Med Star 2018 Health Plan Kick Off 2018







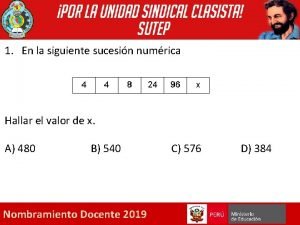
- Slides: 93
Med. Star 2018 Health Plan Kick Off 2018 Med. Star Medicare Choice Overview NOTE: This document is for training purposes only. Do not distribute.
Med. Star 2018 Agenda Med. Star Medicare Choice Overview • • 2018 Benefits and Updates/Changes Stars RAF SNP MOC Provider Resources Fraud, Waste and Abuse Medicare Appendix
2018 Med. Star Medicare Choice Product Training September 2018 For Broker Training Purposes Only - Do Not Distribute 2
What’s Changing for 2018: Service Area Reduction & Benefit Changes 3
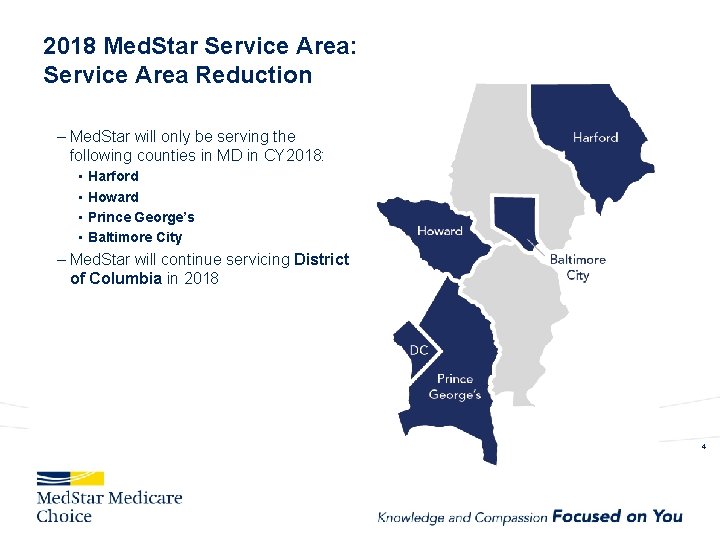
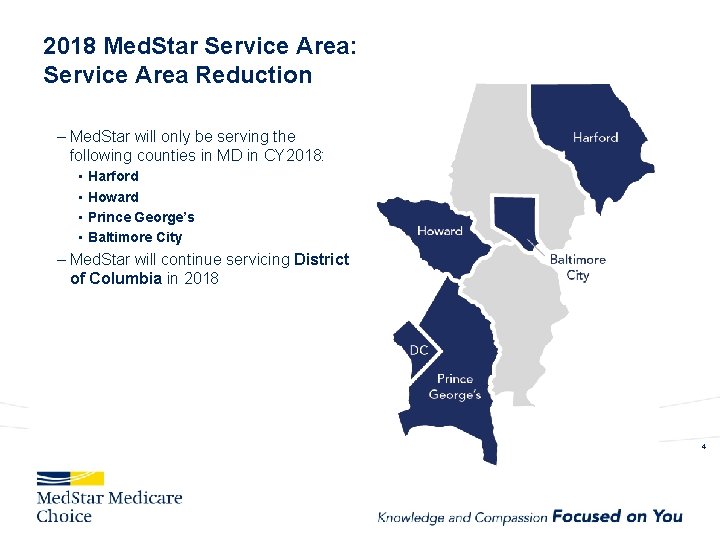
2018 Med. Star Service Area: Service Area Reduction – Med. Star will only be serving the following counties in MD in CY 2018: • • Harford Howard Prince George’s Baltimore City – Med. Star will continue servicing District of Columbia in 2018 4
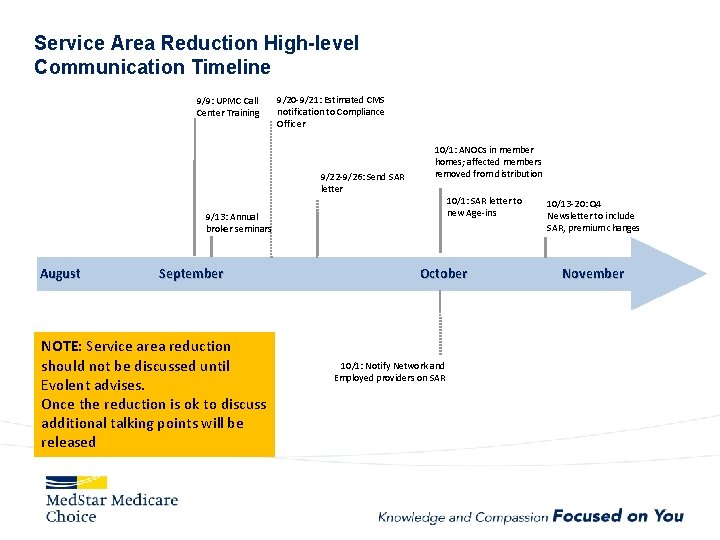
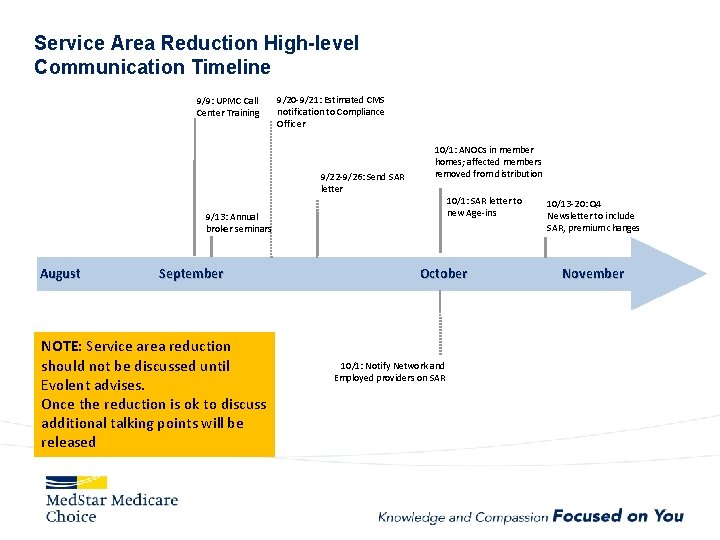
Service Area Reduction High-level Communication Timeline 9/9: UPMC Call Center Training 9/20 -9/21: Estimated CMS notification to Compliance Officer 9/22 -9/26: Send SAR letter 10/1: ANOCs in member homes; affected members removed from distribution 10/1: SAR letter to new Age-ins 9/13: Annual broker seminars August September NOTE: Service area reduction should not be discussed until Evolent advises. Once the reduction is ok to discuss additional talking points will be released October 10/1: Notify Network and Employed providers on SAR 10/13 -20: Q 4 Newsletter to include SAR, premium changes November
Service Area Reduction Impact to Members and Providers - Members will no longer have Med. Star Medicare Choice as of 1/1/18 if they live in a Service area reduction county - Med. Star Medicare Choice will no longer serve Anne Arundel, Baltimore, Charles, Calvert, St. Mary’s - Members will need to pick a new Medicare Advantage plan that is offered in their county or return to Original Medicare - Members will be able to continue to file grievances and appeals through the timely filing period - Providers can continue to file claims and disputes through the timely filing period - Expect to continue to get calls from these termed members and providers servicing these members as run-out from their previous plan year.
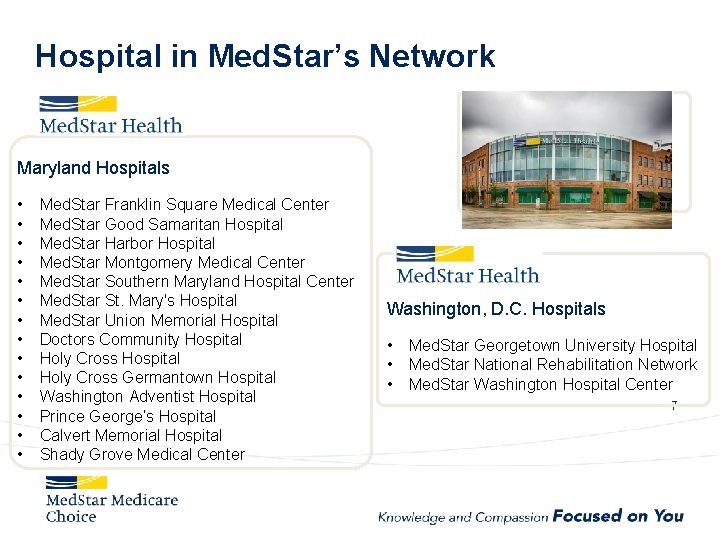
Hospital in Med. Star’s Network Maryland Hospitals • • • • Med. Star Franklin Square Medical Center Med. Star Good Samaritan Hospital Med. Star Harbor Hospital Med. Star Montgomery Medical Center Med. Star Southern Maryland Hospital Center Med. Star St. Mary's Hospital Med. Star Union Memorial Hospital Doctors Community Hospital Holy Cross Germantown Hospital Washington Adventist Hospital Prince George’s Hospital Calvert Memorial Hospital Shady Grove Medical Center Washington, D. C. Hospitals • • • Med. Star Georgetown University Hospital Med. Star National Rehabilitation Network Med. Star Washington Hospital Center 7
In the Community • • • Med. Star Family Choice Med. Star Health Research Institute Med. Star NRH Rehabilitation Network Med. Star Pharmacy Med. Star Physician Partner Med. Star Prompt. Care Med. Star Surgery Center Med. Star Visiting Nurse Association Multispecialty Care Centers Rad. America 8
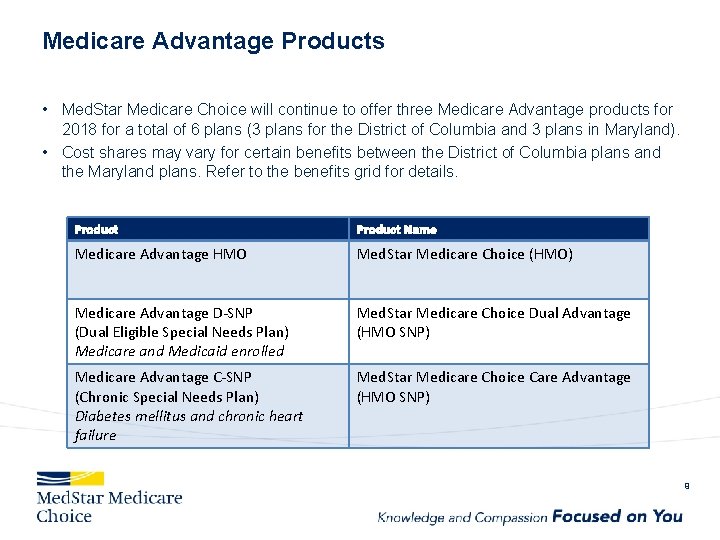
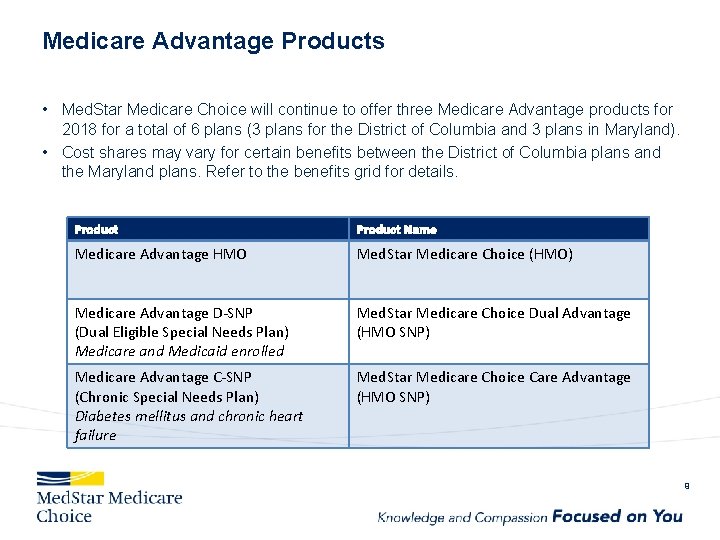
Medicare Advantage Products • Med. Star Medicare Choice will continue to offer three Medicare Advantage products for 2018 for a total of 6 plans (3 plans for the District of Columbia and 3 plans in Maryland). • Cost shares may vary for certain benefits between the District of Columbia plans and the Maryland plans. Refer to the benefits grid for details. Product Name Medicare Advantage HMO Med. Star Medicare Choice (HMO) Medicare Advantage D-SNP (Dual Eligible Special Needs Plan) Medicare and Medicaid enrolled Med. Star Medicare Choice Dual Advantage (HMO SNP) Medicare Advantage C-SNP (Chronic Special Needs Plan) Diabetes mellitus and chronic heart failure Med. Star Medicare Choice Care Advantage (HMO SNP) 9
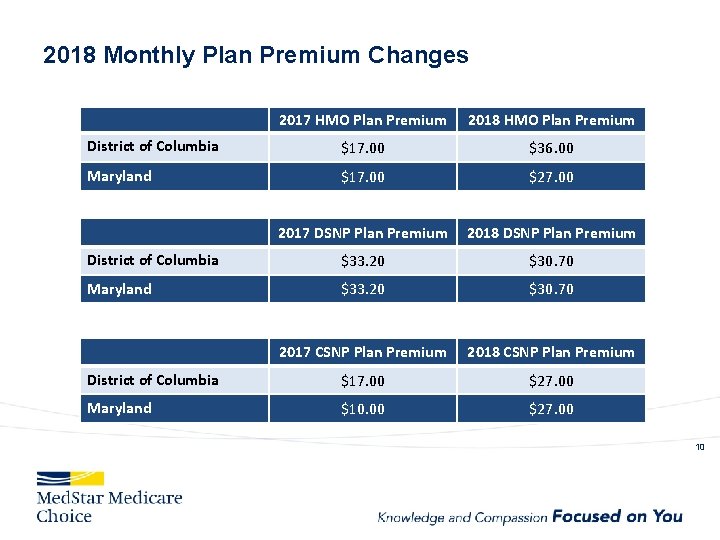
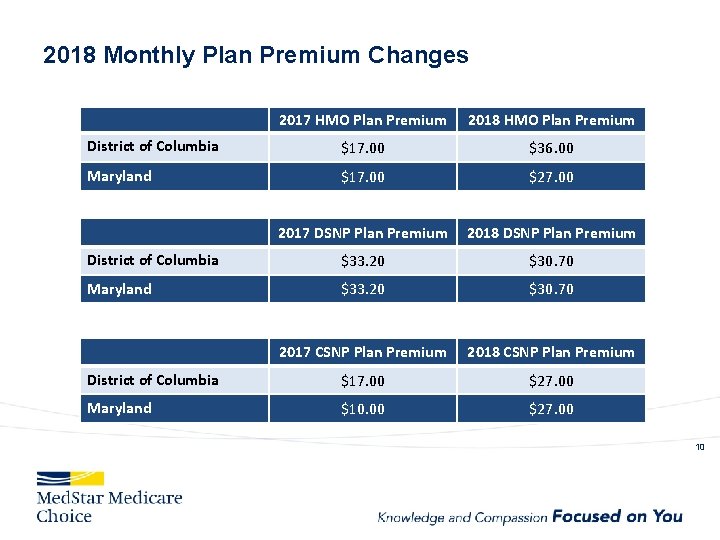
2018 Monthly Plan Premium Changes 2017 HMO Plan Premium 2018 HMO Plan Premium District of Columbia $17. 00 $36. 00 Maryland $17. 00 $27. 00 2017 DSNP Plan Premium 2018 DSNP Plan Premium District of Columbia $33. 20 $30. 70 Maryland $33. 20 $30. 70 2017 CSNP Plan Premium 2018 CSNP Plan Premium District of Columbia $17. 00 $27. 00 Maryland $10. 00 $27. 00 10
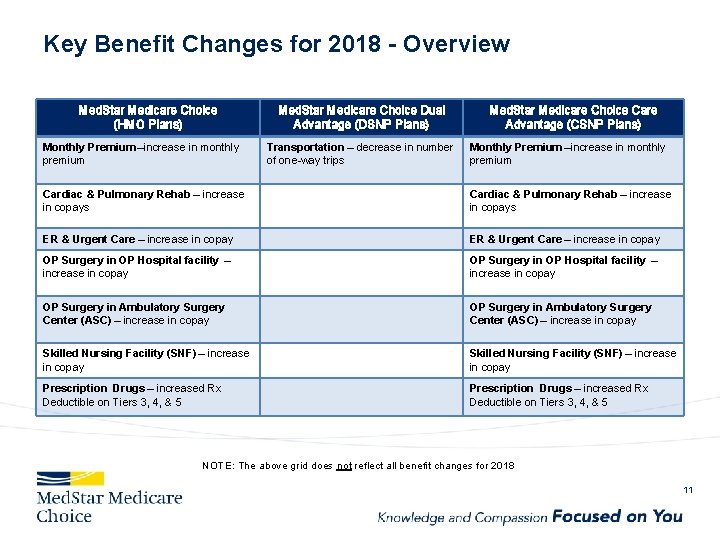
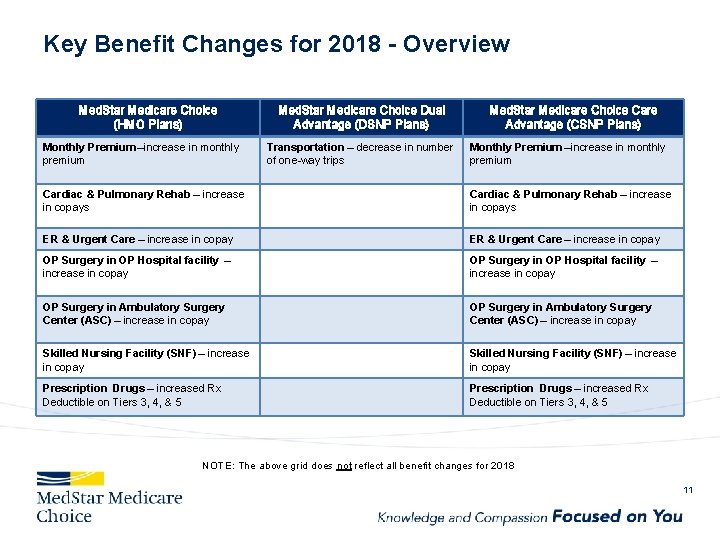
Key Benefit Changes for 2018 - Overview Med. Star Medicare Choice (HMO Plans) Monthly Premium –increase in monthly premium Med. Star Medicare Choice Dual Advantage (DSNP Plans) Transportation – decrease in number of one-way trips Med. Star Medicare Choice Care Advantage (CSNP Plans) Monthly Premium –increase in monthly premium Cardiac & Pulmonary Rehab – increase in copays ER & Urgent Care – increase in copay OP Surgery in OP Hospital facility – increase in copay OP Surgery in Ambulatory Surgery Center (ASC) – increase in copay Skilled Nursing Facility (SNF) – increase in copay Prescription Drugs – increased Rx Deductible on Tiers 3, 4, & 5 NOTE: The above grid does not reflect all benefit changes for 2018 11
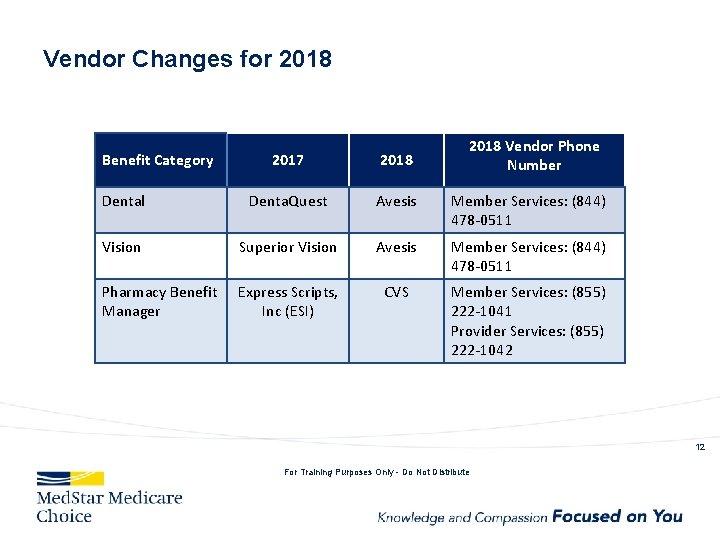
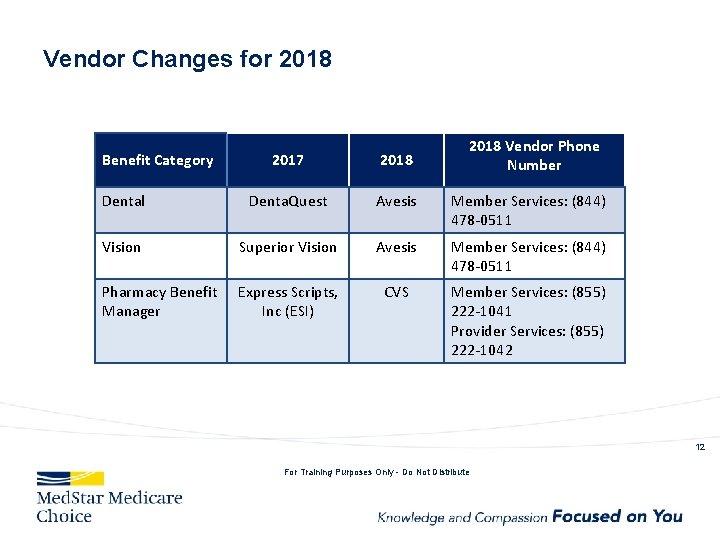
Vendor Changes for 2018 Benefit Category 2018 Vendor Phone Number 2017 2018 Dental Denta. Quest Avesis Member Services: (844) 478 -0511 Vision Superior Vision Avesis Member Services: (844) 478 -0511 Pharmacy Benefit Manager Express Scripts, Inc (ESI) CVS Member Services: (855) 222 -1041 Provider Services: (855) 222 -1042 12 For Training Purposes Only - Do Not Distribute
2018 Med. Star Medicare Choice (HMO) For Broker Training Purposes Only - Do Not Distribute 13
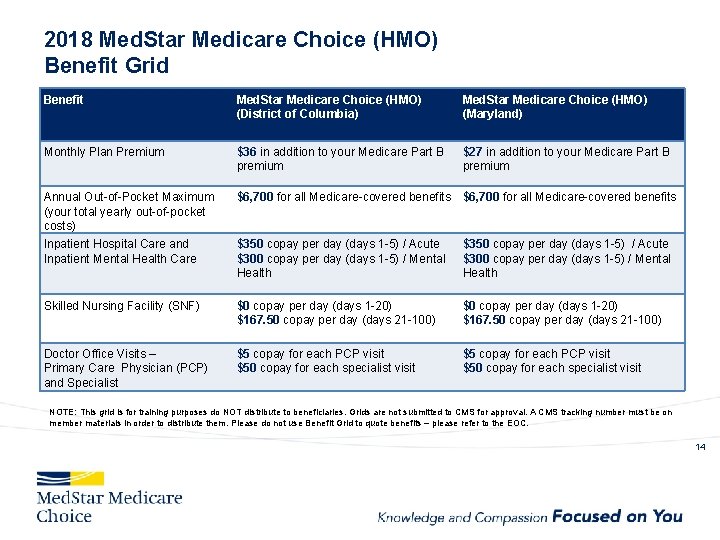
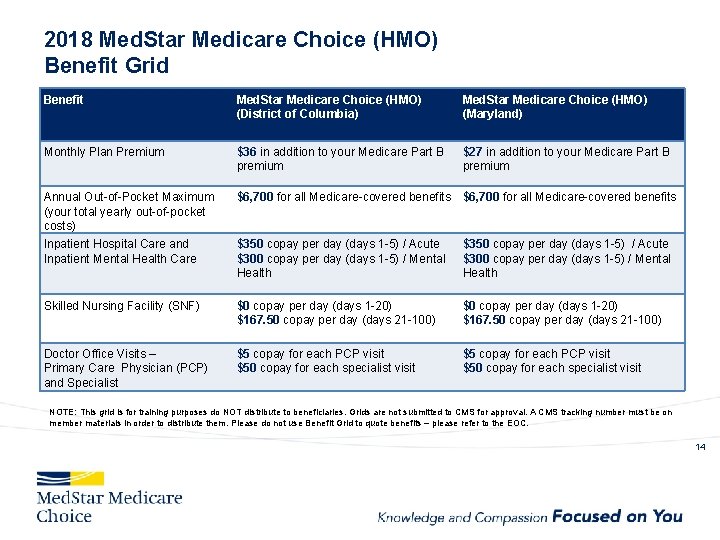
