HDL Cholesterol No Longer Is Good Cholesterol Emerging





- Slides: 50
HDL Cholesterol No Longer Is Good Cholesterol: Emerging Genetic Theories Sunita Dodani & Janice S Dorman University of Pittsburgh (Study proposal)
Presentation Overview • Study background & significance – Basic description & function of lipids, lipoproteins and apoproteins – HDL & apoprotein A-1 – New theories of LDL & HDL role in atherosclerosis – Concept of dysfunctional HDL – Hypothesized causes of dysfunctional. HDL • Study Rationale • Study objectives • Study Design & Methods
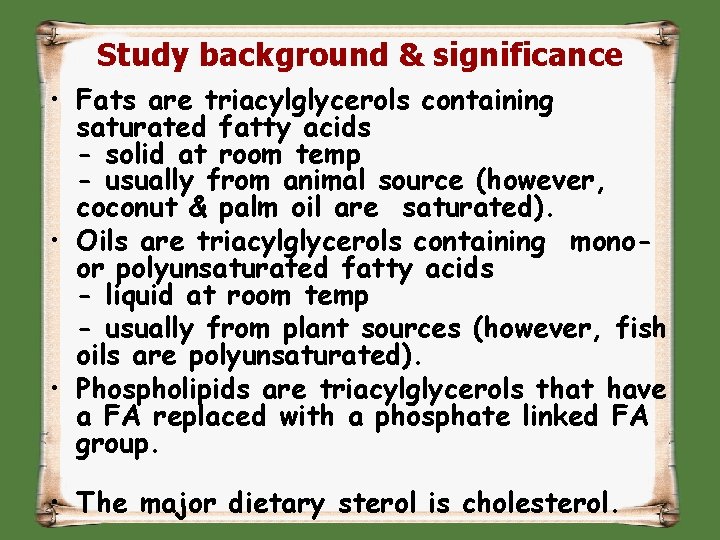
Study background & significance • Fats are triacylglycerols containing saturated fatty acids - solid at room temp - usually from animal source (however, coconut & palm oil are saturated). • Oils are triacylglycerols containing monoor polyunsaturated fatty acids - liquid at room temp - usually from plant sources (however, fish oils are polyunsaturated). • Phospholipids are triacylglycerols that have a FA replaced with a phosphate linked FA group. • The major dietary sterol is cholesterol.

Functions Of Lipids • Major components of cell membranes. • Required to solubilise fat soluble vitamins • Biosynthetic precursors (e. g. steroid hormones from cholesterol) • Protection (e. g. kidneys are shielded with fat in fed state) • Insulation
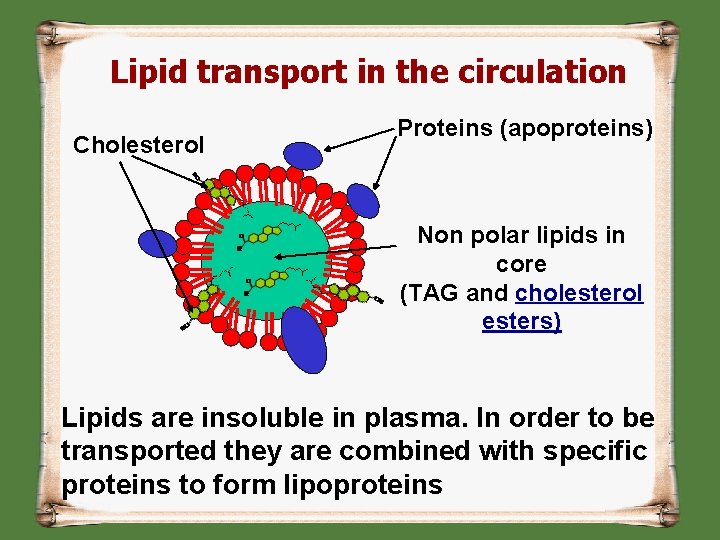
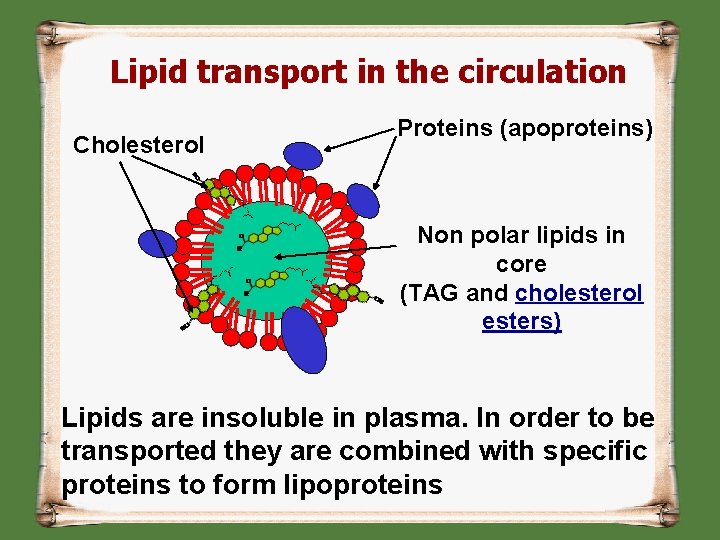
Lipid transport in the circulation Cholesterol Proteins (apoproteins) Non polar lipids in core (TAG and cholesterol esters) Lipids are insoluble in plasma. In order to be transported they are combined with specific proteins to form lipoproteins
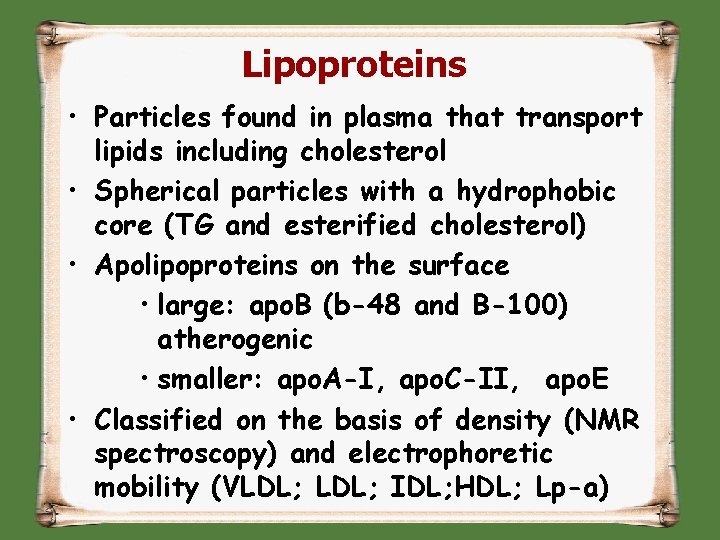
Lipoproteins • Particles found in plasma that transport lipids including cholesterol • Spherical particles with a hydrophobic core (TG and esterified cholesterol) • Apolipoproteins on the surface • large: apo. B (b-48 and B-100) atherogenic • smaller: apo. A-I, apo. C-II, apo. E • Classified on the basis of density (NMR spectroscopy) and electrophoretic mobility (VLDL; IDL; HDL; Lp-a)
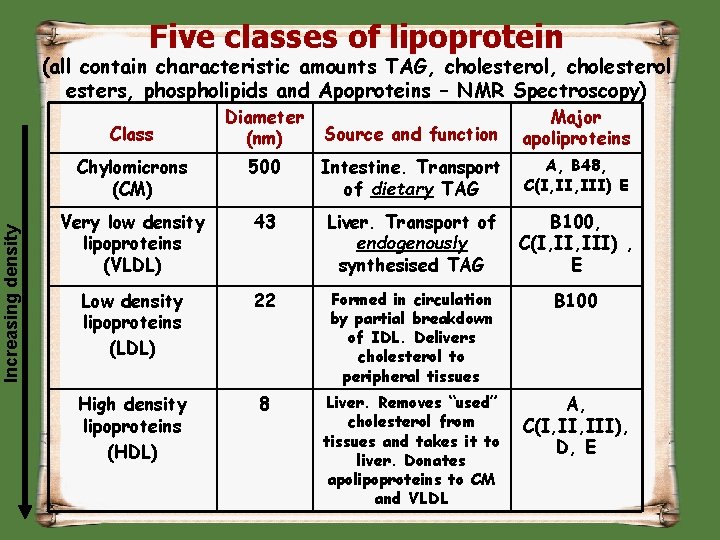
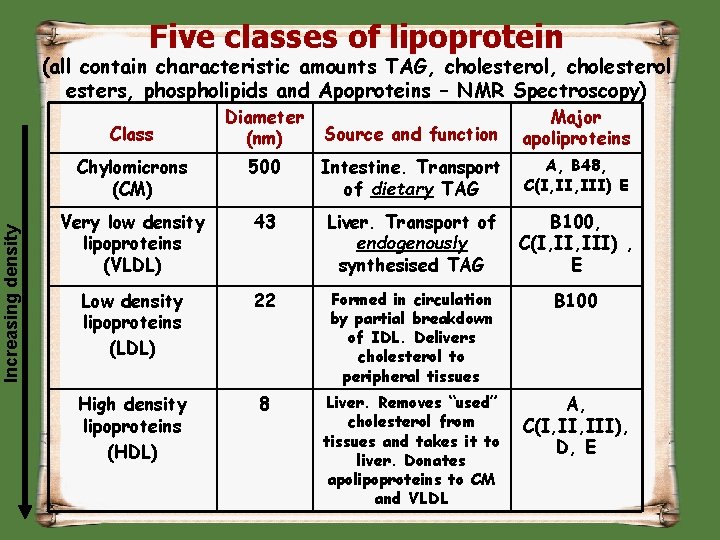
Five classes of lipoprotein (all contain characteristic amounts TAG, cholesterol esters, phospholipids and Apoproteins – NMR Spectroscopy) Increasing density Class Diameter (nm) Source and function Major apoliproteins Chylomicrons (CM) 500 Intestine. Transport of dietary TAG A, B 48, C(I, III) E Very low density lipoproteins (VLDL) 43 Liver. Transport of endogenously synthesised TAG B 100, C(I, III) , E Low density lipoproteins (LDL) 22 Formed in circulation by partial breakdown of IDL. Delivers cholesterol to peripheral tissues B 100 High density lipoproteins (HDL) 8 Liver. Removes “used” cholesterol from tissues and takes it to liver. Donates apolipoproteins to CM and VLDL A, C(I, III), D, E

Lipoprotei n class Density (g/m. L) Diameter (nm) Protein % of dry wt Phosph olipids % Triacylglycerols % of dry wt HDL 1. 0631. 21 5 – 15 33 29 8 LDL 1. 019 – 1. 063 18 – 28 25 21 4 IDL 1. 0061. 019 25 - 50 18 22 31 VLDL 0. 95 – 1. 006 30 - 80 10 18 50 Chylomicrons < 0. 95 100 - 500 1 - 2 7 84 Composition and properties of human lipoproteins
