Immune Reconstitution Inflammatory Syndrome IRIS HAIVN Harvard Medical

- Slides: 36
Immune Reconstitution Inflammatory Syndrome (IRIS) HAIVN Harvard Medical School AIDS Initiative in Vietnam 1
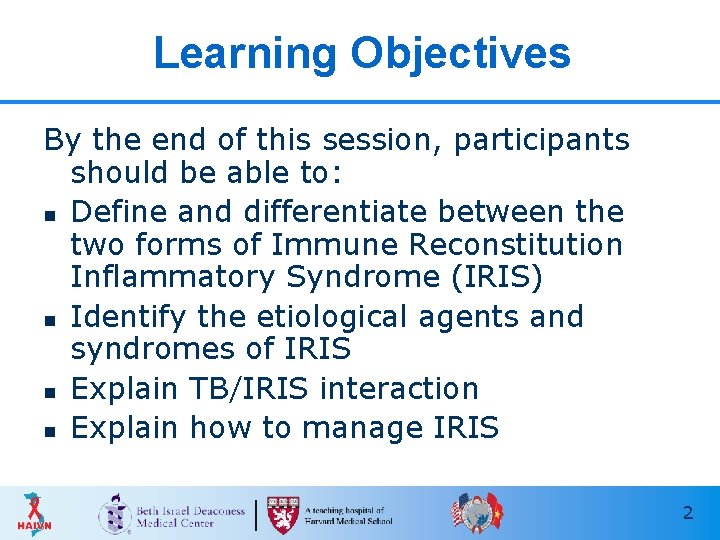
Learning Objectives By the end of this session, participants should be able to: n Define and differentiate between the two forms of Immune Reconstitution Inflammatory Syndrome (IRIS) n Identify the etiological agents and syndromes of IRIS n Explain TB/IRIS interaction n Explain how to manage IRIS 2
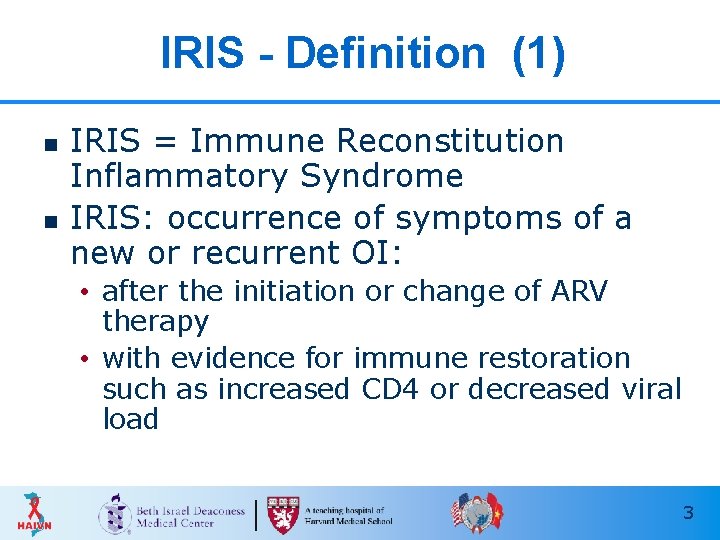
IRIS - Definition (1) n n IRIS = Immune Reconstitution Inflammatory Syndrome IRIS: occurrence of symptoms of a new or recurrent OI: • after the initiation or change of ARV therapy • with evidence for immune restoration such as increased CD 4 or decreased viral load 3
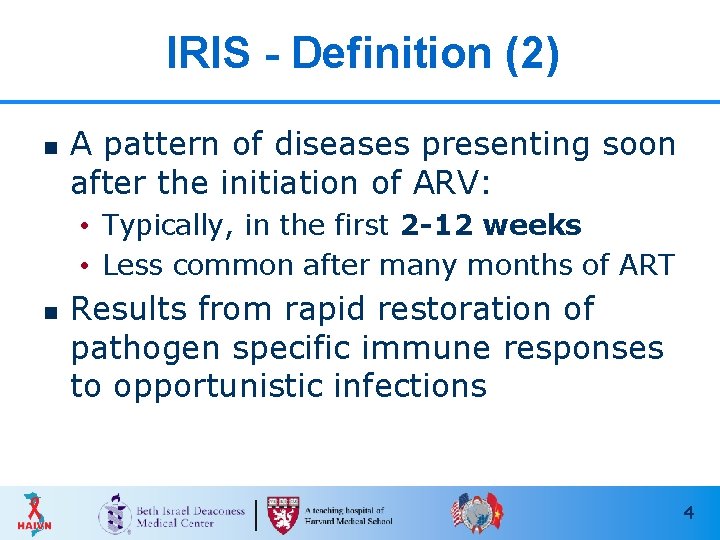
IRIS - Definition (2) n A pattern of diseases presenting soon after the initiation of ARV: • Typically, in the first 2 -12 weeks • Less common after many months of ART n Results from rapid restoration of pathogen specific immune responses to opportunistic infections 4
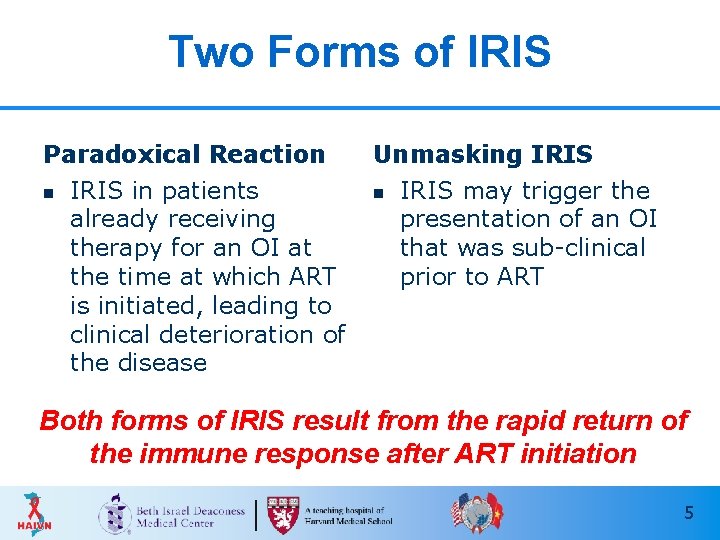
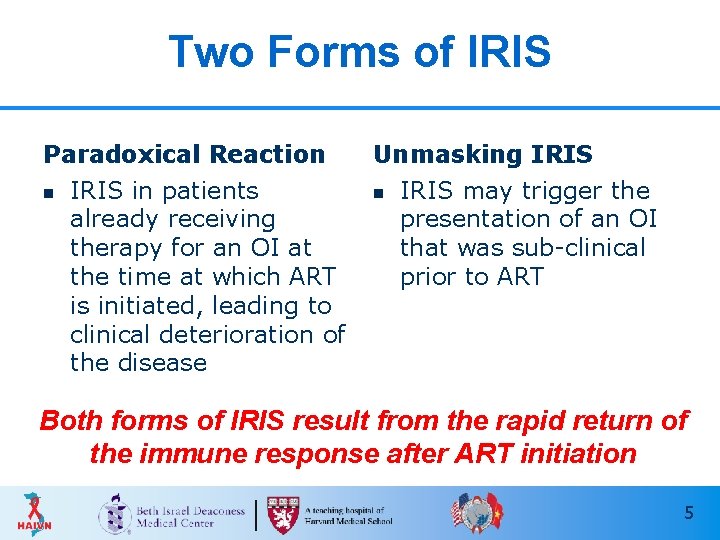
Two Forms of IRIS Paradoxical Reaction n IRIS in patients already receiving therapy for an OI at the time at which ART is initiated, leading to clinical deterioration of the disease Unmasking IRIS n IRIS may trigger the presentation of an OI that was sub-clinical prior to ART Both forms of IRIS result from the rapid return of the immune response after ART initiation 5