2018 Med. Star Medicare Choice (HMO) Benefit Grid Benefit Med. Star Medicare Choice (HMO) (District of Columbia) Med. Star Medicare Choice (HMO) (Maryland) Monthly Plan Premium $36 in addition to your Medicare Part B premium $27 in addition to your Medicare Part B premium Annual Out-of-Pocket Maximum (your total yearly out-of-pocket costs) $6, 700 for all Medicare-covered benefits Inpatient Hospital Care and Inpatient Mental Health Care $350 copay per day (days 1 -5) / Acute $300 copay per day (days 1 -5) / Mental Health Skilled Nursing Facility (SNF) $0 copay per day (days 1 -20) $167. 50 copay per day (days 21 -100) Doctor Office Visits – Primary Care Physician (PCP) and Specialist $5 copay for each PCP visit $50 copay for each specialist visit NOTE: This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC. 14
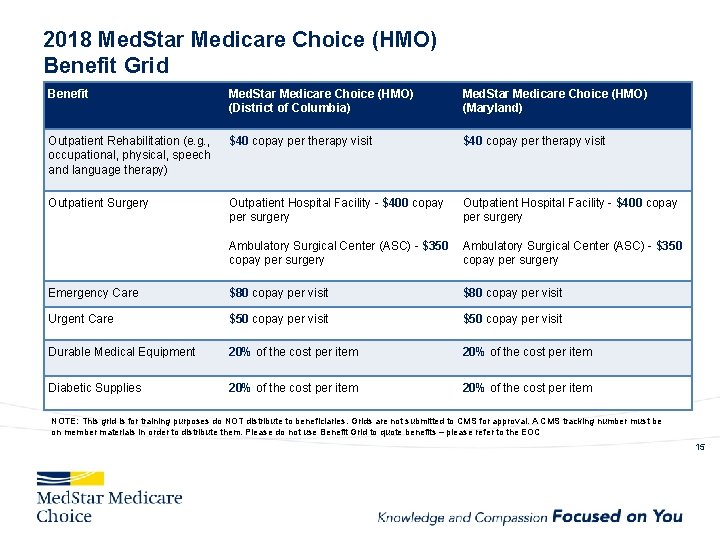
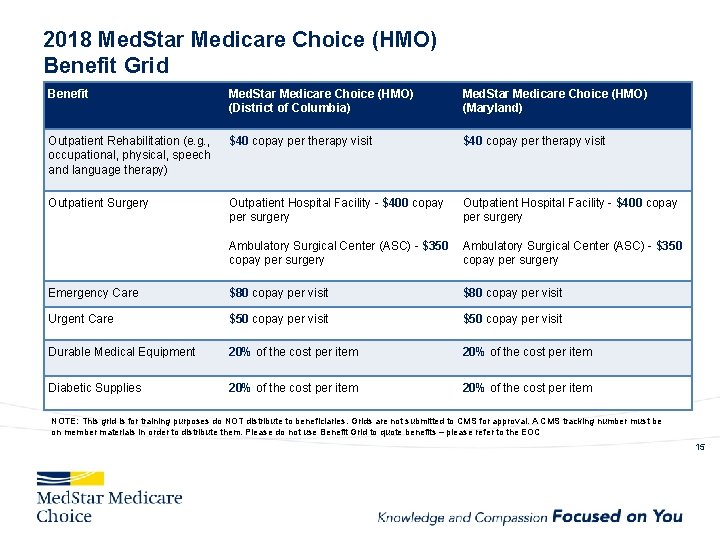
2018 Med. Star Medicare Choice (HMO) Benefit Grid Benefit Med. Star Medicare Choice (HMO) (District of Columbia) Med. Star Medicare Choice (HMO) (Maryland) Outpatient Rehabilitation (e. g. , occupational, physical, speech and language therapy) $40 copay per therapy visit Outpatient Surgery Outpatient Hospital Facility - $400 copay per surgery Ambulatory Surgical Center (ASC) - $350 copay per surgery Emergency Care $80 copay per visit Urgent Care $50 copay per visit Durable Medical Equipment 20% of the cost per item Diabetic Supplies 20% of the cost per item NOTE: This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC 15
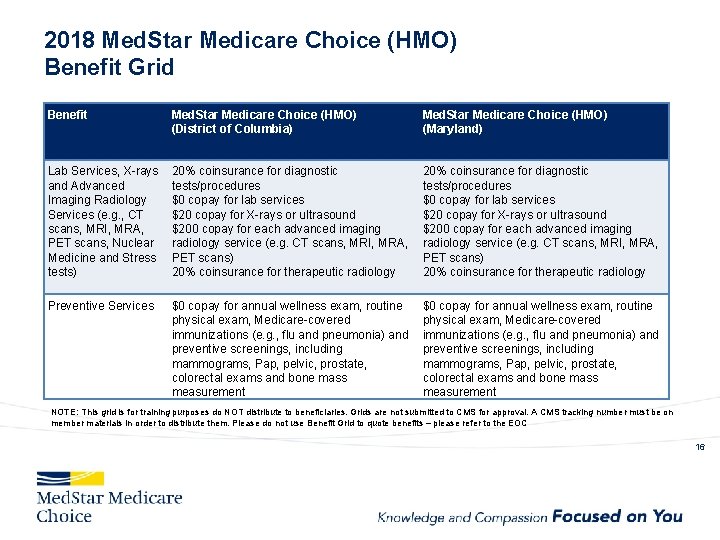
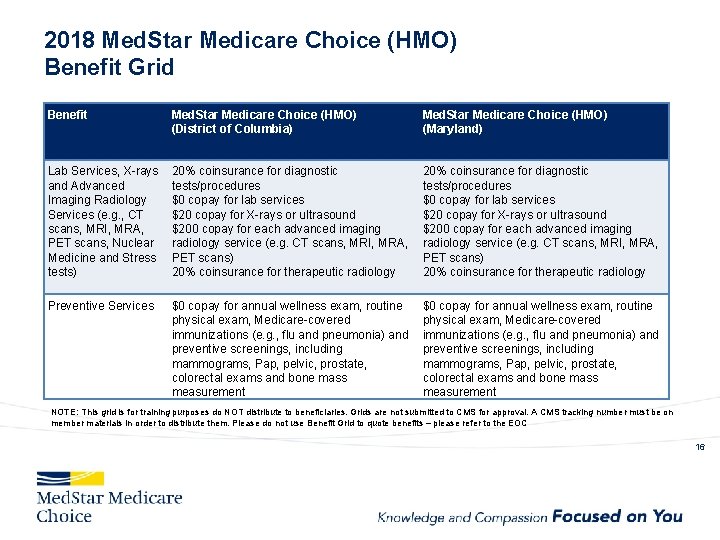
2018 Med. Star Medicare Choice (HMO) Benefit Grid Benefit Med. Star Medicare Choice (HMO) (District of Columbia) Med. Star Medicare Choice (HMO) (Maryland) Lab Services, X-rays and Advanced Imaging Radiology Services (e. g. , CT scans, MRI, MRA, PET scans, Nuclear Medicine and Stress tests) 20% coinsurance for diagnostic tests/procedures $0 copay for lab services $20 copay for X-rays or ultrasound $200 copay for each advanced imaging radiology service (e. g. CT scans, MRI, MRA, PET scans) 20% coinsurance for therapeutic radiology Preventive Services $0 copay for annual wellness exam, routine physical exam, Medicare-covered immunizations (e. g. , flu and pneumonia) and preventive screenings, including mammograms, Pap, pelvic, prostate, colorectal exams and bone mass measurement NOTE: This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC 16
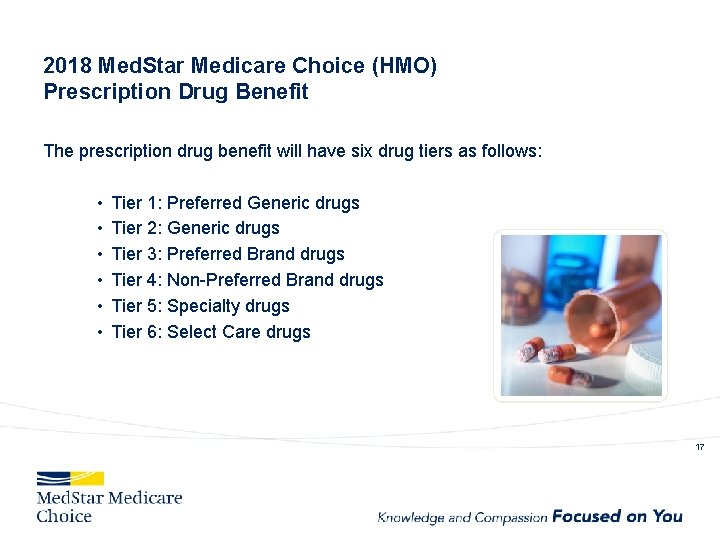
2018 Med. Star Medicare Choice (HMO) Prescription Drug Benefit The prescription drug benefit will have six drug tiers as follows: • • • Tier 1: Preferred Generic drugs Tier 2: Generic drugs Tier 3: Preferred Brand drugs Tier 4: Non-Preferred Brand drugs Tier 5: Specialty drugs Tier 6: Select Care drugs 17
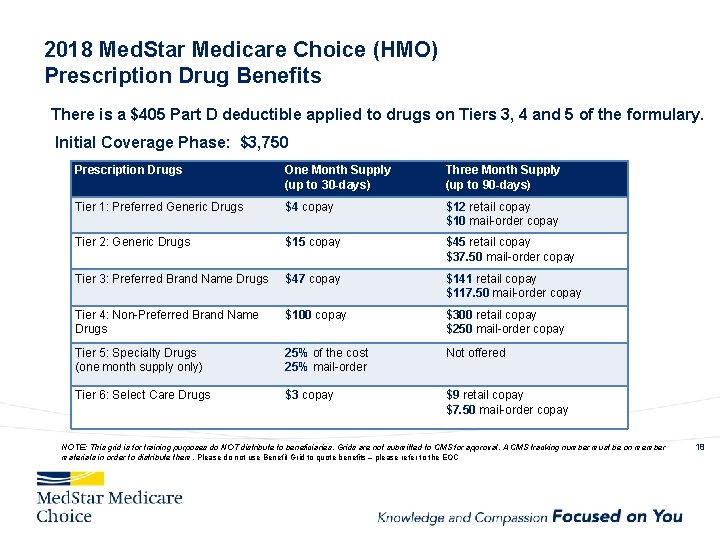
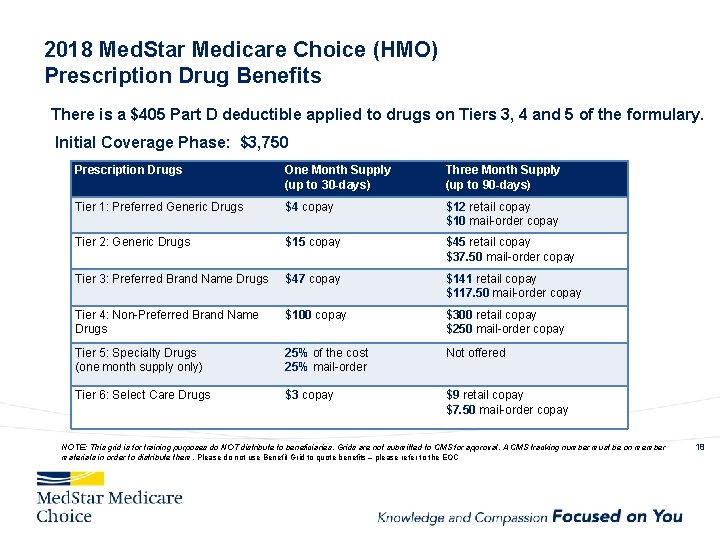
2018 Med. Star Medicare Choice (HMO) Prescription Drug Benefits There is a $405 Part D deductible applied to drugs on Tiers 3, 4 and 5 of the formulary. Initial Coverage Phase: $3, 750 Prescription Drugs One Month Supply (up to 30 -days) Three Month Supply (up to 90 -days) Tier 1: Preferred Generic Drugs $4 copay $12 retail copay $10 mail-order copay Tier 2: Generic Drugs $15 copay $45 retail copay $37. 50 mail-order copay Tier 3: Preferred Brand Name Drugs $47 copay $141 retail copay $117. 50 mail-order copay Tier 4: Non-Preferred Brand Name Drugs $100 copay $300 retail copay $250 mail-order copay Tier 5: Specialty Drugs (one month supply only) 25% of the cost 25% mail-order Not offered Tier 6: Select Care Drugs $3 copay $9 retail copay $7. 50 mail-order copay NOTE: This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC 18
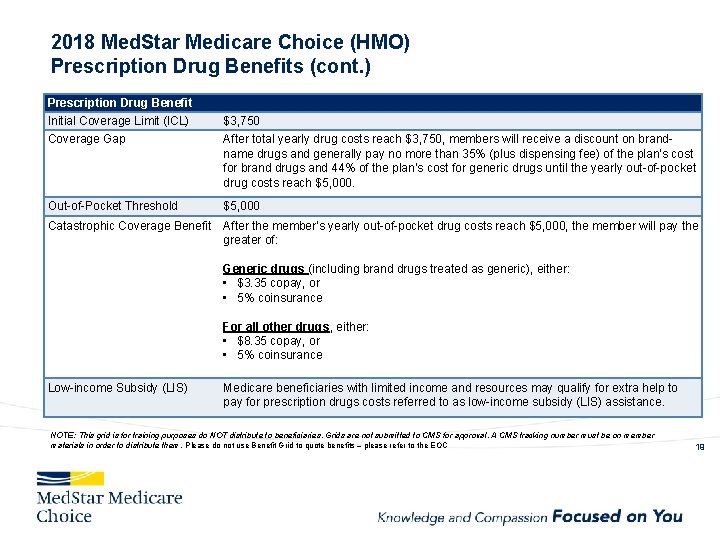
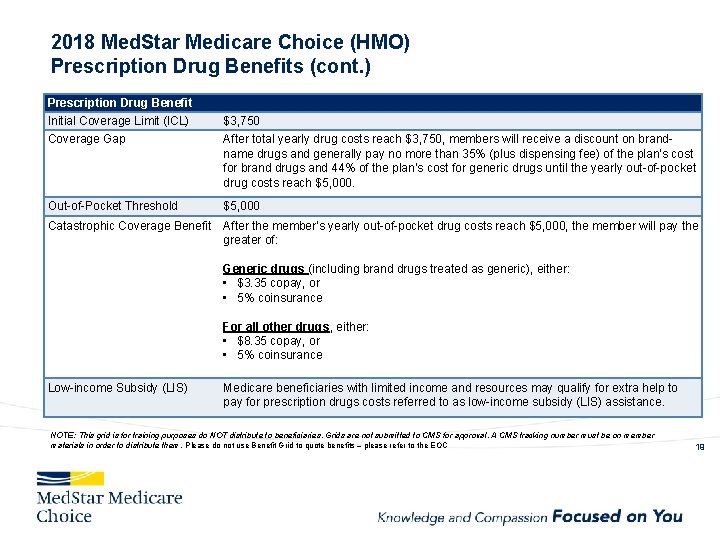
2018 Med. Star Medicare Choice (HMO) Prescription Drug Benefits (cont. ) Prescription Drug Benefit Initial Coverage Limit (ICL) $3, 750 Coverage Gap After total yearly drug costs reach $3, 750, members will receive a discount on brandname drugs and generally pay no more than 35% (plus dispensing fee) of the plan’s cost for brand drugs and 44% of the plan’s cost for generic drugs until the yearly out-of-pocket drug costs reach $5, 000. Out-of-Pocket Threshold $5, 000 Catastrophic Coverage Benefit After the member’s yearly out-of-pocket drug costs reach $5, 000, the member will pay the greater of: Generic drugs (including brand drugs treated as generic), either: • $3. 35 copay, or • 5% coinsurance For all other drugs, either: • $8. 35 copay, or • 5% coinsurance Low-income Subsidy (LIS) Medicare beneficiaries with limited income and resources may qualify for extra help to pay for prescription drugs costs referred to as low-income subsidy (LIS) assistance. NOTE: This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC 19
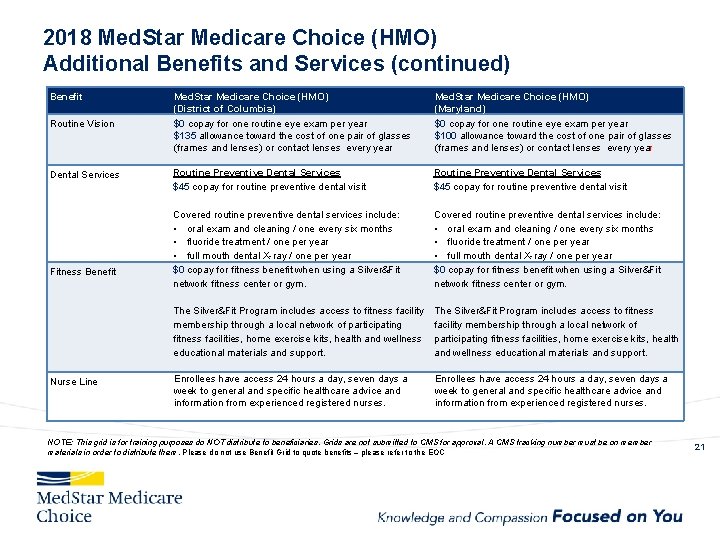
2018 Med. Star Medicare Choice (HMO) Additional Benefits and Services Our Med. Star Medicare Choice plan provides the following additional benefits: Vision Benefit Dental Benefit Fitness Benefit Nurse Line 20
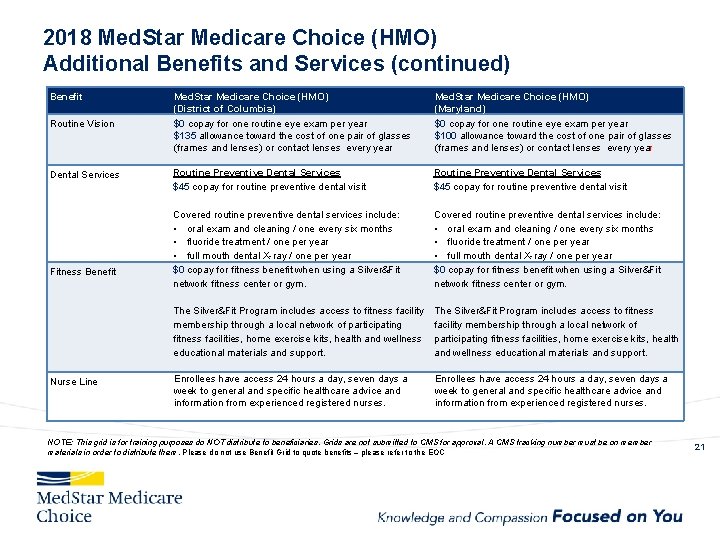
2018 Med. Star Medicare Choice (HMO) Additional Benefits and Services (continued) Benefit Med. Star Medicare Choice (HMO) (District of Columbia) Med. Star Medicare Choice (HMO) (Maryland) Routine Vision $0 copay for one routine eye exam per year $135 allowance toward the cost of one pair of glasses (frames and lenses) or contact lenses every year $0 copay for one routine eye exam per year $100 allowance toward the cost of one pair of glasses (frames and lenses) or contact lenses every year Dental Services Routine Preventive Dental Services $45 copay for routine preventive dental visit Covered routine preventive dental services include: • oral exam and cleaning / one every six months • fluoride treatment / one per year • full mouth dental X-ray / one per year $0 copay for fitness benefit when using a Silver&Fit network fitness center or gym. The Silver&Fit Program includes access to fitness facility membership through a local network of participating fitness facilities, home exercise kits, health and wellness educational materials and support. Enrollees have access 24 hours a day, seven days a week to general and specific healthcare advice and information from experienced registered nurses. Fitness Benefit Nurse Line NOTE: This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC 21