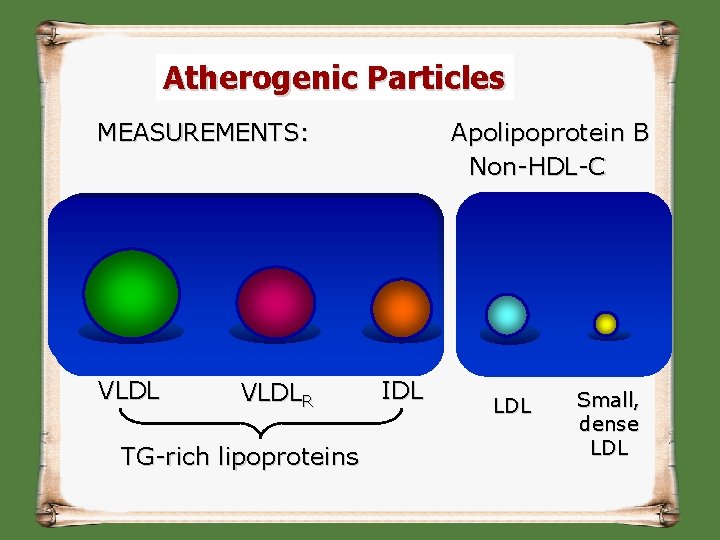
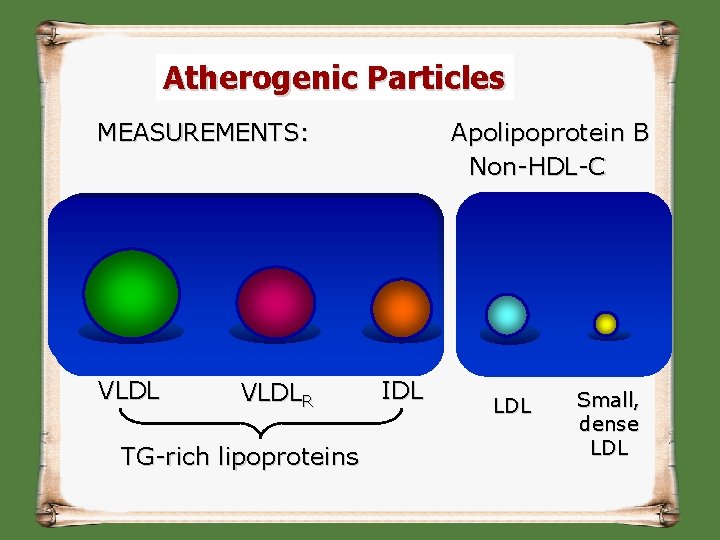
Atherogenic Particles MEASUREMENTS: VLDLR TG-rich lipoproteins Apolipoprotein B Non-HDL-C IDL LDL Small, dense LDL
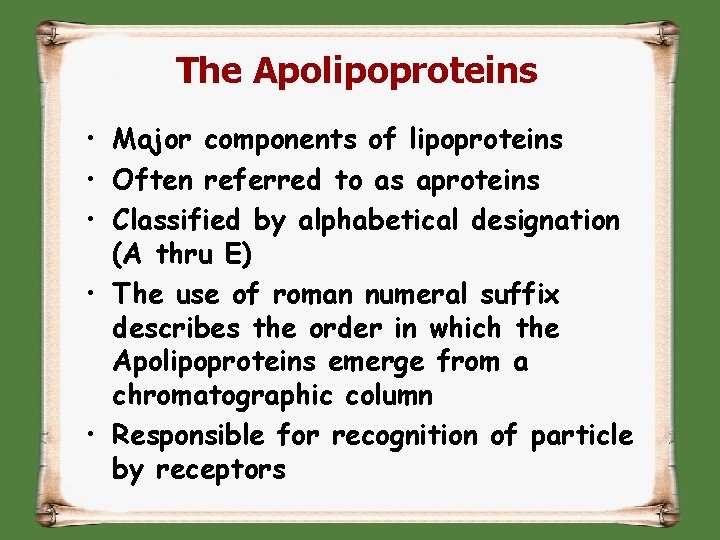
The Apolipoproteins • Major components of lipoproteins • Often referred to as aproteins • Classified by alphabetical designation (A thru E) • The use of roman numeral suffix describes the order in which the Apolipoproteins emerge from a chromatographic column • Responsible for recognition of particle by receptors
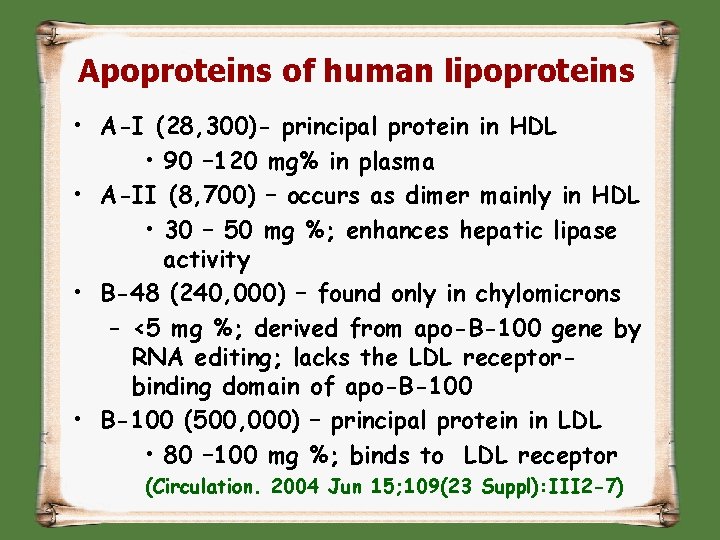
Apoproteins of human lipoproteins • A-I (28, 300)- principal protein in HDL • 90 – 120 mg% in plasma • A-II (8, 700) – occurs as dimer mainly in HDL • 30 – 50 mg %; enhances hepatic lipase activity • B-48 (240, 000) – found only in chylomicrons – <5 mg %; derived from apo-B-100 gene by RNA editing; lacks the LDL receptorbinding domain of apo-B-100 • B-100 (500, 000) – principal protein in LDL • 80 – 100 mg %; binds to LDL receptor (Circulation. 2004 Jun 15; 109(23 Suppl): III 2 -7)
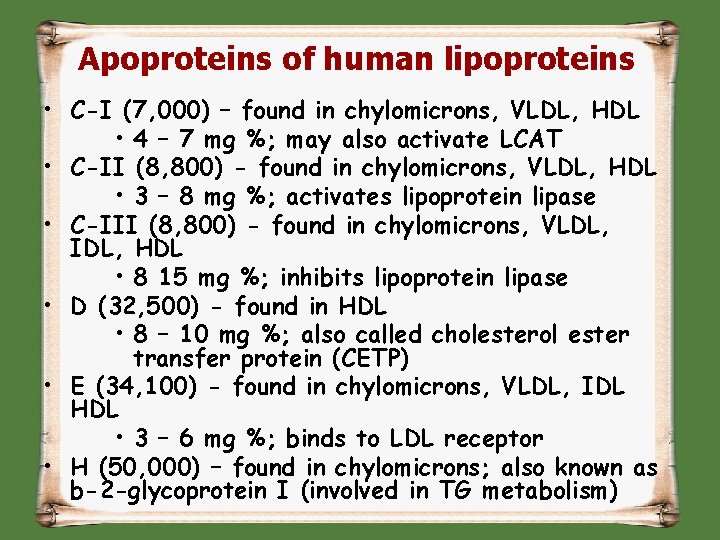
Apoproteins of human lipoproteins • C-I (7, 000) – found in chylomicrons, VLDL, HDL • 4 – 7 mg %; may also activate LCAT • C-II (8, 800) - found in chylomicrons, VLDL, HDL • 3 – 8 mg %; activates lipoprotein lipase • C-III (8, 800) - found in chylomicrons, VLDL, IDL, HDL • 8 15 mg %; inhibits lipoprotein lipase • D (32, 500) - found in HDL • 8 – 10 mg %; also called cholesterol ester transfer protein (CETP) • E (34, 100) - found in chylomicrons, VLDL, IDL HDL • 3 – 6 mg %; binds to LDL receptor • H (50, 000) – found in chylomicrons; also known as b-2 -glycoprotein I (involved in TG metabolism)
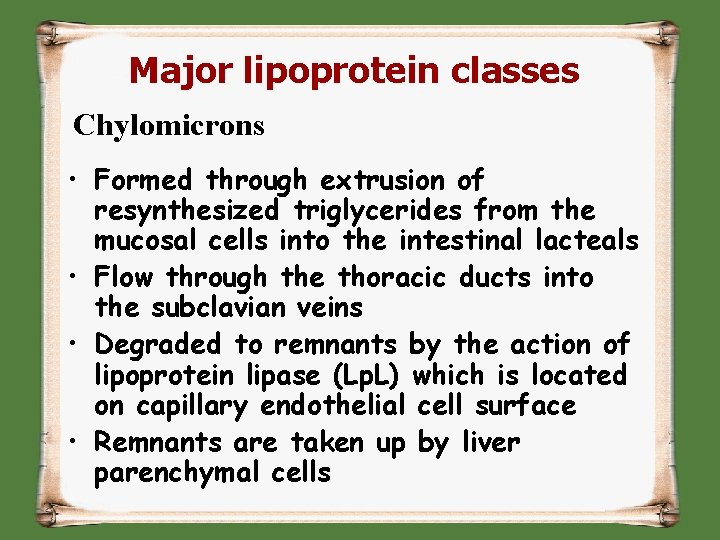
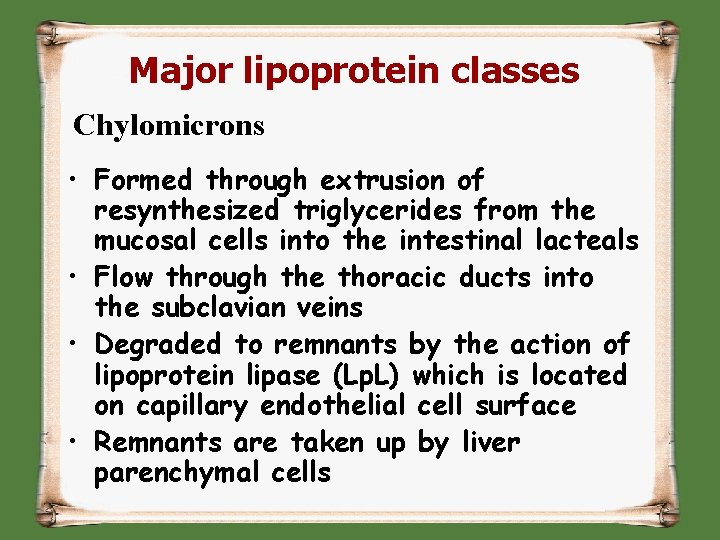
Major lipoprotein classes Chylomicrons • Formed through extrusion of resynthesized triglycerides from the mucosal cells into the intestinal lacteals • Flow through the thoracic ducts into the subclavian veins • Degraded to remnants by the action of lipoprotein lipase (Lp. L) which is located on capillary endothelial cell surface • Remnants are taken up by liver parenchymal cells
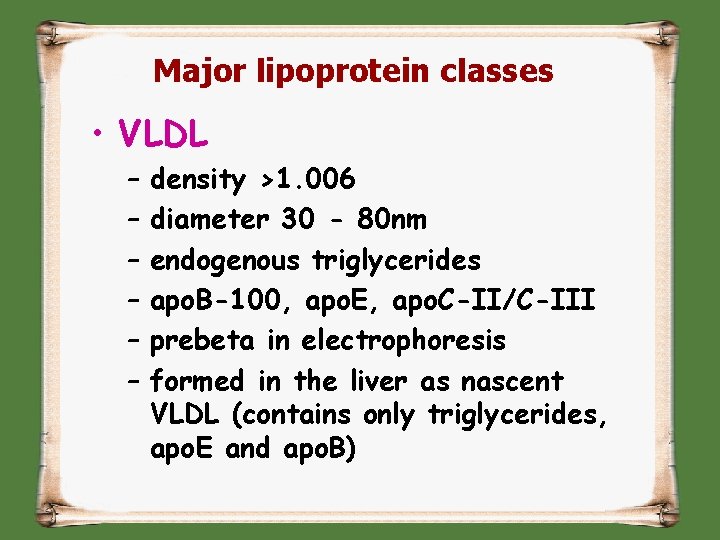
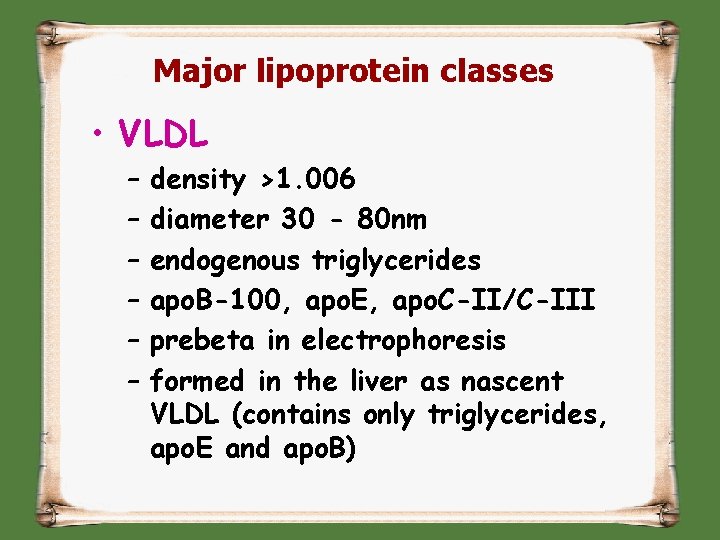
Major lipoprotein classes • VLDL – – – density >1. 006 diameter 30 - 80 nm endogenous triglycerides apo. B-100, apo. E, apo. C-II/C-III prebeta in electrophoresis formed in the liver as nascent VLDL (contains only triglycerides, apo. E and apo. B)
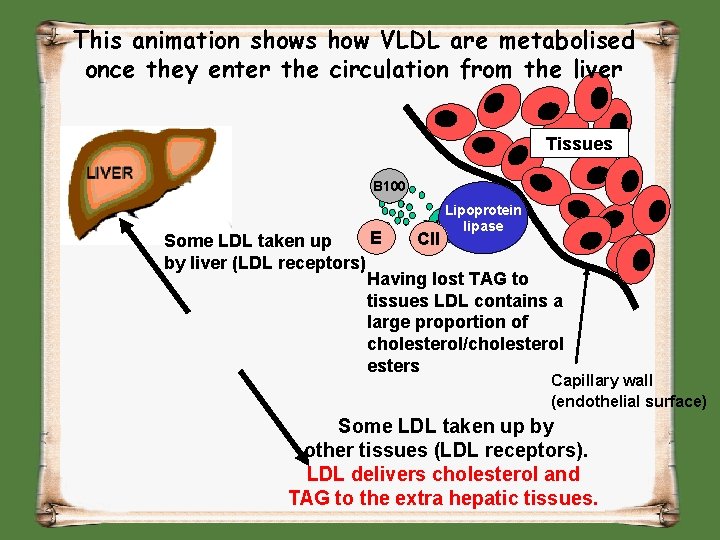
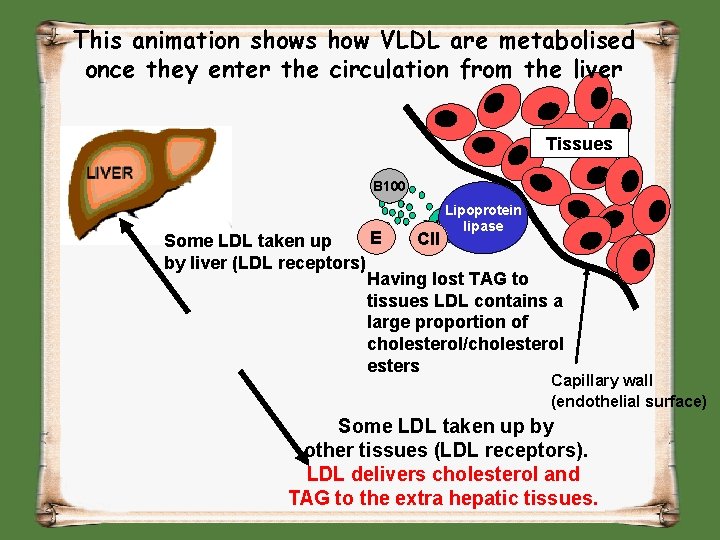
This animation shows how VLDL are metabolised once they enter the circulation from the liver Tissues B 100 VLDL B 100 Lipoprotein LDL lipase E CII Some LDL taken up by liver (LDL receptors) Having lost TAG to tissues LDL contains a large proportion of cholesterol/cholesterol esters Capillary wall (endothelial surface) Some LDL taken up by other tissues (LDL receptors). LDL delivers cholesterol and TAG to the extra hepatic tissues.
