Pediatric HIV Infection HAIVN Harvard Medical School AIDS




- Slides: 38
Pediatric HIV Infection HAIVN Harvard Medical School AIDS Initiative in Vietnam
Learning Objectives By the end of this session, participants should be able to: n Explain how to diagnose children with HIV n Describe WHO clinical staging for children n Explain when and how to initiate cotrimoxazole prophylaxis in children n List the 6 vaccines that are contraindicated in children with AIDS 2
Overview of Pediatric HIV n >90% of global pediatric HIV due to mother-to-child transmission (MTCT) • During pregnancy • During delivery n Most common time for infection • After delivery n Breastfeeding increases transmission risk by 5 -20% 3
Overview of MTCT n n What is the risk of transmission without intervention? The overall MTCT rate is approximately 25 -40% without intervention However, with current prophylactic strategies, the risk of transmission can be reduced to less than 2% 4
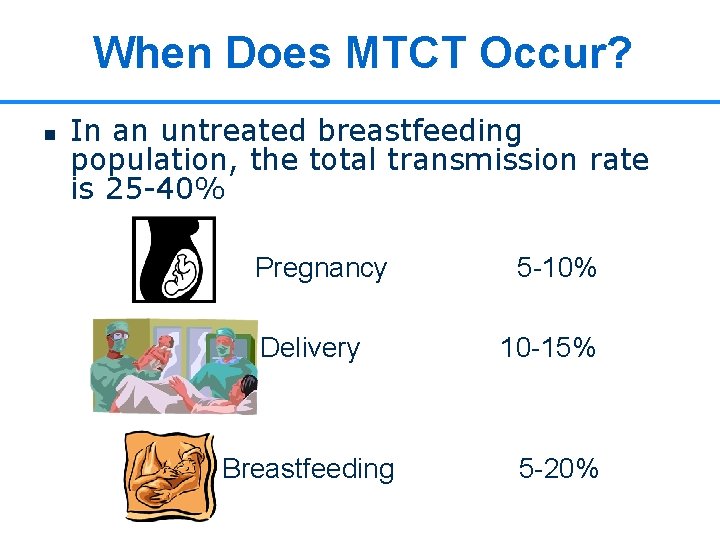
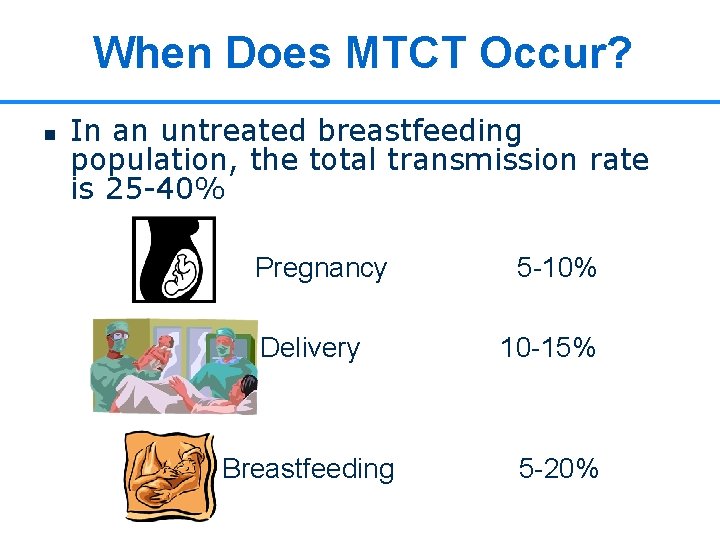
When Does MTCT Occur? n In an untreated breastfeeding population, the total transmission rate is 25 -40% Pregnancy Delivery Breastfeeding 5 -10% 10 -15% 5 -20% 5
Management of HIV-Exposed Infants and Children n n Make diagnosis as soon as possible Give appropriate vaccines and prophylaxis Start antiretroviral therapy when indicated (for HIV-infected infants) Recognize and treat opportunistic infections Support growth and development 6
