Medical University of Sofia Faculty of M Department







- Slides: 94
Medical University of Sofia, Faculty of M Department of Pharmacology and Toxico STEROID HORMONES Glucocorticoids Mineralcorticoids Sex hormones Assoc. Prof. Ivan Lambev e-mail: itlambev@mail. bg
Corticotrophin releasing hormone (CRH) – corticoliberin, is a hypothalamic polypeptide for diagnostic use. It increases ACTH secretion in Cushing's disease secondary to pituitary ACTHsecreting adenoma. Natural corticotrophin is a 39 -amino-acid polypeptide secreted by the anterior pituitary gland; it is obtained from animal pituitaries. The physiological activity resides in the first 24 -amino acids (which are common to many species) and most immunological activity resides in the remaining 15 aminoacids. The pituitary output of corticotrophin responds rapidly to physiological requirements by the familiar negative-feedback homeostatic mechanism.
Since the t 1/2 of corticotrophin is 10 min and the adrenal cortex responds rapidly (within 2 min) it is plain that adjustments of steroid output can be quickly made. Synthetic corticotrophin tetracosactide has the advantage that they are shorter amino acid chains (devoid of amino acids 25– 39) and so are less likely to cause serious allergy, though this can happen. In addition they are not contaminated by animal proteins which are potent allergens. It consists of the biologically active first 24 amino acids of natural corticotrophin (from man or animals) and so it has similar properties, e. g. t 1/2 10 min.
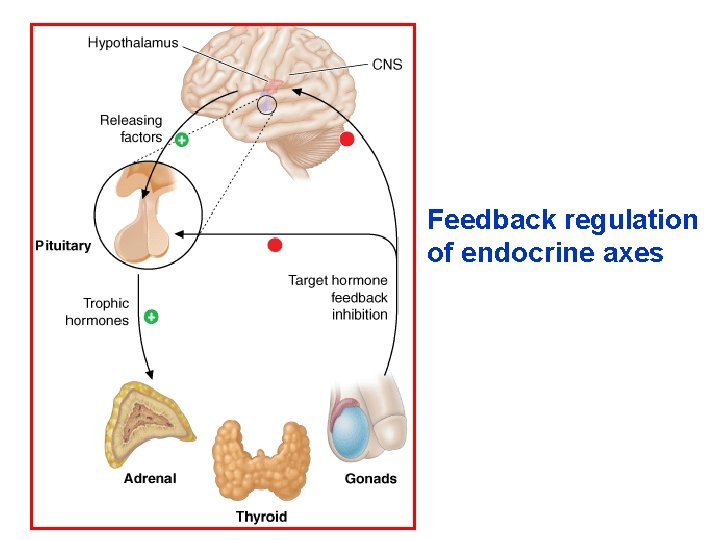
Corticotrophin stimulates the synthesis of corticosteroids (of which the most important is hydrocortisone) and to a lesser extent of androgens, by the cells of the adrenal cortex. It has only a minor effect on aldosterone production. The release of natural corticotrophin by the pituitary gland is controlled by the hypothalamus via corticotrophin releasing hormone (corticoliberin), production of which is influenced by stress as well as by the level of circulating hydrocortisone.
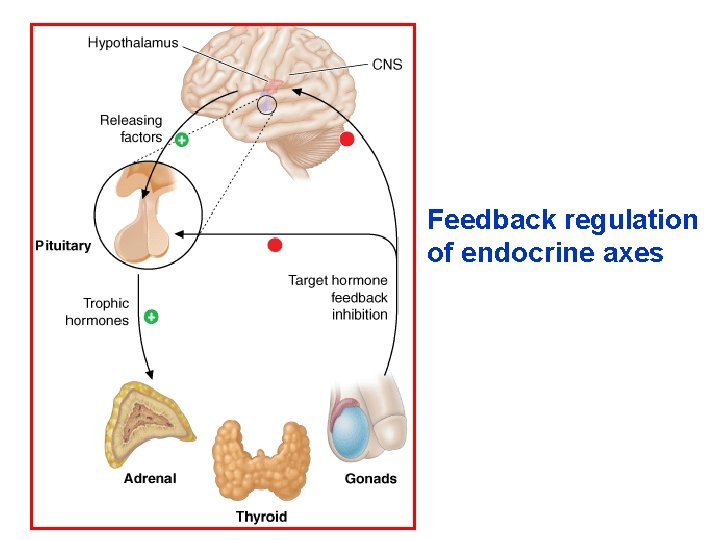
Feedback regulation of endocrine axes
High plasma concentration of any steroid with glucocorticoid effect prevents release of corticotrophin releasing hormone and so of ACTH, lack of which in turn results in adrenocortical hypofunction. This is the reason why catastrophe may follow sudden withdrawal of steroid therapy in the chronically treated patient who has an atrophied cortex. The effects of corticotrophin are those of the steroids (hydrocortisone, androgens) liberated by its action on the adrenal cortex. Prolonged heavy dosage causes the clinical picture of Cushing's syndrome. Corticotrophin is used principally in diagnosis and rarely in treatment.
Diagnostic use: as a test of the capacity of the adrenal cortex to produce cortisol; with the short test, the plasma cortisol (hydrocortisone) concentration is measured before and after an i. m. injection of tetracosactide (Synacthen®). Therapeutic use of ACTH is seldom appropriate because the peptide hormone has to be injected; selective glucocorticoid action (without mineralocorticoid effect) cannot be obtained, and clinical results are irregular.
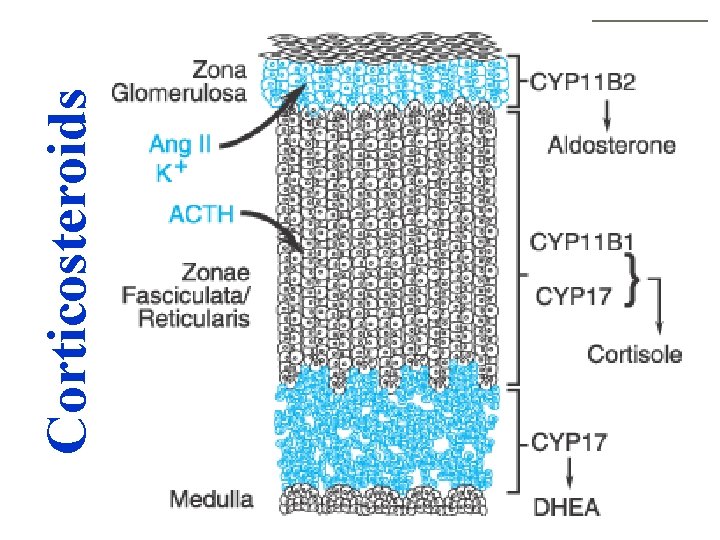
Hormones normally produced by the adrenal cortex include hydrocortisone (cortisol) and some androgens and estrogens, the synthesis and release of which is controlled by the hypothalamicpituitary system, and aldosterone, whose biosynthesis is largely dependent on the renin-angiotensin system. Numerous analogues have been made. When the adrenal cortex fails (Addison's disease) adrenocortical steroids are available for replacement therapy, but their chief use in medicine is for their anti-inflammatory and immunosuppressive effects. These are obtained only when the drugs are given in doses far above those needed for physiological replacement.
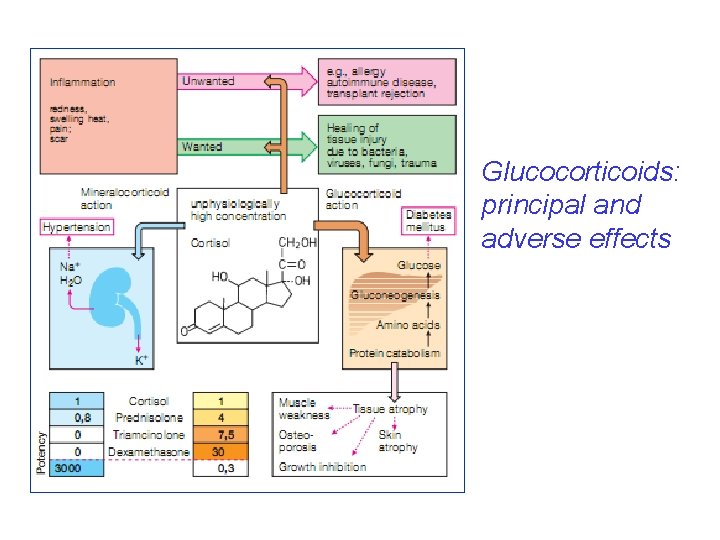