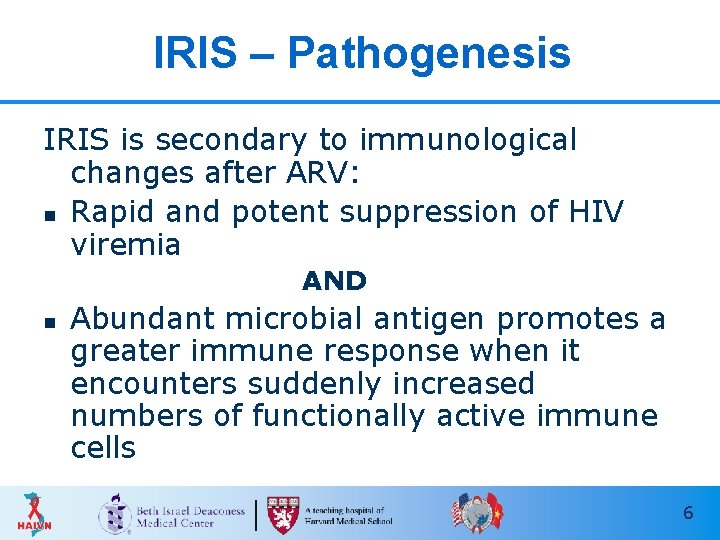
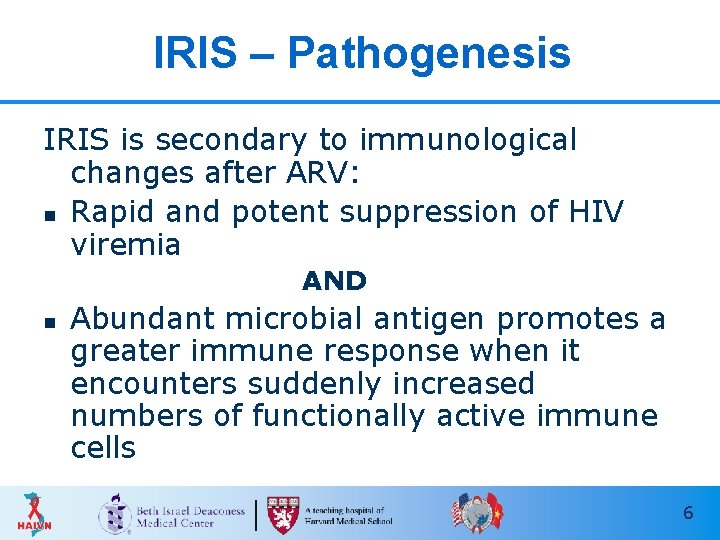
IRIS – Pathogenesis IRIS is secondary to immunological changes after ARV: n Rapid and potent suppression of HIV viremia AND n Abundant microbial antigen promotes a greater immune response when it encounters suddenly increased numbers of functionally active immune cells 6
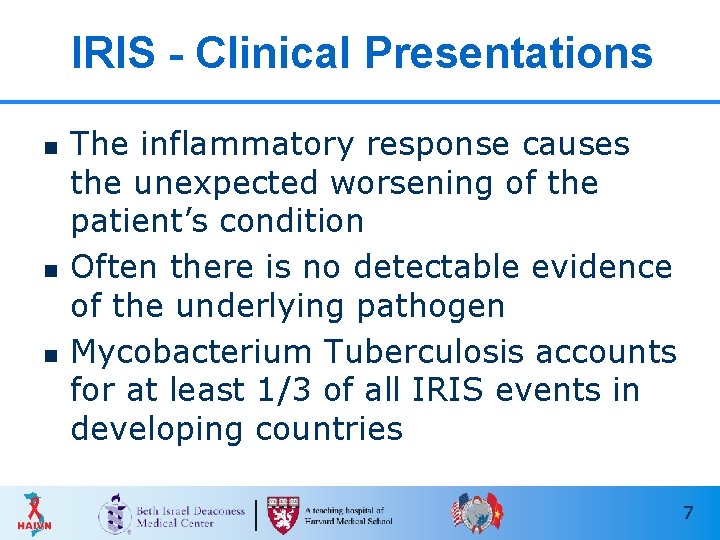
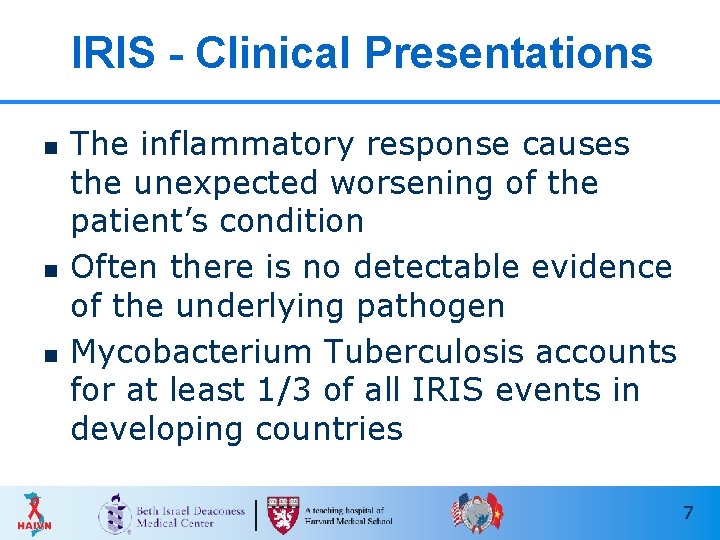
IRIS - Clinical Presentations n n n The inflammatory response causes the unexpected worsening of the patient’s condition Often there is no detectable evidence of the underlying pathogen Mycobacterium Tuberculosis accounts for at least 1/3 of all IRIS events in developing countries 7
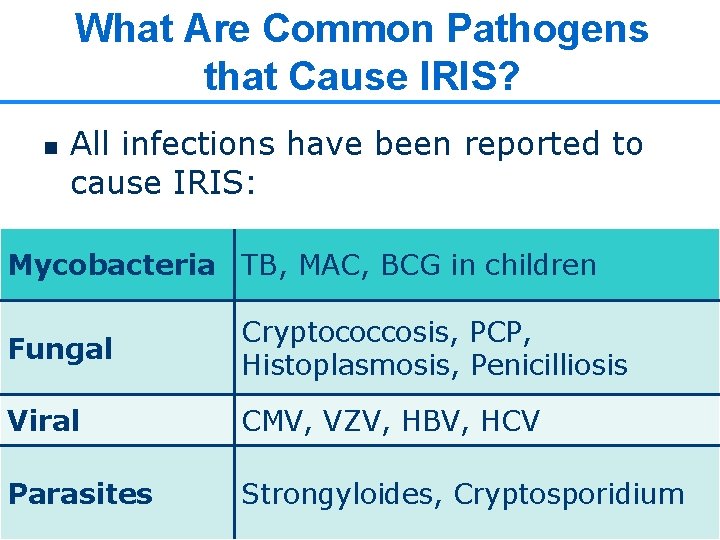
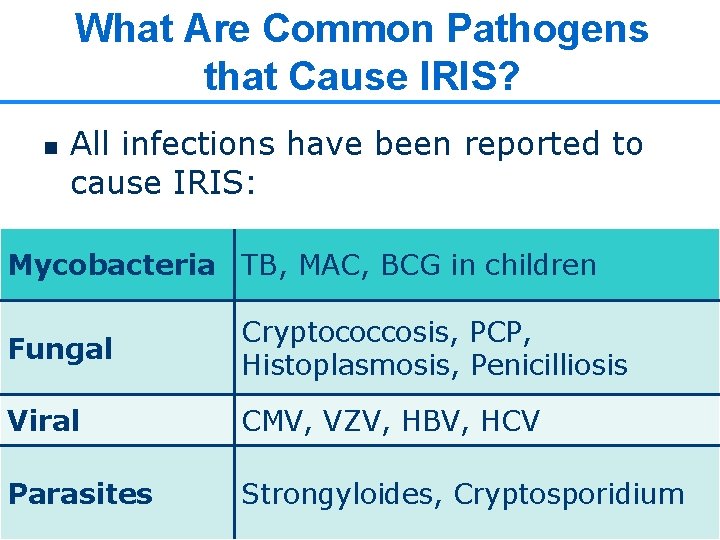
What Are Common Pathogens that Cause IRIS? n All infections have been reported to cause IRIS: Mycobacteria TB, MAC, BCG in children Fungal Cryptococcosis, PCP, Histoplasmosis, Penicilliosis Viral CMV, VZV, HBV, HCV Parasites Strongyloides, Cryptosporidium 8
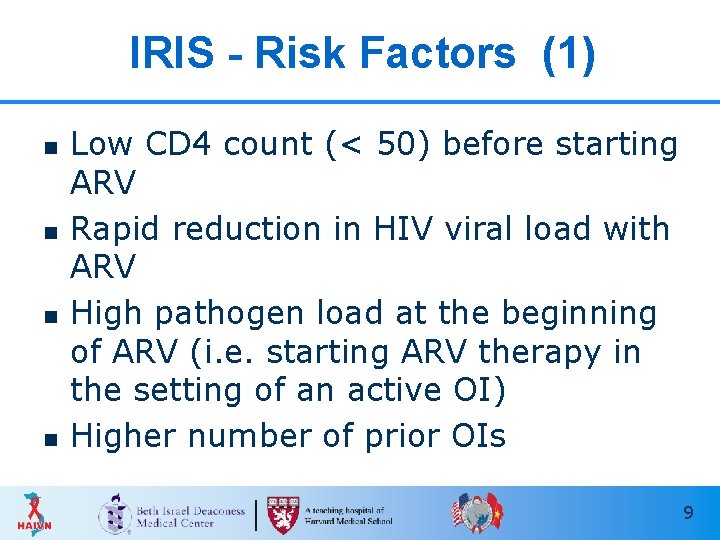
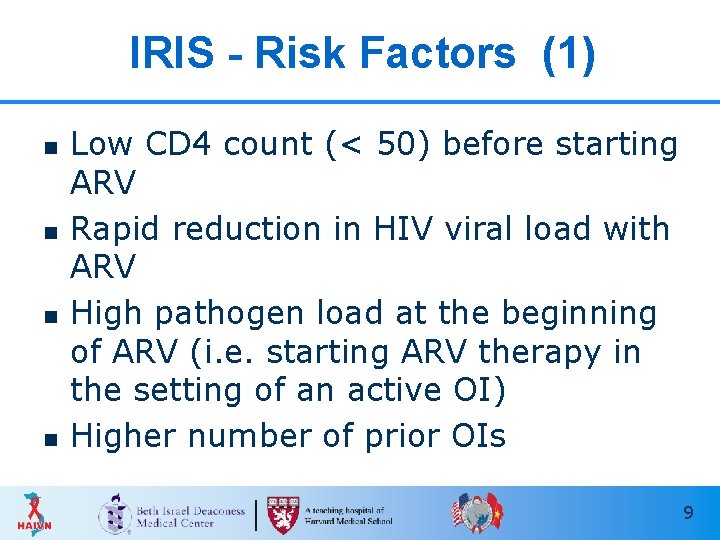
IRIS - Risk Factors (1) n n Low CD 4 count (< 50) before starting ARV Rapid reduction in HIV viral load with ARV High pathogen load at the beginning of ARV (i. e. starting ARV therapy in the setting of an active OI) Higher number of prior OIs 9
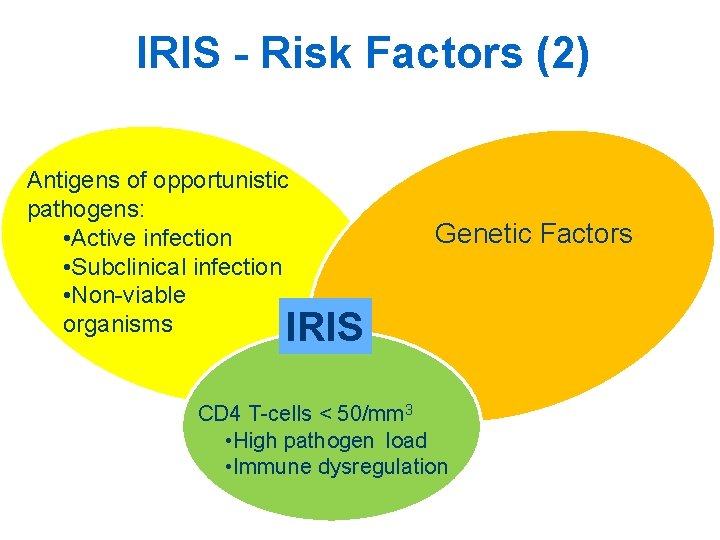
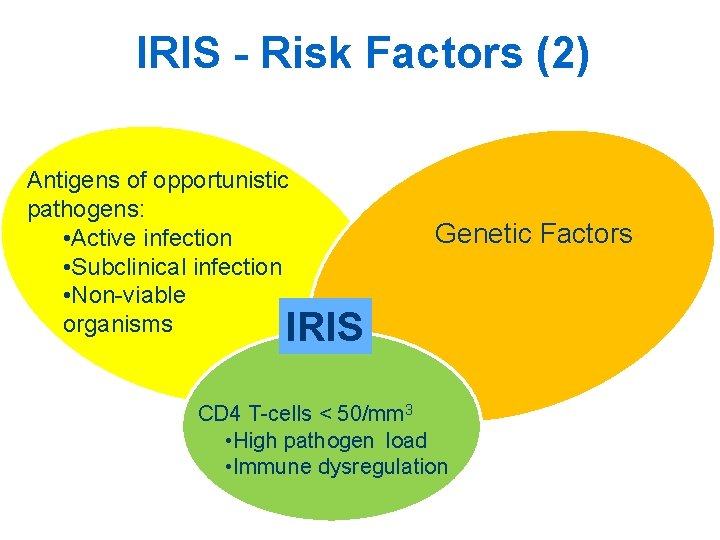