Diagnosis of HIV Infection: > 18 Months n n Confirmed by the same HIV antibody test used for adults HIV infection is diagnosed when the serum gives 3 positive results in 3 tests with 3 different bioproducts Only laboratories certified by Mo. H are authorized to confirm HIV positive test results before reporting the result to patients Guidelines for the Diagnosis and Treatment of HIV/AIDS. Ministry of Health, 2009. 7
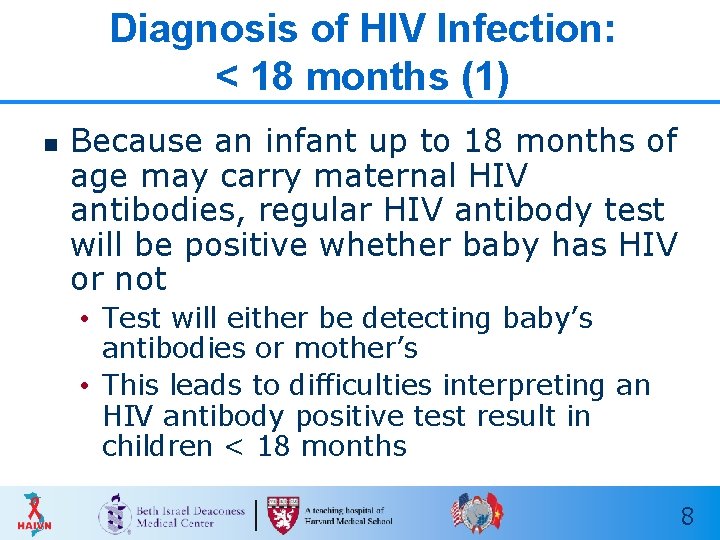
Diagnosis of HIV Infection: < 18 months (1) n Because an infant up to 18 months of age may carry maternal HIV antibodies, regular HIV antibody test will be positive whether baby has HIV or not • Test will either be detecting baby’s antibodies or mother’s • This leads to difficulties interpreting an HIV antibody positive test result in children < 18 months 8
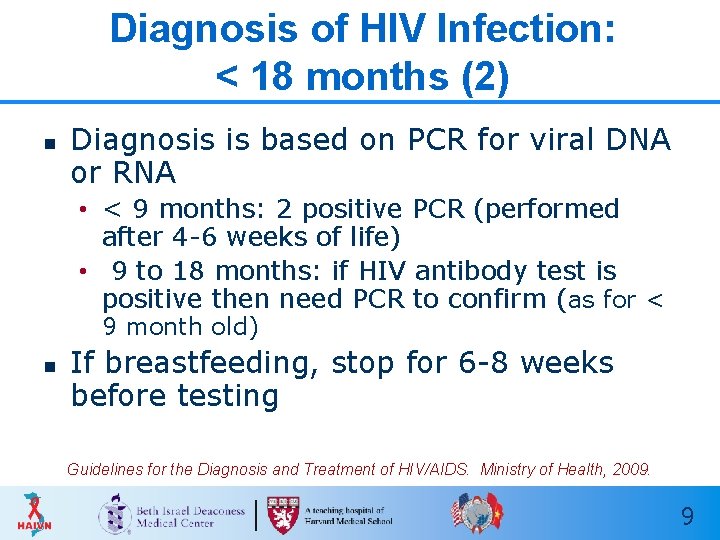
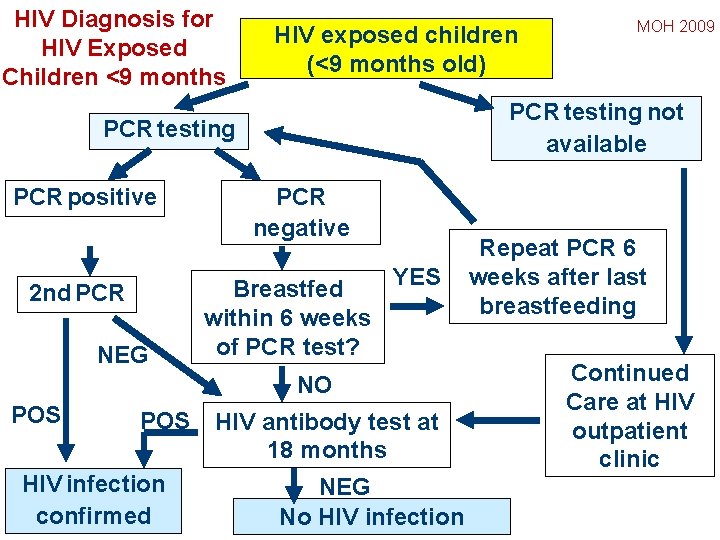
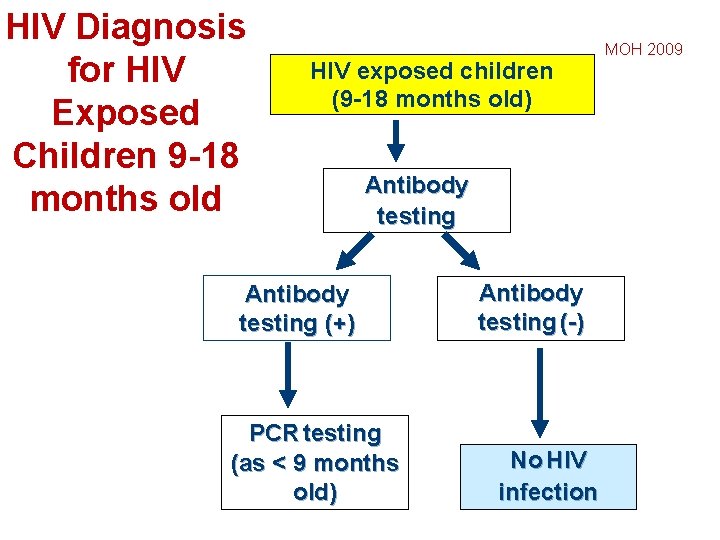
Diagnosis of HIV Infection: < 18 months (2) n Diagnosis is based on PCR for viral DNA or RNA • < 9 months: 2 positive PCR (performed after 4 -6 weeks of life) • 9 to 18 months: if HIV antibody test is positive then need PCR to confirm (as for < 9 month old) n If breastfeeding, stop for 6 -8 weeks before testing Guidelines for the Diagnosis and Treatment of HIV/AIDS. Ministry of Health, 2009. 9
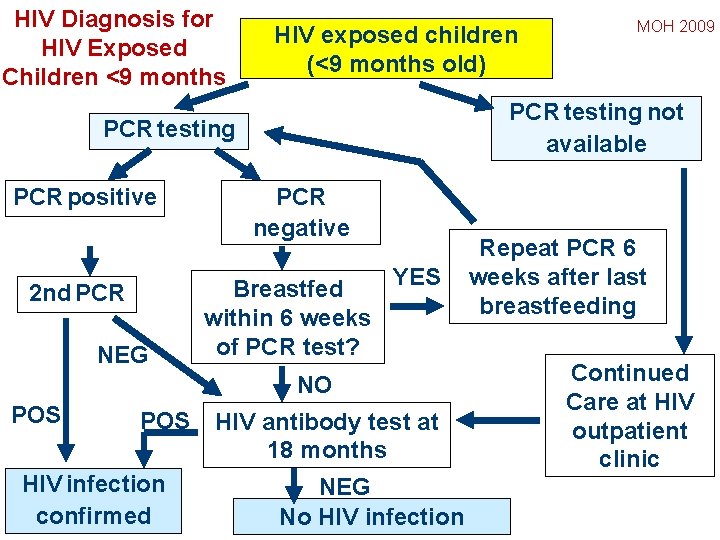
HIV Diagnosis for HIV Exposed Children <9 months HIV exposed children (<9 months old) PCR testing not available PCR testing PCR positive 2 nd PCR NEG PCR negative YES Breastfed within 6 weeks of PCR test? NO POS HIV infection confirmed MOH 2009 HIV antibody test at 18 months NEG No HIV infection Repeat PCR 6 weeks after last breastfeeding Continued Care at HIV outpatient clinic
