Howard Padwa Ph D University of California Los







- Slides: 69
Howard Padwa, Ph. D. University of California, Los Angeles Integrated Substance Abuse Programs Transforming Treatment: Treating Substance Use Disorders as Health Conditions South Carolina Department of Alcohol and Other Drug Abuse Services University of South Carolina Recovery Program Transformation & Innovation Fund Conference September 10, 2015 1
Recovery Program Transformation & Innovation Fund • Four priority areas for Planning and Implementation Grants: – Medication Assisted Treatment – Integration of Behavioral Health Services (mental health, medical) – Adolescent/family services – forming and strengthening partnerships – Infrastructure for accessible, integrated services • Reflect national and historic trend toward treating substance use disorders (SUD) like we treat other health conditions 2
Transformation: Seeing SUDs as Health Conditions • Historically, problematic alcohol/drug use seen as a vice, moral failing, weakness, or choice • Association of substances with racial, political “enemies” • Major policy responses: – Control supply – Punitive approach to users 3
Transformation: Seeing SUDs as Health Conditions • 1940 s-2000 s: Recognition of SUD as a medical problem • Mc. Lellan et al. , “Drug Dependence, A Chronic Medical Illness” published in JAMA (2000) • Compared SUD to diabetes, hypertension, asthma • Similar roles of genetics, personal choice, environment • Comparable outcomes if managed with behavior modification, ongoing monitoring, medications • Clinical argument for increased insurance/primary care involvement, on par with other medical conditions 4

Transformation: Bringing Treatment Out Of Isolation • SUD Treatment Has Been Isolated – Inebriate Asylums, Narcotic Farms – Criminal Justice Settings – Methadone Clinics • Peer support emphasis – 12 -Step focus – Therapeutic Communities • Most SUD treatment occurred in places that only focused on SUD 5
Transformation: Bringing Treatment Out Of Isolation • 2008 Wellstone-Domenici Mental Health and Addiction Equity Parity Act • 2010 Affordable Care Act • Assure coverage of SUD in parity with other health benefits • Encouraging integration of SUD services into other health settings, service systems • Holding SUD services up to same standards as other areas of 6 medicine
Transformation of SUD Services • Two interrelated changes • Treating SUD like other medical conditions • Bringing SUD services in to the health care system 7
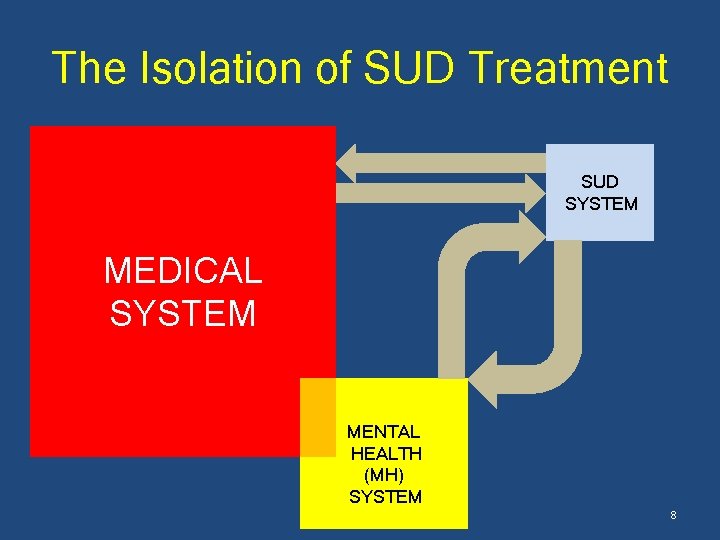
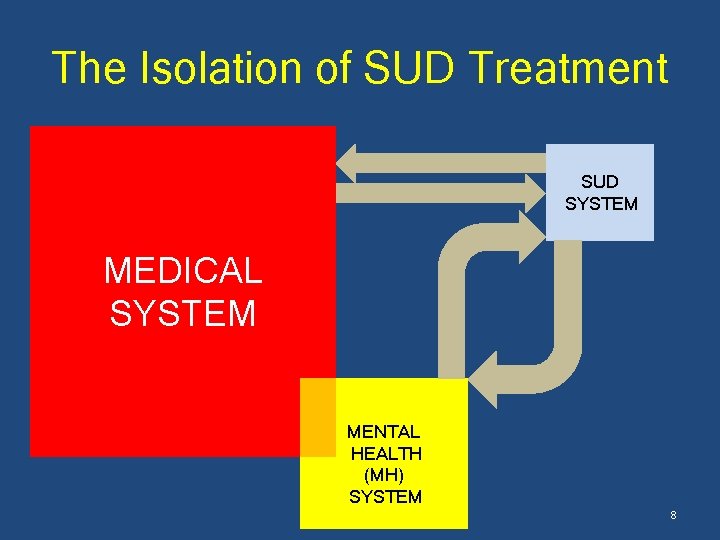
The Isolation of SUD Treatment SUD SYSTEM MEDICAL SYSTEM MENTAL HEALTH (MH) SYSTEM 8
Making Services More Patient-Centered • The burden of coordinating care and meeting population needs “should rest on the system, not the families or consumers who are already struggling because of a serious illness. ” President’s New Freedom Commission, 2003 9
Making Services More Patient-Centered • One of the major goals of health care reform is to move from services that are systemcentered to ones that are patient-centered. • Integration can make services more patientcentered. – For SUD clients – For people who would benefit from SU services but do not receive them 10
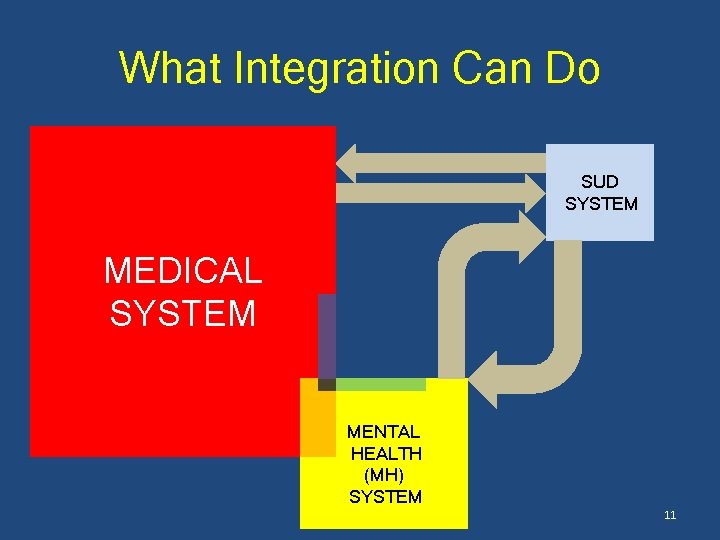
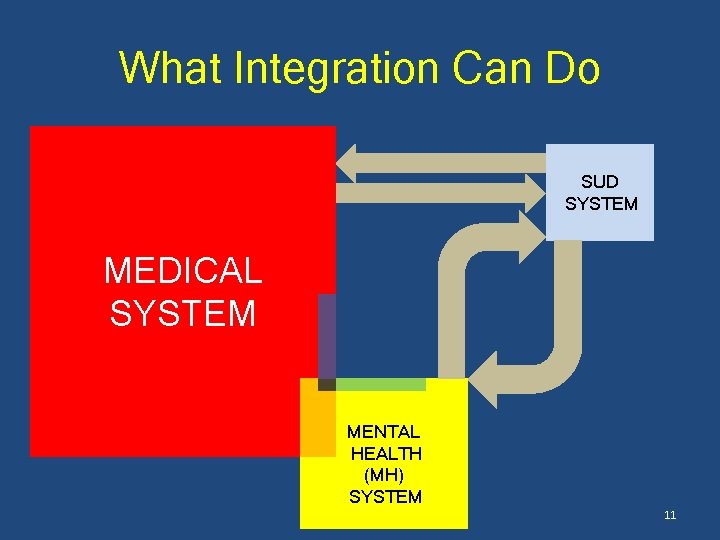
What Integration Can Do SUD SYSTEM MEDICAL SYSTEM MENTAL HEALTH (MH) SYSTEM 11
What Integration Can Do • Help create a “no wrong door” system that includes SUD services 12
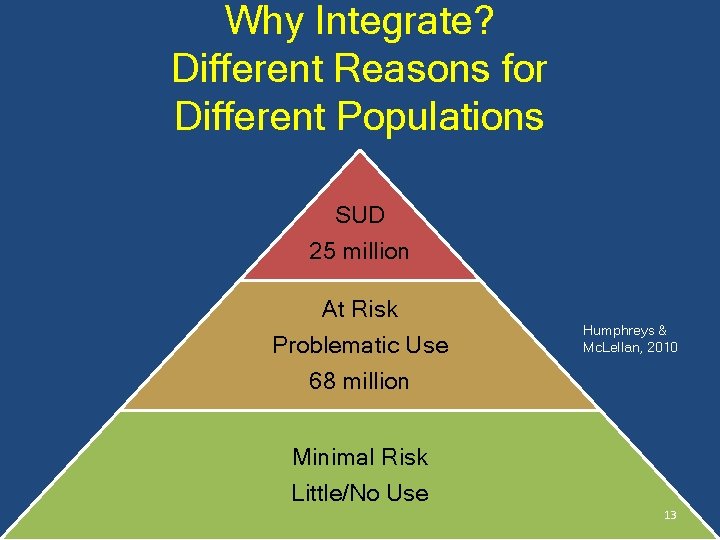
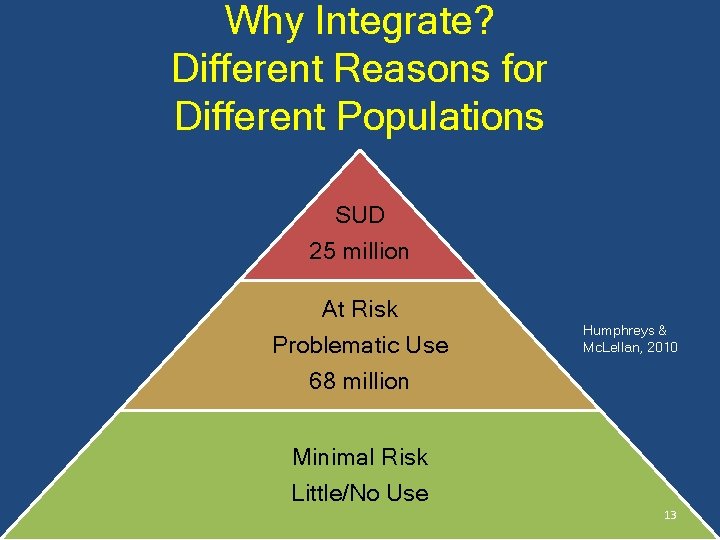
Why Integrate? Different Reasons for Different Populations SUD 25 million At Risk Problematic Use 68 million Humphreys & Mc. Lellan, 2010 Minimal Risk Little/No Use 13

SUD Integration for clients in treatment • Treat people, not disorders • Substance use is rarely the only problem • SUD clients have unmet MH needs • SUD clients have unmet medical needs 14
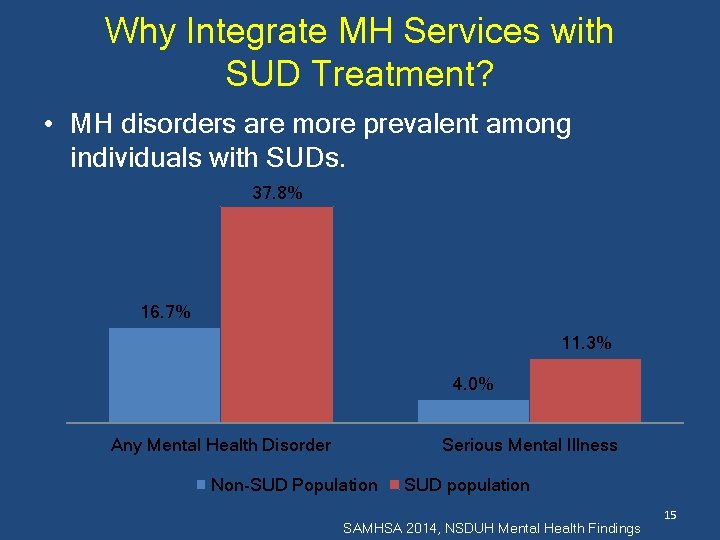
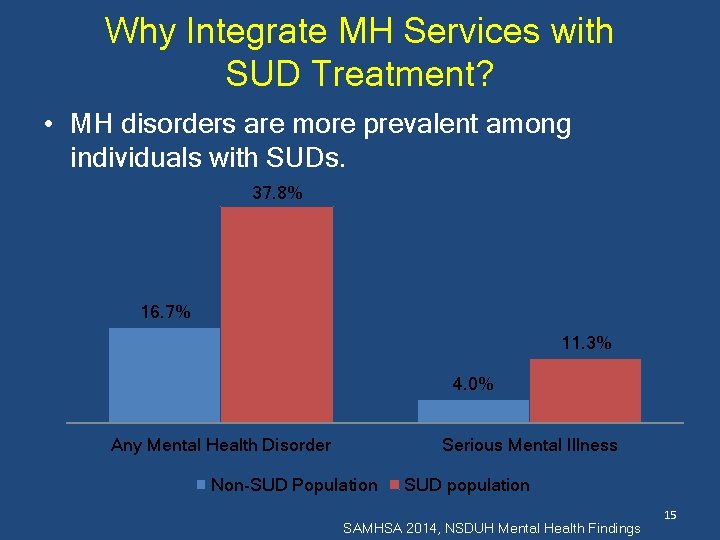
Why Integrate MH Services with SUD Treatment? • MH disorders are more prevalent among individuals with SUDs. 37. 8% 16. 7% 11. 3% 4. 0% Any Mental Health Disorder Serious Mental Illness Non-SUD Population SUD population SAMHSA 2014, NSDUH Mental Health Findings 15
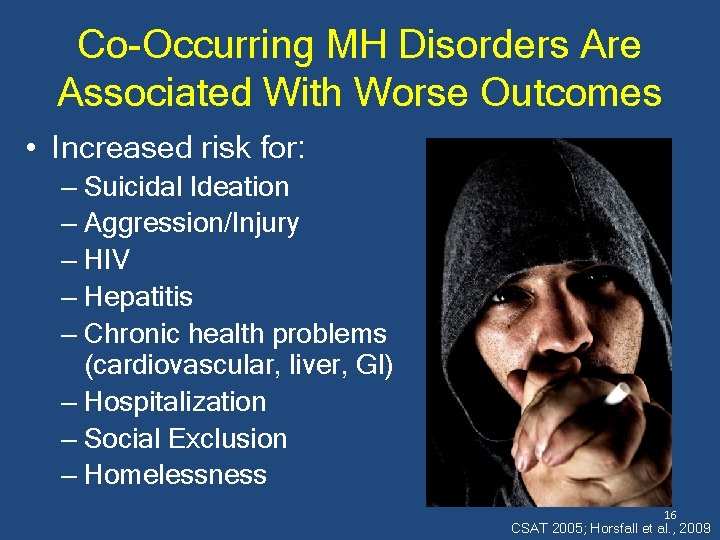
Co-Occurring MH Disorders Are Associated With Worse Outcomes • Increased risk for: – Suicidal Ideation – Aggression/Injury – HIV – Hepatitis – Chronic health problems (cardiovascular, liver, GI) – Hospitalization – Social Exclusion – Homelessness 16 CSAT 2005; Horsfall et al. , 2009
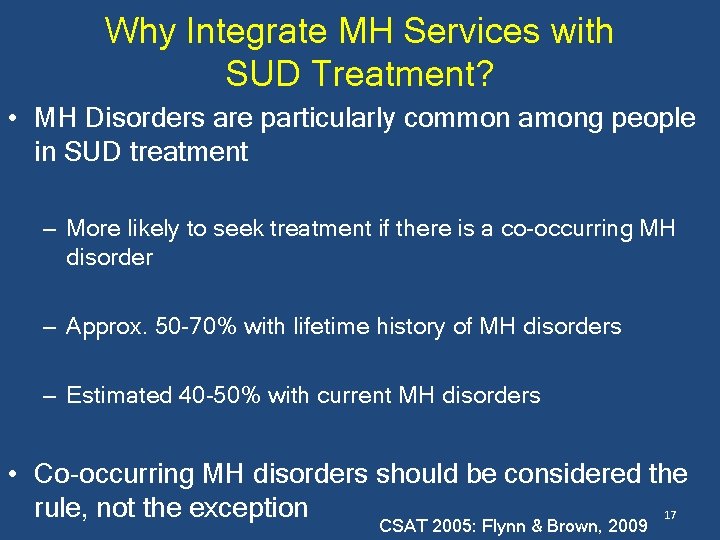
Why Integrate MH Services with SUD Treatment? • MH Disorders are particularly common among people in SUD treatment – More likely to seek treatment if there is a co-occurring MH disorder – Approx. 50 -70% with lifetime history of MH disorders – Estimated 40 -50% with current MH disorders • Co-occurring MH disorders should be considered the rule, not the exception 17 CSAT 2005: Flynn & Brown, 2009
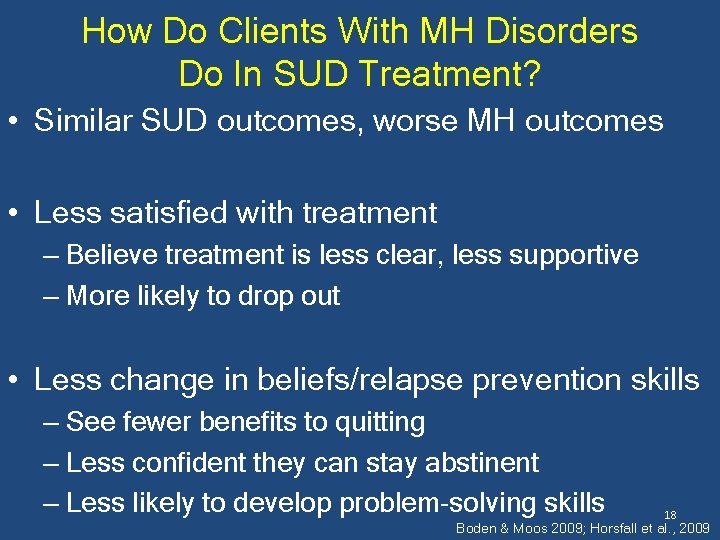
How Do Clients With MH Disorders Do In SUD Treatment? • Similar SUD outcomes, worse MH outcomes • Less satisfied with treatment – Believe treatment is less clear, less supportive – More likely to drop out • Less change in beliefs/relapse prevention skills – See fewer benefits to quitting – Less confident they can stay abstinent – Less likely to develop problem-solving skills 18 Boden & Moos 2009; Horsfall et al. , 2009
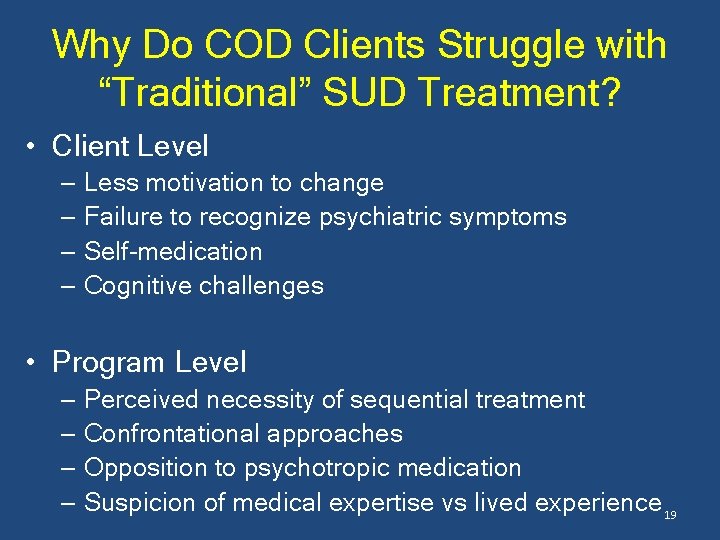
Why Do COD Clients Struggle with “Traditional” SUD Treatment? • Client Level – Less motivation to change – Failure to recognize psychiatric symptoms – Self-medication – Cognitive challenges • Program Level – Perceived necessity of sequential treatment – Confrontational approaches – Opposition to psychotropic medication – Suspicion of medical expertise vs lived experience 19
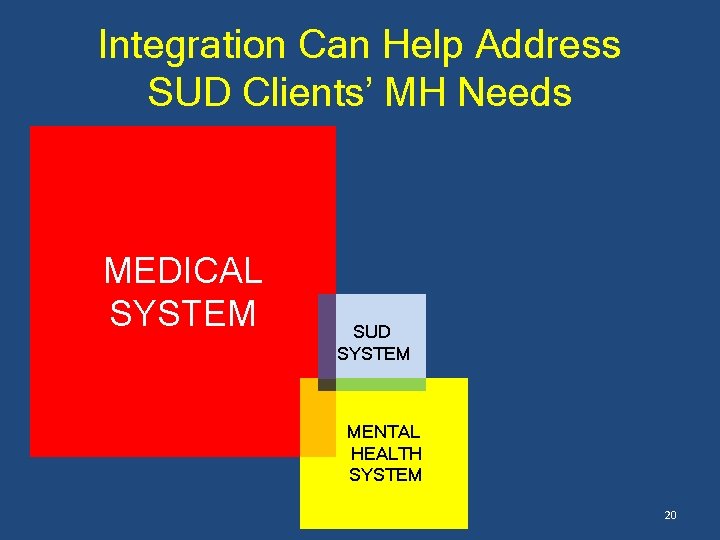
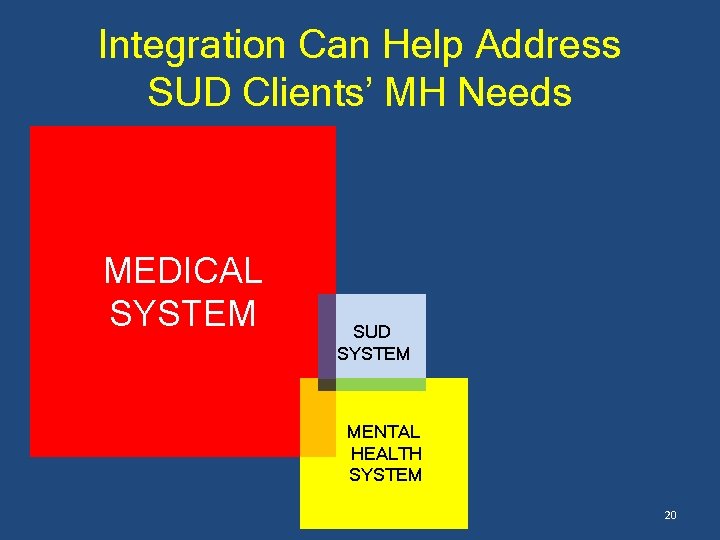
Integration Can Help Address SUD Clients’ MH Needs MEDICAL SYSTEM SUD SYSTEM MENTAL HEALTH SYSTEM 20
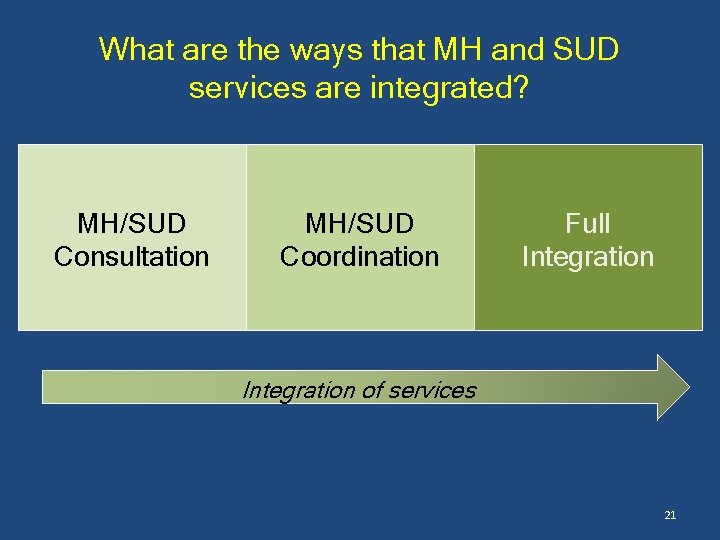
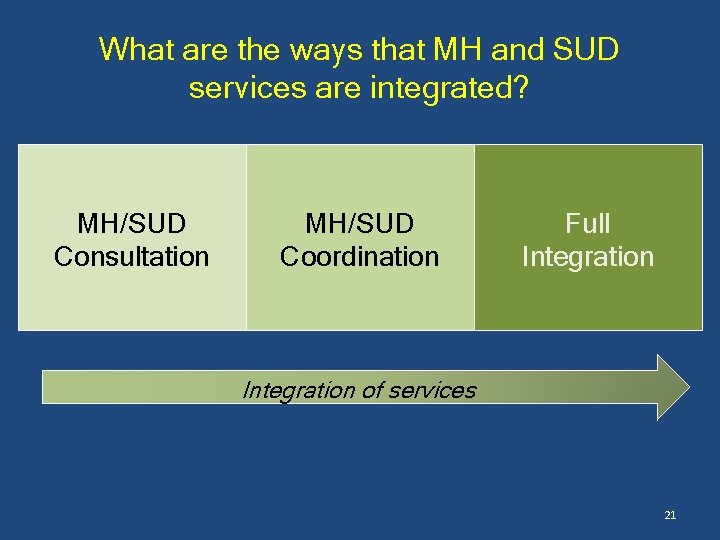
What are the ways that MH and SUD services are integrated? MH/SUD Consultation MH/SUD Coordination Full Integration of services 21
What are the ways that MH and SUD services are integrated? • Informal relationships between SUD and MH providers. MH/SUD Consultation • Referrals/linkages to providers of other specialty when necessary. • Consultation on client needs, engagement, prevention, and early intervention. 22
What are the ways that MH and SUD services are integrated? • Formalized relationships between SUD and MH providers MH/SUD Coordination • Specialty MH and SUD providers will discuss specific clients. • More clinically integrated, with providers working as a team. 23
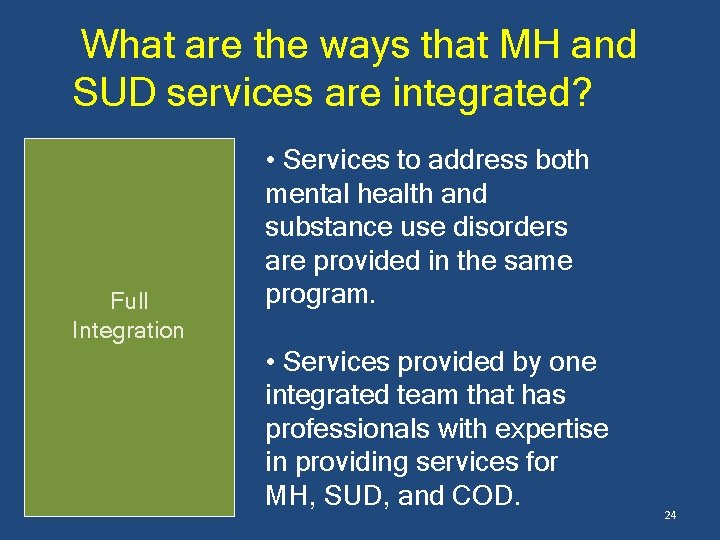
What are the ways that MH and SUD services are integrated? Full Integration • Services to address both mental health and substance use disorders are provided in the same program. • Services provided by one integrated team that has professionals with expertise in providing services for MH, SUD, and COD. 24
What Integrating MH and SUD Services Can Do • Benefits of integration – Improve access to MH services – Make interventions more focused on client needs – Transfer burden of care coordination from the client to the system • Treatment that addresses both MH and SUD at the same time associated with less crises (arrests, hospitalization) • There is not clear evidence of which integration model leads to the best outcomes 25 Mangrum 2006; Drake et al. , 2008; Sterling et al. , 2011
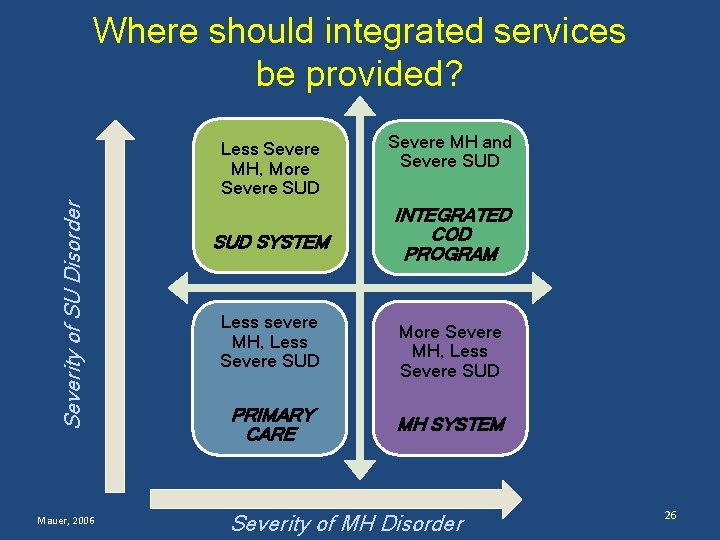
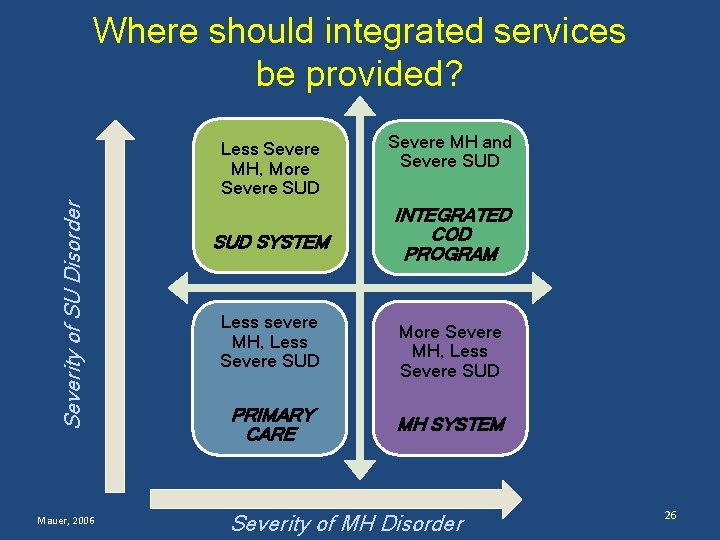
Where should integrated services be provided? Severity of SU Disorder Less Severe MH, More Severe SUD Mauer, 2006 SUD SYSTEM Less severe MH, Less Severe SUD PRIMARY CARE Severe MH and Severe SUD INTEGRATED COD PROGRAM More Severe MH, Less Severe SUD MH SYSTEM Severity of MH Disorder 26
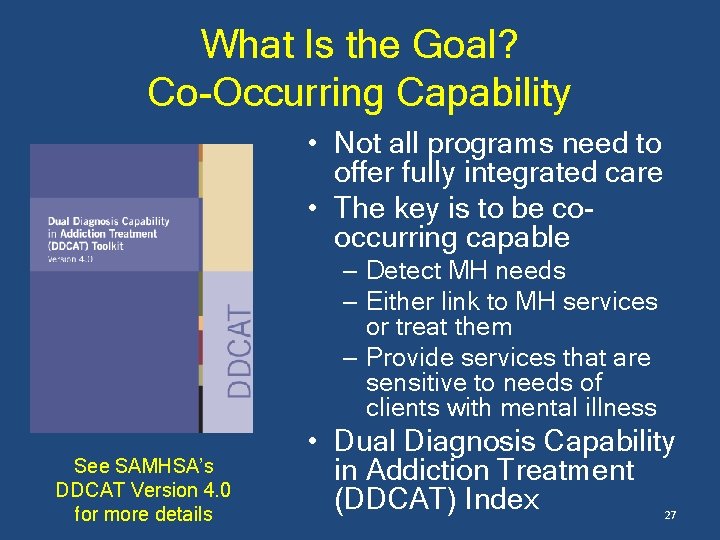
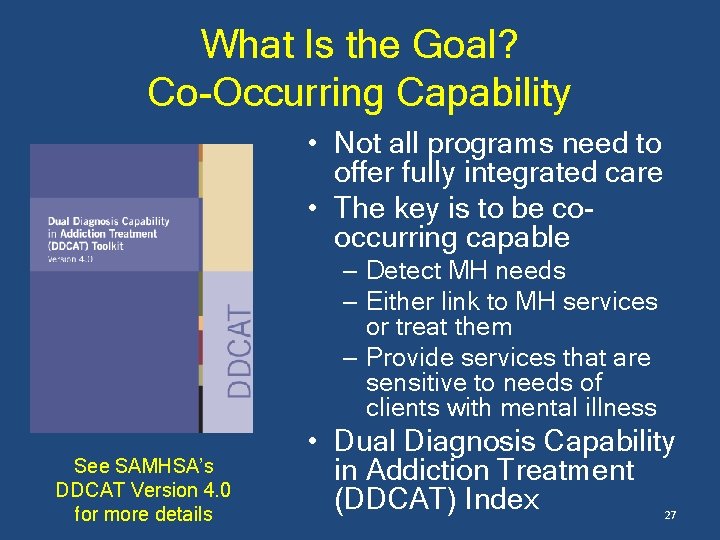
What Is the Goal? Co-Occurring Capability • Not all programs need to offer fully integrated care • The key is to be cooccurring capable – Detect MH needs – Either link to MH services or treat them – Provide services that are sensitive to needs of clients with mental illness See SAMHSA’s DDCAT Version 4. 0 for more details • Dual Diagnosis Capability in Addiction Treatment (DDCAT) Index 27

Co-Occurring Capable Treatment Tools • Diagnostic Services • Medications • Psychoeducation • Motivational Interviewing • Contingency Management • Cognitive Behavioral Therapy Techniques • Relapse Prevention Strategies See the Center for Substance Abuse Treatment’s TIP 42 for more details. 28
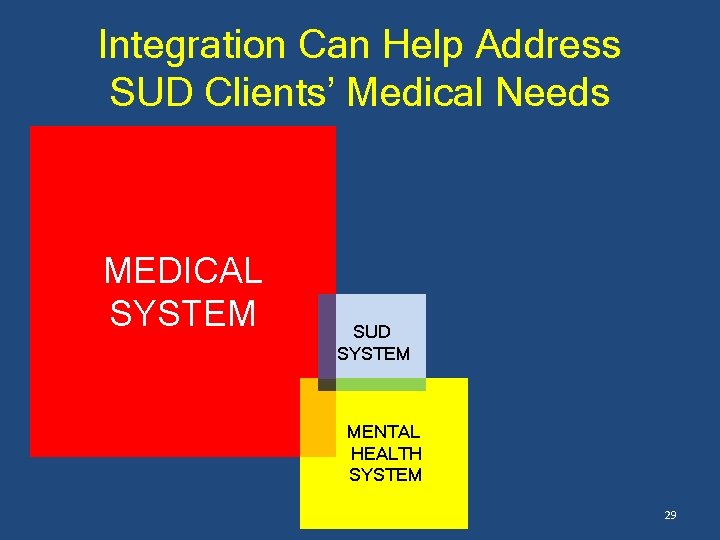
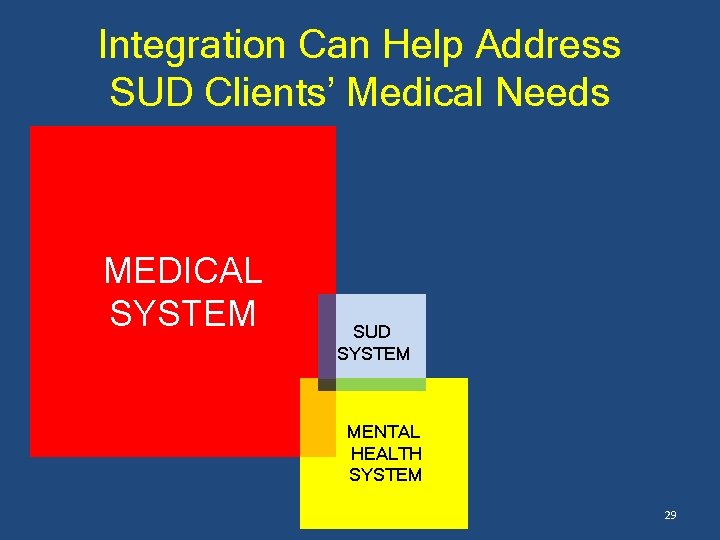
Integration Can Help Address SUD Clients’ Medical Needs MEDICAL SYSTEM SUD SYSTEM MENTAL HEALTH SYSTEM 29
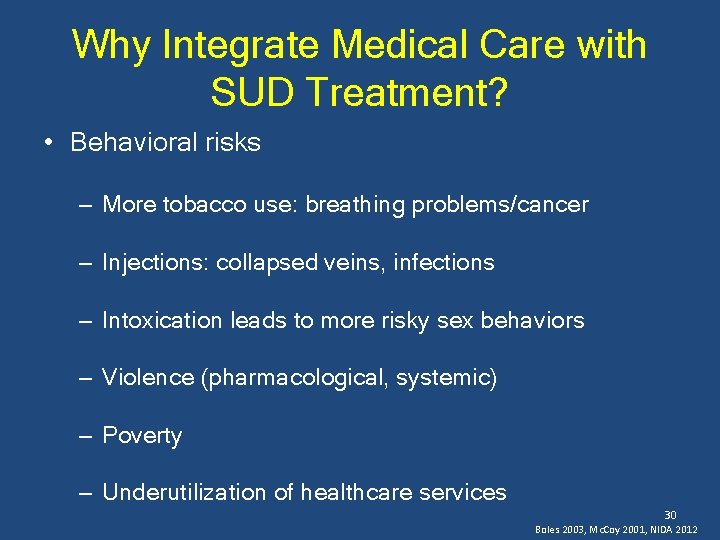
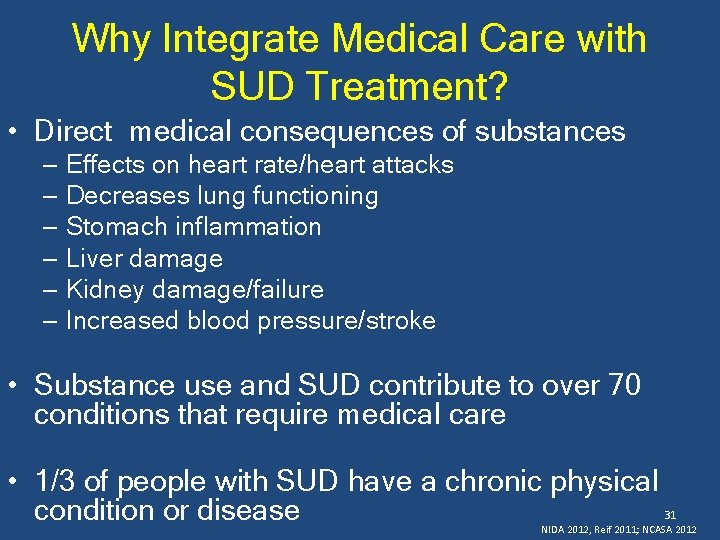
Why Integrate Medical Care with SUD Treatment? • Behavioral risks – More tobacco use: breathing problems/cancer – Injections: collapsed veins, infections – Intoxication leads to more risky sex behaviors – Violence (pharmacological, systemic) – Poverty – Underutilization of healthcare services 30 Boles 2003, Mc. Coy 2001, NIDA 2012
Why Integrate Medical Care with SUD Treatment? • Direct medical consequences of substances – Effects on heart rate/heart attacks – Decreases lung functioning – Stomach inflammation – Liver damage – Kidney damage/failure – Increased blood pressure/stroke • Substance use and SUD contribute to over 70 conditions that require medical care • 1/3 of people with SUD have a chronic physical condition or disease 31 NIDA 2012, Reif 2011; NCASA 2012
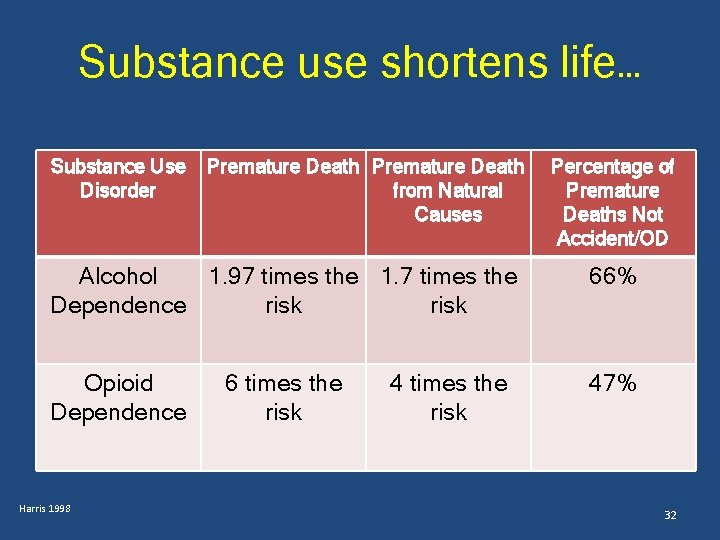
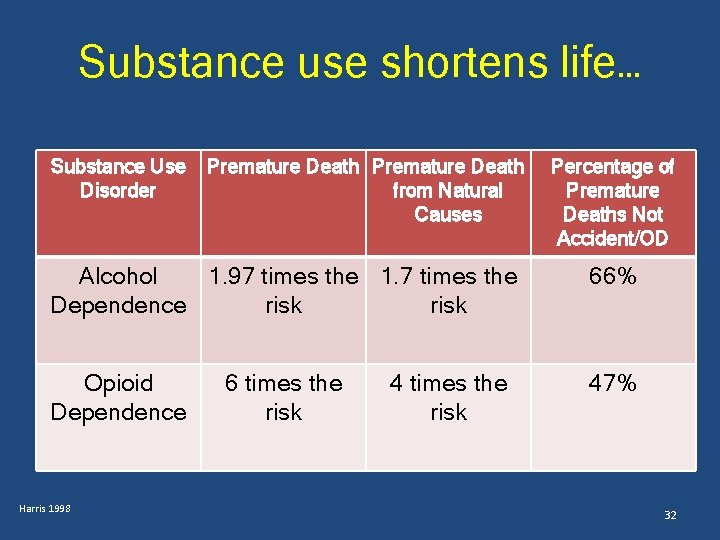
Substance use shortens life… Substance Use Disorder Premature Death from Natural Causes Percentage of Premature Deaths Not Accident/OD Alcohol 1. 97 times the 1. 7 times the Dependence risk 66% Opioid Dependence 47% Harris 1998 6 times the risk 4 times the risk 32
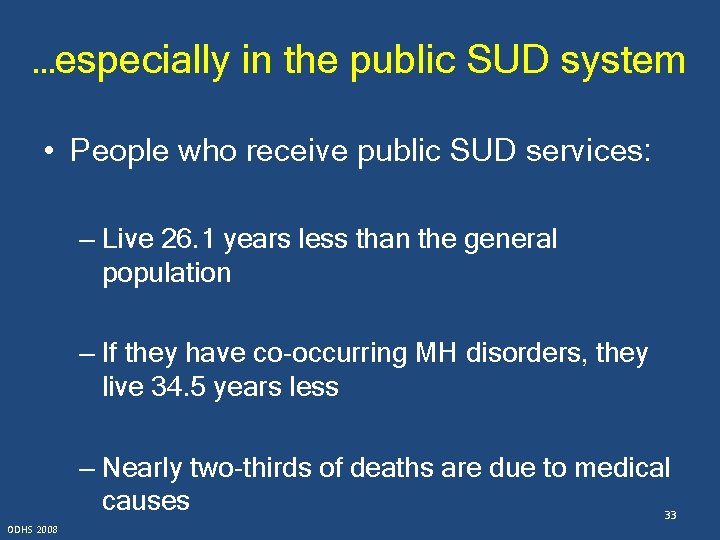
…especially in the public SUD system • People who receive public SUD services: – Live 26. 1 years less than the general population – If they have co-occurring MH disorders, they live 34. 5 years less – Nearly two-thirds of deaths are due to medical causes 33 ODHS 2008
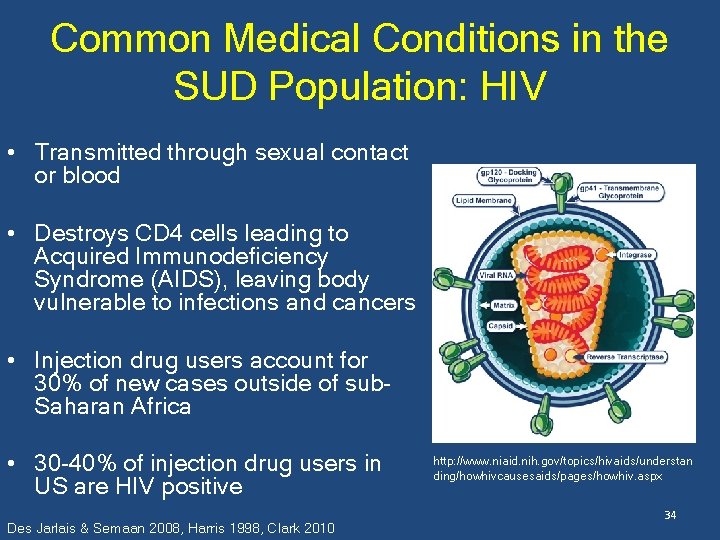
Common Medical Conditions in the SUD Population: HIV • Transmitted through sexual contact or blood • Destroys CD 4 cells leading to Acquired Immunodeficiency Syndrome (AIDS), leaving body vulnerable to infections and cancers • Injection drug users account for 30% of new cases outside of sub. Saharan Africa • 30 -40% of injection drug users in US are HIV positive Des Jarlais & Semaan 2008, Harris 1998, Clark 2010 http: //www. niaid. nih. gov/topics/hivaids/understan ding/howhivcausesaids/pages/howhiv. aspx 34
Common Medical Conditions in the SUD Population: Hepatitis C • Virus that leads to liver inflammation • 60%-85% of cases lead to chronic infection, leading to increased risk of cirrhosis. • High risk of transmission through injection drug use or needle sharing • Most common infectious disease among injection drug users (60 -90%) https: //nccih. nih. gov/health/hepatiti sc/hepatitiscfacts. htm • Injection drug users are largest group infected with Hepatitis C in the US 35 Edlin 2002, Clark 2010
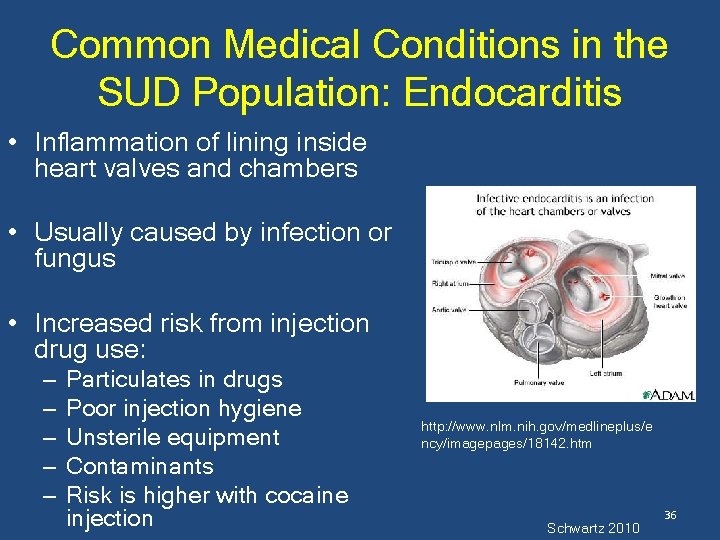
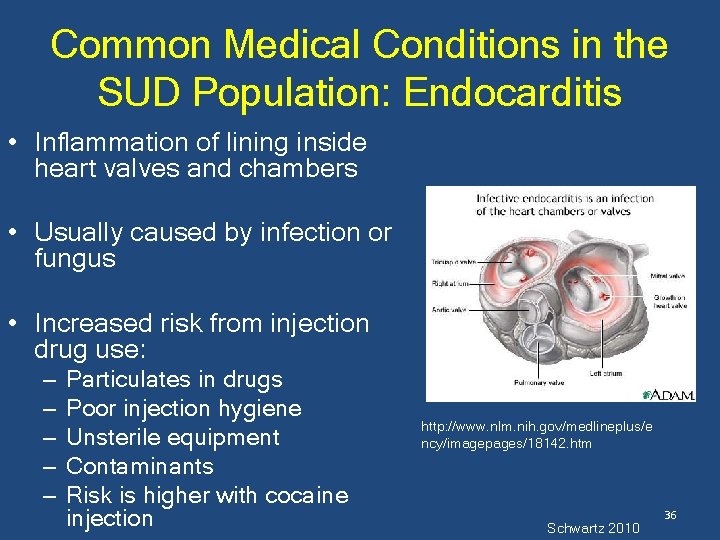
Common Medical Conditions in the SUD Population: Endocarditis • Inflammation of lining inside heart valves and chambers • Usually caused by infection or fungus • Increased risk from injection drug use: – – – Particulates in drugs Poor injection hygiene Unsterile equipment Contaminants Risk is higher with cocaine injection http: //www. nlm. nih. gov/medlineplus/e ncy/imagepages/18142. htm Schwartz 2010 36
Common Medical Conditions in the SUD Population: Lung Disease • Damaged airways and sacs in lungs, causing breathing difficulty • Inhalation of stimulants can cause buildups in lungs • Emphysema associated with IV drug use • Association with tobacco use http: //nihseniorhealth. gov/copd/wh atiscopd/01. html • Asthma twice as prevalent among individuals with SUD 37 Wesselius 1997, Mertens 2003
Common Medical Conditions in the SUD Population: Hypertension • High blood pressure increases risk of stroke, heart attack, brain damage, vision loss • Three drinks per day increases risk • Caused by stimulants • Twice as prevalent in SUD population https: //www. nlm. nih. gov/medlineplus/highblo odpressure. html 38 Sesso 2008, Mac. Mahon 2010, Mertens 2003
Common Medical Conditions in the SUD Population: Type 2 Diabetes • Prevents cells from receiving sugar, leading to buildup in blood • Can lead to blindness, heart disease, stroke, kidney failure, amputation • Binge drinking increases risk • Substance use associated with earlier age of onset • Alcohol worsens diabetes health outcomes 39 Pietraszek 2010, Johnson 2001, Emanuele 1998
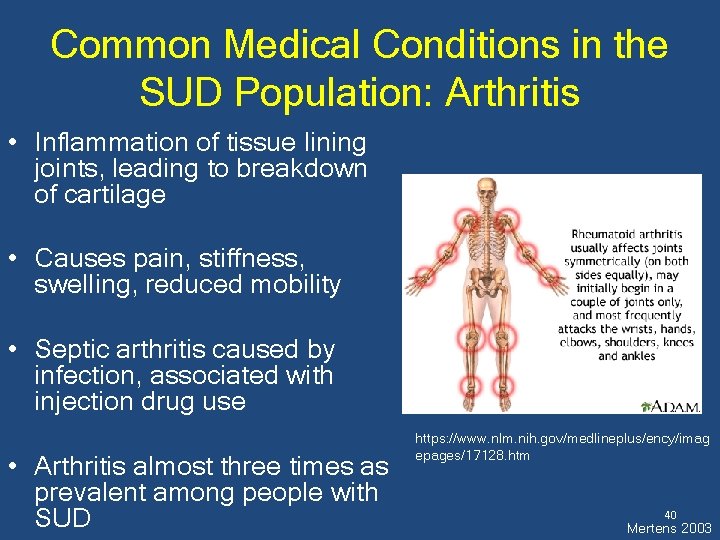
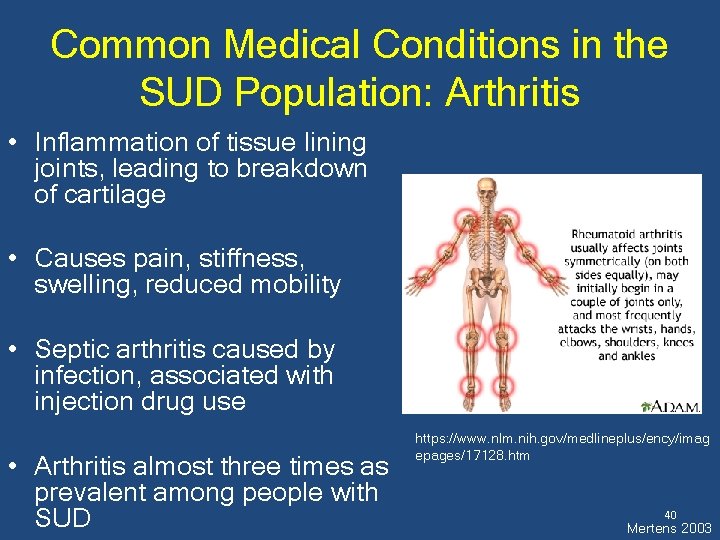
Common Medical Conditions in the SUD Population: Arthritis • Inflammation of tissue lining joints, leading to breakdown of cartilage • Causes pain, stiffness, swelling, reduced mobility • Septic arthritis caused by infection, associated with injection drug use • Arthritis almost three times as prevalent among people with SUD https: //www. nlm. nih. gov/medlineplus/ency/imag epages/17128. htm 40 Mertens 2003
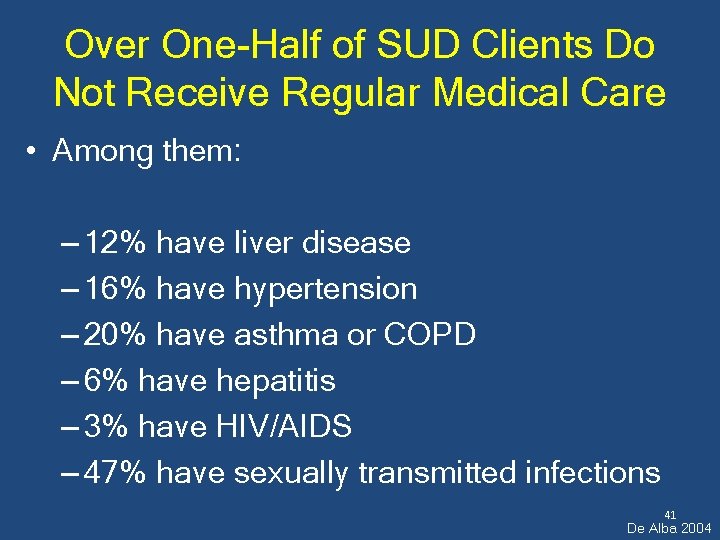
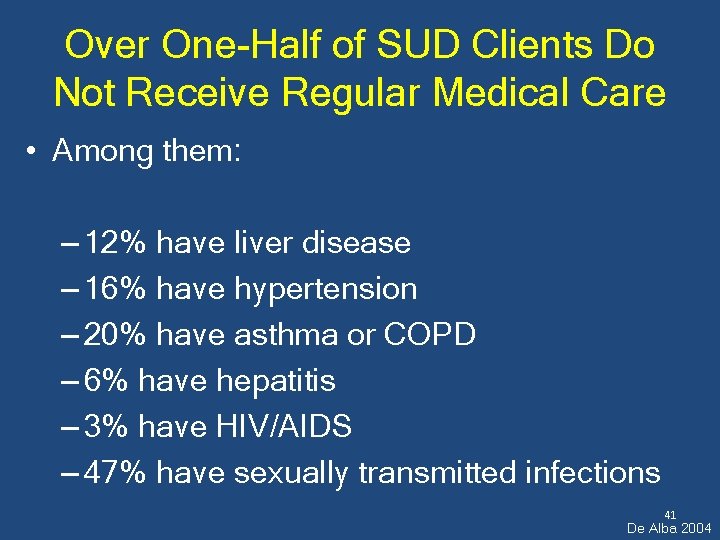
Over One-Half of SUD Clients Do Not Receive Regular Medical Care • Among them: – 12% have liver disease – 16% have hypertension – 20% have asthma or COPD – 6% have hepatitis – 3% have HIV/AIDS – 47% have sexually transmitted infections 41 De Alba 2004

Integration with medical services improves clients’ health… • Decreases hospitalization rates • Decreases number of inpatient days • Decreases ED visits • Increases adherence to HIV antiretroviral therapy • Can cut total medical costs in half Parthasarathy 2003, Weisner 2001, Parry 2007 42
…and it makes treatment more effective!!!! • Primary care reduces drinking and drug use by people with SUD • 2 -10 primary care visits/year triples chances of SUD remission after five years • Integrated SUD/medical services reduces SUD severity after 12 months; off-site referral does not Saitz et al 2005, Friedmann 2003, Mertens 2008 43
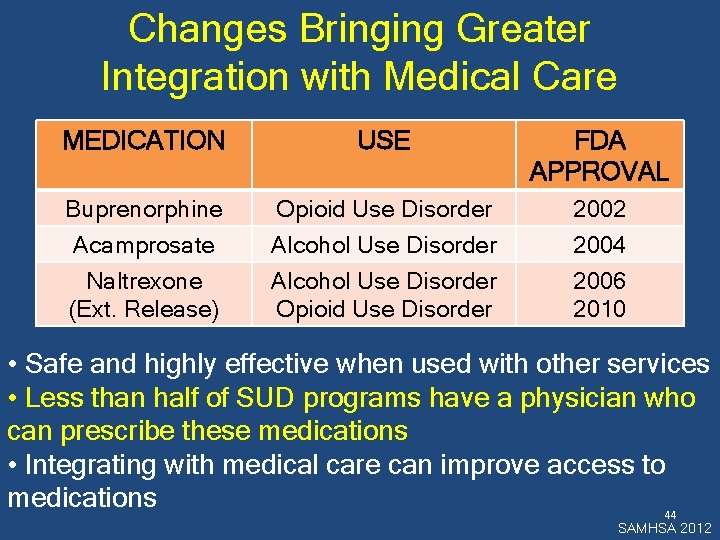
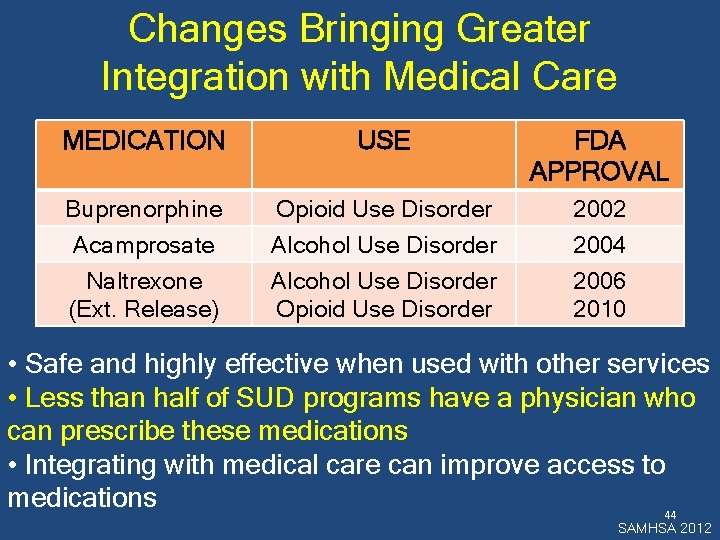
Changes Bringing Greater Integration with Medical Care MEDICATION USE FDA APPROVAL Buprenorphine Opioid Use Disorder 2002 Acamprosate Naltrexone (Ext. Release) Alcohol Use Disorder Opioid Use Disorder 2004 2006 2010 • Safe and highly effective when used with other services • Less than half of SUD programs have a physician who can prescribe these medications • Integrating with medical care can improve access to medications 44 SAMHSA 2012
Changes Bringing Greater Integration with Medical Care • Newly insured population expected to have high levels of SUD need • SUD services among essential benefits under the ACA • Insurance reimbursement will lead to greater links with primary care (like other specialties) 45
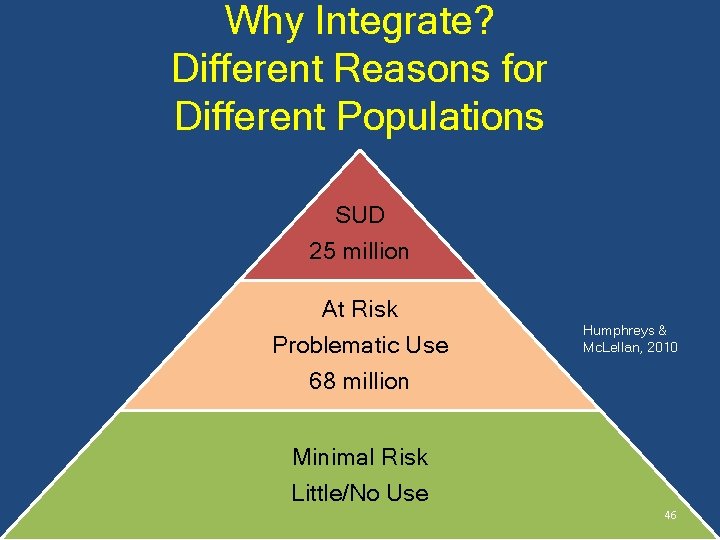
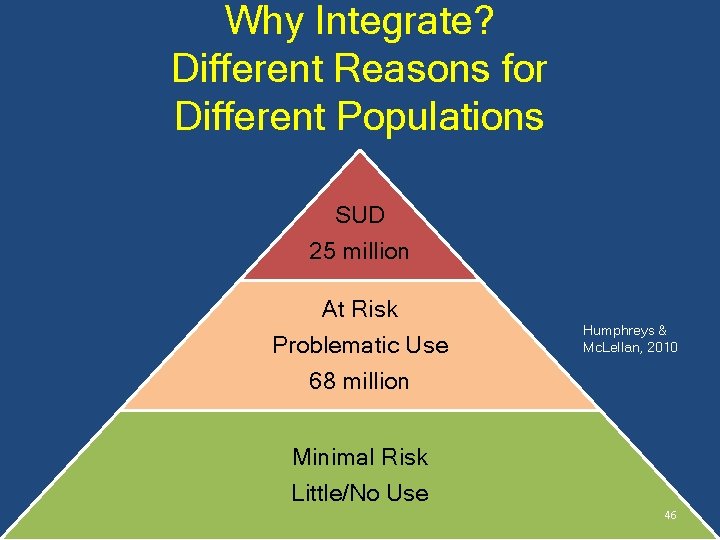
Why Integrate? Different Reasons for Different Populations SUD 25 million At Risk Problematic Use 68 million Humphreys & Mc. Lellan, 2010 Minimal Risk Little/No Use 46
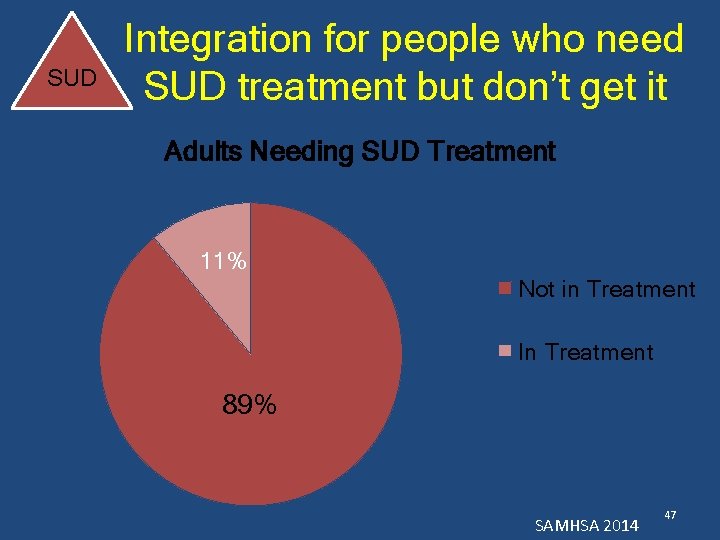
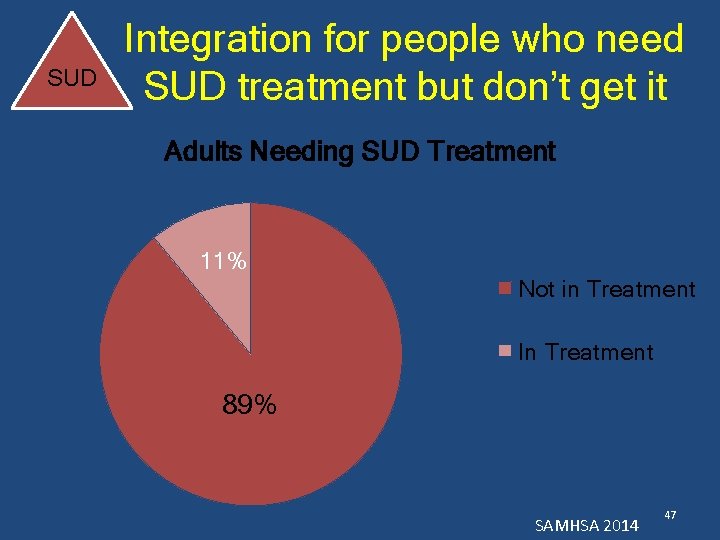
SUD Integration for people who need SUD treatment but don’t get it Adults Needing SUD Treatment 11% Not in Treatment In Treatment 89% SAMHSA 2014 47
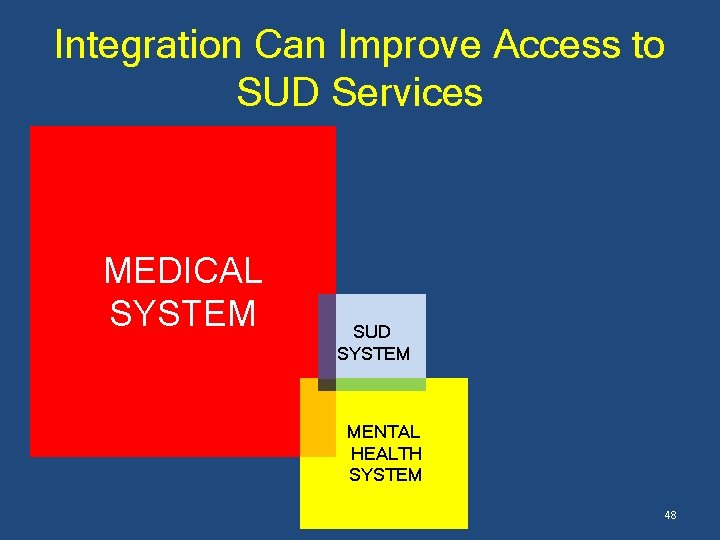
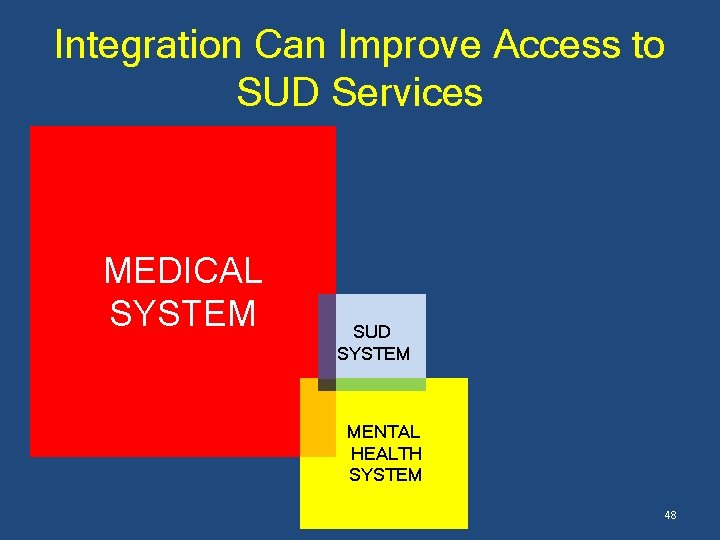
Integration Can Improve Access to SUD Services MEDICAL SYSTEM SUD SYSTEM MENTAL HEALTH SYSTEM 48
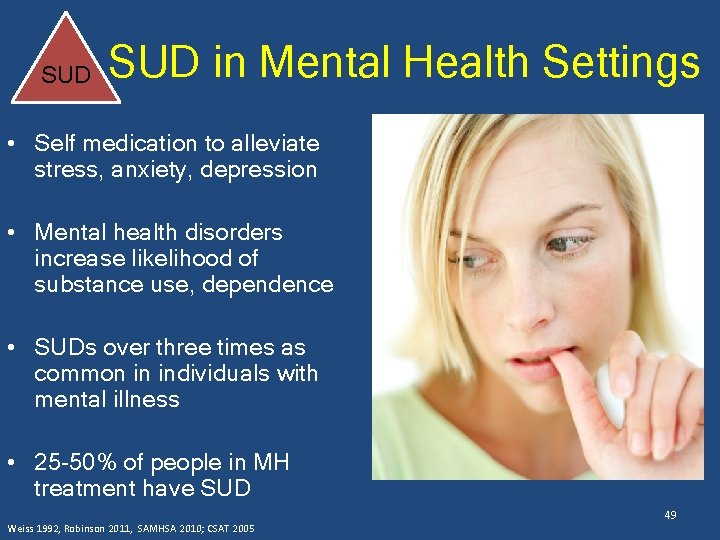
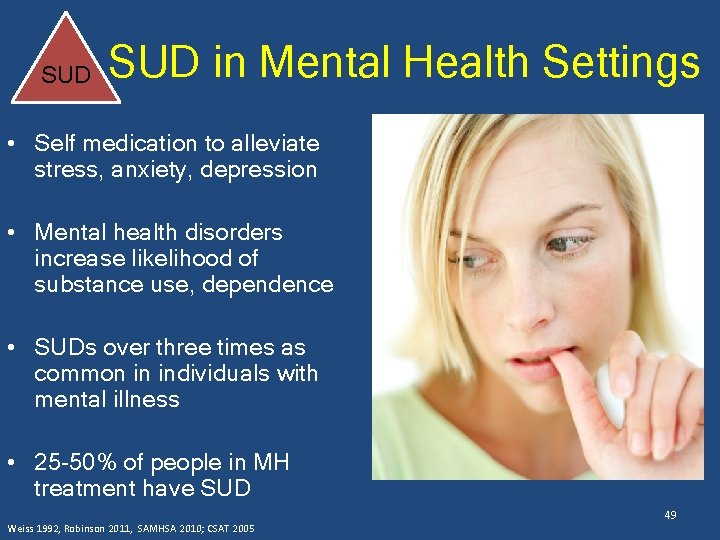
SUD in Mental Health Settings • Self medication to alleviate stress, anxiety, depression • Mental health disorders increase likelihood of substance use, dependence • SUDs over three times as common in individuals with mental illness • 25 -50% of people in MH treatment have SUD Weiss 1992, Robinson 2011, SAMHSA 2010; CSAT 2005 49
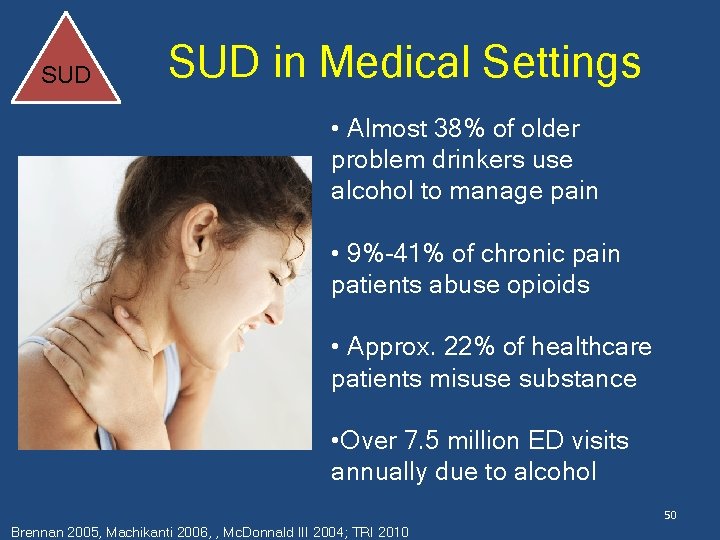
SUD in Medical Settings • Almost 38% of older problem drinkers use alcohol to manage pain • 9%-41% of chronic pain patients abuse opioids • Approx. 22% of healthcare patients misuse substance • Over 7. 5 million ED visits annually due to alcohol 50 Brennan 2005, Machikanti 2006, , Mc. Donnald III 2004; TRI 2010

At Risk Problematic Use Integration for people who don’t need treatment…yet • Excessive drinking and drug use cause changes in brain that can lead to SUD • Use mental health and medical visits as a “teachable moment” to facilitate behavior change – Educate about risks associated with substance use, including SUD – Briefly use motivational interviewing and cognitive behavior techniques Mc. Lellan 2000, Madras 2009 51

At Risk Problematic Use Integration for people who don’t need treatment…yet Screening Brief Intervention Referral to Treatment Madras 2009; Saitz 2015 • Pre-post studies have shown reductions in alcohol/drug use • More rigorous trials showed effect for risky drinking, but not heavy drinking or drug use • Major Challenges: • How “brief” can “brief interventions” be? • How to make the “RT” work 52

At Risk Problematic Use Integration for people who don’t need treatment…yet Screening Brief Intervention Referral to Treatment • SBIRT is feasible and potentially beneficial in places outside of the medical system • Largest potential benefit in places where there at-risk populations or high levels of substance use • Schools and Universities • Juvenile Justice • Jails 53 • Social Services
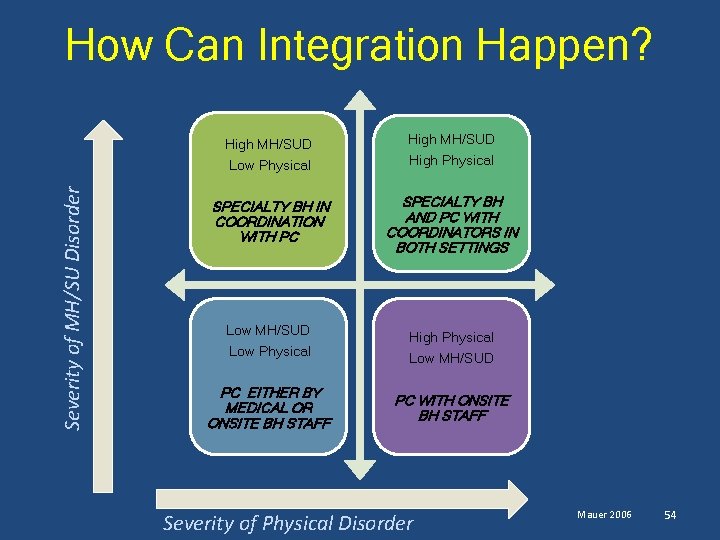
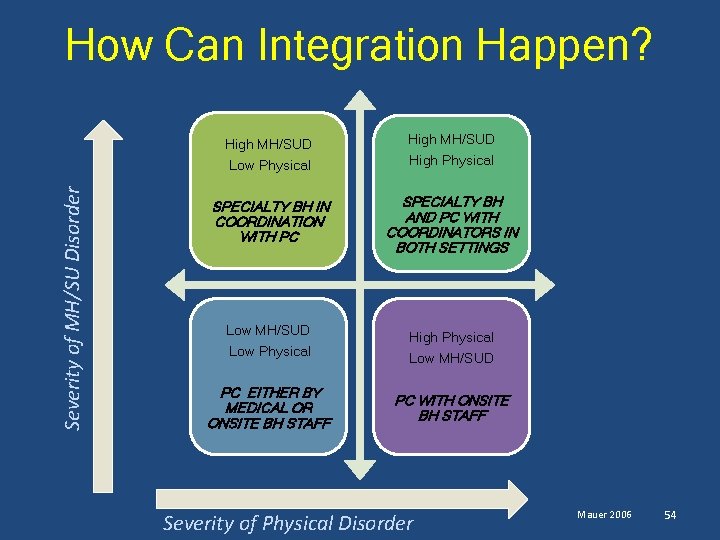
Severity of MH/SU Disorder How Can Integration Happen? High MH/SUD Low Physical High MH/SUD High Physical SPECIALTY BH IN COORDINATION WITH PC SPECIALTY BH AND PC WITH COORDINATORS IN BOTH SETTINGS Low MH/SUD Low Physical PC EITHER BY MEDICAL OR ONSITE BH STAFF High Physical Low MH/SUD PC WITH ONSITE BH STAFF Severity of Physical Disorder Mauer 2006 54
What Does High MH/SUD, High Primary Care Look Like? • There have been early adopters across the country – Been developing integrated care for a long time – Have a lot of resources • For details see: – Treatment Research Institute “Forum on Integration” (2010) – SAMHSA “Innovations in Addiction Treatment: Addiction Treatment Providers Working With Integrated Primary Care Services (2012) 55
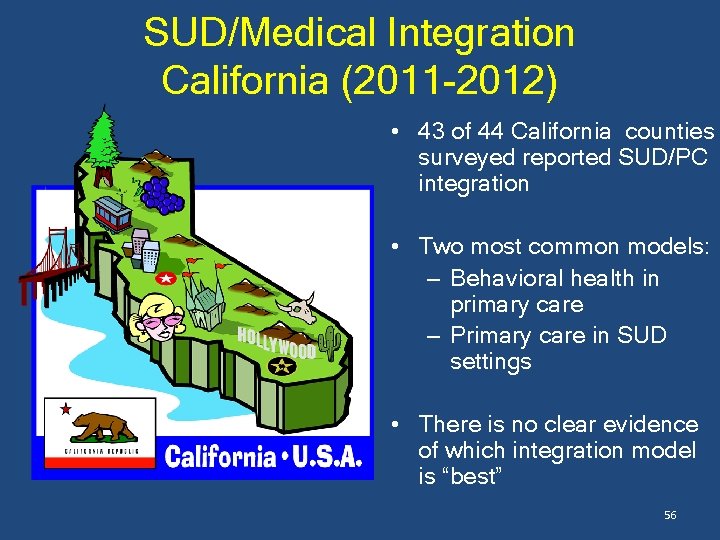
SUD/Medical Integration California (2011 -2012) • 43 of 44 California counties surveyed reported SUD/PC integration • Two most common models: – Behavioral health in primary care – Primary care in SUD settings • There is no clear evidence of which integration model is “best” 56
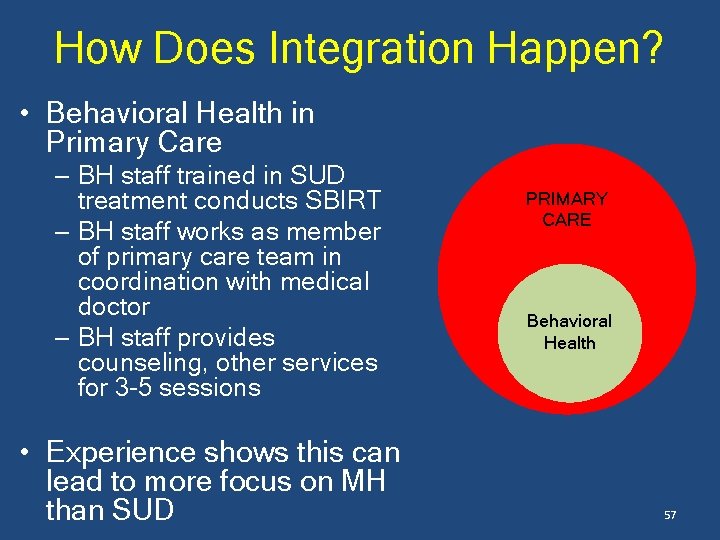
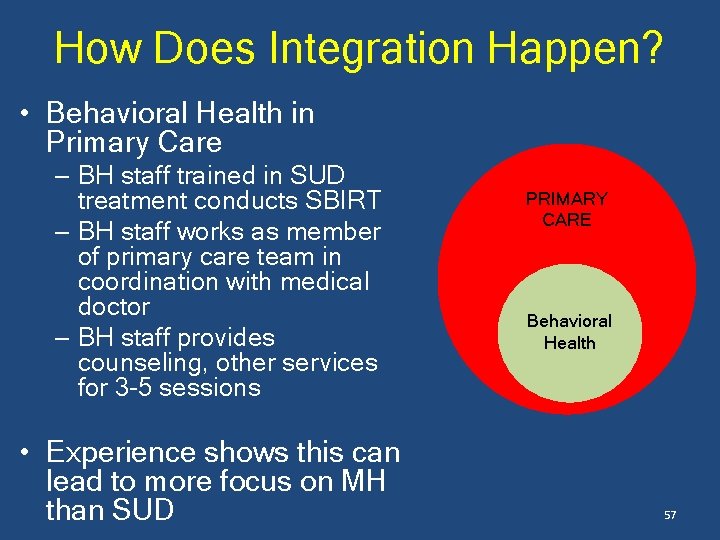
How Does Integration Happen? • Behavioral Health in Primary Care – BH staff trained in SUD treatment conducts SBIRT – BH staff works as member of primary care team in coordination with medical doctor – BH staff provides counseling, other services for 3 -5 sessions • Experience shows this can lead to more focus on MH than SUD PRIMARY CARE Behavioral Health 57
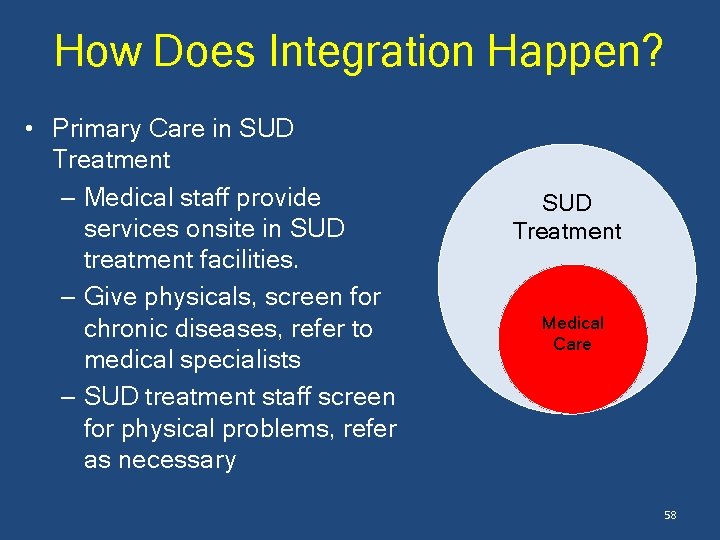
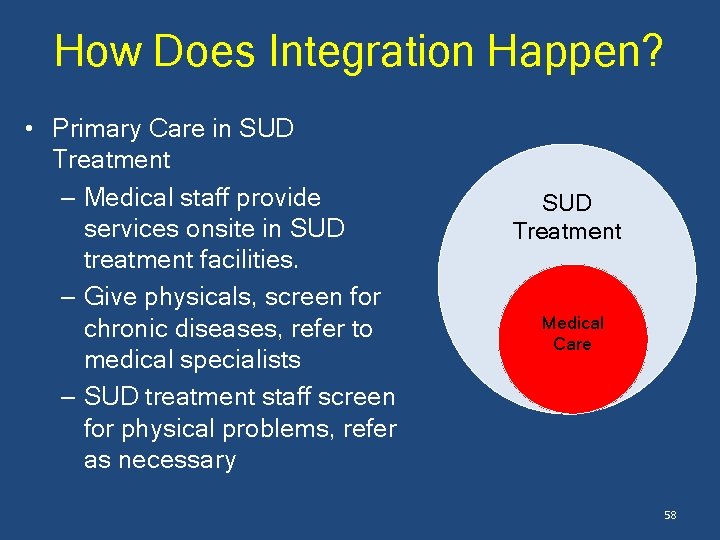
How Does Integration Happen? • Primary Care in SUD Treatment – Medical staff provide services onsite in SUD treatment facilities. – Give physicals, screen for chronic diseases, refer to medical specialists – SUD treatment staff screen for physical problems, refer as necessary SUD Treatment Medical Care 58
Integrating Isn’t Always Easy “Integrated…care is like a pomegranate: overwhelmingly people say they like it, but few buy it. ” Cummings, 2009 59
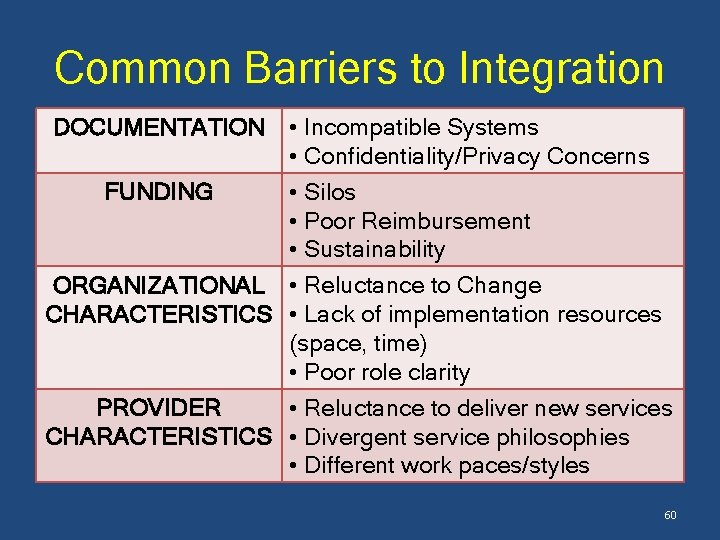
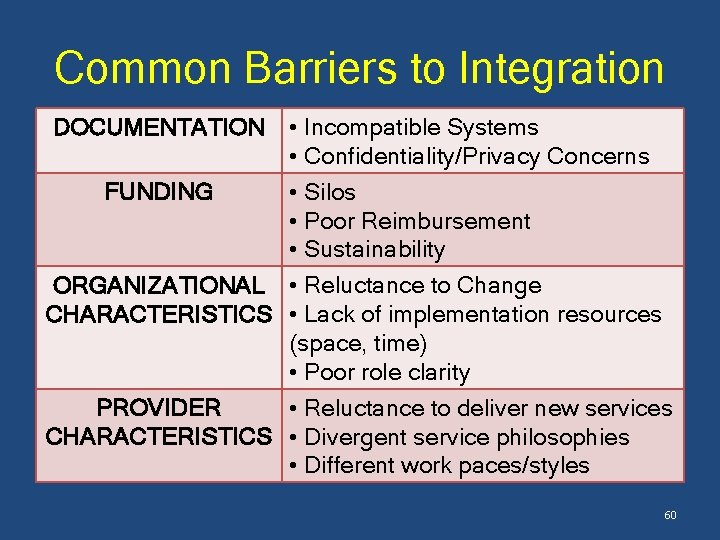
Common Barriers to Integration • Incompatible Systems • Confidentiality/Privacy Concerns FUNDING • Silos • Poor Reimbursement • Sustainability ORGANIZATIONAL • Reluctance to Change CHARACTERISTICS • Lack of implementation resources (space, time) • Poor role clarity PROVIDER • Reluctance to deliver new services CHARACTERISTICS • Divergent service philosophies • Different work paces/styles DOCUMENTATION 60
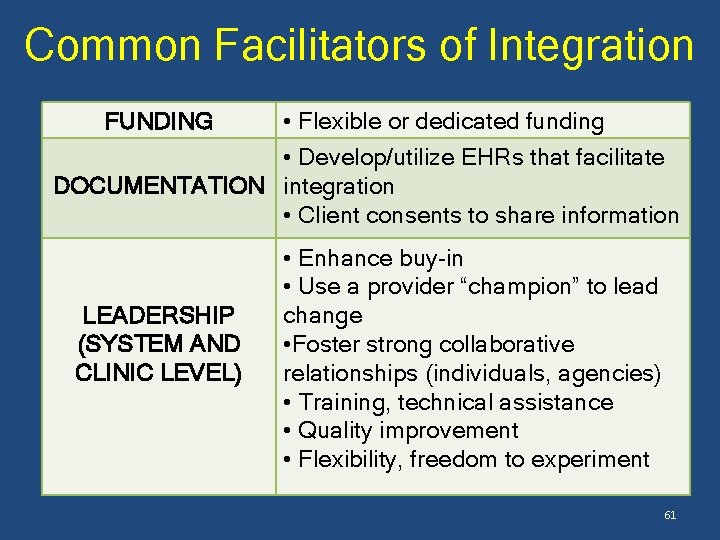
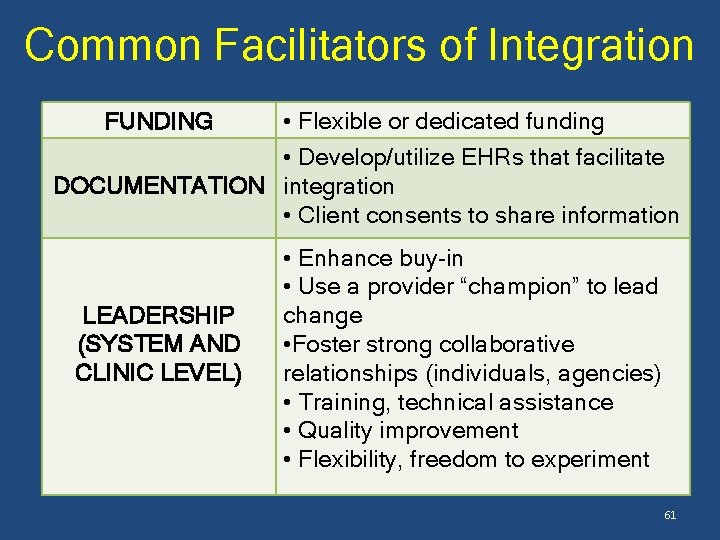
Common Facilitators of Integration • Flexible or dedicated funding • Develop/utilize EHRs that facilitate DOCUMENTATION integration • Client consents to share information FUNDING LEADERSHIP (SYSTEM AND CLINIC LEVEL) • Enhance buy-in • Use a provider “champion” to lead change • Foster strong collaborative relationships (individuals, agencies) • Training, technical assistance • Quality improvement • Flexibility, freedom to experiment 61
Take Away Points • SUD services are being integrated into the mainstream of the US health care system • Integration with mental health and medical services can help: – Better address whole-person needs of clients in treatment – Facilitate access to most modern, evidencebased approaches to SUD care – Close the SUD treatment gap 62
Take Away Points • SUD integration can/should be not only with medical services, but other places where there are likely to be high levels of risk or need • The benefits of integration are clear, but some questions remain: – How can integrated services be enhanced to have maximum benefit ? • Funding and leadership that support service integration can help overcome barriers to implementation 63
QUESTIONS? 64
WORKS CITED • • • Boden, M. T. , & Moos, R. (2009). Dually diagnosed patients' responses to substance use disorder treatment. Journal of Substance Abuse Treatment, 37(4), 335 -345. Boles SM, Miotto K. 2003. Substance abuse and violence: a review of the literature. Aggression and Violent Behavior. 8(2): 155 -174 Brennan PL, Schutte KK, Moos RH. 2005. Pain and use of alcohol to manage pain: prevalence and 3 -year outcmes among older problem and non-problem drinkers. Addiction. 100(6): 777 -786. Center for Substance Abuse Treatment, Substance Abuse Treatment for Persons with Co-Occurring Disorders. Treatment Improvement Protocol (TIP) Series 42. DHHS Publication No. (SMA) 05 -3922. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2005. Clark RE, O’Connell E, Samnaliev M. 2010. Substacne Abuse and Healthcare Costs. Knowledge Asset web site created by the Robert Wood Johnson Foundation’s Substance Abuse Policy Research Program; March 2010. http: //saprp. org/knowledgeassets/knowledge_detail. cfm? KAID=21 Cummings NA, O’Donohue WT, Cummings JL. 2009. The Financial Dimension of Integrated Behavioral/Primary Care. Journal of Clinical Psychology in Medical Settings 16: 31 -34. De Alba I, Samet JH, Saitz R. Burden of Medical Illness in Drug- and Alcohol –dependent Persons Without Primary Care. American Journal on Addictions. 13: 33 -45. Des Jarlais DC, Semaan S. HIV Prevention for Injecting Drug Users: The First 25 Years and Counting. Psychosomatic Medicine. 70(5): 606 -6111 Drake RE, O’Neal EL, Wallach MA. 2008. A systematic review of psychosocial research on psychosocial interventions for people with co-occurring severe mental and substance use disorders. Journal of Substance Abuse Treatment 34(1): 123 -138 Edlin BR. 2002. Prevention and treatment of hepatitis C in injection drug users. Hepatology 36(S 1): S 210 S 219. Emanuele NV, Swade TF, Emanuele MA. 1998. Consequences of Alcohol Use in Diabetics. Alcohol Health 65 and Research World. 22(3): 211 -219.