2018 Med. Star Medicare Choice Dual Advantage (HMO DSNP) Dual Eligible Special Needs Plan (D-SNP) For Broker Training Purposes Only - Do Not Distribute 22
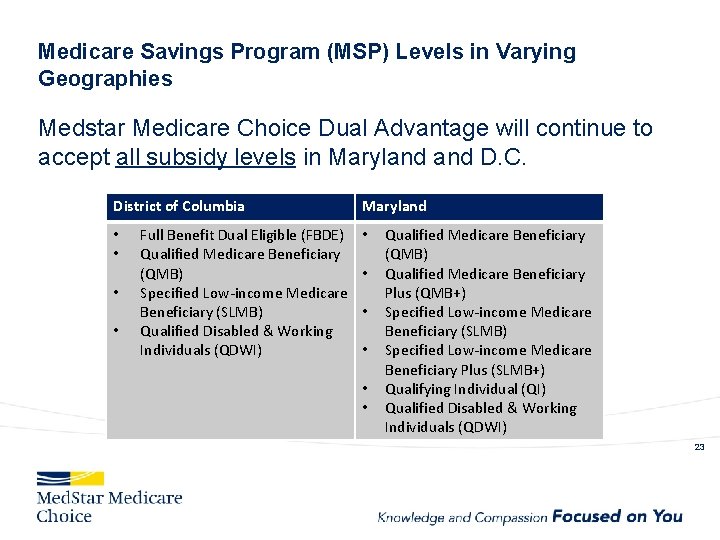
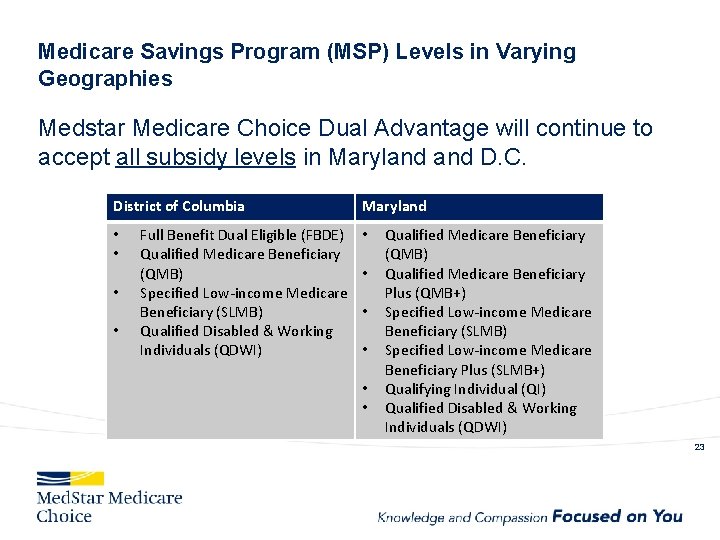
Medicare Savings Program (MSP) Levels in Varying Geographies Medstar Medicare Choice Dual Advantage will continue to accept all subsidy levels in Maryland D. C. District of Columbia • • Full Benefit Dual Eligible (FBDE) Qualified Medicare Beneficiary (QMB) Specified Low-income Medicare Beneficiary (SLMB) Qualified Disabled & Working Individuals (QDWI) Maryland • • • Qualified Medicare Beneficiary (QMB) Qualified Medicare Beneficiary Plus (QMB+) Specified Low-income Medicare Beneficiary (SLMB) Specified Low-income Medicare Beneficiary Plus (SLMB+) Qualifying Individual (QI) Qualified Disabled & Working Individuals (QDWI) 23

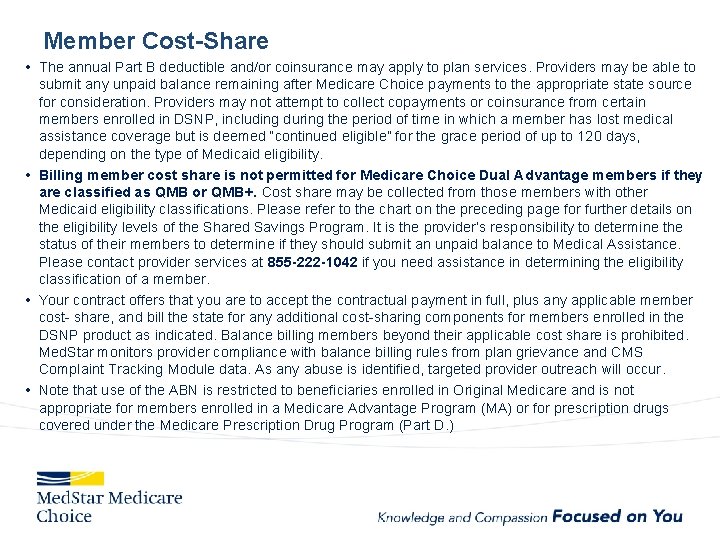
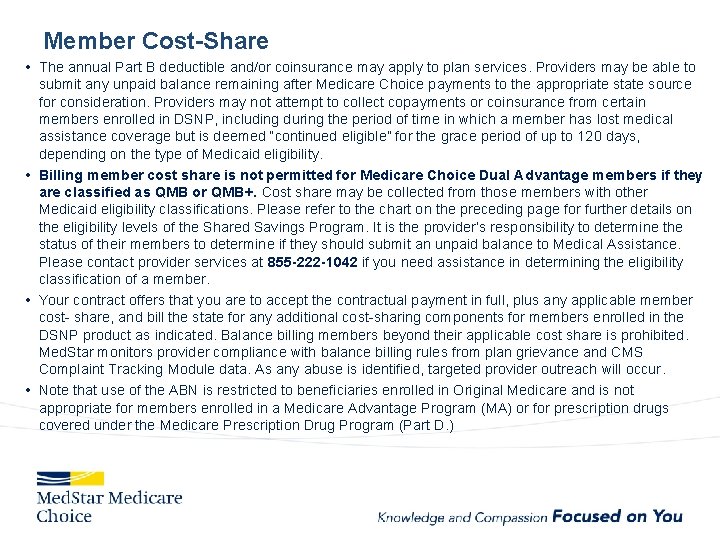
Member Cost-Share • The annual Part B deductible and/or coinsurance may apply to plan services. Providers may be able to submit any unpaid balance remaining after Medicare Choice payments to the appropriate state source for consideration. Providers may not attempt to collect copayments or coinsurance from certain members enrolled in DSNP, including during the period of time in which a member has lost medical assistance coverage but is deemed “continued eligible” for the grace period of up to 120 days, depending on the type of Medicaid eligibility. • Billing member cost share is not permitted for Medicare Choice Dual Advantage members if they are classified as QMB or QMB+. Cost share may be collected from those members with other Medicaid eligibility classifications. Please refer to the chart on the preceding page for further details on the eligibility levels of the Shared Savings Program. It is the provider’s responsibility to determine the status of their members to determine if they should submit an unpaid balance to Medical Assistance. Please contact provider services at 855 -222 -1042 if you need assistance in determining the eligibility classification of a member. • Your contract offers that you are to accept the contractual payment in full, plus any applicable member cost- share, and bill the state for any additional cost-sharing components for members enrolled in the DSNP product as indicated. Balance billing members beyond their applicable cost share is prohibited. Med. Star monitors provider compliance with balance billing rules from plan grievance and CMS Complaint Tracking Module data. As any abuse is identified, targeted provider outreach will occur. • Note that use of the ABN is restricted to beneficiaries enrolled in Original Medicare and is not appropriate for members enrolled in a Medicare Advantage Program (MA) or for prescription drugs covered under the Medicare Prescription Drug Program (Part D. )
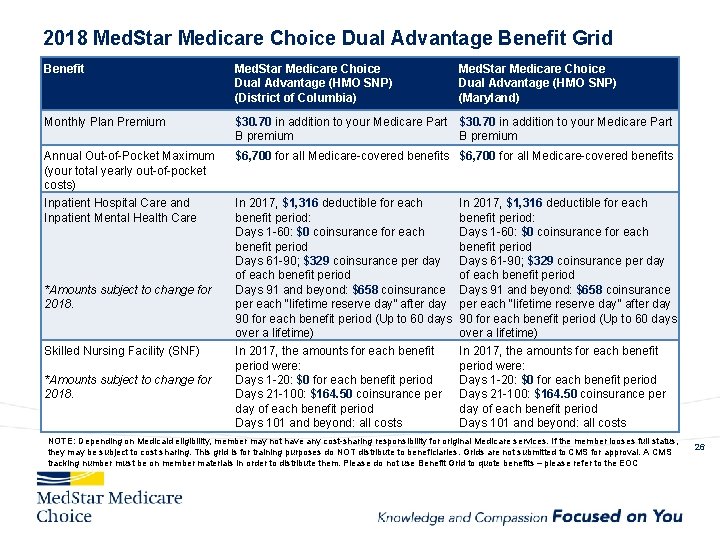
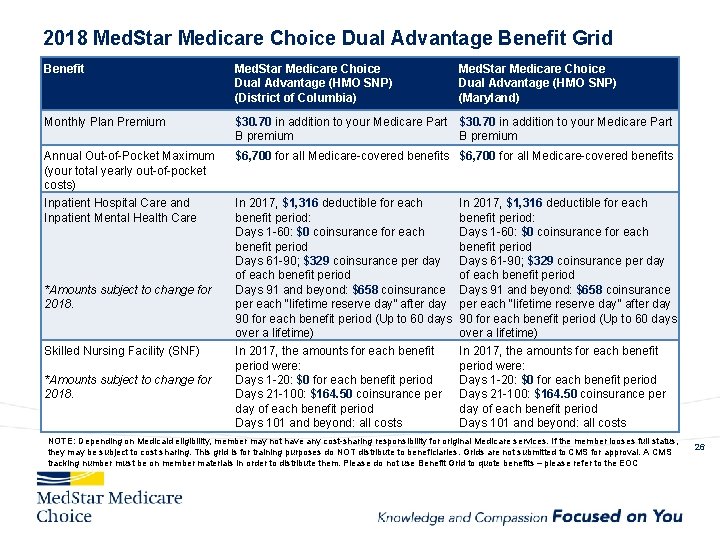
2018 Med. Star Medicare Choice Dual Advantage Benefit Grid Benefit Med. Star Medicare Choice Dual Advantage (HMO SNP) (District of Columbia) Monthly Plan Premium $30. 70 in addition to your Medicare Part B premium Annual Out-of-Pocket Maximum (your total yearly out-of-pocket costs) $6, 700 for all Medicare-covered benefits Inpatient Hospital Care and Inpatient Mental Health Care In 2017, $1, 316 deductible for each benefit period: Days 1 -60: $0 coinsurance for each benefit period Days 61 -90; $329 coinsurance per day of each benefit period Days 91 and beyond: $658 coinsurance per each “lifetime reserve day” after day 90 for each benefit period (Up to 60 days over a lifetime) *Amounts subject to change for 2018. Skilled Nursing Facility (SNF) *Amounts subject to change for 2018. In 2017, the amounts for each benefit period were: Days 1 -20: $0 for each benefit period Days 21 -100: $164. 50 coinsurance per day of each benefit period Days 101 and beyond: all costs Med. Star Medicare Choice Dual Advantage (HMO SNP) (Maryland) In 2017, the amounts for each benefit period were: Days 1 -20: $0 for each benefit period Days 21 -100: $164. 50 coinsurance per day of each benefit period Days 101 and beyond: all costs NOTE: Depending on Medicaid eligibility, member may not have any cost-sharing responsibility for original Medicare services. If the member looses full status, they may be subject to cost sharing. This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC 26
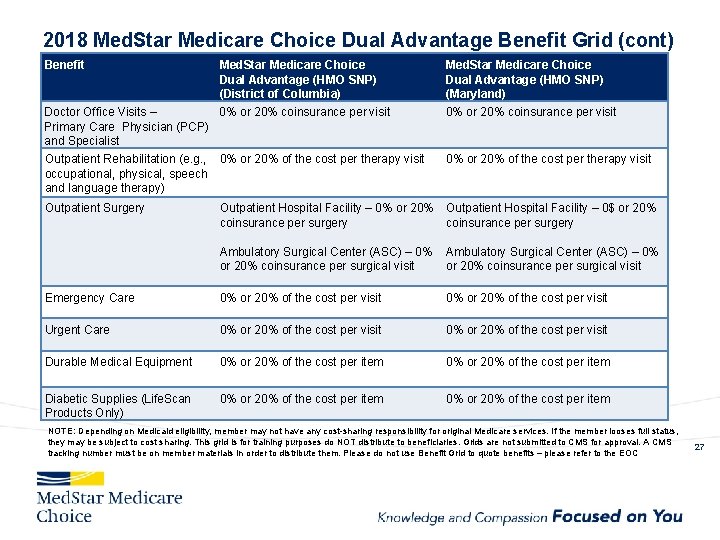
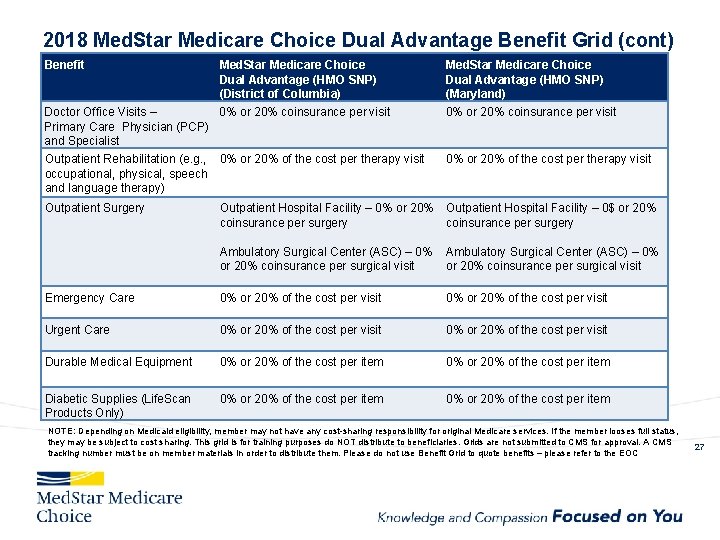
2018 Med. Star Medicare Choice Dual Advantage Benefit Grid (cont) Benefit Med. Star Medicare Choice Dual Advantage (HMO SNP) (District of Columbia) Med. Star Medicare Choice Dual Advantage (HMO SNP) (Maryland) Doctor Office Visits – 0% or 20% coinsurance per visit Primary Care Physician (PCP) and Specialist 0% or 20% coinsurance per visit Outpatient Rehabilitation (e. g. , 0% or 20% of the cost per therapy visit occupational, physical, speech and language therapy) 0% or 20% of the cost per therapy visit Outpatient Surgery Outpatient Hospital Facility – 0% or 20% Outpatient Hospital Facility – 0$ or 20% coinsurance per surgery Ambulatory Surgical Center (ASC) – 0% or 20% coinsurance per surgical visit Emergency Care 0% or 20% of the cost per visit Urgent Care 0% or 20% of the cost per visit Durable Medical Equipment 0% or 20% of the cost per item Diabetic Supplies (Life. Scan Products Only) 0% or 20% of the cost per item NOTE: Depending on Medicaid eligibility, member may not have any cost-sharing responsibility for original Medicare services. If the member looses full status, they may be subject to cost sharing. This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC 27
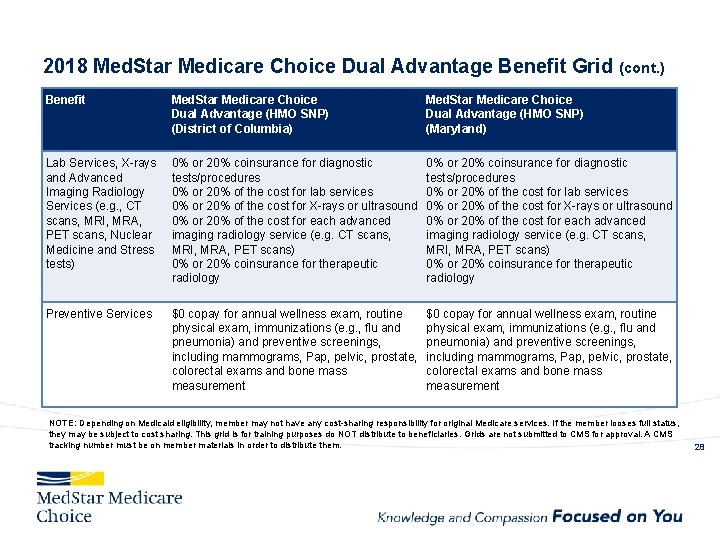
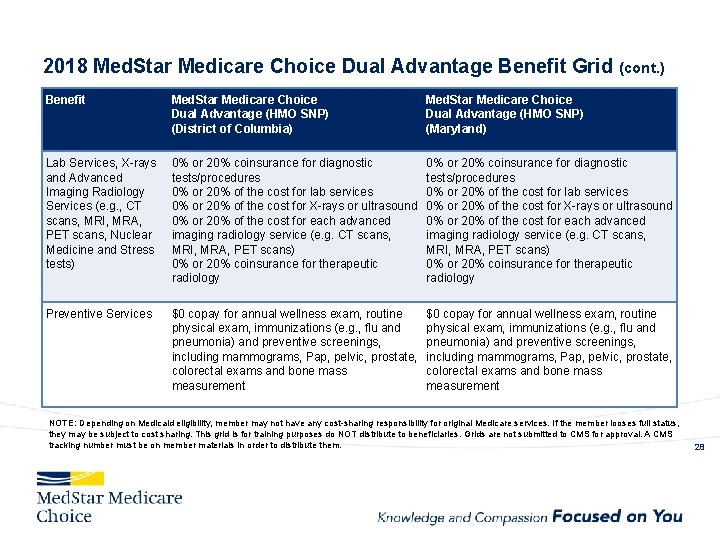
