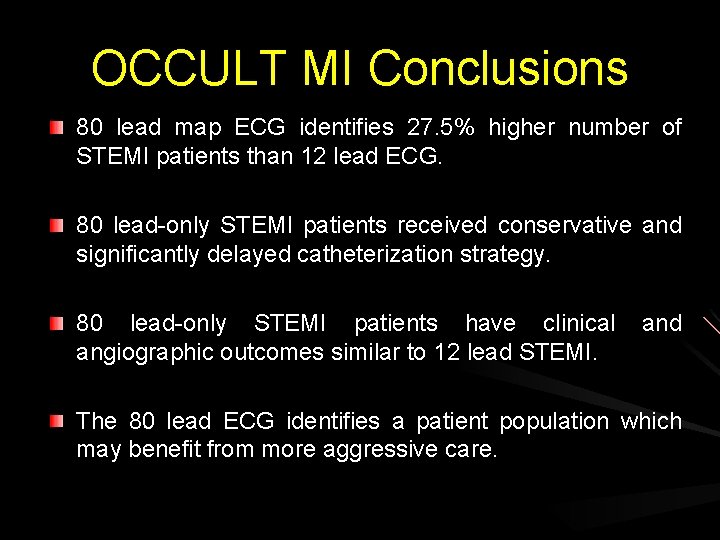
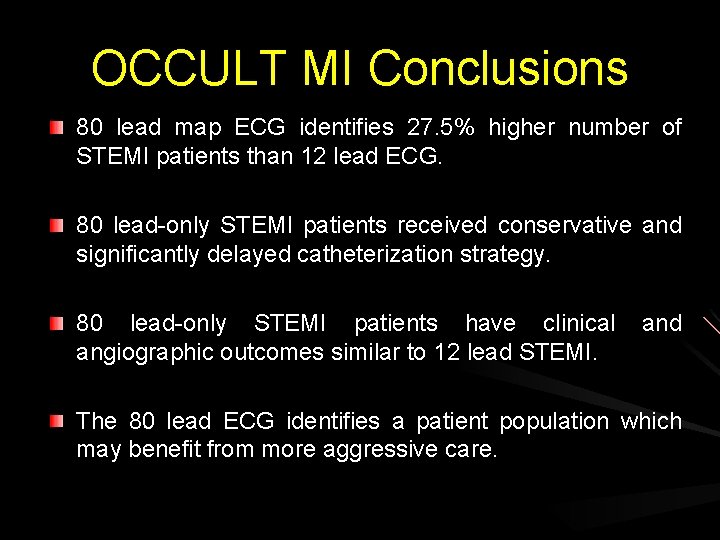
OCCULT MI Conclusions 80 lead map ECG identifies 27. 5% higher number of STEMI patients than 12 lead ECG. 80 lead-only STEMI patients received conservative and significantly delayed catheterization strategy. 80 lead-only STEMI patients have clinical and angiographic outcomes similar to 12 lead STEMI. The 80 lead ECG identifies a patient population which may benefit from more aggressive care.
Summary • The 80 -lead technology increases the sensitivity and specificity of the ECG for MI. • The PRIME system allows for ease of ECG acquisition in clinical care. • OCCULT MI trial confirms that PRIME can identify a high risk patient that may benefit from more aggressive therapy.