Various metabolic effects, which are of the greatest importance to the normal functioning of the body, then become adverse effects. Much successful effort has gone into separating glucocorticoid from mineralocorticoid effects and some steroids, e. g. dexamethasone, have virtually no mineralocorticoid activity. But it has not yet proved possible to separate the glucocorticoid effects from each other, so that if a steroid is used for its anti-inflammatory action the risks, e. g. of osteoporosis or diabetes mellitus, remain.
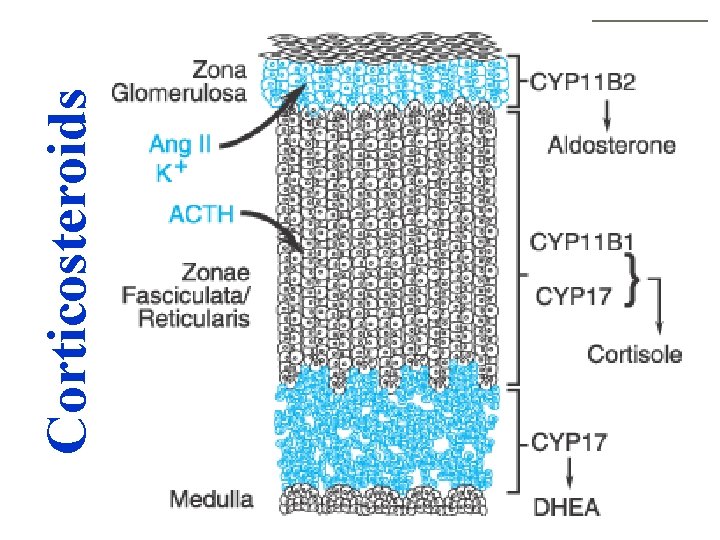
Corticosteroids
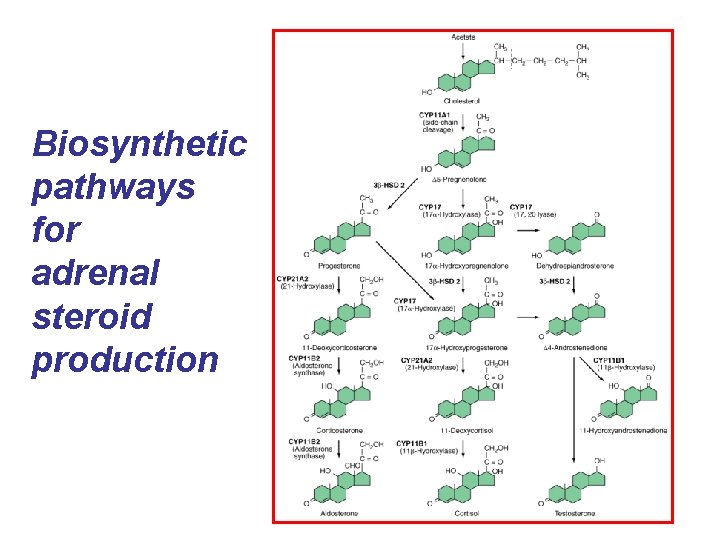
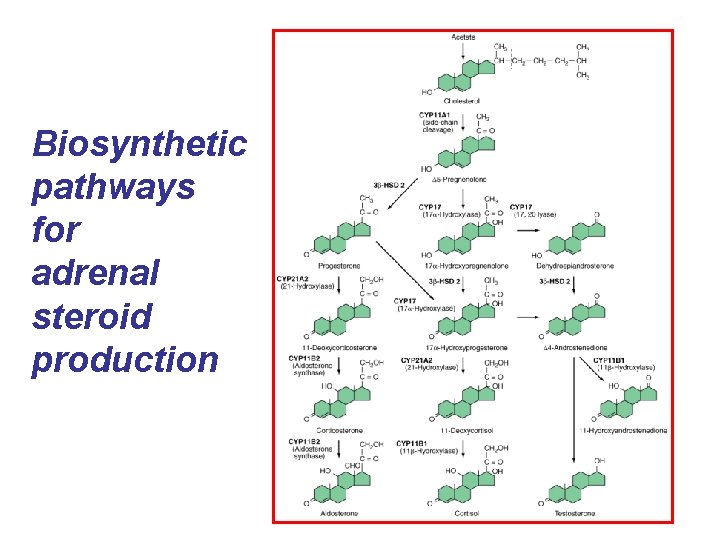
Biosynthetic pathways for adrenal steroid production
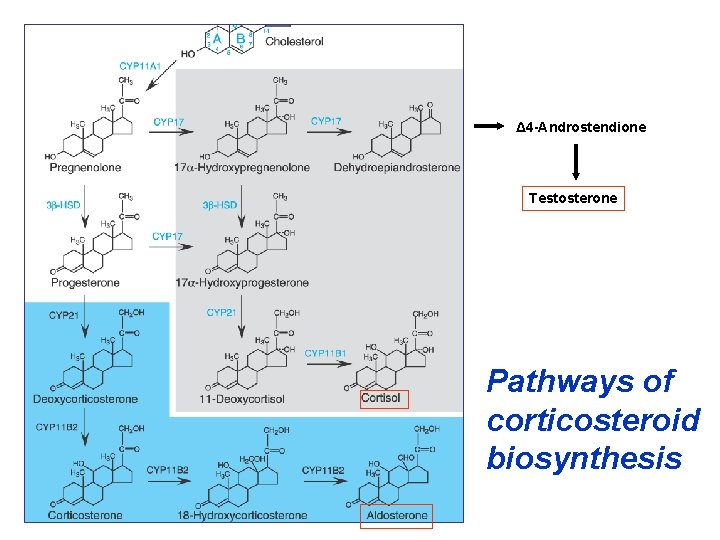
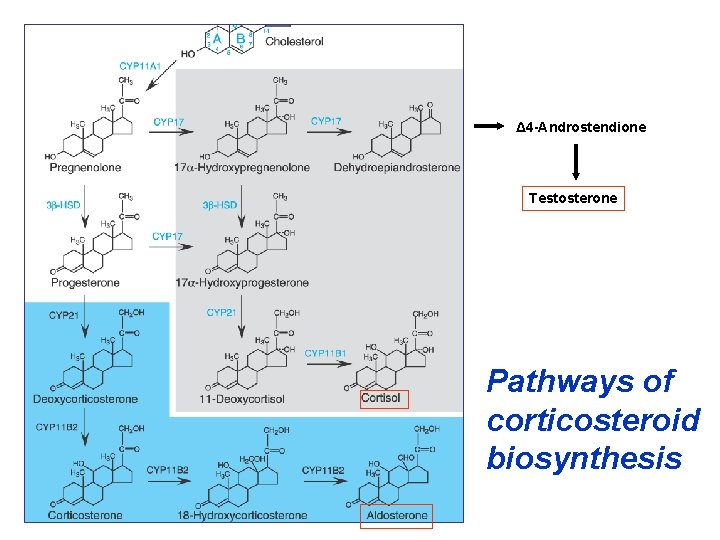
Δ 4 -Androstendione Testosterone Pathways of corticosteroid biosynthesis
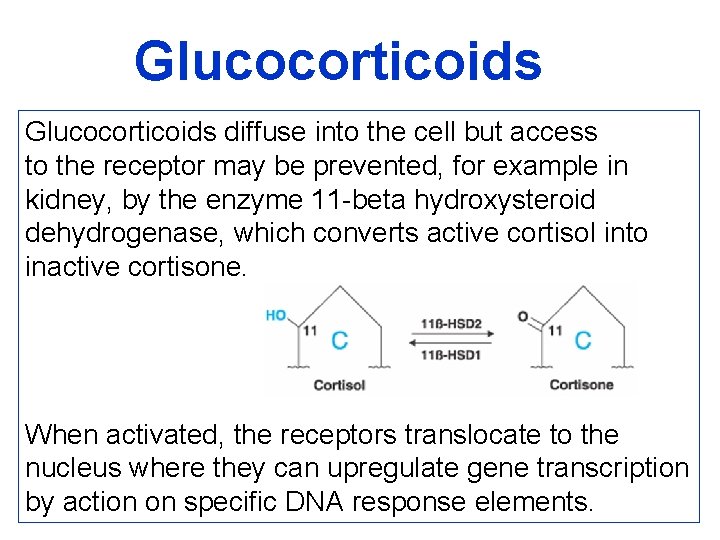
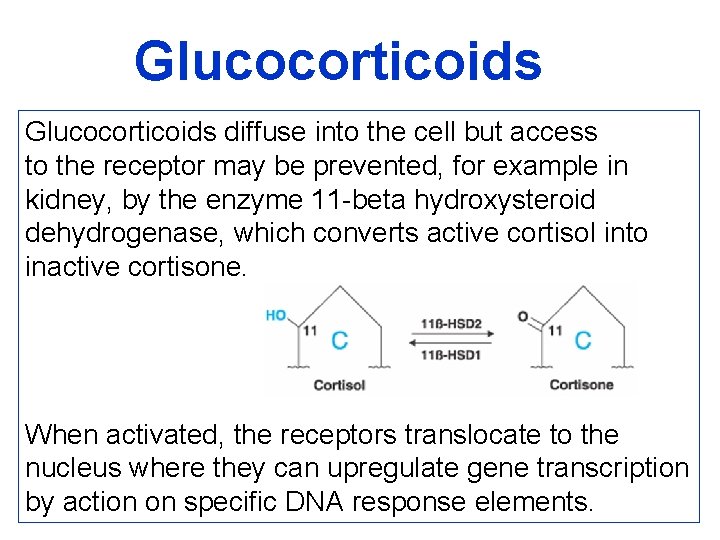
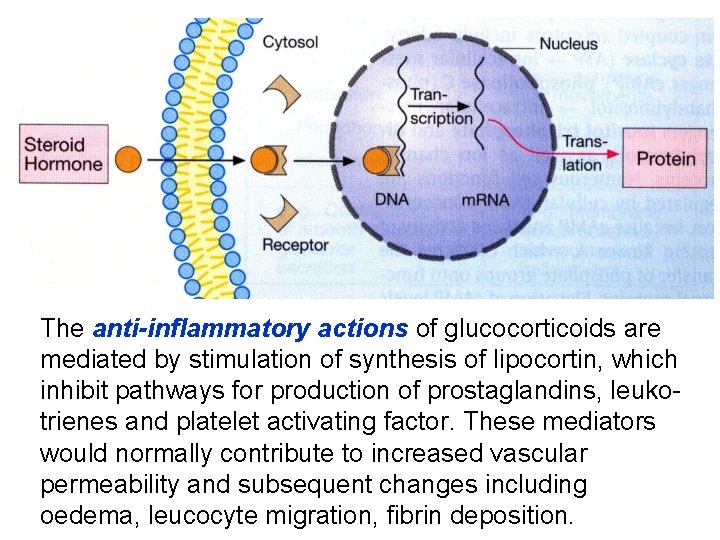
Glucocorticoids diffuse into the cell but access to the receptor may be prevented, for example in kidney, by the enzyme 11 -beta hydroxysteroid dehydrogenase, which converts active cortisol into inactive cortisone. When activated, the receptors translocate to the nucleus where they can upregulate gene transcription by action on specific DNA response elements.
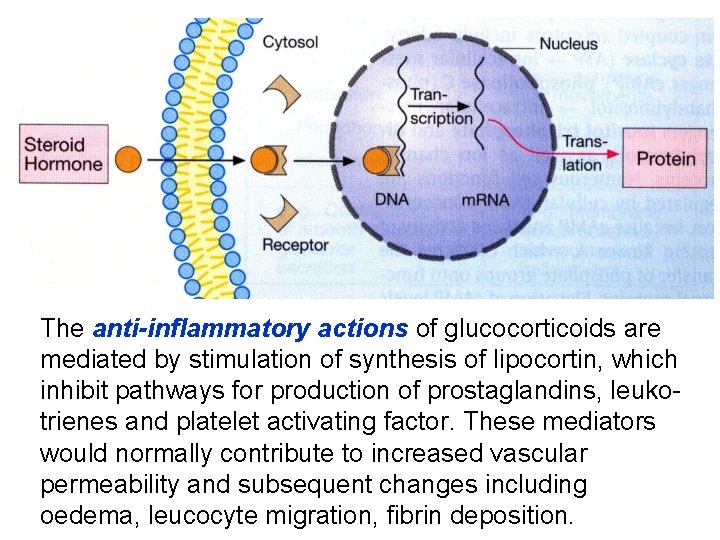
The anti-inflammatory actions of glucocorticoids are mediated by stimulation of synthesis of lipocortin, which inhibit pathways for production of prostaglandins, leukotrienes and platelet activating factor. These mediators would normally contribute to increased vascular permeability and subsequent changes including oedema, leucocyte migration, fibrin deposition.


ACTIONS OF HYDROCORTISONE The effects of hydrocortisone will be described as a basic glucocorticoid hormone. There is a distinction between replacement therapy (physiological effects) and the higher doses of pharmacotherapy. On inorganic metabolism (mineralocorticoid effects): increased retention of sodium by the renal tubule, and increased potassium excretion in the urine.
On organic metabolism (glucocorticoid effects): • Carbohydrate metabolism: gluconeogenesis is increased and peripheral glucose utilization (transport across cell membranes) may be decreased (insulin antagonism) so that hyperglycaemia and sometimes glycosuria result. Latent diabetes becomes overt. • Protein metabolism: anabolism (conversion of amino acids to protein) is decreased but catabolism continues unabated or even faster, so that there is a negative nitrogen balance with muscle wasting. Osteoporosis (reduction of bone protein matrix) occurs, growth slows in children, the skin atrophies and this, with increased capillary fragility, causes bruising and striae.
Healing of peptic ulcers or of wounds is delayed. • Fat deposition: this is increased on shoulders, face and abdomen. • Inflammatory response is depressed; corticosteroids can be a source of danger in infections by limiting useful protective inflammation. Neutrophil and macrophage function are depressed, including the release of chemical mediators and the effects of these on capillaries.
• Allergic responses are suppressed. The antigen-antibody interaction is unaffected, but its injurious inflammatory consequences do not follow. • Antibody production is reduced by heavy doses. • Lymphoid tissue is reduced (including leukaemic lymphocytes). • Renal excretion of urate is increased. • Blood eosinophils are reduced in number. • Euphoria or psychotic states may occur, perhaps due to CNS electrolyte changes. • Anti-vitamin D action.
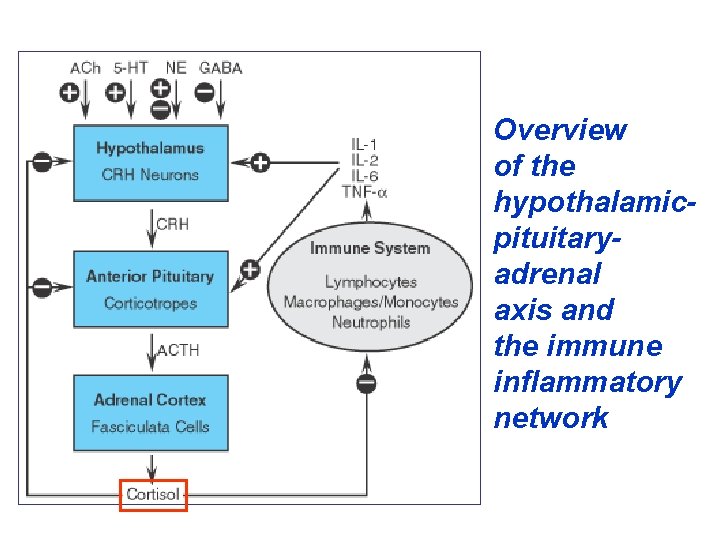
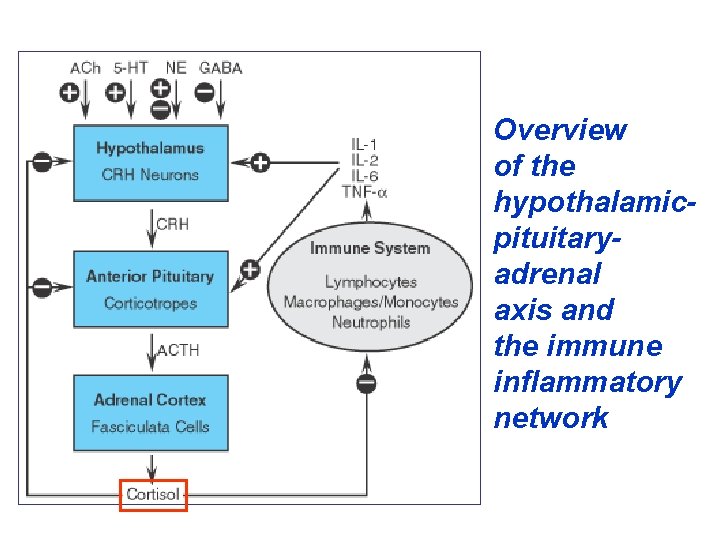
Overview of the hypothalamicpituitaryadrenal axis and the immune inflammatory network

• Reduction of hypercalcaemia chiefly where this is due to excessive absorption of calcium from the gut (sarcoidosis, vitamin D intoxication). • Urinary calcium excretion is increased and renal stones may form. • Growth reduction where new cells are being added (growth in children), but not where they are replacing cells as in adult tissues. • Suppression of hypothalamic/pituitary/adrenocortical feedback system (with delayed recovery) occurs with chronic use, so that abrupt withdrawal leaves the patient in a state of adrenocortical insufficiency.