2018 Med. Star Medicare Choice Dual Advantage Benefit Grid (cont. ) Benefit Med. Star Medicare Choice Dual Advantage (HMO SNP) (District of Columbia) Med. Star Medicare Choice Dual Advantage (HMO SNP) (Maryland) Lab Services, X-rays and Advanced Imaging Radiology Services (e. g. , CT scans, MRI, MRA, PET scans, Nuclear Medicine and Stress tests) 0% or 20% coinsurance for diagnostic tests/procedures 0% or 20% of the cost for lab services 0% or 20% of the cost for X-rays or ultrasound 0% or 20% of the cost for each advanced imaging radiology service (e. g. CT scans, MRI, MRA, PET scans) 0% or 20% coinsurance for therapeutic radiology Preventive Services $0 copay for annual wellness exam, routine physical exam, immunizations (e. g. , flu and pneumonia) and preventive screenings, including mammograms, Pap, pelvic, prostate, colorectal exams and bone mass measurement NOTE: Depending on Medicaid eligibility, member may not have any cost-sharing responsibility for original Medicare services. If the member looses full status, they may be subject to cost sharing. This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. 28
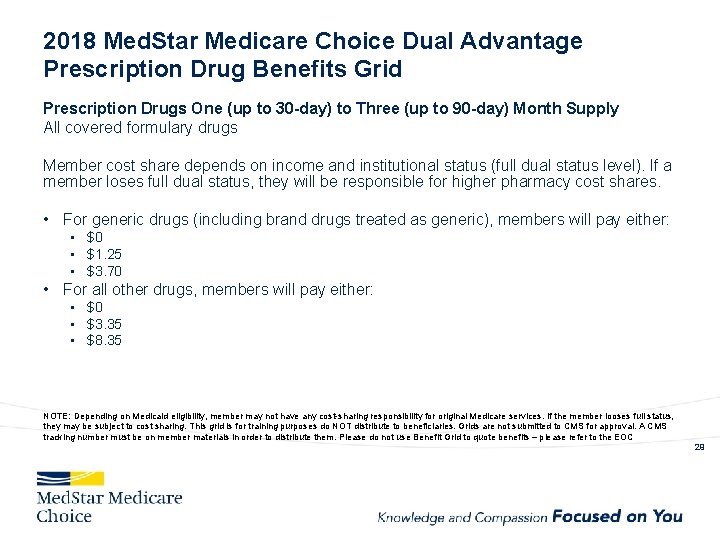
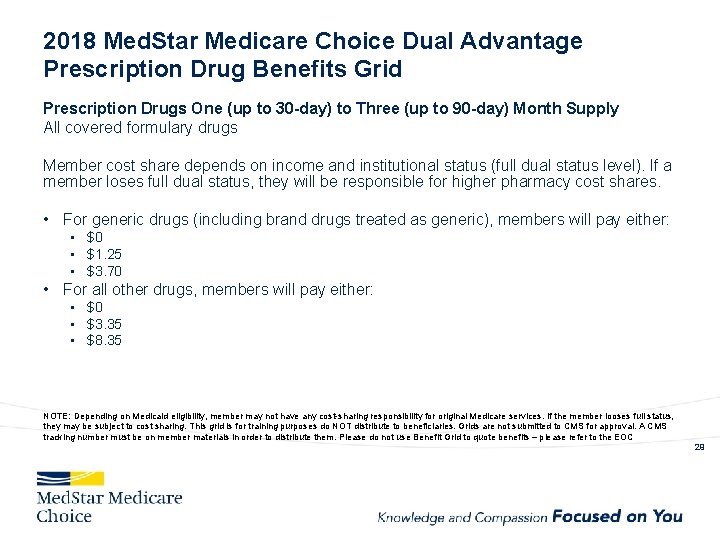
2018 Med. Star Medicare Choice Dual Advantage Prescription Drug Benefits Grid Prescription Drugs One (up to 30 -day) to Three (up to 90 -day) Month Supply All covered formulary drugs Member cost share depends on income and institutional status (full dual status level). If a member loses full dual status, they will be responsible for higher pharmacy cost shares. • For generic drugs (including brand drugs treated as generic), members will pay either: • $0 • $1. 25 • $3. 70 • For all other drugs, members will pay either: • $0 • $3. 35 • $8. 35 NOTE: Depending on Medicaid eligibility, member may not have any cost-sharing responsibility for original Medicare services. If the member looses full status, they may be subject to cost sharing. This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC 29
2018 Med. Star Medicare Choice Dual Advantage Additional Benefits and Services Our Med. Star Medicare Choice Dual Advantage plan provides the following additional benefits and services: Routine Vision Dental Services Transportation Services Nurse Line OTC 30
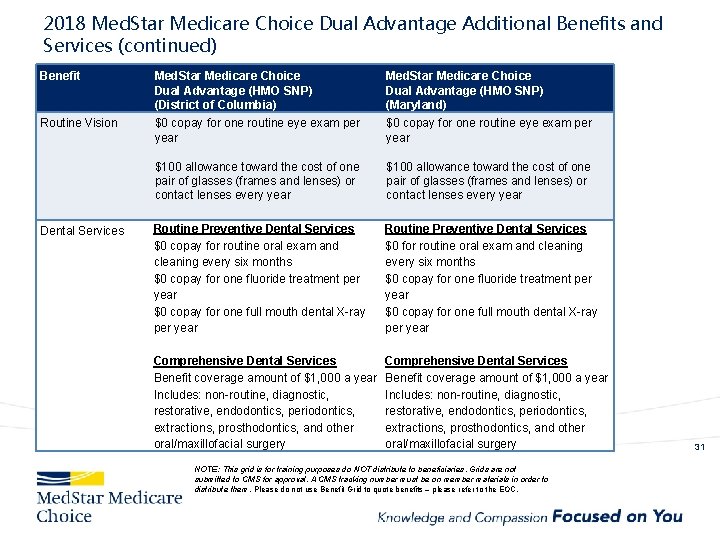
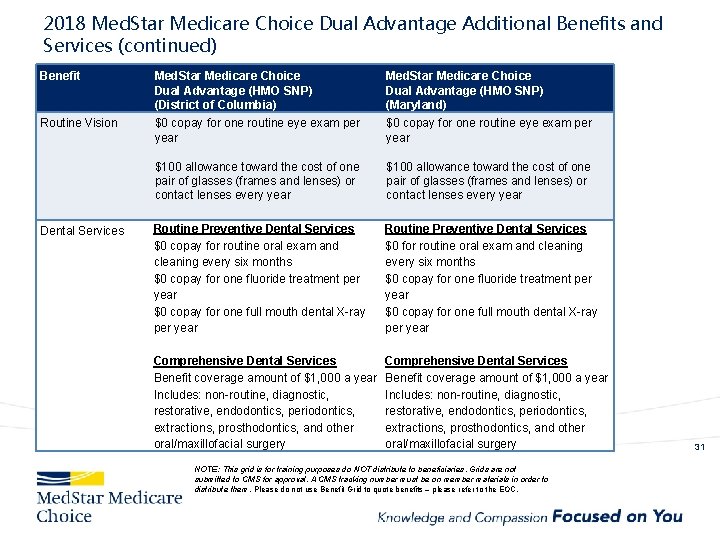
2018 Med. Star Medicare Choice Dual Advantage Additional Benefits and Services (continued) Benefit Med. Star Medicare Choice Dual Advantage (HMO SNP) (District of Columbia) Med. Star Medicare Choice Dual Advantage (HMO SNP) (Maryland) Routine Vision $0 copay for one routine eye exam per year $100 allowance toward the cost of one pair of glasses (frames and lenses) or contact lenses every year Routine Preventive Dental Services $0 copay for routine oral exam and cleaning every six months $0 copay for one fluoride treatment per year $0 copay for one full mouth dental X-ray per year Routine Preventive Dental Services $0 for routine oral exam and cleaning every six months $0 copay for one fluoride treatment per year $0 copay for one full mouth dental X-ray per year Comprehensive Dental Services Benefit coverage amount of $1, 000 a year Includes: non-routine, diagnostic, restorative, endodontics, periodontics, extractions, prosthodontics, and other oral/maxillofacial surgery Dental Services NOTE: This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC. 31
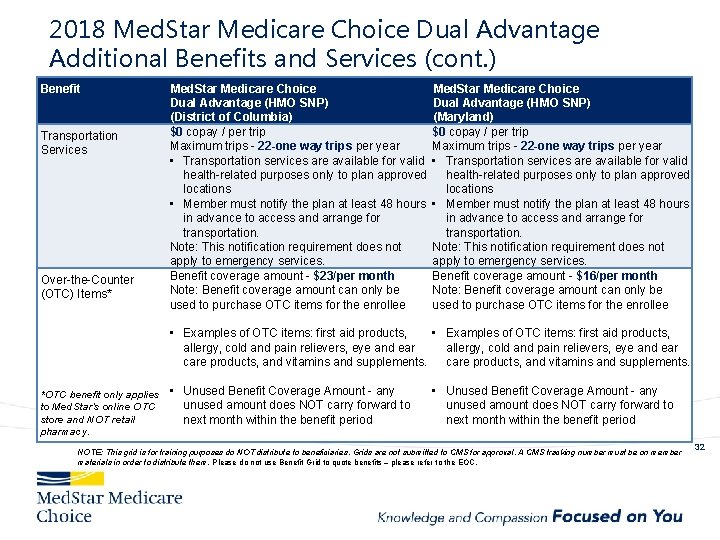
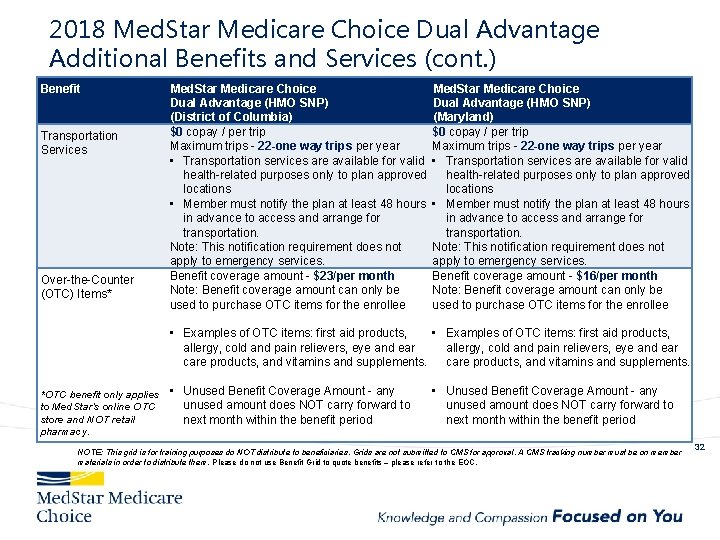
2018 Med. Star Medicare Choice Dual Advantage Additional Benefits and Services (cont. ) Benefit Transportation Services Over-the-Counter (OTC) Items* Med. Star Medicare Choice Dual Advantage (HMO SNP) (District of Columbia) (Maryland) $0 copay / per trip Maximum trips - 22 -one way trips per year • Transportation services are available for valid health-related purposes only to plan approved locations • Member must notify the plan at least 48 hours in advance to access and arrange for transportation. Note: This notification requirement does not apply to emergency services. Benefit coverage amount - $23/per month Benefit coverage amount - $16/per month Note: Benefit coverage amount can only be used to purchase OTC items for the enrollee • Examples of OTC items: first aid products, allergy, cold and pain relievers, eye and ear care products, and vitamins and supplements. *OTC benefit only applies • Unused Benefit Coverage Amount - any unused amount does NOT carry forward to to Med. Star’s online OTC store and NOT retail next month within the benefit period pharmacy. • Unused Benefit Coverage Amount - any unused amount does NOT carry forward to next month within the benefit period NOTE: This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC. 32
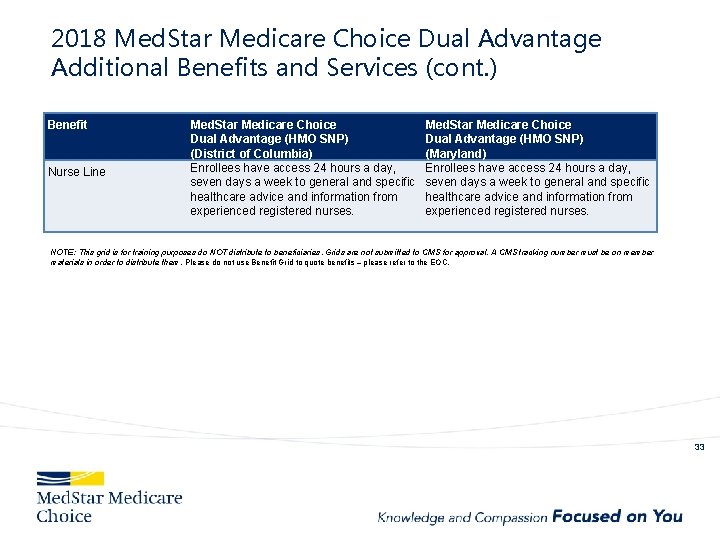
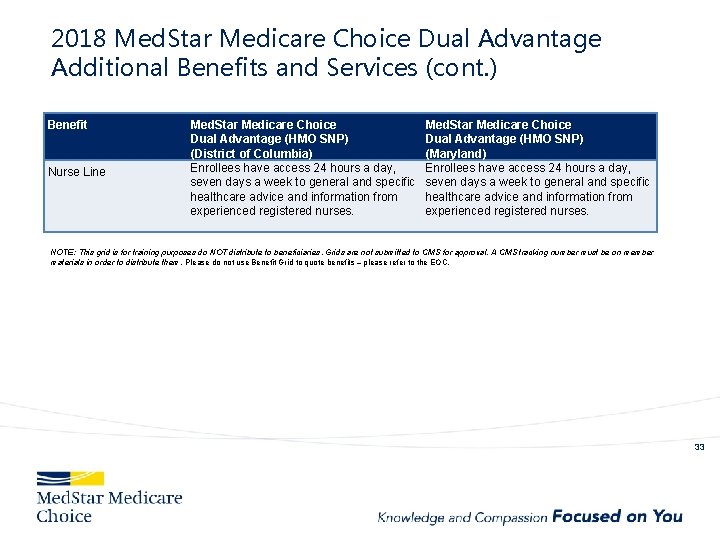
2018 Med. Star Medicare Choice Dual Advantage Additional Benefits and Services (cont. ) Benefit Nurse Line Med. Star Medicare Choice Dual Advantage (HMO SNP) (District of Columbia) Enrollees have access 24 hours a day, seven days a week to general and specific healthcare advice and information from experienced registered nurses. Med. Star Medicare Choice Dual Advantage (HMO SNP) (Maryland) Enrollees have access 24 hours a day, seven days a week to general and specific healthcare advice and information from experienced registered nurses. NOTE: This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC. 33
2018 Med. Star Medicare Choice Care Advantage (HMO CSNP) Chronic Condition Special Needs Plan (C-SNP) For Broker Training Purposes Only - Do Not Distribute 34
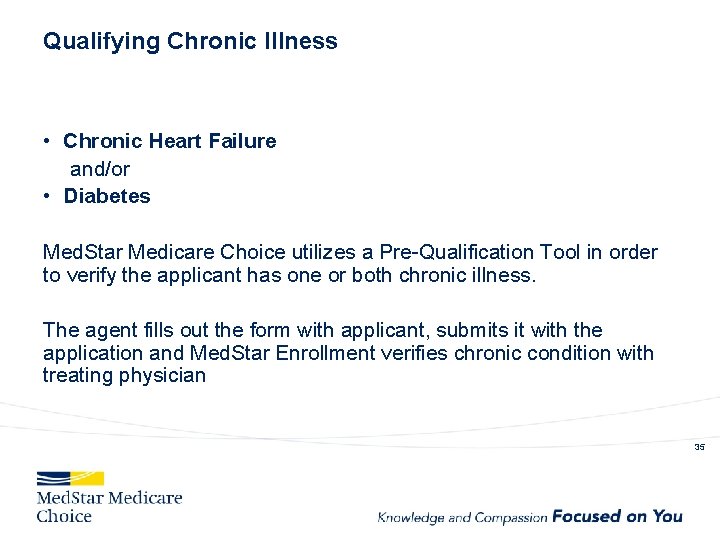
Qualifying Chronic Illness • Chronic Heart Failure and/or • Diabetes Med. Star Medicare Choice utilizes a Pre-Qualification Tool in order to verify the applicant has one or both chronic illness. The agent fills out the form with applicant, submits it with the application and Med. Star Enrollment verifies chronic condition with treating physician 35
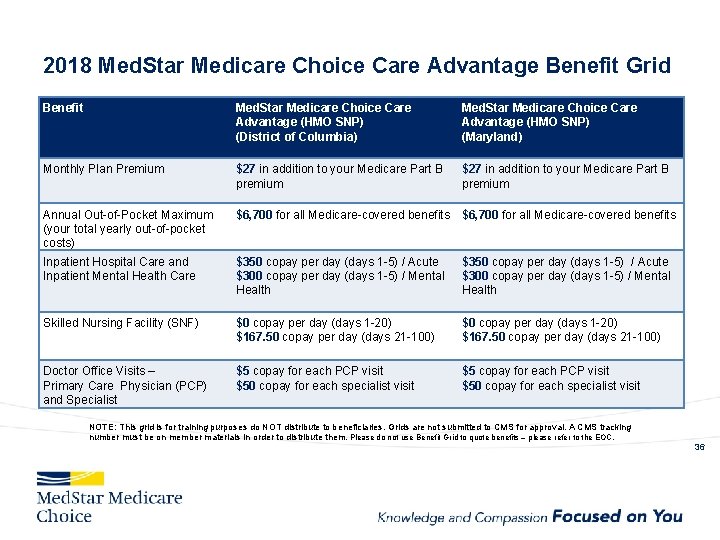
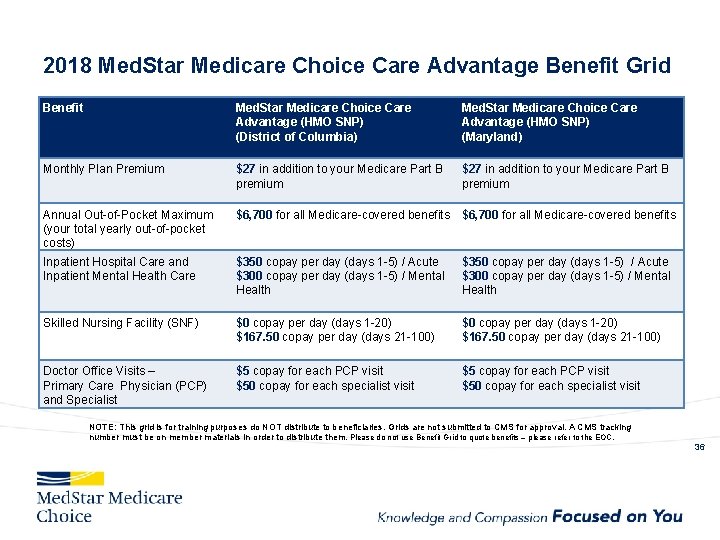