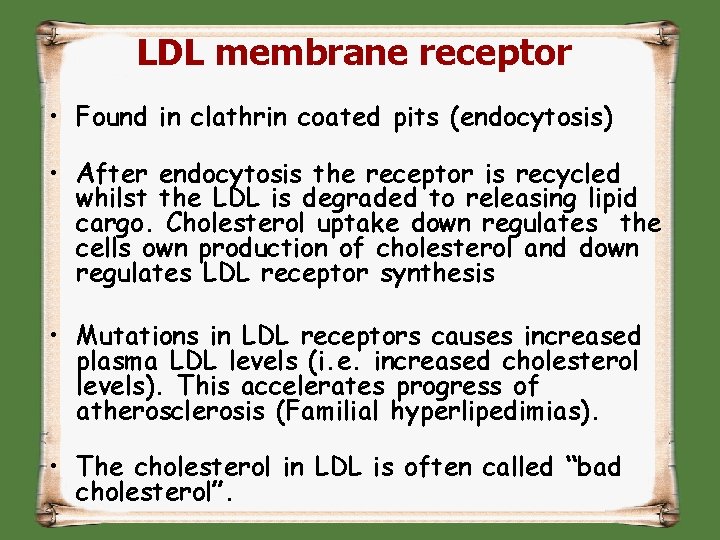
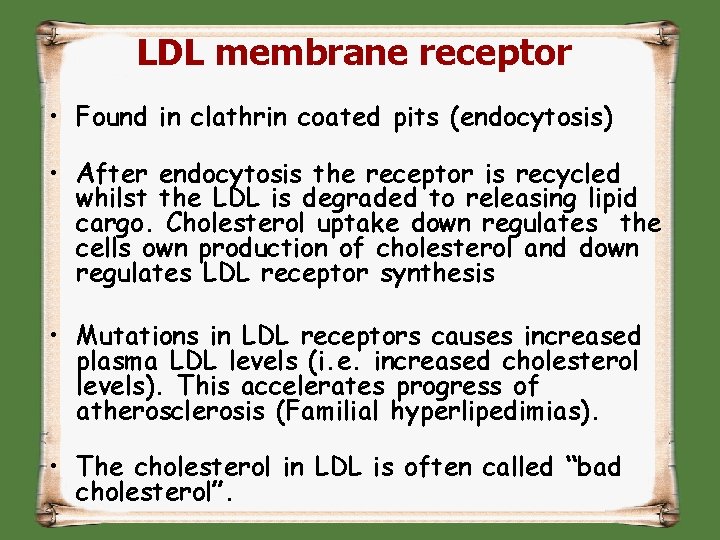
LDL membrane receptor • Found in clathrin coated pits (endocytosis) • After endocytosis the receptor is recycled whilst the LDL is degraded to releasing lipid cargo. Cholesterol uptake down regulates the cells own production of cholesterol and down regulates LDL receptor synthesis • Mutations in LDL receptors causes increased plasma LDL levels (i. e. increased cholesterol levels). This accelerates progress of atherosclerosis (Familial hyperlipedimias). • The cholesterol in LDL is often called “bad cholesterol”.
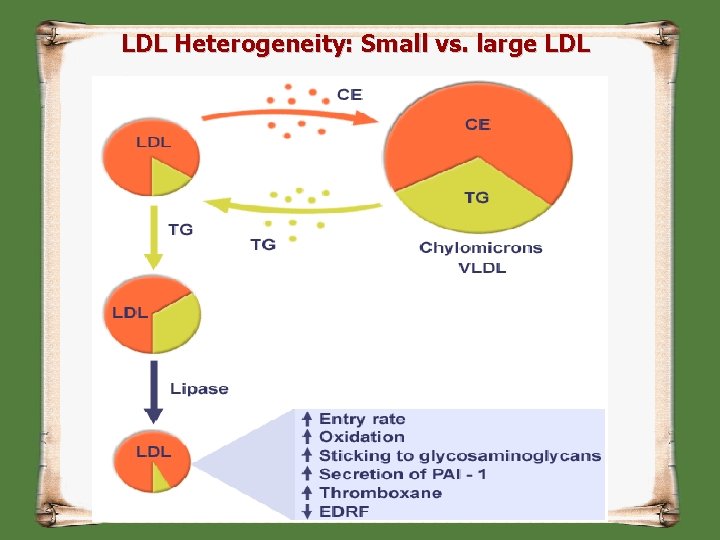
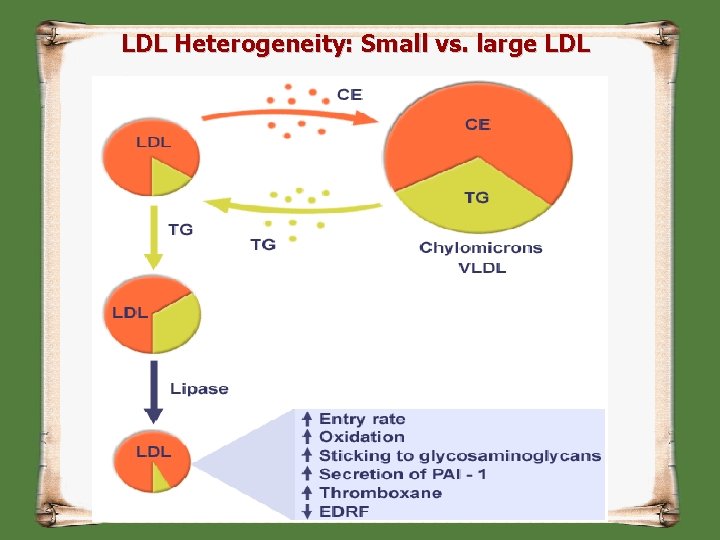
LDL Heterogeneity: Small vs. large LDL

Production of Small Dense LDL Although size (& lipid content) changes, there is always 1 molecule apo B protein / particle Lipoprotein receptors B B TG CE VLDL Lipase Oxidation & modification (CETP) VLDL Lipids. IDL large. LDL dense remnants transferred 1 2 3
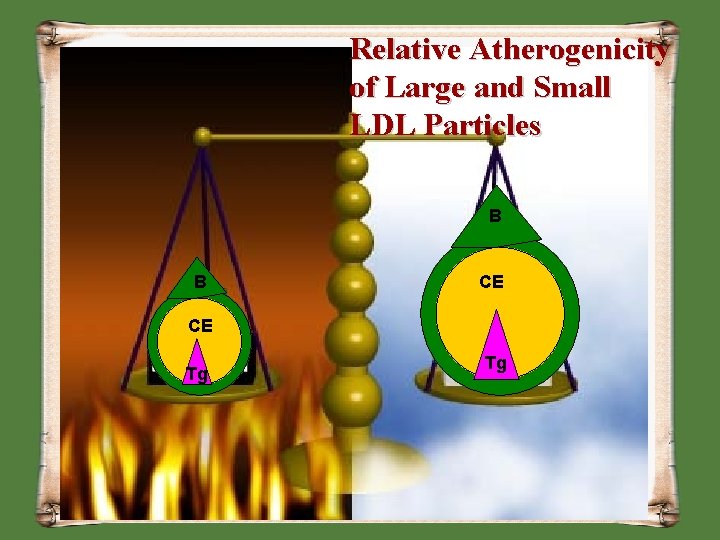
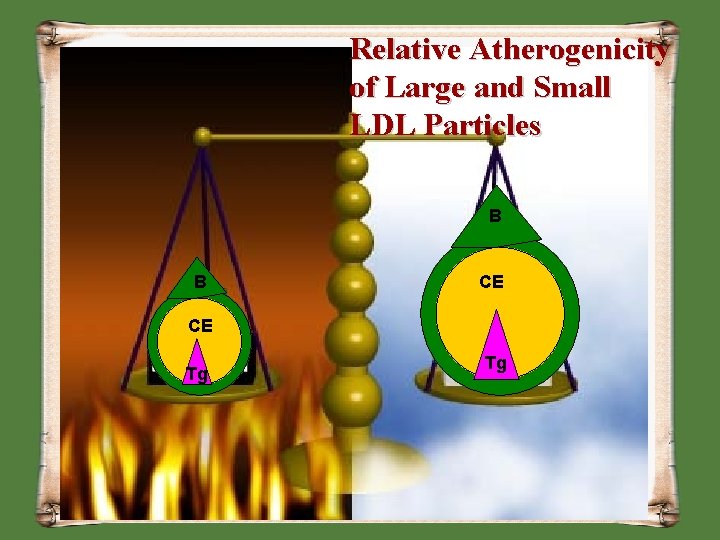
Relative Atherogenicity of Large and Small LDL Particles B B CE CE Tg Tg
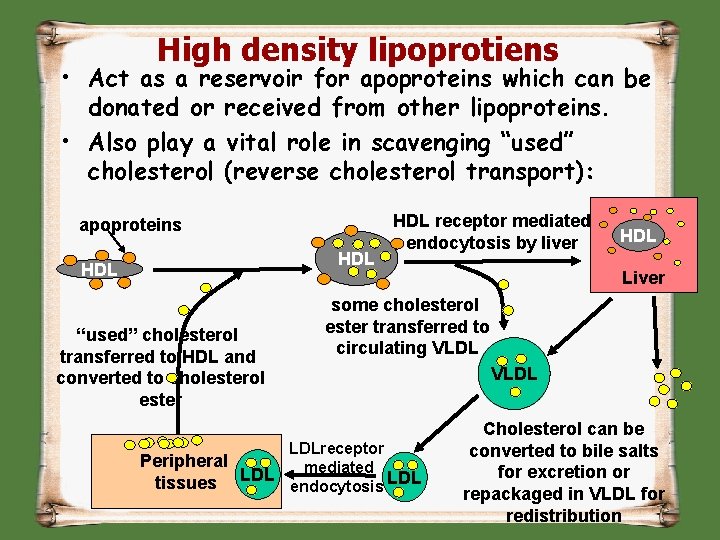
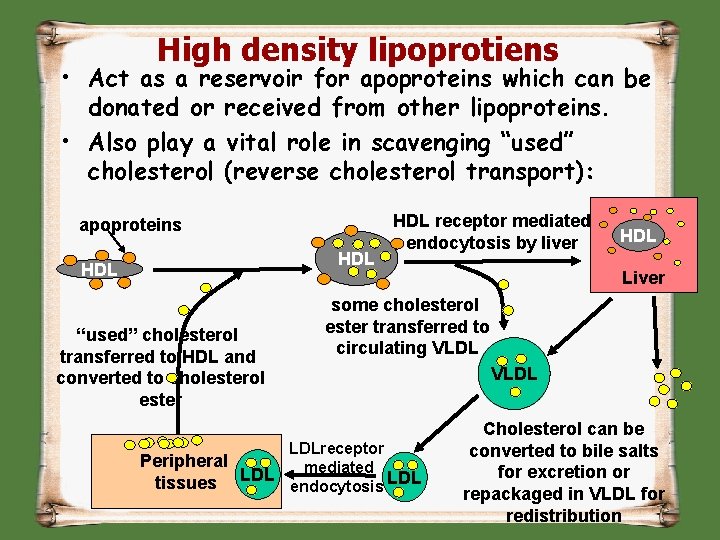
High density lipoprotiens • Act as a reservoir for apoproteins which can be donated or received from other lipoproteins. • Also play a vital role in scavenging “used” cholesterol (reverse cholesterol transport): apoproteins HDL “used” cholesterol transferred to HDL and converted to cholesterol ester HDL receptor mediated endocytosis by liver HDL Liver some cholesterol ester transferred to circulating VLDL LDLreceptor Peripheral mediated LDL tissues endocytosis Cholesterol can be converted to bile salts for excretion or repackaged in VLDL for redistribution
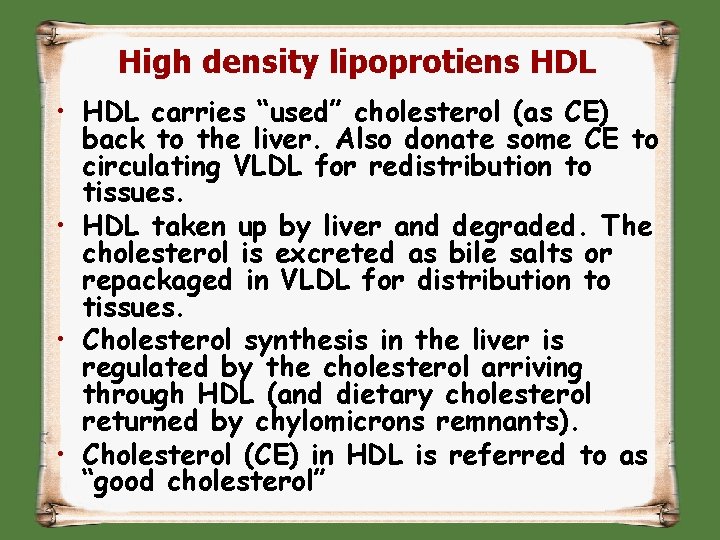
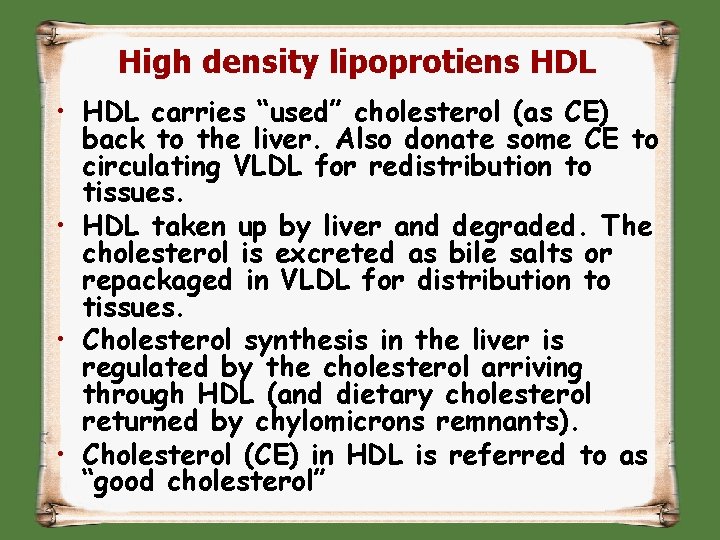
