First trimester screening E Keshavarz MD Langdon Down















- Slides: 84
First trimester screening E. Keshavarz MD
�Langdon Down (London 1866) �Subgroup of idiots…. Down syndrome(mongolian people) �Down’s theory: retrogression of ethnic type �(Darwin’s contemporary scientific reasoning for evolution) �Theory was not true but 100 years later: �Skin: dirty yellowish tinge skin and is deficient in elasticity, giving the appearance of being too large for the body
� 1866: congenital, dating from intrauterine life � 1909: association with maternal age � 1914: no increased within families � 1914: syphilis, TB, epilepsy, alcholism, insanity, nervous e instability , endocrine abnormalities(thyroid , adrenal , pitiutary , thymus) � 1932: diz. t: un. equally monoz. t: equally transmission from mother to the baby *** 1934: unequal migration of chromosomes during cell division…trisomy
� 1960: familial Down syndrome translocation(15: 21), no trisomy 1961: mosaism type of Down syndrome mosaism of normal and trisomic cells 1966: karyotyping of cultured amniotic fluid cells
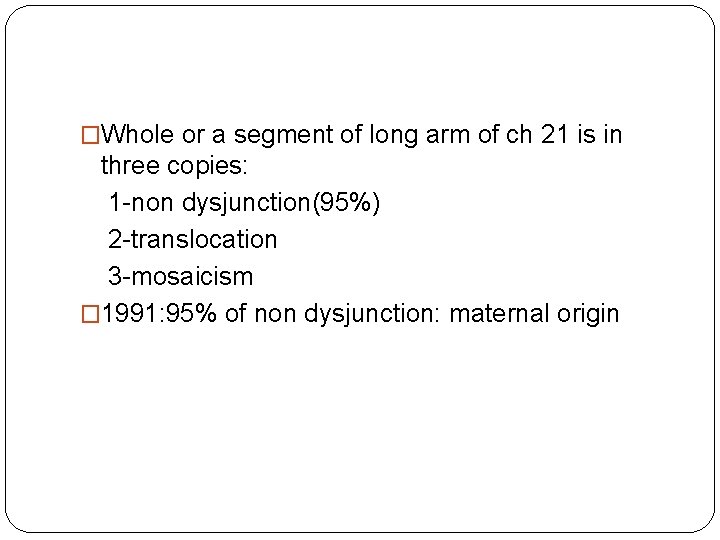
�Whole or a segment of long arm of ch 21 is in three copies: 1 -non dysjunction(95%) 2 -translocation 3 -mosaicism � 1991: 95% of non dysjunction: maternal origin
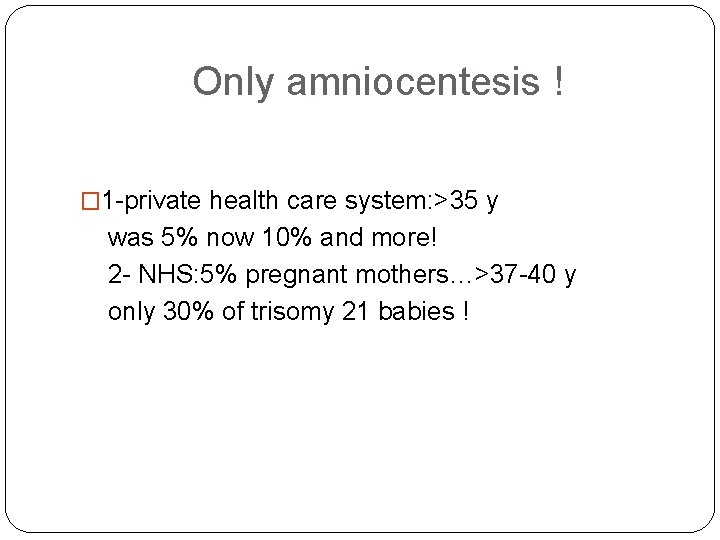
Only amniocentesis ! � 1 -private health care system: >35 y was 5% now 10% and more! 2 - NHS: 5% pregnant mothers…>37 -40 y only 30% of trisomy 21 babies !
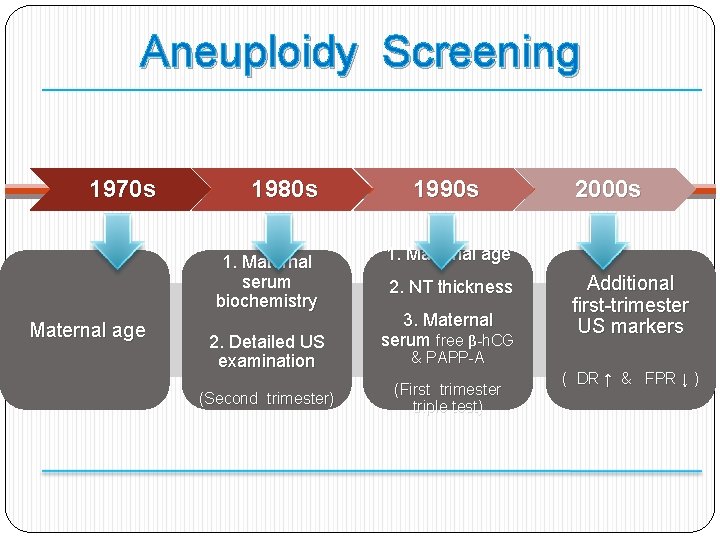
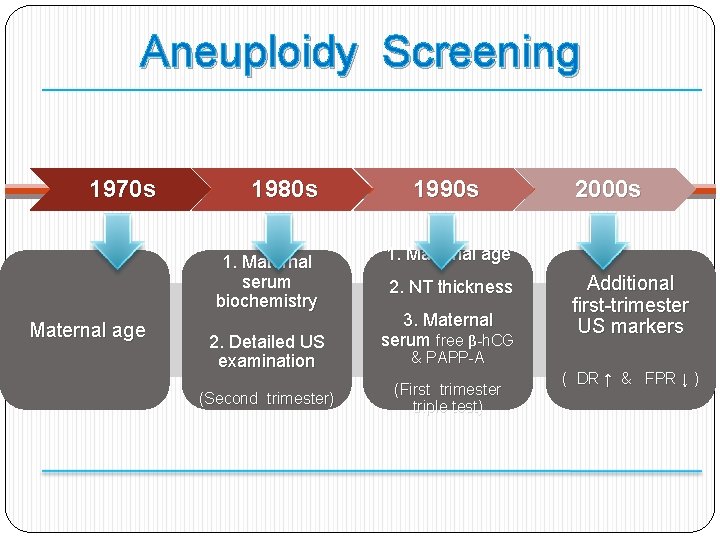
Aneuploidy Screening 1970 s 1980 s 1. Maternal serum biochemistry Maternal age 2. Detailed US examination (Second trimester) 1990 s 2000 s 1. Maternal age 2. NT thickness 3. Maternal serum free β-h. CG Additional first-trimester US markers & PAPP-A (First trimester triple test) ( DR ↑ & FPR ↓ )
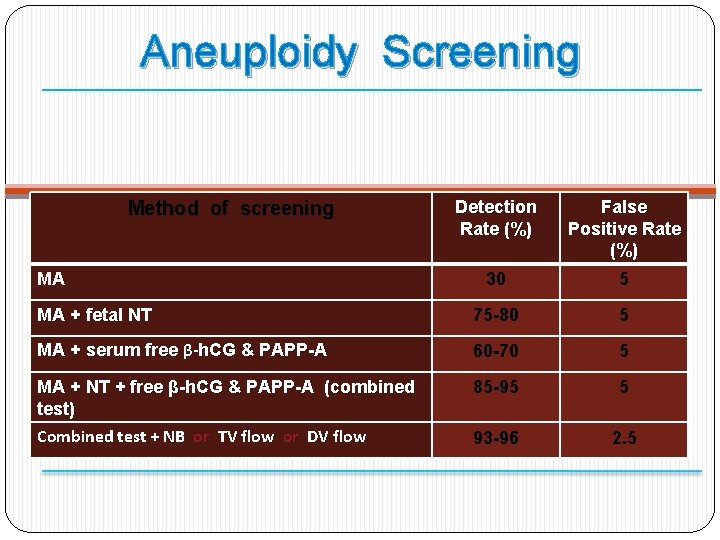
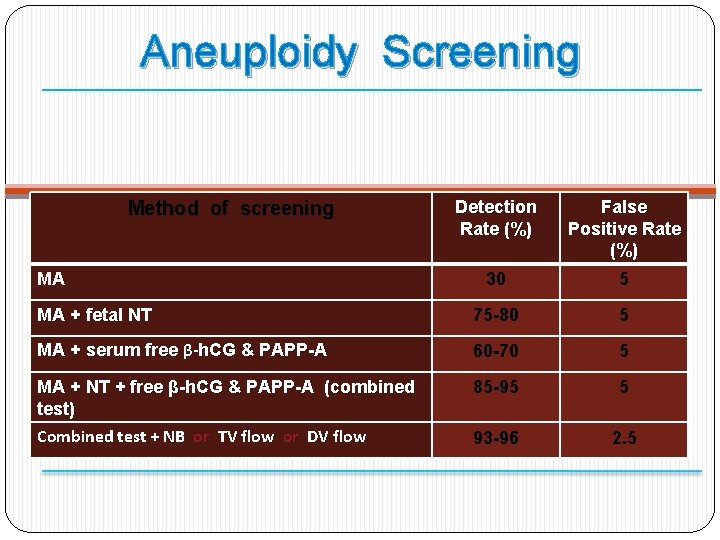
Aneuploidy Screening Detection Rate (%) False Positive Rate (%) 30 5 MA + fetal NT 75 -80 5 MA + serum free β-h. CG & PAPP-A 60 -70 5 MA + NT + free β-h. CG & PAPP-A (combined test) Combined test + NB or TV flow or DV flow 85 -95 5 93 -96 2. 5 Method of screening MA
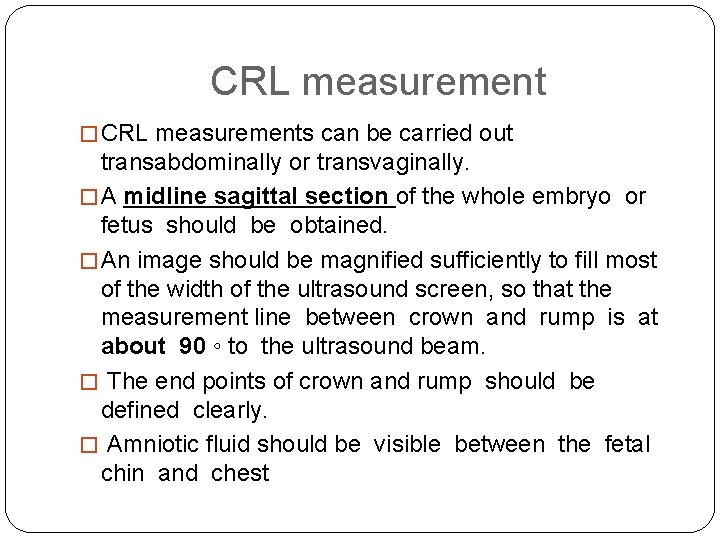
CRL measurement � CRL measurements can be carried out transabdominally or transvaginally. � A midline sagittal section of the whole embryo or fetus should be obtained. � An image should be magnified sufficiently to fill most of the width of the ultrasound screen, so that the measurement line between crown and rump is at about 90 ◦ to the ultrasound beam. � The end points of crown and rump should be defined clearly. � Amniotic fluid should be visible between the fetal chin and chest
� 1 -Mid-sagittal section � 2 -Neutral position � 3 -Horizontal orientation � 4 -Crown and rump clearly visible � 5 -Correct caliper placement � 6 -Good magnification � 1 -Midline facial profile, fetal spine and rump should all be visible in one complete image � 2 -There should be fluid visible between the chin and the chest of the fetus and the ‘profile line’* should form an acute angle with the CRL line before the rump � 3 -Fetus should be horizontal with line connecting crown and rump positioned between 75 ◦ and 105 ◦ (90± 15) To ultrasound beam � 5 -Intersection of calipers should be on outer border of skin covering skull and outer border of skin covering rump � 6 -Fetus should fill more than two-thirds of image, clearly showing crown and rump
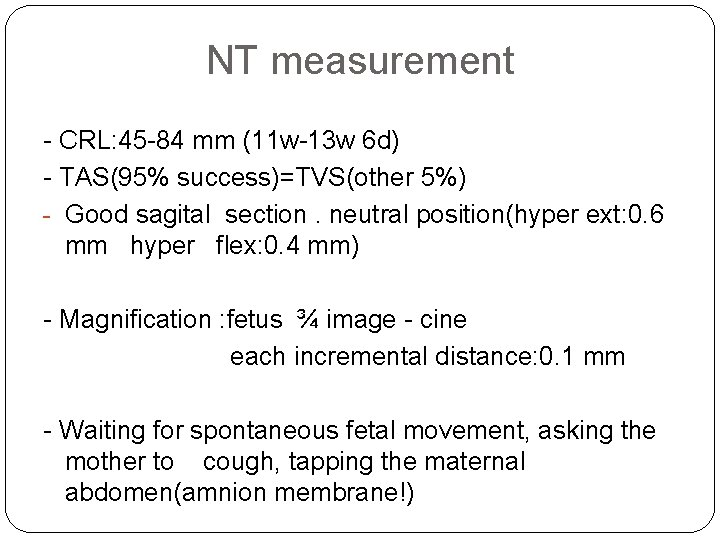
NT measurement - CRL: 45 -84 mm (11 w-13 w 6 d) - TAS(95% success)=TVS(other 5%) - Good sagital section. neutral position(hyper ext: 0. 6 mm hyper flex: 0. 4 mm) - Magnification : fetus ¾ image - cine each incremental distance: 0. 1 mm - Waiting for spontaneous fetal movement, asking the mother to cough, tapping the maternal abdomen(amnion membrane!)