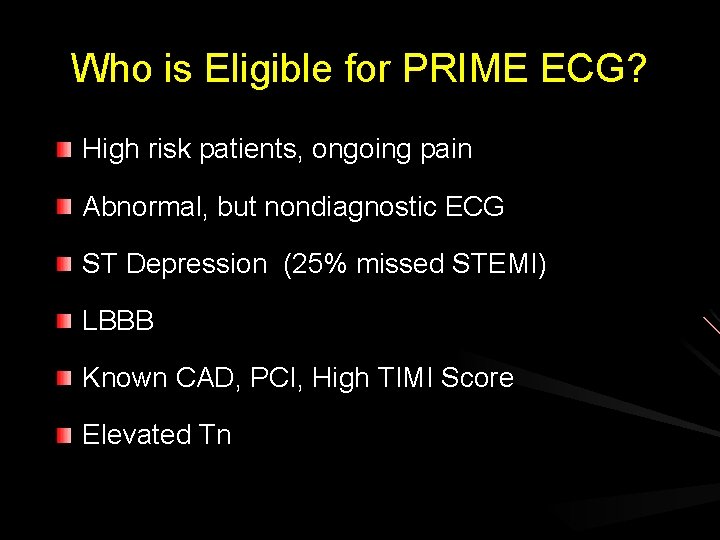
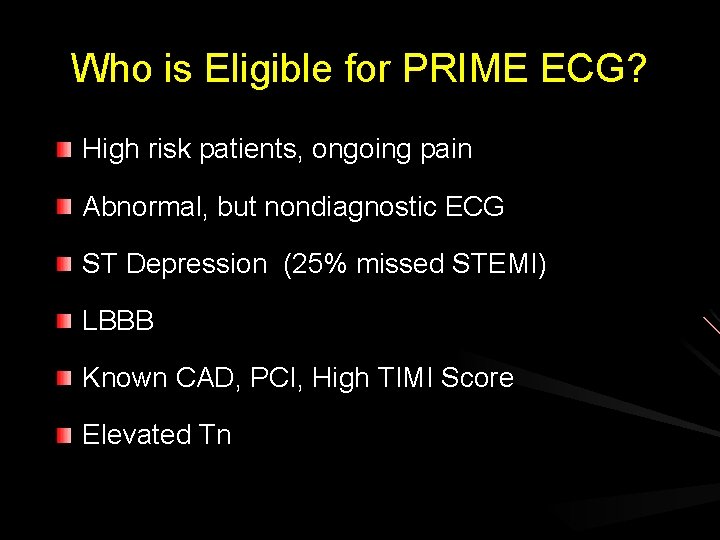
Who is Eligible for PRIME ECG? High risk patients, ongoing pain Abnormal, but nondiagnostic ECG ST Depression (25% missed STEMI) LBBB Known CAD, PCI, High TIMI Score Elevated Tn
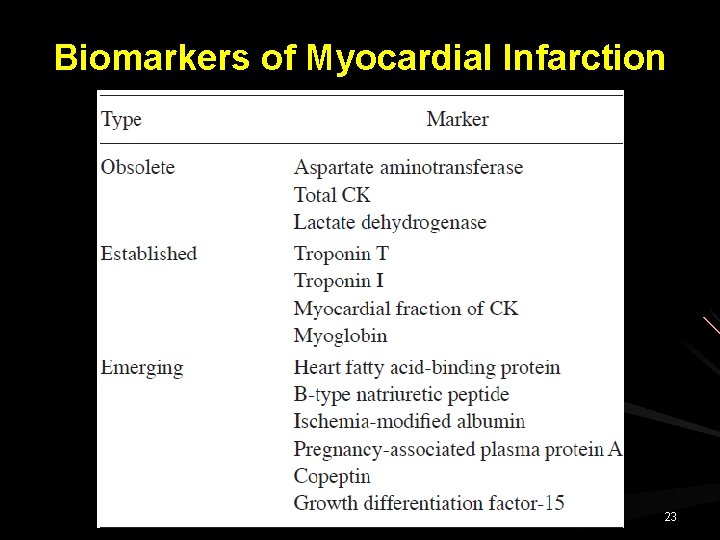
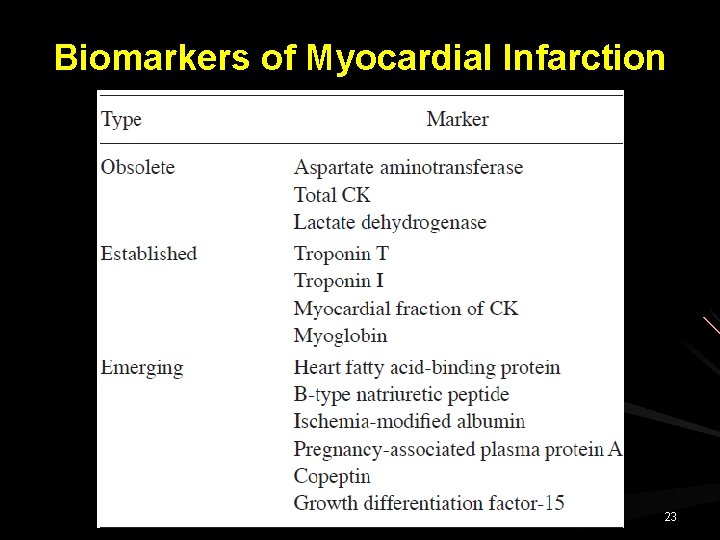
Biomarkers of Myocardial Infarction 23
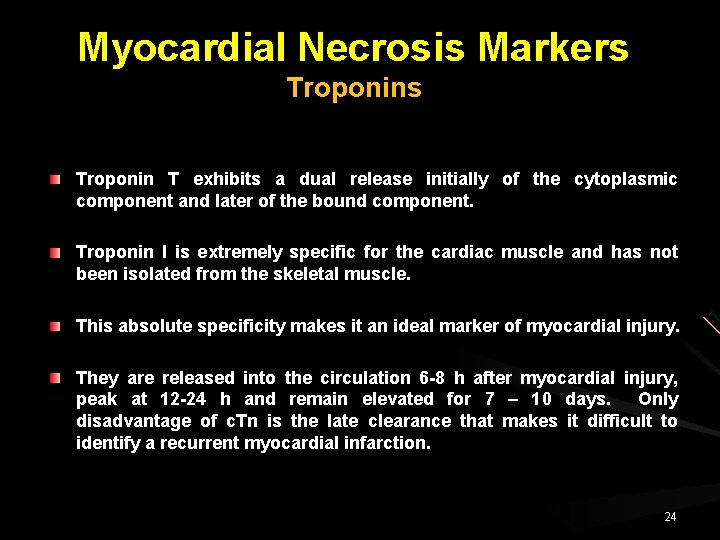
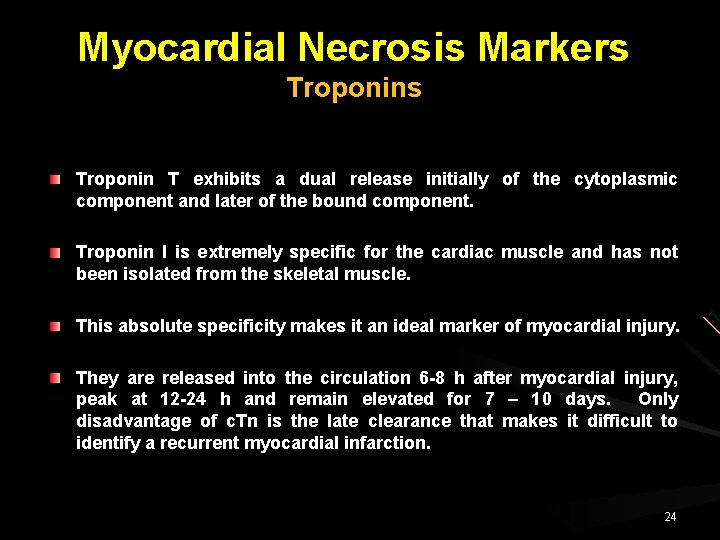
Myocardial Necrosis Markers Troponin T exhibits a dual release initially of the cytoplasmic component and later of the bound component. Troponin I is extremely specific for the cardiac muscle and has not been isolated from the skeletal muscle. This absolute specificity makes it an ideal marker of myocardial injury. They are released into the circulation 6 -8 h after myocardial injury, peak at 12 -24 h and remain elevated for 7 – 10 days. Only disadvantage of c. Tn is the late clearance that makes it difficult to identify a recurrent myocardial infarction. 24
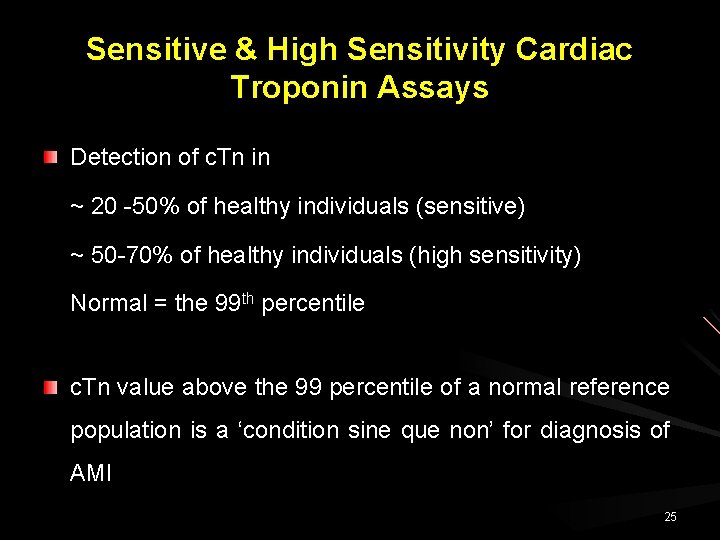
Sensitive & High Sensitivity Cardiac Troponin Assays Detection of c. Tn in ~ 20 -50% of healthy individuals (sensitive) ~ 50 -70% of healthy individuals (high sensitivity) Normal = the 99 th percentile c. Tn value above the 99 percentile of a normal reference population is a ‘condition sine que non’ for diagnosis of AMI 25
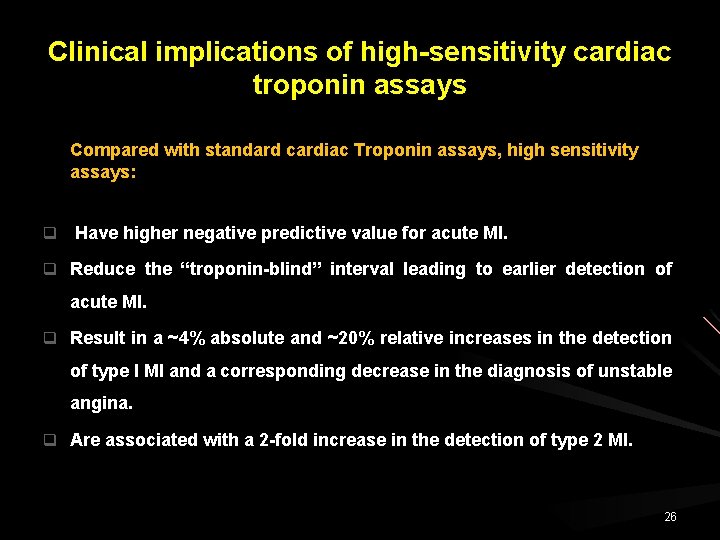
