Intraoperative Mapping of the Corticospinal Tracts with Neurophysiological

- Slides: 38
Intraoperative Mapping of the Corticospinal Tracts with Neurophysiological Assessment and 3 D Ultrasound EYTAN NOV SACKLER SCHOOL OF MEDICINE TEL AVIV UNIVERSITY
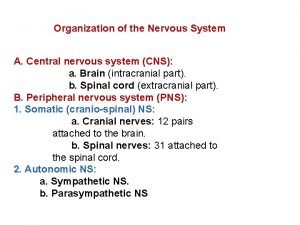
Introduction �Maximal resection is associated with increased survival, better long-term tumor control and reduced malignant conversion of lower-grade lesions. �Aggressive surgery should only be attempted however if there is minimal associated risk.
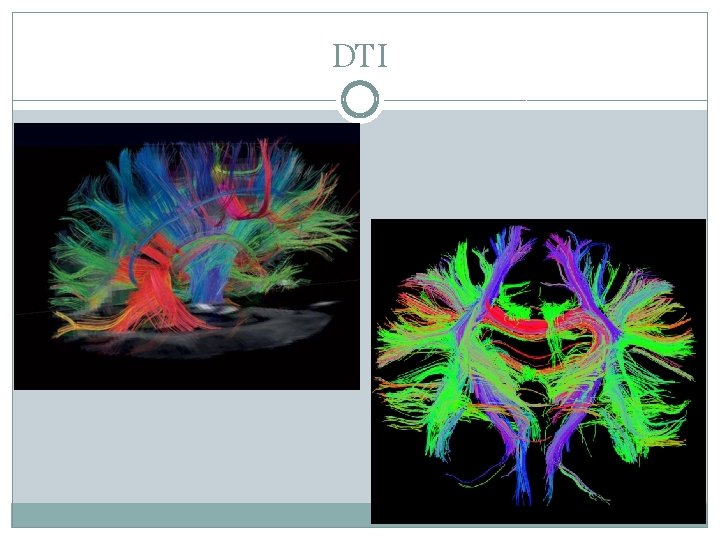
�Neurosurgery has many imaging modalities and systems designed with the purpose of minimizing the risk of intraaxial tumor resection such as: �Preoperative MRI and f. MRI �Diffusion tensor imaging �Intraoperative navigation systems �Neurophysiological montioring intraoperatively
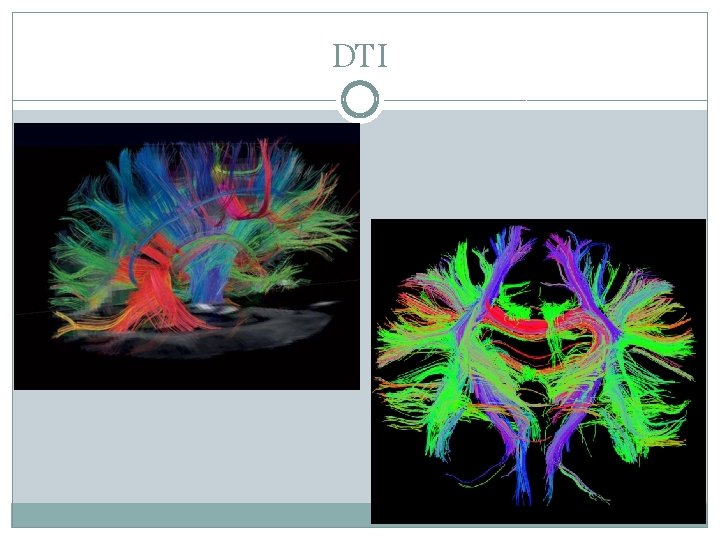
DTI
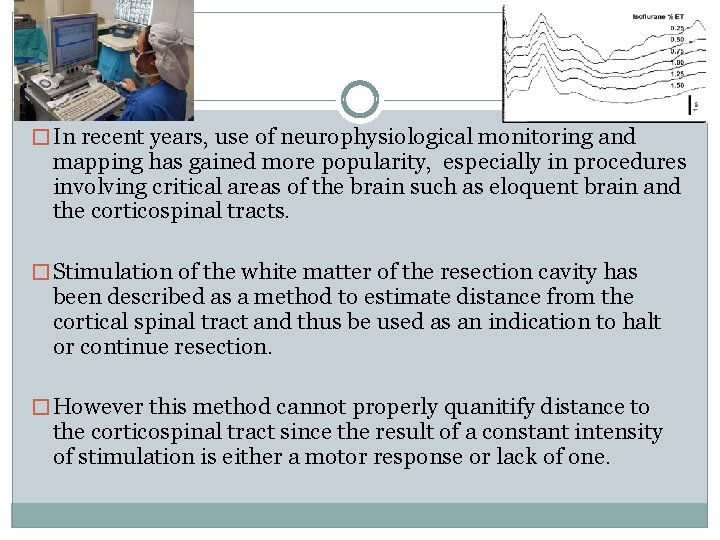
� In recent years, use of neurophysiological monitoring and mapping has gained more popularity, especially in procedures involving critical areas of the brain such as eloquent brain and the corticospinal tracts. � Stimulation of the white matter of the resection cavity has been described as a method to estimate distance from the cortical spinal tract and thus be used as an indication to halt or continue resection. � However this method cannot properly quanitify distance to the corticospinal tract since the result of a constant intensity of stimulation is either a motor response or lack of one.
