GIT Pathology Dr Somaya Taha Saleem GIT Pathology
- Slides: 57
GIT Pathology Dr. Somaya Taha Saleem
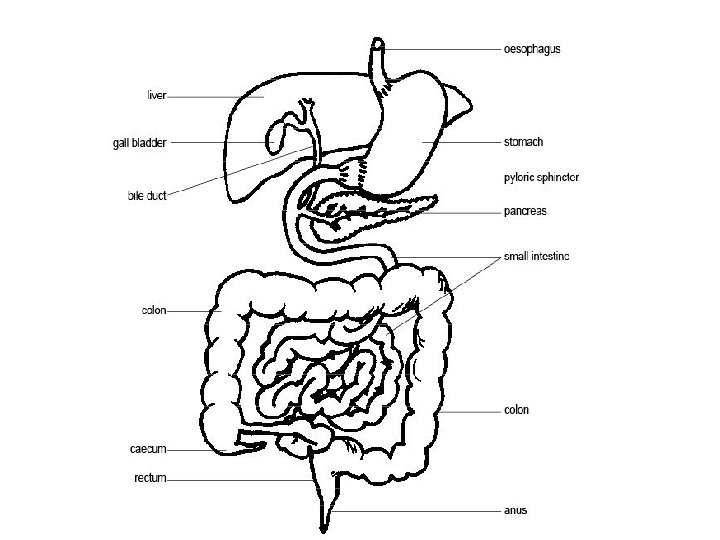
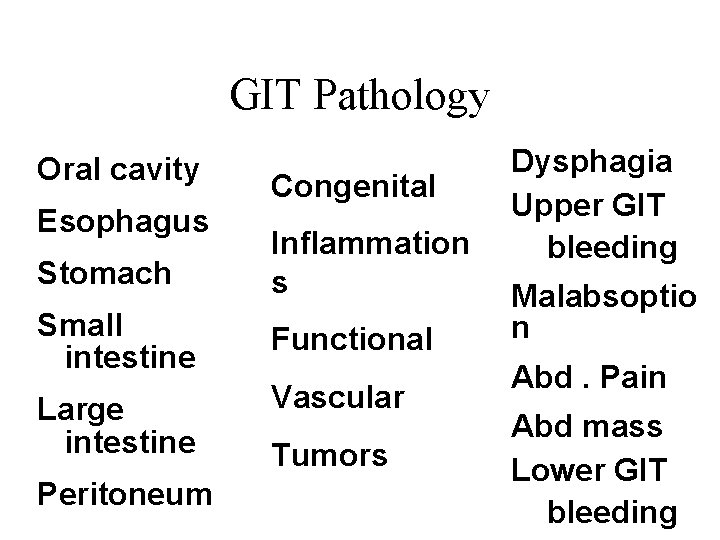
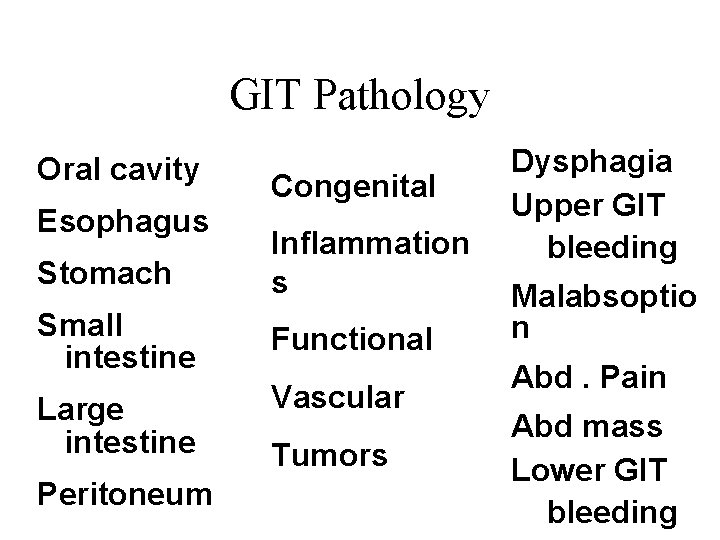
GIT Pathology Oral cavity Esophagus Congenital Stomach Inflammation s Small intestine Functional Large intestine Vascular Peritoneum Tumors Dysphagia Upper GIT bleeding Malabsoptio n Abd. Pain Abd mass Lower GIT bleeding
Key Concepts • Diseases of the gastrointestinal tract and its accessory organs interrupt the body’s normal cycle of digestion, absorption, and metabolism.
Disorders of Oral Cavity and Salivary Glands • Tongue and oral cavity nodules/ulcers. • Tongue and oral cavity plaques. • Parotid gland swelling.
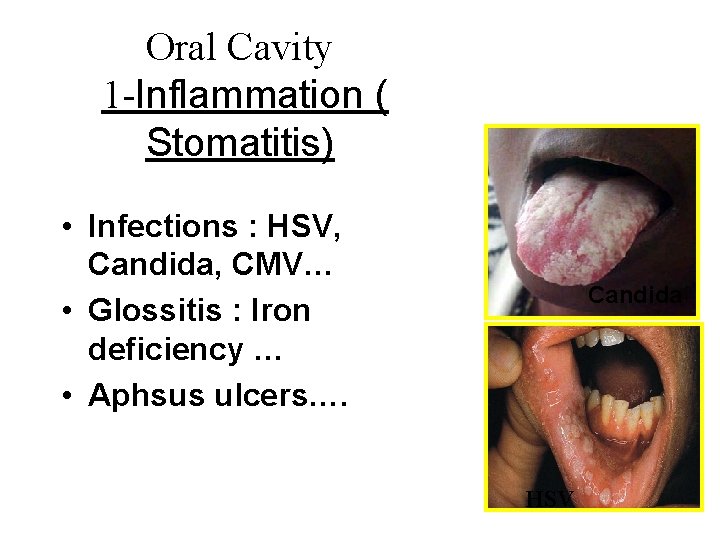
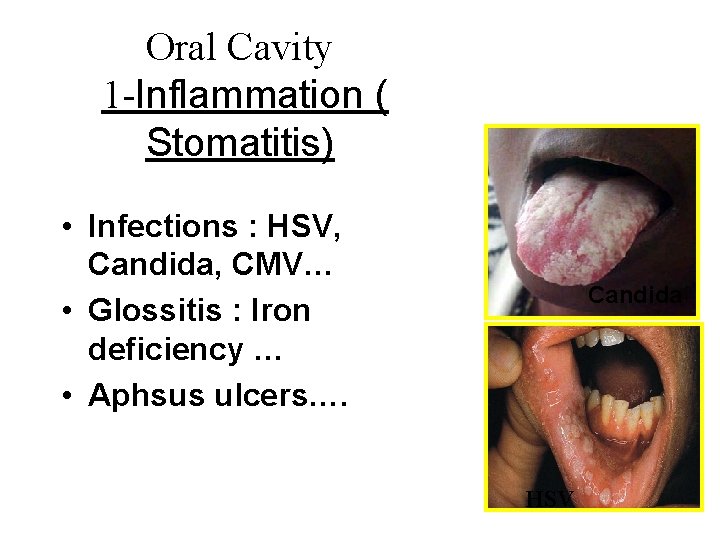
Oral Cavity 1 -Inflammation ( Stomatitis) • Infections : HSV, Candida, CMV… • Glossitis : Iron deficiency … • Aphsus ulcers…. Candida HSV
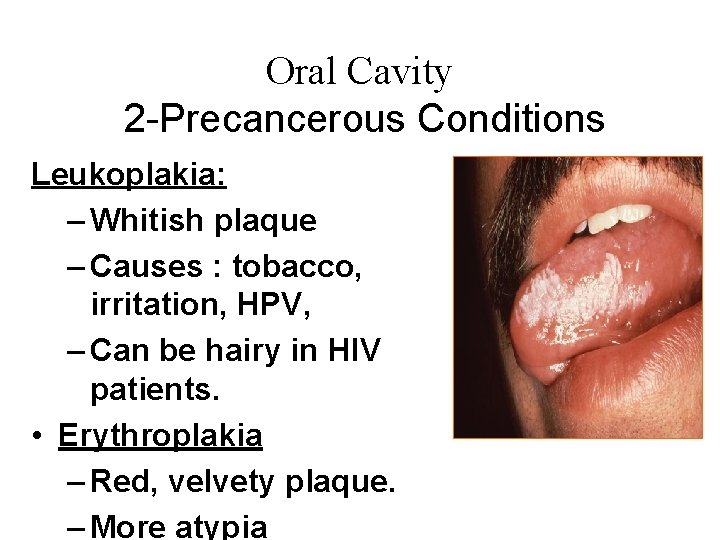
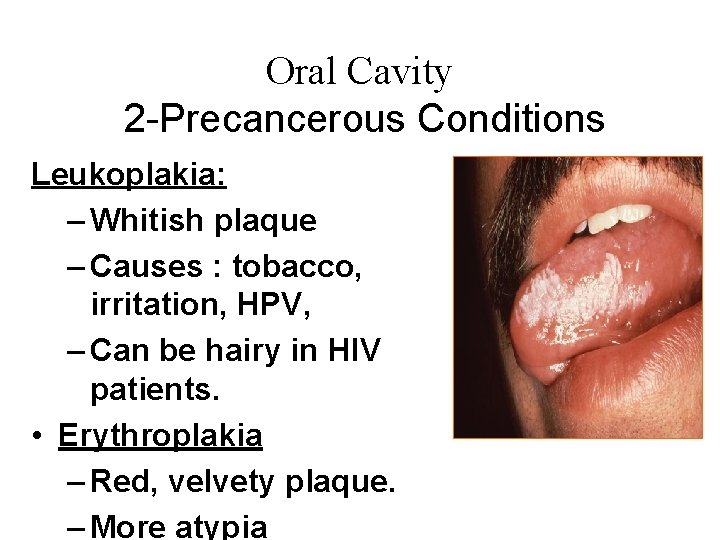
Oral Cavity 2 -Precancerous Conditions Leukoplakia: – Whitish plaque – Causes : tobacco, irritation, HPV, – Can be hairy in HIV patients. • Erythroplakia – Red, velvety plaque. – More atypia
3 -Oral Cavity Tumors Odentogenic tumors (Teeth) – Ameloblastoma – Odentoma – Others Squamous cell carcinoma • Causes: tobacco, HPV, genetic • Pathology: S site: anterior 1/3 of tongue, floor , lip S Shape : nodule or ulcer with everted edge S Well differentiated SSC
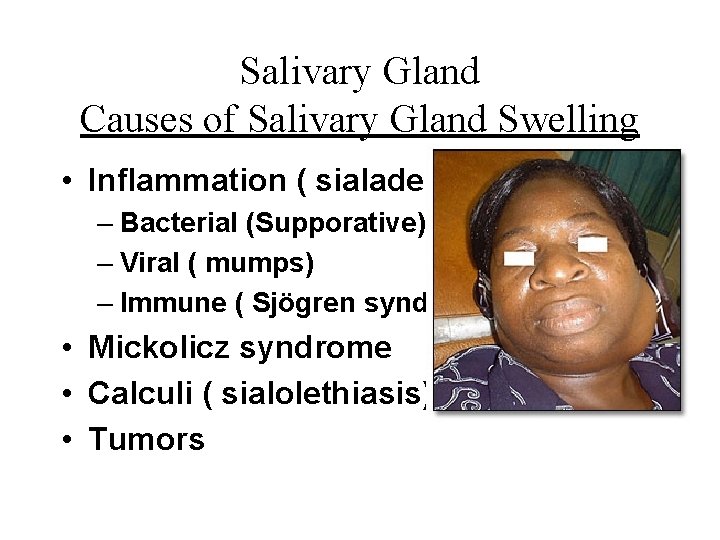