Clinical implications of high-sensitivity cardiac troponin assays Compared with standard cardiac Troponin assays, high sensitivity assays: q Have higher negative predictive value for acute MI. q Reduce the “troponin-blind” interval leading to earlier detection of acute MI. q Result in a ~4% absolute and ~20% relative increases in the detection of type I MI and a corresponding decrease in the diagnosis of unstable angina. q Are associated with a 2 -fold increase in the detection of type 2 MI. 26
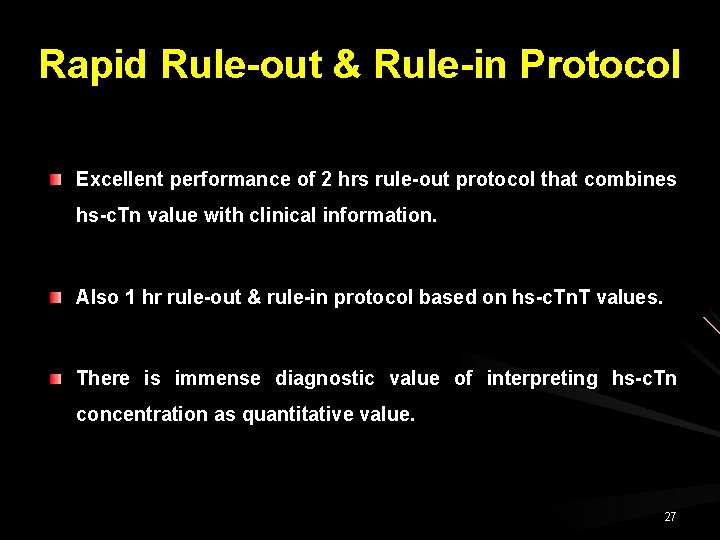
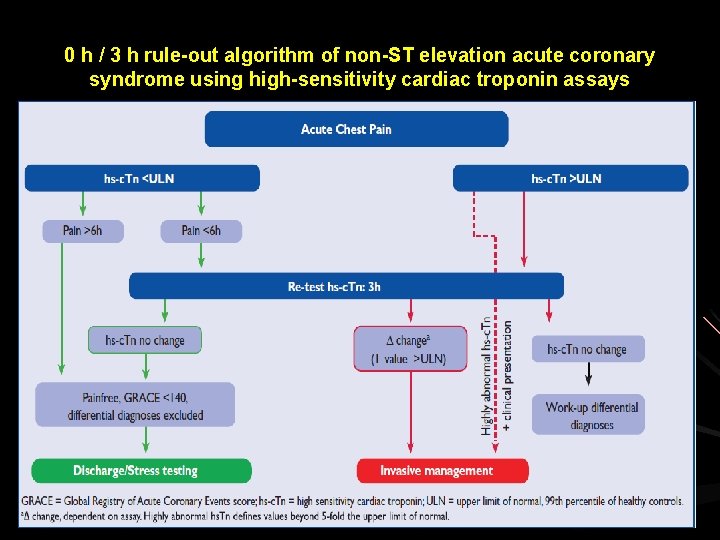
Rapid Rule-out & Rule-in Protocol Excellent performance of 2 hrs rule-out protocol that combines hs-c. Tn value with clinical information. Also 1 hr rule-out & rule-in protocol based on hs-c. Tn. T values. There is immense diagnostic value of interpreting hs-c. Tn concentration as quantitative value. 27
![The use of sensitive or highsensitivity cardiac troponin hsc Tn allows more rapid ruleout The use of sensitive or high-sensitivity cardiac troponin [(h)s-c. Tn] allows more rapid rule-out](https://slidetodoc.com/presentation_image_h/23281574161caaa98a51646b5558302e/image-28.jpg)
The use of sensitive or high-sensitivity cardiac troponin [(h)s-c. Tn] allows more rapid rule-out and more rapid rule-in. 28
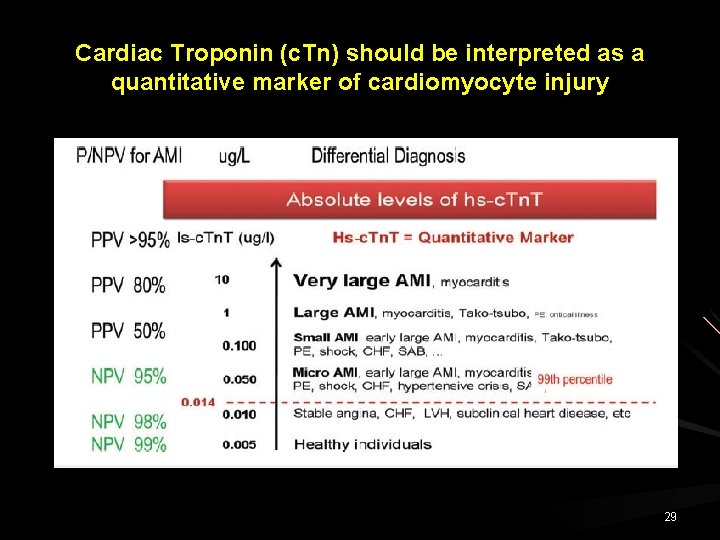
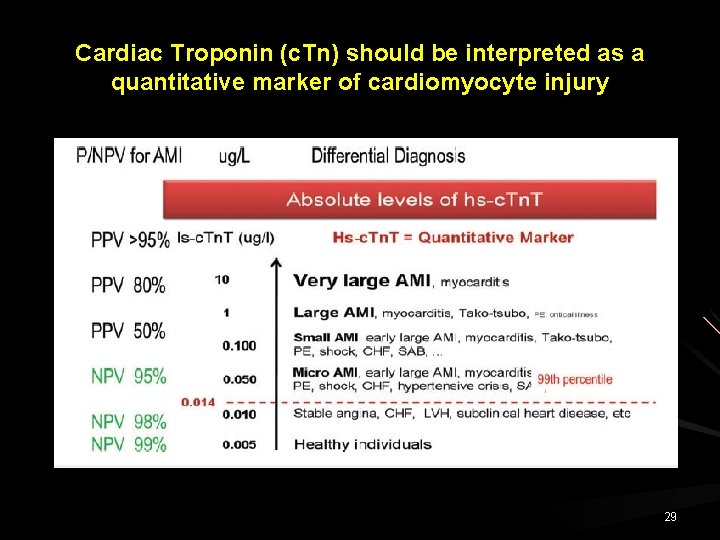
Cardiac Troponin (c. Tn) should be interpreted as a quantitative marker of cardiomyocyte injury 29
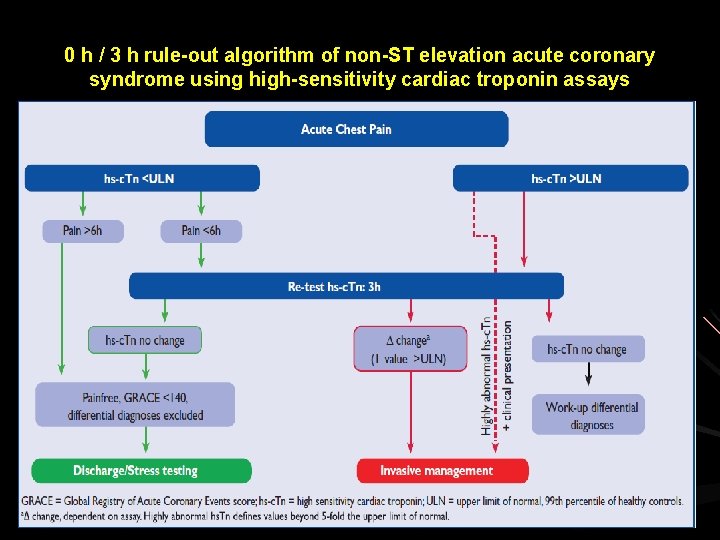
0 h / 3 h rule-out algorithm of non-ST elevation acute coronary syndrome using high-sensitivity cardiac troponin assays 30