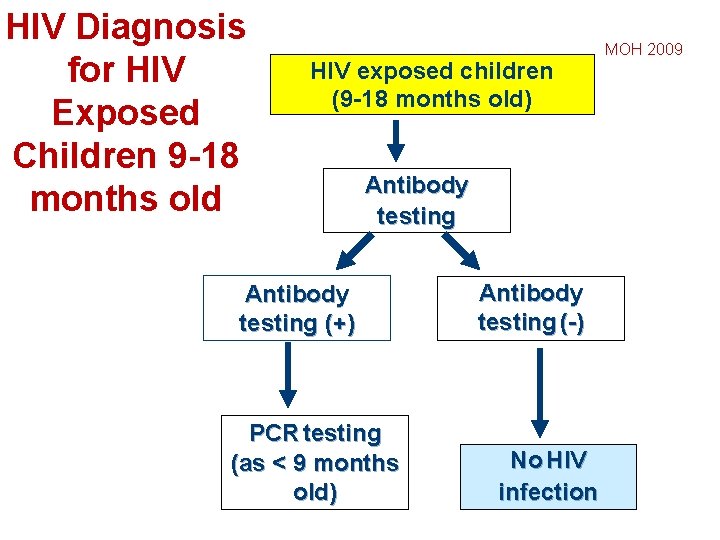
HIV Diagnosis for HIV Exposed Children 9 -18 months old HIV exposed children (9 -18 months old) Antibody testing (+) PCR testing (as < 9 months old) Antibody testing (-) No HIV infection MOH 2009
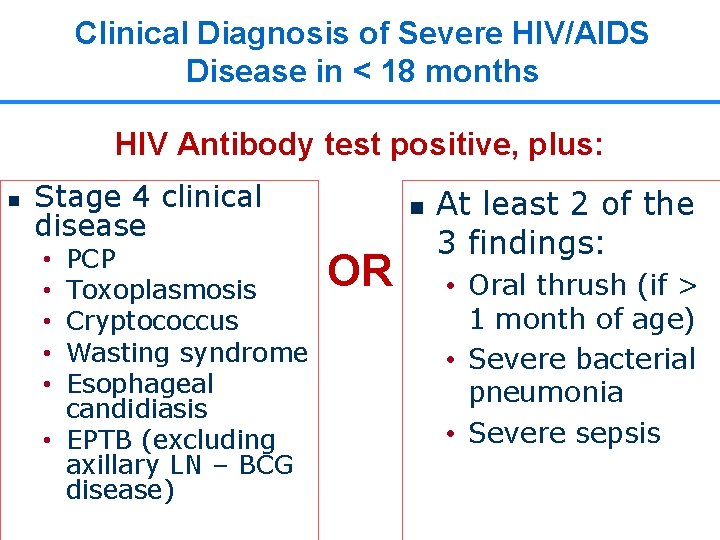
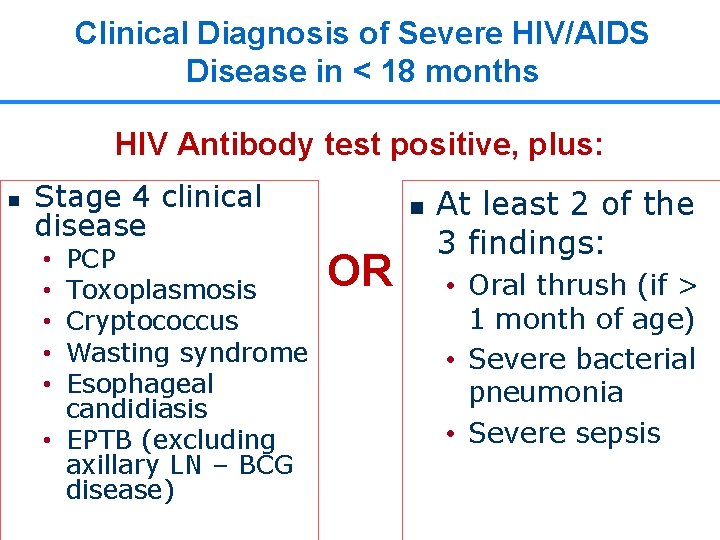
Clinical Diagnosis of Severe HIV/AIDS Disease in < 18 months HIV Antibody test positive, plus: n Stage 4 clinical disease PCP Toxoplasmosis Cryptococcus Wasting syndrome Esophageal candidiasis • EPTB (excluding axillary LN – BCG disease) • • • n OR At least 2 of the 3 findings: • Oral thrush (if > 1 month of age) • Severe bacterial pneumonia • Severe sepsis 12
Staging of Pediatric HIV Infection
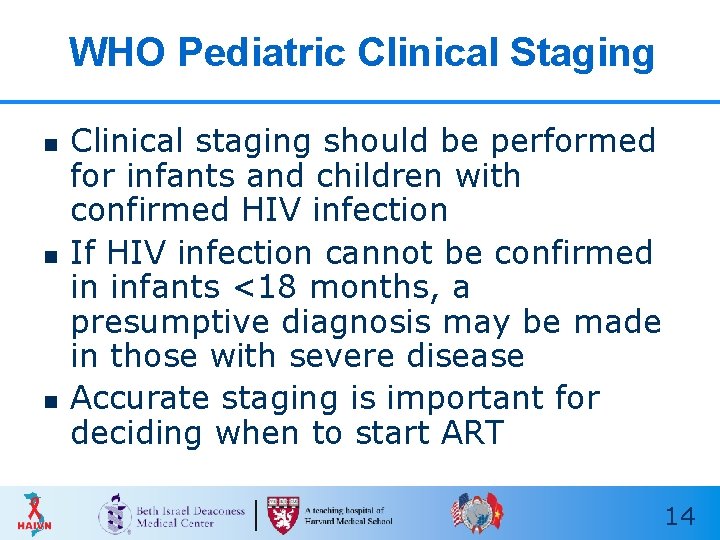
WHO Pediatric Clinical Staging n n n Clinical staging should be performed for infants and children with confirmed HIV infection If HIV infection cannot be confirmed in infants <18 months, a presumptive diagnosis may be made in those with severe disease Accurate staging is important for deciding when to start ART 14
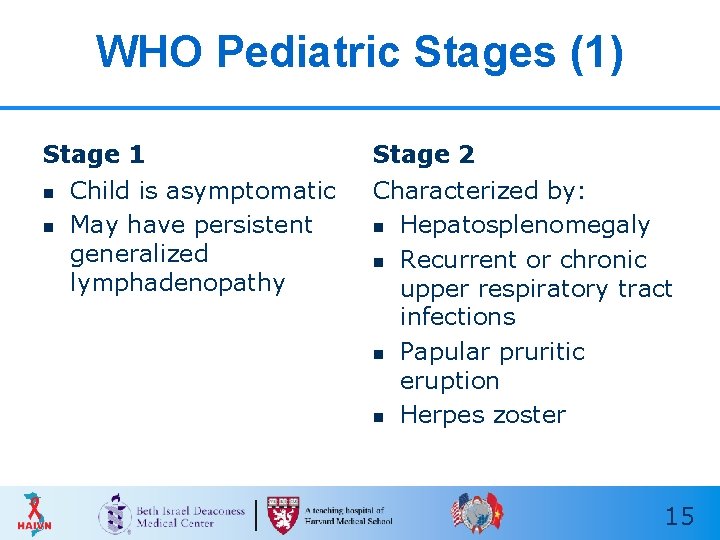
WHO Pediatric Stages (1) Stage 1 n n Child is asymptomatic May have persistent generalized lymphadenopathy Stage 2 Characterized by: n Hepatosplenomegaly n Recurrent or chronic upper respiratory tract infections n Papular pruritic eruption n Herpes zoster 15
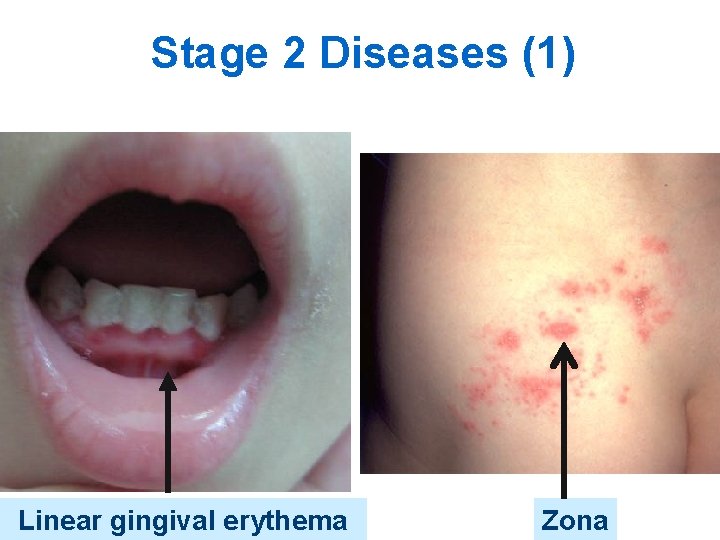
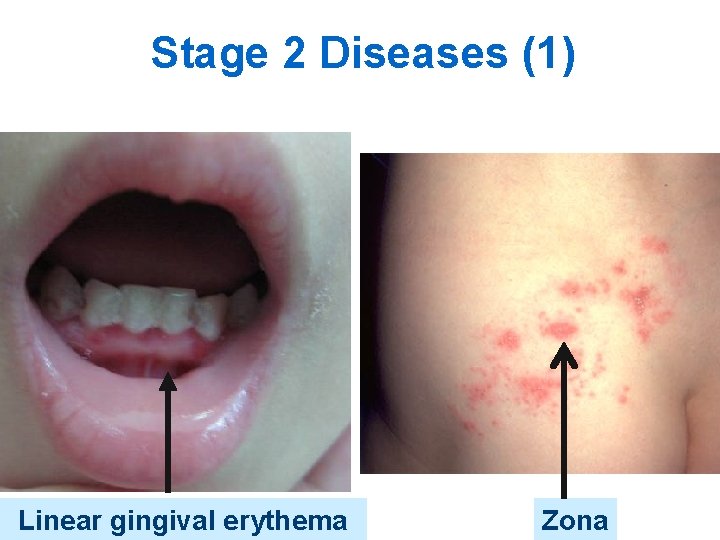