Going the distance… �The aforementioned problem inspired attempts to measure a correlated distance to the CST related to intensity of stimulation, however data was not accurate enough due to the phenomenon of brain shift. �Ozawa and colleagues attempted to overcome the problem of brain shift using diffusion-weighted MR to measure the extent of shift, however this was still less accurate in localizing the corticospinal tracts. (Ozawa N, Muragaki Y, Nakamura R, Hori T, Iseki H: Shift of the pyramidal tract during resection of the intraaxial braintumors estimated by intraoperative diffusion-weighted imaging. Neurol Med Chir (Tokyo) 49: 51– 56, 2009)
Brain Shift
Brain Shift �Navigational systems are dependent on pre-op imaging and spatial registration before the commencement of a procedure. �The brain however is influenced by factors such gravity and deformation (dissection and resection) throughout a procedure thus changing the spatial orientation relative to the images registered with the navigation system. �These shifts thus decrease the effectiveness and accompanying confidence achieved by using navigation systems.
Brain Shift �A study on brain shift concluded that the average displacement during an operation was about 1 cm. �The dominant factor is gravity. �There is a correlation with the size of resection.
Brain Shift �Intraoperative brain movement is greatest along the downward axis regardless of head position. �Surface shift seemed to be unaffected by size of the craniotomy. �There was no correlation found with mannitol use.