Myocardial Necrosis Markers Myoglobin (MYO) MYO is a small cytoplasmic oxygen-binding protein found in the skeletal as well as the cardiac muscle. It is released extremely early into the serum, 1 h after the onset of myocardial injury, peaks at 4 -12 h and returns to baseline values immediately. Major disadvantage of MYO is the lack of specificity to the cardiac tissue due to the presence of large amounts of MYO in the skeletal muscle. Levels of MYO can therefore not be used as a single diagnostic marker, but in conjunction with the Troponins or CK-MB Serum levels of MYO can be used to rule out, rather than diagnose, myocardial infarction. 31
Copeptin C-Terminal part of vasopressin prohormones. Secreted from neurohypophysis and quantify endogenous stress level. Copeptin identify AMI very early after symptom onset, even when c. Tn is still negative. In combination with c. Tn. T, it has added diagnostic value. 32
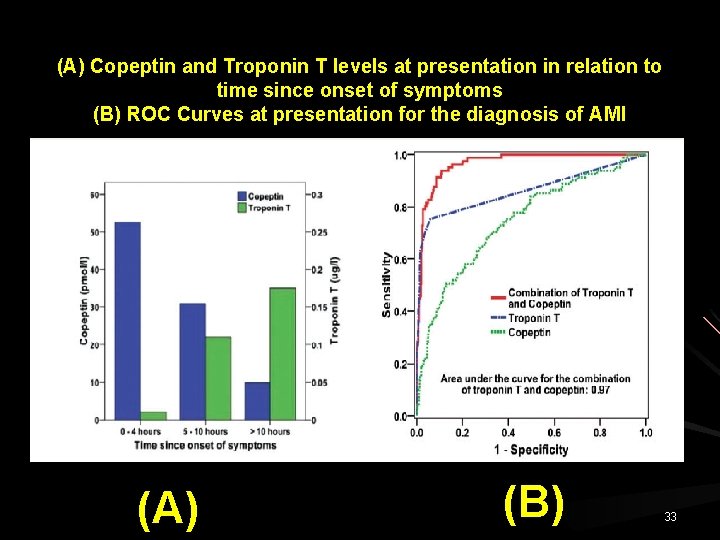
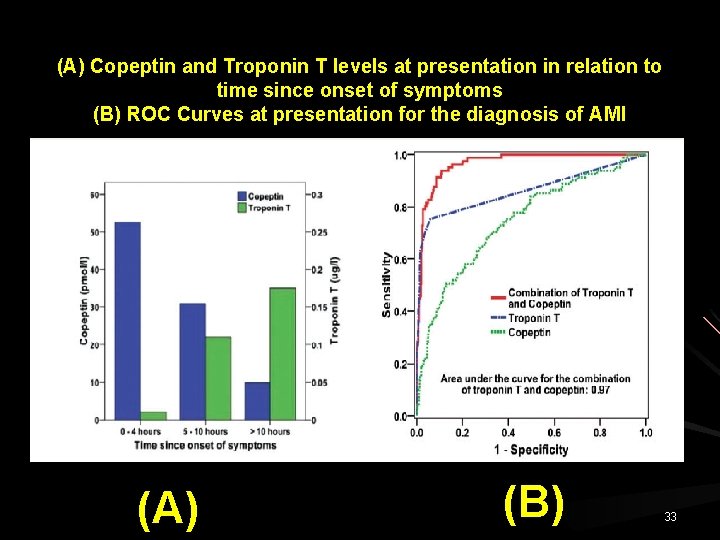
(A) Copeptin and Troponin T levels at presentation in relation to time since onset of symptoms (B) ROC Curves at presentation for the diagnosis of AMI (A) (B) 33
Heart-Type Fatty Acid Binding Protein (H-FABP) H-FABP is a low molecular weight protein involved in myocardial fatty-acid metabolism. It is rapidly released early in myocardial infarction and necrosis into the cytosol. H-FABP has been shown in mouse studies to be an early marker of ischemia and can therefore help with diagnosis of MI earlier. One review of six studies found that the pooled positive predictive value to be 65. 