High density lipoprotiens HDL • HDL carries “used” cholesterol (as CE) back to the liver. Also donate some CE to circulating VLDL for redistribution to tissues. • HDL taken up by liver and degraded. The cholesterol is excreted as bile salts or repackaged in VLDL for distribution to tissues. • Cholesterol synthesis in the liver is regulated by the cholesterol arriving through HDL (and dietary cholesterol returned by chylomicrons remnants). • Cholesterol (CE) in HDL is referred to as “good cholesterol”

Helical Wheel Projection Of A Portion Of Apolipoprotein A-1
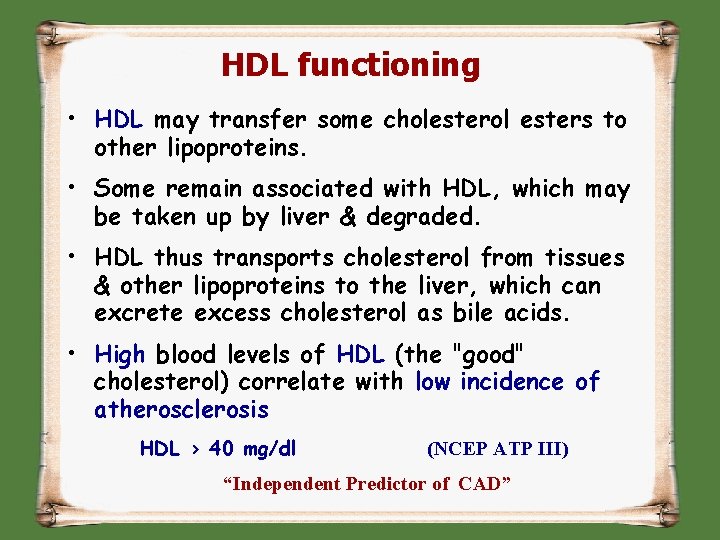
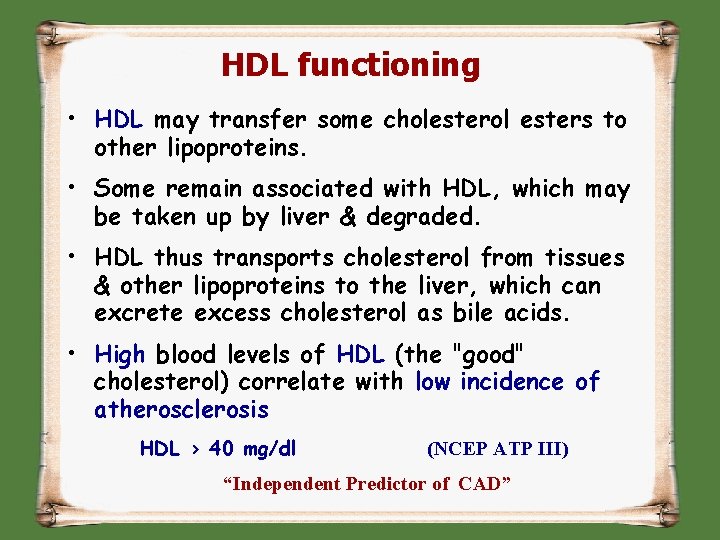
HDL functioning • HDL may transfer some cholesterol esters to other lipoproteins. • Some remain associated with HDL, which may be taken up by liver & degraded. • HDL thus transports cholesterol from tissues & other lipoproteins to the liver, which can excrete excess cholesterol as bile acids. • High blood levels of HDL (the "good" cholesterol) correlate with low incidence of atherosclerosis HDL > 40 mg/dl (NCEP ATP III) “Independent Predictor of CAD”
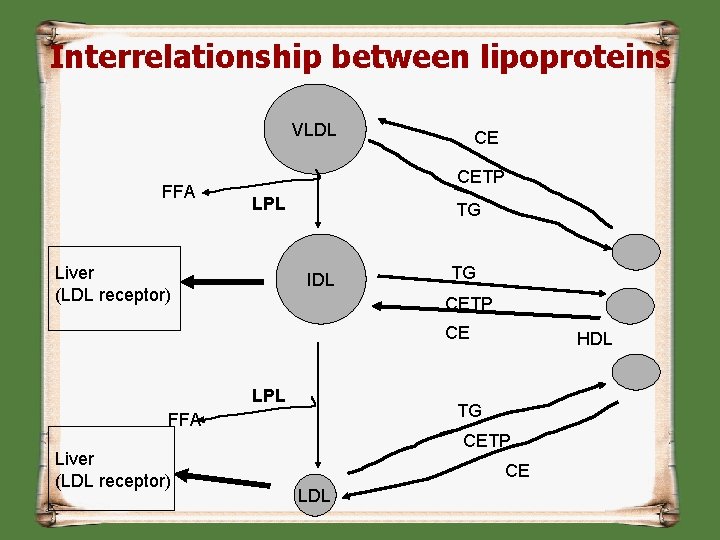
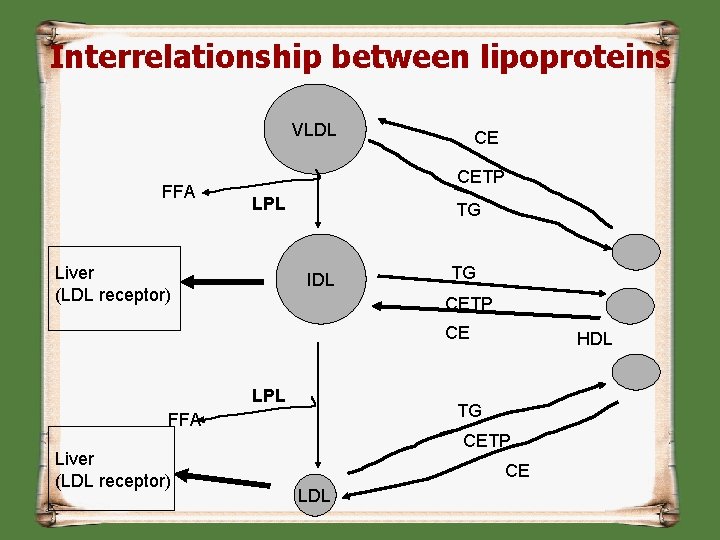
Interrelationship between lipoproteins VLDL FFA CE CETP LPL Liver (LDL receptor) TG IDL TG CETP CE LPL TG FFA Liver (LDL receptor) HDL CETP CE LDL
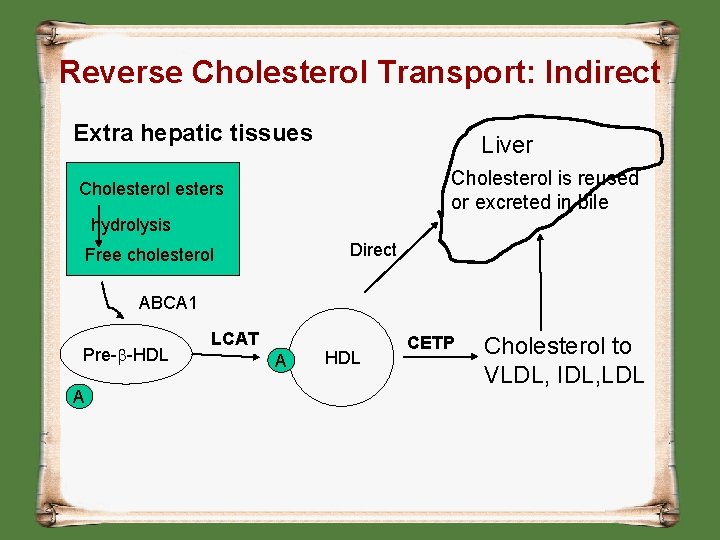
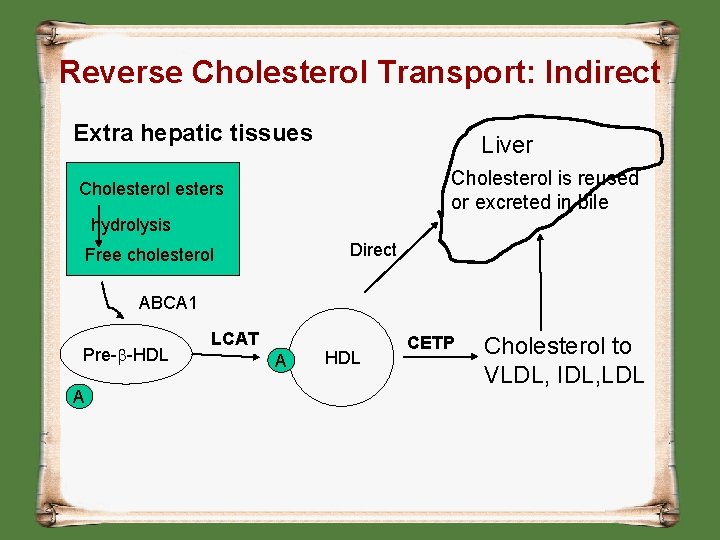
Reverse Cholesterol Transport: Indirect Extra hepatic tissues Liver Cholesterol is reused or excreted in bile Cholesterol esters hydrolysis Direct Free cholesterol ABCA 1 Pre-b-HDL A LCAT A HDL CETP Cholesterol to VLDL, IDL, LDL
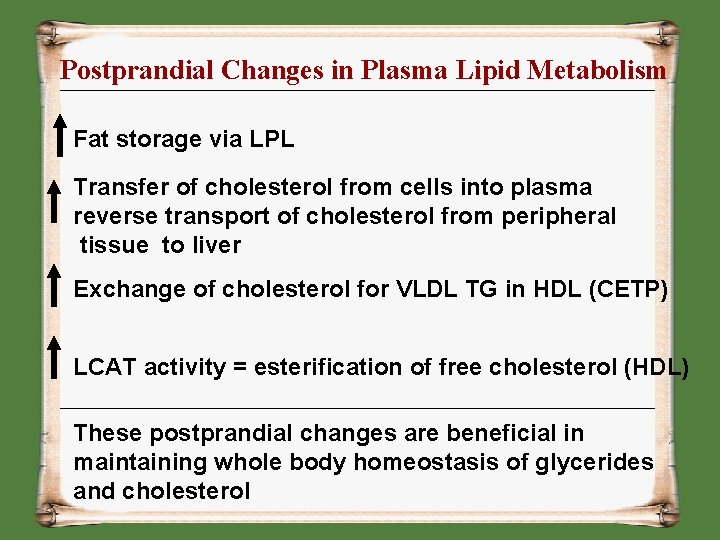
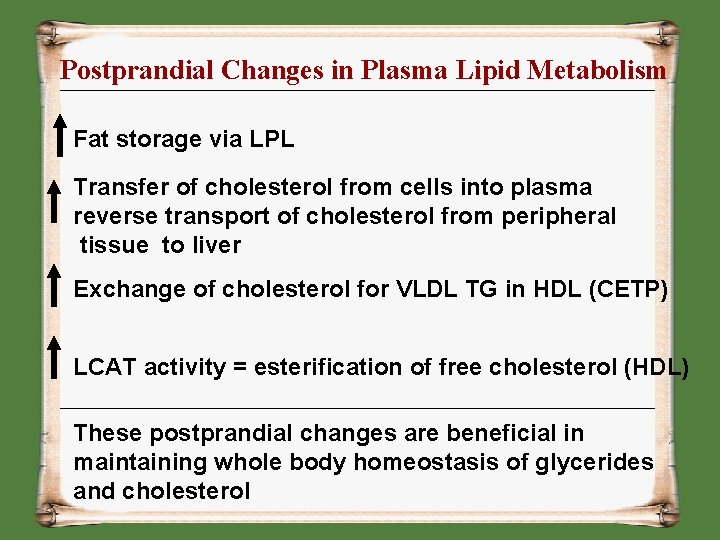
Postprandial Changes in Plasma Lipid Metabolism Fat storage via LPL Transfer of cholesterol from cells into plasma reverse transport of cholesterol from peripheral tissue to liver Exchange of cholesterol for VLDL TG in HDL (CETP) LCAT activity = esterification of free cholesterol (HDL) These postprandial changes are beneficial in maintaining whole body homeostasis of glycerides and cholesterol