The Study � A retrospective study was done at Tel Aviv Sourasky Medical Center looking at the experiences and outcomes using elaborate neurophysiological assessment and tractography-based navigation. � Three-dimensional ultrasound was used intraoperatively to adjust for brain shift. � With the adjustments, accurate distances between the resection cavity and the corticospinal tract could be determined. � This study was published in the Journal of Neurosurgery in August of 2010
Study Participants � 55 patients (35 males, 20 females) with a mean age of 46. 3 years (range 18– 81 years) underwent resection of a supratentorial lesion located within or 2 cm from the corticospinal tract as determined by preoperative MRI. �Patients underwent surgery during a period of 19 months (November 2007–June 2009). �One patient underwent two procedures, which were each evaluated separately.
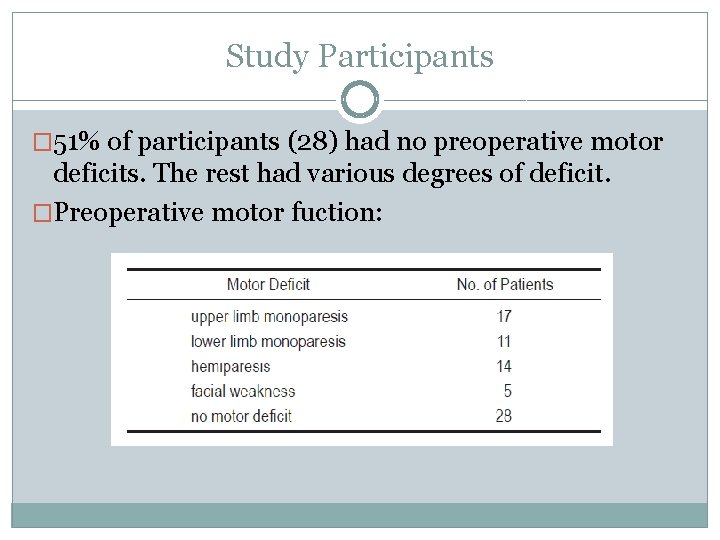
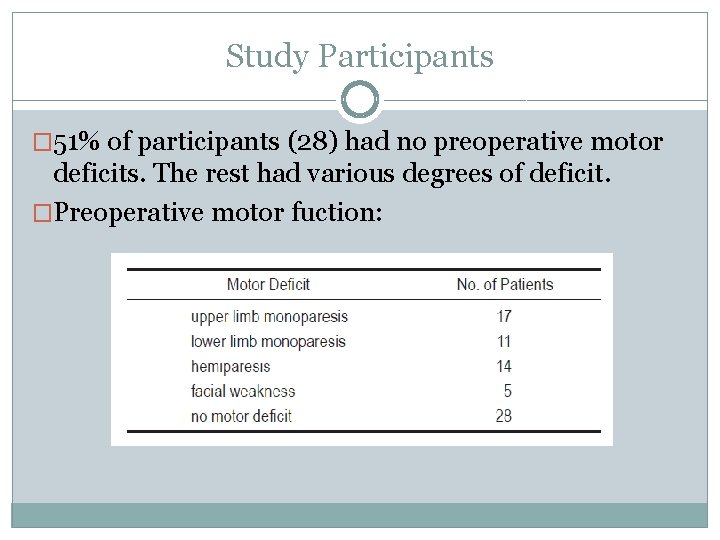
Study Participants � 51% of participants (28) had no preoperative motor deficits. The rest had various degrees of deficit. �Preoperative motor fuction:
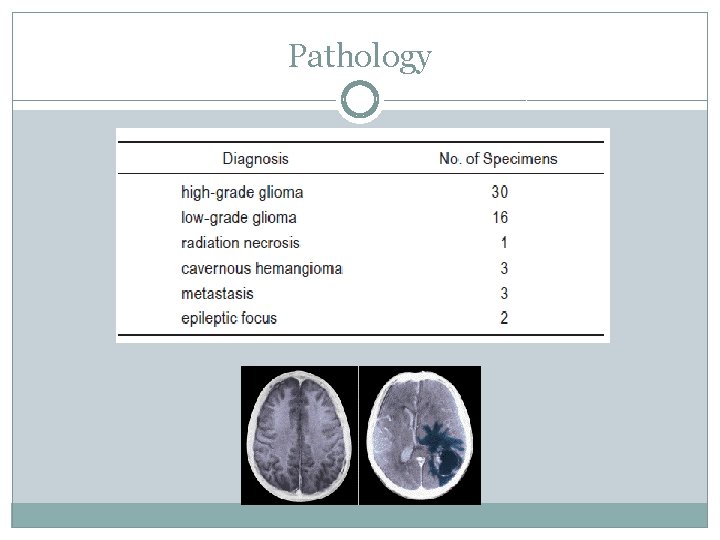
Pathology �The most frequent pathology in the study population was glioblastoma multiforme (40% of cases). �Grade II oligodendroglioma was the most common type of low-grade gliomas encountered (62% of low grade gliomas). �Other lesions included metastasis, cavernous hemangiomas, radiation necrosis, and epileptic foci.
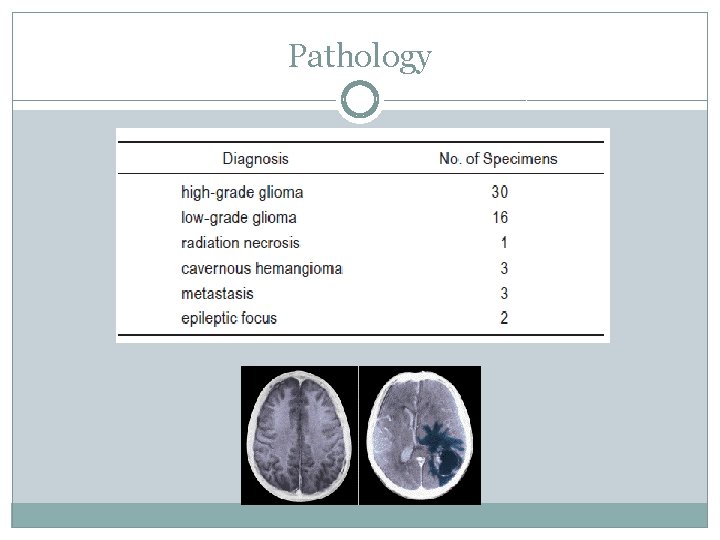
Pathology
Operative Technique � 20 of the patients underwent surgery under general anesthesia. � 35 patients underwent standard awake craniotomies with local anesthesia for craniotomy exposure.