8% and pooled negative predictive value to be 82%. When added to Troponin for risk stratification, a negative Troponin & HFABP level < 5. 8 mcg/L was associated with zero mortality at 6 months, a negative Troponin but H-FABP level > 5. 8 mcg/L was associated with a 4. 93 fold increase in risk of death and 7. 93 fold increase in risk if Troponin was positive & H-FABP > 5. 8 mcg/L 34
Heart-Type Fatty Acid Binding Protein (H-FABP) “Heart-type Fatty Acid Binding Protein and copeptin in combination with cardiac troponin help diagnose myocardial infarction or acute coronary syndrome in the early hours following symptoms”. 35
Noninvasive Imaging – Functional Evaluation TTE should be routinely performed in ED. Useful in identifying myocardial ischemia or necrosis (WMD). In absence of significant WMD, impaired myocardial perfusion detected by contrast echo or reduced regional function using strain & strain rate imaging, has diagnostic & prognostic value. Can detect alternative pathology associated with chest pain viz aortic dissection, PE, aortic valve stenosis. Evaluation of LV systolic function, prognostic significance. 36
Noninvasive Imaging – Functional Evaluation Patient without EKG changes and negative cardiac Troponins, free of chest pain, stress imaging can be performed. Stress imaging is preferred over exercise EKG due to higher diagnostic accuracy. 37
“Contrast stress-echocardiography predicts cardiac events in patients with suspected acute coronary syndrome but nondiagnostic electrocardiogram and normal 12 -hour Troponin” Galibazzi N et al J Am Soc Echocardiogr 2011 38