NT measurement - More than one measurement and record the maximum one - Good work after 80 -100 sonography and at least 10 min - Study on 100, 000 cases: normal: 1. 2 (11 w) to 1. 9(13 w 6 d) abnormal: above the 95 th centile(>=3 mm)
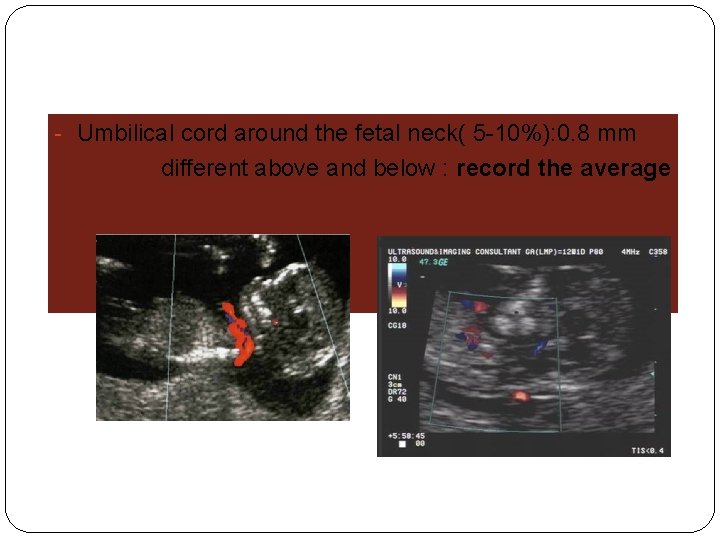
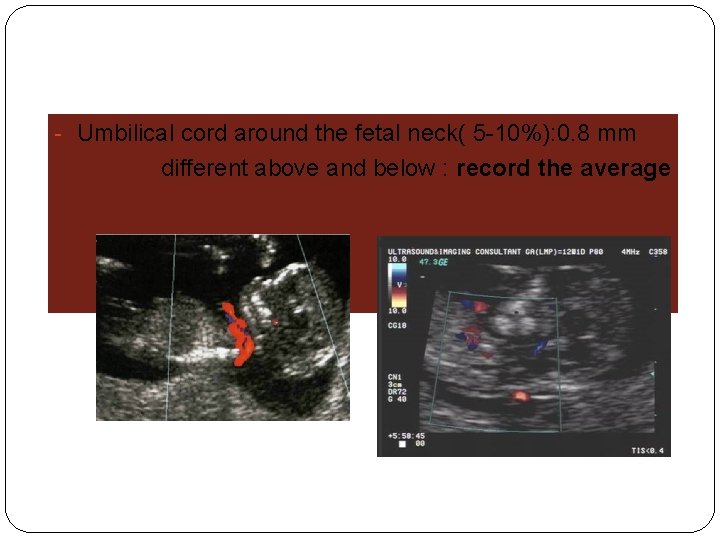
- Umbilical cord around the fetal neck( 5 -10%): 0. 8 mm different above and below : record the average



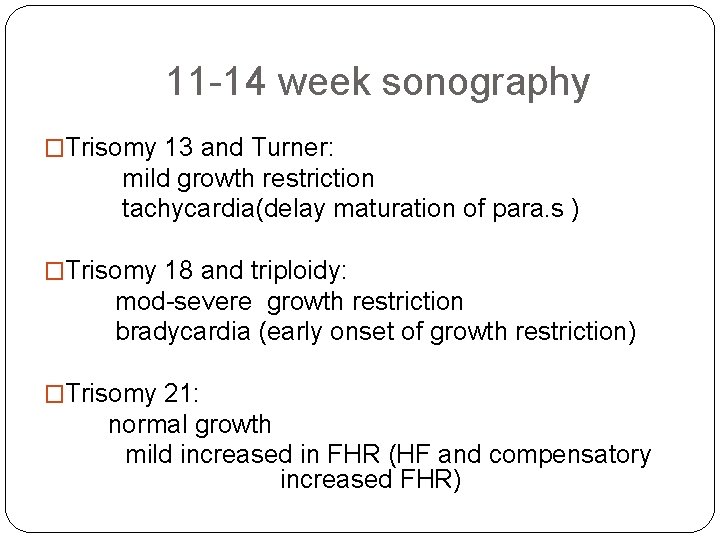
Normal FHR �W 5: 110 bpm �W 9: 170 bpm (due to morphological development of heart) �W 14: 150 bpm (functional maturation of parasympathetic system)
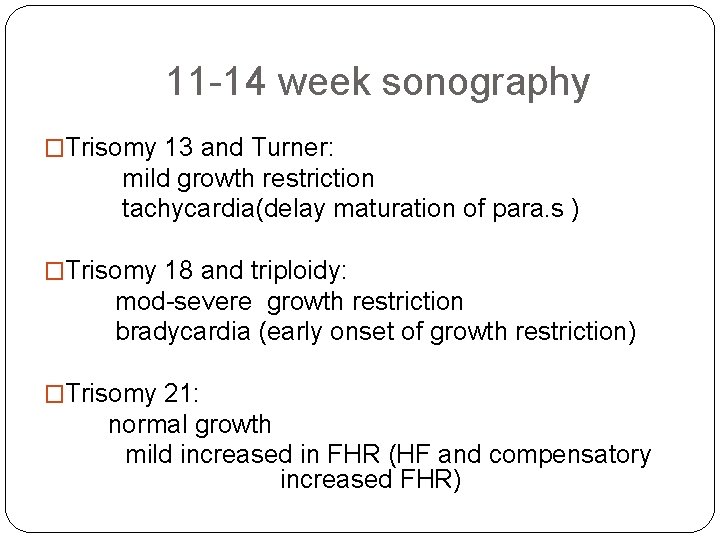
11 -14 week sonography �Trisomy 13 and Turner: mild growth restriction tachycardia(delay maturation of para. s ) �Trisomy 18 and triploidy: mod-severe growth restriction bradycardia (early onset of growth restriction) �Trisomy 21: normal growth mild increased in FHR (HF and compensatory increased FHR)

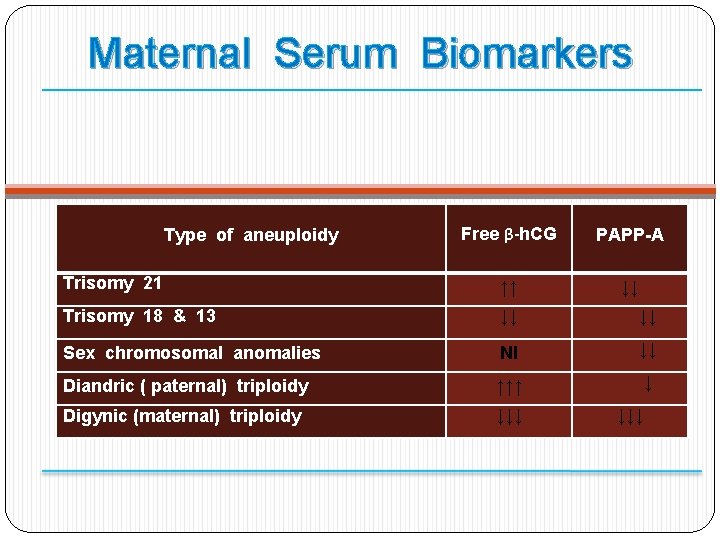
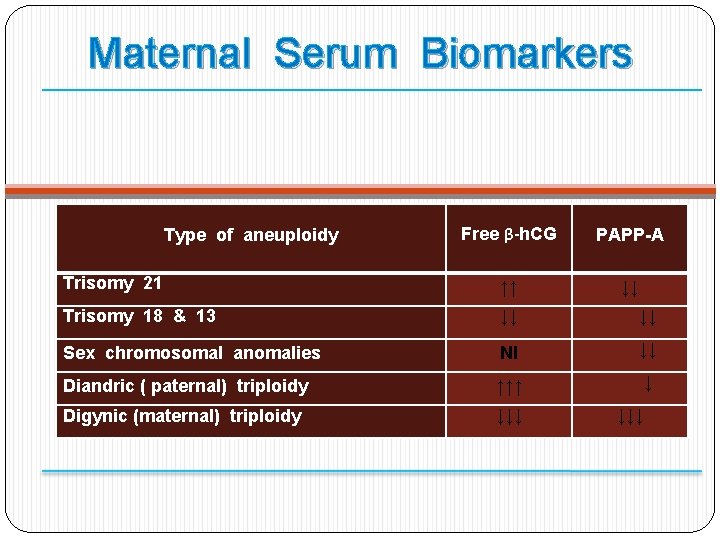
Maternal Serum Biomarkers Free β-h. CG PAPP-A Trisomy 21 ↑↑ ↓↓ Trisomy 18 & 13 ↓↓ ↓↓ Sex chromosomal anomalies Nl ↓↓ Diandric ( paternal) triploidy ↑↑↑ ↓ Digynic (maternal) triploidy ↓↓↓ Type of aneuploidy ↓↓↓
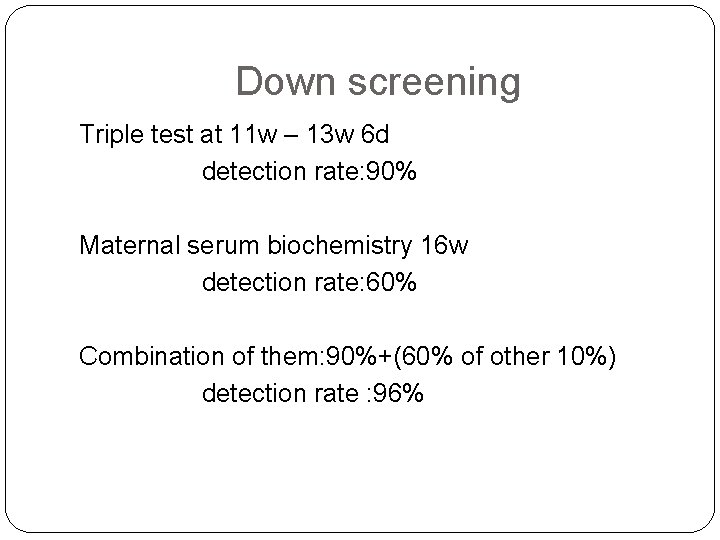
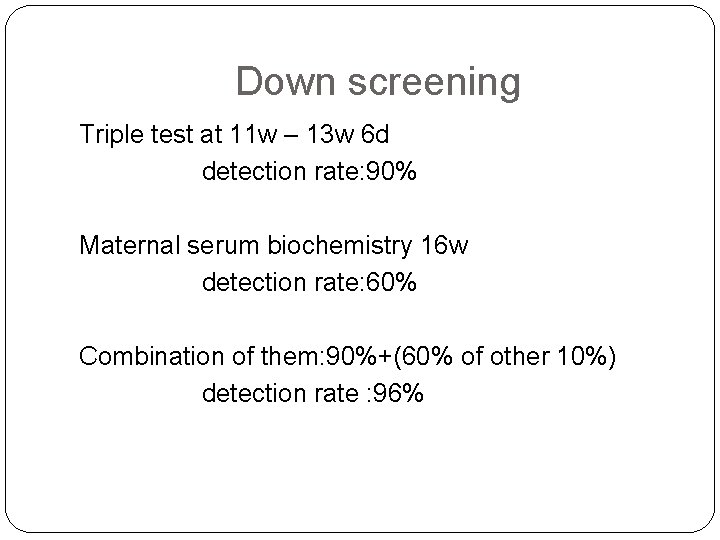
Down screening Triple test at 11 w – 13 w 6 d detection rate: 90% Maternal serum biochemistry 16 w detection rate: 60% Combination of them: 90%+(60% of other 10%) detection rate : 96%
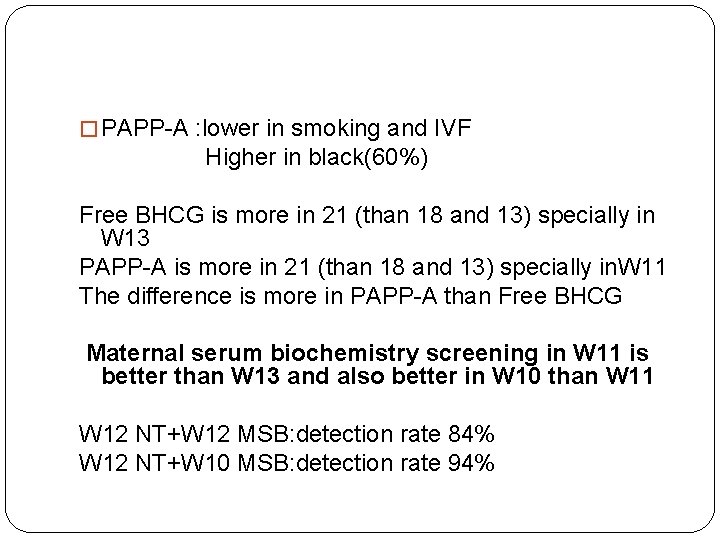
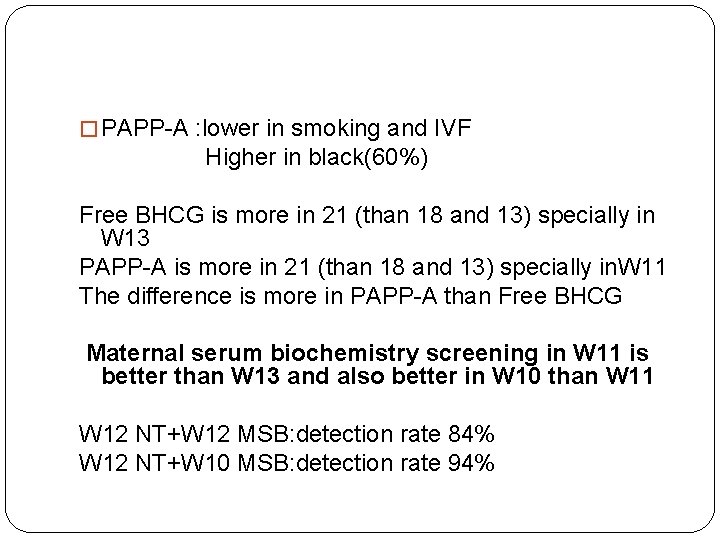
� PAPP-A : lower in smoking and IVF Higher in black(60%) Free BHCG is more in 21 (than 18 and 13) specially in W 13 PAPP-A is more in 21 (than 18 and 13) specially in. W 11 The difference is more in PAPP-A than Free BHCG Maternal serum biochemistry screening in W 11 is better than W 13 and also better in W 10 than W 11 W 12 NT+W 12 MSB: detection rate 84% W 12 NT+W 10 MSB: detection rate 94%
OSCAR �New methods of biochemical testing within 30 min(time-resolved-amplified-cryptateemission)+ NT at the same time: �One Step Clinics for Assessment of Risk