1. LCAT deficiency? 2. CETP deficiency? 3. Apo AI deficiency?
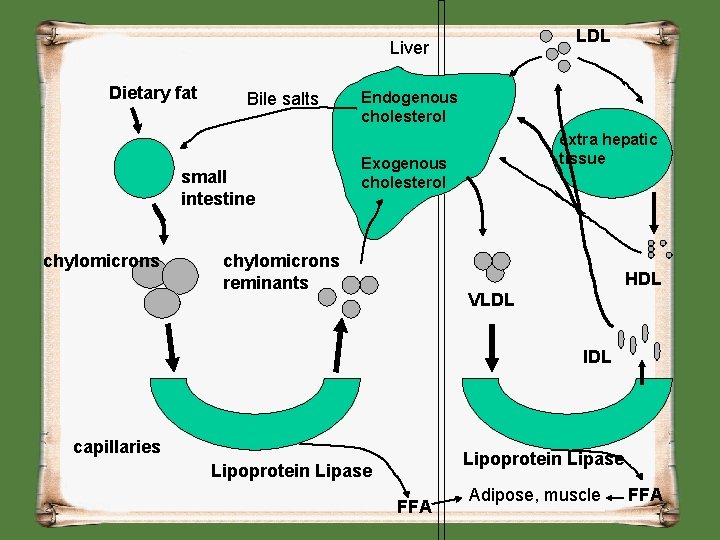
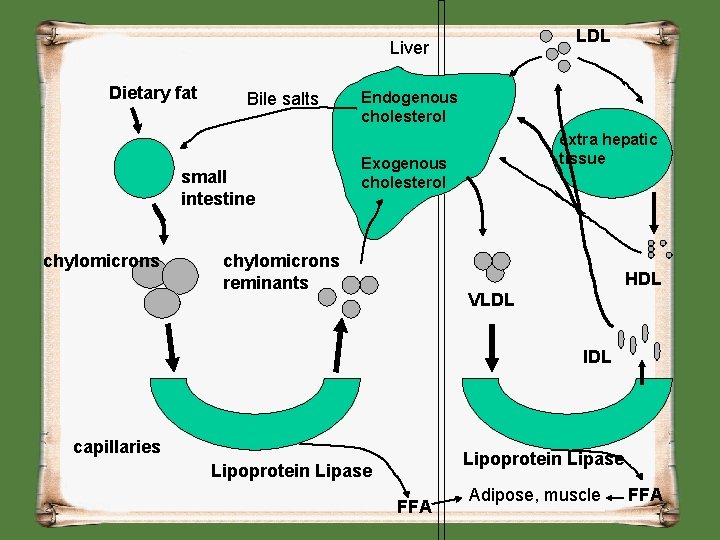
LDL Liver Dietary fat Bile salts small intestine chylomicrons Endogenous cholesterol extra hepatic tissue Exogenous cholesterol chylomicrons reminants HDL VLDL IDL capillaries Lipoprotein Lipase FFA Adipose, muscle FFA
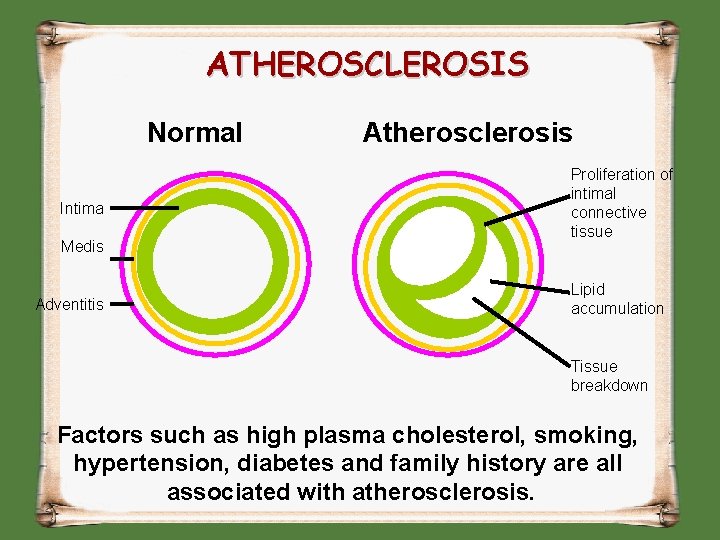
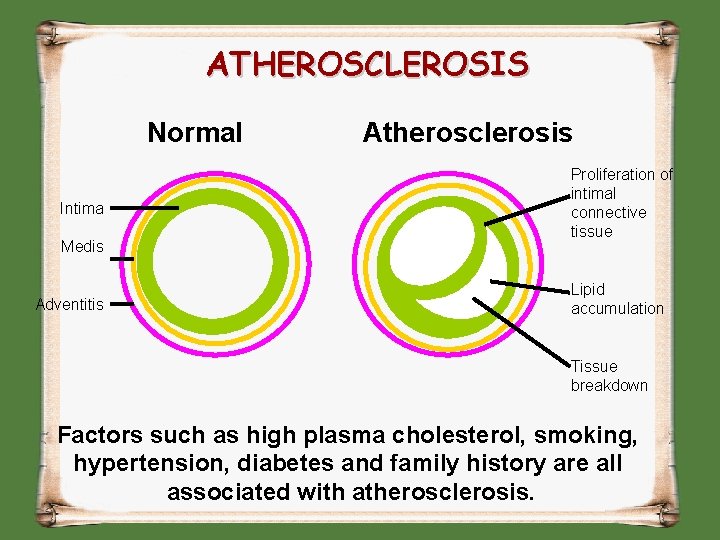
ATHEROSCLEROSIS Normal Intima Medis Adventitis Atherosclerosis Proliferation of intimal connective tissue Lipid accumulation Tissue breakdown Factors such as high plasma cholesterol, smoking, hypertension, diabetes and family history are all associated with atherosclerosis.
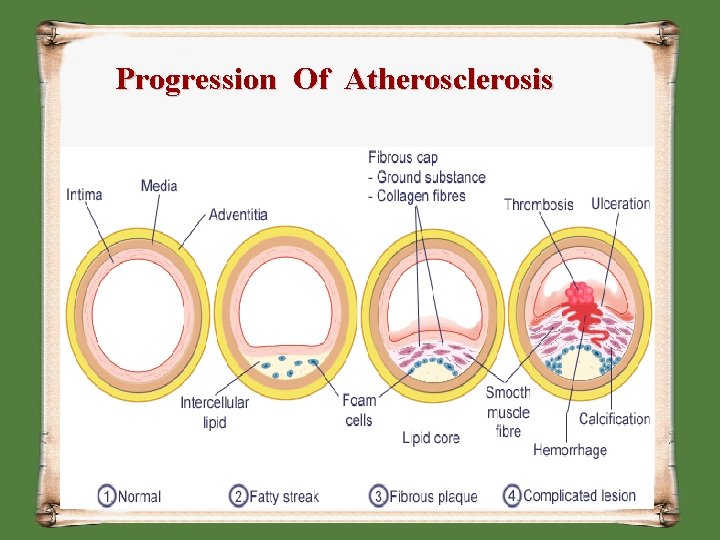
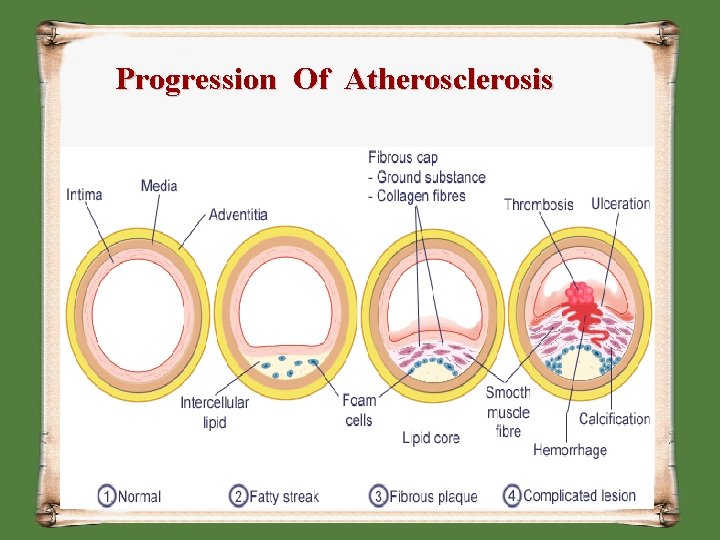
Progression Of Atherosclerosis
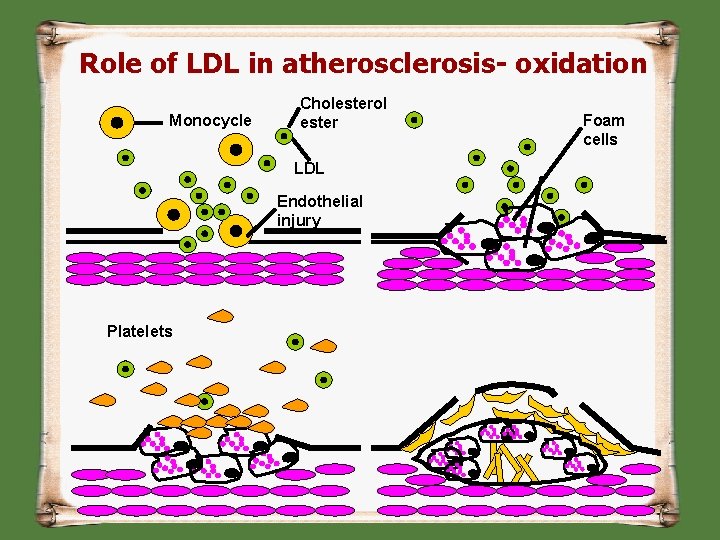
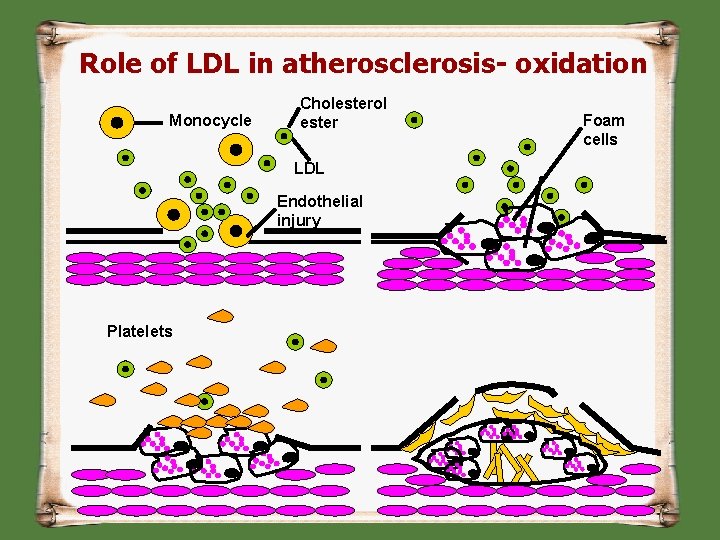
Role of LDL in atherosclerosis- oxidation Monocycle Cholesterol ester LDL Endothelial injury Platelets Foam cells
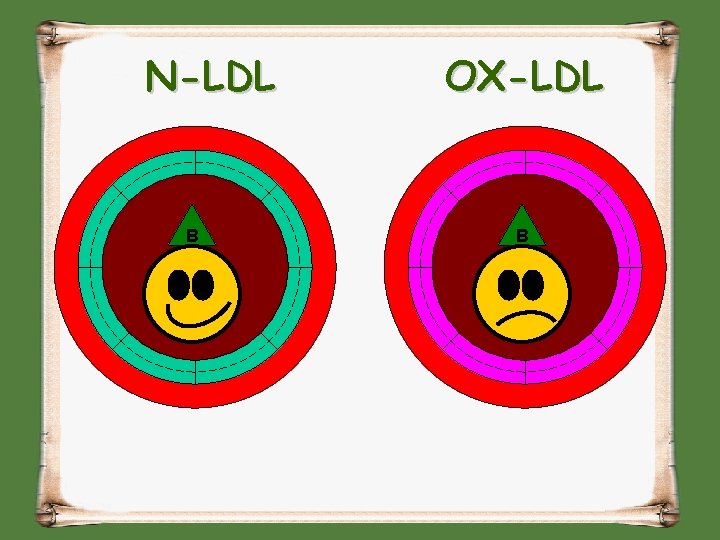
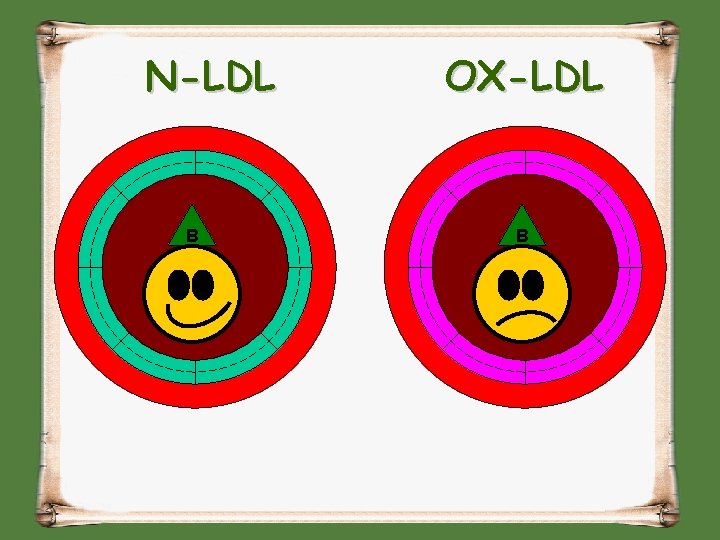
N-LDL B OX-LDL B
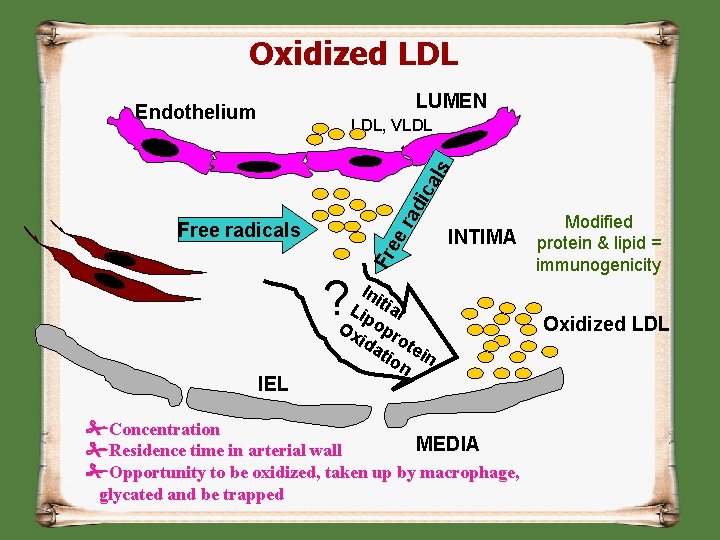
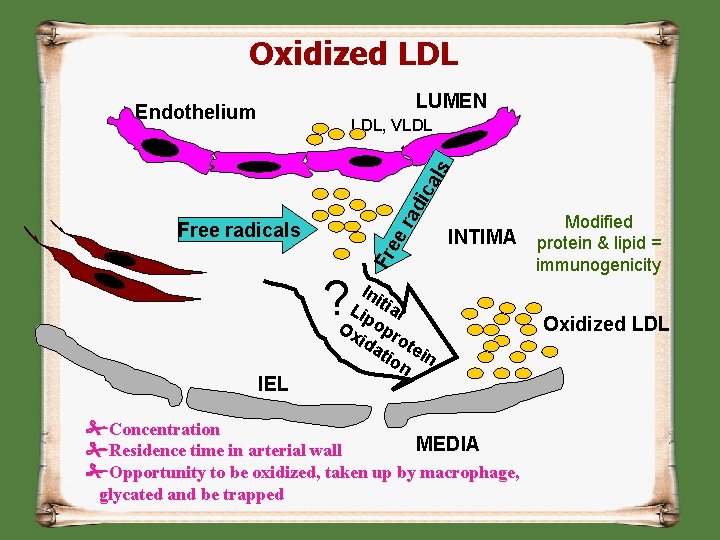
Oxidized LDL LUMEN Endothelium ra dic als LDL, VLDL INTIMA Fr ee Free radicals ? IEL Ini Lip tial Ox opr ida ote tio in n Concentration MEDIA Residence time in arterial wall Opportunity to be oxidized, taken up by macrophage, glycated and be trapped Modified protein & lipid = immunogenicity Oxidized LDL
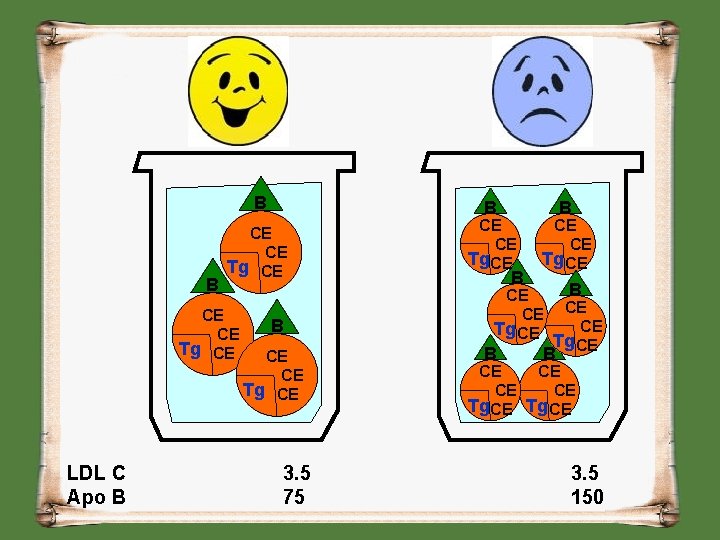
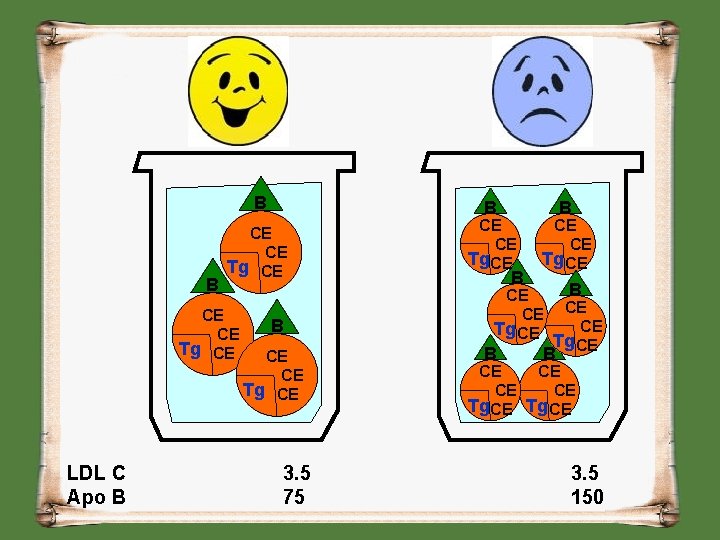
B B CE CE Tg CE LDL C Apo B B B CE Tg CE 3. 5 75 CE Tg CE B B CE Tg CE B CE CE Tg CE B B CE CE CE Tg CE 3. 5 150
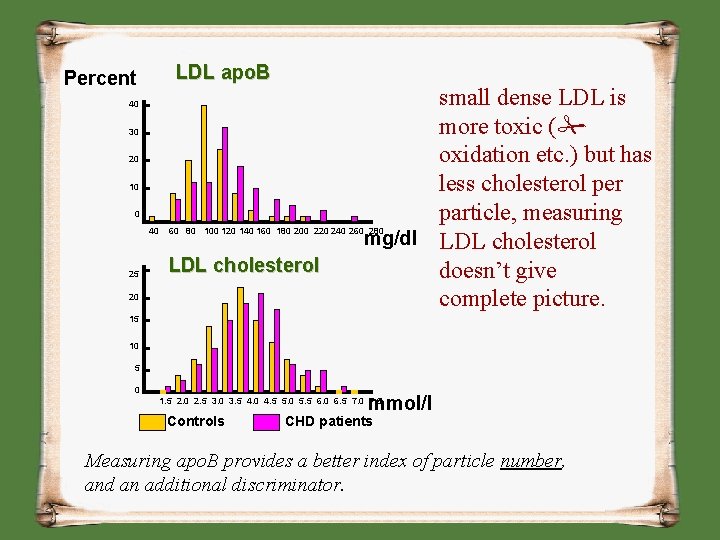
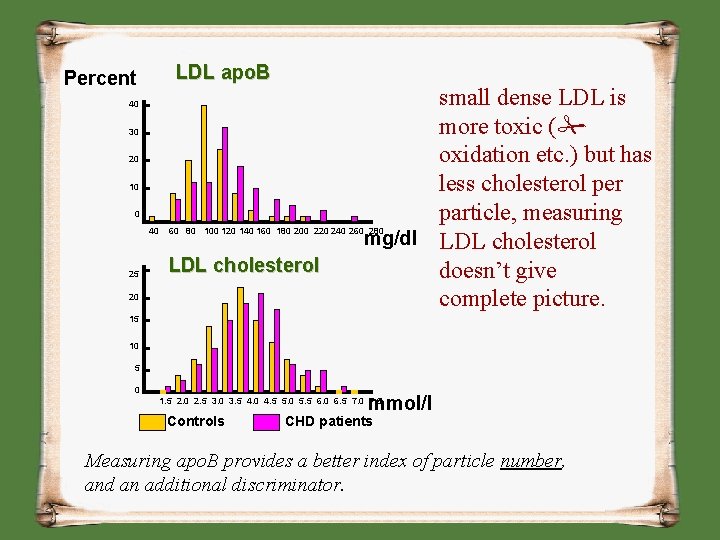