IRIS - Risk Factors (2) Antigens of opportunistic pathogens: • Active infection • Subclinical infection • Non-viable organisms Genetic Factors IRIS CD 4 T-cells < 50/mm 3 • High pathogen load • Immune dysregulation
IRIS – TUBERCULOSIS 11
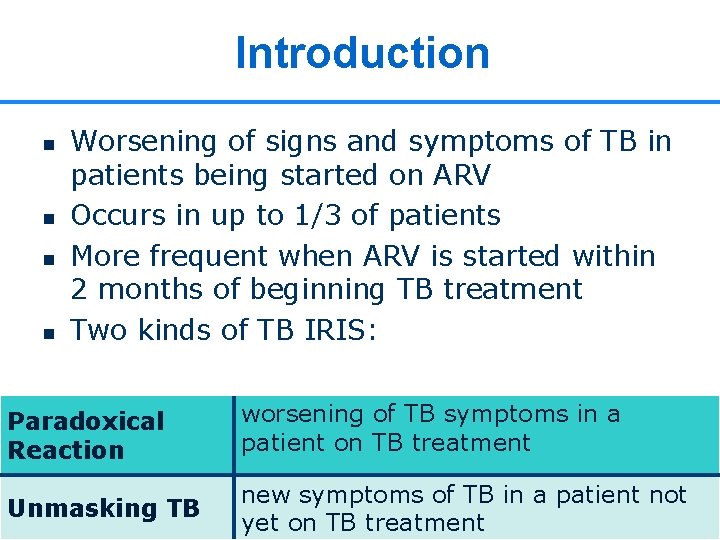
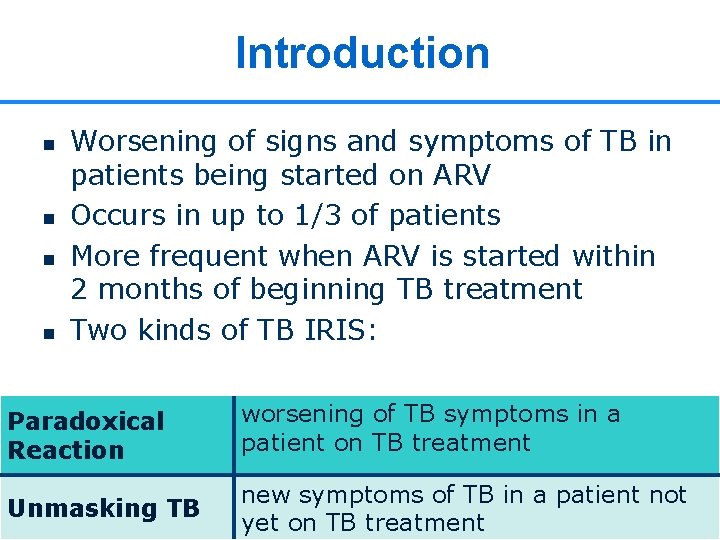
Introduction n n Worsening of signs and symptoms of TB in patients being started on ARV Occurs in up to 1/3 of patients More frequent when ARV is started within 2 months of beginning TB treatment Two kinds of TB IRIS: Paradoxical Reaction worsening of TB symptoms in a patient on TB treatment Unmasking TB new symptoms of TB in a patient not 12 yet on TB treatment
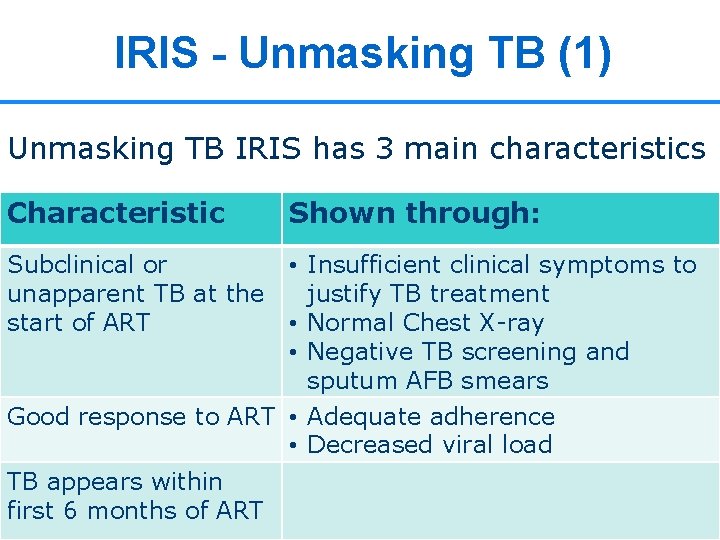
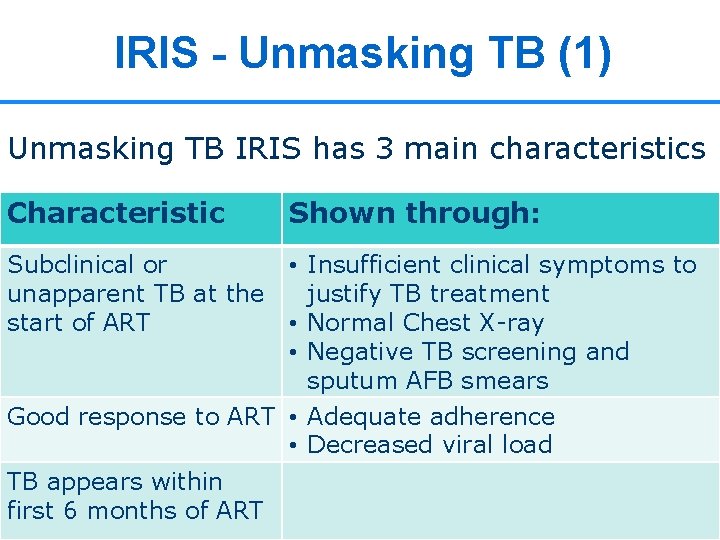
IRIS - Unmasking TB (1) Unmasking TB IRIS has 3 main characteristics Characteristic Subclinical or unapparent TB at the start of ART Shown through: • Insufficient clinical symptoms to justify TB treatment • Normal Chest X-ray • Negative TB screening and sputum AFB smears Good response to ART • Adequate adherence • Decreased viral load TB appears within first 6 months of ART 13
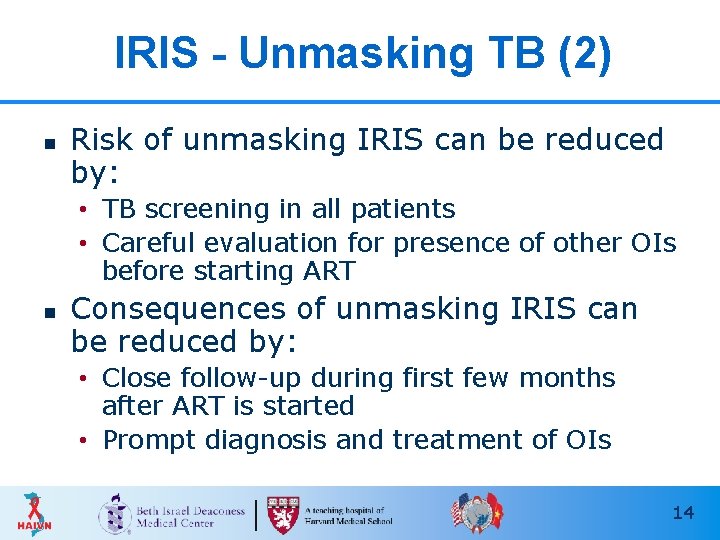
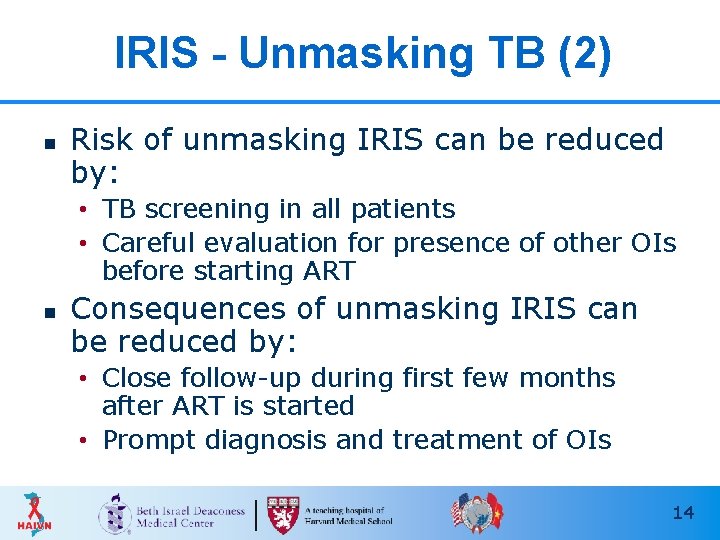
IRIS - Unmasking TB (2) n Risk of unmasking IRIS can be reduced by: • TB screening in all patients • Careful evaluation for presence of other OIs before starting ART n Consequences of unmasking IRIS can be reduced by: • Close follow-up during first few months after ART is started • Prompt diagnosis and treatment of OIs 14
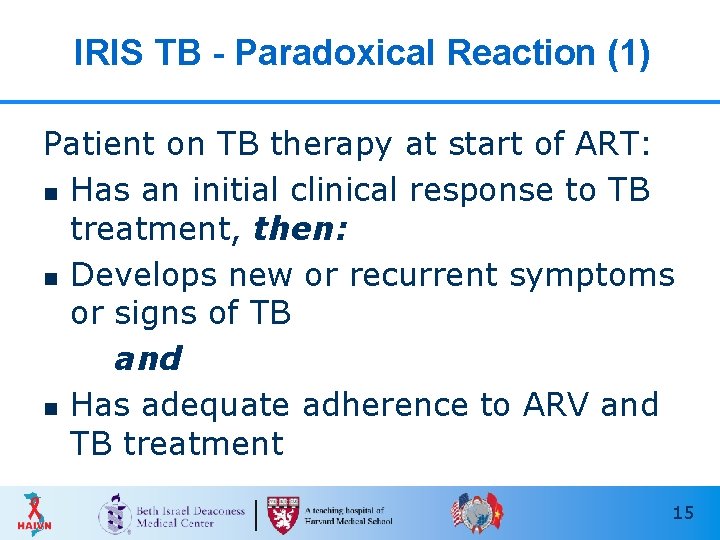
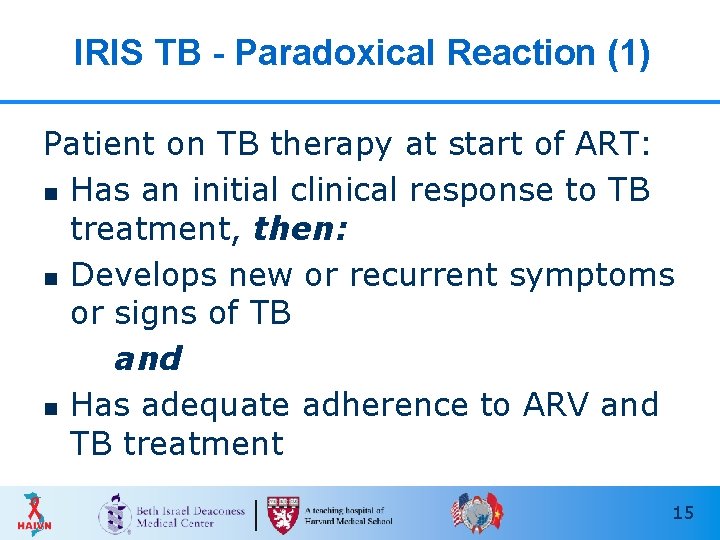