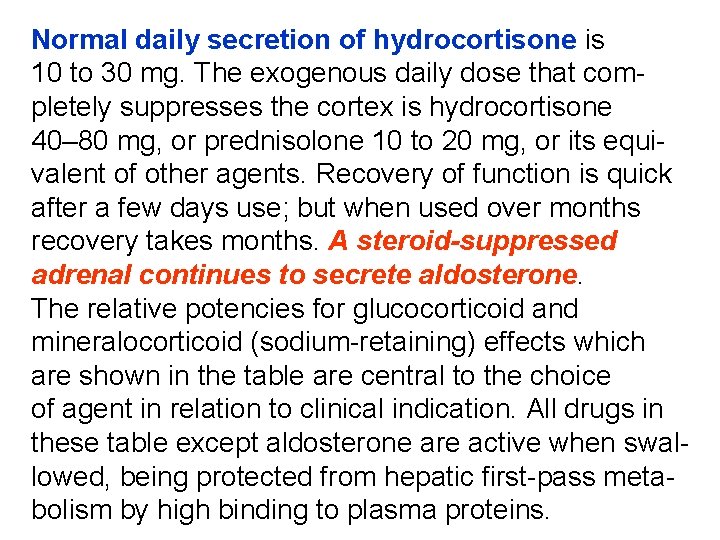
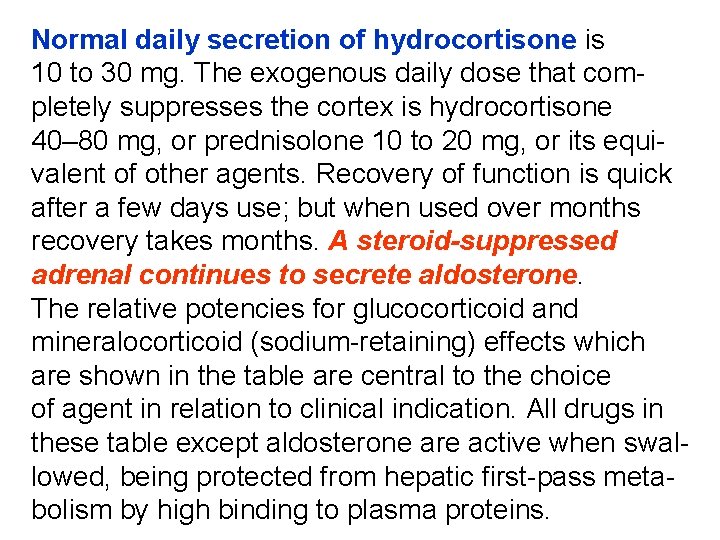
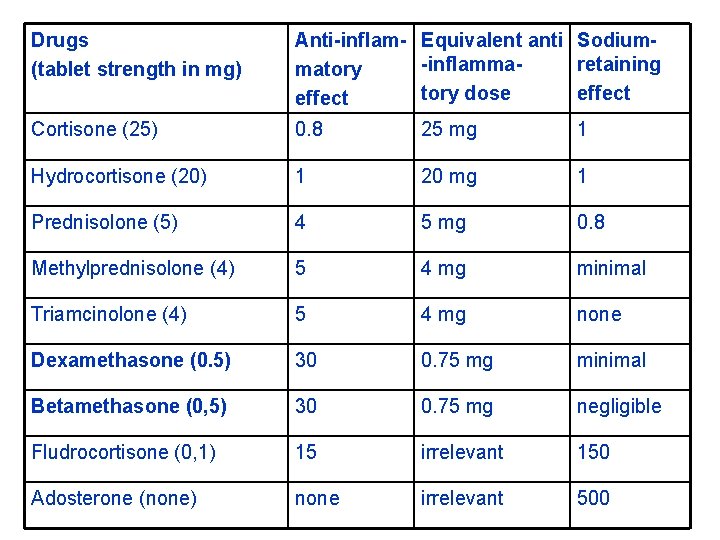
Normal daily secretion of hydrocortisone is 10 to 30 mg. The exogenous daily dose that completely suppresses the cortex is hydrocortisone 40– 80 mg, or prednisolone 10 to 20 mg, or its equivalent of other agents. Recovery of function is quick after a few days use; but when used over months recovery takes months. A steroid-suppressed adrenal continues to secrete aldosterone. The relative potencies for glucocorticoid and mineralocorticoid (sodium-retaining) effects which are shown in the table are central to the choice of agent in relation to clinical indication. All drugs in these table except aldosterone are active when swallowed, being protected from hepatic first-pass metabolism by high binding to plasma proteins.
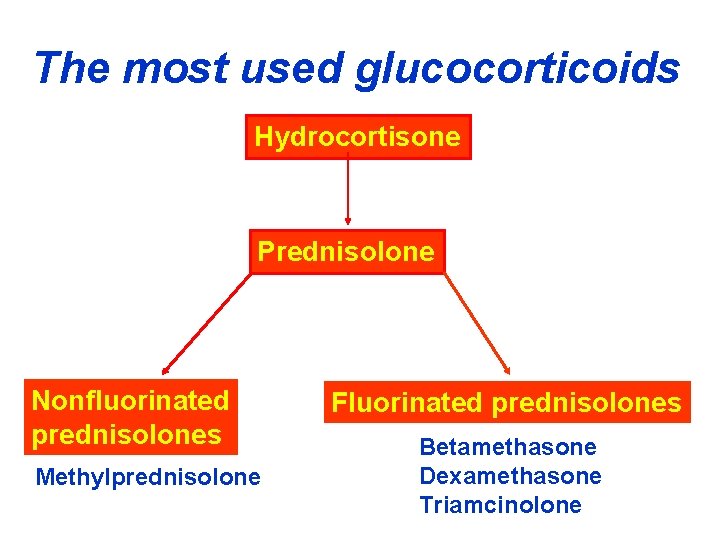
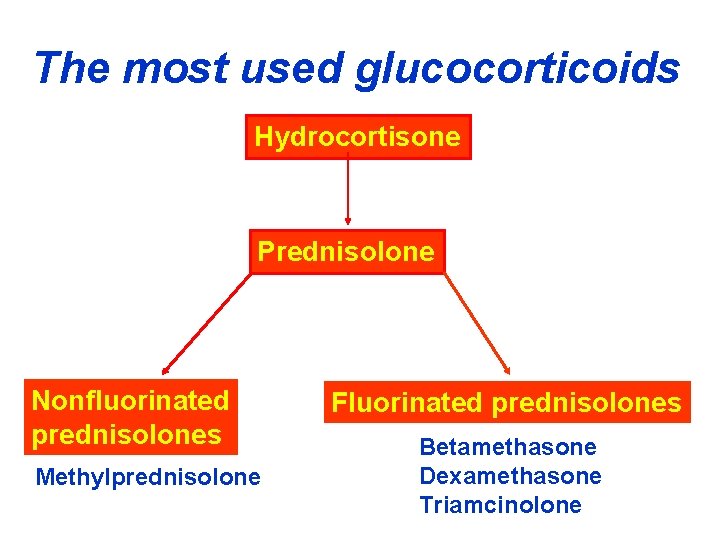
The most used glucocorticoids Hydrocortisone Prednisolone Nonfluorinated prednisolones Methylprednisolone Fluorinated prednisolones Betamethasone Dexamethasone Triamcinolone
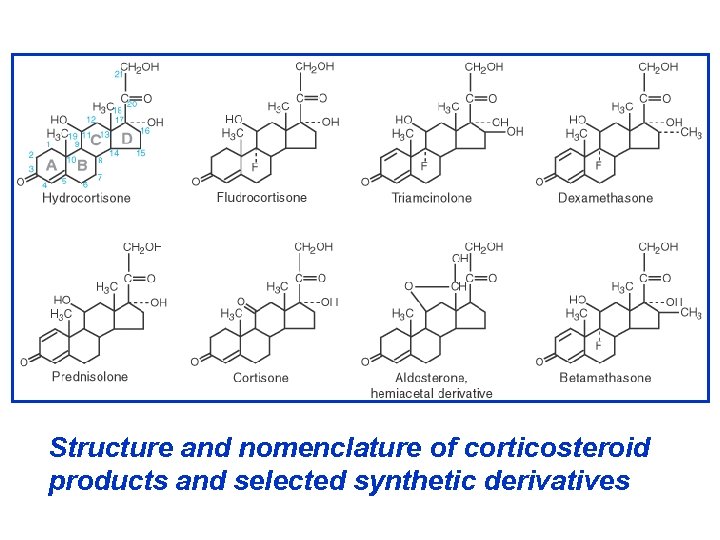
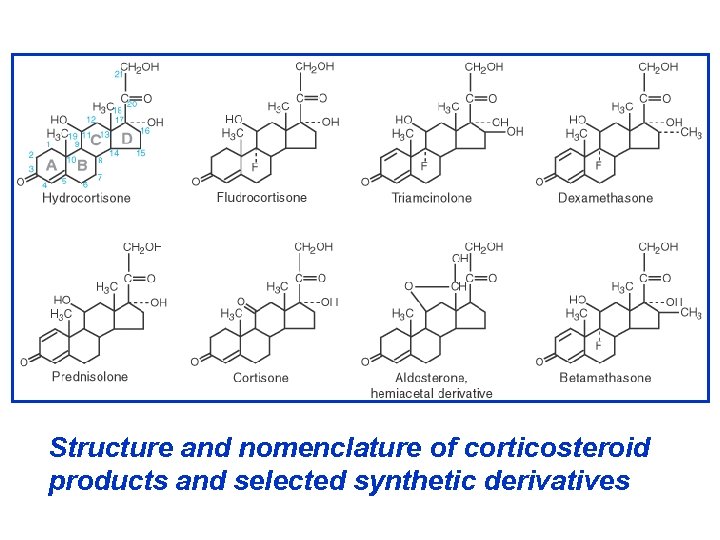
Structure and nomenclature of corticosteroid products and selected synthetic derivatives
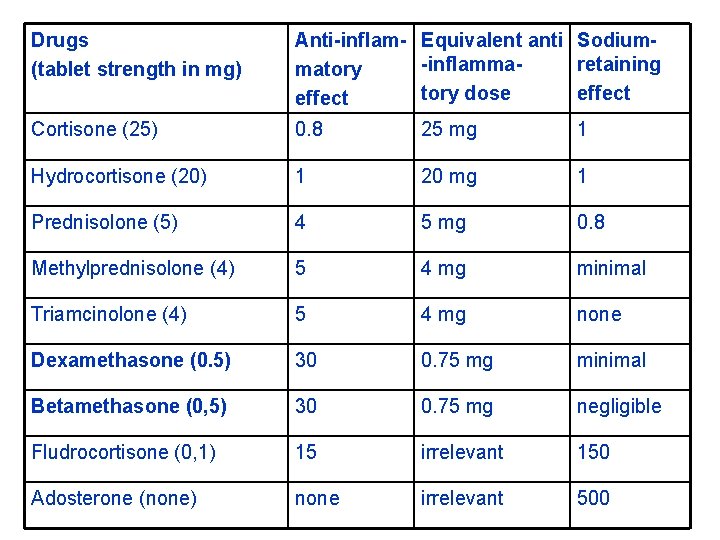
Drugs (tablet strength in mg) Anti-inflam- Equivalent anti Sodium-inflammaretaining matory dose effect Cortisone (25) 0. 8 25 mg 1 Hydrocortisone (20) 1 20 mg 1 Prednisolone (5) 4 5 mg 0. 8 Methylprednisolone (4) 5 4 mg minimal Triamcinolone (4) 5 4 mg none Dexamethasone (0. 5) 30 0. 75 mg minimal Betamethasone (0, 5) 30 0. 75 mg negligible Fludrocortisone (0, 1) 15 irrelevant 150 Adosterone (none) none irrelevant 500
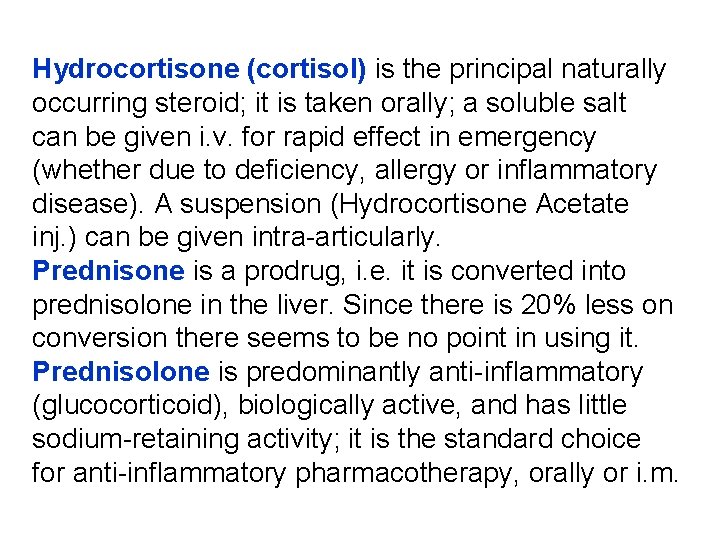
Hydrocortisone (cortisol) is the principal naturally occurring steroid; it is taken orally; a soluble salt can be given i. v. for rapid effect in emergency (whether due to deficiency, allergy or inflammatory disease). A suspension (Hydrocortisone Acetate inj. ) can be given intra-articularly. Prednisone is a prodrug, i. e. it is converted into prednisolone in the liver. Since there is 20% less on conversion there seems to be no point in using it. Prednisolone is predominantly anti-inflammatory (glucocorticoid), biologically active, and has little sodium-retaining activity; it is the standard choice for anti-inflammatory pharmacotherapy, orally or i. m.
Fluorinated glucocorticosteroids Triamcinolone has virtually no sodium retaining (mineralocorticoid) effect but has the disadvantage that muscle wasting may occasionally be severe and anorexia and mental depression may be more common at high dose. Dexamethasone and betamethasone are similar, powerful predominantly anti-inflammatory steroids. They are longer-acting than prednisolone and are used for therapeutic adrenocortical suppression.
Replasment glucocorticoid therapy • Acute adrenal insufficiency • Chronic adrenal insufficiency (Addisson’s disease) • Congenital adrenal hyperplasia (adrenogenital syndrome) Glucocorticoid pharmacotherapy for nonendocrine diseases Steroids are powerful drugs. They may cause dramatic improvement in many severe diseases as well as produce equally severe adverse effects if not properly used.