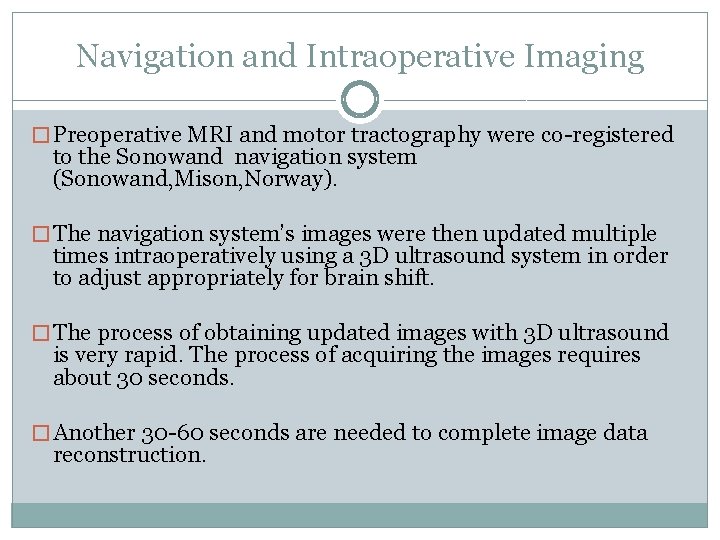
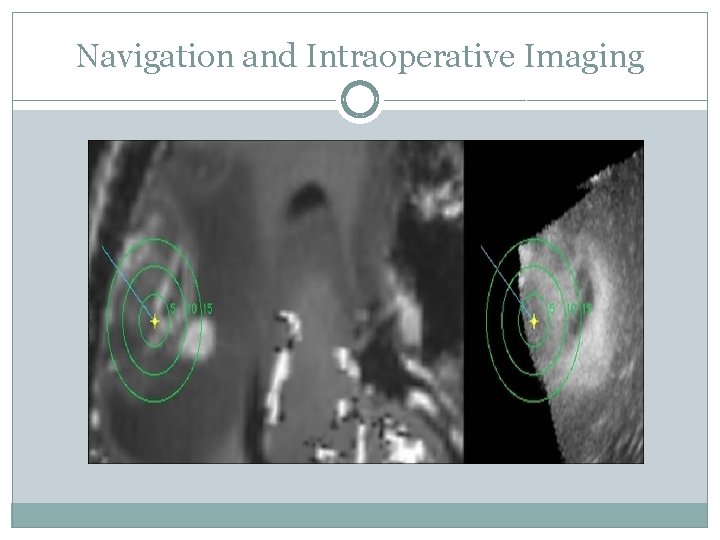
Navigation and Intraoperative Imaging � Preoperative MRI and motor tractography were co-registered to the Sonowand navigation system (Sonowand, Mison, Norway). � The navigation system’s images were then updated multiple times intraoperatively using a 3 D ultrasound system in order to adjust appropriately for brain shift. � The process of obtaining updated images with 3 D ultrasound is very rapid. The process of acquiring the images requires about 30 seconds. � Another 30 -60 seconds are needed to complete image data reconstruction.

Navigation and Intraoperative Imaging
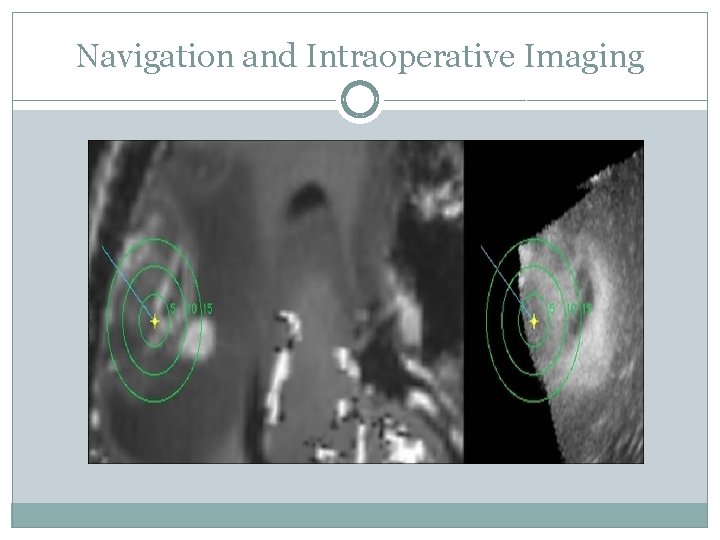
Navigation and Intraoperative Imaging
Navigation and Intraoperative Imaging �Baseline ultrasound scan is first performed after removing bone flap. �These images are then registered to the navigation system. �Throughout the surgery, images are collected in order to maximize navigational accuracy.
Neurophysiological Monitoring �Direct cortical stimulation (Dc. MEP) and subcortical stimulation (Scrt. MEP) were used (Axon Systems Inc. , Hauppauge, NY, USA). � Continuous MEP recordings were generated via a cortical strip electrode placed over the motor cortex. �Collection of the dc. MEP data during resection was set at 1 stimulation every 5– 10 seconds to minimize the facilitation effect, epileptogenic risk, and patient discomfort.