IRIS TB - Paradoxical Reaction (1) Patient on TB therapy at start of ART: n Has an initial clinical response to TB treatment, then: n Develops new or recurrent symptoms or signs of TB and n Has adequate adherence to ARV and TB treatment 15
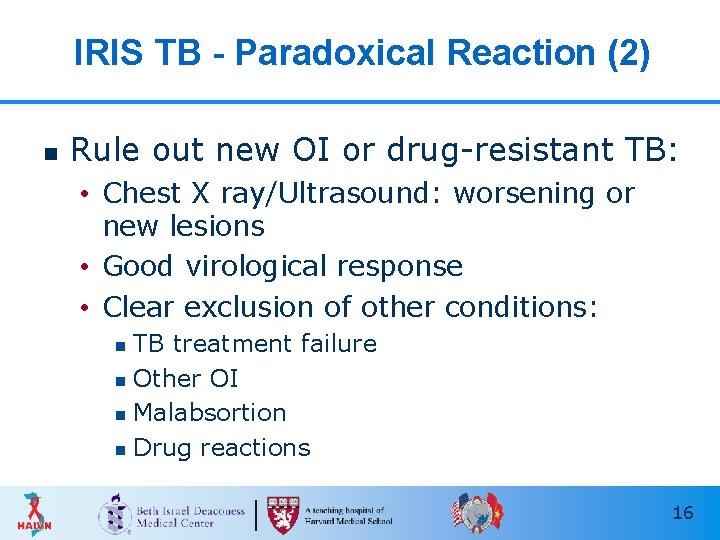
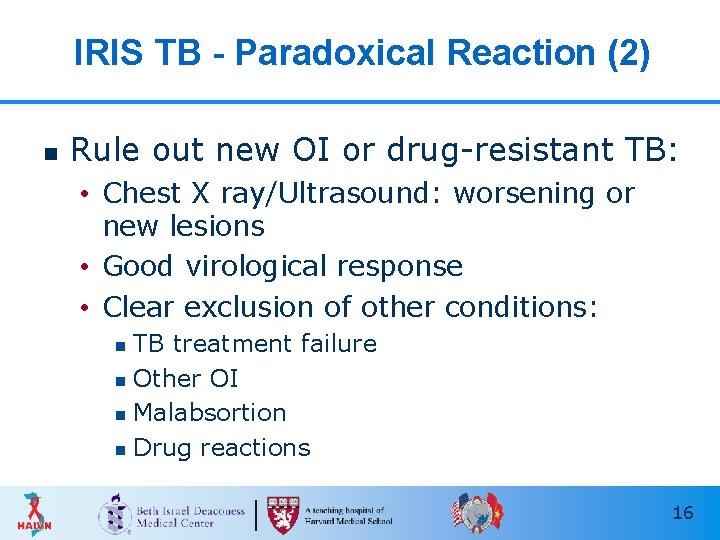
IRIS TB - Paradoxical Reaction (2) n Rule out new OI or drug-resistant TB: • Chest X ray/Ultrasound: worsening or new lesions • Good virological response • Clear exclusion of other conditions: TB treatment failure n Other OI n Malabsortion n Drug reactions n 16
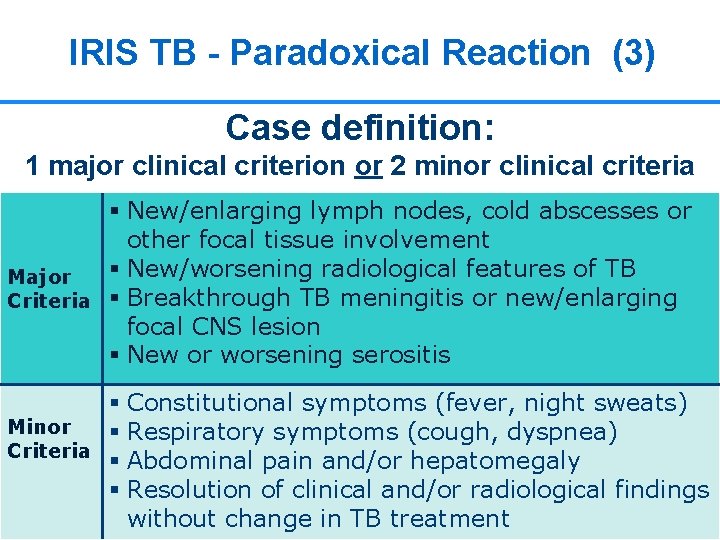
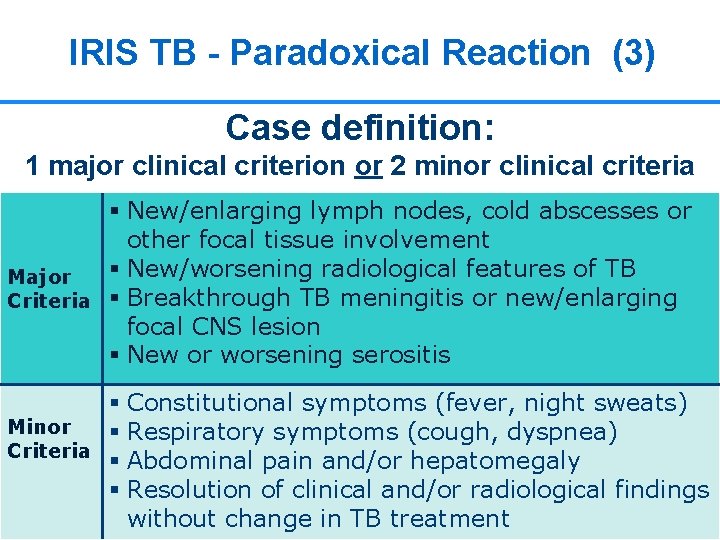
IRIS TB - Paradoxical Reaction (3) Case definition: 1 major clinical criterion or 2 minor clinical criteria § New/enlarging lymph nodes, cold abscesses or other focal tissue involvement § New/worsening radiological features of TB Major Criteria § Breakthrough TB meningitis or new/enlarging focal CNS lesion § New or worsening serositis § Constitutional symptoms (fever, night sweats) Minor § Respiratory symptoms (cough, dyspnea) Criteria § Abdominal pain and/or hepatomegaly § Resolution of clinical and/or radiological findings 17 without change in TB treatment
What Is the Optimal Timing for Starting ART When TB Is Diagnosed? 18
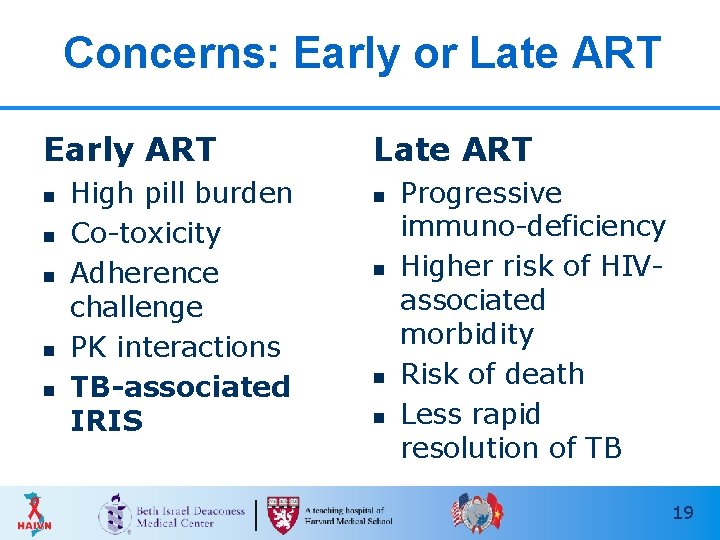
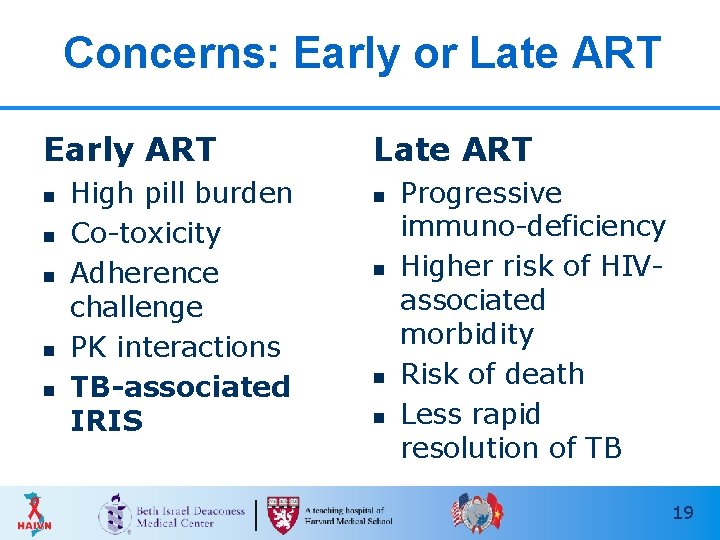
Concerns: Early or Late ART Early ART n n n High pill burden Co-toxicity Adherence challenge PK interactions TB-associated IRIS Late ART n n Progressive immuno-deficiency Higher risk of HIVassociated morbidity Risk of death Less rapid resolution of TB 19