Stage 2 Diseases (1) Linear gingival erythema Zona

Stage 2 Diseases (2) PPE: lower arms and legs, leaves scarring after resolution

Stage 2 Diseases (3) Bilateral parotid enlargement
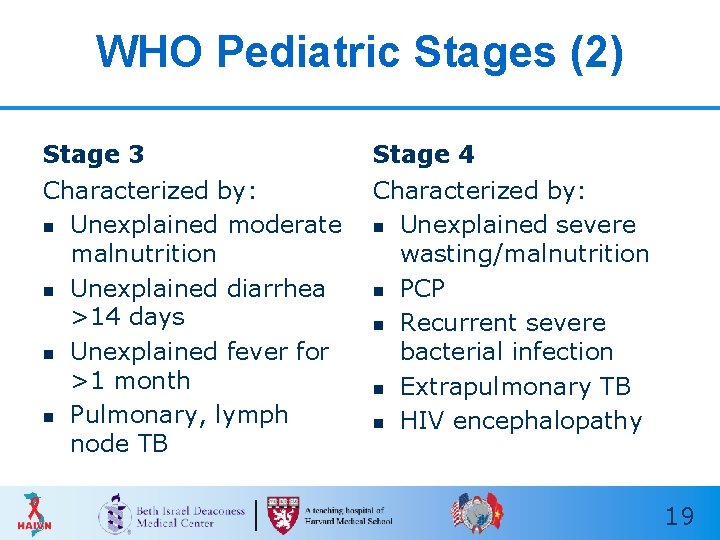
WHO Pediatric Stages (2) Stage 3 Stage 4 Characterized by: n Unexplained moderate malnutrition n Unexplained diarrhea >14 days n Unexplained fever for >1 month n Pulmonary, lymph node TB Characterized by: n Unexplained severe wasting/malnutrition n PCP n Recurrent severe bacterial infection n Extrapulmonary TB n HIV encephalopathy 19
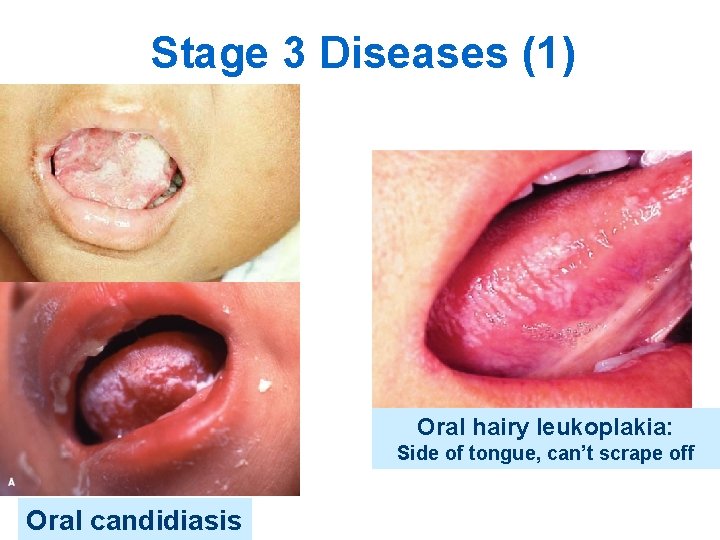
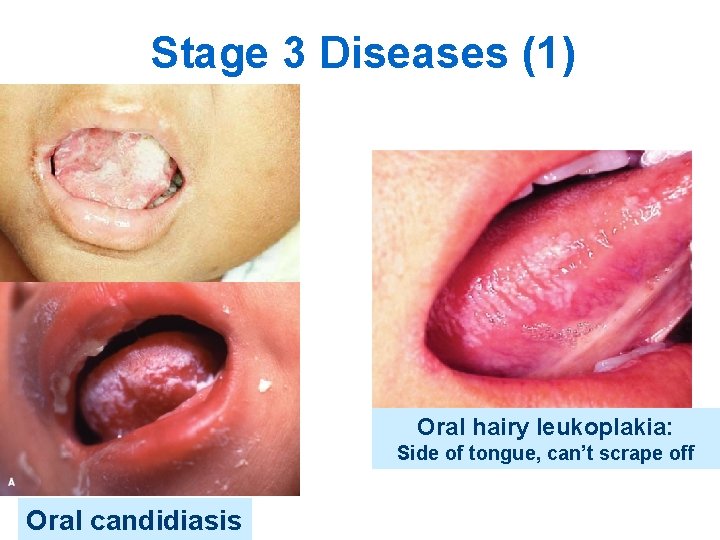
Stage 3 Diseases (1) Oral hairy leukoplakia: Side of tongue, can’t scrape off Oral candidiasis
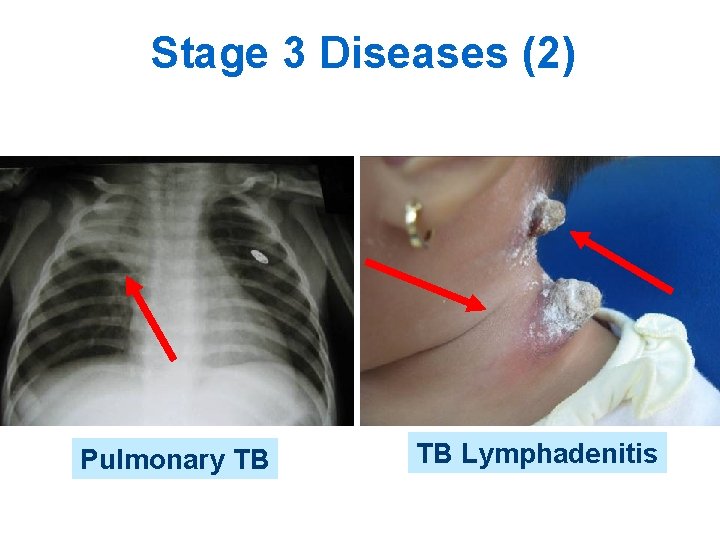
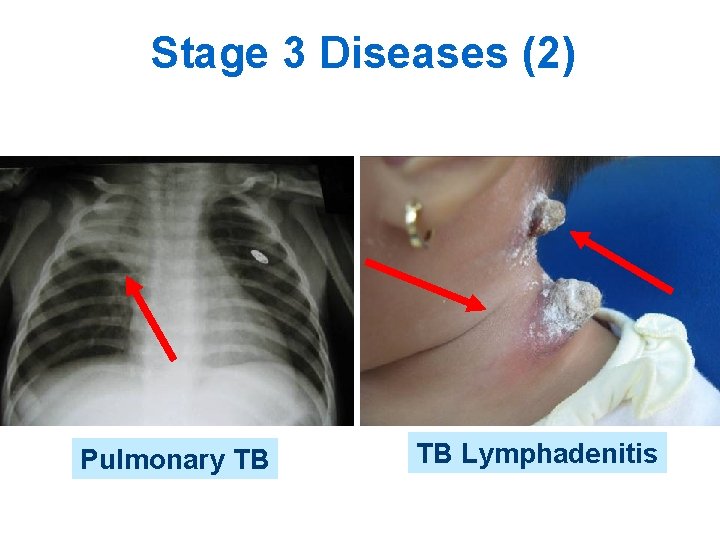
Stage 3 Diseases (2) Pulmonary TB TB Lymphadenitis
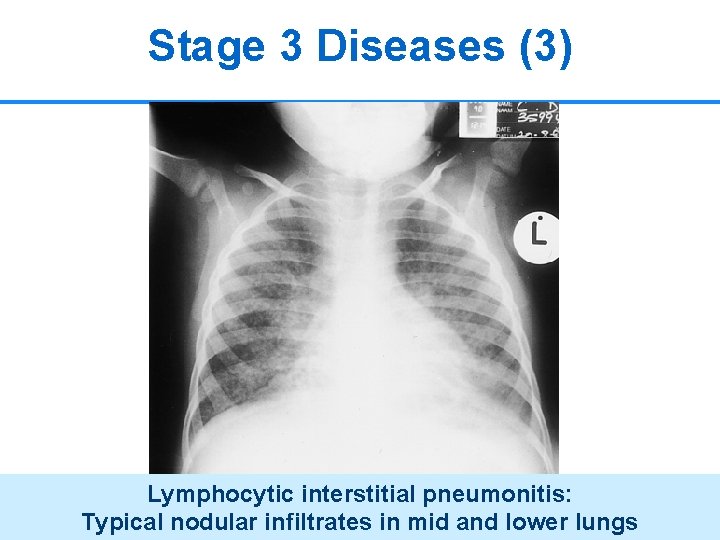
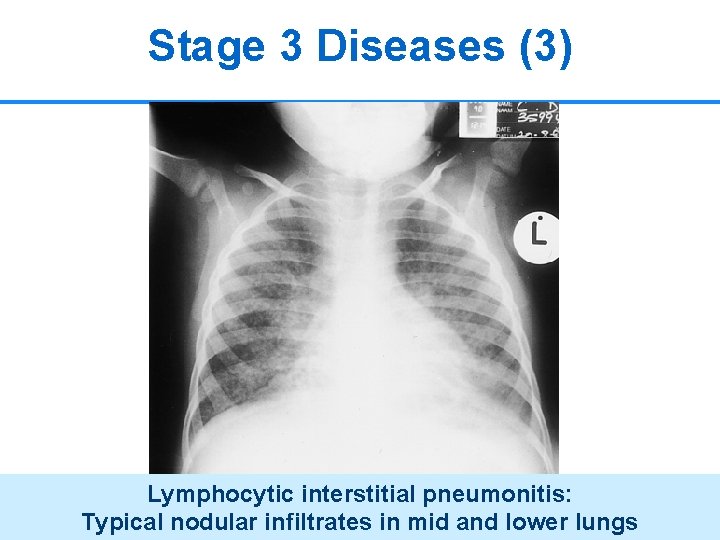
Stage 3 Diseases (3) Lymphocytic interstitial pneumonitis: Typical nodular infiltrates in mid and lower lungs 22

Stage 4 Diseases (1) Herpes Simplex chronic infection (>1 month)
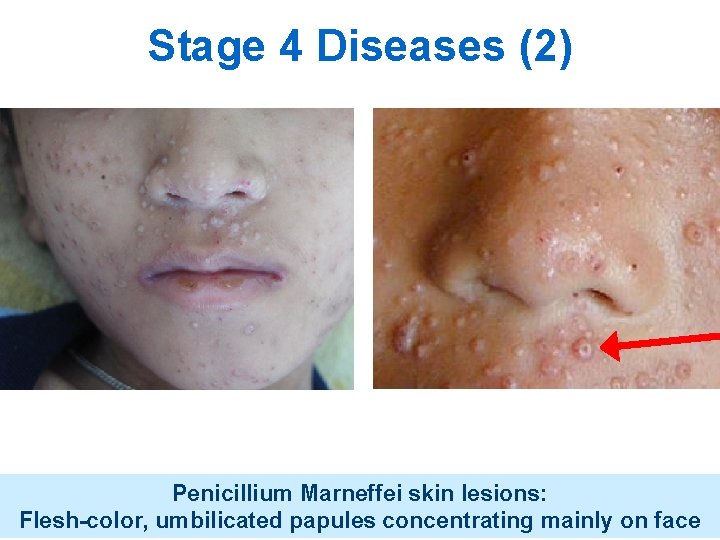
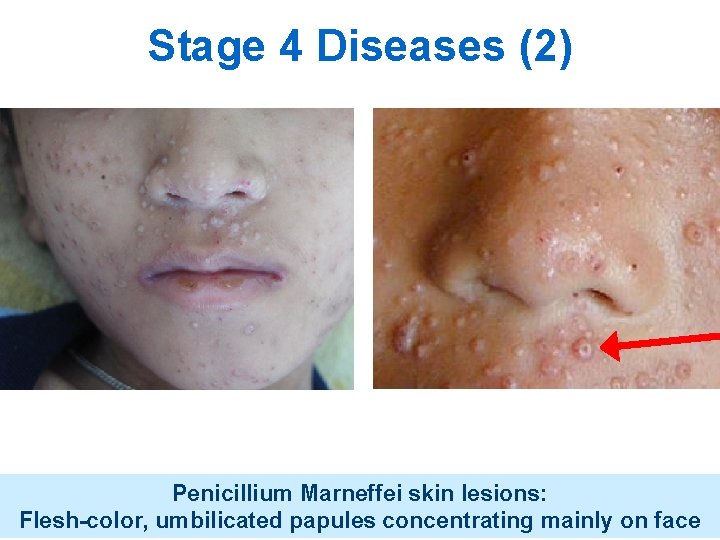
Stage 4 Diseases (2) Penicillium Marneffei skin lesions: Flesh-color, umbilicated papules concentrating mainly on face
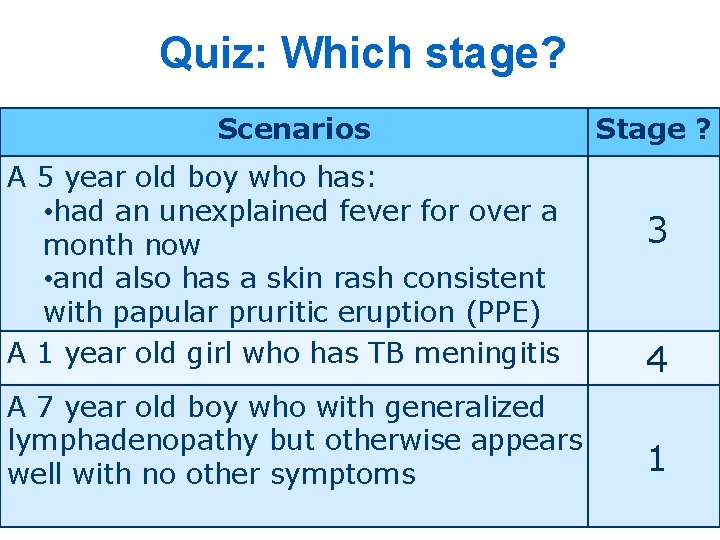
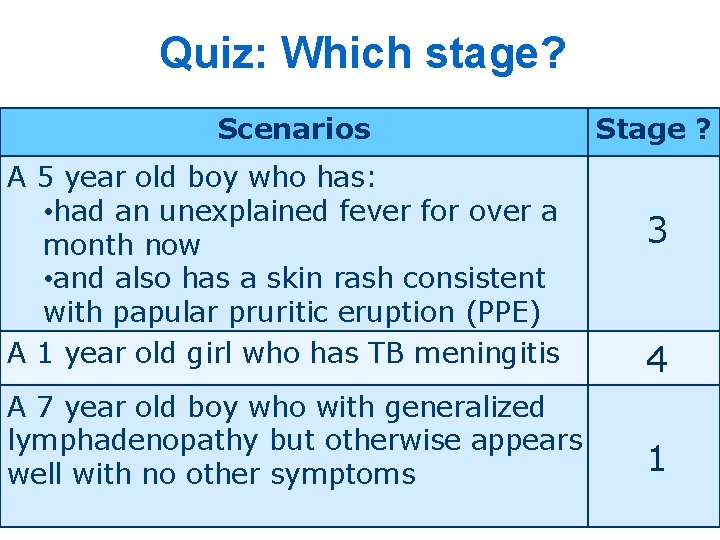