2018 Med. Star Medicare Choice Care Advantage Benefit Grid Benefit Med. Star Medicare Choice Care Advantage (HMO SNP) (District of Columbia) Med. Star Medicare Choice Care Advantage (HMO SNP) (Maryland) Monthly Plan Premium $27 in addition to your Medicare Part B premium Annual Out-of-Pocket Maximum (your total yearly out-of-pocket costs) $6, 700 for all Medicare-covered benefits Inpatient Hospital Care and Inpatient Mental Health Care $350 copay per day (days 1 -5) / Acute $300 copay per day (days 1 -5) / Mental Health Skilled Nursing Facility (SNF) $0 copay per day (days 1 -20) $167. 50 copay per day (days 21 -100) Doctor Office Visits – Primary Care Physician (PCP) and Specialist $5 copay for each PCP visit $50 copay for each specialist visit NOTE: This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC. 36
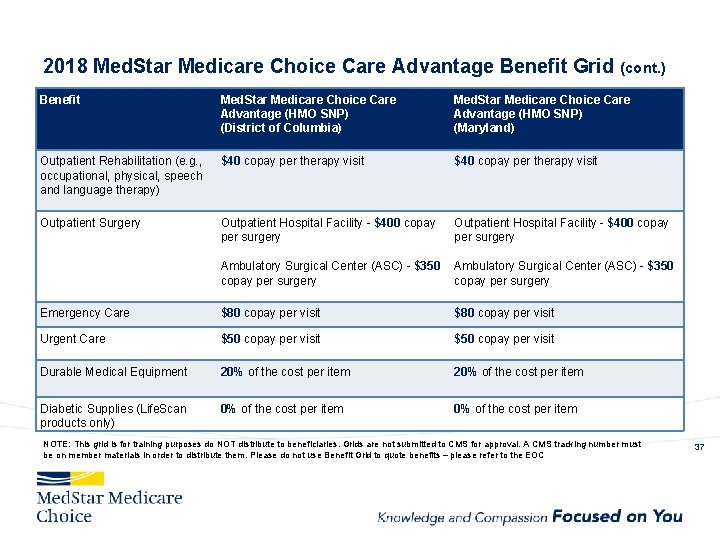
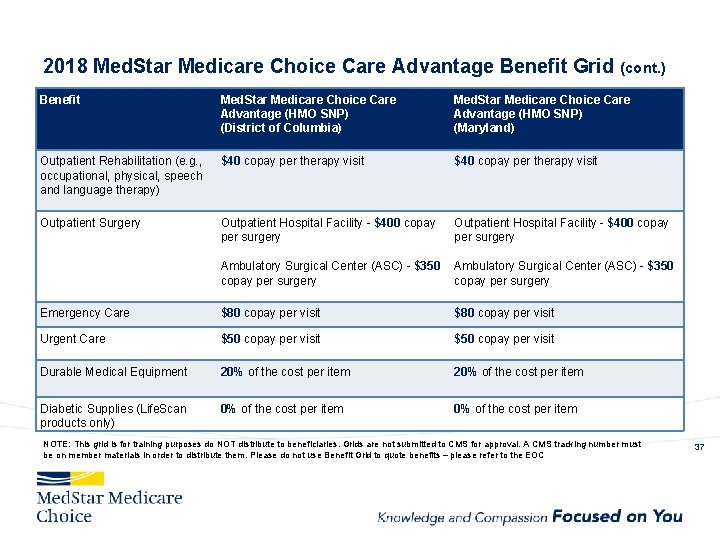
2018 Med. Star Medicare Choice Care Advantage Benefit Grid (cont. ) Benefit Med. Star Medicare Choice Care Advantage (HMO SNP) (District of Columbia) Med. Star Medicare Choice Care Advantage (HMO SNP) (Maryland) Outpatient Rehabilitation (e. g. , occupational, physical, speech and language therapy) $40 copay per therapy visit Outpatient Surgery Outpatient Hospital Facility - $400 copay per surgery Ambulatory Surgical Center (ASC) - $350 copay per surgery Emergency Care $80 copay per visit Urgent Care $50 copay per visit Durable Medical Equipment 20% of the cost per item Diabetic Supplies (Life. Scan products only) 0% of the cost per item NOTE: This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC 37
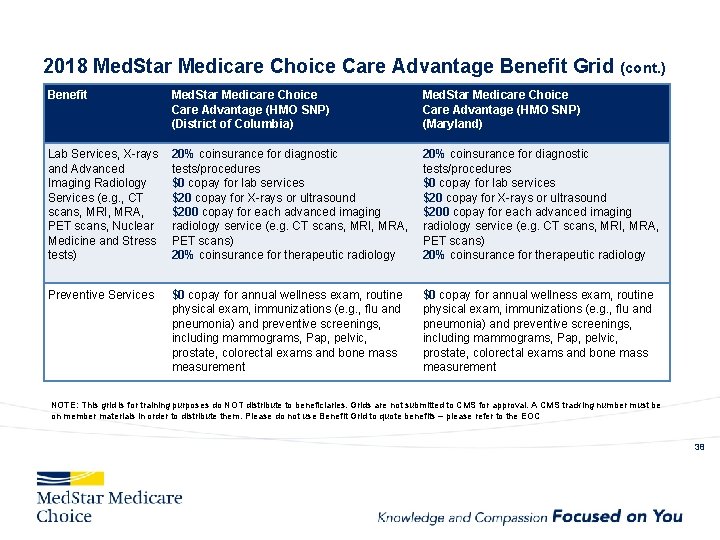
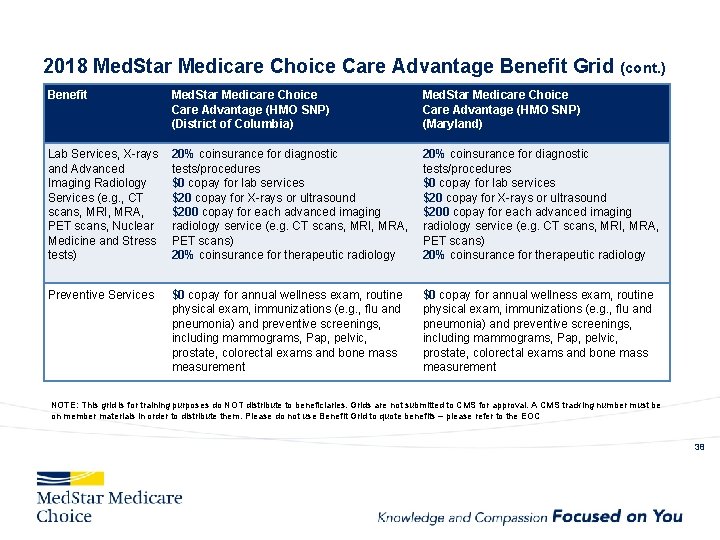
2018 Med. Star Medicare Choice Care Advantage Benefit Grid (cont. ) Benefit Med. Star Medicare Choice Care Advantage (HMO SNP) (District of Columbia) Med. Star Medicare Choice Care Advantage (HMO SNP) (Maryland) Lab Services, X-rays and Advanced Imaging Radiology Services (e. g. , CT scans, MRI, MRA, PET scans, Nuclear Medicine and Stress tests) 20% coinsurance for diagnostic tests/procedures $0 copay for lab services $20 copay for X-rays or ultrasound $200 copay for each advanced imaging radiology service (e. g. CT scans, MRI, MRA, PET scans) 20% coinsurance for therapeutic radiology Preventive Services $0 copay for annual wellness exam, routine physical exam, immunizations (e. g. , flu and pneumonia) and preventive screenings, including mammograms, Pap, pelvic, prostate, colorectal exams and bone mass measurement NOTE: This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC 38
2018 Med. Star Medicare Choice Care Advantage Additional Benefits and Services Our Med. Star Medicare Choice Care Advantage plan provides the following additional benefits and services: Routine Vision Dental Services Fitness Benefit Nurse Line Transportation Services 39
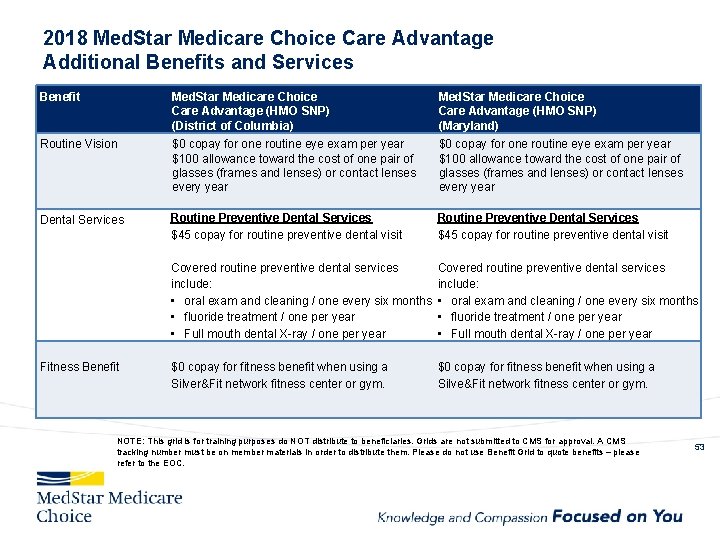
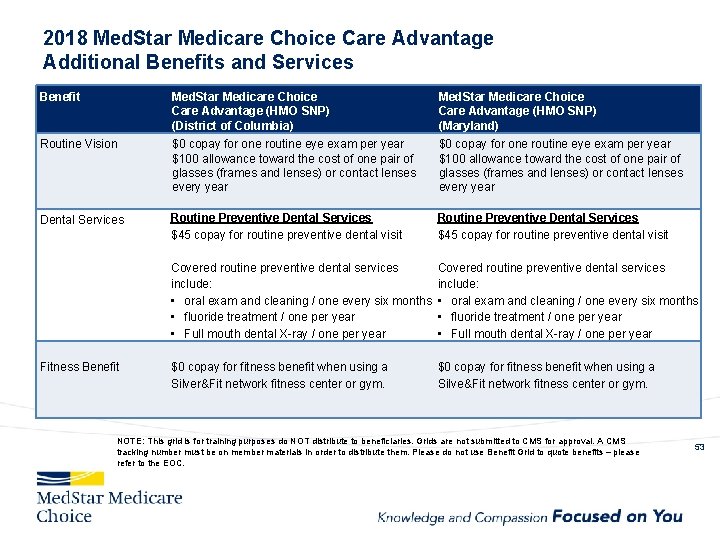
2018 Med. Star Medicare Choice Care Advantage Additional Benefits and Services Benefit Med. Star Medicare Choice Care Advantage (HMO SNP) (District of Columbia) Med. Star Medicare Choice Care Advantage (HMO SNP) (Maryland) Routine Vision $0 copay for one routine eye exam per year $100 allowance toward the cost of one pair of glasses (frames and lenses) or contact lenses every year Dental Services Routine Preventive Dental Services $45 copay for routine preventive dental visit Covered routine preventive dental services include: • oral exam and cleaning / one every six months • fluoride treatment / one per year • Full mouth dental X-ray / one per year $0 copay for fitness benefit when using a Silver&Fit network fitness center or gym. $0 copay for fitness benefit when using a Silve&Fit network fitness center or gym. Fitness Benefit NOTE: This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC. 53
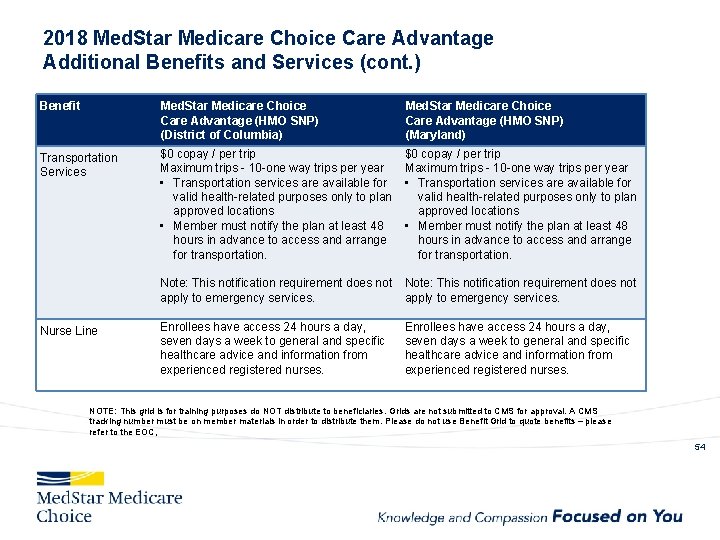
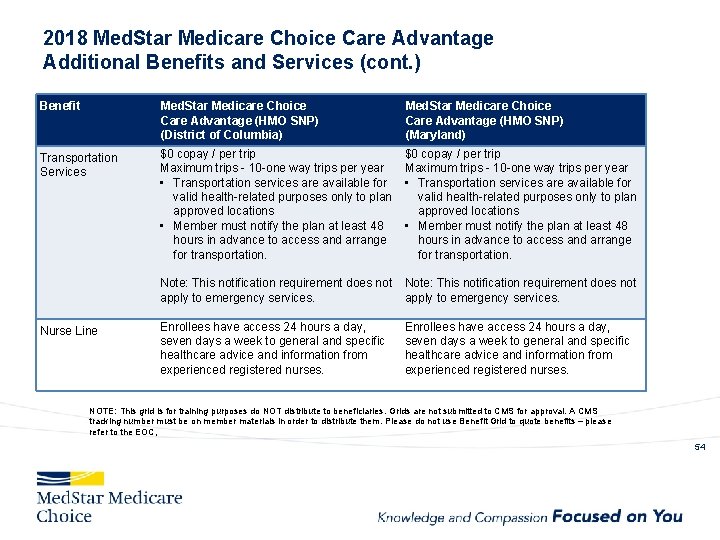
2018 Med. Star Medicare Choice Care Advantage Additional Benefits and Services (cont. ) Benefit Med. Star Medicare Choice Care Advantage (HMO SNP) (District of Columbia) Med. Star Medicare Choice Care Advantage (HMO SNP) (Maryland) Transportation Services $0 copay / per trip Maximum trips - 10 -one way trips per year • Transportation services are available for valid health-related purposes only to plan approved locations • Member must notify the plan at least 48 hours in advance to access and arrange for transportation. Note: This notification requirement does not apply to emergency services. Nurse Line Enrollees have access 24 hours a day, seven days a week to general and specific healthcare advice and information from experienced registered nurses. NOTE: This grid is for training purposes do NOT distribute to beneficiaries. Grids are not submitted to CMS for approval. A CMS tracking number must be on member materials in order to distribute them. Please do not use Benefit Grid to quote benefits – please refer to the EOC, 54
Additional Plan Information 42
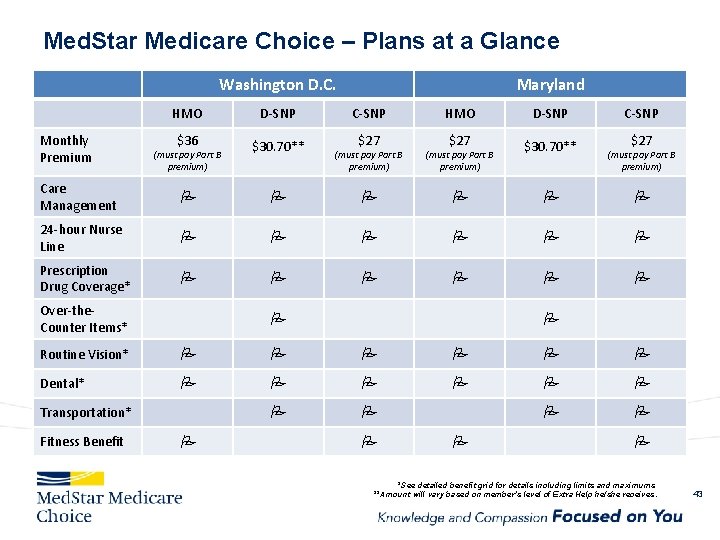
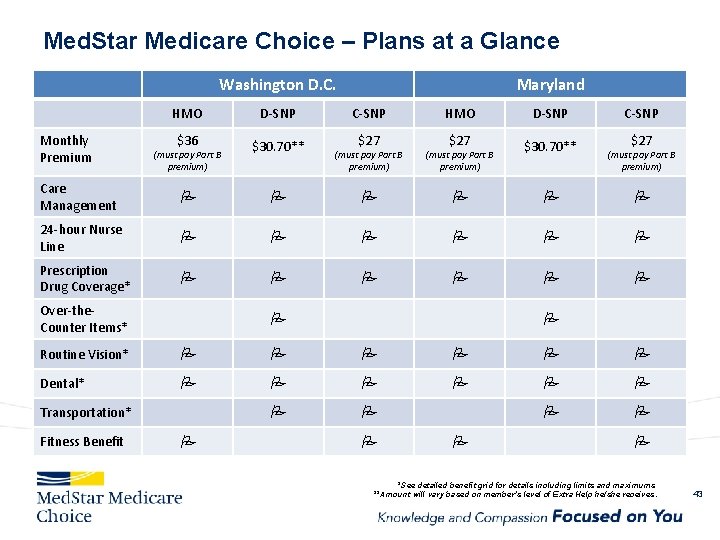
Med. Star Medicare Choice – Plans at a Glance Washington D. C. HMO D-SNP $36 $30. 70** Care Management 24 -hour Nurse Line Prescription Drug Coverage* Monthly Premium Maryland C-SNP D-SNP C-SNP (must pay Part B premium) $27 $30. 70** (must pay Part B premium) Over-the. Counter Items* $27 HMO $27 (must pay Part B premium) Routine Vision* Dental* Transportation* Fitness Benefit *See detailed benefit grid for details including limits and maximums **Amount will vary based on member’s level of Extra Help he/she receives. 43

Med. Star Medicare Choice Website www. Med. Star. Medicare. Choice. com • • Enroll online!! Provider Directory Provider Nomination Form Medical Benefit Summary Member Portal Member Documents And more… 44

Stars Program
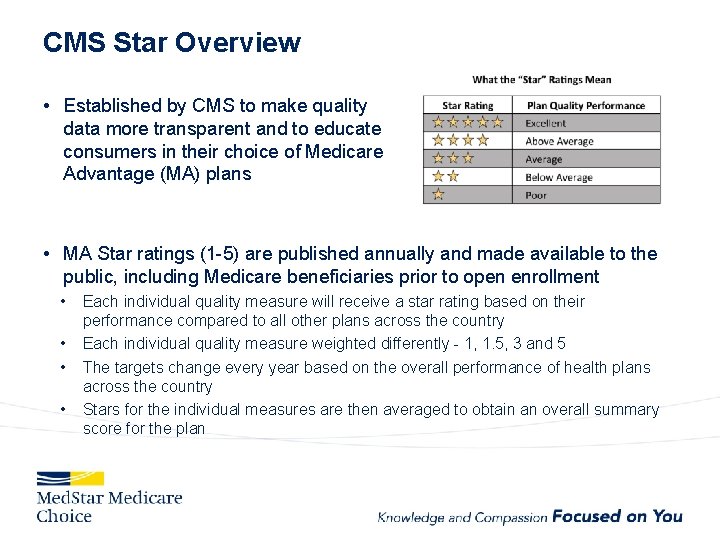
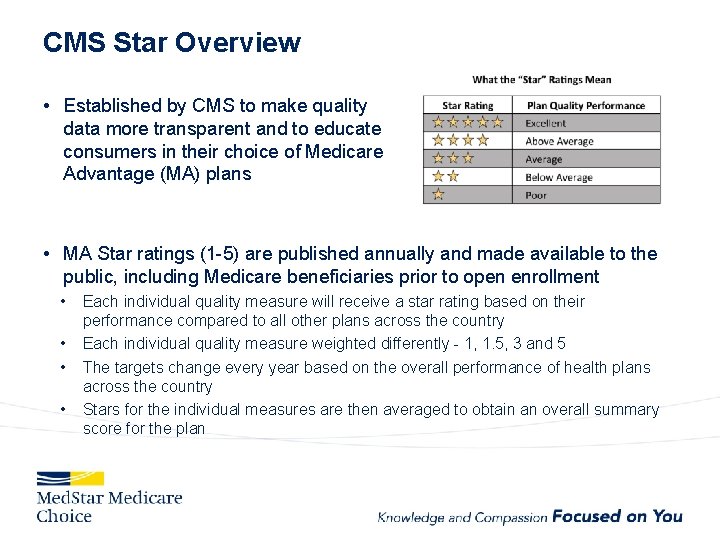
CMS Star Overview • Established by CMS to make quality data more transparent and to educate consumers in their choice of Medicare Advantage (MA) plans • MA Star ratings (1 -5) are published annually and made available to the public, including Medicare beneficiaries prior to open enrollment • • Each individual quality measure will receive a star rating based on their performance compared to all other plans across the country Each individual quality measure weighted differently - 1, 1. 5, 3 and 5 The targets change every year based on the overall performance of health plans across the country Stars for the individual measures are then averaged to obtain an overall summary score for the plan
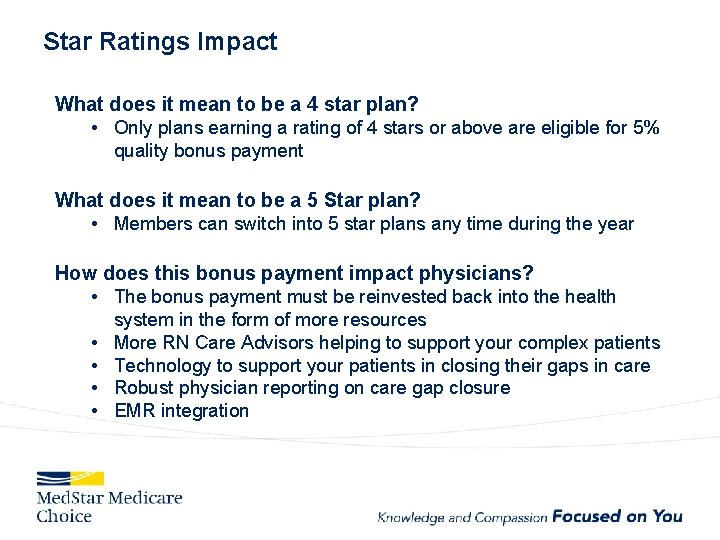
Star Ratings Impact What does it mean to be a 4 star plan? • Only plans earning a rating of 4 stars or above are eligible for 5% quality bonus payment What does it mean to be a 5 Star plan? • Members can switch into 5 star plans any time during the year How does this bonus payment impact physicians? • The bonus payment must be reinvested back into the health • • system in the form of more resources More RN Care Advisors helping to support your complex patients Technology to support your patients in closing their gaps in care Robust physician reporting on care gap closure EMR integration
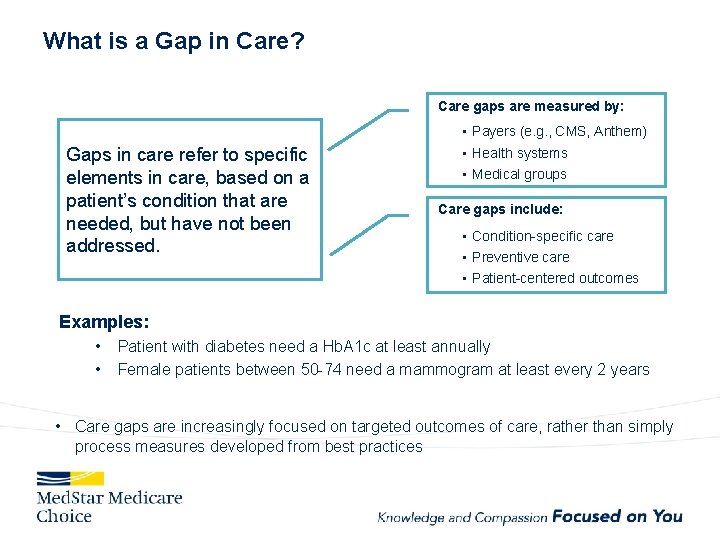
What is a Gap in Care? Care gaps are measured by: Gaps in care refer to specific elements in care, based on a patient’s condition that are needed, but have not been addressed. • Payers (e. g. , CMS, Anthem) • Health systems • Medical groups Care gaps include: • Condition-specific care • Preventive care • Patient-centered outcomes Examples: • • Patient with diabetes need a Hb. A 1 c at least annually Female patients between 50 -74 need a mammogram at least every 2 years • Care gaps are increasingly focused on targeted outcomes of care, rather than simply process measures developed from best practices
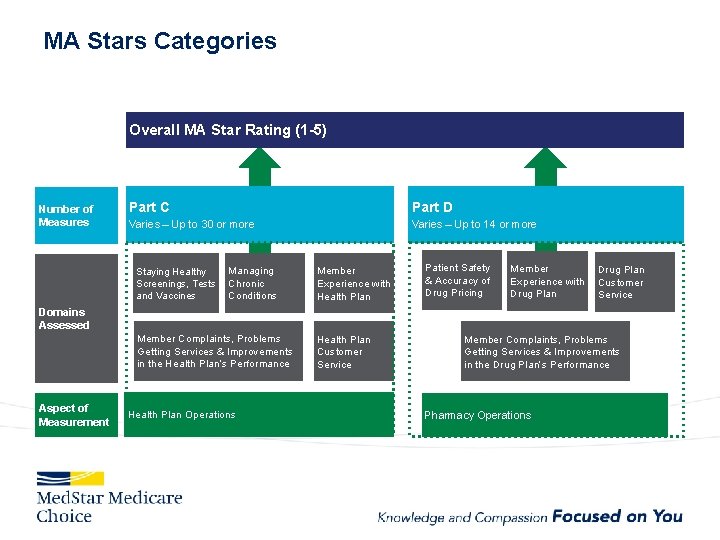
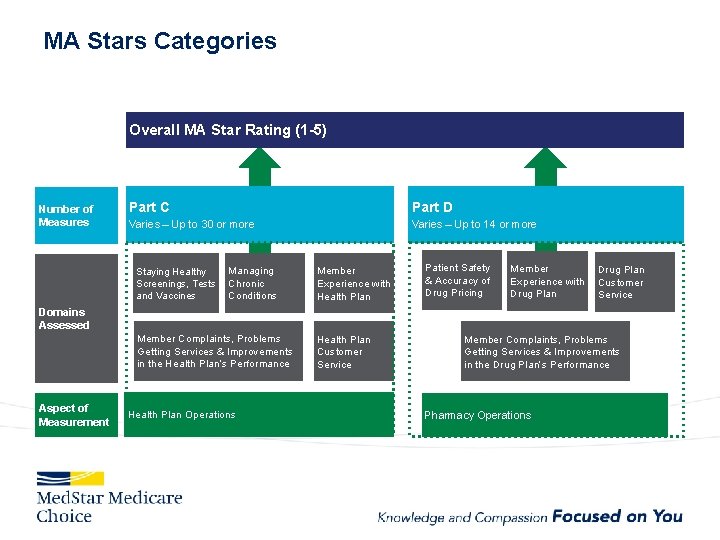
MA Stars Categories Overall MA Star Rating (1 -5) Number of Measures Part C Part D Varies – Up to 30 or more Varies – Up to 14 or more Managing Staying Healthy Screenings, Tests Chronic and Vaccines Conditions Member Experience with Health Plan Member Complaints, Problems Getting Services & Improvements in the Health Plan’s Performance Health Plan Customer Service Patient Safety & Accuracy of Drug Pricing Member Drug Plan Experience with Customer Drug Plan Service Domains Assessed Aspect of Measurement Health Plan Operations Member Complaints, Problems Getting Services & Improvements in the Drug Plan’s Performance Pharmacy Operations
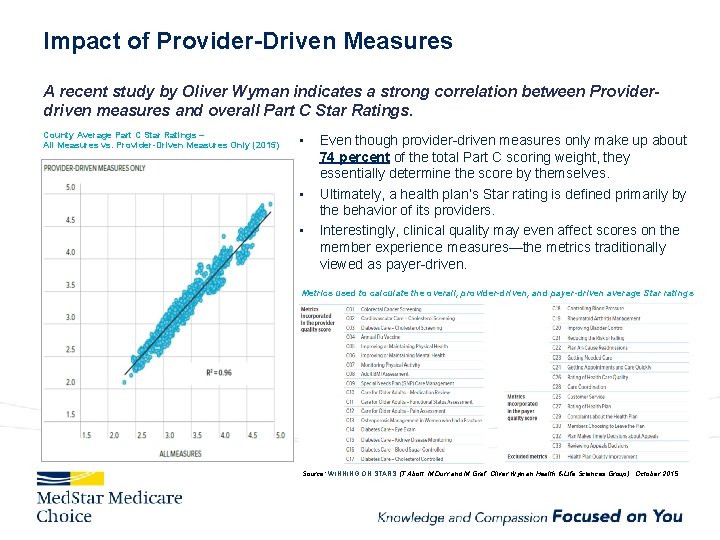
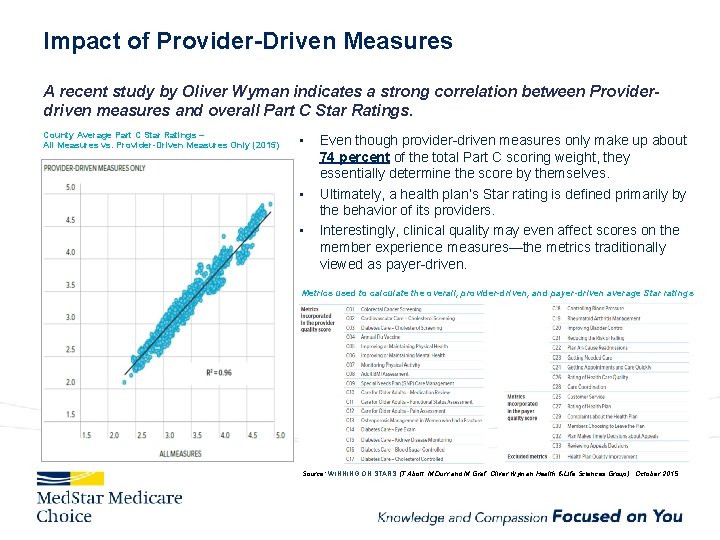
Impact of Provider-Driven Measures A recent study by Oliver Wyman indicates a strong correlation between Providerdriven measures and overall Part C Star Ratings. County Average Part C Star Ratings – All Measures vs. Provider-Driven Measures Only (2015) • • • Even though provider-driven measures only make up about 74 percent of the total Part C scoring weight, they essentially determine the score by themselves. Ultimately, a health plan’s Star rating is defined primarily by the behavior of its providers. Interestingly, clinical quality may even affect scores on the member experience measures—the metrics traditionally viewed as payer-driven. Metrics used to calculate the overall, provider-driven, and payer-driven average Star ratings Source: WINNING ON STARS (T. Abott, M. Durr and M. Graf, Oliver Wyman Health & Life Sciences Group), October 2015

Site Visits to Physician Offices § Our Population Health Managers (PHM): Regina Barnes – Southern Maryland, Shah rbarnes@evolenthealth. com (571) 217 -0115 Michelle Winterstein – D. C. , Inter. Med mwinterstein@evolenthealth. com; 571 -225 -5818 Stephanie Wood - Baltimore swood@evolenthealth. com 571 -214 -1733
CAHPS Background • The Consumer Assessment of Healthcare Providers and Systems (CAHPS) Survey is a patient survey rating health care experiences. • It has been conducted annually since 1995 and focuses on healthcare quality and enrollee experiences. These include: • Coordination of health care services (includes specialist referrals • • • and follow up) Access to providers (getting needed care in a timely manner) Customer service Overall quality of the health plan (including the Part D prescription drug benefit) Overall health care quality CAHPS survey is funded and overseen by the Agency for Healthcare Research and Quality (AHRQ), a government organization.
2017 CAHPS Strategy • It’s important to focus on member experience during every visit • Ensure members receive follow up on all screenings and tests • Encourage all members to have a PCP visit each year • The CAHPS survey typically goes out in the March timeframe • Members generally remember their experiences in the last 90 days Link to the CAHPS survey: http: //www. ma-pdpcahps. org/en/survey-instruments/
Help to Improve our CAHPS Score! Remind physicians that flu immunization is a member self reported measure included in the CAHPS survey The following are best practices to increase flu vaccine rates: • Consider standing orders for MA staff to screen members for flu vaccine during rooming process (consider linking with pneumonia vaccine) • Document administration of the flu vaccine in your EMR • Creation of flu clinic hours for walk in patients and consider expanded hours • Identify priority high risk patients and reach out to coordinate vaccinations with upcoming visits
Keys to Stars Success • Ensure members have a positive experience during every touchpoint • Example: staff asking “is there anything else I can do for you? ” • Remind physicians to close care gaps during every patient encounter • Remember one member and one measure can be the difference in Med. Star Medicare Choice achieving a 4 star rating • Encourage physicians to leverage the RAF visit for assessment and comprehensive care that closes gaps in care
RAF (Risk Adjustment and Patient Assessment Forms)
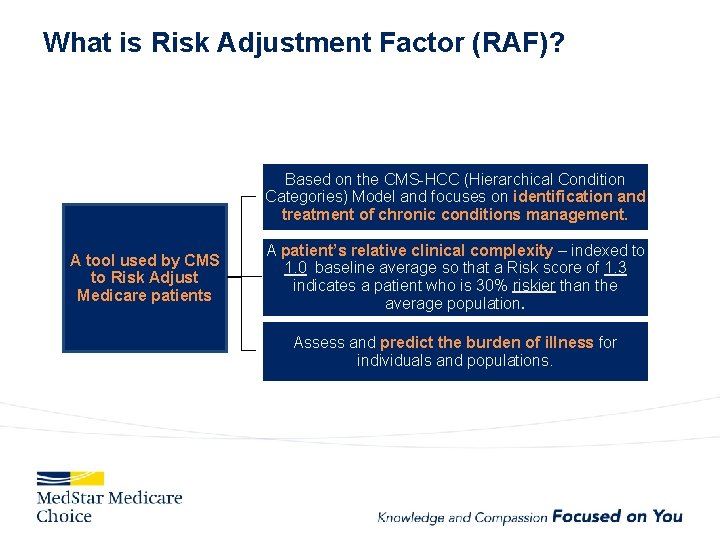
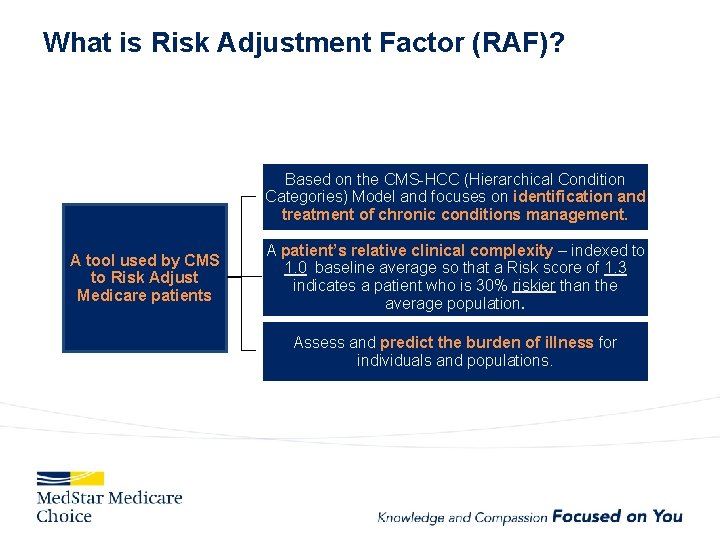
What is Risk Adjustment Factor (RAF)? Based on the CMS-HCC (Hierarchical Condition Categories) Model and focuses on identification and treatment of chronic conditions management. A tool used by CMS to Risk Adjust Medicare patients A patient’s relative clinical complexity – indexed to 1. 0 baseline average so that a Risk score of 1. 3 indicates a patient who is 30% riskier than the average population. Assess and predict the burden of illness for individuals and populations.