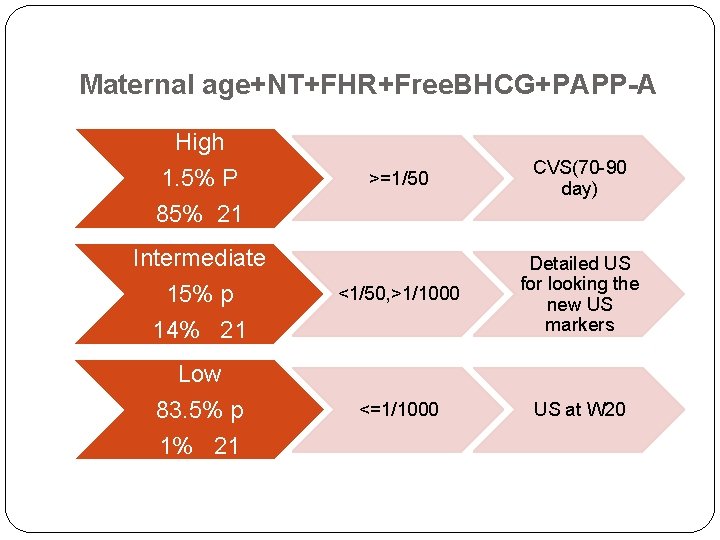
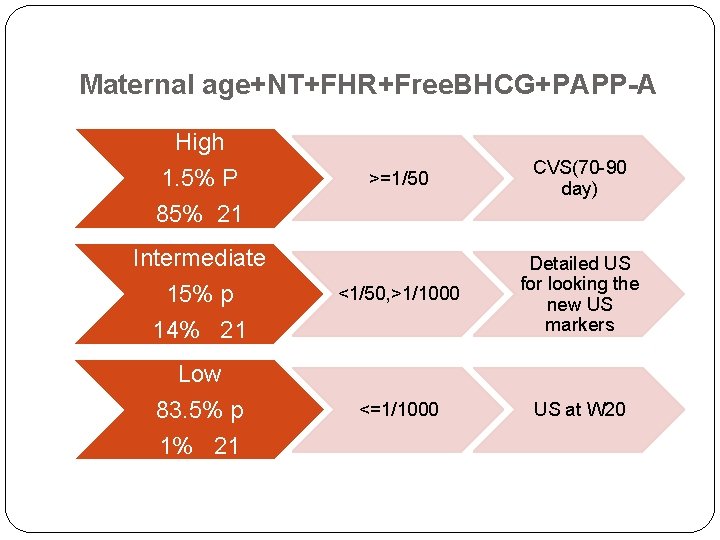
Maternal age+NT+FHR+Free. BHCG+PAPP-A High 1. 5% P >=1/50 CVS(70 -90 day) <1/50, >1/1000 Detailed US for looking the new US markers <=1/1000 US at W 20 85% 21 Intermediate 15% p 14% 21 Low 83. 5% p 1% 21
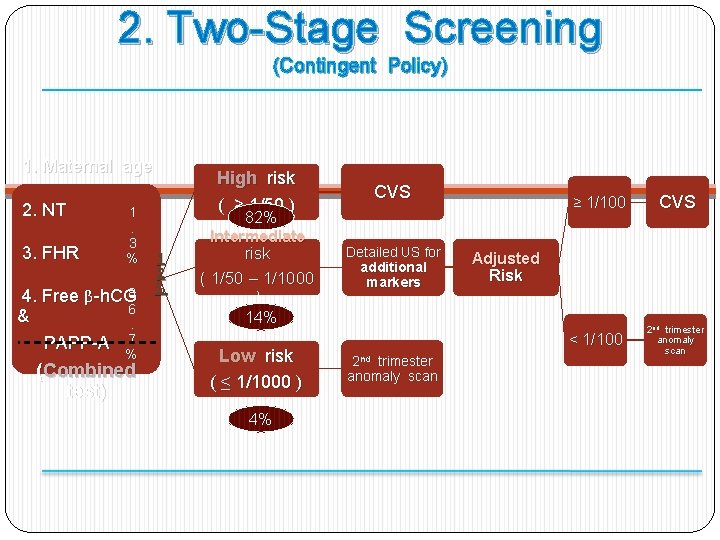
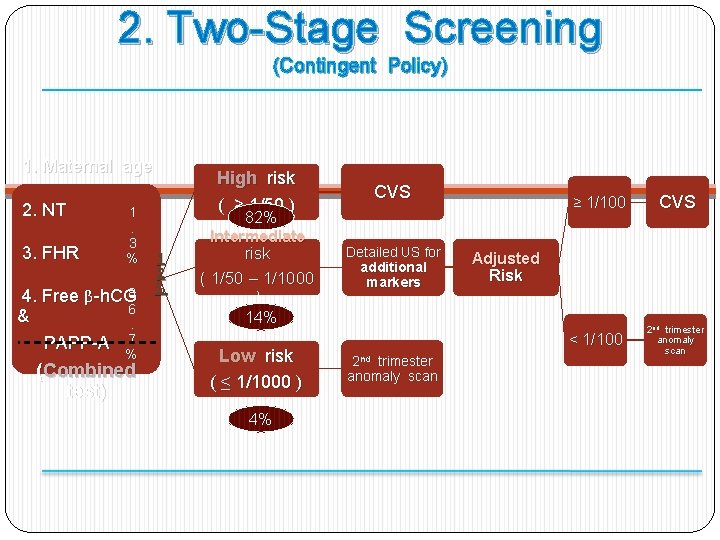
2. Two-Stage Screening (Contingent Policy) 1. Maternal age 2. NT 3. FHR 4. & 1. 3 % 8 Free β-h. CG 6. 7 PAPP-A % (Combined test) High risk ( ≥ 1/50 ) 1 2 % 82% Intermediate risk ( 1/50 – 1/1000 ) CVS Detailed US for additional markers ≥ 1/100 Adjusted Risk 14% Low risk ( ≤ 1/1000 ) 4% < 1/100 2 nd trimester anomaly scan CVS 2 nd trimester anomaly scan
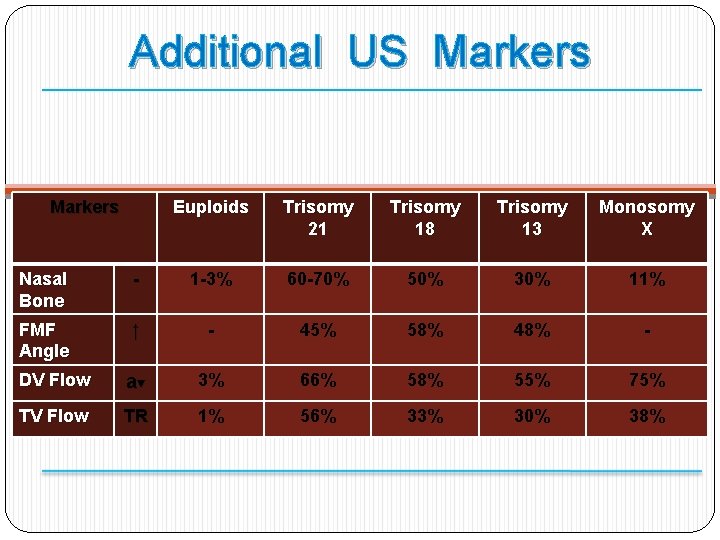
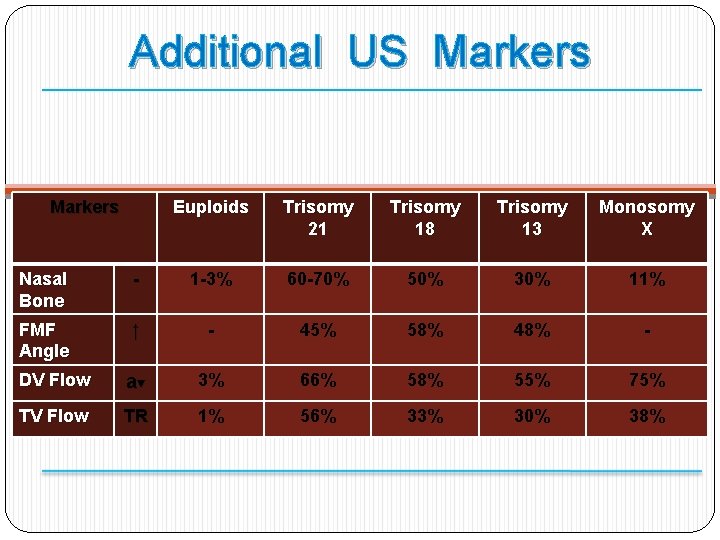
Additional US Markers Euploids Trisomy 21 Trisomy 18 Trisomy 13 Monosomy X Nasal Bone - 1 -3% 60 -70% 50% 30% 11% FMF Angle ↑ - 45% 58% 48% - DV Flow a▼ 3% 66% 58% 55% 75% TV Flow TR 1% 56% 33% 30% 38%
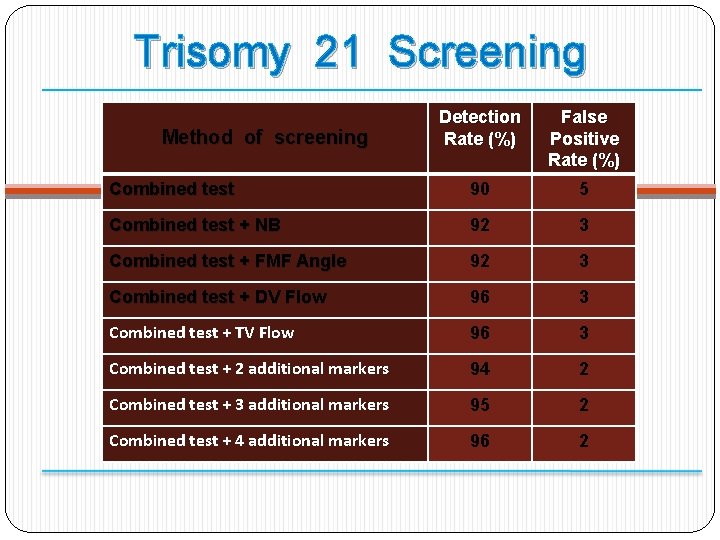
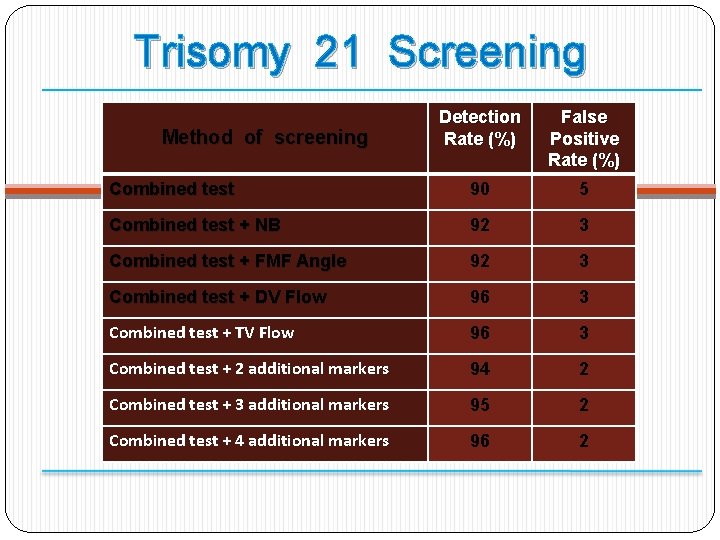
Trisomy 21 Screening Detection Rate (%) False Positive Rate (%) Combined test 90 5 Combined test + NB 92 3 Combined test + FMF Angle 92 3 Combined test + DV Flow 96 3 Combined test + TV Flow 96 3 Combined test + 2 additional markers 94 2 Combined test + 3 additional markers 95 2 Combined test + 4 additional markers 96 2 Method of screening

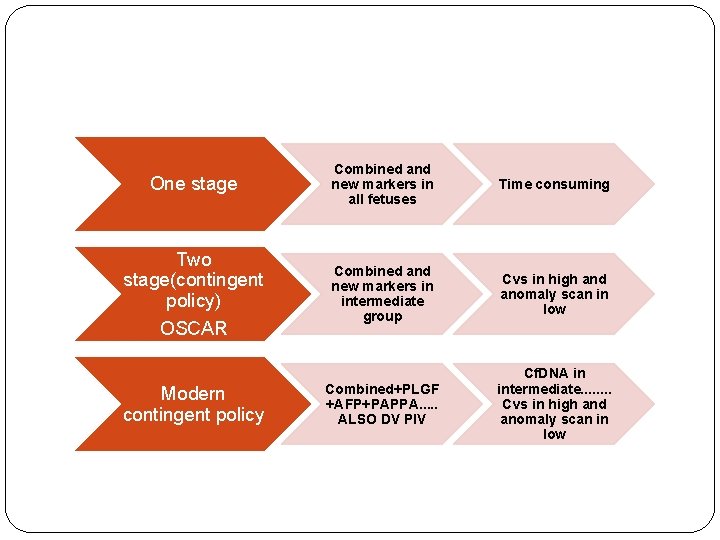
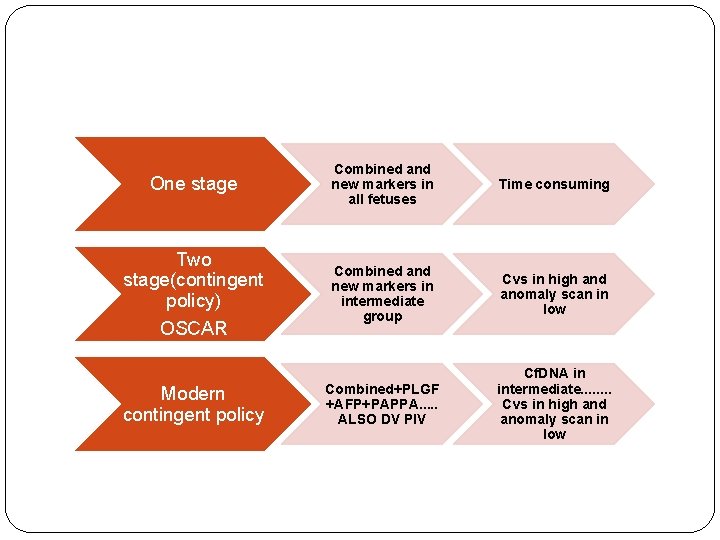
One stage Two stage(contingent policy) OSCAR Modern contingent policy Combined and new markers in all fetuses Time consuming Combined and new markers in intermediate group Cvs in high and anomaly scan in low Combined+PLGF +AFP+PAPPA. . . ALSO DV PIV Cf. DNA in intermediate. . . . Cvs in high and anomaly scan in low
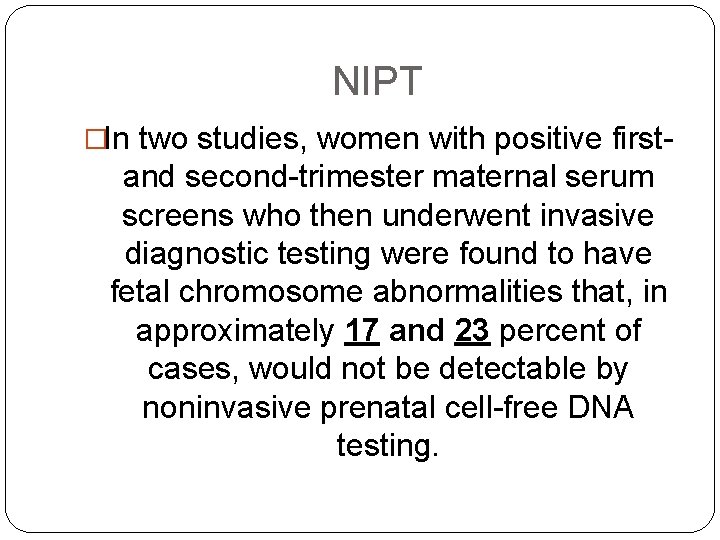
NIPT �In two studies, women with positive first- and second-trimester maternal serum screens who then underwent invasive diagnostic testing were found to have fetal chromosome abnormalities that, in approximately 17 and 23 percent of cases, would not be detectable by noninvasive prenatal cell-free DNA testing.
New US markers � 1 -NB � 2 -Facial angle � 2 -DV PI � 3 -Ductus venusus flow � 4 -Trichospid flow � 3 -TR
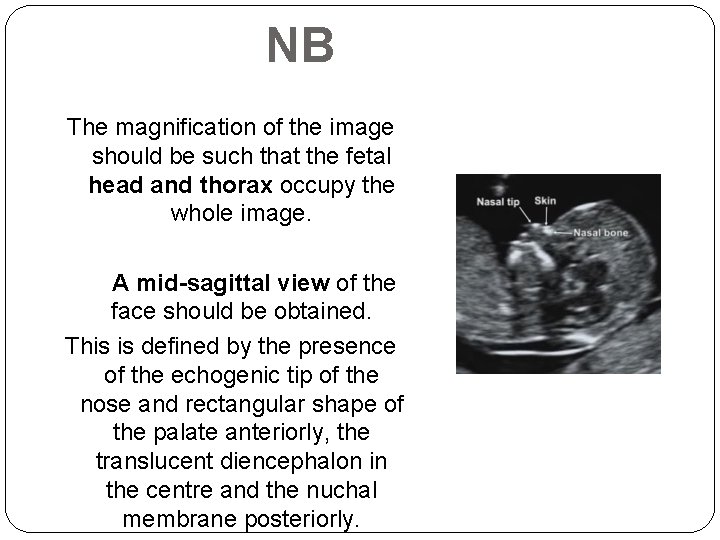
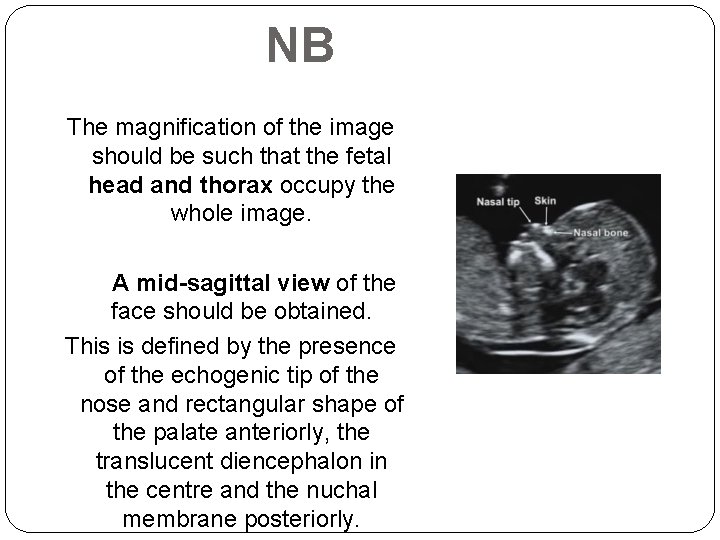
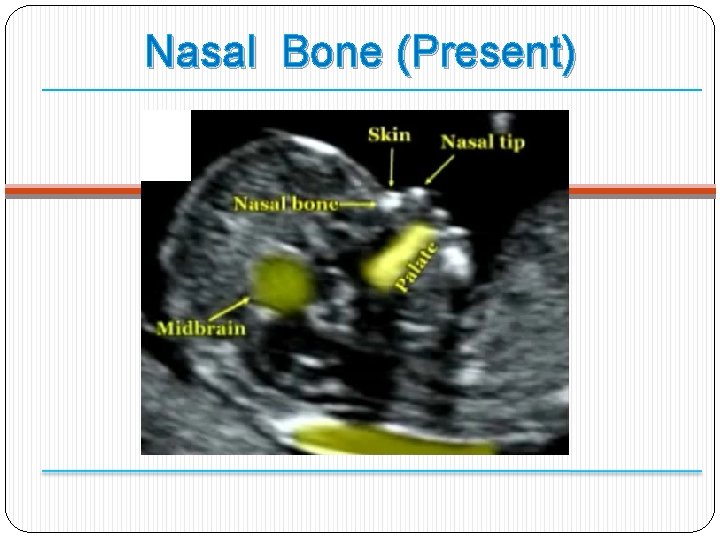
NB The magnification of the image should be such that the fetal head and thorax occupy the whole image. A mid-sagittal view of the face should be obtained. This is defined by the presence of the echogenic tip of the nose and rectangular shape of the palate anteriorly, the translucent diencephalon in the centre and the nuchal membrane posteriorly.
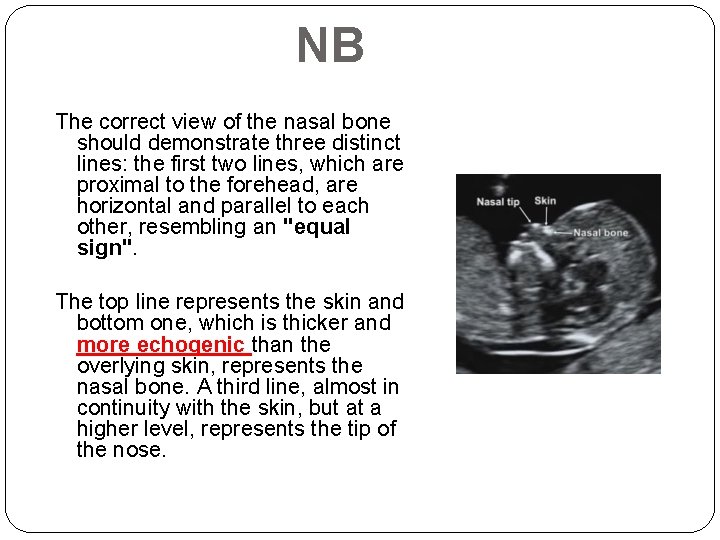
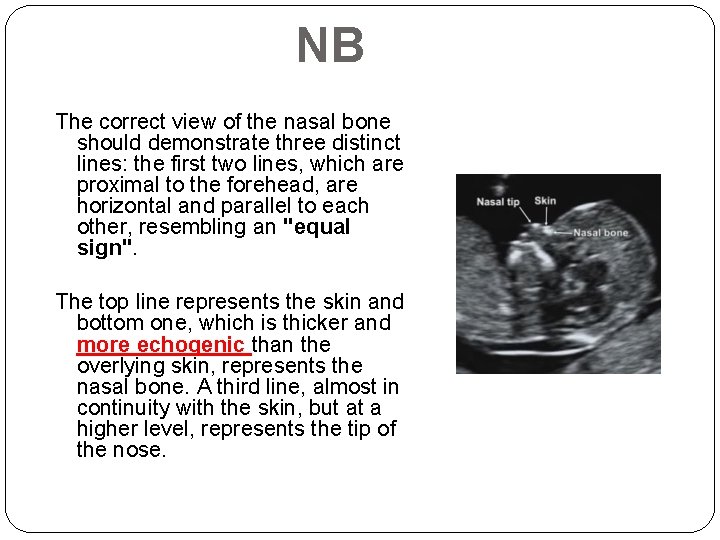
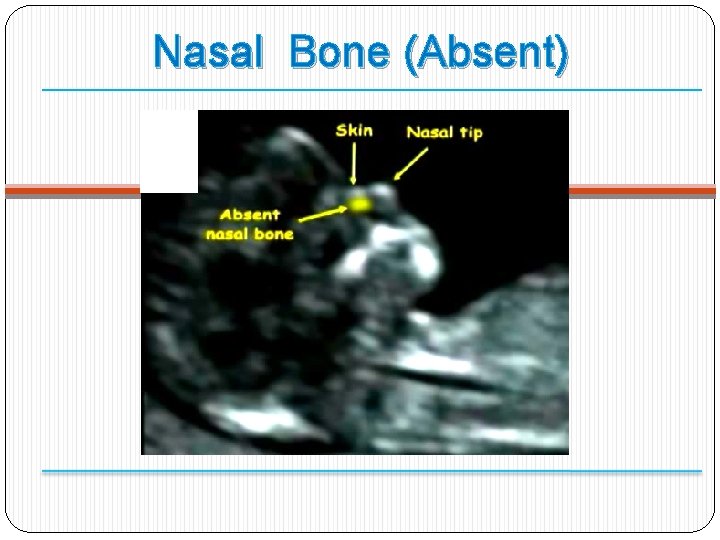
NB The correct view of the nasal bone should demonstrate three distinct lines: the first two lines, which are proximal to the forehead, are horizontal and parallel to each other, resembling an "equal sign". The top line represents the skin and bottom one, which is thicker and more echogenic than the overlying skin, represents the nasal bone. A third line, almost in continuity with the skin, but at a higher level, represents the tip of the nose.
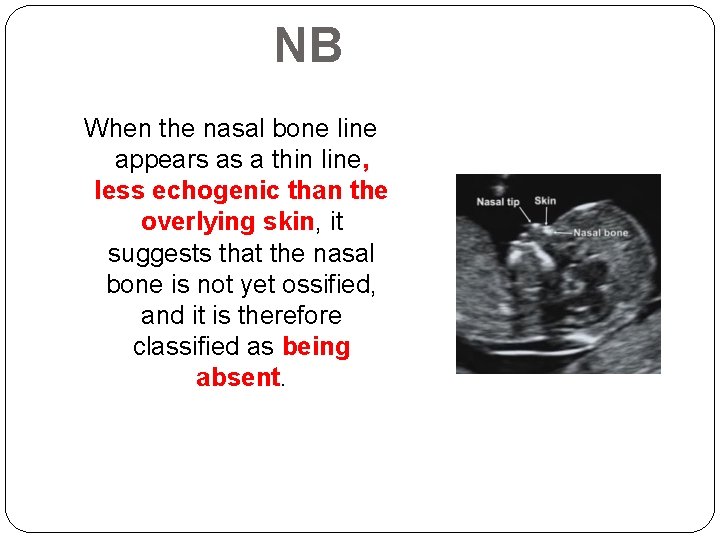
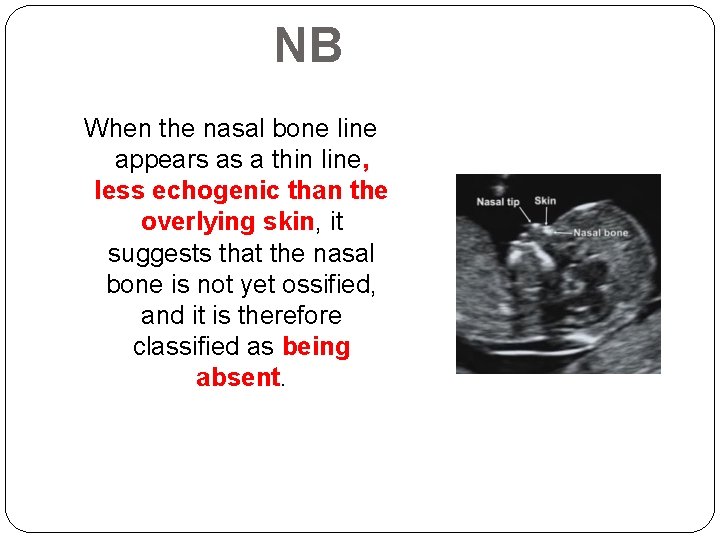
NB When the nasal bone line appears as a thin line, less echogenic than the overlying skin, it suggests that the nasal bone is not yet ossified, and it is therefore classified as being absent.
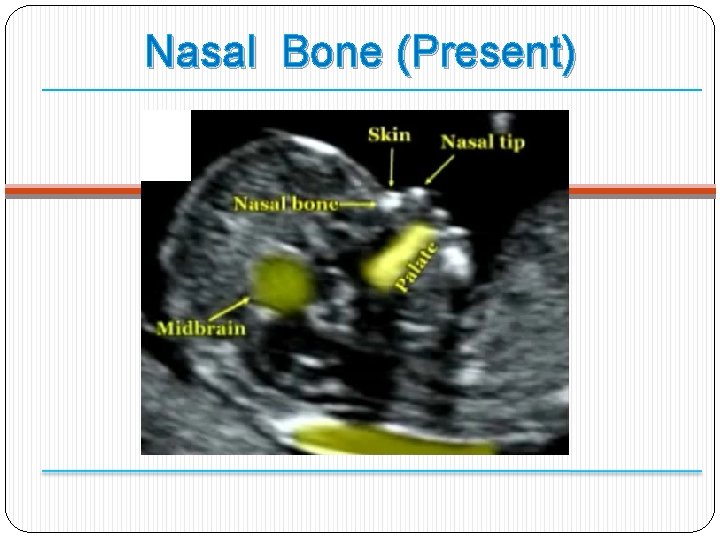
Nasal Bone (Present)
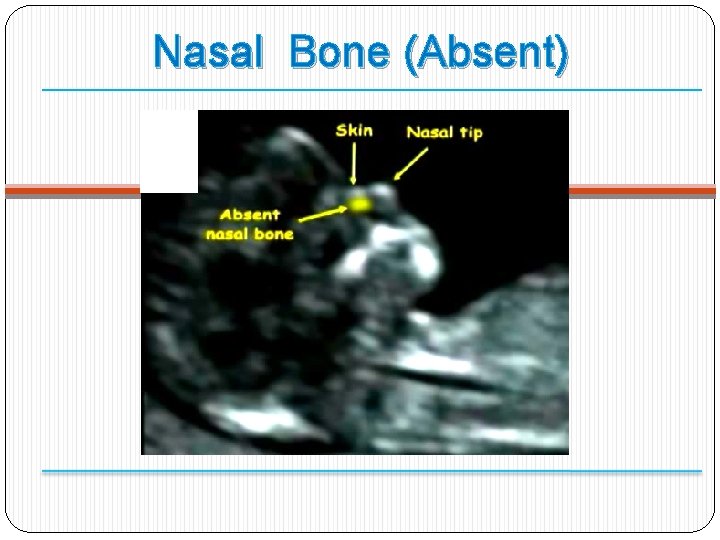
Nasal Bone (Absent)
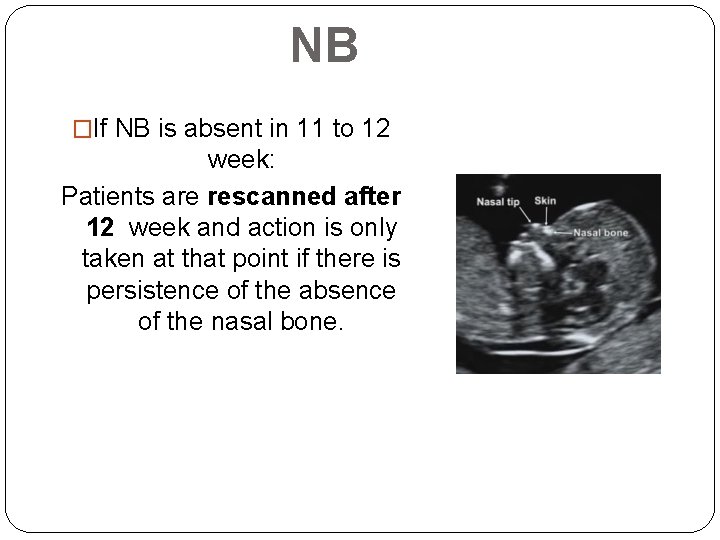
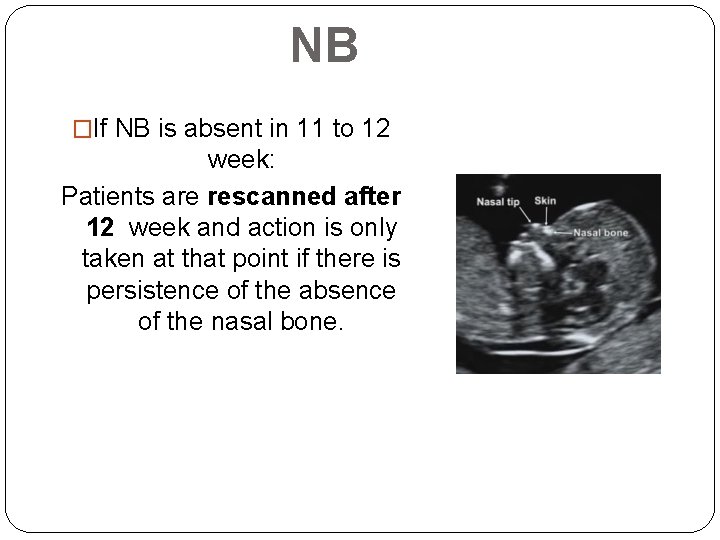
NB �If NB is absent in 11 to 12 week: Patients are rescanned after 12 week and action is only taken at that point if there is persistence of the absence of the nasal bone.
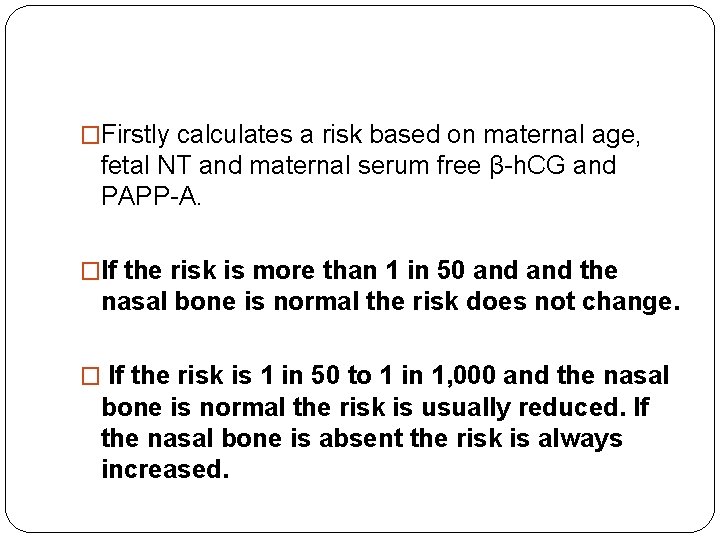
�Firstly calculates a risk based on maternal age, fetal NT and maternal serum free β-h. CG and PAPP-A. �If the risk is more than 1 in 50 and the nasal bone is normal the risk does not change. � If the risk is 1 in 50 to 1 in 1, 000 and the nasal bone is normal the risk is usually reduced. If the nasal bone is absent the risk is always increased.
TR � The magnification of the image should be such that the fetal thorax occupies most of the image. � An apical four-chamber view of the fetal heart should be obtained. � A pulsed-wave Doppler sample volume of 2. 0 to 3. 0 mm should be positioned across the tricuspid valve so that the angle to the direction of flow is less than 30 degrees from the direction of the interventricular septum.

TR � Tricuspid regurgitation is diagnosed if it is found during at least half of the systole and with a velocity of over 60 cm/s, since aortic or pulmonary arterial blood flow at this gestation can produce a maximum velocity of 50 cm/s. � The tricuspid valve could be insufficient in one or more of its three cusps, and therefore the sample volume should be placed across the valve at least three times, in an attempt to interrogate the complete valve

�The incidence of tricuspid regurgitation is related to NT and CRL as well as aneuploidy, being more common when the NT is high and the CRL is low. �If the risk is more than 1 in 50 and tricuspid flow is normal the risk does not change. �If the risk is 1 in 50 to 1 in 1, 000 and the tricuspid flow is normal the risk is usually reduced. If there is tricuspid regurgitation the risk is always increased.
� In addition, there is an increased risk for cardiac defects and therefore such patients should have a follow up specialist fetal cardiac scan.


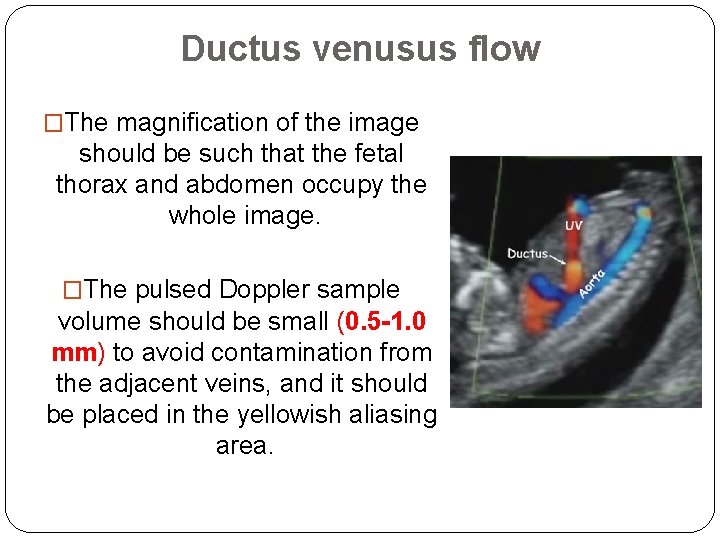
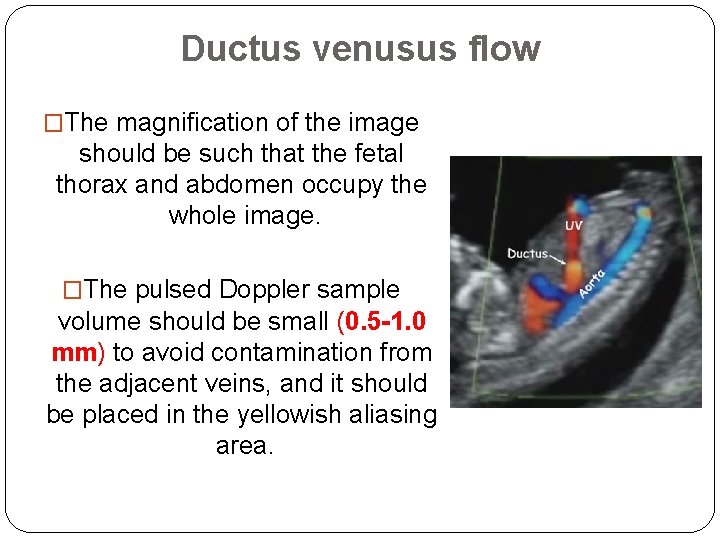
Ductus venusus flow �The magnification of the image should be such that the fetal thorax and abdomen occupy the whole image. �The pulsed Doppler sample volume should be small (0. 5 -1. 0 mm) to avoid contamination from the adjacent veins, and it should be placed in the yellowish aliasing area.
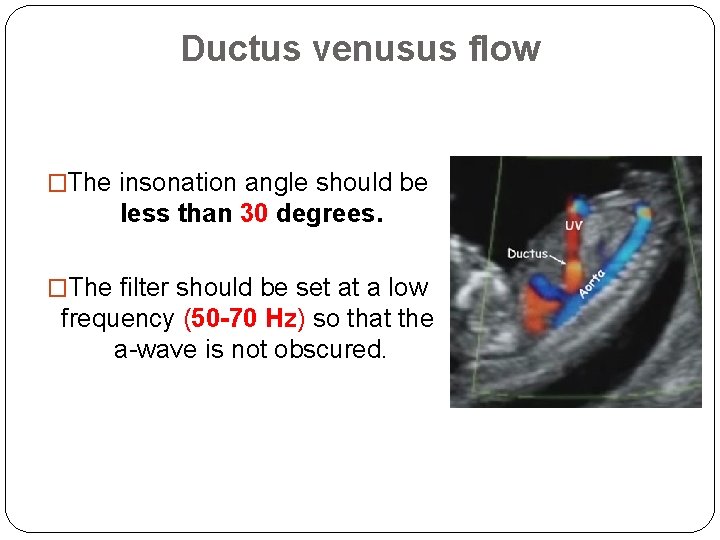
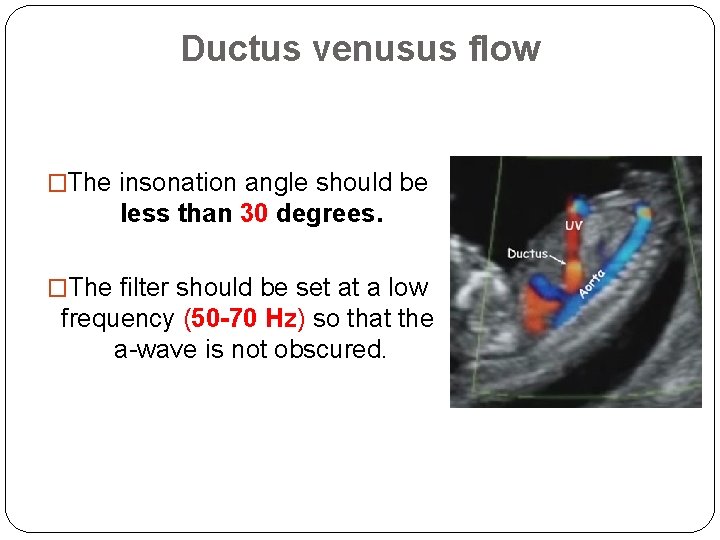
Ductus venusus flow �The insonation angle should be less than 30 degrees. �The filter should be set at a low frequency (50 -70 Hz) so that the a-wave is not obscured.
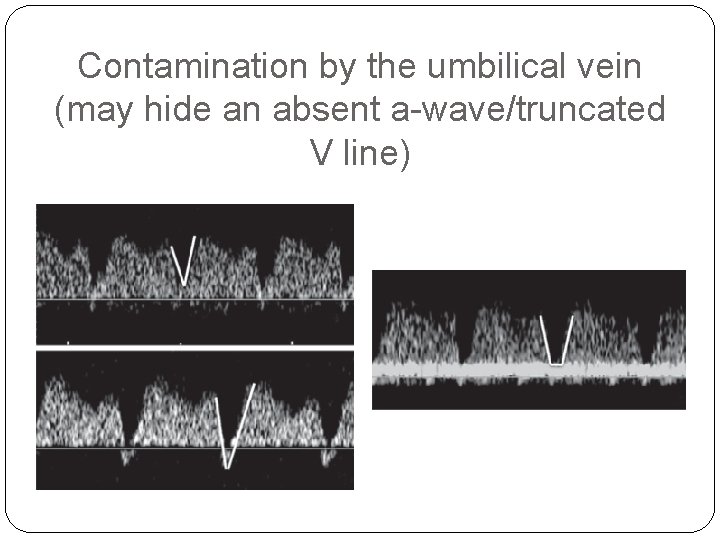
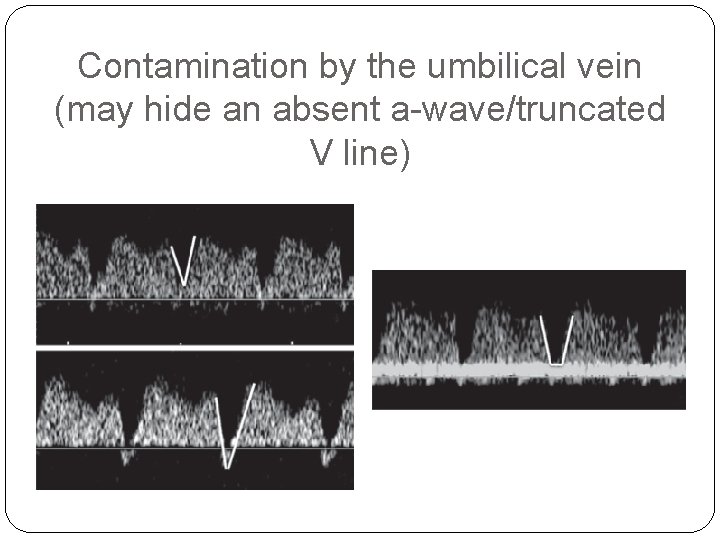
Contamination by the umbilical vein (may hide an absent a-wave/truncated V line)
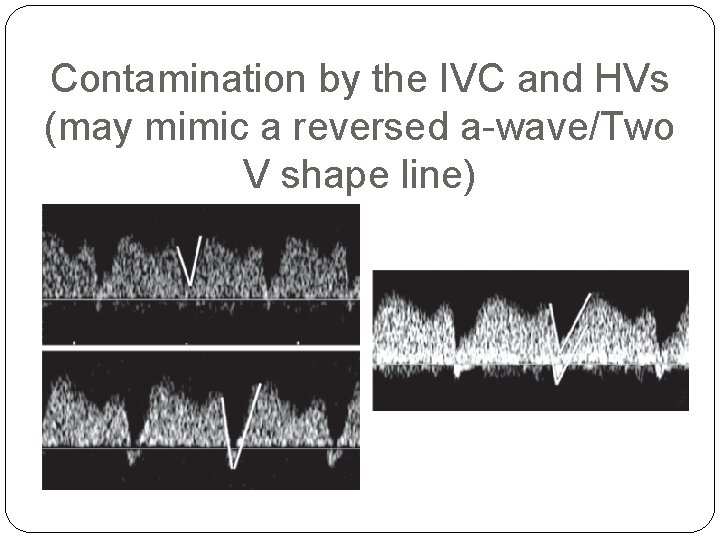
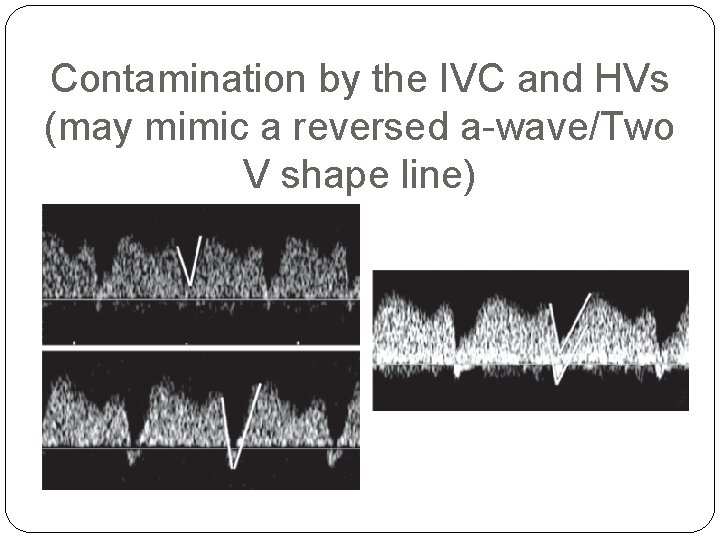
Contamination by the IVC and HVs (may mimic a reversed a-wave/Two V shape line)

�If the risk is more than 1 in 50 and ductus venosus flow is normal the risk does not change. � If the risk is 1 in 50 to 1 in 1, 000 and the ductus venosus flow is normal the risk is usually reduced. If there is reversed a-wave the risk is always increased
�In addition, there is an increased risk for cardiac defects and therefore such patients should have a follow up specialist fetal cardiac scan.
�The incidence of reversed ductus venosus a-wave is related to NT and CRL as well as aneuploidy, being more common when the NT is high , PAPP -A is low and the CRL is low. � 1 -Atrial contraction wave is greater than in later gestation. � 2 -Cardiac afterload is greater in the first trimester because of higher placental resistance. � 3 -Only a small impairment of the cardiac diastolic function might be enough for cardiac dysfunction to become evident as a reversed a-wave
�Abnormal ductus venosus flow in the first trimester may be a predictor of twin-to-twin transfusion syndrome (TTTS). �Previous studies reported that another early manifestation of TTTS is increased NT in at least 1 of the fetuses or a large discordance in NT between the 2 fetuses. �Multiple regression analysis demonstrated that in the prediction of TTTS there was no significant improvement by the addition of NT discordance to the finding of reversed a-wave.
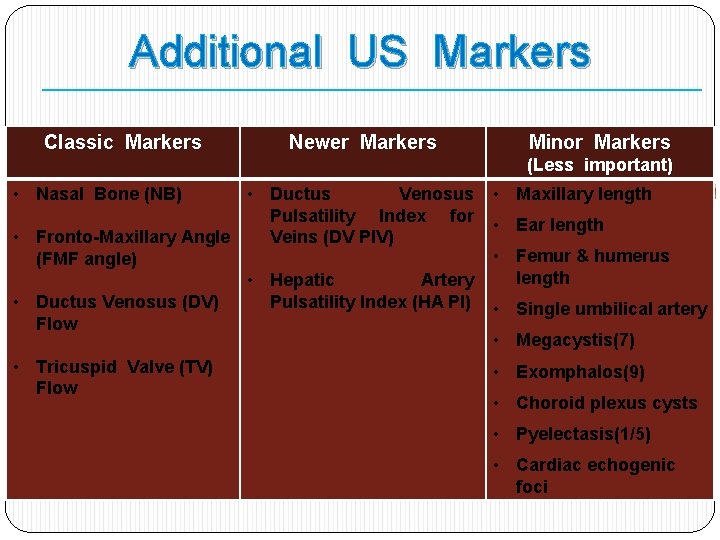
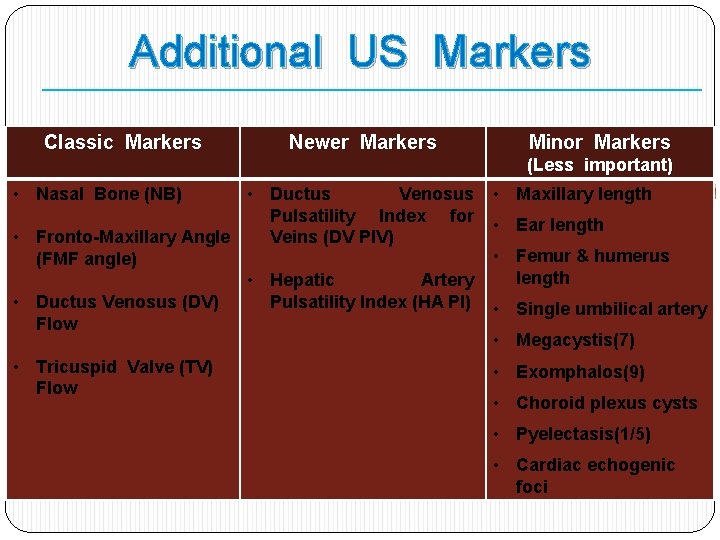
Additional US Markers Classic Markers Newer Markers Minor Markers (Less important) • Nasal Bone (NB) • Ductus Venosus Pulsatility Index for Veins (DV PIV) • Fronto-Maxillary Angle (FMF angle) • Hepatic Artery Pulsatility Index (HA PI) • Ductus Venosus (DV) Flow • Maxillary length • Tricuspid Valve (TV) Flow • Exomphalos(9) • Ear length • Femur & humerus length • Single umbilical artery • Megacystis(7) • Choroid plexus cysts • Pyelectasis(1/5) • Cardiac echogenic foci
Hepatic Artery PI
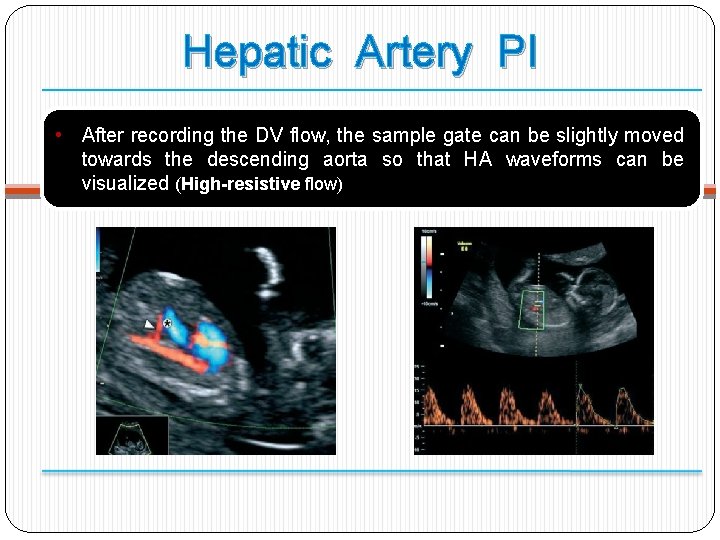
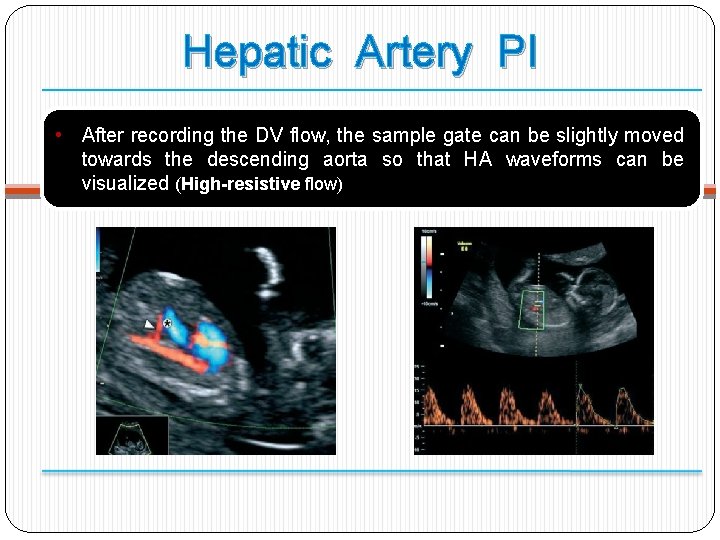
Hepatic Artery PI • After recording the DV flow, the sample gate can be slightly moved towards the descending aorta so that HA waveforms can be visualized (High-resistive flow)
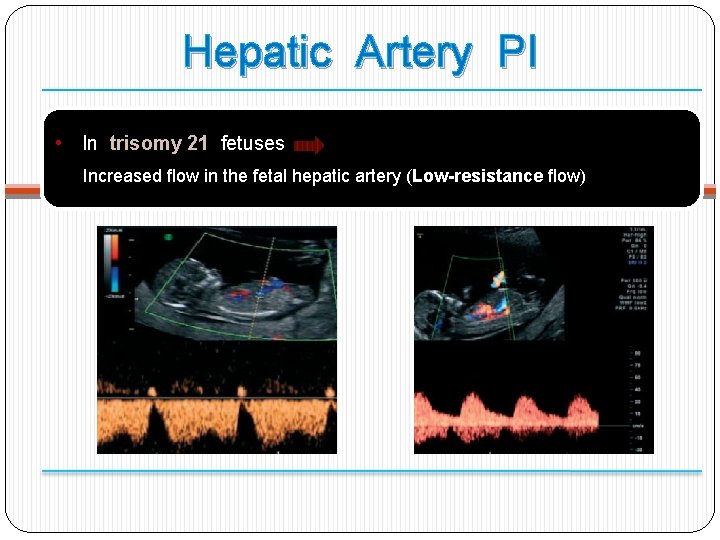
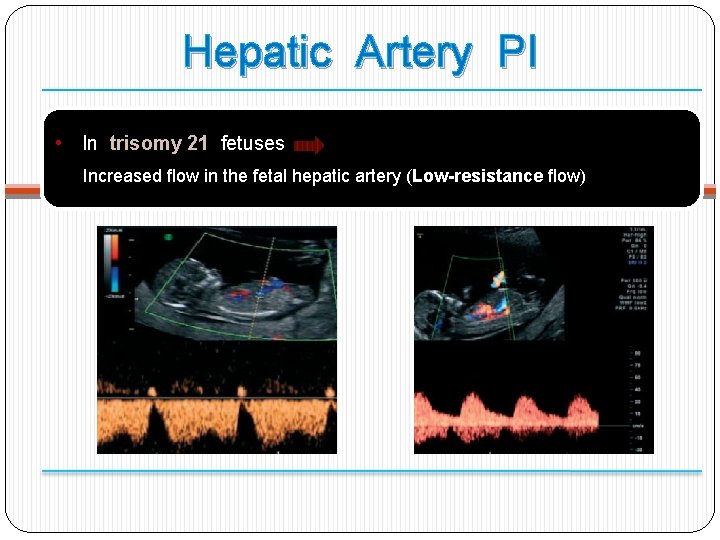
Hepatic Artery PI • In trisomy 21 fetuses Increased flow in the fetal hepatic artery (Low-resistance flow)
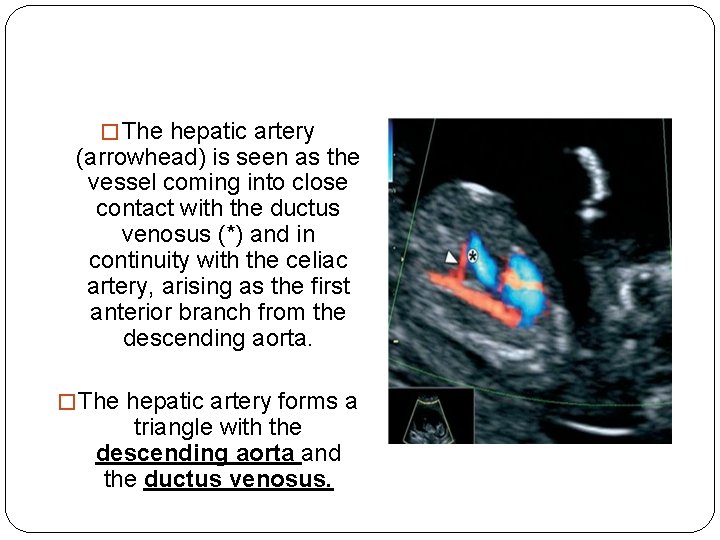
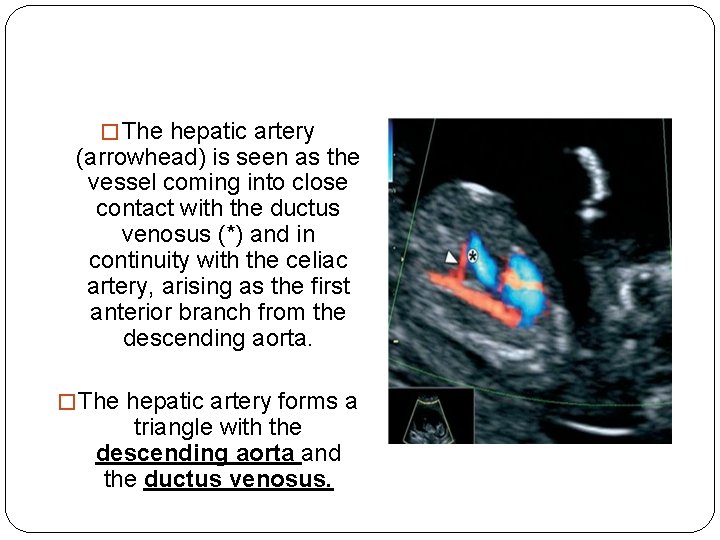
� The hepatic artery (arrowhead) is seen as the vessel coming into close contact with the ductus venosus (*) and in continuity with the celiac artery, arising as the first anterior branch from the descending aorta. � The hepatic artery forms a triangle with the descending aorta and the ductus venosus.
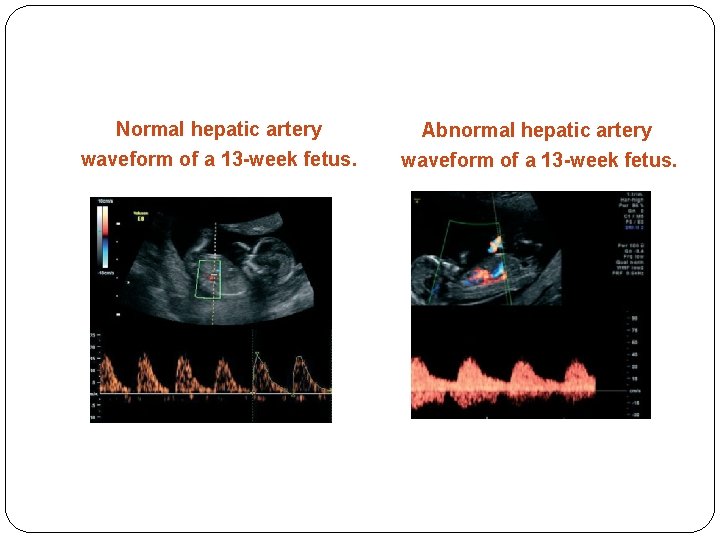
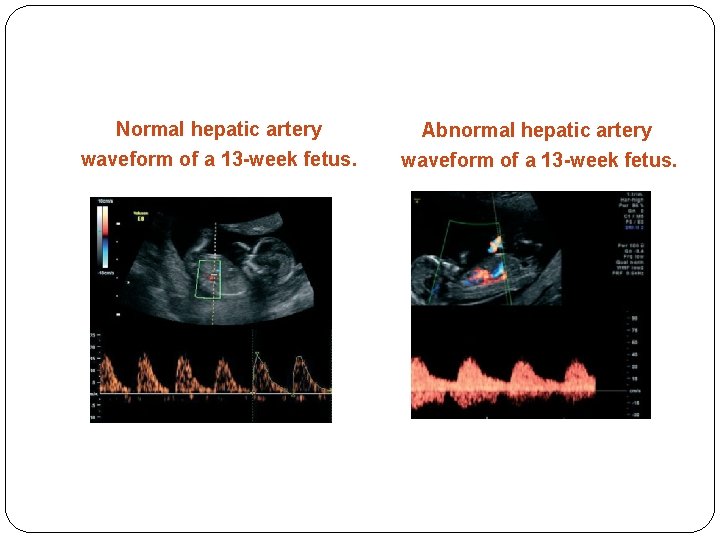
Normal hepatic artery waveform of a 13 -week fetus. Abnormal hepatic artery waveform of a 13 -week fetus.
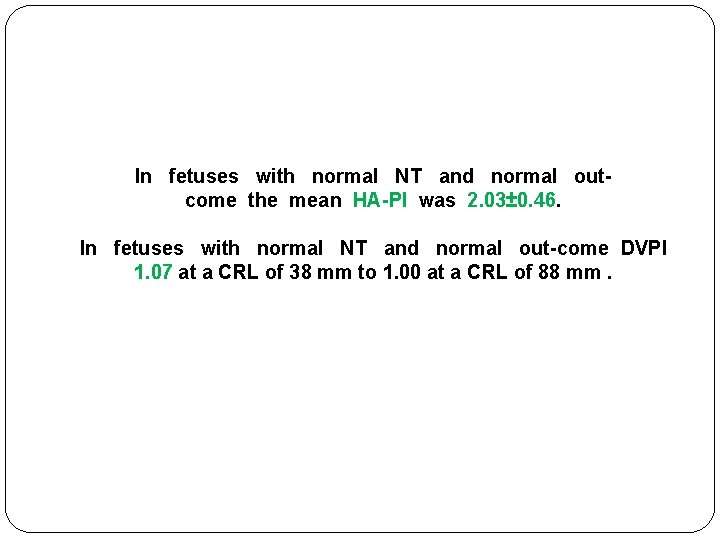
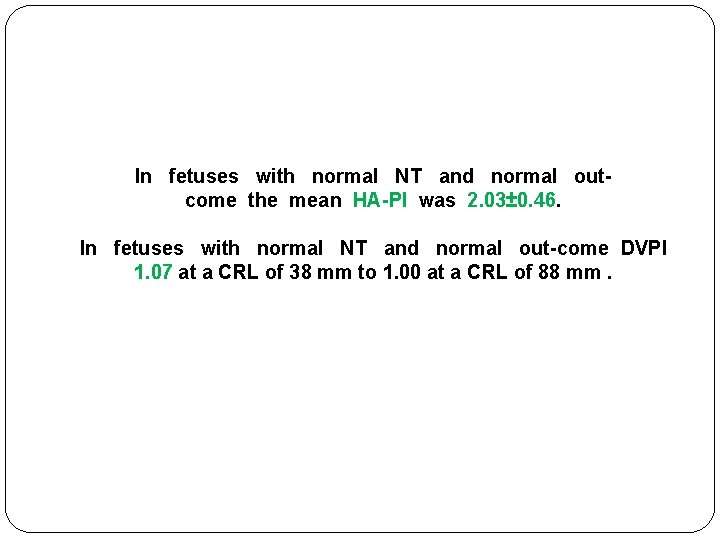
In fetuses with normal NT and normal outcome the mean HA-PI was 2. 03± 0. 46. In fetuses with normal NT and normal out-come DVPI 1. 07 at a CRL of 38 mm to 1. 00 at a CRL of 88 mm.
IT(Intracerebral Translucency )
IT…. open NTD �One of the major failings of the first trimester fetal ultrasound examination had been the inability to consistently diagnose open neural tube defects other than the exencephaly/ anencephaly sequence �A recently described intracranial marker [intracerebral translucency (IT)] may overcome this deficiency. � The fetal image required to evaluate the IT is identical to those needed for the NT, NB and FMF angle evaluation

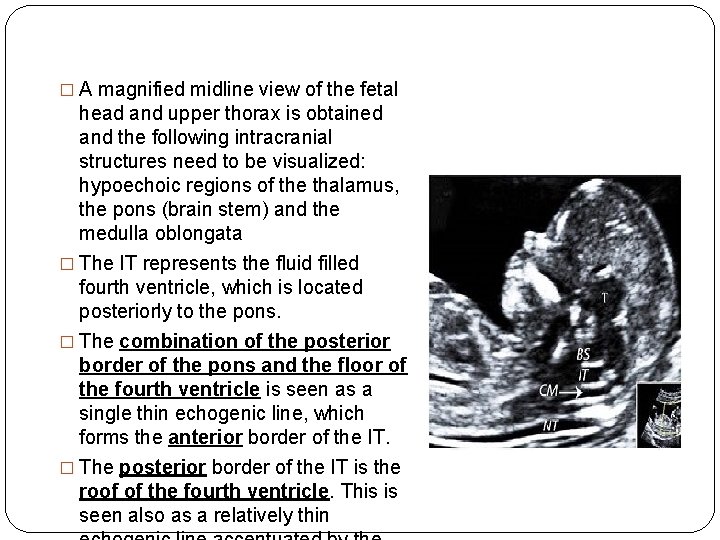
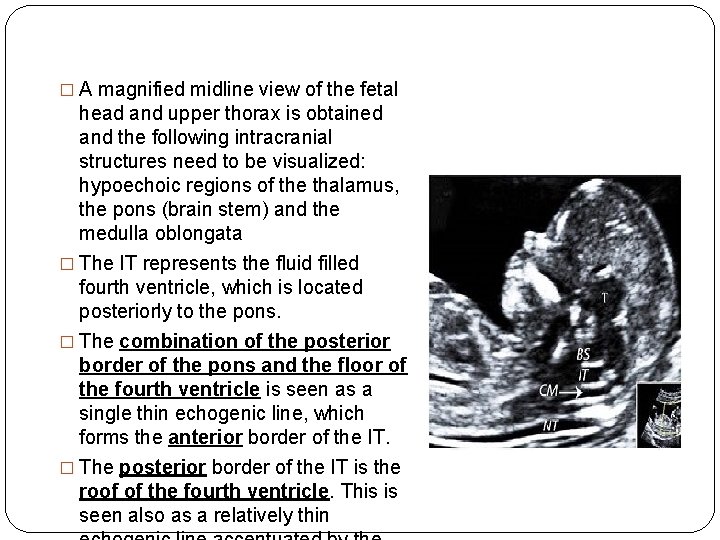
� A magnified midline view of the fetal head and upper thorax is obtained and the following intracranial structures need to be visualized: hypoechoic regions of the thalamus, the pons (brain stem) and the medulla oblongata � The IT represents the fluid filled fourth ventricle, which is located posteriorly to the pons. � The combination of the posterior border of the pons and the floor of the fourth ventricle is seen as a single thin echogenic line, which forms the anterior border of the IT. � The posterior border of the IT is the roof of the fourth ventricle. This is seen also as a relatively thin
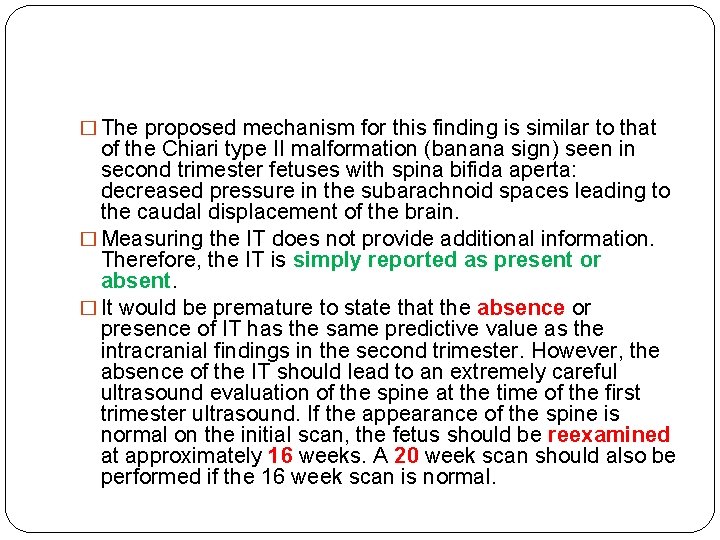
� The proposed mechanism for this finding is similar to that of the Chiari type II malformation (banana sign) seen in second trimester fetuses with spina bifida aperta: decreased pressure in the subarachnoid spaces leading to the caudal displacement of the brain. � Measuring the IT does not provide additional information. Therefore, the IT is simply reported as present or absent. � It would be premature to state that the absence or presence of IT has the same predictive value as the intracranial findings in the second trimester. However, the absence of the IT should lead to an extremely careful ultrasound evaluation of the spine at the time of the first trimester ultrasound. If the appearance of the spine is normal on the initial scan, the fetus should be reexamined at approximately 16 weeks. A 20 week scan should also be performed if the 16 week scan is normal.
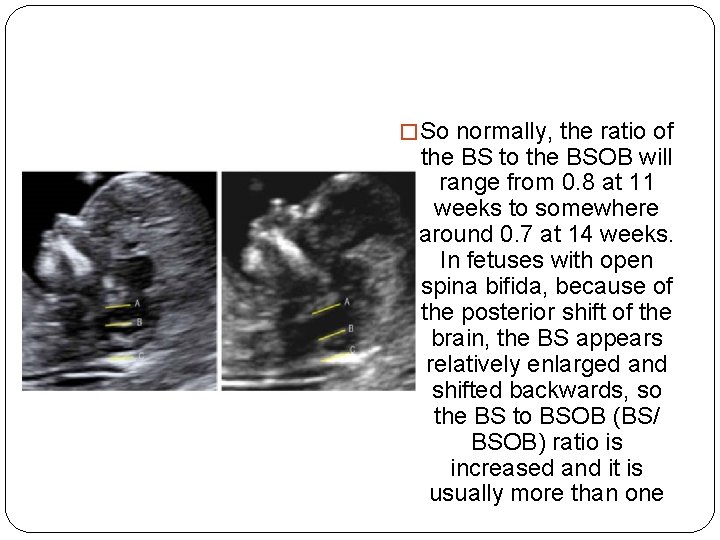
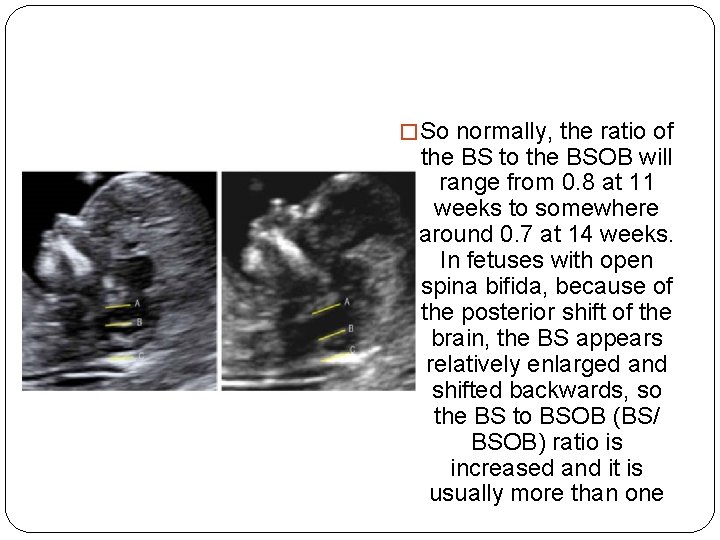
� So normally, the ratio of the BS to the BSOB will range from 0. 8 at 11 weeks to somewhere around 0. 7 at 14 weeks. In fetuses with open spina bifida, because of the posterior shift of the brain, the BS appears relatively enlarged and shifted backwards, so the BS to BSOB (BS/ BSOB) ratio is increased and it is usually more than one

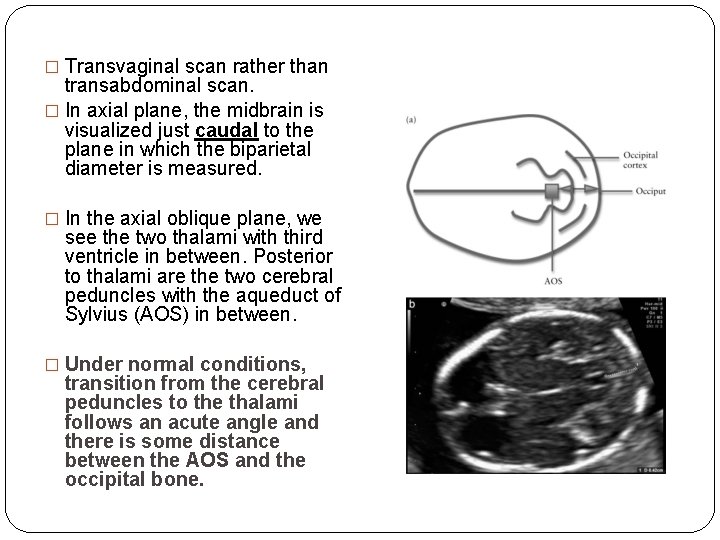
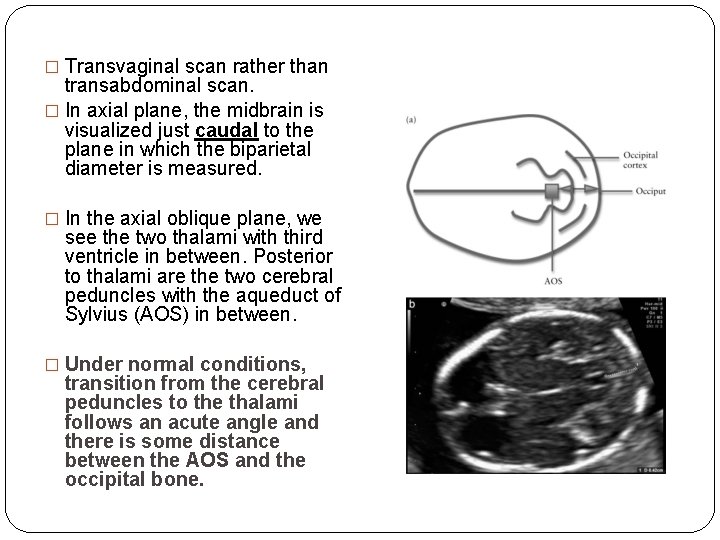
� Transvaginal scan rather than transabdominal scan. � In axial plane, the midbrain is visualized just caudal to the plane in which the biparietal diameter is measured. � In the axial oblique plane, we see the two thalami with third ventricle in between. Posterior to thalami are the two cerebral peduncles with the aqueduct of Sylvius (AOS) in between. � Under normal conditions, transition from the cerebral peduncles to the thalami follows an acute angle and there is some distance between the AOS and the occipital bone.
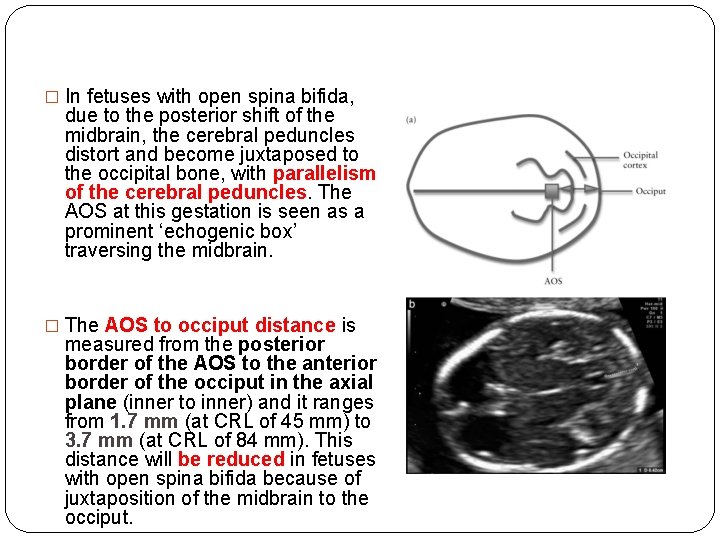
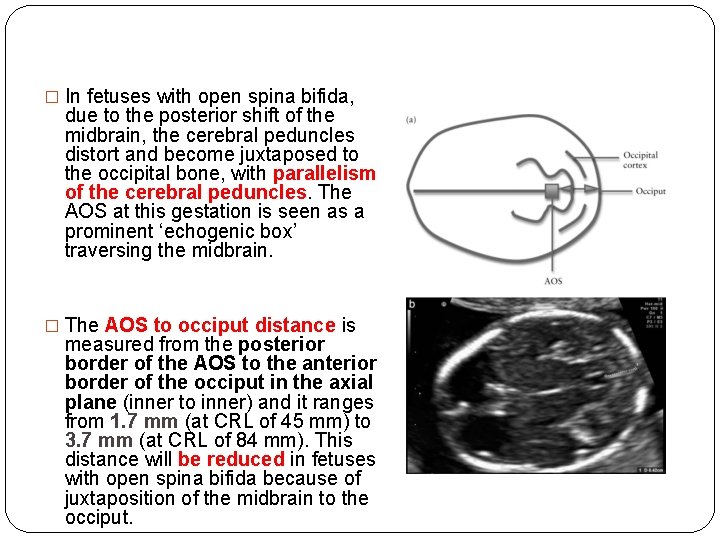
� In fetuses with open spina bifida, due to the posterior shift of the midbrain, the cerebral peduncles distort and become juxtaposed to the occipital bone, with parallelism of the cerebral peduncles. The AOS at this gestation is seen as a prominent ‘echogenic box’ traversing the midbrain. � The AOS to occiput distance is measured from the posterior border of the AOS to the anterior border of the occiput in the axial plane (inner to inner) and it ranges from 1. 7 mm (at CRL of 45 mm) to 3. 7 mm (at CRL of 84 mm). This distance will be reduced in fetuses with open spina bifida because of juxtaposition of the midbrain to the occiput.

Preeclampsia
Preeclampsia �Preeclampsia, which affects about 2% of pregnancies, is a major cause of perinatal and maternal morbidity and mortality �The likelihood of developing preeclampsia is increased by a number of factors in the maternal history, including Afro-Caribbean race, nulliparity, high body mass index and personal or family history of preeclampsia. However, screening by maternal history may detect only about 30% of those that will develop preeclampsia for a false positive rate of 5%.
�measurement of the uterine artery pulsatility index (PI) at 11 -13 weeks' gestation in combination with maternal history(inc) mean arterial pressure(inc) serum PAPP-A(dec…>inc) placental growth factor (PLGF) (dec…>inc) �The factors in the maternal history that appear to make a significant independent contribution to the preeclampsia risk assessment included maternal BMI, age, ethnicity, smoking, and parity.
� early rather than late preeclampsia is associated with an increased risk of perinatal mortality and morbidity and both short-term and long-term maternal complications. � Combination of the above mentioned risk factors was shown to predict 90% of early preeclampsia, 35% of late preeclampsia, and 20% of gestational hypertension. � This compares favorably with screening based on maternal history alone where only 30% of early and 20% of late preeclampsia are predicted for a 5% false positive rate.

�Sagittal section of the uterus must be obtained and the cervical canal and internal cervical os identified. Subsequently, the transducer must be gently tilted from side to side and then colour flow mapping should be used to identify each uterine artery along the side of the cervix and uterus at the level of the internal os. �Pulsed wave Doppler should be used with the sampling gate set at 2 mm to cover the whole vessel and ensuring that the angle of insonation is less than 30º. When three similar consecutive waveforms are obtained the PI must be measured and the mean PI of the left and right arteries be calculated
confirm that the vessel being � 1 -the direction of the blood flow should be towards the transducer when the transabdominal approach is used. This assures that the cervical branches are not being insonated. � 2 -the peak velocity of the insonated vessel should be 60 cm/sec or greater. This assures that the main uterine artery is being insonated rather one of its branches.
Gender Determination
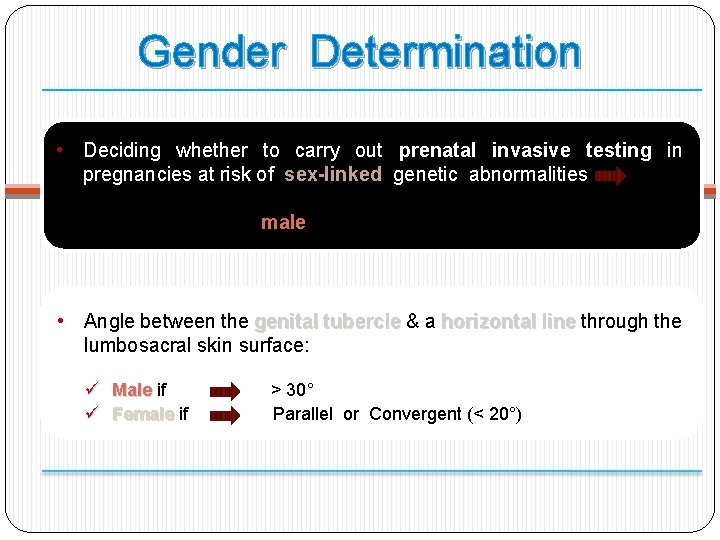
Gender Determination • Deciding whether to carry out prenatal invasive testing in pregnancies at risk of sex-linked genetic abnormalities Just necessary in male fetuses • Angle between the genital tubercle & a horizontal line through the lumbosacral skin surface: ü ü Male if Female if > 30° Parallel or Convergent (< 20°)
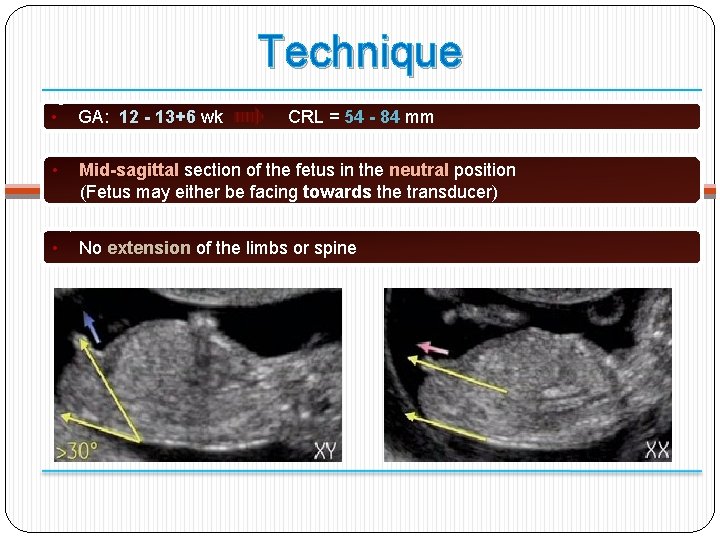
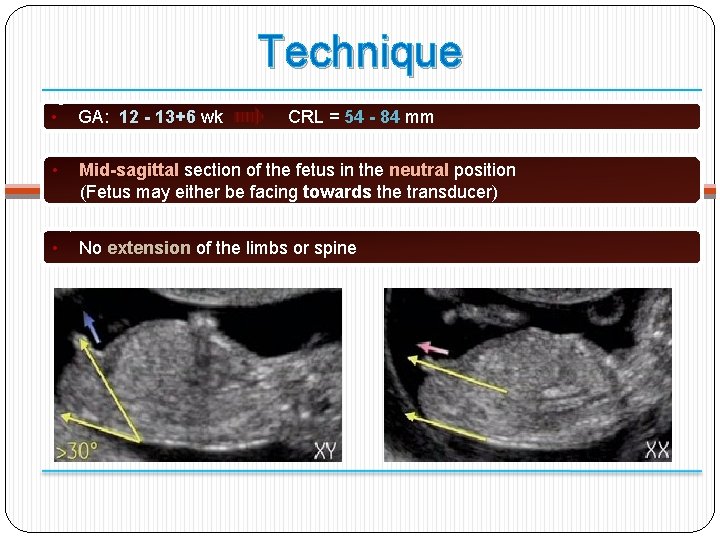
Technique • GA: 12 - 13+6 wk • Mid-sagittal section of the fetus in the neutral position (Fetus may either be facing towards the transducer) • No extension of the limbs or spine CRL = 54 - 84 mm

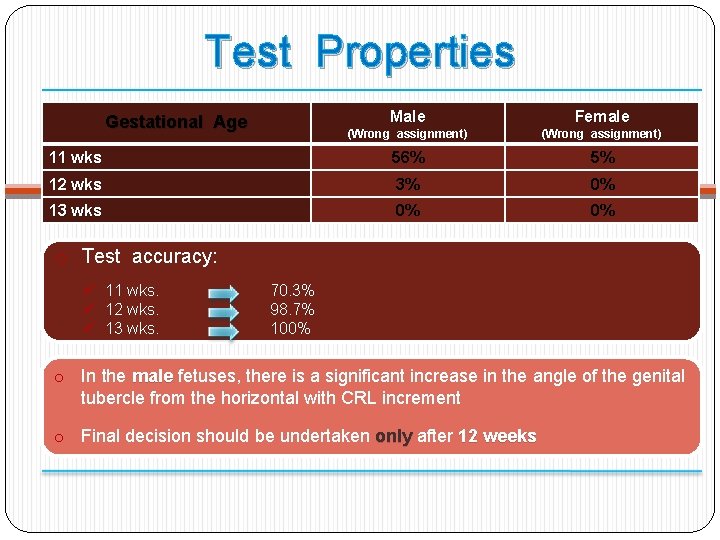
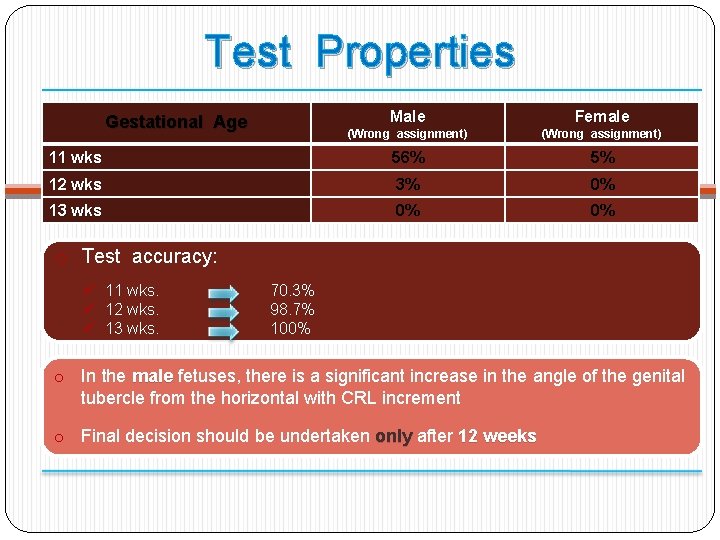
Test Properties Male Female (Wrong assignment) 11 wks 56% 5% 12 wks 3% 0% 13 wks 0% 0% Gestational Age o Test accuracy: ü 11 wks. ü 12 wks. ü 13 wks. 70. 3% 98. 7% 100% o In the male fetuses, there is a significant increase in the angle of the genital tubercle from the horizontal with CRL increment o Final decision should be undertaken only after 12 weeks
Thank you