Quiz: Which stage? Scenarios A 5 year old boy who has: • had an unexplained fever for over a month now • and also has a skin rash consistent with papular pruritic eruption (PPE) A 1 year old girl who has TB meningitis A 7 year old boy who with generalized lymphadenopathy but otherwise appears well with no other symptoms Stage ? 3 4 1
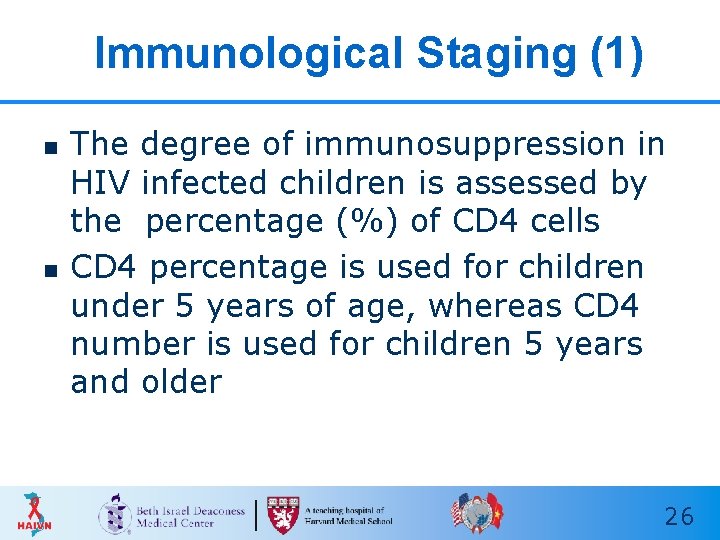
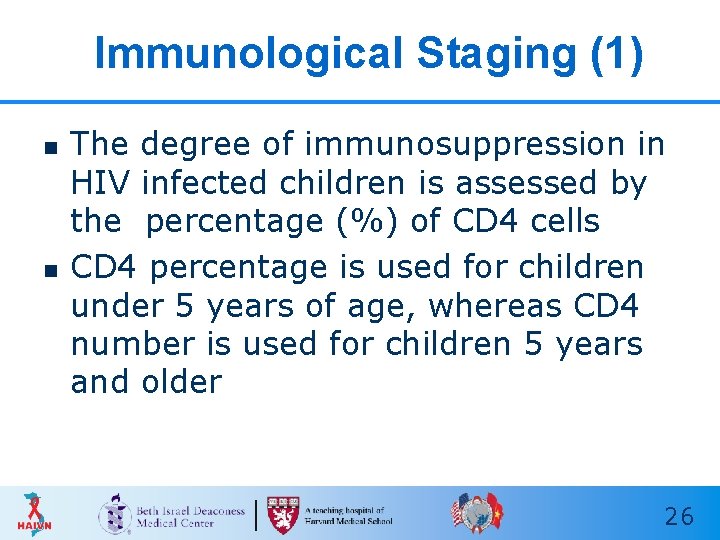
Immunological Staging (1) n n The degree of immunosuppression in HIV infected children is assessed by the percentage (%) of CD 4 cells CD 4 percentage is used for children under 5 years of age, whereas CD 4 number is used for children 5 years and older 26
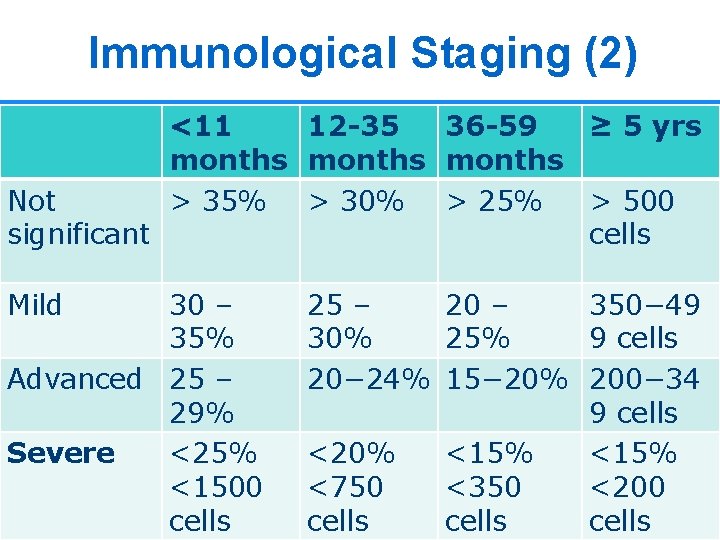
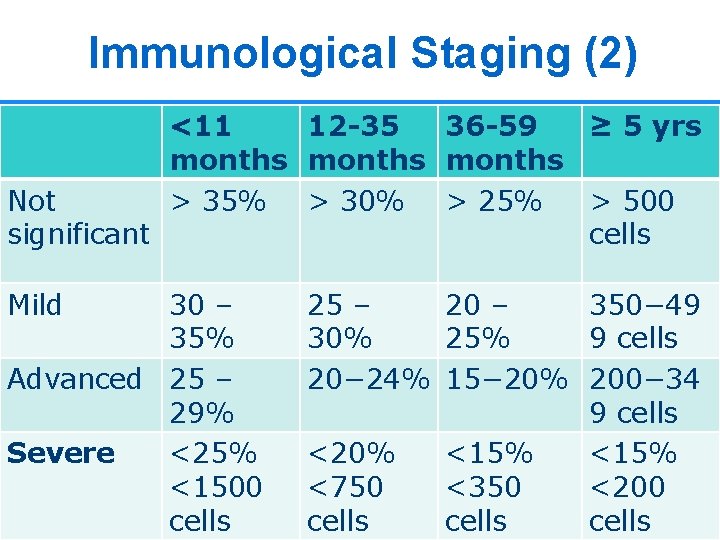
Immunological Staging (2) <11 12 -35 36 -59 ≥ 5 yrs months Not > 35% > 30% > 25% > 500 significant cells Mild 30 – 35% Advanced 25 – 29% Severe <25% <1500 cells 25 – 20 – 350− 49 30% 25% 9 cells 20− 24% 15− 20% 200− 34 9 cells <20% <15% <750 <350 <200 cells 27
Overview on Care and Treatment of Children with HIV/AIDS
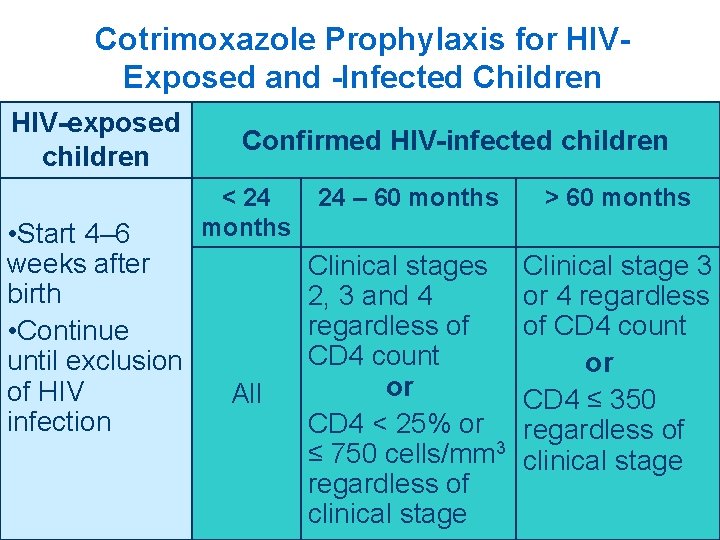
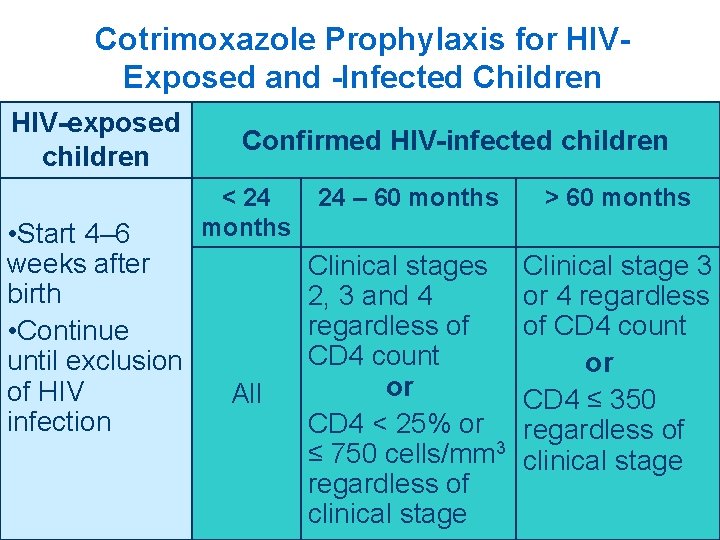
Cotrimoxazole Prophylaxis for HIVExposed and -Infected Children HIV-exposed children • Start 4– 6 weeks after birth • Continue until exclusion of HIV infection Confirmed HIV-infected children < 24 months All 24 – 60 months > 60 months Clinical stages 2, 3 and 4 regardless of CD 4 count or CD 4 < 25% or ≤ 750 cells/mm 3 regardless of clinical stage Clinical stage 3 or 4 regardless of CD 4 count or CD 4 ≤ 350 regardless of clinical stage 29
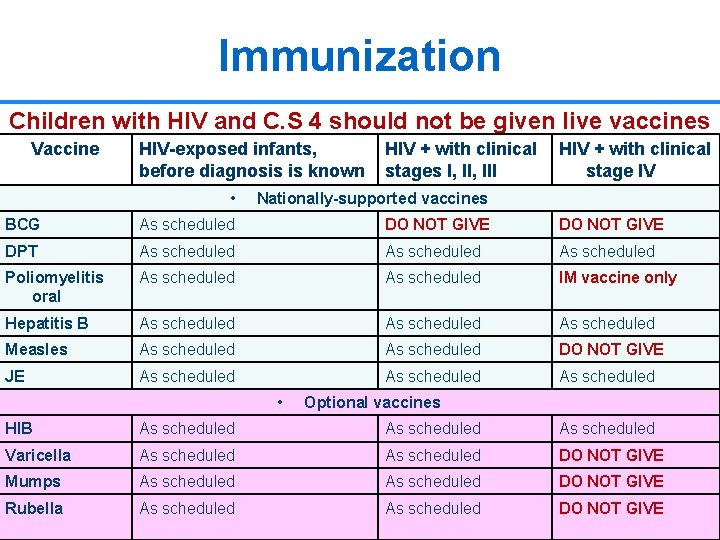
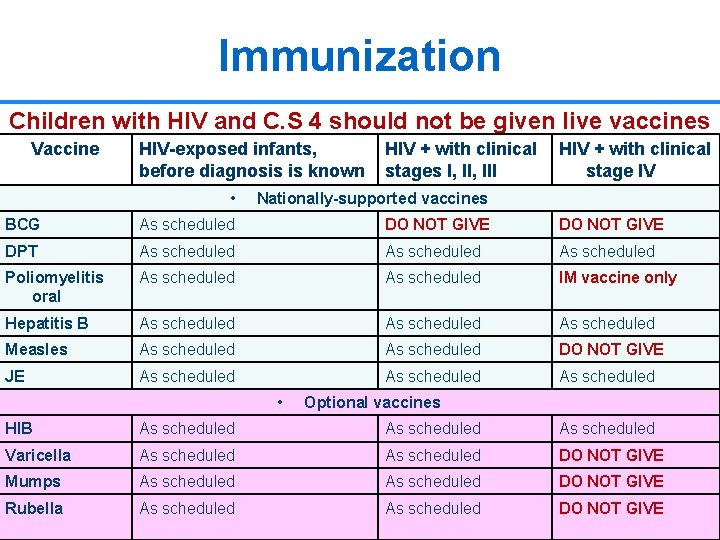