Percent LDL apo. B 40 30 20 10 0 small dense LDL is more toxic ( oxidation etc. ) but has less cholesterol per particle, measuring mg/dl LDL cholesterol doesn’t give complete picture. 40 60 80 100 120 140 160 180 200 220 240 260 280 25 LDL cholesterol 20 15 10 5 0 mmol/l 1. 5 2. 0 2. 5 3. 0 3. 5 4. 0 4. 5 5. 0 5. 5 6. 0 6. 5 7. 0 7. 5 Controls CHD patients Measuring apo. B provides a better index of particle number, and an additional discriminator.
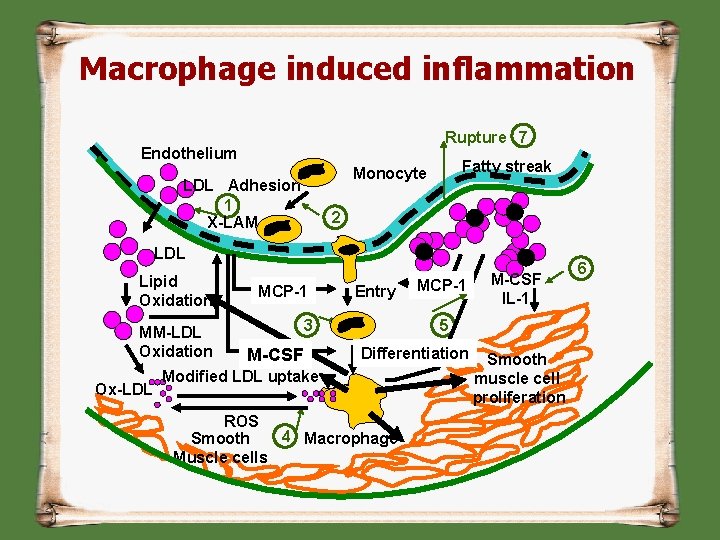
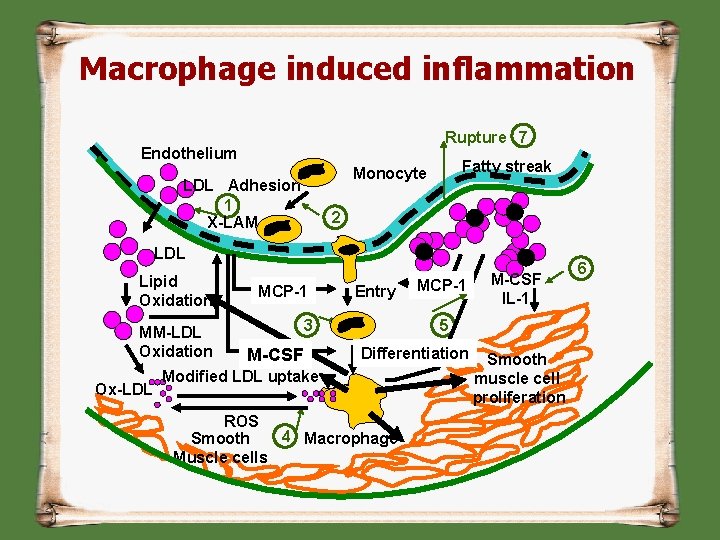
Macrophage induced inflammation Rupture 7 Endothelium Fatty streak Monocyte LDL Adhesion 1 X-LAM 2 LDL Lipid Oxidation MM-LDL Oxidation Ox-LDL MCP-1 Entry 3 M-CSF IL-1 MCP-1 5 Differentiation Modified LDL uptake ROS 4 Macrophage Smooth Muscle cells Smooth muscle cell proliferation 6
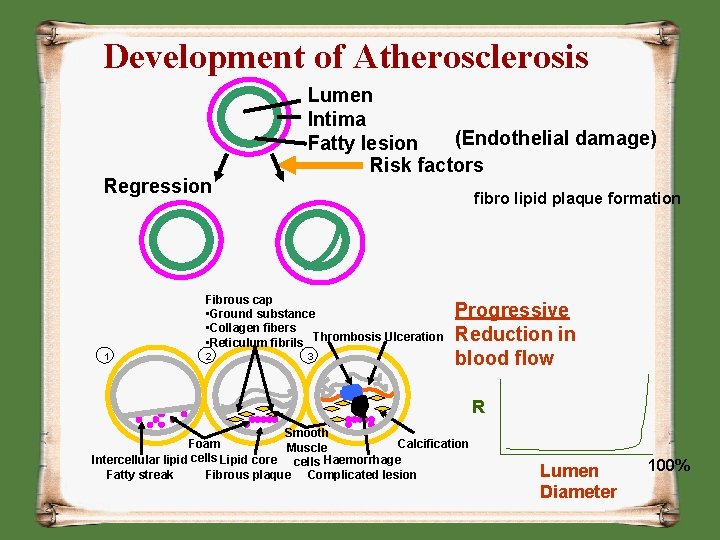
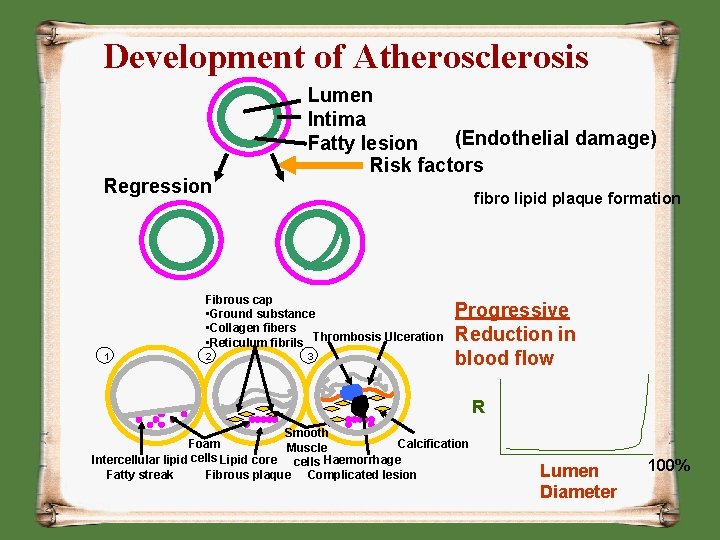
Development of Atherosclerosis Regression Lumen Intima (Endothelial damage) Fatty lesion Risk factors fibro lipid plaque formation Fibrous cap • Ground substance • Collagen fibers • Reticulum fibrils Thrombosis Ulceration 1 2 3 Progressive Reduction in blood flow R Smooth Foam Calcification Muscle cells Intercellular lipid Lipid core cells Haemorrhage Fatty streak Fibrous plaque Complicated lesion Lumen Diameter 100%
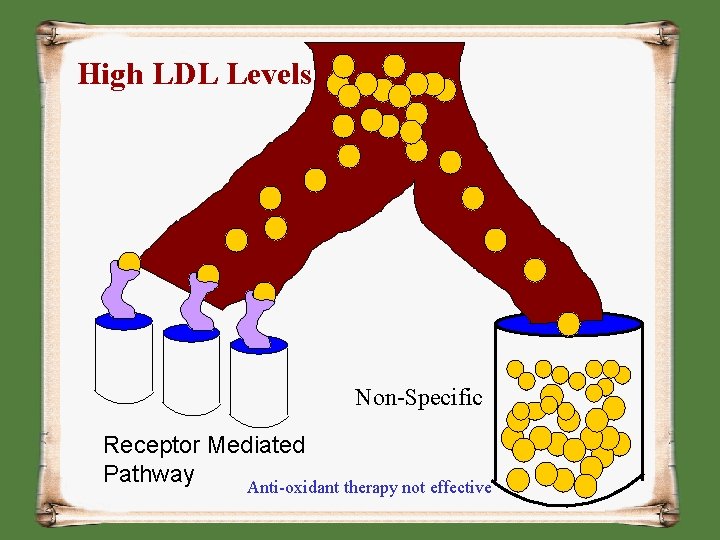
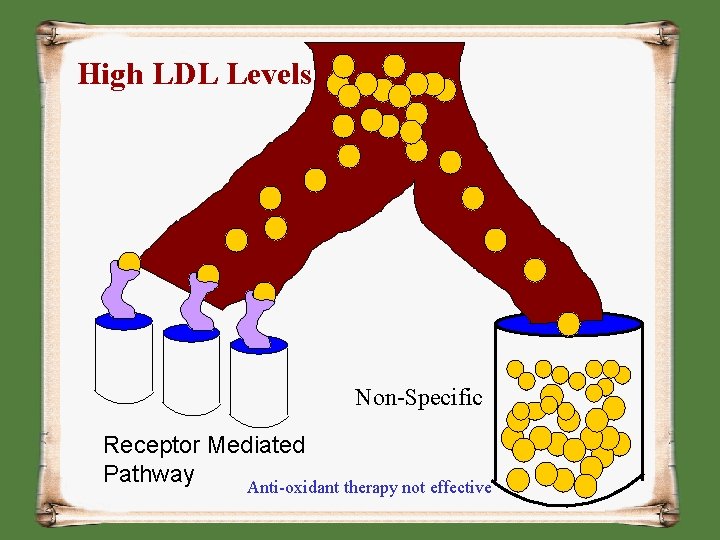
High LDL Levels Non-Specific Receptor Mediated Pathway Anti-oxidant therapy not effective
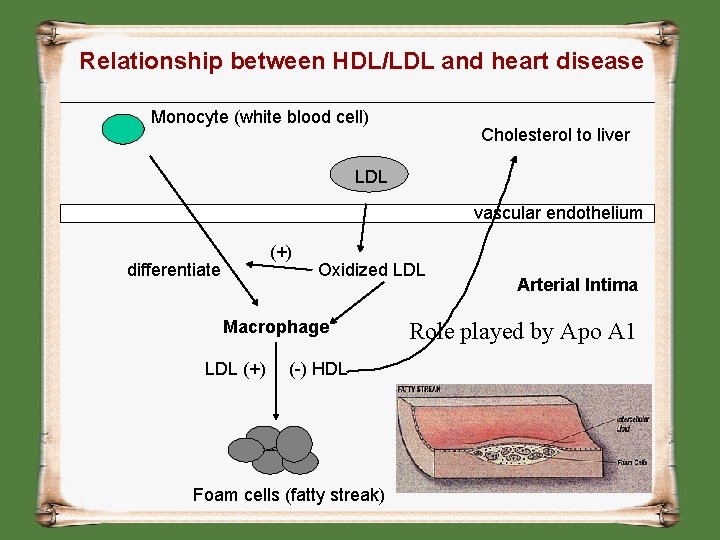
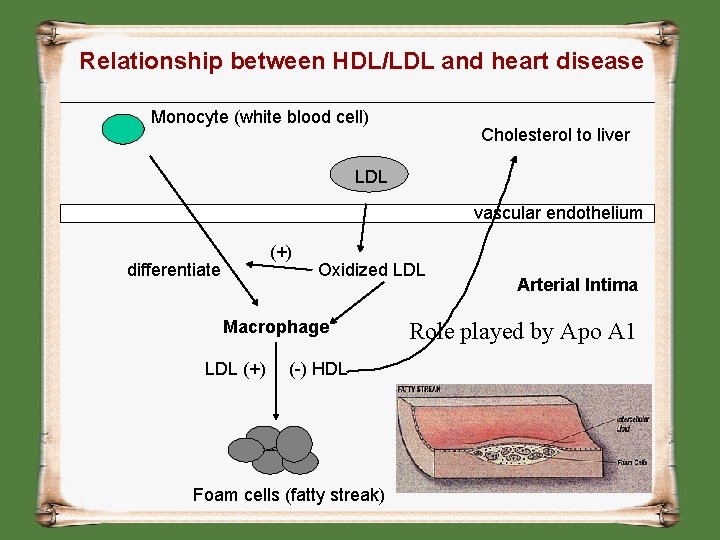
Relationship between HDL/LDL and heart disease Monocyte (white blood cell) Cholesterol to liver LDL vascular endothelium (+) differentiate Oxidized LDL Macrophage LDL (+) (-) HDL Foam cells (fatty streak) Arterial Intima Role played by Apo A 1