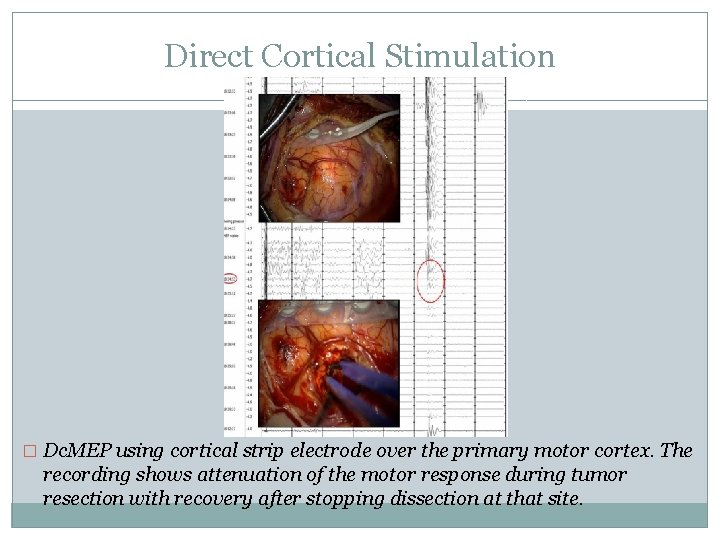
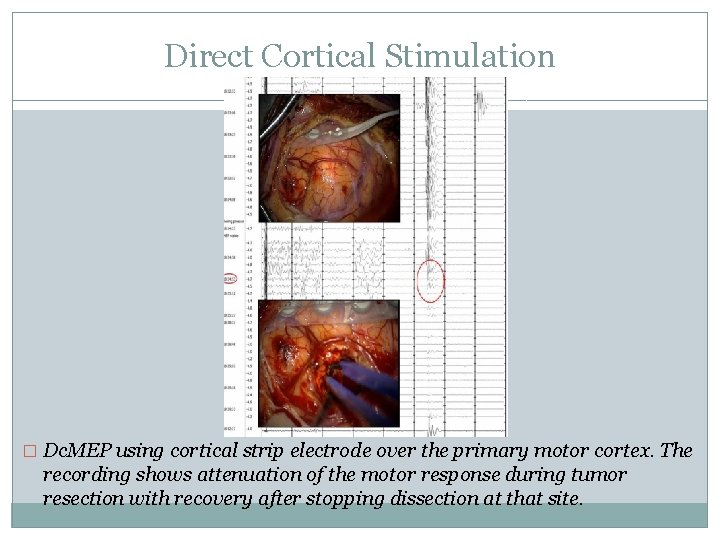
Direct Cortical Stimulation � Dc. MEP using cortical strip electrode over the primary motor cortex. The recording shows attenuation of the motor response during tumor resection with recovery after stopping dissection at that site.
Subcortical Stimulation �Throughout the resection process, subcortical stimulation was applied along the border of the tumor resection bed by using a monopolar handheld probe (Inomed). � The same recording channels and parameters as the direct cortical stimulation were used, except for 2 stimulations/sec instead of slower stimulation. �Stimulation intensity was increased stepwise in 0. 1 m. A increments up to 25 m. A or when an scrt. MEP was detected.
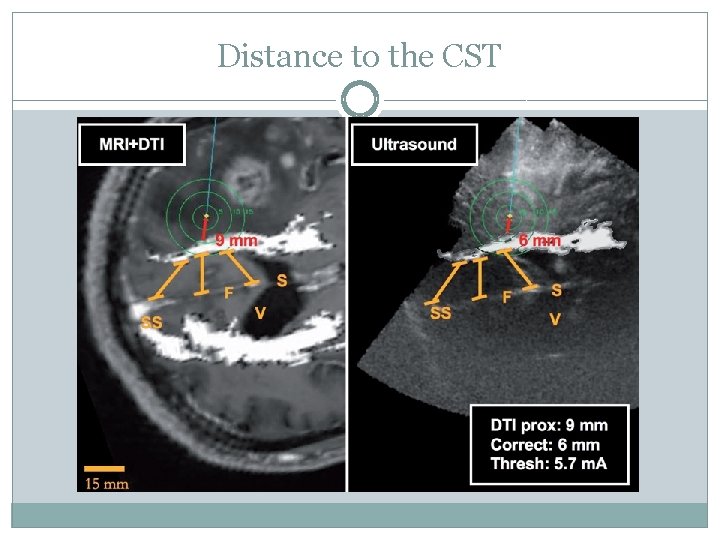
Distance to the CST �Images were acquired with the IOUS system either immediately before or after subcortical stimulations of the resection bed. �Tractography-based navigation images and ultrasound scans were compared according to the corresponding views.
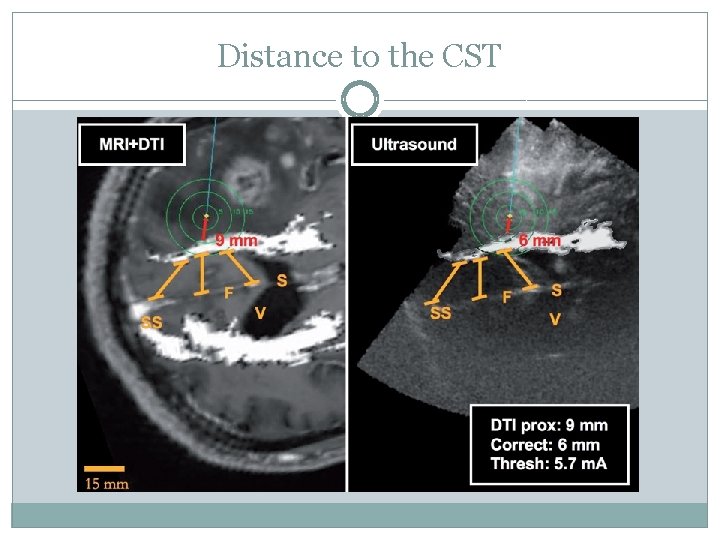
Distance to the CST
Correlation of Stimulation Threshold and Distance to CST � After navigational correction with IOUS, the probe was positioned at a corresponding stimulation point within the resection cavity and angle to best visualize the nearest CST. � At least 3 analogous anatomical reference points within the vicinity of the white matter stimulation point were required for each ultrasound/tractography image set as criteria for inclusion of the image in the distance measurement.
