Respiratory System Diseases Dr Somaya Taha Saleem Respiratory
- Slides: 24
Respiratory System Diseases Dr. Somaya Taha Saleem
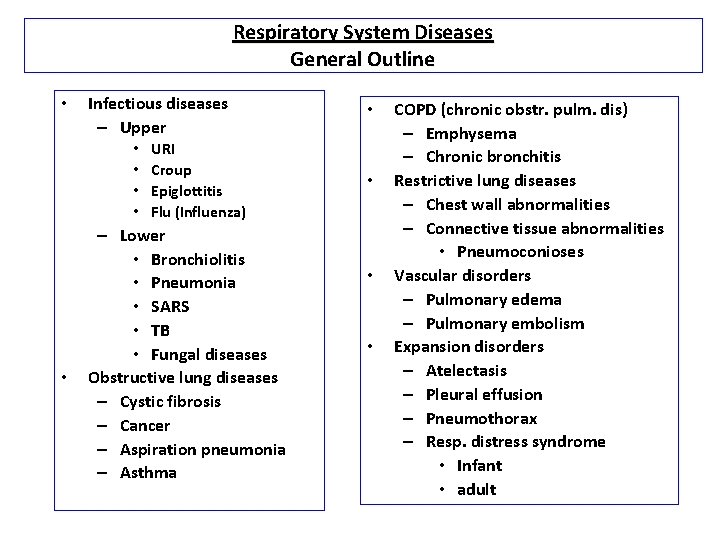
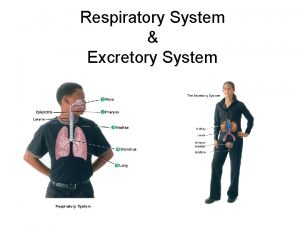
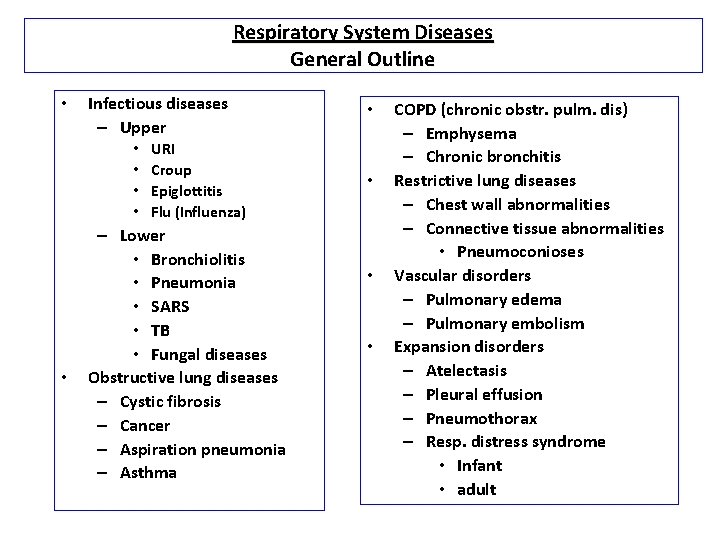
Respiratory System Diseases General Outline • Infectious diseases – Upper • • • URI Croup Epiglottitis Flu (Influenza) – Lower • Bronchiolitis • Pneumonia • SARS • TB • Fungal diseases Obstructive lung diseases – Cystic fibrosis – Cancer – Aspiration pneumonia – Asthma • • COPD (chronic obstr. pulm. dis) – Emphysema – Chronic bronchitis Restrictive lung diseases – Chest wall abnormalities – Connective tissue abnormalities • Pneumoconioses Vascular disorders – Pulmonary edema – Pulmonary embolism Expansion disorders – Atelectasis – Pleural effusion – Pneumothorax – Resp. distress syndrome • Infant • adult
pneumonia Definition : acute inflammatory process involving the alveolar tissue of the lung And associated with fever symptoms and signs in the chest and abnormalities in chest x ray
Pneumonia classification Etiological Infective – Viral – Bacterial – Fungal – Tuberculosis • Non Infective – Toxins – chemical – Aspiration Anatomical • Lobar • Broncho • Interstitial Duration: • Acute • Chronic
Pneumonia classification Most commonly community-acquired may be primary and secondary • Common etiologic agents are Streptococcus pneumoniae • Haemophilus influnzae Commonest in children <2 • Mycoplasma pneumoniae. • staphylococus aureus , Most common pneumonia following viral pneumonias • Klebsiella pneumonae • Pseudomonas aeruoinosa • Legionella pneumophilia Hospital acquired (nosocomial) more > 24 hrs after hospital admission.