Salivary Gland Causes of Salivary Gland Swelling • Inflammation ( sialadenitis) – Bacterial (Supporative) – Viral ( mumps) – Immune ( Sjögren syndrome) • Mickolicz syndrome • Calculi ( sialolethiasis) • Tumors
Salivary gland Tumors Benign Tumors : • Pleomorphic adenoma – Called mixed salivary tumor – The most common( 65%) – Mainly in parotid gland – Micro: mixed cell types – Recur after surgery • Warthin tumor ( adenolymphoma) • Oncocytoma
Salivary Gland Tumors Malignant tumors • Adenocarcinoma (10%) • Mucoepidermoid Ca (15%) • Acinic cell Ca (5%) • Adenoid cystic carcinoma • Others
Oesophagus • Epithelium lined muscular tube from 6 th cervical – 11 th thoracic vertebra Function: • Conduction of food and drink • Sphincters at top and bottom
Clinical features • Heartburn (retrosternal burning pain) • Dysphagia (difficulty in swallowing) • Inflammation • pain • Hematemesis – (vomiting of blood)
Diseases are subdivided into: • Congenital • Mechanical disorders • Inflammation • Esophageal varices • Oesophageal neoplasms
Congenital • Ectopic tissue rest (e. g. gastric mucosa in the upper third of the esophagus) • Atresia – often with fistula to trachea (a segment of the esophagus is represented by only a thin , noncanalised cord, with a proximal blind pouch connected to the pharynx and a lower pouch leading to the stomach. • Tracheoesophageal fistula.
• Oesophageal ring (concentric plates of tissue protruding into the lumen of the distal oesophagous. • Oesophageal webs (ledge like protrusions of the mucosa into the oesophageal lumen ) • Duplication.
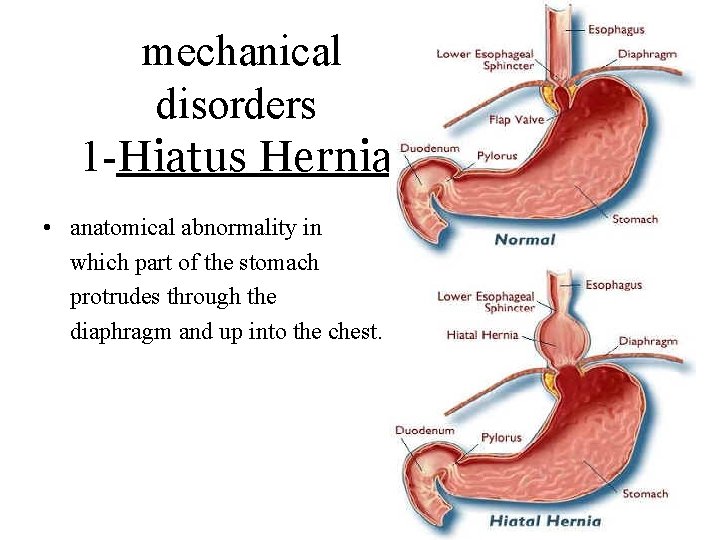
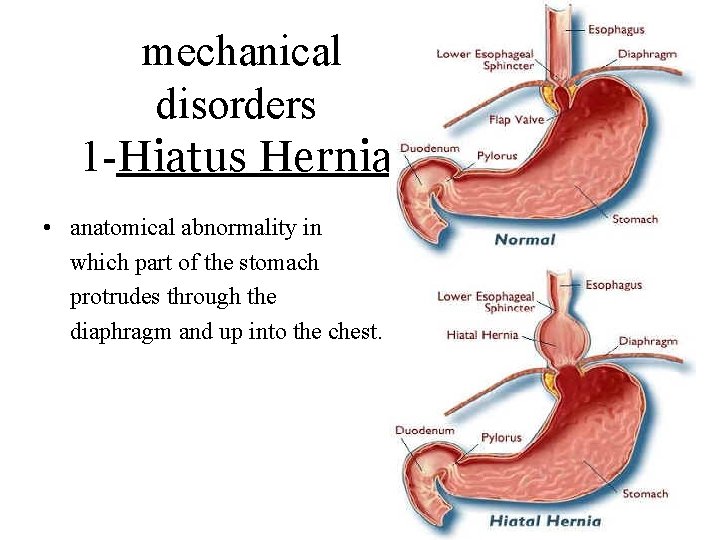
mechanical disorders 1 -Hiatus Hernia • anatomical abnormality in which part of the stomach protrudes through the diaphragm and up into the chest.
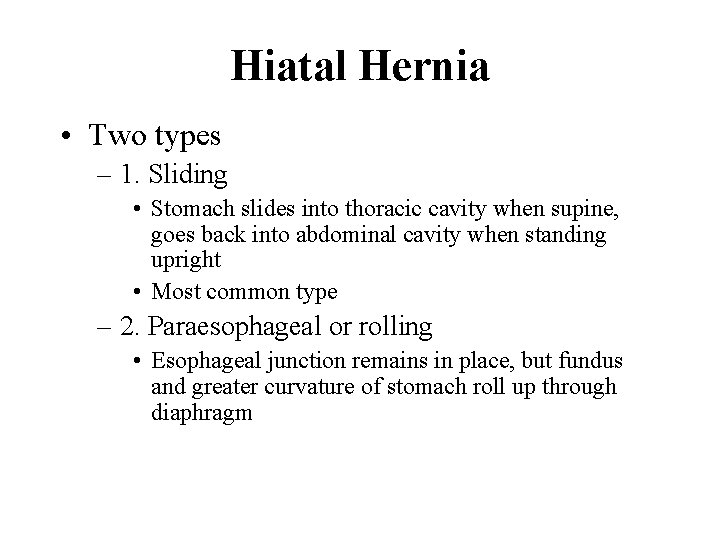
Hiatal Hernia • Two types – 1. Sliding • Stomach slides into thoracic cavity when supine, goes back into abdominal cavity when standing upright • Most common type – 2. Paraesophageal or rolling • Esophageal junction remains in place, but fundus and greater curvature of stomach roll up through diaphragm
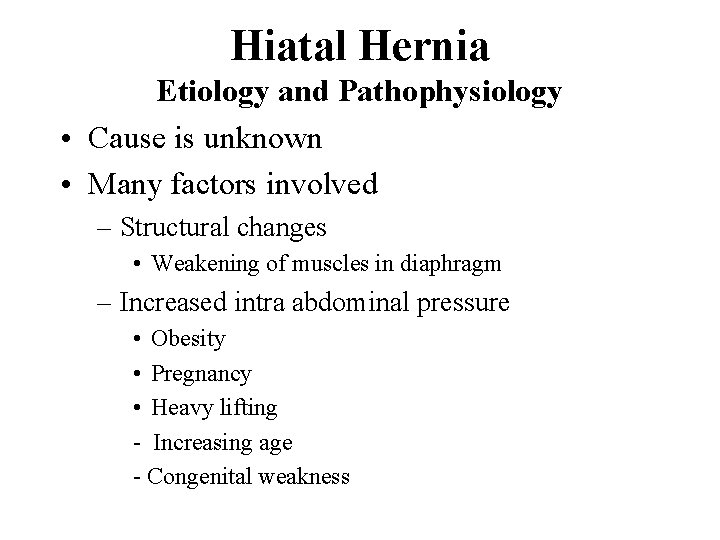
Hiatal Hernia Etiology and Pathophysiology • Cause is unknown • Many factors involved – Structural changes • Weakening of muscles in diaphragm – Increased intra abdominal pressure • Obesity • Pregnancy • Heavy lifting - Increasing age - Congenital weakness
Clinical Manifestations : • Most common abnormality found x-ray of upper GI • More common in older adults and in women • May be asymptomatic • Symptoms include – Heartburn • After meal or lying supine – Dysphagia Diagnosis : – Barium swallow – Endoscopy
Complications • • • GERD Esophagitis Hemorrhage from erosion Stenosis Ulcerations of herniated portion Strangulation of hernia
Achalasia – Motility disorder characterised by absence of oesophageal failure of lower oesophageal sphincter to relax on swallowing’ – decrease or loss of myenteric ganglion cells. - All age , majority between 20 to 40 years – Dysphagia for solids mainly. – Regurgitation (60%-90%), – chest pain (50% -75%), – weight loss, – recurrent aspiration.
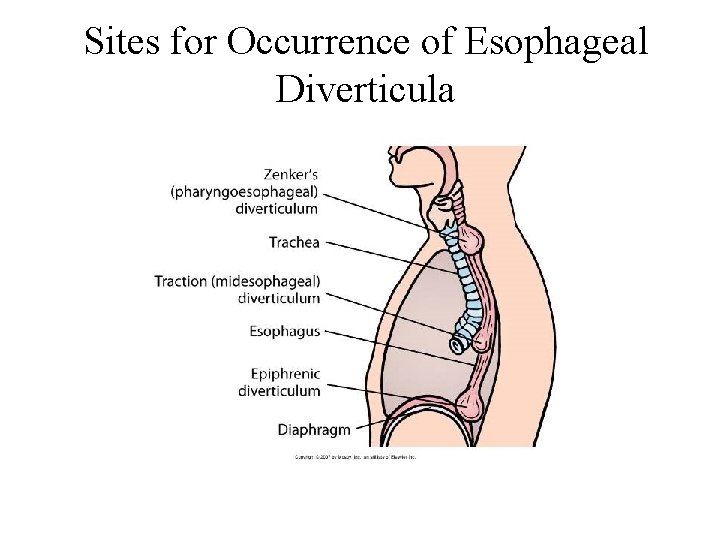
Esophageal Diverticula outpouching of the alimentary tract ( true contains all visceral layers , false diverticulum contains mucosa and submucosa only ) • Occur in three main areas – Zenker’s diverticulum • Most common location (immediately above UES), – Traction diverticulum • Near esophageal midpoint – Epiphrenic diverticulum • Above the LES
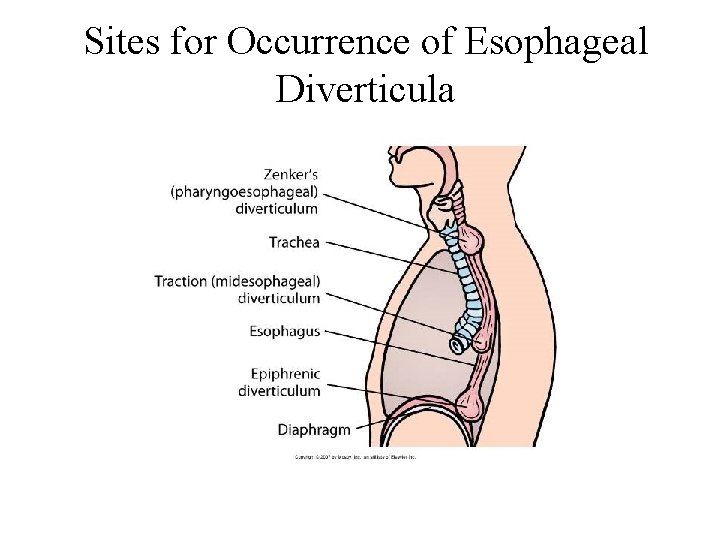
Sites for Occurrence of Esophageal Diverticula
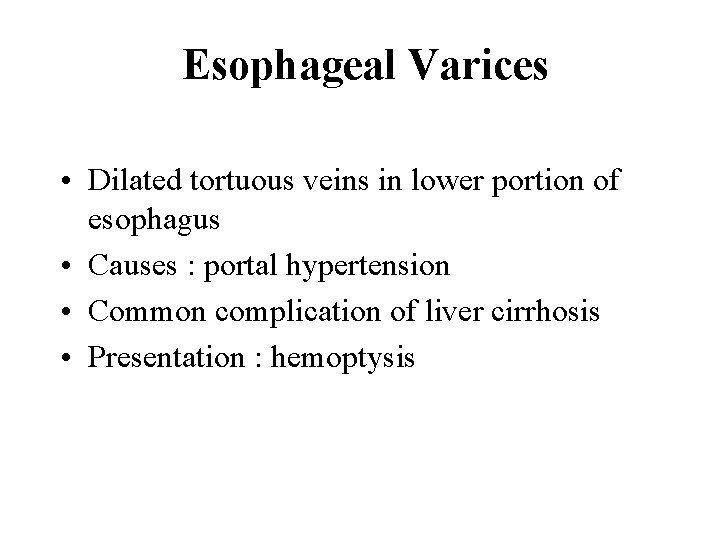
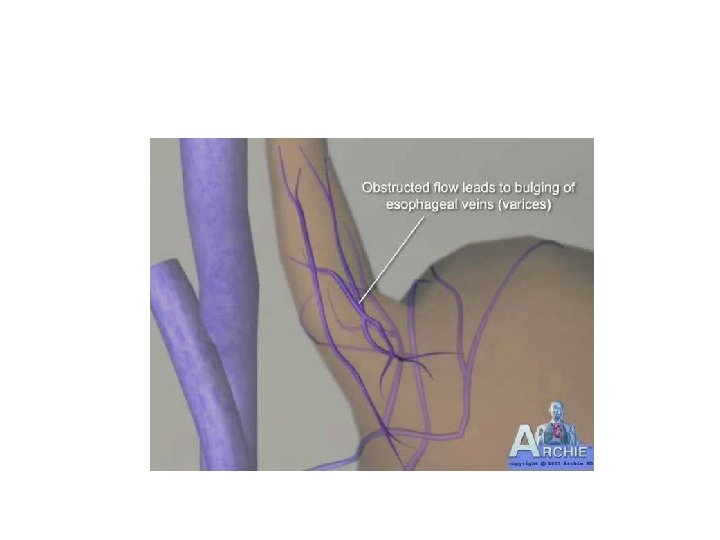
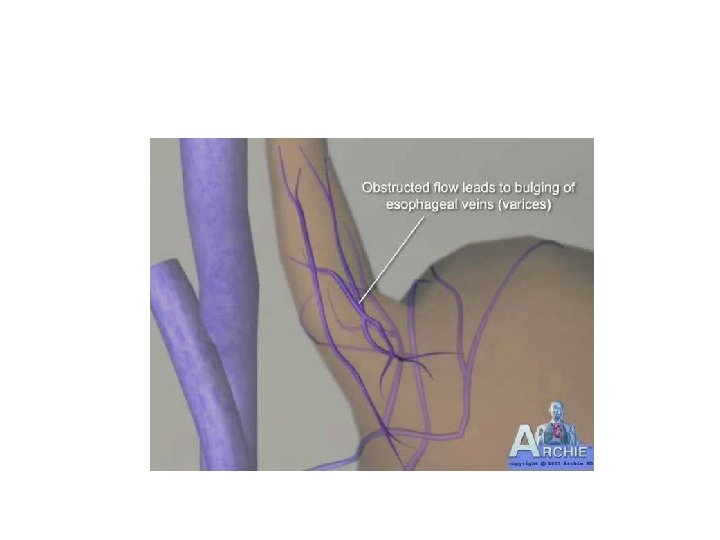
Esophageal Varices • Dilated tortuous veins in lower portion of esophagus • Causes : portal hypertension • Common complication of liver cirrhosis • Presentation : hemoptysis
Inflammation (esophagitis) • Acute infective – Herpes virus, Candida. Both seen most commonly in immunosuppressed. • Ingestion of corrosives • Chronic reflux through lower oesophageal sphincter
Gastroesophageal reflux disease (GERD) Caused by constant regurgitation of acid gastric contents into lower esophagus – Risk factors : Pregnancy, obesity, vomiting, or nasogastric tubes – Constant irritation and inflammation (esophagitis) – Stenosis most common complication • Classic symptom of GERD: frequent and severe heartburn
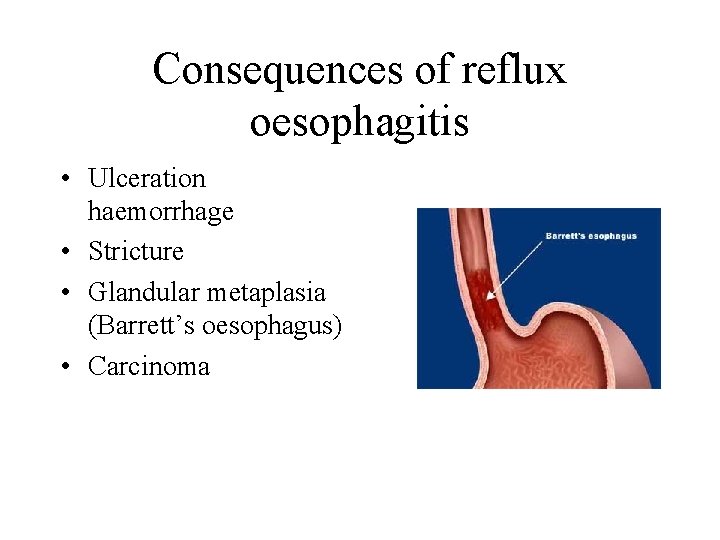