Immunization Children with HIV and C. S 4 should not be given live vaccines Vaccine HIV-exposed infants, before diagnosis is known HIV + with clinical stages I, III HIV + with clinical stage IV • Nationally-supported vaccines BCG As scheduled DO NOT GIVE DPT As scheduled Poliomyelitis oral As scheduled IM vaccine only Hepatitis B As scheduled Measles As scheduled DO NOT GIVE JE As scheduled • Optional vaccines HIB As scheduled Varicella As scheduled DO NOT GIVE Mumps As scheduled DO NOT GIVE Rubella As scheduled DO NOT GIVE 30
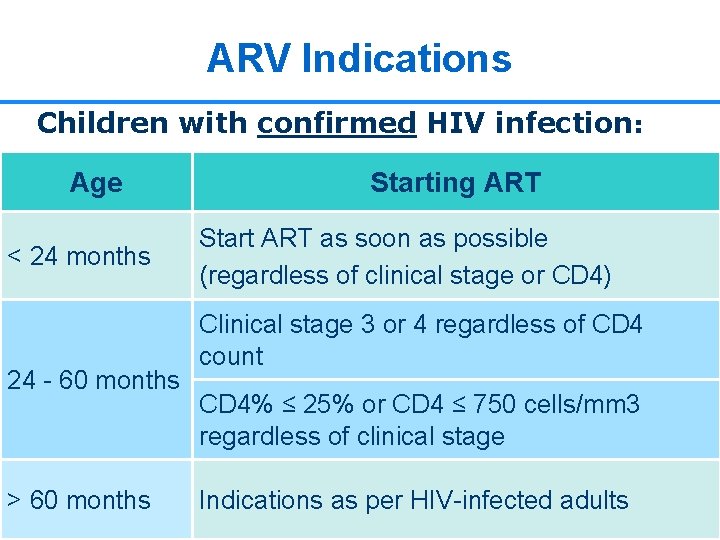
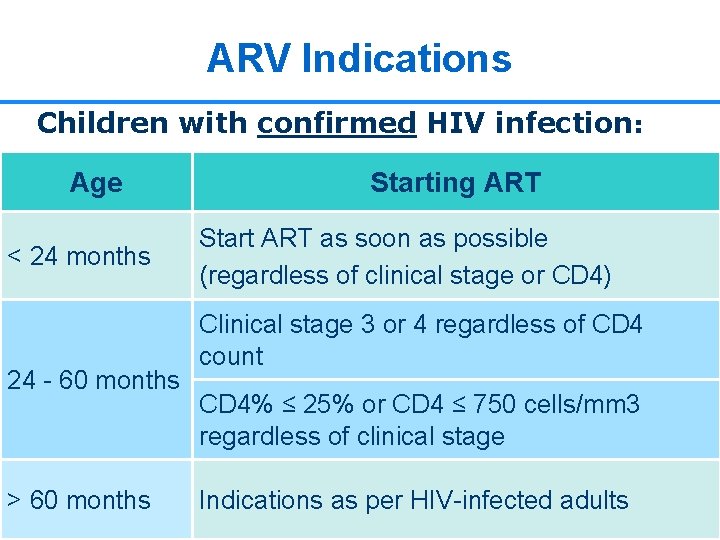
ARV Indications Children with confirmed HIV infection: Age < 24 months 24 - 60 months > 60 months Starting ART Start ART as soon as possible (regardless of clinical stage or CD 4) Clinical stage 3 or 4 regardless of CD 4 count CD 4% ≤ 25% or CD 4 ≤ 750 cells/mm 3 regardless of clinical stage Indications as per HIV-infected adults 31
Common Opportunistic Infections in HIV-infected Children
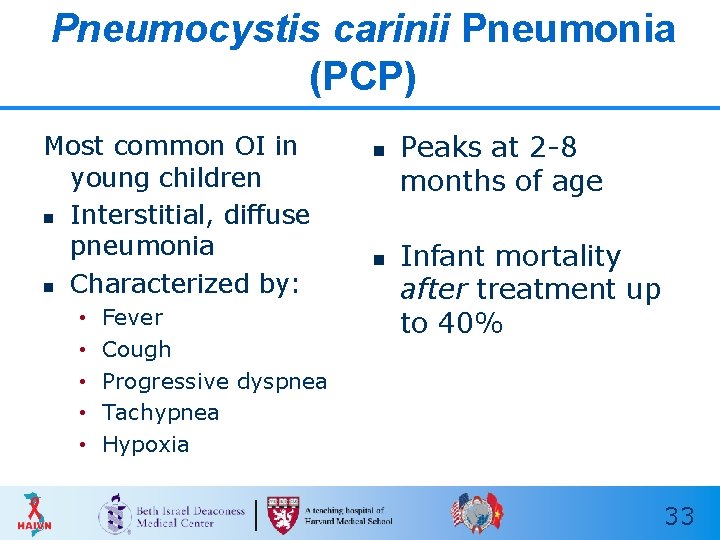
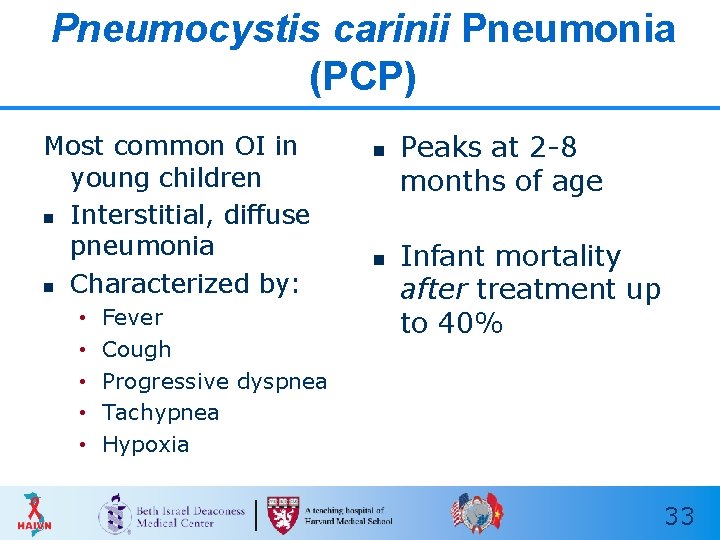
Pneumocystis carinii Pneumonia (PCP) Most common OI in young children n Interstitial, diffuse pneumonia n Characterized by: • • • Fever Cough Progressive dyspnea Tachypnea Hypoxia n n Peaks at 2 -8 months of age Infant mortality after treatment up to 40% 33
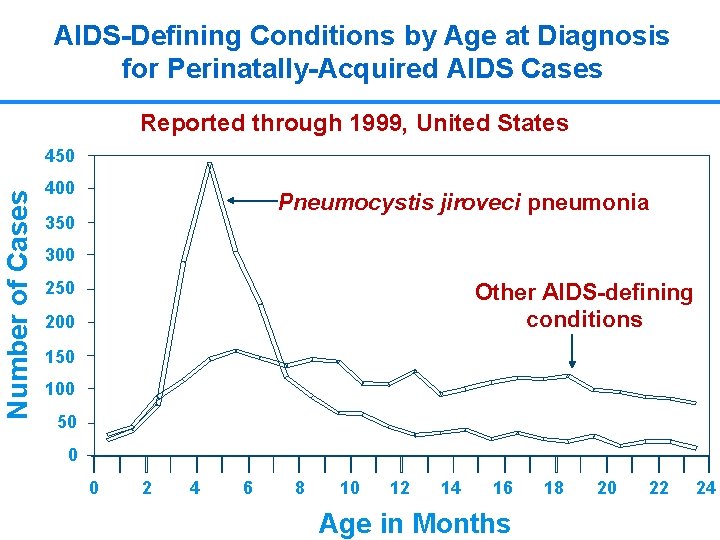
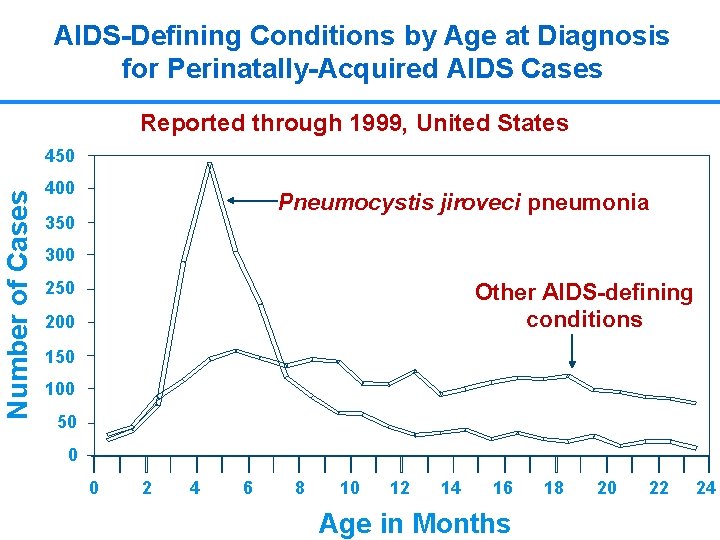
AIDS-Defining Conditions by Age at Diagnosis for Perinatally-Acquired AIDS Cases Reported through 1999, United States Number of Cases 450 400 Pneumocystis jiroveci pneumonia 350 300 250 Other AIDS-defining conditions 200 150 100 50 0 0 2 4 6 8 10 12 14 16 Age in Months 18 20 22 34 24