The use of steroids in nonendocrine disease is emperical and palliative, but may be live saving. The following general principles must be observed: • Single dose (even excessive) is not harmful. • Short courses (even high dose) are not likely to be harmful in the absense of contraindications. • Longterm use is potentially hazardous. • No abrupt withdrawal after a corticoid has been given for more 2 to 3 weeks: may precipitate adrenal insufficiency. • Infection, severe trauma or any stress during corticoid pharmacotherapy: increase the dose.
1. Rheumatoid arthritis: corticoids are on of the last resort drugs. 2. Osteoarthritis. Intrarticular injection of steroid is rare, but may be used to control an acute exacerbation. Repeated injections may cause joint destruction. 3. Rheumatic fever. Corticoids are used only in severe cases with myocarditis and CHF. 4. Collagen diseases: systemic lupus erythematosus, polyarteritis nodosa, dermatomyositis, nephrotic syndrom, glomerulonephritis. 5. Severe allergic reactions 6. Autoimmune diseases: autoimmune haemolytic anaemia, thrombocitopenia, active chronic hepatitis
7. Bronchial asthma 8. Eye diseases (as a eye drops or ointment) in allergic conjunctivitis, iridocyclitis, keratitis. 9. Skin diseases: Topical glucocorticosteroids are used in many exematus skin diseases 10. Intestinal diseases: ulcerative colitis, Crohn’s disease, coeliac disease 11. Cerebral edema due to tumours, tubercular meningitis etc. 12. Malignancies: acute lymphatic leukemia, Hodgkin’s disease and other lymphomas 13. Organ transplantations and skin allograft 14. To test adrenal-pituitary axis etc.
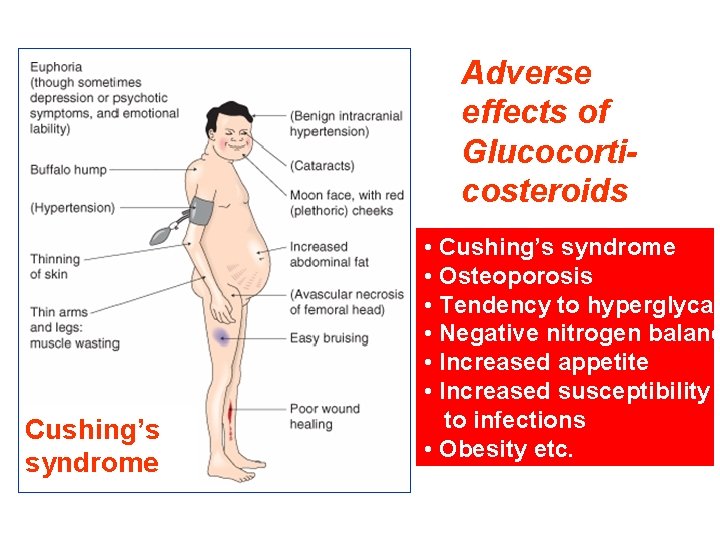
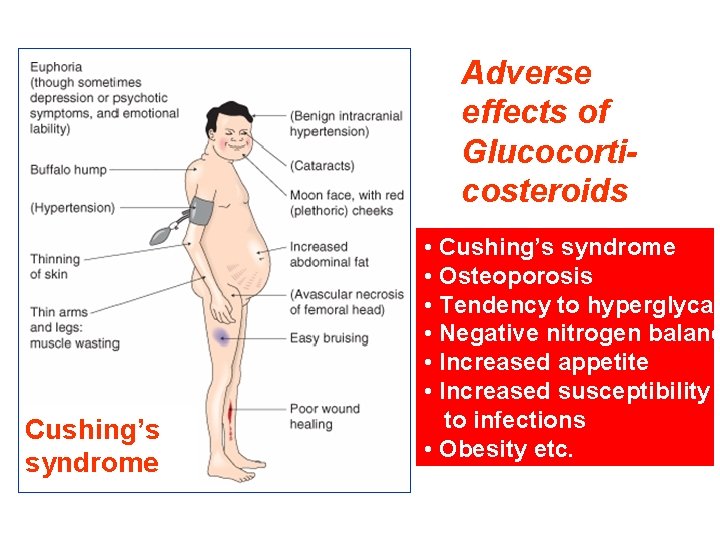
Adverse effects of Glucocorticosteroids Cushing’s syndrome • Cushing’s syndrome • Osteoporosis • Tendency to hyperglycae • Negative nitrogen balanc • Increased appetite • Increased susceptibility to infections • Obesity etc.
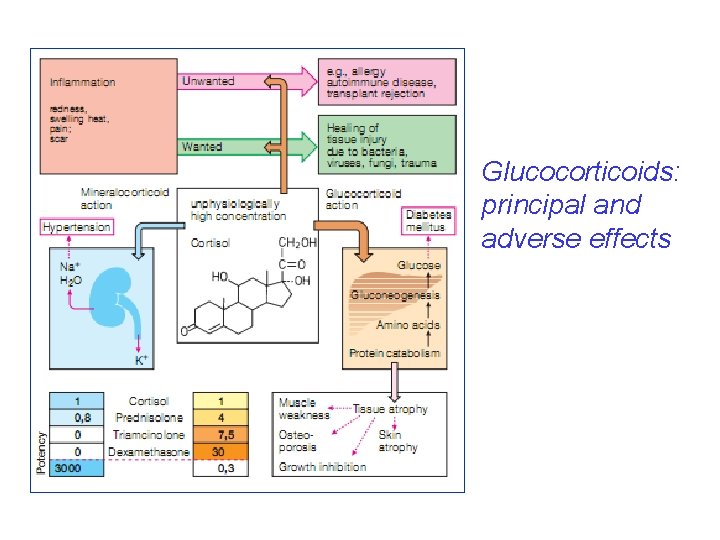
Glucocorticoids: principal and adverse effects
Contraindications • Peptic ulcer • Diabetes mellitus • Hypertension • Pregnancy (risk foetal defects) • Tuberculosis mycoses, virosis (including Herpes simplex keratitis) • Osteoporosis • Psychosis • Epilepsy • Chronic heart failure • Renal failure
Mineralcorticoids Aldosterone (t 1/2 20 min), the principal natural salt retaining hormone, has been used i. m. in acute adrenal insufficiency. After oral administration, it is rapidly inactivated in the first pass through the liver but has no place in routine therapeutics, as fludrocortisone is as effective and is active orally.
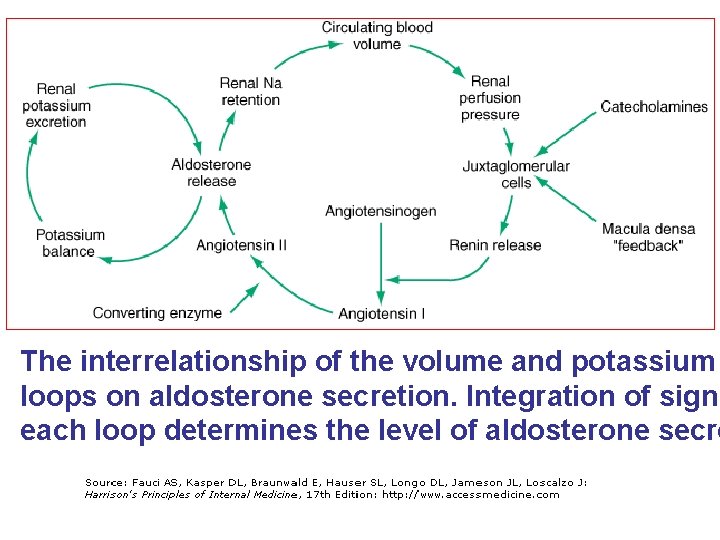
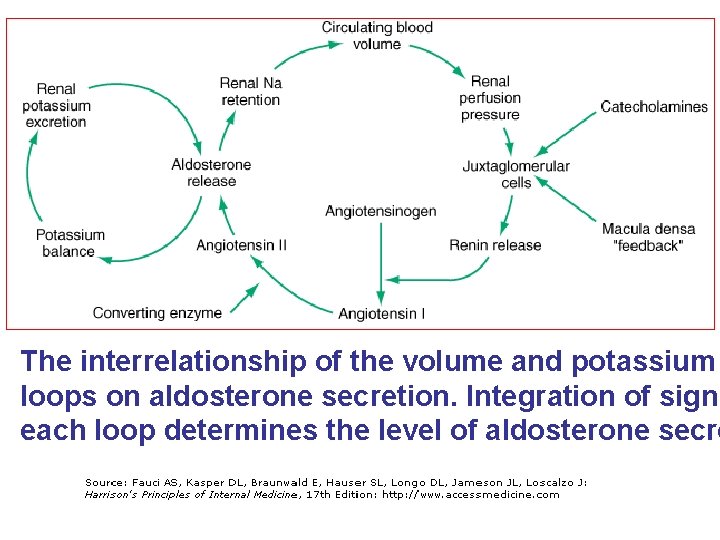
The interrelationship of the volume and potassium loops on aldosterone secretion. Integration of signa each loop determines the level of aldosterone secre
Fludrocortisone has a very great sodium-retaining effect in relation to its anti-inflammatory action and only at high doses need the nonelectrolyte effects be considered. It is used to replace aldosterone where the adrenal cortex is destroyed (Addison's disease). Fludrocortisone is also the drug of choice in most patients with autonomic neuropathy, in whom volume expansion is easier to achieve than a sustained increase in vasoconstrictor tone. Much higher doses of fludrocortisone (0. 5 to 1. 0 mg) are required when the cause of hypotension is a saltlosing syndrome of renal origin, e. g. following an episode of interstitial nephritis.
Sex (gonadal) hormones and antagonists • Androgens and antiandrogens • Estrogens and antiestrogens • Progestins and antiprogestins • Hormonal contraceptives

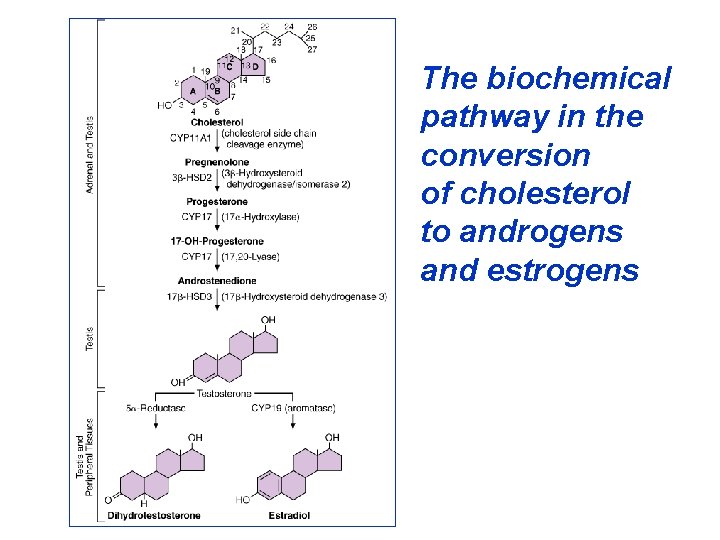
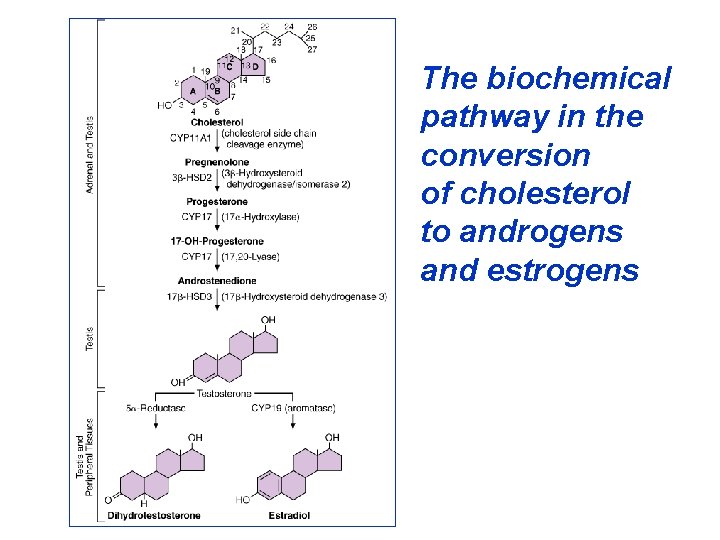
The biochemical pathway in the conversion of cholesterol to androgens and estrogens
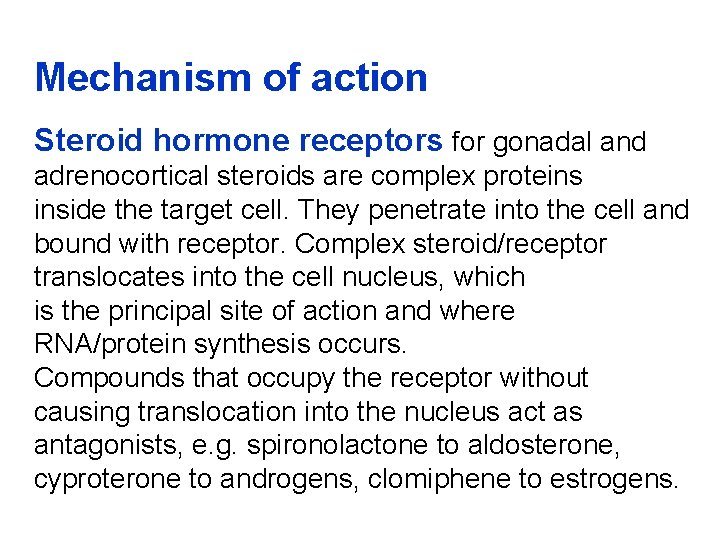
Mechanism of action Steroid hormone receptors for gonadal and adrenocortical steroids are complex proteins inside the target cell. They penetrate into the cell and bound with receptor. Complex steroid/receptor translocates into the cell nucleus, which is the principal site of action and where RNA/protein synthesis occurs. Compounds that occupy the receptor without causing translocation into the nucleus act as antagonists, e. g. spironolactone to aldosterone, cyproterone to androgens, clomiphene to estrogens.