Lobar Pneumonia: Def : inflammation of the lung with filling of the alveolar space with inflammatory exudate affecting the whole lobe Cause : 90% - Strep pneumonia , • Strep pyogens. (Klebsiella in aged, DM, alcoholics) Clinical features : • Young healthy adult • Fever, rigor, night sweating , Cough with or without sputum, dyspnea, Cyanosis , Chest pain , Hemoptysis • Slow shallow respiration
Lobar Pneumonia: Pathology : Four stages: (also in bronchopneumonia) 1 - Congestion 1 -2 days Macro : dark red , wet, congested lobe Micro : alveoli filled with clear fluid , congested capillaries vasodilatation. 2 - Red Hepatization 2 -4 days , Solid, red, granular lobe (liver) Exudation - RBC +fibrin 3 - Gray Hepatizaiton 4 -8 days - Firm , dry , gray (pale) lobe ( Fibrin , Macrophages Neutrophils & RBC). 4 - Resolution – – 8 -16 days , return to normal.
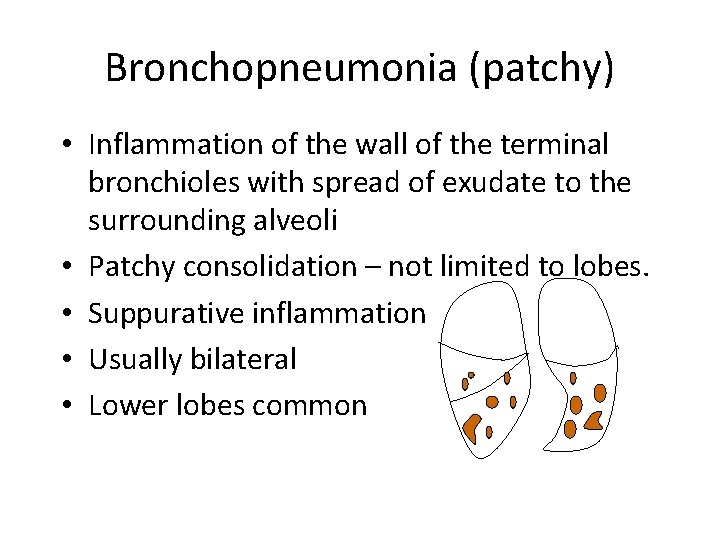
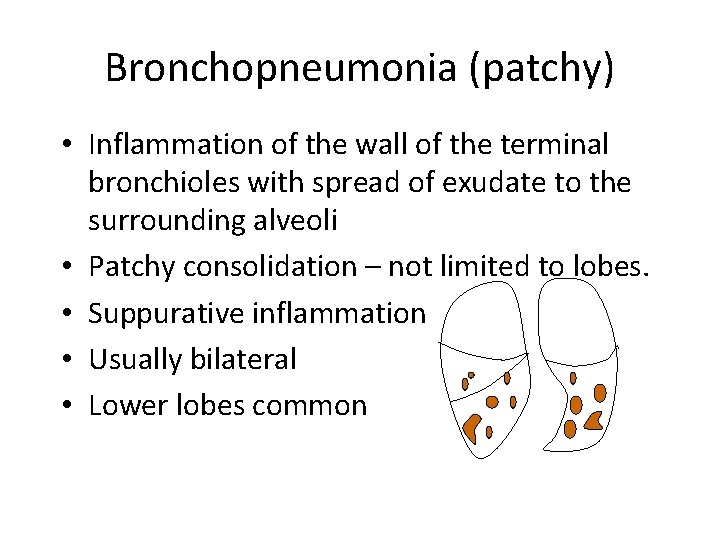
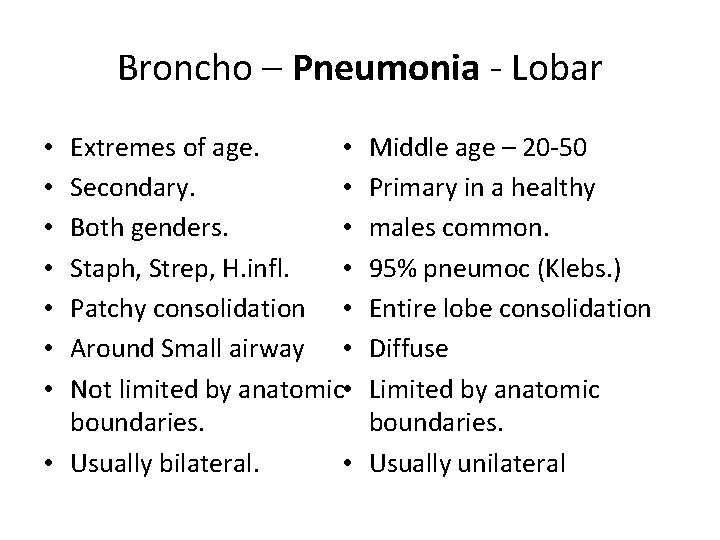
Bronchopneumonia (patchy) • Inflammation of the wall of the terminal bronchioles with spread of exudate to the surrounding alveoli • Patchy consolidation – not limited to lobes. • Suppurative inflammation • Usually bilateral • Lower lobes common