HDL Function • • Removal of CE from LDL Reverse Cholesterol transport Apo A-1 prevent seeding of LDL Apo A-1 prevent oxidized LDL formation
HDL NO More a Good Cholesterol Recent theories § Framingham study of the incidence of coronary heart disease (CHD) & HDL: 44% of the events occurred in men with HDLcholesterol levels of 40 mg/dl and 43% of the events occurred in women with HDLcholesterol levels of 50 mg/dl § A significant number of CHD events occur in patients with normal LDL-cholesterol levels and normal HDL-cholesterol levels. Search for markers with better predictive value
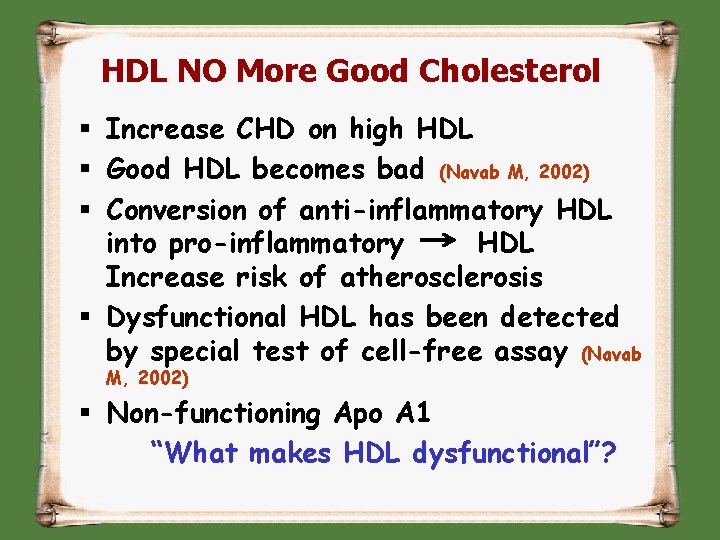
HDL NO More Good Cholesterol § Increase CHD on high HDL § Good HDL becomes bad (Navab M, 2002) § Conversion of anti-inflammatory HDL into pro-inflammatory HDL Increase risk of atherosclerosis § Dysfunctional HDL has been detected by special test of cell-free assay (Navab M, 2002) § Non-functioning Apo A 1 “What makes HDL dysfunctional”?
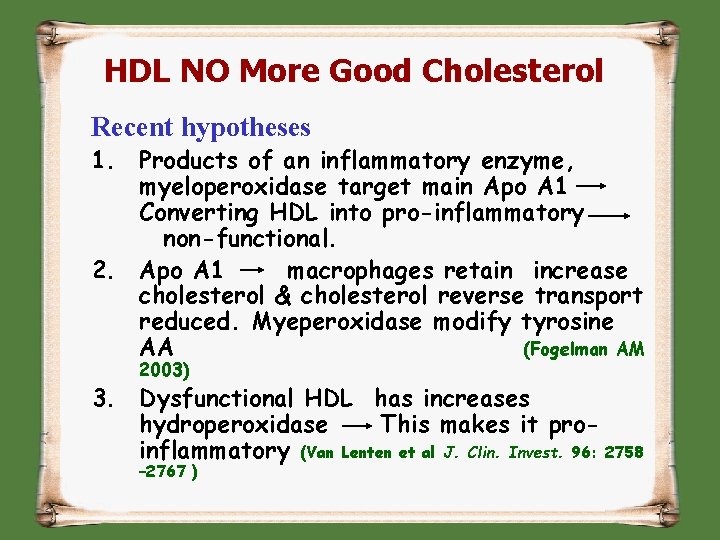
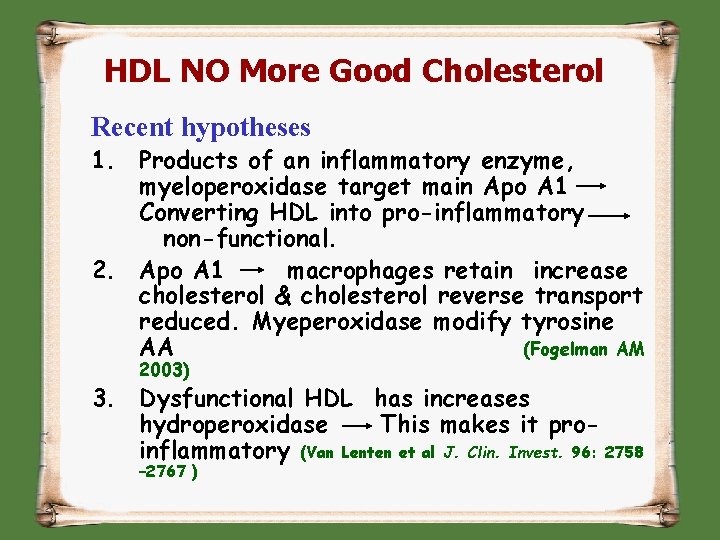
HDL NO More Good Cholesterol Recent hypotheses 1. Products of an inflammatory enzyme, myeloperoxidase target main Apo A 1 Converting HDL into pro-inflammatory non-functional. 2. Apo A 1 macrophages retain increase cholesterol & cholesterol reverse transport reduced. Myeperoxidase modify tyrosine AA (Fogelman AM 2003) 3. Dysfunctional HDL has increases hydroperoxidase This makes it proinflammatory (Van Lenten et al J. Clin. Invest. 96: 2758 – 2767 )
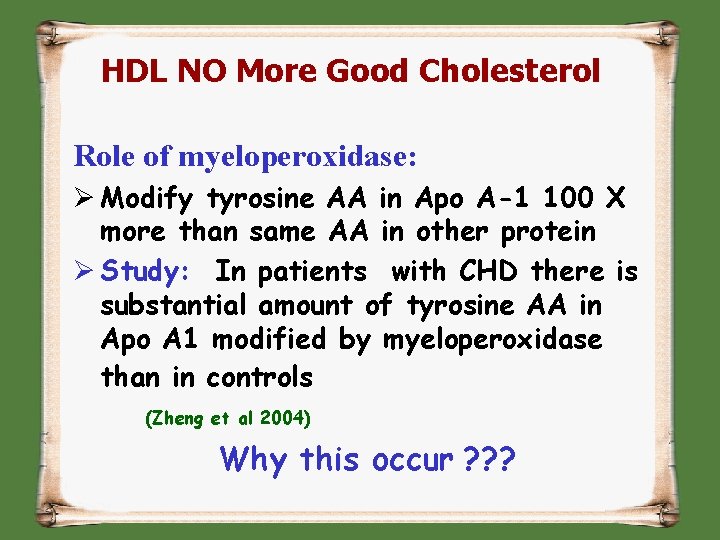
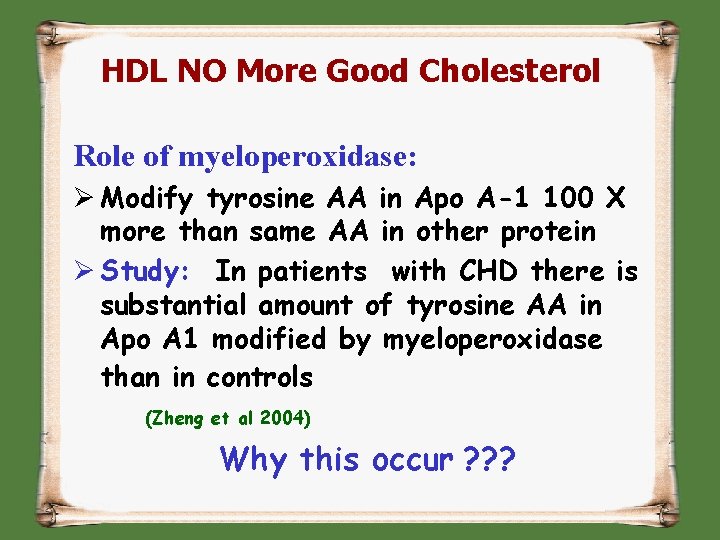
HDL NO More Good Cholesterol Role of myeloperoxidase: Ø Modify tyrosine AA in Apo A-1 100 X more than same AA in other protein Ø Study: In patients with CHD there is substantial amount of tyrosine AA in Apo A 1 modified by myeloperoxidase than in controls (Zheng et al 2004) Why this occur ? ? ?