Pharmacokinetics Steroid sex hormones are well absorbed through the skin. Most are subject to extensive hepatic metabolic inactivation (some so much that oral administration is ineffective or requires very large doses). There is some enterohepatic recirculation, especially of estrogen, and this may be interrupted by severe diarrhoea to cause loss of efficacy. There are some nonsteroid analogues that are more slowly metabolized. Sustained-release (depot) preparations are used. The hormones in the blood extensively bound to sex-hormone-binding globulin. The plasma t 1/2 relates to the duration of cellular action, which is implied in the recommended dosage schedules.
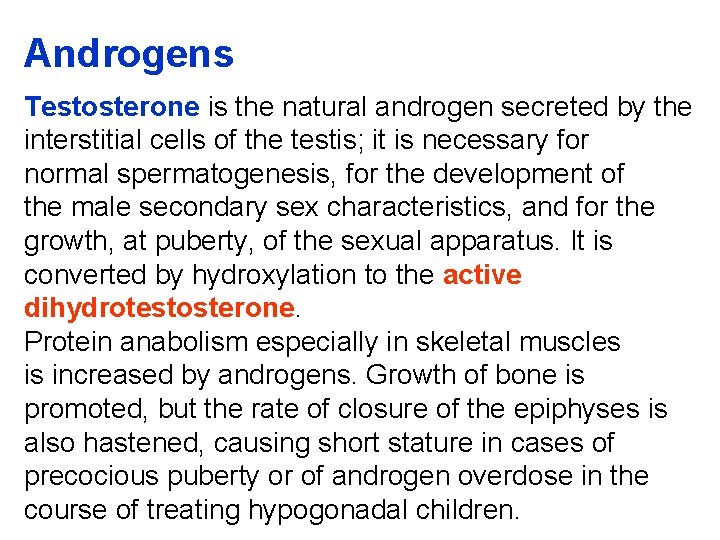
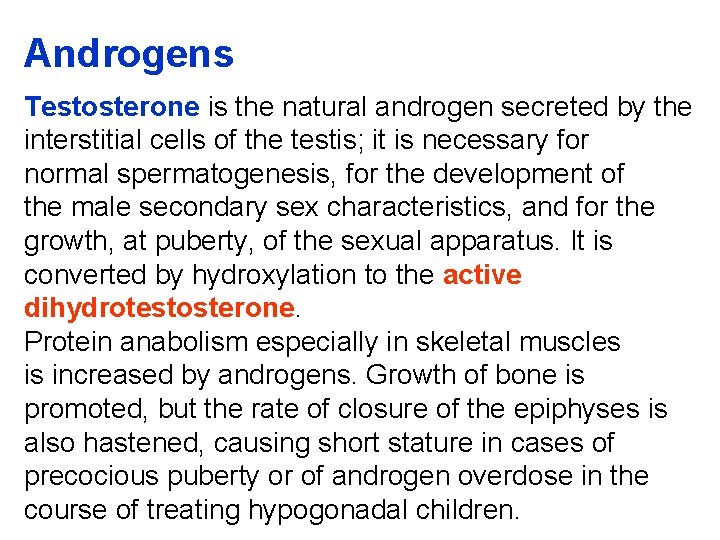
Androgens Testosterone is the natural androgen secreted by the interstitial cells of the testis; it is necessary for normal spermatogenesis, for the development of the male secondary sex characteristics, and for the growth, at puberty, of the sexual apparatus. It is converted by hydroxylation to the active dihydrotestosterone. Protein anabolism especially in skeletal muscles is increased by androgens. Growth of bone is promoted, but the rate of closure of the epiphyses is also hastened, causing short stature in cases of precocious puberty or of androgen overdose in the course of treating hypogonadal children.
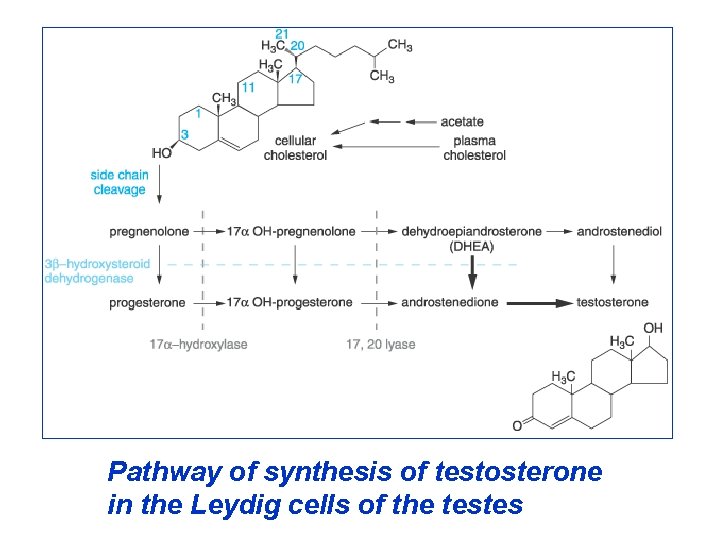
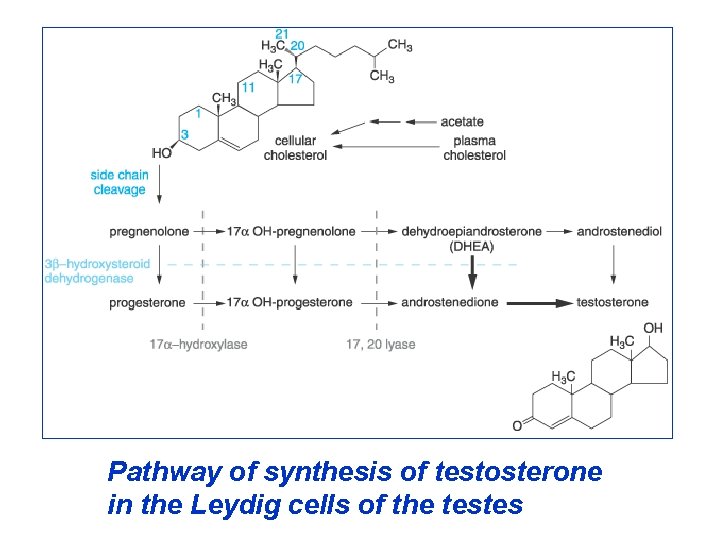
Pathway of synthesis of testosterone in the Leydig cells of the testes
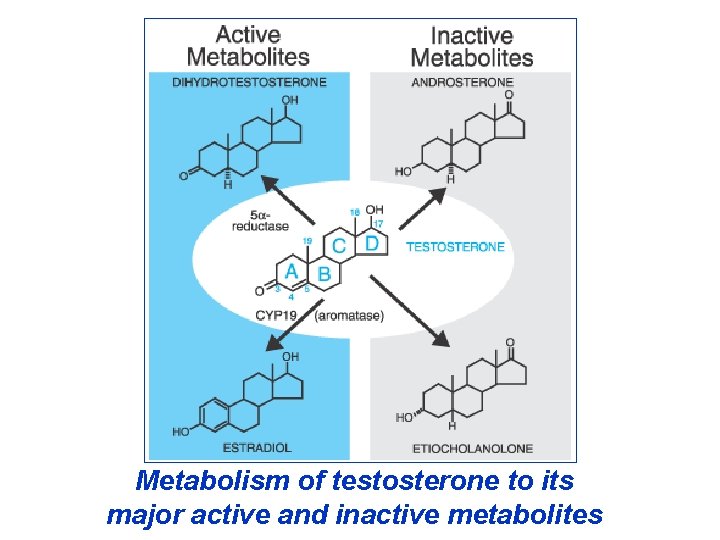
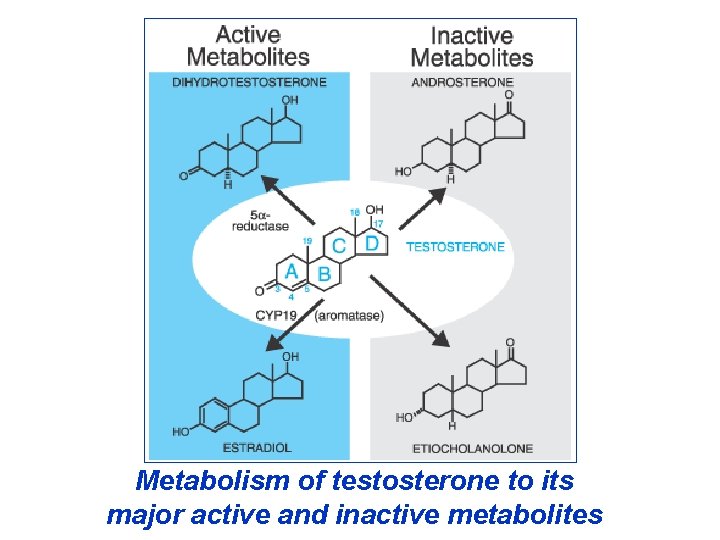
Metabolism of testosterone to its major active and inactive metabolites
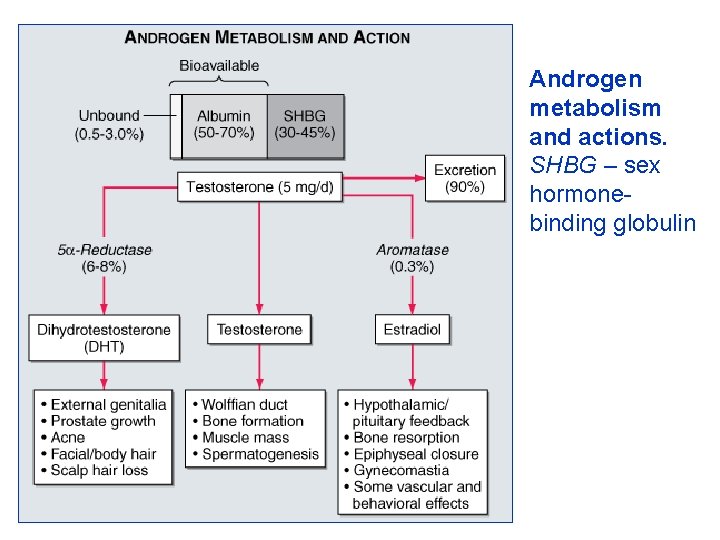
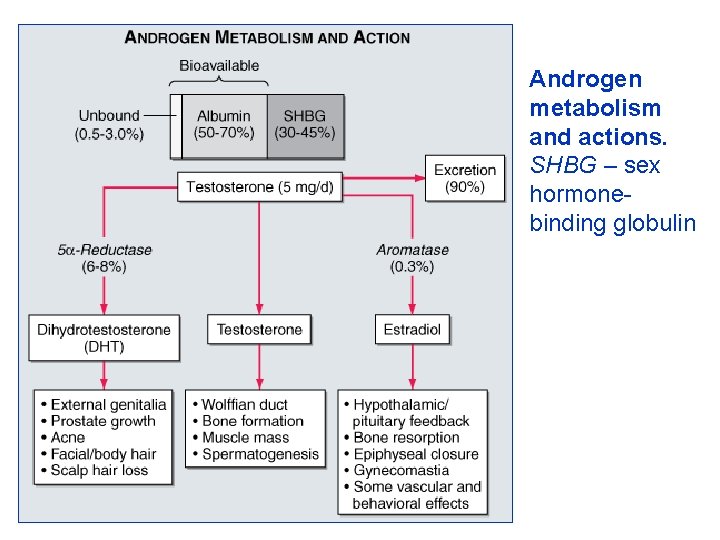
Androgen metabolism and actions. SHBG – sex hormonebinding globulin
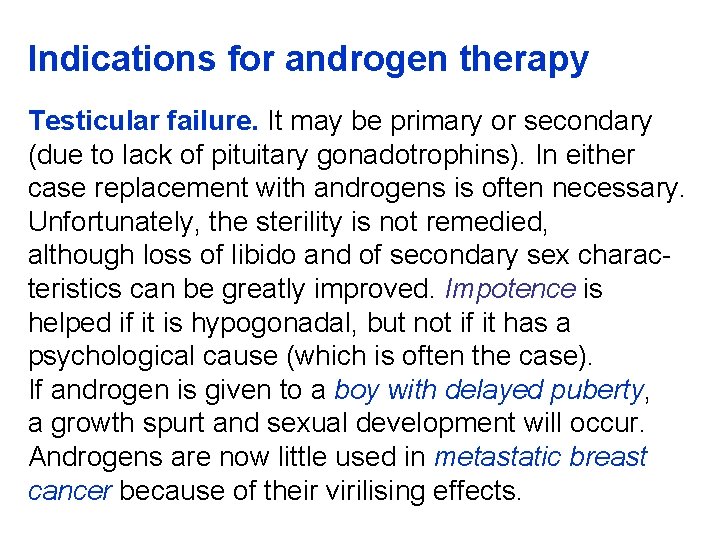
Indications for androgen therapy Testicular failure. It may be primary or secondary (due to lack of pituitary gonadotrophins). In either case replacement with androgens is often necessary. Unfortunately, the sterility is not remedied, although loss of libido and of secondary sex characteristics can be greatly improved. Impotence is helped if it is hypogonadal, but not if it has a psychological cause (which is often the case). If androgen is given to a boy with delayed puberty, a growth spurt and sexual development will occur. Androgens are now little used in metastatic breast cancer because of their virilising effects.
Androgen preparations Testosterone has extensive hepatic first-pass metabolism. It may be given orally or as i. m. depot injections. Mesterolone provides oral therapy. Antiandrogens (androgen antagonists) Estrogens and progestogens are physiological antagonists to androgens. But compounds which compete selectively for androgen receptors have been made. Cyproterone is a derivative of progesterone. It is used for reducing male hypersexuality and in prostatic cancer and severe female hirsutism.
A formulation of cyproterone plus ethinylestradiol (Diane®) is offered for treatment of severe female hirsutism too as well as for severe acne in women; this preparation acts as an oral contraceptive too. Cyproterone causes hepatomas in rats. Cyproterone is unsuitable for male contraception. Flutamide and bicalutamide are nonsteroidal antiandrogens for use in conjunction with the gonadorelins (e. g. goserelin) in the treatment of prostatic carcinoma. Finasteride inhibits conversion of testosterone to dihydrotestosterone. It has antiandrogen activity in tissues where dihydrotestosterone is the principal androgen: this makes it a useful drug in the treatment of benign prostatic hyperplasia.

Spironolactone also has antiandrogen activity and may help hirsutism in women. Androgen secretion may be diminished by continued use of a gonadorelin (LH-RH) analogue. Ketoconazole (antifungal drug) inhibits androgen synthesis and may be used in prostatic carcinoma. Anabolic steroids Androgens are effective protein anabolic agents, but their clinical use for this purpose is limited by virilisation of women. Attempts made to separate anabolic from androgenic action have been partially successful. All anabolic steroids have also androgenic effects.
Anabolic steroids (Nandrolone) may no longer used in osteoporosis. They benefit some patients with aplastic anaemia. Hereditary angioedema may be prevented. Anabolic steroids can prevent the calcium and nitrogen loss in the urine that occurs in patients bedridden for a long time and they have therefore been used in the treatment of some severe fractures. The use of anabolic steroids in conditions of general wasting despite nutritional support may be justifiable in extreme debilitating disease, such as severe ulcerarive colitis, and after major surgery. In the later stages of malignant disease they make the patient feel and look less wretched. Their general use as tonics is scandalous, as is their use in sport.
Estrogens Estrone and estradiol are both natural estrogens. Estrogens are responsible for the normal development of the female genital tract, of the breast and of the female secondary sex characteristics. The pubertal growth spurt is less marked in females than in males, probably because estrogens have less protein anabolic action than do androgens, although they are as effective in promoting closure of epiphyses.
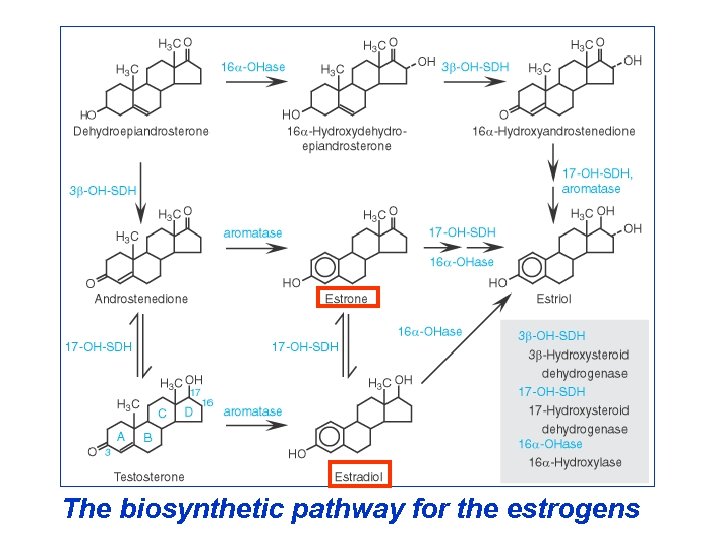
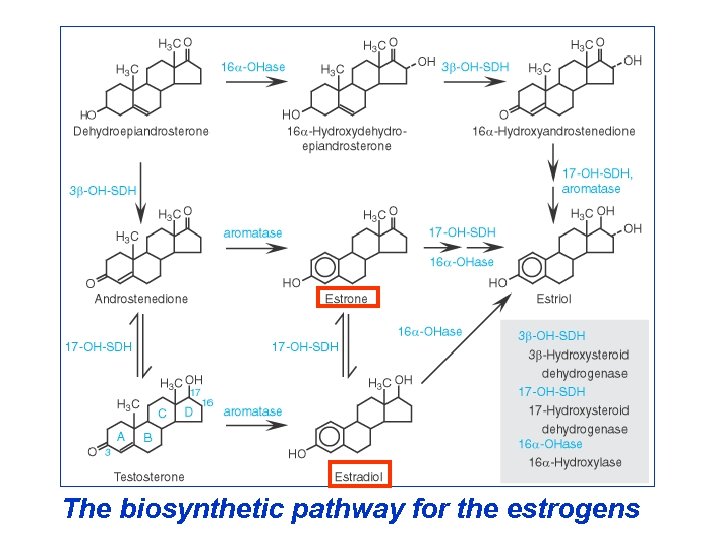
The biosynthetic pathway for the estrogens
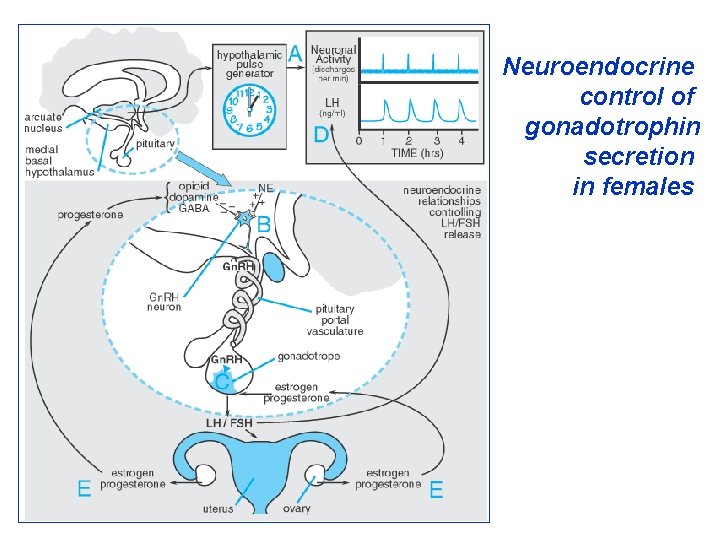
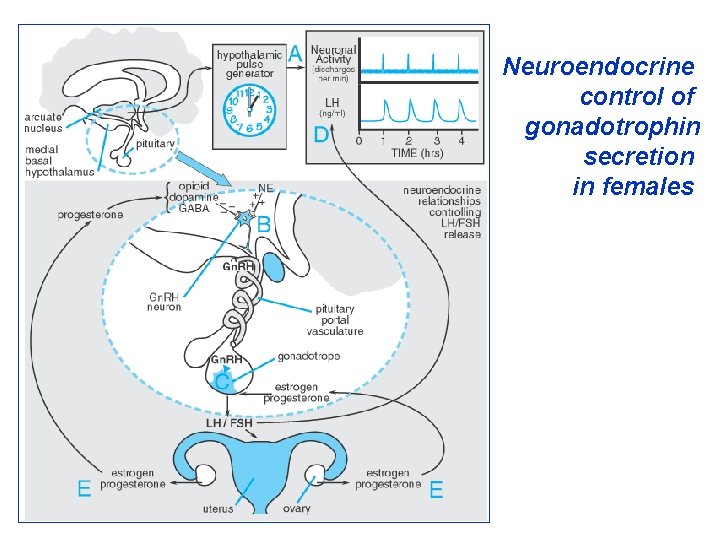
Neuroendocrine control of gonadotrophin secretion in females
Blood estrogen concentrations must be above a critical level for the maintenance of both proliferative and (together with progesterone) secretory phases of the uterine endometrium. If the estrogen level falls too low uterine bleeding follows. Estrogens are necessary for the maintenance of normal pregnancy and for the accompanying breast hyperplasia. The vagina is more sensitive to estrogens than is the endometrium.
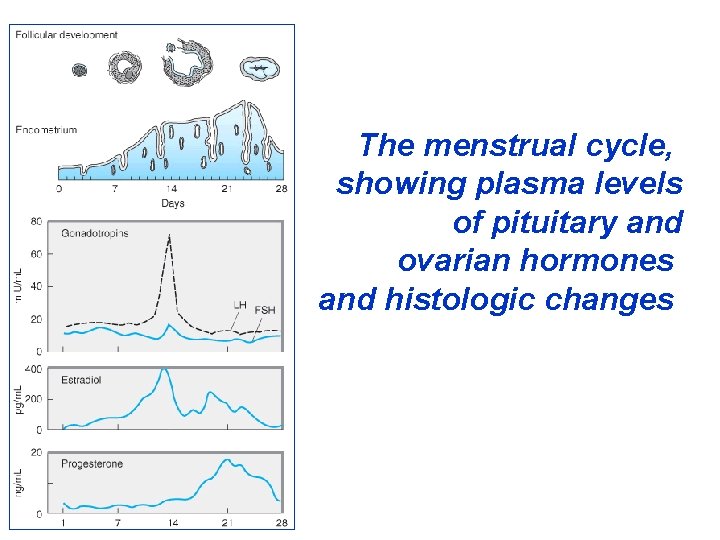
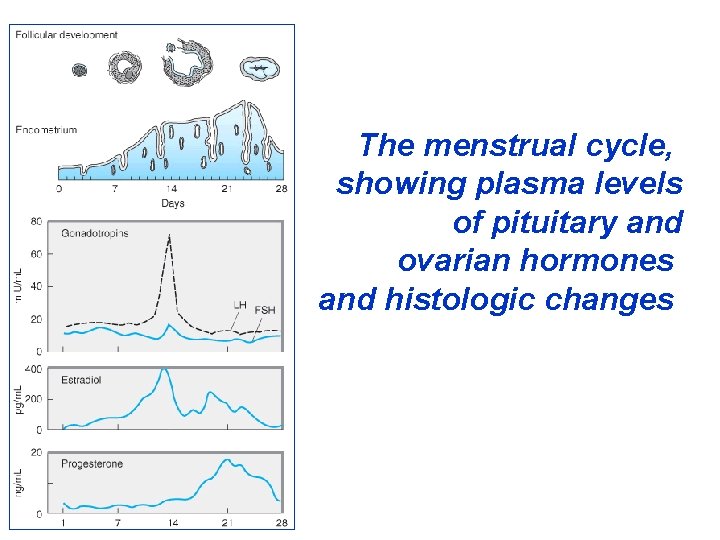
The menstrual cycle, showing plasma levels of pituitary and ovarian hormones and histologic changes
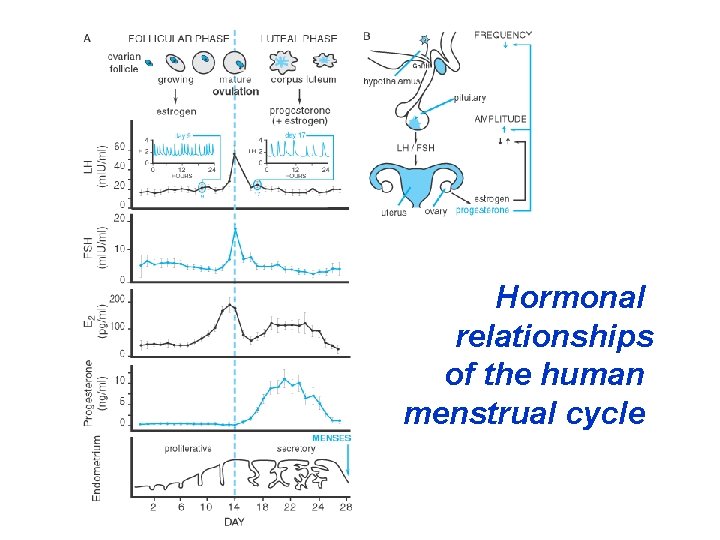
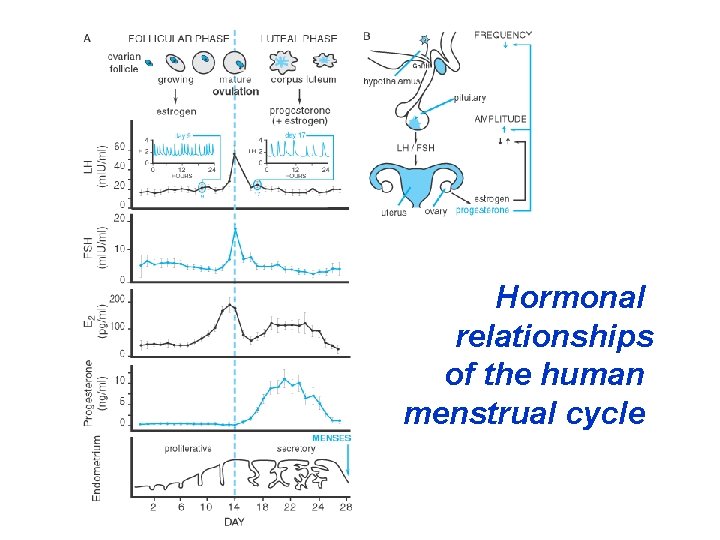
Hormonal relationships of the human menstrual cycle
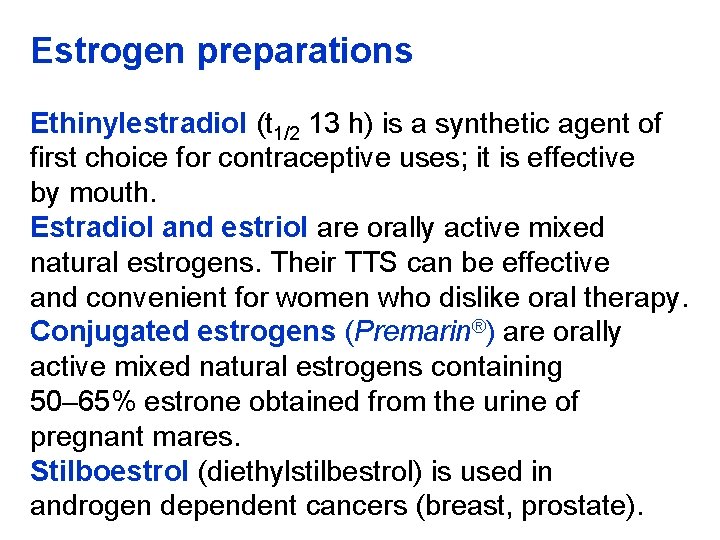
Estrogen preparations Ethinylestradiol (t 1/2 13 h) is a synthetic agent of first choice for contraceptive uses; it is effective by mouth. Estradiol and estriol are orally active mixed natural estrogens. Their TTS can be effective and convenient for women who dislike oral therapy. Conjugated estrogens (Premarin®) are orally active mixed natural estrogens containing 50– 65% estrone obtained from the urine of pregnant mares. Stilboestrol (diethylstilbestrol) is used in androgen dependent cancers (breast, prostate).