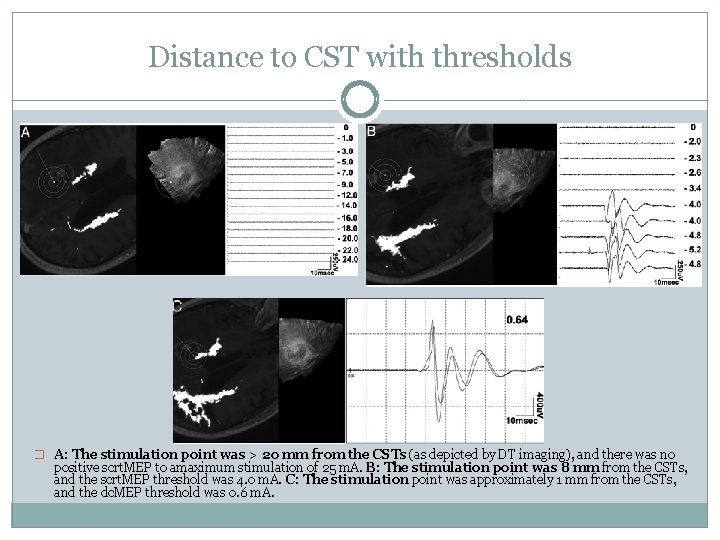
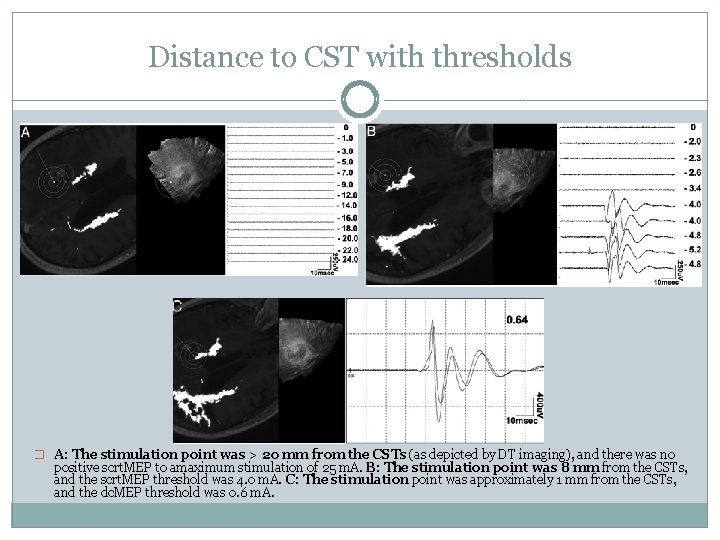
Distance to CST with thresholds � A: The stimulation point was > 20 mm from the CSTs (as depicted by DT imaging), and there was no positive scrt. MEP to amaximum stimulation of 25 m. A. B: The stimulation point was 8 mm from the CSTs, and the scrt. MEP threshold was 4. 0 m. A. C: The stimulation point was approximately 1 mm from the CSTs, and the dc. MEP threshold was 0. 6 m. A.
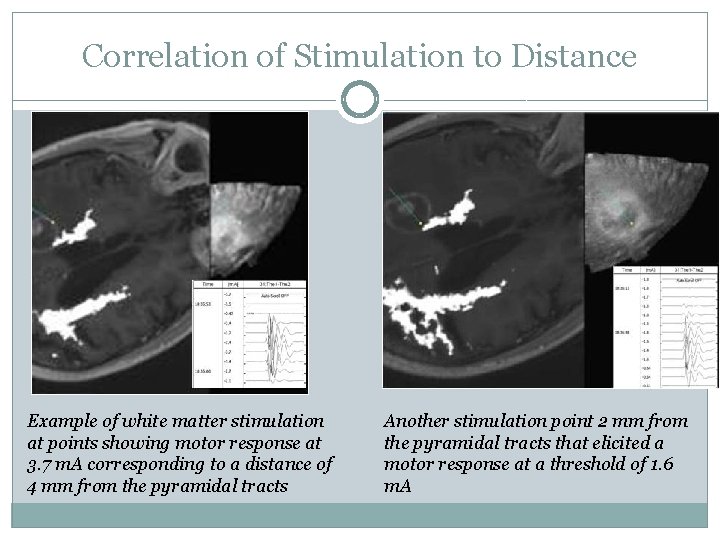
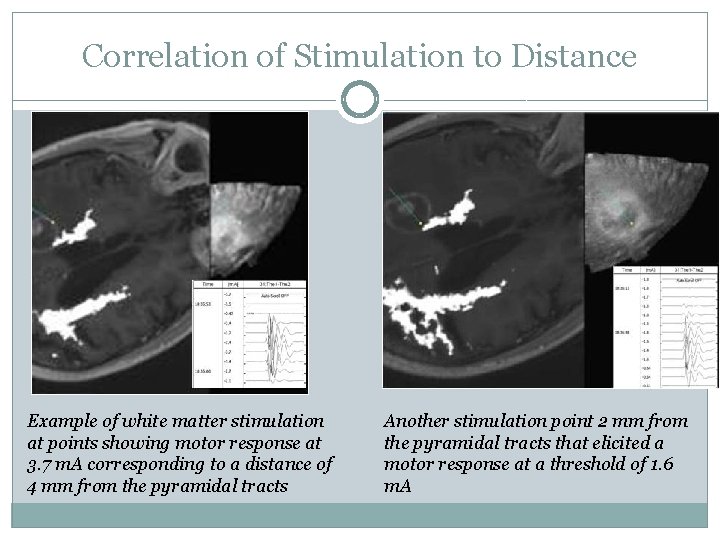
Correlation of Stimulation to Distance Example of white matter stimulation at points showing motor response at 3. 7 m. A corresponding to a distance of 4 mm from the pyramidal tracts Another stimulation point 2 mm from the pyramidal tracts that elicited a motor response at a threshold of 1. 6 m. A