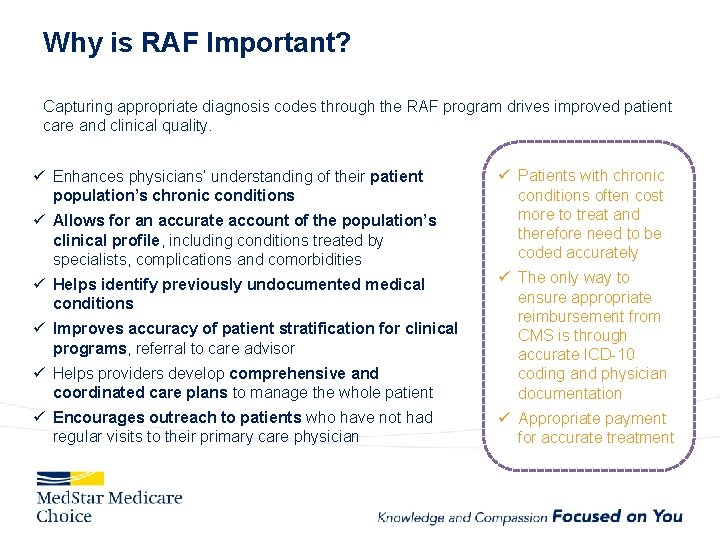
Why is RAF Important? Capturing appropriate diagnosis codes through the RAF program drives improved patient care and clinical quality. ü Enhances physicians’ understanding of their patient population’s chronic conditions ü Allows for an accurate account of the population’s clinical profile, including conditions treated by specialists, complications and comorbidities ü Patients with chronic conditions often cost more to treat and therefore need to be coded accurately ü Helps providers develop comprehensive and coordinated care plans to manage the whole patient ü The only way to ensure appropriate reimbursement from CMS is through accurate ICD-10 coding and physician documentation ü Encourages outreach to patients who have not had regular visits to their primary care physician ü Appropriate payment for accurate treatment ü Helps identify previously undocumented medical conditions ü Improves accuracy of patient stratification for clinical programs, referral to care advisor
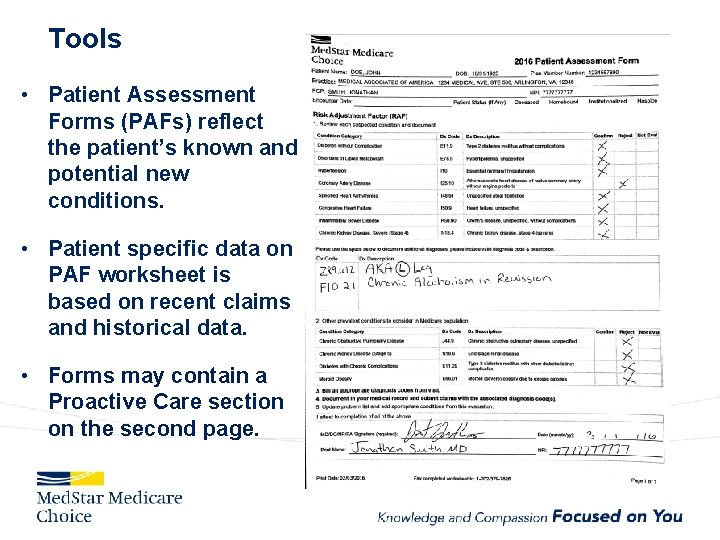
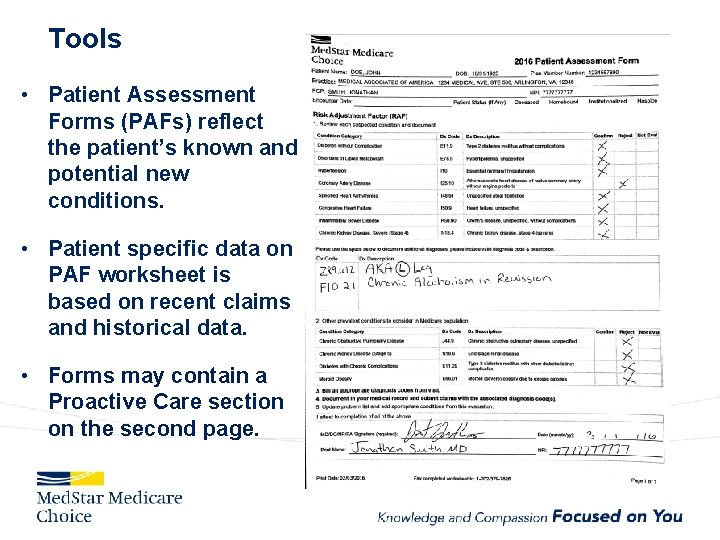
Tools • Patient Assessment Forms (PAFs) reflect the patient’s known and potential new conditions. • Patient specific data on PAF worksheet is based on recent claims and historical data. • Forms may contain a Proactive Care section on the second page.
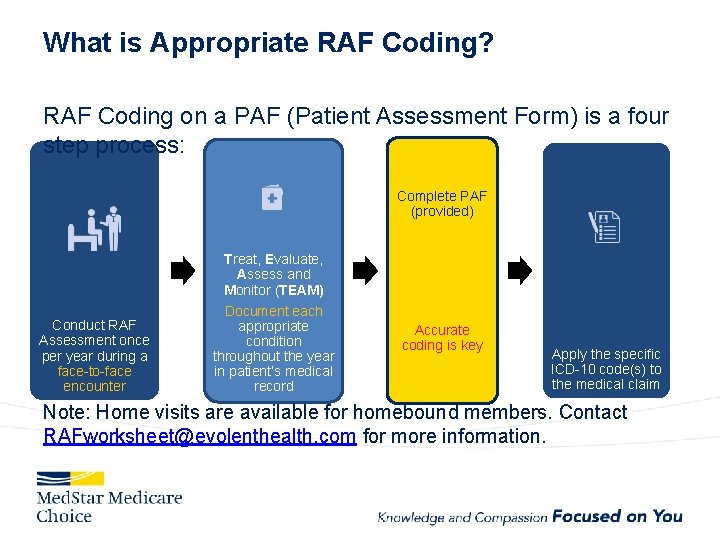
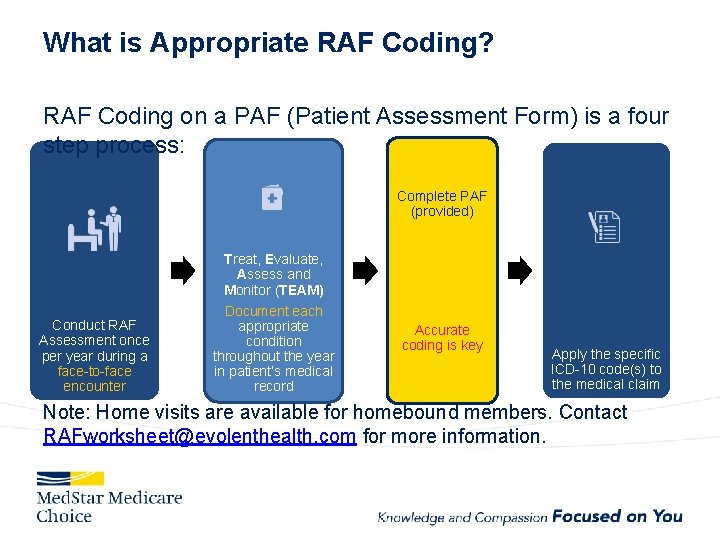
What is Appropriate RAF Coding? RAF Coding on a PAF (Patient Assessment Form) is a four step process: Complete PAF (provided) Conduct RAF Assessment once per year during a face-to-face encounter Treat, Evaluate, Assess and Monitor (TEAM) Document each appropriate condition throughout the year in patient’s medical record Accurate coding is key Apply the specific ICD-10 code(s) to the medical claim Note: Home visits are available for homebound members. Contact RAFworksheet@evolenthealth. com for more information.
Ask of Providers – RAF 1. Conduct RAF Assessment once per year during a faceto-face encounter 2. Document treatment and plan for each condition addressed in the medical record 3. Bill all conditions addressed in the encounter – Work with the Practice’s Billing Vendor if the practice is limited in submitting less than all of a patient’s conditions 4. Complete the PAF Worksheet • Sign the Worksheet (mandatory) 5. Send completed Worksheet to Med. Star Medicare Choice via: • • Fax 202. 379. 7826 Scan/Email to RAFworksheet@evolenthealth. com
Coding Variations • 99429 is billed as an enhanced annual exam • If a patient comes in with a sickness, 99429 can be billed in conjunction with the office visit, e. g. – 99213 for an office visit and 99429 for the RAF visit – Notes • Other codes will require the patient to pay a copay • A modifier 25 is not required • For RAF visits, use 99429 instead of a G code • Support for RAF – RAF Questions: 855. 222. 1041 – General billing questions: Provider Services: 855. 222. 1042
Payment for Providers receive payment/are reimbursed by 1. 2. 3. Conducting an appointment; Submitting the completed PAF worksheet; and Billing the office visit with CPT Code 99429 • Reimbursement for the visit and submission of the accurately completed PAF worksheet is $200. 00 • Copayment, coinsurance and deductible amounts, if any, are waived for these visits • 0. 5 CME Credits are available for viewing the RAF education video – Med. Star. Provider. Network. org
RAF and Proactive Care Together: The Right Care for An Entire Population § Leverage the RAF visit to provide opportunity for assessment and comprehensive care that closes gaps before they occur § Address a member’s gaps in care during the visit § RAF efforts improve the accuracy of patient inclusion in Star measure calculations
SNP MOC (Model of Care)
Profile of a SNP Enrollee • When compared with the general Medicare population, SNP enrollees are: – A larger share of the population in fair/poor health – Greater incidence of cognitive/mental impairments (58% v. 25%) – Greater incidence of functional impairments (44% vs. 26%) – Greater incidence of facility living (13% vs. 1%) – Higher hospitalization rates (26% vs. 18%) – 1. 8 times higher spending on average (~$14, 000+) – More chronic conditions – More transitions of care – Higher proportion of low income, under 65 disabled, and minority beneficiaries
Medicare Choice SNP MOC (Model of Care) o The Model of Care aims to improve the patient’s access, coordination of care, and transitions of care. o Model of Care is best practice as it offers the following benefits: • High level of attention to the patient’s specific health and individual needs • Health Assessments to identify risks and concerns • Individualized attention and coordination of care from assigned Case Advisors • Individualized Care Plan (ICP) • Transition of care across healthcare settings and providers • Network Providers experienced with SNP Members
Medicare Choice SNP MOC Provider Training CMS requires provider training on essential information about special needs plans and special needs members. We offer Flexible Online Training: 1. 2. 3. 4. Start by clicking the link: http: //medstarprovidernetwork. org/mc_earn_175_mce. html Providers will receive an email notification with Login Instructions Complete the training and print the CME Certification Sign the Attestation and 1. 2. 5. Fax to 703. 890. 1636; or Email to pophealthtraining@evolenthealth. com Providers will be eligible to receive 1. 75 CME credits upon training completion.
Medicare Choice SNP MOC - Value to Physician Practices Improved care plan management • Care team helps patients follow doctor’s orders and schedules follow-up appointments • Pharmacists perform medication reconciliation Earlier identification of potential health concerns • Medicare Choice covers a full in-depth physical exam, including elements not covered under Original Medicare • Med. Star’s systems will identify patients to predict who may be at risk for catastrophic medical events Reduced no-show appointments • Transportation benefits increase the likelihood of the patient showing up for their appointment Increased administrative efficiency • No deductibles on office visits • Care Managers use Med. Star’s EMR to coordinate with physicians • Care Advisors will help manage most demanding patients, which may reduce calls to physician offices
Provider Resources

Provider Website
Provider Website Resources Certificate of Coverage Provider Manual Medical Policies & Payment Policies Utilization Management information including Prior Authorization requirements Pharmacy information including protocols and the formulary (and a list of drugs covered under the medical benefit) Behavioral Health Resources Provider Directory Provider Newsletters Notice of Privacy Practices Quick Reference Guide (including contact information) Medical Management services and forms Provider On. Line for access to claim information Training Opportunities
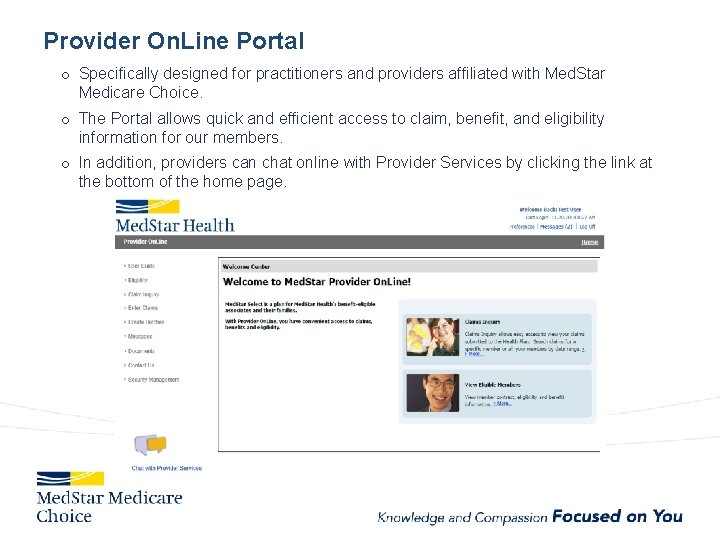
Provider On. Line Portal o Specifically designed for practitioners and providers affiliated with Med. Star Medicare Choice. o The Portal allows quick and efficient access to claim, benefit, and eligibility information for our members. o In addition, providers can chat online with Provider Services by clicking the link at the bottom of the home page.
Provider On. Line Portal 1. Direct Provider Services Communicating • • • Save time by messaging or chatting online with Provider Services through the Provider On. Line Portal. Communications are sent directly to the appropriate service area by selecting applicable topic. Providers have the options to select topics such as, but not limited to, Eligibility, Authorization Inquiry, Claim Inquiry, or Batch Inquiry. Register for the Provider On. Line Portal today! Sign up through https: //secure. togetherforyourhealth. com/Web. Requests/Security. Request. aspx? CL IENT=000101&ID=000001&DIV=0001 For further information on the Provider On. Line Portal, please contact Provider Services as 855. 242. 1042.
Provider On. Line Portal-Continued Providers are able to: 2. Check Eligibility & Benefits • Member eligibility verification in ONE easy step. • Simply enter the Member ID, Last name, and First name, then click search. • Eligibility results for applicable dependents and subscribers display within seconds. The result details show the member's specific benefits and effective date of benefits. 3. Submit Claims • Offers a CST (Claims Submission Tool) that provides a complete Internet Portal solution for services provided by Health plan. 4. Check Claim Status • The Claim Inquiry search allows providers to search by member or claim information online to obtain real-time claim status. • Detailed HCFA and UB claim detail is supplied, including adjustment reasons by clicking on the applicable claim from the search results. • Providers who have questions on claims can compose an email to Provider Services on the claim detail screen directly.
Claims Submission 1. Direct Submission o Submit claims through Provider On. Line (provider portal) online on www. Med. Star. Provider. Network. org o Register online or through Provider Services at 855. 222. 1042 2. Clearinghouse EDI Submission (recommended) o Providers with existing relationships with clearinghouses such as Emdeon, Relay Health, Allscripts may continue submitting claims in the format used by their billing software. o o Clearinghouses will reformat to meet HIPAA standards Electronic Submission: Payer ID 251 MS 3. Paper Claims Submission Paper claims can be submitted to: Claims Processing Center P. O. BOX 1200 Pittsburgh, PA 15230 -1200 Key Reminders Claims must be submitted within 180 days of date of service COB claims – within 180 days of the primary EOP remittance *Applies to all transmission Options
Electronic Prior Authorization Submission-New! • A new module to submit prior authorizations electronically will be available in 2018. Access to web-based submissions through Identifi Practice will be a phased roll-out with select practices kicking off the process in early October 2017. • You will have the option to access this functionality through Provider On. Line through Single Sign On, or you can choose to access Identifi Practice directly. • If you are interested in obtaining access to submission requests through Provider On. Line or through Identifi Practice, please notify MFCProvider. Relations 2@medstar. net to request permission and indicate if you are interested in accessing through Provider On. Line or directly into Identifi Practice. • If you are seeking access through Provider On. Line, you must be a registered user before the Electronic Authorization Submission functionality can be offered. If you are not currently registered with Provider On. Line, instructions are located at Med. Star. Provider. Network. org. A registered Administrator to Provider On. Line within your practice can grant access to additional users. • For technical issues related to Electronic Authorization submission, please contact support@evolenthealth. com.
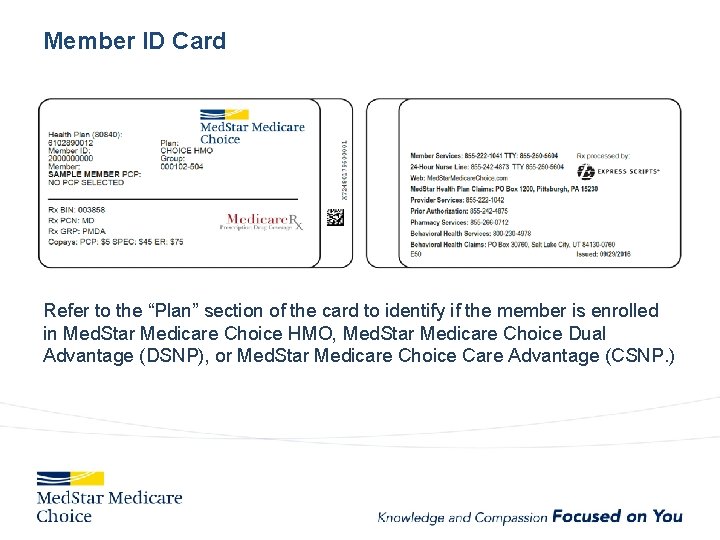
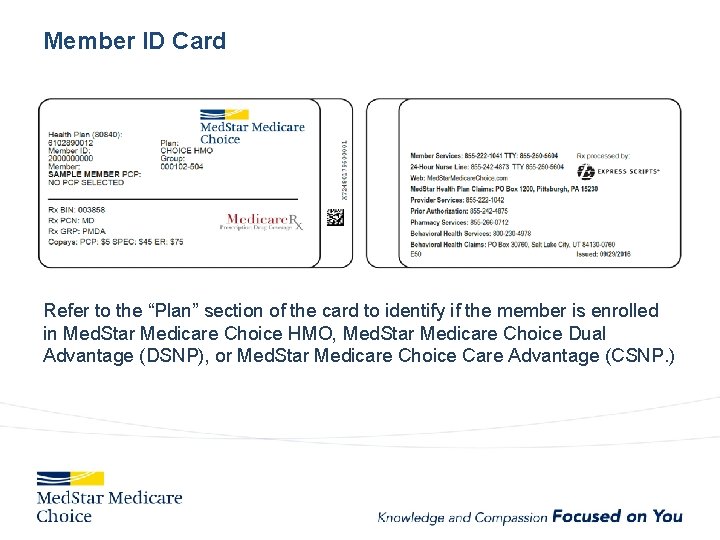
Member ID Card Refer to the “Plan” section of the card to identify if the member is enrolled in Med. Star Medicare Choice HMO, Med. Star Medicare Choice Dual Advantage (DSNP), or Med. Star Medicare Choice Care Advantage (CSNP. )
Provider Appeals and Grievances o Written appeal to Med. Star Health Plan must be submitted by provider within 180 (medical necessity) or 120 (administrative) business days of the denial notification o The QRG is updated frequently and is a good source of information: o http: //medstarprovidernetwork. org/medicare-choice/quick-reference-guide o http: //medstarprovidernetwork. org/medstar-select/quick-reference-guide-frequentlyupdated o Call Medical Management at 855. 242. 4875 to request an expedited review for an appeal. Clinical documentation is required. Use these forms to assist with Appeals, Grievances and Provider Issues found on Med. Star. Provider. Portal. org: • • Administrative Reconsideration Request Claim Appeal Request Formal Appeal Request Provider Claim Project Assistance Request
In-Network Referrals . All providers are expected to utilize participating providers when making referrals. Please refer to the online directory at Med. Star. Provider. Network. org for a list of participating providers, or contract provider services at 855 -222 -1042 for assistance. Please refer laboratory services to the following in-network laboratories: • Laboratories at Med. Star Health facilities • Quest (includes genetic testing services) • Lab. Corp (includes genetic testing services) Please refer dialysis services to participating Dialysis centers: • • • Fresenius Medical Care Da. Vita ARA-Adelphia LLC BMA Capital Dialysis, LLC • • • FMC RAI Howard University Dialysis Center, LLC QCDC Southern Maryland Universal Dialysis Center. LLC
Annual Required Trainings. Med. Star Medicare Choice requires that provider complete the following trainings annually: • • • RAF Training • 0. 5 CME Credit Hours SNP Model of Care Training • 1. 75 CME Credit Hours CMS Mandated General Compliance and FWA Trainings and attestation forms are available on Med. Star. Provider. Network. com at the following link: http: //medstarprovidernetwork. com/medicare-choice/available-providertrainings
Med. Star Health Verbal Consent MD, VA, and DC Regulations Verbal Consent to provide personal health information for an adult to another person is not permitted in MD, DC, or VA. Therefore, for Med. Star, all consent must be in writing before any PHI can be released for an adult member. Members are required to fill out a release form which can be obtained from Member Services. It is in the process of being added to the www. Med. Star. My. Health. org and to www. Med. Star. Provider. Network. org.