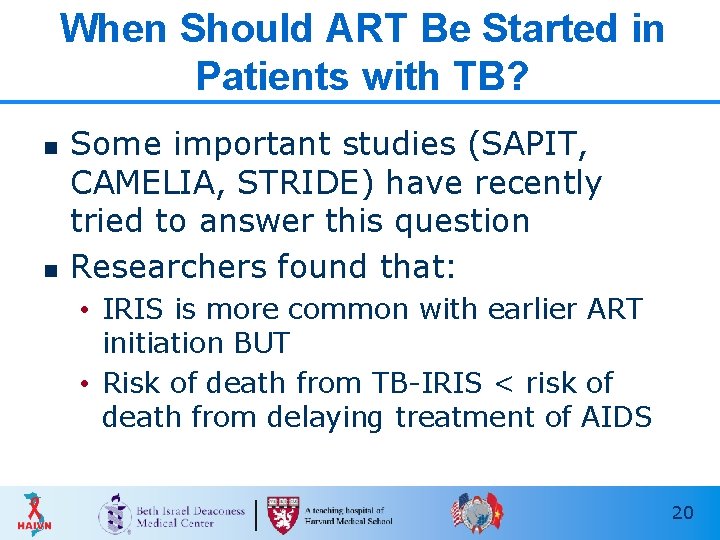
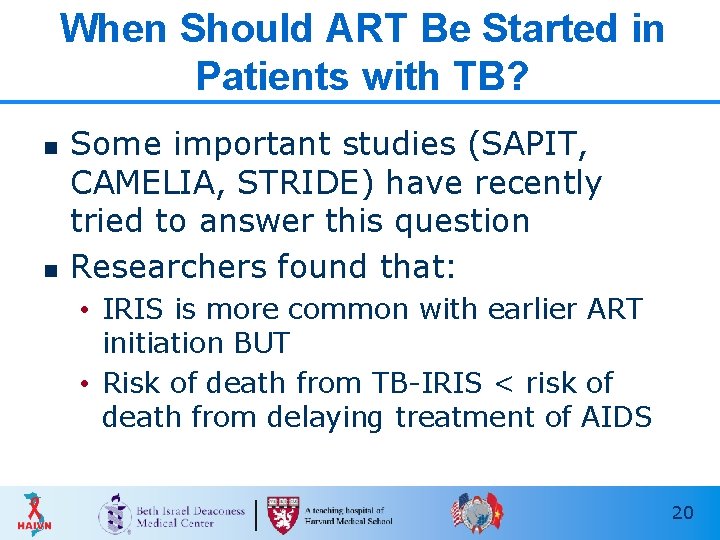
When Should ART Be Started in Patients with TB? n n Some important studies (SAPIT, CAMELIA, STRIDE) have recently tried to answer this question Researchers found that: • IRIS is more common with earlier ART initiation BUT • Risk of death from TB-IRIS < risk of death from delaying treatment of AIDS 20
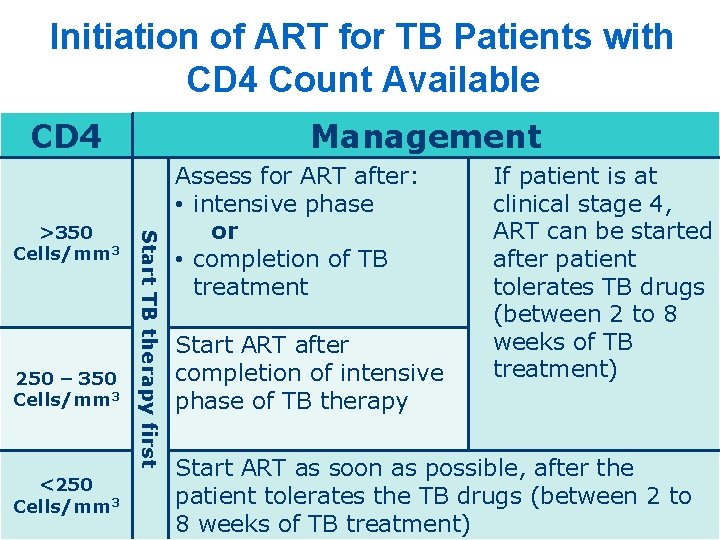
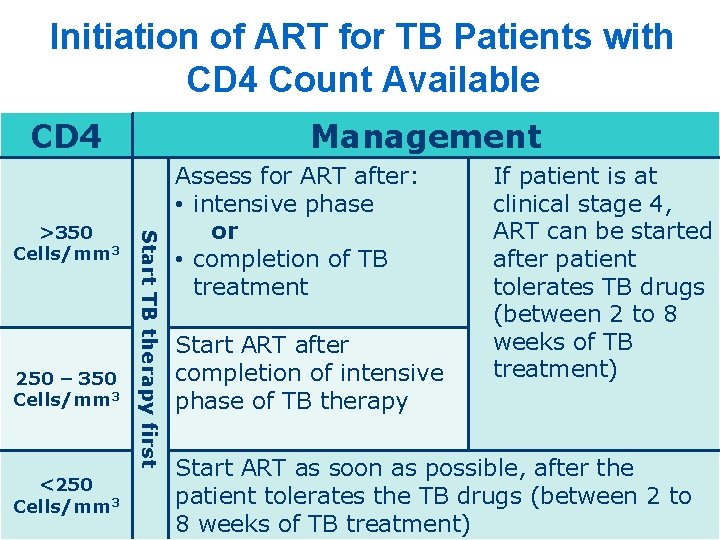
Initiation of ART for TB Patients with CD 4 Count Available CD 4 250 – 350 Cells/mm 3 <250 Cells/mm 3 Start TB therapy first >350 Cells/mm 3 Management Assess for ART after: • intensive phase or • completion of TB treatment Start ART after completion of intensive phase of TB therapy If patient is at clinical stage 4, ART can be started after patient tolerates TB drugs (between 2 to 8 weeks of TB treatment) Start ART as soon as possible, after the patient tolerates the TB drugs (between 2 to 21 8 weeks of TB treatment)
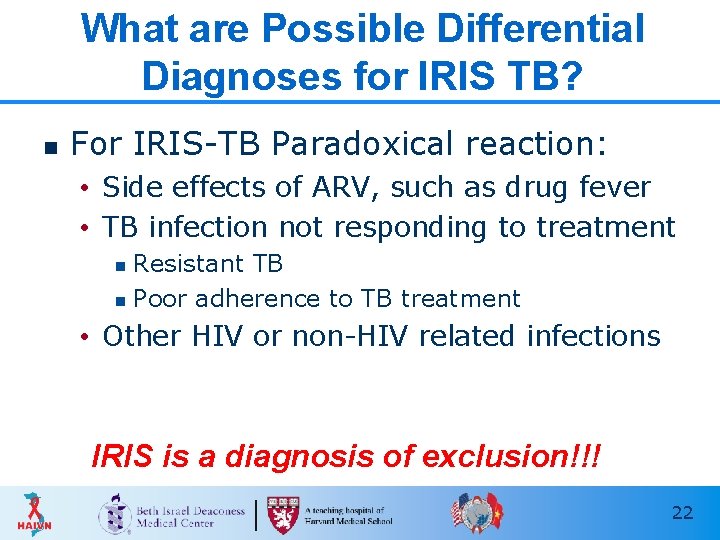
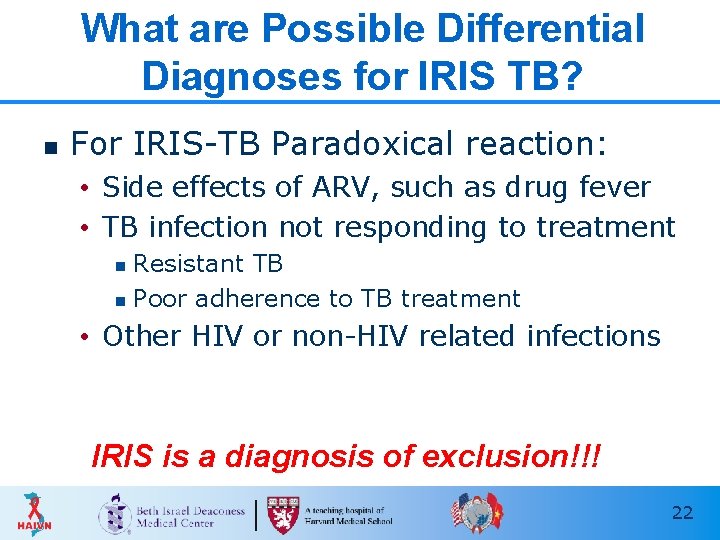
What are Possible Differential Diagnoses for IRIS TB? n For IRIS-TB Paradoxical reaction: • Side effects of ARV, such as drug fever • TB infection not responding to treatment Resistant TB n Poor adherence to TB treatment n • Other HIV or non-HIV related infections IRIS is a diagnosis of exclusion!!! 22
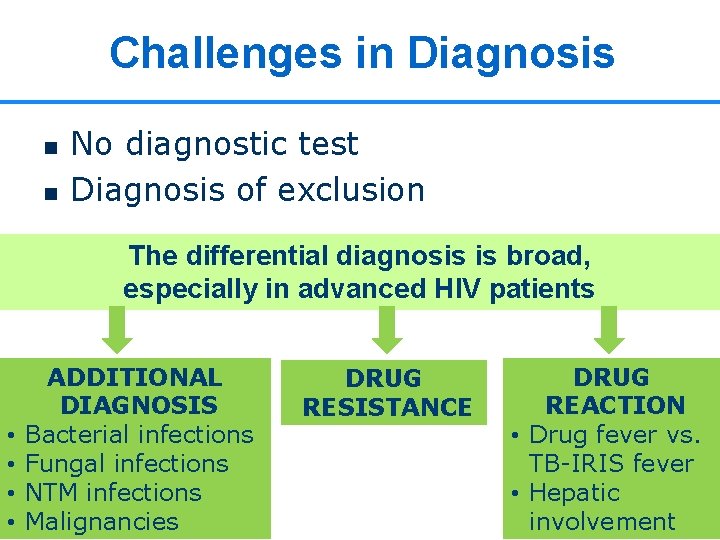
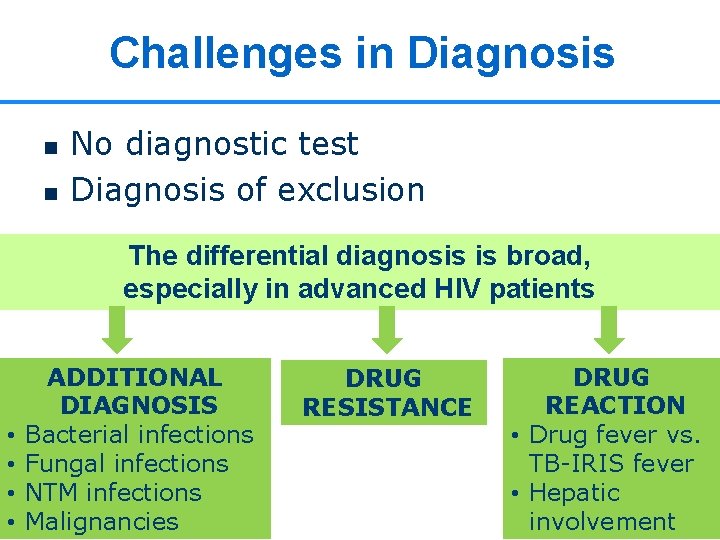