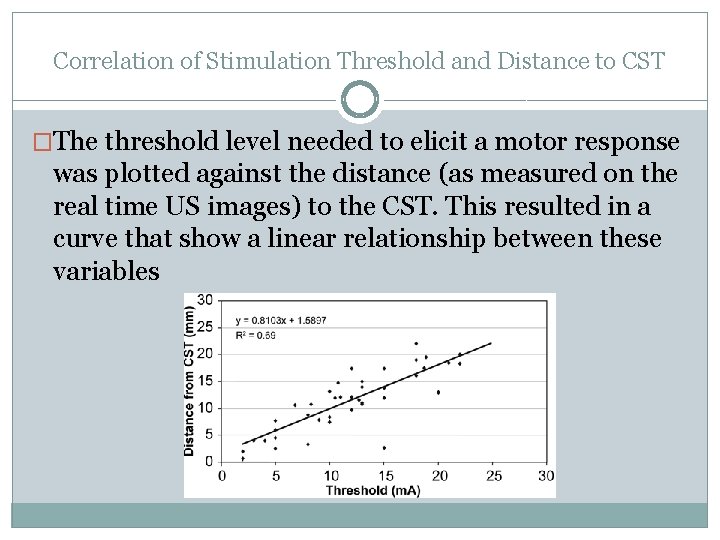
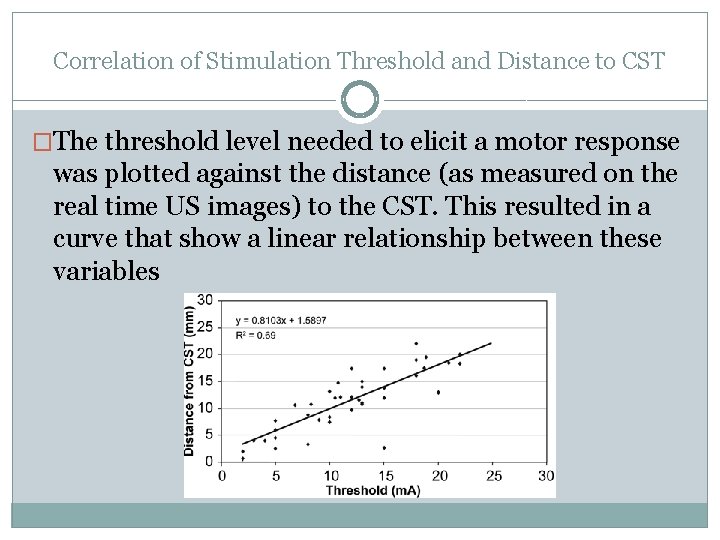
Correlation of Stimulation Threshold and Distance to CST �The threshold level needed to elicit a motor response was plotted against the distance (as measured on the real time US images) to the CST. This resulted in a curve that show a linear relationship between these variables
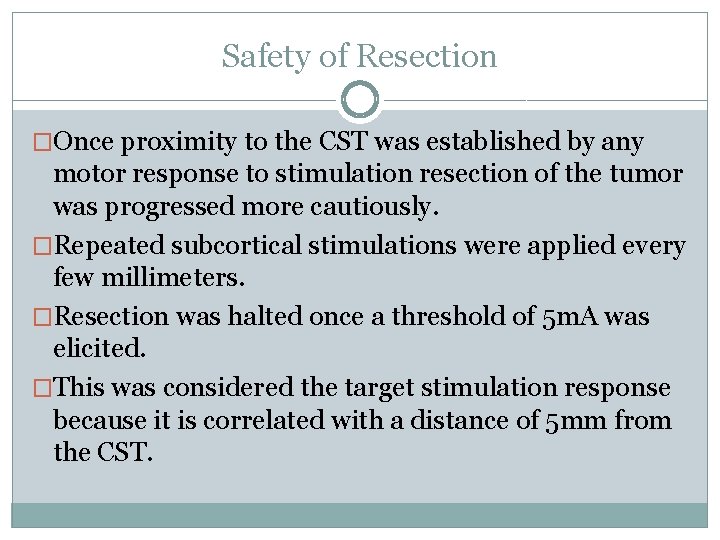
Safety of Resection �Once proximity to the CST was established by any motor response to stimulation resection of the tumor was progressed more cautiously. �Repeated subcortical stimulations were applied every few millimeters. �Resection was halted once a threshold of 5 m. A was elicited. �This was considered the target stimulation response because it is correlated with a distance of 5 mm from the CST.