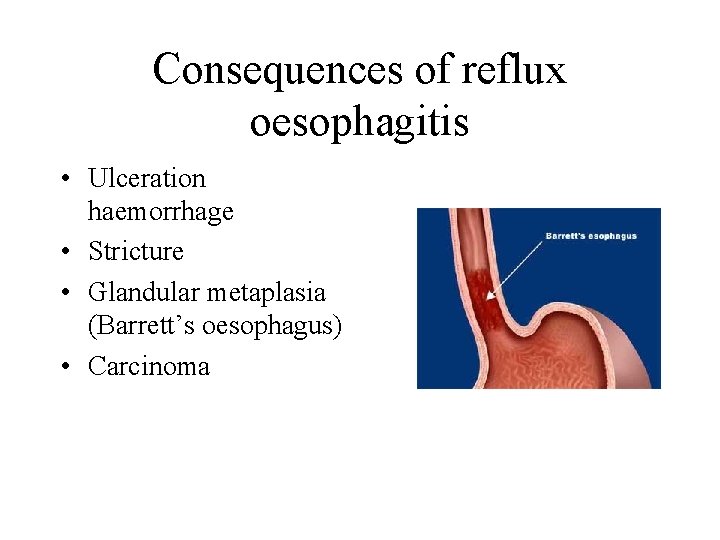
Consequences of reflux oesophagitis • Ulceration haemorrhage • Stricture • Glandular metaplasia (Barrett’s oesophagus) • Carcinoma
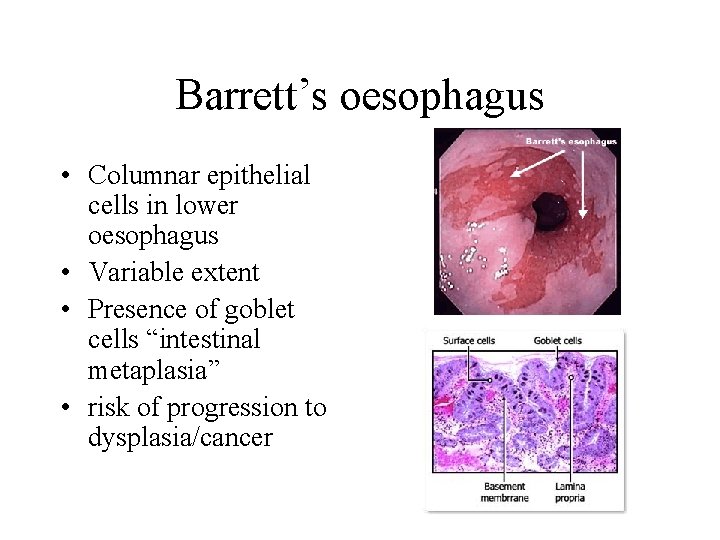
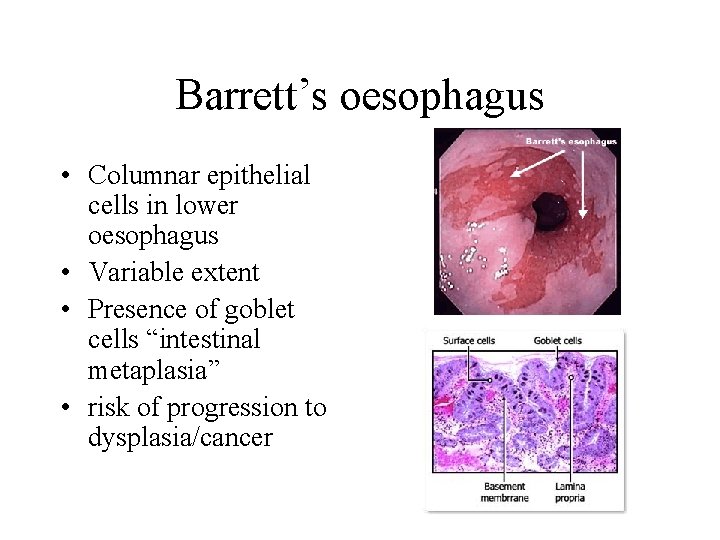
Barrett’s oesophagus • Columnar epithelial cells in lower oesophagus • Variable extent • Presence of goblet cells “intestinal metaplasia” • risk of progression to dysplasia/cancer
Oesophageal neoplasms • Benign tumours (rare): • Malignant tumours Presenting symptom - dysphagia
Oesophagus neoplasm • Benign tumours; Leiomyoma, squamous papilloma , fibrous polyp, lipoma, haemagioma, etc • Malignant tumours; – Carcinoma, Squamous carcinoma, Adenocarcinoma leiomyosarcoma, fibrosarcoma, melanoma
Carcinoma of oesophagus • Risk factors; alcohol, tobacco, vitamin and mineral deficiency, strong family history, multiple cancers, especially head and neck cancers, corrosive esophagitis, Barrett’s esophagus, achalasia, Plummer-Vinson syndrome
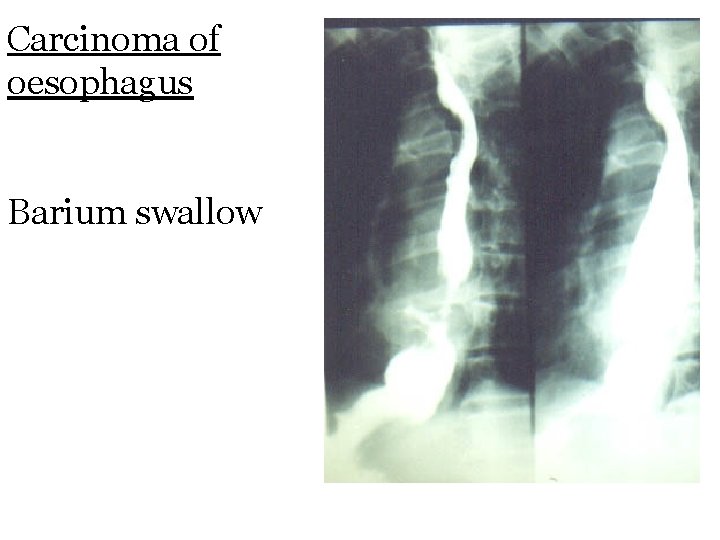
Carcinoma of oesophagus • S&S; None, dysphagia, wt. Loss, chest pain, retrosternal pain, feeling of obstruction, hemoptysis. • 5 year survival rate is 6%-9% • Assessment; Radiologic: plain and Barium studies, CT scan, MRI • Endoscopy; rigid and flexible, endoscopic ultrasound
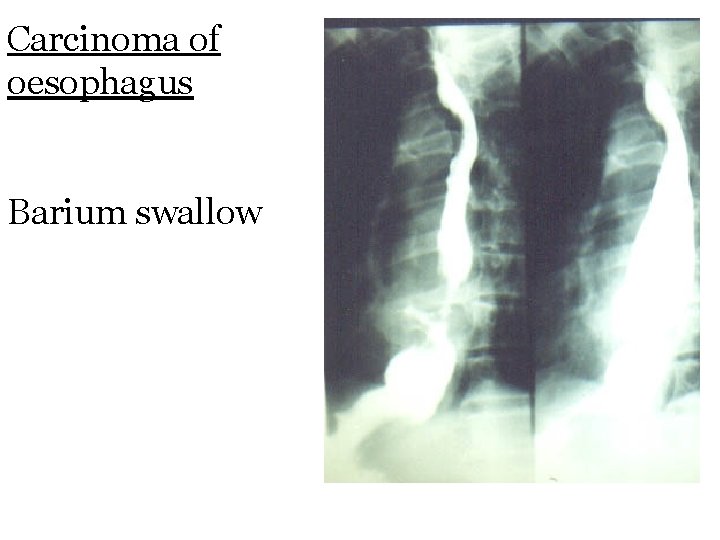
Carcinoma of oesophagus Barium swallow
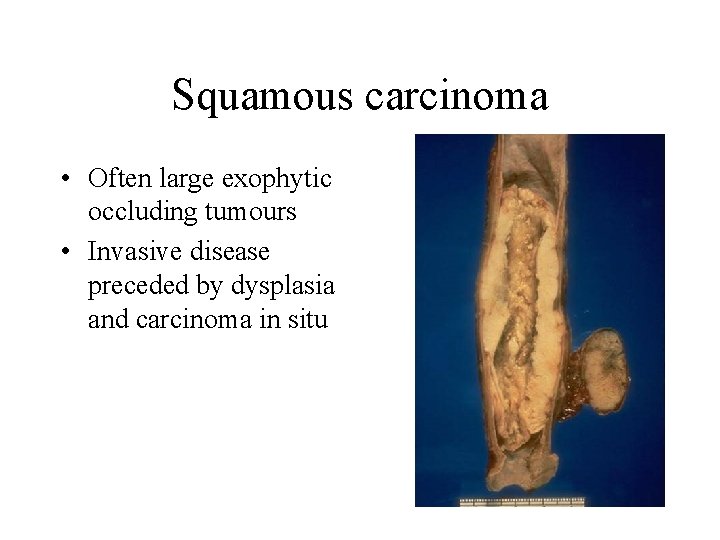
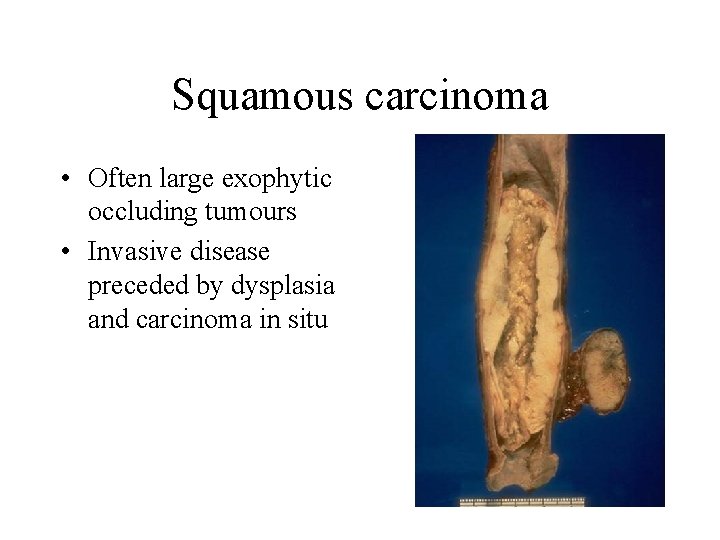
Squamous carcinoma • Often large exophytic occluding tumours • Invasive disease preceded by dysplasia and carcinoma in situ
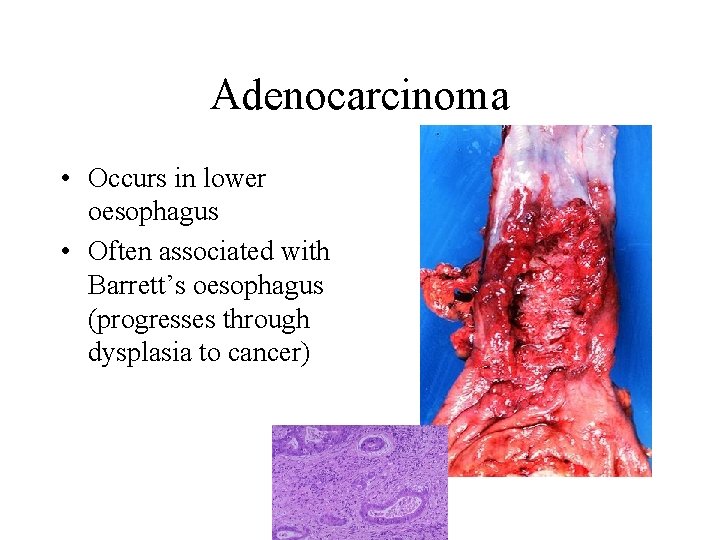
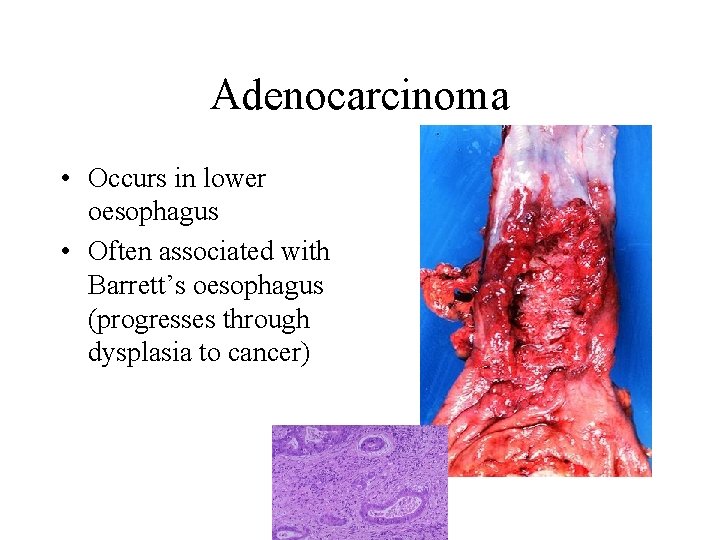
Adenocarcinoma • Occurs in lower oesophagus • Often associated with Barrett’s oesophagus (progresses through dysplasia to cancer)
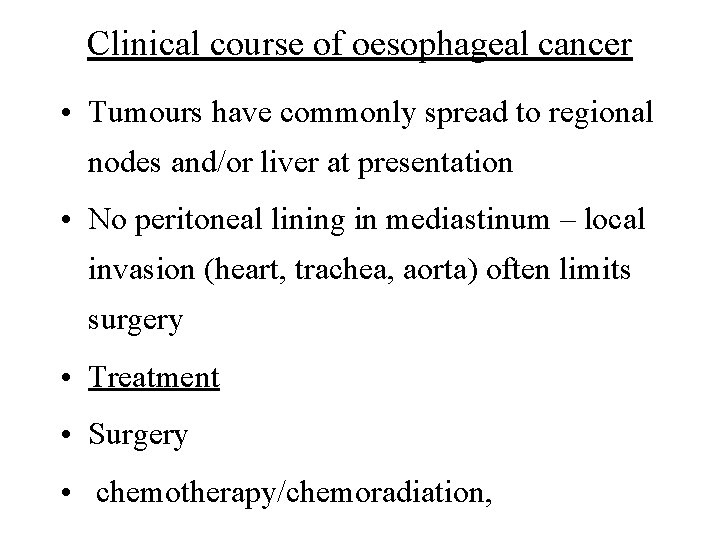
Clinical course of oesophageal cancer • Tumours have commonly spread to regional nodes and/or liver at presentation • No peritoneal lining in mediastinum – local invasion (heart, trachea, aorta) often limits surgery • Treatment • Surgery • chemotherapy/chemoradiation,
DISEASES OF STOMACH
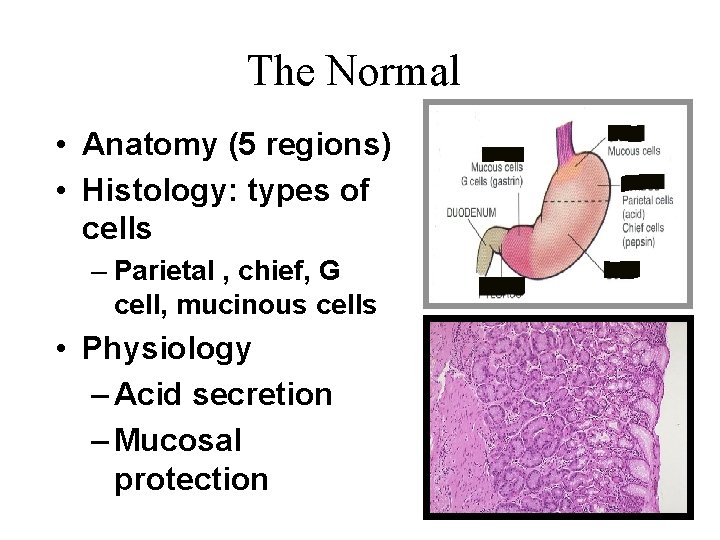
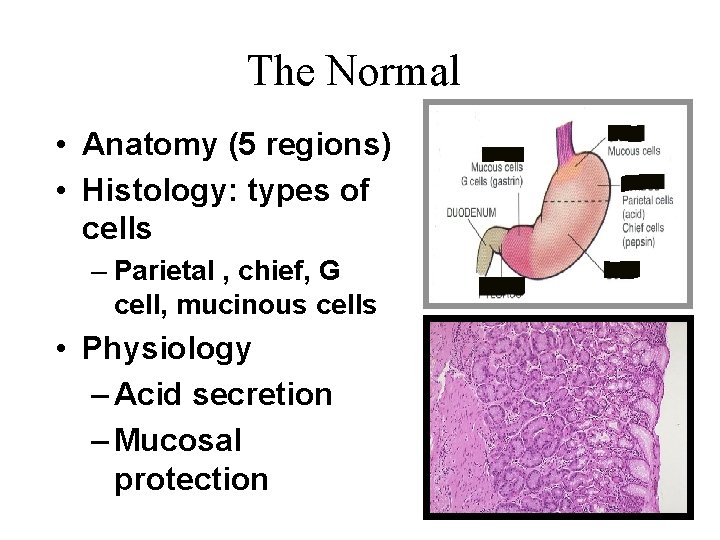
The Normal • Anatomy (5 regions) • Histology: types of cells – Parietal , chief, G cell, mucinous cells • Physiology – Acid secretion – Mucosal protection
Gastric Disorders • Congenital anomalies – Hernia – Heterotopia: pancreatic tissue in stomach – Congenital Pyloric Stenosis • Gastritis • Peptic ulcers diseases • Gastric tumors
GASTRITIS • ACUTE • CHRONIC • AUTOIMMUNE
1 - Gastritis • Inflammation of the gastric mucosa • Types : Acute, chronic Acute gastritis • Causes: – NSADs (Aspirin) – Alcohol, diet, smoking, …. • Pathology: – Hyperemia, neutrophils, odema, errosion
Acute Gastritis Acute mucosal inflammatory process, usually of a transient nature. is an important cause of acute gastrointestinal bleeding. 1. Epigastric pain with 2. dyspepsia , nausea and vomiting. 3. Hematemesis coffee ground vomiting, Melina
Chronic Gastritis: Presence of chronic inflammatory changes in the mucosa leading eventually to mucosal atrophy and epithelial metaplasia. Types of Chronic Gastritis: • A – autoimmune - type A • B – bacterial (helicobacter)- type B • C – chemical- type C
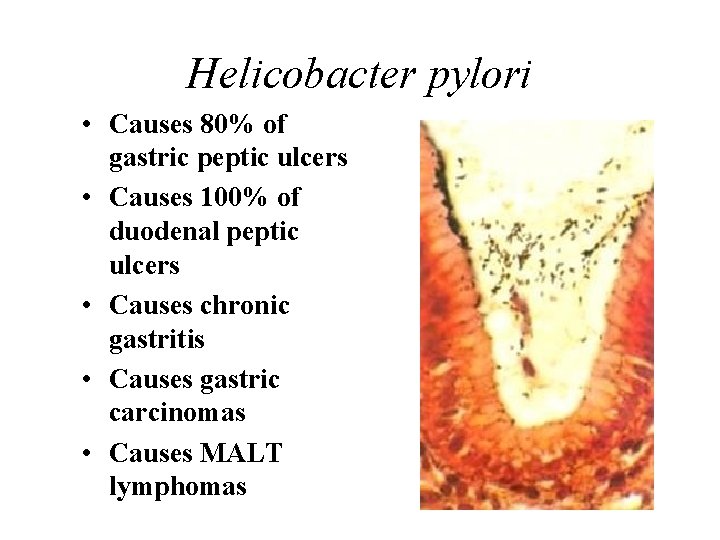
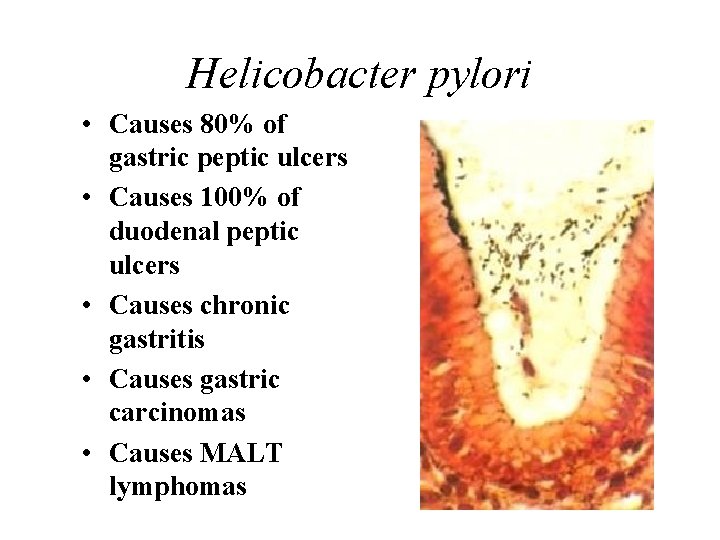
Helicobacter pylori • Causes 80% of gastric peptic ulcers • Causes 100% of duodenal peptic ulcers • Causes chronic gastritis • Causes gastric carcinomas • Causes MALT lymphomas
Clinical Features 1. Upper abdominal discomfort 2. Nausea 3. Vomiting. 4. When severe parietal cell loss occurs in autoimmune gastritis, 5. Development of peptic ulcer and gastric carcinoma.
Consequences of gastritis • Peptic ulcer disease (Helicobacter) • Adenocarcinoma (all types)
Peptic ulcer disease • A surface breach of mucosal lining of GI tract occurring as a result of acid and pepsin attack • Sites: – Duodenum (DU) – Stomach (GU) – Oesophagus Acute & Chronic peptic ulcer
Acute gastric ulcer • Called gastric erosion • Causes: – NSADs ( Asprin) – Stress ( burn) – head injery ( Curling ulcer)
Chronic Peptic Ulcers Chronic , often solitary, lesions that occur in any portion of the gastrointestinal tract exposed to the aggressive action of acidic peptic juices. Male/female ratio for duodenal ulcers is about 3: 1.
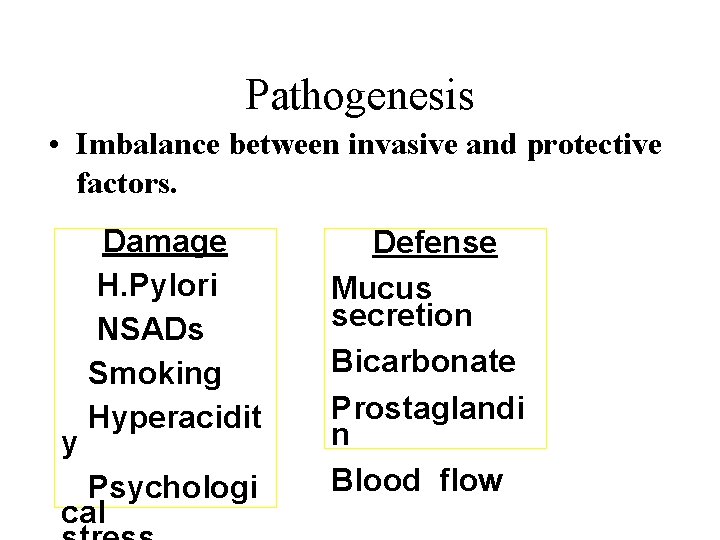
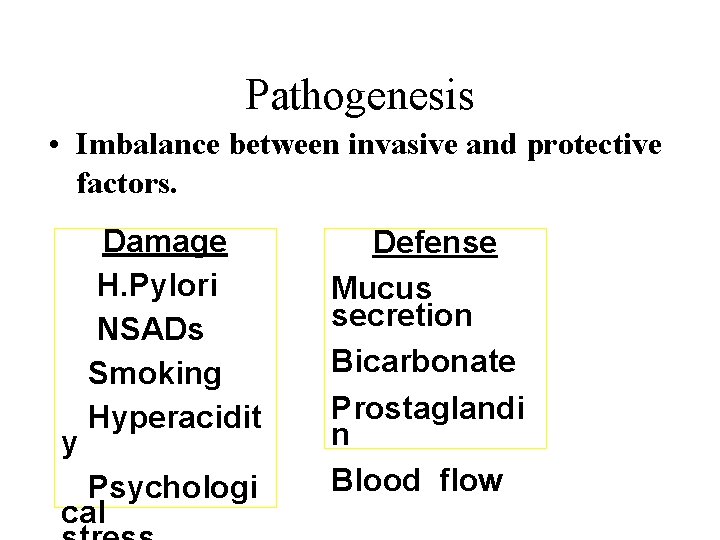
Pathogenesis • Imbalance between invasive and protective factors. y Damage H. Pylori NSADs Smoking Hyperacidit Psychologi cal Defense Mucus secretion Bicarbonate Prostaglandi n Blood flow
Clinical Features 1. Dyspepsia Epigastric pain. 2. Nausea, vomiting and significant weight loss. 3. Bleeding : coffee ground vomiting black stool ( melena)
Complications • Massive bleeding ( hypovolemia) • Chronic bleeding ( anemia) Perforation ( peritonitis) occurs in about 5% of patients. • Scaring ( hourglass deformity) • Malignant transformation, occurs in about 2% of patients.
GASTRIC TUMORS • BENIGN: – POLYPS (nodule or mass that projects above the level of the mucosa). – LEIOMYOMAS – LIPOMAS • MALIGNANT – ADENOCARCINOMA – LYMPHOMA
Treatment : Chemotherapy. Surgical removal.
Thank you