Challenges in Diagnosis n n No diagnostic test Diagnosis of exclusion The differential diagnosis is broad, especially in advanced HIV patients • • ADDITIONAL DIAGNOSIS Bacterial infections Fungal infections NTM infections Malignancies DRUG RESISTANCE DRUG REACTION • Drug fever vs. TB-IRIS fever • Hepatic involvement 23
IRIS Management 24
IRIS – Management (1) Most cases of IRIS can be easily managed by: n Continuing therapy against the primary opportunistic pathogen n Continuing ART n Anti-inflammatory agents n Providing reassurance to the patient 25
IRIS – Management (2) n Corticosteroids might be necessary in case of severe symptoms: • Worsening of meningeal, cerebral or mediastinal disease with compression of vital structures • Severe pain • Prolonged fever n In case of life-threatening forms of IRIS, stopping ARV temporarily should be considered 26
CASE STUDY 27
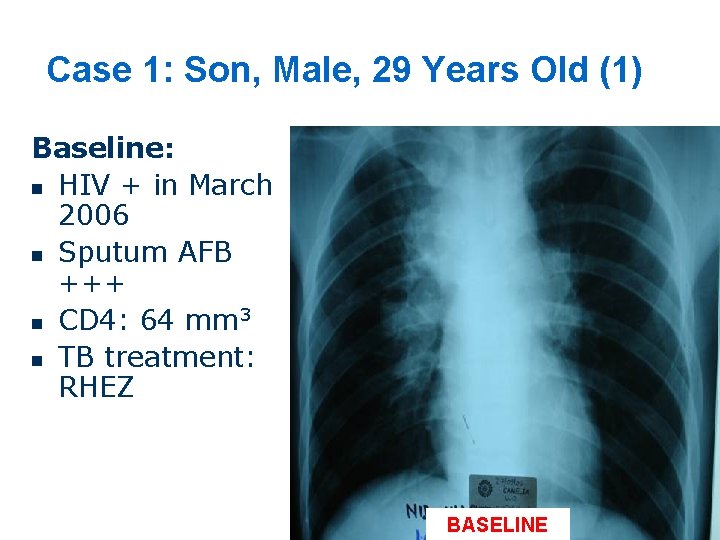
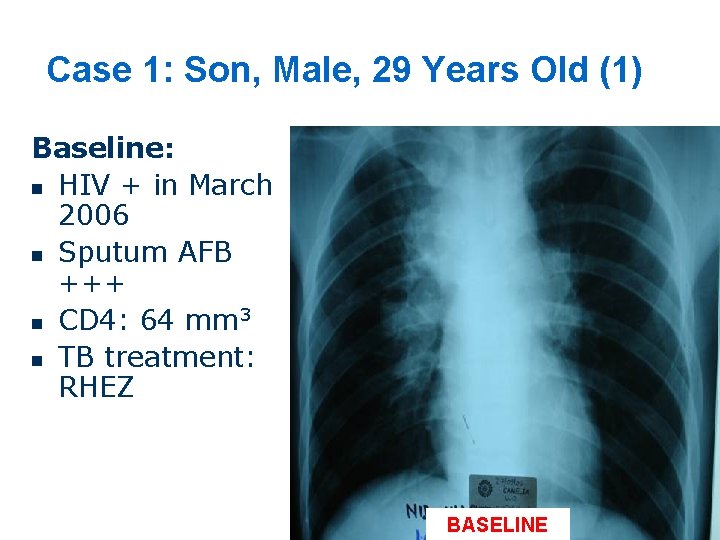
Case 1: Son, Male, 29 Years Old (1) Baseline: n HIV + in March 2006 n Sputum AFB +++ n CD 4: 64 mm 3 n TB treatment: RHEZ BASELINE 28
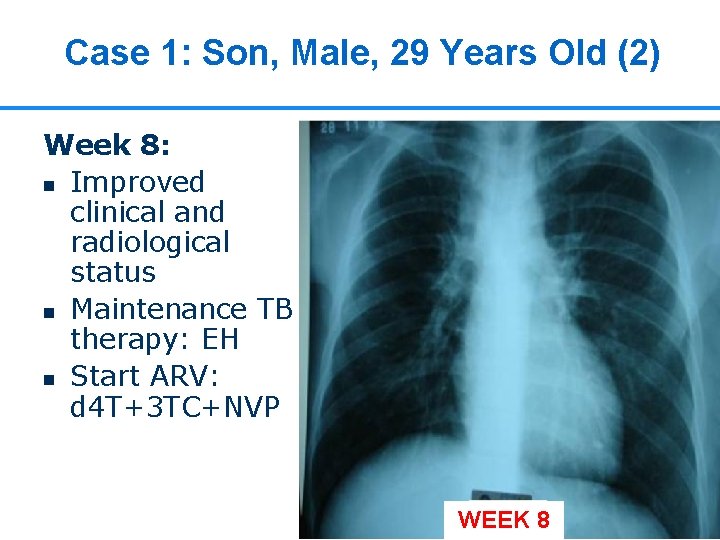
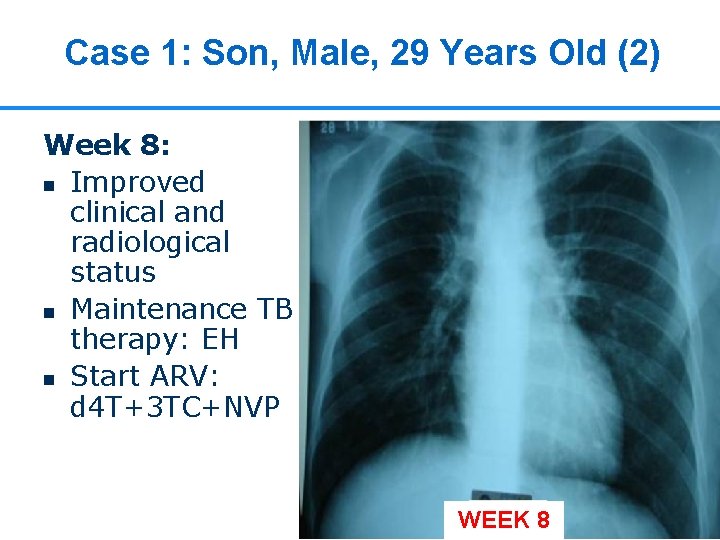
Case 1: Son, Male, 29 Years Old (2) Week 8: n Improved clinical and radiological status n Maintenance TB therapy: EH n Start ARV: d 4 T+3 TC+NVP WEEK 8 29

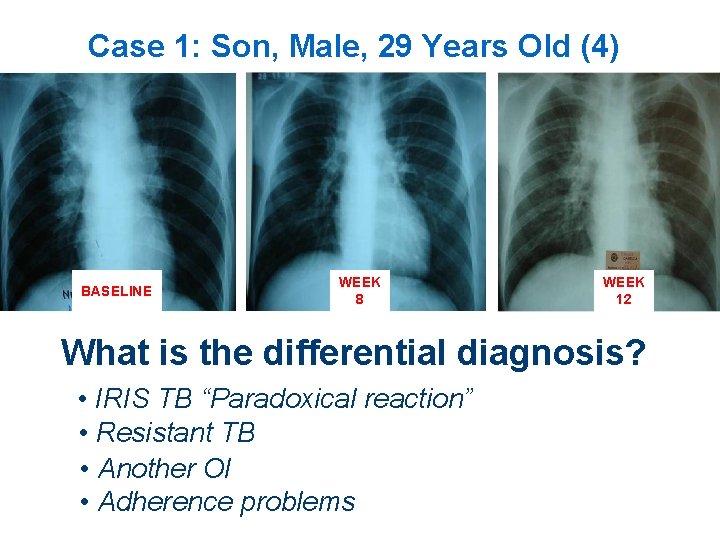
Case 1: Son, Male, 29 Years Old (3) After 1 months on ARV and 3 months of TB treatment: n The patient was hospitalized due to: • high fever • cough Week 12 WEEK 12 30
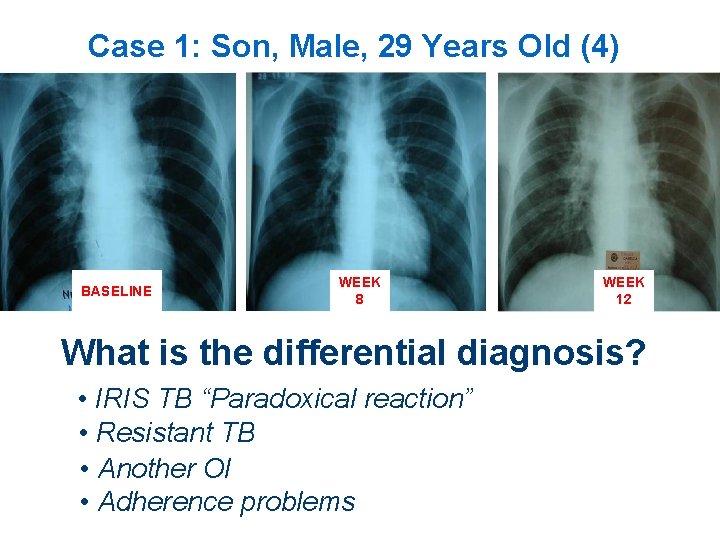