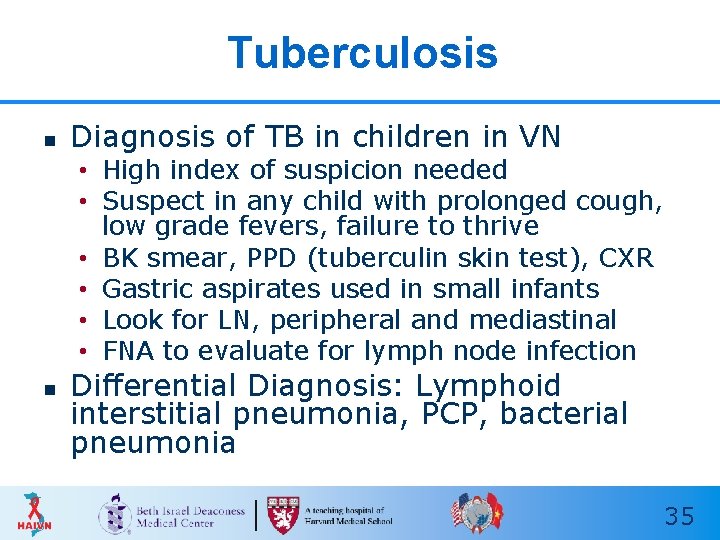
Tuberculosis n Diagnosis of TB in children in VN • High index of suspicion needed • Suspect in any child with prolonged cough, low grade fevers, failure to thrive • BK smear, PPD (tuberculin skin test), CXR • Gastric aspirates used in small infants • Look for LN, peripheral and mediastinal • FNA to evaluate for lymph node infection n Differential Diagnosis: Lymphoid interstitial pneumonia, PCP, bacterial pneumonia 35
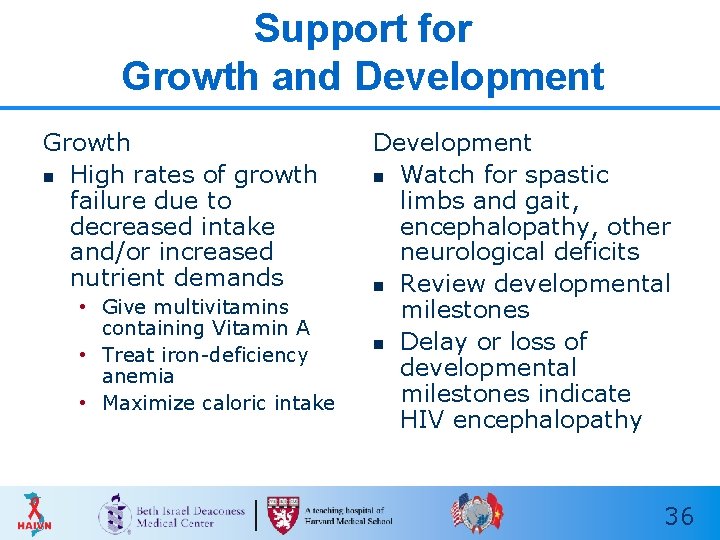
Support for Growth and Development Growth n High rates of growth failure due to decreased intake and/or increased nutrient demands • Give multivitamins containing Vitamin A • Treat iron-deficiency anemia • Maximize caloric intake Development n Watch for spastic limbs and gait, encephalopathy, other neurological deficits n Review developmental milestones n Delay or loss of developmental milestones indicate HIV encephalopathy 36
Key Points n Most children get HIV through motherto child transmission • Children > 18 months are tested with antibody test • Younger children may still carry mother’s antibodies, need different testing strategy n n Use clinical and immunological staging to determine ART eligibility Important to look closely at child’s growth and development markers for clues about health 37

Thank you! Questions?
 Test wiedzy o hiv i aids z odpowiedziami
Test wiedzy o hiv i aids z odpowiedziami Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Causative organism of hiv/aids