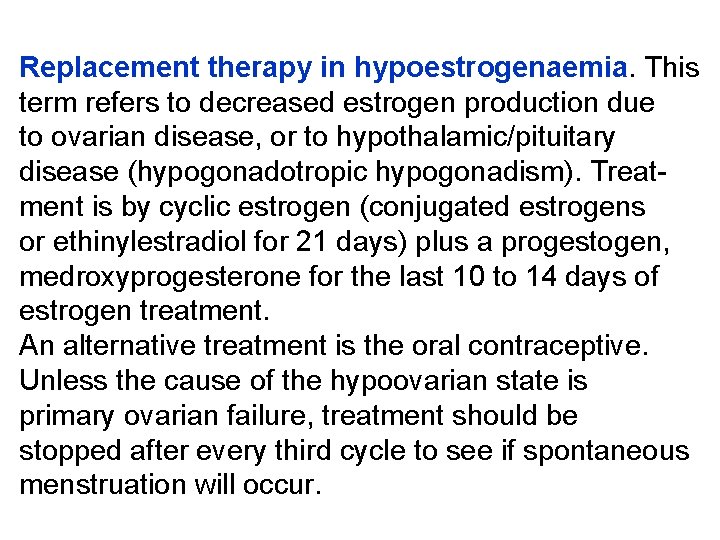
Replacement therapy in hypoestrogenaemia. This term refers to decreased estrogen production due to ovarian disease, or to hypothalamic/pituitary disease (hypogonadotropic hypogonadism). Treatment is by cyclic estrogen (conjugated estrogens or ethinylestradiol for 21 days) plus a progestogen, medroxyprogesterone for the last 10 to 14 days of estrogen treatment. An alternative treatment is the oral contraceptive. Unless the cause of the hypoovarian state is primary ovarian failure, treatment should be stopped after every third cycle to see if spontaneous menstruation will occur.
Postmenopausal hormone replacement therapy (HRT). It is the use of estrogen treatment to reverse or prevent problems due to the loss of ovarian hormone secretion after the menopause, whether physiological or induced. The tissues sensitive to estrogen include brain, bone, skin, cardiovascular and genitourinary system. The two aims of HRT are: (1) To reduce the everyday symptoms of estrogen loss: hot flushes, sleeplessness, lethargy and depression, vaginal dryness. (2) To prevent the long-term complications associated with estrogen deficiency: osteoporotic fractures and coronary heart disease.
All types of HRT (estrogen with or without progestogen) are effective in reducing the hot flushes experienced by more than 50% of postmenopausal women. The benefit is most during the first year of treatment when 80% of women report a reduced likelihood of flushes. The other major value from HRT is the relief of vaginal dryness. Vaginal administration (as a cream, ring, pessary or tablet) is the most effective route for treatment of these symptoms. There are three types of regimen used for HRT: (1) Women without uterus take continuous estrogen alone.
(2) Women require estrogen combined with progestogen to prevent endometrial proliferation. a) In the “sequential” regimen, women take estrogen without break, and add a progestogen from approximately the 14 th to 28 th day of each cycle. The first course is started on the 1 st day of mentruation (if present), and 28 -day cycles of treatment follow thereafter without interval. b) In the “continuous” regimen, appropriate only for women who have been amenorrhoeic for more than one year, fixed dose combinations of estrogen and progestogen are taken without a break.
A popular alternative to estrogen therapy is the drug tibolone (Livial®), which is a synthetic steroid with weak estrogenic, progestogenic androgenic properties. It is administered as a daily oral dose of 2. 5 mg to suppress vasomotor symptoms and to prevent postmenopausal osteoporosis. The main adverse effect is vaginal bleeding, which needs investigation if persistent. Vasomotor menopausal symptoms may occasionally be helped by low doses of clonidine.
Adverse effects of HRT The commonest reasons for withdrawal are irregular or withdrawal bleeding and breast pain. The more serious complications are venous thromboembolism and cancer of the endometrium or breast. These risks are small in absolute terms, particularly so for the risks of cancer during the first 5 years of treatment. The risk of gallstones may be increased up to 2 -fold. The effect of estrogens is on lipid balance favourable, but the addition of a progestin (gestodene or desogestrel) reverses the balance.
Estrogen pharmacoterapy – indications: • Contraception • Menstrual disorders • Senile vaginitis • Inhibition of laction (but no longer) • Androgen-depenent carcinoma (prostate cancer) • To reduce sexual urge in men • Epistaxis in recurrent cases (e. g. teleangiectasia) NB: Atrophic rhinitis may benefit, as also may acne.
Antiestrogens Selective antagonists of the estrogen receptor are used either to induce gonadotrophin release in anovulatory infertility, or to block stimulation of estrogen-receptor-positive carcinomas of the breast. Clomiphene is structurally related to stilbestrol. It is a partial agonist. Clomiphene blocks hypothalamic estrogen receptors so that the negative feedback of natural estrogens is prevented and the pituitary responds by increased secretion of gonadotrophins, which may induce ovulation. Clomiphene is administered during the early follicular phase of the menstrual cycle.
Tamoxifen is a nonsteroid competitive estrogen antagonist on target organs. Although available for anovulatory infertility (20 mg daily on days 2, 3, 4 and 5 of the cycle) its main use now is in the treatment of estrogen-dependent breast cancer. Treatment with tamoxifen delays the growth of metastases and increases survival; if tolerated it should be continued for 5 years. Tamoxifen is also the hormonal treatment of choice in women with estrogen-receptor-positive metastatic breast cancer. Approximately 60% of such patients respond to initial hormonal manipulation, whereas less than 10% of estrogenreceptor-negative tumours respond.
Progesterone and progestins (progestogens) Progesterone (t 1/2 5 min) is produced by the corpus luteum and converts the uterine epithelium from the proliferative to the secretory phase. It is necessary for successful implantation of the ovum, and is essential throughout pregnancy in the last two-thirds of which it is secreted in large amounts by the placenta. It acts particularly on tissues that are sensitized by estrogens. Some synthetic progestogens are less selective, having varying estrogenic androgenic activity, and these may inhibit ovulation, though not very reliably.
Progestogens are of two principal kinds: • Progesterone and its derivatives: dydrogesterone, hydroxyprogesterone, medroxyprogesterone (t 1/2 28 h), etc. • Testosterone derivatives: norethisterone and its prodrug ethynodiol (t 1/2 10 h), levonorgestrel, desogestrel, gestodene, gestronol, norgestimate. Megestrol is used only in cancer; it causes tumours in the breasts of beagle dogs. Clinical uses The clinical uses of progestational agents are ill-defined, apart from contraception, the menopause and postmenopausal HRT.
Other possible uses include • menstrual disorders, e. g. menorrhagia, endometriosis, dysmenorrhoea and premenstrual syndrome (doubtful efficacy) • breast and endometrial cancer. Available progestogens (some used only in combined formulations) include: • oral: norethisterone, dydrogesterone, gestodene, desogestrel, levonorgestrel, megestrol, medroxyprogesterone • suppositories or pessaries: progesterone • injectable: progesterone, hydroxyprogesterone, medroxyprogesterone.
Adverse effects of prolonged use of progestins include virilisation, rised blood pressure and adverse trend in blood lipids. Gestodene, desogestrel and norgestimate may have less affinity for androgen receptors and therefore less unfavourable effect on blood lipids; however the first two of these may have a higher risk of thrombosis. Antiprogestogens Mifepristone is a pure competitive antagonist at progesterone and glucocorticoid receptors. Clinical trials of oral use in hospital outpatients have shown it to be safe and effective in terminating pregnancy.
Other progesterone derivatives Danazol is a derivative of the progestogen – ethisterone. It has partial agonist androgen activity and is described as an “impeded” androgen; it has little progestogen activity. It is a relatively selective inhibitor of pituitary gonadotrophin secretion (LH, FSH) affecting the surge in the mid-menstrual cycle more than basal secretion. This reduces ovarian function, which leads to atrophic changes in endometrium. In males it reduces spermatogenesis. Androgenic unwanted effects occur in women (acne, hirsutism and, rarely, enlargement of the clitoris). It is chiefly used for: endometriosis, fibrocystic, mastitis, gynaecomastia, precocious puberty, menorrhagia and hereditary angioedema.
Hormonal contraception in women comprises: • Estrogen and progestogen (combined and phased administration) • Progestogen alone (e. g. Levonorgestrel) Estrogens alone are not completely reliable. At the necessary dose, they can also cause thromboembolism and endometrial cancer.
Progestogens used alone inhibit ovulation in up to 40% of cycles, render cervical mucus less easily penetrable by sperm and induce a premature secretory change in the endometrium so that implantation does not occur. There is liable to be break-through bleeding and some are a cause of rised blood pressure and an adverse trend in blood lipids and arterial disease. An appropriate dose of estrogen + progestogen gives excellent reliability with good menstrual cycle control. The following account applies to these combined preparations.
Combined hormonal contraceptives are conveniently started on the first day of the cycle (first day of menstruation) and continued for 21 days (this is immediately effective, inhibiting the first ovulation). It is followed by a period of 7 days when no pill is taken, and during which bleeding usually occurs. Thereafter, regardless of bleeding, a new 21 -day course is begun, and so on, i. e. active tablets are taken daily for 3 weeks out of 4. For easy compliance, some combined pills are packaged so that the woman takes one tablet every day without interruption (21 active then 7 dummy).
The pill should be taken about the same time (to within 12 hours) every day to establish a routine. The monthly bleeds that occur 1– 2 days after the cessation of active hormone administration are hormone withdrawal bleeds not natural menstruation. They are not an essential feature of oral contraception, but women are accustomed to monthly bleeds and they provide monthly reassurance of the absence of pregnancy. Numerous field trials have shown that progestinestrogen combinations, if taken precisely as directed, are the most reliable reversible contraceptive known.
Combined oral contraceptives are defined as 2 nd or 3 rd generation by the progestogen component (1 st generation progestogens are obsolete). Those containing a fixed amount of an estrogen and a progestin in each active tablet are termed “monophasic”. Other pills employ variable ratios between estrogen and progestin, in 2 (biphasic) or 3 (triphasic) periods within the menstrual cycle. The dose of progestin is low at the beginning and higher at the end, the estrogen remaining either constant or rising slightly in mid-cycle.
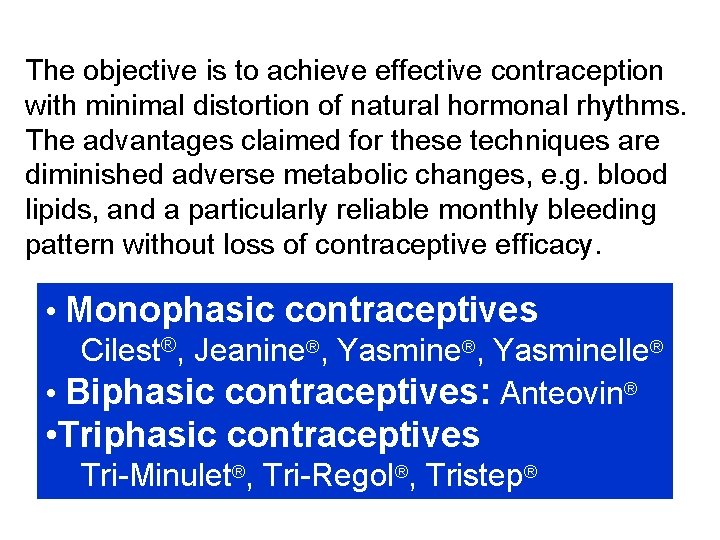
The objective is to achieve effective contraception with minimal distortion of natural hormonal rhythms. The advantages claimed for these techniques are diminished adverse metabolic changes, e. g. blood lipids, and a particularly reliable monthly bleeding pattern without loss of contraceptive efficacy. • Monophasic contraceptives Cilest®, Jeanine®, Yasminelle® • Biphasic contraceptives: Anteovin® • Triphasic contraceptives Tri-Minulet®, Tri-Regol®, Tristep®
It is now appreciated that the earlier preparations had much more estrogen than was necessary for efficacy. It seems probable that 20 mcg is about the limit below which serious loss of efficacy can be expected. Indeed in patients whose hepatic enzymes are likely to be induced, e. g. those taking antiepileptic or some antirheumatic drugs, it is advisable to use a preparation containing 50 mcg or more of estrogen to avoid loss of efficacy due to increased estrogen metabolism (elimination of breakthrough bleeding is a guide to adequacy of dose).