Bronchopneumonia (patchy) • Causes : - Staph, Strep, Pneumo & H. influenza • Clinical features: - Very young or very old patients Fever , vomiting , anorexia Abdominal and chest pain
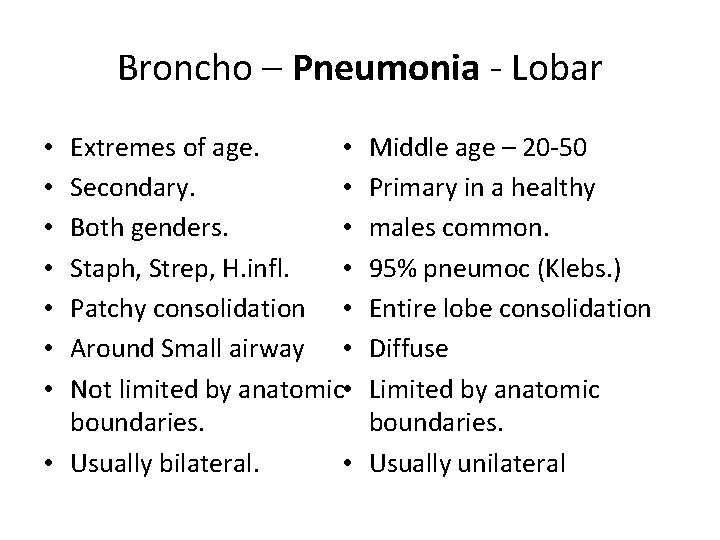
Broncho – Pneumonia - Lobar Extremes of age. • Secondary. • Both genders. • Staph, Strep, H. infl. • Patchy consolidation • Around Small airway • Not limited by anatomic • boundaries. • Usually bilateral. • • Middle age – 20 -50 Primary in a healthy males common. 95% pneumoc (Klebs. ) Entire lobe consolidation Diffuse Limited by anatomic boundaries. Usually unilateral
Complications Healing Organization and fibrosis Pleural effusion Lung abscess Empyema Septicemia Spread of infection
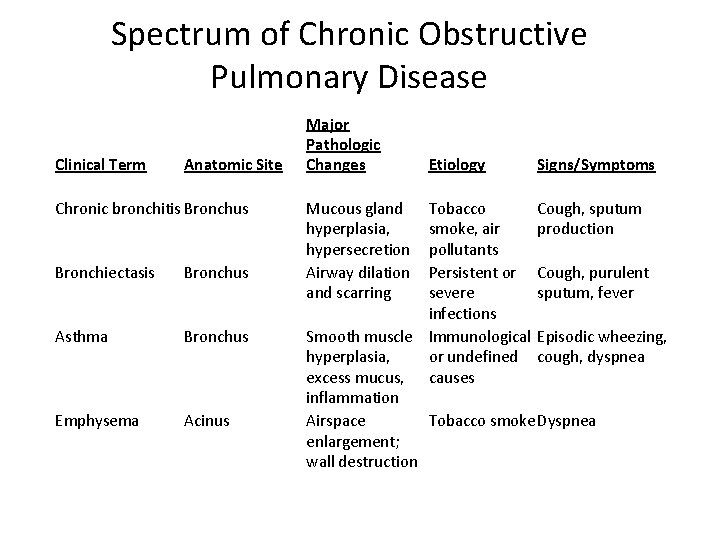
Chronic Obstructive Pulmonary Disease (COPD) • Irreversible progressive obstruction of air flow in lungs • Includes – (1) Chronic Bronchitis – (2) bronchiectasis) – (3) Emphysema – (4) Chronic asthma • General Treatment Plan • (1) broncodilators (2) mucolytic agents (3) expectorants ( 4) anti-inflammatories (5) antihistamines (6) antibiotics
Chronic bronchitis Definition : • Persistent cough with sputum production for at least 3 months in at least 2 consecutive years Chronic bronchitis Causes : long term smoking, certain environmental factors such as textile dust fibers Pathology : Chronic inflammation of airways. hyperplasia of mucosa & destruction of cilia Clinically : Adult, smokers, M>F productive cough, dyspnea , wheezing, Chronic hypoxia
Bronchiectasias Definition : permanent, irreversible dilation & distortion of bronchi Causes : – chronic irritation producing chronic bronchitis – complication of cystic fibrosis – TB Takes years to develop ; Primarily in the lower lobes Clinical presentation : chronic productive cough with foul sputum Complications : Broncbopneumonia and lobar pneumonia , Lung abscess Massive hemoptesis: Iron deficiency anemia , Amyloidosis Pulmonary hypertention , core pumonal , Lung cancer
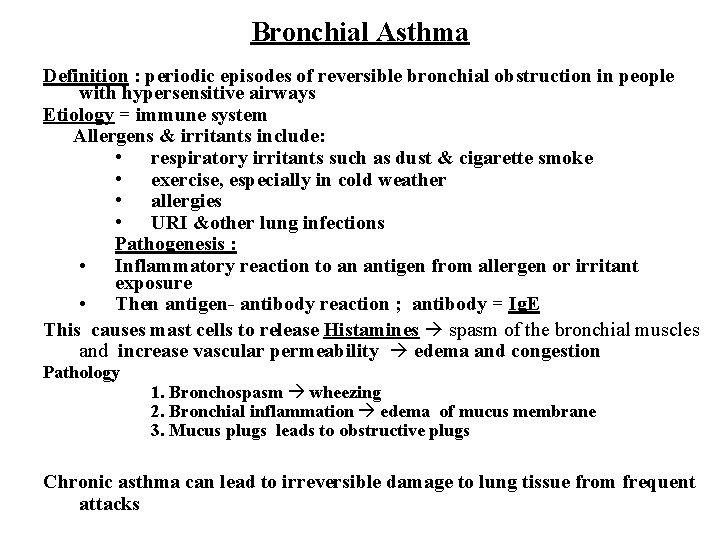
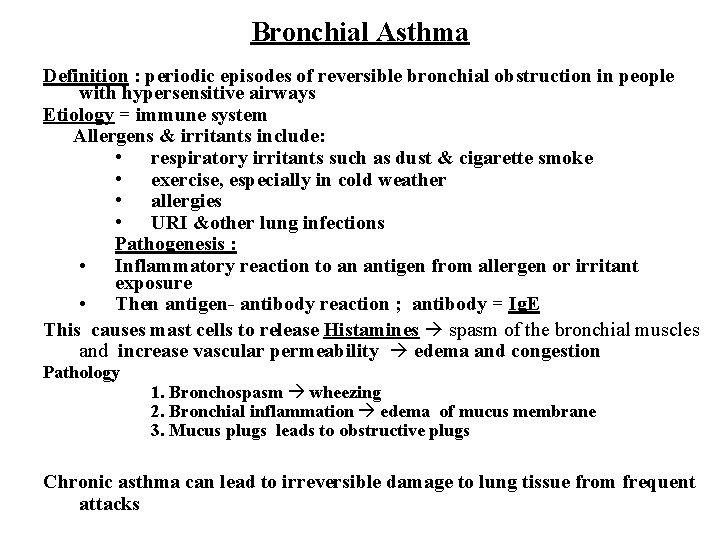
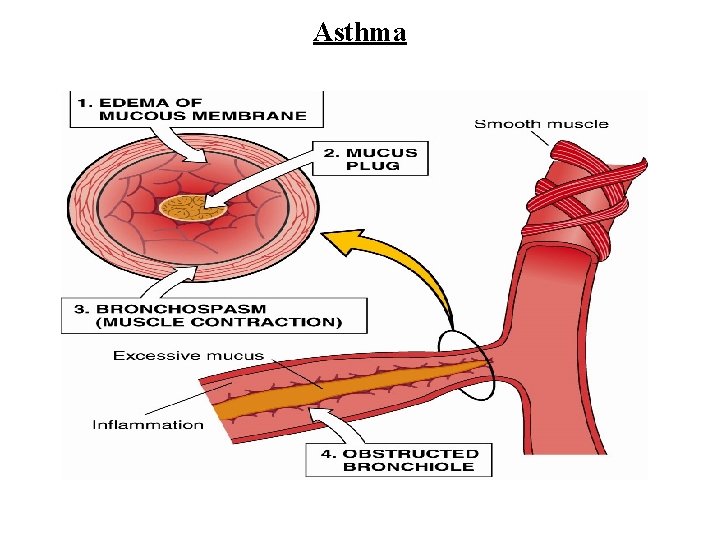
Bronchial Asthma Definition : periodic episodes of reversible bronchial obstruction in people with hypersensitive airways Etiology = immune system Allergens & irritants include: • respiratory irritants such as dust & cigarette smoke • exercise, especially in cold weather • allergies • URI &other lung infections Pathogenesis : • Inflammatory reaction to an antigen from allergen or irritant exposure • Then antigen- antibody reaction ; antibody = Ig. E This causes mast cells to release Histamines spasm of the bronchial muscles and increase vascular permeability edema and congestion Pathology 1. Bronchospasm wheezing 2. Bronchial inflammation edema of mucus membrane 3. Mucus plugs leads to obstructive plugs Chronic asthma can lead to irreversible damage to lung tissue from frequent attacks
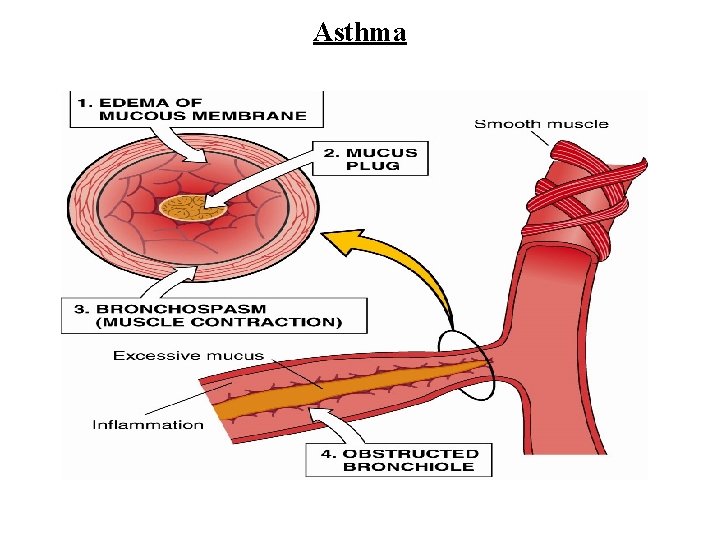
Asthma
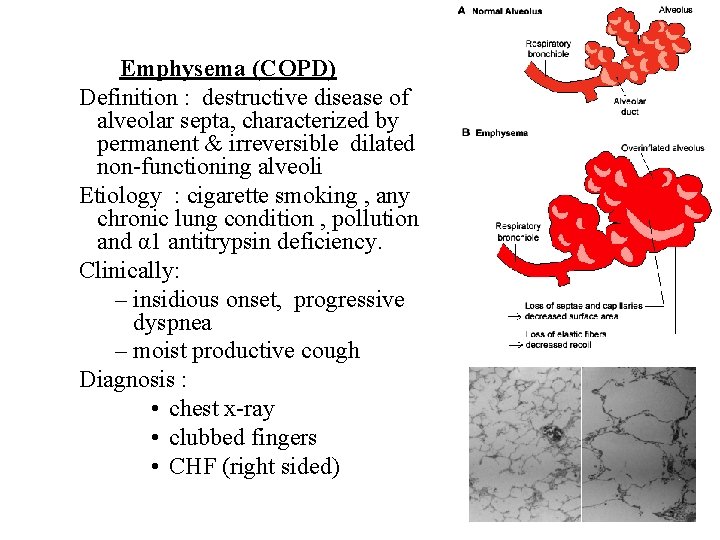
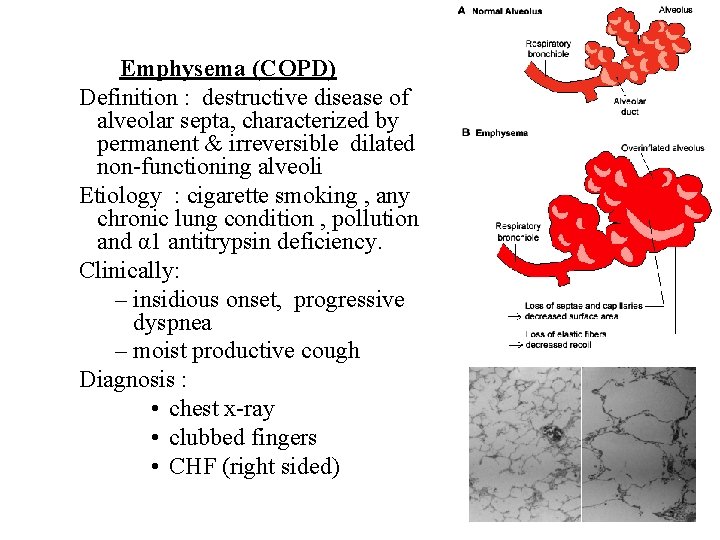
Emphysema (COPD) Definition : destructive disease of alveolar septa, characterized by permanent & irreversible dilated non-functioning alveoli Etiology : cigarette smoking , any chronic lung condition , pollution and α 1 antitrypsin deficiency. Clinically: – insidious onset, progressive dyspnea – moist productive cough Diagnosis : • chest x-ray • clubbed fingers • CHF (right sided)
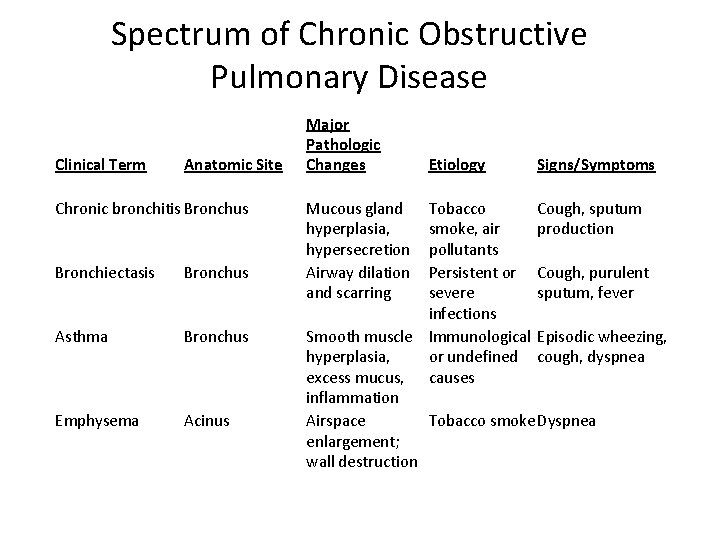
Spectrum of Chronic Obstructive Pulmonary Disease Clinical Term Anatomic Site Chronic bronchitis Bronchus Bronchiectasis Bronchus Asthma Bronchus Emphysema Acinus Major Pathologic Changes Mucous gland hyperplasia, hypersecretion Airway dilation and scarring Etiology Signs/Symptoms Tobacco Cough, sputum smoke, air production pollutants Persistent or Cough, purulent severe sputum, fever infections Smooth muscle Immunological Episodic wheezing, hyperplasia, or undefined cough, dyspnea excess mucus, causes inflammation Airspace Tobacco smoke Dyspnea enlargement; wall destruction
Vascular disorders Pulmonary edema • Pathophysiology – Fluid collection (edema) in all lung tissues • Affects gas exchange • Affects lung expansion – Key = pulmonary capillary pressure increases & fluid moves into alveoli • Capillaries rupture bloody sputum (hemoptysis) • True medical emergency • Etiology – Left sided heart failure , increase hydrostatic pressure – Hypoproteinemia – Lymphatic blockage (e. g. from tumor)
Pulmonary Emboli – Definition = clot of foreign matter that occludes artery in pulmonary system : Depend on the Size of embolus & site – Etiology : – determined by composition of emboli Thrombus , Thromboembolism (most common) , air, fat, fluid – 90% originate from deep veins (primarily in leg) – Old age large bone fractures give fat emboli – Symptoms : • cough, chest pain, fever • if severe ------ dyspnea, tachypnea, hemoptysis • if massive ----- shock & death
Lung carcinoma • leading cause of cancer deaths in both men & woman in US • Etiology and Pathogenesis Tobacco Smoking – cigarettes (87%) Industrial Hazards – ionizing radiation – asbestos - chromates, nickel, arsenic Air Pollution. Genetics
Malignant lung tumours • NON-SMALL CELL – SQUAMOUS CELL CARCINOMA – ADENOCARCINOMA – LARGE CELL CARCINOMA • SMALL CELL CARCINOMA • the SMALL cell carcinomas are WORSE than the non-small cell carcinomas • other primary malignant tumours – lymphomas, sarcomas, carcinoid tumour. • secondary tumours
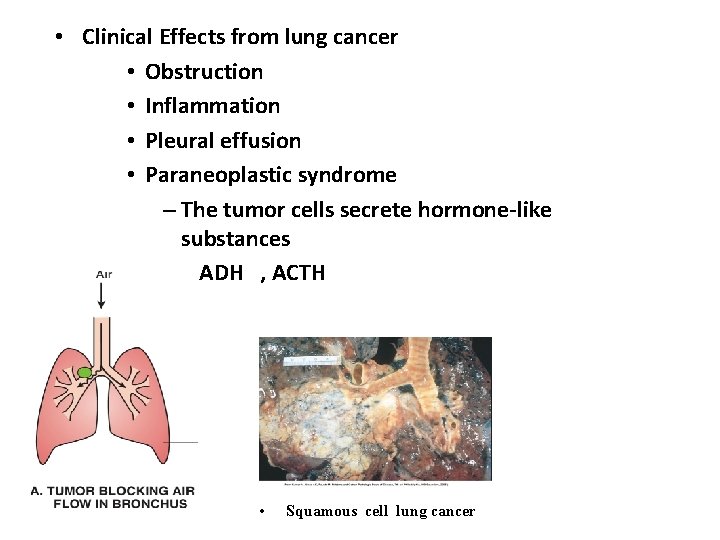
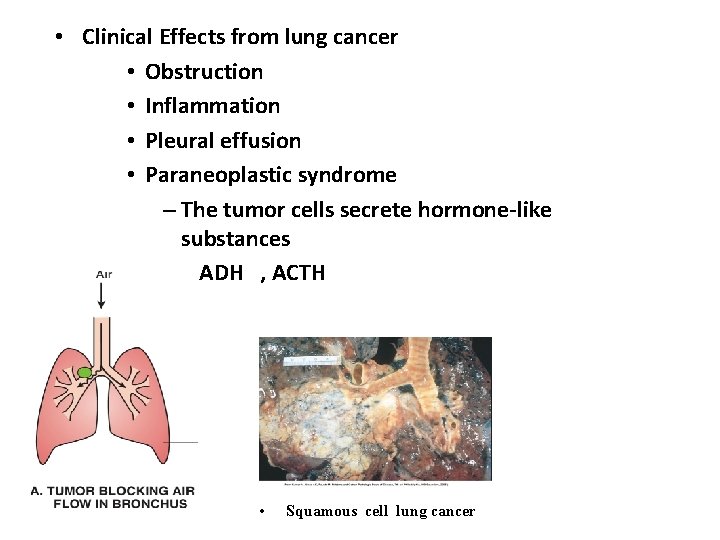
• Clinical Effects from lung cancer • Obstruction • Inflammation • Pleural effusion • Paraneoplastic syndrome – The tumor cells secrete hormone-like substances ADH , ACTH • Squamous cell lung cancer
Thank you
 Diseases of the respiratory system
Diseases of the respiratory system Somaya arianfar
Somaya arianfar Global alliance against chronic respiratory diseases
Global alliance against chronic respiratory diseases What is the conducting zone of the respiratory system
What is the conducting zone of the respiratory system Samina frey
Samina frey Samir saleem
Samir saleem Sea anemone
Sea anemone Saleem beebeejaun
Saleem beebeejaun Dr saleem wani
Dr saleem wani Contrast literary device
Contrast literary device Dr samina saleem
Dr samina saleem Chromosome disorders
Chromosome disorders Site:slidetodoc.com
Site:slidetodoc.com Haithem taha
Haithem taha Taha kass-hout
Taha kass-hout Taha hussein challenges
Taha hussein challenges Taha havakhor
Taha havakhor Operation research by taha
Operation research by taha Mahmud muhammed taha
Mahmud muhammed taha Sharif taha
Sharif taha Sharif taha
Sharif taha Taha kass-hout
Taha kass-hout Renshaw cell inhibition
Renshaw cell inhibition Taha kass-hout
Taha kass-hout Taha kass-hout
Taha kass-hout