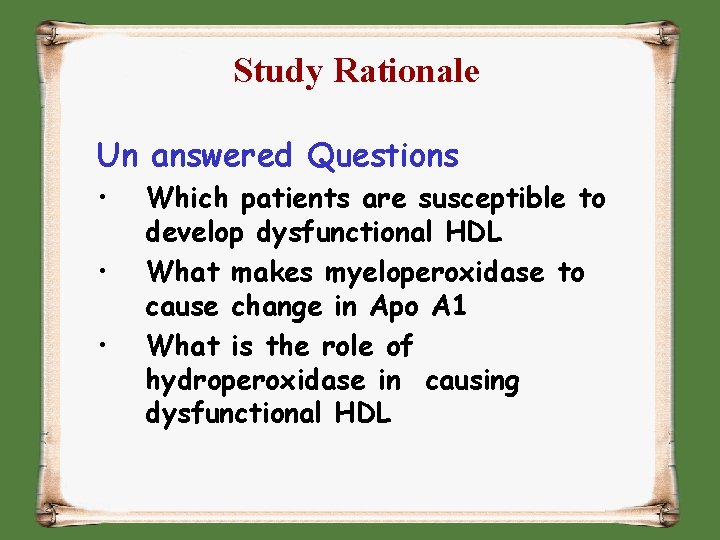
Study Rationale Un answered Questions • • • Which patients are susceptible to develop dysfunctional HDL What makes myeloperoxidase to cause change in Apo A 1 What is the role of hydroperoxidase in causing dysfunctional HDL
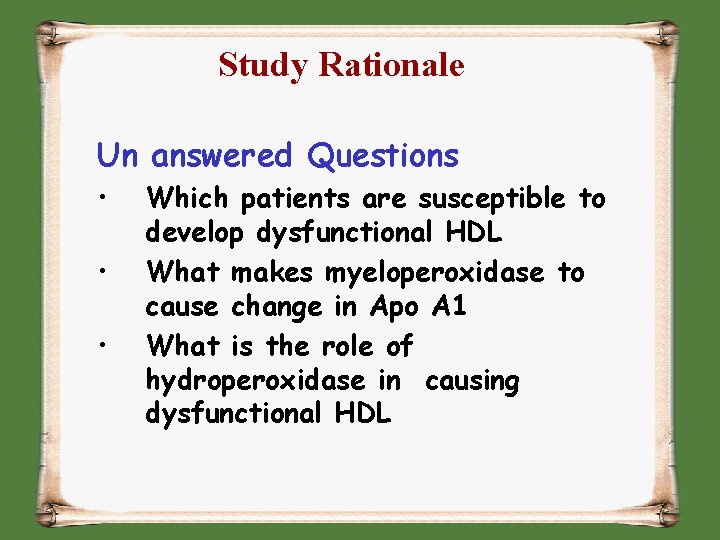
Study Rationale Un answered Questions • • • Which patients are susceptible to develop dysfunctional HDL What makes myeloperoxidase to cause change in Apo A 1 What is the role of hydroperoxidase in causing dysfunctional HDL
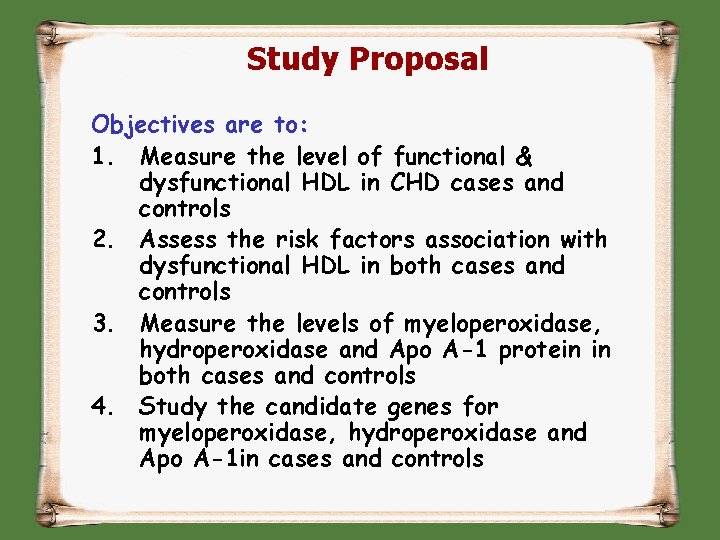
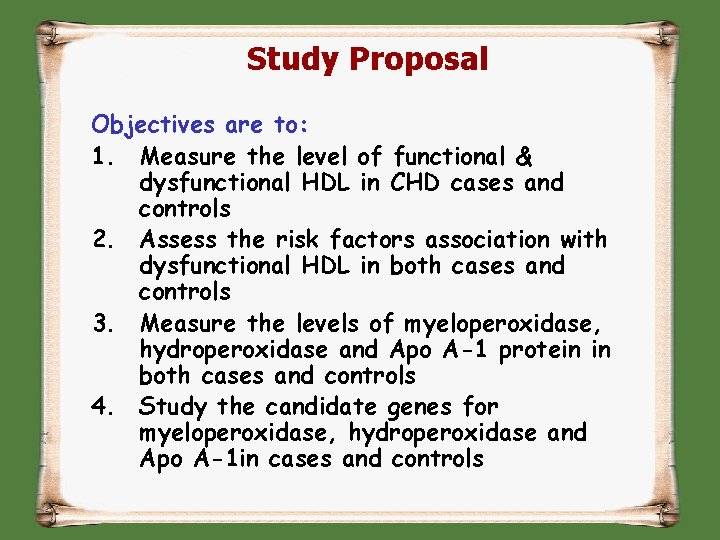
Study Proposal Objectives are to: 1. Measure the level of functional & dysfunctional HDL in CHD cases and controls 2. Assess the risk factors association with dysfunctional HDL in both cases and controls 3. Measure the levels of myeloperoxidase, hydroperoxidase and Apo A-1 protein in both cases and controls 4. Study the candidate genes for myeloperoxidase, hydroperoxidase and Apo A-1 in cases and controls
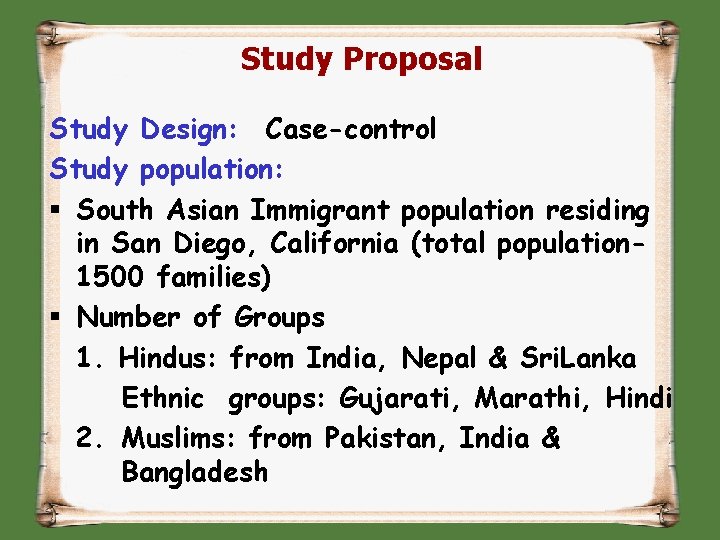
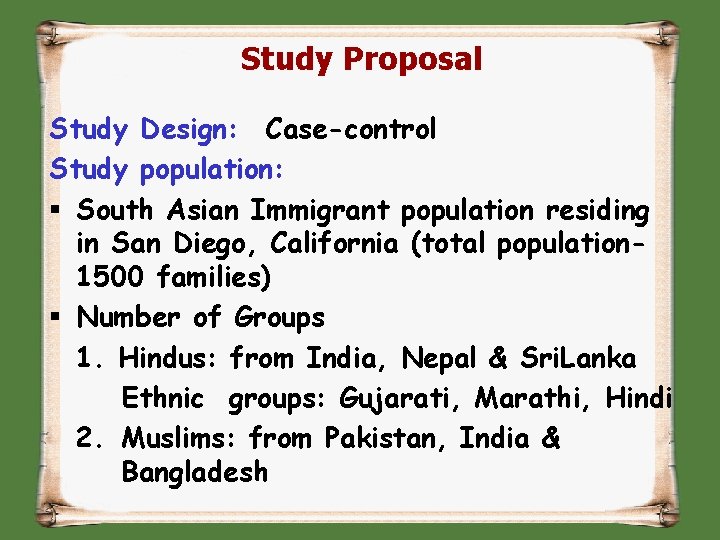
Study Proposal Study Design: Case-control Study population: § South Asian Immigrant population residing in San Diego, California (total population 1500 families) § Number of Groups 1. Hindus: from India, Nepal & Sri. Lanka Ethnic groups: Gujarati, Marathi, Hindi 2. Muslims: from Pakistan, India & Bangladesh
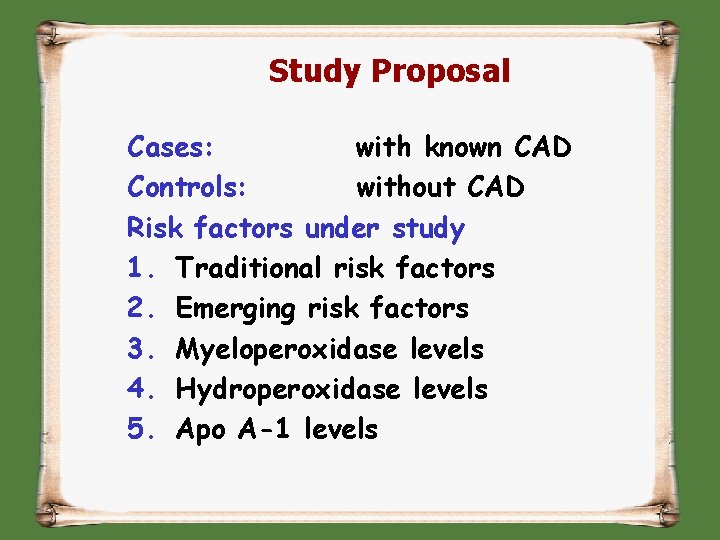
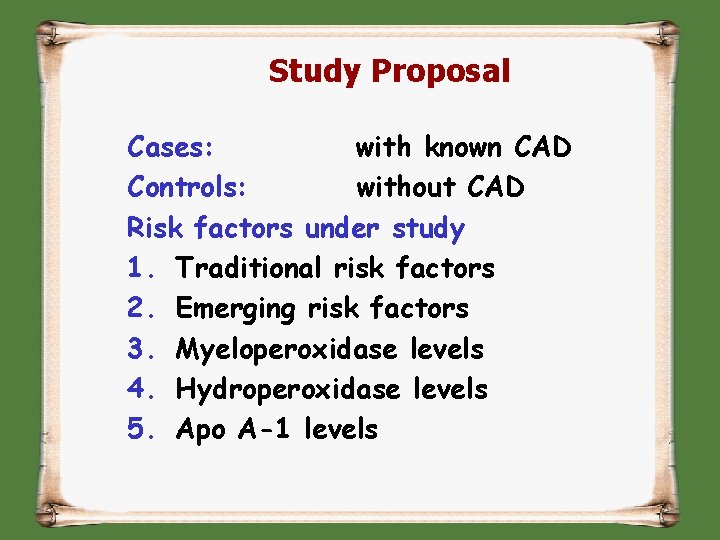
Study Proposal Cases: with known CAD Controls: without CAD Risk factors under study 1. Traditional risk factors 2. Emerging risk factors 3. Myeloperoxidase levels 4. Hydroperoxidase levels 5. Apo A-1 levels

Study Proposal Sample size: Biostatistician Data analysis: Multiple logistic regression
 Good and bad cholesterol
Good and bad cholesterol Good and bad cholesterol
Good and bad cholesterol Nothing compares to your embrace
Nothing compares to your embrace Zoroastrianism good thoughts good words good deeds
Zoroastrianism good thoughts good words good deeds Hello teacher good afternoon
Hello teacher good afternoon Hi hi good morning video
Hi hi good morning video Good afternoon students
Good afternoon students Hdl ldl
Hdl ldl Lenguajes de descripción de hardware
Lenguajes de descripción de hardware Procedural statement
Procedural statement Hdl formation
Hdl formation Chisel hdl
Chisel hdl Hdl survival guide
Hdl survival guide Low hdl
Low hdl Pediatra salim bergamo
Pediatra salim bergamo Hdl designer tutorial
Hdl designer tutorial Hdl genesys
Hdl genesys Hdl level
Hdl level Hdl-mhrcu.433
Hdl-mhrcu.433 Vhdl generic mux
Vhdl generic mux Circolazione enteroepatica
Circolazione enteroepatica Buspro
Buspro Hdl-mcip-rf02.10
Hdl-mcip-rf02.10 Port mapping in verilog
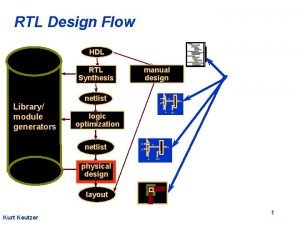
Port mapping in verilog Rtl design flow
Rtl design flow Advanced digital design with the verilog hdl
Advanced digital design with the verilog hdl Verilog hdl: a guide to digital design and synthesis
Verilog hdl: a guide to digital design and synthesis Vhdl hardware description language
Vhdl hardware description language Abel hdl
Abel hdl A stepper motor hdl application must include
A stepper motor hdl application must include Hdl knx
Hdl knx Ram16 hdl
Ram16 hdl Hdl code
Hdl code Hdl is
Hdl is Hdl normal range
Hdl normal range Verilog
Verilog Fungsi hdl
Fungsi hdl Hdl ldl
Hdl ldl Verilog vs vhdl
Verilog vs vhdl Language
Language Hdl level
Hdl level Hdl tomato soup
Hdl tomato soup Hdl-mbus01ip.431
Hdl-mbus01ip.431 Verilog hdl
Verilog hdl Verilog hdl: a guide to digital design and synthesis pdf
Verilog hdl: a guide to digital design and synthesis pdf Hdl vhdl
Hdl vhdl Colesterol hdl
Colesterol hdl Cholesterol total
Cholesterol total What are the 4 macromolecules
What are the 4 macromolecules A dietitian wishes to see if a person's cholesterol
A dietitian wishes to see if a person's cholesterol Function of cholesterol
Function of cholesterol