Fraud, Waste & Abuse
Fraud Waste and Abuse • Fraud is an intentional act of deception, misrepresentation, or concealment in order to gain something of value. • Waste is over-utilization of services and the misuse of resources. • Abuse is excessive or improper use of services or actions that are inconsistent with acceptable business or medical practice. • Sanctions can include revocation of license and suspension of payments. • Penalties can include fines and prison sentences. • You have a responsibility to report any possible cases of fraud, waste and abuse. Calls can be placed anonymously. • Med. Star Health Integrity Hotline: Call 877. 811. 3411 If you identify or suspect fraudulent activities/behaviors, report immediately!
Med. Star Health Compliance Program to Combat Fraud Waste and Abuse What is Med. Star Health doing to combat fraud, waste and abuse? • • Monitor claims for accuracy, ensuring coding reflects service provided. Monitor medical records ensuring documentation supports services rendered. Perform regular internal audits. Establish effective lines of communication with colleagues and staff members and contracted providers. • Ask about potential compliance issues in exit interviews. • Take action when a problem has been identified. • Med. Star Health has a non-retaliation policy – no fear of retribution for reporting fraud.

Medicare Appendix
Medicare Part A Overview What is Medicare Part A? • Medicare Part A is part of original Medicare, which generally includes coverage for hospital care, skilled nursing facility care, nursing home care, hospice and home health services. Medicare Part A Eligibility? • Medicare Part A eligibility is determined if a person is 65 years or older, of any age with disabilities, a citizen or permanent resident of the United States, and they or a spouse worked for at least 10 years in Medicare-covered employment. Medicare Part A Costs? • In most cases, there is no premium for Medicare Part A. However, there are costs that may be associated with coverage under Medicare Part A including, deductibles for inpatient hospital care, co-pays for skilled nursing and inpatient hospital stays, and payments for long-term custodial care. 87
Medicare Part B Overview What is Medicare Part B? • Medicare Part B is part of original Medicare, which is generally medical and preventative care insurance, and covers services such as outpatient and professional medical services. Outpatient services, surgery, labs, x-rays, ambulance, durable medical equipment and supplies, and preventive services are also typically covered expenses. Medicare Part B Eligibility? • Medicare Part B eligibility is determined if a person is 65 years or older, a citizen or permanent resident of the United States, and they or a spouse worked for at least 10 years in Medicare-covered employment. Those with a disability or those who have been diagnosed with End-Stage Renal Kidney disease may also be eligible. Medicare Part B Costs? • Medicare Part B provides insurance to partially cover the costs of medically necessary care, for which most people pay a monthly premium. In addition to the Part B monthly premium, there is a required annual deductible. Also, individuals with Part B coverage are responsible for a percentage of the cost (coinsurance) that part B does not cover. 88
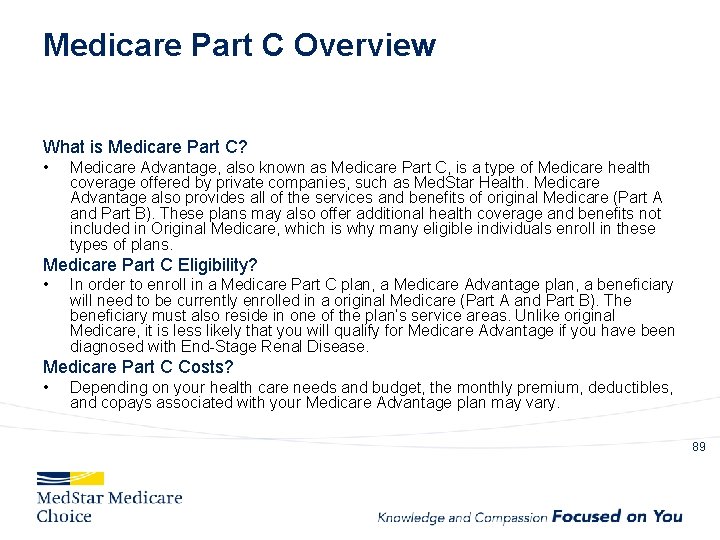
Medicare Part C Overview What is Medicare Part C? • Medicare Advantage, also known as Medicare Part C, is a type of Medicare health coverage offered by private companies, such as Med. Star Health. Medicare Advantage also provides all of the services and benefits of original Medicare (Part A and Part B). These plans may also offer additional health coverage and benefits not included in Original Medicare, which is why many eligible individuals enroll in these types of plans. Medicare Part C Eligibility? • In order to enroll in a Medicare Part C plan, a Medicare Advantage plan, a beneficiary will need to be currently enrolled in a original Medicare (Part A and Part B). The beneficiary must also reside in one of the plan’s service areas. Unlike original Medicare, it is less likely that you will qualify for Medicare Advantage if you have been diagnosed with End-Stage Renal Disease. Medicare Part C Costs? • Depending on your health care needs and budget, the monthly premium, deductibles, and copays associated with your Medicare Advantage plan may vary. 89
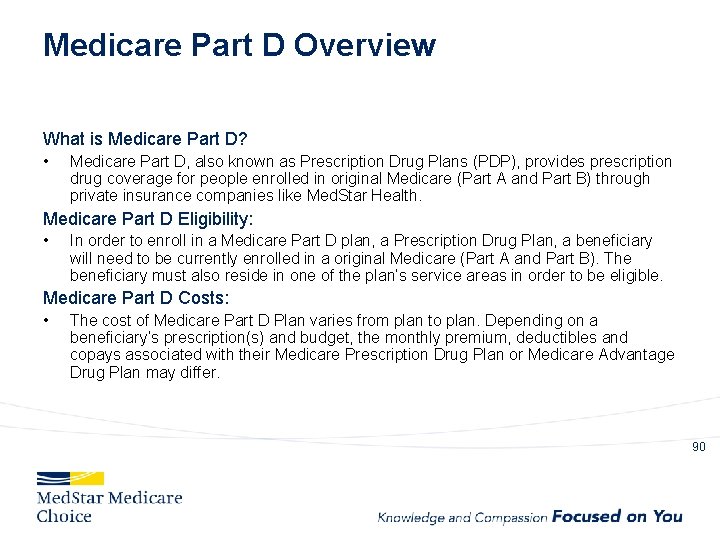
Medicare Part D Overview What is Medicare Part D? • Medicare Part D, also known as Prescription Drug Plans (PDP), provides prescription drug coverage for people enrolled in original Medicare (Part A and Part B) through private insurance companies like Med. Star Health. Medicare Part D Eligibility: • In order to enroll in a Medicare Part D plan, a Prescription Drug Plan, a beneficiary will need to be currently enrolled in a original Medicare (Part A and Part B). The beneficiary must also reside in one of the plan’s service areas in order to be eligible. Medicare Part D Costs: • The cost of Medicare Part D Plan varies from plan to plan. Depending on a beneficiary’s prescription(s) and budget, the monthly premium, deductibles and copays associated with their Medicare Prescription Drug Plan or Medicare Advantage Drug Plan may differ. 90
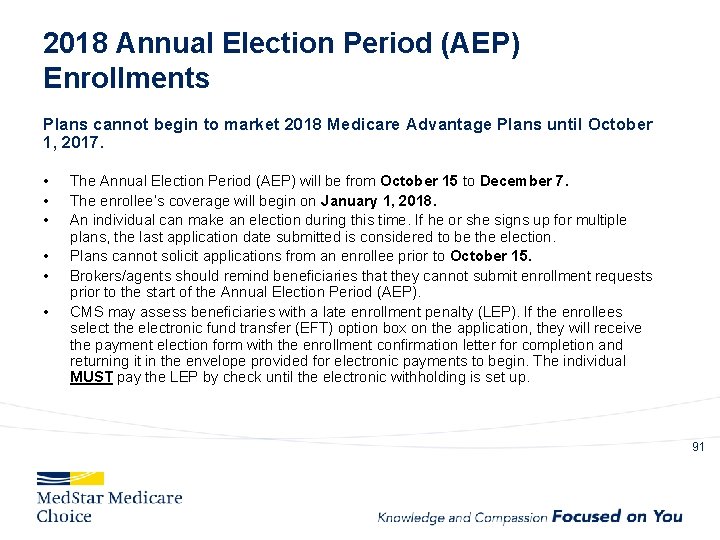
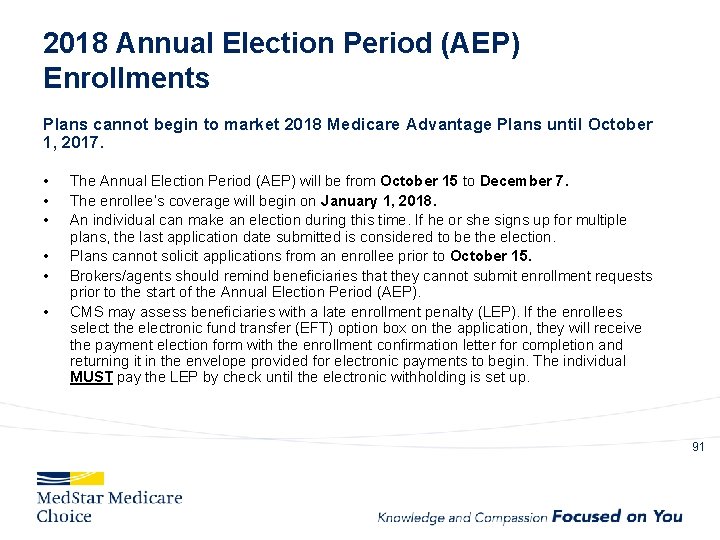
2018 Annual Election Period (AEP) Enrollments Plans cannot begin to market 2018 Medicare Advantage Plans until October 1, 2017. • • • The Annual Election Period (AEP) will be from October 15 to December 7. The enrollee’s coverage will begin on January 1, 2018. An individual can make an election during this time. If he or she signs up for multiple plans, the last application date submitted is considered to be the election. Plans cannot solicit applications from an enrollee prior to October 15. Brokers/agents should remind beneficiaries that they cannot submit enrollment requests prior to the start of the Annual Election Period (AEP). CMS may assess beneficiaries with a late enrollment penalty (LEP). If the enrollees select the electronic fund transfer (EFT) option box on the application, they will receive the payment election form with the enrollment confirmation letter for completion and returning it in the envelope provided for electronic payments to begin. The individual MUST pay the LEP by check until the electronic withholding is set up. 91
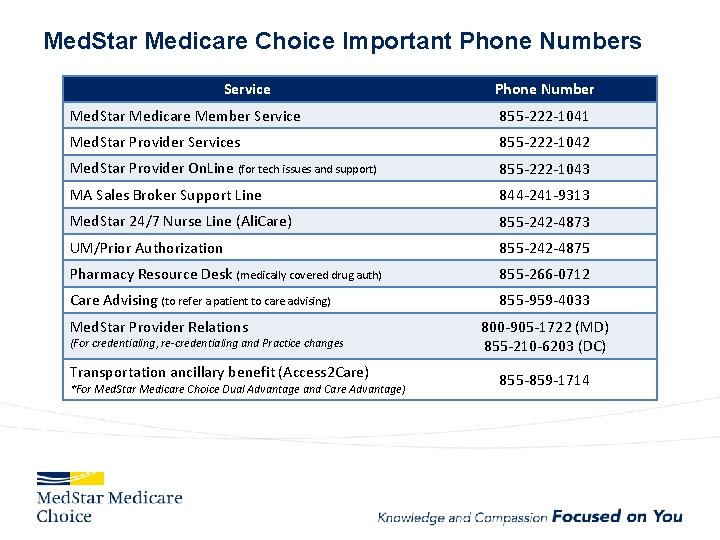
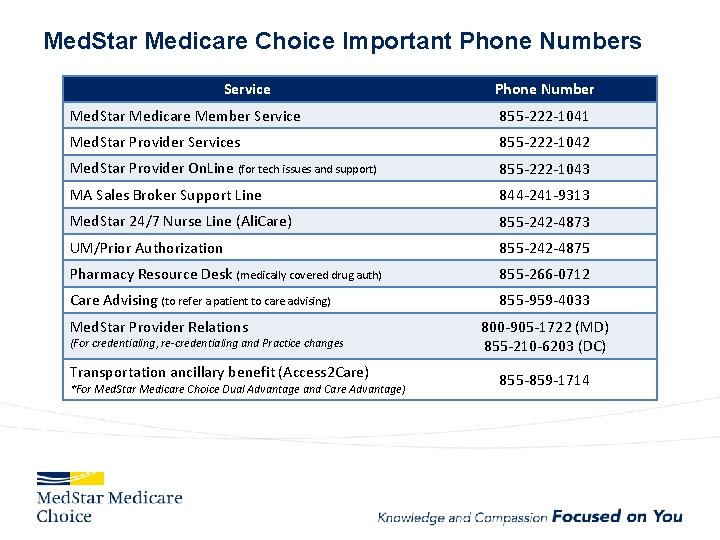
Med. Star Medicare Choice Important Phone Numbers Service Phone Number Med. Star Medicare Member Service 855 -222 -1041 Med. Star Provider Services 855 -222 -1042 Med. Star Provider On. Line (for tech issues and support) 855 -222 -1043 MA Sales Broker Support Line 844 -241 -9313 Med. Star 24/7 Nurse Line (Ali. Care) 855 -242 -4873 UM/Prior Authorization 855 -242 -4875 Pharmacy Resource Desk (medically covered drug auth) 855 -266 -0712 Care Advising (to refer a patient to care advising) 855 -959 -4033 Med. Star Provider Relations (For credentialing, re-credentialing and Practice changes Transportation ancillary benefit (Access 2 Care) *For Med. Star Medicare Choice Dual Advantage and Care Advantage) 800 -905 -1722 (MD) 855 -210 -6203 (DC) 855 -859 -1714
 Myrrh is mine its bitter perfume
Myrrh is mine its bitter perfume Projektbanken aau
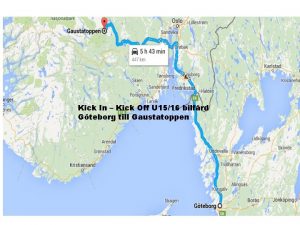
Projektbanken aau Uat kick off
Uat kick off Kick off briefing
Kick off briefing Contoh wbs
Contoh wbs Agenda for mentor meeting
Agenda for mentor meeting Kick off meeting agenda for construction project
Kick off meeting agenda for construction project Inisiasi proyek
Inisiasi proyek Kick off palaveri
Kick off palaveri Kick off mail
Kick off mail Uat sign off email template
Uat sign off email template Kickoff projeto
Kickoff projeto Erp kick off meeting presentation
Erp kick off meeting presentation Outi tasala
Outi tasala Kick off agenda
Kick off agenda Kick off bl
Kick off bl Kick off meeting portugal
Kick off meeting portugal Kick off stage is mandated for
Kick off stage is mandated for Kick off rugby
Kick off rugby Audit kick off meeting agenda
Audit kick off meeting agenda Project kick off meeting speech sample
Project kick off meeting speech sample Mentorship kickoff meeting
Mentorship kickoff meeting Clave kick off
Clave kick off Kuranda tedvir ne demek
Kuranda tedvir ne demek Hvor i det periodiske system står atomer med 5 skaller?
Hvor i det periodiske system står atomer med 5 skaller? Ao* algorithm in artificial intelligence
Ao* algorithm in artificial intelligence What does star stand for fccla
What does star stand for fccla Elbows off the table fingers off the food song
Elbows off the table fingers off the food song Dada la siguiente secuencia rusia 2018 rusia 2018
Dada la siguiente secuencia rusia 2018 rusia 2018 Inspect
Inspect Kicks for life
Kicks for life Rolling thunder kick
Rolling thunder kick Kick's law formula
Kick's law formula Penalty kicks multiplication
Penalty kicks multiplication Kick the ball song
Kick the ball song Gated oscillator
Gated oscillator Ekd system
Ekd system Psk foul
Psk foul Fences act 2 scene 5
Fences act 2 scene 5 Proportional kick
Proportional kick Adductoren tenotomie
Adductoren tenotomie Kick loop
Kick loop What is a corner kick in soccer
What is a corner kick in soccer Mammary gland cow
Mammary gland cow Kick boks tarihçesi
Kick boks tarihçesi Instep soccer kick
Instep soccer kick Kick ogf
Kick ogf Flap your wings
Flap your wings Kicked is transitive or intransitive
Kicked is transitive or intransitive Kick pipe
Kick pipe Kick back
Kick back National business group on health conference 2018
National business group on health conference 2018 Strategic plan 2018 to 2021
Strategic plan 2018 to 2021 Occupational health nurse roles and responsibilities
Occupational health nurse roles and responsibilities National programmes
National programmes Health standards louisiana
Health standards louisiana Difference between health education and promotion
Difference between health education and promotion Whole health circle of health
Whole health circle of health Health and social component 3
Health and social component 3 Health promotion world health organization
Health promotion world health organization Ucf kinesiology masters
Ucf kinesiology masters Chapter 3 health wellness and health disparities
Chapter 3 health wellness and health disparities Difference between health education and health propaganda
Difference between health education and health propaganda Chapter 1 understanding health and wellness lesson 2
Chapter 1 understanding health and wellness lesson 2 Chapter 1 health and wellness fundamentals
Chapter 1 health and wellness fundamentals Optimal health in each of the six components of health
Optimal health in each of the six components of health Ohio state health assessment
Ohio state health assessment Individual service plans
Individual service plans Health education plan
Health education plan First care benefits
First care benefits Health sector transformation plan ii ethiopia
Health sector transformation plan ii ethiopia Traffic light safety plan mental health
Traffic light safety plan mental health Ohsuhealth
Ohsuhealth Family care plan in community health nursing
Family care plan in community health nursing My health action plan
My health action plan Healthplan finder business
Healthplan finder business Flyer taxi
Flyer taxi What do you call this picture
What do you call this picture Unicare
Unicare My mchcp
My mchcp What is the algee action plan
What is the algee action plan Outcome based planning definition
Outcome based planning definition Shibps
Shibps Problem solving plan (plan b flowchart)
Problem solving plan (plan b flowchart) Academic field trip plan a plan b
Academic field trip plan a plan b Long medium and short term planning in primary schools
Long medium and short term planning in primary schools Problem solving plan (plan b flowchart)
Problem solving plan (plan b flowchart) What is micro teaching lesson plan
What is micro teaching lesson plan Problem solving plan (plan b flowchart)
Problem solving plan (plan b flowchart) New jersey plan vs virginia plan
New jersey plan vs virginia plan Stowage plan kapal
Stowage plan kapal Faktor yang mempengaruhi tata letak fasilitas jasa
Faktor yang mempengaruhi tata letak fasilitas jasa Mansplan
Mansplan Virginia plan and new jersey plan venn diagram
Virginia plan and new jersey plan venn diagram