Case 1: Son, Male, 29 Years Old (4) BASELINE WEEK 8 WEEK 12 What is the differential diagnosis? • IRIS TB “Paradoxical reaction” • Resistant TB • Another OI • Adherence problems 31
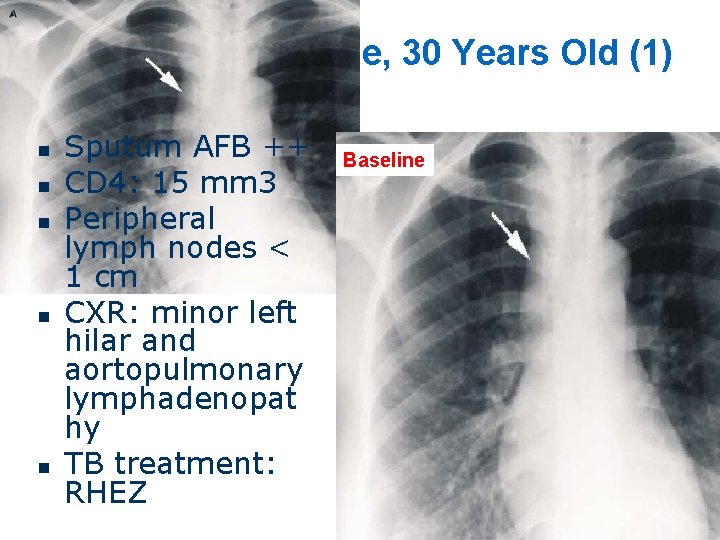
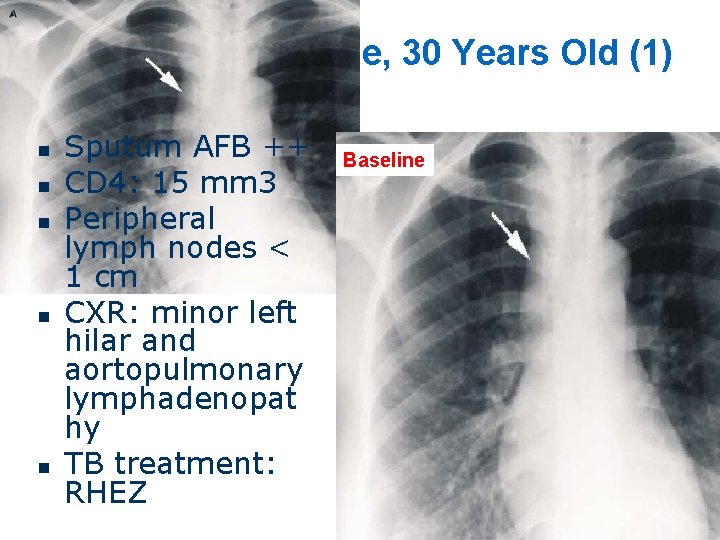
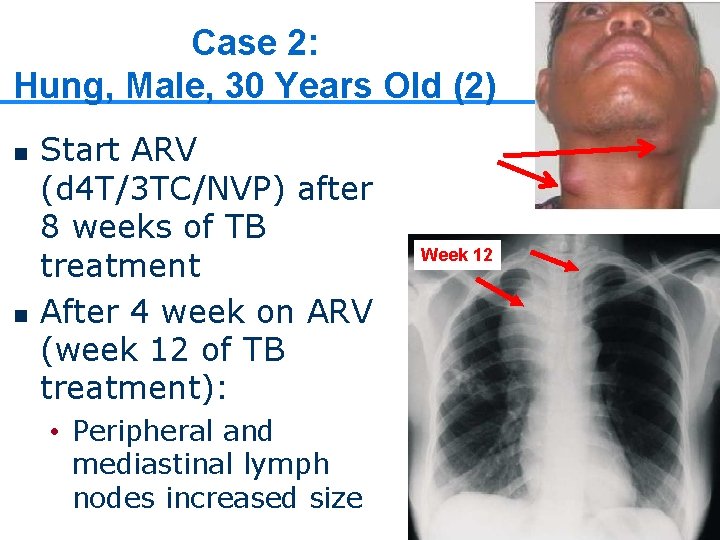
Case 2: Hung, Male, 30 Years Old (1) n n n Sputum AFB ++ CD 4: 15 mm 3 Peripheral lymph nodes < 1 cm CXR: minor left hilar and aortopulmonary lymphadenopat hy TB treatment: RHEZ Baseline
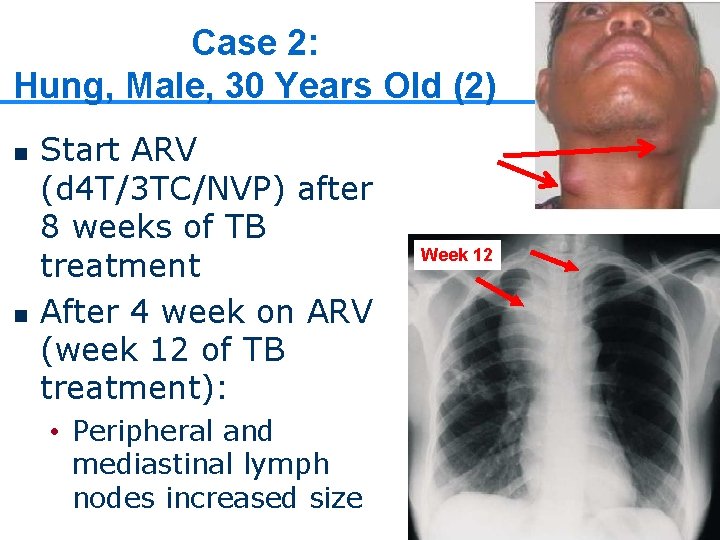
Case 2: Hung, Male, 30 Years Old (2) n n Start ARV (d 4 T/3 TC/NVP) after 8 weeks of TB treatment After 4 week on ARV (week 12 of TB treatment): • Peripheral and mediastinal lymph nodes increased size LN Week 12 33
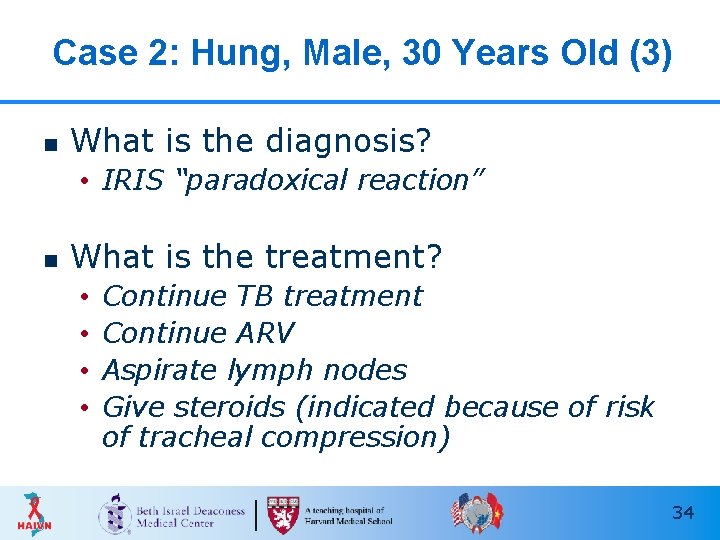
Case 2: Hung, Male, 30 Years Old (3) n What is the diagnosis? • IRIS “paradoxical reaction” n What is the treatment? • • Continue TB treatment Continue ARV Aspirate lymph nodes Give steroids (indicated because of risk of tracheal compression) 34
Key Points n IRIS is caused by a return of the immune response to antigens of opportunistic pathogens • Subclinical infections: Unmasking • Treated infections: Paradoxical n n Typically presents after 2 -12 weeks of ART Diagnosis of exclusion • Rule out adherence problems, new OIs n Treatment consists of: • OI therapy • ART • Anti-inflammatory therapy 35
Thank you! Questions? 36
 Immune reconstitution inflammatory syndrome
Immune reconstitution inflammatory syndrome Dr adria rusli
Dr adria rusli Immune reconstitution therapy
Immune reconstitution therapy Primary immune response and secondary immune response
Primary immune response and secondary immune response Hiv meaning
Hiv meaning Hiv from oral
Hiv from oral Haivn
Haivn Haivn
Haivn Haivn
Haivn Haivn
Haivn Iris hiv
Iris hiv Mucorrhea causes
Mucorrhea causes Mechanical vs inflammatory pain
Mechanical vs inflammatory pain Tromboflibitis
Tromboflibitis Inflammatory breast cancer pictures
Inflammatory breast cancer pictures Treatment of inflammatory breast cancer
Treatment of inflammatory breast cancer Paul charlson
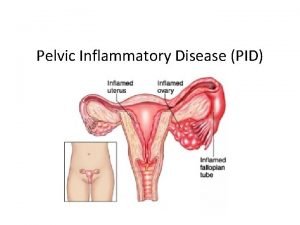
Paul charlson Pelvic inflammatory disease men
Pelvic inflammatory disease men Pelvic inflammatory disease
Pelvic inflammatory disease Pro and anti inflammatory
Pro and anti inflammatory Inflammatory cells
Inflammatory cells Types of colitis
Types of colitis Inflammation
Inflammation Botox injection sites
Botox injection sites Forum romain reconstitution
Forum romain reconstitution Théâtre de dionysos reconstitution
Théâtre de dionysos reconstitution Reconstitution calculation formula
Reconstitution calculation formula Reconstitution of medication
Reconstitution of medication Bagdad au ixe siècle
Bagdad au ixe siècle Medmath
Medmath Le forum rome
Le forum rome Reconstitution du forum romain
Reconstitution du forum romain Herpes zoster
Herpes zoster Delphes reconstitution
Delphes reconstitution Reconstitution of powdered drugs
Reconstitution of powdered drugs Harvard medical
Harvard medical Harvard medical school curriculum
Harvard medical school curriculum