Causative organism of hiv/aids Chapter 17 oral pathology
Chapter 17 oral pathology Kasus hiv aids
Kasus hiv aids Haivn
Haivn Received oral from hiv positive
Received oral from hiv positive What is receptive vaginal sex
What is receptive vaginal sex Haivn
Haivn Haivn
Haivn Haivn
Haivn Harvard medical school curriculum
Harvard medical school curriculum Harvard medical
Harvard medical Harvard class schedule
Harvard class schedule Harvard summer school study abroad
Harvard summer school study abroad Michael luca harvard business school
Michael luca harvard business school Hbsp coursepack
Hbsp coursepack Triệu chứng nhiễm hiv
Triệu chứng nhiễm hiv Hiv reverse transcription
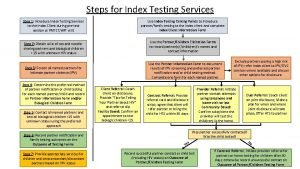
Hiv reverse transcription Hiv index testing steps
Hiv index testing steps Snars 1.1 prognas
Snars 1.1 prognas Phdp in hiv
Phdp in hiv Chii chinonzi hiv
Chii chinonzi hiv Window period hiv
Window period hiv Why do the bodys antibodies fail to protect people from hiv
Why do the bodys antibodies fail to protect people from hiv Iris syndrome
Iris syndrome Hiv
Hiv Hiv risk factors
Hiv risk factors Asante hiv-1 rapid recency assay
Asante hiv-1 rapid recency assay Fiebig hiv
Fiebig hiv Hiv case-based surveillance in ethiopia
Hiv case-based surveillance in ethiopia Triệu chứng nhiễm hiv
Triệu chứng nhiễm hiv Basic hiv course
Basic hiv course Stakeholders in hiv prevention
Stakeholders in hiv prevention Hiv treatments
Hiv treatments What does hiv stand
What does hiv stand Aids 101
Aids 101 Hiv test window period
Hiv test window period