Noninvasive Imaging – Functional Evaluation Cardiac Magnetic Resonance (CMR) Can assess both perfusion and wall motion abnormality. CMR permits detection of scar tissue (late Gadolinium enhancement) and can differentiate it from recent MI. CMR facilitates differential diagnosis between infarction & myocarditis and Takotsubo cardiomyopathy. 39
Noninvasive Imaging – Functional Evaluation Nuclear MPI, useful for risk stratification of patient with chest pain suggestive of ACS. Rest MPI, by detecting fixed perfusion defects suggestive of myocardial necrosis, can be helpful for initial triage of patients presenting with chest pain without EKG changes or elevated cardiac Troponin. Combined stress test imaging further enhances the assessment of ischemia, while a normal study is associated with excellent outcome. Lim SH: J Nucl Cardiol 2013 40
MI with Non-diagnostic EKG Anatomical Evaluation Multi-detector Computed Tomography (MDCT) Allows visualization of coronaries and R/o CAD. Overall high negative predictive value to exclude ACS. Samad J: J Nucl Cardiol 2012 41
“Coronary CT angiography versus standard evaluation in acute chest pain” Hoffmann U, Truong QA et al N Engl J Med 2012
“CT angiography for safe discharge of patients with possible acute coronary syndromes” Litt HI, Gatsonis C et al N Engl J Med 2012
“Outcomes after coronary computed tomography angiography in the emergency department: a systematic review and metaanalysis of randomized, controlled trials” Hulten E, Pickett et al J Am Coll Cardiol 2013
“Triple rule-out computed tomographic angiography for chest pain: a diagnostic systematic review and meta-analysis” Ayaram D, Bellolio MF et al Acad Emerg Med 2013
AMI with Non-diagnostic EKG Principle Diagnostic Tool q History of the Event q Twelve Lead EKG q Serum Markers of Cardiac Injury q Cardiac Imaging ================= Strength, Weaknesses, Predictive Value 46
MI with Non-diagnostic EKG is exactly what the name implies – “Non-diagnostic”. Over reliance on a non-diagnostic EKG is fraught with both error & danger. Few patient with non-diagnostic EKG suffers MI. Sizeable minority will have unstable coronary syndrome. 47
Acute Myocardial Infarction with an Initially Non-Diagnostic Electrocardiogram “Clinical Intuition is Crucial for Decision Making”. Dejan Petrovic et al: Scientific Journal of Faculty of Med 2014 48
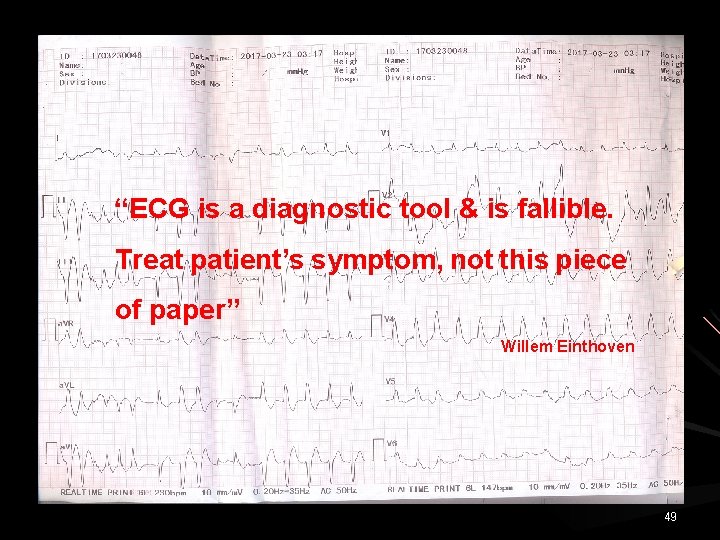
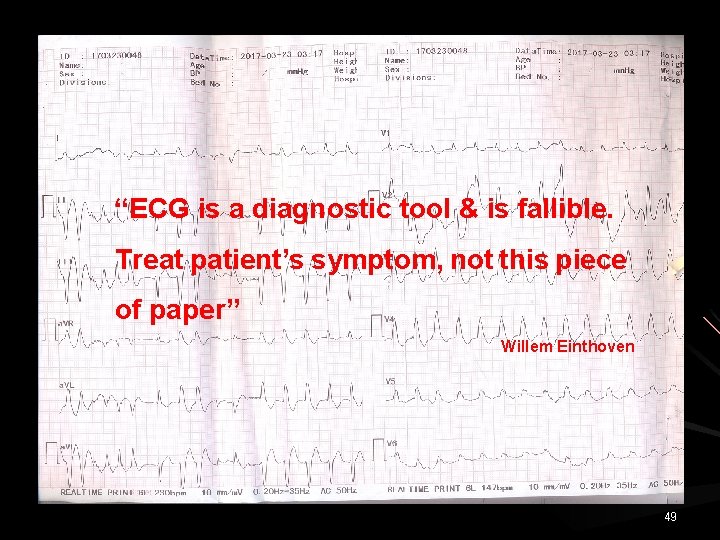
“ECG is a diagnostic tool & is fallible. Treat patient’s symptom, not this piece of paper” Willem Einthoven 49
 Dr vinod sharma national heart institute
Dr vinod sharma national heart institute Ca vinod jain
Ca vinod jain Vinod kurup
Vinod kurup Dma remapping
Dma remapping Vinod panicker
Vinod panicker Vinod dhall
Vinod dhall Vinod vaikuntanathan
Vinod vaikuntanathan Aorldw
Aorldw Advocate vinod sampat fees
Advocate vinod sampat fees Vinod vaikuntanathan
Vinod vaikuntanathan Vinod bidwaik
Vinod bidwaik Vinod ganapathy iisc