WORKS CITED • • • • Flynn PM & Brown BS. 2009. Co-Occurring Disorders in Substance Abuse Treatment: Issues and Prospects. Journal of Substance Abuse Treatment. 34(1): 36 -47 Friedmann PD, Zhang Z, Hendrickson J, et al. 2003. Effect of Primary Medical Care on Addiction and Medical Severity in Substance Abuse Treatment Programs. Journal of General Internal Medicine. 18(1): 1 -8. Harris EC, Barraclough B. 1998, Excess mortality of mental disorder. British Journal of Psychiatry 173: 11 -53 Horsfall, J. , Cleary, M. , Hunt, G. E. , & Walter, G. (2009). Psychosocial treatments for people with co-occurring severe mental illnesses and substance use disorders (dual diagnosis): A review of empirical evidence. Harvard review of psychiatry, 17(1), 24 -34. Humphreys K, Mc. Lellan AT. Brief intervention, treatment and recovery support services for Americans who have substance use disorders: An overview of policy in the Obama Administration. Psychological Services. 2010; 7(4): 275 -284. John son KH, Bazargan M, Cherpitel CJ. 2001. Alcohol, tobacco, and drug use and the onset of type 2 diabetes among inner-city minority patients. Journal of the American Board of Family Medicine. 14(6): 430 -436 Madras BK, Compton WM, Avula D, et al. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites. Drug and Alcohol Dependence. 2009; 99(1 -3): 280 -295. Manchikanti L, Cash KA, Damron KS. 2006. Controlled substance abuse and illicit drug use in chronic pain patients: an evaluation of multiple variables. Pain Physician. 9: 215 -226. Mac. Mahon MJ, Tallentire VR. 2010. Stimulating stuff: the pathological effects of cocaine and amphetamines on the cardiovascular system. British Journal of Diabetes & Vascular Disease. 10: 251 -255 Mangrum, L. F. , Spence, R. T. , & Lopez, M. (2006). Integrated versus parallel treatment of co-occurring psychiatric and substance use disorders. Journal of substance abuse treatment, 30(1), 79 -84 Mauer BJ. 2006. Behavioral Health/Primary Care Integration: The Four Quadrant Model and Evidence-Based Practices. National Council for Community Behavioral Healthcare Mc. Coy CB, Metsch LR, Chitwood DD, et al. 2001. Drug Use and Barriers to Use of Health Care Services. Substance Use & Misuse, 36(6 -7): 789 -806 Mc. Donald III AJ, Wang NW, Camargo Jr. CA. US emergency department visits for alcohol-related diseases and injuries between 1992 and 2000. Archives of Internal Medicine. 2004; 164(5): 531 -537. 66
WORKS CITED • • • • Mc. Lellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug Dependence, a Chronic Medical Illness: Implications for Treatment, Insurance, and Outcomes Evaluation. Journal of the American Medical Association. 2000; 284(13): 1689 -1695. Mertens JR, Flisher AJ, Satre DD. 2008. The role of medical conditions and primary care services in 5 -year substance use outcomes among chemical dependencey treatment patients. Drug and Alcohol Dependence. 98(1 -2): 45 -53 Mertens JR, Yun WL, Parthasarathy S, et al. 2003. Medical and psychiatric conditions of alcohol and drug treatment patients in an HMO: comparison with matched controls. Archives of Internal Medicine 163(20): 2511 -2517. National Institute on Drug Abuse. (accessed February 2012). Medical Consequences of Drug Abuse. http: //www. drugabuse. gov/related-topics/medical-consequences-drug-abuse National Center on Addiction and Substance Abuse, 2012. Addiction Medicine: Closing the Gap Between Science and Practice. New York: The Author Oregon Department of Human Services. 2008. Measuring Premature Mortality Among Oregonians. Oregon Department of Human Services, Addiction and Mental Health Division. National Institute on Drug Abuse. 2011. Drug Abuse and the Link to HIV/AIDS and Other Infectious Diseases. http: //www. drugabuse. gov/sites/default/files/drugaids. pdf Parry CD, Blank MB, Pithey Al. 2007. Responding to the threat of HIV among persons with mental illness and substance abuse. Current Opinion in Psychiatry. 20(3): 235 -241. Parthasarathy S, Mertens JM, Moore C, Weisner C. Utilization and cost impact of integrating substance abuse treatment and primary care. Med Care. 2003; 41(3): 357 -367. Pietraszek A, Gregersen S, Hermansen K. 2919. Alcohol and Type 2 Diabetes: A Review. Nutrition, Metabolism and Cardiovascular Diseases. 20(5): 366 -375 President's New Freedom Commission on Mental Health. Achieving the Promise: Transforming Mental Health Care in America: Final Report, July 2003. Reif S, Larson MJ, Cheng DM, et al. 2011. Chronic disease and recent addiction treatment utilization among alcohol and drug dependent adults. Substance Abuse Treatment, Prevention, and Policy. 6: 28. Robinson J, Sareen J, Cox BJ, et al. 2011. Role of Selanxiety and substance use disorders: a longitudinal 67 investigation. Archives of Genf-medication in the development of comorbid eral Psychiatry 68(8): 800 -807. Saitz, R. (2015). ‘SBIRT’is the answer? Probably not. Addiction, 110(9), 1416 -1417
WORKS CITED • • • Saitz R, Horton NJ, Larson MJ. 2005. Primary medical care and reductions in addiction severity: a prospective cohort study. Addiction 100(1): 70 -78. Schwartz, B. G. , Rezkalla, S. , & Kloner, R. A. (2010). Cardiovascular effects of cocaine. Circulation, 122(24), 2558 -2569. Sesso HD, Cook NR, Buring JE. 2008. Alcohol Consumption and the Risk of Hypertension in Women and Men. Hypertension 51(4): 1080 -1087. Sterling, S. , Chi, F. , & Hinman, A. (2011). Integrating care for people with co-occurring alcohol and other drug, medical, and mental health conditions. Alcohol research & health: the journal of the National Institute on Alcohol Abuse and Alcoholism, 33(4), 338. Substance Abuse and Mental Health Services Administration, Results from the 2013 National Survey on Drug Use and Health: Mental Health Findings, NSDUH Series H-49, HHS Publication No. (SMA) 14 -4887. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2014. Substance Abuse and Mental Health Services Administration (2012). Innovations in Addictions Treatment: Addiction Treatment Providers Working With Integrated Primary Care Services Treatment Research Institute, Inc. 2010. Forum on Integration: A Collaborative for States. Philadelphia (PA): Treatment Research Institute, Inc. Weisner C, Mertens J, Parthasarathy S, et al. Integrating primary medical care with addiction treatment: a randomized control trial. Journal of the American Medical Association. 2001; 286(14): 1715 -1723. Weiss RD, Griffin ML, Mirin SM. Drug abuse as self-medication for depression: an empirical study. 1992. American Journal of Drug and Alcohol Abuse 18(2): 121 -129. Wesselius LJ. 1997. Pulmonary Disorders Associated With use of Illicit Drugs. Clinical Pulmonary Medicine. 4(2) 68
Howard Padwa, Ph. D. hpadwa@ucla. edu 69
 Howard padwa
Howard padwa Gudi padwa 2003
Gudi padwa 2003 Howard university strategic plan
Howard university strategic plan Vyran george
Vyran george Howard university cancer center
Howard university cancer center California state university long beach nursing
California state university long beach nursing Fresno state financial services
Fresno state financial services University of california irvine registrar
University of california irvine registrar Ccu final exam schedule
Ccu final exam schedule University of california
University of california University of california
University of california California university of pennsylvania global online
California university of pennsylvania global online University of southern california
University of southern california Predicitice
Predicitice Regents of university of california v. bakke
Regents of university of california v. bakke Como trabajar los unos los dieces y los cienes
Como trabajar los unos los dieces y los cienes 沈榮麟
沈榮麟 Young authors contest 2022 howard county
Young authors contest 2022 howard county Howard kornfeld md
Howard kornfeld md Tüketici kara kutu modeli
Tüketici kara kutu modeli Ebenezer howard
Ebenezer howard How are howard gardner and jean piaget different?
How are howard gardner and jean piaget different? Howard ikemoto quotes
Howard ikemoto quotes Parc du domaine howard
Parc du domaine howard Multiple intelligences ap psychology
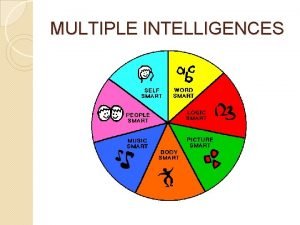
Multiple intelligences ap psychology Howard gardner learning styles
Howard gardner learning styles Le modèle d'howard et sheth
Le modèle d'howard et sheth La ciudad jardin ebenezer howard
La ciudad jardin ebenezer howard Howard w jones
Howard w jones Howard schultz transactional leadership
Howard schultz transactional leadership Howard schultz transformational leadership
Howard schultz transformational leadership Howard schultz transactional leadership
Howard schultz transactional leadership Howard hughes philanthropy
Howard hughes philanthropy Howard county gifted and talented
Howard county gifted and talented Howard koenig
Howard koenig Howard h stevenson
Howard h stevenson Dr howard gardner
Dr howard gardner Howard pickard
Howard pickard Howard r spendelow
Howard r spendelow Howard giles communication accommodation theory
Howard giles communication accommodation theory Gardner's nine intelligences
Gardner's nine intelligences Gail howard
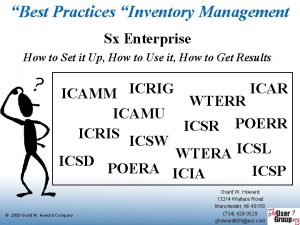
Gail howard Sx enterprise
Sx enterprise Building a life howard stevenson
Building a life howard stevenson Endovalve
Endovalve Howard stern allison
Howard stern allison Minnie howard field
Minnie howard field Howard shore lighthouse
Howard shore lighthouse Howard irwin titanic
Howard irwin titanic Howard shaw singapore
Howard shaw singapore Peter howard jones
Peter howard jones Neuroop
Neuroop Coahuiltecan tattoos
Coahuiltecan tattoos Dr. howard gardner
Dr. howard gardner Howard zinn chapter 9
Howard zinn chapter 9 5 minds of the future
5 minds of the future Jurnal etika profesi humas
Jurnal etika profesi humas Que es la dimension fisica
Que es la dimension fisica Enseñando para cambiar vidas resumen
Enseñando para cambiar vidas resumen Howard gardner hendricks
Howard gardner hendricks Dr julie howard
Dr julie howard Dr howard zhang
Dr howard zhang Kafka franz
Kafka franz Stephen j poplawski
Stephen j poplawski Peter g schultz
Peter g schultz Leslie howard cedeira
Leslie howard cedeira Assael modeli
Assael modeli Howard davies director
Howard davies director Wilson progressive accomplishments
Wilson progressive accomplishments Howard poizner
Howard poizner