Subsequent fertility After stopping the pill, fertility that is normal for the age the woman has now reached is restored, although conception may be delayed for a few months longer in younger and as much as a year in older users. Effect on an existing pregnancy Although progestogens can masculinise the female fetus, the doses for contraception are so low that risk of harming an undiagnosed pregnancy is extremely low, probably less than 1 in 1000 (the background incidence of birth defects is 1– 2%).
Carcinoma of the breast and cervix may be unaffected or very slightly increased in incidence; hepatoma (very rare) is increased. The risk to life seems to be less than that of moderate smoking (10 cigarettes/day). Carcinoma of the ovary and the endometrium are substantially reduced. Total incidence of cancer is unaltered. Effect on menstruation (it is not true menstruation) is generally to regularise it, and often to diminish blood loss, but amenorrhoea can occur. In some women “break-through” intermenstrual bleeding occurs, especially at the outset, but this seldom persists for more than a few cycles. Premenstrual tension and dysmenorrhoea are much reduced.
Libido is greatly subject to psychosocial influences, and removal of fear of pregnancy may permit enthusiasm for the first time. It is likely that direct pharmacological effect (reduction) is rare. There is evidence that the normal increase in female-initiated sexual activity at time of ovulation is suppressed. Cardiovascular complications Incidence of venous thromboembolism is increased in pill users. It is lowest in the 20– 35 mcg pill and rises progressively with the 50 and 100 mcg preparations; it is not known if there is any difference between doses of 20– 35 mcg.
The small increase in hypertension, cerebrovascular event and acute myocardial infarction is principally confined to smokers. Increased arterial disease also appears to be associated with the type of progestogen in the combined pill. The “ 3 rd generation” pills appear to carry a higher risk of venous thrombosis, but may have a lower risk of arterial thrombosis because their lower androgen activity leads to slightly higher HDL levels than older pills. The progestogen-only pill does not significantly affect coagulation.
Major surgery (in patients taking estrogenprogestogen contraceptives and postmenopausal hormone replacement therapy). Because of the added risk of venous thromboembolism (surgery causes a fall in antithrombin) it has been advised that these oral contraceptives should be withdrawn, if practicable, 4 weeks before all lower limb operations or any major elective surgery (and started again at the first menstruation to occur more than 2 weeks after surgery). But increase in clotting factors may persist for many weeks and there is also the risk of pregnancy to be considered (plainly, alternative contraception should be used). An alternative is to use low molecular weight heparin.
Hepatic function may be impaired as may drugmetabolizing capacity. Gallbladder disease is mo common, and highly vascular hepatocellular adenomas occur (rare). Cervical ectropion (erosion) incidence is double (it is a harmless condition). Crohn's disease is more frequent. Decreased glucose tolerance occurs, perhaps due to a peripheral effect reducing the action of insulin. Plasma lipoproteins may be adversely affected; least where the progestogen is desogestrel or low dose norethisterone.
Plasma proteins Estrogens cause an increase in proteins, particularly the globulins that bind hydrocortisone, thyroxine and iron. As a result, the total plasma concentration of the bound substances is increased, though the concentration of free and active substance remains normal. This can be misleading in diagnostic tests, e. g. of thyroid function. This effect on plasma proteins passes off about 6 weeks after cessation of the estrogen.
Absolute contraindications for use of contraceptives include: • A personal history of thromboembolic venous, arterial or cardiac disease or severe or multiple risk factors for these. • Transient cerebral ischaemic attacks without headache. • Infective hepatitis, until 3 months after liver function tests have become normal, and other liver disease including disturbances of hepatic excretion, e. g. cholestatic jaundice, Dubin. Johnson and Rotor syndromes.
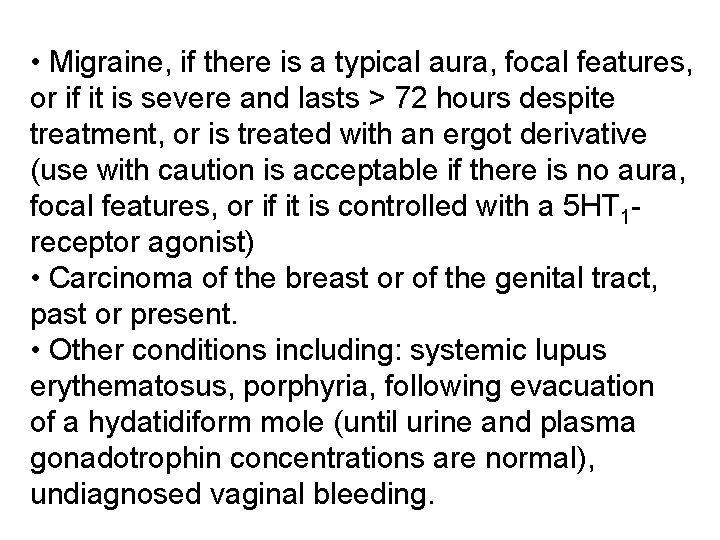
• Migraine, if there is a typical aura, focal features, or if it is severe and lasts > 72 hours despite treatment, or is treated with an ergot derivative (use with caution is acceptable if there is no aura, focal features, or if it is controlled with a 5 HT 1 receptor agonist) • Carcinoma of the breast or of the genital tract, past or present. • Other conditions including: systemic lupus erythematosus, porphyria, following evacuation of a hydatidiform mole (until urine and plasma gonadotrophin concentrations are normal), undiagnosed vaginal bleeding.
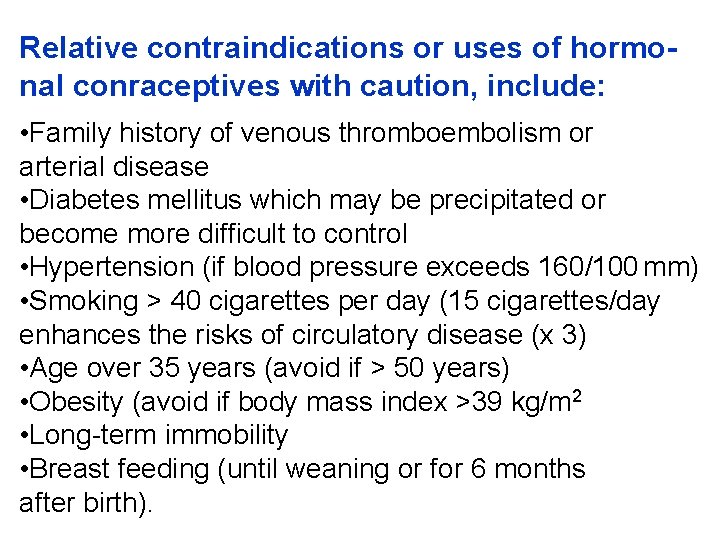
Relative contraindications or uses of hormonal conraceptives with caution, include: • Family history of venous thromboembolism or arterial disease • Diabetes mellitus which may be precipitated or become more difficult to control • Hypertension (if blood pressure exceeds 160/100 mm) • Smoking > 40 cigarettes per day (15 cigarettes/day enhances the risks of circulatory disease (x 3) • Age over 35 years (avoid if > 50 years) • Obesity (avoid if body mass index >39 kg/m 2 • Long-term immobility • Breast feeding (until weaning or for 6 months after birth).


www. drugsupport. data. bg www. pharmsupport 1. data. bg www. pharmsupporttwo. data. bg
 Masaryk university medical faculty
Masaryk university medical faculty Masaryk university medical faculty
Masaryk university medical faculty Nit calicut chemistry department
Nit calicut chemistry department Elearn st kliment
Elearn st kliment University of chemical technology and metallurgy
University of chemical technology and metallurgy Technical university sofia
Technical university sofia Technical university of sofia
Technical university of sofia Medical faculty in novi sad dean
Medical faculty in novi sad dean Herszon kherson maritime college of merchant marine fleet
Herszon kherson maritime college of merchant marine fleet University of bridgeport computer science faculty
University of bridgeport computer science faculty University of bridgeport computer engineering
University of bridgeport computer engineering Hubert kairuki memorial university faculty of medicine
Hubert kairuki memorial university faculty of medicine Semmelweis university faculty of medicine
Semmelweis university faculty of medicine King abdulaziz university faculty of medicine
King abdulaziz university faculty of medicine Florida state university ms in cs
Florida state university ms in cs Mendel university faculty of business and economics
Mendel university faculty of business and economics Singularity executive program
Singularity executive program Territorial matrix vs interterritorial matrix
Territorial matrix vs interterritorial matrix Faculty of engineering university of porto
Faculty of engineering university of porto Webkredit cuni
Webkredit cuni Faculty of veterinary medicine cairo university logo
Faculty of veterinary medicine cairo university logo Faculty of law of the university of zagreb
Faculty of law of the university of zagreb University of montenegro faculty of law
University of montenegro faculty of law University of kragujevac faculty of technical sciences
University of kragujevac faculty of technical sciences University of cologne faculty of management
University of cologne faculty of management Leading university cse faculty members
Leading university cse faculty members Hacettepe university faculty of medicine
Hacettepe university faculty of medicine Brown university computer science
Brown university computer science Conus arteriosus
Conus arteriosus Semmelweis university faculty of medicine
Semmelweis university faculty of medicine Lebanese university faculty of engineering
Lebanese university faculty of engineering Concurrent education york
Concurrent education york Faculty of economics and business debrecen
Faculty of economics and business debrecen Ece clemson
Ece clemson Faculty of veterinary medicine cairo university
Faculty of veterinary medicine cairo university Faculty of mechanical engineering thammasat university
Faculty of mechanical engineering thammasat university Mendel university faculty of business and economics
Mendel university faculty of business and economics Slidetodoc.com
Slidetodoc.com University of pecs faculty of health sciences
University of pecs faculty of health sciences Faculty of education khon kaen university
Faculty of education khon kaen university Faculty of communication arts chulalongkorn university
Faculty of communication arts chulalongkorn university Cairo university faculty of veterinary medicine
Cairo university faculty of veterinary medicine Medical records committee functions
Medical records committee functions Medical education and drugs department
Medical education and drugs department Department of law university of jammu
Department of law university of jammu Department of geology university of dhaka
Department of geology university of dhaka Mechanicistic
Mechanicistic University of bridgeport it department
University of bridgeport it department University of iowa math
University of iowa math Sputonik
Sputonik Texas state university psychology
Texas state university psychology Department of information engineering university of padova
Department of information engineering university of padova Information engineering padova
Information engineering padova Manipal university chemistry department
Manipal university chemistry department Syracuse university psychology department
Syracuse university psychology department Jackson state university finance department
Jackson state university finance department Computer science department columbia
Computer science department columbia Michigan state university astronomy
Michigan state university astronomy Columbia university cs department
Columbia university cs department University of sargodha engineering department
University of sargodha engineering department Claudia arrighi
Claudia arrighi California medical license application
California medical license application Gbmc medical records
Gbmc medical records Difference between medical report and medical certificate
Difference between medical report and medical certificate Torrance memorial tcu
Torrance memorial tcu Cartersville medical center medical records
Cartersville medical center medical records University medical centre maribor
University medical centre maribor Liaoning medical university
Liaoning medical university Vietnam military medical university
Vietnam military medical university M.gorky donetsk national medical university
M.gorky donetsk national medical university Ibn sina university of medical and pharmaceutical sciences
Ibn sina university of medical and pharmaceutical sciences Seoul national university college of medicine
Seoul national university college of medicine Kirovohrad medical university
Kirovohrad medical university Umcap hospital
Umcap hospital Stavropol state medical university
Stavropol state medical university Empp university medical center
Empp university medical center Hospital digomi
Hospital digomi Slowenien university medical center
Slowenien university medical center Columbia university medical center
Columbia university medical center Columbia university medical center
Columbia university medical center Lorenzo azzalini
Lorenzo azzalini Kaohsiung medical university hospital
Kaohsiung medical university hospital Medical academy of lublin
Medical academy of lublin Osh state medical university logo
Osh state medical university logo Mongolian national university of medical sciences
Mongolian national university of medical sciences Hawler medical university college of nursing
Hawler medical university college of nursing Google citations
Google citations Marija molan
Marija molan University of queensland ochsner medical school
University of queensland ochsner medical school Palm harbor university high school medical program
Palm harbor university high school medical program Vitosha park hotel sofia
Vitosha park hotel sofia Muff potter tom and huck
Muff potter tom and huck Technopolis business park
Technopolis business park Acronimo sofia
Acronimo sofia Sofia blast kft
Sofia blast kft