Vinod ganapathy iisc Adjacency matrix multigraph
Adjacency matrix multigraph Dr vishal sharma
Dr vishal sharma Dr pushpa raj sharma
Dr pushpa raj sharma Dr suman sharma
Dr suman sharma Pushpa raj sharma
Pushpa raj sharma Pushpa raj sharma
Pushpa raj sharma Dr pk sharma
Dr pk sharma Cs deepak sharma
Cs deepak sharma Gaurav sharma cisco
Gaurav sharma cisco Pawan sharma bits pilani
Pawan sharma bits pilani Zinc deficiency rash
Zinc deficiency rash Sumit sharma teri
Sumit sharma teri Umesh sharma md
Umesh sharma md Card repertory
Card repertory Dr bikas sharma
Dr bikas sharma Rowena mittal
Rowena mittal Dr rakesh sharma ahmedabad
Dr rakesh sharma ahmedabad Pradeep sharma university of houston
Pradeep sharma university of houston Keerti sharma md
Keerti sharma md Dr vivek sharma
Dr vivek sharma Riju sharma
Riju sharma Facial nerve decompression surgery
Facial nerve decompression surgery Pushpa
Pushpa Pushpa raj sharma
Pushpa raj sharma Dr pushpa raj sharma
Dr pushpa raj sharma Dr pushpa raj sharma clinic
Dr pushpa raj sharma clinic Axtec calender
Axtec calender Concepts of child care
Concepts of child care Amrit sharma morgan stanley
Amrit sharma morgan stanley Dr archana sharma psychologist
Dr archana sharma psychologist Jag sharma
Jag sharma Dr madhurima sharma
Dr madhurima sharma Pushpa raj sharma
Pushpa raj sharma Dipti mishra iiit hyderabad
Dipti mishra iiit hyderabad Ca umesh sharma
Ca umesh sharma Put first things first
Put first things first First in first out
First in first out Sdl first vs code first
Sdl first vs code first