Overall Clinical Results � 37 patients (67%) had no new motor deficits post-op. � 2 patients (4%) improved in their motor function. � 16 patients (29%) showed immediate decline from baseline pre-op. � Of these 16, 6 patients recovered by time of discharge (Within 5 days) and 3 recovered by 2 weeks post-discharge. � The remaining 7 patients were classified as having long-term deficit (did show improvement during last follow up visit).
Stimulation Intensity and Outcomes � Thirty-six (94. 7%) of 38 patients who displayed a motor response to stimulation at thresholds > 3 m. A did not experience any postoperative motor deficits. � Those patients who had deficits however recovered rapidly before discharge had a minimum threshold of > 6. 8 m. A. � Of the 7 patients who displayed an scrt. MEP value < 3. 0 m. A, 5 (71. 4%) deteriorated immediately after surgery. Two of these 5 patients recovered to their preoperative status within 2 weeks of surgery, and the other 3 remained with a long-term deficit. � Using a 3 m. A stimulation threshold value as a predictor of motor function outcome resulted in a sensitivity of 83. 3% and a specificity of 94. 7%, corresponding to a negative predictive value of 97. 3% and a positive predictive value of 71. 4% for motor function
Awake versus General Anesthesia �Whether or not the procedure was done with the patient under general anesthesia had no significant impact on the immediate postoperative motor status, extent of resection, or threshold intensity for eliciting a motor response with subcortical stimulation.
Conclusions �Combining elaborate neurophysiological assessment, tractography-based navigation, and updated 3 D US images provides more accurate localization of the motor pathways. �The linear correlation between distance to the corticospinal tracts and threshold of subcortical stimulation provides an intraoperative technique to preserve motor function. �This technique allows aggressive and safer surgical resection of tumors involving the motor pathways.
Limitations � Edema surrounding lesions can cause inaccuracies in DTI tractography. � Patients with deficits despite high thresholds most likely had vascular compromise. � Experience of the surgeon. � Limited ability to compare outcomes to other surgical methods. � Should have compared extent of resections using current method post-op to other methods.
Summary �Methods of localizing important white matter tracts. �Accounting for brain shift. �Correlating neurophysiological data with distances to CST and clinical outcomes.
What does the future hold?
THANK YOU!
 Corticospinal tract.
Corticospinal tract. Preoperative checklist definition
Preoperative checklist definition Intraoperative cholangiogram
Intraoperative cholangiogram Role of nurse in intraoperative care ppt
Role of nurse in intraoperative care ppt Phases of perioperative nursing
Phases of perioperative nursing Choledocholithiasis
Choledocholithiasis Neuro tract
Neuro tract Spinocerebellar tract lesion
Spinocerebellar tract lesion Parkinson's disease causes
Parkinson's disease causes Pyramidal vs extrapyramidal tract
Pyramidal vs extrapyramidal tract Odontoblastic zone
Odontoblastic zone Ascending tracts
Ascending tracts Rubrospinal tract origin
Rubrospinal tract origin White fiber tracts
White fiber tracts Cerebellar signs
Cerebellar signs Spinal nerves labled
Spinal nerves labled Nervous system tract
Nervous system tract Corticospinal tract
Corticospinal tract Dorsal lateral prefrontal cortex
Dorsal lateral prefrontal cortex Corticospinal tract
Corticospinal tract Terjemahan
Terjemahan The associative mapping is costlier than direct mapping.
The associative mapping is costlier than direct mapping. Forward mapping vs backward mapping
Forward mapping vs backward mapping Thẻ vin
Thẻ vin Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Hát lên người ơi
Hát lên người ơi Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Ví dụ về giọng cùng tên
Ví dụ về giọng cùng tên Phép trừ bù
Phép trừ bù Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Lời thề hippocrates
Lời thề hippocrates đại từ thay thế
đại từ thay thế Hệ hô hấp
Hệ hô hấp Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Cong thức tính động năng
Cong thức tính động năng Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể